Abstract
Throughout the world, approximately 800,000 people die by suicide every year, accounting for 1.5% of all deaths.1 Suicide is the 10th leading cause of death in North America and the foremost cause of death worldwide among persons 15 to 24 years of age.
Epidemiology
The World Health Organization (WHO) estimated that the 2016 suicide rate was 10.6 suicides per 100,000 persons, with 80% of suicides occurring in low- and middle-income countries.2 Across the six WHO regions, the incidence of suicide differed by a factor of 4 between the region with the highest rate (Europe) and the region with the lowest rate (the Eastern Mediterranean, including the Middle East). Explanations for this variation include differences in the classification of suicide, sociocultural attitudes toward suicide, access to lethal means of dying by suicide, and the adequacy of treatment for mental disorders. Worldwide, suicide rates vary according to age and sex, with the highest rates among older people and with higher rates among men (15.6 suicides per 100,000) than among women (7.0 per 100,000).2 Suicide rates have been declining over recent decades in most of these regions, with an estimated 18% reduction from 2000 to 2016. The exception is the Americas; in theUnited States, rates have increased by 1.5% annually since 2000,3 and rates among men 45 to64 years of age increased from 21 suicides per 100,000 in 1999 to 30 per 100,000 in 2017.4
Ecologic studies, which can explain time trends within countries, suggest a contribution of restrictive alcohol policies in lowering suicide rates.5 Changes in suicide rates have also been attributed to restriction of common means of suicide, such as detoxification of domestic gas (i.e., the reduction and eventual elimination of the carbon monoxide content of gas owing to a switch to natural gas) in the United Kingdom, starting in the 1960s,6 decreased availability of alcoholic spirits in Russia,7 and state restrictions of firearms in the United States.8
As extrapolated from household surveys, for each suicide death, there are 20 suicide attempts (defined as self-injurious behavior associated with an intent to die), amounting annually to 16 million attempts and approximately 160 million persons who express suicidal thoughts.9 The epidemiology of self-harm, defined as any type of self-injurious behavior, including suicide attempts and nonsuicidal self-injury, is different from the epidemiology of suicide, with the highest rates of self-harm among women and young people. Among persons who attempt suicide, 1.6% die by suicide within the next 12 months, and 3.9% die by suicide within the next 5 years.10
Risk Factors
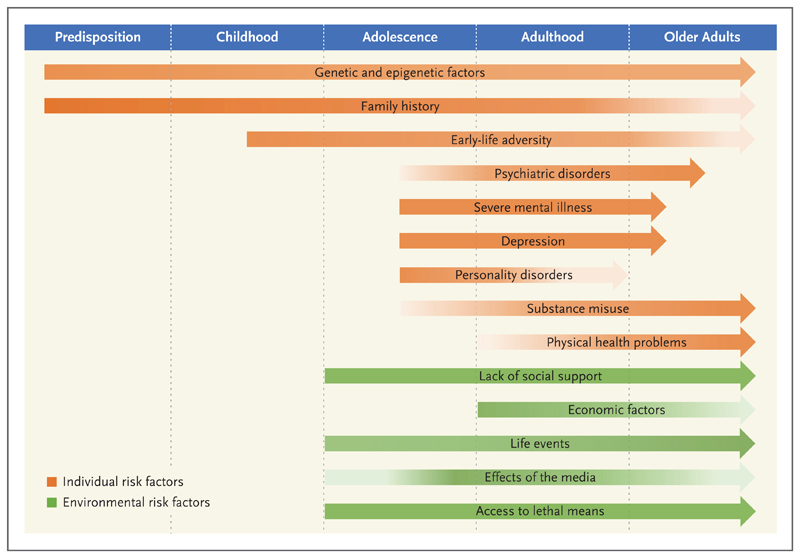
Risk factors for suicide have been investigated at the population and individual levels; in addition, predisposing factors and precipitating events have been examined, mainly at the individual level. Each of these factors can be mediated through genetic, psychological, and personality characteristics, making most explanatory models complex and difficult to interpret. One approach to understanding suicide has been life-course analysis,11 which is based on the premise that risk factors come into play at different stages of life (Fig. 1) and that suicide is the cumulative result of risk factors over a lifetime.
Figure 1. Risk Factors for Suicide and the Strength of the Association throughout Life.
The strength of the association between each risk factor and suicide is indicated by the shading (darker shading indicates a stronger association).
Individual factors, particularly psychiatric disorders,12 have the strongest effect on suicide rates in life-course models. Depression, bipolar disorder, schizophrenia-spectrum disorders, substance use disorders, epilepsy,13 and traumatic brain injury14 each increases the odds of completed suicide by a factor of more than 3. Other predisposing factors include a previous suicide attempt, childhood sexual abuse, a family history of suicidal behavior, and loss of a parent to suicide in early childhood (Table 1). Causality is inferred by the consistent, strong, and temporal associations of these risk factors with suicide, but randomized, controlled trials of treatment aimed at modifiable risk factors have been underpowered to examine their effect on suicide. Information collected on persons who have died by suicide (“psychological autopsy”) indicates that mood disorders and substance use disorders are the major risks.23 In high-income countries, mental illnesses are estimated to be present in half of persons who have died by suicide, with affective disorders (depression and bipolar disorder) involved in a third to half of suicides.24 Suicide also occurs in the absence of an identifiable psychiatric disorder, and even when present, psychiatric disorders have co-occurred with other predisposing and precipitating risk factors in persons who have died by suicide.
