Abstract
Housing is a major pathway through which health disparities emerge and are sustained over time. However, no existing unified conceptual model has comprehensively elucidated the relationship between housing and health equity with attention to the full range of harmful exposures, their cumulative burden and their historical production. We synthesized literature from a diverse array of disciplines to explore the varied aspects of the relationship between housing and health and developed an original conceptual model highlighting these complexities. This holistic conceptual model of the impact of housing on health disparities illustrates how structural inequalities shape unequal distribution of access to health-promoting housing factors, which span four pillars: 1) cost (housing affordability); 2) conditions (housing quality); 3) consistency (residential stability); and 4) context (neighborhood opportunity). We further demonstrate that these four pillars can lead to cumulative burden by interacting with one another and with other structurally-rooted inequalities to produce and reify health disparities. We conclude by offering a comprehensive vision for healthy housing that situates housing’s impact on health through a historical and social justice lens, which can help to better design policies and interventions that use housing to promote health equity.
Keywords: Socioeconomic factors, Housing, Health status disparities, Residence characteristics, Healthy housing
1. Introduction
The United States faces an unprecedented and multifaceted housing crisis. To begin, housing is more unaffordable than ever. Between 1960 and 2016, median rents rose 61% and median home values increased 112% along with a doubling of the number of renters who are cost-burdened (Joint Center for Housing Studies of Harvard University, 2018). In fact, more than half of low-income American households now allocate over 50% of their income to housing (Desmond, 2018). Meanwhile, housing stability is increasingly threatened by high rates of eviction, foreclosure, gentrification, and natural disasters, among other factors largely beyond a household’s control. Housing choice is further restricted for low-socioeconomic and racial and ethnic minority groups due to persistent discrimination and residential segregation. On average, affluent Blacks live in neighborhoods with higher neighborhood poverty than do poor Whites (Logan, 2013).
This housing crisis has significant implications for the health and well-being of American households, especially marginalized groups. Recently, housing and neighborhoods have garnered significant and growing academic interest as determinants of health (Garrison and Pollack, 2018; Taylor, 2018). This burgeoning literature has assessed the relationship between various aspects of housing and health outcomes including: physical health; mental health; chronic and infectious disease; maternal, infant, reproductive, and sexual health; and injury. Disparities in access to health-promoting aspects of housing are patterned along axes of social inequality. Low-income neighborhoods and those with high proportions of racial and ethnic minority groups face greater environmental hazard exposures (Morello-Frosch et al., 2011) and a higher proportion of Black, Hispanic, and low-income households live in substandard housing compared with White and higher-income counterparts (Jacobs, 2011; U.S. Census Bureau, 2017). Groups that experience housing disparities furthermore experience significant health disparities across housing-relevant outcomes (National Academies of Sciences, Engineering, and Medicine et al., 2017). We argue that housing is a critical pathway through which such disparities develop and is potentially an effective means for ameliorating them through a comprehensive understanding of the complexities of housing.
Although there is a significant body of evidence that links housing to health equity, the relationship is not yet clearly and comprehensively elucidated. Much important work to date has identified the effects of a particular exposure on a particular outcome, such as lack of playgrounds in the neighborhood on physical activity or mold in the home on asthma. Furthermore, significant research, such as Jacobs’ (2011) and Adamkiewicz’s et al. (2011) reviews of disparities in environmental housing conditions, has now identified inequitable distribution of certain types of housing exposures. However, the wide diversity of housing and neighborhood exposures studied relevant to health equity make it difficult to comprehend the overall effect across the full range of exposures. Other fields, such as urban planning, history, and sociology, have also identified processes through which housing disparities develop, such as through redlining and exclusionary zoning (Massey and Denton, 1993; Rothstein, 2017). Yet, this research is rarely discussed in the public health literature. Doing so could facilitate a more comprehensive picture of the links between housing insecurity and health disparities, thereby strengthening arguments for housing policy solutions that leverage health as a basis for action. Aggregating these components to understand how housing matters for health, for whom it matters, and why these groups in particular came to be affected is a necessary next step.
Several researchers have made promising steps towards integration in their creation of valuable conceptual models or overviews that have further categorized exposure types and proposed pathways through which housing affects health (see Table 1) (e.g., Braveman et al., 2011; Rauh et al., 2008; Saegert et al., 2011; L. Taylor, 2018). These researchers have begun to move the field toward a multidimensional focus on housing’s effects on health. Taken collectively, these reviews and models point to health-relevant factors of housing that we term the four pillars of housing (see Fig. 1): 1) conditions (housing quality); 2) cost (affordability); 3) consistency (residential stability); and 4) context (neighborhood opportunity). However, no one model provides a unified assessment that includes attention to: all dimensions of housing, the unequal distribution of housing disparities along other axes of inequality, and the historical forces shaping unequal housing opportunities (see Table 1). All three aspects are necessary for a truly comprehensive model.
Table 1.
Existing conceptual models or overviews of housing and health.
| Article | Dimensions of housing discussed | Attention to health disparities? | Attention to historical context? |
|---|---|---|---|
| Braveman et al. (2011) | - Physical conditions within homes - Conditions in the neighborhoods surrounding homes - Housing affordability |
Minor | No |
| Rauh et al. (2008) | - Environmental conditions within the home and neighborhood | Yes | No |
| Saegert et al. (2011) | - Not the focus of the model, but largely discuss mortgage foreclosure and serial displacement | Yes | Yes |
| Taylor (2018) | - Stability - Quality and safety - Affordability - Neighborhood |
Minor | No |
Fig. 1.
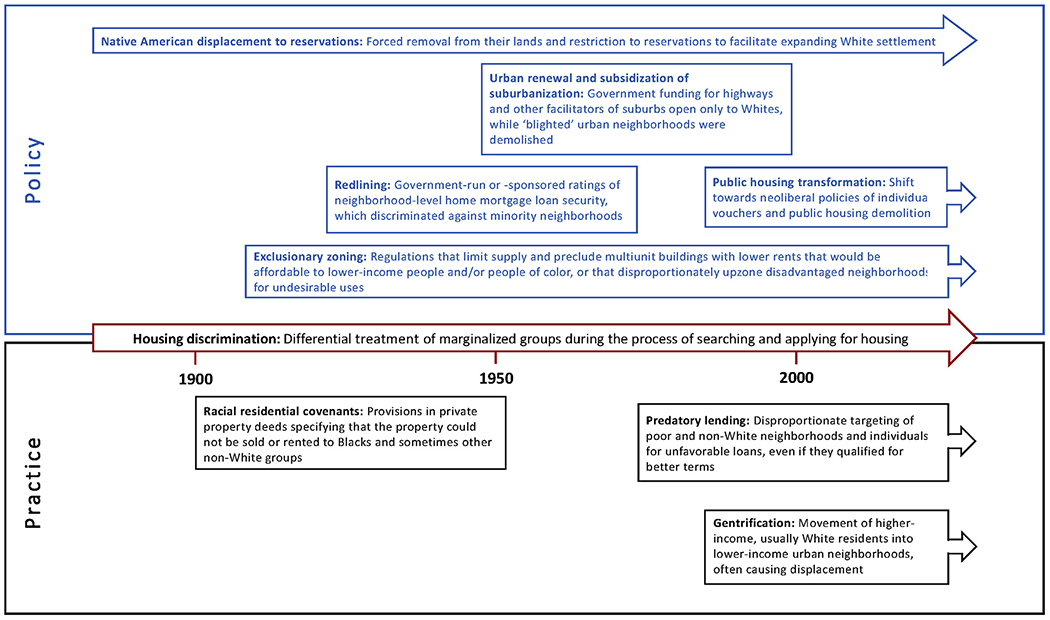
Policies and practices contributing to housing disparities.
Source: Created by the authors based on the evidence described throughout this section.
Incorporating such attention to historical production of housing disparities is important for building a convincing argument for policy action to promote a robust and equitable housing standard. Housing disparities can be traced back to a decades-long legacy of governmental, institutional, and interpersonal discriminatory policies and practices, such as the discriminatory criteria federal agencies used to provide mortgage loans (Massey and Denton, 1993; Rothstein, 2017), suggesting that solutions must also occur at a systemic level. Importantly, America and the broader global community have, at times, espoused and supported peoples’ right to decent housing, such as through the U.S. Housing Act of 1949 (Freeman, 2002; National Housing Act of 1949, Pub L No 81–171, 1949) and the United Nations’ Universal Declaration of Human Rights (United Nations General Assembly, 1948). The American government, however, has engaged with this responsibility only halfheartedly, generally viewing housing as a commodity rather than a right (Pattillo, 2013). Despite the significant scope and impact of the housing crisis as well as recognition of the importance of the housing-health connection by some governmental bodies (e.g., Office of the Surgeon General (US), 2009), insufficient political mobilization has occurred to address shortfalls in the provision of adequate, affordable and stable housing. The number of households receiving federally subsidized housing units, for example, has increased only marginally while the affordability crisis has deepened and more households are in need (Joint Center for Housing Studies of Harvard University, 2018). Furthermore, only one in four eligible households receives housing assistance (Fischer and Sard, 2017), even as the eviction rates reach crisis levels (Desmond, 2012; Desmond, 2015). This reality furthers our argument for an improved policy response.
One critical starting point is to move beyond the false dichotomy of either being homeless or housed, and embrace a more nuanced and complete understanding of housing that recognizes its wide array of health-detrimental aspects (short of homelessness) in the field of public health. It is now clear that the provision of a home is a prerequisite to health, though it is insufficient on its own. For example, New York City and State laws are unusually progressive in providing a legal right to shelter. However, even so, conditions are often poor, exposing residents to hazards such as vermin and lack of heat or ventilation, and regardless shelters are by definition not intended to be long-term and stable homes (Routhier, 2018). Thus, the current housing crisis urgently raises the question of what a minimum standard for equitable, decent housing with respect to health might entail. Such a vision could inform the establishment of societal consensus and be implemented as a joint policy solution. Housing standards and codes have long prioritized economic development and planning, though they often lack a public health perspective and health-based evidence (Braubach et al., 2011). A number of practical health-focused standards have been developed for individual housing aspects, particularly for hazardous physical deficiencies (e.g., lead paint and mold) and their impacts on various physical and mental health outcomes (American Public Health Association & National Center for Healthy Housing, 2014; Centers for Disease Control and Prevention, 2013; U.S. Department of Housing and Urban Development, n.d.; World Health Organization, 2018). While these standards offer valuable guidance on physical housing conditions, no one standard encompasses how physical conditions, affordability, residential stability, and neighborhood characteristics act as pathways by which housing affects health independently and collectively.
In this article, we address these gaps by proposing a holistic conceptual model that encompasses four critical health-relevant dimensions of housing, identifies their unequal social patterning and resulting health disparities, and links them to their sociopolitical origins. For this scoping review, we intentionally drew widely and broadly from journal articles, books, and grey literature, across diverse fields including public health, urban planning, history, public policy, and sociology to ensure the representativeness and comprehensiveness of our model and to bring often-unconnected housing insights into the public health discourse. We ask: What features or characteristics are critical to decent housing? What gaps exist in equitable access to such homes today, and how might we address them? Finally, we offer suggestions for a vision for health equity in housing and argue for the urgency of policy intervention. We organized this review in three parts: first, we provide an overview of the historical roots of housing disparities in the U.S.; second, we describe the four pillars of housing and related health outcomes and propose an original conceptual model that highlights the complexity in the association between housing and health; and third, we offer a comprehensive, rights-based, empirically informed vision for healthy housing that ensures access to affordable, stable, good quality housing in safe neighborhoods that support healthy lifestyles for all.
2. The historical roots of housing disparities in the U.S
The unequal burden of housing disparities faced by marginalized populations does not occur spontaneously or naturally; rather it is related to broader structural disadvantages enforced by institutions and individuals (see Fig. 1). Historically, marginalized groups were denied full control over their residential choices through racist and economically exclusionary ideologies that promulgated racial covenants, redlining, exclusionary zoning, involuntary displacement policies, and other mechanisms of patterned residential disadvantage. Limited access to decent, habitable housing in health-promoting neighborhoods among non-White and lower-income groups has also had intergenerational effects (Massey and Denton, 1993; Rothstein, 2017). Contemporary policies and practices continue to reinforce housing disparities through shifts in federal housing assistance policies, sub-prime loan targeting, and housing discrimination (Goetz, 2013; Hall et al. 2015). Thus, structural inequalities and the mechanisms through which they are enacted to deny marginalized groups full control over their residential choices are an important element of the relationship between housing and health equity.
