Abstract
The 11th Acromegaly Consensus Conference in April 2017 was convened to update recommendations on therapeutic outcomes for patients with acromegaly. Consensus guidelines on the medical management of acromegaly were last published in 2014; since then, new pharmacological agents have been developed and new approaches to treatment sequencing have been considered. Thirty-seven experts in the management of patients with acromegaly reviewed the current literature and assessed changes in drug approvals, clinical practice standards and clinical opinion. They considered current treatment outcome goals with a focus on the impact of current and emerging somatostatin receptor ligands, growth hormone receptor antagonists and dopamine agonists on biochemical, clinical, tumour mass and surgical outcomes. The participants discussed factors that would determine pharmacological choices as well as the proposed place of each agent in the guidelines. We present consensus recommendations highlighting how acromegaly management could be optimized in clinical practice.
Subject terms: Growth disorders, Drug therapy, Pituitary tumours
Acromegaly is usually caused by a pituitary adenoma that secretes growth hormone; treatment of acromegaly and its comorbidities is often complex. In this Consensus Statement, Shlomo Melmed and colleagues provide updated recommendations for the treatment of patients with acromegaly.
Introduction
Acromegaly is caused by excess circulating levels of growth hormone (GH) and insulin-like growth factor 1 (IGF1), which typically result from a GH-secreting pituitary adenoma1. Patients exhibit characteristic acral and soft tissue overgrowth (particularly in the face and hands), arthritis, jaw overbite, respiratory obstruction, hypertension and headache, as well as visual disturbances and cranial nerve palsy from tumour mass effects2. Metabolic dysfunction, including insulin resistance and elevated HbA1c, increases the risk of diabetes mellitus and cardiovascular-related morbidity and mortality3. Treatment of patients with acromegaly is aimed at normalizing GH and/or IGF1 levels to ameliorate signs and symptoms of the disease2,4,5 and reduce excess mortality6–8.
Long-term biochemical control is achieved in fewer than 65% of patients following surgical resection of the tumour despite the use of novel surgical approaches9–15, and only approximately half of patients treated with medical therapy achieve control of IGF1 levels16–19. Radiation therapy remains an option in patients with persistently active disease, but rates of control and safety have only marginally improved with the use of stereotactic radiosurgery instead of conventional fractionated radiotherapy20. Management of acromegaly and the comorbidities of the disorder is complex and requires a comprehensive approach coordinated by a multidisciplinary team of physicians who are experts in the treatment of pituitary tumours21.
In April 2017, the Acromegaly Consensus Group convened to update the most recent consensus guidelines on the medical management of acromegaly, which were published in 2014 (ref.4). Since that publication, new pharmacological agents have been developed and new approaches to treatment sequencing have been considered. Thirty-seven experts in acromegaly management (Box 1) reviewed the current literature and assessed changes in drug approvals, clinical practice standards and clinical opinion since the 2014 consensus publication. Discussions focused on treatment outcome goals; effects of pharmacological agents on biochemical, clinical, tumour volume and surgical outcomes; factors determining pharmacological choices; and the proposed place of available pharmacological agents in the guidelines. Updated consensus recommendations on therapeutic outcomes for patients with acromegaly were graded using the Grading of Recommendations Assessment, Development and Evaluation system22,23 (Box 2), and the key recommendations are presented in Box 3. Key changes from the 2014 consensus recommendations are presented in Table 1.
Table 1.
Key changes from the 2014 to the 2018 consensus recommendations
| Strategy | 2014 consensus recommendation4 | 2018 consensus recommendation |
|---|---|---|
| Management approach | Not addressed | Multidisciplinary team approach at a pituitary tumour centre of excellence, where possible |
| Defining and monitoring biochemical control | GH nadir <1 µg/l after OGTT on sensitive assays |
• GH nadir < 0.4 µg/l after OGTT using ultrasensitive assays • Wait at least 12 weeks after surgery to assess IGF1 levels (delayed decline versus persistent postoperative GH) • Do not measure GH in patients receiving pegvisomant (levels remain elevated) |
| First-line medical therapy in patients with persistent disease after surgery |
• SRL (octreotide LAR or lanreotide autogel) • Cabergoline if IGF1 <2 times the upper limit of normal |
• First-generation SRL (octreotide LAR or lanreotide autogel) • Cabergoline if IGF1 <2.5 times the upper limit of normal |
| Second-line medical therapy if first-generation SRL is not successful in normalizing IGF1 |
Partial response: • Increase SRL dose or decrease dose interval • Add pegvisomant to SRL • Add cabergoline to SRL Minimal or no response: • Switch to pegvisomant |
Partial response: • Increase first-generation SRL dose and/or increase dose frequency of lanreotide autogel • Add cabergoline to SRL if IGF1 is moderately elevated Minimal or no response and tumour concern: • Switch to pasireotide LAR Minimal or no response and impaired glucose metabolism: • Switch to pegvisomant Minimal or no response, tumour concern and impaired glucose metabolism: • Add pegvisomant to first-generation SRL |
| Therapy if biochemical control is not achieved after second-line therapy |
• Optimize pegvisomant dose • Switch to pegvisomant plus dopamine agonist • Add dopamine agonist to SRL |
• Stereotactic radiosurgery or surgical intervention (or reintervention) • Temozolomide for unusually aggressive or proven malignant tumours (in close cooperation with a neuro-oncologist) |
| Use of clinical outcome instruments | Not addressed |
• Objective tools (SAGIT and ACRODAT) can be used to assess and monitor indicators of disease activity • Patient quality of life questionnaires (AcroQoL) are probably of limited value |
ACRODAT, Acromegaly Disease Activity Tool; GH, growth hormone; IGF1, insulin-like growth factor 1; LAR, long-acting release; OGTT, oral glucose tolerance test; SAGIT, Signs and symptoms, Associated comorbidities, GH levels, IGF1 levels and Tumour profile; SRL, somatostatin receptor ligand.
Box 1 11th Acromegaly Consensus Conference participants.
Ariel Barkan (USA), Albert Beckers (Belgium), Nienke Biermasz (Netherlands), Beverly Biller (USA), Cesar Boguszewski (Brazil), Marek Bolanowski (Poland), Marcello Bronstein (Brazil), Felipe Casanueva (Spain), Philippe Chanson (France), David Clemmons (USA), Annamaria Colao (Italy), Diego Ferone (Italy), Maria Fleseriu (USA), Monica Gadelha (Brazil), Ezio Ghigo (Italy), Andrea Giustina (Italy), Mark Gurnell (UK), Anthony Heaney (USA), Andrew Hoffman (USA), Laurence Katznelson (USA), Fahrettin Kelestimur (Turkey), Anne Klibanski (USA), Steven Lamberts (Netherlands), Anton Luger (Austria), Gherardo Mazziotti (Italy), Shlomo Melmed (USA), Pietro Mortini (Italy), Marco Losa (Italy), Sebastian Neggers (Netherlands), Stephan Petersenn (Germany), Roberto Salvatori (USA), Christian Strasburger (Germany), Peter Trainer (UK), Stylianos Tsagarakis (Greece), John Wass (UK), Susan Webb (Spain) and Maria Chiara Zatelli (Italy).
Box 2 Grading of evidence and recommendations.
Grading the evidence
Very low quality (VLQ): expert opinion supported by one or few small uncontrolled studies
Low quality (LQ): supported by large series of small uncontrolled studies
Moderate quality (MQ): supported by one or few large uncontrolled studies or meta-analyses
High quality (HQ): supported by controlled studies or large series of large uncontrolled studies with sufficiently long follow-up
Grading the recommendations
Discretionary recommendation (DR): based on VLQ or LQ evidence
Strong recommendation (SR): based on MQ or HQ evidence
Adapted from ref.4, Macmillan Publishers Ltd.
Box 3 Key 2018 consensus recommendations.
We recommend patients be treated at pituitary tumour centres of excellence, where possible, to receive the best and most cost-effective care.
Surgical resection of the pituitary adenoma by an experienced neurosurgeon is recommended where possible and represents the best opportunity for cure.
Medical therapy is recommended for patients with persistent disease despite surgical resection of the adenoma as well as patients in whom surgery is not appropriate.
For patients with persistent disease after surgery, a first-generation long-acting somatostatin receptor ligand (SRL) is recommended as first-line therapy.
If clinically relevant residual tumour that is unsuitable for resection is present, patients not adequately controlled on first-generation SRLs could be considered for switching to pasireotide long-acting release.
If there is pre-existing clinically relevant impaired glucose metabolism, patients not adequately controlled on first-generation SRLs should be switched to pegvisomant.
