ABSTRACT
Background
Although it is recommended that childcare centers provide foods consistent with dietary guidelines, the impact of implementing sector-specific guidelines on child outcomes is largely unknown.
Objectives
This study aims to examine the impact of a web-based program and support to implement dietary guidelines in childcare centers on children's 1) diet; 2) BMI z scores; and 3) child health-related quality of life (HRQoL).
Methods
This study was a cluster-randomized controlled trial utilizing a Type-3 Hybrid implementation-effectiveness design conducted between October 2016 and March 2018. This study reports on child outcomes. Fifty-four childcare centers in New South Wales, Australia were randomly assigned to the intervention (a web-based menu-planning tool and support) or control group (usual care). The intervention was designed to address barriers and enablers to dietary guideline implementation according to the Theoretical Domains Framework. A quota of 35 consenting childcare centers undertook child-level evaluation of dietary intake where 522 parents consented to completing ≥1 component of data collection for their child. Child consumption of core and discretionary (unhealthy) foods while in care was assessed via dietary observations by blinded research assistants, childcare diet quality was assessed via educator-completed questionnaires, BMI z scores were assessed via measured weight and height, and child HRQoL was assessed via parent report at baseline and 12-mo follow-up.
Results
There was a significant increase in mean child consumption of fruit (0.39 servings; 95% CI: 0.12, 0.65 servings) and dairy foods (0.38 servings; 95% CI: 0.19, 0.57 servings) and a significant reduction in consumption of discretionary foods (−0.40 servings; 95% CI: −0.64, −0.16 servings) in care in the intervention group, relative to control at 12-mo follow-up. No significant differences were observed in diet quality, BMI z scores, or HRQoL.
Conclusions
A web-based intervention to support planning of childcare menus consistent with dietary guidelines can improve child consumption of healthier foods in daycare. This trial was registered at www.anzctr.org.au as ACTRN12616000974404.
Keywords: child diet, obesity, public health nutrition, intervention, childcare centers, dietary guidelines
Introduction
In 2016 the WHO estimated that ∼41 million young children aged <5 y were overweight and obese (1). Children who are overweight or obese are more likely to be overweight as adults (2), increasing their lifetime risk of coronary artery disease, hypertension, type 2 diabetes, osteoarthritis, and some cancers (3, 4). As such, the WHO has called for urgent action to reduce the primary modifiable risk factors for excessive weight gain including poor diet (1). Early childhood is a critical period for developing healthy eating behaviors, with food preferences established in childhood tracking into later life (5–7). However, >90% of preschool-aged children in Australia and the United States do not consume their recommended servings of vegetables, and almost all consume excessive amounts of unhealthy foods (8, 9).
Childcare centers are an important setting for the delivery of population-wide nutrition initiatives because they provide broad reach to young children (10). Leading health organizations (11, 12) and governments, internationally (13, 14) and in Australia (15), recommend that childcare centers provide foods consistent with national dietary guidelines to promote healthy eating.
Although systematic reviews suggest that increasing the availability of healthy foods in childcare centers may improve child diet (16, 17), there have been few rigorous evaluations of food service–based interventions that target the implementation of sector-specific dietary guidelines on childcare menus. A Cochrane systematic review in 2016 identified just 1 quasi-experimental trial that assessed the impact of a food service–based intervention, which included face-to-face training of cooks and monthly site visits by dietitians in 9 Head Start centers, on reducing the saturated fat content of meals consistent with the US Dietary Guidelines (18). Evaluation with 1296 children found significant reductions in child consumption of energy from saturated fat from meals consumed in childcare at 1-y follow-up, as assessed via direct observations (P < 0.001) (19). A randomized controlled trial (RCT) conducted by the research team since publication of the review (20) used a multicomponent 6-mo food-service intervention targeting cooks, which included provision of training and resources, audit and feedback, face-to-face or telephone support by dietitians, and securing executive support from childcare managers. The study reported significant improvements in fruit (P = 0.014) and vegetable (P < 0.001) consumption measured via aggregate plate waste measures with 45 centers. Such findings suggest that food service–based interventions which include provision of training and ongoing support to childcare cooks may be effective in increasing provision of healthier foods and improving child diet. These interventions, however, have utilized resource-intensive, face-to-face approaches delivered by specialist staff, which are likely to have limited reach (20). Effective interventions in this setting need to be amenable to delivery at scale to produce meaningful improvements to child health (18).
As such, this study aims to examine the impact of an implementation intervention consisting primarily of a web-based menu-planning tool, with support targeting cooks to improve the provision of foods in childcare centers in accordance with dietary guidelines, on 1) child dietary intake in care (servings of core food groups and discretionary foods); 2) child diet quality score in care; 3) child BMI z scores; and 4) child health-related quality of life (HRQoL). The web-based method was selected to overcome the reach limitations of previous interventions in this setting and provide an opportunity for scaling up at a population level.
Methods
Ethical approval was obtained from Hunter New England (16/02/17/4.05) and the University of Newcastle (H-2016-0111) Human Research Ethics Committees. Owing to the number of preregistered outcomes, the primary outcome (implementation of guidelines) has been reported in a separate publication. Briefly, there were no significant differences between intervention and control centers in terms of full implementation of dietary guidelines (i.e., meeting guideline recommendations for all 5 core food groups and discretionary foods). However, childcare centers in the intervention group provided significantly more servings of fruit (P < 0.001), vegetables (P = 0.03), dairy (P = 0.03), and meat (P = 0.003), and reduced servings of discretionary foods (P = 0.02) on their menus, compared with control centers at 3 mo. This was maintained for fruit (P = 0.03) and discretionary foods (P = 0.003) at 12 mo (21). This study reports on prospectively registered child outcomes. The reporting of this study adheres to the CONSORT guidelines (22).
