Abstract
Using transboundary pollution from mainland China as an instrument, we show that air pollution leads to higher cardio-respiratory mortality in Hong Kong. However, the air pollution effect has dramatically decreased over the past two decades: before 2003, a 10-unit increase in the Air Pollution Index could lead to a 3.1% increase in monthly cardio-respiratory mortality, but this effect has declined to 0.5% using recent data and is no longer statistically significant. Exploratory analyses suggest that a well-functioning medical system and immediate access to emergency services can help mitigate the contemporaneous effects of pollution on mortality.
Keywords: Air pollution, Health, Transboundary pollution, Healthcare, Emergency service
1. Introduction
Hong Kong (HK) is an autonomous territory, and a former British colony, in southeastern China. The city has about 7.5 million people and among the highest per capita incomes in the world.1 Notably, HK people have the highest life expectancy in the world, with male life expectancy being 81.32 years and female life expectancy being 87.34 years in 2017. Unlike other rich economies in the rest of the world, however, air quality in HK is poor and transboundary air pollution is a serious concern. For example, the annual average concentration of particulate matter (PM10) in HK was 45 μg/m3 from 2000 to 2015, which was more than twice WHO’s recommended level of 20 μg/m3. The NO2 concentration was 63 μg/m3 during this period, roughly 1.5 times higher than the WHO’s corresponding threshold.
This study estimates the causal impact of air pollution on mortality using 16 years’ of micro-level death data from HK. Our identification strategy builds on the fact that transboundary pollution (i.e., pollution transmitted from mainland China) plays an important role in determining HK’s air quality. HK is located near mainland China’s Pearl River Delta Economic Zone (PRDEZ), a major manufacturing center. Emissions from heavy industrial activities in the PRDEZ are brought to HK by wind, creating exogenous variations in local air quality. Using instruments based on the combinations of wind direction, air pollution in the PRDEZ, and distance between the PRDEZ and different districts of HK, we show that air pollution causes more people to die from cardio-respiratory diseases. Specifically, we estimate that a 10-unit increase in the Air Pollution Index (API) can cause a 1.77% increase in monthly cardio-respiratory mortality.2 The elderly are particularly vulnerable to air pollution, with a 10-unit change in the API leading to an 8.41% change in mortality. To understand how the air pollution effect changes over time, we split the sample by different sub-periods and find that the effect has been diminishing in the past two decades. Further analyses reveal that the diminishing effect is likely to be driven by medical improvement initiatives and the advancement of community-based healthcare services after the Severe Acute Respiratory Syndrome (SARS) epidemic, not by changes in avoidance behaviors or public awareness of air pollution.
This study makes two primary contributions to the existing literature. First, this study is among the first efforts to estimate the causal health effects of air pollution in a high-income and high-pollution context. Existing literature mostly focuses on developed countries with a low level of pollution, such as the U.S. and the E.U., or developing countries with a high level of pollution, such as China and India. The high-income high-pollution setting is important because the air pollution effect can be non-linear and the pollution-mortality relationship may be altered by better institutional, and socio-economic background (Arceo et al., 2016; Burnett et al., 2014). Within the small set of studies that focus on HK, most of them are associational studies that may suffer from endogeneity concerns (e.g., Ko et al., 2007; Qiu et al., 2012; Wong et al., 2001; Wong et al., 2002). The only exception is Colmer et al. (2019), a concurrent study that also emphasizes the importance of investigating Hong Kong. Colmer et al. (2019) focus on how air pollution affects birth weight and infant mortality and find that while air pollution can reduce the birth weight of babies, it does not kill them. We differ from Colmer et al. (2019) in that we focus on different health outcomes (mortality for different age groups vs. infant health), adopt a different identification strategy (transboundary pollution vs. thermal inversion), and try to pin down the exact channels through which the pollution-mortality relationship can be moderated.
This paper also provides the first evidence that air pollution impact can be significantly mitigated by better medical institutions and provision of high-quality health care. Specifically, we show that the air pollution effect has significantly reduced after the SARS epidemic, during which HK government made massive investments and structural reforms in healthcare systems. We also find that the air pollution effect is larger for districts that do not have a hospital with Accident and Emergency (A&E) services, highlighting the critical role of emergency care in saving vulnerable people from dying from air pollution attacks. Several alternative explanations, including non-linear dose-response between pollution and mortality, smoking, and avoidance behavior, can be ruled out after further analyzing relevant data. Our finding suggests that a well-established medical system can help mitigate the contemporaneous health effect of air pollution, which also partly explains why HK people can have the longest life expectancy in the world despite breathing relatively dirty air.
The rest of this paper is organized as follows. Section 2 discusses air pollution in HK, existing evidence, and our empirical strategy. Section 3 describes our data and presents some stylized facts about HK and the PRDEZ’s air quality. Section 4 reports the main findings and Section 5 discusses the diminishing air pollution effect. Section 6 concludes.
2. Existing evidence and empirical setup
2.1. Air pollution in Hong Kong
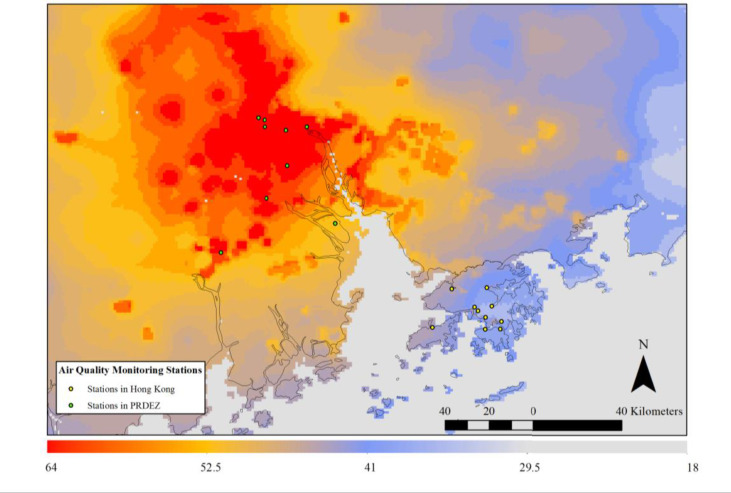
Hong Kong (HK), officially the Hong Kong Special Administrative Region of the People’s Republic of China, is an autonomous territory on the eastern side of the Pearl River Delta Economic Zone (PRDEZ) in South China (Fig. 1 ). The PRDEZ is China’s major manufacturing center, consisting of several highly industrialized cities, including Guangzhou, Dongguan, Foshan, Jiangmen, Shenzhen, Zhuhai, Zhongshan, and parts of Huizhou and Zhaoqing.
Fig. 1.
The annual average of PM2.5 concentrations (μg/m3) for the pearl River Delta region.
Source: PM2.5 concentrations in 2006 are derived from Aerosol Optical Depth (AOD) satellite data. AOD data are extracted from the National Aeronautics and Space Administration (NASA) of the United States.
Air quality is a major concern in HK and transboundary pollution is an important source of HK’s air pollution. In the scientific literature, studies have examined how air pollutants from the PRDEZ affect HK’s air quality. For example, because of the heavy manufacturing and economic activities in the PRDEZ, particulate matter from the PRDEZ can account for approximately 50%–60% of average pollution levels in HK and increase to as high as 70% in certain periods (e.g., Wu et al., 2013; Yuan et al., 2006).
Several factors influence the severity of transboundary pollution in HK, including the baseline air pollution levels in the PRDEZ, wind patterns, and distances between the PRDEZ and different districts of HK. Depending on the wind’s direction, HK’s air pollution can be high or low: when HK is downwind of the PRDEZ, the wind will carry the PRDEZ’s pollutants to HK and the air quality in HK will be negatively affected. In contrast, when HK is upwind of the PRDEZ, HK’s air quality will be improved as regional air pollutants are carried away by the wind.
The PRDEZ’s air pollution affects different districts in HK differentially and the effect depends partly on whether a district is close to or far away from the PRDEZ. In general, western HK, which is closer to the PRDEZ, is more strongly affected by transboundary air pollution. On some extreme occasions, the air pollution level along the western edge of HK could be several times higher than the rest of HK, although there is much less economic and production activity taking place in these areas (Lau et al., 2007).
Under the “one country, two systems” rule, HK has no direct authority to regulate the pollution activities in mainland China even though these can significantly impact HK’s air quality.3 Although in recent years there have been multiple rounds of discussions between HK and the Guangdong governments on coordinating air pollution control, the agreements between the two parties often focus on long-term targets and lack concrete enforcement plans. As a result, transboundary pollution remains a controversial and largely unresolved issue between the mainland and HK.
Fig. 1 presents the annual average of PM2.5 concentrations derived from satellite data for the region.4 We observe that air quality in the PRDEZ is significantly worse than in HK. This is reasonable because the PRDEZ has a significant manufacturing sector, while HK has almost no manufacturing.5 Besides, the northwestern part of HK has higher levels of air pollution than the southeastern part, because it is closer to the PRDEZ. These variations underlay the instrumental variable approach used in this study.
2.2. The air pollution effect and existing evidence in HK
Understanding the impact of air pollution on health is an important research topic in science, public health, and economics. Thus, the literature consists of a large number of studies using different empirical methodologies, reflecting the norms and evolution of different fields. This section is not intended to provide a comprehensive review of the literature; instead, it aims at providing a basic framework summarizing previous findings in HK.
Existing evidence often adopts one of the following four methodologies to estimate the effect of air pollution on health: 1) time-series studies; 2) cross-sectional and cohort-based studies; 3) panel or fixed effects studies; and 4) quasi-experimental studies.
Time-series studies analyze the relationship between the temporal fluctuations in air pollution and health outcomes and try to estimate the contemporaneous effect of air pollution on health. The identification typically relies on the assumption that, after controlling for a set of observed weather confounders and different trends, day-to-day variation in air pollution can be treated as exogenous. A large number of public health studies that rely on time-series models generally find that poorer air quality is associated with worse health outcomes. Early time-series studies mostly focused on developed countries (e.g., Bell et al., 2004; Dockery et al., 1993; Levy et al., 2012; Pope III et al., 2002; Stieb et al., 2002), while in recent years, there has emerged a literature focusing on developing countries (e.g., Aunan and Pan, 2004; Lai et al., 2013; Lu et al., 2015; Shang et al., 2013).
However, time-series studies often suffer from omitted variable bias because not all confounders can be properly controlled for. To address this issue, researchers often include a large set of fixed effects and include flexible functions of time trends and weather conditions in the model. This introduces several potential problems. First, the estimates from time-series analyses tend to be sensitive to different controls and inclusion of trends, making it difficult to assess which estimates are the most reliable. Second, if air pollution is measured with error, overfitting the time-series model can attenuate the estimates and understate the air pollution effect. As a result, it is difficult to determine whether the poorer health outcomes were actually caused by elevated air pollution levels or by other confounding factors (Chay and Greenstone, 2003a, 2003b; Pope III and Burnett, 2007; He et al., 2016). For HK, we find that most previous studies rely on time-series models (Ko et al., 2007; Qiu et al., 2012; Wong et al., 2001; Wong et al., 2002), and similar critiques also apply to those studies.