Table 1. Risk Factors for Suicide.
| Risk Factor | Strength of Association with Suicide | Quality of Evidence* |
|---|---|---|
| Precipitating factors | ||
| Drug and alcohol misuse12 | Strong | High |
| Access to lethal means15 | Moderate | High |
| Life events16 | Moderate | High |
| New diagnosis of terminal or chronic | Moderate | Moderate |
| physical illness17 | ||
| Media effects18 | Weak | Moderate |
| Predisposing factors | ||
| Neuropsychiatric disorders12 | Strong | High |
| Family history of suicidal behavior19 | Strong | High |
| Previous suicide attempt20 | Moderate | High |
| Adverse childhood experiences21 | Moderate | Moderate |
| Socioeconomic deprivation22 | Weak | Low |
Low quality indicates reported associations alone, moderate quality indicates reported associations that have been replicated in different settings, and high quality indicates associations that are supported by evidence from quasi-experimental studies or clinical trials.
Predisposing factors for suicide are thought to interact with precipitating factors, and predisposing factors may have different effects depending on the resilience of the person. Predisposing and precipitating factors together are considered to result in psychological changes, including feeling alone, hopeless, and burdensome, which lead in turn to social isolation. These psychological changes, combined with access to lethal means, can allow for suicidal acts.25
Among precipitating factors, stressful life events precede many suicides and suicide attempts (Table 1). Such events include relationship difficulties (particularly separation or divorce), death of a partner, and death by suicide of someone close16 — in particular, for mothers, death by suicide of adult children.26 Other precipitating factors include receiving a diagnosis of a chronic medical condition, particularly in the first week after a diagnosis of cancer.17 Suicide risk is also increased among assault victims, persons who have been arrested, and prisoners.27
On a population level, natural disasters can act as triggers for suicide, putatively in a dose–response manner in some instances. Paradoxically, terrorist attacks appear to be temporally protective against suicide in exposed populations. Greater social cohesion may have explained lower suicide rates in the New York metropolitan area in the months after the September 11, 2001, attacks.28 There is a small increase in suicide rates after the suicide of a celebrity, and the effect is magnified when press guidelines for avoiding both explicit descriptions of the death and speculation about causes are disregarded.18 The evidence for media influences on adolescents is weaker than the evidence for media influences on adults.
Social factors, particularly economic adversity, modify the influence of many risk factors for suicide.22 People in unskilled professions have an increased risk of suicide, which is partly explained by greater psychosocial stress; however, people in professions with access to lethal means for suicide have high rates, such as farmers, nurses, veterinarians, physicians, and police.29 Religious affiliation of any type has been reported to be protective against suicide, but this has not been shown for minority religious groups, which may be socially isolated.30
Psychological Models of Suicide
A stress-diathesis psychological model explains suicide risk as a combination of stressors in vulnerable persons. Individual vulnerability is considered to express itself in suicidal ideation under stress and is magnified by impulsivity and aggression, which increase the likelihood of acting on suicidal ideas.31 This model has been augmented by an interpersonal psychological model, in which the sense of burdening others and not being accepted in social groups interacts with the feeling of hopelessness that these perceptions will not change. Another aspect of psychological models is the premise that suicidal persons have a reduced fear of death and increased pain tolerance as a result of habituation by previous acts of self-harm.25
Impulsivity is a component of most psychological models of suicide. This trait is partly familial32 and has a disproportionate influence on suicide risk among young people.33 Perfectionism may be another contributory personality trait, leading to isolation out of fear of being stigmatized for an interpersonal crisis. A perfectionist trait also impedes psychological recovery from self-harm or suicidal ideation.34 Rigidity, inflexibility, and rumination impair problemsolving with respect to common stressors, including trying to find solutions to financial problems, unemployment, criminal justice involvement, interpersonal conflicts, and family strife.35
Familial, Genetic, and Other Biologic Factors
A family history of suicide is a risk factor for suicide,19 with some evidence suggesting that a mother's suicidal behavior has a greater influence than a father's suicidal behavior.36 Furthermore,the effect of parental suicide is greater on younger children than on adolescents; that is, the younger children are when they experience suicidal behavior in their parents, the higher their lifetime risk of suicide.37 This familial risk is partially explained by parental mood disorder, traits of impulsivity and aggressiveness, or neurocognitive disorders, all of which are heritable.38 However, studies have not been able to differentiate between behavioral imitation of a family member's suicide and a genetic propensity for suicide as explanatory factors. Twin studies have yielded estimates of the genetic contribution to the risk of suicidal behavior that range from 30 to 50%.39 Despite the apparent heritability of suicidal behavior, risk genes have not been identified.39 Some unreplicated studies have suggested that genetic promoters of inflammation overlap suicide risk and that suicide risk is mediated by immunologic responses to acute infection, but these observations are speculative.