Design and setting
This study is a cluster-randomized controlled trial utilizing a Type-3 Hybrid implementation-effectiveness design (23) to examine the impact of an intervention to increase the implementation of dietary guidelines in 54 childcare centers in New South Wales, Australia on child-level outcomes (24). Such approaches of embedding evaluation of child-level health outcomes within implementation trials have been recommended as a strategy to address existing evidence gaps and provide more valid estimates of potential clinical effectiveness of sector-specific guidelines, and can reduce the time it takes to translate effective guidelines into practice (23). Data collection to assess the impact of the intervention on child diet was undertaken with 35 out of the 54 centers recruited to the trial, and is reported here. Centers were approached in random order to reach a quota of 35 consenting centers. This number of services and children was determined based on sample size calculations to detect a meaningful difference and judged as feasible by the research team. Outcome data were collected at baseline and 12-mo follow-up using a repeat cross-sectional assessment. Repeat cross-sectional assessments are recommended where the impact of the intervention is expected at the setting level (i.e., childcare centers) and where high attrition of participants is expected (25, 26). The repeat cross-sectional design also allows us to describe the impact of the settings-based intervention on the children who are exposed to the intervention, where dietary improvement is expected to occur.
Participants
Eligible centers were required to 1) be users of our partner provider's childcare online reporting software (HubWorks; HubCare ANZ) (∼15% of all childcare services in NSW); 2) prepare and provide ≥1 main and ≥2 mid-meals to children onsite; 3) make menu-planning decisions onsite; and 4) have a menu planner (typically a cook) with sufficient English to engage with the intervention. Centers were excluded if they outsourced menu-planning decisions, catered exclusively for special needs children, or were run by the NSW Department of Education because such services had different operational and catering arrangements.
Eligible children were required to 1) be aged 2–6 y; 2) be present at the center on days of data collection; 3) have no dietary requirements preventing consumption of foods while in care; and 4) have parental consent.
Recruitment
All childcare centers were posted an invitation letter and information statement about the study ∼2 wk before receiving a call from a research assistant to assess eligibility and obtain consent. The first 40 childcare centers (oversampling to obtain 35) were asked during the call if they consented to a 1-d site visit. These centers were asked to distribute information and consent forms to parents of children in the room with the highest number of children aged 2–6 y before the scheduled site visit. Consistent with previous approaches by the research team and to maximize consent (27), research assistants also approached parents at drop-off on the day of the visit.
Randomization and allocation
Centers were randomly assigned after baseline data collection to the intervention or control group in a 1:1 ratio and stratified by socioeconomic status based on Socio-Economic Indexes for Areas (28) classifications using the childcare center's postcode (high/low) by an independent statistician using a random number function in Microsoft Excel 2010. All outcome data assessors were blinded to group allocation. Childcare staff and those delivering the intervention were aware of group allocation; however, parents were not explicitly informed of center allocation.
Intervention
The intervention has been described in detail in a previously published protocol (24). The web-intervention (“feedAustralia”) was planned to be embedded in a mandatory reporting software program [Childcare Management System (CCMS)] developed by the partner provider (24). This was not able to be carried out due to childcare reform at the essential time of integration with CCMS. As a consequence, a stand-alone program was developed allowing childcare centers to access the menu-planning intervention outside of CCMS. To increase uptake of the web-program, design features and strategies targeting the constructs of the Technology Acceptance Model were applied (29) (see Table 1). The intervention was designed to address primary barriers to guideline implementation identified by application of the Theoretical Domains Framework similar to that previously used in an effective intervention by the research team to improve dietary guideline implementation and child diet (20, 30, 31). The 12-mo implementation intervention components are briefly described below:
TABLE 1.
Application of strategies to address constructs in TAM1
| TAM construct | Definition | Strategies |
|---|---|---|
| Perceived ease of use | “the degree to which a person believes that using IT will be free of effort” | • Extensive pilot testing with 5 diverse services to ensure ease of use of recipe entry function, and acceptability of web-interface• Provision of a database of 200 recipes that can be easily added to the menu• Onsite training with childcare managers and menu planners• Provision of comprehensive online resources to support use of the program• Follow-up telephone phone calls to support use of the program as needed• Provision of computer tablets connected to the Internet to facilitate use as required. |
| Perceived usefulness | “the extent to which a person believes that using a new technology will enhance his or her job performance” | • Extensive pilot testing with 5 diverse services to assess the types of functionality that would be most useful to assist menu planners and managers• Automating tasks that menu planners and managers already undertake including review of menus, printing menus, collating recipes, and providing menu information to parents• Seeking managerial support regarding the importance of using the program• Increases accuracy of menu review processes and provides real-time feedback regarding compliance• Provision of menu templates, sample weekly menus that can be easily tailored to meet the needs of the service• Menus and assessment of compliance can be displayed automatically to parents, consistent with service accreditation standards. |
IT, information technology; TAM, Technology Acceptance Model.
Web-based menu-planning program (“feedAustralia”): The program undertook automated assessments on meals and snacks entered by menu planners and provided real-time feedback on the number of servings of each of the core food groups and discretionary foods (32). The feedback also outlined whether the menu was compliant with that recommended by sector-specific nutrition guidelines (32). The calculation of compliance was underpinned by a national nutrition database containing food group and nutrient information developed by the research team (33).
Provision of educational resources: Where menus were not compliant, the program automatically provided childcare centers with suggestions and recipes on how to modify the menus to meet guidelines. The online menu-planning tool (“feedAustralia”) also included >200 healthy recipes that met the guidelines for inclusion in childcare menus as well as complete 1-wk sample menus that were compliant with guidelines.
Reminders: Childcare centers were also prompted fortnightly in the main CCMS to make changes to their menu to increase compliance if noncompliant, or if they had an incomplete menu in the program.
Training, educational resources, and managerial support: A health promotion officer with experience using the program conducted a 3-h training session with the supervisor and menu planner within each childcare service. The training consisted of updating centers with sector-specific nutrition guidelines, the main features of the online menu-planning program and how to use them, and supporting the service to make changes to their menu. To generate service-level support for use of the program, the health promotion officer also undertook action planning to ensure that allocated time and resources were provided to the menu planner to access the program. Centers were also provided with a portable tablet to facilitate access to the program and recipes during food preparation processes.
