Abstract
IMPORTANCE
US life expectancy has not kept pace with that of other wealthy countries and is now decreasing.
OBJECTIVE
To examine vital statistics and review the history of changes in US life expectancy and increasing mortality rates; and to identify potential contributing factors, drawing insights from current literature and from a new analysis of state-level trends.
EVIDENCE
Life expectancy data for 1959–2016 and cause-specific mortality rates for 1999–2017 were obtained from the US Mortality Database and CDC WONDER, respectively. The analysis focused on midlife deaths (ages 25–64 years), stratified by sex, race-ethnicity, socioeconomic status, and geography (including the 50 states). Published research from January 1990 through August 2019 that examined relevant mortality trends and potential contributory factors was examined.
FINDINGS
Between 1959 and 2016, US life expectancy increased from 69.9 years to 78.9 years but declined for 3 consecutive years after 2014. The recent decrease in US life expectancy culminates a period of increasing cause-specific mortality among adults ages 25–64 years that began in the 1990s, ultimately producing an increase in all-cause mortality that began in 2010. During 2010–2017, midlife all-cause mortality rates increased from 328.5 deaths/100,000 to 348.2 deaths/100,000. By 2014, midlife mortality was increasing across all racial groups, caused by drug overdoses, alcohol abuse, suicides, and a diverse list of organ system diseases. The largest relative increases in midlife mortality rates occurred in New England (New Hampshire, 23.3%; Maine, 20.7%; Vermont, 19.9%) and the Ohio Valley (West Virginia, 23.0%; Ohio, 21.6%; Indiana, 14.8%; Kentucky, 14.7%). The increase in midlife mortality during 2010–2017 was associated with an estimated 33,307 excess US deaths, 32.8% of which occurred in four Ohio Valley states.
CONCLUSIONS
US life expectancy increased for most of the past 60 years, but the rate of increase slowed over time and life expectancy decreased after 2014. A major contributor has been an increase in mortality from specific causes (e.g., drug overdoses, suicides, organ system diseases) among young and middle-aged adults of all racial groups, which began as early as the 1990s and produced the largest relative increases in the Ohio Valley and New England. The implications for public health and the economy are substantial, making it vital to understand the root causes.
INTRODUCTION
Life expectancy at birth, a common measure of a population’s health,1 has decreased in the US for three consecutive years.2 This has attracted recent public attention,3 but the core problem is not new, and has been building since the 1980s.4,5 Although life expectancy in developed countries has increased for much of the past century, US life expectancy began to lose pace with other countries in the 1980s6,7 and, by 1998, had declined to a level below the average life expectancy among Organisation for Economic Cooperation and Development countries.8 While life expectancy in these countries has continued to increase,9,10 US life expectancy stopped increasing in 2010 and has been decreasing since 2014.2,11 Despite excessive spending on health care, vastly exceeding that of other countries,12 the US has a longstanding health disadvantage relative to other high-income countries that extends beyond life expectancy to include higher rates of disease and cause-specific mortality rates.6,7,10,13
This Special Communication has two aims: to examine vital statistics and review the history of changes in US life expectancy and increasing mortality rates; and to identify potential contributing factors, drawing insights from current literature and from a new analysis of state-level trends.
METHODS
DATA ANALYSIS
Measures
This report examines longitudinal trends in life expectancy at birth and mortality rates (deaths per 100,000) in the US population, with a focus on midlife, defined here as adults ages 25–64 years. This age range was chosen because the literature has reported increases in mortality rates among both young adults (as young as age 25 years) and middle-aged adults (up to age 64 years); midlife mortality is used as shorthand for both age groups combined (ages 25–64 years). Life expectancy at birth is an estimate of the number of years a newborn is predicted to live, based here on period life table calculations that assume a hypothetical cohort is subject throughout its lifetime to the prevailing age-specific death rates for that year.14 All-cause mortality and cause-specific mortality rates for key conditions were examined, using the International Classification of Disease (ICD-10)15 codes detailed in the online Supplement. Age-specific rates were examined for age groups of 10 years or less, whereas age-adjusted rates were examined for broader age groups. Age-adjustment rates were provided, and calculated, by the National Center for Health Statistics, using methods described elsewhere.16
Data sources
Life expectancy data were obtained from the National Center for Health Statistics17 and US Mortality Database.18 The latter was used for long-term trend analyses because it provided complete life tables for each year from 1959 to 2016 and at multiple geographic levels.19 The analysis examined two time periods. First, life expectancy was examined from a long-term perspective (from 1959 onward) to identify when life expectancy trajectories began to change in the US and the 50 states. Second, knowing from the literature that mortality rates for specific causes (e.g., drug overdoses) began increasing in the 1990s, a detailed analysis of cause-specific mortality trends was conducted for 1999–2017. Mortality rates were obtained from CDC WONDER.20 Pre-1999 mortality data, although available, were not examined because the priority was to understand the conditions responsible for current mortality trends and because changes in coding in the transition from ICD-9 to ICD-1015 could introduce artefactual changes in mortality rates. Methods that are available to make these conversions were therefore not pursued.
Analytic methods
Life expectancy and mortality data were stratified by sex and across the five racial-ethnic groups used by the US Census Bureau21: non-Hispanic (NH) American Indians and Alaskan Natives (AIAN), NH Asians and Pacific Islanders (API), NH blacks (or African Americans), NH whites, and Hispanics. Mortality rates were stratified by geography, including rates for the nine US Census divisions (New England, Mid-Atlantic, East North Central, West North Central, South Atlantic, East South Central, West South Central, Mountain, and Pacific), the 50 states, and urban and rural counties as defined in the online Supplement. Data for the District of Columbia and US territories were not examined.
Changes in mortality rates between two years (two-point comparisons) were deemed significant based on 95% confidence intervals. Trends in life expectancy and mortality over time were examined to identify changes in slope and points of retrogression—a period of progress (increasing life expectancy or decreasing mortality) followed by stagnation (slope statistically equivalent to zero) or a significant reversal. Temporal trends were analyzed using the Joinpoint Regression Program,22 which models consecutive linear segments on a log scale, connected by joinpoints where the segments meet (i.e., years when slopes changed significantly). A modification of the program’s Bayesian Information Criteria method (called BIC323) was substituted for the Monte Carlo permutation tests to reduce computation time. Slopes (annual percent rate change [APC]) were calculated for the line segments linking joinpoints, and the weighted average of the APCs (the average annual percent change [AAPC]) was calculated for three time periods: 1959–2016, 2005–2016, and 2010–2016 for life expectancy and 1999–2017, 2005–2017, and 2010–2017 for mortality rates. Slopes were considered increasing or decreasing if the estimated slope differed significantly from zero. The statistical significance of the APCs and the change in APCs between consecutive segments was determined by two-sided t-testing (p ≤ 0.05). Specific model parameters are available in the online supplement.
Excess deaths attributed to the increase in midlife mortality during 2010–2017 were estimated by multiplying the population denominator for each year by the mortality rate of the previous year, repeating this for each year from 2011 to 2017, and summing the difference between expected and observed deaths.24,25,26 Excess deaths were estimated for each state and census division, allowing for estimates of their relative contribution to the national total.
LITERATURE REVIEW
To add context to the vital statistics described above and more fully characterize what is known about observed trends, the epidemiologic literature was examined for other research on US and state life expectancy and mortality trends. Using PubMed and other bibliographic databases, studies published between January 1990 and August 2019 that examined life expectancy or midlife mortality trends or that disaggregated data by age, sex, race-ethnicity, socioeconomic status, or geography were examined, along with the primary sources they cited. Research on the factors associated with the specific causes of death (e.g., drug overdoses, suicides) responsible for increasing midlife mortality was also reviewed. Research on the methodological limitations of epidemiological data on mortality trends was also examined.
To review contextual factors that may explain observed mortality trends and the US health disadvantage relative to other high-income countries, epidemiologic research was augmented by an examination of relevant literature in sociology, economics, political science, history, and journalism. A snowball technique27,28 was used to locate studies and reports on: (1) the history and timing of the opioid epidemic; (2) the contribution of modifiable risk factors (e.g., obesity) to mortality trends; (3) changes in the prevalence of psychological distress and mental illness; (4) the evidence linking economic conditions and health, (5) relevant economic history and trends in income and earnings, wealth inequality, and austerity during the observation period; (6) changes in subjective social status (e.g., financial precarity) and social capital; and (7) relevant Federal and state social and economic policies, including the role of geography (e.g., rural conditions) and state-level factors. The study was exempt from institutional review under 45 CFR 46.101(b)(4).
RESULTS
LIFE EXPECTANCY
Life expectancy values for 1959–2016 are provided online (Table e1) for the United States, nine census divisions, and 50 states. Between 1959 and 2016, US life expectancy increased by almost 10 years, from 69.9 years in 1959 to 78.9 years in 2016, with the fastest increase (highest APC) occurring during 1969–1979 (APC=0.48, p < 0.01) (Figure 1). Life expectancy began to advance more slowly in the 1980s and plateaued in 2011 (after which the APC differed non-significantly from zero). The NCHS reported that US life expectancy peaked (78.9 years) in 2014 and subsequently decreased significantly for three consecutive years, reaching 78.6 years in 2017.2,9 The decrease was greater among men (0.4 years) than women (0.2 years) and occurred across racial-ethnic groups; between 2014 and 2016, life expectancy decreased among non-Hispanic (NH) whites (from 78.8 to 78.5 years), NH blacks (from 75.3 years to 74.8 years), and Hispanics (82.1 to 81.8 years).17
Figure 1. US life expectancy, 1959–2016.
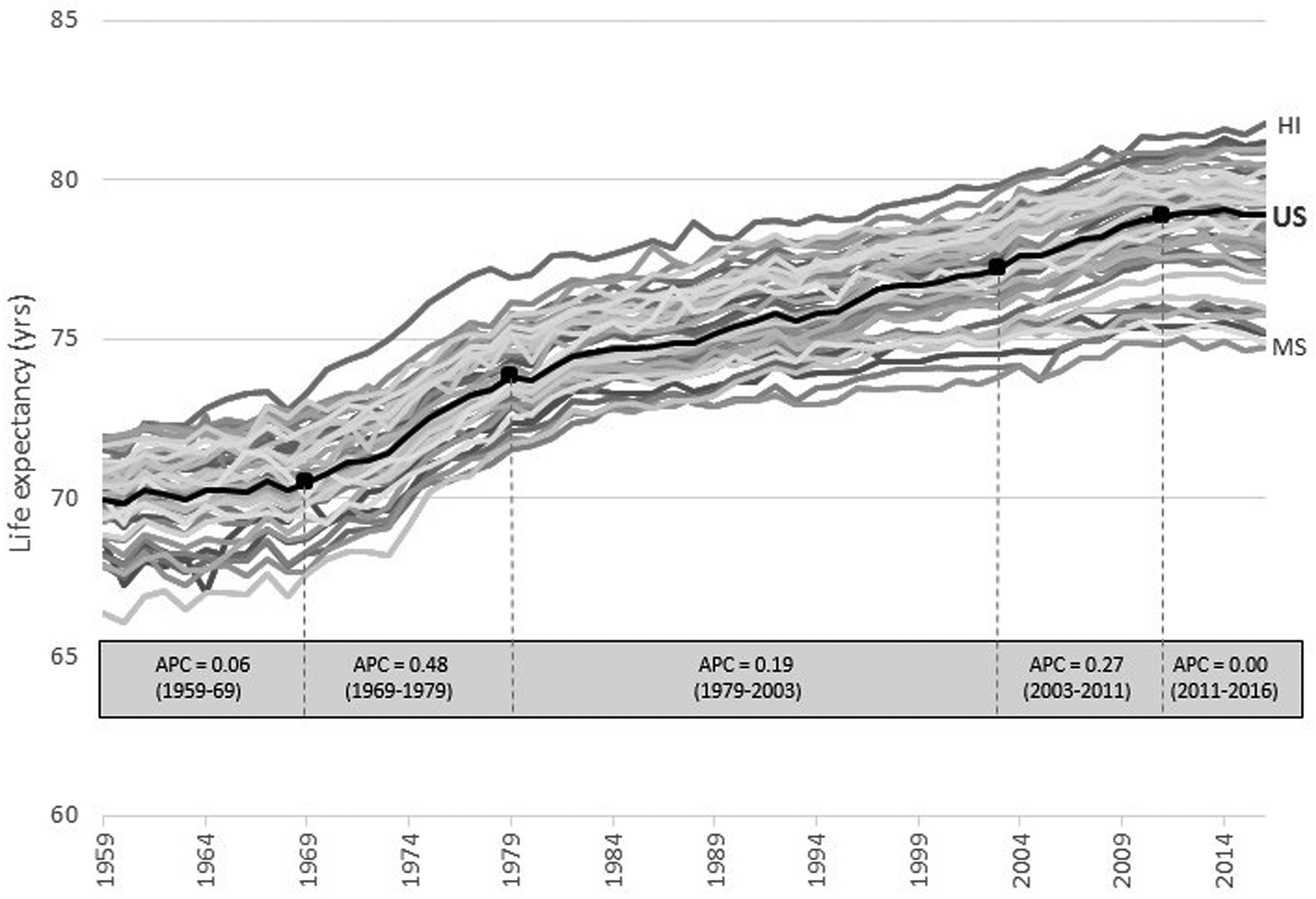
Black line depicts U.S. life expectancy; boldened data points
( ) denote joinpoint
years, when the linear trend (slope) changed significantly based on joinpoint
analysis. APC = average annual percent change for the five time periods
identified on joinpoint analysis (1959–1969, 1969–1979,
1979–2003, 2003–2011, and 2011–2016). Grey lines depict
life expectancy for the 50 states. Life expectancy data obtained from the US
Mortality Database.
) denote joinpoint
years, when the linear trend (slope) changed significantly based on joinpoint
analysis. APC = average annual percent change for the five time periods
identified on joinpoint analysis (1959–1969, 1969–1979,
1979–2003, 2003–2011, and 2011–2016). Grey lines depict
life expectancy for the 50 states. Life expectancy data obtained from the US
Mortality Database.
ALL-CAUSE MORTALITY
The recent decrease in US life expectancy was largely related to increases in all-cause mortality among young and middle-aged adults. During 1999–2017, infant mortality decreased from 736.0 deaths/100,000 to 567.0 deaths/100,000, mortality rates among children and early adolescents (ages 1–14 years) decreased from 22.9 deaths/100,000 to 16.5 deaths/100,000 (Figure 2), and age-adjusted mortality rates among adults ages 65–84 years decreased from 3,774.6 deaths/100,000 to 2,875.4 deaths/100,000.20
Figure 2. Age-specific, all-cause mortality rates among US youth, ages 1–24 years, 1999–2017.
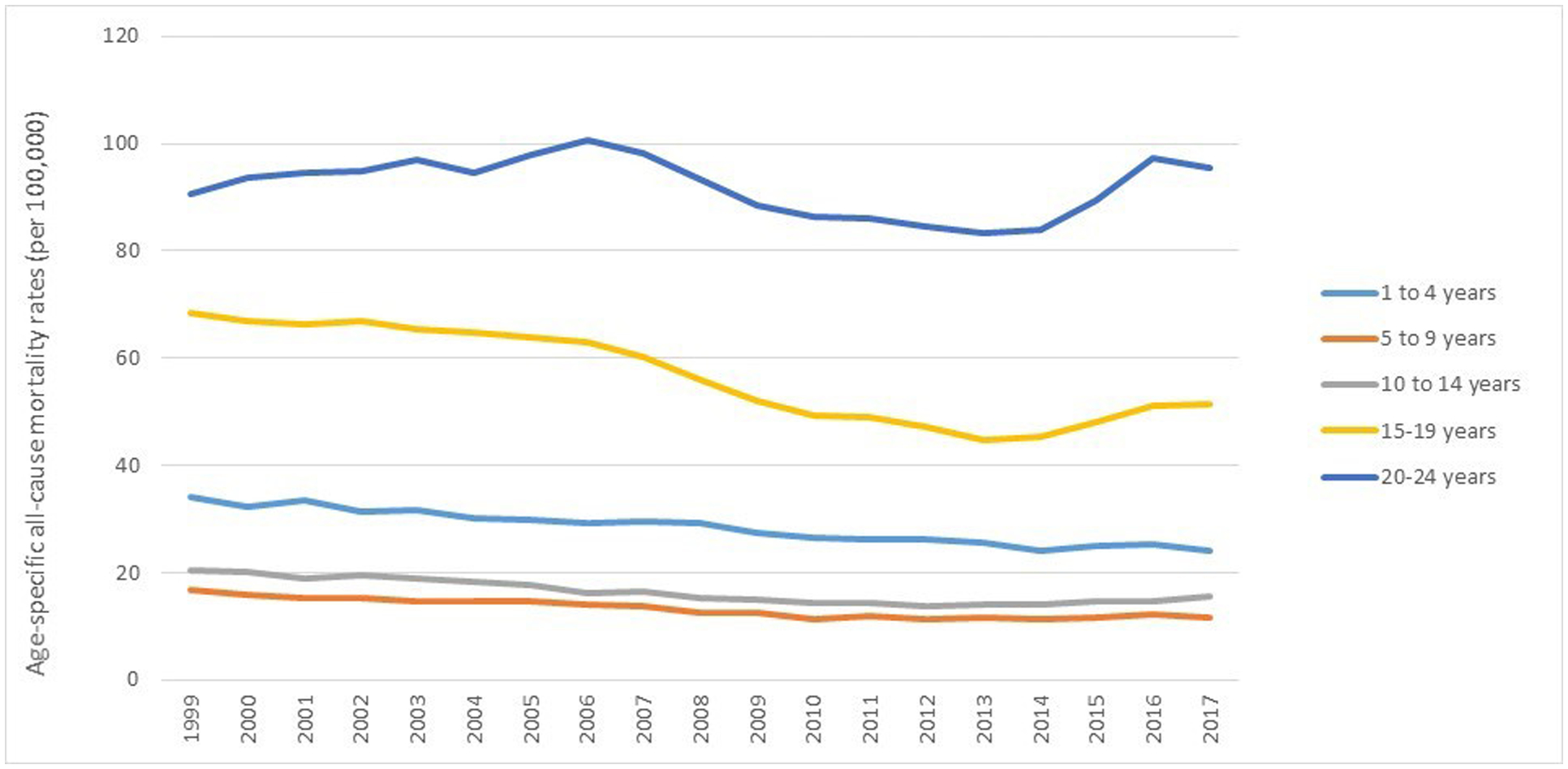
Source: CDC WONDER.