Cross-sectional studies analyze the associations between air pollution levels and health outcomes across different locations at a specific point in time. Many of the cross-sectional studies were conducted in the last century and recent literature has shifted attention to other research designs. The drawbacks of cross-sectional studies are obvious: people’s health and exposure to air pollution across different locations are simultaneously affected by many socioeconomic factors and it is often impossible to account for all these confounders. For HK, Gao et al. (2014) show that children living in high-pollution districts are at higher risk for respiratory morbidities than those living in low-pollution districts.
Cohort-based studies analyze the long-term health effect of air pollution by following people over many years. Existing evidence shows that long-term exposure to air pollution is associated with worse health outcomes in both developed countries (Abbey et al., 1999; Dockery et al., 1993; Pope III et al., 1995) and developing countries (Cao et al., 2011; Zhang et al., 2011; Zhou et al., 2014). For HK, Qiu et al. (2017) and Qiu et al. (2018) use similar approaches and find that long-term exposure to air pollution is associated with the development of Type II diabetes and incident ischemic stroke among the elderly. Yet, aside from potential omitted variable bias mentioned above, cohort-based studies are further complicated by potential sorting (Chay and Greenstone, 2003b; Evans et al., 1984). In the end, people choose where to live and these choices may depend on pollution and other factors. For example, the wealthier individuals tend to migrate to areas with lower pollution, while the poorer individuals may remain in the polluted areas. This implies that the observed association between air quality and mortality could be driven by factors related to sorting, instead of pollution itself.
As large-scale administrative data become more available to researchers, panel data models with fixed effects become increasingly popular. These models are powerful in addressing the endogeneity issue when potential confounders are time-invariant (Currie and Neidell, 2005; Currie et al., 2009). However, the identifying assumption of the fixed effects models can still be too strong because many time-varying variables, such as weather and traffic, can affect both air quality and health outcomes. In addition, estimates from fixed-effects models may suffer from severe attenuation bias if the regressor is measured with error (Wansbeek and Meijer, 2001).
With the economics profession’s increased focus on credible identification in recent years, quasi-experimental approaches have become the favored empirical strategy for estimating the health effects of air pollution. Quasi-experimental studies often explore exogenous variation in air pollution caused by policy or nature that can mimic random assignment of treatment and control groups. Graff Zivin and Neidell (2013) provide a thorough survey of this line of research. Notable examples include, but are not limited to, Chay and Greenstone (2003a, 2003b), Currie and Neidell (2005), Jayachandran (2009), Lleras-Muney (2010), Currie and Walker (2011), Greenstone and Hanna (2014), Luechinger (2014), Cesur et al. (2017), and Schlenker and Walker (2015), Anderson (2019). For the Chinese context, Chen et al. (2013) and Ebenstein et al. (2017) exploit China’s Huai River policy and estimate the impact of air pollution on life expectancy. He et al. (2016) estimate the short-term effects of air pollution on mortality using the Beijing 2008 Olympic Games as a quasi-experiment.
Despite the growing number of quasi-experimental studies, existing evidence either focuses on high-pollution low-income (such as India and mainland China) or low-pollution high-income settings (mostly the U.S.). Since the relationship between exposure to air pollution and health response can be non-linear and depend on local socio-economic background (Arceo et al., 2016; Burnett et al., 2014), the results from previous studies may have limited validity for a high-pollution high-income setting. As mentioned in the introduction, the only exception is the concurrent study by Colmer et al. (2019), who also emphasize the importance of studying HK. Using thermal inversion as the instrument, Colmer et al. (2019) show that air pollution can reduce the birth weights of babies but does not affect infant mortality. They argue that better “institution” in HK, such as the Hospital Authority providing free and high-quality healthcare to the public, may help explain why infants do not die from air pollution. Yet, there is no direct evidence to support this argument in their paper.
This study adds to this literature by providing a more comprehensive analysis of the air pollution effect in HK. As pollution from mainland China creates quasi-random shocks to HK’s local air quality, we utilize this transboundary pollution to identify the air pollution effect. The identification strategy is similar in spirit to Jia and Ku (2019), Deryugina et al. (2019), and Anderson (2019). Anderson (2019) and Deryugina et al. (2019) compare the population groups living downwind and upwind and estimate the effects of air pollution exposure on the population mortality and health cost of the elderly in the United States. Jia and Ku (2019) assess the impact of cross-border air pollution from China to South Korea and find that “yellow dust” (sand) blowing in from China leads to extra deaths in South Korea.
2.3. Empirical strategy
Our analysis exploits the variations in HK’s air quality caused by the PRDEZ’s air pollution. In the first stage, we estimate the following equation:
| (1) |
where is the monthly air pollution level in district at time , is the average monthly air pollution level in the PRDEZ at time , is the wind speed in district at time , is the percentage of days with wind direction as the prevailing wind direction in district at time ,6 and is the distance between the PRDEZ and district . The interactions among , , and are also included in the first-stage regression. are control variables including temperature, temperature squared, and precipitation in district at time , are district fixed effects, are year by month fixed effects, and indicates the error term.
The first-stage regression helps us understand how air pollution in the PRDEZ affects HK’s air quality under different meteorological conditions. captures the effect of different wind directions on HK’s air quality. captures the effect of wind speed on air pollution. For the interaction terms, describes how the distance between different areas in HK and the PRDEZ changes the effect of regional air pollution on HK’s air quality, captures how the local wind direction changes the effect of regional air pollution on HK’s air quality, estimates how the distance between HK and the PRDEZ changes the effect of the local wind direction on HK’s air quality, and captures how the distance between Hong and the PRDEZ and the local wind direction simultaneously change the effect of regional air pollution on HK’s air quality.
The interaction terms are included to improve predictive power in the first stage. We interact the PRDEZ’s air pollution level, , with different wind directions in HK , because the pollution will be more severe when the wind blows air pollutants from PRDEZ to HK. Additionally, because the transboundary pollution also depends on the distance between PRDEZ and HK’s different districts, we further include interactions between distances, regional air pollution level, and wind directions as instruments.
In the second stage, we estimate the following equation:
| (2) |
where is the logarithm of the monthly mortality rate per 10,000 in district at time , and is the predicted air pollution levels from the first stage. and are district and time fixed effects. are unobservable disturbances. is the coefficient of interest, which captures the causal impact of air pollution on mortality.
We use monthly data to avoid estimating the very short-term health effect (i.e., the effect of daily air pollution on mortality) for two reasons. First, many epidemiological studies have investigated the dynamic impacts of air pollution on health outcomes and a general finding is that air pollution can lead to worse health outcomes at a more aggregated level (e.g., Zeger et al., 1999; Schwartz, 2000; Zanobetti et al., 2000; Zanobetti et al., 2002; Costa et al., 2017; Zanobetti and Schwartz, 2008; Deryugina et al., 2019). The reason is that people will develop more complex cardio-respiratory diseases with prolonged exposure to air pollution and the affected population will increase over time. Monthly data therefore allows us to capture the air pollution effect in the medium run. Second, our instruments are based on transboundary air pollution from one region to another and it takes time for the transmission to take place. If we use daily data, current-day pollution in PRDEZ may not be able to strongly affect current-day air quality in HK, especially when weather conditions are relatively stable. It is thus conceptually unappealing for the instrument to work with high-frequency daily data.
For comparison, we also estimate the associations between air pollution and mortality rate using pooled Ordinary Least Squares (OLS) and fixed-effects models. The pooled OLS is estimated by the following equation:
| (3) |
where all the variables are defined as above. captures the effect of air pollution on mortality rate if air pollution is uncorrelated with unobserved health determinants (i.e., ). However, because local air quality and people’s health are often simultaneously determined by many socio-economic and meteorological factors, the assumption that may be violated, which would result in a biased estimate of .
To account for time-invariant confounders, one can further include district fixed effects in Equation (3). Year-month fixed effects can also be included in the regression to account for shocks that are common to all the districts in a particular year and month. In practice, we can estimate the following equation:
| (4) |
The fixed-effects model can alleviate the endogeneity concern to some extent, as many confounding factors are controlled for. However, the fixed effects model may also suffer from omitted variable bias if the unobserved confounders change across locations and over time (such as local weather and traffic conditions).
3. Data
3.1. Air quality and weather data
HK’s air quality data are collected from the Air Quality Monitoring Network administrated by the Environmental Protection Department of the HK Government. The PRDEZ’s air quality data are reported by the local environmental bureaus and collected by the Environmental Central Facility of the Hong Kong University of Science and Technology.
Fig. 1 shows the geographical locations of the air quality monitoring stations in HK and the PRDEZ. There are ten fixed monitoring stations measuring the concentration levels of air pollution in the urban districts of HK.7
We use the Air Pollution Index (API) as the primary explanatory outcome. The API is a comprehensive air pollution measure and is used by both the HK and mainland governments. The calculation of API is based on the concentrations of several air pollutants, including ambient respiratory particulate matter (PM10), sulfur dioxide (SO2), carbon monoxide (CO), ozone (O3), and nitrogen dioxide (NO2). To construct the API, an API sub-index for each pollutant is first calculated and the highest API sub-index calculated will become the API. The API is set with reference to the HK Air Quality Objectives (AQO). Appendix Table S1 shows the sub-index levels for the API and their corresponding concentrations. To make the API values comparable across years and locations, the same calculation method is used to convert concentration levels of each air pollutant to API for both HK and the PRDEZ for the whole study period.8 To construct the instrumental variable, we average the air pollution readings from all the stations in PRDEZ and calculate the regional API.
Weather data, including wind direction, wind speed, temperature, and precipitation, are extracted from the HK Observatory. Each air quality monitoring station in HK is matched with the weather station nearest to it.
3.2. Mortality data
Mortality data are obtained from the Census and Statistics Department of the HK Government. We use the “known death microdata” for the period 2000–2015 in this study. The dataset recorded detailed attributes for each death, including the date of death, age, sex, cause of death, occupation, place of residence, and length of stay in HK.
The classification of cause of death is based on the Ninth and Tenth Revisions of the International Statistical Classification of Diseases and Related Health Problems (ICD-9 and ICD-10). Following previous literature, the mortality data were classified using ICD-9 and ICD-10 into deaths from cardiovascular and respiratory diseases (CVR) and deaths from non-cardiovascular and respiratory diseases (non-CVR).
The place of residence is categorized by 3-digit tertiary planning units (TPUs) code. The whole territory of HK is divided into 289 TPUs by the Planning Department of the HK Government for town planning purposes. These TPUs are then grouped into 151 Large Tertiary Planning Unit Groups (LTPUGs) by the C&SD, where each LTPUG would have a population of at least 10,000 by 2001. The areas of LTPUG ranges from 0.09 to 85.12 km2 with a mean of 7.35 km2. We thus focus on death and air pollution at the LTPUG level, which is referred to as a “district” in this paper.
Mortality data are then matched with air pollution data and LTPUG-level population data. The population data are extracted from HK’s Population By-census in 2006, 2011, and 2016. We conduct a linear interpolation approach to fill the population data in other years. Each LTPUG is assigned to the nearest air quality monitoring station. A map of the LTPUGs is provided in Appendix Fig. S2.
Data for the year of the SARS outbreak, 2003, are dropped in the analysis because it can confound the air pollution effect estimates. Nearly three hundred people died from SARS, but these deaths were not related to air pollution. In addition, during the SARS epidemic, economic activities and daily life of people in HK were significantly changed (Hung, 2003; Siu and Wong, 2004). For example, most people used face masks and avoided going outside during the outbreak, which could affect pollution exposure and reduce their chances of contracting other types of respiratory diseases.