A key driver of contemporary housing disparities has been racial and economic segregation, which remains high in American cities today. As of 2010, the Black-White residential dissimilarity index was 59.1 (Logan, 2013), meaning 59.1% of Blacks would need to move for each neighborhood to have the same percentage of Black residents as the overall metropolitan area (U.S. Census Bureau, 2002). While this represents a decline, it is still undeniably high. Hispanics are slightly less segregated, with a Hispanic-White dissimilarity index of 48.5, which is still significant and not declining (Logan, 2013). High- and low-income households are also highly segregated, which has only increased as American income inequality increases (Reardon and Bischoff, 2011). Furthermore, 71% of Whites own homes, which is a much higher rate than Hispanics (45%) and Blacks (41%) (Goodman et al., 2018); their homes are also worth more (U.S. Census Bureau, 2013). Because home equity accounts for a large proportion of household wealth, particularly for minorities, this points to an overall wealth gap (Kuebler, 2013). The median wealth of White households today is 10 times that of Black households and eight times that of Hispanic households (Kochhar and Cilluffo, 2017).
High levels of residential segregation and homeownership disparities are rooted in historical practices and policies. In the 1930s-60s, the federal government established the Home Owners’ Loan Corporation (HOLC) to provide refinancing assistance to homeowners struggling to pay their mortgages, as well as the Federal Housing Administration (FHA) to underwrite mortgage risk to increase banks’ comfort with mortgage lending and therefore increase individuals’ ability to access a mortgage. The HOLC used a neighborhood appraisal methodology to determine the riskiness of a loan in a given neighborhood, influencing whether and how much assistance residents of that neighborhood could access. This methodology explicitly considered the racial and ethnic identity and income level of neighborhood residents. The resulting practice of ranking non-White neighborhoods as hazardous and credit-unworthy is referred to as ‘redlining.’ FHA underwriting guidelines were similarly explicitly exclusionary and only 2% of FHA mortgage insurance was ultimately available to non-Whites (Woods et al., 2014). Private banks also adopted and expanded the reach of these guidelines. The Veterans Administration technically offered to cosign mortgage loans for returning veterans, but in practice, since banks refused to lend to Blacks, they could not access such loans (Woods et al., 2014).
Land-use zoning has also contributed to the formation and perpetuation of exclusionary and unequal residential patterns: Although the U.S. Supreme Court in Buchanan v. Warley found explicit racial zoning unconstitutional in 1917, land-use zoning with exclusionary effects remained a permissible legal option as seemingly race-neutral. Regardless of their intent, such zoning decisions have had an exclusionary impact (Whittemore, 2017). White and/or wealthier neighborhoods that intended to remain as such were frequently zoned as exclusively single-family or otherwise low-density, or implemented building permit caps or moratoria, limiting and precluding the supply of multiunit buildings with lower rents that would have been be affordable to lower-income people and/or people of color (Hirt, 2015). Additionally, minority and low-income neighborhoods have disproportionately been zoned for undesirable uses (e.g., heavy commercial and industrial uses) exposing residents to environmental hazards such as air and noise pollution, traffic and the denial of development of waterfronts for communal rather than commercial purposes. These negative effects contribute to neighborhood segregation, the perpetuation and concentration of less desirable land uses, which combined have negative impacts on property values and the potential for wealth building (Whittemore, 2017). For example, Maantay’s (2001) analysis of New York City’s industrial zones from 1961 to 1998 found that rezoning to allow waste-related facilities occurred in areas with higher minority and low-income populations, while conversely, rezoning to decrease such land uses occurred in higher-income and lower minority population areas. Far fewer Blacks and Hispanics live in jurisdictions with anti-density zoning (Pendall, 2000). Similarly, greater metropolitan-area segregation and concentrated poverty is significantly correlated with anti-density zoning (Rothwell and Massey, 2009, 2010).
Although, as noted above, racial zoning was deemed unconstitutional, restrictive racial covenants (provisions in private property deeds specifying that the property could not be sold or rented to Blacks and sometimes other non-White groups) were upheld and widely implemented (Jones-Correa, 2000). Real estate agents also supported segregation through policies and practices that barred introducing “any individuals whose presence will clearly be detrimental to property values in that neighborhood,” including due to race or nationality, and even drafted a standard restrictive covenant for clients’ use (Jones-Correa, 2000). When Blacks did manage to overcome these barriers and move into White neighborhoods, they faced threats and violence intended to force them to move and deter others from moving in. This violence could be extreme; in Chicago, for example, 58 homes of Blacks who attempted to move into adjacent White neighborhoods were bombed from 1917 to 1921 (Massey and Denton, 1993). In 1948, the Supreme Court ruled in SheRey v. Kraemer that government enforcement of covenants was illegal. However, despite their legal unenforceability, restrictive covenants were still frequently used (Brooks, 2011). Indeed, the FHA continued to recommend the use of covenants in its guidelines for two years after this ruling (Massey and Denton, 1993).
These policies and practices hardened existing lines of segregation (Aaronson et al., 2017), prevented aspiring non-White homeowners from affording homeownership without extreme difficulty while Whites could do so with relative ease, and reduced the potential equity of homes in non-White neighborhoods. The limited housing options available to poor and non-White individuals constrained them to unaffordable, unstable, and poor-quality housing. A dual housing market was in essence created, in which high demand for limited supply of housing in the restricted neighborhoods available to Blacks allowed landlords to charge high rents for overcrowded, poorly-maintained units (Satter, 2009; K.-Y. Taylor, 2012). Furthermore, unequal access to home equity prevented wealth accumulation across generations, limiting marginalized groups’ ability to afford healthy housing and saddling them with poorer health associated with socioeconomic status (Chetty et al., 2016). Thus, not only is inability to build home equity a consequence of structural inequalities, it also helps to reproduce and concretize them.
Due to setbacks to legal segregation and still-increasing Black migration to cities, it became increasingly challenging to maintain lines of segregation; this resulted in “White Flight” to the suburbs, creating a starkly segregated pattern of White suburbs and Black cities. Massive federal funding for highways and loan program appraisal criteria favoring suburban neighborhoods subsidized and facilitated the residential shift of White homeowners to suburbia. Thus, the city became increasingly minority and low-income in contrast to the Whiter and wealthier suburbs; disinvestment in urban communities of color quickly followed (Avila and Rose, 2009). Marginalized populations also bore the burden of mass displacement during subsequent urban renewal—a federal program in which the government displaced residents by razing ‘blighted’ sites and turning them over at a subsidized cost for private development. The neighborhoods targeted by urban renewal were largely non-White and low-income, to the point that it was dubbed ‘Negro removal’ (Fullilove, 2001). Additionally, far more housing units were destroyed than were created to replace those that displaced families lost (Carpenter and Ross, 2009; Fullilove, 2001); the public housing subsequently built to replace it was highly segregated by race and class (Rothstein, 2017).
Although Blacks have historically been the largest racial and ethnic minority in the U.S. and the focus of most of the available literature on the origins of housing disparities, they are by no means the only group to have experienced structural impacts to housing. For instance, Latino immigration to the U.S. has increased dramatically: they represented 4.7% of the U.S. population in 1970 but 17.3% in 2010 (Massey et al., 2016). Moreover, for centuries, Native Americans have been forcibly displaced, removed from their lands (often in abrogation of legal treaties) to facilitate expanding White settlement.
Today, these groups face continued barriers to renting or purchasing and maintaining a home, albeit in new forms. In what is often referred to as ‘reverse redlining,’ poor and non-White neighborhoods were targeted for predatory lending of subprime loans with high interest rates and unfavorable terms, even if they qualified for better loans (Beeman et al., 2011). When the housing bubble burst and the financial crisis hit, these communities were, in turn, adversely affected; Black, Latino, and racially integrated neighborhoods had much higher foreclosure rates than White neighborhoods (Hall et al., 2015). Marginalized populations’ vulnerability to losing their home is further exacerbated by laws and policies that place them at risk for excessively high property taxes and fees (Atuahene and Hodge, 2018). Making matters worse, many cities have privatized liens on tax-delinquent properties to generate funding by selling them to private, often for-profit, investors who charge crippling interest rates, add additional fees, and ultimately take away people’s property for debts as low as tens of dollars (Kahrl, 2017).
Furthermore, public housing, long a source of affordable housing when none was available in the market, is being reduced. Public housing construction halted in the 1970s, leaving the provision of affordable housing to the private market (Section 8 vouchers and Low-Income Housing Tax Credit); such units can be difficult for residents to secure, and are often less affordable due to rents being set at the market rate rather than as a percentage of household income and located in high-poverty neighborhoods (DeLuca et al., 2013; Mast, 2013; Sharkey, 2012). Housing discrimination based on source of income, though illegal, is rarely enforced and fundamentally threatens housing choice voucher holders, particularly in gentrifying markets and high-opportunity neighborhoods (Aratani et al., 2018). Furthermore, as of 2012, the Department of Housing and Urban Development approve the repositioning of around 20% of the nation’s total public housing stock (285,000 units) through the Rental Assistance Demonstration (RAD) Program , including almost all units in some cities (Goetz, 2013). This trend is demonstrated by the HOPE VI program, which rebuilt public housing complexes into lower-density, mixed-income communities and reduced the number of available public housing units, forcing residents to move and navigate the private housing market with vouchers.
Housing discrimination, which can occur at multiple points in the process of securing a housing unit (e.g., whether a broker or landlord responds to an inquiry and how quickly they do so), still continues (Turner et al., 2013). Many marginalized groups have experienced significant housing discrimination, limiting their ability to select healthy housing and contributing to segregation. Another process, gentrification (the movement of higher-income, often White residents into lower-income neighborhoods) has occurred in many urban areas since the 1990s (Hwang and Lin, 2016), dramatically so in Washington D.C., San Francisco, New York, and Miami. Rising rents and harsh displacement tactics raise concerns for vulnerable long-term residents in the context of gentrification (K. Newman and Wyly, 2006).
In addition to these discriminatory processes, certain groups and locations continue to experience specific issues. For example, there is a severe shortage of any housing, let alone affordable and decent housing, and high rates of homelessness in Native American lands (Pindus et al., 2016) ; those who live in cities must struggle against poverty and discrimination to find adequate housing (Levy et al., 2017). The U.S. Latino population is highly heterogeneous (e.g., country of origin, foreign-born status, and documentation status) whose subgroups experience significant differences in their geographic distribution and marginalization (Massey et al., 2016). Thus, they may face different types of housing challenges (e.g., urban vs. rural), including the degree and impact of experiences of marginalization. For example, the majority of migrant farmworkers are undocumented Mexican immigrants who have little protection against wage exploitation (Donohoe and Koreishi, 2010); they often must find housing on a tight budget in small rural communities with limited supply and tenants have little recourse due to their social and economic vulnerability (American Public Health Association, 2011).
Altogether, these policies, practices, and other processes that shape social and health disparities make marginalized groups more likely to experience substandard housing and neighborhoods with deleterious health effects, while struggling with affordability and at higher risk for residential instability. The overall result, perpetuated housing disparities, is now entrenched in the American housing experience. These historical roots largely play out via mechanisms described in detail in the following section as what we term the four pillars of housing. In addition to tracing the links to health, we also describe the complexity of housing and health disparities in an original conceptual model.
3. The four housing pillars and associations with health outcomes
We now explore each of the four housing pillars, or features of the housing environment, in detail and outline the health outcomes associated with each. The four pillars are: 1) cost, 2) conditions, 3) consistency, and 4) context; the “4 C’s” of healthy housing. Cost represents housing affordability, whether residents can pay the cost of the housing without burden. Conditions encompass the adequacy of physical hardware and environmental conditions of the building and unit. Consistency describes residential stability and residents’ ability to remain in their home for as long as they desire. Finally, context characterizes the presence of positive or adverse health-relevant resources in the surrounding neighborhood.
The full model below (Fig. 2) outlines the unequal structures discussed previously that create housing disparities across the four pillars. In conjunction with various mediators and moderators, these housing disparities then translate into poor health outcomes. Next, we explain each of the pillars and summarize corresponding evidence.
