Abstract
Background
Observational studies have shown differences in process and outcome between the consultations of primary care physicians whose average consultation lengths differ. These differences may be due to self selection. This is the first update of the original review.
Objectives
To assess the effects of interventions to alter the length of primary care physicians' consultations.
Search methods
We searched the following electronic databases until 4 January 2016: the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, ClinicalTrials.gov, and World Health Organization International Clinical Trials Registry Platform (WHO ICTRP).
Selection criteria
Randomised controlled trials and non‐randomised controlled trials of interventions to alter the length of primary care physicians' consultations.
Data collection and analysis
Two review authors independently extracted data and assessed the risk of bias of included studies using agreed criteria and resolved disagreements by discussion. We attempted to contact authors of primary studies with missing data. Given the heterogeneity of studies, we did not conduct a meta‐analysis. We assessed the certainty of the evidence for the most important outcomes using the GRADE approach and have presented the results in a narrative summary.
Main results
Five studies met the inclusion criteria. All were conducted in the UK, and tested short‐term changes in the consultation time allocated to each patient. Overall, our confidence in the results was very low; most studies had a high risk of bias, particularly due to non‐random allocation of participants and the absence of data on participants' characteristics and small sample sizes. We are uncertain whether altering appointment length increases primary care consultation length, number of referrals and investigations, prescriptions, or patient satisfaction based on very low‐certainty evidence. None of the studies reported on the effects of altering the length of consultation on resources used.
Authors' conclusions
We did not find sufficient evidence to support or refute a policy of altering the lengths of primary care physicians' consultations. It is possible that these findings may change if high‐quality trials are reported in the future. Further trials are needed that focus on health outcomes and cost‐effectiveness.
Plain language summary
Effects of interventions aimed at changing the length of time of consultations between family doctors and patients
Review question
Does increasing or decreasing the length of time that primary care physicians allocate to each patient consultation benefit patients, doctors, and the healthcare system?
Background
Doctors not having enough time with patients during consultations has been a matter of concern. It has been suggested that if doctors and patients had more time to talk, then patients might be more satisfied with care and their problems better dealt with, or doctors might prescribe less and talk more about how to make lifestyle changes.
Study characteristics
We identified five studies conducted in the UK that tested whether methods to change consultation length for family doctors provides any benefit. The studies were conducted in single or multiple practices, and the number of appointments ranged from 200 to 2957 consultations. Four studies compared a change in appointment times from 5 to 15 minutes, and one study compared short versus long consultations with or without treatment for patients with no diagnosis.
Key results
All studies tested short‐term changes in the consultation time allocated to each patient. Our confidence in the results of these studies is very low. Consequently, we are not certain whether changing appointment slots leads to an actual increase of the length of the consultation, number of referrals and investigations requested by the doctor, and number of medications prescribed. Likewise, it is unclear whether patients are more satisfied with the health care they receive when appointments are longer. None of the studies reported on the resources associated with lengthening appointments.
Authors' conclusions
There is currently not enough evidence to say whether altering the amount of time that doctors consult with patients provides benefits or not.
Summary of findings
Summary of findings for the main comparison. Altered length compared to usual length for increasing the length of primary care physicians' consultations.
| Altered length compared to usual length for increasing the length of primary care physicians' consultations | |||
| Patient or population: primary care physicians Setting: UK Intervention: increase or decrease in consultation length Comparison: routine consultation length | |||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) |
| Provider performance ‐ length of consultation | It is uncertain whether altering the length of consultations increases the length of primary care physicians’ consultations In all trials the difference in consultation length was less than the change in appointment length, particularly when appointment length was extended |
23 primary care physicians (3 observational studies) |
⊕⊝⊝⊝ Very low 1, 2 |
| Provider performance ‐ referrals | It is uncertain whether altering the length of consultations increases primary care physicians’ referrals The 2 trials assessing the percentage of consultations resulting in specialist referrals found similar results for all groups, although rates were slightly higher with longer appointments |
21 primary care physicians (2 observational studies) |
⊕⊝⊝⊝ Very low 1, 2 |
| Provider performance ‐ examinations | It is uncertain whether altering the length of consultations increases primary care physicians’ examinations 3 trials assessed the percentage of consultations in which 1 or more physical examinations took place |
23 primary care physicians (3 observational studies) | ⊕⊝⊝⊝ Very low 1, 2 |
| Provider performance ‐ prescriptions | It is uncertain whether altering the length of consultations increases primary care physicians’ prescriptions 3 trials assessed the percentage of consultations in which prescriptions were issued |
23 primary care physicians (3 observational studies) |
⊕⊝⊝⊝ Very low 1, 2 |
| Patient satisfaction | It is uncertain whether altering the length of consultations increases patient satisfaction 4 trials assessed patient satisfaction with the care received, none of which used a validated instrument |
43 primary care physicians (4 observational studies) |
⊕⊝⊝⊝ Very low 1, 2,3 |
| Resources ‐ not measured | No studies reported on the effect of altering the length of consultations on resources | (0 studies) | ‐ |
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||
1Downgraded 1 point due to high risk of bias (allocation and selective sampling). 2Downgraded 1 point due to small sample size. 3Downgraded 1 point due to non‐validated assessment (surrogate outcome).
Background
Description of the condition
The brevity of consultations with primary care physicians is a concern of both doctors and the public (Cartwright 1981; Ogden 2004). In a survey of primary care physicians in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, the UK, and the US, over one‐third of physicians reported being somewhat dissatisfied or very dissatisfied with the time they spent per patient in their clinic (Commonwealth Fund 2015). In a recent survey, 24% of general practitioners (GPs) in England agreed that all appointments should be longer than 10 minutes, and 68% agreed that longer appointments should be offered to select groups of patients (BMA 2015).
Description of the intervention
There are marked differences in average consultation length between countries and healthcare systems; for example consultations being longer in the US (Shaw 2014), Belgium, and Switzerland (Deveugele 2002), than in the UK (RCGP 2013), the Netherlands (van den Berg 2009), Germany, and Spain (Deveugele 2002). In England, between 2007/2008 and 2013/2014, the mean length of face‐to‐face GP consultations increased from 8.65 minutes to 9.22 minutes (Hobbs 2016). However, such increases in consultation length may not be sufficient to match increasing demands, such as the need for health promotion and chronic disease management, especially in ageing, multimorbid, and deprived populations (Mercer 2007). But increasing consultation length incurs extra costs and, if not associated with a commensurate increase in effectiveness, would reduce efficiency.
How the intervention might work
The focus of this review was length of consultation, but it is likely that interventions to increase or decrease this will do so by altering the length of appointments. It is known that GPs tend to 'over‐run', that is see patients later than their appointment time, with between one‐fifth and one‐fourth of primary care patients reporting waiting more than 30 minutes for their appointment (Anderson 2007; Potiriadis 2008). Factors contributing to this may include spending more time with patients than is allotted or waiting more time than is allowed for between patients, for example in recordkeeping, or both.
Why it is important to do this review
A non‐systematic review found some observational evidence that doctors whose average consultation length was longer had lower prescribing rates and higher levels of patient satisfaction (Wilson 1991). Results from intervention studies where doctors consulted under different time conditions were less consistent. A further systematic review of observational studies reporting associations between length of consultation and consultation processes and outcome found that doctors who had longer consultations tended to prescribe less, give more lifestyle advice and health promotion, and achieve higher levels of patient satisfaction and enablement (Wilson 2002). However, there may be several confounding factors, such as doctor's style and orientation, that mean that average consultation is simply a marker of other more important attributes that are not amenable to change by extending average consultation length. These could include such elements as trust and patient‐centredness, which have been examined in other Cochrane reviews (Dwamena 2012; Rolfe 2014). This is the first update of the original review (Wilson 2006).
Objectives
To assess the effects of interventions to alter the length of primary care physicians' consultations.
Methods
Criteria for considering studies for this review
Types of studies
Intervention studies using the following designs/methodologies:
randomised controlled trials (RCTs);
non‐randomised controlled trials (NRCTs).
As a previous systematic review identified a scarcity of RCTs within this topic of research (Wilson 2002), we considered that additional relevant evidence would be gathered from NRCTs. We considered NRCTs to be any experimental study in which people are allocated to different interventions using non‐random methods (EPOC 2013c)
Types of participants
Primary care physicians, defined broadly as any medically qualified physician who provides primary health care. Primary health care provides "integrated, easy to access, healthcare services by clinicians who are accountable for addressing a large majority of personal healthcare needs, developing a sustained and continuous relationship with patients, and practising in the context of family and community" (Vanselow 1995, p192). Terms for primary care physicians differ according to setting, and include general practitioners, family doctors, family physicians, family practitioners, and other physicians working in primary health care settings and who fulfil primary health care tasks.