3.3. Summary statistics
We present some stylized facts from our data and summarize the descriptive statistics in this section. As shown in Appendix Fig. S3, there exists a strong correlation between HK and the PRDEZ’s air quality. The trend of air pollution in HK has closely followed the trend in the PRDEZ. The air quality deteriorated from 2000 to 2004 and then started to improve in both the PRDEZ and HK.
Table 1 provides summary statistics of the key variables. The mean API in HK is about 45 during our sample period, 13 units lower than that in the PRDEZ. The distance between the LTPUGs and the PRDEZ’s air quality stations ranges from 103.1 to 131.9 km. About 40% of the time, the wind blows from the PRDEZ to HK (the north and northwest wind). The average monthly standardized mortality rates for CVR and non-CVR diseases are 2.20 and 2.60 per 10,000, respectively.
Table 1.
Summary statistics of the main variables.
| Mean | SD | Min | Max | Obs | |
|---|---|---|---|---|---|
| Monthly Average API in Hong Kong | 44.55 | 10.83 | 15.52 | 76.24 | 24,029 |
| Monthly Average API in the PRDEZ | 58.53 | 11.09 | 32.83 | 94.15 | 23,625 |
| Distance with the PRDEZ (10 km) | 12.18 | 0.88 | 10.31 | 13.19 | 24,300 |
| Standardized Monthly CVR Mortality Rate (per 10,000) | 2.20 | 1.59 | 0.00 | 14.36 | 24,132 |
| Standardized Monthly Non-CVR Mortality Rate (per 10,000) | 2.60 | 1.59 | 0.00 | 14.35 | 24,132 |
| Days with wind direction 0° | 26.11% | 0.22 | 0.00% | 100.00% | 24,201 |
| Days with wind direction 45° | 0.05% | 0.00 | 0.00% | 3.33% | 24,201 |
| Days with wind direction 90° | 39.21% | 0.23 | 0.00% | 96.77% | 24,201 |
| Days with wind direction 135° | 13.75% | 0.18 | 0.00% | 100.00% | 24,201 |
| Days with wind direction 180° | 6.60% | 0.12 | 0.00% | 80.00% | 24,201 |
| Days with wind direction 225° | 5.17% | 0.10 | 0.00% | 100.00% | 24,201 |
| Days with wind direction 270° | 7.19% | 0.12 | 0.00% | 70.97% | 24,201 |
| Days with wind direction 315° | 1.93% | 0.05 | 0.00% | 67.74% | 24,201 |
| Wind Speed (m/s) | 3.52 | 1.84 | 1.16 | 46.56 | 24,201 |
| Precipitation (100 mm) | 5.95 | 6.92 | 0.00 | 49.28 | 24,250 |
| Temperature (°C) | 22.03 | 5.07 | 6.99 | 29.82 | 24,300 |
Notes: All variables are measured at the monthly level. CVR stands for cardiovascular and respiratory diseases. The classification and definition of wind directions are illustrated in Appendix Fig. S1.
4. Main results
4.1. The effects of air pollution on mortality
Table 2 summarizes the IV estimates on the impacts of air pollution on different mortality rates. Existing evidence suggests that short-term and long-term exposure to ambient air pollution primarily affects CVR diseases (Pope III et al., 1995; Chen et al., 2013; He et al., 2016; Ebenstein et al., 2017). We follow the literature and estimate the effect of air pollution separately for CVR (Columns 1–3) and non-CVR causes (Columns 4–6). The dependent variable is the logarithm of the monthly standardized mortality rate per 10,000; the interpretation of the estimated coefficient is therefore percentage change in monthly mortality rate. In all the regressions, district (LTPUG) fixed effects and year-month fixed effects are included. We gradually include precipitation and temperature (and the square of temperature), which are typical confounders in the regressions, to check the robustness of the estimates. We also report the standard errors clustered at different levels to examine the sensitivity of the significance: the LTPUG level, the LTPUG and year level, and the LTPUG and year-quarter level (Cameron et al., 2011).
Table 2.
The effect of air pollution on CVR and Non-CVR mortality rate.
| CVR Mortality, log |
Non-CVR Mortality, log |
Diff. |
||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | ||
| (per 10 units) | ||||||||
| Hong Kong’s API | 0.0182∗∗∗ | 0.0183∗∗∗ | 0.0177∗∗∗ | 0.0097∗ | 0.0097∗ | 0.0086 | 0.0090∗ | |
| (0.0057) | (0.0058) | (0.0059) | (0.0053) | (0.0054) | (0.0054) | (0.0054) | ||
| (0.0069) | (0.0069) | (0.0069) | (0.0056) | (0.0057) | (0.0057) | (0.0048) | ||
| (0.0063) | (0.0063) | (0.0064) | (0.0056) | (0.0058) | (0.0058) | (0.0048) | ||
| Temp and Sq. | Y | Y | Y | Y | Y | |||
| Precipitation | Y | Y | Y | |||||
| Year-month FE | Y | Y | Y | Y | Y | Y | Y | |
| LTPUG FE | Y | Y | Y | Y | Y | Y | Y | |
| Observations | 23,094 | 23,094 | 23,044 | 23,094 | 23,094 | 23,044 | ||
| Number of LTPUG | 135 | 135 | 135 | 135 | 135 | 135 | ||
| First stage F-statistics | 277.2 | 171.0 | 183.2 | 196.0 | 194.3 | 229.0 | ||
| RMSE | 0.66 | 0.66 | 0.66 | 0.60 | 0.60 | 0.60 | ||
| First stage Shea Partial R2 | 0.22 | 0.22 | 0.21 | 0.23 | 0.22 | 0.23 | ||
| R2 | 0.08 | 0.08 | 0.08 | 0.03 | 0.03 | 0.03 | ||
Notes: This table reports the two-stage least squares regression coefficients and standard errors. PRDEZ’s API, local wind conditions, distances to the PRDEZ and their interaction terms are used as the instrumental variables for Hong Kong’s API. The dependent variables are the logarithm of monthly mortality rate for all cardiovascular and respiratory (CVR) deaths and non-CVR deaths. Column 7 presents the akin-to Wald estimator to compare the difference between the coefficients in Column 3 and Column 6. We probe the robustness of estimates accuracy by clustering the standard errors at three different levels: the Large Tertiary Planning Unit Group (LTPUG) level, LTPUG and year, and LTPUG and year-quarter level (multi-way clustering suggested by Cameron Gelbach, and Miller (2011)). The standard errors are respectively reported in the parentheses below the estimated coefficients. Our preferred specification clusters standard errors at the LTPUG level. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
Results in Columns 1 to 3 show that air pollution has a statistically significant impact on CVR deaths. A 10-unit increase in API will result in a 1.77%–1.82% increase in monthly CVR mortality in HK. In contrast, the estimates for non-CVR deaths in Columns 4 to 6 are smaller in magnitude and statistically insignificant at the 5% level. In Column 7, we compare the difference between the estimates in Columns 3 and 6 and find that the difference is statistically significant at the 10% level.
The first-stage regression results, which have a long list of instrument variables for HK’s air pollution, are reported in Appendix Table S2. We see that many instruments are statistically significant, suggesting that the PRDEZ’s air pollution, wind direction, and distances between the PRDEZ and different HK districts can strongly predict HK’s air pollution.
4.2. Results by gender and age group
Air pollution may affect males and females in different ways. Existing evidence on the gender difference in air pollution epidemiology is far from conclusive and the mechanisms are not yet clear (Clougherty, 2009). This is because males and females are different in fundamental ways that can affect the pollution-mortality relationship, including time use, smoking, inner dermal absorption and lung function, and the availability of target organs (McCracken et al., 2007; Becklake and Kauffmann, 1999). We explore the gender heterogeneity in HK and report the results separately for males and females in Table 3 . We find that the impacts of air pollution on males are generally larger and more statistically significant than females. A 10-point change in the API increases the male mortality rate by 2.22%, which is two times larger than its impact on females. In the literature, several other studies also find stronger air pollution effects on males (e.g., Pope III et al., 1995; Galizia and Kinney, 1999; Tanaka, 2015; Ebenstein et al., 2015; Cohen et al., 2017).
Table 3.
The effect of air pollution on CVR mortality rate by gender.
| Male |
Female |
|||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| (per 10 units) | ||||||
| Hong Kong’s API | 0.0236∗∗∗ | 0.0240∗∗∗ | 0.0222∗∗∗ | 0.0107∗ | 0.0107∗ | 0.0109∗ |
| (0.0083) | (0.0084) | (0.0085) | (0.0057) | (0.0060) | (0.0058) | |
| Temp and Sq. | Y | Y | Y | Y | ||
| Precipitation | Y | Y | ||||
| Year-month FE | Y | Y | Y | Y | Y | Y |
| LTPUG FE | Y | Y | Y | Y | Y | Y |
| Observations | 23,094 | 23,094 | 23,044 | 23,094 | 23,094 | 23,044 |
| Number of LTPUG | 135 | 135 | 135 | 135 | 135 | 135 |
| First stage F-statistics | 430.3 | 359.0 | 375.9 | 121.8 | 63.78 | 149.6 |
| RMSE | 0.61 | 0.61 | 0.61 | 0.79 | 0.79 | 0.79 |
| R2 | 0.07 | 0.07 | 0.07 | 0.05 | 0.05 | 0.05 |
Notes: This table reports the two-stage least squares regression coefficients and standard errors. PRDEZ’s API, local wind conditions, distances to the PRDEZ and their interaction terms are used as the instrumental variables for Hong Kong’s API. The dependent variables are the logarithm of the monthly mortality rate for all cardiovascular and respiratory (CVR) deaths. Columns 1–2 and 3–4 show estimates for males and females respectively. Standard errors in parentheses are clustered at the Large Tertiary Planning Unit Group (LTPUG) level. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
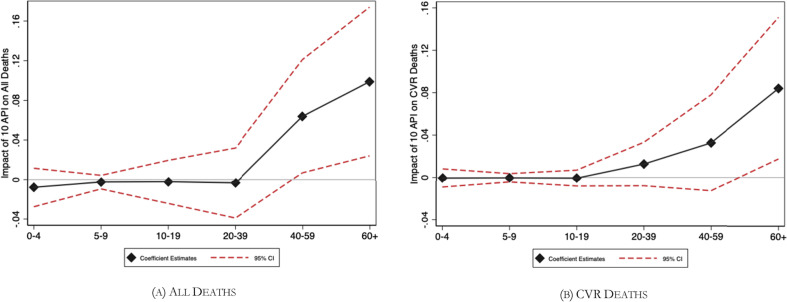
Next, we examine the air pollution effects by age group. Because the exact number of people in each age group is not available at the LTPUG level, we directly estimate the impacts of air pollution on the number of deaths with respect to different age groups. Fig. 2 summarizes the results. In line with the previous studies, we find that the air pollution effect is statistically significant for the elderly group (age>60) (Chen et al., 2013). Specifically, for people who are older than 60, a 10-point increase in API leads to an 8.41% increase in the total number of CVR deaths. The corresponding regression results are reported in Table 4 .
Fig. 2.
The effect of API (per 10 units) on deaths by different age groups.
Table 4.
