Abstract
Patients often have difficulty comprehending or recalling information given to them by their healthcare providers. Use of ‘teach-back’ has been shown to improve patients’ knowledge and self-care abilities, however there is little guidance for healthcare services seeking to embed teach-back in their setting. This review aims to synthesize evidence about the translation of teach-back into practice including mode of delivery, use of implementation strategies and effectiveness. We searched Ovid Medline, CINAHL, Embase and The Cochrane Central Register of Controlled Trials for studies reporting the use of teach-back as an educational intervention, published up to July 2019. Two reviewers independently extracted study data and assessed methodologic quality. Implementation strategies were extracted into distinct categories established in the Implementation Expert Recommendations for Implementing Change (ERIC) project. Overall, 20 studies of moderate quality were included in this review (four rated high, nine rated moderate, seven rated weak). Studies were heterogeneous in terms of setting, population and outcomes. In most studies (n = 15), teach-back was delivered as part of a simple and structured educational approach. Implementation strategies were infrequently reported (n = 10 studies). The most used implementation strategies were training and education of stakeholders (n = 8), support for clinicians (n = 6) and use of audits and provider feedback (n = 4). Use of teach-back proved effective in 19 of the 20 studies, ranging from learning-related outcomes (e.g. knowledge recall and retention) to objective health-related outcomes (e.g. hospital re-admissions, quality of life). Teach-back was found to be effective across a wide range of settings, populations and outcome measures. While its mode of delivery is well-defined, strategies to support its translation into practice are not often described. Use of implementation strategies such as training and education of stakeholders and supporting clinicians during implementation may improve the uptake and sustainability of teach-back and achieve positive outcomes.
Introduction
The healthcare system places a significant burden on patients to participate in their own care such as shared decision-making, providing informed consent or adhering to therapeutic regimens [1, 2]. Self-management of health is becoming increasingly complicated, leading to the need for strategies that support patients to not only understand complex health information, but also to apply this information in everyday life [3]. The ability to understand and use health information is a core component of health literacy, a concept which is consistently associated with health outcomes [4] and identified by the World Health Organization as key to achieving the Sustainable Development Goals [5].
There is a well-recognized communication gap in health care, with several studies identifying that healthcare providers may overestimate their own ability to communicate [6–8]. One survey-based study reported that 75% of surgeons believed they communicated well with their patients, but only 21% of their patients reported satisfactory communication [8]. Another qualitative study reported that 77% of doctors believed their patients were aware of their diagnosis, although only 57% of patients could correctly recall this [9]. These communication gaps can lead to adverse outcomes including compromised safety and increased economic burden [10, 11]. A frequently observed barrier to patient understanding is the continued use of medical terminology by doctors [12–14], with one systematic review reporting that patients want clearer explanations about their condition as they frequently misunderstand terms used in medical consultations [14]. Another major challenge in healthcare communication is patients’ ability to recall the information provided to them. Recall is considered an important mediator for treatment adherence and improved health outcomes [11, 15]. Studies have shown that less than half the information provided about medication and diet is accurately recalled by patients [15, 16], and can be even more challenging for people with low levels of education [3]. Interventions to improve communication at the patient-clinician interface are warranted; with one approach being the use of education and recall communication strategies such as ‘teach-back’ [17].
Teach-back involves asking patients to explain in their own words what a health provider has just told them. Any misunderstandings are then clarified by the health provider and understanding is checked again. This process continues until the patient can correctly recall the information that was given. Use of teach-back has been shown to improve knowledge, skills and self-care abilities in patients with chronic disease [18–25]. Teach-back is recommended as a health literacy-based communication approach in several policy documents and position statements, including the Australian Commission on Safety and Quality [17], the American Heart Association [26] and the American Diabetes Association [27]. Despite these recommendations and the simplicity of its use, teach-back is not consistently utilized [28–30]. This may, in part, be related to organizational or interpersonal barriers including lack of time, limited support by senior staff, or low self-efficacy to use teach-back [29, 31]. Furthermore, there is little guidance for healthcare services seeking to embed teach-back in their setting in a sustainable way. To promote the translation of teach-back into routine practice, it is important to identify strategies that may address any contextual and interpersonal barriers that support the uptake of this evidence-based intervention.
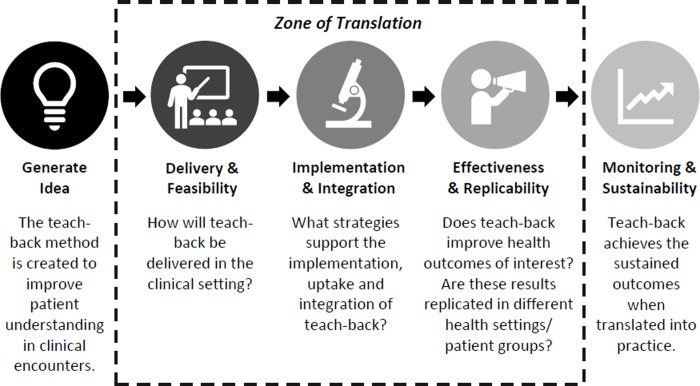
This narrative review aims to synthesize the latest evidence about the translation of teach-back within healthcare settings including: 1) how teach-back is delivered in different settings; 2) what strategies are used to support the implementation and uptake of teach-back; and 3) the effectiveness of teach-back across different healthcare settings and populations. As shown in Fig 1, these components form the ‘zone of translation’ within the translational research process [32], thus providing a conceptual basis for our research questions.
Fig 1. Translation of teach-back into practice; components evaluated in this review adapted from the Sax Institute’s Translational Research Framework [32].
Material and methods
A systematic review was undertaken in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [33].
Search strategy
An electronic search using Ovid Medline, CINAHL, Embase and The Cochrane Central Register of Controlled Trials was performed for published literature from inception to 11 July 2019. A sensitive search strategy was developed using the following search terms: “Teach-Back Communication” or “Teach-back” or “Show-me” or “Closing the loop” or “Closing the cycle” or “Ask-tell-ask” or “Repeat back” or “Verbal exchange” or “Patient-provider communication”. Reference lists from eligible studies, systematic reviews and grey literature were also reviewed for further relevant studies.
