Executive summary
Over the past four decades, rapid urbanisation in China has brought unprecedented health benefits to its urban population, but has also created new challenges for protection of and promotion of health in cities. With the shift from rural to urban living, more people than ever enjoy the health advantages that cities can provide, such as better access to health services and improved sanitation. For example, the average life expectancy of male urban residents in 2010 was estimated to be 7·09 years longer than that of of their counterparts in rural China; urban females lived 6·64 years longer.1 Other changes associated with rapid urbanisation–including large-scale migration, ageing, pollution, shifts in diet and lifestyle, and social inequality–have created new health challenges.2 For example, about 52% of people over 60 years old lived in urban areas in 2015 compared with 34% in 2000,3 thus increasing the burden of senior care in Chinese cities. Non-communicable diseases have replaced infectious diseases as the leading cause of death among urban residents; the percentage of years of life lost because of such diseases as a fraction of all-cause years of life lost increased from 50·0% (95% CI 48·5–53·0) in 1990 to 77·3% (76·5–78·1) in 2015.4 Health inequality also increased in urban areas.5
China has acted to address urban health challenges by passing strict environmental regulations and investing heavily in urban infrastructure. Major reforms have been passed to increase the transparency of environmental governance to control pollution over the short term, while moving to reform whole industries and thus provide long-term solutions. Programmes like the Hygienic Cities movement have invested heavily in urban infrastructure to promote health, including major improvements in urban sanitation.6 China has also increased coverage of and accessibility to health services in urban areas. In 2016, around 93·8% of the urban population was covered by urban medical insurance programmes, a substantial increase from 4·1% in 1998 when the programmes started.7, 8
Meanwhile, cities in China are also testing new strategies for urban health management, such as China's pilot Healthy Cities project.9 Management of chronic diseases and mental disorders in cities has improved dramatically and major progress has been made regarding access to preventive and primary health services. All these efforts have contributed to the reduction of exposure to health risks and health improvement in urban China. However, despite these successes, major gaps remain, including but not limited to an over-reliance on a top-down-approach to environmental management, a narrow focus on health care in urban health management, and a scarcity of intersectoral action.
Given that the urbanisation rate in China is predicted to reach 71% by 2030,10 urban health challenges will continue to emerge and expand. If innovative strategies are not used to address these issues, they will become major obstacles to the achievement of improved health and development for millions of people. It has also become clear that the health sector alone, with its traditional piecemeal approach, cannot effectively resolve the modern challenges to urban health in China. The country is now in a transitional period in which the pursuit of economic growth at any cost is being replaced by sustainable development. In 2013, President Xi Jinping declared China's intention to develop a so-called ecological civilisation (ecocivilisation), the core principles of which involve balancing the relationship between humanity and nature. During this transition, health is recognised as the centrepiece of sustainable development in China, as highlighted in the Healthy China 2030 plan that was adopted in 2016.11 As a result, people-centred and health-oriented urban development will hopefully prevail in China; however, major efforts, political will, and investments will be needed to put this vision into practice.
The Tsinghua–Lancet Commission on Healthy Cities in China aimed to characterise, understand, and address urban health challenges in the unique context of China's rapid and dynamic urban development. Experts from a wide range of disciplines examined environmental and social determinants of health, identified key stakeholders, and assessed actions for the prevention, management, and control of adverse health outcomes associated with the country's urban experience. We conclude that key efforts are needed to combat urban health challenges in China and these should be unified with the Healthy Cities movement, which uses a systems approach to urban health management and provides a clear path to the realisation of the Healthy China 2030 plan.
Actions taken to build healthy cities in China have contributed to global knowledge on the development of healthy cities in other parts of the world. China's strategic, simultaneous rollout of diverse trials in different cities—in areas such as health education and promotion—and its rapid adoption of effective approaches at the national scale is a valuable lesson for other countries facing rapid urbanisation. Despite such successes, we believe that there is room for substantial improvement and make the following five key recommendations.
Integrate health into all policies
China should take advantage of new, human-centred urbanisation strategies. For example, cities should integrate health into urban planning and design as a first step towards the integration of health into all policies.
Increase participation
Cities should increase participation by residents, the private sector, non-governmental organisations (NGOs), and community groups in health management. This increase can be achieved through investment in community capacity building and engagement with the private sector.
Promote intersectoral action
To motivate and sustain intersectoral action in the design, building, and management of healthy cities, cities should develop ways to assess the health effects of urban management by use of measures that span multiple and diverse sectors.
Set local goals for 2030 and assess progress periodically
Cities should view the health goals specified in the Healthy China 2030 plan as long-term goals that are achieved through the building of healthy cities. Indicator systems should be put in place to assess progress and inform the public.
Enhance research and education on healthy cities
To develop new theories and practical solutions, cities should increase investment and form partnerships with universities, research institutes, and the private sector to support research and education on the best ways to create healthy cities.
Introduction
Health, defined as “a state of wellbeing emergent from conductive interactions between individual's potentials, life's demands, and social and environmental determinants,”12 is a fundamental right of every human being.13 Good health and wellbeing has been adopted as a key Sustainable Development Goal by the international community,14 and although recognition of the importance of health is universal, it is particularly important in China because the quest for health is deeply embedded in Chinese culture.
The earliest recorded discussion on healthy living is attributed to Zhuangzi (around 369–286 BCE), who stated that to stay healthy one should “conform to nature”. In other words, health is the result of a lifestyle in which human beings and nature are in harmony.15 This philosophy underpins the basic principles of traditional Chinese medicine, which takes a systems view of health. In traditional chinese medicine, human health is seen as the consequence of harmonisation between human beings and their environments and between the various parts of the human body and the focus is on disease prevention rather than treatment.16 Concepts from traditional Chinese medicine, such as the maintenance of regular daily activities (rest, diet, and exercise) and avoidance of negative health effects from environmental factors (eg, Fengshui) have become essential parts of Chinese culture. These concepts have much in common with the guidelines for healthy lifestyles promoted by WHO.17
Health is increasingly at the centre of China's approach to sustainable development. Policy makers in China have started to acknowledge that health is not only a fundamental right but is also the cornerstone for economic growth and development. Economic growth is not always accompanied by prosperity and can create serious challenges and threats to the health and welfare of populations;18 therefore, overlooking the importance of health during development will yield heavy future costs. For example, the environmental pollution associated with rapid economic growth has already taken a massive economic toll in China. In 2007 alone, particulate matter with a diameter of less than 2·5 μm (PM2·5) affected the productivity of about 72 million workers in 30 Chinese provinces, causing an estimated economic loss of ¥346·3 billion (US$44·4 billion, about 1·1% of the national gross domestic product [GDP]).19 Total economic losses attributed to the public health effects of pollution from particulate matter with a diameter of less than 10 μm (PM10) and sulphur dioxide (SO2) pollution in 74 cities were estimated to be as high as ¥439·8 billion ($70·9 billion, about 2·3% of these cities' GDP) in the first half of 2015.20
China will also have a massive future burden of non-communicable diseases—most of which will affect urban areas—that will strain future health systems and limit economic growth in the country. Total annual premature deaths from such diseases are expected to increase from 3·11 million in 2013 to 3·52 million in 2030.21 Between 2012 and 2030, economic losses attributable to five key non-communicable diseases–ischaemic heart disease, cerebrovascular disease, diabetes, breast cancer, and chronic obstructive pulmonary disease–will total $23·03 trillion USD,22 which is more than twice of China's total GDP in 2015 ($11·07 trillion). If urgent actions are not taken, this epidemic will affect China's capacity to achieve its other goals for sustainable development.
At the same time, a better educated Chinese urban population has become more health conscious over the past few decades and has become increasingly concerned about environmental pollution and health care. The China Urban Life Quality Indicator Survey, which has been done annually among residents of 38 cities since 2000, found that environmental issues were one of the top six issues of concern between 2000 and 2006; health care was among the top six issues for 11 consecutive years.23 Concerns about environmental pollution and associated health risks over the past decade mirrored increases in severe PM2·5 pollution. A survey of perceived health risks from air pollution in Shanghai, Wuhan, and Nanchang found that more than 57% of respondents were not satisfied with current air quality; 46% of participants expressed anxiety about exposure to polluted air.24 Through social media, urban citizens in China are increasingly speaking out on issues that they believe are affecting their health and wellbeing. Environmental petitions and complaints have increased by more than 20% annually in recent years and mass protests for environmental issues are occurring across China.25 These new trends show a willingness on the part of the Chinese people to break away from the norm of focusing on economic growth and avoid politics. In response to these challenges, the central government has proposed the formation of a so-called ecologically civilised society that actively and structurally addresses these concerns. Local leaders in China are increasingly under pressure from the central government and the public to shift from growth-centred development to sustainable development policies that protect environmental quality and health.26
The Healthy China 2030 plan released by the State Council of China in 2016 acknowledges the confluence of health challenges, trends, and the public's health concerns. The plan lays the foundations for health policy in China over the next 15 years and is a dramatic departure from traditional strategies (panel 1 ). In the past, health was just one of various goals for societal advancement and the central focus of health management was on the improvement of the health-care system.27 By contrast, the new plan presents health as the foundation for all socioeconomic development, calls for the integration of health into all policies, and emphasises the importance of addressing the environmental and social determinants of health.