The effect of air pollution by age group.
| CVR Mortality, log (1) |
Non-CVR Mortality, log (2) |
|
|---|---|---|
| Age 0 to 4 | −0.0006 | −0.0081 |
| (0.0044) | (0.090) | |
| Age 5 to 9 | −0.0004 | 0.0023 |
| (0.0021) | (0.0031) | |
| Age 10 to 19 | −0.0006 | 0.0021 |
| (0.0039) | (0.0094) | |
| Age 20 to 39 | 0.0127 | −0.0118 |
| (0.0105) | (0.0191) | |
| Age 40 to 59 | 0.0327 | 0.0459 |
| (0.0232) | (0.0278) | |
| Age 60+ | 0.0841∗∗ | 0.0440 |
| (0.0355) | (0.0367) |
Notes: This table reports the two-stage least squares regression coefficients and standard errors. Each cell reports a separate regression of the logarithm of monthly cardiovascular and respiratory (CVR) deaths and non-CVR deaths on Hong Kong’s API. PRDEZ’s API, local wind conditions, distances to the PRDEZ and their interaction terms are used as the instrumental variables for Hong Kong’s API. Weather, LTPUG fixed effects and year-month fixed effects are controlled for each regression. Standard errors in parentheses are clustered at the Large Tertiary Planning Unit Group (LTPUG) level. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
Infants, children, and young adults do not die from air pollution in HK. Note that our finding that air pollution does not lead to more deaths in the infant and young children group differs from many previous studies (e.g., Chay and Greenstone, 2003a; Currie and Neidell, 2005; Currie et al., 2009; Currie and Walker, 2011; Greenstone and Hanna, 2014), but is consistent with Colmer et al. (2019), who find that although HK’s bad air decreases the birth weights, it does not cause more infants deaths.
4.3. Lagged effect
Many time-series studies show that the effects of air pollution on health can be cumulative; the lagged effect can range from a few days to a few weeks. In Table 5 , we examine this issue by including the lagged pollution measure in the regressions. Current and lagged IVs are used in the first stage to predict current and lagged API and we include two lags in the regressions.
Table 5.
The effect of air pollution on mortality rate with lags.
| CVR Mortality, log (1) |
Non-CVR Mortality, log (2) |
|
|---|---|---|
| (per 10 units) | ||
| Hong Kong’s API | 0.0120∗∗ | 0.0001 |
| (0.0056) | (0.0048) | |
| Hong Kong’s API, Lag = 1 | 0.0002 | 0.0054 |
| (0.0052) | (0.0053) | |
| Hong Kong’s API, Lag = 2 | 0.0065 | 0.0032 |
| (0.0046) | (0.0047) | |
| Temp and Sq. | Y | Y |
| Precipitation | Y | Y |
| Year-month FE | Y | Y |
| LTPUG FE | Y | Y |
| Observations | 22,184 | 22,184 |
| Number of LTPUG | 135 | 135 |
| First stage F-statistics | 236.4 | 61.25 |
| RMSE | 0.66 | 0.60 |
| R2 | 0.08 | 0.03 |
Notes: This table reports the two-stage least squares regression coefficients and standard errors. Current and lagged PRDEZ’s API, local wind conditions distances to the PRDEZ and their interaction terms are used as the instrumental variables for current and lagged Hong Kong’s API. The dependent variables are the logarithm of monthly mortality rate for cardiovascular and respiratory (CVR) deaths and non-CVR deaths for the period 2000 to 2015. Standard errors in parentheses are clustered at the Large Tertiary Planning Unit Group (LTPUG) level. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
Column 1 shows that the effect of air pollution on CVR deaths is only statistically significant for the current API. One- and two-month lagged API are both statistically insignificant with a smaller magnitude. Column 2 shows that there is no statistically significant relationship between air pollution and non-CVR deaths. These results suggest that there is no significant lag effect at the monthly level.
4.4. Test for nonlinearities
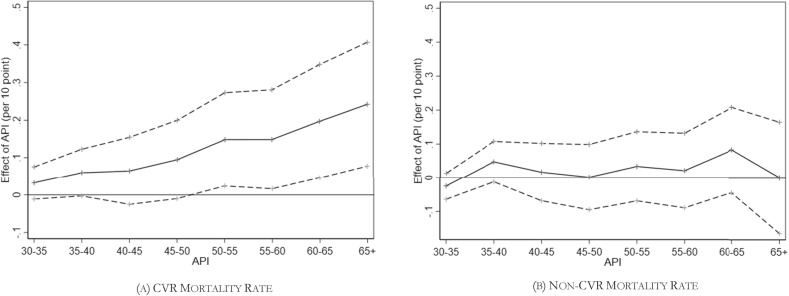
Our baseline specification assumes that the causal relationship between air pollution and mortality is linear. In this section, we investigate whether air pollution’s effect on mortality is nonlinear following the empirical strategy in Graff Zivin and Neidell (2012). To do so, we create dummy variables for every 5 points of API and omit API <30 points as the reference group. For comparison, we conduct the analysis separately for CVR and non-CVR mortality.
Fig. 3 presents the dose-response curves.9 Our observation is that the effect of API on the monthly CVR mortality rate (Fig. 3a) is roughly linear. For the non-CVR mortality rate (Fig. 3b), the effect remains statistically insignificant. We therefore conclude that there is no obvious nonlinear effect of air pollution on mortality in HK.
Fig. 3.
Dose-response curves of the air pollution effects.
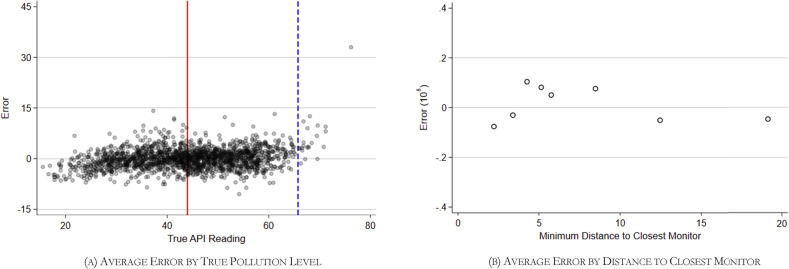
4.5. Test for non-classical measurement error
As there may exist systematic differences between districts with actual monitors and those without, there is a concern that the non-classical measurement error of air pollution could potentially bias our estimates (Lleras-Muney, 2010; Knittel et al., 2016). To address this issue, we conduct a rich set of formal tests following Knittel et al., (2016). We first predict air pollution of each HK’s air quality monitor using all other surrounding monitors within 20 miles, weighted inversely by distance. The discrepancy between each monitor’s predicted pollution level and the monitor’s actual recorded value is interpreted as the “error.” Second, to test how the “error” and its variance depend on the true pollution level and distance to the closest monitor, we run an OLS regression of the “error” on the monitor and year-month fixed effects. Third, we obtain the residuals from the previous regression and estimate a regression model where the residual is a function of the spline in true levels of pollution and distance to nearest monitors10 :
| (5) |
Fig. 4 a displays the average true pollution level versus the error. The vertical solid red line and the vertical dashed blue line indicate the mean and mean plus 2 standard deviations, respectively. We conclude from Fig. 4a that the unexplained error is small in magnitude and are not correlated with the true pollution levels. Fig. 4b presents the average errors by distance to the nearest monitor, suggesting no clear relationship between the bias or variance in the unexplained errors and the distance to the nearest monitor.
Fig. 4.
Error in assigned pollution by true pollution level and distance to closest monitor.
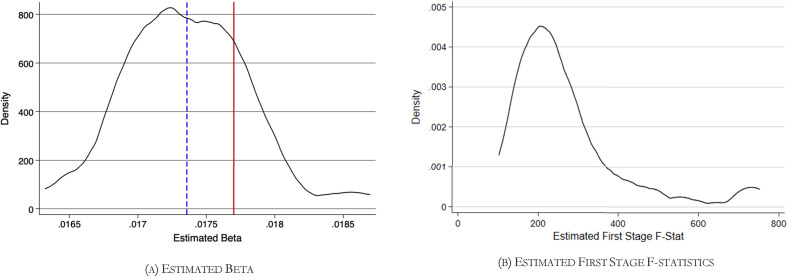
In addition, we perform a Monte Carlo simulation to further test the robustness in IV estimates according to Knittel et al. (2016). For each iteration of the simulation, we construct a ‘pseudo-pollution measure’ as each district’s air pollution level. The pseudo-pollution measure’ adds three components compared to the baseline model. In practice, each district’s ‘pseudo-pollution measure’ is constructed from the following equation:
| (6) |
where the first term represents the baseline’s matched monitor’s air quality in district i at year-month t. The other items represent the predicted errors which we obtained from the above spline analysis and an additional error component that allows for autocorrelation in errors across time within the monitor. is a draw from the standard normal distribution. We then replace our “true pollution” by the “pseudo-pollution” and estimate the baseline IV regression. We repeat this process 100 times. Fig. 5 shows the density of our simulated estimates. The dashed blue line and solid red line represent the mean value of simulated estimates and our baseline model’s estimate, respectively. Our baseline estimate (without measurement error) is 0.0177. The simulation indicates the mean estimate (with measurement errors) is 0.0174 with a range from 0.0163 to 0.0187. Pollution measurement error only increases the noise of our estimates at a very small magnitude (less than 2% of the true coefficient). These analyses suggest that the non-classical measurement error is not severe and will thus not affect our findings.
Fig. 5.
Monte Carlo results: Density of estimates and first-stage F-Statistics.
4.6. Robustness checks
We check the robustness of our main findings in several different ways and summarize our findings here. Interested readers can find a complete set of results underlying these sensitivity analyses in the online Appendix. First, some LTPUGs are located relatively far away from air quality monitoring stations and the air pollution levels in these districts may be measured with error. We exclude LTPUGs that are far away from their nearest stations and report the findings in Appendix Table S4. We use samples within 12 km, 10 km, and 8 km radius from monitoring stations and repeat the IV estimations for each subsample. We find that all the estimates are quantitatively similar. In addition, in Appendix Table S5, we use two alternative ways to match LTPUGs with air quality monitors. In Columns 1–2, each LTPUG is matched with the HK’s air quality monitoring station nearest to its centroid. In Columns 3–4, each LTPUG’s air quality is calculated as a distance-based weighted average from all HK’s air quality monitoring stations. Again, all the findings remain the same.
Second, our empirical strategy relies on the fact that HK’s local air pollution can be exogenously affected by air pollution levels in PRDEZ under different meteorological conditions. We check the robustness of the results in Appendix Table S6 by only using the local wind patterns as the instruments. Excluding the API in PRDEZ from the IV regressions can help address the potential concern that air pollution in PRDEZ may be affected by policies in HK. As shown in Appendix Table S6, doing so generates quantitatively similar results.
Third, we check whether the results still hold using alternative air pollution measures. In our data, PM10 is the primary pollutant in constructing the API 40.8% of the time during our sample period.11 Presumably, the health impact is driven mostly by the primary pollutant, so we can estimate the same set of regressions using PM10 as the air pollution measure. The results are reported in Appendix Table S7. The PRDEZ’s PM10 concentration are used as instruments in the first stage. We find that a 10 μg/m3 increase in PM10 concentration leads to a 0.94%–0.99% increase in CVR mortality rate and this effect is statistically significant at the 1% level. The relationship between PM10 and the non-CVR mortality rate, however, is statistically insignificant in all regressions. These findings are again consistent with our baseline results.