Methods
Meeting participants were assigned specific topics related to acromegaly treatment and outcomes. Literature searches were conducted using PubMed for English-language papers published between April 2013 and March 2017. Search terms included “acromegaly” and terms associated with each topic: “biochemical outcomes”, “tumour volume”, “clinical symptoms”, “somatostatin receptor ligand”, “dopamine agonist”, “GH receptor antagonist”, “estrogen”, “selective estrogen receptor modulator”, “mortality”, “complications”, “surgical outcomes” and “guidelines”. After a brief presentation on each topic to the entire group, participants were divided into subgroups for further discussion of the topic and reported their findings to the entire group. Participants developed consensus recommendations on the basis of all presentations, discussions and reports. All participants then voted on each recommendation. After the meeting, the Scientific Committee graded the evidence supporting the recommendations, and then graded the consensus recommendations on the basis of the quality of evidence (Box 2).
Treatment outcome goals
Biochemical outcomes
Excess GH and/or IGF1 in patients with acromegaly leads to metabolic, cardiovascular and musculoskeletal comorbidities, which, in turn, increase mortality as a result of cardiovascular, cerebrovascular and respiratory abnormalities1,7. Treatment is aimed at normalizing IGF1 levels, as doing so usually reflects adequate disease control, decreases risk of developing complications from comorbidities24 and might also reduce excess mortality6,25. However, large variability exists between the different IGF1 assays (moderate quality (MQ)). Pre-analytical and analytical factors can confound results26, and differences in normative data and reference ranges make it difficult to compare results across assays27,28. It is therefore recommended that, whenever possible, endocrinologists use the same assay when monitoring IGF1 levels over time and that the selected assays adhere to accepted performance standards26 (strong recommendation (SR)). Newer techniques, such as mass spectrometry29, might offer an improvement over older immunoassays but might not be routinely available.
GH nadir levels <1 µg/l after an oral glucose tolerance test (OGTT) were first defined by our Consensus Group as reflective of postoperative cure in 2000 (ref.30). Data from large observational studies continue to show improved long-term outcomes and reduced mortality in patients who achieve GH <1 µg/l after surgery11,25,31 (MQ). When ultrasensitive GH assays are available, we recommend an OGTT GH cut-off of 0.4 µg/l (SR). Although this lower cut-off might not further improve metabolic outcomes32, nor markedly influence the percentage of patients who achieve biochemical remission31, it is better suited to the lower limits of detection of the newer assays33–35. GH nadir levels during an OGTT are also affected by factors such as patient age, BMI, sex and oestrogen use, and we recommend that these factors are considered when interpreting results of this test26,36 (discretionary recommendation (DR)).
The hypothalamic-controlled episodic pattern of GH secretion that is seen in healthy individuals is retained in patients with acromegaly37, but might not correlate with levels of IGF1 in patients who have been treated with medical therapy38 (low quality (LQ)). We recommend monitoring biochemical control by measuring both GH and IGF1 levels (SR). However, we recommend that normalizing levels of IGF1 is a key goal, as it is the best reflection of disease control38 (DR). As GH levels remain elevated with pegvisomant therapy, measuring GH in patients receiving pegvisomant should not be done18 (high quality (HQ)). Monitoring of GH levels can be used to directly monitor tumour activity39 (very low quality (VLQ)), but we recommend waiting at least 12 weeks after surgery to assess IGF1 levels, as the postoperative decline in IGF1 levels can be delayed compared with that of GH levels11,40 (SR). Discordant reported IGF1 and GH values have been observed in patients following surgery as well as in those treated with somatostatin receptor ligands (SRLs)41,42 (MQ), which is probably the result of discrepancies in the assays used (MQ) and/or of biological factors, such as sex, glucose metabolism and GH receptor polymorphism, affecting results43,44 (VLQ). As the clinical importance of such a finding remains to be established, performing an OGTT in patients treated with an SRL is not likely to be clinically useful38.
Tumour volume
Reducing tumour size and preventing further tumour growth are clinically relevant goals for patients with acromegaly and macroadenomas (≥10 mm), as the presence of these larger tumours is independently associated with poor clinical outcomes45. Most current series evaluating tumour response to SRL therapy use a volume reduction cut-off of 20–25% to define significant reduction (LQ), as it seems unlikely that lower thresholds could be determined owing to methodological variability. However, accurately measuring volume in clinical practice might be hampered by technical differences in methods, tumour shape and intra-observer inconsistencies46 (VLQ). For routine measurements in standard clinical practice, we recommend that reduction in a single tumour dimension, such as diameter, rather than tumour volume, might be simpler to measure and is sufficient to assess meaningful mass change46,47 (DR). T2-weighted MRI hypointensity at diagnosis predicts tumour shrinkage in patients receiving SRL therapy (MQ), and we recommend that this factor might be a useful marker of tumour responsiveness48 (DR).
Clinical symptoms
Prevention and management of disease-associated symptoms and comorbidities are critical to improving clinical outcomes in patients with acromegaly49. Cardiovascular and respiratory effects are major causes of morbidity and mortality6,8,25 (HQ), and impaired glucose metabolism further contributes to increased cardiovascular risk50,51 (HQ). We recommend assessing and aggressively managing disease-associated comorbidities, specifically hypertension and cardiac hypertrophy, diabetes mellitus and glucose intolerance, sleep apnoea and osteopathy (SR). In patients with uncontrolled disease, these comorbidities should be aggressively managed to prevent excess mortality. When GH and/or IGF1 levels are controlled, regular 6-month follow-up is prudent. Clinician-reported outcome instruments such as SAGIT (Signs and symptoms, Associated comorbidities, GH levels, IGF1 levels and Tumour profile) and ACRODAT (Acromegaly Disease Activity Tool) provide objective measurements of acromegaly signs and symptoms, comorbidities, tumour profile, GH levels and IGF1 levels (VLQ), and we recommend that they can be used to assess and monitor indicators of disease activity52,53 (DR). Patient-reported health-related quality of life should also be considered. However, results from the acromegaly-specific questionnaire AcroQoL do not consistently correlate with biochemical control54–56, and interpretation of discordant biochemical and quality of life results remains unclear. Routine use of this tool in clinical practice is probably of limited value (DR).
Pituitary tumour centres of excellence
Treatment of acromegaly is best accomplished by a multidisciplinary team of experts meeting together in person or virtually21 (MQ). With this structure, termed a pituitary tumour centre of excellence, in addition to neurosurgeons expert in transsphenoidal pituitary surgery and endocrinologists well versed in the full spectrum of medical therapies, the management team should comprise neuroradiologists well trained in pituitary and parasellar imaging; neuropathologists with expertise in molecular analysis; and radiation oncologists with specific knowledge in treating intracranial tumours (LQ). The availability of skilled nurses experienced in relevant pituitary therapies and patient education is important. We recommend that patients are treated at pituitary tumour centres of excellence to receive the best and most cost-effective care (SR). However, as patient access to such centres might be limited21, consensus recommendations are provided to optimize acromegaly therapeutic outcomes in routine clinical practice.
Biochemical results of medical therapy
Medical therapy is recommended for patients with persistent disease despite surgical resection of the adenoma as well as for patients in whom surgery is not appropriate (SR). The SRLs octreotide, lanreotide and pasireotide, as well as the dopamine agonist cabergoline, bind cognate receptors in the adenoma and suppress GH secretion; the GH antagonist pegvisomant blocks GH action in the periphery and blocks generation of IGF1 (refs57–59).
Somatostatin receptor ligands
First-generation somatostatin receptor ligands
Biochemical control rates of approximately 55% have been reported with the first-generation SRLs octreotide and lanretotide60; however, data from rigorously conducted trials using currently available long-acting formulations show lower rates of 25–45%16,17,19,61 (MQ). As patient selection bias, initial IGF1 levels, previous surgery, adverse effects and treatment compliance can all impact the likelihood of achieving biochemical control, in practice, biochemical response to first-generation SRLs is likely to be higher than that observed in trials published in the past 10 years but lower than in earlier trials (LQ)62. Octreotide long-acting release (LAR) is administered once monthly by intramuscular injection; lanreotide autogel is administered once monthly subcutaneously by the patient, their caregiver or a health-care provider. As efficacy rates are similar for the two agents19,60, preference for route of delivery and/or associated cost might influence treatment choice63 (VLQ).