Panel 1. Healthy China 2030.
The Healthy China 2030 plan was released by the State Council of China on Oct 25, 2016. It specifies that health management in China will focus on the promotion of healthy lifestyles, optimisation of health services, improvements in health care coverage, provision and protection of a healthy environment, and development of service industries in health care.
Health will be highly prioritised in the development of public policy and incorporated into all stages of policy making. All actions will be guided by four principles: health first, reform and innovation, science-guided development, and equity.
Health inequality between urban and rural areas and among different regions and population segments will be addressed through equal access to basic health services. Ultimately, the goal is to achieve health for all citizens. To achieve this aim, all citizens will need access to services and health issues at different stages of the life course will need to be addressed. The plan also identifies specific goals, such as to increase the average life expectancy of Chinese people to 79 years by 2030 (appendix). Action items for each focus area, such as to improve health literacy and to strength health education, are also included.
The successful implementation of this plan will be determined by various political and socioeconomic factors. Given their large and increasing share of population and dominance in the political and economic systems, cities are key to the realisation of a healthy China. Healthy cities will be crucial to the achievement of the ambitious goals of the plan, as directly acknowledged in the document: “Building healthy cities, towns and villages is the key to a healthy China”.11 And yet, because the plan is intended only to provide broad guidelines, these now need be translated to detailed strategies and specific actions to yield the desired results.
In this Commission, we examine the challenges and opportunities cities face in building a healthy China and make specific policy recommendations. In section 1, we detail why cities are the key to a healthy China. In section 2, we examine major health challenges and modifiable risk factors in urban China. In section 3, we analyse current practices for dealing with health challenges in urban China, with a particular focus on the health outcomes arising from these practices and on remaining gaps. In section 4, we discuss principles and specific actions that cities in China can adopt to address these gaps. China is not the only country facing substantial urban health challenges—many cities in developing countries and emerging economies, particularly rapidly developing ones, have similar problems. Lessons learned from China could, therefore, benefit cities in other parts of the world.
Section 1. Cities are key to health management in China
Since the launch of economic reform in 1978, rapid urbanisation has changed China from an agrarian society into an urbanised society. Because of their dominant role in Chinese society and the large urban population, cities hold the key to health management in China.
Urbanisation in China: current status and projections
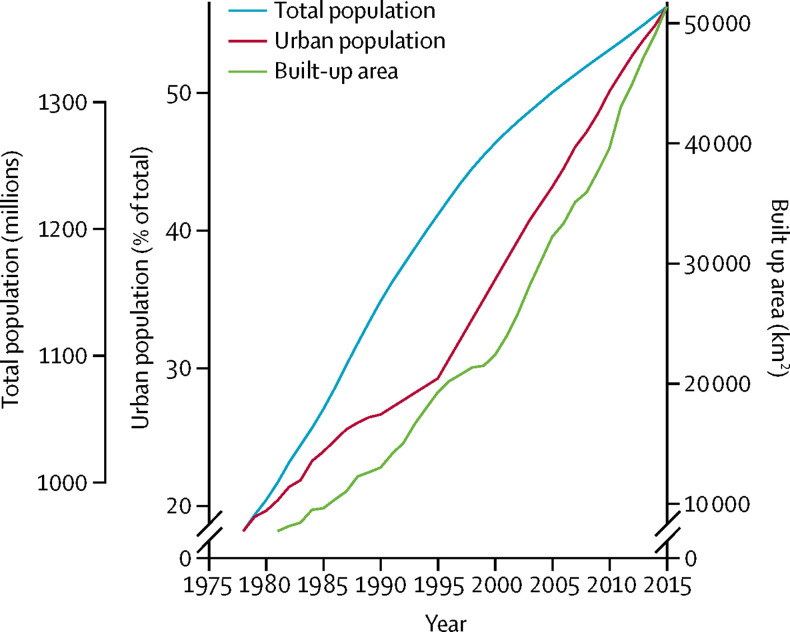
When China began major economic reforms under the leadership of Deng Xiaoping in 1978, the country was primarily an agrarian society, with the largest rural population in the world (about 790 million). China has since had the largest rural-to-urban migration in human history, with the rate of urbanisation increasing from 17·9% to 56·1%, and the urban population from 170 million to 771 million, between 1978 and 2015 (figure 1 ).29 China's urbanisation rate is estimated to increase to 60% by 2020, with an additional 100 million people moving from rural to urban areas by that time.30 In the long term, China's urban population is expected to keep increasing as a result of pro-urbanisation development policies and the replacement of the so-called one-child policy with a universal two-child policy in 2016. The total urban population is likely to reach 1070 million by 2030.10
Figure 1.
Total population, urban population, and total built-up area, 1978–2015
Source: National Bureau of Statistics of China.28
Notably, rates of population increase have been unequal across Chinese cities. Megacities such as Beijing, Shanghai, Guangzhou, and Shenzhen have the fastest rates of growth, while cities in northeast China show a net loss of population (appendix). These regional disparities in population growth will probably continue. Population density is predicted to peak in Beijing (at 25% higher than 2010 densities) and Shanghai (at 36% higher than 2010 densities) around 2030.31
In line with this population growth, the number of cities in China has increased from 193 in 1978 to 656 in 2015. Panel 2 shows how cities are defined in China. Simultaneously, the total built-up area in China increased from less than 10 000 km2 in 1978 to about 52 100 km2 in 2015 (figure 1), reflecting the vast scope of the construction of new cities and the expansion of existing ones.35 The fastest rates of urbanisation have been in eastern China, where the built-up area in 9 cities increased by more than 20-times between 1990 and 2010.36
Panel 2. Definitions of major geographic terms used in this study.
-
•
City can be translated as Shi (市) or Cheng Shi (城市) in Chinese and they refer to different geographic units.
-
•
Shi (市) refers to an administrative division and in China there are four types: municipalities directly under the central government (Zhi Xia Shi [直辖市]), of which there are four (Beijing, Shanghai, Tianjin, and Chongqing); vice-provincial city (Fu Sheng Ji Shi [副省级市]), of which there are 15; prefecture-level city (Di Ji Shi [地级市]), of which there are 276; and county-level city (Xian Ji Shi [县级市]), of which there are 361. Each Shi (市) is responsible for urban and rural areas in its boundary.32
-
•
Cheng Shi (城市) refers to an urban area, including urban districts and townships. Urban districts are continuous built-up areas in city districts, seats of districts, or cities that do not have city districts. Townships are continuous built-up areas in county seats and towns. In urban districts and townships, residential committees are the basic administrative unit of governance.33
-
•
The urban population is the number of people who live in urban areas.
