To the Editor:
Neighborhood socioeconomic deprivation has been associated with worsened mental health,1–4 but previous studies may suffer from confounding due to self-selection, in that individuals with poor mental health are more likely to reside in deprived neighborhoods (eFigure 1).5 Refugees in particular are uniquely vulnerable to mental health problems, due to their involuntary and sudden displacement.6,7
We leveraged a natural policy experiment where incoming refugees were dispersed quasi-randomly to neighborhoods across Sweden (see eAppendix 1). We estimated the effect of neighborhood deprivation on mental health among refugees. We compared these estimates to the association among non-refugee immigrants who were not subject to the dispersal policy to evaluate the possibility of selection bias in correlational analyses.
We constructed a dataset using Swedish registers.8 We included adult immigrants who arrived in Sweden during 1987–1991, when the dispersal policy was in effect (Supplemental Methods, eFigures 2–3).
The outcome was date of diagnosis with depression and/or anxiety. We created an index of neighborhood deprivation, split into tertiles, and examined (1) neighborhood deprivation on arrival and (2) neighborhood deprivation 10 years after.9 While the former is likely to be unconfounded among quasi-randomly assigned refugees, the latter is likely to reflect self-selection among refugees, making estimates more comparable to those among non-refugee immigrants. Baseline covariates included: age, gender, education, marital status, family size, region of placement, region of origin, and year of arrival.
Cox models were used to estimate the association of neighborhood deprivation (1) on arrival and (2) 10 years later with diagnosis of depression/anxiety. We stratified by refugees versus non-refugee immigrants and adjusted for the covariates above. We included fixed effects for initially assigned municipality (see eAppendix 2). We also examined differences by gender.
Our sample included 48,056 refugees and 97,254 non-refugee immigrants (eTable 1). Over two-thirds were under 35. Refugees were more likely to be male, with lower educational attainment and larger families. Most refugees were from Iran (27%) and the Middle East and North Africa (27%). Diagnosis of depression and/or anxiety was higher in refugees (39%) than non-refugee immigrants (20%) (see eAppendix 3).