Types of interventions
Any intervention to alter consultation length. We did not include interventions involving changes in standard appointment length if there was no aim to alter consultation length or those that examined the effect of a single extended appointment. We excluded studies conducted with secondary care medical practitioners or with non‐medical primary care professionals.
Types of outcome measures
Main outcomes
Provider performance (e.g. consultation length, prescribing, investigation, referral rates)
Patient satisfaction with care
Other outcomes
Healthcare behaviours (e.g. adherence to care plans)
Health status outcomes
Resources associated with the intervention
For all of the above outcomes we sought information about how sustainable any reported changes were over time.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases on 4 January 2016.
Cochrane Central Register of Controlled Trials (CENTRAL) (2015, Issue 12, part of the Cochrane Library) (including Cochrane Effective Practice and Organisation of Care (EPOC) Group Specialised Register)
MEDLINE, In‐Process and Other Non‐Indexed Citations and Ovid MEDLINE 1946 to 4 January 2016, OvidSP
EMBASE, 1974 to 31 December 2015, OvidSP
ClinicalTrials.gov, 2000 to 4 January 2016
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP), 2007 to 4 January 2016
The Effective Practice and Organisation of Care (EPOC) Group Information Specialist developed the search strategies in consultation with the review authors. We have presented search strategies in Appendix 1.
Searching other resources
We searched Science Citation Index for forward citations of the studies included in the original version of the review (Wilson 2006), and PDQ‐Evidence for related systematic reviews.
Data collection and analysis
Selection of studies
One review author (DGB) screened all references, excluding those that were not eligible based on the inclusion criteria. Two review authors (DGB, ADW) then independently applied these criteria to the references shortlisted for full‐text screening. Any disagreements were resolved by discussion.
Data extraction and management
Two review authors (ADW, SC) independently extracted data on study characteristics using agreed‐upon criteria, resolving any disagreements by discussion.
Assessment of risk of bias in included studies
Two review authors (DGB, GJI) independently assessed the risk of bias using standard Cochrane and EPOC criteria for RCTs and NRCTs (EPOC 2013):
adequate sequence generation;
allocation concealment;
blinding (performance and detection bias);
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective reporting; and
free of other bias, namely baseline outcomes.
We did not set thresholds for inclusion. We assessed risk of bias as high (authors describe the item and it does not meet EPOC criteria), low (authors describe item and it meets expected standards), or unclear (authors do not report relevant information), and prepared a summary table for each study, providing justification for our judgement.
Measures of treatment effect
We planned to analyse dichotomous data as odds ratio and continuous data as mean difference or standardised mean difference and 95% confidence interval. However, given the heterogeneity of the included studies, we did not pool data.
Unit of analysis issues
We did not anticipate any unit of analysis issues and did not encounter any issues related with study design, as we did not pool data for analysis.
Dealing with missing data
Where data were missing we attempted to contact authors.
Assessment of heterogeneity
We used the I² statistic to measure heterogeneity among the trials in each analysis (Higgins 2011).
Data synthesis
Given the heterogeneity of included studies, we did not perform a meta‐analysis. Instead, we summarised the results and characteristics of all included studies in tables. We created a 'Summary of findings' table using the following outcomes: provider performance (length of consultation, referrals and investigations, and prescriptions), patient satisfaction, and resources used. We employed the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the certainty of the evidence as it relates to the studies which contribute data to the prespecified outcomes (Guyatt 2008). We used methods and recommendations described by the EPOC group, in EPOC 2013b, and in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and used GRADEpro software (GRADEpro 2015). We justified all decisions to downgrade or upgrade the certainty of the evidence of studies using footnotes and made comments to aid readers' understanding of the review where necessary.
Subgroup analysis and investigation of heterogeneity
We did not plan to conduct a subgroup analysis and did not conduct a subgroup analysis a posteriori.
Sensitivity analysis
We did not plan to conduct a sensitivity analysis and did not conduct a subgroup analysis a posteriori.
Results
Description of studies
Results of the search
We retrieved 1717 records, of which we excluded 1712. We shortlisted five references for full‐text assessment, none of which were eligible for inclusion (Figure 1). For this update we identified no new studies and one ongoing study (ISRCTN34092919). The original review identified five studies (seven records), which we have included in this update.
1.
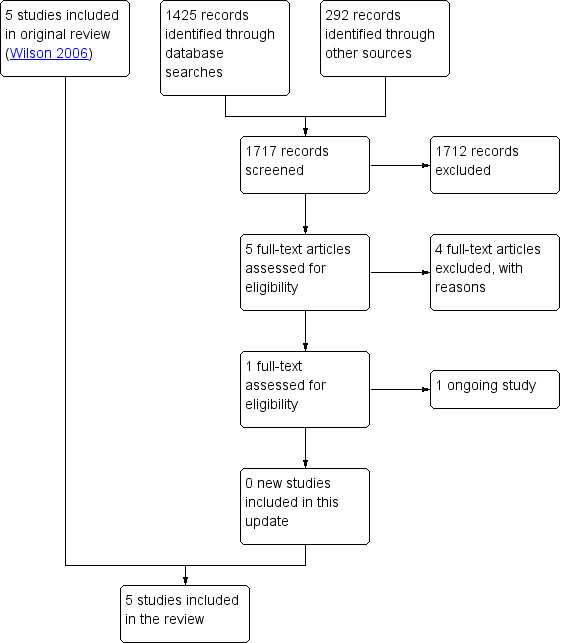
Flow diagram.
Included studies
We identified five eligible studies: two were RCTs (Edwards 2004; Thomas 1978), and three were NRCTs (Morrell 1986; Ridsdale 1989; Wilson 1992). All five studies were conducted in the UK (see Characteristics of included studies).
The earliest trial was conducted by a single general practitioner (GP) without an appointment system (Thomas 1978). He randomly allocated patients in whom no diagnosis could be made to one of four management options: short consultation and prescription; long consultation and prescription; short consultation, no prescription; long consultation, no prescription. Short consultations averaged 3.7 minutes, and long consultations were 10 minutes. The outcome measure was whether the patient returned within four weeks with either the same or a different complaint.
In a trial involving five doctors in one academic practice, patients were allocated non‐randomly to consulting sessions of appointment lengths of 5, 7.5, or 10 minutes, spread over representative times of the day and days of the week (Morrell 1986). Process measures included consultation length, number of problems and psychological problems recorded, rates of examination, prescribing, investigation and referral, and verbal content. Outcomes included patient satisfaction (using a questionnaire that had not been validated) and re‐consultation rates. Doctor stress was also assessed by blood pressure measurement and a questionnaire (not described).
In a similar trial involving two doctors in a suburban practice (Ridsdale 1989), patients were allocated to consulting session booked at 5‐, 10‐, or 15‐minute intervals. Patients who had consulted in the previous four weeks were excluded. Process and outcome measures were the same as Morrell except that referral, investigation rates, and doctor stress were not assessed.
The fourth trial involved 16 doctors in 10 practices that usually had appointments of between 5 and 7.5 minutes but wished to increase appointment length (Wilson 1992). The intervention was sessions booked at 10‐minute intervals and spread across representative times and days of the week. Control sessions were booked at the usual interval. Process measures included consultation length, number of problems identified, health promotion interventions and prescribing, investigation and referral rates. Outcomes included re‐consultation rate and patient satisfaction measured using a questionnaire that had not been validated. Doctor stress was measured using a validated mood adjective checklist.
Edwards 2004 assessed the effects of GP training in shared decision making and risk communication, but also randomised patients to routine or longer appointments. The principal outcome measure was the COMRADE instrument to measure patients' assessment of communication and their confidence in decision making (Edwards 2003). Anxiety, enablement, health status, satisfaction, intention to adhere to chosen treatment, and perceived support in decision were also measured.
Excluded studies
One study, Ridsdale 1992, met our inclusion criteria, but on closer examination we excluded it as it described a secondary analysis of previously published work. We excluded another study that described a one‐off multidisciplinary consultation (Chan 2011). A third study described a multifaceted innovation, of which one element was longer consultations (Batal 2015) (see Characteristics of excluded studies).
Risk of bias in included studies
We assessed this using Effective Practice and Organisation of Care (EPOC) criteria (EPOC 2013), as shown in the Characteristics of included studies and Figure 2 and Figure 3.