Study selection
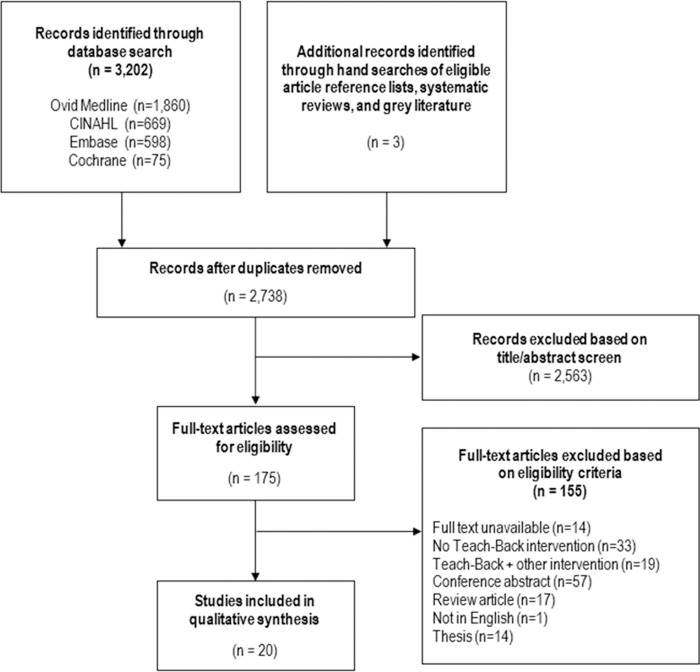
One author screened the titles and abstracts of potentially relevant studies against the eligibility criteria. Of potentially relevant studies identified from this initial screening, full length articles were attained and assessed independently by two authors. If there were discrepancies from the first two independent reviews, the authors discussed the conflicting results until consensus was reached. Reasons for exclusion at this stage were recorded and detailed in Fig 2.
Fig 2. Study selection.
Eligibility criteria
Study design and participants
Studies were included if they were conducted as a randomized controlled trial (RCT), non-randomized trial, quasi-experimental study, case-control study, analytic cohort study or before and after study that implemented a teach-back intervention. This review included participants of all ages who were patients, clients or consumers with any health condition.
Teach-back intervention
Eligible studies included at least one group that participated in a teach-back intervention. A teach-back intervention was defined as ‘a structured education approach in which something is explained, the recipient’s understanding is checked by explaining back to the educator what they have just been told or demonstrating what they have been shown, any misunderstandings are then clarified, and understanding is checked again’. For the purposes of this review, structured education approaches were defined as those that were not complex in nature (i.e. not comprised of multiple, interacting components which were expected to lead to the primary outcome through several different pathways) [34]. Given that previous reviews have evaluated teach-back in conjunction with additional strategies (e.g. discharge care bundles, motivational interviewing) [18, 19], studies that delivered a teach-back intervention in combination with other comprehensive strategies were excluded from this review; unless the sole effect of teach-back could be extracted separately.
Quality assessment
All studies were assessed for methodological quality by two independent reviewers using the Effective Public Health Practice Project (EPHPP) quality assessment tool for quantitative studies [35]. This tool was developed for use in RCTs, controlled clinical trials, case-control and observational study designs and includes eight domains of quality assessment: selection bias (were participants representative of the target population); study design; confounders (controlled for in the analysis); blinding (outcome assessors/participants); data collection methods (use of valid tools); withdrawals and dropouts; intervention integrity (consistency of the intervention); and analysis (use of appropriate statistical methods). The final two domains are not included in the overall methodological quality score. The EPHPP tool leads to an overall methodological rating score of strong, moderate or weak, and has been evaluated for content and initial construct validity and inter-rater reliability [35]. If consensus could not be reached by the two independent reviewers, a third reviewer was called upon to complete an independent quality assessment.
Data synthesis
Data from included studies were independently extracted by two authors. The following information was extracted from each study: lead author, publication year, country of study, study design, participant characteristics (% female, mean age, health condition), intervention description, outcome data (outcome measures and effect size), mode of delivery and implementation strategies. Implementation strategies were extracted into distinct categories established in the Implementation Expert Recommendations for Implementing Change (ERIC) project [36, 37]. In the ERIC project, a panel of experts in the field of implementation science and clinical practice compiled a list of 73 implementation strategies and grouped them into 9 categories, with the intention of guiding implementation research and clinical practice (S1 Table). The extracted data were evaluated against the ERIC framework to determine how teach-back has been previously implemented within healthcare settings. Data synthesis was primarily done by the first author and checked for consistency by the corresponding author.
Results
Literature search
The electronic search identified 2,738 studies for screening of eligibility after duplicate studies were removed. Of these, 2,563 studies were excluded based on title and abstract and full text was obtained for the remaining 175 studies. Based on the authors’ decisions, 20 studies met the eligibility criteria and were included in this review (Fig 2).
Study characteristics
Of the 20 studies, there were nine RCTs, two controlled clinical trials, four pre-post studies, one before and after study, three prospective cohort studies and one cross-sectional study. Most studies were from the USA (n = 10) or Iran (n = 7); with one study each from Australia, China and India. Studies were conducted across hospitals (n = 8), emergency departments (EDs; n = 3), outpatient clinics (n = 4), primary care practices (n = 2), community health centers (n = 1) and nursing homes (n = 1). There was a broad range of participant characteristics across studies. One study included children aged 6–13 years old; two studies focused on older adults aged ≥60 years; one study included young adults aged 20–30 years; two studies included people aged 30–55 years; and 15 studies included all adults aged ≥18 years. Studies included people with chronic conditions such as heart disease (n = 2), chronic obstructive pulmonary disease (n = 2), Type II Diabetes (n = 4), breast cancer (n = 1) and asthma (n = 2); post-surgical inpatients (n = 2); and people discharged from the ED (n = 2). Eleven studies included a higher percentage of females. Patient characteristics are summarized in Table 1.
Table 1. Study and participant characteristics.