Table e2 presents age-specific, all-cause mortality rates for infants, children ages 1–4 years, and subsequent age deciles. Individuals ages 25–64 years (and even those ages 15–24 years) experienced retrogression: all-cause mortality rates were in decline in 2000, reached a nadir in 2010, and increased thereafter. The increase was greatest in midlife—among young and middle-aged adults (ages 25–64 years), whose age-adjusted all-cause mortality rates increased by 6.0% during 2010–2017 (from 328.5 deaths/100,000 to 348.2 deaths/100,000) (Figure 3). The increase in midlife mortality was greatest among younger adults (ages 25–34 years), whose age-specific rates increased by 29.0% during this period (from 102.9 deaths/100,000 to 132.8 deaths/100,000).20 Rising death rates among middle-aged adults (ages 45–64 years) were less related to mortality among those ages 45–54 years, which decreased (from 407.1 deaths/100,000 to 401.5 deaths per 100,000), than among those ages 55–64 years, whose age-specific rates increased during 2010–2017 (from 851.9 deaths/100,000 to 885.8 deaths/100,000).20
Figure 3. Age-adjusted, all-cause mortality rates, US adults ages 25–64 years, 25–44 years, and 45–64 years, 1999–2017.
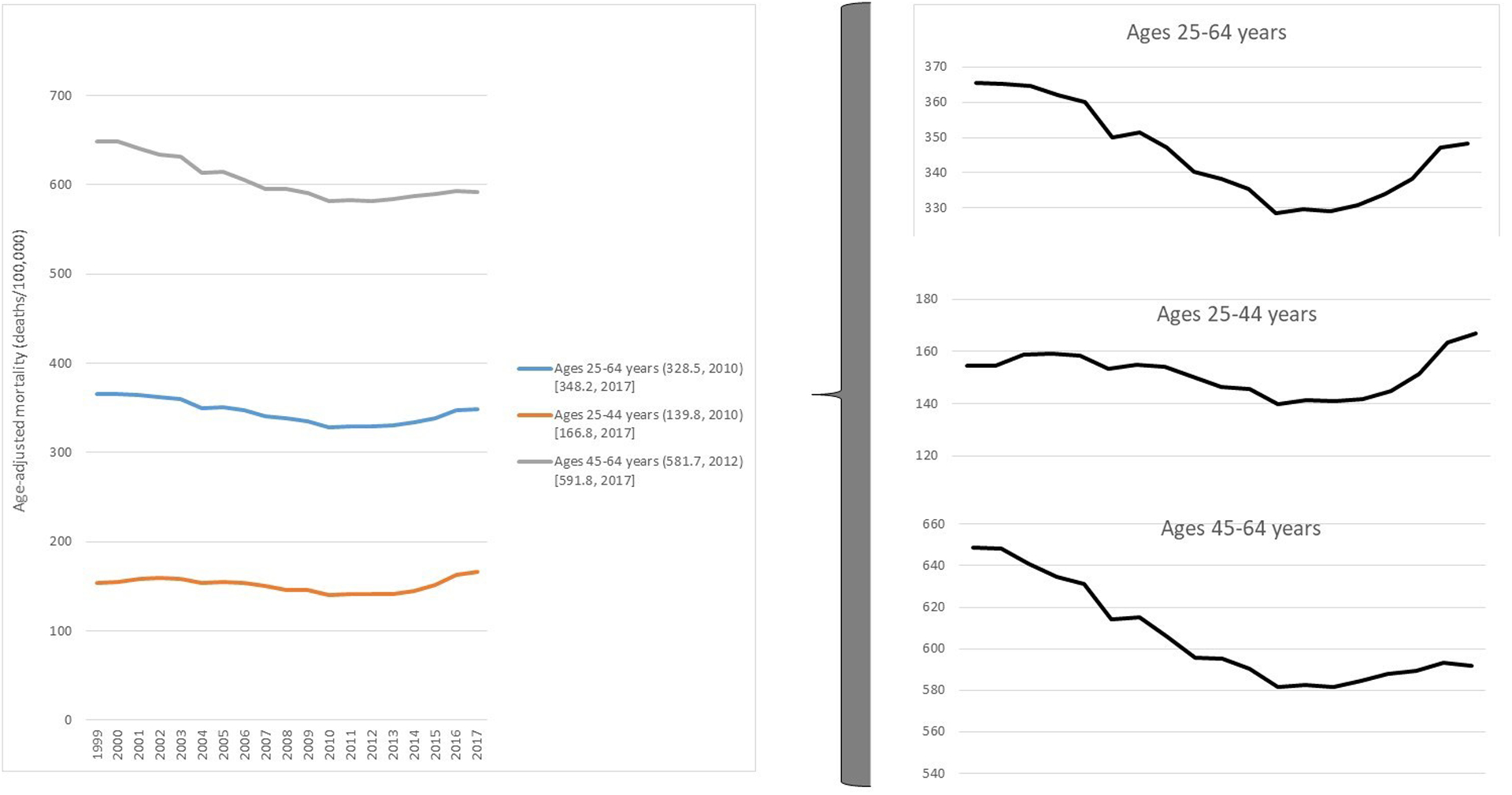
The lowest mortality rates per 100,000 (and corresponding years) are listed in parentheses; 2017 mortality rates are listed in brackets. Source: CDC WONDER.
CAUSE-SPECIFIC MORTALITY
Although all-cause mortality in midlife did not begin increasing in the US until 2010, midlife mortality rates for specific causes (e.g., drug overdoses, hypertensive diseases) began increasing earlier (Figure 4).29,30 Table e3 presents absolute and relative changes in age-specific mortality rates by cause of death between 1999 and 2017 (and between 2010 and 2017) for every age group (by age decile), from infancy onward. The table shows that mortality rates increased primarily in midlife for 35 causes of death. The increase in cause-specific mortality was not always restricted to midlife; younger and older populations were often affected, although typically not as greatly (in relative or absolute terms) as those ages 25–64 years.
Figure 4. Age-specific mortality rates for selected causes, by age decile, 1999–2017.
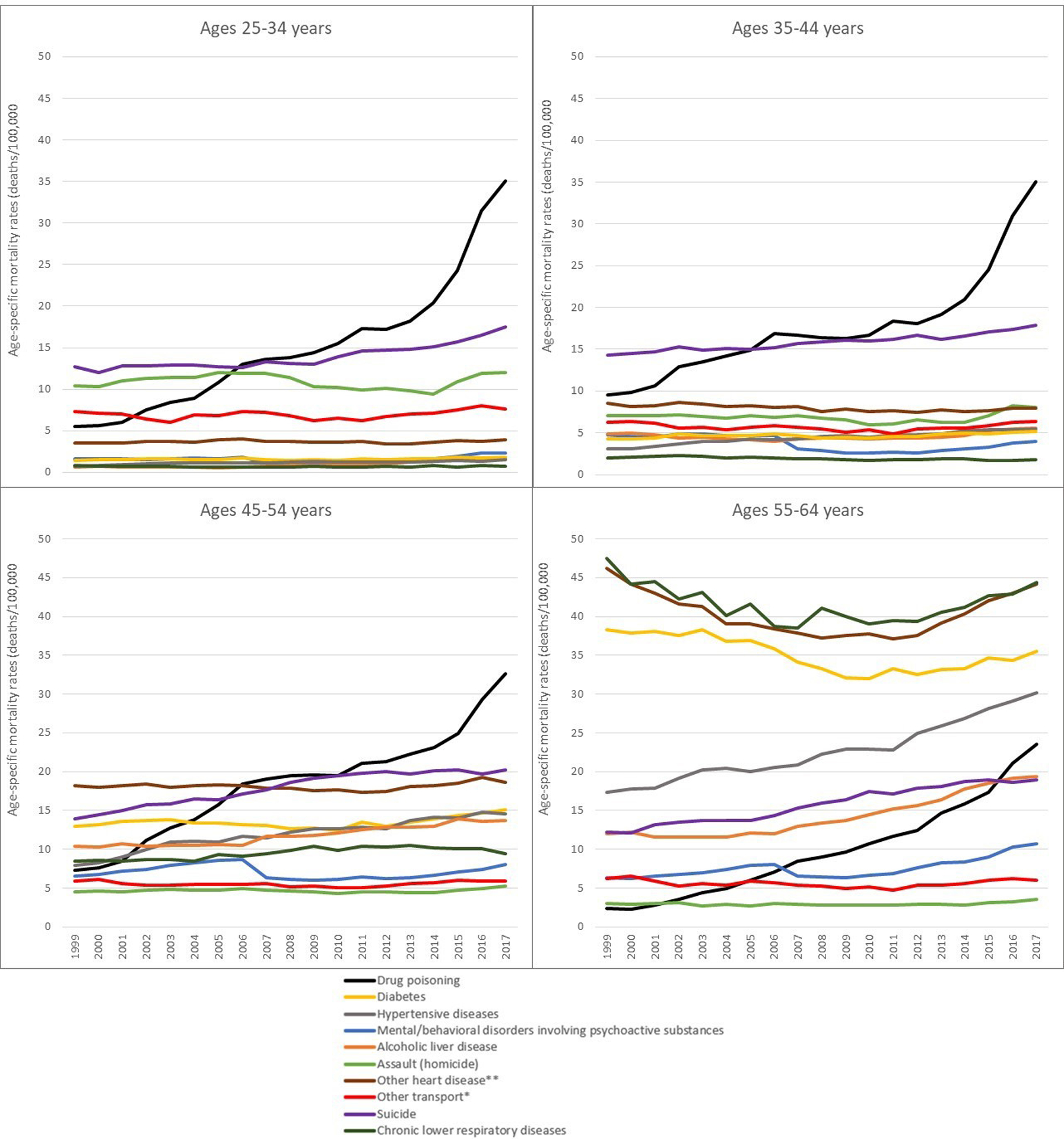
* Other transport accidents include land, water, air, space, and other transport accidents (V80-V99).
** Other heart disease (I30-I51) includes arrhythmias and heart failure.
Other causes of death (and corresponding ICD-10 codes) include diabetes mellitus (E10-E14), mental and behavioral disorders due to psychoactive substance use (F10-F19), hypertensive diseases (I10-I15), accidental drug poisoning (X40-X44), intentional self-harm (suicide) (X60-X84), and assault (homicide) (X85-Y09). Source: CDC WONDER.
Year-by-year midlife mortality rates by cause for 1999–2017 (Table e4) show that retrogression occurred across multiple causes of death, in which progress in lowering midlife mortality was reversed. From 1999 to 2009, these cause-specific increases were not reflected in all-cause mortality trends because they were offset by large, co-occurring reductions in mortality from ischemic heart disease, cancer, HIV infection, motor vehicle injuries, and other leading causes of death.31,32,33 However, increases in cause-specific mortality rates before 2010 slowed the rate at which all-cause mortality decreased (and life expectancy increased) and eventually culminated in a reversal. The end result was that all-cause mortality increased after 2010 (and life expectancy decreased after 2014).34,35
Drug overdoses, alcoholic liver disease, and suicides
A major cause of increasing midlife mortality was a large increase in fatal drug overdoses, beginning in the 1990s.28,33,36 Between 1999 and 2017, midlife mortality from drug overdoses increased by 386.5% (from 6.7 deaths/100,000 to 32.5 deaths/100,000).20 Age-specific rates increased for each age subgroup: rates for those ages 25–34 years, 35–44 years, and 45–54 years increased by 531.4% (from 5.6 deaths/100,000 to 35.1 deaths/100,000), 267.9% (from 9.5 deaths/100,000 to 35.0 deaths/100,000), and 350.9% (from 7.2 deaths/100,000 to 32.7 deaths/100,000), respectively. The largest relative increase in overdose deaths (909.2%, from 2.3 deaths/100,000 to 23.5 deaths/100,000) occurred among those ages 55–64 years.20 Midlife mortality rates also increased for chronic liver disease and cirrhosis;29,32,37,38 during 1999–2017, age-adjusted death rates for alcoholic liver disease increased by 40.6% (from 6.4 deaths/100,000 to 8.9 deaths/100,000); age-specific rates among young adults ages 25–34 years increased by 157.6% (from 0.6 deaths/100,000 to 1.7 deaths/100,000).20 The age-adjusted suicide rate at ages 25–64 years increased by 38.3% (from 13.4 deaths/100,000 to 18.6 deaths/100,000), and by 55.9% (from 12.2 deaths/100,000 to 19.0 deaths/100,000) among those ages 55–64 years.20 As others have reported39, suicide rates also increased among those younger than age 25 years. Table e3 shows that, across all age groups, the largest relative increase in suicide rates occurred among children ages 5–14 years (from 0.6 deaths/100,000 to 1.3 deaths/100,000).
Organ system diseases and injuries
The increase in deaths caused by drugs, alcohol, and suicides was accompanied by significant increases in midlife mortality from organ system diseases and injuries, some beginning in the 1990s.26,29,32 Data for several examples are provided online (Tables e3 and e4). For example, between 1999 and 2017, age-adjusted midlife mortality rates for hypertensive diseases and obesity increased by 78.9% (from 6.1 deaths/100,000 to 11.0 deaths/100,000) and 114.0% (from 1.3 deaths/100,000 to 2.7 deaths/100,000) (Table e4), respectively.20 The increase in mortality from hypertension is consistent with other reports.40 Early studies reported increasing midlife mortality from heart disease and lung (notably chronic pulmonary) disease, hypertension, stroke, diabetes, and Alzheimer disease,29,32,41 but the trend appears to be even broader. According to one study, the increase in midlife mortality among NH whites during 1999–2016 was associated with an estimated 41,303 excess deaths due to drug overdoses (N=33,003) and suicides (N=8,300) but also more than 30,000 excess deaths from organ system diseases (e.g., hypertensive diseases [N=5,318], alcoholic liver disease [N=3,901], infectious diseases [N=2,149], liver cancer [N=1,931]), mental and behavioral disorders, obesity, pregnancy, and injuries (e.g., pedestrian-vehicle accidents).26 Table e3 shows that the increase in organ disease mortality extended beyond midlife and, for certain diseases, was more pronounced in older age groups. For example, the largest increases in mortality from degenerative neurologic diseases (e.g., Alzheimer disease) occurred among those ages 75 and older.
Decomposition analyses, which quantify the relative contribution of specific causes of death to mortality patterns, have confirmed the large role played by organ system diseases.10,29,31 For example, a decomposition analysis of the decline in US life expectancy between 2014 and 2015 found that respiratory and cardiovascular diseases contributed almost as much as external causes (including drug overdoses) among US women; among men, drug overdoses explained almost all of the life expectancy decline.10 In a more recent decomposition analysis, Elo et al.31 examined changes in life expectancy among US whites between 1990–1992 and 2014–2016, stratifying the results by sex and geography. Deaths from mental and nervous system disorders were second only to drug overdoses in influencing changes in life expectancy and were the leading contributors to decreased life expectancy among white females. Among white females, respiratory disease mortality was a larger contributor to changes in life expectancy than either suicides or alcohol-related causes and accounted for more deaths in rural areas than drug overdoses (Table e5).