Fig. 2.
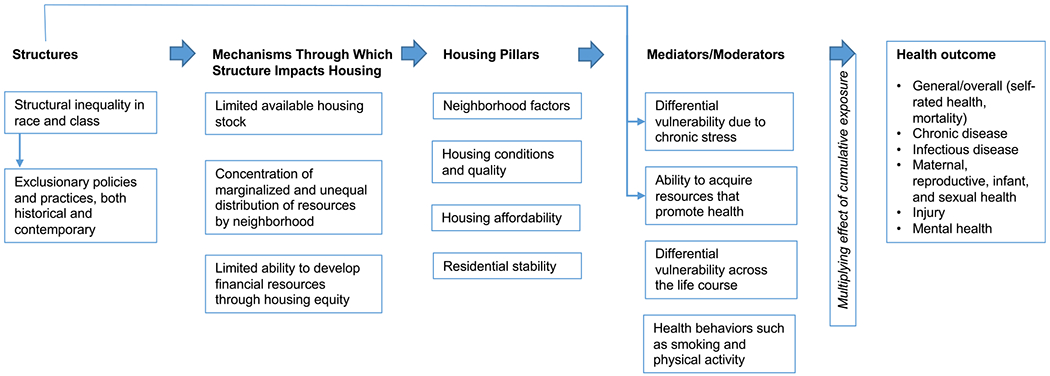
The housing and health disparities conceptual model.
3.1. Cost
Significant disparities exist in housing affordability, including, by income, race, and ethnicity. General societal consensus dictates that lower-income households should not spend above 30% of their income on rent, at which point they are considered ‘rent-burdened.’ In contrast, wealthier households may have sufficient disposable income to voluntarily spend more than 30% of income for higher-quality housing without being rent-burdened, but lower-income households lack this flexibility. Ninety percent of households below the federal poverty line now meet this definition, but this is true for only 20% of those at 200% or more of the poverty line. About half of Black and Latino households are rent-burdened, compared to only a third of White households (Desmond, 2015).
Affordability has a number of direct and indirect pathways to health, although this link is considerably understudied (Meltzer and Schwartz, 2016). Living in unaffordable housing is associated with poorer self-rated health, hypertension, arthritis, and mental health (Meltzer and Schwartz, 2016; Pollack et al., 2010; Bentley et al., 2011; Burgard et al., 2012). Additionally, unaffordability impacts health indirectly by draining financial resources that could otherwise be used for necessary-health services or prescriptions (Meltzer and Schwartz, 2016; Pollack et al., 2010) and health-related expenses such as food (Fletcher et al., 2009) and child development resources (S. Newman and Holupka, 2016).
Housing operating costs, such as utilities, are also burdensome and consequential for health. Low-income households are more likely to reside in older, poorer-quality, less energy-efficient homes and to allocate a greater share of their income to energy expenditures (Hernández, 2013). Energy insecurity is associated with chronic stress related to worries over energy bills and home conditions and adverse physical health outcomes related to thermal discomfort and related conditions such as excess dampness and extreme home temperatures (Hernández, 2016b).
A prevalent coping strategy among low-income people to address high rent burdens is ‘doubling up’ and overcrowding, which can provide significant and valuable savings. For example, a study of low-in-come mothers in large cities found that almost 50% had doubled up at some point before their child was nine (Pilkauskas et al., 2014). Despite the financial benefits, overcrowding is associated with adverse health outcomes. Research has demonstrated its link to mental health outcomes (Campagna, 2016), tuberculosis (Braubach et al., 2011), behavioral issues such as hostility (Chambers et al., 2015), and children’s educational outcomes (Lopoo and London, 2016), among others. Overcrowding in the home can exert a particularly strong effect on children, who need quiet space to concentrate on schoolwork and have less of a world outside the home (Solari and Mare, 2012).
Homeowners experiencing mortgage delinquency or foreclosure are at higher risk for adverse mental health outcomes, including psychological distress, anxiety, depression, substance use, and suicide (Alley et al., 2011; Tsai, 2015); one study found that Americans over 50 who were mortgage-delinquent were nine times as likely to develop elevated depressive symptoms (Alley et al., 2011). Other evidence points to foreclosure’s adverse effect on physical health (Burgard et al., 2012; Cannuscio et al., 2012). As previously discussed, marginalized groups were heavily targeted for subprime loans and were therefore more vulnerable to foreclosure, disproportionately exposing them to these adverse health outcomes.
3.2. Conditions
Numerous physical characteristics of housing can affect the health of its inhabitants. Black, Native American, Hispanic, and low-income homes have higher rates of housing condition inadequacies (Jacobs, 2011; U.S. Census Bureau, 2017). Marginalized populations are more likely to experience a range of factors that determine the likelihood and degree of exposure to harmful conditions in the home such as older deteriorating housing stock, outdated infrastructure, and deferred maintenance; such exposures are often exacerbated by unequal power dynamics between landlords and tenants (Adamkiewicz et al., 2011; Grineski and Hernández, 2010).
Inability to maintain thermal comfort can affect residents’ health by interfering with the body’s ability to thermoregulate. Cold is associated with depression (Liddell and Guiney, 2015) and a range of physical health outcomes including high blood pressure, respiratory conditions, and general self-rated health (Lloyd et al., 2008; Ormandy and Ezratty, 2012; Pierse et al., 2013). Lower-income residents are more likely to not only experience more difficulty affording any energy bill, but to live in energy-inefficient homes that are more difficult to warm (Hernández, 2016b). Interventions that improve thermal comfort (e.g., insulating) significantly improve physical and mental health and have been robustly examined in the literature (Liddell and Guiney, 2015; Thomson et al., 2013).
Pests can cause and trigger attacks of allergic sensitization and eventually, asthma (Do et al., 2016; Olmedo et al., 2011). Pest prevalence is higher in the homes of marginalized populations (U.S. Census Bureau, 2017), likely because they are more likely to live in dilapidated housing that facilitates entry (Peters et al., 2007; Rauh et al., 2002). As a result, health conditions associated with pests are also more common in these populations; asthma, for example, disproportionately burdens low-income Black and Puerto Rican children (Centers for Disease Control and Prevention, 2019; Holt et al., 2013). Dampness and mold also affect low-income households at a higher rate (U.S. Census Bureau, 2017). The association between such environments and health outcomes has been well-documented, predominantly regarding respiratory health (including allergic rhinitis, persistent colds, asthma, sneezing, and chronic bronchitis), with some evidence pointing to mental health as well (Institute of Medicine (US) Committee on Damp Indoor Spaces and Health, 2004).
A wide range of harmful environmental exposures come from within the home. Lead is highly toxic and exposure to it has well-documented, significant, irreversible adverse health effects, even at low levels (e.g., neurological problems and related cognitive and behavioral issues) (Centers for Disease Control and Prevention, 2012). Exposure is highly unevenly distributed, concentrated in lower-socioeconomic individuals and neighborhoods (Sampson and Winter 2016). An overlapping inequitably patterned issue is reliable in-home access to safe drinking water free from contaminants (e.g., heavy metals or bacteria) (Balazs and Ray, 2014; McDonald and Jones, 2018). Additionally, secondhand smoke continues to be associated with the deaths of 42,000 non-smokers each year (Max et al., 2012). The 27.6–28.9 million residents of multi-unit housing, mostly disadvantaged group members, that do not allow smoking in their individual units, are still exposed to secondhand smoke each year (King et al., 2013). Accordingly, significant disparities exist in secondhand smoke exposure: 67.9% of Black children are exposed compared to 37.2% of White children each year (Homa et al.,2015), and exposure increases as socioeconomic status decreases (Gan et al., 2015). Other indoor toxic environmental exposures such as levels of numerous pollutants affected by related socioeconomic factors, and thereby may also be associated with socioeconomic disparities (Adamkiewicz et al., 2011).
Physical conditions of the home can also cause injury; the home is the second-most-common location for unintentional fatal injuries (Runyan et al., 2005). Injury is the leading cause of death for people ages 1–44 (Centers for Disease Control and Prevention, 2018), and rates are particularly high for older adults, who are more frail, and young children (Runyan et al., 2005). Housing risk factors for falls include inadequate lighting, lack of window guards, and structural deficiencies (e.g., uneven floors). Meanwhile, lack of functioning smoke alarms, carbon monoxide detectors, sprinklers, and other fire suppression requirements can lead to injury and death. Fire-related injuries and death are higher in lower-income groups, potentially due to their likelihood to live in older homes and homes with greater risks and fewer protections (Gielen et al., 2012; Shai, 2006). Beyond risk of injury, for people with functional impairments, appropriate building design and construction are important for basic access to important home amenities such as kitchen shelving or toilets (Office of the Surgeon General (US), 2009).
Social disorder and crime also occur within multi-unit buildings, thereby affecting residents’ sense of safety within residential environments. Historically, given the high degree of isolation and disinvestment in large public housing complexes, crime rates have been high in some buildings, and residents have cited drug-dealing and gangs as major building-related concerns (Popkin et al., 1999, 2002). While such safety is largely a social concern, physical conditions such as the presence or absence of features that restrict access to residents and facilitate surveillance (e.g., properly-locking doors) also contribute to safety concerns (Tillyer and Walter, 2018). Importantly, safety is under-explored in settings beyond public housing, but could potentially arise as a concern in any type of housing or community setting. As will be discussed further in the Context section, violence can be a health concern in its own right, but social disorder and fear of violence can also contribute to mental health issues (e.g., stress, anxiety and depression), limit interactions with neighbors, and reduce opportunities for physical activity outside (Hernández, 2016a).
3.3. Consistency
Residential stability encompasses residents’ capacity to willingly remain in their homes free from harassment or dispossession. While individuals may move voluntarily for many reasons (e.g., for a new job or a larger home), there are a number of reasons that involuntary moves (displacement) could occur, including inability to afford rising rents or mortgage payments, eviction or foreclosure, natural disaster, and government policies. Scholars variously operationalize residential instability as being behind on rent or mortgage payment, making more than a given number of moves within a given period of time, experiencing homelessness, being evicted, experiencing foreclosure, overcrowding, and/or doubling up (Burgard et al., 2012; Sandel et al., 2018; Vijayaraghavan et al., 2013). High residential mobility rates are largely due to forced displacement, primarily eviction, rather than to voluntary moves (Desmond et al., 2015) and displacement occurs along axes of inequality. Low-income families move far more often than higher-in-come counterparts; 26% of households below the poverty line move each year compared to less than 12% of those above 150% of the poverty line (Ihrke et al., 2011). Furthermore, “serial forced displacement” for marginalized populations describes the compounding effect of multiple instances of displacement over time via various mechanisms (e.g., through gentrification, natural disasters and planned shrinkage). Often, the most marginalized, especially African Americans, are forced to move frequently and against their will (Fullilove and Wallace, 2011; Saegert et al., 2011).
Housing stability has numerous health implications. Evidence indicates that residential instability is associated with a wide range of adverse health outcomes, including poorer self-rated health, health care access, and mental health outcomes (Jaworsky et al., 2016; K. W. Reid et al., 2008; Suglia et al., 2011). Children and adolescents are particularly vulnerable to impacts of residential instability, including poorer overall health, developmental and behavioral problems, and lower school readiness and educational outcomes (Cutts et al., 2011; Ziol-Guest and McKenna, 2014). Precarious employment and low wages impact one’s ability to afford healthy housing and other health-related resources (Desmond and Gershenson, 2016).
Health implications have also been identified for specific displacement mechanisms. Mindy Fullilove (2001) proposes that state urban renewal programs affected health through three pathways: 1) directly causing stress; 2) forcibly displacing residents to live in poor housing and/or in unhealthful neighborhoods; and 3) requiring resettlement resource expenditures that could otherwise have been used for health-promoting purposes (e.g., healthy food and recreation). Evidence on contemporary public housing transformation initiatives has similarly often shown disappointing effects for low-income households (Goetz and Chappie, 2010; Keene and Geronimus, 2011). For example, Keene and Geronimus (2011) use the weathering framework to posit that HOPE VI contributed to chronic stress and increased allostatic load through loss of protective social resources, promotion of health-demoting stereotypes about low-income Black communities, and psychological trauma associated with community uprooting.