| Author (year) | Setting | Study design | Participants | Primary Outcome(s) | Key Findings | Study Quality | |||
|---|---|---|---|---|---|---|---|---|---|
| N (I/C) | Age (years), mean (±SD) | % Female | Population/ Condition | ||||||
| Ahmadidarrehsima et al. (2016) [38] | Hospital, Iran | Controlled Clinical Trial | 50 (25/25) | I: 56(46–60)† C: 40 (40–54)† |
100% | Breast Cancer | Happiness | ↑ Oxford Happiness Inventory score in the TB group compared to the control group immediately post intervention (62.9 vs 29.8; p<0.001). | Strong |
| Ahrens & Wigres (2013) [3] | Hospital, USA | Before & After | 121 (60/61) | NR | NR | Neurological Patients | Patient Satisfaction | ↑ Patient satisfaction from 29.7% to 77.3% post-TB implementation. | Moderate |
| Badaczewski et al. (2017) [40] | Paediatric Care Centre, USA | Cross-sectional | 44 | 9 (6–13)† | 34% | Asthma | Patient-centered Interactions | ↑ Patient-centered communication (OR = 4.97; 95% CI: 4.47–5.53) and engagement of parents during pediatric clinical encounters following TB. | Weak |
| Bahri et al. (2018) [41] | Community Health Centre, Iran | RCT | 66 (32/34) | I: 53.5 (1.5) C: 53.3 (1.6) |
100% | Post-menopausal Women | Self-care Management | ↑ Knowledge about self-care and self-care activities in the TB group compared to the control group 1 month after the intervention (p<0.001). | Moderate |
| George et al. (2018) [42] | Hospital, India | Before & After | 98 | 18–70‡ | 38% | Type II diabetes | Medication Adherence | Patients in the low and medium medication adherence groups showed an improvement in medication adherence 2 months post-TB (p<0.05). Patients who were categorized in the high adherence group did not show any change after TB (that is they continued to be highly adherent). | Weak |
| Ghiasvand et al. (2017) [43] | Hospital, Iran | RCT | 80 (40/40) | I: 24.5 (4.5) C: 24.5 (4.5) |
100% | Women with Post-partum Depression | Quality of Life | ↑ Post-partum quality of life in the TB group compared to control group at 8-week follow-up (124.7 vs 115.0; p<0.001). | Moderate |
| Griffey et al. (2015) [44] | Emergency Department, USA |
RCT | 408 (212/196) | I: 36.0 (13.2) C: 34.7 (12.8) |
60% | Low Health Literacy | Comprehension & Satisfaction | ↑ Comprehension of post-ED medications (p<0.02), self-care (p<0.03) and follow-up instructions (p<0.001) in TB patients compared to standard care post-intervention. ↔ Comprehension or patient satisfaction between groups. |
Strong |
| Haney & Shepherd (2014) [45] | Hospital, USA | Prospective Cohort | 23 | NR | NR | Heart Failure (high-risk) | Hospital Re-admissions | ↓ 30-day re-admission rate from 18% to 13% over 6-months. | Weak |
| Kandula et al. (2011) [46] | Outpatient Clinic, USA | Two-Group, Pre-Post Study | 171 (58/113) | I: 52.8 (9.7) C: 56.2 (9.9) |
75% | Type II Diabetes | Knowledge Retention | ↑ Immediate recall of information in the TB + Education vs Education Only group. ↔ Compared to education only, TB + Education did not improve knowledge retention at 2-week follow-up. |
Weak |
| Kiser et al. (2012) [47] | Primary Care Centre, USA | RCT | 99 (67/32) | I: 63 (43–84)† C: 63 (44–83)† |
65% | COPD | Inhaler Technique | ↑ Inhaler technique score in the TB group compared to usual care group (mean change: 1.6 vs -0.5; p<0.001). | Moderate |
| Liu et al. (2018) [48] | Nursing Home, China | RCT | 260 (126/134) | I: 79.2 (8.8) C: 79.1 (9.2) |
49% | Older People | Health Literacy | ↑ Health literacy score in the TB group compared to the control group immediately post-intervention (110.1 vs 74.9; p<0.001). | Strong |
| Mahmoudir-ad et al. (2015) [49] | Outpatient Clinic, Iran | Controlled Clinical Trial | 70 (35/35) | I: 51.8 (4.2) C: 50.0 (5.6) |
75% | Type II Diabetes | Self-care Management | ↑ Foot self-care scores in the TB group compared to the control group at 3-month follow-up (29.3 vs 19.2; p<0.001). | Moderate |
| Moadab et al. (2015) [50] | Hospital, Iran | RCT | 60 (30/30) | I: 25.2 (2.9) C: 25.5 (2.7) |
100% | Post-Caesarean Surgery | Anxiety | ↓ Anxiety level scores in patients post-TB compared to control patients awaiting caesarean surgery (50.8 vs 59.4; p<0.001). | Moderate |
| Mollazadeh & Maslakpak (2018) [51] | Outpatient Clinic, Iran | RCT | 84 (42/42) | I: 38 (12.4) C: 41.3 (11.7) |
33% | Kidney Transplant Recipients | Self-care Management | ↑ Self-management scores in the TB group compared to the control group at 2-month follow-up (82.5 vs 74.4; p<0.001). | Strong |
| Morony et al. (2018) [52] | Telephone Call Centre, Australia | RCT | 637 (261/376) | I: 31.1 (6.4) C: 31.5 (6.6) |
87% | Telephone Health Service Users | Self-care Management | ↑ Confidence to act (OR = 2.44; p = 0.06) and knowledge of healthcare services (OR = 2.68; p = 0.06) in TB callers compared to control group callers. | Moderate |
| Negarandeh et al. (2013) [53] | Outpatient Clinic, Iran | RCT | 83 (43/40) | I: 50.3 (8.5) C: 49.1 (8.8) |
46% | Type II Diabetes | Knowledge Retention & Medication/ Diet Adherence | ↑ Mean scores of knowledge, and adherence to medication and diet in the TB group compared to the control group at 6-week follow-up (p< 0.001). | Moderate |
| Peter et al. (2015) [54] | Hospital, USA | Two-Group, Pre-Post Study | 469 (180/289) | NR | NR | Heart Failure (high-risk) | Comprehension & Hospital Re-admissions | ↑ Patient understanding of their disease. ↓ 12% in re-admission rates for heart failure patients 1 years post-TB implementation. |
Weak |
| Press et al. (2011) [55] | Hospital, USA | Prospective Cohort | 42 | 51.7 (17.4) | 73% | COPD & Asthma | Inhaler Technique | After one round of TB, 86% of participants achieved correct inhaler use. After a second-round of TB, all participants achieved correct use. | Moderate |
| Slater et al. (2017) [56] | Emergency Department, USA | Two-Group, Pre-Post Study | 209 (105/104) | I: 38.0 (14.0) C: 41.0 (18.0) |
68% | Emergency Department Patients | Knowledge Retention | ↑ Retention of discharge instructions (diagnosis, medications, follow-up instructions) in the TB group compared to the control group (recall rate 82.1% vs 70.0%; p<0.05). | Weak |
| Waszak et al. (2018) [57] | Emergency Department, USA | Prospective Cohort | 52 | NR | NR | Emergency Department Patients | Knowledge Retention | 100% of patients clearly understood how to take opioids, and 80.8% learned something new about how to take, store, or dispose of their medications safely. | Weak |
I = Intervention Group; C = Control Group; SD = Standard Deviation; COPD = Chronic obstructive pulmonary disease; TB = Teach-Back; NR = Not reported.
†Median (Interquartile range).
‡Range.
Methodological quality
The methodological quality of included studies varied (Tables 1 and S2). Four studies were rated as high quality, nine as moderate quality and seven as weak. Common methodologic limitations identified across studies included omission of reporting if outcome assessors were blinded to intervention/exposure study of participants, participants being blinded to the research questions and whether individuals selected to participate in the study were likely to be representative of the target population.
Delivery of teach-back
Teach-back interventions were delivered by either healthcare personnel, including nurses (n = 9), primary care providers (n = 2) and pharmacists (n = 1); or by research staff (n = 8). Fifteen studies [38, 39, 41, 43, 45–51, 53–55, 57] used teach-back as part of a structured educational approach. This teach-back enhanced education ranged from brief sessions to more complex training. Nine studies [38, 41, 43, 46, 48, 49, 51, 53, 54] comprised more than one education session over the study period (range 2–11); brochures or written information were given in five studies [39, 42, 47, 53, 57] to aid the teach-back process; and demonstration of a technique was used in two studies [47, 55]. There were four studies in which teach-back was delivered as a less structured approach; two of these focused on training clinicians to use teach-back as part of their routine care [31, 40], and two studies [44, 56] trained nursing staff to use teach-back when providing discharge instructions in the ED (Table 2).