Ongoing support: Ongoing support was provided over 2–4 phone calls to childcare service cooks. The purpose of these calls was to provide technical support with using the program and overcome any reported barriers to using the program. The number of phone calls provided to each service was tailored depending on engagement with the program and menu compliance as assessed via analytics data collected via the program. Centers could also seek support via an online “helpdesk” feature available within the program. The helpdesk feature, however, was poorly accessed with no center accessing this.
Control group
Control centers received usual care. All centers in the state (New South Wales) have access to nutrition guidelines and menu-planning tools (34) and may also receive additional nutrition support from their local health promotion team as part of a state-wide government-funded obesity prevention program (35). To preclude intervention contamination, centers were not provided with any of the aforementioned intervention components and could not access the web-based menu-planning tool.
Data collection procedures and measures
Baseline (October 2016–April 2017) and follow-up data were collected ∼12 mo apart (October 2017–March 2018), staggered due to the geographical spread of the centers and center availability. Parents from 35 centers consented to 1) having research assistants observe their child's food intake in care (dietary observations), 2) having their child's weight and height measured, and 3) completing a survey. Parents could consent to undertake either component of data collection.
To minimize selection bias, research assistants blinded to center allocation sought consent for dietary observations from all parents. After obtaining consent, research assistants randomly selected 6–9 children per center for dietary observations because 1 individual could only observe ≤3 children each. Parents of children selected for dietary observations were asked to report their child's dietary intake outside of care via an online or telephone survey. The remaining parents were asked to complete a telephone survey reporting on their child's HRQoL. To reduce respondent burden, parents completed only questions related to child dietary intake or HRQoL, not both. In addition, educators were asked to complete a questionnaire for each consenting child, reporting on child diet quality, which was developed and validated by the research team for the purpose of this study (36).
Outcomes
The prospectively registered child-level outcomes were:
1) Number of servings of the 5 core and discretionary food groups defined by the Australian Guide to Healthy Eating (AGHE) (37) consumed in care (see Table2 for food group serving sizes)
TABLE 2.
Recommended daily intake of food groups for children in care according to the Caring for Children resources
| Food group | Recommended daily servings1 | How is 1 serving defined?2 |
|---|---|---|
| Vegetables and legumes/beans | 2 | 75 g (100–350 kJ) (½ cup cooked vegetables, 1 cup raw salad vegetables) |
| Fruit | 1 | 150 g (350 kJ) (1 medium apple, 2 small apricots, 1 cup diced fruit) |
| Whole-grain-cereal foods and breads | 2 | 500 kJ (1 slice of bread, ½ cup cooked rice) |
| Lean meat and poultry, fish, eggs, tofu, seeds, and legumes | 0.75 | 500–600 kJ (65 g cooked lean red meat, 1 large egg, 1 cup canned legumes) |
| Milk, yogurt, cheese, and alternatives | 1 | 500–600 kJ (1 cup milk, ¾ cup yogurt, 40 g hard cheese) |
Number of servings recommended to be provided across an 8-h period of care for children aged 2–5 y according to the Caring for Children guidelines 2014.
According to the Caring for Children guidelines 2014 and Australian Dietary Guidelines.
Trained blinded research assistants observed child food consumption in care for 8 h, using an adapted protocol of the Dietary Observation for ChildCare food record tool (38). Direct observations are the gold standard for assessing dietary intake in care given the amount of spillage and food sharing that occur in this setting (38). The research assistants documented the types and portions of foods and beverages served and remaining at the end of each meal for 3 children each. Intake was calculated as the amount of foods served minus foods wasted or remaining. The data were entered into FoodWorks version 9 (Xyris) and converted into servings of food groups by a dietitian using the menu-planning program. All research assistants attended a half-day training course conducted by dietitians with experience undertaking dietary observations in childcare centers. Before undertaking data collection, research assistants needed to score >90% on a certification test estimating the food groups and serving sizes of 5 plates of food frequently served in childcare. Repeated training and testing were undertaken for those who failed to obtain the required level of proficiency.
2) Childcare educator–reported child diet quality
Child diet quality was assessed using a modified version of a Short Food Survey previously validated in a sample of Australian children, completed by educators for children aged 2–6 y within each room (39). An additional 9 items were added to this survey to enhance estimation of serving sizes and to overcome limitations previously reported by the authors. The final questionnaire consisted of 47 items, assessing frequency and portion sizes of each AGHE food group, the number of times discretionary food was consumed, variety, and the quality of foods (e.g., wholemeal/wholegrain cereals, lean meats) consumed by an individual child (36). Educators were provided with a picture of example serving sizes to help with estimating intake. Diet quality scores consisted of the total score from 10 domains with a maximum score of 10 for each domain (total of 100 for the best possible diet quality).
3) Child BMI z scores
Child height and weight were objectively measured in the childcare center by trained research assistants using a standardized protocol (40). Weight and height were measured using a calibrated digital scale (NUWEIGH LOF842) and standing portable stadiometer (Charder HM 200P) on a hard, flat surface. Two measurements of weight and height were taken, and the means of each were used. BMI was calculated as kg/m2, with BMI z scores calculated according to age and sex (41). Children were grouped into healthy weight (5th–85th percentile) and nonhealthy weight (>85th percentile) (4).
4) Child HRQoL
Consenting parents whose children were not randomly selected for dietary observation completed the HRQoL telephone interview. Parents were asked to complete the parent proxy version of the KIDSCREEN-10, an 11-item generic HRQoL measure for children (42). KIDSCREEN-10 can be used to assess changes in trials (43) and has demonstrated reliability and validity (42). Each item is scored on a 5-point Likert scale with higher scales representing better HRQoL. Items were summed to create a score out of 100.
5) Child diet outside of care
For children selected for dietary observations, parents also completed a 50-item online or telephone survey reporting only on child diet outside of care to allow for assessment of compensatory dietary intake (i.e., whether children changed their diets outside of care) as a result of receiving the intervention. The survey was based on a previously validated survey in young children (39).
