Abstract
Objectives:
To establish whether existing exercise programmes offered to people with sarcopenia or frailty adhere to the current evidence base.
Methods:
We conducted a national survey of practitioners delivering exercise programmes to older people with sarcopenia or frailty in the UK. The link to the online survey was distributed through email lists of professional societies, practice networks and social media. Questions covered target population and programme aims, type, duration and frequency of exercise, progress assessment and outcome measures.
Results:
One hundred and thirty-six responses were received. 94% of respondents reported prescribing or delivering exercise programmes to people with sarcopenia or frailty. Most programmes (81/135 [60%]) were primarily designed to prevent or reduce falls. Resistance training was the main focus in only 11/123 (9%), balance training in 61/123 (50%) and functional exercise in 28/123 (23%). Exercise was offered once a week or less by 81/124 (65%) of respondents. Outcome measures suitable for assessing the effect of resistance training programmes were reported by fewer than half of respondents (hand grip: 13/119 [11%]; chair stands: 55/119 [46%]).
Conclusions:
Current UK exercise programmes offered to older people with sarcopenia or frailty lack the specificity, frequency or duration of exercise likely to improve outcomes for this patient group.
Keywords: Exercise, Frailty, Resistance training, Sarcopenia, Survey
Introduction
Sarcopenia and frailty are important clinical syndromes that commonly affect older people. Both are associated with multiple adverse outcomes – falls, hospital admission, disability, dependency and earlier death[1-4]. The importance of timely identification of frailty is now well-recognised, and frailty case finding is receiving increasing attention in clinical recommendations and guidelines[5,6] and in the UK, frailty case finding has formed a mandatory part of the General Practice (primary care) contract, underpinned by population screening tools such as the electronic Frailty Index[7]. Sarcopenia and physical frailty show considerable overlap; 45% of those diagnosed with frailty met the criteria for sarcopenia in one recent study[8].
There is now a growing body of evidence that resistance training is both safe and effective in improving muscle strength, physical performance and activities of daily living in both those at risk of sarcopenia and frailty, and those with established sarcopenia and frailty[9,10]. Recent consensus guidance recommends that those at risk of, or with established sarcopenia or frailty, should be offered exercise training with a prominent resistance component (which can be part of a multimodal exercise programme)[11]. Recent systematic reviews examining the impact of differences in exercise intensity in trials for sarcopenia or frailty note that although training gains can be achieved at <50% 1-repetition maximum (1RM) intensity, the best results are seen at 80% of 1RM or higher[12]. Most exercise programmes included in systematic reviews for both sarcopenia and frailty have delivered 2-3 training sessions per week for at least 10 weeks; the mean programme duration for trials conducted with older people living with frailty was 23 weeks[13-15]. If exercise training in sarcopenia or frailty is to be based on current evidence, such programmes should therefore deliver exercise training with the above characteristics of modality, intensity, duration and frequency.
Despite the growing research evidence in this field, a previous survey of healthcare professionals engaged in treating older people[16] showed that few NHS organisations in the UK routinely diagnose sarcopenia (in part due to the lack of routine measurement of muscle mass and strength) and even fewer offer exercise training to patients with a diagnosis of sarcopenia. Whilst frailty is much more widely diagnosed, only half to two-thirds of centres offered exercise training or physiotherapy routinely to those diagnosed with frailty. Even for related conditions such as falls, where exercise training is strongly indicated and frequently used, recent data confirms that many programmes do not adhere to the evidence base, frequently being shorter, less intensive, or lacking key components, when compared to the programmes tested successfully in clinical trials[17].
The recent publication of the UK Chief Medical Officer Physical Activity guidelines with multiple references to the value of strength training[18], increased awareness of sarcopenia coupled with widespread frailty screening should drive an increase in demand for exercise training for these conditions. If such programmes are to be effective, it is essential that they are designed, commissioned and delivered in accordance with the emerging evidence base. Effective implementation in practice requires active management and guidance, as implementation of falls prevention programmes has shown[19]. We surveyed exercise professionals who reported delivering exercise programmes to patients with sarcopenia or frailty, to understand the characteristics of such programmes as currently implemented and whether they were consistent with current evidence for exercise training in sarcopenia and frailty.