Table 2. Implementation characteristics of teach-back.
| Author (year) | Person(s) Delivering Teach-Back | Mode of Delivery | Implementation Strategies (36, 37) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Evaluative & Iterative Strategies | Provide Interactive Assistance | Adapt & Tailor to Context | Develop Stakeholder Inter-relationships | Train & Educate Stakeholders | Support Clinicians |
Engage Consumers |
Utilize Financial Strategies | Change Infra-structure | |||
| Ahmadidarrehsima et al. (2016) [38] | Researcher | 8–11 breast cancer self-management education sessions with TB lasting 1.5 to 2 hours. | - | - | - | - | - | - | - | - | - |
| Ahrens & Wigres (2013) [39] | Nurse | Verbal and written medication side-effect education with TB implemented during hourly rounding (the ‘‘Always Ask” program). | ✓ | ✓ | ✓ | ✓ | |||||
| Badaczewski et al. (2017) [40] | Primary Care Provider | Primary care clinicians were provided with 3 one-hour interactive training sessions with TB on health literacy. TB occurrence during clinical encounters was measured using a Teach-back Loop Score. | ✓ | ✓ | |||||||
| Bahri et al. (2018) [41] | Researcher | Four 45-minute education sessions with TB on menopausal self-care using a video projector. | - | - | - | - | - | - | - | - | - |
| George et al. (2018) [42] | Pharmacist | Medium adherent patients were provided with a medication information leaflet and patient counseling with TB; Low adherent patients were provided with audio-visual aids, a medication information leaflet and patient counseling with TB. | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Ghiasvand et al. (2017) [43] | Researcher | Two 1-hour education sessions with TB on post-partum self-care. | - | - | - | - | - | - | - | - | - |
| Griffey et al. (2015) [44] | Nurse + Researcher | Standard discharge instructions with TB. | ✓ | ✓ | ✓ | ||||||
| Haney & Shepherd (2014) [45] | Nurse | One 60-minute self-management education session with TB. | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Kandula et al. (2011) [46] | Researcher | Two video education modules on Diabetes with TB. | - | - | - | - | - | - | - | - | - |
| Kiser et al. (2012) [47] | Researcher | One education session of correct inhaler use including visual demonstration with TB + a take-home information sheet. | - | - | - | - | - | - | - | - | - |
| Liu et al. (2018) [48] | Graduate Students | Two health literacy education sessions with TB delivered over 6-months. | ✓ | ✓ | ✓ | ||||||
| Mahmoudirad et al. (2015) [49] | Researcher | Up to three 45-minute education sessions on foot self-care with TB. | - | - | - | - | - | - | - | - | - |
| Moadab et al. (2015) [50] | Primary Care Provider | One 30-45-minute tailored education session on caesarian surgery with TB pre-op. | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Mollazadeh & Maslakpak (2018) [51] | Nurse | Five 60-minute tailored self-care education sessions with TB over 3 months. | ✓ | ||||||||
| Morony et al. (2018) [52] | Nurse | Telephone callers (nurses) were trained in using TB with callers when providing comprehensive information and advice. | ✓ | ✓ | ✓ | ||||||
| Negarandeh et al. (2013) [53] | Nurse | Three 20-minute Diabetes education sessions with TB + a take-home information sheet. | |||||||||
| Peter et al. (2015) [54] | Nurse | TB-enhanced, structured education on heart failure self-care over 3-days. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Press et al. (2011) [55] | Researcher | One education session of correct inhaler use including visual demonstration with TB. | - | - | - | - | - | - | - | - | - |
| Slater et al. (2017) [56] | Nurse | Standard discharge instructions with TB. | ✓ | ✓ | |||||||
| Waszak et al. (2018) [57] | Nurse | One dual-modal (verbal and written) education session on opioid use with TB. |
✓ | ✓ | ✓ | ||||||
- = Not Relevant (researcher-led implementation); NR = Not Reported; TB = Teach-back.
Implementation strategies
Implementation strategies were infrequently reported within studies. Of the 20 included studies, only 10 [39, 40, 44, 48, 51–54, 56, 57] reported sufficient information regarding implementation of teach-back. Of the remaining 10 studies, three [42, 45, 50] did not report any details related to implementation and seven [38, 41, 43, 46, 47, 49, 55] delivered teach-back via research staff, meaning that implementation strategies were not relevant in clinical practice, but for research purposes only (Table 2).
Train and educate stakeholders
Providing training and education to staff who were employing teach-back was the most used implementation strategy (n = 8 studies) [39, 40, 44, 48, 52, 54, 56, 57]. Education and training programs differed but generally focused on four main concepts: 1) identifying the needs of the patient; 2) establishing the preferred learning style of the patient; 3) choosing the appropriate resources; and 4) demonstration of how to use teach-back during a patient interaction. Seven studies [39, 44, 48, 52, 54, 56, 57] provided a one-time education/training program in teach-back, and one study [40] provided three 1-hour interactive training sessions in health literacy and use of teach-back. One study [54] utilized an online education module, five studies [44, 48, 52, 56, 57] implemented a group education session, three studies [40, 44,56] provided interactive role-playing scenarios and one study provided written education materials [39].
Use of evaluative and iterative strategies
Four studies [39, 51, 52, 54] reported the use of evaluative and iterative strategies. Two of the studies [52, 54] developed a quality monitoring system to ensure teach-back was being undertaken appropriately, with one of these [54] also providing continued auditing of the teach-back standard. One study [39] implemented a weekly email update to inform nurses delivering teach-back on their progress and improvements, and one study [51] developed a needs assessment checklist to inform a targeted education approach for each patient.
Provide interactive assistance
Providing interactive or technical assistance were reported in two studies [44, 54]. This included techniques such as documentation and tracking of the use of teach-back encounters via patient electronic medical records (EMRs).
Adapt and tailor to context
No studies reported an interpersonal focus by tailoring or adapting the teach-back intervention to the specific patient population.
Develop stakeholder interrelationships
Developing stakeholder relationships, an important process for sustainability, was reported in only two studies [39, 54]. One of these studies [54] designated teach-back champions on each ward to guide and motivate nurses in the use of teach-back. These champions were provided with an additional 2-hour ‘‘train-the-trainer” workshop. The other study [39] organized implementation team meetings between nurses (administers of teach-back) and a newly convened patient perception team (made up of managers, bedside nurses, and individuals who had been treated at the hospital) to achieve nursing feedback and support for the intervention.
Support for clinicians
Ongoing support for clinicians implementing teach-back was reported in six studies [39, 40, 52, 54, 56, 57] and mainly focused on developing clinical reminders for teach-back use. This included use of prompts such as posters and flyers on the wards [39, 40, 56, 57], reminder cards [56], notes on white boards in patients’ rooms [54] and electronic prompting processes such as reminder emails or videos [39, 52, 57].