-
•
Urban agglomeration is a spatially compact, economically highly integrated cluster of cities. Such clusters centre on a mega city, with three or more metropolitan areas or large cities forming the core region. The core region is connected to peripherals with highly developed networks for transportation and other infrastructure, within the reach of a daily commute. China has proposed the development of five national-level urban agglomerations, nine regional-level urban agglomerations, and six subregional-level urban agglomerations.34
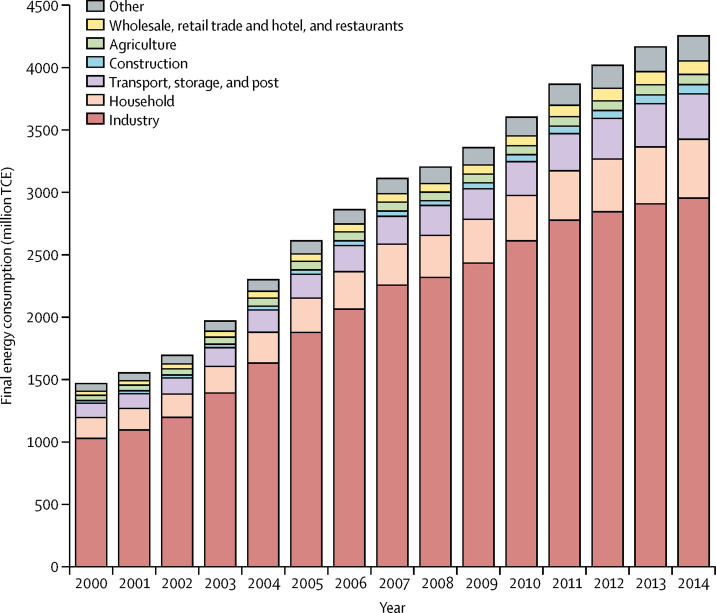
Urbanisation in China has been driven mainly by industrialisation, which led to a long period of thriving economic development. Between 1990 and 2014, the industrial sector has been responsible for an increase of at least 40% in GDP37—more than any other sector in China—making it the most important sector for driving economic development and urbanisation in this period. Migrants from rural areas provide the labour force that is required for rapid industrialisation and urbanisation in China. In fact, it is the migration of 226 million rural residents to urban centrer between 2001 and 2010 that has dominated the increase in the country's urban population over the past 40 years of rapid urbanisation.38 According to the latest survey by the National Bureau of Statistics,39 which examined 445 Chinese cities, there were 137·4 million migrant workers and 39·1 million family members of migrant workers living in urban areas at the end of 2015. Most migrants (61·3%) lived in east China, with the remaining migrants split among central (16·4%), western (19·5%), and northeastern (2·8%) China. About 59·9% of rural migrants lived in cities with more than 1 million residents.39 Migrant workers are expected to continue to contribute to the growth of the urban labour force through to 2030, with an estimated 6 million new migrant workers leaving rural areas for cities each year between 2013 and 2030.40 Although cities, especially large cities, are projected to continue to attract migrants, provinces in central China are likely to keep supplying migrants to more developed regions.31
China's urban population is rapidly ageing while it grows. The Fourth National Survey on Urban and Rural Elderly in China showed that by 2015 about 52% of people older than 60 years were living in urban areas, compared with 34% in 2000.3 Developed cities tend to experience ageing populations earlier than less developed cities. For example, Shanghai first surpassed the threshold where 10% of its population was older than 60 years in 1982 (when the national figure was just 5%);41 whereas Beijing did not reach this threshold until 2000. Within megacities, the ageing population also showed a tendency towards suburbanisation, with seniors moving from the centre of the city to its edge and from outer suburbs to the urban fringe.42
The rapid ageing of the urban population in China is the result of improved socioeconomic conditions in combination with unique and intensive government interventions in population planning, namely the late, long, and few and one-child policies, which led to a 70% decrease in fertility rate in less than 20 years. The former policy was introduced in the early 1970s and promoted delayed marriages, long intervals between childbirths, and fewer children. The one-child policy was launched in 1979–80 and restricted most urban couples to one child each.43 Improved socioeconomic conditions in urban areas contributed to longer life expectancy. The average life expectancy of male urban residents in 2010 was estimated to be 7·09 years longer than that of their rural counterparts, with female urban residents living 6·64 years longer.1
Even with the shift in January, 2016 away from the one-child policy to a universal two-child policy, ageing of the Chinese population is projected to continue. It is estimated that the percentage of people aged 65 years or older will increase to 18–20% of the total population by 2030.10, 44 The pace of population ageing in China has been even faster than that in most developed countries.45 Projected fertility rates and expected population age structures show that, in the decades to come, most older people in China will live in urban areas. By 2030, around 207 million people aged 65 years or older are projected to live in urban areas, compared with 52 million in 2010; 93 million people will live in rural areas by 2030, compared with 67 million in 2010.10 The ageing urban population poses a serious challenge to the management of urban health in China.
Cities hold the key to a healthy China
Two defining factors underscore the role of cities in the creation of a healthy China. First, the health of 771 million urban residents is, naturally, a major element in the achievement of national health goals. Second, cities are best positioned to implement comprehensive health management in China.
Cities play a dominant role in Chinese society, not only because most of the population are urban dwellers but also because cities have substantial political and economic power. For example, in 2013, five national-level urban agglomerations (Beijing–Tianjin–Hebei, Yangtze River Delta, Pearl River Delta, Yangtze River Mid-reach, and Chengdu–Chongqing) accounted for just 9·1% of total land area in China but contributed half of GDP and had 65% of total foreign direct investment.46 Meanwhile, the income gap between urban and rural dwellers is widening. The ratio of per capita disposable income in urban areas to that in rural areas has increased from about 2·57 in 1978 to 2·73 in 2015.28 Given the increase in urban population over the same period, this has led to a growing share of national household wealth in urban areas.
Since 1978, when the central government devolved political and economic power to cities following economic reforms, cities in China have had broad administrative resources that allow them to form local development strategies, set local taxation rates, and control the use of urban land.47 This decentralisation of power gives cities autonomy in the promotion of economic development but also enables them to delay or block the implementation of central governance reforms that are deemed incompatible with local development goals.48 Although regional governance arrangements, such as the development of urban agglomerations, have re-emerged in response to pressure from provincial governments and the central government, these efforts have primarily aimed to enhance coordination among cities in development and are unlikely to change the dominant role of cities in local governance.49
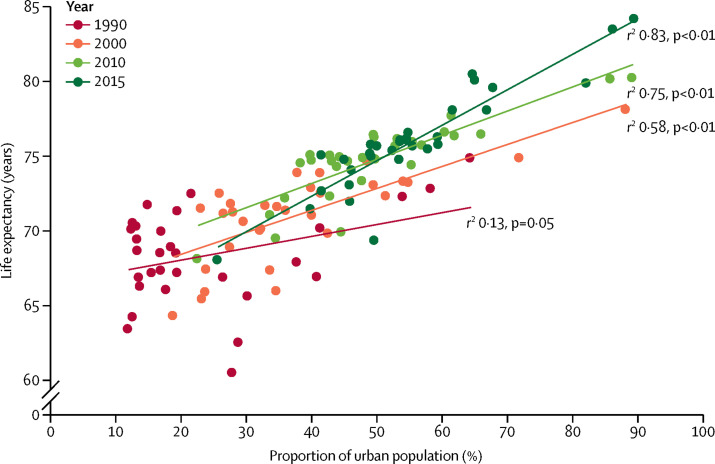
In parallel with their increasing social influence and political and economic power, cities in China have been going through a transformation of living standards, with major consequences for population health and wellbeing. Cities can offer considerable advantages over rural areas in terms of the provision of clean water, rapid transit, sanitation, education, health care, and other public services.50 For example, in 2015, the number of medical practitioners (including assistant medical practitioners), per 1000 residents in urban areas was 3·72 compared with 1·55 in rural areas, nurses 4·58 versus 1·39, and hospital beds 8·27 versus 3·71.51 According to multiple measures, cities in China benefit from improved health care and social development; most notably, substantially increased life expectancy. In 2010, life expectancy for urban male residents was 74–81 years across China's provinces compared with 67–74 years for rural male residents. Similarly, urban female residents had a life expectancy of 77–84 years compared with 69–78 years for rural female residents.1 Data from the past three national censuses (1990, 2000, and 2010) and a 1% sample census in 2015 show that the positive correlation between average life expectancy and the proportion of urban population at the provincial level became stronger as the latter increased (figure 2 ).
Figure 2.
Life expectancy and proportion of urban population in each province, 1990, 2000, 2010, and 2015
However, the health and social advantages enjoyed by the urban population in China are challenged by the various consequences of China's rapid urban development, including a massive and ageing urban population, environmental pollution, large-scale internal migration, lifestyle changes, and rising social inequality.52, 53 Health-care systems in urban China are particularly strained by growing urban populations,54, 55 rapidly increasing prevalence of non-communicable diseases,4 and rising health inequalities (with respect to disease burdens and life expectancy).5, 56 These trends represent cracks in the foundation of health and wellbeing in Chinese cities that need urgently to be addressed.