2.
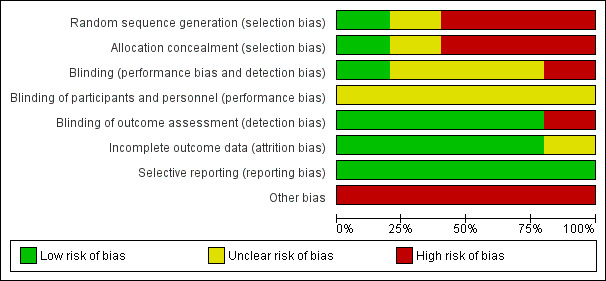
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
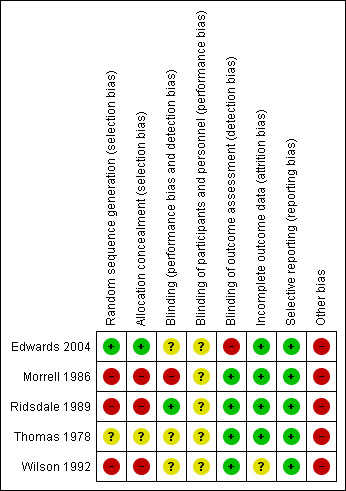
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Only Thomas 1978 and Edwards 2004 allocated patients randomly. Non‐random allocation in the other trials risked potential problems with case mix. In Morrell 1986, 71% of 5‐minute appointments were patient initiated, compared with 56% and 53% of 7.5‐ and 10‐minute appointments. This was due to greater availability of the shorter appointments. As patient‐initiated consultations are more likely to be for acute illness, comparison of examination rates and other outcomes is problematic. Case mix was not reported by Ridsdale 1989, but found to be similar by Wilson 1992 in terms of new or old problems, age, and sex of patients in each arm of the trial.
Blinding
In the four trials involving more than one doctor, the unit of analysis was the patient, and only two of these trials accounted for clustering effects by doctor (Edwards 2004; Ridsdale 1989). Only one study included a sample size calculation (Morrell 1986), and in this it was acknowledged that the study was insufficiently powered to detect changes in uncommon events. The trials with altering appointment length had multiple outcome measures assessed by a variety of methods including encounter sheets, patient questionnaire, and audiotape analysis. Levels of agreement for extraction of data from the medical record and audiotape were variable.
Incomplete outcome data
Four trials were at low risk of attrition bias, as all participants were accounted for or dropouts were justified and unlikely to bias results (Edwards 2004; Morrell 1986; Ridsdale 1989; Thomas 1978). The fifth trial had an unclear risk of attrition bias (Wilson 1992).
Selective reporting
All studies were at low risk of bias for selective reporting.
Other potential sources of bias
The design of all trials prevented concealment of allocation to participating doctors, although patients were not aware of what arm they had been allocated to. None of the trials reported baseline assessments.
Effects of interventions
See: Table 1
Provider performance
Consultation length
Three trials examined the effect of changing appointment length on the length of a consultation (Morrell 1986; Ridsdale 1989; Wilson 1992) (Analysis 1.1). We are uncertain whether altering the length of consultation leads to an increased length of primary care consultations (3 studies, 23 primary care physicians, very low‐certainty evidence). In Morrell 1986, consultation length was measured by audiotape analysis. For 5‐, 7.5‐, and 10‐minute appointments, the median lengths of doctor‐initiated appointments were 4.3, 6.4, and 7.0 minutes, and for patient‐initiated appointments they were 5.5, 6.7, and 7.9 minutes. Audiotape was also used to estimate length in Ridsdale 1989. The mean duration of consultations in 5‐, 10‐, and 15‐minute appointments were 6.6 (95% confidence interval (CI) 6.2 to 7.0), 8.0 (95% CI 7.5 to 8.5), and 9.2 minutes (95% CI 8.6 to 9.8). In Wilson 1992, consultation length was assessed by observation and rounded to the nearest minute. Median (mean) duration was 7 (8.25) minutes in the longer 10‐minute appointments and 6 (7.16) minutes in the control group (P < 0.001, Mann‐Whitney test). In all trials the difference in consultation length was less than the change in appointment length, particularly when appointment length was extended.
1.1. Analysis.
Comparison 1 Provider performance, Outcome 1 Consultation length.
| Consultation length | ||
|---|---|---|
| Study | Results | Notes |
| Morrell 1986 |
Appointment length 5 min ‐ Median length (range) Doctor initiated (n=65): 4.3 min (0.7‐15.6) Patient initiated (n=155): 5.5 (1.5‐20.9) Appointment length 7.5 min ‐ Median length (range) Doctor initiated (n=96): 6.4 min (1.6‐19.5) Patient initiated (n=117): 6.7 (1.4‐21.3) Appointment length 10 min ‐ Median length (range) Doctor initiated (n=88): 7.0 min (1.7‐29.9) Patient initiated (n=102): 7.9 (10‐19.8) |
Time measured using tape records between patient entering and leaving consulting room |
| Ridsdale 1989 |
Appointment length 5 min ‐ Mean (95% CI) N=339; 6.6 (6.2 to 7.0) Appointment length 7.5 min ‐ Mean (95% CI) N=259; 8.0 (7.5 to 8.5) Appointment length 10 min ‐ Mean (95% CI) N=319; 9.2 (8.6 to 9.8) |
Time measured using tape records between patient entering and leaving consulting room CI reported by authors |
| Wilson 1992 |
Appointment length 6‐7.5 min ‐ Mean N=1496; 7.16 Appointment length 10 min ‐ Mean N=1461; 8.25 (P < 0.001) |
Time measured by observing patient entering and leaving consulting room Duration rounded to the nearest minute Mann‐Whitney U test; P value reported by authors |
Recording of problems, referral and investigation, prescribing, and re‐consultation rates
We are uncertain whether changing the length of GP consultations increases the recording of problems, referral rates to specialists, and investigations (2 studies, 21 primary care physicians, very low‐certainty evidence), prescriptions (3 studies, 23 primary care physicians, very low‐certainty evidence), and re‐consultation rates (Analysis 1.2).
1.2. Analysis.
Comparison 1 Provider performance, Outcome 2 Recording of problems, referral and investigation, prescribing, and re‐consultation rates.
| Recording of problems, referral and investigation, prescribing, and re‐consultation rates | ||
|---|---|---|
| Study | Results | Notes |
| Morrell 1986 |
Two or more problems recorded (%) 5 min (n=275): 11 7.5 min (n=262): 16 10 min (n=243): 22 Referred to specialist (%) 5 min (n=275): 8 7.5 min (n=262): 9 10 min (n=243): 10 Psychological problem recorded (%) 5 min (n=275): 9 7.5 min (n=262): 14 10 min (n=243): 12 Prescription issued (%) 5 min (n=275): 59 7.5 min (n=262): 63 10 min (n=243): 62 Investigations (%) 5 min (n=275): 9 7.5 min (n=262): 10 10 min (n=243): 10 Asked to book return consultations (%) 5 min (n=275): 16 7.5 min (n=262): 12 10 min (n=243): 18 |
Information collected using tape records from the appointments. For about 20% of the patients, information was collected from patient records or questionnaires. |
| Ridsdale 1989 |
Two or more problems recorded (%) 5 min (n=348): 14 10 min (n=277): 19 15 min (n=336): 14 Psychological problem recorded (%) 5 min (n=348): 8 10 min (n=277): 8 15 min (n=336): 5 Prescription issued (%) 5 min (n=348): 61 10 min (n=277): 63 15 min (n=336): 58 Re‐consultations within 4 weeks (%) 5 min (n=348): 30 10 min (n=277): 29 15 min (n=336): 31 |
Information collected using tape records from the appointments. Coded by blinded rater. |
| Thomas 1978 |
Re‐consultations within 4 weeks (%) Short appointments (n=100): 27 Long appointments ((n=100): 20 Mean difference: 7%, 95% CI ‐4.7 to 18.6 |
Information collected from patient's records. |
| Wilson 1992 |
Two or more problems recorded (%) 6‐7.5 min (n=1496): 32 10 min (n=1461): 35 Referred to specialist (%) 6‐7.5 min (n=1496): 5.0 10 min (n=1461): 5.7 Prescription issued (%) 6‐7.5 min (n=1496): 55.7 10 min (n=1461): 56.9 Investigations (%) 6‐7.5 min (n=1496): 8.8 10 min (n=1461): 10.6 Re‐consultations within 12 weeks (%) 6‐7.5 min (n=1496): 27 10 min (n=1461): 20 |
Information collected from patient's records. |
Morrell 1986 found the percentage of consultations with more than one problem recorded was greater as appointment length increased (11% in 5‐minute appointments, 16% in 7.5‐minute appointments, and 22% in 10‐minute appointments, P value < 0.001, Chi² test for trend). Ridsdale 1989 reported the percentage of patients in 5‐, 10‐, and 15‐minute appointments with more than one problem recorded as 14%, 19%, and 14%, respectively. In Wilson 1992, 32% of patients in control appointments and 35% in 10‐minute appointments reported more than one problem (unpublished data).