Fourth, using the same identification strategy, we can further examine the health impacts of different pollutants. The results are summarized in Appendix Table S8. Here, we estimate the pollutant-mortality relationship separately for SO2, O3, and NO2, using the PRDEZ’s respective pollutant concentrations as instruments. Among them, the effect of SO2 is statistically significant, but we do not find a statistically significant effect of O3 or NO2. These results suggest that the mortality effect of air pollution in HK is driven mostly by PM10 and SO2.
Next, we report the results at the daily, weekly, and quarterly level using the same IV strategy in Table 6 . Daily level analysis in Column 1 indicates that a 10-unit increase in daily API will lead to a 0.04% increase in CVR mortality rate. The impact at the weekly level is 0.10%, twice larger than the daily estimate (Column 2). At the monthly and quarterly level, we obtain similar coefficients (0.177 and 0.164). From daily to quarterly level analysis, we can observe an increasing trend in the estimated coefficient and the effect size stabilizes when we use monthly data. These results are consistent with the previous literature that using daily data tends to generate smaller estimates than using more aggregated data. In addition, results in Table 6 also indicate that the health impact of air pollution became larger as we use more aggregated data, suggesting harvesting effects is not going to be an important issue when assessing the air pollution effect in the medium and long run.
Table 6.
The effect of air pollution on CVR mortality rate at different time scales.
| Daily Level (1) |
Weekly Level (2) |
Monthly Level (3) |
Quarterly Level (4) |
|
|---|---|---|---|---|
| Hong Kong’s API | 0.0004∗∗∗ | 0.0010∗ | 0.0177∗∗∗ | 0.0164∗∗∗ |
| (per 10 units) | (0.0001) | (0.0005) | (0.0059) | (0.0059) |
| Week FE | Y | Y | ||
| Year-Month FE | Y | Y | Y | |
| Year-Quarter FE | Y | |||
| Year FE | ||||
| Temp and Sq. | Y | Y | Y | Y |
| Precipitation | Y | Y | Y | Y |
| LTPUG FE | Y | Y | Y | Y |
| Observations | 661,068 | 99,138 | 23,044 | 8481 |
| Number of LTPUG | 135 | 135 | 135 | 135 |
| First stage F-statistics | 44.53 | 74.35 | 183.2 | 43.68 |
| RMSE | 0.52 | 0.83 | 0.66 | 0.51 |
| R2 | 0.01 | 0.03 | 0.08 | 0.08 |
Notes: This table reports the two-stage least squares regression coefficients and standard errors. PRDEZ’s API, local wind conditions, distances to the PRDEZ and their interaction terms are used as the instrumental variables for Hong Kong’s API. The dependent variables are the logarithm of mortality rate for all cardiovascular and respiratory (CVR) deaths at different levels. Column 3 presents the results corresponding to Column 3 of Table 2. Standard errors in parentheses are clustered at the Large Tertiary Planning Unit Group (LTPUG) level. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
In Appendix Table S9, we report the OLS estimates and fixed-effects model estimates. Based on these models, we draw the following conclusions. First, the estimated effects vary greatly across different specifications. For example, if nothing is controlled for, a 10-unit increase in API is associated with a 0.92% change in the CVR mortality rate and the estimate is statistically significant at the 1% level. Adding controls and fixed effects significantly change the point estimates and the significance level. These findings suggest that associational estimates can suffer from severe omitted variable bias. Second, in the most restrictive model (i.e., Column 6), a 10-unit increase in API is associated with a 0.67% change in CVR mortality rate. This estimate is substantially smaller than the IV estimate (1.77%) in Table 2, suggesting the potential attenuation bias in the fixed-effects models. These findings are consistent with several quasi-experimental studies (e.g., Schlenker and Walker, 2015; He et al., 2016; Deryugina et al., 2019), which also find that estimates of the air pollution effects obtained using a quasi-experimental design were much larger than estimates obtained from associational approaches.
Finally, many environmental epidemiology papers use non-accidental deaths as the outcome measure. For comparison, we report the results for the non-accidental mortality rate in Appendix Table S10. We estimate that a 10-unit change in API can lead to a 1.44%–1.54% change in the monthly non-accidental mortality rate, a 10 μg/m3 increase in PM10 concentration can cause a 0.67%–0.73% increase in the outcome, and a 10 ppb increase in SO2 concentration can raise the monthly non-accidental mortality rate by 0.6%.
5. Diminishing air pollution effect
5.1. Air pollution effects over time
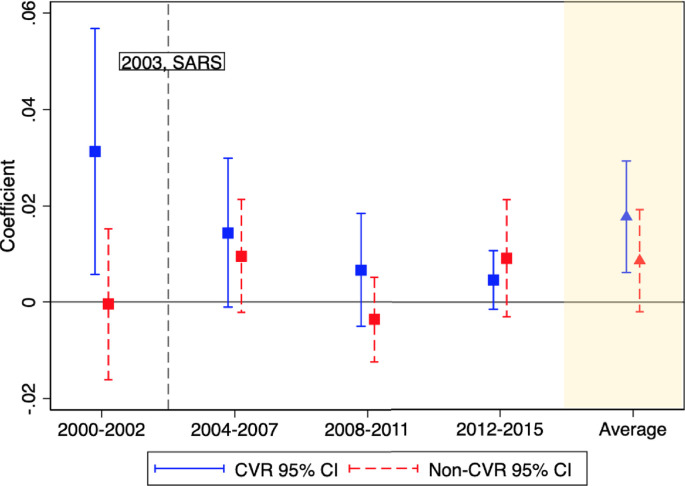
We examine the air pollution effect over time by splitting our sample into different periods: 2000 to 2002, 2004 to 2008, and 2009 to 2015.12 Fig. 6 displays the estimates with 95% confidence intervals. The baseline estimates are plotted on the left for comparison. The corresponding regression results are reported in Table 7 . In Panel A, we focus on CVR mortality. We see that the effect is the largest using 2000–2002 data: a 10-unit increase in API will lead to a 3.13% increase in the CVR mortality rate (Column 1). Using data from more recent years, we find the air pollution effect on CVR mortality rate becomes smaller and statistically insignificant (Columns 2 to 4). In other words, the air pollution effect on mortality in HK is diminishing over the years. For non-CVR mortality, all the coefficients are small in magnitude and statistically insignificant (Panel B).13
Fig. 6.
Diminishing Air Pollution Impact. Notes: The square dots represent the estimated impacts of a 10-point increase in the API on CVR mortality and non-CVR mortality using data from different periods. The vertical lines represent the corresponding 95% confidence intervals.
Table 7.
Diminishing air pollution effect.
| Before SARS |
After SARS |
|||
|---|---|---|---|---|
| (1) 2000–2002 |
(2) 2004–2007 |
(3) 2008–2011 |
(4) 2012–2015 |
|
| Panel A. CVR Mortality, log(per 10 units) | ||||
| Hong Kong’s API | 0.0313∗∗ | 0.0144∗ | 0.0067 | 0.0046 |
| (0.0130) | (0.0079) | (0.0060) | (0.0031) | |
| Panel B. Non-CVR Mortality, log(per 10 units) | ||||
| Hong Kong’s API | −0.0004 | 0.0096 | −0.0036 | 0.0091 |
| (0.0080) | (0.0060) | (0.0045) | (0.0062) | |
| Temp and Sq. | Y | Y | Y | Y |
| Precipitation | Y | Y | Y | Y |
| Year-month FE | Y | Y | Y | Y |
| LTPUG FE | Y | Y | Y | Y |
| Observations | 3960 | 6310 | 6375 | 6399 |
| Number of LTPUG | 134 | 135 | 134 | 134 |
Notes: This table reports the two-stage least squares regression coefficients and standard errors. PRDEZ’s API, local wind conditions, distances to the PRDEZ and their interaction terms are used as the instrumental variables for Hong Kong’s API. The dependent variables are the logarithm of monthly mortality rate for cardiovascular and respiratory (CVR) and Non-CVR deaths for the 4 periods: 2000 to 2002, 2004 to 2007, 2008 to 2011, and 2012 to 2015. The year of SARS outbreak, 2003, is excluded as the daily life of citizens, and hence exposure to air pollution could be affected tremendously. Standard errors in parentheses are clustered at the Large Tertiary Planning Unit Group (LTPUG) level. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
We choose the Year 2003 as the point to split the sample because many factors that affect population health in HK, especially the healthcare infrastructure, were drastically changed after the 2003 SARS epidemic. The SARS epidemic started in the Guangdong province of China and spread to HK in February 2003. It differed from previous epidemic infectious diseases in its explosive spread, which caught the health and hospital authorities by surprise. Before it was contained in late June 2003, there were over 1700 cases of SARS infections in HK, resulting in 299 deaths.14
The SARS epidemic in HK caused broad social, economic, and humanitarian repercussions (Hung, 2003; Siu and Wong, 2004). Particularly, it unveiled some basic failings of HK’s healthcare system, including overcrowded wards, poor ventilation in some hospitals, lack of isolation facilities, inadequate intensive care facilities, and difficulty in isolating and cohorting patients with suspected SARS infection (Hung, 2003). Following the SARS, numerous healthcare improvements were carried out. For example, after reviewing the medical practices at the time, the Hospital Authority (HA) of HK built additional isolation beds, revamped the Intensive Care Units (ICU), rationalized existing beds, adopted a series of infection control practices, and launched massive staff training programs. The HA also worked closely with the HK Government to construct longer-term isolation facilities and set over 200 improvement targets at the beginning of 2004. In addition, the Centre for Health Protection was established to deal with public health issues and to help prevent communicable and non-communicable diseases. Since pneumonia is one of the leading causes of death in HK, various improvement measures were also adopted to reduce the transmission of respiratory diseases.
In addition, the HA enhanced community-based services and paid particular attention to the vulnerable groups, including the elderly. Several community-based teams, including Community Nursing Service, Community Geriatric Assessment, and Community Psychiatric Teams, were established. The provision of community-based healthcare among the elderly population has increased rapidly since 2003 (see Appendix Fig. S4). After 2003, HA also launched a Visiting Medical Officer Scheme, which provided outreach, medical consultation, and after-care services to residential care homes for the elderly, introduced Family Medicine practice in clinics, and enlarged the proportion of doctors undergoing training in community care.
These changes have significantly improved the availability of quality medical services in HK and are considered an important contributor to longevity in HK. While it is difficult to demonstrate empirically that the improvement in healthcare availability and quality (which are difficult to measure) causally mitigated the effect of air pollution on mortality, we believe this channel is highly likely. Below, we offer additional supporting evidence for this argument and try to rule out several alternative explanations.
5.2. Access to emergency services and the air pollution effect
A large number of medical studies have shown that air pollution often triggers acute cardiovascular diseases, such as strokes and heart attacks (see Mustafić et al., 2012; Shah et al., 2013; Cohen et al., 2017 for recent reviews). Air pollution also damages the immune system and increases the risk of various respiratory diseases, such as acute upper respiratory tract infections. When one’s life is threatened by such acute diseases, immediate access to emergency care is critical. For example, if a patient is struck by acute ischemic stroke, the treatment modality is highly time-dependent and better outcomes can only be achieved when treatment is administered soon enough. Treatment within 60 min of symptom onset, known as the Golden Hour, can produce desirable health outcomes with significantly lower rates of morbidity and mortality (Ebinger et al., 2015). As a result, we conjecture that access to immediate emergency care and the quality of healthcare service may have important implications for the air pollution effect.