Other data
Child demographics
Parents reported their child's sex, date of birth, and number of days attending the center via the parental consent forms.
Sample size calculations
Prospective sample size calculations were only undertaken for child consumption of core and discretionary food groups and as such are considered the primary outcome for this article. We aimed to recruit 204 children (6 children selected per center from 34 centers) to enable the detection of differences of between 0.4 and 0.8 servings for each core food group [assuming an intracluster correlation coefficient (ICC) of 0.4 and an SD between 0.4 and 0.9 based on our previous study] and 0.2 servings for discretionary foods (assuming an ICC of 0.1 and SD of 0.4), with an α of 0.01 (accounting for multiple dietary outcomes) and 80% power. Improvements of this magnitude for fruit and vegetables are suggested to be associated with reductions in risk of chronic disease (44, 45).
Statistical analysis
All analyses were undertaken using SAS version 9.3 (SAS Institute). For continuous outcomes, group differences were assessed through a group-by-time interaction in mixed-effects linear regression models, which included a random effect to account for potential clustering. For dichotomous outcomes, a logistic regression adjusting for baseline scores and clustering was undertaken. A complete-case analysis was performed using all available data at follow-up, with these data presented as the primary analysis. In addition, an intention-to-treat analysis was undertaken, through the use of multiple imputation at the level of center for missing data at follow-up, with the MI Procedure (46). All statistical analyses were 2-tailed with an α value of 0.01.
Results
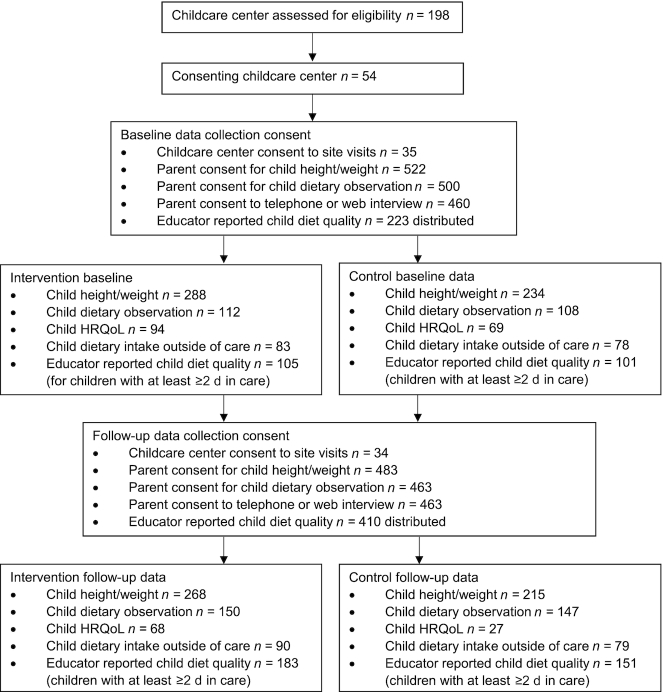
Of the 54 childcare centers consenting to the primary trial, the first 40 centers were approached in random order to participate in the current study. The first 35 centers who consented (65%) received a site visit to undertake child-level data collection (see Figure 1).
FIGURE 1.
CONSORT diagram flowchart of participants. HRQoL, health-related quality of life.
At baseline, 63.4% of parents consented to their child's height and weight being measured (n = 522); 60.8% consented to dietary observations (n = 500); and 55.9% consented to complete a survey (n = 460). At 12-mo follow-up, 1 childcare center had withdrawn from the study (see Figure 1); 63.1% of parents consented to height and weight measurements (n = 483); 60.4% consented to dietary observations (n = 463); and 60.4% consented to complete a survey (n = 463). At baseline, 206 educators (92.4%) completed the dietary survey and at follow-up 81.5% (n = 334) returned a survey.
Table 3 presents demographic characteristics of children whose parents consented to ≥1 data collection component.
TABLE 3.
Child demographics reported by parents at baseline and follow-up1
| Baseline (n = 522) | 12-mo follow-up (n = 483) | |
|---|---|---|
| Child age | 4.6 y ± 8.2 mo | 4.5 y ± 8.8 mo |
| Child sex female | 258 (49.6) | 222 (46.8) |
| Attendance at childcare center, d/wk | 3.25 ± 1.1 | 3.36 ± 1.12 |
| Children who attend for ≥3 d/wk | 381 (73.0) | 284 (60.3) |
Values are mean ± SD or n (%).
Child dietary intake (via observations and parent report)
At 12-mo follow-up, children attending intervention centers consumed significantly more fruit (0.39 servings; P = 0.005) and dairy (0.38 servings; P < 0.001) and significantly fewer discretionary items (−0.40; P = 0.002) and servings of breads and cereals (−0.62; P < 0.001) than the control group (see Table 4). There were no significant differences in child consumption of vegetables (0.05, P = 0.66) and meat/meat alternatives (0.04, P = 0.59), relative to the control group. Parents reported on child dietary intake outside of care and found no compensatory dietary behaviors for consumption of core (P = 0.15–0.84) and discretionary foods (P = 0.09).
TABLE 4.