Two trials looked at the percentage of consultations in which a psychological problem was recorded. In Morrell 1986 this was 9%, 14%, and 12% for 5‐, 7.5‐, and 10‐minute appointments, respectively. The authors stated that the likelihood of recording psychological problems increased with the length of the consultation, but did not present the analysis. Ridsdale 1989 found the same number of recorded psychological problems irrespective of consultation length (8%, 8%, and 5% for 5‐, 10‐, and 15‐minute appointments, respectively).
The two trials assessing the percentage of consultations resulting in specialist referrals found similar results for all groups, although rates were slightly higher with longer appointments. In Morrell 1986, rates were 8%, 9%, and 10% for 5‐, 7.5‐, and 10‐minute appointments, and in Wilson 1992 they were 5.0% and 5.7% for control and 10‐minute appointments (unpublished data).
Similarly, the two trials assessing percentage of consultations resulting in one or more investigations found these were slightly higher with longer appointments, although with wide overlapping confidence intervals. In Morrell 1986, these were 9%, 10%, and 10% for 5‐, 7.5‐, and 10‐minute appointments, and in Wilson 1992, they were 5.0% and 5.7% for control and 10‐minute appointments, respectively (unpublished data).
Three studies examined the percentage of consultations including a prescription, but none found any consistent relationship. In Morrell 1986, rates were 59%, 63%, and 62% for 5‐, 7.5‐, and 10‐minute appointments; in Ridsdale 1989, they were 61%, 63%, and 58% for 5‐, 10‐, and 15‐minute appointments; and in Wilson 1992, they were 55.7% and 56.9% for control and 10‐minute appointments. Two trials examined antibiotic prescribing. In Morrell 1986, antibiotics were more likely to be prescribed with shorter appointments (rates of 15%, 10%, and 11% for 5‐, 7.5‐, and 10‐minute appointments, respectively). The study authors reported that the higher proportion of patient‐initiated consultations with the short appointments did not account for this. However, Ridsdale 1989 found no relationship between consultation length and antibiotics prescription (rates of 22%, 26%, and 22% for 5‐, 10‐, and 15‐minute appointments).
None of the four trials reporting data on re‐consultation found any consistent relationship between re‐consultation rates and appointment length. In Thomas 1978, 27% of patients who had a short consultation consulted again within a month, compared to 20% who had a long consultation; in Morrell 1986, a return consultation was booked in 16%, 12%, and 18% for 5‐, 7.5‐, and 10‐minute appointments; and in Ridsdale 1989 the percentage of patients returning within 4 weeks was 30%, 29%, and 31% for 5‐, 10‐, and 15‐minute appointments, respectively. Wilson 1992 reported re‐consultation rates within 3 months of 42% and 46% for control and 10‐minute appointments (unpublished data).
Examination
All three trials with altering appointment length assessed the percentage of consultations in which one or more physical examinations took place (Analysis 1.3). In Morrell 1986, results were presented separately for patient‐ and doctor‐initiated consultations. For the former, more examinations took place with shorter appointments (77%, 76%, and 69% for 5‐, 7.5‐, and 10‐minute appointments, difference not tested statistically); for the latter, more examinations took place with longer appointments (41%, 55%, and 63% for 5‐, 7.5‐, and 10‐minute appointments, P value < 0.01). The authors suggested that some of these differences may be explained by case mix, with more patients with acute illness presenting in shorter appointments. Ridsdale 1989 found no consistent relationship (82%, 83%, 83% for 5‐, 10‐, and 15‐minute appointments), and neither did Wilson 1992 (65% and 64% for control and 10‐minute appointments, unpublished data).
1.3. Analysis.
Comparison 1 Provider performance, Outcome 3 Examinations.
| Examinations | ||
|---|---|---|
| Study | Results | Notes |
| Morrell 1986 |
Any extra examination (%) Doctor initiated 5 min (n=80): 41 7.5 min (n=117): 55 10 min (n=114): 63 Patient initiated 5 min (n=195): 77 7.5 min (n=145): 76 10 min (n=129): 69 Blood pressure measured (%) Doctor initiated 5 min (n=80): 18 7.5 min (n=117): 27 10 min (n=114): 29 Patient initiated 5 min (n=195): 7 7.5 min (n=145): 8 10 min (n=129): 12 Vaginal examination (female patients) (%) Doctor initiated 5 min (n=80): 2 7.5 min (n=117): 10 10 min (n=114): 10 Patient initiated 5 min (n=195): 5 7.5 min (n=145): 11 10 min (n=129): 7 |
|
| Ridsdale 1989 |
Any extra examination (%) 5 min (n=348): 82 7.5 min (n=277): 83 10 min (n=336): 83 Blood pressure measured (%) 5 min (n=348): 22 7.5 min (n=277): 17 10 min (n=336): 16 Vaginal examination (female patients) (%) 5 min (n=348): 3 7.5 min (n=277): 2 10 min (n=336): 7 |
|
| Wilson 1992 |
Any extra examination (%) 6 min (n=1496): 65 10 min (n=1461): 64 Blood pressure measured (%) 6 min (n=1496): 19 10 min (n=1461): 24 |
|
Two of the three trials examining percentage of consultations in which blood pressure was recorded found that this occurred more frequently with longer appointments. In Morrell 1986, rates for 5‐, 7.5‐, and 10‐minute appointments were 7%, 8%, and 12% in patient‐initiated consultations and 18%, 27%, and 29% in doctor‐initiated consultations. In Ridsdale 1989, all three groups had similar rates of blood pressure recording (22%, 17%, and 16% for 5‐, 10‐, and 15‐minute appointments), but in Wilson 1992 this was 19% in control appointments and 24% in extended 10‐minute appointments (P value < 0.001).
Two trials assessed the rate of vaginal examination for women over 16 years of age. In Morrell 1986, rates for 5‐, 7.5‐, and 10‐minute appointments were 2%, 10%, and 10% in patient‐initiated consultation and 5%, 11%, and 7% in doctor‐initiated consultations. Ridsdale 1989 found that more vaginal examinations took place with long appointments (3%, 2%, 7% for 5‐, 10‐, and 15‐minute appointments; odds ratio 2.9, 95% CI 1.3 to 6.6).
Health promotion
Two trials assessed health promotion statements using audiotape (Analysis 1.4). Morrell 1986 assessed the number of health education items mentioned by the doctor and calculated the percentage of consultations in which the number of items recorded was greater than the overall median. This increased from 14.5 in 5‐minute appointments to 16.9 in 7.5‐minute appointments and 22.1 in 10‐minute appointments (P value < 0.001, Chi² test for trend). Wilson 1992 analysed audio recordings of a subsample of consultations and calculated the percentage of consultations in which discussion of a health promotion topic took place. This showed a non‐statistically significant increase from 24.4% in control consultations to 28.4% in those booked for 10 minutes. This trial went on to examine the proportion of consultations in which a health promotion item was recorded in the medical record, calculating a rate of 8.8% for control consultations and 15.5% for 10‐minute appointments (P value < 0.001, Chi² test). Wilson 1992 also used a patient questionnaire as a source of information about health promotion. The proportion of current smokers reporting discussion of smoking was 19.8% for control consultations and 31.8% for 10‐minute appointments (P value < 0.001, Chi² test). However, there was little difference in rates of reported advice about diet and alcohol (rates of 11.3%, 11.4%; and 5.0%, 7.0% with control and 10‐minute appointments, respectively).