In the context of climate change, natural disasters are increasingly a major threat for displacement as they can instantly damage and destroy massive amounts of housing. Marginalized groups’ homes are more likely to be adversely impacted by natural disasters and are less likely to be able to return home. Studies of Hurricane Katrina found that Black and subsidized housing residents were less likely to return home following rebuilding, due not only to greater property damage, but also to racially discriminatory government housing programs and policies, including demolition of undamaged public housing units (Green et al., 2013; Kamel, 2012). This permanent displacement was associated with lower likelihood of retaining access to primary care facilities and higher likelihood of adverse mental health outcomes including higher psychological distress, higher perceived stress, and symptoms of severe mental illness (Fussell and Lowe, 2014; Hori and Schafer, 2010).
Residential stability is closely linked to affordability. A major reason that individuals may be housing insecure is because they cannot afford the rent, mortgage payments, or property taxes. Renters typically have less housing security because they are vulnerable to rent increases and, as described earlier, marginalized populations are more likely to be renters. Being behind on rental payments or worrying about having enough money to pay rent is also associated with depression and frequent mental distress (Burgard et al., 2012; Liu et al., 2014). A recent study found that residents displaced from gentrifying neighborhoods experience adverse mental health outcomes, emergency department visits, and hospitalizations (Lim et al., 2017). While eviction is significantly understudied, the limited evidence available indicates that marginalized populations, particularly low-income Black women, are disproportionately affected. For example, in Milwaukee, Black women represent 9.6% of the population but 30% of evictions; one in five reports being evicted in their lifetime, compared to one in 15 White women (Desmond and Shollenberger, 2015). One analysis of low-in-come urban mothers found that evicted mothers were more likely to have depression and to report worse overall health for both themselves and their children (Desmond and Kimbro, 2015).
Finding stability post-displacement can pose significant continued health challenges. Households may need to move very quickly, have few resources to do so, and less ability to compete for scarce housing stock, thereby creating risk of moving to more disadvantaged neighborhoods and future displacements (e.g., in the case of a disaster) (Bullard and Wright, 2009; Desmond and Shollenberger, 2015; Ding et al., 2016). Additionally, landlords look to publicly-available eviction records when screening tenants; therefore, a legal analysis concludes that “any tenant who has been named in an eviction proceeding is effectively barred from obtaining safe, decent, and healthy housing” (Gold, 2016). Thus, residents are limited to a small pool of available, affordable, decent quality housing (Desmond et al., 2015; Gold, 2016). Residential instability also increases employment insecurity; a forced move results in an 11–22 percentage point increase in the likelihood of losing one’s job, thus impacting one’s ability to afford healthy housing and other health-related resources (Desmond and Gershenson, 2016).
3.4. Context
A rapidly growing body of research indicates that neighborhood characteristics and resources exert an effect on residents’ health independent of individual-level attributes. As previously discussed, strong patterns of segregation by race and income persist in American neighborhoods and there is a well-documented relationship between segregation and concentrated poverty with poor health outcomes (Andersen et al., 2018; Williams and Collins, 2001). This association is likely attributable to the highly unequal distribution of health-relevant neighborhood risk exposures including, for example, violence, the siting of environmental hazards, and aspects of the built environment.
Reliable and affordable public transportation can affect access to health care, and provide means by which to secure employment and engage in other health-related activities (e.g., visiting friends and family, attending religious services or going to the gym) (Mackett and Thoreau, 2015). Relatedly, walkable neighborhoods (Sallis et al., 2009) and availability of green spaces, parks, and playgrounds (Cohen et al., 2007; Han et al., 2013) can increase physical activity and thereby reduce obesity and related conditions. This is particularly important for marginalized groups since they have higher rates of obesity and related health outcomes (“Overweight and Obesity Rates for Adults by Race/Ethnicity,” 2017). Green spaces are also linked to reduced stress (Sturm and Cohen, 2014). However, neighborhood disparities exist in walk-ability (Watson, 2016) and in the amount and quality of parks (Duncan et al., 2013; Rigolon, 2016), attributed to unequal access to high-quality resources via conditions of segregation (Arroyo-Johnson et al., 2016; García et al., 2016; Kelly et al., 2007).
A growing concern related to climate change is how features of the built environment can protect against or exacerbate extreme weather, due to increased frequency and intensity of heat waves, warmer weather (Anderson and Bell, 2011; White-Newsome et al., 2012), and flooding (Slater and Villarini, 2016). Elevated heat risk from lack of tree canopy or impervious surfaces (Mitchell and Chakraborty, 2014) is associated with higher neighborhood poverty and higher percentage of minority residents (Jesdale et al., 2013), and correspondingly higher land surface temperature, particularly in highly-segregated areas. Accordingly, there are significant disparities in heat-related morbidity and mortality (Klein Rosenthal et al., 2014; C. E. Reid et al., 2009).
Finally, the presence and condition of certain buildings and facilities can affect residents’ health. Robust evidence demonstrates that environmental hazards (e.g., waste processing facilities, Superfund cleanup sites, and highways) are disproportionately sited in low-income communities and/or communities of color (Sicotte and Swanson, 2007), exposing residents to environmental toxins (Bell and Ebisu, 2012). Unsurprisingly, these relationships are stronger in more highly-segregated areas with a larger concentration of marginalized groups (Ard, 2016; Morello-Frosch and Lopez, 2006). Additionally, the presence of blight (i.e., abandoned buildings and lots in a state of visible disrepair) is associated with risk of violent assault (Branas et al., 2012), and correspondingly, evidence indicates that blight remediation programs (e.g., greening lots and remediating doors and windows) reduce firearm violence and stress and increase physical activity (Branas et al., 2011, 2016). Researchers have also found links between blight and fire, which creates injury hazard (Schachterle et al., 2012); adverse birth outcomes (Nowak and Giurgescu, 2017); sexual health implications; and overall mortality risk (Cohen et al., 2003).
Neighborhood institutions, such as retail stores and local services, can also affect health. The availability of supermarkets rather than convenience stores is strongly associated with a healthy diet rich in fruits and vegetables and lower levels of obesity, a relationship that is even stronger for Blacks than for Whites (Larson et al., 2009; Morland et al., 2002). However, low-income and minority neighborhoods disproportionately have more fast-food outlets and lack retailers selling fresh and healthy food (Bower et al., 2014; Kwate, 2008). Similar retail trends are evident for tobacco (Lee et al., 2017) and liquor (Romley et al., 2007). Disparities in healthcare services exist across neighborhoods (Gaskin et al., 2012), particularly in more segregated cities.
Neighborhood social characteristics, too, have been linked to health outcomes. Collective efficacy, a strong sense of social connectedness and solidarity across members of a group, can prevent adverse health outcomes by enforcing positive social norms of behavior, providing a supportive and trusting environment, and advocating more forcefully for desired resources. Violence and crime are a health outcome in their own right. Black, Hispanic, and low-income individuals are more likely to be victims of serious violent crimes (Beard et al., 2017; Sackett, 2015) and to be exposed to violence in their community (Friedson and Sharkey, 2015). Exposure to violence affects mental health (Clark et al., 2008; Curry et al., 2008) and birth outcomes of pregnant women (Kane, 2011; Okah et al., 2014). It can also contribute to numerous acute physical health issues (A. W. Wright et al., 2017; R. J. Wright, 2006) and long-term biological weathering (Aiyer et al., 2014).
3.5. Mediators and moderators between the four pillars of housing and poor health
The pillars of housing do not exist in isolation from one another, but together form a web of housing-related factors that may impact the health and well-being of individuals and households. The effect of any one housing exposure on a health outcome is additionally influenced by other relevant social and housing factors. Furthermore, other forms of social inequality and vulnerability, may also affect the same health outcomes and can moderate or mediate housing exposures’ effects. These multiple exposures may have a cumulative impact—an effect that is compounding and exponential, rather than additive (Corburn, 2017). Multiple housing exposures may coexist and affect residents in a single home due to shared origins of structural inequality (Adamkiewicz et al., 2014). Additionally, residents with limited resources may have to make trade-offs in their housing choices (e.g., a less expensive home in a neighborhood with fewer health-promoting resources), accepting hazards in one domain to achieve stability in others (Coley et al., 2014; Hernández, 2016a).
Individuals may have differential susceptibility in their exposure to housing disparities for various reasons, which in turn influence health impacts. From a life course perspective, risk can vary significantly across life stages: children are uniquely vulnerable to adverse effects of environmental exposures due to behavioral and biological characteristics (Landrigan et al., 2010); the prenatal period is also a sensitive window during which the developing fetus may be affected by housing factors (Perera et al., 2012); and the elderly experience increased vulnerability due to the impact of aging and frailty on the body’s ability to adapt to stress (Fedarko, 2011). Furthermore, marginalized groups also experience oppression and inequality in many dimensions beyond housing, which interact with housing disparities, as described previously, but also have a separate effect that can exacerbate the impact of housing disparities. Psychosocial stress due to discrimination and life difficulties while high among racial and ethnic minorities, can, over time, cumulatively disrupt regulation of body systems and impose a physiological burden, resulting in wide-ranging premature health deterioration known as weathering (Geronimus et al., 2006). Emerging research on differential vulnerability suggests that weathering can modify the association between housing exposures and health outcomes, amplifying the adverse effects. For example, the relationship between lead and adverse health outcomes is stronger for marginalized groups who have higher stress and allostatic loads (Zota et al., 2013).
To demonstrate how a health outcome can be influenced by housing disparities across multiple pillars and vary based on the factors described above, we explore the example of asthma – a condition with striking disparities in population distribution (Holt et al., 2013). Asthma is affected by the confluence of and interaction between social inequities and resultant housing disparities. A range of neighborhood and housing aspects are associated with higher asthma risk and are more common among marginalized populations, including traffic-related air pollution, pests, dampness and mold, indoor thermal conditions, and exposure to community violence (Beck et al., 2016; Corburn et al., 2006). Furthermore, asthma is exacerbated by social exposures (Bryant-Stephens, 2009); chronic, toxic stress from accumulated discrimination and disadvantage can not only increase vulnerability to housing factors associated with asthma, but also increase asthma’s severity by causing airway inflammation and other physiological changes (Rosenberg et al., 2014). Other risk factors related to asthma (e.g., low birth weight) are also common among marginalized populations (Alexander and Currie, 2017).
These factors interact to create an amplified effect greater than one in isolation. For example, studies have found that exposure to traffic-related air pollution is associated with asthma only when a child has also been exposed to community violence (Clougherty and Kubzansky, 2008), or is more strongly associated when a child or parent has high levels of chronic stress (Chen et al., 2008; Shankardass et al., 2009). Similarly, another study found that the degree of a child’s neighborhood racial composition explains whether or not a child with low birth weight developed asthma, pointing to the moderating effect of low birth weight and neighborhood segregation (Alexander and Currie, 2017).
4. Discussion
An expansive body of literature indicates severe health implications of housing insecurity across four pillars that are disproportionately borne by marginalized populations. The philosopher Norman Daniels (2001) has argued that health care has a special moral importance because it enables normal functioning and thus equality of opportunity; we extend this claim to housing. Given the impacts of inadequate housing on wide-ranging aspects of health and well-being, access to decent housing is essential to opportunity. Further, disparities in access to decent housing did not emerge naturally, but were socially produced and imposed upon the marginalized largely through discriminatory private and governmental actions, inequitable policies, and a failure to create protective policies. Housing disparities are fundamentally unjust and merit remedial action because of their significant impact, their concentration among the most vulnerable, and their socially created and unnatural origins that represent a failure of American government to uphold its responsibilities. Policy interventions that work with public and private housing providers and local authorities to create more equitable housing opportunities are therefore justified and long-overdue.
It is urgent for public health practitioners to act on housing as a tool to reduce, rather than exacerbate, health disparities. To do so, the field of public health should adopt a vision for equitable, healthy housing and identify strategies to achieve it. The vision is articulated as follows:
Health equity in housing would entail opportunities for all individuals, regardless of race/ethnicity, socioeconomic status, household composition, or zip code, to benefit from developments in modem building, science, fair maintenance practices, community planning, and creative uses of space through programming, to foster a culture of health and social connections.
Indoors: Homes and buildings would be newly built, renovated, and maintained to reflect standards such as energy efficiency, adequate space, appropriate ventilation, good lighting, and smoke-free policies. Meanwhile, hazards such as lead paint, asbestos, mold and pest infestation would be effectively abated.