Imaging and postmortem studies have shown changes in serotonergic pathways that are correlated with suicide, but these associations have not been validated. One hypothesis is that changes in the medial prefrontal cortex lead to an overvaluing of social signs of rejection, deficits in emotional responses, and poor decision making.40 One study showed that persons who experienced adversity in early life have an overactive hypothalamic–pituitary–adrenal axis in response to stress, which increases anxiety and acts as a mediator of suicidal behavior.41
Assessment of Suicide Risk
Models for predicting suicide risk have been used to improve clinical decision making, assist in the identification of high-risk groups,42 and translate evidence-based risk factors into improved risk assessment. These models can provide transparency and consistency in decision making about suicide risk. However, models used in clinical practice vary in content and in the degree of validation and often have been developed for other purposes, such as assessing patients for depression or rating the severity of current suicidal ideation rather than predicting the future risk of suicide (Table 2). Risk models for suicide have been used in emergency departments to assess persons who have harmed themselves, but these models have a poor balance between sensitivity and specificity and do not provide probability scores.48 Thus, these assessment tools may increase the clinical workload by requiring psychiatric assessment or hospitalization in cases of false positive risks of suicide. In the case of some of these tools, most of the patients who ultimately died by suicide were predicted to be at low risk. Nevertheless, structured tools can provide a baseline assessment during initial contact with health care providers, offer a checklist to identify risk factors, and lead to interventions for those persons who are predicted to be at high risk for suicide.49,50 An advantage of empirically derived prediction models over subjective clinical judgment is that they attempt to incorporate the relative strength of risk factors and their interactions. The alternative to these instruments is unstructured clinical approaches, in which clinical impressions are derived about suicide risk. Some studies have shown that these unstructured approaches may be more inaccurate and subject to a range of cognitive biases on the part of the assessor, including an overemphasis on predisposing factors51 and risk aversion.52
Table 2. Tools for Assessing Suicide Risk.
| Tool* | Intended Population | Outcome When Originally Developed | Scale or Prediction Tool | Selection of Variables and Weighting | No. of Items | No. of Suicides in External Validation |
|---|---|---|---|---|---|---|
| Beck Hopelessness Scale43 | General population (17–70 yr) | Hopelessness symptoms | Rating scale | Not tested, unweighted | 20 | 62 |
| Beck Depression Inventory43 | General population (≥13 yr) | Depressive symptoms | Rating scale | Not tested, unweighted | 21 | 76 |
| Scale for Suicide Ideation43 | General population | Suicidal ideation | Rating scale | Not tested, unweighted | 20 | 30 |
| Patient Health Questionnaire (PHQ-9)43 | Primary care | Depressive symptoms | Rating scale | Not tested, unweighted | 9 | 46 |
| Beck's Suicide Intent Scale43 | Self-harm | Suicidal ideation | Rating scale | Not tested, unweighted | 20 | 76 |
| ReACT Self-Harm Rule43 | Self-harm | Repeated self-harm and suicide | Prediction tool | Multivariable model, unweighted | 4 | 92 |
| Columbia Suicide Severity Rating Scale (C-SSRS)44 | General population, at risk groups | Suicidal intent and behavior | Prediction tool | Decision tree, unweighted | 5 | 10 |
| Army STARRS suicide prediction tool45 | U.S. military, after psychiatric hospitalization | Suicide | Prediction tool | Multivariable model, weighted | 14 | Not available |
| Army STARRS suicide prediction tool46 | U.S. military, after outpatient psychiatric visit | Suicide | Prediction tool | Multivariable model, weighted | 61 | Not available |
| OxMIS tool47 | Severe mental illness | Suicide | Prediction tool | Multivariable model, weighted | 17 | 139 |
OxMIS denotes Oxford Mental Illness and Suicide, and STARRS Study to Assess Risk and Resilience in Servicemembers.
The U.S. National Strategy for Suicide Prevention recommends the use of suicide prediction tools,53 and the European Psychiatric Association endorses using these tools as adjuncts to an individual psychiatric assessment.54 Despite the putative advantages of such tools, current evidence to support their routine use in emergency departments and in primary care is weak.49 The shortcomings of current evidence are reflected in suggestions that new risk-assessment models should be developed for specific populations, should not be evaluated on the basis of one performance metric (e.g., positive predictive value), should be considered as adjuncts to clinical decision making instead of being applied independently, and should have a high negative predictive value (to screen out low-risk persons and thus preserve resources).47 Although machine-learning approaches based on large data sets may provide information on the causes of suicide, their role in suicide risk assessment is not known.
Interventions to Reduce Suicide Risk
Population-Based Measures
Suicide prevention strategies can be used at the population level or can be targeted at high-risk groups or individuals. Population measures include restricting access to the means of suicide, particularly if certain methods are lethal and frequently used in a particular population. Worldwide, hanging accounts for approximately 40% of deaths by suicide, and pesticides account for 14 to 20%.55 Pesticide restrictions have been evaluated in 16 countries, and bans of the sale of highly hazardous pesticides were associated with reductions in suicides in Sri Lanka, Bangladesh, and South Korea.55 However, a trial of safe household storage of pesticides in Sri Lanka did not reduce suicides in a randomized trial with a cluster design.56 Other common methods of sui-cide are jumping from heights and medication overdoses. Erection of barriers at potential suicide spots, such as bridges, tall buildings, and railway tracks, and smaller pack sizes of certain nonprescription medications that are used for suicide, such as acetaminophen and preparations with dextropropoxyphene, have led to reductions in suicide deaths by these means.
