Abstract
We regularly face primary challenges in deciding what to eat to maintain young and healthy skin, defining a healthy diet and the role of diet in aging. The topic that currently attracts maximum attention is ways to maintain healthy skin and delay skin aging. Skin is the primary barrier that protects the body from external aggressions. Skin aging is a complex biological process, categorized as chronological aging and photo-aging, and is affected by internal factors and external factors. With the rapid breakthrough of medicine in prolonging human life and the rapid deterioration of environmental conditions, it has become urgent to find safe and effective methods to treat skin aging. For diet, as the main way for the body to obtain energy and nutrients, people have gradually realized its importance to the skin. Therefore, in this review, we discuss the skin structure, aging manifestations, and possible mechanisms, summarize the research progress, challenges, possible directions of diet management, and effects of foodborne antioxidants on skin aging from the perspective of food and nutrition.
Keywords: diet, skin aging, nutritional level, eating habits, foodborne antioxidants, anti-aging
1. Introduction
Skin is the organ with the largest contact area between the human body and the external environment and is a barrier that separates the human body from the environment. It not only protects the body from external environmental damage and avoids water loss from the body, but also has a certain cosmetic effect [1]. The aging of organs occurs throughout our life. As the largest organ of the human body, the skin shows obvious signs of aging due to age, ultraviolet radiations (UVR) exposure, and chemical pollution. With the development of science and technology and improvement in human living standards, people pay more attention to skin aging and try to have a better understanding of it. Many people, especially women, spend a significant portion of their daily expenses on cosmetics and medicines for the treatment and prevention of skin aging. This huge demand continues to drive research into the prevention and treatment of skin aging [2].
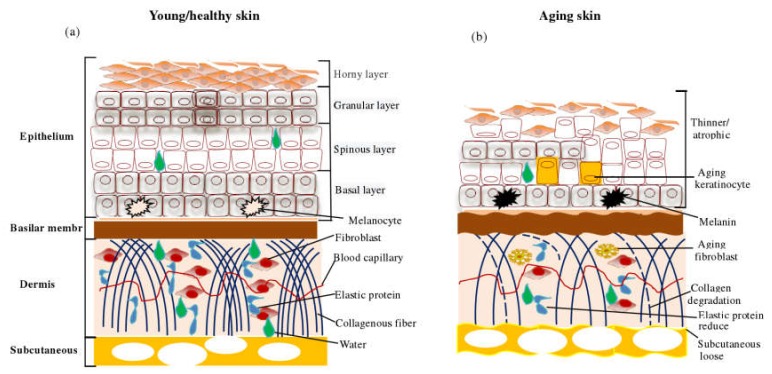
Animal skin is composed of three layers, including epidermis, dermis, and subcutaneous tissue [3] (Figure 1). During development, skin epidermal cells rapidly differentiate into four layers of stratum corneum, granular layer, spinous layer, and the basal layer. Stem cells (SC) and transient amplification cells (TA) located at the base layer promote the regeneration of human skin epidermis. Epidermal regeneration and SC behavior are regulated by external signaling pathways such as the Wnt signaling pathway [4,5]. Dermis refers to the part above the subcutaneous fat below the epidermis, which is the connective tissue composed of fibroblasts, responsible for the synthesis and secretion of collagen and other matrix proteins (such as fibronectin, elastin, and glycans) to the extracellular environment, giving the skin elasticity, strength, and ability to resist external interference [6,7]. Fibroblasts are also involved in skin aging [8], carcinogenesis [9], wound healing [10], fibrosis [11], and other pathological processes. Subcutaneous layer refers to the fat layer immediately below the dermis layer, which surrounds the hair follicles and plays a major role in connecting the skin with muscles and bones, storing energy, secreting hormones, and keeping warm. Subcutaneous adipose tissue is also involved in regulating the speed of hair regeneration, balancing the internal environment of the skin, and promoting skin repair after damage and infection [12,13].
Figure 1.
(a) Schematic diagram of skin structure, (b) Schematic diagram of skin structure after aging. This picture is a comparison of the changes between young skin and aging skin.
Aging refers to the body’s ability to adapt to the environment’s physiology and psychology, which progressively decreases and gradually leads to death. It is mainly characterized by the accumulation of macromolecular damage, impaired tissue renewal, gradual loss of physiological function integrity, and increased risk of death [14]. Aging is caused by a combination of internal factors (such as hormone levels, genotypes, endocrine metabolism, etc.), and external factors (such as ultraviolet radiation, nutritional levels, chemical pollution, etc.). Skin aging can be divided into chronological aging and photo-aging (or internal aging and external aging). As the name suggests, the chronological aging of the skin occurs throughout the body, and photo-aging occurs on the body’s light-exposed sites [15,16]. Chronological aging caused by internal factors occurs naturally and is not easy to change, but it is possible to delay photo-aging by altering external factors [17]. Reasonable diet and balanced nutrition are important measures to delay aging and prolong life. Therefore, in this review, we briefly introduce the composition of the skin, internal and external changes that occur during skin aging, and the molecular mechanism, focus on the perspective of food nutrition, and review the recent progress in research on diet management, nutrition regulation, and foodborne antioxidants in inducing and delaying skin aging. We hope that our views will enrich the reader’s understanding of diet to improve skin aging and also provide a basis for subsequent research.
2. Changes and Molecular Mechanisms in Skin Aging
2.1. Apparent Changes in Skin Aging
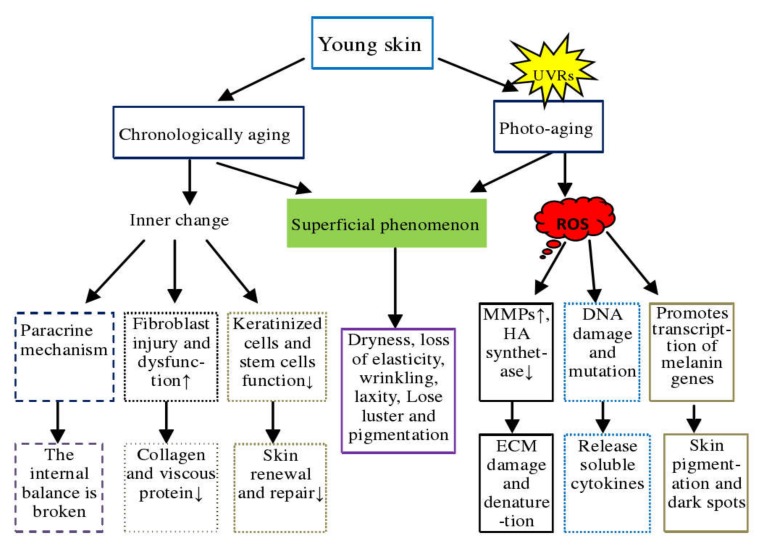
Aging is characterized by the accumulation of macromolecular damage within cells, impaired ability of stem cells to promote tissue regeneration, and restore the loss of physiological integrity [7]. Chronological aging and photo-aging are two processes of skin aging that although related, have different clinical manifestations and pathogenesis (Figure 2). Chronological aging usually appears after a certain age and is affected by factors such as ethnicity, individual, and skin site. It is mainly characterized by dry skin, dullness, lack of elasticity, and fine wrinkles [18]. Histological features include epidermal atrophy, reduction in the number of dermal fibroblasts and collagen fibers, slackening, thinness, and even function disorganized. The primary causes are: first, the SC dysfunction in keratinocytes, decreased regenerative ability of stem cells in the basal layer of the epidermis leading to a decline in skin renewal and repair ability, ultimately causing aging [19], and second, due to the accumulation of damage and aging skin dysfunction, fibroblasts lose the ability to reshape the extracellular matrix or have a reduced ability to synthesize and secrete collagen or viscous proteins. Third, aging fibroblasts alter intracellular homeostasis through certain paracrine mechanisms [20,21].
Figure 2.
Comparison of chronological aging and photo-aging of the skin. In the figure, "↑" means "rise or increase"; "↓" means "fall or decrease"; DNA= deoxyribonucleic acid; ECM= extracellular matrix; UVRs = ultraviolet radiations; ROS= reactive oxygen species; MMPs = Matrix metalloproteinases; HA= Hyaluronic acid.
Photo-aging is caused by long-term exposure to ultraviolet radiation, mainly manifested as skin wrinkles, relaxation, roughness, yellowish or grayish-yellow, capillary expansion, and pigmented spot formation, etc. [16,19]. The photo-aging site is affected by the wavelength of ultraviolet light, which can be divided into A, B, C categories depending on the length of the wavelength. UV-A (320–400 nm) has low energy but strong penetrating power, which mainly affects the dermis of the skin. It accelerates the hydrolysis of skin collagen by promoting the production of matrix metalloproteinases (MMPs), leading to tissue destruction and progressive degeneration of dermal extracellular matrix [22,23,24]. UV-A also inhibits the synthesis of hyaluronic acid (HA) by down-regulating the synthesis of hyaluronic acid synthase, thereby changing the composition of skin proteoglycans [20]. UV-B acts on keratinocytes in the skin epithelial layer, potentially induces DNA damage and mutation in keratinocytes, stimulates the release of soluble cytokines from keratinocytes, and causes skin cells to show symptoms such as aging, inflammation, apoptosis, and carcinogenesis [25,26]. However, keratinocytes have a strong antioxidant capacity in response to UV-B exposure, are more resistant than fibroblasts to the lethal effects of oxidants, and are more sensitive to reactive oxygen species (ROS)-induced apoptosis [27]. Further, aging skin fibroblasts cause pigmentation and dark spots by promoting the transcription of the melanin gene [28].
2.2. Molecular Mechanism of Skin Aging
Researchers have used many models in recent years to explain the molecular mechanism of skin aging and the mechanism of its alleviation. These models include cell aging, oxidative stress, high-frequency chromosomal abnormalities, single-gene mutations, and chronic inflammation [29]. We summarize here the progress in recent years on the research on the molecular mechanism of skin aging, as fellows.
-
a.
Oxidative stress. Oxidative stress plays an important role in skin aging and skin damage processes, and its main feature is increased intracellular ROS. The skin’s oxidative metabolism and UV exposure lead to the production of ROS. The accumulation of ROS causes DNA damage, induces skin inflammatory response, reduces antioxidant enzymes, activates nuclear factor kappa B (NF-kB) and activator protein1 (AP–1) to inhibit collagen production, and increases matrix metalloproteinases to decompose collagen and binding proteins in the dermis, which eventually leads to skin aging [30,31,32,33].
-
b.
DNA damage and gene mutation. Earlier studies reviewed the mechanisms of UV-induced DNA damage and classified them into direct damage and indirect damage. Direct damage occurs when DNA absorbs the UV-B photon, leading to rearrangement in the nucleotide sequence, resulting in DNA strand deletion or mutation. During indirect damage, DNA molecules absorb UV-A and promote electron and energy transfer to oxygen molecules to form free radicals’ singlet oxygen ions, causing DNA damage [34,35]. DNA damage can be repaired by photolytic enzymes, while UV-induced skin DNA damage can be prevented by applying sunscreen [36,37].
-
c.
Shortening of the telomere. Telomeres are a small piece of DNA-protein complex at the end tips of eukaryotic linear chromosomes, which are important components in maintaining the chromosomal integrity and controlling the cell cycle. A telomere is shortened with cell division and is associated closely with cell division and senescence [38,39]. Telomerase is an enzyme responsible for telomere elongation, and its synthesis is essential for telomere maintenance and long-term survival of the organism. Epithelial stem cells with short telomeres have a poor proliferative capacity, which can be corrected by introducing telomerase. The reactive oxygen generated by UV radiation induces telomere mutation, cell death, or senescence. Nevertheless, some studies opine that the relationship between telomeres and aging may be speculation and, therefore, this relationship needs to be demonstrated [38,39,40,41,42].
-
d.
The role of microRNA. miRNAs are a type of conserved non-coding RNA. Chronic UV-B alters the expression of mir–34 family proteins in the skin. MiR–34 in human dermal fibroblast (HDFs) cells regulates cell function and expression of MMP–1, α1 type1 collagen (COL1A1), and elastin. miRNA 378b inhibits mRNA expression of COL1A1 by interfering with Sirtuin 6 (SIRT6) in HDFs, miRNA 217 regulates the senescence of human skin fibroblast by directly targeting DNA methyltransferase 1, and miR–23a–3p controls cellular senescence by targeting enzymes to control hyaluronic acid synthesis. These studies thus show that microRNAs regulate the skin aging process [43,44,45,46,47].
-
e.
Accumulation of advanced glycation end products (AGEs). AGEs are the products of excess sugar and protein binding, usually derived from body synthesis and food intake. The nonenzymatic glycosylation aging theory has been widely recognized by many scholars. As the final product of nonenzymatic glycosylation reaction, AGEs accumulate in photo-aging skin, affect protein function in the dermis, and promote skin aging [48,49,50].
-
f.
Aging due to inflammation. Continuous UV radiation exposure induces oxidative stress in epidermal cells, causing cell damage, fat oxidation, and finally leads to cell inflammation. When the degree of inflammation exceeds the ability of macrophages to clear up, macrophages also begin secreting pro-inflammatory factors and ROS to accelerate dermal inflammation and injury [51,52]. With the continuous advancement in dermatology in the past two decades, methods such as stem cell transplantation, hormone therapy, telomerase modification, and use of antioxidants and retinoic acid have been promoted to address skin aging. However, some of these treatment methods have certain disadvantages and serious side effects. For example, hormone therapy increases the risk of breast cancer, retinoic acid may cause osteoporosis, and telomerase modification increases the risk of skin cancer. Therefore, improving skin condition through diet management is being increasingly accepted by people.