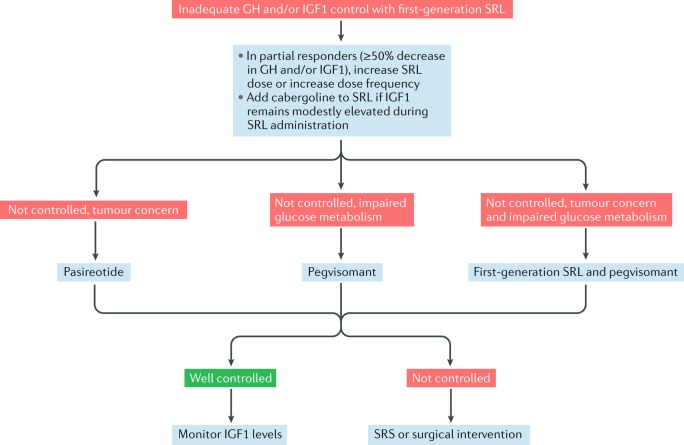
Studies have shown that higher doses of octreotide LAR (60 mg every 28 days) as well as higher doses (180 mg every 28 days) and more frequent dosing (120 mg every 21 days) of lanreotide autogel can improve biochemical control rates in patients who are inadequately controlled on standard doses but are responsive to SRL therapy64,65 (MQ). The maximal dosing of first-generation SRLs remains to be clarified. Careful patient selection, including considering degree of responsiveness to standard dosing, baseline IGF1 levels and treatment adverse effect profiles, is recommended before implementing such strategies (DR) (Fig. 1).
Fig. 1. A proposed algorithm for the treatment of acromegaly in patients inadequately controlled with first-generation somatostatin receptor ligands lanreotide autogel and octreotide long-acting release.
In partial responders (≥50% decrease in growth hormone (GH) and/or insulin-like growth factor 1 (IGF1)), increase somatostatin receptor ligand (SRL) dose and/or dose frequency. If IGF1 remains modestly elevated during SRL administration, add cabergoline to SRL. If disease control is not achieved, patients should be switched to the second-generation SRL pasireotide if there is clinically relevant residual tumour on imaging and/or clinical concern of tumour growth (tumour concern). Patients with impaired glucose tolerance should be switched to the GH antagonist pegvisomant. Patients with impaired glucose tolerance and tumour concern should be treated with a combination of a first-generation SRL and pegvisomant. Those who remain uncontrolled despite second-line medical therapy should be considered for stereotactic radiosurgery (SRS) or surgical intervention.
Second-generation somatostatin receptor ligands
Biochemical control rates with pasireotide LAR are higher than those achieved with octreotide LAR in patients who have not previously been treated with an SRL61 (MQ). However, normalized levels of IGF1 are still achieved in fewer than half of patients treated with pasireotide LAR, and nearly 70% of patients treated with pasireotide LAR exhibited hyperglycaemia-associated adverse effects66 (MQ). As patients with inadequately controlled disease on octreotide LAR or lanreotide autogel show improved biochemical control after switching to pasireotide LAR66, we recommend pasireotide LAR be considered a second-line therapy (SR) (Fig. 1). Elevated HbA1c and fasting plasma levels of glucose at baseline are strong predictors for developing hyperglycaemia during treatment with pasireotide LAR67 (MQ). We recommend that patients considered for treatment with pasireotide LAR should be carefully screened and monitored for glycaemic adverse effects (SR), and pasireotide LAR should preferably be used in those with normal glucose tolerance. Blood levels of glucose should be monitored weekly for the first 3 months of treatment and in the first 4–6 weeks after dose increases. Monitoring should continue throughout treatment, as clinically appropriate.
Somatostatin receptor ligands in development
New formulations of SRLs are currently in clinical development, including oral octreotide capsules, parenteral octreotide bound in a liquid crystal mix and a parenteral multi-ligand SRL with high selectivity for GH suppression68,69. A phase III study of oral octreotide in patients well controlled on octreotide LAR showed that biochemical control rates were maintained after switching to oral octreotide, and patient acceptability and compliance were improved owing to route of administration70 (LQ). Additional studies with oral octreotide are currently underway71,72.
Dopamine agonist
Cabergoline monotherapy results in biochemical control rates of approximately 35%; similar benefits have also been seen with the addition of cabergoline to an SRL in patients with inadequate control on SRL therapy73 (LQ). However, the benefits are largely limited to patients with mildly elevated levels of IGF1 at baseline, with the greatest benefit seen in those with IGF1 levels ≤1.5 times the upper limit of normal (MQ). We recommend that cabergoline should therefore be considered as a first-line medical therapy or as an addition to first-generation SRL in patients with IGF1 levels <2.5 times the upper limit of normal (DR).
GH receptor antagonist
Pegvisomant monotherapy administered as second-line therapy yields biochemical control rates of 90% or more in clinical trials18,74 (HQ) and closer to 60% in real-world surveillance studies75,76 (MQ). This difference is probably primarily attributable to differences in doses, as patients in clinical practice are less likely to be uptitrated to the maximum dose despite higher efficacy rates being seen at higher doses77 (VLQ). Pegvisomant is approved for use at doses ranging from 10 mg per day to 30 mg per day, and we recommend that the daily dose should be increased to the recommended highest dose as needed (SR). Patient-specific factors such as age and BMI have been identified as predictive of the dose of pegvisomant that is required for normalization of IGF1 levels78,79 (LQ), but we recommend that physicians should regularly monitor IGF1 levels throughout therapy to determine whether normalization can be achieved by adapting the dose regimen59 (SR). Surveillance studies show that high doses of up to 60 mg per day have been used in patients with persistently elevated IGF1 levels80; however, use of doses above 30 mg per day is not approved, has not been prospectively studied and therefore is not recommended in clinical practice (DR).
Similarly, pegvisomant has shown high efficacy rates when given in combination with an SRL and delivered once or twice weekly81,82 (MQ) and might show continued effectiveness after discontinuing the SRL83 (LQ). Analysis of surveillance data suggests a biochemical control rate of approximately 75% in patients treated with pegvisomant monotherapy as first-line therapy84, but prospective data are lacking (VLQ).
Oestrogens and SERMs
Oestrogens and selective oestrogen receptor modulators (SERMs) reduce levels of IGF1 in patients with acromegaly when used alone or in combination with an SRL or cabergoline85 (VLQ). SERMs might have an additional benefit in men with acromegaly and hypogonadism, as these agents also increase levels of testosterone86,87 (VLQ). However, as published evidence is limited, optimal use of these agents remains undetermined, and sex-specific adverse effects should also be considered.
Clinical outcomes of medical therapy
Although biochemical control is the primary aim of acromegaly treatment, physicians should also consider the effect of therapy on disease-related morbidity and mortality. As a result, physicians should implement strategies to prevent, address and manage acromegaly complications.
Mortality
The increased mortality that is associated with acromegaly is largely ameliorated in patients with adequately controlled disease, who have mortality similar to that of the general population6,7 (MQ). In addition, patients followed up in the long term show a shift away from cardiovascular disease to cancer as a leading cause of death25,88,89 (LQ). A continuum of benefit results from normalizing GH and IGF1 levels, leading to improved outcomes of disease-related comorbidities and reduced mortality risk25. However, the effects of specific treatment modalities on mortality in patients not cured with surgery are unclear. Data linking conventional radiotherapy with increased mortality might not apply to stereotactic radiosurgery given the potential improvements in treatment outcomes20,90,91 (VLQ), but effects on mortality have not been sufficiently investigated. Data on the long-term impact of medical therapy on all-cause mortality are few and inconclusive.
Complications
Cardiomyopathy, hypertension, valvular disease, arrhythmias and sodium and fluid retention leading to expanded extracellular fluid volume are seen in more than 60% of patients with acromegaly and are a major cause of disease-associated morbidity and mortality3,49 (HQ). Surgery, SRLs and pegvisomant can all improve left ventricular hypertrophy in patients who achieve biochemical control92–94 (MQ); improvement in hypertension and arrhythmias has also been shown in patients effectively treated with medical therapy93,95 (LQ). A study published in 2012 that examined potential adverse valvular effects associated with high-dose cabergoline in other diseases found no such effect in patients with acromegaly, which is reassuring96. As cardiac comorbidities might persist despite biochemical control of acromegaly, regular monitoring of patients is recommended (SR).
Vertebral fractures have been observed in up to 60% of patients with acromegaly97–99 (MQ). These fractures can be present despite disease control100,101 and are frequently asymptomatic97. Normal BMD on dual X-ray absorptiometry might offer false reassurance, as BMD does not predict fracture risk in patients with acromegaly97,98,101 (MQ). Bone turnover is probably a better indicator of bone quality101,102 (LQ), and proactive evaluations of vertebral fractures with the morphometric approach are recommended at diagnosis and annually thereafter103 (SR). Assessment of bone microarchitecture in men with acromegaly has shown that alterations in both cortical and trabecular bone occur, which further corroborates the limitations of using areal BMD to assess fracture risk in these patients104.
Soft tissue and bony craniofacial overgrowth result in considerable airway obstruction and respiratory complications in at least 25% of patients with acromegaly and might not be reversible despite the achievement of adequate biochemical control49 (MQ). We recommend that screening questionnaires for obstructive sleep apnoea are used in clinical practice, with sleep studies ordered as needed to confirm the diagnosis (SR). We also recommend that management strategies such as continuous positive airway pressure therapy should be considered for patients with persistent symptoms independent of acromegaly treatment105 (DR).