Methods
We conducted an on-line survey, aimed at exercise professionals in the UK, including physiotherapists. The survey was constructed in SurveyMonkey and ran from 1st April 2019 to 30th June 2019. The questions comprising the survey are provided in the Supplementary Material. The survey comprised 18 questions in total, and was organised into four sections relating to: the respondents (role and place of work); the exercise programme (original purpose and primary aim); the programme components in more detail (particularly types of exercise component, frequency of sessions, duration, group size, equipment used, outcome and progression measures). Most questions included a free text option.
The weblink to the survey was distributed via the British Geriatrics Society (BGS) Sarcopenia and Frailty Research Special Interest Group mailing list, the AGILE (Chartered Society of Physiotherapy professional network for physiotherapists working with older people’s) mailing list and newsletter, the Chartered Society of Physiotherapy bi-monthly newsletter (Frontline), the NHS England Future Collaboration Platform ‘Supporting People Living with Frailty’ forum, together with links promoted using Twitter via the authors, the BGS and AGILE. Contacts were also asked to retweet and to pass on the weblink to local colleagues who delivered exercise programmes to older people.
Data from SurveyMonkey were downloaded as Microsoft Excel files before analysis using SPSS v24 (IBM, New York, USA). Descriptive statistics were generated for each questionnaire response.
Results
A total of 136 individuals responded to the questionnaire. 119 (88%) delivered exercise programmes in clinical practice posts; two (1%) were in research posts, four (3%) held joint clinical and research posts, and nine (7%) did not directly deliver exercise training; two did not respond to this question. Respondents worked for 99 different organisations, including NHS Trusts, clinical commissioning groups, private practices, and third sector providers. Most respondents (96/114 [84%]) reported practising in England; 11/114 (10%) were based in Scotland and 7/114 (6%) were based in Wales. No respondents reported being based in Northern Ireland.
Programme characteristics
128/136 (94%) of respondents reported prescribing or delivering exercise programmes to people with sarcopenia or frailty, with the majority (88/136; 65%) delivering programmes to both these groups. However, the primary purpose of the majority of programmes was to modify falls risk, as shown in Figure 1. Table 1 gives additional information about the programmes delivered, including information on group size, number of sessions offered, and duration of sessions. Not all respondents gave group size or number of sessions; some exercise practitioners misinterpreted the question and described the number of instructors or frequency of sessions in these free-text responses. Of those saying ‘other’, almost all noted that the frequency was determined by patient need.
Figure 1.
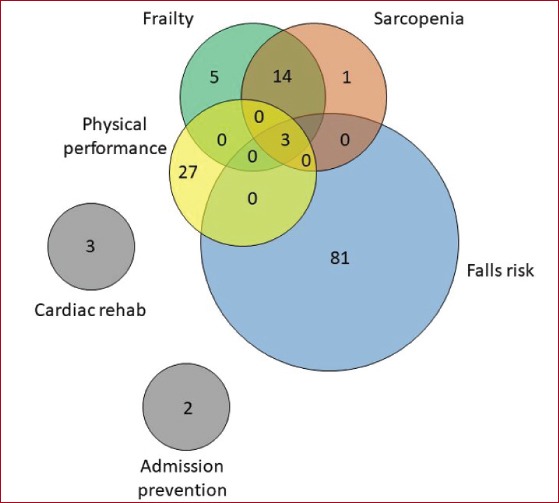
Primary purpose of programme.
Table 1.
Characteristics of programmes.
| Is programme based on an existing exercise programme? | Yes | 80/131 (61%) |
| No | 51/131 (39%) | |
| If yes, which exercise programme? | FaME | 31/80 (39%) |
| Otago | 50/80 (63%) | |
| Other | 11/80 (14%) | |
| Group based? | Group | 48/129 (37%) |
| One to one | 32/129 (25%) | |
| Mix of group and 1:1 | 49/129 (38%) | |
| Mean group size (SD) (n=93) | 9.5 (5.5) | |
| Median number of sessions offered (IQR) (n=74) | 8.5 (6 to 12) | |
| Frequency of sessions | 1x/wk | 81 (60%) |
| 2x/wk | 20 (15%) | |
| 3x/wk | 0 (0%) | |
| More than 3x/wk | 7 (5%) | |
| Other | 16 (12%) | |
| Duration of sessions | Less than 30 mins | 16 (12%) |
| 30 to 60 mins | 87 (64%) | |
| Greater than 60 mins | 21 (15%) |
Exercise programme composition
Figures 2a and 2b show the main focus of the exercises used in each programme, together with all of the modalities of exercise used in the programmes. Table 2 shows the modalities of exercise used in programmes with different primary purposes. Even for programmes where training to counteract sarcopenia or frailty was the main purpose, resistance training was deployed in only 13/20 (65%) of programmes. Exercises were undertaken in seated and standing positions within 112/121 (93%) of programmes; in sitting only in 2/121 (2%), and in standing only in 7/121 (6%). Programmes targeted upper limbs in 101/136 (74%) of cases, lower limbs in 118/136 (87%) of cases, and core stability/strength in 98/136 (72%) of cases. Figure 3 shows the aids to resistance training that were used in programmes
Figure 2.