3. Diet Management and Skin Aging
Food is the foundation of our lives, and diet is the main way for the body to obtain the required substances for growth and maintenance. Human beings group themselves into different ethnicity, religions, nationalities, and catering cultures. More than 2000 years ago, the Chinese medical book "Yellow Emperors Internal Classic. Su Wen" contained a balanced diet principle of "five grains for nutrition, five fruits for help, five animals for benefit, and five vegetables for filling", and the folk also includes "what to eat and what to add". Modern science has proven that an imbalance in nutrition and poor eating habits are important causes of skin aging. The effect of nutrients and dietary habits on skin aging is mentioned in Table 1.
Table 1.
Summary of key effects of nutrients and diet in skin aging.
| Nutrients/Diet | Relationship with the Skin | References |
|---|---|---|
| Water | Maintain skin internal balance and tissue function (e.g., aging and inflammation) | [56,57] |
| Proteins | Constitution and repair of skin tissues (involved in protein synthesis and metabolism), mediation of skin physiological functions and supply of energy. | [74] |
| Trace Elements | ||
| Copper | Involved in extracellular matrix, synthesis and stabilization of skin proteins, and angiogenesis. | [63] |
| Zinc | Participates in the proliferation and differentiation of epidermal keratinocytes. | [60,61] |
| Iron | Closely related to the activity of antioxidant enzymes in skin cells. | [64,65] |
| Selenium | 1. Essential for the development and function of skin keratinocytes.2. Related to skin antioxidant enzyme activity. | [67] |
| Vitamins | ||
| VA | Commonly used anti-aging ingredients prevent skin aging by regulating the expression of genes and matrix metalloproteinases. | [97,98] |
| VB | Associated with skin inflammation and pigmentation. | [99] |
| VC | Involved in skin collagen synthesis and elimination of intracellular reactive oxygen species. | [100] |
| VD | Reduces skin DNA damage, inflammation, and photocarcinogenesis. | [101] |
| VE | Prevent skin aging by inhibiting lipid peroxidation. | [102,103] |
| Diet | ||
| Fat | High fat is associated with skin inflammation, essential fatty acids are involved in skin lipid synthesis and metabolism. | [92,104] |
| Tobacco | Change skin cuticle thickness, accelerate skin pigmentation and skin necrosis. | [76,77,78,79] |
| Alcohol | Promote the proliferation of keratinocytes, change the skin permeability, destroy the barrier function of the skin, affect the skin lipid composition. | [81,82] |
| Sugar and baked goods | Associated with skin thickness, AGEs, autophagy, and inflammation. | [93,94,95,96] |
3.1. Nutrition Level
Nutrition is closely associated with skin health and is required for all biological processes of skin from youth to aging or disease. Nutrition levels and eating habits can repair damaged skin and can also cause damage to the skin. In recent years, a number of people have closely linked health-nutrition-eating habits and skin health, besides, clinical research and epidemiology have successfully combined nutrition with tissues and organ health and have confirmed that nutritional levels and eating habits have a certain degree of impact on skin health and aging.
Water is a vital constituent of the body and facilitates maintenance of balance and tissue function in the body. Water in the body and cells mainly serves the role of nutrient, solvent, transportation carrier, maintains body volume, and regulates body temperature [53,54,55]. Lack of water in the body can cause tissue dehydration and functional disorders (such as aging and inflammation). Skin is no exception, and the appearance of the skin on lips and limb is a direct reflection of the body’s moisture status. So how much water every day is good for the skin? Studies show that it is better to have more water and drinking more than 2 L of water per day significantly affects skin physiology and promotes superficial and deep hydration of the skin. However, the effects of water on the skin may be different from that of the water intake, and these effects are obvious in people who drink less water [56,57].
Trace elements include iron, iodine, zinc, and copper, etc., and refer to elements whose content in the human body is less than 0.01–0.005% of the body mass. Despite being less abundant in the body, trace elements have strong physiological and biochemical effects [58]. Trace elements are closely related to skin immunity and inflammation, and the homeostasis of copper and zinc ions in psoriasis patients may be a potential target for treating psoriasis [59]. Zinc content in the skin ranks third among all tissues and is an essential element for the proliferation and differentiation of skin epidermal keratinocytes [60,61]. Bauer et al. [62] demonstrated that enhanced dietary zinc-rich amino acid complexes may affect the proliferation of goat horn and interphalangeal skin keratinocytes. However, the role of trace zinc or amino acid has not been further clarified. In the skin, copper is involved in the extracellular matrix formation, synthesis and stabilization of skin proteins, and angiogenesis. Clinical studies have shown that copper aids in improving skin elasticity, reducing facial fine lines and wrinkles, and promoting wound healing [63]. Iron is a catalyst for bio-oxidation. Studies have shown that ultraviolet radiation and iron content in women’s post-menopausal skin cells increase rapidly, reduce the skin’s antioxidant capacity, and lead to aging [64,65]. The lack of selenium in the diet weakens the UV-B-induced antioxidative ability of mice skin, making the skin more sensitive to oxidative stress due to ultraviolet radiation [66]. Se-enriched proteins are also essential in keratinocyte development and function [67]. There are some studies on the lack of other trace elements and their effects on the skin, as well as in vitro experiments of trace elements, which are not described here.
Vitamin deficiency affects skin health. The lack of vitamins in the body can cause skin disorders. For example, lack of vitamin C causes the symptoms of scurvy such as fragile skin and impaired wound healing. Vitamins, as skin antioxidant defense ingredients, are mostly taken from food, so the content of vitamins in the diet is closely related to skin antioxidant capacity and physiological functions [68,69,70].
Proteins form an important part of body tissues and organs. Their primary physiological functions are to construct and repair tissues, mediate physiological functions, and supply energy. All tissue cells in the body are constantly renewed, and only adequate protein intake can maintain normal tissue renewal and repair. Skin is no exception, and the skin renewal cycle is generally considered to be 28 days. Protein deficiency or excessive intake can cause metabolic disorders and affect physical health [71]. Excessive intake of plant protein increases kidney load, and excess animal protein intake increases the risk of osteoporosis [72,73]. Conversely, protein deficiency causes a series of diseases such as reduced resistance, slow growth, weight loss, apathy, irritability, anemia, thinness, and edema. Countries around the world recommend standard protein intakes based on age, sex, work, and physiological period. Studies have shown that ingesting sufficient protein can help in healing pressure ulcers in rats, while both excess and inadequate protein intake are detrimental to ulcer healing. Dietary protein supplementation can also enhance cellular protein synthesis and metabolism [74]. The effects of dietary protein and its hydrolyzed peptides improving skin aging have been described in detail in Section 4.1 of this paper. There may be some other nutrients that have not been discussed in this article but affect the skin aging and needs to be continuously supplemented.
3.2. Eating Habits
Dietary habits refer to the preference for food or drink, are an important part of the dietary culture and influenced by regional, historical, cultural, product, and other factors. Although the incidence of vitamin, trace elements, and protein deficiencies in developed western countries are very low, imbalanced or incomplete diet can also lead to diseases and aging, thereby affecting skin health. Data from epidemiological and experimental studies suggest an important role of diet and dietary patterns in the pathogenesis of many age-related diseases [75].
Tobacco use is one of the major public health hazards in the world. Millions of people worldwide die each year due to smoking, so tobacco is also called a "poisonous weed". Smoking can change skin cuticle thickness and accelerates skin pigmentation. The thickness of the stratum corneum correlates positively with pigmentation and negatively with years of smoking, and this skin pigmentation is more obvious in the upper lip than in the gums [76,77]. Some clinical observations and investigations have also shown a certain correlation between smoking, external aging, and facial skin aging [78,79]. Further, after cosmetic surgery, smoking can cause complications such as postoperative infections, delayed wound healing, and skin necrosis [80]. While we cannot conclude completely on the harmful effect of alcohol on the body, alcohol and acetone produced by alcohol metabolism can promote the proliferation of skin keratinocytes, thereby enhancing skin permeability and damaging its barrier function. Alcohol also affects the metabolism of triglycerides and cholesterol and affects the lipid composition of the skin [81,82]. Studies by Goodman et al. [83] revealed that aging causes changes in facial skin and volume and is closely related to smoking and heavy drinking, and the degree of facial aging increases with the amount and time of exposure to tobacco and alcohol. On the contrary, quitting smoking and alcohol can delay the aging of facial skin. Dysfunction of alcohol metabolism in the aldehyde dehydrogenase 2 (ALDH2) gene knockout mouse or human allele also confirmed that alcohol can cause increased skin pigmentation, although the downstream mechanism of action is unclear [84]. While there are some studies on the relationship between alcohol intake and skin diseases, the relationship between alcohol intake and disease needs to be accurately determined based on real situations [85].
A high-fat diet is closely related to various diseases such as obesity, diabetes, fatty liver, and skin aging. Raman spectroscopy studies have shown that dietary fat intake is closely related to the body’s adipose tissue and the lipid composition of the skin [86]. High-fat diets delay healing of the skin by promoting skin oxidative stress and inflammatory responses, reducing protein synthesis, and may also cause morphological changes in skin and damage to matrix remodeling [87,88]. Psoriasis is a systemic chronic skin inflammatory disease that affects 2–5% of the population in western countries. The free fatty acids content in serum is an important parameter to reflect the severity of obesity-related diseases. A high-fat diet led to an increase in free fatty acid content in mice, which is an important factor that aggravates skin inflammatory psoriasis. Moreover, a high-fat diet can promote skin inflammation and cancer by enhancing the expression of inflammatory factors and tumor necrosis factor in the skin by UV-B [89,90,91]. Studies by Zhang and others [92] showed that after high-fat diet, the epidermal fatty acid-binding protein (E-FABP) of mice was significantly upregulated in the skin, which promoted the formation of lipid droplets and the activation of NLRP3 inflammator, and greatly increased the incidence of skin lesions in mice. In general, the effect of a high-fat diet is mainly to cause aging of the skin by causing skin oxidative stress to produce inflammatory damage.
Some studies have also shown a close association between sugar and some food processing methods (such as grilling, frying, baking, etc.) with skin aging, and their mechanisms are related to skin advanced glycation end products. A high-sugar diet, ultraviolet irradiation, and eating barbecued fried foods, lead to the accumulation of AGEs and acceleration of skin aging. However, strict control of blood sugar for four months can reduce the production of glycosylated collagen by 25%, and low-sugar food prepared by boiling can also reduce the production of AGEs [93,94,95]. When the mice were fed with carbohydrate-controlled diets for 50 weeks, the epidermis and dermis were significantly thinned, autophagy was inhibited, and inflammation was exacerbated. Mechanistically, long-term intake of carbohydrates in mice promotes skin aging by activating the mammalian target of rapamycin (mTOR) [96]. Further, high-salt, spicy, and extremely vegetarian diets are also considered to be detrimental to skin health. Therefore, scientific, reasonable, healthy, and diverse eating habits and eating some antioxidant-rich foods are essential to maintaining skin health.
4. Foodborne Antioxidants and Skin Aging
According to free radical theory, lipid peroxidation, DNA damage, and inflammation are the primary causes of skin aging, disease, and dysfunction. This led to a medical revolution that emphasized antioxidants and free radical scavengers for the prevention and treatment of skin aging [105,106]. Oxygen-free radicals are ubiquitous in the process of cell metabolism and can interact with DNA, proteins, and polyunsaturated fatty acids in the body, causing breaks in the DNA chain and oxidative damage, protein–protein cross-linking, protein–DNA cross-linking, and lipid metabolism oxidation, etc. ROS can cause various cardiovascular diseases, cancers, and aging. In vivo oxidation eventually leads to aging of the organism, so exogenous antioxidant supplements, with food being an important source, have become a topic of research [107]. Therefore, this section lists the key studies on the effect of natural antioxidants such as collagen peptides, polyphenols, vitamins, polysaccharides, and fatty acids extracted from foods on alleviating skin aging (Table 2). Some antioxidants are also extracted from food, and their effect of alleviating skin aging is studied through local skin penetration in vitro. However, they then do not belong to diet, hence, they are not summarized here.
Table 2.