Impaired glucose metabolism and diabetes mellitus, which are present in up to half of patients with acromegaly, are infrequently affected by treatment with first-generation SRLs106 (MQ) but can be exacerbated by pasireotide61,67. By contrast, pegvisomant might have a beneficial effect on insulin sensitivity, glucose tolerance and fatty acid metabolism, mainly owing to its consequent suppression of hepatic glucose production107,108 (MQ). Close monitoring of glycaemia is recommended for all patients and particularly for those treated with pasireotide (SR). We recommend that hyperglycaemia is treated promptly (SR).
Patients with acromegaly are at increased risk of colorectal adenomatous polyps and colorectal cancer109. However, a conclusive association between the frequency of colonoscopic surveillance and cancer-specific mortality in patients with acromegaly but not concurrent high-risk factors, such as known polyps or a family history of polyps, has not been shown110 (MQ). We recommend cancer screening be carried out as recommended for the general population (DR).
Tumour volume and surgical outcomes
SRLs induce tumour shrinkage via direct and indirect antiproliferative effects111. Approximately half of patients show considerable tumour reduction within the first few months of treatment with primary or adjuvant SRLs (MQ); these changes typically, but not necessarily, correlate with biochemical control46,47,112–115 (LQ). Pasireotide might exert a greater effect on tumour control than octreotide and lanreotide66 (LQ). Patients with acromegaly owing to genetic causes, such as AIP mutations and X-linked acrogigantism, might exhibit larger tumours that could be less responsive to therapy than tumours in patients with sporadic acromegaly116–118 (VLQ).
Although preoperative treatment with SRLs can reduce tumour size and improve surgical cure rates in patients with macroadenomas119,120 (LQ), routine use of SRLs for this purpose is not recommended, as evidence for a benefit on postoperative outcomes remains unclear121 (DR).
Increased tumour growth associated with pegvisomant therapy has been reported, particularly in patients who switch from an SRL to pegvisomant122,123 (LQ). However, large observational studies carefully examining reported cases found it to be rare75 and not more frequent than in patients on SRL therapy (MQ); furthermore, the mechanisms underlying the effect remain unclear. Nevertheless, the possibility of tumour growth with pegvisomant should be taken into consideration when selecting treatment, and ongoing imaging surveillance is advised for patients with notable residual tumour who are treated with pegvisomant (SR) (Fig. 1). Data on the effects of cabergoline on tumour volume are insufficient to form a recommendation58 (VLQ).
Imaging frequency to assess tumour volume should be individualized to each patient. We recommend that baseline tumour size and location, current medical therapy and its presumed effect on tumour mass, as well as persistent activity or biochemical relapse of the disease, should all be considered (DR).
Factors in pharmacological choices
Although the initial therapy choice will largely be driven by tumour and biochemical characteristics, we recommend that other patient-specific and disease-specific factors should be considered to appropriately individualize the therapeutic approach45 (DR). For example, although reduction of acromegaly disease activity might lead to improvements in insulin sensitivity, worsening of hyperglycaemia can occur during therapy, largely owing to inhibition of insulin secretion by SRLs (MQ). This factor is particularly relevant with the use of pasireotide but might also be relevant for the use of first-generation SRLs (LQ). Thus, for patients with impaired glucose metabolism and/or for those who experience worsening hyperglycaemia on SRL therapy, we recommend that pegvisomant or cabergoline can be considered as alternative options (DR). We also recommend that hyperglycaemia owing to acromegaly-directed therapy should be managed to aggressively control glucose levels (SR).
We recommend that tumour location (that is, proximity to the optic chiasm) as well as tumour size and the presence of local effects of the tumour mass (such as visual field defects and headache) should be used to determine treatment choice on the basis of the likely effect of therapy on tumour volume (SR).
Well-studied clinical and pathological predictors of responsiveness should also be considered. Tumours showing dense GH granulation on pathology demonstrate greater responsiveness to first-generation SRL therapy than sparsely granulated adenomas45,124,125 (LQ), whereas T2-hyperintense tumours are less likely to respond to SRL therapy than other tumours48,126 (LQ).
Other pathological markers, including immunohistochemistry to assess somatostatin receptor type 2 (SST2) and SST5 expression as well as dopamine receptor status124,127, might be useful for individualizing treatment decisions (VLQ). These markers, however, require further prospective validation and harmonization of scoring systems to determine a personalized approach to use, as they are not approved for routine laboratory use and still remain investigational128.
Proposed place in the guidelines
First-line medical therapy
Surgical resection of the pituitary adenoma by an experienced neurosurgeon is recommended where possible and represents the optimal opportunity for cure (SR). Primary medical therapy with an SRL might be considered if surgery is contraindicated or if a poor likelihood of success is expected owing to patient-specific and/or tumour-specific factors (DR).
For patients with persistent disease after surgery, a first-generation long-acting SRL is recommended as first-line medical therapy (SR). The choice between octreotide LAR and lanreotide autogel is determined by availability, convenience of administration and patient preference (DR). Cabergoline can be attempted as a first-line medical therapy in patients with acromegaly and mildly elevated levels of IGF1 of <2.5 times the upper limit of normal (DR).
Second-line medical therapy
We recommend that additional therapies are necessary when first-line medical therapy is not successful in normalizing levels of IGF1 (SR) (Fig. 1). For patients who achieve partial response (a decrease in GH and/or IGF1 ≥50%) after using a long-acting first-generation SRL as first-line medical therapy, we recommend that increasing the dose of the SRL and/or increasing the dose frequency of lanreotide autogel should be attempted (DR). We recommend the addition of cabergoline to continued SRL treatment when levels of IGF1 remain modestly elevated during SRL administration. If a tumoural remnant is surgically resectable, which would enable a considerable decrease in tumour mass, a second surgical intervention might be proposed before re-initiating SRL treatment.
If biochemical control is not achieved after administering the maximal dose of first-generation SRL, we recommend that treatment should be individualized on the basis of the presence or absence of clinically relevant residual tumour and impaired glucose tolerance (SR). If a clinically relevant residual tumour that is unsuitable for resection is present, we recommend that patients should be switched from first-generation SRL to pasireotide LAR (DR); if severe hyperglycaemia occurs, patients should be switched to pegvisomant (DR). However, if there is pre-existing clinically relevant impaired glucose metabolism, patients should be switched from first-generation SRL to pegvisomant (DR). If there is clinically relevant residual tumour and pre-existing impaired glucose metabolism, maintaining first-generation SRL and adding pegvisomant is recommended (DR).
Additional considerations
If biochemical control is not achieved after second-line therapy, stereotactic radiosurgery or surgical intervention or reintervention should be reconsidered, as appropriate (SR). Use of temozolomide should be limited to patients with unusually aggressive or proven malignant pituitary tumours129. In such cases, close cooperation with a neuro-oncologist is advisable (DR).
Conclusions
Our recommendations for management of acromegaly have markedly changed since the previous consensus published in 2014 (ref.4). With the availability of pasireotide LAR, patients now have more treatment options and are more likely to achieve biochemical control. At the same time, clinicians should be vigilant about tailoring treatment approaches to account for the full clinical disease spectrum, taking into account biochemical control rates as well as tumour profile and glucose metabolism. Further study of current and emerging agents will help to better define the patient populations most likely to benefit from each treatment strategy and to tailor acromegaly treatments to individual patient needs.
Acknowledgements
The 11th Acromegaly Consensus Conference was supported by educational grants from Ipsen Ltd, Novartis Pharmaceuticals and Pfizer. Scientific sponsorship of the meeting was provided by Cedars-Sinai Medical Center, Los Angeles, CA, USA.