Intervention impact on child diet, BMI z scores, and HRQoL at ∼12 mo postintervention1
| Intervention | Control | Complete case analysis2 | Multiple imputation analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 12-mo follow-up | Baseline | 12-mo follow-up | Intervention vs. control differential change | Intervention vs. control differential change | ||||
| Outcomes | ICC | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Effect size (95% CI) | P value | Effect size (95% CI) | P value |
| Child consumption as assessed via direct observations3 (baseline: n = 220; follow-up: n = 297) | |||||||||
| Vegetables, servings | 0.3 | 0.65 ± 0.63 | 0.73 ± 0.72 | 0.56 ± 0.53 | 0.57 ± 0.54 | 0.02 (−0.19, 0.23) | 0.85 | 0.05 (−0.16, 0.25) | 0.66 |
| Fruit, servings | 0.4 | 0.72 ± 0.77 | 0.86 ± 0.72 | 0.79 ± 1.09 | 0.57 ± 0.66 | 0.39 (0.12, 0.65) | 0.005* | 0.38 (0.12, 0.63) | 0.003* |
| Cereals and breads, servings | 0.4 | 1.50 ± 1.04 | 1.10 ± 0.72 | 1.26 ± 0.64 | 1.43 ± 0.99 | −0.62 (−0.89, −0.35) | <0.001* | −0.57 (−0.83, −0.31) | <0.001* |
| Meat and alternatives, servings | 0.6 | 0.41 ± 0.66 | 0.51 ± 0.64 | 0.30 ± 0.38 | 0.35 ± 0.45 | 0.01 (−0.13, 0.16) | 0.86 | 0.04 (−0.10, 0.18) | 0.59 |
| Dairy and alternatives, servings | 0.4 | 0.59 ± 0.66 | 0.66 ± 0.56 | 0.88 ± 0.58 | 0.56 ± 0.57 | 0.38 (0.19, 0.57) | <0.001* | 0.41 (0.22, 0.59) | <0.001* |
| Discretionary, times consumed | 0.7 | 0.58 ± 0.68 | 0.28 ± 0.72 | 0.60 ± 0.85 | 0.67 ± 0.85 | −0.40 (−0.64, −0.16) | 0.002* | −0.37 (−0.61, −0.14) | 0.002* |
| Child diet quality (as assessed via educator-completed questionnaires) (baseline: n = 183; follow-up: n = 275) | |||||||||
| Diet quality score (/100)4 | 72.27 ± 12.88 | 75.43 ± 12.76 | 66.58 ± 12.45 | 73.01 ± 10.09 | −1.91 (−5.96, 2.14) | 0.34 | −2.99 (−6.63, 0.64) | 0.11 | |
| BMI z scores (assessed via measured weight and height) (baseline: n = 427; follow-up: n = 389) | |||||||||
| BMI z scores5 | 0.44 ± 1.01 | 0.41 ± 0.91 | 0.48 ± 0.94 | 0.63 ± 1.05 | −0.17 (−0.45, 0.11) | 0.24 | −0.12 (−0.40, 0.16) | 0.39 | |
| HRQoL scores assessed via parent report (baseline: n = 162; follow-up: n = 93) | |||||||||
| KidScreenScore6 (/100) | 76.02 ± 11.82 | 73.67 ± 9.18 | 77.64 ± 11.31 | 74.91 ± 9.42 | 0.39 (−5.83, 6.61) | 0.90 | 1.68 (−3.30, 6.65) | 0.51 | |
Data were analyzed through a group-by-time interaction using general linear mixed models, adjusted for baseline data and clustering at the childcare level. *P value < 0.01 is considered significant. HRQoL, health-related quality of life; ICC, intracluster correlation coefficient.
Complete case analysis—analysis using all available data for child dietary intake for baseline and follow-up in the groups to which children were originally assigned.
Main outcome for this publication.
Assessed in 105 children in the intervention group at baseline and 183 at follow-up with complete data for 88 and 144, respectively; and 101 children were in the control group at baseline and 151 at follow-up with complete data for 95 and 131, respectively.
Assessed in 288 children in the intervention group at baseline and 268 at follow-up with complete data for 237 and 230, respectively; and 234 children were in the control group at baseline and 215 at follow-up with complete data for 190 and 159, respectively.
Assessed in 94 children in the intervention group at baseline and 68 at follow-up with complete data for 93 and 66, respectively; and 69 children were in the control group at baseline and 27 at follow-up and all provided complete data.
Childcare educator–reported child diet quality
There were no significant differences in overall child diet quality scores based on educator report between those in the intervention and control groups at 12-mo follow-up (mean difference: −1.91; 95% CI: −5.96, 2.14; P = 0.34).
Child BMI z scores
At 12-mo follow-up, there were no significant differences between groups for child BMI z scores (mean difference: −0.2; 95% CI: −0.5, 0.1; P = 0.2) or the proportion of children in the healthy weight range [intervention (n = 230, 78%), control (n = 159, 69%); OR: 1.3; 95% CI: 0.7, 2.6; P = 0.4].
Child HRQoL
There were no significant differences in child HRQoL between groups at 12-mo follow-up (n = 93; mean difference: 0.39; 95% CI: −5.83, 6.61; P = 0.90).
Sensitivity analysis
There were no changes to the statistical significance for all reported outcomes when undertaking multiple imputation analyses (see Table 4).
Discussion
To our knowledge, this is the first trial internationally to examine the impact of a web-based menu-planning tool to support the implementation of dietary guidelines in childcare centers on child dietary intake. The trial found increased consumption of fruit and dairy foods and reduced consumption of discretionary foods and breads and cereals in care as assessed via direct observations. Such findings are encouraging given the amenability of web-based interventions to be delivered at scale with minimal investment, because even modest improvements in child dietary intake can make meaningful contributions to improvement in public health nutrition.
The study adds to the limited evidence base assessing the impact of strategies to enhance the implementation of dietary guidelines in childcare centers on child dietary intake and supports the positive findings from the quasi-experimental trial included in a recent Cochrane review (19). The results are also consistent with the previous RCT conducted by the authors (20). Such findings are encouraging given the research team used a highly intensive face-to-face approach across 6 mo, whereas our current study used a lower-intensity approach, primarily delivered via online methods. Whereas this previous study which examined the impact of face-to-face training and support provision for cooks by dietitians to improve menu guideline adherence (20) found improvements in child consumption of vegetables, this study did not. Such findings suggest that although the web-based intervention was able to overcome many important barriers to healthy eating, there may be unique barriers related to consumption of vegetables that need to be better targeted by the online program (47, 48). Given this, further research that examines mechanisms of intervention effect is needed to better identify “how” to optimize the intervention in order to maximize its effect on child diet. In addition, because this intervention primarily targets interpersonal and organizational constructs, future interventions should consider including strategies that target child-level constructs including psychological constructs (i.e., perceived modeling, dietary intention, norms, and liking) to increase consumption of healthier options such as vegetables (49).