Summary of the key in vivo studies investigating the potential effects of foodborne antioxidants in the skin aging.
| References/Country/Study Type | Antioxidants/Source | Participants/Age | Induction Factors | Group/Dose/Time | Main Result | Main Conclusion |
|---|---|---|---|---|---|---|
| Effects of Oral Collagen Peptides on Skin Aging | ||||||
| [133]/China/animal | High-, medium- and low-antioxidant peptides (HCP, MCP and LCP)/silver carp skin | KM mice/5 week (25 ± 2 g) |
3UV-A + 1UV-B | Tg: HCP, MCP, LCP (0,200 mg/kg.bw.d)/0/1/2 weeks | 1. ACPs significantly alleviated skin composition and antioxidant index abnormalities induced by UVs. 2. HCP has the best protection effect on skin photoaging, and the difference between MCP and LCP is not obvious. |
ACPs have the potential to resist photoaging of the skin. |
| [134]/China/animal | Gelatin (SG)and gelatin hydrolysate (SGH)/ salmon skin |
ICR male mice/ 20 to 22 g |
UV-B | Tg: SG (100, 500 mg/kg.bw.d), SGH (100, 500 mg/kg.bw.d); Cg: Vc 100 mg/kg.bw.d/5 week | 1. Antioxidant activity of SG and SGH is related to dose, molecular weight and amino acid composition. 2. SG and SGH alleviate oxidative damage by enhancing antioxidant enzyme activity and thymus index |
SGH has the potential to be used as an antioxidant in health products and cosmetics. |
| [135]/Korea/animal | Collagen peptide (CP)/ tilapia scale |
SKH–1 hairless mice/ 6 weeks old |
UV-B | Tg:CP (0,500, 1000 mg/kg.bw.d) Cg: N–acetyl glucosamine (1000 mg/kg.bw.d)/ 9 weeks |
1. Oral CP increased skin hydration, reduced wrinkle formation, changed the expression of HAS–1,–2, and maintained the stability of HA. 2. CP regulate the expression of skin moisturizing factor filagglutinin and total chain protein |
CP can be used as a nutrient to relieve UV-B-induced skin wrinkles, dehydration and water loss. |
| [136]/Brazil/cell | Collagen Hydrolysate (CH)/cow | HDFs | Cg:CH (0.5, 1.0, 2.5 and 5.0 mg/mL)/48 h | 1. CH regulates cell metabolism without cytotoxicity. 2. CH maintains intracellular protein stability by inhibiting the activity of MMP 1 and 2. |
This CH has protective effects on skin cells and has the potential to become a food supplement. | |
| [137]/Korea/clinical | Low-molecular-weight Collagen peptide (LMWCP)/ catfish’s skin |
Women/40–60 years old | Age | Tg:LMWCP; 1000 mg/d. Cg: placebo; (0/6/12) weeks | Oral LMWCP protects photoaged skin by improving skin wrinkles, hydration and elasticity | LMWCP can be used as a functional food ingredient to relieve skin photoaging. |
| [138]/China/animal | Collagen hydrolysates (CHs)/Nile tilapia skin | ICRmice/38 ± 4 g, 9-month-old | Age | Tg:CHs (0%, 2.5%, 5%, 10%); Ng: weaned mice; Cg: (WC, 10% whey protein hydrolysates)/180 days |
1. CHs significantly improves skin visual appearance, tissue structure and matrix homeostasis. 2. CHs alleviates oxidative stress by increasing skin antioxidant activity |
CHs can be used as a functional nutritional food against skin aging, but its molecular mechanism is not clear. |
| [139]/China/animal | Elastin peptides (EH)/bovine arteries | Female mice/ (20 ± 2 g) | UV | Nc:vehicle-treated mice; Mg:vehicle-treated + UV. EH group:UV + EH (100 mg/kg.bw.d)/8 weeks | EH can significantly reduce UV-induced epidermal hyperplasia and fibroblast apoptosis, and increase skin hydroxyproline and water content | EH has the potential to prevent and regulate skin photoaging |
| [140]/China/animal | Collagen peptides (CPs)/silver carp skin |
Mice/(8, 13-month-old (28 ± 2, 45 ± 5 g) | Age | Cg: young mice (normal saline); Tg: old mice (CPs: 400 mg/kg.bw.d); Mg: Old mice (normal saline)/2 months | 1. CPs promotes skin collagen synthesis by regulating cytokines in skin and serum. 2. Intake of CPs inhibited platelet release. |
CPs has the potential to be an anti-aging, anti- cancer and anti- cardiovascular health product |
| [141]/Canada/cell | Collagen peptides (CPs)/Chicken meat | HDFs cells/ human skin |
DCF-DA | Tg: Two peptides, hydrolyzed by two enzymes (0, 2.5 mg/mL)/24 h | Two chicken collagen peptides have significant effects on inflammatory changes, oxidative stress, type I collagen synthesis, and cell proliferation in skin HDFs | CPs hydrolyzed by different enzymes have different protective and regulatory effects on skin fibroblasts |
| [142]/Canada/cell | Collagen peptides (CPs)/porcine/ bovine/tilapia/hen skin |
HDFs/ human skin |
UV-A | Tg: Four kinds of collagen peptides (0, 0.5, 1, 2, 4 mg/mL)/24 h | 1. Bovine CH inhibits the MMP–1 production. 2. Tilapia CH promotes cell viability and type I collagen generation, while inhibiting ROS and MMP–3 generation. 3. Hen CH promotes collagen production and reduces ROS, MMP–1 and 9 generation and the expression of apoptotic genes. |
Hen CH protects HDFs from UV-A-induced damage better than pigs, cattle and tilapia. |
| [143]/China/animal | High, low molecular weight collagen hydrolysates (HMCH/LMCH)/Silver Carp | Mice/5weeks (25 ± 2 g) | UV-A + UV-B | Tg1:UV + LMCH (HMCH)(50, 100, 200 mg/kg.bw.d)/6 weeks; Tg2:UV+LMCH (HMCH) (200 mg/kg.bw.d)/ 2 weeks |
1. Both HMCH and LMCH increase skin components and antioxidant enzyme activity in skin and serum. 2. LMCH is more effective than HMCH. 3. Skin hydroxyproline, HA, and moisture content depend on peptide dose. |
LMCH extracted from silver carp skin can be used as a dietary supplement to prevent skin aging. |
| [144]/Japan /clinical |
High, low purity collagen hydrolysate (H-CP/L- CP)/fish gelatin | Female/(35–55 years old) | Age | H-CP group: 5 g/d; L-CP group: 5 g/d; Cp: placebo; 0/4/8 weeks. | H-CP is more significant than L-CP in improving facial skin moisture, elasticity, wrinkles, and roughness. | L-CP and H-CP are both effective dietary supplements to improve skin conditions. |
| [145] /Thailand /cell/animal |
Collagen hydrolysate (HC)/Lates calcarifer skin | HDFs/human; Wistar rats (214 ± 26 g) | Mice Tg: (0,2000,5000 mg/kg.bw.d)/15d; Cell Tg: (50, 100, 150 and 200 µg/mL)/24 h. |
1. Animal and cell experiments prove that HC is non-toxic. 2. HC can promote the growth of fibroblasts and the synthesis of cellular collagen, but not as effective as HC combined with VC. |
Single HC or HC combined with VC can be used as nutritional health products for skin care. | |
| [146]/China /cell |
Gelatin hydrolysates (CGH)/Cod skin | HDF cells/ Mouse skin |
UV-B | Tg: CGH (0, 0.001, 0.01, 0.1,1, 10) mg/mL /24 h. |
1. CGH inhibits the expression of MMP–1 in fibroblasts induced by UV-B. 2. Purified MMP–1 inhibitory peptides have significant inhibitory effects on MMP–1, p-ER and p-p38. |
CGH can be used as a functional supplement for skin care. |
| [147]/China /cell/animal |
High, medium, low antioxidant peptide (HCP/ MCP/LCP)/Silver carp skin; Serum collagen peptides (SCP)/ rat serum |
SD rat (8 week); ESF cells/skin | UV-A | Rats Tg (HCP, MCP and LCP)/(2.4 g/kg.bw.d)/2 h; Cell Tg: (SHCP, SMCP and SLCP)/(0, 50, 200 µM/mL)/24 h. | 1. SCP is the active component of serum metabolites, which shows repair effect by removing ROS. 2. SCP promotes collagen synthesis and inhibits its degradation by activating TGF-β/Smad3 pathway and inhibiting the expression of AP–1 and MMP–1,3,SHCP is the best one. |
CP promotes photoaging skin repair by activating the TGF- TGF/Smad pathway and inhibiting collagen reduction. |
| [148]/China /animal |
Alcalase, Collagenase Collagen peptide (ACP/CCP)/ bovine bone |
Mice/(8, 13-month-old (28 ± 2, 45 ± 5 g) | Age | Cg: young mice (normal saline); Tg: old mice/ACP (200, 400, and 800 mg/kg.bw.d), CCP (400 mg/kg.bw.d)/8 weeks | Oral CPs improve skin relaxation, increase collagen content and antioxidant enzyme activity, repair collagen fibers, and normalize the ratio of skin collagen. ACP is better than CCP. | CP can alleviate the chronological aging of the skin and has the potential to become an anti-aging functional food. |
| [149]/Korea /animal/cell |
Collagen peptide NS (CPNS)/fish scale | HDF cells /human, Mice/8 weeks old (25–30 g) |
UV-B | Cell Tg: CPNS (0, 50, 100, 250, 500 µg/mL)/24 h; Mice Tg: CPNS (300, 500 mg/kg.bw.d)/12weeks | 1. CPNS treatment reduced the production of MMP–1 and increased the synthesis of type 1 procollagen in HFD cells. 2. Oral CPNS significantly reduced skin wrinkle formation, epidermal water loss, epidermal thickness, and increased hydration. |
CPNS are a potential food supplement to prevent skin aging. |
| [150]/China /animal |
Gelatin/Amur sturgeon swim bladder | Female SD rat/6 months old |
Age | Cg (8% whey protein); Tg (8%, 4%, 2%)/12 months. | 1. Oral administration of 3.85 g/kg.bw.d gelatin significantly improved skin histological structure and collagen ratio. 2. Skin antioxidant activity increased. |
The gelatin improves the foundation for the development of anti-aging foods. |
| [110]/China /animal |
Protein hydrolysate (WPH)/Walnut | SD rats/ 180–200 g |
UV-A + UV-B | Cg:( distilled water); Tg: UV-R + WPH (0, 0.32, 0.98, 2.88 g/L)/18 weeks | 1. WPH significantly enhances skin elasticity and promotes the biosynthesis of Col I, Hyp, and HA. 2. WPH inhibits MMP–1 activity and repairs skin damage. 3. WPH repair effect becomes dose dependent, high dose is best. |
WPH has potential as a functional food ingredient against photoaging. |
| Effects of Oral Polyphenol on Skin Aging | ||||||
| [151,152] /China/cell /animal |
Polyphenol extract (HPE)/hawthorn | HDFs and HaCaT/human; mice/5–6 weeks old | UV-B | Cell Tg: HPE (0, 5, 10 µg/mL)/24 h; Mice Tg: HPE (0, 100, 300 mg/kg.bw.day)/12 weeks |
1. HPE treatment can promote cell proliferation, increase intracellular collagen and reduce MMP–1 production. 2. Oral HPE reduces UV-B-induced skin damage by eliminating ROS, reducing DNA damage and inhibiting p53 expression. |
HPE can be used as an anti-aging food or cosmetic ingredient. |
| [153]/Spain /clinical |
Products rich in polyphenol (NutroxsunTM)/rosemary and citrus | Adult female | UV-B + UV-A | Long-term: NutroxsunTM (250 mg/day)/ 2 weeks; Short-term: NutroxsunTM (100, 250 mg/day)/24, 48 h |
1. Dietary NutroxsunTM reduces UV- induced skin changes, wrinkles and elasticity improvements. 2. The improvement effect between two doses is not obvious. |
Long-term oral NutroxsunTM can be used as a nutritional supplement to improve skin conditions. |
| [154]/Korea /cell |
Polyphenolic- rich extract (SSE and SSW)/Spatholobus Suberectus stem |
HaCaT/Human skin | UV-B | Tg1: SSE (0, 3, 10, 30, 300 µg/mL); Tg2: SSW (0, 3, 10, 30, 300 µg/mL)/24 h | 1. SSE and SSW inhibited ROS production and cell damage. 2. SSE repairs skin by upregulating the expression of enzymes and proteins in cells, blocking UV-B-induced MAPKs phosphorylation and its downstream transcription factor. |
SSE can be used as a natural biomaterial to inhibit UV-B-induced photoaging. |
| [155]/China /animal |
Rambutan peel phenolics (RPP)/Nephelium lappaceum; Leu-Ser-Gly-Tyr-Gly-Pro (LSGYGP)/synthetic |
Male BALB/c nude mice/20–22 g | UV-B | Single group: RPP (100 mg/kg.bw. d), SGYGP (100 mg/kg.bw.d); Composite group: (50 RPP+ 50 LSGYGP) mg/kg.bw.d, (100 RPP + 100 LSGYGP)mg/kg.bw.d/10 weeks | 1. RPP and LSGYGP improve skin biochemical indicators, tissue structure and collagen levels. 2. RPP enhances the regulation of oxidative stress and inflammatory factor levels. 3. LSGYGP significantly affects skin collagen and HA content. |
Oral RPP and LSGYGP can alleviate UV-B- induced skin aging. |
| [156]/Korea /animal |
Polyphenols/Flavonoid hesperidin exerts | Male hairless mice/6- week-old |
UV-B | Cg: water; Tg: UV-B + hesperidin (0, 100 mg/kg.bw.d)/12 weeks | 1. Oral hesperidin inhibited UV-B-induced skin thickening and wrinkle formation. 2. Hesperidin inhibited UV-B-induced expression of MMP–9 and cytokines, and protected collagen fiber loss. |
Oral hesperidin regulates MMP–9 expression by inhibiting MAPK- dependent signaling pathways to relieve skin photo-aging. |
| [157]/Korea /cell |
Polyphenols/3,5,6,7,8,3,4-heptam-ethoxy flavone (HMF)/C. unshiu peels | HDFn cells/human dermal | UV-B | HMF (0, 50, 100, 200 µg/mL)/24 h | 1. HMF protects UV-induced HDFn cell damage by inhibiting MMP–1 expression through phosphorylated MAPK signals. 2. HMF regulates the expression of Smad3 and Smad7 proteins in a dose-dependent manner. |
HMF has the potential to be an anti-aging cosmetic or food supplement. |
| [158]/Korea /cell |
Polyphenols/ Tectorigenin/ Belamcanda chinensis L |
HaCaT cells/human | UV-B | Tg: Tectorigenin (0, 0.1, 1,10 µM); Cg: VC (200 µM)/24 h |
1. Tectorigenin lowers ROS levels by increasing intracellular antioxidant enzymes. 2. Tectorigenin reduces mmp–1 and inhibits collagen degradation. 3. Tectorigenin inhibits apoptosis by regulating the levels of caspase–3 and bcl–2 related proteins. |
Tectorigenin alleviates skin damage by inhibiting UV-B-induced cellular oxidation, apoptosis and collagen degradation. |
| Effects of Oral Polysaccharides on Skin Aging | ||||||
| [116]/China /animal |
Polysaccharides (TP)/T. fuciformis |