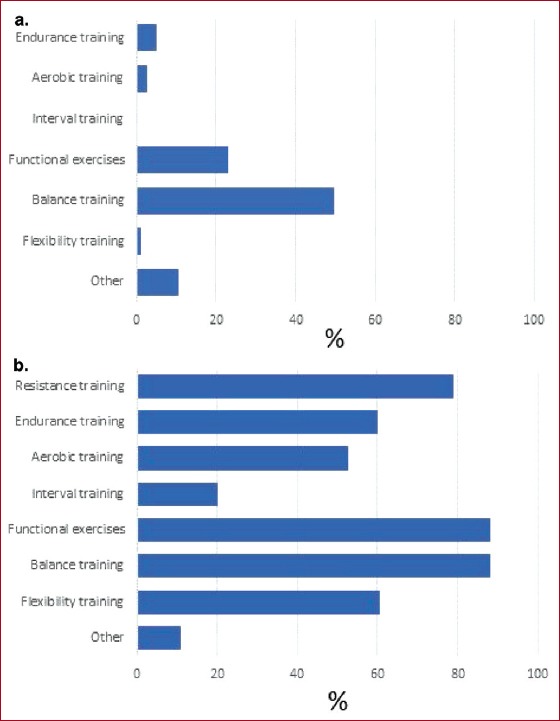
a) Main focus of exercise in programme. b) All types of exercise included in each programme.
Table 2.
Primary purpose of programme vs contents:
| Primary purpose of programme | Content of programme | ||||||
|---|---|---|---|---|---|---|---|
| Resistance training | Muscle endurance | Aerobic training | Interval training | Functional exercises | Balance training | Flexibility training | |
| Sarcopenia or frailty (n=20) | 13 (65%) | 9 (45%) | 9 (45%) | 2 (10%) | 15 (75%) | 16 (80%) | 9 (45%) |
| Falls risk (n=81) | 62 (77%) | 47 (58%) | 39 (48%) | 17 (21%) | 66 (81%) | 67 (83%) | 46 (57%) |
| Physical performance (n=27) | 19 (70%) | 16 (59%) | 13 (48%) | 4 (15%) | 24 (89%) | 23 (85%) | 18 (67%) |
| Other (n=7) | 4 (57%) | 2 (29%) | 4 (57%) | 2 (29%) | 4 (57%) | 3 (43%) | 2 (29%) |
Figure 3.
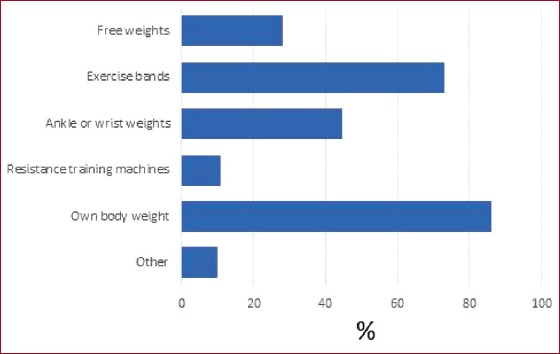
Aids to resistance training.
Exercise intensity assessment and progression
Most respondents (77/120; 64%) used regular, individualised review to determine progression of participants through the programme. Eight (7%) progressed all participants at the same rate, 25 (21%) allowed participants to determine their own progression, no progression occurred in one programme, and nine (8%) used other means. Methods of assessing the correct intensity of work varied widely; 73/136 (57%) used measures of maximum repetition (e.g. 1 repetition maximum or 10 repetition maximum) to determine intensity; practitioner judgement without formal assessment was used in 25 (18%) of programmes, and the Borg rating of perceived exertion scale[20] was used in seven (5%).