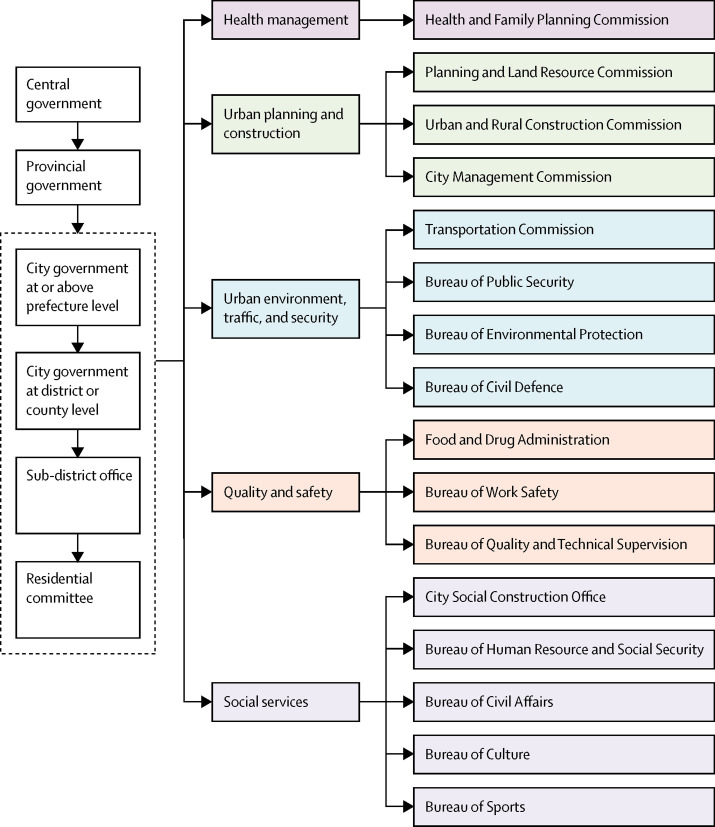
To deal with these challenges, policies and actions that tackle social and environmental determinants of health will be required. Under China's unique governance structure (figure 3 ), cities are the most suitable entities to implement the new comprehensive health policies specified in the Healthy China 2030 plan. Although, in the past, health management policy focused on health care (making it largely the business of the health sector), cities in China are uniquely equipped to drive health care forward because future strategies will require a focus on a much broader set of social and environmental determinants, which are clearly beyond the scope of what the health sector can accomplish alone. In urban China, health departments sit at the same level in the governance structure as other municipal departments. Because departments compete for authority and resources to meet their individual goals, it is difficult to establish effective interdepartmental collaborations across sectors.57 Thus, city-level governments uniquely possess the required political power, economic and human resources, and institutional structures to implement the new health policies. Cities already allocate the largest portion of public health investment; for example, the split of public expenditures on health in 2011 was 10:20:70 for national, provincial, and city (including prefecture-level and county-level expenditures) levels.58 These resources will be key to the achievement of future gains in health in China, particularly because many health issues, such as those associated with infectious diseases, can only be tackled through coordinated actions across the urban–rural spectrum.59 Cities are often better positioned to start and lead such efforts because China's governance system has historically used cities to control the countryside.60
Figure 3.
Governance structure relevant to urban health management
Municipal governments at or above the prefecture and district or county levels consist of bureaus that are responsible for different aspects of city life. Sub-district offices are branches of district or county governments. Residential committees are self-governance organisations that allow for some sovereign decision making on community issues. All levels work together in a linked governance network.
Section 2. Major challenges to urban health in China
Cities in China are facing many health challenges caused by the fast-paced changes in lifestyle and environments associated with urbanisation. In particular, non-communicable diseases, emerging infectious diseases, injuries, mental disorders, and the need to provide care for a rapidly ageing urban population are eroding the urban health advantage to city residents. At the same time, cities need to keep control of rising healthy expenditure and reduce health inequity.
Non-communicable diseases
Status
In China, non-communicable diseases have replaced communicable diseases as the primary contributor to overall disease burden. Cardiovascular diseases, cancer, and respiratory diseases were among the leading causes of early death in 2015.4 Non-communicable diseases are becoming more prevalent because rapid ageing of the population increases the pool of susceptible older adults, treatment advances prolong life, and lifestyle and environmental changes increase risks.
Cardiovascular diseases
Stroke has been consistently ranked as the top cause of death in China in three Global Burden of Disease studies4, 61, 62 since 2010. Other cardiovascular diseases, such as ischaemic heart disease, are also among the top ten causes of death, and mortality caused by coronary heart disease is rising. In 2013, the mortality rate for cardiovascular diseases among urban residents in China reached 259 per 100 000 people, accounting for 41·9% of all-cause deaths, which was a 69% increase in mortality from 2003 (174 per 100 000 people).63
Cancer
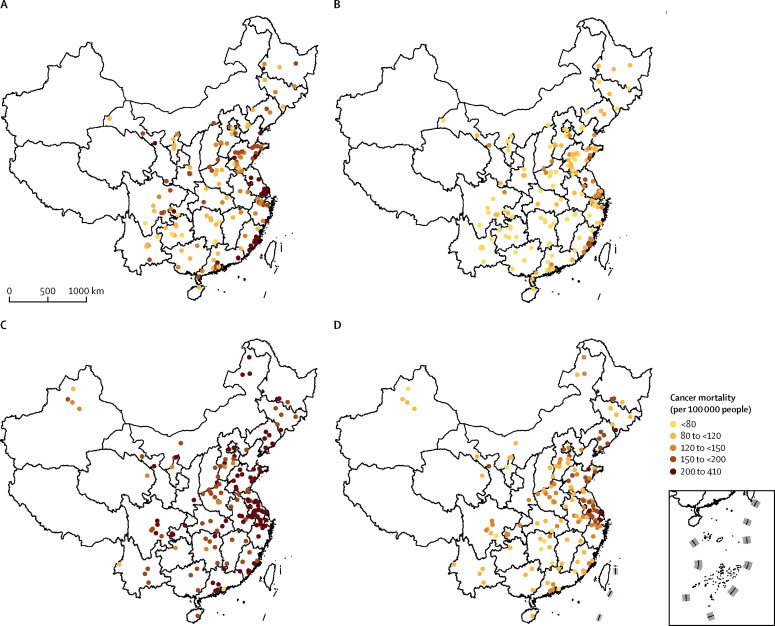
Cancer is a major public health problem and has been the leading collective cause of death in China since 2010.64 Cancer incidence and cancer-related mortality in urban China have both changed in recent decades (figure 4 ). At the national level, the number of cancer-related deaths in 22 cancer registries increased substantially from 51 090 in 2000 to 88 800 in 2011 (a 78% increase).64 The estimated age-standardised incidence rate in urban areas increased from 135 per 100 000 people in 1989 to 149 per 100 000 people in 2008, with the greatest increase seen between 2000 and 2008.65 The rise in overall cancer incidence is significant in the more industrially developed east China and larger cities, especially for lung, colorectal, and breast cancer.66 There were mixed trends in cancer-related mortality: although mortality caused by cancers of the stomach, oesophagus, nasopharynx, and cervix uteri decreased, lung and breast cancer mortality increased between 1987 and 2009.67 In urban China, the 2015 age-standardised estimate for all-cancer incidence was 192 per 100 000 people and for all-cancer mortality was 110 per 100 000 people.64
Figure 4.
Total cancer mortality, 1990–1992 and 2013
1990–92: (A) men and (B) women. 2013: (C) men and (D) women. The inset shows the islands of the South China Sea. Source: National Cancer Center of China.
Respiratory diseases
It was estimated that the prevalence rate among adults (>18 years) in urban China in 2013 was 3·32% (95% CI 3·17–3·47) for chronic obstructive pulmonary disease, 2·01% (1·90–2·13) for asthma, and 0·61% (0·55–0·68) for asthma–chronic obstructive pulmonary disease overlap syndrome.68 Children bear a substantial burden of respiratory disease. Prevalence of asthma among children younger than 14 years increased from 1·6% in 2000 to 2·1% in 2010 in 33 cities, with children aged 3–6 years having the highest prevalence in both years and onset before 6 years old seen in nearly 80% of cases. This increase in prevalence was mainly observed in megacities, provincial capitals, and eastern coastal cities.69 Children are at risk from not only ambient air pollution but also indoor air pollution. A 2008–09 survey70 of 31 049 children aged 2–14 years in seven cities in northeastern China showed that recent home renovation and polyvinyl chloride flooring projects contributed significantly to respiratory symptoms and asthma.
Diabetes
In 1994, China conducted a national survey on diabetes in 19 provinces and municipalities according to the WHO standard; the results showed that diabetes prevalence among urban adults (25–64 years old) was 2·9%.71 The 2010 study72 of non-communicable disease surveillance in China found the age-standardised prevalence of diabetes for urban residents older than 18 years to be 14·3%. In 2013, this value decreased slightly to 12%.73 However, 47% of the urban adult population was estimated to have either diabetes or prediabetes, which is only slightly lower than the estimate (49–52%) for the US population.74 The speed at which urban populations in China are catching up with their counterparts in developed countries with respect to such health risks is alarming.