SD rats/6~7 weeks old (180–220 g) | UV-A + UV-B | Cg: no irradiation; Tg group: UV + TP (0, 100, 200, 300 mg/kg.bw.d)/12 weeks |
Oral TP can alleviate UV-induced skin structural changes, repair collagen damage, maintain the I/III collagen ratio and enhance skin antioxidant enzyme activity. | TP has the potential to become a skin-protective functional food additive. |
| [117]/Korea /cell |
Polysaccharide (HFPS)/Hizikia fusiforme | HDF cells | UV-B | Cg: no irradiation; Tp: UV + HFPS (0, 25, 50, 100 µg/mL)/24 h |
1. HFPS significantly reduces cell ROS and increases the pure activity rate. 2.HFPS inhibits UV-induced skin damage by regulating NF-κB, ap–1 and MAPKs signaling pathways. | HFPS has a strong anti-ultraviolet effect and is a potential pharmaceutical, food, and cosmetic ingredient. |
| [118]/China /cell |
Polysaccharide (LBP)/Lycium barbarum |
HaCaT cells | UV-B | Tg1: LBP (0, 50, 100, 300, 600, 1500, 3000 µg/mL) 24 h; Tp2: UV-B + LBP (0, 300 µg/mL)/24 h |
LBP mainly eliminates ROS and reduces DNA damage. In part, the Nrf2/ARE pathway is activated to inhibit the p38 MAP pathway, thereby inhibiting the activation of caspase–3 and the expression of mmp–9 to protect the aging cells. | LBP may be used as a protective agent or food additive against skin oxidative damage. |
| [119]/China /cell |
Polysaccharide (GL-PS)/Ganoderma lucidum |
Fibroblast/men foreskin | UV-B | Tg: UV-B + GL-PS (0, 10, 20, 40 µg/mL) 24 h; Tg: no UV-B and GL-PS/24 h | After GL-PS treatment, cell activity increased, senescent cells decreased, CICP protein expression increased, MMP–1 protein expression decreased, and cell ROS level decreased. | GL-PS protects UV-B- induced cell photoaging by eliminating intracellular ROS, which will provide strategies for subsequent studies. |
| [120]/China /animal |
Polysaccharide (SFP)/Sargassum fusiforme | Female KM mice/7 weeks old (20–25 g) | UV-B | Cg: UV-B + sodium hyaluronate (400 mg/kg. bw/d); SFP Tg: UV-B + SFP (0, 200, 400, 600 mg/kg.bw/d)/9 weeks | 1. SFP regulates mouse chest, spleen index and skin water content. 2. SFP increases skin antioxidant enzyme activity, reduces ROS, and reduces oxidative damage.3.SFP inhibits MMP–1 and 9 levels in the skin. |
SFP can be a potential functional food additive for skin protection. |
| [121]/China /cell/animal |
Purified, crude polysaccharide (TLH–3,TLH)/ Tricholoma lobayense |
HELF cells/human; Mice/8 weeks (23 ± 2 g) |
t-BHP/D-galactose | Cell Tg: TLH–3 (0, 50, 100, 200, 400 µg/mL), Pc: Vc (50 ug/mL)/24 h; Mice Tg: TLH–3 and TLH (200 mg/kg. bw/d),Pc: Vc (100 mg/kg. bw/d)/5 weeks | 1. TLH–3 relieves cell senescence by regulating the expression of bcl–2, bax, caspase–3 proteins, inhibiting senescence-related enzyme levels. 2. TLH–3 reduced skin pathological lesions by reducing IL–6, LPF, AGEs, and enhanced MAO activity. |
TLH–3 is an active polysaccharide that protects cells and mice from oxidative stress aging. |
| Effects of Oral Vitamins on Skin Aging | ||||||
| [159]/China /cell |
Vitamin Coenzyme Q10 (CoQ10) | ESF and HaCaT cells/ Human |
UV-A, UV-B | Cg: ESF, HaCat (CoQ10 (0, 0.5, 1, 2 µM))/24 h; Tg: ESF, HaCat (UV-A or UV-B + CoQ10 (0, 1, 5, 10 µM))/24 h | 1. CoQ10 treatment promoted ESF cell proliferation, type IV collagen and elastin gene expression. 2. CoQ10 treatment inhibited UV-induced IL–1a production in HaCaT cells. |
CoQ10 has anti-aging effect on chronological aging and photo-aging and can be used in food and cosmetics. |
| [122]/Japan /clinical |
VC, VE, and Astaxanthin (AX) | Female/(mean age 37.26 years) | - | Tg1:AX (6 mg) + VC (1000 mg) + VE (10 mg)/d; Tg2:VC (1000 mg) + VE (10 mg)/d/20 weeks | Tg 1 significantly improved skin moisture content, skin elasticity and wrinkles; Tg 2 did not improve the skin significantly. |
Oral formulations containing astaxanthin and vitamin C and E have skin-improving effects. |
| [160]/Iran /animal |
Silymarin, Vitamin C |
Balb/C mice/6 weeks old (30 ± 2 g) | UV-B | Cg: Silymarin (100),VC (40 mg/kg.bw/d)/; Tg: UV-B + Silymarin (0, 100 mg/kg.bw/d), UV-B + VC: (0, 40 mg/kg.bw/d)/4 weeks. |
Oral VC enhances skin antioxidant enzyme activity, reduces skin wrinkle formation and thickness increase in mice induced by UV-B. | Salicylic acid and vitamin C can be used as food or cosmetic ingredients to resist skin photo-aging. |
| [161]/Korea /cell |
Niacinamide (NIA) | HaCaT/ human |
PM2.5 | Cg: NIA (0, 12.5, 25, 50, 100, or 200 µM); Tg: NIA (0, 12.5, 25, 50, 100, or 200 µM) + PM2.5 (50 µM)/24 h | NIA treatment can inhibit the oxidation of lipid, protein, DNA and other molecules induced by PM 2.5, as well as inhibit apoptosis and ROS production. | NIA protects cells from PM 2.5-induced oxidative stress and cell damage. |
| Effects of Oral Fatty Acids on Skin Aging | ||||||
| [125]/Brazil /animal |
0live oil | Swiss mice/8–12 weeks age | Rotational stress | Stress group: stress + olive (1.5 g/kg.bw. d), Cg: olive (1.5 g/kg. bw/d)/29 d | Olive inhibited skin ROS, lipid peroxidation, protein carbonylation, phenolamine synthesis, MMP–8 expression and promotes collagen deposition in mice through NF-κB and NRF2 pathways. | Oral administration of olive oil can reduce mice skin aging induced by stress. |
| [126]/Korea /animal |
7-MEGATM500/> 50% of palmitoleic acid containing fish oil, omega–7 | H–1 mice/5-week old (18–20 g) | UV-B | Cg: 30% EtOH; Tp: 7-MEGATM500 (50, 100, 200 mg/kg.bw/d)/4 weeks | 1.7-MEGATM 500 improves skin histological indicators and significantly down-regulated the expression levels of MMP–3 and c-jun genes and proteins in the skin. | 7-MEGATM500 can alleviate UV-B induced skin photoaging in mice |
| [129]/Korea /cell |
Fermented Fish Oil (FFO) |
HaCaT/ human |
PM2.5 | Cg: PM2.5; Tp:PM2.5 + FFO (0, 20 µg/mL)/24 h |
FFO can inhibit PM 2.5-induced intracellular ROS, Ca 2+ levels and MMPs–1,2,9 production, and block the MAPK/AP–1 pathway. | FFO can alleviate PM 2.5 induced skin aging. |
| [162]/Japan /animal |
Coconut oil | Female mice/(6 weeks old) | DNFB | Cg: Coconut or soybean oil (4%)/2 months; Tg: Coconut or soybean oil (4%)/after 2 months + DNFB | Oral coconut oil improves BDFB-induced skin inflammation in mice. Mechanistically related to elevated mead acid in serum inhibiting directional migration of neutrophils. | Dietary coconut oil improved skin contact allergies in mice by producing midic acid. |
Cg = control group; Tg = test group; Ng = normal group; Mg = model group; mg/kg.bw.d = mg/kg. body weight/day; DNFB = 1-fluoro-2,4-dinitro-benzene; HaCaT = Human skin epidermal keratinocytes; t-BHP = tert-butyl hydroperoxide; DCF-DA = dichlorofluorescein diacetate; HAS-1,-2 = hyaluronic acid synthases1and 2; MAO = monoamine oxidase; Co Q10 = Coenzyme Q10; LPF = lipofuscin pigment; NF-κB = nuclear factor kappa B; IL-6 = Interleukin-6; IL-1 = Interleukin-1; NRF2 = nuclear factor erythroid-2p45-related factor2; ARE = antioxidant response element; p38 MAP = p38 mitogen-activated protein; MAPKs = Mitogen-activated protein kinases; TGF-β/Smad3 = Transforming growth factor-β/Recombinant Human Mothers Against Decapentaplegic Homolog 3; p-ERK = phosphorylated extracellular regulated kinase; p-p38 = phospho-p38.
4.1. Collagen Peptide
Collagen is a long cylindrical polymeric protein, the main component of animal extracellular matrix (EMC), and the most abundant and widely distributed functional protein in mammals, accounting for 25% to 30% of the total protein; some organisms constitute even up to 80% or more collagen, which have unique physiological functions and are widely used in food, medicine, tissue engineering, cosmetics, and other fields [108]. Traditionally, collagen is thought to improve skin health, but later research found that collagen peptides with smaller molecular weight are easier to absorb and have more significant effects. While collagen is mainly absorbed and utilized in the form of peptides in mice, with a utilization rate of about 50%, collagen peptides can be almost completely absorbed and utilized by the body [109]. Collagen peptide is a series of small molecular peptides obtained from the proteolytic hydrolysis of collagen. Because of their small molecular weight, easy absorption, anti-inflammatory, and antioxidant characteristics, collagen peptides have been studied as a new favorite in recent years as exogenous antioxidants to relieve skin aging. Collagen peptides mainly come from animal skin, bones, tendons, muscles, and other tissues. The research on animal-derived collagen peptides and other protein peptides in alleviating skin aging in recent years is summarized in Table 2. Nevertheless, due to associated risk of diseases such as mad cow disease, foot-and-mouth disease, etc., and religious controversy of animal-derived collagen peptides, in recent years, people have also evaluated the effects of non-collagen peptides such as walnut protein peptides and whey protein peptides on alleviating skin aging in mice [110]. There are also some cases about the combined application of protein peptides and other nutrients, although, they have not been summarized because the functions of various nutrients cannot be distinguished.
Mechanistically, collagen peptides and other protein peptides may relieve skin aging through either of the three pathways. First, the protein or peptide enters the blood circulation after digestion and absorption, and then participates in the skin fibroblasts as a precursor of collagen synthesis, thereby protecting the aging skin. Second, collagen peptides that enter skin cells incur anti-aging effects by removing ROS from cells, protecting the cell’s endogenous antioxidant defense system, and reducing oxidative damage and inflammatory responses in cells. In the third pathway, protein peptides entering skin cells promote collagen and hyaluronic acid synthesis and inhibit the production of inflammation by regulating cytokines and activating TGF–β/Smad or other signaling pathways, while, these peptides concurrently also prevent skin collagen degradation by inhibiting the expression of proteases such as nuclear transcription factor activating protein–1 (AP–1), MMP–1 and MMP–3.
4.2. Polyphenols
Polyphenols are secondary metabolites of plants and exist widely in vegetables, fruits, tea, and other plants. Due to their obvious antioxidant properties, polyphenols have become one of the most important compounds to be used in cosmetics and nutritional cosmetology to combat skin aging. In recent years, tea polyphenols, curcumin, flavonoids, silymarin, and grape resveratrol have been the most studied polyphenols with anti-aging properties. Polyphenols reduce oxidative damage and inflammation in the skin through their antioxidant and anti-inflammatory effects, mainly by inhibiting collagen degradation, increased collagen synthesis, and inhibiting inflammation, which involves the regulation of matrix metalloproteinases, cytokines, and signaling pathways (e.g., Nrf2, NF-κB, MAPK, etc.) [111,112]. This article lists some experimental cases of food-derived polyphenol extracts to alleviate skin aging (Table 2), but most of the anti-aging effect of polyphenols has been verified in vitro through topical administration on target skin cells. Nonetheless, the clinical application of polyphenols in dermatology is still in its infancy, and there are relatively few reports on the cytotoxicity of polyphenols [113,114].
4.3. Polysaccharides
Polysaccharides are polymer carbohydrates formed by the dehydration and condensation of multiple monosaccharides. Due to their pharmacological effects, such as improving immune function, anti-tumor, anti-virus, anti-glucose, anti-oxidative, lowering blood lipids, and low cytotoxicity, polysaccharides are an ideal functional food and drug active ingredient [115]. Polysaccharides have been the research focus from the past five years, and there are several reports on various types of polysaccharides. In general, the research mainly focuses on the isolation and extraction of polysaccharides, structural identification, modification, and determination of physiological and pharmacological activities of polysaccharides and their derivatives. Antioxidant activity is one of the properties of polysaccharides, particularly in terms of relief from skin aging. Polysaccharides such as agaric polysaccharides, Lycium polysaccharides, algal polysaccharides, lingzhi polysaccharides, and mushroom polysaccharides have been found to alleviate skin aging. Dietary polysaccharides have a positive effect on the improvement of aging skin. Mechanistically, oral polysaccharides enhance skin antioxidant enzyme activity, remove ROS, and reduce oxidative damage. They regulate the expression of Bcl–2, Bax, and Caspase–3 by activating Nrf2/ARE and other pathways, and inhibit apoptosis. Finally, polysaccharides inhibit collagen degradation by inhibiting the expression of enzymes such as MMP–1 and MMP–9, maintaining a stable collagen ratio, repairing skin structure, and maintaining skin moisture content [116,117,118,119,120,121].