SEX-RELATED PATTERNS
Absolute and relative increases in midlife mortality rates were higher among men than women.20 Between 2010 and 2017, men ages 25–44 years experienced a larger relative increase in age-specific mortality rates than did women of that age, whereas women aged 45–64 years experienced a slightly larger relative increase in mortality than men of their age (see Figure e1). Similarly, although men across age groups generally had higher cause-specific mortality rates and larger relative increases in mortality than did women, a pronounced female disadvantage emerged for certain major causes of death. For example, between 1999 and 2017, the relative increase in midlife fatal drug overdoses was 485.8% among women (from 3.5 deaths/100,000 to 20.2 deaths/100,000), 1.4 times higher than among men (350.6%, from 10.0 deaths/100,000 to 44.8 deaths/100,000). The relative increase in midlife mortality among women was 3.4 times higher for alcoholic liver disease (increasing from 3.2 deaths/100,000 to 5.8 deaths/100,000 among women and from 9.8 deaths/100,000 to 12.2 deaths/100,000 among men) and 1.5 times higher for suicide (increasing from 5.8 deaths/100,000 to 8.7 deaths/100,000 among women and 21.3 deaths/100,000 to 28.6 deaths/100,000 among men). This is consistent with reports elsewhere of gender-specific influences on mortality and a growing health disadvantage among US women, including smaller gains in life expectancy than among US men, larger relative increases in mortality from certain causes, and inferior health outcomes in comparison with women in other high-income countries.11,31,42,43,44,45,46
RACIAL AND ETHNIC PATTERNS
Figure 5 stratifies mortality rates by race-ethnicity for adults ages 25–64 years, and Figure e2 does this for age subgroups (25–44 years and 45–64 years). Midlife mortality rates among NH AIAN and NH blacks exceeded those of other racial and ethnic groups,20 consistent with other reports.47,48 During 1999–2017, (other curves have the same overall direction of NH AIAN from beginning to end of the period – this paragraph needs to be carefully reviewed and edited to match the figure) – retrogression occurred in all racial-ethnic groups except NH AIAN adults, who experienced steady increases in midlife mortality rates on a larger relative scale than any other group.5,20,32,36 Retrogression in the NH white population preceded its occurrence in NH black and Hispanic populations (Figure 5), perhaps explaining why early studies reported that midlife mortality rates had not increased in these groups and focused their research on the white population.29,32,35,36,40 Mortality patterns varied significantly by race-ethnicity and age, as illustrated online (Figure e3), where absolute and relative changes in age-specific mortality rates for men and women are plotted separately for 20 combinations of race and age. Among the findings are that rates generally decreased after 1999 among NH API adults over age 35 and Hispanic adults over age 45 and—as Masters et al. reported28—that rates increased after 2010 among NH white women aged 45–54 years—but not men of that age.
Figure 5. Age-adjusted mortality rates, US adults ages 25–64 years, by race-ethnicity, 1999–2017.
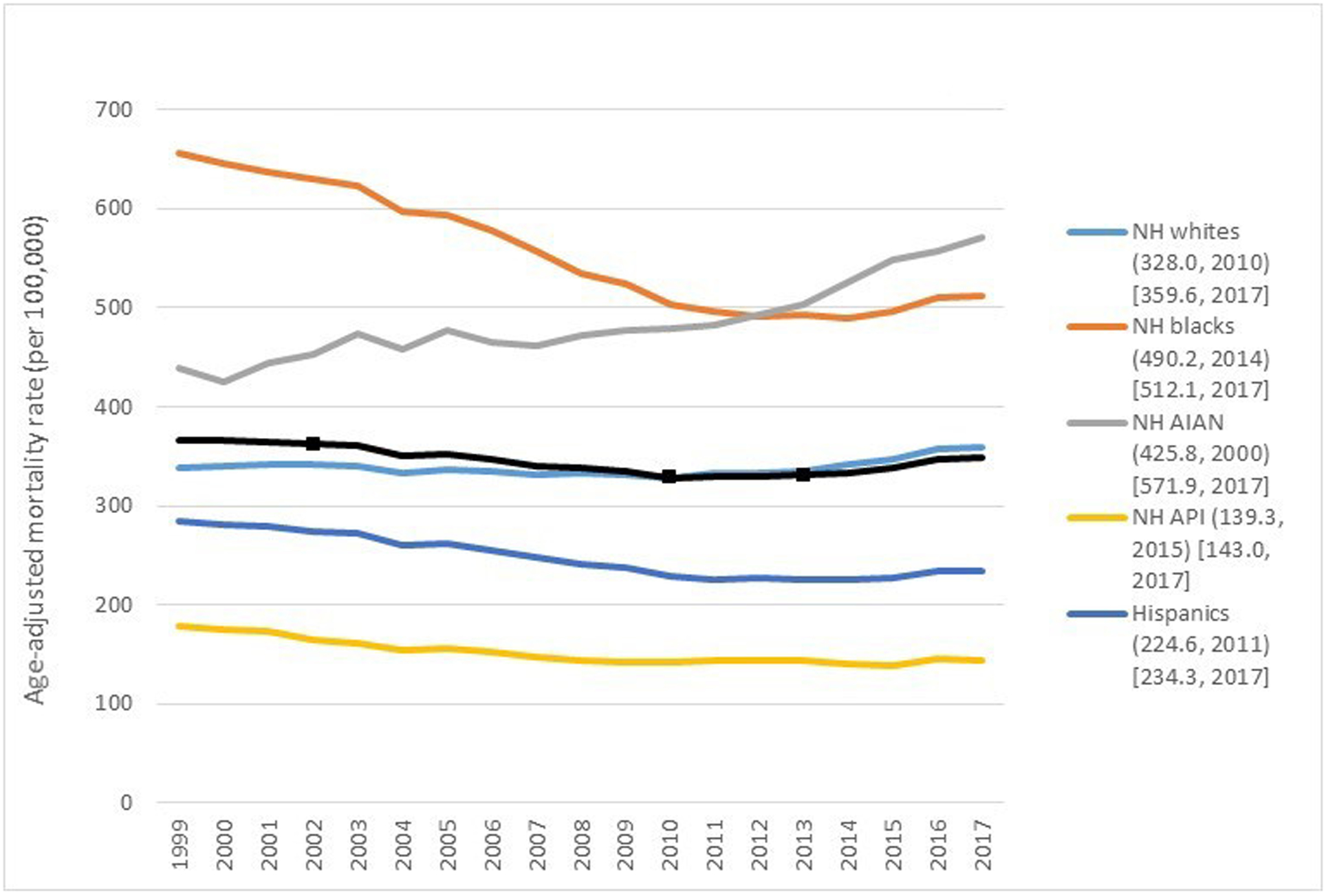
Boldened data points ( ) denote joinpoint years, when the linear trend (slope) changed significantly
based on joinpoint analysis. AIAN = American Indians and Alaskan Natives, API =
Asians and Pacific Islanders (API), NH = non-Hispanic. The lowest mortality
rates per 100,000 (and corresponding years) are listed in parentheses; 2017
mortality rates are listed in brackets. Source: CDC WONDER.
) denote joinpoint years, when the linear trend (slope) changed significantly
based on joinpoint analysis. AIAN = American Indians and Alaskan Natives, API =
Asians and Pacific Islanders (API), NH = non-Hispanic. The lowest mortality
rates per 100,000 (and corresponding years) are listed in parentheses; 2017
mortality rates are listed in brackets. Source: CDC WONDER.
Consistent with the larger US population, populations of color began experiencing increases in cause-specific mortality rates long before experiencing the retrogression in all-cause mortality.20,29,36 Midlife death rates in these populations increased across multiple, diverse conditions. One study reported that midlife mortality rates increased for 12 causes in the NH AIAN population, 17 causes in NH black population, 12 causes in the Hispanic population, and six causes in the NH API population.26 Each of these groups experienced large increases in fatal drug overdoses; between 2010 and 2017, the largest relative increase (171.6%) occurred among NH blacks (Figure 6).27,49 As shown online in Table e6, each of the five racial and ethnic groups also experienced increases in midlife deaths from alcoholic liver diseases, suicides, and hypertensive diseases, among others.26,47 For example, in the NH black population, midlife mortality from neurologic diseases increased from 10.2 deaths/100,000 to 14.1 deaths/100,000 between 1999 and 2017. The reversal (retrogression) in mortality rates that occurred among NH black and Hispanic populations erased years of progress in lowering mortality rates (and reducing racial-ethnic disparities). The increase intensified recently for certain conditions (notably drug overdoses50), with non-whites experiencing larger relative and absolute year-to-year increases in death rates than whites.26
Figure 6. Age-adjusted mortality from accidental drug overdoses, by race-ethnicity, 1999–2017.
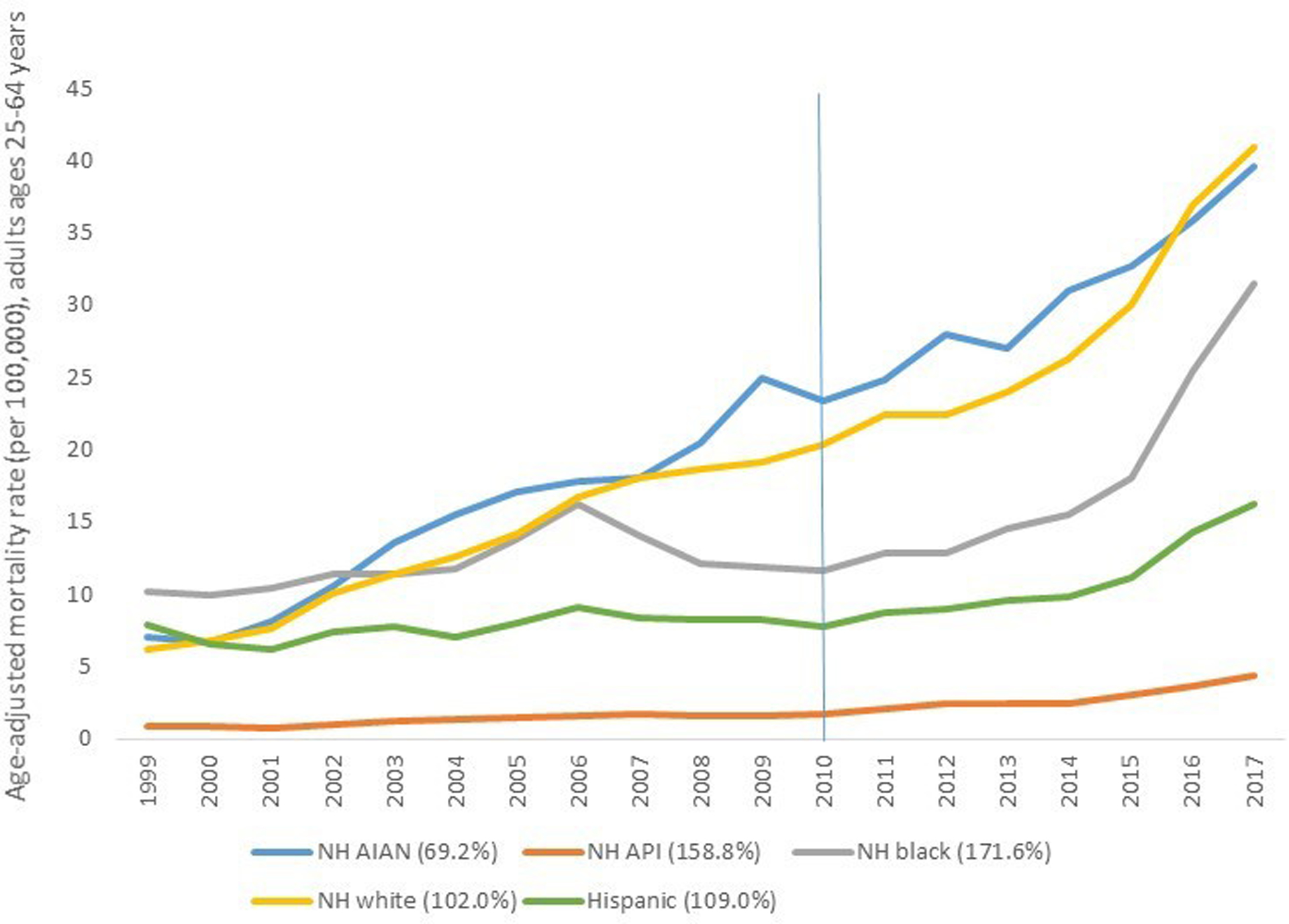
Source: CDC WONDER. Values in parentheses denote relative increases in age-adjusted mortality rates by race-ethnicity between 2010 and 2017. AIAN = American Indians and Alaskan Natives, API = Asians and Pacific Islanders (API), NH = non-Hispanic.
SOCIOECONOMIC PATTERNS
Although an extensive literature links health to education, wealth, and employment,32,51,52,53,54,55,56,57,58 direct evidence of their association with changes in life expectancy or mortality is limited, hampered by limited data to link deaths and socioeconomic history at the individual level. A growing body of evidence, however, indicates that the decline in US life expectancy and mortality risks have been greater among individuals with limited education (e.g., less than high school) and income.32,35,59,60,61,62,63,64,65,66,67 The gradient in life expectancy based on income has also widened over time,68 with outcomes at the lower end of the distribution explaining much of the US disadvantage relative to other countries.69
GEOGRAPHIC PATTERNS
Census divisions and states
The range in life expectancy across the 50 states widened after 1984, reaching 7.0 years in 2016 (Figure 1).18 States’ life expectancy rankings also shifted over time, as illustrated in Figure 7. In 1959, Kansas had the nation’s highest life expectancy (71.9 years), but its position declined over time, ranking 29th by 2016. In 1959, life expectancy in Oklahoma (71.1 years), 10th highest in the nation, exceeded that of New York (69.6 years), which ranked 35th. By 2016, New York’s life expectancy (80.9 years) was 3rd in the nation and Oklahoma’s life expectancy (75.8 years) ranked 45th. State life expectancy trajectories often changed acutely after the 1990s, a finding that was more apparent when it occurred in adjacent states. For example, life expectancy in Colorado and Kansas differed by only 0.3 years in 1990 but increased to 1.5 years in 2016; the difference between Alabama and Georgia increased from 0.1 years to 2.3 years.18
Figure 7. Life expectancy, selected states, 1990–2016.
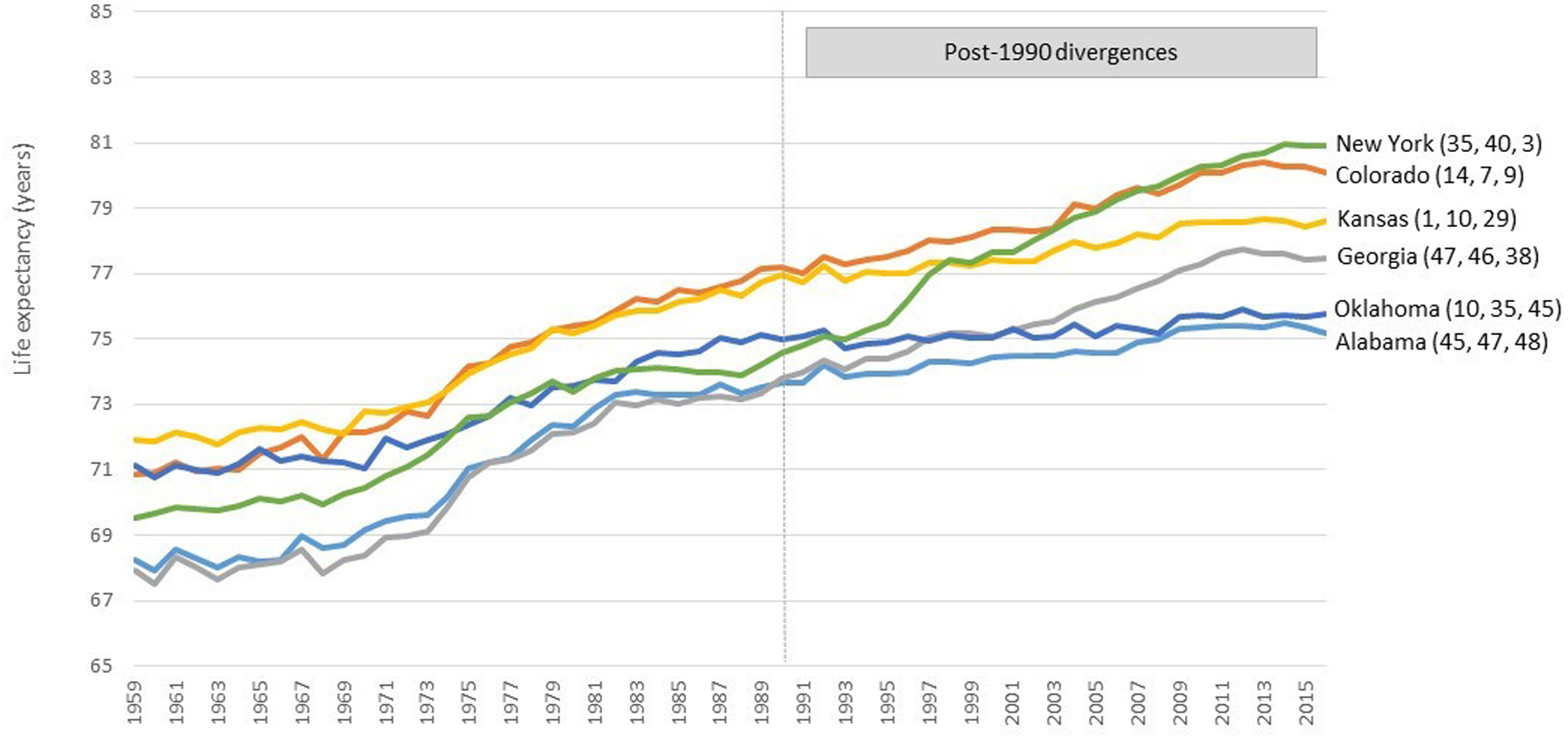
Source: US Mortality Database. Graph highlights divergences in state-level life expectancy that began in the 1990s, featuring neighboring states (Alabama/Georgia and Colorado/Kansas). Values in parentheses refer to state life expectancy rankings (among the 50 states) in 1959, 1990, and 2016, respectively. As the 1990s began, life expectancy in Oklahoma exceeded that of New York.