The intervention, however, did not have a significant impact on child diet quality as assessed via the survey completed by childcare educators. The diet quality measure attempts to capture both the quantity and quality of foods consumed by children in care. Whereas the web-based program recommended use of higher-quality (i.e., whole-grain and low-fat foods) ingredients in recipes and supporting resources, the primary component of the intervention focused on supporting services to provide adequate quantities (servings) of core foods and reduce discretionary foods because this was the main challenge to guideline implementation reported by childcare staff. Further, the use of educator report in terms of the lack of direct knowledge of the types of foods consumed (50), and the need for educators to recall children's dietary intake over a period of 1 mo may have contributed to these findings. Future iterations of the web intervention may need to consider how to better integrate strategies to improve diet quality, in order to increase the impact of the intervention on child dietary outcomes.
There were also no significant differences in child BMI z scores, consistent with previous childcare-based trials (51, 52). There were, however, positive effects favoring the intervention, where a 9% absolute difference in the percentage of children in the healthy-weight group was observed at follow-up. Other authors have similarly reported challenges with observing significant differences in weight due to the rapid changes in body composition among this age group in 12 mo (53). Although nonsignificant, the effect size is promising and consistent with the reductions in servings of discretionary food consumed reported in this study. The relatively short study time-frame, the intervention focus on generally improving diet (rather than reducing energy), as well as the focus of the program on child diet while in care only may not have been of sufficient extent or intensity to have had an impact on BMI. Similarly, the relatively short intervention period as well as challenges with obtaining parent follow-up data may have reduced our ability to detect a difference in child HRQoL scores. However, such findings warrant further investigation given mixed findings from previous childcare-based trials targeting dietary intake.
Strengths of this study include the randomized design, preregistered dietary outcomes, and use of dietary observations to assess child consumption of food while attending care. However, a number of limitations exist. First, the use of questionnaires completed by educators and parents to assess child diet quality and HRQoL is likely subject to recall and social desirability bias. Despite this, no other validated measures to assess child diet quality while attending care exist, given the need to consider intake over extended periods of time. There was low completion of the telephone survey (54%) for HRQoL owing to challenges contacting parents at follow-up. Centers participating in this study were also limited to those already using the software of our partner provider, which may limit the generalizability of findings. This study utilized a repeat cross-sectional analysis which is recommended for interventions which exert their impact at the cluster level (i.e., improving provision of food at a center level on child diet). We attempted to undertake a cohort analysis; however, as expected there was high attrition of children, with only 14% (n = 31) of children at baseline retained at follow-up owing to changeover of rooms and transition to school. Future studies should consider integrating strategies to maximize child retention at follow-up including increasing the number of days of onsite recruitment and liaising with childcare staff and parents to confirm child attendance on the day of data collection. Although this study is unable to provide an indication of change within individual children, it provides robust evidence of intervention impact for children who were exposed to the intervention. Child-level data collection was undertaken with 35 out of the 54 childcare centers participating in the larger trial. This approach was selected owing to the prohibitively high cost of undertaking dietary observations with all childcare centers participating in the study, because centers were spread across a large geographic area. To reduce selection bias, centers were approached in random order. There were no significant differences in the characteristics of centers participating in the evaluation (i.e., size, locality, and socioeconomic status) compared with those not participating in this evaluation, suggesting that this nested sample was representative of the larger sample of centers recruited to the trial.
In conclusion, this study is the first to our knowledge to demonstrate that use of a web-based menu-planning program together with support to implement dietary guidelines can improve some measures of child diet in care. Future research assessing the longer-term impact of the intervention on child diet and BMI z scores may be warranted to provide a better understanding of the health impact.
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—SLY, LW, JHW, VF, CR, MF, RW, AG, RS, KG, NP, FGS, and SG: designed the research; SLY, AG, FGS, SG, CB, NP, and LW: conducted the research; DS and ROR: provided in-kind funding, software, and programming expertise to support the development of the feedAustralia program; CL: conducted statistical analysis and supported development of the statistical analyses plan; SLY: wrote the paper; SLY, AG, and LW: had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis; and all authors: contributed to the conception or design of the work, data acquisition, interpretation of the data, took part in revising the manuscript, agree to be accountable for all aspects of the work, and read and approved the final manuscript. ROR is Chief Executive Officer of Healthy Australia Ltd and HubHello Pty Ltd. DS is the Head of Social Impact Program Development of Healthy Australia Ltd and HubHello Pty Ltd. All other authors report no conflicts of interest.
Notes
Supported by National Health and Medical Research Council (NHMRC) project grant APP1102943 (to LW) and Cancer Council NSW (CCNSW) program grant PG16-05 (to JW). Pilot funding was also provided from the Hunter Cancer Research Alliance (to SLY) and the Priority Research Centre for Health Behaviour, University of Newcastle (to SLY). Hunter New England Population Health, Hunter Medical Research Institute, and the University of Newcastle provided infrastructure funding. Healthy Australia Ltd provided in-kind support for programming of the web program (“feedAustralia”). Healthy Australia Ltd co-developed the web program and were members of the advisory group which supported decisions related to the design and delivery of the web-based program. SLY is a postdoctoral research fellow funded by (2015–2018) National Heart Foundation award 100547 and currently Australian Research Council grant DE170100382. MF is a clinical research fellow funded by Hunter New England Population Health and the Health Research and Translation Centre, Partnerships, Innovation and Research, Hunter New England Local Health District. RW is a postdoctoral fellow funded by NHMRC Translating Research into Practice grant APP1113377. RS is a postdoctoral fellow funded by NHMRC Translating Research into Practice grant APP1150661. LW is a Hunter New England Clinical Research Fellow and is supported by Heart Foundation Future Leader Fellowship award 101175 and NHMRC Career Development Fellowship award APP1128348.