4.4. Vitamins
Many vitamins have been tested for their antioxidant properties. They can reduce ROS in aging skin cells to low-activity molecules and reduce oxidative damage to key components of skin cells. Most research has focused on vitamins A, B (B3, B12), E, D, C, coenzyme Q10, and lipoic acid. Retinoids are the most common anti-aging drugs that have been used (such as retinoic acid prevents skin aging by regulating genes and MMPs) to treat and prevent photo-aging of the skin [97,98]. B vitamins have been shown to prevent skin aging mainly by preventing skin inflammation and pigmentation [99]. Vitamin C is a powerful antioxidant, its concentration in the skin is closely related to skin biological functions, and it is often used as a positive control for skin aging tests. It acts as an enzymatic factor and antioxidant to promote collagen synthesis and eliminate cellular ROS to relieve skin aging [100]. There seems to be a contradictory conclusion that vitamins D can alleviate skin photo-aging, because light not only synthesizes vitamins D but also causes skin aging. However, research shows that vitamin D can reduce DNA damage, inflammation, and photocarcinogenesis caused by ultraviolet rays, and thus, protect the skin [101]. A combination of vitamin E and C can help activate vitamins E, which protects skin against chemical stimuli and UV-induced irritation and damage by inhibiting lipid peroxidation in the skin [102,103]. Coenzyme Q10 is a vitamin-like substance widely present in meat foods, and its anti-aging function has been proven [122]. However, due to the instability, poor water solubility, and low utilization of vitamins during storage, vitamins are often used in combination with other antioxidant ingredients (such as collagen, astaxanthin, carotenoids, etc.) to enhance their anti-aging effects.
4.5. Fatty Acids
Lipids are an important part of the skin and are closely related to skin epidermal barrier function, membrane structure, internal environment balance, and damage repair. Skin aging is accompanied by a decrease in fat content, mainly due to a decrease in the ability of cells within the skin to synthesize and secrete fat [123]. Besides, the amount of dietary fat intake is closely related to the lipid composition of the body and skin tissues, and insufficient intake of essential fatty acids or abnormal fat metabolism leads to serious skin diseases [86,124]. Omega-3 and omega-6 polyunsaturated fatty acids play an important role as human skin barriers, and also have certain effects in the prevention and treatment of skin inflammation [104]. Oral olive oil can reduce skin aging induced by chronic psychological stress by acting on the NF-B NRF2 pathway in mice [125] (Table 2). Oral 7-MEGATM 500 (a product containing more than 50% palmitoleic acid containing fish oil, omega-7) has been shown to relieve UV-B and H2O2-induced skin oxidative stress, inflammation, aging, and promotes skin regeneration in mice [126,127]. The fatty acids extracted from W. somnifera seeds have good anti-inflammatory effects and exert an enhanced effect on psoriasis by reducing the release of pro-inflammatory factors (TNF-α and IL–6) [128]. The fermented fish oil protects skin aging by inhibiting PM2.5-induced ROS, MMP-s, and blocking the mitogen-activated protein kinase/activator protein 1 (MAPK/AP–1) pathway [129]. The effect of dietary and in vitro topical fatty acids on skin aging has been reviewed in detail by Wang and Wu [130].
4.6. Other Anti-Aging Nutrients
In addition to the aforementioned foodborne antioxidants that can be used as functional food ingredients to relieve skin aging, the combined use of different types of antioxidants has also been reported. Some studies have reported that dietary probiotics and their products can also alleviate skin aging. For example, probiotic fermentation can enhance the skin anti-photo-aging activity of Agastache rugosa leaves, and some probiotic extracts also have the potential to improve aging skin. [131,132]. There may be some foodborne antioxidants, which have not been mentioned in this article and need to be discussed subsequently.
5. Conclusions and Prospects
Skin aging is a complex and long biological process, which is affected by genetic and environmental factors. Although stem cell transplantation, injection of hyaluronic acid, and retinoic acid have certain therapeutic effects, each method has corresponding disadvantages. With the improvement of people’s requirements for the effectiveness, safety, and durability of treatment methods, prevention, and relief from skin aging through dietary management have become an inevitable trend. Therefore, after analyzing and summarizing relevant literature, we draw the following key conclusions:
People’s current understanding of diet to improve skin aging is still insufficient. While it is difficult for us to accurately define what is a healthy diet, and to quantify the relationship between diet and skin aging that convince the public, it is difficult for them to change their original lifestyle and diet, even if people have such knowledge.
The issues of accurately quantifying the skin improvement effect of each nutrient intake, and the negative effects of smoking, drinking, grilling, etc., on skin aging still need to be addressed.
The functional anti-aging ingredients in food mainly relieve skin aging in three ways. First, anti-aging ingredients (such as protein peptides and essential fatty acids) enter the skin as a precursor after digestion and absorption and participate in the synthesis and metabolism of skin components. Second, anti-aging ingredients relieve skin oxidative damage by removing cellular ROS and enhancing antioxidant enzyme activity. Third, the anti-aging component acts as an enzymatic factor, and regulates the expression of enzymes such as MMPs and AP–1, inhibiting the degradation of skin components and maintaining the integrity of the skin structure.
The limitations of foodborne antioxidants such as unstable storage, low skin bioavailability, and poor solubility, can be improved by chemical modification, collagen drug delivery, and a combination of supplements.
Only oral supplementation is not enough to improve the skin. The combination of oral and external skin penetration should be the safest and the most effective way to improve skin aging.
Diet causes skin aging or improves skin aging and is difficult to simply apply to clinical research. While on the one hand, there is an ethical controversy, on the other hand, the experimental period is too long to control the diet of volunteers for a single, long duration, and the uniformity of clinical experimental conditions is not guaranteed, resulting in vague experimental results and insufficient credibility.
Improvement in skin aging through diet should not be rushed, because skin aging caused by diet and improvement of aging performance by diet are long-term processes. There is also the problem of metabolic processing of food and nutrients until they reach the skin. They have to travel a long way, and there is still a lot to study in this process.
Author Contributions
C.C. and Z.X. wrote the manuscript, their contributions to this article are the same; C.G. and Y.W. revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financially supported by by Yunling Scholars of Yunnan Province(to C.G.).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Blanpain C., Fuchs E. Epidermal stem cells of the skin. Annu. Rev. Cell Dev. Biol. 2006;22:339–373. doi: 10.1146/annurev.cellbio.22.010305.104357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang S., Duan E. Fighting against skin aging: The way from bench to bedside. Cell Transplant. 2018;27:729–738. doi: 10.1177/0963689717725755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphree R.W. Impairments in skin integrity. Nurs. Clin. 2017;52:405–417. doi: 10.1016/j.cnur.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Veltri A., Lang C., Lien W.H. Concise review: Wnt signaling pathways in skin development and epidermal stem cells. Stem Cells. 2018;36:22–35. doi: 10.1002/stem.2723. [DOI] [PubMed] [Google Scholar]
- 5.Hsu Y.C., Li L., Fuchs E. Emerging interactions between skin stem cells and their niches. Nat. Med. 2014;20:847. doi: 10.1038/nm.3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arseni L., Lombardi A., Orioli D. From structure to phenotype: Impact of collagen alterations on human health. Int. J. Mol. Sci. 2018;19:1407. doi: 10.3390/ijms19051407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orioli D., Dellambra E. Epigenetic regulation of skin cells in natural aging and premature aging diseases. Cells. 2018;7:268. doi: 10.3390/cells7120268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim H., Park S.Y., Moon S., Lee J., Kim S. Autophagy in human skin fibroblasts: Impact of Age. Int. J. Mol. Sci. 2018;19:2254. doi: 10.3390/ijms19082254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liberato T., Pessotti D.S., Fukushima I., Kitano E.S., Serrano S.M., Zelanis A. Signatures of protein expression revealed by secretome analyses of cancer associated fibroblasts and melanoma cell lines. J. Proteom. 2018;174:1–8. doi: 10.1016/j.jprot.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 10.DesJardins-Park H.E., Foster D.S., Longaker M.T. Fibroblasts and wound healing: An update. Regen. Med. 2018;13:491. doi: 10.2217/rme-2018-0073. [DOI] [PubMed] [Google Scholar]
- 11.Pincha N., Hajam E.Y., Badarinath K., Batta S.P.R., Masudi T., Dey R., Andreasen P.A., Kawakami T., Samuel R., George R., et al. PAI1 mediates fibroblast–mast cell interactions in skin fibrosis. J. Clin. Investig. 2018;128:1807–1819. doi: 10.1172/JCI99088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guerrero-Juarez C.F., Plikus M.V. Emerging nonmetabolic functions of skin fat. Nat. Rev. Endocrinol. 2018;14:163. doi: 10.1038/nrendo.2017.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Driskell R., Lichtenberger B., Hoste E., Kretzschmar K., Simons B.D., Charalambous M., Ferron S., Hérault Y., Pavlovic G., Ferguson-Smith A.C., et al. Distinct fibroblast lineages determine dermal architecture in skin development and repair. Nature. 2013;504:277–281. doi: 10.1038/nature12783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.López-Otín C., Blasco M.A., Partridge L., Serrano M., Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krutmann J., Bouloc A., Sore G., Bernard B.A., Passeron T. The skin aging exposome. J. Dermatol. Sci. 2017;85:152–161. doi: 10.1016/j.jdermsci.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Fisher G.J., Kang S., Varani J., Bata-Csorgo Z., Wan Y., Datta S., Voorhees J.J. Mechanisms of photoaging and chronological skin aging. Arch. Dermatol. 2002;138:1462–1470. doi: 10.1001/archderm.138.11.1462. [DOI] [PubMed] [Google Scholar]
- 17.Yanyan F., Xiongming P. Natural aging and photoaging of skin. Int. J. Dermatovener. 2004;30:354–356. [Google Scholar]
- 18.Landau M. Exogenous factors in skin aging. Curr. Probl. Dermatol. 2007;35:1–13. doi: 10.1159/000106405. [DOI] [PubMed] [Google Scholar]
- 19.Fuchs E. Epithelial skin biology: Three decades of developmental biology, a hundred questions answered and a thousand new ones to address. Curr. Top. Dev. Biol. 2016;116:357–374. doi: 10.1016/bs.ctdb.2015.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tigges J., Krutmann J., Fritsche E., Haendeler J., Schaal H., Fischer J.W., Kalfalah F., Reinke H., Reifenberger G., Stühler K., et al. The hallmarks of fibroblast ageing. Mech. Ageing Dev. 2014;138:26–44. doi: 10.1016/j.mad.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Quan T., Qin Z., Voorhees J.J., Fisher G.J. Cysteine-rich protein 61 (CCN1) mediates replicative senescence-associated aberrant collagen homeostasis in human skin fibroblasts. J. Cell. Biochem. 2012;113:3011–3018. doi: 10.1002/jcb.24179. [DOI] [PubMed] [Google Scholar]