The recent decrease in US life expectancy and increase in midlife mortality rates was concentrated in certain states, with the largest changes observed in New England and East North Central states and smaller changes in the Pacific and West South Central divisions (Figure 8). The chart book in the online supplement contains 120 graphs of life expectancy (and all-cause mortality) trends for the US, nine census divisions, and 50 states, as modeled by Joinpoint Regression Program. It shows that, in the years leading up to 2016, life expectancy trended downward in four census divisions and 31 states—beginning in 2009 (N=3), 2010 (N=4), 2011 (N=6), 2012 (N=9), 2013 (N=6), and 2014 (N=3)—and decreased significantly (based on APC) in Kentucky, Ohio, and New Hampshire.
Figure 8. Estimated excess deaths from increasing midlife mortality, 2010–2017.
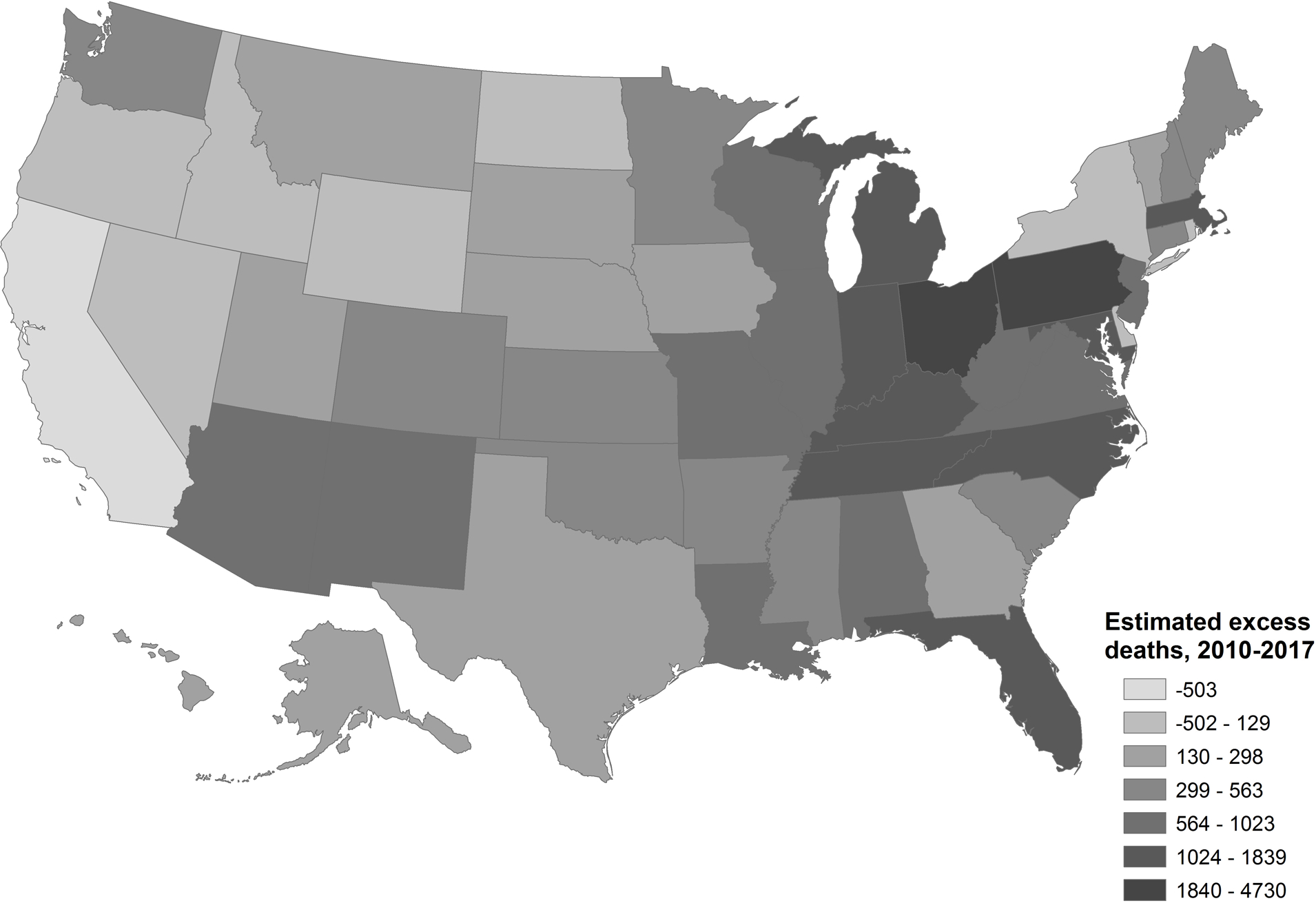
Estimated number of deaths caused by year-to-year increases in age-adjusted mortality rates among adults ages 25–64 years during 2010–2017. The map displays the number of estimated excess deaths (numerator) and not the population size (denominator) to clarify which states contributed the largest absolute number of deaths and exerted the largest influence on national trends. For example, although New Hampshire experienced a large (23.3%) relative increase in midlife mortality rates between 2010 and 2017, that state had a relatively small population (0.4% of US population) and therefore accounted for only 1.2% of excess deaths in the US. See text for more details about methods used to calculate excess deaths.
Table 1 presents APC and AAPC data for life expectancy trends in the US, nine census divisions, and 50 states. The table displays the APC for the two most recent time intervals, how the slope changed between intervals, and the AAPC for 2010–2016. For example, life expectancy in New Hampshire increased significantly (APC = 0.2) from 1978 to 2012 but decreased significantly thereafter (APC = −0.4), with the joinpoint year of 2012 marking a statistically significant (p ≤ 0.05) unfavorable reduction in slope (−6.3E-3). For the period of 2010–2016, the slope was significantly negative (AAPC = −0.20). Unfavorable reductions in slope occurred from 2009 onward in 38 states—i.e., life expectancy either decreased more rapidly or increased more slowly—and the slope change was significant (p < 0.05) in every census division and in 29 states. The largest decreases in life expectancy (based on AAPC for 2010–2016) occurred in New Hampshire, Kentucky, Maine, Ohio, West Virginia, South Dakota, New Mexico, Utah, Indiana, Mississippi, and Tennessee. Other states did not experience decreases in life expectancy; for example, life expectancy increased significantly in the Pacific division and in 13 states (Virginia, Delaware, South Carolina, Texas, Hawaii, New York, Oregon, New Jersey, Montana, Wyoming, Alabama, Arkansas, and Oklahoma).
Table 1.
Joinpoint analysis of life expectancy trends--US, census divisions, and states
| Trends in last two segments (years, APC [95% CI) | Change in slope (% change, 95% CI) |
AAPCǂ (2010–16) | ||||
|---|---|---|---|---|---|---|
| Penultimate APCǂ | Last APCǂ | |||||
| UNITED STATES | 2003–2011 | 0.27 (0.21 to 0.34) | 2011–2016 | 0.00 (−0.12 to 0.12) | −0.27 (−0.40 to −0.14) | 0.05 (−0.05 to 0.14) |
| Div 1: New England | 1977–2012 | 0.22 (0.22 to 0.23) | 2012–2016 | −0.09 (−0.32 to 0.14) | −0.32 (−0.54 to −0.10) | 0.01 (−0.14 to 0.16) |
| Connecticut | 2000–2010 | 0.31 (0.26 to 0.36) | 2010–2016 | 0.04 (−0.06 to 0.14) | −0.27 (−0.38 to −0.16) | 0.04 (−0.06 to 0.14) |
| Maine | 1978–2011 | 0.19 (0.18 to 0.20) | 2011–2016 | −0.16 (−0.34 to 0.02) | −0.35 (−0.52 to −0.17) | −0.10 (−0.25 to 0.04) |
| Massachusetts | 1977–2013 | 0.23 (0.22 to 0.24) | 2013–2016 | −0.17 (−0.59 to 0.24) | −0.40 (−0.81 to 0.00) | 0.03 (−0.17 to 0.23) |
| New Hampshire | 1978–2012 | 0.22 (0.21 to 0.23) | 2012–2016 | −0.41 (−0.66 to −0.15) | −0.63 (−0.88 to −0.38) | −0.20 (−0.36 to −0.03) |
| Rhode Island | 1979–2012 | 0.20 (0.19 to 0.21) | 2012–2016 | −0.06 (−0.36 to 0.24) | −0.26 (−0.55 to 0.03) | 0.03 (−0.16 to 0.22) |
| Vermont | 1977–2009 | 0.24 (0.23 to 0.25) | 2009–2016 | −0.05 (−0.15 to 0.06) | −0.28 (−0.39 to −0.18) | −0.05 (−0.15 to 0.06) |
| Div 2: Mid-Atlantic | 1988–2010 | 0.31 (0.29 to 0.32) | 2010–2016 | 0.10 (−0.01 to 0.21) | −0.21 (−0.31 to −0.10) | 0.10 (−0.01 to 0.21) |
| New Jersey | 1988–2012 | 0.30 (0.28 to 0.32) | 2012–2016 | 0.05 (−0.16 to 0.25) | −0.25 (−0.45 to −0.05) | 0.13 (0.00 to 0.26) |
| New York | 1998–2012 | 0.31 (0.28 to 0.34) | 2012–2016 | 0.10 (−0.07 to 0.27) | −0.21 (−0.38 to −0.05) | 0.17 (0.06 to 0.28) |
| Pennsylvania | 1981–2014 | 0.19 (0.19 to 0.20) | 2014–2016 | −0.41 (−1.03 to 0.21) | −0.60 (−1.21 to 0.00) | −0.01 (−0.21 to 0.19) |
| Div 3: East North Central | 1980–2012 | 0.19 (0.18 to 0.20) | 2012–2016 | −0.10 (−0.28 to 0.08) | −0.29 (−0.46 to −0.11) | 0.00 (−0.12 to 0.11) |
| Illinois | 1994–2012 | 0.29 (0.26 to 0.31) | 2012–2016 | −0.03 (−0.23 to 0.18) | −0.31 (−0.51 to −0.11) | 0.08 (−0.05 to 0.21) |
| Indiana | 1981–2011 | 0.14 (0.13 to 0.15) | 2011–2016 | −0.10 (−0.24 to 0.05) | −0.24 (−0.38 to −0.10) | −0.06 (−0.18 to 0.06) |
| Michigan | 1978–2011 | 0.20 (0.19 to 0.20) | 2011–2016 | −0.05 (−0.16 to 0.06) | −0.25 (−0.36 to −0.14) | −0.01 (−0.10 to 0.08) |
| Ohio | 1983–2012 | 0.15 (0.14 to 0.16) | 2012–2016 | −0.22 (−0.41 to −0.04) | −0.37 (−0.55 to −0.19) | −0.10 (−0.22 to 0.02) |
| Wisconsin | 2002–2009 | 0.25 (0.17 to 0.34) | 2009–2016 | −0.03 (−0.09 to 0.04) | −0.28 (−0.39 to −0.18) | −0.03 (−0.09 to 0.04) |
| Div 4: West North Central | 2001–2010 | 0.20 (0.15 to 0.25) | 2010–2016 | −0.02 (−0.09 to 0.06) | −0.21 (−0.30 to −0.13) | −0.02 (−0.09 to 0.06) |
| Iowa | 1980–2010 | 0.16 (0.15 to 0.16) | 2010–2016 | −0.04 (−0.13 to 0.05) | −0.20 (−0.28 to −0.11) | −0.04 (−0.13 to 0.05) |
| Kansas | 2001–2011 | 0.16 (0.12 to 0.20) | 2011–2016 | −0.03 (−0.14 to 0.08) | −0.19 (−0.30 to −0.08) | 0.00 (−0.08 to 0.09) |
| Minnesota | 2000–2009 | 0.26 (0.20 to 0.32) | 2009–2016 | 0.00 (−0.07 to 0.08) | −0.26 (−0.35 to −0.16) | 0.00 (−0.07 to 0.08) |
| Missouri | 1999–2012 | 0.18 (0.16 to 0.21) | 2012–2016 | −0.11 (−0.28 to 0.06) | −0.29 (−0.46 to −0.12) | −0.01 (−0.12 to 0.10) |
| Nebraska | 1979–2011 | 0.17 (0.16 to 0.18) | 2011–2016 | −0.04 (−0.18 to 0.11) | −0.20 (−0.34 to −0.06) | 0.00 (−0.12 to 0.12) |
| North Dakota | 2002–2005 | 0.39 (−0.69 to 1.48) | 2005–2016 | 0.01 (−0.04 to 0.06) | −0.37 (−1.43 to 0.68) | 0.01 (−0.04 to 0.06) |
| South Dakota | 1982–2013 | 0.16 (0.15 to 0.18) | 2013–2016 | −0.32 (−0.80 to 0.16) | −0.48 (−0.95 to −0.01) | −0.08 (−0.31 to 0.16) |
| Div 5: South Atlantic | 2003–2012 | 0.30 (0.23 to 0.37) | 2012–2016 | −0.06 (−0.28 to 0.16) | −0.36 (−0.59 to −0.13) | 0.06 (−0.09 to 0.20) |
| Delaware | 1969–1977 | 0.60 (0.46 to 0.73) | 1977–2016 | 0.21 (0.20 to 0.22) | −0.39 (−0.52 to −0.25) | 0.21 (0.20 to 0.22) |
| Florida | 2005–2013 | 0.33 (0.22 to 0.44) | 2013–2016 | −0.14 (−0.55 to 0.26) | −0.47 (−0.88 to −0.06) | 0.09 (−0.11 to 0.30) |
| Georgia | 2003–2012 | 0.31 (0.22 to 0.40) | 2012–2016 | −0.12 (−0.39 to 0.16) | −0.42 (−0.71 to −0.14) | 0.02 (−0.16 to 0.21) |
| Maryland | 2001–2012 | 0.36 (0.31 to 0.41) | 2012–2016 | −0.11 (−0.33 to 0.12) | −0.47 (−0.69 to −0.24) | 0.05 (−0.10 to 0.20) |
| North Carolina | 2000–2012 | 0.26 (0.22 to 0.30) | 2012–2016 | −0.09 (−0.30 to 0.12) | −0.35 (−0.56 to −0.14) | 0.02 (−0.11 to 0.16) |
| South Carolina | 1972–1979 | 0.79 (0.61 to 0.96) | 1979–2016 | 0.20 (0.19 to 0.21) | −0.59 (−0.76 to −0.41) | 0.20 (0.19 to 0.21) |
| Virginia | 1969–1979 | 0.53 (0.47 to 0.60) | 1979–2016 | 0.22 (0.21 to 0.23) | −0.31 (−0.37 to −0.25) | 0.22 (0.21 to 0.23) |
| West Virginia | 1996–2014 | 0.05 (0.03 to 0.06) | 2014–2016 | −0.37 (−1.07 to 0.35) | −0.41 (−1.11 to 0.28) | −0.09 (−0.32 to 0.14) |
| Div 6: East South Central | 2005–2011 | 0.20 (0.07 to 0.33) | 2011–2016 | −0.10 (−0.23 to 0.03) | −0.31 (−0.49 to −0.13) | −0.05 (−0.16 to 0.06) |
| Alabama | 1969–1982 | 0.49 (0.45 to 0.53) | 1982–2016 | 0.09 (0.09 to 0.10) | −0.39 (−0.43 to −0.35) | 0.09 (0.09 to 0.10) |
| Kentucky | 1992–2013 | 0.09 (0.08 to 0.11) | 2013–2016 | −0.38 (−0.73 to −0.03) | −0.47 (−0.81 to −0.13) | −0.14 (−0.31 to 0.03) |
| Mississippi | 2005–2010 | 0.31 (0.06 to 0.55) | 2010–2016 | −0.06 (−0.18 to 0.06) | −0.36 (−0.63 to −0.10) | −0.06 (−0.18 to 0.06) |
| Tennessee | 2003–2011 | 0.23 (0.14 to 0.32) | 2011–2016 | −0.10 (−0.26 to 0.06) | −0.33 (−0.51 to −0.16) | −0.05 (−0.17 to 0.08) |
| Div 7: West South Central | 2003–2011 | 0.25 (0.19 to 0.31) | 2011–2016 | 0.03 (−0.08 to 0.14) | −0.22 (−0.34 to −0.10) | 0.07 (−0.02 to 0.15) |
| Arkansas | 1973–1978 | 0.68 (0.44 to 0.92) | 1978–2016 | 0.09 (0.08 to 0.10) | −0.58 (−0.82 to −0.35) | 0.09 (0.08 to 0.10) |
| Louisiana | 2005–2010 | 0.42 (0.18 to 0.66) | 2010–2016 | 0.02 (−0.10 to 0.14) | −0.40 (−0.66 to −0.14) | 0.02 (−0.10 to 0.14) |
| Oklahoma | 1987–1995 | −0.03 (−0.10 to 0.05) | 1995–2016 | 0.06 (0.05 to 0.07) | 0.09 (0.01 to 0.16) | 0.06 (0.05 to 0.07) |
| Texas | 1972–1977 | 0.65 (0.42 to 0.88) | 1977–2016 | 0.19 (0.19 to 0.20) | −0.45 (−0.67 to −0.23) | 0.19 (0.19 to 0.20) |
| Div 8: Mountain | 2005–2010 | 0.31 (0.15 to 0.48) | 2010–2016 | 0.01 (−0.07 to 0.10) | −0.30 (−0.48 to −0.12) | 0.01 (−0.07 to 0.10) |
| Arizona | 2006–2009 | 0.60 (−0.22 to 1.42) | 2009–2016 | 0.05 (−0.05 to 0.16) | −0.55 (−1.34 to 0.25) | 0.05 (−0.05 to 0.16) |
| Colorado | 2002–2012 | 0.24 (0.19 to 0.29) | 2012–2016 | −0.07 (−0.28 to 0.13) | −0.31 (−0.52 to −0.11) | 0.03 (−0.10 to 0.16) |
| Idaho | 1991–2010 | 0.16 (0.14 to 0.17) | 2010–2016 | −0.02 (−0.11 to 0.08) | −0.17 (−0.27 to −0.08) | −0.02 (−0.11 to 0.08) |
| Montana | 1977–1988 | 0.34 (0.27 to 0.41) | 1988–2016 | 0.12 (0.11 to 0.13) | −0.22 (−0.29 to −0.15) | 0.12 (0.11 to 0.13) |
| Nevada | 2005–2010 | 0.40 (0.20 to 0.61) | 2010–2016 | 0.06 (−0.05 to 0.16) | −0.34 (−0.56 to −0.12) | 0.06 (−0.04 to 0.16) |
| New Mexico | 1983–2013 | 0.13 (0.12 to 0.15) | 2013–2016 | −0.27 (−0.70 to 0.16) | −0.40 (−0.82 to 0.02) | −0.07 (−0.28 to 0.14) |
| Utah | 2004–2009 | 0.28 (0.10 to 0.45) | 2009–2016 | −0.07 (−0.14 to 0.00) | −0.34 (−0.53 to −0.16) | −0.07 (−0.13 to 0.00) |
| Wyoming | 1971–1984 | 0.57 (0.49 to 0.64) | 1984–2016 | 0.12 (0.11 to 0.14) | −0.44 (−0.51 to −0.37) | 0.12 (0.11 to 0.14) |
| Div 9: Pacific | 1988–2013 | 0.27 (0.26 to 0.28) | 2013–2016 | 0.01 (−0.24 to 0.26) | −0.26 (−0.51 to −0.02) | 0.14 (0.02 to 0.26) |
| Alaska | 1984–2010 | 0.21 (0.18 to 0.23) | 2010–2016 | −0.04 (−0.27 to 0.18) | −0.25 (−0.47 to −0.03) | −0.04 (−0.27 to 0.18) |
| California | 1988–2014 | 0.30 (0.29 to 0.31) | 2014–2016 | −0.12 (−0.70 to 0.45) | −0.42 (−0.98 to 0.14) | 0.16 (−0.03 to 0.34) |