1.4. Analysis.
Comparison 1 Provider performance, Outcome 4 Health promotion.
| Health promotion | ||
|---|---|---|
| Study | Results | Notes |
| Morrell 1986 |
Detected on audiotape (%) 5 min (n=220): 14.5 7.5 min (n=213): 16.9 10 min (n=190): 22.1 |
Number of eligible appointments between brackets |
| Wilson 1992 |
Detected on audiotape (%) 6 min (n=180): 24.4 10 min (n=275): 28.4 Extracted from medical record (%) 6 min (n=1432): 8.8 10 min (n=1411): 15.5 Extracted from patient questionnaire (%) Current smoker reporting advice 6 min (n=212): 19.8 10 min (n=258): 31.8 Discussion of diet 6 min (n=839): 11.3 10 min (n=950): 11.4 Discussion of alcohol 6 min (n=839): 5.0 10 min (n=956): 7.0 |
Number of eligible appointments between brackets |
General practitioner stress
Two trials examined GP stress (Analysis 1.5). In Morrell 1986, doctors' heart rates were monitored throughout the consultation, indicating similar mean heart rate for all the appointments. Doctors also completed a five‐item stress questionnaire at the beginning and end of each session, also with similar results between groups. Wilson 1992 assessed doctor stress and arousal before and after each consultation using a validated mood adjective checklist. Stress scores were lower and arousal scores were higher at the end of the 10‐minute appointment session than in the shorter control sessions (P value < 0.001).
1.5. Analysis.
Comparison 1 Provider performance, Outcome 5 General practitioner stress.
| General practitioner stress | ||
|---|---|---|
| Study | Results | Notes |
| Morrell 1986 |
Reporting insufficient time for patient's problems (%) 5 min: 23 7.5 min: 6 10 min: 2 Stress score ‐ Mean (SD) 5 min: 11.0 (0.8) 7.5 min: 9.8 (0.5) 10 min: 10.6 (0.7) Pulse rate ‐ Mean (SD) 5 min: 72.4 (4.2) 7.5 min: 70.3 (3.5) 10 min: 70.3 (3.4) |
Heart rate measured with a fitted cardiac monitor. Stress rating scale not described. |
| Wilson 1992 |
Stress score ‐ Median (IQR), P value 1st control session: ‐1 (‐8, 4), NS 2nd control session: ‐1 (‐6, 3), NS Experimental session: ‐3 (‐7, 0), P < 0.001 Arousal score ‐ Median (IQR) 1st control session: 1 (‐1, 5), P < 0.05 2nd control session: 2 (‐1, 5) P < 0.05 Experimental session: 2 (0, 8), P < 0.001 |
26 cards with printed adjectives (e.g., tired), rated 1‐4 Stress score 17‐68, arousal score 8‐32 Higher scores indicate higher stress/arousal Wilcoxon test, as reported by the authors |
Patient satisfaction with care
Four trials assessed patient satisfaction with the care received, none of which used a validated instrument (Analysis 2.1). Three of these studies compared increased consultation length with usual care (Morrell 1986; Ridsdale 1989; Wilson 1992). We are uncertain whether altering the length of consultation increased patient satisfaction (3 studies, 23 primary care physicians, very low‐certainty evidence). Morrell 1986 used a four item questionnaire to assess satisfaction and reported similar levels for all patients regardless of consultation length. Using a similar questionnaire, Ridsdale 1989 found that more patients allocated to the 5‐minute consultations felt that they had little or very little time available. Wilson 1992 used a 12‐item satisfaction questionnaire and failed to detect any effects of appointment length on patient satisfaction (unpublished data). Edwards 2004 employed a single‐item questionnaire to ask patients about their confidence in their GP's decision and intention to adhere to treatment, reporting that longer appointments were associated with an increase in both outcomes (difference 2.1, 95% CI 0.7 to 3.5; and difference 0.7, 95% CI 0.04 to 1.36, respectively).
2.1. Analysis.
Comparison 2 Patient satisfaction with care, Outcome 1 Patient satisfaction with care.
| Patient satisfaction with care | ||
|---|---|---|
| Study | Results | Notes |
| Edwards 2004 |
Confidence in decision made Difference 2.1, 95% CI 0.7 to 3.5 Expectation to adhere to chosen treatment Difference 0.7, 95% CI 0.04 to 1.36 |
Single item Difference and 95% CI reported by the authors |
| Morrell 1986 |
Little or very little time available (%) 5 min (245): 3.7 7.5 min (224): 1.8 10 min (208): 0.5 Felt very free to discuss problems (%) 5 min (238): 67.2 7.5 min (219): 74.9 10 min (207): 78.7 Very satisfied with information received (%)* 5 min (134): 89.6 7.5 min (128): 90.6 10 min (134): 93.3 Received information about management (%)** 5 min (143): 91.6 7.5 min (124): 96.0 10 min (107): 97.2 |
4‐item questionnaire (not described) * Of those who needed information ** For those receiving a prescription |
| Ridsdale 1989 |
Little or very little time available (%) 5 min (340): 9 10 min (261): 5 15 min (319): 3 Felt very free to discuss problems (%) 5 min (334): 66 10 min (257): 68 15 min (314): 71 Very satisfied with information received (%)* 5 min (218): 91 10 min (170): 91 15 min (200): 91 Very free to tell doctors about ideas and concerns (%) 5 min (328): 62 10 min (248): 60 15 min (306): 68 |
4‐item questionnaire (not described) * Of those who needed information |
| Wilson 1992 | Patients in both groups reported similar satisfaction levels * | 12‐item satisfaction questionnaire * U npublished data |
Healthcare behaviours
None of the included studies reported on healthcare behaviours.
Health status
One study assessed the effects of interventions to alter consultation length on patient health status (Edwards 2004), using the physical and mental components of the 12‐Item Short Form Health Survey (SF‐12, Ware 1996) (Analysis 3.1). The authors reported that patients allocated to different consultation lengths obtained similar scores on both components.
3.1. Analysis.
Comparison 3 Health status, Outcome 1 Health status.
| Health status | ||
|---|---|---|
| Study | Results | Notes |
| Edwards 2004 | Patiens allocated to consultations with different length scored equally on mental and physical components. |
12‐Item Short Form Health Survey (SF‐12) No other data reported for group comparison based on consultation length |
Resources associated with the intervention and any consequent changes in clinical care
None of the included studies reported on resources associated with interventions to change the length of primary care physicians' consultations.
Enablement
One study reported the effects of interventions to alter consultation length on patient enablement (Edwards 2004), using the Patient Enablement Instrument (PEI, Howie 1998) (Analysis 4.1). The authors reported that patients allocated to different consultation lengths had similar enablement levels.
4.1. Analysis.
Comparison 4 Enablement, Outcome 1 Enablement.
| Enablement | ||
|---|---|---|
| Study | Results | Notes |
| Edwards 2004 | Patients allocated to different consultation length had similar enablement | Patient Enablement Instrument (PEI); 6‐item, score range 0‐12 No other data reported for group comparison based on consultation length |
Discussion
Summary of main results
This systematic review evaluated the effectiveness of interventions aimed at changing the length of primary care physicians' consultations. We are uncertain whether altering the length of consultation leads to changes in provider's performance, namely length of primary care consultations (3 studies, 23 primary care physicians), referrals and examinations (2 studies, 21 primary care physicians), and prescriptions (3 studies, 23 primary care physicians) (very low‐certainty evidence for all outcomes). We are also uncertain whether altering the length of consultation increases patient satisfaction (3 studies, 23 primary care physicians, very low‐certainty evidence). However, there was some evidence that greater time availability led to greater patient satisfaction (Edwards 2004), as has been shown in larger observational studies. None of the included studies assessed the effects of altering consultation length on resource use.
Overall completeness and applicability of evidence
The number of eligible studies was small, and all studies had methodological weaknesses, particularly due to lack of randomisation and consequent questions about comparability of case mix. All had short follow‐up durations and tested multiple hypotheses, some of which the studies were underpowered to detect, and all were conducted in the UK. Potential effects of a more sustained change to longer consultations, for example on chronic disease control, have not been examined in intervention studies, nor has any study included an economic analysis. Only one of the studies was conducted in the past decade, with the remaining studies conducted more than 25 years ago. We did not identify any new studies for this update, although we did identify one ongoing study.
In summary, none of the differences found in observational studies have been replicated when an intervention was introduced to enable doctors to consult more slowly. One explanation for this is that doctors who consult more slowly are self‐selecting, and so average consultation length is a marker of some other attribute, such as the patient‐centredness of the doctor, which is related to performance. Another is that the intervention evaluated, short‐term changes in appointment length in the absence of any clear objective, is insufficient to change behaviour. Other studies have found that more focussed interventions, for example to improve consultation skills, have resulted in more time being spent with patients (Verby 1979).