Engage consumers
Only one study [48] engaged patients in the development of an implementation plan for the delivery of teach-back. This study solicited feedback from recipients through interviews on the teach-back process to inform the delivery of the intervention moving forward.
Changes in infrastructure
Three studies [44, 54, 57] employed a change in infrastructure, primarily through the EMR system. This included adding teach-back prompts to the EMR [40, 54] and making patient education materials and documentation of teach-back available within the EMR [57].
Utilize financial strategies
Utilizing financial strategies was one of the least utilized implementation strategies, applied in only one study [48]. This study organized a prize-winning knowledge contest among patients each month as an incentive to reinforce the educational effect of teach-back and stimulate interest in patients to participate.
Outcome measures and effectiveness of teach-back
Although there was variability among studies in relation to study populations, settings and outcomes, 19 studies (95%) reported positive findings for primary outcome measures. The outcomes measured fell into three distinct categories: 1) knowledge, skills and attitudes (disease knowledge, comprehension and retention, patient satisfaction); 2) behavior change (self-care practices, medication adherence); and 3) objective health-related outcomes (hospital re-admissions, quality of life). Three studies [44, 48, 52] measured health literacy, however only one study measured health literacy change as an outcome [48]. In this RCT of older people (aged ≥60 years), health literacy scores–measured by the Chinese Citizen Health Literacy Questionnaire–significantly increased in the teach-back group compared to the control group (110.1 vs 74.9; p = 0.001) [48]. The three studies that involved patients discharged from ED [44, 56, 57] reported increased knowledge of post-discharge procedures after teach-back compared to standard discharge instructions. Most studies were conducted among participants with chronic conditions (n = 12). Studies that included participants with Type II diabetes reported significant improvements in medication adherence [42, 53], diet changes [53] and foot self-care [49] following teach-back compared to usual care control groups. The two studies in heart failure patients measured hospital re-admissions, with both studies reporting a minor reduction in re-admission rates [45, 54]. Demonstration of proper inhaler technique using teach-back in people with chronic obstructive pulmonary disease lead to significant improvements in inhaler technique in two studies [47, 55]. One study in children with asthma found that teach-back was associated with increased patient-centered communication (OR = 4.97; 95% CI: 4.47–5.53) and increased engagement of parents during pediatric clinical encounters [40]. Other outcomes showing improvements following teach-back included happiness in breast cancer patients [38], quality of life in post-partum women [43], anxiety in women awaiting caesarean surgery [50] and patient satisfaction in participants using a maternal and child health call center [52]. Most outcomes were measured immediately post-intervention (n = 11); studies with follow-up ranged from 2 weeks to 1 year. Outcome measures and key findings are summarized in Table 1.
Discussion
To our knowledge, this is the first systematic review appraising the translation of teach-back into clinical practice. We found that implementation of teach-back is not well described in the literature. The most frequently utilized implementation strategies were training and education of stakeholders (e.g. educational materials, training modules) and reminding clinicians to implement the intervention (e.g. clinical reminders/prompts). Findings from this review can inform healthcare services and providers about key strategies to optimize the routine uptake and sustainability of this effective health literacy-based communication technique.
Delivery and feasibility
Teach-back was most commonly delivered as part of a structured, but simple educational approach, with this ‘teach-back enhanced education’ being reported as effective across a wide range of settings, populations and outcome measures. Settings included hospitals, outpatient clinics, the ED, and community health centers. Many health interventions are designed for a specific setting and are generally not implemented in a different setting to that which it was intended for [58]. Findings from this review reflect the broad application of teach-back enhanced education across multiple settings, including the ED. Delivering health interventions or programs in the ED is challenging given the high-pace and perplexing nature of this setting. Previous studies have shown that ED clinicians rarely confirm comprehension of instructions with their patients and that patient comprehension of ED discharge instructions is poor [59, 60]. Three studies in this review were undertaken in the ED setting [44, 56, 57] and reported increased knowledge of post-discharge procedures, higher levels of diagnosis knowledge and improved recall of follow-up instructions compared to standard discharge care. These results highlight the success of teach-back in reinforcing ED discharge instructions and should be considered by ED clinicians as a key component when providing patients with information.
Implementation and integration
The most used implementation strategy in the included studies was training and educating the healthcare providers who were delivering teach-back. Education sessions were often structured and focused on the importance of tailoring teach-back to patient needs, reflecting best-practice communication techniques [61]. However, while education is essential to introduce a new intervention it is well-established that training alone is not sufficient to effect ongoing change and uptake into standard clinical practice [62]. Successful implementation requires a multifaceted approach that is guided by an implementation plan or framework, and incorporates an identified need for improvement, collaboration between stakeholders and health services, flexibility in responding to feedback, using data to drive practice change, and a culture receptive to change [63]. Among the studies in this review, only one reported using almost all implementation strategies in the ERIC framework [54]. The authors took a staged approach to implementation, initially establishing a multidisciplinary working group. This group developed a structured teach-back protocol; clinicians were trained in identification of the key learner for each patient and educated in use of teach-back through an online learning module; teach-back prompts and feedback were provided within the patient EMR; and teach-back champions were trained and assigned to individual wards. This detailed and systematic implementation plan resulted in significant improvements in patients’ understanding of their disease, improved compliance among nurses regarding the use of teach-back in educating patients, and a sustained drop in readmission rates for patients with heart failure one-year post-implementation.
The lack of involvement from consumers in the implementation of teach-back was surprising, given the consumer-focus of teach-back and the current global interest in the involvement of consumers in the design and implementation of healthcare interventions. Three studies [51, 53, 54] mentioned assessing the patients’ understanding before providing teach-back in order to tailor the intervention to fit the individual’s learning needs, however this is part of standard teach-back practice.
In terms of process evaluation, no studies in this review assessed implementation fidelity. This concept refers to the extent to which an intervention has been implemented in practice as it was intended to [64]. Implementation fidelity has been frequently recommended as an essential component of undertaking intervention trials [65], yet was not examined in any of the studies included in this review. Therefore, a key message from our review is that there is a need to improve reporting of implementation fidelity within intervention trials assessing the teach-back method. This would allow researchers and clinicians to identify the association between successful implementation and improved outcomes and promote the integration of teach-back into routine practice.
Effectiveness and replicability
The overwhelming effectiveness of teach-back reported in 95% of studies, and across such a broad range of patient groups and outcomes, supports the use of teach-back enhanced education in clinical practice. Additionally, the studies were of moderate quality which limits the degree of caution for interpreting this conclusion. Systematic reviews of studies examining educational interventions (without teach-back) have shown inconclusive or even negative findings [66, 67]. Most studies in this review delivered teach-back as part of a simple educational program and compared outcomes against participants receiving ‘general education’. This demonstrates that teach-back is a valuable addition to patient education in health care settings. However, most learning-related outcomes were measured immediately post-intervention; therefore, research demonstrating that teach-back has long-term effects on patient knowledge and recall is warranted. Further, outcomes such as patient knowledge, recall of information and medication adherence are feasible outcome measures within healthcare settings. Providing feedback to clinicians through demonstration of positive outcomes may be one useful strategy to build support for continued use of teach-back.