| Hawaii | 1977–1997 | 0.14 (0.12 to 0.16) | 1997–2016 | 0.18 (0.16 to 0.20) | 0.04 (0.02 to 0.07) | 0.18 (0.16 to 0.20) |
| Oregon | 1971–1979 | 0.46 (0.35 to 0.58) | 1979–2016 | 0.17 (0.16 to 0.18) | −0.29 (−0.40 to −0.18) | 0.17 (0.16 to 0.18) |
| Washington | 1980–2013 | 0.19 (0.19 to 0.20) | 2013–2016 | −0.03 (−0.32 to 0.26) | −0.22 (−0.51 to 0.06) | 0.08 (−0.06 to 0.22) |
Table presents slopes for the two most recent linear trends in life expectancy during 1959–2016. For the penultimate and most recent time periods, the table presents the annual percent change (APC), the years marking the beginning and end of each time period, and the degree to which the slope changed between the two comparison periods. The table also presents the average annual percent change (AAPC) for 2010–2016. The AAPC over any fixed interval is calculated using a weighted average of the slope coefficients of the underlying joinpoint regression line with weights equal to the length of each segment over the interval. The final step of the calculation transforms the weighted average of slope coefficients to an annual percent change. Life expectancy data obtained from the US Mortality Database.
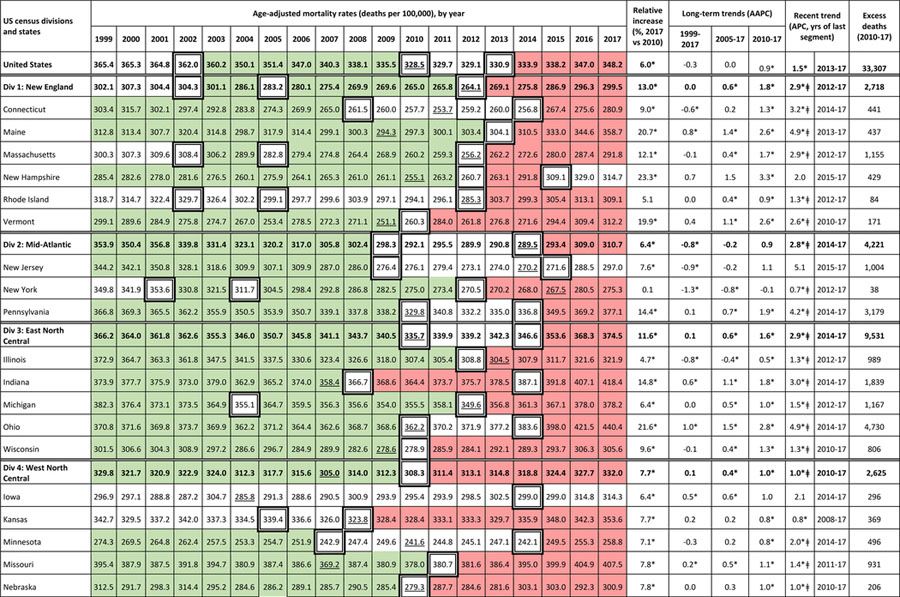
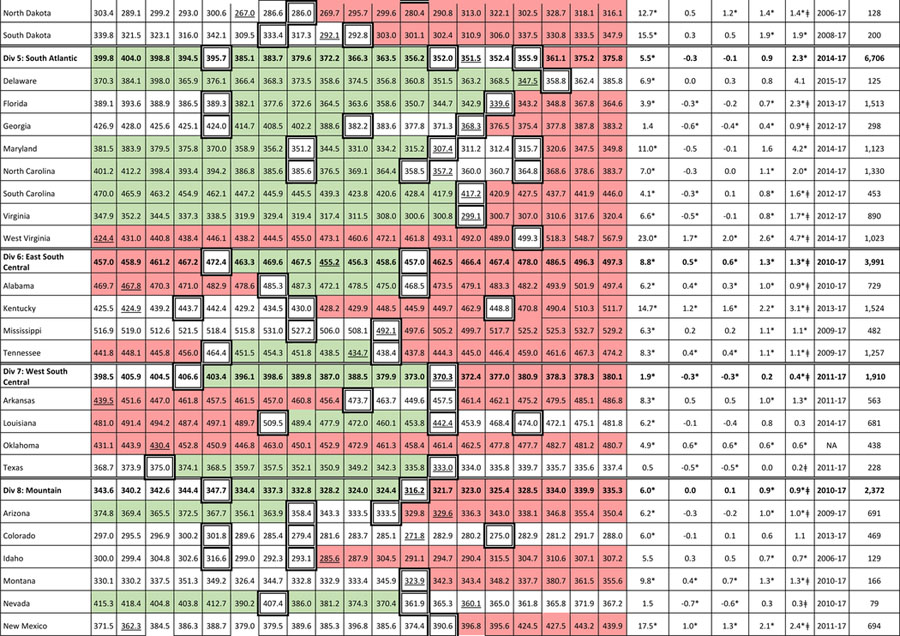
Table 2 shows the increase in midlife mortality rates during 1999–2017. The table’s green and red colors signify favorable (negative APC) and unfavorable (positive APC) mortality trends based on joinpoint analysis (bolded boxes represent joinpoints). Many states experienced retrogression—declining mortality followed by a mortality reversal. For example, in Connecticut, a period of decreasing midlife mortality during 1999–2008 (green shading) was followed by a statistically stable period in 2008–2014 (clear shading)—during which the lowest mortality rate (253.7 deaths/100,000) was reached in 2011—and then by a significant increase in midlife mortality during 2014–2017 (red shading). The remaining columns explain that midlife mortality in Connecticut increased by 9.0% between 2010 and 2017 (p ≤ 0.05), that what appeared to be a long-term decrease in mortality during 1999–2017 (AAPC = −0.6) obscured progressively less favorable trends in recent time periods (AAPC = 0.2, 2005–2017; AAPC = 1.3, 2010–2017), and that the increase in mortality (APC = 3.2) in the most recent time period (2014–2017) was dually significant, differing significantly from zero (*) and from the slope of the prior segment (ǂ). The final column notes that year-to-year changes in mortality during 1999–2017 caused an estimated 441 excess midlife deaths in Connecticut.
Table 2.
Age-adjusted all-cause mortality rates, adults ages 25–64 years, for the US, census divisions, and states (1999–2017)
 |
 |
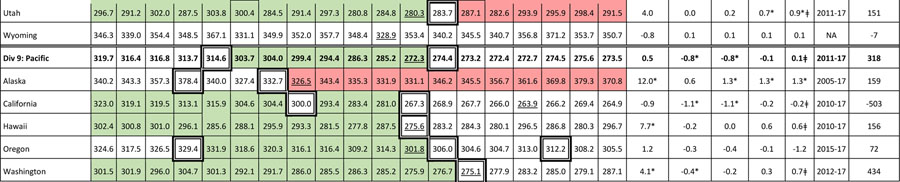 |
Table presents age-adjusted, all-cause mortality rates (per 100,000) among US adults ages 25–64 years for 1999–2017, along with the relative increase in mortality rates between 1999 and 2017, and the slopes modeled by the Joinpoint Regression Program. See text and Supplement for methods. Slopes presented here include the average annual percent change (AAPC) for three time periods—1999–2017, 2005–2017, and 2010–2017—and the annual percent change (APC) for the most recent linear trend in the joinpoint model. Also shown are the estimated number of excess deaths in the US caused by year-to-year changes in midlife mortality rates between 1999 and 2017. Green shading depicts years during which mortality rates decreased (statistically significant negative APC), red shading denotes years of increasing mortality (statistically significant positive APC), and cells with no color depict periods when the APC did not differ significantly from zero. Cells with bolded borders denote joinpoint years, when changes occurred in the modeled linear trends. Underlined mortality rates denote the lowest mortality rates (nadir) for 1999–2017. Asterisks (*) denote a slope (APC or AAPC) that differed significantly from zero (p < 0.05) and hashtags (ǂ) denote a statistically significant slope change estimate, a measure of the change in slope from that of the previous time period; see Table e7 for 95% confidence intervals. NA = Not applicable; joinpoint plotted a single trend line for 1999–2017, thus no last segment. Mortality rates obtained from CDC WONDER.
The increase in midlife mortality was geographically widespread. Table 2 shows that the AAPC for 2010–2017 was positive in eight census divisions and all but four states (California, New York, Oregon, and Texas). Thirty-seven states experienced statistically significant increases in midlife mortality (positive APC) in the years leading up to 2017. However, the trend was concentrated in certain states. Between 2010 and 2017, the largest relative increases in mortality occurred in New England (New Hampshire, 23.3%; Maine, 20.7%; Vermont, 19.9%, Massachusetts 12.1%) and the Ohio Valley (West Virginia, 23.0%; Ohio, 21.6%; Indiana, 14.8%; Kentucky, 14.7%), as well as in New Mexico (17.5%), South Dakota (15.5%), Pennsylvania (14.4%), North Dakota (12.7%), Alaska (12.0%), and Maryland (11.0%). In contrast, the nation’s most populous states (California, Texas, and New York) experienced relatively small increases in midlife mortality.
Five states (Iowa, New Mexico, Oklahoma, West Virginia, and Wyoming) experienced a nearly continuous increase in midlife mortality (only positive APC segments) throughout 1999–2017, the largest (33.8%) occurring in West Virginia. Thirty-eight states experienced progress (declining mortality) as the millennium began, followed by retrogression (time segments beginning in 1999–2003 with negative APCs, followed by periods of increasing mortality with positive APCs). These reversals occurred earlier in some states than others; for example, midlife mortality rates in Iowa and North Dakota reached a nadir in 2004, whereas nadirs in New Jersey and New York did not occur until 2014 and 2015, respectively. Cause-specific mortality trends also varied by state, sometimes in opposite directions. For example, whereas rates of firearm-related suicides increased nationwide during 1999–2017, they remained stable or decreased in California, Connecticut, Maryland, New Jersey, and New York.20
Between 2010 and 2017, year-to-year changes in midlife mortality accounted for an estimated 33,307 excess US deaths (Table 2). Population sizes influenced states’ individual contribution to national mortality trends. For example, although several New England states (New Hampshire, Maine, and Vermont) experienced large (20–23%) relative increases in midlife mortality during 2010–2017, these states accounted for only 3.0% of excess deaths due to their small populations. The East North Central division accounted for 28.6% of excess deaths, and Ohio, Pennsylvania, Indiana, and Kentucky (which include 10.8% of the US population) accounted for the largest number of excess deaths: these four states accounted for approximately one third (32.8%) of excess deaths. Eight of the 10 states with the largest number of excess deaths were in the Industrial Midwest or Appalachia.
Counties and cities
As a group, rural US counties experienced larger increases in all-cause midlife mortality than did metropolitan counties,29,31 but more complex patterns emerged when county data were disaggregated by population size, sex, race-ethnicity, age, and causes of death. For example, although the relative increase in midlife drug overdose deaths during 1999–2017 among NH whites was higher in rural (749.4%, from 4.0 deaths/100,000 to 33.8 deaths/100,000) than metropolitan (531.2%, from 6.7 deaths/100,000 to 42.5 deaths/100,000) counties, the largest relative increase in overdose deaths (857.8%, from 4.7 deaths/100,000 to 45.2 deaths/100,000) occurred in the suburbs of large cities (populations ≥1 million), where Hispanic populations also experienced their largest increase in midlife overdose deaths.20 Among NH blacks, the largest increase in overdose deaths occurred in small cities (populations < 250,000), but the largest increase among blacks aged 55–64 years was in large cities.29 The largest increase in midlife suicides among NH AIAN and Hispanic adults was in metropolitan areas, whereas the largest increase among non-Hispanic blacks and whites occurred in rural counties.20 Among young whites (ages 25–34 years), the largest increase in suicides occurred in the suburbs.29 Mortality patterns for men and women also varied significantly across urban and rural areas, with residents of large cities experiencing the greatest increases in life expectancy.31
Geographic disparities in mortality were associated with demographic characteristics, and with community contextual factors independent of individual and household characteristics. For example, a multivariate analysis of drug-related mortality in 2006–2015 found that drug deaths were higher in counties with certain demographic characteristics (e.g., older adults, active duty military or veterans, Native Americans) and in counties with mining-dependent economies, high economic and family distress indices, vacant housing, or high rent. Mortality rates were lower in counties with more religious establishments, recent in-migrants, and dependence on public sector (i.e., government) employment.70 Similarly, studies in five states (California, Kansas, Missouri, Minnesota, and Virginia) found that increases in midlife mortality from “stress-related conditions” (drug overdoses, alcohol poisoning, alcoholic liver disease, and suicides) were highest in counties with prolonged exposure to high poverty, unemployment, and stagnant household income. Examples included the Central Valley and northern rural counties of California71, the Ozark and Bootheel regions of Missouri72, and the southwestern coalfields of Virginia.73
DISCUSSION
US life expectancy increased from 1959 to 2014 but the rate of increase was greatest in 1969–1979 and slowed thereafter, losing pace with other high-income countries, plateauing in 2011, and decreasing after 2014. A major contributor was an increase in all-cause mortality among young and middle-aged adults, which began in 2010, and an increase in cause-specific mortality rates in this midlife age group, which began as early as the 1990s and involved deaths from drug overdoses, alcohol abuse, and suicides, and diverse organ system diseases, such as hypertensive diseases and diabetes. Although NH whites experienced the largest absolute number of deaths, all racial groups and the Hispanic population were affected. For certain causes of death (e.g., fatal drug overdoses, alcoholic liver disease, and suicide), women experienced larger relative increases in mortality than men, although the absolute mortality rates for these causes were higher in men than women.