Outdoors: Amenities such as green space, community rooms, play areas, and quiet zones, along with active design elements such as well-lit and easily accessible stairways and walkways, would be standard practice rather than luxury items, afforded to renters and homeowners at all income levels and adapted for multiple housing types (i.e., multiple-unit housing and single-family homes/communities).
Health equity in housing would also involve development subsidies to expand affordable housing at a wider range of income levels and siting of affordable housing developments in high-opportunity neighborhoods.
Lastly, land-use and zoning policies would support health-promoting institutions and recreational opportunities while also retaining stability for local residents and small businesses as new developments are introduced. The distribution of hazardous facilities would be more even across communities.
Housing plus health equity strategies should span all four pillars of housing by: 1) encouraging the physical design and programming of residential space to promote health; 2) adopting a health-in-all-policies approach to housing and community development; 3) preserving, improving and better connecting existing affordable housing; and 4) expanding supportive housing options for populations facing the greatest barriers to access. Additionally, given that the origins of housing disparities are rooted in unjust actions and inequitable neglect by policymakers, effectively-targeted solutions to preventing and alleviating housing disparities must occur at the policy level and should include comprehensive solutions to correct past injustices. Furthermore, because the policies and processes that caused housing disparities emerged from a denial of the full humanity and equality of marginalized groups (or what Atuahene refers to as “dignity takings”), and because housing disparities continue to be exacerbated by inequalities also caused by this denial, this vision should include more than material compensation, but also pathways towards broader integration and empowerment (“dignity restoration”) (Atuahene, 2016).
Admittedly, such a vision of housing is rooted in a normative notion of equity and could raise concerns regarding cost. However, costs may be at least in part mitigated by downstream savings. Investments that ensure decent housing quality, stability, affordability and neighborhood conditions could produce cost-offsets, most obviously in health care, but also in sectors such as energy, education, and the economy (Braubach et al., 2011). Public administrators who make siloed decisions about housing or healthcare may fail to recognize how deferred costs in one realm may create additional expenses in the other. For example, asthma caused by deficient housing is not only a health issue, but a social and economic problem; one recent study estimates the total cost of asthma in the United States as $81.9 billion per year (Nurmagambetov et al., 2018). Poorly controlled asthma results in preventable emergency room visits, lost productivity at work (Akinbami et al., 2011), lower academic achievement, and fewer long-run life chances (United States Department of Labor, Bureau of Labor Statistics, 2018). By these measures, housing investments may be significantly lower-cost than they appear in the long run.
5. Conclusion
This review offers a conceptual model for the relationship between housing and health equity, identifying key aspects of housing that relate to health, assessing exposure disparities, and demonstrating the origins of this unequal exposure in structural inequality. Historically and contemporaneously, race and class have shaped different housing opportunities for marginalized groups in the U.S., such that low-income and racial/ethnic minority groups are more likely to inhabit substandard housing in neighborhoods with adverse health attributes. They also struggle with residential instability and lack of affordability. These housing issues are associated with a comprehensive range of health consequences, whose impact on marginalized residents is especially severe given the likelihood of multiple simultaneous exposures and individual vulnerability due to chronic stress.
The notion that decent housing is a luxury rather than a right presents a fundamental threat to health and social equity. There is a critical need to shift the present discourse, and even more importantly, practice, such that adequate attention is given to the underlying housing conditions that support health, well-being, and a sense of community. Paramount to achieving health equity is recognizing housing as an important source of health and well-being, not just among stakeholders in public health, but also in the multi-sectorial fields that intersect with housing. Advancing this narrative will require interdisciplinary collaboration between clinicians, public health practitioners, city and regional planners, housing developers, and architects to consider the health impacts of housing affordability, conditions, stability, and the surrounding community.
Acknowledgements
The authors gratefully acknowledge the contributions of Dr. Ronald Bayer in reviewing an earlier draft of this manuscript and Samantha Sawyer for providing editorial support. DH has no conflicts of interest to report. CS reports employment at a wellness real estate and technology company whose work and offerings include the design of indoor spaces to improve the health and wellness of occupants of the space (beginning after the manuscript was drafted). The writing of this manuscript was partially supported by a JPB Environmental Health Fellowship granted to Diana Hernández and managed by the Harvard T.H. Chan School of Public Health Grant; and a Career Development Grant from the National Institute of Environmental Health Sciences (NIEHS) under Grant P30ES009089.
References
- Aaronson D, Hartley D, Mazumder B, 2017. The Effects of the 1930s HOLC “Redlining” Maps. Federal Reserve Bank of Chicago; Retrieved from. https://www.chicagofed.org/publications/working-papers/2017/wp2017-12. [Google Scholar]
- Adamkiewicz G, Spengler JD, Harley AE, Stoddard A, Yang M, Alvarez-Reeves M, Sorensen G, 2014. Environmental conditions in low-income urban housing: clustering and associations with self-reported health. Am. J. Public Health 104 (9), 1650–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adamkiewicz G, Zota AR, Fabian MP, Chahine T, Julien R, Spengler JD, Levy JI, 2011. Moving environmental justice indoors: understanding structural influences on residential exposure patterns in low-income communities. Am. J. Public Health Washington 101 (S1), S238–S245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiyer SM, Heinze JE, Miller AL, Stoddard SA, Zimmerman MA, 2014. Exposure to violence predicting cortisol response during adolescence and early adulthood: understanding moderating factors. J. Youth Adolesc. 43 (7), 1066–1079. 10.1007/s10964-014-0097-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Liu X, 2011. Asthma prevalence, health care use, and mortality: United States, 2005-2009. Natl. Health Stat. Rep (32), 1–14. [PubMed] [Google Scholar]
- Alexander D, Currie J, 2017. Is it who you are or where you live? Residential segregation and racial gaps in childhood asthma. J. Health Econ. 55,186–200. 10.1016/j.jhealeco.2017.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alley DE, Lloyd J, Pagán JA, Pollack CE, Shardell M, Cannuscio C, 2011. Mortgage delinquency and changes in access to health resources and depressive symptoms in a nationally representative cohort of Americans older than 50 years. Am. J. Public Health Washington 101 (12), 2293–2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Public Health Association, 2011, November 1 Improving housing for farm-workers in the United States is a public health imperative. Retrieved March 11, 2018, from. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/09/10/32/improving-housing-for-farmworkers-in-the-united-states-is-a-public-health-imperative.
- American Public Health Association, National Center for Healthy Housing, 2014. National healthy housing standard. Retrieved from. https://www.apha.org/~/media/files/pdf/factsheets/national_healthy_housing_standard.ashx.
- Andersen SW, Blot WJ, Shu X-O, Sonderman JS, Steinwandel M, Hargreaves MK, Zheng W, 2018. Associations between neighborhood environment, health behaviors, and mortality. Am. J. Prev. Med 54 (1), 87–95. 10.1016/j.amepre.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GB, Bell ML, 2011. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. Communities. Environ. Health Perspect. 119 (2), 210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aratani Y, Lazzeroni S, Brooks-Gunn J, Hernández D, 2018. Housing subsidies and early childhood development: a comprehensive review of policies and demonstration projects. Housing Policy Debate 29 (2), 1–24. 10.1080/10511482.2018.1515099. [DOI] [Google Scholar]
- Ard K, 2016. By all measures: an examination of the relationship between segregation and health risk from air pollution. Popul. Environ 38 (1), 1–20. 10.1007/s11111-015-0251-6. [DOI] [Google Scholar]
- Arroyo-Johnson C, Woodward K, Milam L, Ackermann N, Komaie G, Goodman MS, Hipp JA, 2016. Still separate, still unequal: social determinants of playground safety and proximity disparities in St. Louis. J. Urban Health 93 (4), 627–638. 10.1007/s11524-016-0063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atuahene B, 2016. Dignity takings and dignity restoration: creating a new theoretical framework for understanding involuntary property loss and the remedies required. Law Soc. Inq. 41 (4), 796–823. 10.1111/lsi.12249. [DOI] [Google Scholar]
- Atuahene B, Hodge T, 2018. Stategraft. [Google Scholar]
- Avila E, Rose MH, 2009. Race, culture, politics, and urban renewal: an introduction. J. Urban Hist 35 (3), 335–347. 10.1177/0096144208330393. [DOI] [Google Scholar]
- Balazs CL, Ray I, 2014. The drinking water disparities framework: on the origins and persistence of inequities in exposure. Am. J. Public Health 104 (4), 603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard JH, Morrison CN, Jacoby SF, Dong B, Smith R, Sims CA, Wiebe DJ, 2017. Quantifying disparities in urban firearm violence by race and place in Philadelphia, Pennsylvania: a cartographic study. Am. J. Public Health 107 (3), 371–373. 10.2105/AJPH.2016.303620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AF, Huang B, Ryan PH, Sandel MT, Chen C, Kahn RS, 2016. Areas with high rates of police-reported violent crime have higher rates of childhood asthma morbidity. J. Pediatr 173, 175–182. e1 10.1016/j.jpeds.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeman A, Silfen Glasberg D, Casey C, 2011. Whiteness as property: predatory lending and the reproduction of racialized inequality. Crit. Sociol 37 (1), 27–45. 10.1177/0896920510378762. [DOI] [Google Scholar]
- Bell ML, Ebisu K, 2012. Environmental inequality in exposures to airborne particulate matter components in the United States. Environ. Health Perspect. 10.1289/ehp.1205201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley R, Baker E, Mason K, Subramanian SV, Kavanagh AM, 2011. Association between housing affordability and mental health: a longitudinal analysis of a nationally representative household survey in Australia. Am. J. Epidemiol. 174 (7), 753–760. 10.1093/aje/kwr161. [DOI] [PubMed] [Google Scholar]
- Bower KM, Thorpe RJ, Rohde C, Gaskin DJ, 2014. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev. Med. 58 (Suppl. C), 33–39. 10.1016/j.ypmed.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branas CC, Cheney RA, MacDonald JM, Tam VW, Jackson TD, Have T, R T, 2011. A difference-in-differences analysis of health, safety, and greening vacant urban space. Am. J. Epidemiol. 174 (11), 1296–1306. 10.1093/aje/kwr273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branas CC, Rubin D, Guo W, 2012. Vacant Properties and Violence in Neighborhoods. ISRN Public Health, New York, 10.5402/2012/246142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branas CC, South E, Kondo MC, Hohl BC, Bourgois P, Wiebe DJ, MacDonald JM, 2018. Citywide cluster randomized trial to restore blighted vacant land and its effects on violence, crime, and fear. Proc. Natl. Acad. Sci, 201718503. 10.1073/pnas.1718503115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braubach M, Jacobs DE, Ormandy D, 2011. Environmental Burden of Disease Associated with Inadequate Housing: A Method Guide to the Quantification of Health Effects of Selected Housing Risks in the WHO European Region. Retrieved from World Health organization Regional Office for Europe, http://www.euro.who.int/_data/assets/pdf_file/0017/145511/e95004sum.pdf. [Google Scholar]
- Braveman P, Dekker M, Egerter S, Sadegh-Nobari T, Pollack C, 2011. Housing and Health (No. 7). Retrieved from Robert Wood Johnson Foundation website, http://www.rwjf.org/en/library/research/2011/05/housing-and-health.html. [Google Scholar]
- Brooks RRW, 2011. Covenants without courts: enforcing residential segregation with legally unenforceable agreements. Am. Econ. Rev 101 (3), 360–365. [Google Scholar]
- Bryant Stephens T, 2009. Asthma disparities in urban environments. J. Allergy Clin. Immunol 123 (6), 1199–1206. 10.1016/j.jaci.2009.04.030. [DOI] [PubMed] [Google Scholar]
- Bullard RD, Wright B, 2009. Race, place, and environmental justice after Hurricane Katrina: struggles to reclaim, rebuild, and revitalize new Orleans and the Gulf coast. Retrieved from, http://ebookcentral.proquest.com/lib/columbia/detail.action?docID=708972.