Data on the association between firearm possession and suicide differ according to country and culture. In the United States, there were 14,542 homicides and 23,854 suicides involving firearms in 2017.4 Analyses of individual-level data,15 area-level data in large cities,57 and state-level data58 have shown associations between firearm ownership and suicide, and gun restrictions have been associated with lower overall suicide rates as well as lower rates of suicide with firearms.8 The latter observation has been confirmed in trends in four states that implemented restrictive changes in firearm legislation during the 2009–2013 period.59
Population approaches to suicide prevention have focused mostly on institutionalized or incarcerated populations. These approaches include removing ligature points that present opportunities for hanging in psychiatric hospitals and prisons. The introduction of early intervention services for psychosis reduced suicides in Hong Kong.60 Several studies have not confirmed the effectiveness of broad, school-based suicide prevention programs, and the justification for such initiatives has been questioned.61 However, a pan-European study that involved raising awareness of mental health and suicide risk among students showed a reduction in suicide attempts.62 Future innovations may include safety-planning apps that assist in identifying and removing lethal means of suicide, obtaining peer support, and accessing crisis support services. In the United States, Britain, and other high-income countries, national suicide prevention strategies have highlighted groups at high risk for suicide that should receive targeted interventions (Table 3 and the Supplementary Appendix, available with the full text of this article at NEJM.org).
Table 3. Suicide Risk and Interventions in Specific Subgroups.* .
| Subgroup | Suicide Rate no./100,000 |
Risk Factors | Interventions (Outcome to Be Prevented) |
|---|---|---|---|
| Children, adolescents, and young adults (age 10–24 yr) | 10 | Negative life events, mental disorders, substance misuse, access to lethal means | Psychological treatment — psychotherapy based on understanding one's mental state (self-harm in girls) |
| Older adults (age ≥70 yr) | 43 | Functional disability, social isolation, malignant diseases, chronic diseases | Telephone counseling (suicide); multifaceted program of psychoeducation, depression screening, group therapy, and clear referral pathways (suicide among rural women); integration of mental health into primary health care (self-harm) |
| Discharged psychiatric patients (first 90 days after discharge) | 178 | Recent self-harm, severe mental illness, first psychotic episode | Pharmacologic treatment for underlying disorders; psychological treatment — cognitive behavioral therapy, problem-solving therapy, or both (suicide) |
| Prisoners | 23 | Housing in single-occupancy cell, remanded status, life sentence, violent-offense conviction, psychiatric disorders, alcohol use disorders | Removal of ligature points (suicide) |
| Military and veteran populations | 20 | Early separation from service, recent deployment, lower rank, younger age, clinical depression, multiple disorders | Safety planning intervention, which involves prioritizing coping strategies and telephone contact to monitor risk (self-harm) |
| Nonheterosexuals | Same as rate for general population | Same as risk factors for general population | Addressing suicidal risks openly with clinicians and addressing internalized stigma (self-harm) |
| People who have harmed themselves | 439 (1-yr rate) | Past self-harm, physical health problems, male sex, suicidal intent, violent selfharm (use of firearms, hanging, or cutting), age of 45–64 yr (vs. younger age) | Psychological treatment — cognitive behavioral therapy, problem-solving therapy, or both (self-harm) |
Suicide rates refer to those in the United States, but the interventions are applicable to subgroups in all high-income (and possibly middle-income) countries. More detailed descriptions and references are provided in the Supplementary Appendix, available with the full text of this article at NEJM.org.
Pharmacologic Treatments
Most of the evidence in support of pharmacologic treatment to prevent suicide in populations with mental illness comes from observational studies. The few randomized trials of such treatment have been underpowered to study suicide and have relied on proxy outcomes (e.g., suicidal ideas or depressive symptoms). Trials of antipsychotic medications as compared with placebo in patients with schizophrenia have shown reductions in suicide rates, but these results have been uncertain because of the small numbers of suicides.63 In contrast, trials of lithium in patients with bipolar disorder or depression have been associated with more convincing reductions in suicide.64 Most randomized trials of psychopharmacologic intervention have excluded patients with a history of suicidal ideation or behavior and those who are actively suicidal, limiting the generalizability of the findings. Specific pharmacoepidemiologic approaches, called “within-individual designs,” that account for factors that remain stable in an individual patient (e.g., background genetic risk and environmental adversities) have shown a 14% decrease in the incidence of suicidal acts and completed suicide among people treated with lithium for bipolar disorder65 and a 19% reduction among young people with attention deficit-hyperactivity disorder and high rates of coexisting psychiatric disorders who were treated with psychostimulants.66 Medications for opiate use disorders (methadone and buprenorphine) have been associated with reduced rates of completed suicide among persons with addictions.67 Treatments being investigated for suicide prevention in patients with depression include the anesthetic ketamine, electroconvulsive therapy, and repetitive transcranial magnetic stimulation, but these approaches have not been sufficiently studied.