By 2010, increases in cause-specific mortality rates at ages 25–64 years had reversed years of progress in lowering mortality from other causes (e.g., ischemic heart disease, cancer, HIV infection)—and all-cause mortality began increasing. The trend began earlier (e.g., the 1990s) in some states and only recently in others (e.g., New York, New Jersey). Gaps in life expectancy across states began widening in the 1980s, with substantial divergences occurring in the 1990s. Changes in life expectancy and midlife mortality were greatest in the eastern US—notably the Ohio Valley, Appalachia, and upper New England—whereas many Pacific states were less affected. The largest relative increases in midlife mortality occurred among adults with less education and in rural areas or other settings with evidence of economic distress or diminished social capital.
POTENTIAL EXPLANATIONS
The increase in midlife mortality after 1999 was greatly influenced by the increase in drug overdoses. Heroin use increased substantially in the 1960s and 1970s, as did crack cocaine abuse in the 1980s, disproportionately affecting (and criminalizing) the black population.74,75 Mortality from drug overdoses increased exponentially from the 1970s onward.76 The sharp increase in overdose deaths that began in the 1990s primarily affected whites and came in three waves: (1) the introduction of OxyContin in 1996 and overuse of prescription opioids, followed by (2) increased heroin use, often by patients who became addicted to prescription opioids,77 and (3) the subsequent emergence of potent synthetic opioids (e.g., fentanyl analogues)—the latter triggering a large post-2013 increase in overdose deaths.27,78,79 That whites first experienced a larger increase in overdose deaths than non-whites may reflect their greater access to health care (and thus prescription drugs).5,80 That NH black and Hispanic populations experienced the largest relative increases in fentanyl deaths after 201181 may explain the retrogression in overdose deaths observed in these groups.48 Geographic differences in the promotion and distribution of opioids may also explain the concentration of midlife deaths in certain states.82
However, the increase in opioid-related deaths is only part of a more complicated phenomenon and does not fully explain the increase in midlife mortality rates from other causes, such as alcoholic liver disease or suicides (85.2% of which involve firearms or other non-poisoning methods83). Opioid-related deaths also cannot fully explain the US health disadvantage, which began earlier (in the 1980s) and involved multiple diseases and non-drug injuries.5,6,7 Two recent studies estimated that drug overdoses accounted for 15% or less of the gap in life expectancy between the US and other high-income countries in 2013 and 2014, respectively.84,85
The National Research Council examined the US health disadvantage in detail and identified nine domains in which the US had poorer health outcomes than other high-income countries: these included not only drug-related deaths but also adverse birth outcomes, injuries and homicides, adolescent pregnancy and sexually transmitted infections, HIV and AIDS, obesity and diabetes, heart disease, chronic lung disease, and disability.7 Compared to the average mortality rates of 16 other high-income countries, the US has lower mortality from cancer and cerebrovascular diseases but higher mortality rates from most other major causes of death, including: circulatory disorders (e.g., ischemic heart and hypertensive diseases), external causes (e.g., drug overdoses, suicide, homicide), diabetes, infectious diseases, pregnancy and childbirth, congenital malformations, mental and behavioral disorders, and diseases of the respiratory, nervous, genitourinary, and musculoskeletal systems.86 According to one estimate, if the slow rate of increase in US life expectancy persists, it will take the US more than a century to reach the average life expectancy that other high-income countries had achieved by 2016.10
Tobacco use and obesity
Exposure to behavioral risk factors could explain some of these trends. Although tobacco use in the US has decreased, higher smoking rates in prior decades could have produced delayed effects on current tobacco-related mortality and life expectancy patterns, especially among older adults.6,87,88 For example, a statistical model that accounted for the lag between risk factor exposure and subsequent death estimated that much of the gap in life expectancy at age 50 that existed in 2003 between the US and other high-income countries—41% of the gap in men and 78% of the gap in women—was attributable to smoking.89 Smoking explained 50% or more of the geographic differences in mortality within the US in 2004.87,90 However, it is unclear whether smoking, which has declined in prevalence, continues to have as large a role in current life expectancy patterns or in explaining increases in mortality among younger adults is unclear.
The obesity epidemic, a known contributor to the US health disadvantage,6 could potentially explain an increase in midlife mortality rates for diseases linked to obesity, such as hypertensive heart disease91 and renal failure.92 As long ago as 2005, the increasing prevalence of obesity prompted Olshansky et al. to predict a forthcoming decrease in US life expectancy.93 By 2011, Preston et al. estimated that increases in obesity had reduced life expectancy at age 40 by 0.9 years.94 Elo et al. noted that changes in obesity prevalence had the largest correlation with geographic variations in life expectancy of any variable they examined.31
However, neither smoking nor obesity can fully explain current mortality patterns, such as those among younger adults and increasing mortality from conditions without known causal links to these risk factors. Suggesting that other factors may be at play, Muennig and Glied noted that Australia and other countries with patterns of smoking and obesity similar to the US achieved greater gains in survival between 1975 and 2005.13
Deficiencies in health care
Deficiencies in the health care system could potentially explain increased mortality from some conditions. Although the US health care system excels on certain measures, countries with higher life expectancy outperform the US in providing universal access to health care, removing costs as a barrier to care, care coordination, and amenable mortality.95,96,97 In a difficult economy that imposes greater costs on patients98, adults in midlife may have greater financial barriers to care than children and older adults, who benefit from the Children’s Health Insurance Program and Medicare coverage, respectively.99 Although poor access or deficiencies in quality could introduce mortality risks among patients with existing behavioral health needs or chronic diseases, these factors would not account for the underlying precipitants (e.g., suicidality, obesity), which originate outside the clinic. Physicians contributed to the overprescription of opioids100, and iatrogenic factors could potentially explain increases in midlife mortality from other causes, but empirical evidence is limited. Nor would systemic deficiencies in the health care system explain why midlife death rates increased for some chronic diseases while decreasing greatly for others (e.g., ischemic heart disease, cancer, and HIV infection).
Psychological distress
Despair has been invoked as a potential cause for the increase in deaths related to drug, alcohol, and suicides (referred to by some as ‘deaths of despair’).29,35,65,101 Some studies suggest that psychological distress, anxiety, and depression have increased in the US, especially among adolescents and young adults.65,102,103,104,105,106,107,108 Psychological distress and mental illness are risk factors for substance abuse and suicides82,109,110 and may complicate organ system diseases, as when hopelessness erodes motivation to pursue health care or manage chronic illnesses.111 Chronic stress has neurobiological and systemic effects on allostatic load and end organs and may increase pain sensitivity (and thus analgesic needs).112,113,114,115 However, the evidence that the prevalence of psychological distress or mental illness increased during the relevant time period is inconclusive. Epidemiological data about mental illness have methodological limitations,116,117 and some surveillance studies report no increase in prevalence rates.118,119 Moreover, even if the prevalence of certain mental illnesses did increase, a causal link to the full spectrum of midlife mortality deaths has not been established.
Socioeconomic conditions
Three lines of evidence suggest a potential association between mortality trends and economic conditions, the first being timing. The US health disadvantage and increase in midlife mortality began in the 1980s and 1990s, a period marked by a major transformation in the nation’s economy, substantial job losses in manufacturing and other sectors, contraction of the middle class, wage stagnation, and reduced intergenerational mobility.120,121,122,123,124,125 Income inequality widened greatly, surpassing levels in other countries, concurrent with the deepening US health disadvantage.126,127,128,129,130,131,132 The second line of evidence concerns affected populations: those most vulnerable to the new economy (e.g., adults with limited education, women) experienced the largest increases in death rates. The third line of evidence is geographic: increases in death rates were concentrated in areas with a history of economic challenges, such as rural America133,134 and the Industrial Midwest,135,136 and were lowest in the Pacific division and populous states with more robust economies (e.g., Texas, New York). One theory for the larger life expectancy gains in metropolitan areas is an increase in the population with college degrees.31
Socioeconomic pressures and unstable employment could explain some of the observed increases in mortality spanning multiple causes of death. Financial hardship and insecurity limit access to health care and the social determinants of health (e.g., education, food, housing, transportation) and increase the risk of chronic stress, disease, disability, pessimism, and pain.100,137,138,139,140,141,142,143,144 One study estimated that a 1% increase in county unemployment rates was associated with a 3.6% increase in opioid deaths.145 However, the evidence to date has not proven that economic conditions are responsible for the recent increase in midlife mortality;146 correlations with state and local indicators (e.g., employment, poverty rates) are not always consistent, and the causal link between income inequality and health is debated.147,148
The causes of economic despair may be more nuanced; perceptions and frustrated expectations may matter as much as absolute income or net worth.149,150 For example, ethnographers describe the dismay among working-class whites over their perceived loss of social position and uncertain future,100,151,152,153,154,155 a popular (but unsubstantiated) thesis for why this historically privileged population experienced larger increases in midlife deaths than did minority groups (e.g., NH blacks) with greater social and economic disadvantages.156,157,158,159 Also unclear is the extent to which household socioeconomic status acts as a proxy for important contextual conditions in communities (e.g., social environment, services infrastructure, economy, labor market) that also shape health.5,81,160,161,162,163
The above explanations are not independent and collectively shape mortality patterns; major contributors like smoking, drug abuse, and obesogenic diets are shaped by environmental conditions, psychological distress, and socioeconomic status. The same economic pressures that force patients to forego medical care can also induce stress and unhealthy coping behaviors and can fracture communities. Fenelon, whose research quantified the contribution of smoking to mortality, also noted that it may “represent one critical piece of a broader cultural, socioeconomic, and behavioral puzzle that has implications for numerous health-related behaviors and outcomes.”89
Methodologic considerations
Any theory for decreasing life expectancy, whether opioids, despair, poverty, or social division, must account for the timing of exposure and lagged effects on outcomes. Whereas observed increases in mortality could occur shortly after increased exposure to certain causes, such as fentanyl or lethal firearms, increases in premature mortality from chronic conditions may require decades of prolonged exposure (Table e8). Some mortality patterns exhibit period effects, such as the increase in opioid deaths that began in the 1990s, and affected multiple age cohorts, whereas other causes show cohort-based variation. For example, Masters et al. identified a specific cohort—NH whites born in the 1950s—at heightened risk of midlife mortality from obesity, heart disease, diabetes, and hypertension.28 Zang et al. documented a heightened mortality risk among cohorts born during 1973–91.164
Any theory for decreasing US life expectancy must explain why this trend is less pronounced in other industrialized countries.10 A National Research Council panel, charged with this question, focused its research on how the US differs in terms of health care, unhealthy behaviors, socioeconomic factors, the physical and social environment, and public polices and priorities.7 Social protection policies deserve special attention: countries with higher life expectancy spend more of their budgets on social services143,165 and outperform the US in terms of education, child poverty, and other measures of wellbeing.5,7
Causal theories must also explain why US mortality trends have affected some states (and counties) more than others, and why their trajectories often diverged in the 1990s. The causes of geographical disparities may be compositional, as when states became more populated by people with risk factors for midlife mortality (e.g., rural whites with limited education) or large, growing cities that skew state averages. State statistics are also influenced by demographic shifts (e.g., immigration, depopulation, and in-migration) and economic trends. For example, the divergence in life expectancy between Oklahoma and New York (Figure 7) may reflect the fate of different economies, one reliant on agriculture and mining and the other on service industries (e.g., finance, information technology). The clustering of midlife deaths in certain states, such as recent increases in upper New England states or rural areas, may reflect differences in drug abuse rates and in the distribution and marketing of illicit drugs.27,81,145,166,167,168
To some extent, however, divergent state health trajectories may reflect different policy choices.169 Policy differences seem more likely to explain disparities between adjacent states (e.g., Colorado/Kansas, Alabama/Georgia; Figure 7), where marked regional differences in demography or economies are uncommon. Many states diverged in the 1990s, soon after neoliberal policies aimed at free markets and devolution shifted resources (e.g., block grants) and authorities to the states.120,170,171,172 States enacted different policies on the social determinants of health, such as education spending, minimum wage laws, earned income tax credits, economic development, mass transit, safety net services, and public health provisions (e.g., tobacco taxes, Medicaid expansion, preemption laws, gun control).173,174,175,176,177,178 These decisions may have had health implications.179 For example, Dow et al. found that changes in state policies on minimum wage and earned income tax credits predicted non-drug suicide trends.180 In this study, the five states that experienced stable or reduced rates of firearm-related suicides during 1999–2017, countering the national trend, were those with stricter gun control laws.181
RESEARCH AND POLICY CONSIDERATIONS
Moving from speculation to evidence about root causes will require innovative research methods, including cohort studies, multivariate modeling, investigation of migration effects, and the application of machine learning to historical datasets. Fully understanding the timing of US mortality trends will also require interdisciplinary research involving epidemiology, demography, sociology, political science, history, economics, and the law. Clarifying the role of state policies may be especially important, given the divergent state trajectories reported here.
The implications of increasing midlife mortality are broad, affecting working-age adults and thus employers, the economy, health care, and national security. The trends also affect children, whose parents are more likely to die in midlife and whose own health could be at risk when they reach that age, or sooner. Recent data suggest that all-cause mortality rates are increasing among those ages 15–19 years and 20–24 years (increasing from 44.8 deaths/100,000 to 51.5 deaths per 100,000 and from 83.4 deaths/100,000 to 95.6 deaths/100,000, respectively, during 2013–2017) (Figure 2). Evidence-based strategies to improve population health seem warranted, such as policies to promote education, increase household income, invest in communities, and expand access to health care, affordable housing, and transportation.182,183,184,185,186 The increase in mortality from substance abuse, suicides, and organ system diseases argues for strengthening of behavioral health services and the capacity of health systems to manage chronic diseases.187
LIMITATIONS
This review and analysis have several limitations. First, mortality data are subject to errors, among them inaccurate ascertainment of cause of death, race misclassification and undercounting, and numerator-denominator mismatching.188,189 These are especially problematic in interpreting AIAN mortality rates, although disparities persist in this population even in studies that circumvent these challenges.190 Other limitations include the weak statistical power of annual state mortality rates and their inability to account for sub-state variation, the limits of age adjustment, age-aggregation bias, and the omission of cause-specific mortality data from before 1999.191 Purported rate increases may also reflect lagged selection bias.192 Second, errors in coding, such as the misclassification of suicides as overdoses193, or changes (or geographic differences) in coding practices could also introduce errors. For example, some increases in maternal mortality rates may reflect heightened surveillance and the addition of a pregnancy checkbox on death certificates.194,195,196 Changes in coding or awareness may explain the increase in age-adjusted mortality rates from mental and nervous system disorders, an international trend.197 Third, state mortality rates may also reflect demographic changes, such as immigration patterns (and the immigrant paradox198,199,200) or the out-migration of highly educated, healthy individuals.5
CONCLUSION
US life expectancy increased for most of the past 60 years, but the rate of increase slowed over time and life expectancy decreased after 2014. A major contributor has been an increase in mortality from specific causes (e.g., drug overdoses, suicides, organ system diseases) among young and middle-aged adults of all racial groups, which began as early as the 1990s and produced the largest relative increases in the Ohio Valley and New England. The implications for public health and the economy are substantial, making it vital to understand the root causes.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Latoya Hill, MPH and Christine M. Orndahl, BS for sharing their expertise with the Joinpoint Regression Program and for their extensive assistance with data analysis and mapping. This project was partially funded by grant R01AG055481-03 from the National Institute on Aging.