Among non-refugee immigrants, moderate-deprivation neighborhoods on arrival were associated with greater depression/anxiety compared with low-deprivation neighborhoods (hazard ratio [HR] 1.04, 95% confidence interval [CI] 1.00, 1.09) (Figure). Meanwhile, refugees placed in high-deprivation neighborhoods on arrival had lower rates of depression/anxiety (HR 0.96, 95%CI 0.92, 1.00). Estimates were close to the null, and thus susceptible to being explained by small amounts of bias.
Figure. Association of neighborhood deprivation with poor mental health during 30-year follow-up.
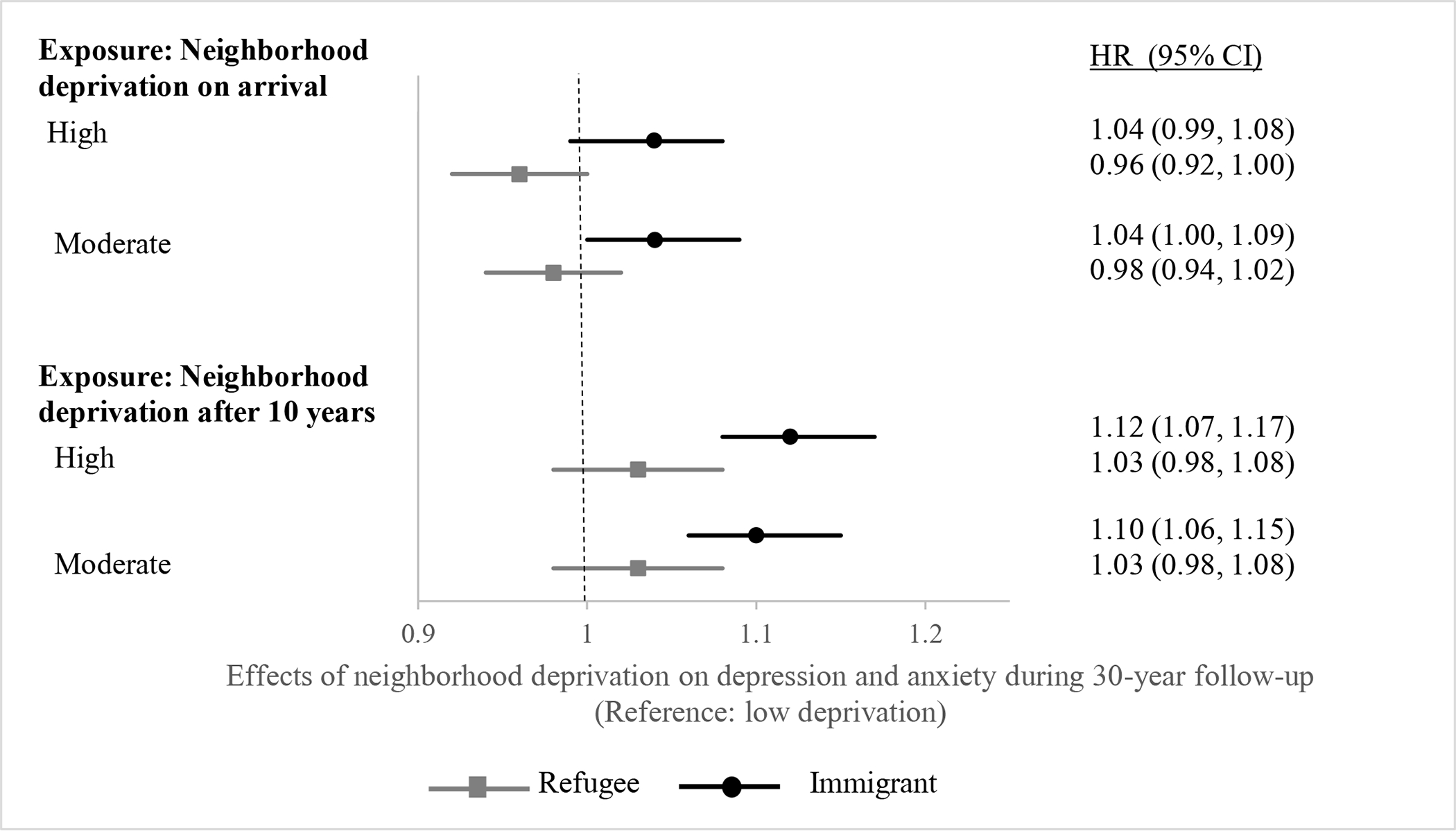
Refugees on arrival: n=48,056; after 10 years: n=31,749
Non-refugee immigrants on arrival: n=97,254; after 10 years: n=51,593
Note: Analyses involved Cox proportional hazards models, adjusting for characteristics listed in eTable 1, year of arrival to account for secular trends, and fixed effects for initial municipality. Models incorporated shared frailty at the municipality level to account for correlated observations within families and municipalities.
Among non-refugee immigrants, neighborhood deprivation 10 years after arrival was more strongly associated with depression/anxiety (high-deprivation HR 1.12, 95%CI 1.07, 1.17; moderate-deprivation HR 1.10, 95%CI 1.06, 1.15). Among refugees, the association of neighborhood deprivation 10 years after arrival with depression/anxiety was 1.03 (95%CI 0.98, 1.08) for both high- and moderate-deprivation neighborhoods.
Among non-refugee immigrants, the association of high neighborhood deprivation on arrival and 10 years after arrival was greater for men (HR 1.28, 95%CI 1.18, 1.38) than women (HR 1.06, 95%CI 1.01, 1.12). Among refugees, the association of high neighborhood deprivation 10 years after arrival was greater for women (HR 1.07, 95%CI 0.99, 1.16) than men (HR 0.98, 95%CI 0.91, 1.06) (eFigure 4, eAppendix 4).
We used a natural experiment and longitudinal Swedish registers to study the association of neighborhood deprivation with mental health among refugees and non-refugee immigrants, contrasting quasi-experimental and correlational approaches. For refugees quasi-randomly assigned to neighborhoods, high neighborhood deprivation on arrival was associated with lower depression/anxiety, although effect estimates were close to the null and thus susceptible to small amounts of bias (e.g., due to misclassification or under-diagnosis). For neighborhood deprivation 10 years after arrival, estimates for refugees started to resemble those of non-refugee immigrants, perhaps due to the growing role of self-selection. Among non-refugee immigrants, high neighborhood deprivation on arrival and 10 years after arrival were consistently associated with depression and/or anxiety, perhaps because self-selection is likely to play a larger role in the absence of quasi-random placement.