Psychological Treatments
Studies of psychological treatments for suicide prevention have mainly addressed how suicidal ideas and thoughts develop and their conversion into plans for self-harm; alternatively, they have focused on mental states associated with suicide, such as depressive and anxiety symptoms. A meta-analysis that included various psychological treatments showed that at the end of the treatment period, interventions that directly addressed suicidal thoughts and behaviors and provided strategies for coping with them had better outcomes than treatment for anxiety and depression, but these differences were diminished after 1 year.68 Trials of cognitive behavioral therapy have shown a reduction in suicidal thoughts,69 presumed to be mediated by reducing hopelessness. Mindfulness-based cognitive therapy, which combines cognitive behavioral techniques with meditation and deep breathing, has improved mood stability and problem solving in suicidal persons.70 Dialectical behavioral therapy, a form of cognitive therapy involving both individual and group-based treatment that focuses on keeping people in therapy and helping them learn to manage emotions and learn mindfulness skills, has reduced self-harm in 12 trials but with small effect sizes.71 A study of family therapy as compared with usual treatment for adolescents who had harmed themselves showed no reduction in suicides with family therapy.72 Another study showed that Internet-administered self-help treatments may offer approaches for hard-to-reach groups, such as persons who have had negative health care experiences or persons with financial or time constraints that impede access to care,73 but these findings were not replicated in a similar trial.74
Integrating Assessment and Treatment
It is advantageous to consider the following five points in assessing and managing the risk of suicide. First, a person who presents with suicidal thoughts may be at risk for suicide even if there are few overt symptoms of a psychiatric disorder. Second, suicide risk should be assessed by considering predisposing and precipitating factors, including recent life events. Third, the risk of suicide should be managed through regular follow-up and brief psychological therapy; for persons with symptoms of mental illness, pharmacologic treatment should also be considered. Fourth, the suicidal person, family members, and those who provide care should all take part in ensuring a safe environment, with removal of the means of suicide such as guns. Finally, if the risk of suicide is considered to be high or uncertain, the person should be referred immediately to mental health services, and the use of risk-assessment tools should be considered to aid risk stratification and communication among services. Mental health professionals have emphasized that developing and maintaining a therapeutic relationship is central to reducing suicide risk.75
The following steps can be taken in evaluating someone who has inflicted self-harm: inquire nonjudgmentally about the incident to establish the intent of the self-harm; determine how ideation was acted on; assess the risk of repetition, using structured approaches that can be supplemented with risk-assessment tools; identify psychological, social, and psychiatric needs; and establish an individual treatment plan that incorporates safety planning and restriction of lethal methods.
Management of suicidality calls for a comprehensive approach to assessment and treatment. Assessment should focus on past suicidal behavior, openly addressing ongoing suicidal ideas and psychosocial needs. Assessment of the risk of self-harm and completed suicide may increasingly draw on new technologies such as clinical decision-making tools and safety planning to establish evidence-based practices.
Supplementary Material
Acknowledgments
We thank Matthias Burghart for technical and bibliographic assistance.
Footnotes
No potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
Contributor Information
Seena Fazel, Department of Psychiatry, Warneford Hospital, University of Oxford, Oxford, United Kingdom
Bo Runeson, The Department of Clinical Neuroscience, Karolinska Institutet, Stockholm
References
- 1.Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ 2019. 2016;364:l94. doi: 10.1136/bmj.l94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Age-standardized suicide rates (per 100 000 population), both sexes, 2016. World Health Organization; Geneva: 2018. https://www.who.int/gho/mental_health/suicide_rates/en/ [Google Scholar]
- 3.Stone DM, Simon TR, Fowler KA, et al. Vital signs: trends in state suicide rates — United States, 1999-2016 and circumstances contributing to suicide — 27 states, 2015. MMWR Morb Mortal Wkly. 2018;67:617–24. doi: 10.15585/mmwr.mm6722a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Multiple cause of death, 1999-2017. https://wonder.cdc.gov/mcd.htmlCDC Wonder Online Database. [Google Scholar]
- 5.Xuan Z, Naimi TS, Kaplan MS, et al. Alcohol policies and suicide: a review of the literature. Alcohol Clin Exp. 2016;40:2043–55. doi: 10.1111/acer.13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kreitman N. The coal gas story: United Kingdom suicide rates, 1960-71. Br J Prev Soc Med. 1976;30:86–93. doi: 10.1136/jech.30.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Razvodovsky YE. Beverage-specific alcohol sale and suicide in Russia. Crisis. 2009;30:186–91. doi: 10.1027/0227-5910.30.4.186. [DOI] [PubMed] [Google Scholar]