- Burgard SA, Seefeldt KS, Zelner S, 2012. Housing instability and health: findings from the Michigan recession and recovery study. Soc. Sci. Med 75 (12), 2215–2224. 10.1016/j.socscimed.2012.08.020. [DOI] [PubMed] [Google Scholar]
- Campagna G, 2016. Linking crowding, housing inadequacy, and perceived housing stress. J. Environ. Psychol 45, 252–266. 10.1016/j.jenvp.2016.01.002. [DOI] [Google Scholar]
- Cannuscio CC, Alley DE, Pagán JA, Soldo B, Krasny S, Shardell M, Lipman TH, 2012. Housing strain, mortgage foreclosure, and health. Nurs. Outlook 60 (3), 134–142. el. 10.1016/j.outlook.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter DM, Ross JK, 2009. Testing O’Connor and Thomas: does the use of eminent domain target poor and minority communities? Urban Stud. 46 (11), 2447–2461. 10.1177/0042098009342597. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention, 2012, June 7 CDC response to advisory committee on childhood lead poisoning prevention recommendations in “low level lead exposure harms children: a renewed call of primary prevention”. https://www.cdc.gov/nceh/lead/acclpp/cdc_response_lead_exposure_recs.pdf.
- Centers for Disease Control and Prevention, 2013. Healthy homes assessment tools. comment>Retrieved September 23, 2018, from https://www.cdc.gov/nceh/lead/tools/assessement_tools.htm.
- Centers for Disease Control and Prevention, 2018. WISQARS (Web-based injury Statistics query and reporting system). Retrieved February 9, 2018, from, https://www.cdc.gov/injury/wisqars/index.html.
- Centers for Disease Control and Prevention, 2019. Most recent national asthma data (2017 National Health Interview Survey). Retrieved July 10, 2019, from, https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm.
- Chambers EC, Fuster D, Suglia SF, Rosenbaum E, 2015. Depressive symptomology and hostile affect among Latinos using housing rental assistance: the AHOME study. J. Urban Health 92 (4), 611–621. 10.1007/s11524-015-9965-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Schreier HMC, Strunk RC, Brauer M, 2008. Chronic traffic-related air pollution and stress interact to predict biologic and clinical outcomes in asthma. Environ. Health Perspect 116 (7), 970–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Cutler D, 2016. The association between income and life expectancy in the United States, 2001–2014. J. Am. Med. Assoc 315 (16), 1750–1766. 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark C, Ryan L, Kawachi I, Canner MJ, Berkman L, Wright RJ, 2008. Witnessing community violence in residential neighborhoods: a mental health hazard for urban women. J. Urban Health 85 (1), 22–38. 10.1007/sll524-007-9229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty JE, Kubzansky LD, 2008. Traffic-related air pollution and stress: effects on asthma. Environ. Health Perspect 116 (9), A376–A377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DA, Mason K, Bedimo A, Scribner R, Basolo V, Farley TA, 2003. Neighborhood physical conditions and health. Am. J. Public Health 93 (3), 467–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DA, McKenzie TL, Sehgal A, Williamson S, et al. , 2007. Contribution of public parks to physical activity. Am. J. Public Health 97 (3), 509–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coley RL, Kull M, Leventhal T, Lynch AD, 2014. Profiles of housing and neighborhood contexts among low-income families: links with children’s well-being. Cityscape: J. Policy Dev. Res 16 (1), 37–60. [Google Scholar]
- Corburn J, 2017. Concepts for studying urban environmental justice. Curr. Environ. Health Rep 4 (1), 61–67. 10.1007/s40572-017-0123-6. [DOI] [PubMed] [Google Scholar]
- Corburn J, Osleeb J, Porter M, 2006. Urban asthma and the neighbourhood environment in New York City. Health Place 12 (2), 167–179. 10.1016/j.healthplace.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Curry A, Latkin C, Davey-Rothwell M, 2008. Pathways to depression: the impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland, USA. Soc. Sci. Med 67 (1), 23–30. 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, Frank DA, 2011. U.S. housing insecurity and the health of very young children. Am. J. Public Health 101 (8), 1508–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels N, 2001. Justice, health, and healthcare. Am. J. Bioeth 1 (2), 2–16. [DOI] [PubMed] [Google Scholar]
- DeLuca S, Garboden PME, Rosenblatt P, 2013. Segregating shelter: how housing policies shape the residential locations of low-income minority families. Ann. Am. Acad. Pol. Soc. Sci 647 (1), 268–299. 10.1177/0002716213479310. [DOI] [Google Scholar]
- Desmond M, 2012. Eviction and the reproduction of urban poverty. Am. J. Sociol 118 (1), 88–133. 10.1086/666082. [DOI] [Google Scholar]
- Desmond M, 2015. Unaffordable America: Poverty, Housing, and Eviction. Fast Focus - Institute for Research on Poverty, pp. 22. [Google Scholar]
- Desmond M, 2018. Heavy is the house: rent burden among the American urban poor. Int. J. Urban Reg. Res 42 (1), 160–170. 10.1111/1468-2427.12529. [DOI] [Google Scholar]
- Desmond M, Gershenson C, 2016. Housing and employment insecurity among the working poor. Soc. Probl 63 (1), 46–67. 10.1093/socpro/spv025. [DOI] [Google Scholar]
- Desmond M, Gershenson C, Kiviat B, 2015. Forced relocation and residential instability among urban renters. Soc. Serv. Rev. 89 (2), 227–262. 10.1086/681091. [DOI] [Google Scholar]
- Desmond M, Kimbro RT, 2015. Eviction’s fallout: housing, hardship, and health. Soc. Forces 94 (1), 295–324. 10.1093/sf/sov044. [DOI] [Google Scholar]
- Desmond M, Shollenberger T, 2015. Forced displacement from rental housing: prevalence and neighborhood consequences. Demography 52 (5), 1751–1772. 10.1007/s13524-015-0419-9. [DOI] [PubMed] [Google Scholar]
- Ding L, Hwang J, Divringi E, 2016. Gentrification and residential mobility in Philadelphia. Reg. Sci. Urban Econ 61, 38–51. 10.1016/j.regsciurbeco.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do DC, Zhao Y, Gao P, 2016. Cockroach allergen exposure and risk of asthma. Allergy 71 (4), 463–474. 10.1111/all.12827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohoe MT, Koreishi S, 2010. Historical and contemporary factors contributing to the plight of migrant farmworkers in the United States. Soc. Med 5 (1), 64–73. [Google Scholar]
- Duncan DT, Kawachi I, White K, Williams DR, 2013. The geography of recreational open space: influence of neighborhood racial composition and neighborhood poverty. J. Urban Health 90 (4), 618–631. 10.1007/s11524-012-9770-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedarko NS, 2011. The biology of aging and frailty. Clin. Geriatr. Med. 27 (1), 27–37. 10.1016/j.cger.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer W, Sard B, 2017. Chart Book: Federal Housing Spending Is Poorly Matched to Need. Center on Budget and Policy Priorities, Washington, DC. [Google Scholar]
- Fletcher JM, Andreyeva T, Busch SH, 2009. Assessing the effect of changes in housing costs on food insecurity. J. Child. Poverty 15 (2), 79–93. 10.1080/10796120903310541. [DOI] [Google Scholar]
- Freeman L, 2002. America’s affordable housing crisis: a contract unfulfilled. Am. J. Public Health 92 (5), 709–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedson M, Sharkey P, 2015. Violence and neighborhood disadvantage after the crime decline. Ann. Am. Acad. Pol. Soc. Sci 660 (1), 341–358. 10.1177/0002716215579825. [DOI] [Google Scholar]
- Fullilove MT, 2001. Root shock: the consequences of African American dispossession. J. Urban Health 78 (1), 72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullilove MT, Wallace R, 2011. Serial forced displacement in American cities, 1916–2010. J. Urban Health 88 (3), 381–389. 10.1007/s11524-011-9585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fussell E, Lowe SR, 2014. The impact of housing displacement on the mental health of low-income parents after Hurricane Katrina. Soc. Sci. Med 113 (Suppl. C), 137–144. 10.1016/j.socscimed.2014.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan WQ, Mannino DM, Jemal A, 2015. Socioeconomic disparities in secondhand smoke exposure among U.S. never-smoking adults: the National Health and Nutrition Examination Survey 1988–2010. Tob. Control 24 (6), 568–573. 10.1136/tobaccocontro1-2014-051660. [DOI] [PubMed] [Google Scholar]
- García JJ, Gee GC, Jones M, 2016. A critical race theory analysis of public park features in Latino immigrant neighborhoods. Du Bois Rev. Camb 13 (2), 397–411. 10.1017/S1742058X16000187. [DOI] [Google Scholar]
- Garrison VH, Pollack CE, 2018. Guest editors’ introduction: the health-housing nexus: new answers to key questions. Cityscape 20 (2), 3–6. [Google Scholar]
- Gaskin DJ, Dinwiddie GY, Chan KS, McCleary RR, 2012. Residential segregation and the availability of primary care physicians. Health Serv. Res 47 (6), 2353–2376. 10.1111/j.1475-6773.2012.01417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J, 2006. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. Am. J. Public Health Washington 96 (5). 826–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gielen AC, Shields W, McDonald E, Frattaroli S, Bishai D, Ma X, 2012. Home safety and low-income urban housing quality. Pediatrics 130 (6), 1053–1059. 10.1542/peds.2012-1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz EG, 2013. New Deal Ruins: Race, Economic Justice, and Public Housing Policy. Cornell University Press, Ithaca. [Google Scholar]
- Goetz EG, Chappie K, 2010. You gotta move: advancing the debate on the record of dispersal. Housing Policy Debate 20 (2), 209–236. 10.1080/10511481003779876. [DOI] [Google Scholar]
- Gold AE, 2016. No home for justice: how eviction perpetuates health inequity among low-income and minority tenants. Geo. J. Poverty L. Pol’y 24, 59. [Google Scholar]
- Goodman L, McCargo A, Zhu J, 2018, February 12 A closer look at the fifteen-year drop in black homeownership. Retrieved March 13, 2018, from Urban Institute website: https://www.urban.org/urban-wire/closer-look-fifteen-year-drop-black-homeownership. [Google Scholar]
- Green RD, Kouassi M, Mambo B, 2013. Housing, race, and recovery from Hurricane Katrina. Rev. Black Political Econ. 40 (2), 145–163. 10.1007/s12114-011-9116-0. [DOI] [Google Scholar]
- Grineski SE, Hernández AA, 2010. Landlords, fear, and children’s respiratory health: an untold story of environmental injustice in the central city. Local Environ. 15 (3), 199–216. https://doi.org/l0.1080/13549830903575562. [Google Scholar]
- Hall M, Crowder K, Spring A, 2015. Neighborhood foreclosures, racial/ethnic transitions, and residential segregation. Am. Sociol. Rev 80 (3), 526–549. 10.1177/0003122415581334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Cohen D, McKenzie TL, 2013. Quantifying the contribution of neighborhood parks to physical activity. Prev. Med 57 (5), 483–487. 10.1016/j.ypmed.2013.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández D, 2013. Energy insecurity: a framework for understanding energy, the built environment, and health among vulnerable populations in the context of climate change. Am. J. Public Health 103 (4), E32–E34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández D, 2016a. Affording housing at the expense of health: exploring the housing and neighborhood strategies of poor families. J. Fam. Issues 37 (7), 921–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández D, 2016b. Understanding ‘energy insecurity’ and why it matters to health. Soc. Sci. Med 167 (Suppl. C), 1–10. 10.1016/j.socscimed.2016.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirt S, 2015. The rules of residential segregation: U.S. housing taxonomies and their precedents. Plan. Perspect 30 (3), 367–395. 10.1080/02665433.2014.985602. [DOI] [Google Scholar]
- Holt EW, Theall KP, Rabito FA, 2013. Individual, housing, and neighborhood correlates of asthma among young urban children. J. Urban Health 90 (1), 116–129. 10.1007/s11524-012-9709-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homa DM, Neff LJ, King BA, Caraballo RS, Bunnell RE, Babb SD, Prevention (CDC), 2015. Vital signs: disparities in nonsmokers’ exposure to secondhand smoke—United States, 1999–2012. MMWR Morb. Mortal. Wkly. Rep 64 (4), 103–108. [PMC free article] [PubMed] [Google Scholar]
- Hori M, Schafer MJ, 2010. Social costs of displacement in Louisiana after Hurricanes Katrina and Rita. Popul. Environ 31 (1/3), 64–86. [Google Scholar]
- Hwang J, Lin J, 2016. What have we learned about the causes of recent gentrification? Cityscape 18 (3), 9–26. [Google Scholar]
- Ihrke DK, Faber CS, Koerber WK, 2011. Geographical Mobility: 2008 to 2009. U.S. Census Bureau. [Google Scholar]
- Institute of Medicine (US) Committee on Damp Indoor Spaces and Health, 2004. Damp indoor spaces and health. Retrieved from. http://www.ncbi.nlm.nih.gov/books/NBK215643/. [PubMed]
- Jacobs DE, 2011. Environmental health disparities in housing. Am. J. Public Health 101 (S1), S115–S122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaworsky D, Gadermann A, Duhoux A, Naismith TE, Norena M, To MJ, Palepu A, 2016. Residential stability reduces unmet health care needs and emergency department utilization among a cohort of homeless and vulnerably housed persons in Canada. J. Urban Health 93 (4), 666–681. 10.1007/s11524-016-0065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesdale BM, Morello-Frosch R, Cushing L, 2013. The racial/ethnic distribution of heat risk-related land cover in relation to residential segregation. Environ. Health Perspect 121 (7), 811–817. 10.1289/ehp.1205919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint Center for Housing Studies of Harvard University, 2018. The state of the nation’s housing 2018. Retrieved from, http://www.jchs.harvard.edu/sites/default/files/Harvard_JCHS_State_of_the_Nations_Housing_2018.pdf.