Hong Kong has stunningly efficient emergency services, in which the ambulance service is almost free and pledged to arrive at the patient’s address within 12 min upon request. In 2014, for example, the total number of ambulance transportations was more than 20,000, with 95% of them arriving in less than 12 min.15 Whether a patient can receive immediate healthcare thus largely depends on the distance between the patient’s address and the nearby hospital. In light of this, we explore the heterogeneity of the air pollution effect based on whether an LTPUG has immediate access to a hospital with an Accident and Emergency (A&E) service. In HK, 20 hospitals provide A&E services and the locations of these hospitals did not change during our sample period. We generate 2-km buffer zones surrounding all the hospitals with A&E services and compare the air pollution effects for LTPUGs that are located within and outside those buffer zones. We use the 2-km buffer zone because it roughly divides all the LTPUGs into two groups with equal sample sizes (Appendix Fig. S5).16
Table 8 summarizes our findings separately for these two groups. Columns 1 and 2 report the results for districts located within the 2 km radius of A&E services and Columns 3 and 4 report the results for districts located outside the radius. The estimates are statistically insignificant for both CVR and non-CVR mortality rates in Columns 1 and 2, suggesting that air pollution is less likely to kill people in districts with A&E services. In contrast, air pollution has a statistically significant impact on CVR mortality for people living far away from hospitals with A&E services. These results suggest that easy access to emergency medical services can reduce pollution-related deaths, which are consistent with our argument that the availability of high-quality medical service is important for mitigating the air pollution effect. In addition, we check the robustness by varying the buffer zones of A&E services to 1.5 km and 3 km and report the results in Appendix Table S11. The estimates are quantitatively similar and indicate the same pattern that closer to A&E services is associated with less mortality from air pollution.
Table 8.
Availability of accident and emergency (A&E) services in hospitals and the air pollution effect.
| A&E Hospitals within 2 km |
No A&E Hospitals within 2 km |
|||
|---|---|---|---|---|
| (1) CVR, log |
(2) Non-CVR, log |
(3) CVR, log |
(4) Non-CVR, log |
|
| (per 10 units) | ||||
| Hong Kong’s API | 0.0070 | 0.0038 | 0.0251∗∗∗ | 0.0134 |
| (0.0060) | (0.0063) | (0.0090) | (0.0083) | |
| Temp and Sq. | Y | Y | Y | Y |
| Precipitation | Y | Y | Y | Y |
| Year-month FE | Y | Y | Y | Y |
| LTPUG FE | Y | Y | Y | Y |
| Observations | 12,057 | 12,057 | 10,987 | 10,987 |
| Number of LTPUG | 71 | 74 | 64 | 64 |
| RMSE | 0.60 | 0.55 | 0.71 | 0.65 |
| R2 | 0.10 | 0.05 | 0.07 | 0.03 |
Notes: This table reports the two-stage least squares regression coefficients and standard errors. PRDEZ’s API, local wind conditions, distances to the PRDEZ and their interaction terms are used as the instrumental variables for Hong Kong’s API. The dependent variables are the logarithm of monthly mortality rate for all cardiovascular and respiratory (CVR) deaths and non-CVR deaths. Columns 1–2 and 3–4 show estimates for the population who lives within and outside the 2 km zone to hospitals with A&E services respectively. Standard errors in parentheses are clustered at the Large Tertiary Planning Unit Group (LTPUG) level. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
In Appendix Table S12, we also separately examine the impacts of air pollution and A&E services over time. The results show that the impacts of air pollution on populations with easier access to A&E services remain statistically insignificant during the entire period of time. For regions with A&E services outside 2 km, however, the impact has reduced from 7.00% to 1.47% and becomes statistically insignificant at the end of the period.
5.3. Other explanations
In this section, we discuss several alternative explanations for the declining air pollution effect, including a potential non-linear dose-response relationship between air pollution and health, smoking, and people’s avoidance behavior in response to pollution.
First, it is unlikely that the nonlinearity of the air pollution effect drives our main findings. As shown in Appendix Fig. S7, the API in HK was between 40 and 50 during most of the time and there were no dramatic improvements or deteriorations in air quality in Hong Kong during the sample period. Particularly, the API between 2000 and 2002, during which we find the largest air pollution effect, was not very different from the later periods (e.g. 2004 to 2007). This result suggests that the diminishing air pollution effect is not driven by changes in air pollution levels.
Second, existing literature also suggests that smokers can be more sensitive to air pollution, in that they have a higher relative risk of all-cause mortality, cardiopulmonary mortality, and lung cancer (Hoek et al., 2002; Pope III et al., 2002; Hamra et al., 2015). This argument is often used to explain the finding that males are more likely to die from air pollution than females. If this argument were true and if there were fewer and fewer smokers over the years, the air pollution effect could decrease. To examine this hypothesis, we collect data from the HK Government and compare the smoking population over time. We find that, somewhat to our surprise, the percentage of smokers has remained almost unchanged during the entire period (see data in Appendix Table S13 and Appendix Fig. S8). In other words, it is also unlikely that smoking is contributing to the diminishing air pollution effect.
The last hypothesis is that people’s awareness of air pollution might have increased over the years, so more people adopt avoidance behaviors against air pollution. In the literature, studies find that people take actions to avoid exposure to air pollution (e.g., Neidell, 2004; Neidell, 2009; Zhang and Mu, 2018; Liu et al., 2018; Ito and Zhang, 2020). To test this hypothesis, we collect data from Google Trends and examine how air pollution is correlated with online searches for keywords related to “air pollution.”
The results are reported in Table 9 . In Panel A, we see that API is not statistically significantly associated with the search volumes for PM2.5, PM10, or API but is positively associated with search volume for air pollution. These results suggest people’s knowledge about air pollution is relatively limited and thus do not dig into the technical terms describing specific air pollutants. In Panels B and C, we show that the associations between API and people’s searches for air pollution are stable in all the years during which the Google Trends data are available, suggesting that HK people’s responses to air pollution do not change much over time.
Table 9.
Air pollution and avoidance behaviors.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Panel A. The Associations between API and Avoidance Measures | |||||
| Search for “PM2.5" (Log) | Search for “PM10” (Log) | Search for “API” (Log) | Search for “Air Pollution” (Log) | Search for “Air Pollution (in Chinese)" (Log) | |
| Hong Kong’s API (per 10 units) |
0.38 | 6.63 | 2.35 | 25.2∗∗∗ | 28.1∗∗∗ |
| (6.10) | (4.16) | (1.63) | (5.62) | (6.59) | |
| Sample | 2004–2015 | 2004–2015 | 2004–2015 | 2004–2015 | 2004–2015 |
| Observations | 144 | 144 | 144 | 144 | 144 |
| R2 | 0.00 | 0.03 | 0.01 | 0.30 | 0.16 |
| Panel B. The Associations between API and Search Index for “Air Pollution” (Log) | |||||
| Hong Kong’s API (per 10 units) |
29.3∗∗∗ | 21.0∗∗∗ | 26.7∗∗∗ | 23.7∗∗∗ | 25.2∗∗∗ |
| (1.16) | (3.43) | (7.66) | (5.60) | (5.62) | |
| Sample | 2004–2006 | 2007–2009 | 2010–2012 | 2013–2015 | 2004–2015 |
| Observations | 36 | 36 | 36 | 36 | 144 |
| R2 | 0.28 | 0.38 | 0.38 | 0.46 | 0.30 |
| Panel C. The Associations between API and Search Index for “Air Pollution (in Chinese)" (Log) | |||||
| Hong Kong’s API (per 10 units) |
51.3∗∗∗ | 24.5∗∗∗ | 24.3∗∗ | 20.4∗∗∗ | 28.1∗∗∗ |
| (12.1) | (7.28) | (10.5) | (3.88) | (6.59) | |
| Sample | 2004–2006 | 2007–2009 | 2010–2012 | 2013–2015 | 2004–2015 |
| Observations | 36 | 36 | 36 | 36 | 144 |
| R2 | 0.21 | 0.19 | 0.24 | 0.45 | 0.16 |
Notes: This table reports the OLS regression results. The independent variable is the average API in Hong Kong and the dependent variables are the Google Trends for different keywords. Google Trends points range from 0 to 100, with a higher score indicating more online searches. We use data from 2004 to 2015, as Google Trends data only became available since 2004. Standard errors are reported in the parentheses. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
In Table 10 , we further examine the relationship between API and searches for air pollution-related avoidance measures. The regression results show that, while people are to some extent aware of air pollution, this awareness does not lead to meaningful avoidance behaviors. In particular, there is no correlation between API and searches for masks and air purifiers, the two most commonly used defensive measures against air pollution. We also use HK’s search volume for watching films as a way to measure indoor activities and again see no correlation. Therefore, we conclude that people in HK adopt minimal avoidance behaviors against air pollution, so the diminishing air pollution effect cannot be driven by awareness or avoidance of air pollution.17 These patterns are different from what we observe in mainland Chinese cities, in which people search for and buy more masks and air filters when air quality is bad (Zhang and Mu, 2018; Liu et al., 2018; Ito and Zhang, 2020).
Table 10.
Air pollution and other measures of avoidance behaviors.
| Search for “Mask" |
Search for “Mask (Chinese)" |
Search for “Air Purifier" |
Search for “Air Purifier (Chinese)" |
Search for “Film" |
Search for “Film (Chinese)” |
|
|---|---|---|---|---|---|---|
| (1) % |
(2) % |
(3) % |
(4) % |
(5) % |
(6) % |
|
| Hong Kong’s API (per 10 units) |
−0.75 | −3.63 | 1.91 | 0.20 | 1.65 | −2.25 |
| (1.82) | (9.32) | (3.70) | (10.00) | (1.14) | (2.30) | |
| Observations | 144 | 144 | 144 | 144 | 144 | 144 |
| R2 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.00 |
Notes: This table reports the OLS regression results. The independent variable is the average API in Hong Kong and the dependent variables are the Google Trends indices for different keywords. Google Trends indices range from 0 to 100, with a higher score indicating more online searches. We use data from 2004 to 2015, as Google Trends data only became available since 2004. Standard errors are reported in the parentheses. ∗∗∗ p < 0.01, ∗∗p < 0.05, ∗p < 0.1.
6. Conclusion
In many metropolitan cities in the developing world, income levels are rising quickly, while air pollution levels remain high. HK offers a future scenario for these cities as it has a high level of income, yet faces severe air pollution. In this study, we estimate the causal effect of air pollution on mortality using 16 years of data from in HK. To address the endogeneity problem, we use an instrumental variable approach based on transboundary air pollution from mainland China. Our analyses show that a 10-unit increase in the API will cause a 1.77% increase in the monthly cardio-respiratory mortality rate and the elderly are particularly vulnerable to air pollution.
The key finding in this study is that the effect of air pollution on mortality has dramatically declined and becomes statistically insignificant after the SARS epidemic in 2003. We argue that medical improvement initiatives and the development of community-based services implemented after SARS are likely to drive the declining air pollution effect. Empirically, we show people with immediate access to emergency healthcare are less susceptible to air pollution in comparison to those without, and the diminishing impacts are not driven by several alternative explanations. As pre-mature deaths are considered as the largest social cost of air pollution (other costs include morbidity, reduced productivity, etc.), our findings suggest that better socio-economic conditions and a well-functioning medical system can help reduce the damage of air pollution, at least in the short run. Governments and policymakers should thus consider the role of healthcare when formulating air pollution policies.