Finally, comprehending medical diagnoses and treatments requires a level of intermediate or proficient health literacy. It is well established that patients with low health literacy have less ability to understand and recall health information [68, 69], although few studies examined the effectiveness of teach-back to improve comprehension and recall across patients with differing literacy levels. Three studies in this review [44, 48, 52] measured health literacy in participants, although only Liu et al. measured health literacy change as an outcome. In this RCT of older people (aged ≥60 years), health literacy scores significantly increased in the teach-back group compared to the control group [48]. A second RCT reported that teach-back significantly improved comprehension of post-ED care (i.e. medications, self-care, and follow-up instructions) among patients with limited health literacy, compared to standard ED discharge instructions [44]. Similarly, Morony et al. reported improved knowledge of healthcare services among people with inadequate health literacy following a nurse-delivered teach-back teleconsultation [52]. Health providers are the most trusted source of health information for people [70], and therefore have a responsibility to deliver information to their patients that is clear, understandable and practical [71]. This is especially true for those with limited literacy skills, who are more likely to solely rely on their clinician for health information [72]. Teach-back may be a feasible, practical and cost-effective intervention to address this health literacy-based communication gap in health care.
Strengths and limitations
The strengths of this review include our rigorous methodology and comprehensive search strategy. We have confidence that we identified all published studies that met our inclusion criteria as we used various synonyms of “teach-back” in our search strategy. Furthermore, we excluded studies that delivered a teach-back intervention in combination with other comprehensive strategies so we could examine the sole effect of teach-back. This differed from all previous reviews on the teach-back method [18, 19]. Limitations of our review should also be considered. Searches were limited to published studies, subjecting this review to the possibility of publication bias. Only half of the included studies provided a detailed description of implementation–three studies provided no information on implementation and teach-back was delivered by research staff in seven studies (implementation strategies not relevant in clinical practice)–which limited the main aim of this review. Additionally, given the heterogeneity of outcome measures, it was not possible to conduct a meta-analysis. It would be useful to understand the link between implementation and health outcomes; however, this was not possible due to the lack of detail regarding implementation and heterogeneity of implementation strategies in the included studies.
Conclusions
Teach-back is effective across a wide range of settings, populations and outcome measures, although implementation techniques are not well described. Use of recognized implementation strategies such as training and education of stakeholders (e.g. educational materials, training modules) and supporting clinicians to apply the intervention (e.g. clinical reminders/prompts) may support the uptake and sustainability of teach-back. In clinical practice, teach-back provides a low-cost and effective technique that can be used to enhance structured, simple education to achieve positive outcomes in communication at the patient-clinician interface. Further research examining the long-term benefits and barriers to translation of teach-back is recommended.
Supporting information
(DOCX)
(DOCX)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
JT is supported by an Australian National Health and Medical Research Council (NHMRC) Postgraduate Scholarship (1151089) and AB is supported by a MRFF NHMRC TRIP Fellowship (1150745). This work was funded in part by the Nurses Board of Victoria Legacy Limited (NBVLL) and the views expressed in this article do not represent those of the NBVLL.
References
- 1.Allegrante JP, Wells MT, Peterson JC. Interventions to Support Behavioral Self-Management of Chronic Diseases. Annual Review of Public Health. 2019;40(1):127–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Osuna E, Pérez-Carrión A, Pérez-Cárceles MD, Machado F. Perceptions of health professionals about the quality of communication and deliberation with the patient and its impact on the health decision making process. Journal Of Public Health Research. 2018;7(3):1445-. 10.4081/jphr.2018.1445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laws MB, Lee Y, Taubin T, Rogers WH, Wilson IB. Factors associated with patient recall of key information in ambulatory specialty care visits: Results of an innovative methodology. PLoS ONE. 2018;13(2):e0191940 10.1371/journal.pone.0191940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Annals of Internal Medicine. 2011;155(2):97–107. 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Shanghai Declaration on promoting health in the 2030 Agenda for Sustainable Development. http://www.who.int/healthpromotion/conferences/9gchp/shanghaideclaration/en/. Accessed May 2019. 2016. [DOI] [PubMed]
- 6.Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010;10(1):38–43. [PMC free article] [PubMed] [Google Scholar]
- 7.Coran JJ, Koropeckyj-Cox T, Arnold CL. Are Physicians and Patients in Agreement? Exploring Dyadic Concordance. Health Education & Behavior. 2013;40(5):603–11. [DOI] [PubMed] [Google Scholar]
- 8.Tongue JR, Epps HR, Forese LL. Communication skills for patient-centered care. J Bone Joint Surg Am. 2005;87:652–8. [Google Scholar]
- 9.Olson DP, Windish DM. Communication Discrepancies Between Physicians and Hospitalized PatientsPatient-Physician Communication Discrepancies. JAMA Internal Medicine. 2010;170(15):1302–7. [DOI] [PubMed] [Google Scholar]
- 10.Okunrintemi V, Spatz Erica S, Di Capua P, Salami Joseph A, Valero-Elizondo J, Warraich H, et al. Patient–Provider Communication and Health Outcomes Among Individuals With Atherosclerotic Cardiovascular Disease in the United States. Circulation: Cardiovascular Quality and Outcomes. 2017;10(4):e003635 10.1161/CIRCOUTCOMES.117.003635 [DOI] [PubMed] [Google Scholar]
- 11.Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Education and Counseling. 2009;74(3):295–301. 10.1016/j.pec.2008.11.015 [DOI] [PubMed] [Google Scholar]
- 12.Links AR, Callon W, Wasserman C, Walsh J, Beach MC, Boss EF. Surgeon use of medical jargon with parents in the outpatient setting. Patient Education and Counseling. 2019;102(6):1111–8. 10.1016/j.pec.2019.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayes E, Dua R, Yeung E, Fan K. Patient understanding of commonly used oral medicine terminology. Bdj. 2017;223:842 10.1038/sj.bdj.2017.991 [DOI] [PubMed] [Google Scholar]
- 14.Chou L, Ellis L, Papandony M, Seneviwickrama KLMD, Cicuttini FM, Sullivan K, et al. Patients’ perceived needs of osteoarthritis health information: A systematic scoping review. PLoS ONE. 2018;13(4):e0195489 10.1371/journal.pone.0195489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richard C, Glaser E, Lussier M-T. Communication and patient participation influencing patient recall of treatment discussions. Health Expectations. 2017;20(4):760–70. 10.1111/hex.12515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessels RPC. Patients' memory for medical information. J R Soc Med. 2003;96(5):219–22. 10.1258/jrsm.96.5.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Australian Commission on Safety and Quality in Health Care. Health literacy: Taking action to improve safety and quality. Sydney, ACSQHC; 2014.