Outcome measures
A wide range of outcome measures were reported, as shown in Table 3. The majority of programmes used outcome measures strongly related to falls – particularly balance measures including the Berg Balance Scale[21] and the Tinetti Balance and Gait Test[22]. This remained the case even for programmes where frailty and sarcopenia were the primary focus; it is noteworthy that use of measures of muscle strength or power such as grip strength[23], the Short Physical Performance Battery (SPPB)[24], or the sit to stand test[25], were reported as being used by fewer than half of respondents.
Table 3.
Outcome measures used vs primary purpose of exercise programme.
| Hand grip | Walk speed (short course) | SPPB | Timed up and go | Sit to stand | Tinetti | Berg | Six min walk | Shuttle walk | QoL | Falls efficacy/ confidence | Other functional test | Person-centred goals | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sarcopenia or frailty (n=20) | 2 (10%) | 6 (30%) | 0 (0%) | 8 (40%) | 9 (45%) | 7 (35%) | 3 (15%) | 2 (10%) | 0 (0%) | 1 (5%) | 3 (15%) | 1 (5%) | 0 (0%) |
| Falls risk (n=81) | 5 (6%) | 10 (12%) | 0 (0%) | 56 (69%) | 34 (42%) | 19 (23%) | 31 (38%) | 4 (5%) | 0 (0%) | 4 (5%) | 20 (25%) | 14 (17%) | 1 (1%) |
| Physical performance (n=27) | 5 (19%) | 7 (26%) | 0 (0%) | 17 (63%) | 10 (37%) | 9 (33%) | 7 (26%) | 0 (0%) | 0 (0%) | 4 (15%) | 1 (4%) | 7 (26%) | 3 (11%) |
| Other (n=7) | 1 (14%) | 0 (0%) | 0 (0%) | 2 (29%) | 2 (29%) | 0 (0%) | 1 (14%) | 1 (14%) | 0 (0%) | 1 (14%) | 0 (0%) | 0 (0%) | 0 (0%) |
Discussion
Despite almost all respondents stating they delivered exercise programmes to older people with sarcopenia or frailty, our survey results suggest that current programmes are not optimised for addressing these conditions. This may be a direct result of previous commissioning trends, which have focussed on commissioning falls prevention exercise programmes rather than exercise directed at sarcopenia or frailty. It may also reflect the nature of exercise training provision in the UK which has focussed on educating staff on provision of exercise to reduce falls.
Given that reversing sarcopenia or frailty is not the main focus of most of the programmes, it is not surprising that our survey suggests that current programmes are not optimised for addressing these conditions. Both balance training and lower limb strength training (often delivered via functional exercises reflecting real-life tasks rather than using free weights or resistance training machines) are important components of falls prevention programmes[26]. Falls programmes often use measures with prominent balance and gait components to measure progress, for instance the Berg Balance scale and the Tinetti score[21,22]. Measures of muscle strength were not used in the majority of programmes reported in this survey and resistance training was the main focus of the programme in fewer than 10% of cases. The frequency and duration of programmes was less than that used in most trials for sarcopenia or frailty, and the methods used to provide resistance training may not have been sufficient to generate an optimum training effect[12].
What is more surprising, given the strong research base[26] and presence of robust training opportunities, is that most programmes were not of sufficient intensity, duration or of the right composition to achieve their stated main purpose of preventing falls either. These finding reinforce previous audit results[19] and indicate the challenge of implementing the evidence base within real-life clinical settings, specifically within the financial, human and time constraints of the NHS. This may be indicative of a lack of free/reasonably priced, accessible, customised exercise programmes that can be quickly implemented by busy clinicians without significant modification. It may also be indicative of a lack of access to environments with resistance training equipment accessible to older people under supervision of appropriately qualified Physiotherapists and other exercise professionals. Given resistance training is type-specific (for example training should focus on the type of gain that is required – power vs strength, closed vs open chain) there may also be a specific training requirement to support staff to prescribe the right type of resistance training for the desired outcome.
Recently updated guidance on the diagnosis of sarcopenia issued by the European Working Group on Sarcopenia[27] allows the diagnosis of probable sarcopenia to be made by measurement of muscle function (grip strength or chair rise time) without measuring muscle mass and recommends that a diagnosis of probable sarcopenia should trigger interventions including resistance exercise training as recommended by current guidance[11,27]. This simplification is likely to improve the rate of sarcopenia diagnosis, which has until now been made in only a few NHS organisations due to the practical barriers of measuring muscle mass[16]. It seems likely that increasing numbers of individuals will receive diagnoses of sarcopenia or frailty, and effective exercise programmes need to be available which provide adequate resistance-based exercise to improve muscle strength if we are to avoid the deleterious outcomes of these conditions.