Author contributions
All authors researched data for the article. M.D.B., P.C., A.K., F.F.C., J.A.H.W., C.J.S., A.L. and D.R.C. made substantial contributions to discussion of the content. S.M. and A.G. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Competing interests
S.M. is a consultant for Chiasma, Ionis, Ipsen and Strongbridge Pharma and receives research grants from Pfizer. M.D.B. is a consultant for Ipsen and Novartis, a speakers bureau member for Ipsen and has received research grants from Novartis. P.C. has received unrestricted research and educational grants from Ipsen, Novartis and Pfizer as head of the Department of Endocrinology and Reproductive Diseases, Hôpitaux Universitaires Paris-Sud,has served as investigator for clinical trials funded by Antisense, Chiasma, Ipsen, Italpharmaco, Novartis and Pfizer and is a consultant for Ipsen, Novartis and Pfizer. All fees and honoraria are paid to his institution. A.K. is a consultant for Chiasma and Crinetics and has received research grants from Ipsen. F.F.C. is a speakers bureau member for Pfizer and has received research grants from Ipsen and Pfizer. C.J.S. is an advisory board member for Pfizer and a speakers bureau member for Pfizer and Ipsen. A.L. is a consultant for Ipsen and Novartis, a speakers bureau member for Ipsen, Novartis and Pfizer and has received research grants from Pfizer. D.R.C. is a consultant for Crinetics, Ipsen and Pfizer. A.G. is a consultant for Ipsen, Novartis and Pfizer. J.A.H.W. declares no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Melmed S. Acromegaly pathogenesis and treatment. J. Clin. Invest. 2009;119:3189–3202. doi: 10.1172/JCI39375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melmed S. Medical progress: Acromegaly. N. Engl. J. Med. 2006;355:2558–2573. doi: 10.1056/NEJMra062453. [DOI] [PubMed] [Google Scholar]
- 3.Colao A, Ferone D, Marzullo P, Lombardi G. Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr. Rev. 2004;25:102–152. doi: 10.1210/er.2002-0022. [DOI] [PubMed] [Google Scholar]
- 4.Giustina A, et al. Expert consensus document: A consensus on the medical treatment of acromegaly. Nat. Rev. Endocrinol. 2014;10:243–248. doi: 10.1038/nrendo.2014.21. [DOI] [PubMed] [Google Scholar]
- 5.Katznelson L, et al. Acromegaly: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2014;99:3933–3951. doi: 10.1210/jc.2014-2700. [DOI] [PubMed] [Google Scholar]
- 6.Holdaway IM, Bolland MJ, Gamble GD. A meta-analysis of the effect of lowering serum levels of GH and IGF-I on mortality in acromegaly. Eur. J. Endocrinol. 2008;159:89–95. doi: 10.1530/EJE-08-0267. [DOI] [PubMed] [Google Scholar]
- 7.Dekkers OM, Biermasz NR, Pereira AM, Romijn JA, Vandenbroucke JP. Mortality in acromegaly: a metaanalysis. J. Clin. Endocrinol. Metab. 2008;93:61–67. doi: 10.1210/jc.2007-1191. [DOI] [PubMed] [Google Scholar]
- 8.Sherlock M, et al. Mortality in patients with pituitary disease. Endocr. Rev. 2010;31:301–342. doi: 10.1210/er.2009-0033. [DOI] [PubMed] [Google Scholar]
- 9.Shimon I, Cohen ZR, Ram Z, Hadani M. Transsphenoidal surgery for acromegaly: endocrinological follow-up of 98 patients. Neurosurgery. 2001;48:1239–1243. doi: 10.1097/00006123-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Hazer DB, et al. Treatment of acromegaly by endoscopic transsphenoidal surgery: surgical experience in 214 cases and cure rates according to current consensus criteria. J. Neurosurgery. 2013;119:1467–1477. doi: 10.3171/2013.8.JNS13224. [DOI] [PubMed] [Google Scholar]
- 11.Babu H, et al. Long-term endocrine outcomes following endoscopic endonasal transsphenoidal surgery for acromegaly and associated prognostic factors. Neurosurgery. 2017;81:357–366. doi: 10.1093/neuros/nyx020. [DOI] [PubMed] [Google Scholar]
- 12.Jane JA, Jr., et al. Endoscopic transsphenoidal surgery for acromegaly: remission using modern criteria, complications, and predictors of outcome. J. Clin. Endocrinol. Metab. 2011;96:2732–2740. doi: 10.1210/jc.2011-0554. [DOI] [PubMed] [Google Scholar]
- 13.Anik I, et al. Endoscopic transsphenoidal approach for acromegaly with remission rates in 401 patients: 2010 Consensus Criteria. World Neurosurg. 2017;108:278–290. doi: 10.1016/j.wneu.2017.08.182. [DOI] [PubMed] [Google Scholar]
- 14.Mortini P, Barzaghi LR, Albano L, Panni P, Losa M. Microsurgical therapy of pituitary adenomas. Endocrine. 2018;59:72–81. doi: 10.1007/s12020-017-1458-3. [DOI] [PubMed] [Google Scholar]
- 15.Chen CJ, et al. Microsurgical versus endoscopic transsphenoidal resection for acromegaly: a systematic review of outcomes and complications. Acta Neurochir. 2017;159:2193–2207. doi: 10.1007/s00701-017-3318-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mercado M, et al. A prospective, multicentre study to investigate the efficacy, safety and tolerability of octreotide LAR (long-acting repeatable octreotide) in the primary therapy of patients with acromegaly. Clin. Endocrinol. 2007;66:859–868. doi: 10.1111/j.1365-2265.2007.02825.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Melmed S, et al. Rapid and sustained reduction of serum growth hormone and insulin-like growth factor-1 in patients with acromegaly receiving lanreotide Autogel therapy: a randomized, placebo-controlled, multicenter study with a 52 week open extension. Pituitary. 2010;13:18–28. doi: 10.1007/s11102-009-0191-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trainer PJ, et al. Treatment of acromegaly with the growth hormone-receptor antagonist pegvisomant. N. Engl. J. Med. 2000;342:1171–1177. doi: 10.1056/NEJM200004203421604. [DOI] [PubMed] [Google Scholar]
- 19.Murray RD, Melmed S. A critical analysis of clinically available somatostatin analog formulations for therapy of acromegaly. J. Clin. Endocrinol. Metab. 2008;93:2957–2968. doi: 10.1210/jc.2008-0027. [DOI] [PubMed] [Google Scholar]
- 20.Abu Dabrh AM, et al. Radiotherapy versus radiosurgery in treating patients with acromegaly: A systematic review and meta-analysis. Endocr. Pract. 2015;21:943–956. doi: 10.4158/EP14574.OR. [DOI] [PubMed] [Google Scholar]
- 21.Casanueva FF, et al. Criteria for the definition of Pituitary Tumor Centers of Excellence (PTCOE): A Pituitary Society Statement. Pituitary. 2017;20:489–498. doi: 10.1007/s11102-017-0838-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guyatt GH, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swiglo BA, et al. A case for clarity, consistency, and helpfulness: state-of-the-art clinical practice guidelines in endocrinology using the grading of recommendations, assessment, development, and evaluation system. J. Clin. Endocrinol. Metab. 2008;93:666–673. doi: 10.1210/jc.2007-1907. [DOI] [PubMed] [Google Scholar]
- 24.Reid TJ, et al. IGF-1 levels across the spectrum of normal to elevated in acromegaly: relationship to insulin sensitivity, markers of cardiovascular risk and body composition. Pituitary. 2015;18:808–819. doi: 10.1007/s11102-015-0657-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mercado M, et al. Successful mortality reduction and control of comorbidities in patients with acromegaly followed at a highly specialized multidisciplinary clinic. J. Clin. Endocrinol. Metab. 2014;99:4438–4446. doi: 10.1210/jc.2014-2670. [DOI] [PubMed] [Google Scholar]
- 26.Clemmons DR. Consensus statement on the standardization and evaluation of growth hormone and insulin-like growth factor assays. Clin. Chem. 2011;57:555–559. doi: 10.1373/clinchem.2010.150631. [DOI] [PubMed] [Google Scholar]
- 27.Chanson P, et al. Reference values for IGF-I serum concentrations: comparison of six immunoassays. J. Clin. Endocrinol. Metab. 2016;101:3450–3458. doi: 10.1210/jc.2016-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mavromati M, et al. Classification of patients with GH disorders may vary according to the IGF-I assay. J. Clin. Endocrinol. Metab. 2017;102:2844–2852. doi: 10.1210/jc.2017-00202. [DOI] [PubMed] [Google Scholar]
- 29.Bystrom C, et al. Clinical utility of insulin-like growth factor 1 and 2; determination by high resolution mass spectrometry. PLoS One. 2012;7:e43457. doi: 10.1371/journal.pone.0043457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giustina A, et al. Criteria for cure of acromegaly: a consensus statement. J. Clin. Endocrinol. Metab. 2000;85:526–529. doi: 10.1210/jcem.85.2.6363. [DOI] [PubMed] [Google Scholar]
- 31.Starke RM, et al. Endoscopic versus microsurgical transsphenoidal surgery for acromegaly: outcomes in a concurrent series of patients using modern criteria for remission. J. Clin. Endocrinol. Metab. 2013;98:3190–3198. doi: 10.1210/jc.2013-1036. [DOI] [PubMed] [Google Scholar]