REFERENCES
- 1.Riley JC. Rising Life Expectancy: A Global History. Cambridge University Press; 2001. June 4. [Google Scholar]
- 2.Murphy SL, Xu JQ, Kochanek KD, Arias E. Mortality in the United States, 2017 NCHS Data Brief, no 328 Hyattsville, MD: National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- 3.Bernstein L. U.S. life expectancy declines again, a dismal trend not seen since World War I. Washington Post, November 21, 2018. [Google Scholar]
- 4.Woolf SH, Aron LY. The US health disadvantage relative to other high-income countries: findings from a National Research Council/Institute of Medicine report. JAMA. 2013;309:771–2. [DOI] [PubMed] [Google Scholar]
- 5.Muennig PA, Reynolds M, Fink DS, Zafari Z, Geronimus AT. America’s declining well-being, health, and life expectancy: not just a white problem. Am J Public Health. 2018;108(12):1626–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crimmins EM, Preston SH, Cohen B, eds. International Differences in Mortality at Older Ages: Dimensions and Sources National Research Council and Committee on Population. Washington, DC: National Academies Press, 2011. [PubMed] [Google Scholar]
- 7.Woolf SH, Aron L, eds. U.S. Health in International Perspective: Shorter Lives, Poorer Health. Panel on Understanding Cross-National Health Differences Among High-Income Countries National Research Council, Committee on Population, Division of Behavioral and Social Sciences and Education, and Board on Population Health and Public Health Practice, Institute of Medicine. Washington, DC: The National Academies Press, 2013. [PubMed] [Google Scholar]
- 8.Woolf SH, Aron L. Failing health of the United States. BMJ. 2018;360:k496. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. Health, United States, 2017: With Special Feature on Mortality. Hyattsville, MD: National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- 10.Ho JY, Hendi AS. Recent trends in life expectancy across high income countries: retrospective observational study. BMJ. 2018;362:k2562. doi: 10.1136/bmj.k2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Acciai F, Firebaugh G. Why did life expectancy decline in the United States in 2015? A gender-specific analysis. Soc Sci Med. 2017;190:174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018; 319(10):1024–1039. [DOI] [PubMed] [Google Scholar]
- 13.Muennig PA, Glied SA. What changes in survival rates tell us about us health care. Health Aff (Millwood). 2010;29(11):2105–13. [DOI] [PubMed] [Google Scholar]
- 14.Arias E. United States life tables, 2008 National Vital Statistics Reports; Vol 61 No 3 Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 15.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. World Health Organization, 1992. [Google Scholar]
- 16.National Center for Health Statistics. Underlying Cause of Death 1999–2017. Accessed 9-6-19 at https://wonder.cdc.gov/wonder/help/ucd.html#Top15.
- 17.National Center for Health Statistics. Table 15. Life expectancy at birth, at age 65, and at age 75, by sex, race, and Hispanic origin: United States, selected years 1900–2016. Accessed 3-26-19 at https://www.cdc.gov/nchs/hus/contents2017.htm?search=Life_expectancy
- 18.United States Mortality Database. University of California, Berkeley (USA). Available at usa.mortality.org (data downloaded on 3-5-19)
- 19.Barbieri M. Overview of the United States Mortality DataBase (USMDB). Society of Actuaries, 2018. [Google Scholar]
- 20.Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999–2017 on CDC WONDER Online Database, released December, 2018.
- 21.US Census Bureau. About Race. Accessed 9-23-19 at https://www.census.gov/topics/population/race/about.html
- 22.Joinpoint Regression Program, Version 4.7.0.0 – February 2019; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute.
- 23.National Cancer Institute. BIC3. Surveillance Research Program. Accessed 9-23-19 at https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/model-selection-method/bic-3
- 24.Elie C, De Rycke Y, Jais J, Landais P. Appraising relative and excess mortality in population-based studies of chronic diseases such as end-stage renal disease. Clin Epidemiol. 2011;3:157–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woolf SH, Johnson RE, Fryer GE Jr, Rust G, Satcher D. The health impact of resolving racial disparities: an analysis of US mortality data. Am J Public Health 2004;94:2078–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Woolf SH, Chapman DA, Buchanich JM, Bobby KJ, Zimmerman EB, Blackburn SM. Changes in midlife death rates across racial and ethnic groups in the United States: systematic analysis of vital statistics. BMJ. 2018;362:k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005. 5;331(7524):1064–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wohlin C. Guidelines for snowballing in systematic literature studies and a replication in software engineering Proceedings of the 18th International Conference on Evaluation and Assessment in Software Engineering. Article No. 38. New York: Association for Computing Machinery, 2014. 10.1145/2601248.2601268 [DOI] [Google Scholar]
- 29.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65:1445–52. [DOI] [PubMed] [Google Scholar]
- 30.Masters RK, Tilstra AM, Simon DH. Explaining recent mortality trends among younger and middle-aged White Americans. Int J Epidemiol. 2018;47(1):81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stein EM, Gennuso KP, Ugboaja DC, Remington PL. The epidemic of despair among white Americans: trends in the leading causes of premature death, 1999–2015. Am J Public Health 2017;107:1541–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.US Burden of Disease Collaborators, et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elo I, Hendi AS, Ho JY, Vierboom YC, Preston SH. Trends in non-Hispanic white mortality in the United States by metropolitan-nonmetropolitan status and region, 1990–2016. Popul Dev Rev. 2019. doi: 10.1111/padr.12249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kochanek KD, Arias E, Bastian BA. The effect of changes in selected age-specific causes of death on non-Hispanic white life expectancy between 2000 and 2014. NCHS Data Brief. 2016;(250):1–8. [PubMed] [Google Scholar]
- 35.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Pap Econ Act. 2017;2017:397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ruhm CJ. Drug mortality and lost life years among U.S. midlife adults, 1999–2015. Am J Prev Med. 2018;55(1):11–18. [DOI] [PubMed] [Google Scholar]
- 37.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shiels MS, Chernyavskiy P, Anderson WF, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet. 2017;389:1043–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miron O, Yu KH, Wilf-Miron R, Kohane IS. Suicide rates among adolescents and young adults in the United States, 2000–2017. JAMA. 2019;321(23):2362–2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shah NS, Lloyd-Jones DM, O’Flaherty M, et al. Trends in cardiometabolic mortality in the United States, 1999–2017. JAMA. 2019;322(8):780–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Squires D, Blumenthal D. Mortality Trends Among Working-Age Whites: The Untold Story. Issue Brief (Commonw Fund) 2016;3:1–11. [PubMed] [Google Scholar]
- 42.Astone NM, Martin S, Aron L. Death Rates for US Women Ages 15 to 54: Some Unexpected Trends. Washington, DC: Urban Institute, 2015. [Google Scholar]
- 43.Montez JK, Zajacova A. Explaining the widening education gap in mortality among U.S. white women. J Health Soc Behav. 2013;54:166–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Montez JK, Zajacova A. Why is life expectancy declining among low-educated women in the United States? Am J Public Health. 2014;104(10):e5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kindig DA, Cheng ER. Even as mortality fell in most US counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Aff (Millwood). 2013;32:451–8. [DOI] [PubMed] [Google Scholar]
- 46.National Academy of Sciences, Engineering, and Medicine. Improving the Health of Women in the United States: Workshop Summary. Washington, DC: National Academies Press, 2016. [PubMed] [Google Scholar]
- 47.Espey DK, Jim MA, Cobb N, et al. Leading causes of death and all-cause mortality in American Indians and Alaska Natives. Am J Public Health. 2014;104(S3):S303–S311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH. Vital signs: racial disparities in age-specific mortality among Blacks or African Americans--United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2017;66(17):444–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999–2015. NCHS Data Brief. 2017;(273):1–8. [PubMed] [Google Scholar]
- 50.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;67:1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Woolf SH, Braveman P. Where health disparities begin: the role of social and economic determinants—and why current policies could make matters worse. Health Affairs. 2011;30:1852–9. [DOI] [PubMed] [Google Scholar]
- 52.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100(Suppl 1):S186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Halliday TJ. Earnings growth and movements in self‐reported health. Review of Income and Wealth. 2017;63(4):760–76. [Google Scholar]
- 54.Ruckert A, Labonté R. Health inequities in the age of austerity: the need for social protection policies. Soc Sci Med. 2017;187:306–311 [DOI] [PubMed] [Google Scholar]
- 55.Benach J, Vives A, Amable M, Vanroelen C, Tarafa G, Muntaner C. Precarious employment: understanding an emerging social determinant of health. Annu Rev Public Health. 2014;35:229–53. [DOI] [PubMed] [Google Scholar]
- 56.Meraya AM, Dwibedi N, Tan X, Innes K, Mitra S, Sambamoorthi U. The dynamic relationships between economic status and health measures among working-age adults in the United States. Health Econ. 2018;27(8):1160–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Braveman P, Acker J, Arkin E, et al. Wealth Matters for Health Equity: Executive Summary. Princeton, NJ: Robert Wood Johnson Foundation, 2018. [Google Scholar]
- 58.Toffolutti V, Suhrcke M. Does austerity really kill? Econ Hum Biol. 2019;33:211–223 [DOI] [PubMed] [Google Scholar]
- 59.Jemal A, Ward E, Anderson RN, Murray T, Thun MJ. Widening of socioeconomic inequalities in US death rates, 1993–2001. PLoS ONE. 2008;3(5):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Aff (Millwood). 2008;27(2):350–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cristia JP. Rising mortality and life expectancy differentials by lifetime earnings in the United States. J Health Econ. 2009;28(5):984–95. [DOI] [PubMed] [Google Scholar]
- 62.Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood). 2012;31(8):1803–13. [DOI] [PubMed] [Google Scholar]
- 63.Montez JK, Zajacova A. Trends in mortality risk by education level and cause of death among US White women from 1986 to 2006. Am J Public Health. 2013;103(3):473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.National Academies of Sciences, Engineering and Medicine. The Growing Gap in Life Expectancy by Income: Implications for Federal Programs and Policy Responses. Washington, DC: National Academies Press, 2015. [PubMed] [Google Scholar]
- 65.Sasson I. Trends in life expectancy and lifespan variation by educational attainment: United States, 1990–2010. Demography. 2016;53:269–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gaydosh L, Hummer RA, Hargrove TW, et al. The depths of despair among US adults entering midlife. Am J Public Health. 2019;109(5):774–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sasson I, Hayward MD. Association between educational attainment and causes of death among white and black US adults, 2010–2017. JAMA. 2019;322(8):756–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kinge JM, Modalsli JH, Øverland S, et al. Association of household income with life expectancy and cause-specific mortality in Norway, 2005–2015. JAMA. 2019. doi: 10.1001/jama.2019.4329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Monnat SM. Factors associated with county-level differences in U.S. drug-related mortality rates. Am J Prev Med. 2018;54(5):611–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Woolf SH, Chapman DA, Buchanich JM, et al. Why Are Death Rates Rising Among Whites in California? The Role of Stress-Related Conditions. Richmond: Center on Society and Health, Virginia Commonwealth University, 2017. [Google Scholar]
- 72.Woolf SH, Chapman DA, Buchanich JM, et al. Why Are Death Rates Rising Among Whites in Missouri? The Role of Stress-Related Conditions. Richmond: Center on Society and Health, Virginia Commonwealth University, 2017. [Google Scholar]
- 73.Woolf SH, Chapman DA, Buchanich JM, et al. Why Are Death Rates Rising in Virginia’s White Population? The Role of Stress-Related Conditions. Richmond: Center on Society and Health, Virginia Commonwealth University, 2018. [Google Scholar]
- 74.Stobbe M. Opioid epidemic shares chilling similarities with past drug crises. Associated Press, October 29, 2017. Accessed 9-11-19 at https://www.statnews.com/2017/10/29/opioid-epidemic-shares-chilling-similarities-with-past-drug-crises/ [Google Scholar]
- 75.Cohen A. How white users made heroin a public health problem. The Atlantic, August 12, 2015. Accessed 9-11-19 at https://www.theatlantic.com/politics/archive/2015/08/crack-heroin-and-race/401015/ [Google Scholar]
- 76.Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361(6408). pii: eaau1184. doi: 10.1126/science.aau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users - United States, 2002–2013. MMWR Morb Mortal Wkly Rep. 2015;64(26):719–25. [PMC free article] [PubMed] [Google Scholar]
- 78.Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019. February 1 pii: S0955-3959(19)30018-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dowell D, Noonan RK, Houry D. Underlying factors in drug overdose deaths. JAMA. 2017;318(23):2295–2296. doi: 10.1001/jama.2017.15971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78. [DOI] [PubMed] [Google Scholar]
- 81.Spencer MR, Warner M, Bastian BA, Trinidad JP, Hedegaard H. Drug overdose deaths involving fentanyl, 2011–2016 National Vital Statistics Reports; Vol 68 no 3 Hyattsville, MD: National Center for Health Statistics; 2019. [PubMed] [Google Scholar]
- 82.Rigg KK, Monnat SM, Chavez MN. Opioid-related mortality in rural America: Geographic heterogeneity and intervention strategies. Int J Drug Policy. 2018;57:119–129. [DOI] [PubMed] [Google Scholar]
- 83.Stone DM, Simon TR, Fowler KA, et al. Vital signs: trends in state suicide rates — United States, 1999–2016 and circumstances contributing to suicide — 27 states, 2015. MMWR Morb Mortal Wkly Rep. 2018;67:617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ho JY. The contemporary American drug overdose epidemic in international perspective. Popul Dev Rev. 2019, 45:7–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barbieri M. The contribution of drug-related deaths to the US disadvantage in mortality. Int J Epidemiol. 2019;48(3):945–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.World Health Organization. WHO Mortality Database, accessed 9-13-19 at http://apps.who.int/healthinfo/statistics/mortality/whodpms/.