Current evidence supports the role of resistance training as an effective modality to improve sarcopenia and frailty. Although there is only limited evidence on the dose-response relationship for resistance training and outcomes in these groups, evidence from healthy older people and from those living with frailty and sarcopenia supports a greater training effect at 70-80% of 1-repetition maximum intensity, and a greater training effect with longer duration of training (up to one year)[12,28]. The duration, mode, intensity and monitoring described by practitioners in our survey appears unlikely to deliver optimum gains in strength and function for older people with sarcopenia or frailty. Flexibility in programme delivery is essential – not everyone with severe sarcopenia or severe frailty may be able to use a particular mode of resistance (e.g. free weights) but an accurate, consistent, objective approach to measurement of muscle strength would enable better individualisation of resistance training and would avoid underdosing of exercise.
Strengths and limitations
We were able to survey practitioners across many different healthcare organisations, collecting detailed information on how programmes were delivered in practice. However, our survey relies on the self-report of practitioners, rather than on direct observation of what practitioners actually did. For some responses (e.g. use of 10-repetition maximum to decide intensity and progression), the precise way that such evaluations were deployed and used are unclear and may differ between practitioners. Exercise is delivered in a variety of contexts by a range of practitioners. The distribution methods for our survey were weighted towards NHS staff, particularly physiotherapists, and additional groups (e.g. via the British Association of Sports and Exercise Scientists; inclusion of more community postural stability instructors and non-NHS exercise practitioners) would further improve the generalisability of our findings. A final limitation is that we did not collect information on exit routes from programmes in this survey. It is possible that exit routes to maintenance programmes did exist, and thus provided a longer duration of intervention than was evident from the programmes reported in this survey, but this requires further study.
Implications for practice
Exercise training requires time and resource for exercise professionals to deliver, and significant commitment by patients to take part in exercise programmes. It is therefore important that such programmes are conducted in a way that delivers the best possible outcomes for patients. At present, many exercise programmes offered to patients with sarcopenia or frailty do not appear to be optimised for these conditions. Longer programmes, with higher intensity training, focussed on resistance exercise is probably required. In tandem, outcomes relevant to resistance exercise need to form part of the monitoring and evaluation of such programmes. Such outcomes are not measured in a consistent or appropriate way at present; indeed some programmes do not appear to assess intensity or progression in any formal way. This may reflect a belief that it is not possible to individualise assessment satisfactorily using such measurements, but it could equally reflect a lack of guidance on the most appropriate methods to use in this group of patients. Consensus on the optimum model of care to deliver effective exercise training for patients with sarcopenia or frailty does not currently exist, but developing consensus on preferred models across patients, clinicians, funders and policymakers is probably necessary to make progress in this area. Whilst programmes need to treat sarcopenia and frailty in line with the current evidence base, such programmes need to have sufficient flexibility to encompass the diverse range of needs of older people – many of whom will also be at risk of falls.
Our findings suggest that current provision of falls prevention exercise services may fail to meet optimum characteristics for best outcomes. Rather than developing a new, parallel set of programmes specifically for people with sarcopenia and frailty, there is an opportunity to work closely with existing Falls Prevention Services to adapt existing programmes so that they are optimised for those with falls and for those sarcopenia and frailty given the overlap between these conditions. Such ‘Falls, Sarcopenia and Frailty’ programmes could be developed from existing falls prevention programmes, and strong advocacy of such an approach would help to make the case nationally for sufficient investment in exercise programmes to deliver programmes of appropriate frequency and duration for large numbers of people with falls, sarcopenia and frailty. Making these changes will require raising awareness of the need for resistance training programmes for sarcopenia and frailty and will likely require additional training and guidance for exercise practitioners in these conditions. A successful approach is likely to require providing the tools for busy clinicians to implement effective exercise within the limited time available. This may come in the form of a pre-prepared programme, free of copyright and at reasonable price that clinicians can use with minimal modification other than choosing the starting level according to the ability of their patient. It may also require partnerships to be developed between NHS providers and local private exercise providers to allow access to resistance training equipment not readily available within the NHS. Access would ideally be partnered with dedicated specialist supervision from physiotherapists or other exercise professionals with appropriate training in providing exercise to those with sarcopenia or frailty. These initiatives will need leadership and coordination at a national level to successfully influence funders, commissioners and policymakers to commission and deliver exercise programmes that adhere to evidence-based guidelines for these three conditions.