- 18.Ha Dinh TT, Bonner A, Clark R, Ramsbotham J, Hines S. The effectiveness of the teach‐back method on adherence and self‐management in health education for people with chronic disease: a systematic review. JBI Database of Systematic Reviews and Implementation Reports. 2016;14(1):210–47. 10.11124/jbisrir-2016-2296 [DOI] [PubMed] [Google Scholar]
- 19.Dantic DE. A critical review of the effectiveness of ‘teach-back’ technique in teaching COPD patients self-management using respiratory inhalers. Health Education Journal. 2013. [Google Scholar]
- 20.Negarandeh R, Mahmoodi H, Noktehdan H, Heshmat R, Shakibazadeh E. Teach back and pictorial image educational strategies on knowledge about diabetes and medication/dietary adherence among low health literate patients with type 2 diabetes. Prim Care Diabetes.7(2):111–8. 10.1016/j.pcd.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 21.Davis KK, Mintzer M, Himmelfarb CRD, Hayat MJ, Rotman S, Allen J. Targeted intervention improves knowledge but not self-care or readmissions in heart failure patients with mild cognitive impairment. European Journal of Heart Failure. 2012;14(9):1041–9. 10.1093/eurjhf/hfs096 [DOI] [PubMed] [Google Scholar]
- 22.DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, et al. A heart failure self-management program for patients of all literacy levels: A randomized, controlled trial [ISRCTN11535170]. BMC Health Services Research. 2006;6:30-. 10.1186/1472-6963-6-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krumholz HM, Amatruda J, Smith GL, Mattera JA, Roumanis SA, Radford MJ, et al. Randomized trial of an education and support intervention to preventreadmission of patients with heart failure. Journal of the American College of Cardiology. 2002;39(1):83–9. 10.1016/s0735-1097(01)01699-0 [DOI] [PubMed] [Google Scholar]
- 24.White M, Garbez R, Carroll M, Brinker E, Howie-Esquivel J. Is “Teach-Back” Associated With Knowledge Retention and Hospital Readmission in Hospitalized Heart Failure Patients? Journal of Cardiovascular Nursing. 2013;28(2):137–46. 10.1097/JCN.0b013e31824987bd [DOI] [PubMed] [Google Scholar]
- 25.Peter D, Robinson P, Jordan M, Lawrence S, Casey K, Salas-Lopez D. Reducing readmissions using teach-back. Journal of Nursing Administration. 2015;45(1):35–52. 10.1097/NNA.0000000000000155 [DOI] [PubMed] [Google Scholar]
- 26.Rasmusson K, Flattery M, Baas LS. American Association of Heart Failure Nurses Position Paper on Educating Patients with Heart Failure. Heart & Lung: The Journal of Acute and Critical Care. 2015;44(2):173–7. [DOI] [PubMed] [Google Scholar]
- 27.Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Hess Fischl A, et al. Diabetes Self-management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care. 2015;38(7):1372–82. 10.2337/dc15-0730 [DOI] [PubMed] [Google Scholar]
- 28.Jenkins V, Solis-Trapala I, Langridge C, Catt S, Talbot DC, Fallowfield LJ. What Oncologists Believe They Said and What Patients Believe They Heard: An Analysis of Phase I Trial Discussions. Journal of Clinical Oncology. 2011;29(1):61–8. 10.1200/JCO.2010.30.0814 [DOI] [PubMed] [Google Scholar]
- 29.Brooks C, Ballinger C, Nutbeam D, Mander C, Adams J. Nursing and allied health professionals' views about using health literacy screening tools and a universal precautions approach to communication with older adults: a qualitative study. Disability And Rehabilitation. 2019:1–7. [DOI] [PubMed] [Google Scholar]
- 30.Klingbeil C, Gibson C. The Teach Back Project: A System-wide Evidence Based Practice Implementation. J Pediatr Nurs. 2018;42:81–5. 10.1016/j.pedn.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 31.Morony S, Weir K, Duncan G, Biggs J, Nutbeam D, McCaffery KJ. Enhancing communication skills for telehealth: development and implementation of a Teach-Back intervention for a national maternal and child health helpline in Australia. BMC Health Services Research. 2018;18(1):162 10.1186/s12913-018-2956-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sax Insitute, NSW Ministry of Health. (2013). Translational Research Framework: Testing innovation in policy, programs and service delivery. Retrieved from https://www.saxinstitute.org.au/wp-content/uploads/Translational-Research-Framework.pdf
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petticrew M. When are complex interventions ‘complex’? When are simple interventions ‘simple’?: Oxford University Press; 2011. [DOI] [PubMed] [Google Scholar]
- 35.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1(3):176–84. 10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- 36.Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10 10.1186/s13012-014-0196-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10 10.1186/s13012-014-0196-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmadidarrehsima S, Rahnama M, Afshari M, Asadi Bidmeshki E. Effectiveness of Teach-Back Self-Management Training Program on Happiness of Breast Cancer Patients. Asian Pac J Cancer Prev. 2016;17(10):4555–61. 10.22034/APJCP.2016.17.10.4555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahrens SL, Wirges AM. Using Evidence to Improve Satisfaction With Medication Side-Effects Education on a Neuro-Medical Surgical Unit. J Neurosci Nurs. 2013;45(5):281–7. 10.1097/JNN.0b013e31829d8ca5 [DOI] [PubMed] [Google Scholar]
- 40.Badaczewski A, Bauman LJ, Blank AE, Dreyer B, Abrams MA, Stein REK, et al. Relationship between Teach-back and patient-centered communication in primary care pediatric encounters. Patient Educ Couns. 2017;100(7):1345–52. 10.1016/j.pec.2017.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bahri N, Saljooghi S, Noghabi AD, Moshki M. Effectiveness of the teach-back method in improving self-care activities in postmenopausal women. Prz. 2018;17(1):5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.George NE, Sunny S, Sam AM, Sabu AS, Rodrigues PA. Effect of medication related educational interventions on improving medication adherence in patients with type 2 diabetes mellitus. Asian Journal of Pharmaceutical and Clinical Research. 2018;11(1):167–70. [Google Scholar]
- 43.Ghiasvand F, Riazi H, Hajian S, Kazemi E, Firoozi A. The effect of a self-care program based on the teach back method on the postpartum quality of life. Electron Physician. 2017;9(4):4180–9. 10.19082/4180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Griffey RT, Shin N, Jones S, Aginam N, Gross M, Kinsella Y, et al. The impact of teach-back on comprehension of discharge instructions and satisfaction among emergency patients with limited health literacy: A randomized, controlled study. J Commun Healthc. 2015;8(1):10–21. 10.1179/1753807615Y.0000000001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haney M, Shepherd J. Can teach-back reduce hospital readmissions? American Nurse Today. 2014;9(3):50–2. [Google Scholar]