There are three caveats in this study. First, while a diminishing effect of air pollution on mortality is observed, it does not mean that air pollution becomes less important in HK. The long-term effects of air pollution on mortality and morbidity remain poorly understood. Second, while the heterogeneity results between districts with and without immediate A&E services suggest quality medical service can be important, this finding does not have a causal interpretation. To what extent the A&E services causally affect the air pollution-mortality relationship requires exogenous changes in the A&E service availability, which is missing in this study. Finally, the API is a comprehensive air quality measure and is determined by the pollutant with the highest concentration level in the standard. Our analyses do not identify which between which pollutants are more health-damaging and tell little about how the interactions of different air pollutants can affect human health. Further studies are needed to investigate these issues.
Acknowledgment
We are indebted to the Editor, Roger H. von Haefen, and two anonymous referees for their valuable suggestions. We thank Jimmy Fung, Seema Jayachandra, Alexis Lau, Yatang Lin, Jay Shimshack, and Jian Zhen Yu for helpful comments. Financial supports from the University Grants Committee of HK (General Research Fund, Project No. 16500617) are gratefully acknowledged. All the remaining errors are ours.
Footnotes
The GDP per capita of the HK is 46,000 USD as of 2017. Source: https://www.ceicdata.com/en/indicator/hong-kong/gdp-per-capita.
The API is a comprehensive measure of air pollution and is adopted by HK and mainland China. The index is constructed by PM10, SO2, CO, O3, and NO2 concentrations and readers can find the details of constructing API in the Data section.
“One Country, Two Systems” is a constitutional principle formulated by Deng Xiaoping to accomplish the peaceful reunification of China by resolving the sovereignty questions of Hong Kong, Macao and perhaps Taiwan arising from a complicated historical background. Under the principle, mainland China adopts the socialism with Chinese characteristics system, while Hong Kong and Macao have their own governmental systems, legal, economic and financial affairs.
The PM2.5 concentrations are derived from Aerosol Optical Depth (AOD) satellite data using the GEOS-Chem chemical transport model (van Donkelaar et al., 2014). The AOD data are extracted from the National Aeronautics and Space Administration (NASA) of the United States. For illustrative purposes, we use data from 2006 in Fig. 1.
According to the HK government, local emission sources mainly include motor vehicles, marine vessels, and power plants. Details can be found at https://www.gov.hk/en/residents/environment/air/airquality.htm.
Wind data are categorized into eight wind directions: 0° (north wind), 45° (northeast wind), 90° (east wind), 135° (southeast wind), 180° (south wind), 225° (southwest wind), 270° (west wind), and 315° (northwest wind). In practice, wind direction of 315° is dropped to avoid collinearity. The classification of wind directions is shown in Appendix Fig. S1.
There are six other air pollution monitoring stations in Hong Kong. One of them is located far away from the city and measures the background air quality, two were built after the study period, and the rest measure roadside air pollution.
More details about API can be found in He et al. (2016).
The knot points for linear splines are at mile distance of 3, 6, 9, 12, and 15 miles, and the API units of 20, 32, 44, 56, and 68.
PM10 contributes most of the primary pollution in API construction during our sample period. The contributions of other pollutants are: PM2.5 (22.6%), CO (0.4%), NO2 (36.0%), O3 (0.1%), and SO2 (0.0%).
Year 2003 data are dropped from this analysis because several hundred people died from SARS, but these deaths are unrelated to air pollution.
We further examine whether the diminishing effects could be driven by the changes in unexplained errors because of the non-classical measurement errors. To do so, we apply the tests on non-classical measurement errors for different time periods. The distribution of the errors is displayed in Fig. S6 where the division of different time periods is the same as Table 7. The distribution patterns in both density and box graphs indicate that the unexplained error is uncorrelated with time.
Source: World Health Organization: http://www.who.int/csr/sars/country/2003_07_04/en/.
In Appendix Fig. S5, we observe that both groups of LTPUGs are dispersed equally in different areas of HK and are equally close to subway (the Massive Transport Railway) stations.
These findings are consistent with some earlier studies. For example, DeGolyer (2008) conducted two surveys in 2000 and 2008 to understand HK residents’ awareness of air pollution. In the survey, people were explicitly asked whether they were concerned with air pollution; the share of people worrying about air pollution remained very similar in both surveys.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jeem.2020.102316.
Contributor Information
Chun Wai Cheung, Email: cwcheungad@connect.ust.hk.
Guojun He, Email: gjhe@me.com.
Yuhang Pan, Email: yhyhpan@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abbey David E., Nishino Naomi, McDonnell William F. Long-term inhalable particles and other air pollutants related to mortality in nonsmokers. Am. J. Respir. Crit. Care Med. 1999;159(2):373–382. doi: 10.1164/ajrccm.159.2.9806020. [DOI] [PubMed] [Google Scholar]
- Anderson Michael L. As the wind blows: the effects of long-term exposure to air pollution on mortality. J. Eur. Econ. Assoc. 2019 doi: 10.1093/jeea/jvz051. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arceo Eva, Hanna Rema, Oliva Paulina. Does the effect of pollution on infant mortality differ between developing and developed countries? Evidence from Mexico city. Econ. J. 2016;126(591):257–280. [Google Scholar]
- Aunan Kristin, Pan Xiao-Chuan. Exposure-response functions for health effects of ambient air pollution applicable for China: a meta-analysis. Sci. Total Environ. 2004;329(1):3–16. doi: 10.1016/j.scitotenv.2004.03.008. [DOI] [PubMed] [Google Scholar]
- Becklake Margaret R., Francine Kauffmann. Gender differences in airway behaviour over the human life span. Thorax. 1999;54(12):1119–1138. doi: 10.1136/thx.54.12.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell Michelle L., McDermott Aidan, Zeger Scott L. Ozone and short-term mortality in 95 US urban communities, 1987-2000. J. Am. Med. Assoc. 2004;292(19):2372–2378. doi: 10.1001/jama.292.19.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett Richard T., Pope III C. Arden, Ezzati Majid. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ. Health Perspect. 2014;122(4):397–403. doi: 10.1289/ehp.1307049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron Colin A., Gelbach Jonah B., Miller Douglas L. Robust inference with multiway clustering. J. Bus. Econ. Stat. 2011;29(2):238–249. [Google Scholar]
- Cao Jie, Yang Chunxue, Li Jianxin. Association between long-term exposure to outdoor air pollution and mortality in China: a cohort study. J. Hazard Mater. 2011;186(2–3):1594–1600. doi: 10.1016/j.jhazmat.2010.12.036. [DOI] [PubMed] [Google Scholar]
- Cesur Resul, Tekin Erdal, Ulker Aydogan. Air pollution and infant mortality: evidence from the expansion of natural gas infrastructure. Econ. J. 2017;127(600):330–362. [Google Scholar]
- Chay Kenneth Y., Greenstone Michael. 2003. “Air Quality, Infant Mortality, and the Clean Air Act of 1970.” NBER Working Paper. [Google Scholar]
- Chay Kenneth Y., Greenstone Michael. The impact of air pollution on infant mortality: evidence from geographic variation in pollution shocks induced by a recession. Q. J. Econ. 2003;118(3):1121–1167. [Google Scholar]
- Chen Yuyu, Ebenstein Avraham, Greenstone Michael, Li Hongbin. Evidence on the impact of sustained exposure to air pollution on life expectancy from chinas Huai River policy. Proc. Natl. Acad. Sci. Unit. States Am. 2013;110(32):12936–12941. doi: 10.1073/pnas.1300018110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty Jane E. A growing role for gender analysis in air pollution epidemiology. Environ. Health Perspect. 2009;118(2):167–176. doi: 10.1289/ehp.0900994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa Amine Farias. Air pollution and deaths among elderly residence of São paulo, Brazil: an analysis of mortality displacement. Environ. Health Perspect. 2017;125:349–354. doi: 10.1289/EHP98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A.J. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet. 2017;389(10082):1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colmer Jonathan, Lin Dajun, Liu Siying, Shimshack Jay P. ” Working Paper; 2019. Can growth conquer all? The pollution-mortality relationship in high-income, high-pollution Hong Kong. [Google Scholar]
- Currie Janet, Neidell Matthew J. “Air pollution and infant health: what can we learn from California’s recent experience? Q. J. Econ. 2005;120(3):1003–1030. [Google Scholar]
- Currie Janet, Neidell Matthew J., Schmieder Johannes F. Air pollution and infant health: lessons from New Jersey. J. Health Econ. 2009;28(3):688–703. doi: 10.1016/j.jhealeco.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie Janet, Reed Walker. Traffic congestion and infant health: evidence from E-ZPass. Am. Econ. J. Appl. Econ. 2011;3(1):65–90. [Google Scholar]
- DeGolyer Michael E. Environment & Public Health; ”: 2008. Hong Kong’s Silent Epidemic: Public Opinion Survey on Air Pollution. [Google Scholar]
- Deryugina Tatyana, Heutel Garth, Miller Nolan H., Molitor David, Reif Julian. The Mortality and Medical Costs of Air Pollution: Evidence from Changes in Wind Direction. American Economic Review. 2019;109(12):4178–4219. doi: 10.1257/aer.20180279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dockery Douglas W., Pope III C. Arden, Xu Xiping. An association between air pollution and mortality in six U.S. Cities. N. Engl. J. Med. 1993;329:1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- Ebenstein Avraham, Fan Maoyong, Greenstone Michael, He Guojun, Zhou Maigeng. New evidence on the impact of sustained exposure to air pollution on life expectancy from chinas Huai River policy. Proc. Natl. Acad. Sci. Unit. States Am. 2017;114(39):10384–10389. doi: 10.1073/pnas.1616784114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebenstein Avraham, Fan Maoyong, Greenstone Michael, He Guojun, Yin Peng, Zhou Maigeng. Growth, pollution, and life expectancy: China from 1991-2012. Am. Econ. Rev. 2015;105(5):226–231. [Google Scholar]
- Ebinger Martin, Kunz Alexander, Wendt Matthias. Effects of golden Hour thrombolysis: a prehospital acute neurological treatment and optimization of medical care in stroke (phantom-S) substudy. JAMA Neurology. 2015;72(1):25–30. doi: 10.1001/jamaneurol.2014.3188. [DOI] [PubMed] [Google Scholar]
- Evans J.S., Tosteson T., Kinney P.L. Cross-sectional mortality studies and air pollution risk assessment. Environ. Int. 1984;10(1):55–83. [Google Scholar]