Risk factors
The rising incidence of non-communicable diseases and mortality related to these diseases in urban China has been attributed to demographic, environmental, and lifestyle changes caused by economic growth and rapid urbanisation, including ageing population, environmental pollution, low levels of physical activity, unbalanced diets, smoking, and alcohol consumption.63, 66, 75
Air pollution
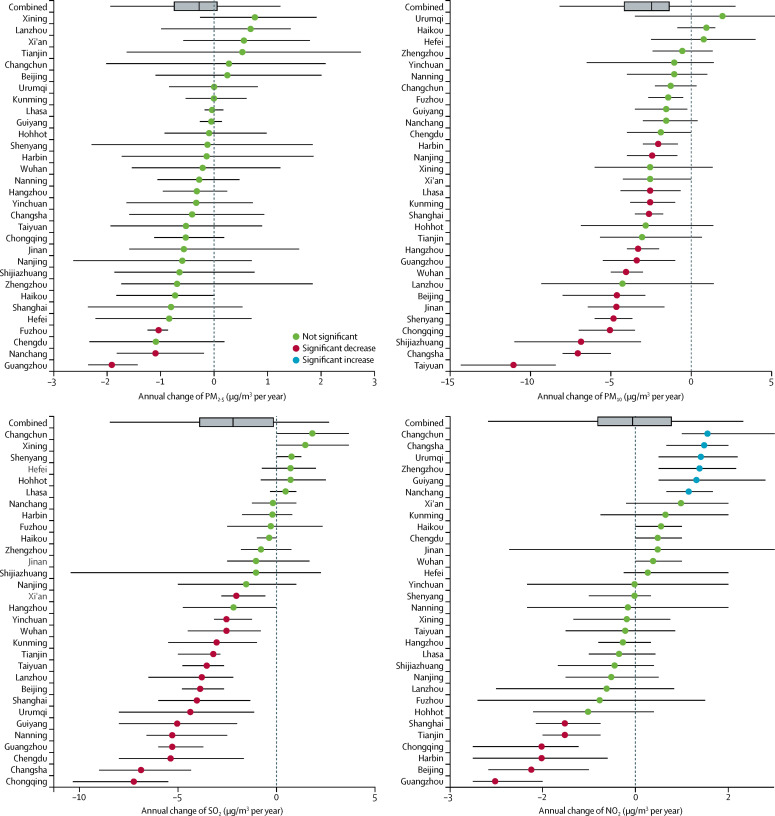
Air pollution is the most challenging environmental issue faced by cities in China. According to the 2016 Report on the State of Environment in China,76 only 84 (25%) of 338 cities reached the target enforcement levels in 2016. Over the past decade, concentrations of PM10, SO2, nitrogen dioxide (NO2), and PM2·5 have started to decrease, although ozone (O3) concentrations continue to rise. These trends reflect China's commendable efforts to mitigate SO2, nitrogen oxides (NOx), and primary fine particle emissions. Efforts to control volatile organic compounds emissions have been somewhat successful,77, 78, 79, 80 as shown in figure 5 .
Figure 5.
Annual concentrations of major pollutants in 31 major cities, 2003–12
Theil-Sen estimator and corresponding 95% CIs are represented by dots and lines. Source: data for PM2·5 were obtained from satellite-derived products and other data were from China Statistical Yearbook of Environment 2003–12.81 PM2·5=particulate matter with a diameter of less than 2·5 μm. PM10=particulate matter with a diameter of less than 10 μm.
Urbanisation is undeniably linked to the increase in air pollution in China. PM2·5 concentrations in urban environments are highly correlated with urban population, with larger cities generally having worse PM2·5 pollution than do smaller cities.82 The dramatic increase in the use of coal for power generation and industrial and domestic heating is one of the key causes of this pollution.83 In 1970, China produced less than 10% of the world's coal, but that figure increased to nearly 50% by 2012.84 Coal combustion generates substantial pollution, contributing 90% of SO2 emissions, 70% of dust, and 67% of NOx emissions in China.85 Coal consumption in China will gradually decrease in the coming decades because of the slowing economy and the adoption of clean technologies. The International Energy Agency predicted that coal demand in China will decrease by 15% for 2016–40 but that the share of coal in the power mix will still be about 45% in 2040.86 Rapid urbanisation is also linked to the drastic increase in the ownership of private vehicles and a surge in the use of diesel trucks.87 Nationwide in 2006, vehicles are estimated to account for 24% of national NOx emissions, 29% of non-methane volatile organic compounds, and 20% of carbon monoxide (CO) emissions, with even higher fractions in urban areas.88
It is often overlooked that most of urban dwellers' exposure to ambient pollution occurs indoors.89 Because people spend most of their time indoors, indoor air pollutants can cause substantial damage to health.90 Volatile compounds, including 1,3-butadiene, formaldehyde, 1,4-dichlorobenzene, and benzene, are indoor air pollutants that are significantly associated with increased cancer risk among Chinese urban working men (2·93 [95% CI 1·65–4·71] additional cases per 10 000 people exposed) and women (2·27 [1·27–3·65] additional cases per 10 000 people exposed); 70% of the increase in risk is due to exposure at home.91 These compounds are released from building materials and decorative products, including plastic furniture and home decorations, polymeric floor and wall coverings, synthetic wood products, and synthetic cleaning agents.90, 92 Indoor heating and cooking with coals and biomass are also important sources of particulate matter and CO in some urban residences in regions that need heating in winter and in less economically developed regions.93
Throughout cities in China, lung cancer has increased with worsening air quality. According to the National Central Cancer Registry, 348 107 (57·5%) of 605 946 new lung cancer diagnoses in 2010 were in people who came from urban areas. The age-standardised incidence rate in urban areas (36·4 per 100 000 people) is also higher than it is in rural areas (33·3 per 100 000 people).94
Air pollution directly affects cardiovascular diseases. A nationwide time-series analysis done in 272 cities between 2013 and 2015 showed that each 10 μg/m−3 increase in daily concentrations of PM2·5 was associated with increments of 0·27% in mortality from cardiovascular diseases, 0·30% from coronary heart diseases, and 0·23% from stroke.95
Worsening air quality also contributes to increasing mortality from respiratory disease. It has been estimated that an increase of 10 000 tonnes of industrial SO2 would increase mortality from respiratory diseases by 0·03 per 10 000 people in 116 prefectural-level cities, with spatial spillover effects leading to an increase in mortality of 1·54 per 10 000 people in neighbouring cities. For soot emissions, the same increase would increase mortality from respiratory diseases by 0·07 per 10 000 people, with spatial spillover effects also leading to an increase of 4·12 per 10 000 people in neighbouring cities.96
The overall toll of air pollution on the health of urban residents of China is substantial. According to the latest estimate by WHO,75 ambient air pollution in cities led to an age-standardised death rate of 70 per 100 000 people in 2012, which is much higher than the worldwide average of 47 per 100 000 people. The loss of disability-adjusted life-years was estimated to be 1546 per 100 000 people.
Water pollution
Surface water and groundwater in urban China are often polluted. In 2016, a water quality survey of 6124 monitoring wells installed in 225 prefecture-level cities found that 45·4% of wells were poor quality and 14·7% were very poor quality, according to Ministry of Environmental Protection standards.76 Major pollutants of urban water supplies include nitrates, heavy metals, petroleum hydrocarbons, pesticides, and organic chemicals. The increase in water pollutants in urban China is mostly driven by industrial sources, thus are a result of economic growth.97 These increases are accompanied by emerging problems with organic contamination of urban water supplies; for example, with hormones, antibiotics, surfactants, endocrine disruptors, human and veterinary pharmaceuticals, X-ray contrast media, and human metabolites.98
With respect to provision of safe drinking water for the urban population, China's issues are compounded: water shortages are widespread and water pollution worsens these shortages. Two-thirds of cities face water shortages,99 mainly because of low water availability per person and spatiotemporal mismatches of supply and demand. Annual water availability per person in China is only 34% of the world average.100 To manage the shortage of available water supplies, some cities limit water consumption on certain days or times, with adverse consequences for industrial output and domestic life. Cities sometimes switch to lower quality supplies to meet excess demand, with dire consequences for public health. The 2005 national survey of safety of potable water sources showed that 638 cities and towns were using sources that did not meet the drinking water standards, directly affecting 56·95 million people.101 Although this situation has improved, 86 (10%) of 897 water quality monitoring sites of potable water sources in prefecture-level cities and above still failed to meet national standards in 2016.76 Key contaminants of urban drinking water supplies that have been detected at concentrations that are harmful to health include nitrates, arsenic contents, and disinfection byproducts.102, 103 These contaminants are associated with increased risk of cancer and skin and kidney disease.104
Low levels of physical activity
In China, as in cities around the world, urban residents are increasingly sedentary. A study105 on children and youth aged 9–17 years in 11 cities showed that only 22·6% of boys and 11·3% of girls met the physical activity recommendations of at least 60 min per day of moderate-to-vigorous physical activity. Similar trends have been seen among adults in China's cities. Work and domestic physical activity levels of adults fell by nearly half over 20 years (1991–2011) and were negatively associated with living in more urbanised areas.106 Alarmingly, in urban adults participation in moderate or vigorous physical activity outside of work was as low as 7·9% in the International Collaborative Study of Cardiovascular Disease in Asia107 done between 2000 and 2001.