- 87.Staetsky L. Diverging trends in female old-age mortality: A reappraisal. Demographic Research. 2009;21(30):885–914. [Google Scholar]
- 88.Fenelon A, Preston SH. Estimating smoking-attributable mortality in the United States. Demography. 2012;49(3):797–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Preston SH, Glei DA, Wilmoth JR. Contribution of smoking to international differences in life expectancy In: Crimmins EM, Preston SH, Cohen B, eds. International Differences in Mortality at Older Ages: Dimensions and Sources National Research Council and Committee on Population. Washington, DC: National Academies Press, 2011, 105–131. [PubMed] [Google Scholar]
- 90.Fenelon A. Geographic divergence in mortality in the United States. Popul Dev Rev. 2013;39(4):611–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jiang J, Ahn J, Huang WY, Hayes RB. Association of obesity with cardiovascular disease mortality in the PLCO trial. Prev Med. 2013;57(1):60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kovesdy CP, Furth SL, Zoccali C; World Kidney Day Steering Committee. Obesity and kidney disease: hidden consequences of the epidemic. Can J Kidney Health Dis. 2017;4: 10.1177/2054358117698669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–45. [DOI] [PubMed] [Google Scholar]
- 94.Preston SH, Vierboom YC, Stokes A. The role of obesity in exceptionally slow US mortality improvement. Proc Natl Acad Sci U S A. 2018;115:957–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gay J, Devaux M, de Looper M, Paris V. Mortality Amenable to Health Care in 31 OECD countries: Estimates and Methodological Issues. (No. 55, OECD Health Working Papers). Paris: OECD, 2011. [Google Scholar]
- 96.Mossialos E, Djordjevic A, Osborn R, Sarnak D, eds. International Profiles of Health Care Systems. New York: The Commonwealth Fund, 2017. [Google Scholar]
- 97.GBD 2016 Healthcare Access and Quality Collaborators. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391(10136):2236–2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rae M, Copeland R, Cox C. Tracking the Rise in Premium Contributions and Cost-Sharing for Families with Large Employer Coverage. Peterson-Kaiser Health System Tracker, August 14, 2019. Accessed 9-13-19 at https://www.healthsystemtracker.org/brief/tracking-the-rise-in-premium-contributions-and-cost-sharing-for-families-with-large-employer-coverage/ [Google Scholar]
- 99.Adams EK, Johnston EM, Guy G, Joski P, Ketsche P. Children’s Health Insurance Program expansions: what works for families? Glob Pediatr Health. 2019;6:2333794X19840361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Madras BK. The surge of opioid use, addiction, and overdoses: responsibility and response of the US health care system. JAMA Psychiatry. 2017;74(5):441–442. [DOI] [PubMed] [Google Scholar]
- 101.Graham C, Pinto S. Unequal hopes and lives in the USA: optimism, race, place, and premature mortality. J Popul Econ. 2019;32:665–733 [Google Scholar]
- 102.Zack MM, Moriarty DG, Stroup DF, Ford ES, Mokdad AH. Worsening trends in adult health-related quality of life and self-rated health-United States, 1993–2001. Public Health Rep. 2004;119(5):493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Salomon JA, Nordhagen S, Oza S, Murray CJ. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol. 2009;170(3):343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018;48(8):1308–1315. [DOI] [PubMed] [Google Scholar]
- 105.Goldman N, Glei DA, Weinstein M. Declining mental health among disadvantaged Americans. Proc Natl Acad Sci U S A. 2018. July 10;115(28):7290–7295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Blue Cross Blue Shield. Major Depression: The Impact on Overall Health. Accessed 5-2-19 at https://www.bcbs.com/the-health-of-america/reports/major-depression-the-impact-overall-health [PDF in folder]
- 107.Twenge JM, Gentile B, DeWall CN, Ma D, Lacefield K, Schurtz DR. Birth cohort increases in psychopathology among young Americans, 1938–2007: A cross-temporal meta-analysis of the MMPI. Clin Psychol Rev. 2010;30(2):145–54. [DOI] [PubMed] [Google Scholar]
- 108.Twenge JM. Time period and birth cohort differences in depressive symptoms in the US, 1982–2013. Social Indicators Research. 2015;121(2):437–54. [Google Scholar]
- 109.Davis MA, Lin LA, Liu H, Sites BD. Prescription opioid use among adults with mental health disorders in the United States. J Am Board Fam Med. 2017;30(4):407–417. [DOI] [PubMed] [Google Scholar]
- 110.Goesling J, Henry MJ, Moser SE, et al. Symptoms of depression are associated with opioid use regardless of pain severity and physical functioning among treatment-seeking patients with chronic pain. J Pain 2015;16:844–51. [DOI] [PubMed] [Google Scholar]
- 111.Goodridge D, Bandara T, Marciniuk D, et al. Promoting chronic disease management in persons with complex social needs: A qualitative descriptive study. Chron Respir Dis. 2019. Jan-Dec;16:1479973119832025. doi: 10.1177/1479973119832025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.McKewen B, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.McEwen BS. Neurobiological and systemic effects of chronic stress. Chronic Stress (Thousand Oaks). 2017. Jan-Dec;1. doi: 10.1177/2470547017692328. Epub 2017 Apr 10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Crettaz B, Marziniak M, Willeke P, et al. Stress-induced allodynia--evidence of increased pain sensitivity in healthy humans and patients with chronic pain after experimentally induced psychosocial stress. PLoS One. 2013. August 7;8(8):e69460. doi: 10.1371/journal.pone.0069460. eCollection 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Burke NN, Finn DP, McGuire BE, Roche M. Psychological stress in early life as a predisposing factor for the development of chronic pain: Clinical and preclinical evidence and neurobiological mechanisms. Add J Neurosci Res. 2017;95(6):1257–1270. [DOI] [PubMed] [Google Scholar]
- 116.Hidaka BH. Depression as a disease of modernity: explanations for increasing prevalence. J Affect Disord. 2012;140(3):205–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015;17(3):327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Olfson M, Wang S, Wall M, Marcus SC, Blanco C. Trends in serious psychological distress and outpatient mental health care of US adults. JAMA Psychiatry. 2018. November 28. doi: 10.1001/jamapsychiatry.2018.3550. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2018. [Google Scholar]
- 120.Monnat Shannon M. Deaths of Despair and Support for Trump in the 2016 Election. Penn State University; 2016. [Accessed May 18, 2017]. via: http://aese.psu.edu.proxy.library.vcu.edu/directory/smm67/Election16.pdf. [Google Scholar] [Google Scholar]
- 121.Labonté R, Stuckler D. The rise of neoliberalism: how bad economics imperils health and what to do about it. J Epidemiol Community Health. 2016;70(3):312–8. [DOI] [PubMed] [Google Scholar]
- 122.Cowie J. Stayin’ Alive: The 1970s and the Last Days of the Working Class. New Press; 2010. [Google Scholar]
- 123.Pew Research Center. The American Middle Class Is Losing Ground. Washington, DC: Pew Research Center, 2015. [Google Scholar]
- 124.Silva JM. We’re Still Here: Pain and Politics in the Heart of America. Oxford University Press; 2019. [Google Scholar]
- 125.Chen VT. Cut Loose: Jobless and Hopeless in an Unfair Economy. Univ of California Press; 2015. July 20. [Google Scholar]
- 126.Morris M, Western B. Inequality in earnings at the close of the 20th century. Ann Rev Sociol. 1999;25:623–57. [Google Scholar]
- 127.Lindert PH. Three centuries of inequality in Britain and America In: Atkinson AB, Bourguignon F, eds. Handbook of Income Distribution. Vol. 1 Amsterdam: Elsevier; 2000. pp. 167–216. [Google Scholar]
- 128.Saez E. Striking it Richer: The Evolution of Top Incomes in the United States. Berkeley: University of California, 2010. [Google Scholar]
- 129.Alvaredo F, Atkinson AB, Piketty T, Saez E. The top 1 percent in international and historical perspective. Journal of Economic Perspectives. 2013;27(3):3–20. [Google Scholar]
- 130.Monnat SM, Raffalovich LE, Tsao HS. Trends in the family income distribution by race/ethnicity and income source, 1988–2009. Popul Rev. 2012;51(1):85–115. [PMC free article] [PubMed] [Google Scholar]
- 131.Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389(10077):1475–1490. [DOI] [PubMed] [Google Scholar]
- 132.US Government Accountability Office. Retirement Security: Income and Wealth Disparities Continue Through Old Age. GAO 19–587. Washington, DC: US Government Accountability Office, 2019. [Google Scholar]
- 133.Fuguitt GV, Brown DL, Beale CL. Rural and Small Town America. New York: Russell Sage: 1989. [Google Scholar]
- 134.Monnat SM, Beeler Pickett C. Rural/urban differences in self-rated health: examining the roles of county size and metropolitan adjacency. Health Place. 2011. January;17(1):311–9. [DOI] [PubMed] [Google Scholar]
- 135.Alexander B. Glass house: the 1% economy and the shattering of the all-American town. St. Martin’s Press; 2017. February 14. [Google Scholar]
- 136.Goldstein A. Janesville: An American Story. Simon and Schuster, 2018. [Google Scholar]
- 137.Cohen N, Galea S. Population Mental Health: Evidence, Policy, and Public Health Practice. Taylor & Francis; 2011. [Google Scholar]
- 138.Dowd JB, Palermo T, Chyu L, Adam E, McDade TW. Race/ethnic and socioeconomic differences in stress and immune function in The National Longitudinal Study of Adolescent Health. Soc Sci Med. 2014;115:49–55. [DOI] [PubMed] [Google Scholar]
- 139.Weissman J, Pratt LA, Miller EA, Parker JD. Serious psychological distress among adults: United States, 2009–2013 NCHS Data Brief, No 203 Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 140.Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Coben JH, Tiesman HM, Bossarte RM, Furbee PM. Rural–urban differences in injury hospitalizations in the US Am J Prev Med. 2004;36(1):49–55. [DOI] [PubMed] [Google Scholar]
- 142.Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014:104(2):E52–E59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Payne K. The Broken Ladder: How Inequality Affects the Way We Think, Live, and Die. Penguin, 2017. [Google Scholar]
- 144.Leana C. The cost of financial precarity Stanford Innovation Review. Spring; 2019;42–47. [Google Scholar]
- 145.Hollingsworth A, Ruhm CJ, Simon K. Macroeconomic conditions and opioid abuse. J Health Econ. 2017;56:222–233. [DOI] [PubMed] [Google Scholar]
- 146.Ruhm CJ. Drivers of the fatal drug epidemic. J Health Econ. 2019;64:25–42. [DOI] [PubMed] [Google Scholar]
- 147.Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med. 2015;128:316–26. [DOI] [PubMed] [Google Scholar]
- 148.Coburn D. Income inequality, welfare, class and health: a comment on Pickett and Wilkinson, 2015. Soc Sci Med. 2015;146:228–32. [DOI] [PubMed] [Google Scholar]
- 149.Euteneuer F1. Subjective social status and health. Curr Opin Psychiatry. 2014;27(5):337–43. [DOI] [PubMed] [Google Scholar]
- 150.Cherlin A. You can’t separate money from culture. New York Times, May 6, 2018. Accessed 5-22-19 at https://www.nytimes.com/2018/05/06/opinion/trump-supporters-economy-racism.html [Google Scholar]
- 151.Lamont M, Lamont M. The Dignity of Working Men: Morality and the Boundaries of Race, Class, and Immigration. Harvard University Press, 2009. [Google Scholar]
- 152.Gest J. The New Minority: White Working-class Politics in an Age of Immigration and Inequality. New York, NY: Oxford University Press, 2016. [Google Scholar]
- 153.Metzl JM. Dying of Whiteness: How the Politics of Racial Resentment Is Killing America’s Heartland. Hachette UK, 2019. [Google Scholar]
- 154.Hochschild AR. Strangers in their Own Land: Anger and Mourning on the American Right. The New Press, 2018. [Google Scholar]
- 155.Putnam RD. Our Kids: The American Dream in Crisis. New York: Simon and Schuster, 2015. [Google Scholar]
- 156.Cherlin AJ. Psychological health and socioeconomic status among non-Hispanic whites. Proc Natl Acad Sci U S A. 2018;115(28):7176–7178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Blacksher E. Shrinking poor white life spans: class, race, and health justice. Am J Bioeth. 2018;18(10):3–14. [DOI] [PubMed] [Google Scholar]
- 158.Brown L, Tucker-Seeley R. Commentary: Will ‘deaths of despair’ among whites change how we talk about racial/ethnic health disparities? Ethn Dis. 2018;28(2):123–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Guo J. If white America is in ‘crisis,’ what have black Americans been living through? Washington Post Wonkblog, April 4, 2017. [Google Scholar]
- 160.Zoorob MJ, Salemi JL. Bowling alone, dying together: the role of social capital in mitigating the drug overdose epidemic in the United States. Drug Alcohol Depend. 2017;173:1–9. [DOI] [PubMed] [Google Scholar]
- 161.Cherlin AJ. You can’t separate money from culture. New York Times, May 6, 2018. [Google Scholar]
- 162.Putnam RD. Tuning in, tuning out: the strange disappearance of social capital in America. PS Political Sci Politics. 1995;28(4):664–683. [Google Scholar]
- 163.Putnam RD. Bowling Alone; America’s Declining Social Capital. New York: Simon & Schuster, 2001. [Google Scholar]
- 164.Zang E, Zheng H, Yang YC, Land KC. Recent trends in US mortality in early and middle adulthood: racial/ethnic disparities in inter-cohort patterns. Int J Epidemiol. 2019;48(3):934–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bradley EH, Elkins BR, Herrin J, Elbel B. Health and social services expenditures: associations with health outcomes. BMJ Qual Saf. 2011;20(10):826–31. [DOI] [PubMed] [Google Scholar]
- 166.Rigg KK, Monnat SM. Urban vs. rural differences in prescription opioid misuse among adults in the United States: informing region specific drug policies and interventions. Int J Drug Policy. 2015;26(5):484–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kiang MV, Basu S, Chen J, Alexander MJ. Assessment of changes in the geographical distribution of opioid-related mortality across the United States by opioid type, 1999–2016. JAMA Netw Open. 2019;2(2):e190040. doi: 10.1001/jamanetworkopen.2019.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Quinones S. Dreamland: The True Tale of America’s Opiate Epidemic. New York: Bloomsbury Press, 2015. [Google Scholar]
- 169.Zajacova A, Montez JK. Macro-level perspective to reverse recent mortality increases. Lancet. 2017;389(10073):991–992. [DOI] [PubMed] [Google Scholar]
- 170.Conlan TJ. From new federalism to devolution: twenty-five years of intergovernmental reform. Brookings Institution Press; 2010. December 1. [Google Scholar]
- 171.Montez JK, Zajacova A, Hayward MD. Explaining inequalities in women’s mortality between U.S. states. SSM Popul Health. 2016;2:561–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Montez JK. Deregulation, devolution, and state preemption laws’ impact on U.S. mortality trends. Am J Public Health. 2017. 107, 1749–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: Mechanisms and causal evidence. Ann N Y Acad Sci. 2010. February;1186:56–68. [DOI] [PubMed] [Google Scholar]
- 174.Muennig PA, Mohit B, Wu J, Jia H, Rosen Z. Cost effectiveness of the earned income tax credit as a health policy investment. Am J Prev Med. 2016;51(6):874–881. [DOI] [PubMed] [Google Scholar]
- 175.Bhatt CB, Beck-Sagué CM. Medicaid expansion and infant mortality in the United States. Am J Public Health. 2018;108(4):565–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Pew Charitable Trusts. Colorado Dives into Evidence-Based Policymaking. Issue brief, 2018. Accessed 6-4-19 at https://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2018/13/colorado-dives-into-evidence-based-policymaking
- 177.Montez JK, Zajacova A, Hayward MD, Woolf SH, Chapman D, Beckfield J. Educational disparities in adult mortality across U.S. states: how do they differ, and have they changed since the mid-1980s? Demography. 2019;56(2):621–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Pomeranz JL, Pertschuk M. State preemption: a significant and quiet threat to public health in the United States. Am J Public Health. 2017;107:900–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Sullivan J. Better State Budget, Policy Decisions Can Improve Health. Washington, DC: Center on Budget and Policy Priorities, 2019. Accessed 7-10-19 at https://www.cbpp.org/research/state-budget-and-tax/better-state-budget-policy-decisions-can-improve-health [Google Scholar]
- 180.Dow WH, Godoy A, Lowenstein CA, Reich M. Can Economic Policies Reduce Deaths of Despair? NBER Working Paper No. 25787. Cambridge, MA: National Bureau of Economic Research, 2019. [Google Scholar]
- 181.Giffords Law Center to Prevent Gun Violence. Annual gun law scorecard (website). https://lawcenter.giffords.org/scorecard/
- 182.Project Hope. Health Policy Briefs (website). Health Affairs, accessed 6-1-19 at https://www.healthaffairs.org/briefs
- 183.Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health Final report of the Commission on Social Determinants of Health. Geneva: World Health Organization, 2008. [Google Scholar]
- 184.Malmusi D, Borrell C. Social and Economic Policies Matter for Health Equity. Barcelona: Addenda, 2015. [DOI] [PubMed] [Google Scholar]
- 185.Centers for Disease Control and Prevention. Community Guide (website). Community Task Force on Preventive Services. https://www.thecommunityguide.org/
- 186.Lustig A, Cabrera M. Promoting Health and Cost Control in States: How States Can Improve Community Health & Well-being through Policy Change. Washington, DC: Trust for America’s Health, 2019. [Google Scholar]
- 187.Jonas WB, Schoomaker E, Marzolf JR, Gaudet T. Finding the cause of the crises: opioids, pain, suicide, obesity, and other “epidemics.” NEJM Catalyst, May 15, 2019. Accessed 5-22-19 at https://catalyst.nejm.org/cause-crises-whole-health-whole-person/ [Google Scholar]
- 188.Arias E, Schauman WS, Eschbach K, et al. The validity of race and Hispanic origin reporting on death certificates in the United States. National Center for Health Statistics. Vital Health Stat. 2008;2(148). [PubMed] [Google Scholar]
- 189.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: A summary of current research, 1999. National Center for Health Statistics. Vital Health Stat. 2(128). 1999. [PubMed] [Google Scholar]
- 190.Sancar F, Abbasi J, Bucher K. Mortality among American Indians and Alaska Natives. JAMA. 2018;319(2):112. [DOI] [PubMed] [Google Scholar]
- 191.Gelman A, Auerbach J. Age-aggregation bias in mortality trends. Proc Natl Acad Sci USA. 2016;113(7):E816–E817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Dowd JB, Hamoudi A. Is life expectancy really falling for groups of low socio-economic status? Lagged selection bias and artefactual trends in mortality. Int J Epidemiol. 2014;43(4):983–8. [DOI] [PubMed] [Google Scholar]
- 193.Rockett IRH, Connery HS. Variation in deaths from intentional injury and substance use. JAMA. 2018;320(6):601. [DOI] [PubMed] [Google Scholar]
- 194.Davis NL, Hoyert DL, Goodman DA, Hirai AH, Callaghan WM. Contribution of maternal age and pregnancy checkbox on maternal mortality ratios in the United States, 1978–2012. Am J Obstet Gynecol. 2017;217(3):352.e1–352.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Joseph KS, Lisonkova S, Muraca GM, et al. Factors underlying the temporal increase in maternal mortality in the United States. Obstet Gynecol. 2017;129(1):91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.MacDorman MF, Declercq E, Thoma ME. Trends in maternal mortality by sociodemographic characteristics and cause of death in 27 states and the District of Columbia. Obstet Gynecol. 2017;129(5):811–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Mackenbach JP, Karanikolos M, Looman CWN. The rise of mortality from mental and neurological diseases in Europe, 1979–2009: Observational study. BMC Public Health. 2014. 14(1): 840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- 199.Hummer RA, Rogers RG. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Soc Sci Med. 2000;81:459–76. [PubMed] [Google Scholar]
- 200.Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, Davis D, Escamilla-Cejudo JA. Hispanic health in the USA: a scoping review of the literature. Public Health Rev. 2016;37:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