There are two major explanations for our findings. First, quasi-experimental neighborhood assignment may reduce confounding due to selection. Prior studies have shown strong associations between neighborhood deprivation and mental health.1,3–5 These estimates may be confounded by unobserved socioeconomic and health characteristics (eFigure 1).2,10 Refugees were able to move neighborhoods after their initial placement. By comparing estimates among refugees on arrival to estimates 10 years later, we found that estimates 10 years after arrival start to resemble those of non-refugee immigrants, suggesting that the coefficients in non-refugee immigrants may in part represent self-selection (see eAppendix 4).
A second explanation is that immigration status may lead to differential effects. Refugees, particularly women, may experience discrimination and fewer opportunities for integration in low-deprivation neighborhoods. For non-refugee immigrants, low-deprivation neighborhoods may reflect financial stability, while high-deprivation neighborhoods may offer fewer economic opportunities, particularly for men.11 Alternately, neighborhood factors may be less important for refugees than past trauma or the support provided by the Swedish government.12,13
By demonstrating differences using two analytic approaches, we provide insight into self-selection bias in the prior neighborhood-health literature, and we shed light on the possible differential effect of neighborhood deprivation on depression/anxiety by immigration status.
Supplementary Material
Acknowledgments:
The authors would like to thank the UCSF Primary Care Research Fellowship for their valuable review of the manuscript.
Sources of funding: This work was supported in part by the National Institutes of Health (grants K08HL132106 and 1R01AG063385 to RH). This project has received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation program (grant agreement No 787592). ER was supported by a fellowship training grant, National Research Service Award (NRSA) T32HP19025.
Footnotes
Publisher's Disclaimer: This is the pre-publication version of a manuscript that has been accepted for publication. This version does not include post-acceptance editing and formatting. Readers who wish to access the final published version of this manuscript and any ancillary material related to it should access the manuscript on the journal’s website: https://journals.lww.com/epidem/Citation/publishahead/Neighborhood_deprivation_and_mental_health_among.98442.aspx, or in the print issue in which the article appears. Those who cite this manuscript should cite the published version, as it is the official version of record.
Conflicts of interest: None declared.
Data access: The data are not available for replication because the Swedish registry database is provided to us under a data use agreement which requires that we do not disclose individual-level data.
REFERENCES
- 1.Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med 2015;128:316–26. [DOI] [PubMed] [Google Scholar]
- 2.Lofors J, Ramirez-Leon V, Sundquist K. Neighbourhood income and anxiety: a study based on random samples of the Swedish population. Eur J Public Health 2006;16(6):633–9. [DOI] [PubMed] [Google Scholar]
- 3.Graif C, Arcaya MC, Diez Roux AV. Moving to opportunity and mental health: Exploring the spatial context of neighborhood effects. Soc Sci Med 2016;162:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sundquist K, Ahlen H. Neighbourhood income and mental health: A multilevel follow-up study of psychiatric hospital admissions among 4.5 million women and men. Health & Place 2006;12(4):594–602. [DOI] [PubMed] [Google Scholar]
- 5.Kling JR, Liebman JB, Katz LF. Experimental Analysis of Neighborhood Effects. Econometrica 2007;75(1):83–119. [Google Scholar]
- 6.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA 2009;302(5):537–49. [DOI] [PubMed] [Google Scholar]
- 7.Brandt L, Henssler J, Muller M, Wall S, Gabel D, Heinz A. Risk of Psychosis Among Refugees: A Systematic Review and Meta-analysis. JAMA Psychiatry 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO. External review and validation of the Swedish national inpatient register. BMC Public Health 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White JS, Hamad R, Li X, Basu S, Ohlsson H, Sundquist J, Sundquist K. Long-term effects of neighbourhood deprivation on diabetes risk: quasi-experimental evidence from a refugee dispersal policy in Sweden. The Lancet Diabetes & Endocrinology 2016;4(6):517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med 2004;58(10):1929–52. [DOI] [PubMed] [Google Scholar]
- 11.Mousa S Boosting Refugee Outcomes: Evidence from Policy, Academia, and Social Innovation. In: Lab SIP, ed, 2018. [Google Scholar]
- 12.Rasmussen A, Crager M, Baser RE, Chu T, Gany F. Onset of posttraumatic stress disorder and major depression among refugees and voluntary migrants to the United States. J Trauma Stress 2012;25(6):705–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Åslund O, Fredriksson P. Peer Effects in Welfare Dependence: Quasi-Experimental Evidence. The Journal of Human Resources 2009;44(3):798–825. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