None of the studies considered how the intervention could increase or decrease inequities, and likewise none of the studies considered how patients' characteristics, including education and socioeconomic status, could have contributed to the observed effect. As disadvantaged populations are at higher risk of worse health outcomes and have poorer access to health care (Marmot 2005; Starfield 2011), it would be relevant to consider the potential effect of the interventions for these subgroups.
Certainty of the evidence
Three of the five studies included in this review were not randomised controlled trials, and only these contributed to the certainty of evidence. Along with the high risk of bias for allocation, these studies also had other high risk of bias, namely the absence of clinical data for patient characteristics. The relatively small sample size, with 23 primary care physicians recruited by the three studies, increased the imprecision of the evidence and contributed to the overall very low‐certainty evidence for the outcomes measured, length of consultation, referrals and examinations, prescriptions, and patient satisfaction.
Potential biases in the review process
For this update, only one review author screened titles and abstracts, after which two review authors independently applied the eligibility criteria to the full text and evaluated risk of bias. We did not identify any unpublished data for inclusion in the review, so there is a risk that we might have missed relevant data.
Agreements and disagreements with other studies or reviews
A previous systematic review identified 10 studies reporting on the relationship between consultation length, process, and outcomes in general practice (Wilson 2002). Results showed that doctors who had longer consultations were less likely to prescribe medications and more likely to provide lifestyle advice and suggest preventive activities. For that review study designs other than RCTs and NRCTs were eligible, and the authors identified some methodological weaknesses of the included studies, namely the lack of representative GP samples and practices with lower list sizes per doctor. Furthermore, consultation length was often averaged and not specifically reported. The authors were unable to conclude that consultation length is the most relevant aspect of the consultation, as other factors, including doctor attributes, might also have an effect on the outcomes (Wilson 2002). A recent review on the association of consultation length and patient's perception of care identified nine studies, concluding that it is not the length of the consultation in itself, but instead other variables, namely the increased time the physician will have for other tasks such as management of psychosocial problems, that improves consultation outcome (Lemon 2014).
Authors' conclusions
Implications for practice.
The findings of this review do not provide sufficient evidence to support or refute a policy of altering consultation lengths of primary care physicians.
Implications for research.
Future studies on the effects of altering time availability should be focussed on health outcomes, and include a health economic analysis. They will need to be adequately powered and should aim to recruit a representative sample of doctors. There is a case for an extended randomised controlled trial of longer appointments, which could measure the intervention's effects on the whole system, including accessibility and availability of care, long‐term effects on consultation rates, and outcome measures such as patient enablement and control of chronic disease as examined in observational studies. Additionally, there is a need to evaluate interventions offering longer consultations to select patients, such as those with multimorbidity or complex medical conditions, or both.
What's new
| Date | Event | Description |
|---|---|---|
| 4 January 2016 | New citation required but conclusions have not changed | The methods of the review have been updated to align with current Cochrane guidance. New authors added. This review includes five studies. |
| 4 January 2016 | New search has been performed | Searches revised and updated. No new studies identified. |
History
Protocol first published: Issue 1, 2002 Review first published: Issue 1, 2006
| Date | Event | Description |
|---|---|---|
| 12 November 2008 | Amended | Minor edits. |
| 15 May 2008 | New search has been performed | One new study, no change to conclusions. |
| 7 May 2008 | Amended | Converted to new review format. |
| 13 October 2005 | New citation required and conclusions have changed | Substantive amendment. |
Acknowledgements
The original review was funded by the Scientific Foundation Board of the Royal College of General Practitioners (Wilson 2006). For this update, we would like to acknowledge the support of the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Effective Practice and Organisation of Care Group (EPOC). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service, or the Department of Health. We would like to acknowledge the contribution of Paul Miller, EPOC's Information Specialist, for conducting the searches, and Julia Worswick, EPOC's Managing Editor, for all the editorial support.
Appendices
Appendix 1. Search strategies (4 January 2016)
MEDLINE (OVID)
1. exp "appointments and schedules"/
2. "referral and consultation"/
3. office visits/
4. appointment?.tw.
5. consult*.tw.
6. or/1‐5
7. exp time factors/
8. time management/
9. quality of health care/
10. (time or length or duration or shorte? or lengthen or longer or interval*).tw.
11. or/7‐10
12. family practice/
13. general practice/
14. physicians, family/
15. physicians, primary care/
16. general practitioners/
17. primary health care/
18. ((general or family) adj practi*).tw.
19. family physic*.tw.
20. primary care.tw.
21. primary health care.tw.
22. or/12‐21
23. 6 and 11 and 22
24. exp randomized controlled trial/
25. controlled clinical trial.pt.
26. randomi#ed.ti,ab.
27. placebo.ab.
28. randomly.ti,ab.
29. Clinical Trials as topic.sh.
30. trial.ti.
31. exp animals/ not humans/
32. or/24‐30
33. 32 not 31
34. 23 and 33
EMBASE (OVID)
1. *consultation/
2. appointment?.tw.
3. consult*.tw.
4. or/1‐3
5. *time/
6. *time management/
7. (time or length or duration or shorte? or lengthen or longer or interval*).tw.
8. *health care quality/
9. or/5‐8
10. *general practice/
11. *general practitioner/
12. *primary health care/
13. ((general or family) adj practi*).tw.
14. family physic*.tw.
15. primary care.tw.
16. primary health care.tw.
17. or/10‐16
18. 4 and 9 and 17
19. random*.ti,ab.
20. factorial*.ti,ab.
21. (crossover* or cross over*).ti,ab.
22. ((doubl* or singl*) adj blind*).ti,ab.
23. (assign* or allocat* or volunteer* or placebo*).ti,ab.
24. crossover procedure/
25. single blind procedure/
26. randomized controlled trial/
27. double blind procedure/
28. or/19‐27
29. exp animal/ not human/
30. 28 not 29
31. 18 and 30
Cochrane ‐ Wiley
#1 [mh "appointments and schedules"]
#2 [mh "referral and consultation"]
#3 [mh "office visits"]
#4 appointment*:ti,ab
#5 consult*:ti,ab
#6 {or #1‐#5}
#7 [mh "time factors"]
#8 [mh "time management"]
#9 [mh "quality of health care"]
#10 (time or length or duration or shorte* or lengthen or longer or interval*):ti,ab
#11 {or #7‐#10}
#12 [mh "family practice"]
#13 [mh "general practice"]
#14 [mh "physicians, family"]
#15 [mh "physicians, primary care"]
#16 [mh "general practitioners"]
#17 [mh "primary health care"]
#18 ((general or family) next practi*):ti,ab
#19 family physic*:ti,ab
#20 primary care:ti,ab
#21 primary health care:ti,ab
#22 {or #12‐#21}
ClinicalTrials.gov
1. ("length of consultation" OR "duration of consultation" OR "shorter consultation" OR "shorten consultation" OR "lengthen consultation")
2. ("longer consultation" OR "consultation time" OR "consultation length" OR "consultation duration")
3. ("length of appointment" OR "duration of appointment" OR "shorter appointment" OR "shorten appointment" OR "lengthen appointment")
4. ("longer appointment" OR "appointment time" OR "appointment length" OR "appointment duration")
WHO ICTRP
length of consultation* OR duration of consultation* OR shorter consultation* OR shorten consultation* OR lengthen consultation* OR longer consultation* OR consultation* time OR consultation* length OR consultation* duration OR length of appointment* OR duration of appointment* OR shorter appointment* OR shorten appointment* OR lengthen appointment* OR longer appointment* OR appointment* time OR appointment* length OR appointment* duration
Data and analyses
Comparison 1. Provider performance.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Consultation length | Other data | No numeric data | ||
| 2 Recording of problems, referral and investigation, prescribing, and re‐consultation rates | Other data | No numeric data | ||
| 3 Examinations | Other data | No numeric data | ||
| 4 Health promotion | Other data | No numeric data | ||
| 5 General practitioner stress | Other data | No numeric data |
Comparison 2. Patient satisfaction with care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Patient satisfaction with care | Other data | No numeric data |
Comparison 3. Health status.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health status | Other data | No numeric data |
Comparison 4. Enablement.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Enablement | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Edwards 2004.