- 32.Ku CR, et al. No differences in metabolic outcomes between nadir GH 0.4 and 1.0 ng/mL during OGTT in surgically cured acromegalic patients (observational study) Medicine. 2016;95:e3808. doi: 10.1097/MD.0000000000003808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clemmons DR. Clinical laboratory indices in the treatment of acromegaly. Clin. Chim. Acta. 2011;412:403–409. doi: 10.1016/j.cca.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 34.Bidlingmaier M, Freda PU. Measurement of human growth hormone by immunoassays: current status, unsolved problems and clinical consequences. Growth Horm. IGF Res. 2010;20:19–25. doi: 10.1016/j.ghir.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verrua E, et al. Reevaluation of acromegalic patients in long-term remission according to newly proposed consensus criteria for control of disease. Int. J. Endocrinol. 2014;2014:581594. doi: 10.1155/2014/581594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arafat AM, et al. Growth hormone response during oral glucose tolerance test: the impact of assay method on the estimation of reference values in patients with acromegaly and in healthy controls, and the role of gender, age, and body mass index. J. Clin. Endocrinol. Metab. 2008;93:1254–1262. doi: 10.1210/jc.2007-2084. [DOI] [PubMed] [Google Scholar]
- 37.Ribeiro-Oliveira A, Jr., Abrantes MM, Barkan AL. Complex rhythmicity and age dependence of growth hormone secretion are preserved in patients with acromegaly: further evidence for a present hypothalamic control of pituitary somatotropinomas. J. Clin. Endocrinol. Metab. 2013;98:2959–2966. doi: 10.1210/jc.2013-1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carmichael JD, Bonert VS, Mirocha JM, Melmed S. The utility of oral glucose tolerance testing for diagnosis and assessment of treatment outcomes in 166 patients with acromegaly. J. Clin. Endocrinol. Metab. 2009;94:523–527. doi: 10.1210/jc.2008-1371. [DOI] [PubMed] [Google Scholar]
- 39.Oldfield EH, et al. Correlation between GH and IGF-1 during treatment for acromegaly. J. Neurosurgery. 2017;126:1959–1966. doi: 10.3171/2016.8.JNS161123. [DOI] [PubMed] [Google Scholar]
- 40.Shin MS, et al. Long-term changes in serum IGF-1 levels after successful surgical treatment of growth hormone-secreting pituitary adenoma. Neurosurgery. 2013;73:473–479. doi: 10.1227/01.neu.0000431480.87160.84. [DOI] [PubMed] [Google Scholar]
- 41.Machado EO, et al. Prevalence of discordant GH and IGF-I levels in acromegalics at diagnosis, after surgical treatment and during treatment with octreotide LAR. Growth Horm. IGF Res. 2008;18:389–393. doi: 10.1016/j.ghir.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Brzana JA, et al. Discordant growth hormone and IGF-1 levels post pituitary surgery in patients with acromegaly naive to medical therapy and radiation: what to follow, GH or IGF-1 values? Pituitary. 2012;15:562–570. doi: 10.1007/s11102-011-0369-1. [DOI] [PubMed] [Google Scholar]
- 43.Schilbach K, Strasburger CJ, Bidlingmaier M. Biochemical investigations in diagnosis and follow up of acromegaly. Pituitary. 2017;20:33–45. doi: 10.1007/s11102-017-0792-z. [DOI] [PubMed] [Google Scholar]
- 44.Bianchi A, et al. Influence of growth hormone receptor d3 and full-length isoforms on biochemical treatment outcomes in acromegaly. J. Clin. Endocrinol. Metab. 2009;94:2015–2022. doi: 10.1210/jc.2008-1337. [DOI] [PubMed] [Google Scholar]
- 45.Cuevas-Ramos D, et al. A structural and functional acromegaly classification. J. Clin. Endocrinol. Metab. 2015;100:122–131. doi: 10.1210/jc.2014-2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Colao A, Auriemma RS, Pivonello R. The effects of somatostatin analogue therapy on pituitary tumor volume in patients with acromegaly. Pituitary. 2016;19:210–221. doi: 10.1007/s11102-015-0677-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Giustina A, et al. Meta-analysis on the effects of octreotide on tumor mass in acromegaly. PLOS One. 2012;7:e36411. doi: 10.1371/journal.pone.0036411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Potorac I, et al. Pituitary MRI characteristics in 297 acromegaly patients based on T2-weighted sequences. Endocr. Relat. Cancer. 2015;22:169–177. doi: 10.1530/ERC-14-0305. [DOI] [PubMed] [Google Scholar]
- 49.Pivonello R, et al. Complications of acromegaly: cardiovascular, respiratory and metabolic comorbidities. Pituitary. 2017;20:46–62. doi: 10.1007/s11102-017-0797-7. [DOI] [PubMed] [Google Scholar]
- 50.Berg C, et al. Cardiovascular risk factors in patients with uncontrolled and long-term acromegaly: comparison with matched data from the general population and the effect of disease control. J. Clin. Endocrinol. Metab. 2010;95:3648–3656. doi: 10.1210/jc.2009-2570. [DOI] [PubMed] [Google Scholar]
- 51.Frara S, Maffezzoni F, Mazziotti G, Giustina A. Current and emerging aspects of diabetes mellitus in acromegaly. Trends Endocrinol. Metab. 2016;27:470–483. doi: 10.1016/j.tem.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 52.Giustina A, et al. SAGIT(R): clinician-reported outcome instrument for managing acromegaly in clinical practice—development and results from a pilot study. Pituitary. 2016;19:39–49. doi: 10.1007/s11102-015-0681-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van der Lely AJ, et al. Development of ACRODAT(R), a new software medical device to assess disease activity in patients with acromegaly. Pituitary. 2017;20:692–701. doi: 10.1007/s11102-017-0835-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Webb SM, Badia X, Surinach NL, Spanish AcroQol Study, G. Validity and clinical applicability of the acromegaly quality of life questionnaire, AcroQoL: a 6-month prospective study. Eur. J. Endocrinol. 2006;155:269–277. doi: 10.1530/eje.1.02214. [DOI] [PubMed] [Google Scholar]
- 55.Mangupli R, Camperos P, Webb SM. Biochemical and quality of life responses to octreotide-LAR in acromegaly. Pituitary. 2014;17:495–499. doi: 10.1007/s11102-013-0533-x. [DOI] [PubMed] [Google Scholar]
- 56.Chin SO, et al. Change in quality of life in patients with acromegaly after treatment with octreotide LAR: first application of AcroQoL in Korea. BMJ Open. 2015;5:e006898. doi: 10.1136/bmjopen-2014-006898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gadelha MR, Wildemberg LE, Bronstein MD, Gatto F, Ferone D. Somatostatin receptor ligands in the treatment of acromegaly. Pituitary. 2017;20:100–108. doi: 10.1007/s11102-017-0791-0. [DOI] [PubMed] [Google Scholar]
- 58.Kuhn E, Chanson P. Cabergoline in acromegaly. Pituitary. 2017;20:121–128. doi: 10.1007/s11102-016-0782-6. [DOI] [PubMed] [Google Scholar]
- 59.Giustina A, et al. Pegvisomant in acromegaly: an update. J. Endocrinol. Invest. 2017;40:577–589. doi: 10.1007/s40618-017-0614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carmichael JD, Bonert VS, Nuno M, Ly D, Melmed S. Acromegaly clinical trial methodology impact on reported biochemical efficacy rates of somatostatin receptor ligand treatments: a meta-analysis. J. Clin. Endocrinol. Metab. 2014;99:1825–1833. doi: 10.1210/jc.2013-3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Colao A, et al. Pasireotide versus octreotide in acromegaly: a head-to-head superiority study. J. Clin. Endocrinol. Metab. 2014;99:791–799. doi: 10.1210/jc.2013-2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Colao A, Auriemma RS, Pivonello R, Kasuki L, Gadelha MR. Interpreting biochemical control response rates with first-generation somatostatin analogues in acromegaly. Pituitary. 2016;19:235–247. doi: 10.1007/s11102-015-0684-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salvatori R, et al. Effectiveness of self- or partner-administration of an extended-release aqueous-gel formulation of lanreotide in lanreotide-naive patients with acromegaly. Pituitary. 2010;13:115–122. doi: 10.1007/s11102-009-0207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Giustina A, et al. High-dose intramuscular octreotide in patients with acromegaly inadequately controlled on conventional somatostatin analogue therapy: a randomised controlled trial. Eur. J. Endocrinol. 2009;161:331–338. doi: 10.1530/EJE-09-0372. [DOI] [PubMed] [Google Scholar]
- 65.Giustina A, et al. High-dose and high-frequency lanreotide autogel in acromegaly: a randomized, multicenter study. J. Clin. Endocrinol. Metab. 2017;102:2454–2464. doi: 10.1210/jc.2017-00142. [DOI] [PubMed] [Google Scholar]
- 66.Gadelha MR, et al. Pasireotide versus continued treatment with octreotide or lanreotide in patients with inadequately controlled acromegaly (PAOLA): a randomised, phase 3 trial. The lancet. Diabetes Endocrinol. 2014;2:875–884. doi: 10.1016/S2213-8587(14)70169-X. [DOI] [PubMed] [Google Scholar]
- 67.Schmid HA, et al. Effect of pasireotide on glucose- and growth hormone-related biomarkers in patients with inadequately controlled acromegaly. Endocr. 2016;53:210–219. doi: 10.1007/s12020-016-0895-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Melmed S. New therapeutic agents for acromegaly. Nat. Rev. Endocrinol. 2016;12:90–98. doi: 10.1038/nrendo.2015.196. [DOI] [PubMed] [Google Scholar]
- 69.Maffezzoni F, Frara S, Doga M, Mazziotti G, Giustina A. New medical therapies of acromegaly. Growth Horm. IGF Res. 2016;30–31:58–63. doi: 10.1016/j.ghir.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 70.Melmed S, et al. Safety and efficacy of oral octreotide in acromegaly: results of a multicenter phase III trial. J. Clin. Endocrinol. Metab. 2015;100:1699–1708. doi: 10.1210/jc.2014-4113. [DOI] [PubMed] [Google Scholar]
- 71.US National Library of Medicine. ClinicalTrials.govhttps://clinicaltrials.gov/ct2/show/NCT03252353 (2018).