- Jones-Correa M, 2000. The origins and diffusion of racial restrictive covenants. Political Sci. Q 115 (4), 541–568. 10.2307/2657609. [DOI] [Google Scholar]
- Kahrl AW, 2017. Investing in distress: tax delinquency and predatory tax buying in urban America. Crit. Sociol 43 (2), 199–219. 10.1177/0896920515598565. [DOI] [Google Scholar]
- Kamel N, 2012. Social marginalisation, federal assistance and repopulation patterns in the new Orleans metropolitan area following Hurricane Katrina. Urban Stud. 49 (14), 3211–3231. 10.1177/0042098011433490. [DOI] [Google Scholar]
- Kane RJ, 2011. The ecology of unhealthy places: violence, birthweight, and the importance of territoriality in structurally disadvantaged communities. Soc. Sci. Med 73 (11), 1585–1592. 10.1016/j.socscimed.2011.08.035. [DOI] [PubMed] [Google Scholar]
- Keene DE, Geronimus AT, 2011. “Weathering” HOPE VI: the importance of evaluating the population health impact of public housing demolition and displacement. J. Urban Health 88 (3), 417–435. 10.1007/s11524-011-9582-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly CM, Schootman M, Baker EA, Barnidge EK, Lemes A, 2007. The association of sidewalk walkability and physical disorder with area-level race and poverty. J. Epidem. Community Health Lond 61 (11), 978 10.1136/jech.2006.054775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King BA, Babb SD, Tynan MA, Gerzoff RB, 2013. National and state estimates of secondhand smoke infiltration among U.S. Multiunit housing residents. Nicotine Tob. Res. 15 (7), 1316–1321. 10.1093/ntr/nts254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein Rosenthal J, Kinney PL, Metzger KB, 2014. Intra-urban vulnerability to heat-related mortality in New York City, 1997–2006. Health Place 30, 45–60. 10.1016/j.healthplace.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochhar R, Cilluffo A, 2017, November 1 How wealth inequality has changed in the U.S. since the Great Recession, by race, ethnicity and income. Retrieved March 13, 2018, from Pew Research Center website: http://www.pewresearch.org/fact-tank/2017/11/01/how-wealth-inequality-has-changed-in-the-u-s-since-the-great-recession-by-race-ethnicity-and-income/. [Google Scholar]
- Kuebler M, 2013. Closing the wealth gap: a review of racial and ethnic inequalities in homeownership. Sociol. Compass 7 (8), 670–685. 10.1111/soc4.12056. [DOI] [Google Scholar]
- Kwate NOA, 2008. Fried chicken and fresh apples: racial segregation as a fundamental cause of fast food density in black neighborhoods. Health Place 14 (1), 32–44. 10.1016/j.healthplace.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Landrigan PJ, Rauh VA, Galvez MP, 2010. Environmental justice and the health of children. Mt. Sinai J. Med. 77 (2), 178–187. 10.1002/msj.20173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC, 2009. Neighborhood environments: disparities in access to healthy foods in the U.S. Am. J. Prev. Med 36 (1), 74–81. e10 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lee JGL, Sun DL, Schleicher NM, Ribisl KM, Luke DA, Henriksen L, 2017. Inequalities in tobacco outlet density by race, ethnicity and socioeconomic status, 2012, USA: results from the ASPiRE Study. J. Epidemiol. Community Health jech-2016-208475. 10.1136/jech-2016-208475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DK, Biess J, Baum A, Pindus N, Murray B, 2017. Housing needs of American Indians and Alaska natives in urban areas: a report from the assessment of American Indian, Alaska native, and native Hawaiian housing needs. Retrieved from, https://www.huduser.gov/portal/sites/default/files/pdf/NAHSG-UrbanStudy.pdf.
- Liddell C, Guiney C, 2015. Living in a cold and damp home: frameworks for understanding impacts on mental well-being. Public Health 129 (3), 191–199. 10.1016/j.puhe.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Lim S, Chan PY, Walters S, Culp G, Huynh M, Gould LH, 2017. Impact of residential displacement on healthcare access and mental health among original residents of gentrifying neighborhoods in New York City. PLoS One 12 (12), e0l90139 10.1371/journal.pone.0190139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Njai RS, Greenlund KJ, Chapman DP, Croft JB, 2014. Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 U.S. states, 2009. Prev. Chronic Dis 11 10.5888/pcd11.130334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd EL, McCormack C, McKeever M, Syme M, 2008. The effect of improving the thermal quality of cold housing on blood pressure and general health: a research note. J. Epidemiol. Community Health 62 (9), 793–797. [DOI] [PubMed] [Google Scholar]
- Logan JR, 2013. The persistence of segregation in the 21st century metropolis. City Community 12 (2), 160–168. 10.1111/cico.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopoo LM, London AS, 2016. Household crowding during childhood and long-term education outcomes. Demography 53 (3), 699–721. 10.1007/s13524-016-0467-9. [DOI] [PubMed] [Google Scholar]
- Maantay J, 2001. Zoning, equity, and public health. Am. J. Public Health 91 (7), 1033–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackett RL, Thoreau R, 2015. Transport, social exclusion and health. J. Transp. Health 2 (4), 610–617. [Google Scholar]
- Massey DS, Denton NA, 1993. American Apartheid: Segregation and the Making of the Underclass. Harvard University Press, Cambridge, MA. [Google Scholar]
- Massey DS, Durand J, Pren KA, 2016. The precarious position of Latino immigrants in the United States: a comparative analysis of ethnosurvey data. Ann. Am. Acad. Pol. Soc. Sci 666 (1), 91–109. 10.1177/0002716216648999. [DOI] [Google Scholar]
- Mast RD, 2013. Comparing households in HUD rental assistance programs with PUMS data. Cityscape 15 (3), 237–247. [Google Scholar]
- Max W, Sung H-Y, Shi Y, 2012. Deaths from secondhand smoke exposure in the United States: economic implications. Am. J. Public Health 102 (11), 2173–2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald YJ, Jones NE, 2018. Drinking water violations and environmental justice in the United States, 2011–2015. Am. J. Public Health 108 (10), 1401–1407. 10.2105/AJPH.2018.304621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer R, Schwartz A, 2016. Housing affordability and health: evidence from New York City. Housing Policy Debate 26 (1), 80–104. 10.1080/10511482.2015.1020321. [DOI] [Google Scholar]
- Mitchell BC, Chakraborty J, 2014. Urban heat and climate justice: a landscape of thermal inequity in Pinellas County, Florida. Geogr. Rev. N. Y 104 (4), 459–480. [Google Scholar]
- Morello-Frosch R, Lopez R, 2006. The riskscape and the color line: examining the role of segregation in environmental health disparities. Environ. Res 102 (2), 181–196. 10.1016/j.envres.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD, 2011. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff. 30 (5), 879–887. [DOI] [PubMed] [Google Scholar]
- Morland K, Wing S, Roux AD, 2002. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am. J. Public Health 92 (11), 1761–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences Engineering Medicine, Negussie Y, Geller A, Weinstein JN, 2017. In: In: Baciu A, Negussie Y, Geller A, Weinstein JN (Eds.), The State of Health Disparities in the United States Retrieved from, https://www.ncbi.nlm.nih.gov/books/NBK425844/.
- National Housing Act of 1949, Pub L No 81-171. Pub. L. No. 81 S. 1070.