- 22.Imokawa G., Ishida K. Biological mechanisms underlying the ultraviolet radiation-induced formation of skin wrinkling and sagging I: Reduced skin elasticity, highly associated with enhanced dermal elastase activity, triggers wrinkling and sagging. Int. J. Mol. Sci. 2015;16:7753–7775. doi: 10.3390/ijms16047753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bernerd F., Vioux C., Asselineau D. Evaluation of the protective effect of sunscreens on in vitro reconstructed human skin exposed to UV-B or UV-A irradiation. Photochem. Photobiol. 2000;71:314–320. doi: 10.1562/0031-8655(2000)071<0314:EOTPEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Bernerd F., Asselineau D. An organotypic model of skin to study photodamage and photoprotection in vitro. J. Am. Acad. Dermatol. 2008;58:155–159. doi: 10.1016/j.jaad.2007.08.050. [DOI] [PubMed] [Google Scholar]
- 25.Bernerd F., Marionnet C., Duval C. Solar ultraviolet radiation induces biological alterations in human skin in vitro: Relevance of a well-balanced UV-A/UV-B protection. Indian J. Dermatol. Venereol. Leprol. 2012;78:15. doi: 10.4103/0378-6323.97351. [DOI] [PubMed] [Google Scholar]
- 26.Fagot D., Asselineau D., Bernerd F. Matrix Metalloproteinase-1 Production Observed After Solar-Simulated Radiation Exposure is Assumed by Dermal Fibroblasts but Involves a Paracrine Activation Through Epidermal Keratinocytes. Photochem. Photobiol. 2004;79:499–506. doi: 10.1562/YG-03-11-R1.1. [DOI] [PubMed] [Google Scholar]
- 27.D’Errico M., Lemma T., Calcagnile A., De Santis L.P., Dogliotti E. Cell type and DNA damage specific response of human skin cells to environmental agents. Mutat. Res. Fundam. Mol. Mech. Mutagen. 2007;614:37–47. doi: 10.1016/j.mrfmmm.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 28.Duval C., Cohen C., Chagnoleau C., Flouret V., Bourreau E., Bernerd F. Key regulatory role of dermal fibroblasts in pigmentation as demonstrated using a reconstructed skin model: Impact of photo-aging. PLoS ONE. 2014;9:e114182. doi: 10.1371/journal.pone.0114182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naylor E.C., Watson R.E., Sherratt M.J. Molecular aspects of skin ageing. Maturitas. 2011;69:249–256. doi: 10.1016/j.maturitas.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 30.Kammeyer A., Luiten R.M. Oxidation events and skin aging. Ageing Res. Rev. 2015;21:16–29. doi: 10.1016/j.arr.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 31.Zouboulis C.C., Makrantonaki E. Clinical aspects and molecular diagnostics of skin aging. Clin. Dermatol. 2011;29:3–14. doi: 10.1016/j.clindermatol.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 32.Natarajan V.T., Ganju P., Ramkumar A., Grover R., Gokhale R.S. Multifaceted pathways protect human skin from UV radiation. Nat. Chem. Boil. 2014;10:542. doi: 10.1038/nchembio.1548. [DOI] [PubMed] [Google Scholar]
- 33.Gonzaga E.R. Role of UV light in photodamage, skin aging, and skin cancer. Am. J. Clin. Dermatol. 2009;10:19–24. doi: 10.2165/0128071-200910001-00004. [DOI] [PubMed] [Google Scholar]
- 34.Ravanat J.L., Douki T., Cadet J. Direct and indirect effects of UV radiation on DNA and its components. J. Photochem. Photobiol. B Biol. 2001;63:88–102. doi: 10.1016/S1011-1344(01)00206-8. [DOI] [PubMed] [Google Scholar]
- 35.Panich U., Sittithumcharee G., Rathviboon N., Jirawatnotai S. Ultraviolet radiation-induced skin aging: The role of DNA damage and oxidative stress in epidermal stem cell damage mediated skin aging. Stem Cells Int. 2016;2016:1–14. doi: 10.1155/2016/7370642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu Z., Wang L., Zhong D. Dynamics and Mechanisms of Ultraviolet-Damaged DNA Repair by Photolyases. Volume 3. Jenny Stanford Publishing; New York, NY, USA: 2017. pp. 109–144. [Google Scholar]
- 37.Narbutt J., Philipsen P., Harrison G., Morgan K., Lawrence K., Baczynska K., Grys K., Rogowski-Tylman M., Olejniczak-Staruch I., Tewari A., et al. Sunscreen applied at ≥ 2 mg cm−2 during a sunny holiday prevents erythema, a biomarker of ultraviolet radiation-induced DNA damage and suppression of acquired immunity. Br. J. Dermatol. 2018;180:604–614. doi: 10.1111/bjd.17277. [DOI] [PubMed] [Google Scholar]
- 38.Blackburn E.H. Structure and function of telomeres. Nature. 1991;350:569. doi: 10.1038/350569a0. [DOI] [PubMed] [Google Scholar]
- 39.Shay J.W. Telomeres and aging. Curr. Opin. Cell Biol. 2018;52:1–7. doi: 10.1016/j.ceb.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 40.Siegl-Cachedenier I., Flores I., Klatt P., Blasco M.A. Telomerase reverses epidermal hair follicle stem cell defects and loss of long-term survival associated with critically short telomeres. J. Cell Biol. 2007;179:277–290. doi: 10.1083/jcb.200704141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buckingham E.M., Klingelhutz A.J. The role of telomeres in the ageing of human skin. Exp. Dermatol. 2011;20:297–302. doi: 10.1111/j.1600-0625.2010.01242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simons M.J. Questioning causal involvement of telomeres in aging. Ageing Res. Rev. 2015;24:191–196. doi: 10.1016/j.arr.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Blackstone B.N., Wilgus T., Roy S., Wulff B., Powell H.M. Skin Biomechanics and miRNA expression Following.Chronic UV-B Irradiation. Adv. Wound Care. 2020;9:79–89. doi: 10.1089/wound.2019.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang B., Du R., Xiao X., Deng Z.L., Jian D., Xie H.F., Li J. Microrna-217 modulates human skin fibroblast senescence by directly targeting DNA methyltransferase 1. Oncotarget. 2017;8:33475. doi: 10.18632/oncotarget.16509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Röck K., Tigges J., Sass S., Schütze A., Florea A.-M., Fender A.C., Theis F.J., Krutmann J., Boege F., Fritsche E., et al. miR-23a-3p Causes Cellular Senescence by Targeting Hyaluronan Synthase 2: Possible Implication for Skin Aging. J. Investig. Dermatol. 2015;135:369–377. doi: 10.1038/jid.2014.422. [DOI] [PubMed] [Google Scholar]
- 46.Joo D., An S., Choi B.G., Kim K., Choi Y.M., Ahn K.J., An I.-S., Cha H.J. MicroRNA-378b regulates α-1-type 1 collagen expression via sirtuin 6 interference. Mol. Med. Rep. 2017;16:8520–8524. doi: 10.3892/mmr.2017.7657. [DOI] [PubMed] [Google Scholar]
- 47.Li T., Yan X., Jiang M., Xiang L. The comparison of microRNA profile of the dermis between the young and elderly. J. Dermatol. Sci. 2016;82:75–83. doi: 10.1016/j.jdermsci.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 48.Yoshinaga E., Kawada A., Ono K., Fujimoto E., Wachi H., Harumiya S., Nagai R., Tajima S. Nε-(carboxy- methyl) lysine modification of elastin alters its biological properties: Implications for the accumulation of abnormal elastic fibers in actinic elastosis. J. Investig. Dermatol. 2012;132:315–323. doi: 10.1038/jid.2011.298. [DOI] [PubMed] [Google Scholar]
- 49.Farrar M.D. Advanced glycation end products in skin ageing and photoageing: What are the implications for epidermal function. Exp. Dermatol. 2016;25:947–948. doi: 10.1111/exd.13076. [DOI] [PubMed] [Google Scholar]
- 50.Radjei S., Gareil M., Moreau M., Leblanc E., Schnebert S., Friguet B., Nizard C., Petropoulos I. The glyoxalase enzymes are differentially localized in epidermis and regulated during ageing and photoageing. Exp. Dermatol. 2016;25:492–494. doi: 10.1111/exd.12995. [DOI] [PubMed] [Google Scholar]
- 51.Handoko H.Y., Rodero M.P., Boyle G.M., Ferguson B., Engwerda C.R., Hill G., Muller H.K., Khosrotehrani K., Walker G.J. UV-B-Induced Melanocyte Proliferation in Neonatal Mice Driven by CCR2-Independent Recruitment of Ly6clowMHCIIhi Macrophages. J. Investig. Dermatol. 2013;133:1803–1812. doi: 10.1038/jid.2013.9. [DOI] [PubMed] [Google Scholar]
- 52.Zhuang Y., Lyga J. Inflammaging in skin and other tissues-the roles of complement system and macrophage. Inflamm. Allergy Drug Targets Former. Curr. Drug Targets Inflamm. Allergy. 2014;13:153–161. doi: 10.2174/1871528113666140522112003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Popkin B.M., D’Anci K.E., Rosenberg I.H. Water, hydration, and health. Nutr. Rev. 2010;68:439–458. doi: 10.1111/j.1753-4887.2010.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jéquier E., Constant F. Water as an essential nutrient: The physiological basis of hydration. Eur. J. Clin. Nutr. 2010;64:115. doi: 10.1038/ejcn.2009.111. [DOI] [PubMed] [Google Scholar]
- 55.Arnaud M.J., Noakes T.D. Should humans be encouraged to drink water to excess? Eur. J. Clin. Nutr. 2011;65:875. doi: 10.1038/ejcn.2011.40. [DOI] [PubMed] [Google Scholar]
- 56.Palma M.L., Monteiro C., Tavares L., Julia M., Rodrigues L.M. Relationship between the dietary intake of water and skin hydration. Biomed. Biopharm. Res. 2012;9:173–181. doi: 10.19277/BBR.9.2.39. [DOI] [Google Scholar]
- 57.Palma L., Marques L.T., Bujan J., Rodrigues L.M. Dietary water affects human skin hydration and biomechanics. Clin. Cosmet. Investig. Dermatol. 2015;8:413. doi: 10.2147/CCID.S86822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weidong Y., Jiesheng L., Xichun P. Chapter1, pp. 1–10. Trace Elements and Health. Huazhong University of Science and Technology Press; Wuhan, China: 2007. [Google Scholar]
- 59.Chen W., Zhou X., Zhu W. Trace Elements Homeostatic Imbalance in Psoriasis: A Meta-Analysis. Biol. Trace Elem. Res. 2019;191:313–322. doi: 10.1007/s12011-018-1626-1. [DOI] [PubMed] [Google Scholar]
- 60.Ogawa Y., Kawamura T., Shimada S. Zinc and skin biology. Arch. Biochem. Biophys. 2016;611:113–119. doi: 10.1016/j.abb.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 61.Ogawa Y., Kinoshita M., Shimada S., Kawamura T. Zinc and skin disorders. Nutrients. 2018;10:199. doi: 10.3390/nu10020199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bauer B.U., Rapp C., Mülling C.K., Meissner J., Vogel C., Humann-Ziehank E. Influence of dietary zinc on the claw and interdigital skin of sheep. J. Trace Elem. Med. Biol. 2018;50:368–376. doi: 10.1016/j.jtemb.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 63.Borkow G. Using copper to improve the well-being of the skin. Curr. Chem. Boil. 2014;8:89–102. doi: 10.2174/2212796809666150227223857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reelfs O., MEggleston I., Pourzand C. Skin protection against UV-A-induced iron damage by multiantioxidants and iron chelating drugs/prodrugs. Curr. Drug Metab. 2010;11:242–249. doi: 10.2174/138920010791196265. [DOI] [PubMed] [Google Scholar]
- 65.Pelle E., Jian J., Zhang Q., Muizzuddin N., Yang Q., Dai J., Maes D., Pernodet N., Yarosh D.B., Frenkel K., et al. Menopause increases the iron storage protein ferritin in skin. J. Cosmet. Sci. 2013;64:175–179. [PubMed] [Google Scholar]
- 66.Zhu X., Jiang M., Song E., Jiang X., Song Y. Selenium deficiency sensitizes the skin for UV-B-induced oxidative damage and inflammation which involved the activation of p38 MAPK signaling. Food Chem. Toxicol. 2015;75:139–145. doi: 10.1016/j.fct.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 67.Sengupta A., Lichti U.F., Carlson B.A., Ryscavage A.O., Gladyshev V.N., Yuspa S.H., Hatfield D.L. Selenoproteins are essential for proper keratinocyte function and skin development. PLoS ONE. 2010;5:e12249. doi: 10.1371/journal.pone.0012249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alqanatish J.T., Alqahtani F., Alsewairi W.M., Al-Kenaizan S. Childhood scurvy: An unusual cause of refusal to walk in a child. Pediatr. Rheumatol. 2015;13:23. doi: 10.1186/s12969-015-0020-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ellinger S., Stehle P. Efficacy of vitamin supplementation in situations with wound healing disorders: Results from clinical intervention studies. Curr. Opin. Clin. Nutr. Metab. Care. 2009;12:588–595. doi: 10.1097/MCO.0b013e328331a5b5. [DOI] [PubMed] [Google Scholar]