- 72.US National Library of Medicine. ClinicalTrials.govhttps://clinicaltrials.gov/ct2/show/NCT02685709 (2018).
- 73.Sandret L, Maison P, Chanson P. Place of cabergoline in acromegaly: a meta-analysis. J. Clin. Endocrinol. Metab. 2011;96:1327–1335. doi: 10.1210/jc.2010-2443. [DOI] [PubMed] [Google Scholar]
- 74.van der Lely AJ, et al. Long-term treatment of acromegaly with pegvisomant, a growth hormone receptor antagonist. Lancet. 2001;358:1754–1759. doi: 10.1016/s0140-6736(01)06844-1. [DOI] [PubMed] [Google Scholar]
- 75.van der Lely AJ, et al. Long-term safety of pegvisomant in patients with acromegaly: comprehensive review of 1288 subjects in ACROSTUDY. J. Clin. Endocrinol. Metab. 2012;97:1589–1597. doi: 10.1210/jc.2011-2508. [DOI] [PubMed] [Google Scholar]
- 76.Freda PU, et al. Long-term treatment with pegvisomant as monotherapy in patients with acromegaly: Experience from acrostudy. Endocr. Pract. 2015;21:264–274. doi: 10.4158/EP14330.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ragonese M, et al. How to improve effectiveness of pegvisomant treatment in acromegalic patients. J. Endocrinol. Invest. 2017;41:575–581. doi: 10.1007/s40618-017-0773-0. [DOI] [PubMed] [Google Scholar]
- 78.Sievers C, et al. Prediction of therapy response in acromegalic patients under pegvisomant therapy within the German ACROSTUDY cohort. Pituitary. 2015;18:916–923. doi: 10.1007/s11102-015-0673-2. [DOI] [PubMed] [Google Scholar]
- 79.Franck SE, et al. A multivariable prediction model for pegvisomant dosing: monotherapy and in combination with long-acting somatostatin analogues. Eur. J. Endocrinol. 2017;176:421–430. doi: 10.1530/EJE-16-0956. [DOI] [PubMed] [Google Scholar]
- 80.van der Lely AJ, et al. Treatment with high doses of pegvisomant in 56 patients with acromegaly: experience from ACROSTUDY. Eur. J. Endocrinol. 2016;175:239–245. doi: 10.1530/EJE-16-0008. [DOI] [PubMed] [Google Scholar]
- 81.Neggers SJ, de Herder WW, Janssen JA, Feelders RA, van der Lely AJ. Combined treatment for acromegaly with long-acting somatostatin analogs and pegvisomant: long-term safety for up to 4.5 years (median 2.2 years) of follow-up in 86 patients. Eur. J. Endocrinol. 2009;160:529–533. doi: 10.1530/EJE-08-0843. [DOI] [PubMed] [Google Scholar]
- 82.Neggers SJ, et al. Long-term efficacy and safety of pegvisomant in combination with long-acting somatostatin analogs in acromegaly. J. Clin. Endocrinol. Metab. 2014;99:3644–3652. doi: 10.1210/jc.2014-2032. [DOI] [PubMed] [Google Scholar]
- 83.Muhammad A, et al. What is the efficacy of switching to weekly pegvisomant in acromegaly patients well controlled on combination therapy? Eur. J. Endocrinol. 2016;174:663–667. doi: 10.1530/EJE-15-1150. [DOI] [PubMed] [Google Scholar]
- 84.Tritos NA, et al. Effectiveness of first-line pegvisomant monotherapy in acromegaly: an ACROSTUDY analysis. Eur. J. Endocrinol. 2017;176:213–220. doi: 10.1530/EJE-16-0697. [DOI] [PubMed] [Google Scholar]
- 85.Stone JC, Clark J, Cuneo R, Russell AW, Doi SA. Estrogen and selective estrogen receptor modulators (SERMs) for the treatment of acromegaly: a meta-analysis of published observational studies. Pituitary. 2014;17:284–295. doi: 10.1007/s11102-013-0504-2. [DOI] [PubMed] [Google Scholar]
- 86.Balili I, Barkan A. Tamoxifen as a therapeutic agent in acromegaly. Pituitary. 2014;17:500–504. doi: 10.1007/s11102-013-0534-9. [DOI] [PubMed] [Google Scholar]
- 87.Duarte FH, Jallad RS, Bronstein MD. Clomiphene citrate for treatment of acromegaly not controlled by conventional therapies. J. Clin. Endocrinol. Metab. 2015;100:1863–1869. doi: 10.1210/jc.2014-3913. [DOI] [PubMed] [Google Scholar]
- 88.Ritvonen E, et al. Mortality in acromegaly: a 20-year follow-up study. Endocr. Relat. Cancer. 2015;23:469–480. doi: 10.1530/ERC-16-0106. [DOI] [PubMed] [Google Scholar]
- 89.Maione L, et al. Changes in the management and comorbidities of acromegaly over three decades: the French Acromegaly Registry. Eur. J. Endocrinol. 2017;176:645–655. doi: 10.1530/EJE-16-1064. [DOI] [PubMed] [Google Scholar]
- 90.Ayuk J, et al. Growth hormone and pituitary radiotherapy, but not serum insulin-like growth factor-I concentrations, predict excess mortality in patients with acromegaly. J. Clin. Endocrinol. Metab. 2004;89:1613–1617. doi: 10.1210/jc.2003-031584. [DOI] [PubMed] [Google Scholar]
- 91.Sherlock M, et al. ACTH deficiency, higher doses of hydrocortisone replacement, and radiotherapy are independent predictors of mortality in patients with acromegaly. J. Clin. Endocrinol. Metab. 2009;94:4216–4223. doi: 10.1210/jc.2009-1097. [DOI] [PubMed] [Google Scholar]
- 92.Jaffrain-Rea ML, et al. Impact of successful transsphenoidal surgery on cardiovascular risk factors in acromegaly. Eur. J. Endocrinol. 2003;148:193–201. doi: 10.1530/eje.0.1480193. [DOI] [PubMed] [Google Scholar]
- 93.Colao A, Auriemma RS, Galdiero M, Lombardi G, Pivonello R. Effects of initial therapy for five years with somatostatin analogs for acromegaly on growth hormone and insulin-like growth factor-I levels, tumor shrinkage, and cardiovascular disease: a prospective study. J. Clin. Endocrinol. Metab. 2009;94:3746–3756. doi: 10.1210/jc.2009-0941. [DOI] [PubMed] [Google Scholar]
- 94.Kuhn E, et al. Long-term effects of pegvisomant on comorbidities in patients with acromegaly: a retrospective single-center study. Eur. J. Endocrinol. 2015;173:693–702. doi: 10.1530/EJE-15-0500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Colao A, et al. Efficacy of 12-month treatment with the GH receptor antagonist pegvisomant in patients with acromegaly resistant to long-term, high-dose somatostatin analog treatment: effect on IGF-I levels, tumor mass, hypertension and glucose tolerance. Eur. J. Endocrinol. 2006;154:467–477. doi: 10.1530/eje.1.02112. [DOI] [PubMed] [Google Scholar]
- 96.Maione L, et al. No evidence of a detrimental effect of cabergoline therapy on cardiac valves in patients with acromegaly. J. Clin. Endocrinol. Metab. 2012;97:E1714–1719. doi: 10.1210/jc.2012-1833. [DOI] [PubMed] [Google Scholar]
- 97.Wassenaar MJ, et al. High prevalence of vertebral fractures despite normal bone mineral density in patients with long-term controlled acromegaly. Eur. J. Endocrinol. 2011;164:475–483. doi: 10.1530/EJE-10-1005. [DOI] [PubMed] [Google Scholar]
- 98.Claessen KM, et al. Progression of vertebral fractures despite long-term biochemical control of acromegaly: a prospective follow-up study. J. Clin. Endocrinol. Metab. 2013;98:4808–4815. doi: 10.1210/jc.2013-2695. [DOI] [PubMed] [Google Scholar]
- 99.Bonadonna S, et al. Increased prevalence of radiological spinal deformities in active acromegaly: a cross-sectional study in postmenopausal women. J. Bone Miner. Res. 2005;20:1837–1844. doi: 10.1359/JBMR.050603. [DOI] [PubMed] [Google Scholar]
- 100.Mazziotti G, et al. Prevalence of vertebral fractures in men with acromegaly. J. Clin. Endocrinol. Metab. 2008;93:4649–4655. doi: 10.1210/jc.2008-0791. [DOI] [PubMed] [Google Scholar]
- 101.Mazziotti G, et al. Bone turnover, bone mineral density, and fracture risk in acromegaly: a meta-analysis. J. Clin. Endocrinol. Metab. 2015;100:384–394. doi: 10.1210/jc.2014-2937. [DOI] [PubMed] [Google Scholar]