- 8.Kaufman EJ, Morrison CN, Branas CC, Wiebe DJ. State firearm laws and interstate firearm deaths from homicide and suicide in the United States: a crosssectional analysis of data by county. JAMA Intern Med. 2018;178:692–700. doi: 10.1001/jamainternmed.2018.0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization; Geneva: 2014. Preventing suicide: a global imperative. [Google Scholar]
- 10.Olfson M, Wall M, Wang S, Crystal S, Gerhard T, Blanco C. Suicide following deliberate self-harm. Am J Psychiatry. 2017;174:765–74. doi: 10.1176/appi.ajp.2017.16111288. [DOI] [PubMed] [Google Scholar]
- 11.Gunnell D, Lewis G. Studying suicide from the life course perspective: implications for prevention. Br J Psychiatry. 2005;187:206–8. doi: 10.1192/bjp.187.3.206. [DOI] [PubMed] [Google Scholar]
- 12.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13:153–60. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fazel S, Wolf A, Långström N, Newton CR, Långström P. Premature mortality in epilepsy and the role of psychiatric comorbidity: a total population study. Lancet. 2013;382:1646–54. doi: 10.1016/S0140-6736(13)60899-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fazel S, Wolf A, Pillas D, Lichtenstein P, Långström N. Suicide, fatal injuries, and other causes of premature mortality in patients with traumatic brain injury: a 41-year Swedish population study. JAMA Psychiatry. 2014;71:326–33. doi: 10.1001/jamapsychiatry.2013.3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anglemyer A, Horvath T, Rutherford G. The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis. Ann Intern Med. 2014;160:101–10. doi: 10.7326/M13-1301. [DOI] [PubMed] [Google Scholar]
- 16.Agerbo E. Midlife suicide risk, partner's psychiatric illness, spouse and child bereavement by suicide or other modes of death: a gender specific study. J Epidemiol Community Health. 2005;59:407–12. doi: 10.1136/jech.2004.024950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang F, Fall K, Mittleman MA, et al. Suicide and cardiovascular death after a cancer diagnosis. N Engl J Med. 2012;366:1310–8. doi: 10.1056/NEJMoa1110307. [DOI] [PubMed] [Google Scholar]
- 18.Niederkrotenthaler T, Fu KW, Yip PSF, et al. Changes in suicide rates following media reports on celebrity suicide: a meta-analysis. J Epidemiol Community Health. 2012;66:1037–42. doi: 10.1136/jech-2011-200707. [DOI] [PubMed] [Google Scholar]
- 19.Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. Lancet. 2002;360:1126–30. doi: 10.1016/S0140-6736(02)11197-4. [DOI] [PubMed] [Google Scholar]
- 20.Runeson B, Haglund A, Lichtenstein P, Tidemalm D. Suicide risk after nonfatal self-harm: a national cohort study, 2000-2008. J Clin Psychiatry. 2016;77:240–6. doi: 10.4088/JCP.14m09453. [DOI] [PubMed] [Google Scholar]
- 21.van Geel M, Vedder P, Tanilon J. Relationship between peer victimization, cyberbullying, and suicide in children and adolescents: a meta-analysis. JAMA Pediatr. 2014;168:435–42. doi: 10.1001/jamapediatrics.2013.4143. [DOI] [PubMed] [Google Scholar]
- 22.Rehkopf DH, Buka SL. The association between suicide and the socio-economic characteristics of geographical areas: a systematic review. Psychol Med. 2006;36:145–57. doi: 10.1017/S003329170500588X. [DOI] [PubMed] [Google Scholar]
- 23.Yoshimasu K, Kiyohara C, Miyashita K. Suicidal risk factors and completed suicide: meta-analyses based on psychological autopsy studies. Environ Health Prev Med. 2008;13:243–56. doi: 10.1007/s12199-008-0037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry. 2004;4:37. doi: 10.1186/1471-244X-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pitman A, Osborn D, King M, Erlangsen A. Effects of suicide bereavement on mental health and suicide risk. Lancet Psychiatry. 2014;1:86–94. doi: 10.1016/S2215-0366(14)70224-X. [DOI] [PubMed] [Google Scholar]
- 27.Fazel S, Ramesh T, Hawton K. Suicide in prisons: an international study of prevalence and contributory factors. Lancet Psychiatry. 2017;4:946–52. doi: 10.1016/S2215-0366(17)30430-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Claassen CA, Carmody T, Stewart SM, et al. Effect of 11 September 2001 terrorist attacks in the USA on suicide in areas surrounding the crash sites. Br J Psychiatry. 2010;196:359–64. doi: 10.1192/bjp.bp.109.071928. [DOI] [PubMed] [Google Scholar]
- 29.Milner A, Spittal MJ, Pirkis J, LaMontagne AD. Suicide by occupation: systematic review and meta-analysis. Br J Psychiatry. 2013;203:409–16. doi: 10.1192/bjp.bp.113.128405. [DOI] [PubMed] [Google Scholar]
- 30.Lawrence RE, Oquendo MA, Stanley B. Religion and suicide risk: a systematic review. Arch Suicide Res. 2016;20:1–21. doi: 10.1080/13811118.2015.1004494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–9. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 32.McGirr A, Alda M, Séguin M, Cabot S, Lesage A, Turecki G. Familial aggregation of suicide explained by cluster B traits: a three-group family study of suicide controlling for major depressive disorder. Am J Psychiatry. 2009;166:1124–34. doi: 10.1176/appi.ajp.2009.08111744. [DOI] [PubMed] [Google Scholar]