Whilst more research would help to optimise the best modes of delivery of exercise to people with sarcopenia and frailty, a more rapid and effective way of driving improvement would be to benchmark existing practice across the range of different exercise programmes currently being delivered (such as those described in our survey) by comparing the characteristics of these programmes with the outcomes achieved in real-world clinical practice. Such an approach also provides an opportunity to improve practice and outcomes by feeding back information on the most effective programmes to practitioners via a series of improvement cycles. Similar programmes in related fields have been successful in driving change in practice. The Royal College of Physicians Falls and Fragility Fracture Audit Programme (FFFAP), which incorporates the National Hip Fracture Database, has led to significant improvements in hip fracture care, in part by benchmarking and feedback[29]. For example, within the FFFAP, the recent Physiotherapy Hip Sprint audit has been a key driver in the development of hip fracture rehabilitation standards by the Chartered Society of Physiotherapists[30]. Conducting and disseminating results to drive change from randomised controlled trials takes many years, and a programme of benchmarking, feedback and toolkit provision would provide a more rapid route to driving innovation, spreading best practice, reducing ineffective service provision and optimising outcomes from exercise programmes for older people with sarcopenia and frailty.
Acknowledgements
MDW and AAS acknowledge support from the NIHR Newcastle Biomedical Research Centre.
The authors gratefully acknowledge the assistance of the British Geriatrics Society and AGILE in helping to distribute the survey analysed in this work.
AC is part-funded by the National Institute for Health Research Yorkshire and Humber Applied Research Collaboration. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Footnotes
Edited by: Yannis Dionyssiotis
References
- 1.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393:2636–46. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 2.Dodds R, Sayer AA. Sarcopenia and frailty:new challenges for clinical practice. Clin Med (Lond) 2016;16:455–8. doi: 10.7861/clinmedicine.16-5-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beaudart C, Zaaria M, Pasleau F, Reginster JY, Bruyère O. Health Outcomes of Sarcopenia:A Systematic Review and Meta-Analysis. PLoS One. 2017;12:e0169548. doi: 10.1371/journal.pone.0169548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner G, Clegg A British Geriatrics Society;Age UK;Royal College of General Practitioners. Best practice guidelines for the management of frailty:a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing. 2014;43:744–7. doi: 10.1093/ageing/afu138. [DOI] [PubMed] [Google Scholar]
- 6.Walston J, Buta B, Xue QL. Frailty Screening and Interventions:Considerations for Clinical Practice. Clin Geriatr Med. 2018;34:25–38. doi: 10.1016/j.cger.2017.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clegg A, Bates C, Young J, Ryan R, Nichols L, Teale EA, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45:353–60. doi: 10.1093/ageing/afw039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gingrich A, Volkert D, Kiesswetter E, Thomanek M, Bach S, Sieber CC, et al. Prevalence and overlap of sarcopenia, frailty, cachexia and malnutrition in older medical inpatients. BMC Geriatr. 2019;19:120. doi: 10.1186/s12877-019-1115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cruz-Jentoft AJ, Landi F, Schneider SM, Zuniga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults:a systematic review Report of the International Sarcopenia Initiative (EWGSOP and IWGS) Age Ageing. 2014;43:748–59. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Apóstolo J, Cooke R, Bobrowicz-Campos E, Santana S, Marcucci M, Cano A, et al. Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults:a systematic review. JBI Database System Rev Implement Rep. 2018;16:140–232. doi: 10.11124/JBISRIR-2017-003382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, et al. International Clinical Practice Guidelines for Sarcopenia (ICFSR):Screening, Diagnosis and Management. J Nutr Health Aging. 2018;22:1148–61. doi: 10.1007/s12603-018-1139-9. [DOI] [PubMed] [Google Scholar]