- Galizia Audrey, Kinney Patrick L. Long-term residence in areas of high ozone: associations with respiratory health in a nationwide sample of nonsmoking young adults. Environ. Health Perspect. 1999;107(8):675–679. doi: 10.1289/ehp.99107675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Yang, Chan Emily YY., Li Liping. Chronic effects of ambient air pollution on respiratory morbidities among Chinese children: a cross-sectional study in Hong Kong. BMC Publ. Health. 2014;14:105. doi: 10.1186/1471-2458-14-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graff Zivin Joshua, Neidell Matthew. The impact of pollution on worker productivity. Am. Econ. Rev. 2012;102(7):3652–3673. doi: 10.1257/aer.102.7.3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graff Zivin Joshua, Neidell Matthew. Environment, health, and human capital. J. Econ. Lit. 2013;51(3):689–730. [Google Scholar]
- Greenstone Michael, Hanna Rema. Environmental regulations, air and water pollution, and infant mortality in India. Am. Econ. Rev. 2014;104(10):3038–3072. [Google Scholar]
- Hamra Ghassan B., Guha Neela, Cohen Aaron. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ. Health Perspect. 2015;122(9):906–911. doi: 10.1289/ehp/1408092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Guojun, Fan Maoyong, Zhou Maigeng. The effect of air pollution on mortality in China: evidence from the 2008 beijing olympic games. J. Environ. Econ. Manag. 2016;79:18–39. [Google Scholar]
- Hoek Gerard, Brunekreef Bert, Goldbohm Sandra. Association between mortality and indicators of traffic-related air pollution in The Netherlands: a cohort study. Lancet. 2002;360(9341):1203–1209. doi: 10.1016/S0140-6736(02)11280-3. [DOI] [PubMed] [Google Scholar]
- Hung Lee Shiu. The SARS epidemic in Hong Kong: what lessons have we learned? J. R. Soc. Med. 2003;96(8):374–378. doi: 10.1258/jrsm.96.8.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito Koichiro, Zhang Shuang. Willingness to pay for clean air: evidence from air purifier markets in China. J. Polit. Econ. 2020 In press. [Google Scholar]
- Jayachandran Seema. Air quality and early-life mortality: evidence from Indonesia’s wildfires. J. Hum. Resour. 2009;44(4):916–954. [Google Scholar]
- Jia Ruixue, Ku Hyejin. Is chinas pollution the culprit for the choking of South Korea? Evidence from the asian dust. Econ. J. 2019;129(624):3154–3188. [Google Scholar]
- Knittel Christopher R., Miller Douglas L., Sanders Nicholas J. Caution, drivers! Children present: traffic, pollution, and infant health. Rev. Econ. Stat. 2016;98(2):350–366. [Google Scholar]
- Ko F.W.S., Tam W., Wong T.W., Lai C.K.W. Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clin. Exp. Allergy. 2007;37(9):1312–1319. doi: 10.1111/j.1365-2222.2007.02791.x. [DOI] [PubMed] [Google Scholar]
- Lai Hak-Kan, Tsang Hilda, Wong Chit-Ming. Meta-analysis of adverse health effects due to air pollution in Chinese populations. BMC Publ. Health. 2013;13(1):360. doi: 10.1186/1471-2458-13-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau Alexis, Lo Andrew, Gray Joe. HKUST and Civic Exchange; 2007. Relative Significance of Local vs. Regional Sources: Hong Kongs Air Pollution. [Google Scholar]
- Levy Jonathan I., Diez David, Dou Yiping. A meta-analysis and multisite time-series analysis of the differential toxicity of major fine particulate matter constituents. Am. J. Epidemiol. 2012;175(11):1091–1099. doi: 10.1093/aje/kwr457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Tong, He Guojun, Lau Alexis. Avoidance behavior against air pollution: evidence from online search indices for anti-pm2.5 masks and air filters in Chinese cities. Environ. Econ. Pol. Stud. 2018;20:325–363. [Google Scholar]
- Lleras-Muney Adriana. The needs of the army: using compulsory relocation in the military to estimate the effect of air pollutants on childrens health. J. Hum. Resour. 2010;45(3):549–590. [Google Scholar]
- Luechinger Simon. Air pollution and infant mortality: a natural experiment from power plant desulfurization. J. Health Econ. 2014;37:219–231. doi: 10.1016/j.jhealeco.2014.06.009. [DOI] [PubMed] [Google Scholar]
- Lu Feng, Xu Dongqun, Cheng Yibin. Systematic review and meta-analysis of the adverse health effects of ambient PM2.5 and PM10 pollution in the Chinese population. Environ. Res. 2015;136:196–204. doi: 10.1016/j.envres.2014.06.029. [DOI] [PubMed] [Google Scholar]
- McCracken John P. Chimney stove intervention to reduce long-term wood smoke exposure lowers blood pressure among Guatemalan women. Environ. Health Perspect. 2007;115(7):996–1001. doi: 10.1289/ehp.9888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustafić Hazrije. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. J. Am. Med. Assoc. 2012;307(7):713–721. doi: 10.1001/jama.2012.126. [DOI] [PubMed] [Google Scholar]
- Neidell Matthew J. Air pollution, health, and socio-economic status: the effect of outdoor air quality on childhood asthma. J. Health Econ. 2004;23(6):1209–1236. doi: 10.1016/j.jhealeco.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Neidell Matthew J. Information, avoidance behavior, and health: the effect of ozone on asthma hospitalizations. J. Hum. Resour. 2009;44(2):450–478. [Google Scholar]
- Pope III C. Arden, Burnett Richard T. Confounding in air pollution epidemiology: the broader context. Epidemiology. 2007;18(4):424–426. doi: 10.1097/EDE.0b013e318065c008. [DOI] [PubMed] [Google Scholar]
- Pope III C. Arden, Burnett Richard T., Thun Michael J., Calle Eugenia E., Krewski Daniel, Ito Kazuhiko, Thurston George D. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. J. Am. Med. Assoc. 2002;287(9):1132–1141. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope III C. Arden, Thun Michael J., Namboodiri Mohan M. Particulate air pollution as a predictor of mortality in a prospective study of U.S. Adults. Am. J. Respir. Crit. Care Med. 1995;151(3):669–674. doi: 10.1164/ajrccm/151.3_Pt_1.669. [DOI] [PubMed] [Google Scholar]
- Qiu Hong, Schooling C. Mary, Sun Shengzhi. Long-term exposure to fine particulate matter air pollution and type 2 diabetes mellitus in elderly: a cohort study in Hong Kong. Environ. Int. 2018;113:350–356. doi: 10.1016/j.envint.2018.01.008. [DOI] [PubMed] [Google Scholar]
- Qiu Hong, Sun Shengzhi, Tsang Hilda. Fine particulate matter exposure and incidence of stroke: a cohort study in Hong Kong. Neurology. 2017;88(18):1709–1717. doi: 10.1212/WNL.0000000000003903. [DOI] [PubMed] [Google Scholar]
- Qiu Hong, Yu Ignatius Tak-sun, Tian Linwei. Effects of coarse particulate matter on emergency hospital admissions for respiratory diseases: a time-series analysis in Hong Kong. Environ. Health Perspect. 2012;120(4):572–576. doi: 10.1289/ehp.1104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlenker Wolfram, Walker Reed. Airports, air pollution, and contemporaneous health. Rev. Econ. Stud. 2015;83(2):768809. [Google Scholar]
- Schwartz J. Harvesting and long term exposure effects in the relation between air pollution and mortality. Am. J. Epidemiol. 2000;151(5):440–448. doi: 10.1093/oxfordjournals.aje.a010228. [DOI] [PubMed] [Google Scholar]
- Shah Anoop SV. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet. 2013;382(9897):1039–1048. doi: 10.1016/S0140-6736(13)60898-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang Yu, Sun Zhiwei, Cao Junji, Wang Xinming, Zhong Liuju, Bi Xinhui, Hong Li, Liu Wenxin, Zhu Tong, Huang Wei. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013;54:100–111. doi: 10.1016/j.envint.2013.01.010. [DOI] [PubMed] [Google Scholar]
- Siu Alan, Wong Y.C. Richard. Economic impact of SARS: the case of Hong Kong. Asian Econ. Pap. 2004;3(1):62–83. [Google Scholar]
- Stieb David M., Judek Stan, Burnett Richard T. Meta-analysis of time-series studies of air pollution and mortality: effects of gases and particles and the influence of cause of death, age, and season. J. Air Waste Manag. Assoc. 2002;52(4):470–484. doi: 10.1080/10473289.2002.10470794. [DOI] [PubMed] [Google Scholar]
- Tanaka Shinsuke. Environmental regulations on air pollution in China and their impact on infant mortality. J. Health Econ. 2015;42:90–103. doi: 10.1016/j.jhealeco.2015.02.004. [DOI] [PubMed] [Google Scholar]
- van Donkelaar Aaron, Martin Randall V., Brauer Michael, Boys Brian L. Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environ. Health Perspect. 2014;123(2):135–143. doi: 10.1289/ehp.1408646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wansbeek Tom, Meijer Erik. Measurement error and latent variables. A Companion to Theoretical Econometrics. 2001:162–179. [Google Scholar]
- Wong Chit-Ming, Ma Stefan, Hedley Anthony Johnson. Effect of air pollution on daily mortality in Hong Kong. Environ. Health Perspect. 2001;109(4):335–340. doi: 10.1289/ehp.01109335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong Chit-Ming, Tam WS, Yu TS, Wong AH. Associations between daily mortalities from respiratory and cardiovascular diseases and air pollution in Hong Kong, China. Occup. Environ. Med. 2002;59:30–35. doi: 10.1136/oem.59.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Dongwei, Fung Jimmy Chi Hung, Yao Teng, Lau Alexis Kai Hon. A study of control policy in the Pearl River Delta region by using the particulate matter source apportionment method. Atmos. Environ. 2013;76:147–161. [Google Scholar]
- Yuan Zibing, Lau Alexis Kai Hon, Zhang Hongyi, Yu Jian Zhen, Louie Peter K.K., Fung Jimmy C.H. Identification and spatiotemporal variations of dominant PM10 sources over Hong Kong. Atmos. Environ. 2006;40(10):1803–1815. [Google Scholar]
- Zanobetti Antonella. Generalized additive distributed lag models: quantifying mortality displacement. Biostatistics. 2000;1(3):279–292. doi: 10.1093/biostatistics/1.3.279. [DOI] [PubMed] [Google Scholar]
- Zanobetti Antonella. The temporal pattern of mortality responses to air pollution: a multicity assessment of mortality displacement. Epidemiology. 2002;13(1):87–93. doi: 10.1097/00001648-200201000-00014. [DOI] [PubMed] [Google Scholar]
- Zanobetti Antonella, Schwartz Joel. Mortality displacement in the association of ozone with mortality: an analysis of 48 cities in the United States. Am. J. Respir. Crit. Care Med. 2008;177:184–189. doi: 10.1164/rccm.200706-823OC. [DOI] [PubMed] [Google Scholar]
- Zeger Scott L., Dominici Francesca, Samet Jonathan. harvesting-resistant estimates of air pollution effects on mortality. Epidemiology. 1999;10(2):171–175. [PubMed] [Google Scholar]
- Zhang Junjie, Mu Quan. Air pollution and defensive expenditures: evidence from particulate-filtering facemasks. J. Environ. Econ. Manag. 2018;92:517–536. [Google Scholar]
- Zhang Pengfei, Dong Guanghui, Sun Baijun. Long-term exposure to ambient air pollution and mortality due to cardiovascular disease and cerebrovascular disease in shenyang, China. PloS One. 2011;6(6):1–8. doi: 10.1371/journal.pone.0020827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Maigeng, Liu Yunning, Wang Lijun. Particulate air pollution and mortality in a cohort of Chinese men. Environ. Pollut. 2014;186:1–6. doi: 10.1016/j.envpol.2013.11.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.