- 33.McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychol Med. 2008;38:407–17. doi: 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- 34.O'Connor RC. The relations between perfectionism and suicidality: a systematic review. Suicide Life Threat Behav. 2007;37:698–714. doi: 10.1521/suli.2007.37.6.698. [DOI] [PubMed] [Google Scholar]
- 35.Morrison R O'Connor RC. A systematic review of the relationship between rumination and suicidality. Suicide Life Threat Behav. 2008;38:523–38. doi: 10.1521/suli.2008.38.5.523. [DOI] [PubMed] [Google Scholar]
- 36.Kuramoto SJ, Stuart EA, Runeson B, Lichtenstein P, Långström N, Wilcox HC. Maternal or paternal suicide and off-spring's psychiatric and suicide-attempt hospitalization risk. Pediatrics. 2010;126(5):e1026–e1032. doi: 10.1542/peds.2010-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilcox HC, Kuramoto SJ, Lichtenstein P, Långström N, Brent DA, Runeson B. Psychiatric morbidity, violent crime, and suicide among children and adolescents exposed to parental death. J Am Acad Child Adolesc Psychiatry. 2010;49:514–23. doi: 10.1097/00004583-201005000-00012. [DOI] [PubMed] [Google Scholar]
- 38.Brent DA, Mann JJ. Familial pathways to suicidal behavior — understanding and preventing suicide among adolescents. N Engl J Med. 2006;355:2719–21. doi: 10.1056/NEJMp068195. [DOI] [PubMed] [Google Scholar]
- 39.Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387:1227–39. doi: 10.1016/S0140-6736(15)00234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Heeringen K, Mann JJ. The neuro-biology of suicide. Lancet Psychiatry. 2014;1:63–72. doi: 10.1016/S2215-0366(14)70220-2. [DOI] [PubMed] [Google Scholar]
- 41.Turecki G. The molecular bases of the suicidal brain. Nat Rev Neurosci. 2014;15:802–16. doi: 10.1038/nrn3839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Olfson M, Marcus SC, Bridge JA. Focusing suicide prevention on periods of high risk. JAMA. 2014;311:1107–8. doi: 10.1001/jama.2014.501. [DOI] [PubMed] [Google Scholar]
- 43.Runeson B, Odeberg J, Pettersson A, Edbom T, Jildevik Adamsson I, Waern M. Instruments for the assessment of suicide risk: A systematic review evaluating the certainty of the evidence. PLoS One. 2017;12(7):e0180292. doi: 10.1371/journal.pone.0180292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lindh Å U, Waern M, Beckman K, Renberg ES, Dahlin M, Runeson B. Short term risk of non-fatal and fatal suicidal behaviours: the predictive validity of the Columbia-Suicide Severity Rating Scale in a Swedish adult psychiatric population with a recent episode of self-harm. BMC Psychiatry. 2018;18:319. doi: 10.1186/s12888-018-1883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kessler RC, Warner CH, Ivany C, et al. Predicting suicides after psychiatric hospitalization in US Army soldiers: the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2015;72:49–57. doi: 10.1001/jamapsychiatry.2014.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kessler RC, Stein MB, Petukhova MV, et al. Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Mol Psychiatry. 2017;22:544–51. doi: 10.1038/mp.2016.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fazel S, Wolf A, Larsson H, Mallett S, Fanshawe TR. The prediction of suicide in severe mental illness: development and validation of a clinical prediction rule (OxMIS) Transl Psychiatry. 2019;9:98. doi: 10.1038/s41398-019-0428-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chan MK, Bhatti H, Meader N, et al. Predicting suicide following self-harm: systematic review of risk factors and risk scales. Br J Psychiatry. 2016;209:277–83. doi: 10.1192/bjp.bp.115.170050. [DOI] [PubMed] [Google Scholar]
- 49.Bolton JM, Gunnell D, Turecki G. Suicide risk assessment and intervention in people with mental illness. BMJ. 2015;351:h4978. doi: 10.1136/bmj.h4978. [DOI] [PubMed] [Google Scholar]
- 50.Fazel S, Wolf A. Suicide risk assessment tools do not perform worse than clinical judgement. Br J Psychiatry. 2017;211:183. doi: 10.1192/bjp.211.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pease JL, Forster JE, Davidson CL, Holliman BD, Genco E, Brenner LA. How Veterans Health Administration suicide prevention coordinators assess suicide risk. Clin Psychol Psychother. 2017;24:401–10. doi: 10.1002/cpp.2011. [DOI] [PubMed] [Google Scholar]
- 52.Berman NC, Stark A, Cooperman A, Wilhelm S, Cohen IG. Effect of patient and therapist factors on suicide risk assessment. Death Stud. 2015;39:433–41. doi: 10.1080/07481187.2014.958630. [DOI] [PubMed] [Google Scholar]
- 53.Washington: DC: Department of Health and Human Services; Sep, 2012. 2012 National Strategy for Suicide Prevention: goals and objectives for action: a report of the U.S. Surgeon General and of the National Action Alliance for Suicide Prevention. https://www.ncbi.nlm.nih.gov/books/n/surgnssp/pdf/ [PubMed] [Google Scholar]
- 54.Wasserman D, Rihmer Z, Rujescu D, et al. The European Psychiatric Association (EPA) guidance on suicide treatment and prevention. Eur Psychiatry. 2012;27:129–41. doi: 10.1016/j.eurpsy.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 55.Gunnell D, Knipe D, Chang S-S, et al. Prevention of suicide with regulations aimed at restricting access to highly hazardous pesticides: a systematic review of the international evidence. Lancet Glob Health. 2017;5(10):e1026–e1037. doi: 10.1016/S2214-109X(17)30299-1. [DOI] [PubMed] [Google Scholar]