- 70.Evans J.R., Lawrenson J.G. Antioxidant vitamin and mineral supplements for slowing the progression of age-related macular degeneration. Cochrane Database Syst. Rev. 2017 doi: 10.1002/14651858.CD000254.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pasini E., Corsetti G., Aquilani R., Romano C., Picca A., Calvani R., Dioguardi F. Protein- amino acid metabolism disarrangements: The hidden enemy of chronic age-related conditions. Nutrients. 2018;10:391. doi: 10.3390/nu10040391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bellizzi V., Calella P., Carrero J.J., Fouque D. Very low-protein diet to postpone renal failure: Pathophysiology and clinical applications in chronic kidney disease. Chronic Dis. Transl. Med. 2018;4:45–50. doi: 10.1016/j.cdtm.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shams-White M.M., Chung M., Fu Z., Insogna K.L., Karlsen M.C., LeBoff M.S., Shapses S.A., Sackey J., Shi J., Wallace T.C., et al. Animal versus plant protein and adult bone health: A systematic review and meta-analysis from the National Osteoporosis Foundation. PLoS ONE. 2018;13:e0192459. doi: 10.1371/journal.pone.0192459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Strasser B., Volaklis K., Fuchs D., Burtscher M. Role of dietary protein and muscular fitness on longevity and aging. Aging Dis. 2018;9:119. doi: 10.14336/AD.2017.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hanjani N.A., Vafa M. Protein restriction, epigenetic diet, intermittent fasting as new approaches for preventing age-associated diseases. Int. J. Prev. Med. 2018;9:58. doi: 10.4103/ijpvm.IJPVM_397_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Haresaku S., Hanioka T., Tsutsui A., Watanabe T. Association of lip pigmentation with smoking and gingival melanin pigmentation. Oral Dis. 2007;13:71–76. doi: 10.1111/j.1601-0825.2006.01249.x. [DOI] [PubMed] [Google Scholar]
- 77.Sandby-Moller J., Poulsen T., Wulf H.C. Epidermal thickness at different body sites: Relationship to age, gender, pigmentation, blood content, skin type and smoking habits. Acta Derm. Venereol. 2003;83:410–413. doi: 10.1080/00015550310015419. [DOI] [PubMed] [Google Scholar]
- 78.Fatani A.Z., Alshamrani H.M., Alshehri K.A., Almaghrabi A.Y., Alzahrani Y.A., Abduljabbar M.H. Awareness on the association between skin aging and smoking: Impact on smoking quitting. Imam J. Appl. Sci. 2020;5:33. [Google Scholar]
- 79.Dupati A., Helfrich Y.R. Effect of cigarette smoking on skin aging. Expert Rev. Dermatol. 2014;4:371–378. doi: 10.1586/edm.09.33. [DOI] [Google Scholar]
- 80.Theocharidis V., Katsaros I., Sgouromallis E., Serifis N., Boikou V., Tasigiorgos S., Kokosis G., Economopoulos K. Current evidence on the role of smoking in plastic surgery elective procedures: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthetic Surg. 2018;71:624–636. doi: 10.1016/j.bjps.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 81.Farkas A., Kemény L., Széll M., Dobozy A. Ethanol and acetone stimulate the proliferation of Ha Ca T keratinocytes: The possible role of alcohol in exacerbating psoriasis. Arch. Dermatol. Res. 2003;295:56–62. doi: 10.1007/s00403-003-0399-2. [DOI] [PubMed] [Google Scholar]
- 82.Park H., Kim K. Association of alcohol consumption with lipid profile in hypertensive men. Alcohol Alcohol. 2012;47:282–287. doi: 10.1093/alcalc/ags019. [DOI] [PubMed] [Google Scholar]
- 83.Goodman G.D., Kaufman J., Day D., Weiss R., Kawata A.K., Garcia J.K., Santangelo S., Gallagher C.J. Impact of Smoking and Alcohol Use on Facial Aging in Women: Results of a Large Multinational, Multiracial, Cross-sectional Survey. J. Clin. Aesthet. Dermatol. 2019;12:28–39. [PMC free article] [PubMed] [Google Scholar]
- 84.Kuprys P.V., Tsukamoto H., Gao B., Jia L., McGowan J., Coopersmith C.M., Moreno M.C., Hulsebus H., Meena A.S., Souza-Smith F.M., et al. Summary of the 2018 Alcohol and Immunology Research Interest Group (AIRIG) meeting. Alcohol. 2019;77:11–18. doi: 10.1016/j.alcohol.2018.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gandini S., Masala G., Palli D., Cavicchi B., Saieva C., Ermini I., Baldini F., Gnagnarella P., Caini S. Alcohol, alcoholic beverages, and melanoma risk: A systematic literature review and dose–response meta-analysis. Eur. J. Nutr. 2018;57:2323–2332. doi: 10.1007/s00394-018-1613-5. [DOI] [PubMed] [Google Scholar]
- 86.Meksiarun P., Maeda Y., Hiroi T., Andriana B.B., Sato H. Analysis of the effects of dietary fat on body and skin lipids of hamsters by Raman spectroscopy. Analyst. 2015;140:4238–4244. doi: 10.1039/C5AN00076A. [DOI] [PubMed] [Google Scholar]
- 87.Rosa D.F., Sarandy M.M., Novaes R.D., Freitas M.B., do Carmo Gouveia Pelúzio M., Gonçalves R.V. High-fat diet and alcohol intake promotes inflammation and impairs skin wound healing in Wistar rats. Mediat. Inflamm. 2018;2018:4658583. doi: 10.1155/2018/4658583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rosa D.F., Sarandy M.M., Novaes R.D., da Matta S.L.P., Goncalves R.V. Effect of a high-fat diet and alcohol on cutaneous repair: A systematic review of murine experimental models. PLoS ONE. 2017;12:e0176240. doi: 10.1371/journal.pone.0176240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Vaid M., Singh T., Prasad R., Katiyar S.K. Intake of high-fat diet stimulates the risk of ultraviolet radiation-induced skin tumors and malignant progression of papillomas to carcinoma in skh-1 hairless mice. Toxicol. Appl. Pharmacol. 2014;274:147–155. doi: 10.1016/j.taap.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 90.Herbert D., Franz S., Popkova Y., Anderegg U., Schiller J., Schwede K., Lorz A., Simon J.C., Saalbach A. High-Fat Diet Exacerbates Early Psoriatic Skin Inflammation Independent of Obesity: Saturated Fatty Acids as Key Players. J. Investig. Dermatol. 2018;138:1999–2009. doi: 10.1016/j.jid.2018.03.1522. [DOI] [PubMed] [Google Scholar]
- 91.Higashi Y., Yamakuchi M., Fukushige T., Ibusuki A., Hashiguchi T., Kanekura T. High-fat diet exacerbates imiquimod-induced psoriasis-like dermatitis in mice. Exp. Dermatol. 2018;27:178–184. doi: 10.1111/exd.13484. [DOI] [PubMed] [Google Scholar]
- 92.Zhang Y., Li Q., Rao E., Sun Y., Grossmann M.E., Morris R.J., Cleary M.P., Li B. Epidermal fatty acid binding protein promotes skin inflammation induced by high-fat diet. Immunity. 2015;42:953–964. doi: 10.1016/j.immuni.2015.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nguyen H.P., Katta R. Sugar sag: Glycation and the role of diet in aging skin. Skin Ther. Lett. 2015;20:1–5. [PubMed] [Google Scholar]
- 94.Draelos Z.D. Aging skin: The role of diet: Facts and controversies. Clin. Dermatol. 2013;31:701–706. doi: 10.1016/j.clindermatol.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 95.Danby F.W. Nutrition and aging skin: Sugar and glycation. Clin. Dermatol. 2010;28:409–411. doi: 10.1016/j.clindermatol.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 96.Wu Q., Shuang E., Yamamoto K., Tsuduki T. Carbohydrate-restricted diet promotes skin senescence in senescence-accelerated prone mice. Biogerontology. 2019;20:71–82. doi: 10.1007/s10522-018-9777-1. [DOI] [PubMed] [Google Scholar]
- 97.Fuchs E., Green H. Regulation of terminal differentiation of cultured human keratinocytes by vitamin A. Cell. 1981;25:617–625. doi: 10.1016/0092-8674(81)90169-0. [DOI] [PubMed] [Google Scholar]
- 98.Fisher G.J., Talwar H.S., Lin J., Voorhees J.J. Molecular mechanisms of photoaging in human skin in vivo and their prevention by all-trans retinoic acid. Photochem. Photobiol. 1999;69:154–157. doi: 10.1111/j.1751-1097.1999.tb03268.x. [DOI] [PubMed] [Google Scholar]
- 99.Brescoll J., Daveluy S. A review of vitamin B12 in dermatology. Am. J. Clin. Dermatol. 2015;16:27–33. doi: 10.1007/s40257-014-0107-3. [DOI] [PubMed] [Google Scholar]
- 100.Pullar J.M., Carr A.C., Vissers M. The roles of vitamin C in skin health. Nutrients. 2017;9:866. doi: 10.3390/nu9080866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gordon-Thomson C., Tongkao-on W., Song E.J., Carter S.E., Dixon K.M., Mason R.S. Sunlight, Vitamin D and Skin Cancer. Volume 17. Springer; New York, NY, USA: 2014. Protection from ultraviolet damage and photocarcinogenesis by vitamin D compounds; pp. 303–328. [DOI] [PubMed] [Google Scholar]
- 102.Wu Y., Zheng X., Xu X.-G., Li Y.-H., Wang B., Gao X., Chen H., Yatskayer M., Oresajo C. Protective effects of a topical antioxidant complex containing vitamins C and E and ferulic acid against ultraviolet irradiation-induced photodamage in Chinese women. J. Drugs Dermatol. JDD. 2013;12:464–468. [PubMed] [Google Scholar]
- 103.Schempp C.M., Meinke M.C., Lademann J., Ferrari Y., Brecht T., Gehring W. Topical antioxidants protect the skin from chemical-induced irritation in the repetitive washing test: A placebo-controlled, double-blind study. Contact Dermat. 2012;67:234–237. doi: 10.1111/j.1600-0536.2012.02114.x. [DOI] [PubMed] [Google Scholar]
- 104.Balić A., Vlašić D., Žužul K., Marinović B., Bukvić Mokos Z. Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases. Int. J. Mol. Sci. 2020;21:741. doi: 10.3390/ijms21030741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Callaghan T.M., Wilhelm K.P. A review of ageing and an examination of clinical methods in the assessment of ageing skin. Part I: Cellular and molecular perspectives of skin ageing. Int. J. Cosmet. Sci. 2008;30:313–322. doi: 10.1111/j.1468-2494.2008.00454.x. [DOI] [PubMed] [Google Scholar]
- 106.Ratnam D.V., Ankola D.D., Bhardwaj V., Sahana D.K., Kumar M.R. Role of antioxidants in prophylaxis and therapy: A pharmaceutical perspective. J. Control. Release. 2006;113:189–207. doi: 10.1016/j.jconrel.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 107.Kandola K., Bowman A., Birch-Machin M.A. Oxidative stress-a key emerging impact factor in health, ageing, lifestyle and aesthetics. Int. J. Cosmet. Sci. 2015;37:1–8. doi: 10.1111/ics.12287. [DOI] [PubMed] [Google Scholar]
- 108.Nagai T., Suzuki N. Isolation of collagen from fish waste material-skin, bone and fins. Food Chem. 2000;68:277–281. doi: 10.1016/S0308-8146(99)00188-0. [DOI] [Google Scholar]
- 109.Wang L., Wang Q., Qian J., Liang Q., Wang Z., Xu J., He S., Ma H. Bioavailability and Bioavailable Forms of Collagen after Oral Administration to Rats. J. Agric. Food Chem. 2015;63:3752–3756. doi: 10.1021/jf5057502. [DOI] [PubMed] [Google Scholar]
- 110.Xu D., Li D., Zhao Z., Wu J., Zhao M. Regulation by walnut protein hydrolysate on the components and structural degradation of photoaged skin in SD rats. Food Funct. 2019;10:6792–6802. doi: 10.1039/C8FO01833B. [DOI] [PubMed] [Google Scholar]
- 111.Davinelli S., Bertoglio J.C., Polimeni A., Scapagnini G. Cytoprotective polyphenols against chronological skin aging and cutaneous photodamage. Curr. Pharm. Des. 2018;24:99–105. doi: 10.2174/1381612823666171109102426. [DOI] [PubMed] [Google Scholar]
- 112.Chuang S.Y., Lin Y.K., Lin C.F., Wang P.W., Chen E.L., Fang J.Y. Elucidating the skin delivery of aglycone and glycoside flavonoids: How the structures affect cutaneous absorption. Nutrients. 2017;9:1304. doi: 10.3390/nu9121304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Korkina L., De Luca C., Pastore S. Plant polyphenols and human skin: Friends or foes. Ann. N. Y. Acad. Sci. 2012;1259:77–86. doi: 10.1111/j.1749-6632.2012.06510.x. [DOI] [PubMed] [Google Scholar]
- 114.Masaki H. Role of antioxidants in the skin: Anti-aging effects. J. Dermatol. Sci. 2010;58:85–90. doi: 10.1016/j.jdermsci.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 115.He W., Yuan Z., He X. Research progress on pharmacological effects of astragalus polysaccharides. Chin. J. Biochem. Med. 2012;5:692–694. [Google Scholar]
- 116.Wen L., Gao Q., Ma C.-W., Ge Y., You L., Liu R.H., Fu X., Liu N. Effect of polysaccharides from Tremella fuciformis on UV-induced photoaging. J. Funct. Foods. 2016;20:400–410. doi: 10.1016/j.jff.2015.11.014. [DOI] [Google Scholar]
- 117.Wang L., Lee W., Oh J.Y., Cui Y.R., Ryu B., Jeon Y.J. Protective effect of sulfated polysaccharides from celluclast-assisted extract of Hizikia fusiforme against ultraviolet B-Induced skin damage by regulating NF-κB, AP-1, and MAPKs signaling pathways in vitro in human dermal fibroblasts. Mar. Drugs. 2018;16:239. doi: 10.3390/md16070239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Li H., Li Z., Peng L., Jiang N., Liu Q., Zhang E., Liang B., Li R., Zhu H. Lycium barbarum polysaccharide protects human keratinocytes against UV-B-induced photo-damage. Free Radic. Res. 2017;51:200–210. doi: 10.1080/10715762.2017.1294755. [DOI] [PubMed] [Google Scholar]
- 119.Zeng Q., Zhou F., Lei L., Chen J., Lu J., Zhou J., Cao K., Gao L., Xia F., Ding S., et al. Ganoderma lucidum polysaccharides protect fibroblasts against UV-B-induced photoaging. Mol. Med. Rep. 2016;15:111–116. doi: 10.3892/mmr.2016.6026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ye Y., Ji D., You L., Zhou L., Zhao Z., Brennan C. Structural properties and protective effect of Sargassum fusiforme polysaccharides against ultraviolet B radiation in hairless Kun Ming mice. J. Funct. Foods. 2018;43:8–16. doi: 10.1016/j.jff.2018.01.025. [DOI] [Google Scholar]