- 12.Beckwée D, Delaere A, Aelbrecht S, Baert V, Beaudart C, Bruyere O, et al. Exercise Interventions for the Prevention and Treatment of Sarcopenia. A Systematic Umbrella Review. J Nutr Health Aging. 2019;23:494–502. doi: 10.1007/s12603-019-1196-8. [DOI] [PubMed] [Google Scholar]
- 13.Moore SA, Hrisos N, Errington L, Rochester L, Rodgers H, Witham M, et al. Exercise as a treatment for sarcopenia:An umbrella review of systematic review evidence. doi: 10.1016/j.physio.2019.08.005. Physiotherapy 2019 [epub ahead of print] DOI:https://doi.org/10.1016/j.physio.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Lopez P, Pinto RS, Radaelli R, Rech A, Grazioli R, Izquierdo M, et al. Benefits of resistance training in physically frail elderly:a systematic review. Aging Clin Exp Res. 2018;30:889–99. doi: 10.1007/s40520-017-0863-z. [DOI] [PubMed] [Google Scholar]
- 15.Jadczak AD, Makwana N, Luscombe-Marsh N, Visvanathan R, Schultz TJ. Effectiveness of exercise interventions on physical function in community-dwelling frail older people:an umbrella review of systematic reviews. JBI Database System Rev Implement Rep. 2018;16:752–75. doi: 10.11124/JBISRIR-2017-003551. [DOI] [PubMed] [Google Scholar]
- 16.Offord NJ, Clegg A, Turner G, Dodds RM, Sayer AA, Witham MD. Current practice in the diagnosis and management of sarcopenia and frailty –results from a UK-wide survey. J Frailty Sarcopenia Falls. 2019;4:71–7. doi: 10.22540/JFSF-04-071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Royal College of Physicians. Older people's experience of therapeutic exercise as part of a falls prevention service. 2016. [[Accessed 01/12/2019]]. Downloaded from: https://www.rcplondon.ac.uk/projects/outputs/older-peoples-experience-therapeutic-exercise-part-falls-prevention-service .
- 18.Department of Health and Social Care. UK Chief Medical Officers'Physical Activity guidelines. 2019. [[Accessed 13/01/2020]]. Dowloaded from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf .
- 19.Carpenter H, Audsley S, Coupland C, Gladman J, Kendrick D, Lafond N, et al. PHysical activity Implementation Study In Community-dwelling AduLts (PHISICAL):study protocol. Inj Prev. 2019;25:453–8. doi: 10.1136/injuryprev-2017-042627. [DOI] [PubMed] [Google Scholar]
- 20.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exercise. 1982;14:377–81. [PubMed] [Google Scholar]
- 21.Tinetti ME. Performance-oriented Assessment of Mobility Problems in Elderly Patients. J Am Geriatr Soc. 1986;34:119–26. doi: 10.1111/j.1532-5415.1986.tb05480.x. [DOI] [PubMed] [Google Scholar]
- 22.Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly:validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7–S11. [PubMed] [Google Scholar]
- 23.Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies:towards a standardised approach. Age Ageing. 2011;40:423–9. doi: 10.1093/ageing/afr051. [DOI] [PubMed] [Google Scholar]
- 24.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function:association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 25.Bohannon RW. Reference values for the five-repetition sit-to-stand test:a descriptive meta-analysis of data from elders. Percept Mot Skills. 2006;103:215–22. doi: 10.2466/pms.103.1.215-222. [DOI] [PubMed] [Google Scholar]
- 26.Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, et al. Exercise to prevent falls in older adults:an updated systematic review and meta-analysis. Br J Sports Med. 2017;51:1750–8. doi: 10.1136/bjsports-2016-096547. [DOI] [PubMed] [Google Scholar]
- 27.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia:revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borde R, Hortobágyi T, Granacher U. Dose-Response Relationships of Resistance Training in Healthy Old Adults:A Systematic Review and Meta-Analysis. Sports Med. 2015;45:1693–720. doi: 10.1007/s40279-015-0385-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Healthcare Quality Improvement Partnership. National Hip Fracture Database Annual Report. 2018. [[Accessed 01/12/19]]. Downloaded from: https://www.hqip.org.uk/resource/national-hip-fracture-database-nhfd-annual-report-2018/#.XeN4tfZ2tPY .
- 30.Royal College of Physicians of London 2019. Recovering after a hip fracture:helping people understand physiotherapy in the NHS. [[Accessed 01/12/2019]]. Downloaded from: https://www.fffap.org.uk/FFFAP/landing.nsf/phfsa.html .