- Newman K, Wyly EK, 2006. The right to stay put, revisited: gentrification and resistance to displacement in New York City. Urban Stud. 43 (1), 23–57. [Google Scholar]
- Newman S, Holupka CS, 2016. Housing affordability and children’s cognitive achievement. Health Aff. 35 (11), 2092–2099. 10.1377/hlthaff.2016.0718. [DOI] [PubMed] [Google Scholar]
- Nowak AL, Giurgescu C, 2017. The built environment and birth outcomes: a systematic review. MCN Am. J. Matern./Child Nurs. 42 (1), 14–20. 10.1097/NMC.0000000000000299. [DOI] [PubMed] [Google Scholar]
- Nurmagambetov T, Kuwahara R, Garbe P, 2018. The economic burden of asthma in the United States, 2008–2013. Ann. Am. Thoracic Soc. 15 (3), 348–356. 10.1513/AnnalsATS.201703-259OC. [DOI] [PubMed] [Google Scholar]
- Office of the Surgeon General (US), 2009. The Surgeon General’s call to action to promote healthy homes. Retrieved from. http://www.ncbi.nlm.nih.gov/books/NBK44192/. [PubMed]
- Okah FA, Oshodi A, Liu Y, Cai J, 2014. Community violence and pregnancy health behaviors and outcomes. South. Med. J 107 (8), 513–517. 10.14423/SMJ.0000000000000143. [DOI] [PubMed] [Google Scholar]
- Olmedo O, Goldstein IF, Acosta L, Divjan A, Rundle AG, Chew GL, Perzanowski MS, 2011. Neighborhood differences in exposure and sensitization to cockroach, mouse, dust mite, cat, and dog allergens in New York City. J. Allergy Clin. Immunol.St. Louis 128 (2), 284–292. e7. 10.1016/j.jaci.2011.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormandy D, Ezra tty V, 2012. Health and thermal comfort: from WHO guidance to housing strategies. Energy Policy 49, 116–121. 10.1016/j.enpol.2011.09.003. [DOI] [Google Scholar]
- Overweight and Obesity Rates for Adults by Race/Ethnicity, 2017, October 16 Retrieved March 14, 2018, from The Henry J. Kaiser Family Foundation website: https://www.kff.org/other/state-indicator/adult-overweightobesity-rate-by-re/. [Google Scholar]
- Pattillo M, 2013. Housing: commodity versus right. Annu. Rev. Sociol. 39 (1), 509–531. 10.1146/annurev-soc-071312-145611. [DOI] [Google Scholar]
- Pendall R, 2000. Local land use regulation and the chain of exclusion. J. Am. Plan. Assoc. 66 (2), 125–142. 10.1080/01944360008976094. [DOI] [Google Scholar]
- Perera F, Vishnevetsky J, Herbstman JB, Calafat AM, Xiong W, Rauh V, Wang S, 2012. Prenatal bisphenol A exposure and child behavior in an inner-city cohort. Environ. Health Perspect 120 (8), 1190–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters JL, Levy JI, Rogers CA, Burge HA, Spengler JD, 2007. Determinants of allergen concentrations in apartments of asthmatic children living in public housing. J. Urban Health 84 (2), 185–197. 10.1007/s11524-006-9146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierse N, Arnold R, Keall M, Howden-Chapman P, Crane J, Cunningham M, Group HS, 2013. Modelling the effects of low indoor temperatures on the lung function of children with asthma. J. Epidemiol. Community Health 67 (11), 918–925. [DOI] [PubMed] [Google Scholar]
- Pilkauskas NV, Garfinkel I, McLanahan SS, 2014. The prevalence and economic value of doubling up. Demography 51 (5), 1667–1676. 10.1007/s13524-014-0327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pindus N, Kingsley GT, Biess J, Levy D, Simington J, Hayes C, 2017. Housing needs of American Indians and Alaska natives in tribal areas: a report from the assessment of American Indian, Alaska Native, and Native Hawaiian housing needs. Retrieved from U.S. Department of Housing and Urban Development - Office of Policy Development and Research website: https://www.huduser.gov/portal/sites/default/files/pdf/HNAIHousingNeeds.pdf. [Google Scholar]
- Pollack CE, Griffin BA, Lynch J, 2010. Housing affordability and health among homeowners and renters. Am. J. Prev. Med 39 (6), 515–521. 10.1016/j.amepre.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Popkin SJ, Gwiasda VE, Rosenbaum DP, Amendolia JM, Johnson WA, Olson LM, 1999. Combating crime in public housing: a qualitative and quantitative longitudinal analysis of the Chicago Housing Authority’s Anti-Drug Initiative. Justice Q. JQ 16 (3), 519–557. 10.1080/07418829900094251. [DOI] [Google Scholar]
- Popkin SJ, Levy D, Harris LE, Comey J, Cunningham MK, Buron L, 2002. HOPE VI Panel Study: Baseline Report. Urban Institute, pp. 283. [Google Scholar]
- Rauh VA, Chew GR, Garfinkel RS, 2002. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ. Health Perspect 110 (Suppl. 2), 323–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauh VA, Landrigan PJ, Claudio L, 2008. Housing and health: intersection of poverty and environmental exposures. Ann. N. Y. Acad. Sci 1136 (1), 276–288. 10.1196/annals.1425.032. [DOI] [PubMed] [Google Scholar]
- Reardon SF, Bischoff K, 2011. Income inequality and income segregation. Am. J. Sociol 116 (4), 1092–1153. 10.1086/657114. [DOI] [PubMed] [Google Scholar]
- Reid CE, O’Neill MS, Gronlund CJ, Brines SJ, Brown DG, Diez-Roux AV, Schwartz J, 2009. Mapping community determinants of heat vulnerability. Environ. Health Perspect 117 (11), 1730–1736. 10.1289/ehp.0900683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid KW, Vittinghoff E, Kushel MB, 2008. Association between the level of housing instability, economic standing and health care access: a meta-regression. J. Health Care Poor Underserved Baltim 19 (4), 1212–1228. [DOI] [PubMed] [Google Scholar]
- Rigolon A, 2016. A complex landscape of inequity in access to urban parks: a literature review. Landsc. Urban Plan 153, 160–169. 10.1016/j.landurbplan.2016.05.017. [DOI] [Google Scholar]
- Romley JA, Cohen D, Ringel J, Sturm R, 2007. Alcohol and environmental justice: the density of liquor stores and bars in urban neighborhoods in the United States. J. Stud. Alcohol Drugs 68 (1), 48–55. 10.15288/jsad.2007.68.48. [DOI] [PubMed] [Google Scholar]
- Rosenberg SL, Miller GE, Brehm JM, Celedón JC, 2014. Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J. Allergy Clin. Immunol.St. Louis 134 (5), 1009–1015. 10.1016/j.jaci.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein R, 2017. The Color of Law: A Forgotten History of How Our Government Segregated America. Liveright Publishing Corporation, New York. [Google Scholar]
- Rothwell J, Massey DS, 2009. The effect of density zoning on racial segregation in U.S. Urban areas. Urban Aff. Rev 44 (6), 779–806. 10.1177/1078087409334163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothwell J, Massey DS, 2010. Density zoning and class segregation in U.S. metropolitan areas. Soc. Sci. Q 91 (5), 1123–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Routhier G, 2018. State of the homeless 2018. Retrieved from Coalition For The Homeless website: http://www.coalitionforthehomeless.org/state-of-the-homeless-2018/. [Google Scholar]
- Runyan CW, Casteel C, Perkis D, Black C, Marshall SW, Johnson RM, Viswanathan S, 2005. Unintentional injuries in the home in the United States: Part I: Mortality. Am. J. Prev. Med 28 (1), 73–79. 10.1016/j.amepre.2004.09.010. [DOI] [PubMed] [Google Scholar]
- Sackett C, 2016. Neighborhoods and violent crime Evidence matters. Retrieved from. https://www.huduser.gov/portal/periodicals/em/summerl6/highlight2.html.
- Saegert S, Fields D, Libman K, 2011. Mortgage foreclosure and health disparities: serial displacement as asset extraction in African American populations. J. Urban Health 88 (3), 390–402. 10.1007/s11524-011-9584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Saelens BE, Frank LD, Conway TL, Slymen DJ, Cain KL, Kerr J, 2009. Neighborhood built environment and income: examining multiple health outcomes. Soc. Sci. Med 68 (7), 1285–1293. 10.1016/j.socscimed.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Winter AS, 2016. The racial ecology of lead poisoning: toxic inequality in Chicago neighborhoods, 1995-2013. Du. Bois Rev.: Soc. Sci. Res. Race 13 (2), 261–283. 10.1017/S1742058X16000151. [DOI] [Google Scholar]
- Sandel M, Sheward R, deCuba SE, Coleman SM, Frank DA, Chilton M, Cutts D, 2018. Unstable housing and caregiver and child health in renter families. Pediatrics, e20172199 10.1542/peds.2017-2199. [DOI] [PubMed] [Google Scholar]
- Satter B, 2009. Family Properties: Race, Real Estate, and the Exploitation of Black Urban America. Metropolitan Books, New York. [Google Scholar]
- Schachterle SE, Bishai D, Shields W, Stepnitz R, Gielen AC, 2012. Proximity to vacant buildings is associated with increased fire risk in Baltimore, Maryland, homes. Injury Prev. Lond 18 (2), 98 10.1136/injuryprev-2011-040022. [DOI] [PubMed] [Google Scholar]
- Shai D, 2006. Income, housing, and fire injuries: a census tract analysis. Public Health Rep. 121 (2), 149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankardass K, McConnell R, Jerrett M, Milam J, Richardson J, Berhane K, 2009. Parental stress increases the effect of traffic-related air pollution on childhood asthma incidence. Proc. Natl. Acad. Sci 106 (30), 12406–12411. 10.1073/pnas.0812910106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey P, 2012. Residential mobility and the reproduction of unequal neighborhoods. Cityscape 14 (3), 9–31. [Google Scholar]
- Sicotte D, Swanson S, 2007. Whose risk in Philadelphia? Proximity to unequally ha-zardous industrial facilities. Soc. Sci. Q 88 (2), 515–534. [Google Scholar]
- Slater LJ, Villarini G, 2016. Recent trends in U.S. flood risk. Geophys. Res. Lett 43 (24) 12,428–12,436. https://doi.org/l0.1002/2016GL071199. [Google Scholar]
- Solari CD, Mare RD, 2012. Housing crowding effects on children’s wellbeing. Soc. Sci. Res 41 (2), 464–476. 10.1016/j.ssresearch.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturm R, Cohen D, 2014. Proximity to urban parks and mental health. J. Ment. Health Policy Econ 17 (1), 19–24. [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Duarte CS, Sandel MT, 2011. Housing quality, housing instability, and maternal mental health. J. Urban Health 88 (6), 1105–1116. 10.1007/s11524-011-9587-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor K-Y, 2012. Back story to the neoliberal moment: race taxes and the political economy of Black urban housing in the 1960s. Souls 14 (3–4), 185–206. 10.1080/10999949.2012.764836. [DOI] [Google Scholar]
- Taylor L, 2018. Housing and Health: an Overview of the Literature. Health Affairs Health Policy Brief, 10.1377/hpb20180313.396577. [DOI] [Google Scholar]
- Thomson H, Thomas S, Sellstrom E, Petticrew M, 2013. Housing improvements for health and associated socio-economic outcomes. Cochrane Database Syst. Rev 10.1002/14651858.CD008657.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tillyer MS, Walter RJ, 2018. Low-Income Housing and Crime: the Influence of Housing Development and Neighborhood Characteristics. Crime & Delinquency 0011128718794185 10.1177/0011128718794185. [DOI] [Google Scholar]
- Tsai AC, 2015. Home foreclosure, health, and mental health: a systematic review of individual, aggregate, and contextual associations. PLoS One 10 (4), e0123182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner MA, Santos R, Levy DK, Wissoker DA, 2013. Housing Discrimination against Racial and Ethnic Minorities 2012. Office of Policy Development and Research. U.S. Department of Housing and Urban Development. [Google Scholar]
- United Nations General Assembly, 1948. Universal Declaration of Human Rights. Retrieved from, https://www.un.org/en/universal-declaration-human-rights/.
- United States Department of Labor, Bureau of Labor Statistics, 2018, March 27 Unemployment Rates and Earnings by Educational Attainment. Retrieved May 14, 2018, from U.S. Bureau of Labor Statistics website: https://www.bls.gov/emp/ep_chart_001.htm. [Google Scholar]
- U.S. Census Bureau, 2002. Racial and Ethnic Residential Segregation in the United States: 1980-2000. Retrieved from, https://www.census.gov/hhes/www/housing/resseg/pdf/app_b.pdf.
- U.S. Census Bureau, 2013. 2013 national - value, purchase price, and source of down payment - owner-occupied units. Retrieved from . https://www.census.gov/programs-surveys/ahs.html.
- U.S. Census Bureau, 2017. Housing Problems - All Occupied Units (National). Retrieved from. https://www.census.gov/programs-surveys/ahs.html.
- U.S. Department of Housing and Urban Development HUD’s healthy homes program. Retrieved September 23, 2018, from, https://www.hud.gov/program_offices/healthy_homes/hhi.
- Vijayaraghavan M, Kushel MB, Vittinghoff E, Kertesz S, Jacobs D, Lewis CE, Bibbins-Domingo K, 2013. Housing instability and incident hypertension in the CARDIA cohort. J. Urban Health 90 (3), 427–441. 10.1007/s11524-012-9729-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson KB, 2016. Disparities in Adolescents’ Residence in Neighborhoods Supportive of Physical activity—United States, 2011–2012. MMWR Morbidity and Mortality Weekly Report, 65. [DOI] [PubMed] [Google Scholar]
- White-Newsome JL, Sanchez BN, Jolliet O, Zhang Z, Parker EA, Timothy Dvonch J, O’Neill MS, 2012. Climate change and health: indoor heat exposure in vulnerable populations. Environ. Res 112, 20–27. 10.1016/j.envres.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittemore AH, 2017. Racial and class bias in zoning: rezonings involving heavy commercial and industrial land use in Durham (NC), 1945–2014. J. Am. Plan. Assoc 83 (3), 235–248. 10.1080/01944363.2017.1320949. [DOI] [Google Scholar]
- Williams DR, Collins C, 2001. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 116 (5), 404–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods LL, Shaw-Ridley M, Woods CA, 2014. Can health equity coexist with housing inequalities? A contemporary issue in historical context. Health Promot. Pract 15 (4), 476–482. [DOI] [PubMed] [Google Scholar]
- World Health organization, 2018. WHO Housing and health guidelines. Retrieved from. https://www.who.int/sustainable-development/publications/housing-health-guidelines/en/.
- Wright AW, Austin M, Booth C, Kliewer W, 2017. Systematic review: exposure to community violence and physical health outcomes in youth. J. Pediatr. Psychol 42 (4), 364–378. 10.1093/jpepsy/jsw088. [DOI] [PubMed] [Google Scholar]
- Wright RJ, 2006. Health effects of socially toxic neighborhoods: the violence and urban asthma paradigm. Clin. Chest Med 27 (3), 413 10.1016/j.ccm.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Ziol-Guest KM, McKenna CC, 2014. Early childhood housing instability and school readiness. Child Dev. 85 (1), 103–113. 10.1111/cdev.12105. [DOI] [PubMed] [Google Scholar]
- Zota AR, Shenassa ED, Morello-Frosch R, 2013. Allostatic load amplifes the effect of blood lead levels on elevated blood pressure among middle-aged U.S. adults: a cross-sectional study. Environ. Health 12, 64 10.1186/1476-069X-12-64. [DOI] [PMC free article] [PubMed] [Google Scholar]