- 46.Kandula NR, Malli T, Zei CP, Larsen E, Baker DW. Literacy and Retention of Information After a Multimedia Diabetes Education Program and Teach-Back. J Health Commun. 2011;16:89–102. 10.1080/10810730.2011.604382 [DOI] [PubMed] [Google Scholar]
- 47.Kiser K, Jonas D, Warner Z, Scanlon K, Shilliday BB, DeWalt DA. A randomized controlled trial of a literacy-sensitive self-management intervention for chronic obstructive pulmonary disease patients. J Gen Intern Med. 2012;27(2):190–5. 10.1007/s11606-011-1867-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu YB, Li YF, Liu L, Chen YL. Effectiveness of the teach-back method for improving the health literacy of senior citizens in nursing homes. Jpn J Nurs Sci. 2018;15(3):195–202. 10.1111/jjns.12192 [DOI] [PubMed] [Google Scholar]
- 49.Mahmoudirad G, Hoseini MS, Madarshahian F. The effect of teach-back education on foot self-care among npatients with type ii diabetes mellitus. 2015. [Google Scholar]
- 50.Moadab NH, Elahi N, Moradbeygi K, Mahboubi M, Latifi SM, Elhami S. The comparison between effectiveness of teach-back method and accompany person on anxiety in women undergo cesarean section. Research Journal of Medical Sciences. 2015;9(3):43–8. [Google Scholar]
- 51.Mollazadeh F, Maslakpak MH. The Effect of Teach-Back Training on Self Management in Kidney Transplant Recipients: A Clinical Trial. International Journal of Community Based Nursing & Midwifery. 2018;6(2):146–55. [PMC free article] [PubMed] [Google Scholar]
- 52.Morony S, Weir KR, Bell KJL, Biggs J, Duncan G, Nutbeam D, et al. A stepped wedge cluster randomised trial of nurse-delivered Teach-Back in a consumer telehealth service. PLoS ONE. 2018;13(10):e0206473 10.1371/journal.pone.0206473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Negarandeh R, Mahmoodi H, Noktehdan H, Heshmat R, Shakibazadeh E. Teach back and pictorial image educational strategies on knowledge about diabetes and medication/dietary adherence among low health literate patients with type 2 diabetes. Prim Care Diabetes. 2013;7(2):111–8. 10.1016/j.pcd.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 54.Peter D, Robinson P, Jordan M, Lawrence S, Casey K, Salas-Lopez D. Reducing Readmissions Using Teach-Back. Journal of Nursing Administration. 2015;45(1):35–42. 10.1097/NNA.0000000000000155 [DOI] [PubMed] [Google Scholar]
- 55.Press VG, Arora VM, Shah LM, Lewis SL, Ivy K, Charbeneau J, et al. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. J Gen Intern Med. 2011;26(6):635–42. 10.1007/s11606-010-1624-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Slater BA, Huang Y, Dalawari P. The Impact of Teach-Back Method on Retention of Key Domains of Emergency Department Discharge Instructions. J Emerg Med. 2017;53(5):e59–e65. 10.1016/j.jemermed.2017.06.032 [DOI] [PubMed] [Google Scholar]
- 57.Waszak DL, Mitchell AM, Ren D, Fennimore LA. A Quality Improvement Project to Improve Education Provided by Nurses to ED Patients Prescribed Opioid Analgesics at Discharge. J Emerg Nurs. 2018;44(4):336–44. 10.1016/j.jen.2017.09.010 [DOI] [PubMed] [Google Scholar]
- 58.Talevski J, Sanders KM, Duque G, Connaughton C, Beauchamp A, Green D, et al. Effect of Clinical Care Pathways on Quality of Life and Physical Function After Fragility Fracture: A Meta-analysis. J Am Med Dir Assoc. 2019;20(7):926 e1- e11. [DOI] [PubMed] [Google Scholar]
- 59.Engel KG, Heisler M, Smith DM, Robinson CH, Forman JH, Ubel PA. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53(4):454–61 e15. 10.1016/j.annemergmed.2008.05.016 [DOI] [PubMed] [Google Scholar]
- 60.Vashi A, Rhodes KV. "Sign right here and you're good to go": a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57(4):315–22 e1. [DOI] [PubMed] [Google Scholar]
- 61.King A, Hoppe RB. "Best practice" for patient-centered communication: a narrative review. J Grad Med Educ. 2013;5(3):385–93. 10.4300/JGME-D-13-00072.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sullivan G, Blevins D, Kauth MR. Translating clinical training into practice in complex mental health systems: Toward opening the 'Black Box' of implementation. Implement Sci. 2008;3 10.1186/1748-5908-3-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ayton DR, Barker AL, Morello RT, Brand CA, Talevski J, Landgren FS, et al. Barriers and enablers to the implementation of the 6-PACK falls prevention program: A pre-implementation study in hospitals participating in a cluster randomised controlled trial. PLoS ONE. 2017;12(2):e0171932 10.1371/journal.pone.0171932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Breitenstein SM, Gross D, Garvey CA, Hill C, Fogg L, Resnick B. Implementation fidelity in community-based interventions. Res Nurs Health. 2010;33(2):164–73. 10.1002/nur.20373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587–92. 10.1016/j.ijnurstu.2012.09.010 [DOI] [PubMed] [Google Scholar]
- 66.Boyde M, Turner C, Thompson DR, Stewart S. Educational interventions for patients with heart failure: a systematic review of randomized controlled trials. J Cardiovasc Nurs. 2011;26(4):E27–35. 10.1097/JCN.0b013e3181ee5fb2 [DOI] [PubMed] [Google Scholar]
- 67.Gorina M, Limonero JT, Alvarez M. Effectiveness of primary healthcare educational interventions undertaken by nurses to improve chronic disease management in patients with diabetes mellitus, hypertension and hypercholesterolemia: A systematic review. Int J Nurs Stud. 2018;86:139–50. 10.1016/j.ijnurstu.2018.06.016 [DOI] [PubMed] [Google Scholar]
- 68.Hersh L, Salzman B, Snyderman D. Health Literacy in Primary Care Practice. Am Fam Physician. 2015;92(2):118–24. [PubMed] [Google Scholar]
- 69.McCarthy DM, Waite KR, Curtis LM, Engel KG, Baker DW, Wolf MS. What did the doctor say? Health literacy and recall of medical instructions. Med Care. 2012;50(4):277–82. 10.1097/MLR.0b013e318241e8e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ramsey I, Corsini N, Peters MDJ, Eckert M. A rapid review of consumer health information needs and preferences. Patient Education and Counseling. 2017;100(9):1634–42. 10.1016/j.pec.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 71.Australian Commission on Safety and Quality in Health Care. Australian Charter of Healthcare Rights. 2008. Available at: https://www.safetyandquality.gov.au/national-priorities/charter-of-healthcare-rights/. Accessed May 2019.
- 72.Wolf MS, Linsk NL, Mitchell CG, Schechtman B. HIV prevention in practice: an assessment of the public health response of physicians and nurses in the Midwest. J Community Health. 2004;29(1):63–73. 10.1023/b:johe.0000007445.73199.7b [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.