- 102.Parkinson C, Kassem M, Heickendorff L, Flyvbjerg A, Trainer PJ. Pegvisomant-induced serum insulin-like growth factor-I normalization in patients with acromegaly returns elevated markers of bone turnover to normal. J. Clin. Endocrinol. Metab. 2003;88:5650–5655. doi: 10.1210/jc.2003-030772. [DOI] [PubMed] [Google Scholar]
- 103.Mazziotti G, Chiavistelli S, Giustina A. Pituitary diseases and bone. Endocrinol. Metab. Clin. North Am. 2015;44:171–180. doi: 10.1016/j.ecl.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 104.Silva PPB, et al. Bone microarchitecture and estimated bone strength in men with active acromegaly. Eur. J. Endocrinol. 2017;177:409–420. doi: 10.1530/EJE-17-0468. [DOI] [PubMed] [Google Scholar]
- 105.Attal P, Chanson P. Endocrine aspects of obstructive sleep apnea. J. Clin. Endocrinol. Metab. 2010;95:483–495. doi: 10.1210/jc.2009-1912. [DOI] [PubMed] [Google Scholar]
- 106.Mazziotti G, et al. Effects of somatostatin analogs on glucose homeostasis: a metaanalysis of acromegaly studies. J. Clin. Endocrinol. Metab. 2009;94:1500–1508. doi: 10.1210/jc.2008-2332. [DOI] [PubMed] [Google Scholar]
- 107.Drake WM, et al. Insulin sensitivity and glucose tolerance improve in patients with acromegaly converted from depot octreotide to pegvisomant. Eur. J. Endocrinol. 2003;149:521–527. doi: 10.1530/eje.0.1490521. [DOI] [PubMed] [Google Scholar]
- 108.Higham CE, Rowles S, Russell-Jones D, Umpleby AM, Trainer PJ. Pegvisomant improves insulin sensitivity and reduces overnight free fatty acid concentrations in patients with acromegaly. J. Clin. Endocrinol. Metab. 2009;94:2459–2463. doi: 10.1210/jc.2008-2086. [DOI] [PubMed] [Google Scholar]
- 109.Rokkas T, Pistiolas D, Sechopoulos P, Margantinis G, Koukoulis G. Risk of colorectal neoplasm in patients with acromegaly: a meta-analysis. World J. Gastroenterol. 2008;14:3484–3489. doi: 10.3748/wjg.14.3484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lois K, et al. The role of colonoscopic screening in acromegaly revisited: review of current literature and practice guidelines. Pituitary. 2015;18:568–574. doi: 10.1007/s11102-014-0586-5. [DOI] [PubMed] [Google Scholar]
- 111.Theodoropoulou M, Stalla GK. Somatostatin receptors: from signaling to clinical practice. Front. Neuroendocrinol. 2013;34:228–252. doi: 10.1016/j.yfrne.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 112.Bevan JS. Clinical review: The antitumoral effects of somatostatin analog therapy in acromegaly. J. Clin. Endocrinol. Metab. 2005;90:1856–1863. doi: 10.1210/jc.2004-1093. [DOI] [PubMed] [Google Scholar]
- 113.Melmed S, et al. A critical analysis of pituitary tumor shrinkage during primary medical therapy in acromegaly. J. Clin. Endocrinol. Metab. 2005;90:4405–4410. doi: 10.1210/jc.2004-2466. [DOI] [PubMed] [Google Scholar]
- 114.Caron PJ, et al. Tumor shrinkage with lanreotide Autogel 120 mg as primary therapy in acromegaly: Results of a prospective multicenter clinical trial. J. Clin. Endocrinol. Metab. 2014;99:1282–1290. doi: 10.1210/jc.2013-3318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mazziotti G, Giustina A. Effects of lanreotide SR and Autogel on tumor mass in patients with acromegaly: a systematic review. Pituitary. 2010;13:60–67. doi: 10.1007/s11102-009-0169-z. [DOI] [PubMed] [Google Scholar]
- 116.Daly AF, et al. Clinical characteristics and therapeutic responses in patients with germ-line AIP mutations and pituitary adenomas: an international collaborative study. J. Clin. Endocrinol. Metab. 2010;95:E373–E383. doi: 10.1210/jc.2009-2556. [DOI] [PubMed] [Google Scholar]
- 117.Beckers A, et al. X-Linked acrogigantism syndrome: clinical profile and therapeutic responses. Endocr. Relat. Cancer. 2015;22:353–367. doi: 10.1530/ERC-15-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hernandez-Ramirez LC, et al. Landscape of familial isolated and young-onset pituitary adenomas: Prospective diagnosis in AIP mutation carriers. J. Clin. Endocrinol. Metab. 2015;100:E1242–E1254. doi: 10.1210/jc.2015-1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Carlsen SM, et al. Preoperative octreotide treatment in newly diagnosed acromegalic patients with macroadenomas increases cure short-term postoperative rates: a prospective, randomized trial. J. Clin. Endocrinol. Metab. 2008;93:2984–2990. doi: 10.1210/jc.2008-0315. [DOI] [PubMed] [Google Scholar]
- 120.Nunes VS, Correa JM, Puga ME, Silva EM, Boguszewski CL. Preoperative somatostatin analogues versus direct transsphenoidal surgery for newly-diagnosed acromegaly patients: a systematic review and meta-analysis using the GRADE system. Pituitary. 2015;18:500–508. doi: 10.1007/s11102-014-0602-9. [DOI] [PubMed] [Google Scholar]
- 121.Fleseriu M, Hoffman AR, Katznelson L, AACE Neuroendocrine and Pituitary Scientific Committee American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: management of acromegaly patients: what is the role of pre-operative medical therapy? Endocr. Pract. 2015;21:668–673. doi: 10.4158/EP14575.DSCR. [DOI] [PubMed] [Google Scholar]
- 122.Buhk JH, et al. Tumor volume of growth hormone-secreting pituitary adenomas during treatment with pegvisomant: a prospective multicenter study. J. Clin. Endocrinol. Metab. 2010;95:552–558. doi: 10.1210/jc.2009-1239. [DOI] [PubMed] [Google Scholar]
- 123.Marazuela M, et al. Somatotroph tumor progression during pegvisomant therapy: a clinical and molecular study. J. Clin. Endocrinol. Metab. 2011;96:E251–E259. doi: 10.1210/jc.2010-1742. [DOI] [PubMed] [Google Scholar]
- 124.Brzana J, Yedinak CG, Gultekin SH, Delashaw JB, Fleseriu M. Growth hormone granulation pattern and somatostatin receptor subtype 2A correlate with postoperative somatostatin receptor ligand response in acromegaly: a large single center experience. Pituitary. 2013;16:490–498. doi: 10.1007/s11102-012-0445-1. [DOI] [PubMed] [Google Scholar]
- 125.Kiseljak-Vassiliades K, et al. Growth hormone tumor histological subtypes predict response to surgical and medical therapy. Endocr. 2015;49:231–241. doi: 10.1007/s12020-014-0383-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Puig-Domingo M, et al. Magnetic resonance imaging as a predictor of response to somatostatin analogs in acromegaly after surgical failure. J. Clin. Endocrinol. Metab. 2010;95:4973–4978. doi: 10.1210/jc.2010-0573. [DOI] [PubMed] [Google Scholar]
- 127.Neto LV, et al. Expression analysis of dopamine receptor subtypes in normal human pituitaries, nonfunctioning pituitary adenomas and somatotropinomas, and the association between dopamine and somatostatin receptors with clinical response to octreotide-LAR in acromegaly. J. Clin. Endocrinol. Metab. 2009;94:1931–1937. doi: 10.1210/jc.2008-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Melmed S. Pituitary medicine from discovery to patient-focused outcomes. J. Clin. Endocrinol. Metab. 2016;101:769–777. doi: 10.1210/jc.2015-3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dillard TH, et al. Temozolomide for corticotroph pituitary adenomas refractory to standard therapy. Pituitary. 2011;14:80–91. doi: 10.1007/s11102-010-0264-1. [DOI] [PubMed] [Google Scholar]