The NHMRC and CCNSW played no role in the conduct of the trial. The content of this publication is the responsibility of the authors and does not reflect the views of the NHMRC or CCNSW. Healthy Australia Ltd provided input on data analysis and interpretation of the data via review of the manuscript.
Data described in the article, code book, and analytic code will be made available upon request pending appropriate ethical approval.
Abbreviations used: AGHE, Australian Guide to Healthy Eating; CCMS, Childcare Management System; HRQoL, health-related quality of life; ICC, intracluster correlation coefficient; RCT, randomized controlled trial.
References
- 1. World Health Organization. Global strategy on diet, physical activity and health: childhood overweight and obesity. [Internet]. Geneva: WHO; 2018; [cited 18 October, 2018]. Available from: http://www.who.int/dietphysicalactivity/childhood/en/. [Google Scholar]
- 2. Deshmuth-Taskar P, Nicklas TA, Morales M, Yang SL, Zakeri I, Berenson GS. Tracking of overweight status from childhood to young adulthood: the Bogalusa Heart Study. Eur J Clin Nutr. 2006;60(1):48–57. [DOI] [PubMed] [Google Scholar]
- 3. Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W et al.. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365(20):1876–85. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Obesity and overweight. [Internet]. Geneva: WHO; 2018; [cited 30 October, 2018]. Available from: http://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight. [Google Scholar]
- 5. Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviors from childhood to adulthood: a systematic review. Maturitas. 2011;70(3):266–84. [DOI] [PubMed] [Google Scholar]
- 6. Mikkilä V, Räsänen L, Raitakari OT, Pietinen P, Viikari J. Longitudinal changes in diet from childhood into adulthood with respect to risk of cardiovascular diseases: the Cardiovascular Risk in Young Finns Study. Eur J Clin Nutr. 2004;58(7):1038–45. [DOI] [PubMed] [Google Scholar]
- 7. Movassagh EZ, Baxter-Jones ADG, Kontulainen S, Whiting SJ, Vatanparast H. Tracking dietary patterns over 20 years from childhood through adolescence into young adulthood: the Saskatchewan Pediatric Bone Mineral Accrual Study. Nutrients. 2017;9(9):990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fox MK, Gearan E, Cannon J, Briefel R, Deming DM, Eldridge AL, Reidy KC. Usual food intakes of 2- and 3-year old U.S. children are not consistent with dietary guidelines. BMC Nutr. 2016;2:67. [Google Scholar]
- 9. Australian Institute of Health and Welfare (AIHW). Australia's health 2018. Canberra: AIHW; 2018. [Google Scholar]
- 10. Early Learning: Everyone Benefits. State of early learning in Australia 2017. Canberra: Early Childhood Australia; 2017. [Google Scholar]
- 11. Institute of Medicine. Early childhood obesity prevention policies. Washington (DC): Institute of Medicine; 2011. [Google Scholar]
- 12. World Health Organization. Report of the Commission on Ending Childhood Obesity. Geneva: WHO; 2016. [Google Scholar]
- 13. Benjamin-Neelon SE. Position of the Academy of Nutrition and Dietetics: benchmarks for nutrition in child care. J Acad Nutr Diet. 2018;118(7):1291–300. [DOI] [PubMed] [Google Scholar]
- 14. Public Health England. Example menus for early years settings in England. Part 1: guidance. London: Public Health England; 2017. [Google Scholar]
- 15. Australian Children's Education & Care Quality Authority (ACECQA). National Quality Standard. [Internet]. Sydney: ACECQA; 2018; [cited 18 October, 2018]. Available from: https://www.acecqa.gov.au/nqf/national-quality-standard. [Google Scholar]
- 16. Black AP, D'Onise K, McDermott R, Vally H, O'Dea K. How effective are family-based and institutional nutrition interventions in improving children's diet and health? A systematic review. BMC Public Health. 2017;17:818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stacey FG, Finch M, Wolfenden L, Grady A, Jessop K, Wedesweiler T, Bartlem K, Jones J, Sutherland R, Vandevijvere S et al.. Evidence of the potential effectiveness of center-based childcare policies and practices on child diet and physical activity: consolidating evidence from systematic reviews of intervention trials and observational studies. Curr Nutr Rep. 2017;6(3):228–46. [Google Scholar]
- 18. Wolfenden L, Jones J, Williams CM, Finch M, Wyse RJ, Kingsland M, Tzelepis F, Wiggers J, Williams AJ, Seward K et al.. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst Rev. 2016;10:CD011779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Williams CL, Bollella MC, Strobino BA, Spark A, Nicklas TA, Tolosi LB, Pittman BP “Healthy-Start”: outcome of an intervention to promote a heart healthy diet in preschool children. J Am Coll Nutr. 2002;21(1):62–71. [DOI] [PubMed] [Google Scholar]
- 20. Seward K, Wolfenden L, Finch M, Wiggers J, Wyse R, Jones J, Yoong SL. Improving the implementation of nutrition guidelines in childcare centers improves child dietary intake: findings of a randomized trial of an implementation intervention. Public Health Nutr. 2018;21(3):607–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Grady A, Wolfenden L, Wiggers J, Rissel C, Finch M, Flood V, O'Rourke R, Stacey F, Wyse R, Lecathelinais C et al.. Effectiveness of a web-based menu-planning intervention to improve childcare service compliance with dietary guidelines: a randomized controlled trial. J Med Internet Res. 2020;22(2):e13401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schulz KF, Altman DG, Moher D; for the CONSORT group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomized trials. BMJ. 2010;340:c332. [DOI] [PubMed] [Google Scholar]
- 23. Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yoong SL, Grady A, Wiggers J, Flood V, Rissel C, Finch M, Searles A, Salajan D, O'Rourke R, Daly J et al.. A randomized controlled trial of an online menu planning intervention to improve childcare service adherence to dietary guidelines: a study protocol. BMJ Open. 2017;7(9):e017498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hayes RJ, Moulton LH. Cluster randomized trials. 2nd ed New York: Chapman and Hall; 2017. [Google Scholar]