Surveys of urban residents confirm that associations between walkable features of the built environment and walking—as established through research in other countries–are also true for China.108 The proximity of non-residential locations, parks, non-park physical activity facilities, and pedestrian infrastructure are positively associated with physical activity, while density of development has negative effects. These negative effects might be explained by the scarcity of recreational space in high-density developments and a perception of overcrowding.109 Rapid urban expansion and an increase in car dependency have exacerbated urban and environmental challenges to health that mirror those in western cities (eg, substantial deviations from traditional high-density, pedestrian-oriented and cyclist-oriented urban areas), including issues like longer commutes, traffic congestion, and air pollution.110, 111 By contrast to the low-density suburbs that are common in some western countries (eg, USA), emerging suburbs in China's large cities are characterised by high-density development, with housing in the suburban peripheries and much longer commute times between home and work, which remains mostly in urban centres.110
Physical activity is also negatively associated with car ownership and screen time (ie, time spent watching television or using a computer), but is positively associated with bicycle ownership and blue-collar jobs.107 As suburban expansion continues to retreat from urban centres, suburban residents have long commutes and few public transport options. This trend, combined with the rising disposable income of urban residents, has resulted in an exponential increase of cars in cities; the number of cars owned by urban residents increased from 0·17 million in 1984 to 88·4 million by 2012.112 By 2035, total number of vehicles in China is predicted to reach 565 million, of which 345 million (61%) will be privately-owned cars in urban areas.113 Screen time is especially important in mediating physical activities among youth, particularly as high screen time is also associated with depression, anxiety, and lower satisfaction with school life in urban areas.114
Unbalanced diets
People in cities have higher food consumption per person and different diets than those in rural areas. Between 1980 and 2010, urban dwellers derived 46·7% of food energy from meats, vegetables, and fruits, whereas the rural population obtained most of their food energy from cereals (71·0%). This disparity is because urban residents have more disposable income and a greater array of food choices.115 The urban population also consumes more processed food than the rural population; the China Health and Nutrition Survey116 showed that residents in three megacities (Beijing, Shanghai, and Chongqing) got 21·8% of their energy from processed foods in 2011, compared with only 10·2% in rural residents in nine provinces.
Tobacco and harmful use of alcohol
Urban residents are more exposed to advertising of tobacco than their rural counterparts are.117 In 2015, the prevalence of current tobacco smoking in urban residents older than 15 years was 26·1% (95% CI 23·3–29·1), including a staggering 49% (45·0–53·0) of men and 2·7% (1·8–3·9) of women. These values did not significantly differ from those in 2010, when the population-standardised prevalence of current tobacco smoking was 47·5% for urban men and 2·5% for urban women.117 The prevalence of current smoking in rural men decreased from 56·9% in 2010 to 55·4% in 2015, while the rate for rural women increased slightly from 2·5% in 2010 to 2·8% in 2015.
Urban residents in China also maintain high levels of alcohol consumption. The 2010 China Chronic Disease and Risk Factor Surveillance study118 measured the current drinking rate—defined as having consumed alcohol in the 12 months before the survey—of urban residents over 18 years at 39·8%, which was higher than that of rural residents (34·9%). Although the current drinking rate was higher in urban residents than in rural residents, the harmful drinking rate (ie, >61 g pure alcohol per drinking day for men and >41 g for women) was higher in rural residents than in urban residents. In 2010, harmful drinking rate was 7·5% among current drinkers in urban areas, compared with 10·2% in rural drinkers. The 2013 update of the survey73 found that the current drinking rate in urban areas was 39·1% (35·4% in rural areas) and the harmful drinking rate in urban areas was 7·3% (10·3% in rural areas). Drinking is more acceptable than smoking in Chinese culture. For example, a study in northern China showed that 41·4% of urban residents and 32·1% of rural residents believe that alcoholism requires no treatment.119 The sale and consumption of alcohol are only weakly regulated by the government.120
Extreme weather events
Urban living is linked to climate-related health risks, such as urban heat island effects. A study121 in Hong Kong found that for each 1°C the daily high temperature increased over 29°C, all-cause mortality rose by 4·1% (95% CI 0·7 to 7·6%) in areas with strong urban heat island effects, but only 0·7% (95% CI −2·4 to 3·9%) in areas where such effects were absent. China is projected to become warmer in the 21st century, with the number of days during which air temperature exceeds 35°C in southern China increasing by 30 by 2050 under a moderate growth scenario (ie, representative concentration pathways 4·5).122 The associated increase in extreme heat events could have important public health consequences in cities, especially for vulnerable populations, such as children and elderly people. Under the representative concentration pathways 4·5 scenario with medium population growth, heat-related deaths among people older than 65 years in Beijing would increase by 13·1 times compared with expectations under the baseline 1980s climate. Even with adaptation measures in place, the increase is expected to be significant.123 Future climate change is also anticipated to increase risks of other diseases, such as infectious diseases, mental illness, respiratory diseases, and injuries. In China, the interaction between climate and risk factors can be acute because of its large population and the predicted pace of climate change.124
Metabolic risk factors
Metabolic disorders are major risk factors for cardiovascular disease in China and are epidemic in the urban Chinese population. A survey125 of 33 urban communities in northeast China (2009–10) reported an overall prevalence of metabolic disorders of 27·4%. Male adults with higher education level and higher family income had a higher prevalence of metabolic disorders than their counterparts with lower education and family income. Higher levels of physical activity were associated with decreased prevalence of metabolic syndrome among men. The situation in children and adolescents is even more worrisome. Between 1991 and 2011, the prevalence of overweight and obesity in children (aged 6–17 years) more than doubled from 15·7% to 32·7%; in the same period, obesity more than tripled from 3·6% to 13·7%.126 This rising trend is more substantial in economically developed regions. Between 1980 and 2010, the prevalence of overweight and obesity increased from 3·8% to 32·6% for male students (aged 7–18 years) and from 3% to 19·1% for female students in large coastal cities. Even in the least developed cities, overweight and obesity increased from 0·7% to 17·6% for male students and 1·2% to 9·4% for female students.127
High incidence of metabolic disorders also leads to other non-cardiovascular diseases. For example, fatty liver disease, which is estimated to affect 27% of the urban population, is related to obesity and metabolic disorders.128 Obesity also interacts with other risk factors. For example, a study129 done in seven northeastern cities of China found that obesity increased children's susceptibility to the adverse health effects of ambient air pollution by amplifying the association between long-term air pollution exposure and blood pressure.
Infectious diseases
Status
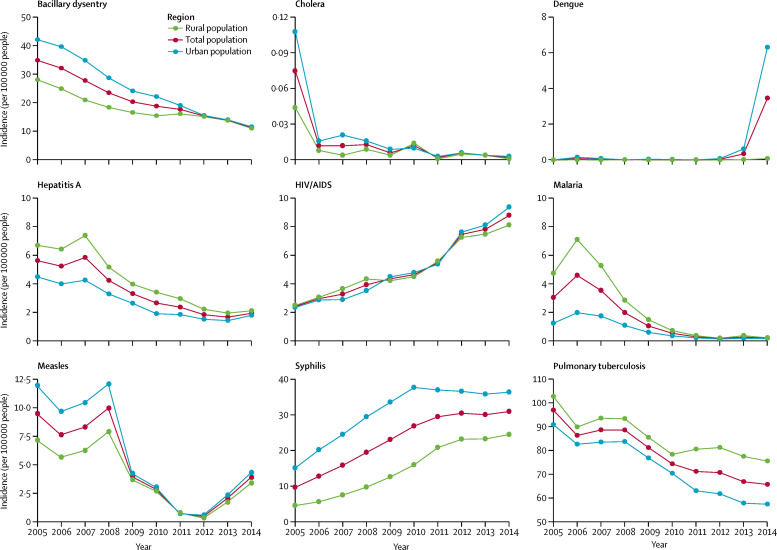
Urbanisation has altered patterns of infectious disease occurrence in China (figure 6 ). The incidence of diseases caused by environmental pathogens or carried by environmental vectors is decreasing in urban areas, mostly because of improved living environments, investments in infrastructure, advances in treatment and prevention technologies, and a strong political commitment to infectious disease control.130 At the same time, the large population, extensive transportation networks within and between cities, and large-scale rural–urban migration maintain a high risk of emerging infectious diseases from both domestic and international origins.131 The trend of mortality from infectious disease between 1990 and 2010 reflect the contrasting effects of these factors. Between 1990 and 2000, relative risk of mortality from infectious disease in urban residents (5–89 years old) decreased by 44%; however, the rate in 2010 was almost the same as in 2000 and there was even a slight increase of 14% between 2000 and 2005.132
Figure 6.
National reported incidence (per 100 000 people) of nine infectious diseases in rural and urban areas in China, 2005–14
Source: China Center for Disease Control and Prevention.