| Methods | RCT. Patients randomised to usual surgery time or longer consultations (up to 15 min) | |
| Participants | 20 practices; 20 doctors; 747 patients with 1 of 4 conditions: non‐valvular atrial fibrillation, prostatism, menorrhagia, menopause‐related problems | |
| Interventions | Longer appointments in a "research clinic" (up to 15 min). Study also examined doctor training in shared decision making and risk communication | |
| Outcomes | Patient confidence in decision, patient expectation to adhere to chosen treatment SF‐12, enablement, anxiety, satisfaction, perceived support in decision | |
| Notes | Analysis: by multilevel modelling | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generation |
| Allocation concealment (selection bias) | Low risk | Randomisation was concealed from those implementing the interventions or assessments |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear who introduced data/performed analysis |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding for personnel implementing the intervention not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Main outcome is patient‐reported (mailed questionnaire) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12% drop‐out at 1 month; some non‐response analysis done |
| Selective reporting (reporting bias) | Low risk | No protocol found; all prespecified outcomes are reported |
| Other bias | High risk | No baseline measurements (pre‐clinical data for patient characteristics) Selection bias due to questionnaire response |
Morrell 1986.
| Methods | NRCT. Non‐randomised to surgery sessions with 5‐, 7.5‐, or 10‐minute appointments | |
| Participants | 1 practice; 5 doctors; 60 surgery sessions; 780 consultations | |
| Interventions | 5‐, 7.5‐, and 10‐minute appointments (usual appointment length 6.7 min) | |
| Outcomes | Consultation length, examination, prescribing and referral, investigation rates, number of problems and psychological problems identified, language content; re‐consultation in 4 weeks | |
| Notes | Analysis: Logistic regression allowing for age and sex of patient. As case mix varied between groups, doctor‐ and patient‐initiated consultations were analysed separately for several outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequential allocation of patients to 1 of 3 arms |
| Allocation concealment (selection bias) | High risk | Sequential allocation of patients to 1 of 3 arms |
| Blinding (performance bias and detection bias) All outcomes | High risk | Non‐blinded assessment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding for personnel implementing the intervention not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Objective outcome (consultation length) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data obtained for 96% of consenting participants |
| Selective reporting (reporting bias) | Low risk | No protocol found; all prespecified outcomes are reported |
| Other bias | High risk | No baseline measurements (pre‐clinical data for patient characteristics) Selection bias ‐ more acute illness |
Ridsdale 1989.
| Methods | NRCT. Non‐randomised to surgery sessions with 5‐, 10‐, or 15‐minute appointments | |
| Participants | 1 practice; 2 doctors; 914 consultations | |
| Interventions | 5‐, 10‐, or 15‐minute appointments (usual appointment length 10 minutes) | |
| Outcomes | Consultation length, examination, number of problems and psychological problems identified, language content. Re‐consultation in 4 weeks | |
| Notes | Analysis: regression, accounting for age and sex of patient and consulting doctor | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐systematic consecutive allocation |
| Allocation concealment (selection bias) | High risk | Non‐systematic consecutive allocation; GPs aware of allocation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Rater blinded to group allocation |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding for personnel implementing the intervention not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Objective outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low number of incomplete outcome data (95% follow‐up) |
| Selective reporting (reporting bias) | Low risk | No protocol found; all prespecified outcomes are reported |
| Other bias | High risk | No baseline assessment (pre‐clinical data for patient characteristics) |
Thomas 1978.
| Methods | RCT. Random allocation by participating doctor ‐ method not stated | |
| Participants | 1 practice; 1 doctor; 52 surgery sessions; 200 patients in whom no diagnosis could be made | |
| Interventions | Patients randomly assigned to 1 of 4 groups: long consultation with or without treatment; short consultation with or without treatment. The participating doctor terminated short consultations as soon as possible and aimed to make the long consultations last for more than 10 minutes | |
| Outcomes | Re‐consultation | |
| Notes | Analysis: Chi² | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not enough information provided |
| Allocation concealment (selection bias) | Unclear risk | Not enough information provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not enough information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not enough information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Objective outcome (re‐consultation) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for |
| Selective reporting (reporting bias) | Low risk | No protocol found; all prespecified outcomes are reported |
| Other bias | High risk | No baseline assessment (pre‐clinical data for patient characteristics) |
Wilson 1992.
| Methods | NRCT. Non‐randomised to surgery sessions with usual or 10‐minute appointments (run in control sessions not included) | |
| Participants | 10 practices; 16 doctors; 208 surgery sessions; 2957 consultations | |
| Interventions | 10‐minute appointments | |
| Outcomes | Consultation length, examination, prescribing referral and investigation rates, health promotion procedures and examinations; re‐consultation | |
| Notes | Analysis: by patient, no account for clustering by doctor | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐RCT (consecutive weeks) |
| Allocation concealment (selection bias) | High risk | Non‐RCT (consecutive weeks) |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Unclear whether Research associates who reviewed clinical notes were blinded or not |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding for personnel implementing the intervention not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Objective outcome (consultation length) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not enough information provided |
| Selective reporting (reporting bias) | Low risk | No protocol found; all prespecified outcomes are reported |
| Other bias | High risk | No baseline assessment (pre‐clinical data for patient characteristics) |
GP: general practitioner NRCT: non‐randomised controlled trial RCT: randomised controlled trial SF‐12: 12‐Item Short Form Health Survey
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Batal 2015 | Multifaceted innovation, one element of which is longer consultations |
| Chan 2011 | One‐off multidisciplinary consultation |
| Ridsdale 1992 | Secondary analysis |
Characteristics of ongoing studies [ordered by study ID]
ISRCTN34092919.
| Trial name or title | Living well with multiple morbidity: The development and evaluation of a primary care‐based complex intervention to support patients with multiple morbidities |
| Methods | Exploratory cluster randomised controlled trial; patients unblinded to group allocation |
| Participants | Patients 30 to 65 years of age, with 2 or more long‐term conditions |
| Interventions | CARE Plus intervention, which includes longer consultations with general practitioner or nurse, and setting specific healthcare goals. Patients will be given a self help pack, and healthcare professionals will receive training and support Control group: usual care |
| Outcomes | Main outcomes: health‐related quality of life; well‐being (measured at baseline, 6 months, 12 months) Other outcomes: anxiety and depression; self efficacy; self esteem; self‐rated general health; medication compliance; patient enablement; health service utilisation |
| Starting date | Registered 28 November 2012 |
| Contact information | |
| Notes | Trial registry ISRCTN34092919 |
Differences between protocol and review
We updated the methods used in the original review to align with current Cochrane guidance, including the methodological standards for the conduct and reporting of Cochrane intervention reviews (MECIR 2012). We added a new outcome (enablement) that had not been initially defined. We also revised the search strategy and added two new authors.
Contributions of authors
ADW and SC conceived and designed the review. ADW prepared the protocol. For the original review, ADW and SC screened the references, extracted data, and wrote the review. For the first update, DGB and ADW screened the references, DGB and GJI assessed risk of bias, and DGB and ADW analysed the certainty of evidence and built the 'Summary of findings' table. All authors revised and approved the final version of the review.
Sources of support
Internal sources
National Institute for Health Research, via Cochrane Infrastructure to the Effective Practice and Organisation of Care Group, UK.