- 26. Murray DM. Design and analysis of group-randomized trials. New York: Oxford University Press; 1998. [Google Scholar]
- 27. Wolfenden L, Kypri K, Freund M, Hodder R. Obtaining active parental consent for school-based research: a guide for researchers. Aust N Z J Public Health. 2009;33(3):270–5. [DOI] [PubMed] [Google Scholar]
- 28. Australian Bureau of Statistics (ABS). Census of population and housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011. Canberra: ABS; 2013. [Google Scholar]
- 29. Venkatesh V, Bala H. Technology Acceptance Model 3 and a research agenda on interventions. Decision Sci. 2008;39(2):273–315. [Google Scholar]
- 30. Grady A, Seward K, Finch M, Fielding A, Stacey F, Jones J, Wolfenden L, Yoong SL. Barriers and enablers to implementation of dietary guidelines in early childhood education centers in Australia: application of the Theoretical Domains Framework. J Nutr Educ Behav. 2018;50(3):229–37. [DOI] [PubMed] [Google Scholar]
- 31. Seward K, Wolfenden L, Wiggers J, Finch M, Wyse R, Oldmeadow C, Presseau J, Clinton-McHarg T, Yoong SL. Measuring implementation behavior of menu guidelines in the childcare setting: confirmatory factor analysis of a theoretical domains framework questionnaire (TDFQ). Int J Behav Nutr Phys Act. 2017;14:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. NSW Ministry of Health. Caring for children. Birth to 5 years. North Sydney: NSW Ministry of Health; 2014. [Google Scholar]
- 33. Food Standards Australia New Zealand (FSANZ). Australian food composition tables. Canberra: FSANZ; 2010. [Google Scholar]
- 34. Australian Government Department of Health & Ageing. Healthy eating and physical activity for early childhood (Director/Coordinator book). Canberra: Commonwealth of Australia; 2013. [Google Scholar]
- 35. Healthy Kids. About Munch & Move. [Internet]. North Sydney: NSW Ministry of Health; 2019; [cited 4 December, 2019]. Available from: https://www.healthykids.nsw.gov.au/campaigns-programs/about-munch-move.aspx. [Google Scholar]
- 36. Grady A, Finch M, Fielding A, Seward K, Hendrie G, Golley R, Jones J, Yoong S. Adaptation, acceptability and feasibility of a Short Food Survey to assess the dietary intake of children during attendance at childcare. Public Health Nutr, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Australian Government. Australian Guide to Healthy Eating. [Internet]. Canberra: National Health and Medical Research Council; 2017; [cited 22 November, 2018]. Available from: https://www.eatforhealth.gov.au/guidelines/australian-guide-healthy-eating. [Google Scholar]
- 38. Ball SC, Benjamin SE, Ward DS. Development and reliability of an observation method to assess food intake of young children in child care. J Am Diet Assoc. 2007;107(4):656–61. [DOI] [PubMed] [Google Scholar]
- 39. Hendrie GA, Viner Smith E, Golley RK. The reliability and relative validity of a diet index score for 4–11-year-old children derived from a parent-reported short food survey. Public Health Nutr. 2014;17(7):1486–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. NSW Health, Centre for Population Health. Growth assessment in children and weight status assessment in adults. Sydney: NSW Health; 2017. [Google Scholar]
- 41. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: WHO; 2006. [Google Scholar]
- 42. Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J, Power M, Duer W, Abel T, Czemy L et al.. Reliability, construct and criterion validity of the KIDSCREEN-10 score: a short measure for children and adolescents’ well-being and health-related quality of life. Qual Life Res. 2010;19(10):1487–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Waters E, Gibbs L, Tadic M, Ukoumunne OC, Magarey A, Okely AD, de Silva A, Armit C, Green J, O'Connor T et al.. Cluster randomised trial of a school-community child health promotion and obesity prevention intervention: findings from the evaluation of fun ’n healthy in Moreland!. BMC Public Health. 2017;18:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136(10):2588–93. [DOI] [PubMed] [Google Scholar]
- 45. He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007;21(9):717–28. [DOI] [PubMed] [Google Scholar]
- 46. White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomized trials with missing outcome data. BMJ. 2011;342:d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Appleton KM, Hemingway A, Saulais L, Dinnella C, Monteleone E, Depezay L, Morizet D, Perez-Cueto FJA, Bevan A, Hartwell H. Increasing vegetable intakes: rationale and systematic review of published interventions. Eur J Nutr. 2016;55(3):869–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Krolner R, Rasmussen M, Brug J, Klepp K-I, Wind M, Due P. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part II: qualitative studies. Int J Behav Nutr Phys Act. 2011;8:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McClain AD, Chappuis C, Nguyen-Rodriguez ST, Yaroch AL, Spruit-Metz D. Psychosocial correlates of eating behavior in children and adolescents: a review. Int J Behav Nutr Phys Act. 2009;12(6):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cleland P, Byrne R, Vidgen H, Irvine S, Farrell A, Gallegos D. Empirical insights into educator knowledge, confidence and intentions in promoting children's Learning, Eating, Active Play and Sleep (LEAPS). Australas J Early Child. 2018;43(2):55–63. [Google Scholar]
- 51. Kong A, Buscemi J, Stolley MR, Schiffer LA, Kim Y, Braunschweig CL, Gomez-Perez SL, Blumstein LB, Van Horn L, Dyer AR et al.. Hip-Hop to Health Jr. randomized effectiveness trial. 1-year follow-up results. Am J Prev Med. 2016;50(2):136–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Natale RA, Lopez-Mitnik G, Uhlhorn SB, Asfour L, Messiah SE. Effect of a child care center-based obesity prevention program on body mass index and nutrition practices among preschool-aged children. Health Promot Pract. 2014;15(5):695–705. [DOI] [PubMed] [Google Scholar]
- 53. Vanderwall C, Eickhoff J, Clark RR, Carrel AL. BMI z-score in obese children is a poor predictor of adiposity changes over time. BMC Pediatr. 2018;18:187. [DOI] [PMC free article] [PubMed] [Google Scholar]