Risk factors
The expansion of modern urban transportation systems can contribute to changes in the speed and scale of the spread of infectious diseases. In particular, increasing contact rates among people in crowded urban areas, who are then connected to distant populations through transportation networks, make pandemic control difficult as conventional spatial barriers to transmission break down. The booming aviation industry and growth of international trade and tourism further increase the risk of imported infectious diseases.133 For example, a flight from Hong Kong to Beijing on March 15, 2003, is widely regarded as responsible for the long-distance transmission of severe acute respiratory syndrome,134 and national highways further promoted the spread of the disease to places adjacent to Beijing, such as Shanxi, Hebei and Inner Mongolia.135 Another example is the 2009 outbreak of influenza A H1N1 (swine flu) in China, which was originally caused by cases imported through international air travel from Mexico;136 the subsequent domestic spread of the epidemic is thought to have been mostly through domestic flights and ground transportation (railways and highways). A 50% reduction in trans-city and local travel would have resulted in an estimated 50·2% reduction of total cases.137 International travellers also increase the risk of vector-borne diseases faced by China, as was the case for the unprecedented 2014 outbreak of dengue in Guangzhou, which accounted for 52% of all cases in China for 1990–2015.138
Increasing volumes of rural-urban migration might also exacerbate the threat of infectious diseases in urban areas. Many migrants live in urban villages, construction sites, dilapidated private housing, illegal basements, and former underground air-raid bunkers.139 Crowding and unhealthy living conditions in these environments can expose this group to a higher risk of diseases (such as tuberculosis) than that of the general urban population.59 Crowded living conditions and other socioeconomic constraints can also make it difficult for migrants to relocate with their spouses. The prevalence of multiple sexual partners and commercial sex among rural migrants are significantly higher than among non-migrants.140 Migrants also tend to be less knowledgeable about prevention strategies for sexually transmitted diseases, thus increasing their vulnerability.141
Since the early 2000s, urbanisation in China has been associated with rising HIV transmission in conjunction with a major expansion of the commercial sex industry and high mobility of female sex workers.142 By 2014, there were 500 000 reported cases of people living with HIV/AIDS and 160 000 reported deaths. Some social groups are particularly vulnerable; HIV/AIDS among men who have sex with men is a growing concern, with HIV prevalence at 7·7% in 2014. The increasing number of illicit drug users in urban China has also increased transmission risks. Among injection drug users in 2014, the HIV rate was estimated at 6·0%.143 Since China embraced globalisation and open markets, the use of illicit drugs has become increasingly prevalent in cities. In 1991, the number of registered illicit drug users of all types in China was 148 000, but this figure increased to 2·5 million by 2016.144, 145 Although official statistics do not distinguish between urban and rural areas, it can be reasonably assumed that the former bear the bulk of the burden.
Injuries and injury-related deaths
Status
Injuries, including road injuries and self-harm, were among the top ten causes of death in China in 2015.4 In urban areas, traffic-related deaths were the leading cause of injury-related death, followed by falls and suicides.111, 146 The standardised death rate caused by road injuries during 2004–05 was nearly double the 1992 figure. A reduction in injury rates to those of countries with low injury-related mortality would recover 65% of the life expectancy lost because of injury in urban China, amounting to a saving of 436·4 million years of life based on 2005 population counts.147 The high incidence of injuries in cities has caused substantial economic losses. For example, the costs of health care, social security and welfare resulting from pedestrian-related injuries alone in Shanghai were about 13·5% of its GDP in 2006.148
The burden of injury-associated mortality mostly falls on senior citizens, children, women, and migrants. In Shanghai, 56·8% of all pedestrian-related deaths for 2001–10 were in people aged 65 or older, with the mortality rate estimated to be 13·61 per 100 000 people.148 Injury was the leading cause of death of children aged 1–4 years (43·0% of all deaths) and 5–14 years (50·1% of all deaths) in urban China.149 Furthermore, in both urban and rural areas, the probability of being injured is higher for children from poor families than for those from wealthy families.150 Urban women have lower injury-related mortality than do urban men; the number of injury-related deaths reported for urban women was 2912–4081 per year for 2004–10, compared with 5733–7734 per year for urban men.146 Violent injuries to women in urban areas is an increasing and alarming issue, with prevalence reaching 10·7% (95% CI 7·8–15·5) in 21 cities in 2011. A high male-to-female ratio, population growth rate, and unemployment rate were associated with increased risk of injuries caused by physical attacks against women in cities. This situation is an issue of public health and human rights.151
Urban migrants experience a higher burden of morbidity and mortality from occupational injury than do non-migrants. For example, 85% of deaths in the construction industry were among migrant workers in 2004.152 Children in migrant households had higher incidence of injury than did children in resident households. In Guangzhou for 2008–12, the adjusted incidence rate of injury-related death of children in migrant households was 3·5 times higher than that in resident households.153
Risk factors
Injuries and injury-related mortalities in urban China are rising because of increasing exposure to risk factors, which include the expanding urban population, rising motorisation rate, intensive construction, and urban development. For example, the high pedestrian-related death rates among elderly people are partly due to the ageing urban population and increasing car ownership rate in cities.148 Large-scale rural-to-urban migration by migrants and their concentration in high-risk occupations contribute to the high prevalence of occupational injuries among migrants.152
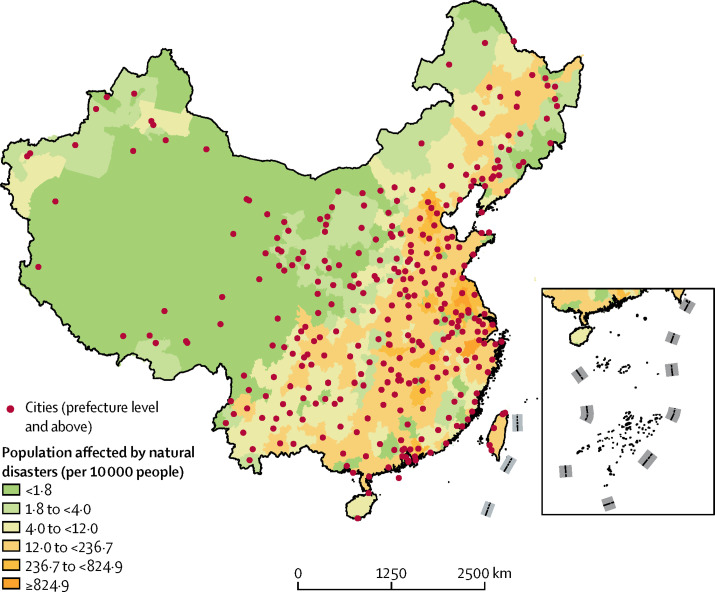
Besides these factors, natural hazards are a growing risk factor for injuries and injury-related death in Chinese cities. Although rapid urbanisation and economic growth have enabled cities to mobilise more resources to prepare for and respond to such disasters, vulnerability to natural disasters will probably continue to rise in cities with rapid population growth as a result of poor implementation of urban planning, construction of low-quality infrastructure and housing, strained social services, and segmented disaster management systems.154, 155 Large and growing populations live in disaster-prone regions because of a legacy of restricted regional planning (figure 7 ). More than half of the cities in China with a population of more than 500 000 people are located in areas with substantial seismic risk;157 dozens of large cities are located in areas where risk of land subsidence is high or in mountainous zones with high risk of landslides.154 This situation has occasionally led to major loss of life and property; for example, the 2010 landslide in Zhouqu, Gansu province killed nearly 1500 people.158
Figure 7.