- 56.Pearson M, Metcalfe C, Jayamanne S, et al. Effectiveness of household lockable pesticide storage to reduce pesticide selfpoisoningin rural Asia: a communitybased, cluster-randomised controlled trial. Lancet. 2017;390:1863–72. doi: 10.1016/S0140-6736(17)31961-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Miller M, Warren M, Hemenway D, Azrael D. Firearms and suicide in US cities. Inj Prev. 2015;21(e1):e116–e119. doi: 10.1136/injuryprev-2013-040969. [DOI] [PubMed] [Google Scholar]
- 58.Siegel M, Rothman EF. Firearm ownership and suicide rates among US men and women, 1981-2013. Am J Public Health. 2016;106:1316–22. doi: 10.2105/AJPH.2016.303182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Anestis MD, Anestis JC. Suicide rates and state laws regulating access and exposure to handguns. Am J Public Health. 2015;105:2049–58. doi: 10.2105/AJPH.2015.302753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chan SKW, Chan SWY, Pang HH, et al. Association of an early intervention service for psychosis with suicide rate among patients with first-episode schizophreniaspectrum disorders. JAMA Psychiatry. 2018;75:458–64. doi: 10.1001/jamapsychiatry.2018.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kutcher S, Wei Y, Behzadi P. School- and community-based youth suicide prevention interventions: hot idea, hot air, or sham? Can J Psychiatry. 2017;62:381–7. doi: 10.1177/0706743716659245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wasserman D, Hoven CW, Wasserman C, et al. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. Lancet. 2015;385:1536–44. doi: 10.1016/S0140-6736(14)61213-7. [DOI] [PubMed] [Google Scholar]
- 63.Leucht S, Tardy M, Komossa K, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012;379:2063–71. doi: 10.1016/S0140-6736(12)60239-6. [DOI] [PubMed] [Google Scholar]
- 64.Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346:f3646. doi: 10.1136/bmj.f3646. [DOI] [PubMed] [Google Scholar]
- 65.Song J, Sjölander A, Joas E, et al. Suicidal behavior during lithium and valproate treatment: a within-individual 8-year pro spective study of 50,000 patients with bipolar disorder. Am J Psychiatry. 2017;174:795–802. doi: 10.1176/appi.ajp.2017.16050542. [DOI] [PubMed] [Google Scholar]
- 66.Chen Q, Sjölander A, Runeson B, D'Onofrio BM, Lichtenstein P, Larsson H. Drug treatment for attention-deficit/hyper-activity disorder and suicidal behaviour: register based study. BMJ. 2014;348:g3769. doi: 10.1136/bmj.g3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Molero Y, Zetterqvist J, Binswanger IA, Hellner C, Larsson H, Fazel S. Medications for alcohol and opioid use disorders and risk of suicidal behavior, accidental overdoses, and crime. Am J Psychiatry. 2018;175:970–8. doi: 10.1176/appi.ajp.2018.17101112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Meerwijk EL, Parekh A, Oquendo MA, Allen IE, Franck LS, Lee KA. Direct versus indirect psychosocial and behavioural interventions to prevent suicide and suicide attempts: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:544–54. doi: 10.1016/S2215-0366(16)00064-X. [DOI] [PubMed] [Google Scholar]
- 69.Mewton L, Andrews G. Cognitive behavioral therapy for suicidal behaviors: improving patient outcomes. Psychol Res Behav Manag. 2016;9:21–9. doi: 10.2147/PRBM.S84589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chesin M, Interian A, Kline A, Benjamin-Phillips C, Latorre M, Stanley B. Reviewing mindfulness-based interventions for suicidal behavior. Arch Suicide Res. 2016;20:507–27. doi: 10.1080/13811118.2016.1162244. [DOI] [PubMed] [Google Scholar]
- 71.DeCou CR, Comtois KA, Landes SJ. Dialectical behavior therapy is effective for the treatment of suicidal behavior: a meta-analysis. Behav Ther. 2019;50:60–72. doi: 10.1016/j.beth.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 72.Cottrell DJ, Wright-Hughes A, Collinson M, et al. Effectiveness of systemic family therapy versus treatment as usual for young people after self-harm: a pragmatic, phase 3, multicentre, randomised controlled trial. Lancet Psychiatry. 2018;5:203–16. doi: 10.1016/S2215-0366(18)30058-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Spijker BA, van Straten A, Kerkhof AJ. Effectiveness of online self-help for suicidal thoughts: results of a randomised controlled trial. PLoS One. 2014;9(2):e90118. doi: 10.1371/journal.pone.0090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van Spijker BA, Werner-Seidler A, Batterham PJ, et al. Effectiveness of a webbased self-help program for suicidal thinking in an Australian community sample: randomized controlled trial. J Med Internet Res. 2018;20(2):e15. doi: 10.2196/jmir.8595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dunster-Page C, Haddock G, Wainwright L, Berry K. The relationship between therapeutic alliance and patient's suicidal thoughts, self-harming behaviours and suicide attempts: a systematic review. J Affect Disord. 2017;223:165–74. doi: 10.1016/j.jad.2017.07.040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.