External sources
No sources of support supplied
Declarations of interest
ADW was an author on one of the studies included in the review. SC, DGB, GJI: none.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Edwards 2004 {published data only}
- Edwards A, Elwyn G, Hood K, Atwell C, Robling M, Houston H, et al. Study Steering Group. Patient‐based outcome results from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Family Practice 2004;21(4):347‐54. [PUBMED: 15249521] [DOI] [PubMed] [Google Scholar]
Morrell 1986 {published data only}
- Morrell DC, Evans ME, Morris RW, Roland MO. The "five minute" consultation: effect of time constraint on clinical content and patient satisfaction. British Medical Journal (Clinical Research Ed.) 1986;292(6524):870‐3. [PUBMED: 3083919] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roland MO, Bartholomew J, Courtenay MJF, Morris RW, Morrell DC. The 'five minute consultation': effect of time constraint on verbal communication. British Medical Journal (Clinical Research Ed.) 1986;292(6524):874‐6. [PUBMED: 3083920] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ridsdale 1989 {published data only}
- Ogden J, Bavalia K, Bull M, Frankum S, Goldie C, Gosslau M, et al. “I want more time with my doctor”: a quantitative study of time and the consultation. Family Practice 2004;21(5):479‐83. [DOI] [PubMed] [Google Scholar]
- Ridsdale L, Carruthers M, Morris R, Ridsdale J. Study of the effect of time availability on the consultation. Journal of the Royal College of General Practitioners 1989;39(329):488‐91. [PUBMED: 2558202] [PMC free article] [PubMed] [Google Scholar]
Thomas 1978 {published data only}
- Thomas KB. Time and the consultation in general practice. British Medical Journal 1978;2(6143):1000. [PUBMED: 709173] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 1992 {published and unpublished data}
- Wilson A, McDonald P, Hayes L, Cooney J. Health promotion in the general practice consultation: a minute makes a difference. BMJ 1992;304(6821):227‐30. [PUBMED: 1739798] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson A, McDonald P, Hayes L, Cooney J. Longer booking intervals in general practice: effects on doctors' stress and arousal. British Journal of General Practice 1991;41(346):184‐7. [PUBMED: 1878267] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Batal 2015 {published data only}
- Batal HA, Kulasekaran V, Long J, Durfee MJ, Everhart R, Brewer D, et al. The intensive outpatient clinic: Targeting super‐utilizers at Denver health. Journal of General Internal Medicine 2015;30:S547. [Google Scholar]
Chan 2011 {published data only}
- Chan W‐S, Whitford DL, Conroy R, Gibney D, Hollywood B. A multidisciplinary primary care team consultation in a socio‐economically deprived community: An exploratory randomised controlled trial. BMC Health Services Research 2011;11:15. [DOI: 10.1186/1472-6963-11-15] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ridsdale 1992 {published data only}
- Ridsdale L, Morgan M, Morris R. Doctors' interviewing technique and its response to different booking time. Family Practice 1992;9(1):57‐60. [PUBMED: 1634029] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN34092919 {published data only}
- ISRCTN34092919. Living well with multiple morbidity. http://www.controlled‐trials.com/ISRCTN34092919 (accessed 8 March 2016). [DOI: 10.1186/ISRCTN34092919] [DOI]
Additional references
Anderson 2007
- Anderson RT, Camacho FT, Balkrishnan R. Willing to wait? The influence of patient wait time on satisfaction with primary care. BMC Health Services Research 2007;7:31. [DOI: 10.1186/1472-6963-7-31] [DOI] [PMC free article] [PubMed] [Google Scholar]
BMA 2015
- British Medical Association. National Survey of GPs. The Future of General Practice 2015. London: ICM Research, 2015. [Google Scholar]
Cartwright 1981
- Cartwright A, Anderson R. General Practice Revisited: A Second Study of Patients and Their Doctors. London: Tavistock, 1981. [Google Scholar]
Commonwealth Fund 2015
- Commonwealth Fund. 2015 International Survey of Primary Care Doctors. New York: Commonwealth Fund, 2015. [Google Scholar]
Deveugele 2002
- Deveugele M, Derese A, Brink‐Muinen, Bensing J, Maeseneer J. Consultation length in general practice: Cross sectional study in six European countries. BMJ 2002;325(7362):472. [DOI: 10.1136/bmj.325.7362.472] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dwamena 2012
- Dwamena F, Holmes‐Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient‐centred approach in clinical consultations. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD003267.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Edwards 2003
- Edwards A, Elwyn G, Hood K, Robling M, Atwell C, Holmes‐Rovner M, et al. The development of COMRADE: A patient‐based outcome measure to evaluate the effectiveness of risk communication and treatment decision making in consultations. Patient Education and Counselling 2003;50(3):311‐22. [DOI] [PubMed] [Google Scholar]
EPOC 2013
- Effective Practice, Organisation of Care (EPOC). Suggested risk of bias criteria for EPOC reviews. EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2015. http://epoc.cochrane.org/epoc‐specific‐resources‐review‐authors (accessed 3 March 2016).
EPOC 2013b
- Effective Practice, Organisation of Care (EPOC). EPOC worksheets for preparing a Summary of Findings (SoF) table using GRADE. EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2013. http://epoc.cochrane.org/epoc‐specific‐resources‐review‐authors (accessed 8 March 2016).
EPOC 2013c
- Effective Practice, Organisation of Care (EPOC). What study designs should be included in an EPOC review?. EPOC Resources for review authors.. Oslo: Norwegian Knowledge Centre for the HealthServices;, 2013.
GRADEpro 2015 [Computer program]
- GRADEpro GDT. GRADEpro GDT for Windows. McMaster University, 2015.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist G, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. for the GRADE Working Group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐6. [DOI: 10.1136/bmj.39489.470347.AD] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Hobbs 2016
- Hobbs F, Bankhead C, Mukhtar T. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England. The Lancet 2016;387(10035):2323–30. [DOI: 10.1016/S0140-6736(16)00620-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Howie 1998
- Howie JG, Heaney DJ, Maxwell M, Walker JJ. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Family Practice 1998;15(2):165‐71. [DOI] [PubMed] [Google Scholar]
Lemon 2014
- Lemon TI, Smith RH. Consultation content not consultation length improves patient satisfaction. Journal of Family Medicine and Primary Care 2014;3(4):333‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marmot 2005
- Marmot M. Social determinants of health inequalities. The Lancet 2005;365(9464):1099‐104. [DOI: 10.1016/S0140-6736(05)71146-6] [DOI] [PubMed] [Google Scholar]
MECIR 2012
- Methodological Expectations of Cochrane Intervention Reviews (MECIR). Standards for the reporting of new Cochrane Intervention Reviews. Version 1.1. 17 December 2012. http://editorial‐unit.cochrane.org/sites/editorial‐unit.cochrane.org/files/uploads/MECIR%20Reporting%20standards%201.1_17122012_2.pdf (accessed 8 March 2016).
Mercer 2007
- Mercer S, Fitzpatrick B, Gourlay G, Voit G, McConnachie A, Watt G. More time for complex consultations in a high‐deprivation practice is associated with increased patient enablement. British Journal of General Practice 2007;57:960‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ogden 2004
- Ogden J, Bavalia K, Bull M, Frankum S, Goldie C, Gosslau M, et al. “I want more time with my doctor”: a quantitative study of time and the consultation. Family Practice 2004;21(5):479‐83. [DOI] [PubMed] [Google Scholar]
Potiriadis 2008
- Potiriadis M, Chondros P, Gilchrist G, Hegarty K, Blashki G, Gunn JM. How do Australian patients rate their general practitioner? A descriptive study using the General Practice Assessment Questionnaire. Medical Journal of Australia 2008;189(4):215‐9. [DOI] [PubMed] [Google Scholar]
RCGP 2013
- Royal College of General Practitioners. The 2022 GP: A vision for General Practice in the future NHS. http://www.rcgp.org.uk/campaign‐home/˜/media/files/policy/a‐z‐policy/the‐2022‐gp‐a‐vision‐for‐general‐practice‐in‐the‐future‐nhs.ashx (accessed 10 March 2016).
Rolfe 2014
- Rolfe A, Cash‐Gibson L, Car J, Sheikh A, McKinstry. Interventions for improving patients' trust in doctors and groups of doctors. Cochrane Database of Systematic Reviews 2014, Issue 3. [DOI: 10.1002/14651858.CD004134.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shaw 2014
- Shaw MK, Davis SA, Fleischer AB Jr, Feldman SR. The duration of office visits in the United States, 1993 to 2010. American Journal of Managed Care 2014;20(10):820‐6. [PubMed] [Google Scholar]
Starfield 2011
- Starfield B. The hidden inequity in health care. International Journal for Equity in Health 2011;10:15. [DOI: 10.1186/1475-9276-10-15] [DOI] [PMC free article] [PubMed] [Google Scholar]
van den Berg 2009
- Berg MJ, Bakker DH, Westert GP, Zee J, Groenewegen PP. Do list size and remuneration affect GPs' decisions about how they provide consultations?. BMC Health Service Research 2009;9:39. [DOI: 10.1186/1472-6963-9-39] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vanselow 1995
- Vanselow NA, Donaldson MS, Yordy KD. A new definition of primary care. JAMA 1995;273(3):192. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Verby 1979
- Verby JE, Holden P, Davis RH. Peer review of consultations in primary care: The use of audiovisual recordings. British Medical Journal 1979;1(6179):1686‐8. [PUBMED: 466180] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1996
- Ware J Jr, Kosinski M, Keller SD. A 12‐Item Short‐Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care 1996;34(3):220‐33. [DOI] [PubMed] [Google Scholar]
Wilson 1991
- Wilson A. Consultation length in general practice: a review. British Journal of General Practitioners 1991;41(344):119‐22. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Wilson 2002
- Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: A systematic review. British Journal of General Practice 2002;52(485):1012‐20. [PUBMED: 12528590] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Wilson 2006
- Wilson AD, Childs S. Effects of interventions aimed at changing the length of primary care physicians’ consultation. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD003540.pub2] [DOI] [PubMed] [Google Scholar]