- 121.Pan W.-J., Ding Q.-Y., Wang Y., Wang D.-D., Lu Y., Yang W.-W., Cai Z.-N., Cheng X.-D., Zhang W.-N., Chen Y. A bioactive polysaccharide TLH-3 isolated from Tricholoma lobayense protects against oxidative stress-induced premature senescence in cells and mice. J. Funct. Foods. 2018;42:159–170. doi: 10.1016/j.jff.2017.12.070. [DOI] [Google Scholar]
- 122.Suganuma K., Shiobara M., Sato Y., Nakanuma C., Maekawa T., Ohtsuki M., Yazawa K., Imokawa G. Anti-aging and functional improvement effects for the skin by functional foods intakes: Clinical effects on skin by oral ingestion of preparations containing Astaxanthin and Vitamins C and E. Jichi Med. Univ. J. 2012;35:25–33. [Google Scholar]
- 123.Pappas A., Fantasia J., Chen T. Age and ethnic variations in sebaceous lipids. Derm. Endocrinol. 2013;5:319–324. doi: 10.4161/derm.25366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Horrobin D.F. Essential fatty acids in clinical dermatology. J. Am. Acad. Dermatol. 1989;20:1045–1053. doi: 10.1016/S0190-9622(89)70130-4. [DOI] [PubMed] [Google Scholar]
- 125.Romana-Souza B., Monte-Alto-Costa A. Olive oil reduces chronic psychological stress-induced skin aging in mice through the NF-κB and NRF2 pathways. J. Funct. Foods. 2019;54:310–319. doi: 10.1016/j.jff.2019.01.036. [DOI] [Google Scholar]
- 126.Park K.H., Kim J., Jung S., Sung K.H., Son Y.K., Bae J.M., Kim B.H. Alleviation of ultraviolet B-induced photoaging by 7-MEGATM 500 in hairless mouse skin. Toxicol. Res. 2019;35:353. doi: 10.5487/TR.2019.35.4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Song I.B., Gu H., Han H.J., Lee N.Y., Cha J.Y., Son Y.K., Kwon J. Effects of 7-MEGA? 500 on oxidative stress, inflammation, and skin regeneration in H2O2-treated skin cells. Toxicol. Res. 2018;34:103–110. doi: 10.5487/TR.2018.34.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Balkrishna A., Nain P., Chauhan A., Sharma N., Gupta A., Ranjan R., Varshney A. Super Critical Fluid Extracted Fatty Acids from Withania somnifera Seeds Repair Psoriasis-Like Skin Lesions and Attenuate Pro-Inflammatory Cytokines (TNF-α and IL-6) Release. Biomolecules. 2020;10:185. doi: 10.3390/biom10020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hyun Y.J., Piao M.J., Kang K.A., Zhen A.X., Fernando P.D.S.M., Kang H.K., Ahn Y.S., Hyun J.W. Effect of Fermented Fish Oil on Fine Particulate Matter-Induced Skin Aging. Mar. Drugs. 2019;17:61. doi: 10.3390/md17010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wang X., Wu J. Modulating effect of fatty acids and sterols on skin aging. J. Funct. Foods. 2019;57:135–140. doi: 10.1016/j.jff.2019.04.011. [DOI] [Google Scholar]
- 131.Tsuji R., Komano Y., Ohshio K., Ishii N., Kanauchi O. Long-term administration of pDC stimulative lactic acid bacteria, Lactococcus lactis strain Plasma, prevents immune-senescence and decelerates individual senescence. Exp. Gerontol. 2018;111:10–16. doi: 10.1016/j.exger.2018.06.028. [DOI] [PubMed] [Google Scholar]
- 132.Shin D., Lee Y., Huang Y.H., Lim H.W., Jang K., Kim D.D., Lim C.J. Probiotic fermentation augments the skin anti-photoaging properties of Agastache rugosa through up-regulating antioxidant components in UV-B-irradiated HaCaT keratinocytes. BMC Complement. Altern. Med. 2018;18:196. doi: 10.1186/s12906-018-2194-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang L., Zheng Y., Cheng X., Meng M., Luo Y., Li B. The anti-photoaging effect of antioxidant collagen peptides from silver carp (Hypophthalmichthys molitrix) skin is preferable to tea polyphenols and casein peptides. Food Funct. 2017;8:1698–1707. doi: 10.1039/C6FO01499B. [DOI] [PubMed] [Google Scholar]
- 134.Chen T., Hou H., Lu J., Zhang K., Li B. Protective effect of gelatin and gelatin hydrolysate from salmon skin on UV irradiation- induced photoaging of mice skin. J. Ocean Univ. China. 2016;15:711–718. doi: 10.1007/s11802-016-2953-5. [DOI] [Google Scholar]
- 135.Kang M.C., Yumnam S., Kim S.Y. Oral intake of collagen peptide attenuates ultraviolet B irradiation- induced skin dehydration in vivo by regulating hyaluronic acid synthesis. Int. J. Mol. Sci. 2018;19:3551. doi: 10.3390/ijms19113551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zague V., do Amaral J.B., Rezende Teixeira P., de Oliveira Niero E.L., Lauand C., Machado-Santelli G.M. Collagen peptides modulate the metabolism of extracellular matrix by human dermal fibroblasts derived from sun-protected and sun-exposed body sites. Cell Biol. Int. 2018;42:95–104. doi: 10.1002/cbin.10872. [DOI] [PubMed] [Google Scholar]
- 137.Kim D.U., Chung H.C., Choi J., Sakai Y., Lee B.Y. Oral intake of low-molecular-weight collagen peptide improves hydration, elasticity, and wrinkling in human skin: A randomized, double-blind, placebo- controlled study. Nutrients. 2018;10:826. doi: 10.3390/nu10070826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wang L., Jiang Y., Wang X., Zhou J., Cui H., Xu W., He Y., Ma H., Gao R. Effect of oral administration of collagen hydrolysates from Nile tilapia on the chronologically aged skin. J. Funct. Foods. 2018;44:112–117. doi: 10.1016/j.jff.2018.03.005. [DOI] [Google Scholar]
- 139.Liu Y., Su G., Zhou F., Zhang J., Zheng L., Zhao M. Protective effect of bovine elastin peptides against photoaging in mice and identification of novel antiphotoaging peptides. J. Agric. Food Chem. 2018;66:10760–10768. doi: 10.1021/acs.jafc.8b04676. [DOI] [PubMed] [Google Scholar]
- 140.Song H., Zhang L., Luo Y., Zhang S., Li B. Effects of collagen peptides intake on skin ageing and platelet release in chronologically aged mice revealed by cytokine array analysis. J. Cell. Mol. Med. 2018;22:277–288. doi: 10.1111/jcmm.13317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Offengenden M., Chakrabarti S., Wu J. Chicken collagen hydrolysates differentially mediate anti- inflammatory activity and type I collagen synthesis on human dermal fibroblasts. Food Sci. Hum. Wellness. 2018;7:138–147. doi: 10.1016/j.fshw.2018.02.002. [DOI] [Google Scholar]
- 142.Wang X., Hong H., Wu J. Hen collagen hydrolysate alleviates UV-A-induced damage in human dermal fibroblasts. J. Funct. Foods. 2019;63:103574. doi: 10.1016/j.jff.2019.103574. [DOI] [Google Scholar]
- 143.Song H., Meng M., Cheng X., Li B., Wang C. The effect of collagen hydrolysates from silver carp (Hypophthalmichthys molitrix) skin on UV-induced photoaging in mice: Molecular weight affects skin repair. Food Funct. 2017;8:1538–1546. doi: 10.1039/C6FO01397J. [DOI] [PubMed] [Google Scholar]
- 144.Inoue N., Sugihara F., Wang X. Ingestion of bioactive collagen hydrolysates enhance facial skin moisture and elasticity and reduce facial ageing signs in a randomised double-blind placebo-controlled clinical study. J. Sci. Food Agric. 2016;96:4077–4081. doi: 10.1002/jsfa.7606. [DOI] [PubMed] [Google Scholar]
- 145.Benjakul S., Karnjanapratum S., Visessanguan W. Hydrolysed collagen from Lates calcarifer skin: Its acute toxicity and impact on cell proliferation and collagen production of fibroblasts. Int. J. Food Sci. Technol. 2018;53:1871–1879. doi: 10.1111/ijfs.13772. [DOI] [Google Scholar]
- 146.Lu J., Hou H., Fan Y., Yang T., Li B. Identification of MMP-1 inhibitory peptides from cod skin gelatin hydrolysates and the inhibition mechanism by MAPK signaling pathway. J. Funct. Foods. 2017;33:251–260. doi: 10.1016/j.jff.2017.03.049. [DOI] [Google Scholar]
- 147.Liu Z., Li Y., Song H., He J., Li G., Zheng Y., Li B. Collagen peptides promote photoaging skin cell repair by activating the TGF-β/Smad pathway and depressing collagen degradation. Food Funct. 2019;10:6121–6134. doi: 10.1039/C9FO00610A. [DOI] [PubMed] [Google Scholar]
- 148.Song H., Zhang S., Zhang L., Li B. Effect of orally administered collagen peptides from bovine bone on skin aging in chronologically aged mice. Nutrients. 2017;9:1209. doi: 10.3390/nu9111209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lee H.-J., Jang H.-L., Ahn D.-K., Kim H.-J., Jeon H.Y., Seo D.B., Lee J.-H., Choi J.K., Kang S.-S. Orally administered collagen peptide protects against UV-B-induced skin aging through the absorption of dipeptide forms, Gly-Pro and Pro-Hyp. Biosci. Biotechnol. Biochem. 2019;83:1146–1156. doi: 10.1080/09168451.2019.1580559. [DOI] [PubMed] [Google Scholar]
- 150.Wang L., Wang X., Bai F., Fang Y., Wang J., Gao R. The anti-skin-aging effect of oral administration of gelatin from the swim bladder of Amur sturgeon (Acipenser schrenckii) Food Funct. 2019;10:3890–3897. doi: 10.1039/C9FO00661C. [DOI] [PubMed] [Google Scholar]
- 151.Liu S., You L., Zhao Y., Chang X. Hawthorn polyphenol extract inhibits UV-B-induced skin photoaging by regulating MMP expression and type I procollagen production in mice. J. Agric. Food Chem. 2018;66:8537–8546. doi: 10.1021/acs.jafc.8b02785. [DOI] [PubMed] [Google Scholar]
- 152.Liu S., Sui Q., Zou J., Zhao Y., Chang X. Protective effects of hawthorn (Crataegus pinnatifida) polyphenol extract against UV-B-induced skin damage by modulating the p53 mitochondrial pathway in vitro and in vivo. J. Food Biochem. 2019;43:e12708. doi: 10.1111/jfbc.12708. [DOI] [PubMed] [Google Scholar]
- 153.Nobile V., Michelotti A., Cestone E., Caturla N., Castillo J., Benavente-García O., Pérez-Sánchez A., Micol V. Skin photoprotective and antiageing effects of a combination of rosemary (Rosmarinus officinalis) and grapefruit (Citrus paradisi) polyphenols. Food Nutr. Res. 2016;60:31871. doi: 10.3402/fnr.v60.31871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kwon K.R., Alam M.B., Park J.H., Kim T.H., Lee S.H. Attenuation of UV-B-induced photo-aging by polyphenolic-rich Spatholobus Suberectus stem extract via modulation of MAPK/AP-1/MMPs signaling in human keratinocytes. Nutrients. 2019;11:1341. doi: 10.3390/nu11061341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Xiao J., Liu B., Zhuang Y. Effects of rambutan (Nephelium lappaceum) peel phenolics and Leu-Ser-Gly-Tyr-Gly-Pro on hairless mice skin photoaging induced by ultraviolet irradiation. Food Chem. Toxicol. 2019;129:30–37. doi: 10.1016/j.fct.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 156.Cheon H.I., Bae S., Ahn K.J. Flavonoid Silibinin Increases Hair-Inductive Property Via Akt and Wnt/β-Catenin Signaling Activation in 3-Dimensional-Spheroid Cultured Human Dermal Papilla Cells. J. Microbiol. Biotechnol. 2019;29:321–329. doi: 10.4014/jmb.1810.10050. [DOI] [PubMed] [Google Scholar]
- 157.Kim H.I., Jeong Y.U., Kim J.H., Park Y.J. 3, 5, 6, 7, 8, 3′, 4′-Heptamethoxyflavone, a citrus flavonoid, inhibits collagenase activity and induces type I procollagen synthesis in HDFn cells. Int. J. Mol. Sci. 2018;19:620. doi: 10.3390/ijms19020620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Noh D., Choi J.G., Huh E., Oh M.S. Tectorigenin, a Flavonoid-Based Compound of Leopard Lily Rhizome, Attenuates UV-B-Induced Apoptosis and Collagen Degradation by Inhibiting Oxidative Stress in Human Keratinocytes. Nutrients. 2018;10:1998. doi: 10.3390/nu10121998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Zhang M., Dang L., Guo F., Wang X., Zhao W., Zhao R. Coenzyme Q10 enhances dermal elastin expression, inhibits IL-1α production and melanin synthesis in vitro. Int. J. Cosmet. Sci. 2012;34:273–279. doi: 10.1111/j.1468-2494.2012.00713.x. [DOI] [PubMed] [Google Scholar]
- 160.Ahmadi Ashtiani H.R., Rastegar H., Salarian A.A., Rahmani F., Rezazadeh S., Sedghi Zadeh H. Study the Effect of Silymarin and Vitamin C in Skin Aging Induced by UV-B Rays on the Mice Skin Redox System. J. Med. Plants. 2019;3:130–144. [Google Scholar]
- 161.Zhen A.X., Piao M.J., Kang K.A., Fernando P.D.S.M., Kang H.K., Koh Y.S., Yi J.M., Hyun J.W. Niacinamide Protects Skin Cells from Oxidative Stress Induced by Particulate Matter. Biomol. Ther. 2019;27:562–569. doi: 10.4062/biomolther.2019.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Tiwari P., Nagatake T., Hirata S.-I., Sawane K., Saika A., Shibata Y., Morimoto S., Honda T., Adachi J., Abe Y., et al. Dietary coconut oil ameliorates skin contact hypersensitivity through mead acid production in mice. Allergy. 2019;74:1522–1532. doi: 10.1111/all.13762. [DOI] [PubMed] [Google Scholar]