Cities considered at risk of natural disasters
Natural disasters include storm surges, landslides, cold waves, heatwaves, floods, and earthquakes. The inset shows the islands of the South China Sea. Source: World Atlas of Natural Disaster Risk.156
Poor implementation of urban design can contribute to increased vulnerability. For example, urban flood damage is becoming more common; between 2008 and 2010, nearly two-thirds of surveyed Chinese cities (n=351) reported severe flooding and more than a third had more than three major floods.159 Major contributing factors included the rapid expansion of impervious surfaces over natural land, modification of river channels, and difficulty in the development of flood protection infrastructure because of existing underground structures and high-density built-up environments.160 By 2050, the frequency of heavy rainstorms in China might increase by as much as 33%, further increasing flooding risk.122 China's coastal cities are especially vulnerable to sea level rises, land subsidence, and extreme weather. It is projected that these forces will lead to the breaching of nearly half of the seawalls and embankments in Shanghai by 2100, meaning nearly half of the city's land area will be at risk of serious flooding.161
Mental disorders
Status
Urban residents in China are more depressed than ever before. The prevalence of major depressive disorders in urban adults was 1·7% for 2001–10.162 Based on the 2012 China National Health and Wellness Survey, the prevalence of mental health disorders was 6% in urban areas.163 Highly populated cities along the eastern coast (such as Shenyang and Shanghai) and cities in west China that have high population densities had poorer depression scale scores than did other cities.164 The prevalence of mental health problems is high among migrant workers. For example, a survey165 in Shenzhen estimated that 34·4% of migrant workers had mental health problems. However, only a small portion of people have been diagnosed and treated. For example, only 8·3% of those with a major depressive disorder were diagnosed and of those, just 51·5% were currently being treated.161 Rising medical costs are a further economic burden for patients, with the average annual cost per patient increasing from $1095 in 2005 to $3665 in 2013.166 Major depressive disorders substantially affect individuals and society. People with such disorders reported lower health-related quality of life scores and had lower productivity and resource utilisation.163
Risk factors
The continued socioeconomic transformations of urban communities, rises in income inequality, and fading interpersonal trust are leading risk factors of mental disorders.167 For example, the perception of a connection to one's neighbourhood was shown to have a strong negative association with severity of post-traumatic stress disorder symptoms and risk of depression in young adults (15–19 years old) in Shanghai.168 Among migrant workers, the major risk factors for mental disorders are undesirable working and living conditions.165 Other factors, such as drug use, alcohol abuse, and homelessness, have contributed to the increased prevalence of mental health problems.162
Caring for urban elderly people
Survey data and self-reported health data highlight a decline in the general health of elderly residents in China's cities. Nearly half of elderly people have non-communicable diseases and this trend is predicted to last into 2020.169 Chronic respiratory disease, cerebrovascular disease, and ischaemic heart disease are the three largest contributors to the probability of death for people aged 50–75 years.56 Diseases commonly associated with ageing are also prevalent. For example, according to a national survey done in 2008–09, the prevalence of dementia in individuals aged 65 years or older in urban areas was 4·4% (95% CI 3·9–4·9) compared with 6·2% (5·5–7·0) in rural areas. For Alzheimer's disease, prevalence was 2·4% (2·0–2·8) in urban areas and 4·4% (3·7–5·0) in rural areas. For vascular dementia, prevalence was 1·6% (1·3–1·7) in urban areas and 1·4% (1·0–1·6) in rural areas.170 The self-reported health status of elderly urban residents decreased significantly in China between 2001 and 2013, with mean scores for self-reported physical health declining from 70·86 (SD 28·08) to 61·46 (23·16) and mental health scores declining from 75·63 (25·73) to 64·59 (21·76).171
The increasing health needs of elderly people and dwindling resources are main contributing factors for declining health among elderly urban residents. According to 2010 census data, of people aged 65 years or older in urban areas, roughly 78% were classified as healthy, 18% were unhealthy but able to care for themselves, and 4% required assistance. Nationwide, the demand for health-care services increased by 15·2% in 2015 compared with a decade ago. Health expenditure on elderly people as a percentage of GDP increased from 2·1% in 1993 to 3·4% in 2013.45 Notably, rising health costs have substantially burdened older people. For example, the average monthly pension for 79·74 million retired enterprise workers was ¥2200 ($354) in 2015.172 In comparison, an analysis of national household survey data (2007–11) on medical spending on five major chronic diseases among urban residents, including those aged 65 years or older, found that the annual cost per capita for residents with cardiovascular disease was ¥8954 (about $1356), and ¥8914 (about $1350) for residents with diabetes.173
Elderly people in urban China often rely on their families for financial support and care. Family support accounted for 24% of financial resources for people aged 65 years or older in 2010. However, increased life expectancy, the one-child policy, and changing cultural patterns have led to more elderly people to living alone than ever before. The 2010 census estimated that there were 6·32 million households of people aged 65 years or older who lived alone in urban areas.45 The situation is more severe in large cities. In Beijing, 50% of empty-nest families and 80% of healthy retired urban residents live alone.174 Elderly people who have lost their only child face the greatest challenges in meeting their care needs. As of 2015, an estimated 1·6 million families in China are in this situation, a number that is expected to increase to 4·5 million by 2050.175
The shortage of family care has generated substantial pressure to develop a long-term care system, consisting of institutional and community care facilities in urban China. By the end of 2014, there were 16 549 nursing homes in urban areas, providing 2·65 million beds; 1·28 million people used these facilities. Compared with 1978, the number of nursing homes and people served increased by more than 22 times and the number of beds increased by more than 2654 times.176 Despite substantial progress, the long-term care system in urban China still cannot meet the huge demand. The total number of people who used the system was less than 2% of the urban population aged 65 years or older, implying a huge gap between supply and demand. In addition to this shortage of facilities, affordability, efficacy, and regulatory oversight are major challenges.177
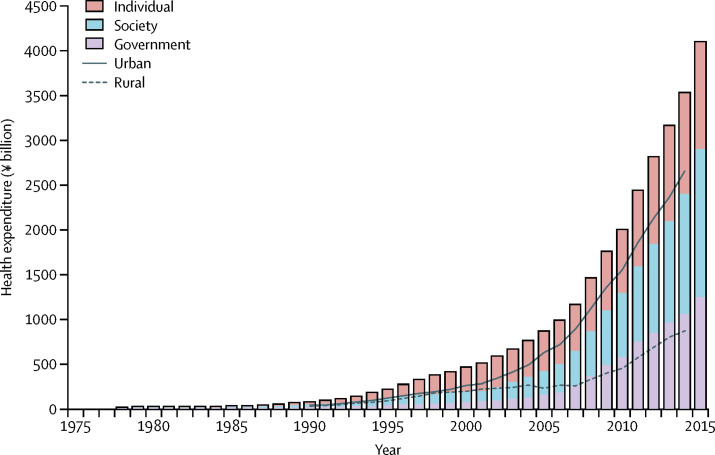
Rising health expenditures
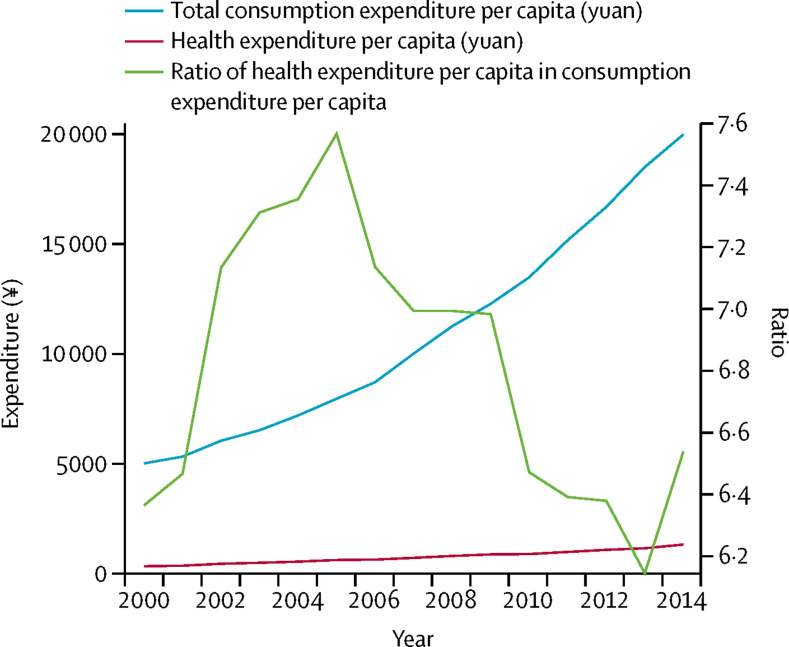
Along with rising industrialisation and urbanisation and an ageing population, Chinese people are facing the dual health threats of infectious and chronic diseases. Meanwhile, the desire for better health services and attention to health have also risen in tandem with higher living standards. The result of which was a sharp rise in health expenditure in China, especially in urban areas (figure 8 ).
Figure 8.
Health expenditure, 1978–2015
Source: National Health and Planning Commission.51 The bars show the expenditure by government, society (mainly from institutions and enterprises), and individuals. The lines show expenditure in urban and rural areas.
According to government statistics, health expenditure in urban areas was ¥2·66 trillion ($4394 billion) in 2014, which was 75% of the national total.51 Health expenditures paid by individuals decreased from 59% in 2000 (the highest since 1978) to 32% in 2014; the government contributed 15·5% in 2000 and 30·0% in 2014, whereas society (mainly from institutions and enterprises) contributed 25·6% in 2000 and 38·1% in 2014.178 This change reflects an improved structure of health financing. However, compared with other major economies in the world, the public share of health expenditure is relatively low. According to the Word Bank, the percentage of general governmental expenditures on health as a fraction of total government expenditures was 10·4% in China in 2014, compared with 19·7% in Germany and 21·3% in the USA.179 Health expenditure per capita and as a share of consumption expenditures are also changing in urban China (figure 9 ). Still, because the share of health expenditure covered by the public health-care system has been steadily increasing, the ratio of personal health expenditure to personal consumption expenditure has not grown between 2000 and 2014.
Figure 9.
Health expenditure per capita and its share in the consumption expenditure in urban China, 2000–14
Sources: China Health Statistical Yearbook 2003–09180 and China Statistical Yearbook of Health and Family Planning 2015.181
Given the need to improve the health conditions of elderly people and the expected response of health spending to rising incomes, the share of health expenditures in GDP is projected to increase substantially over the coming decades in China.182 Per capita medical expenses are forecasted to increase constantly, with an average annual growth rate of 2·2% between 2010 and 2030.183 China's total public health expenditure is expected to reach 6–10% of GDP under different scenarios.182
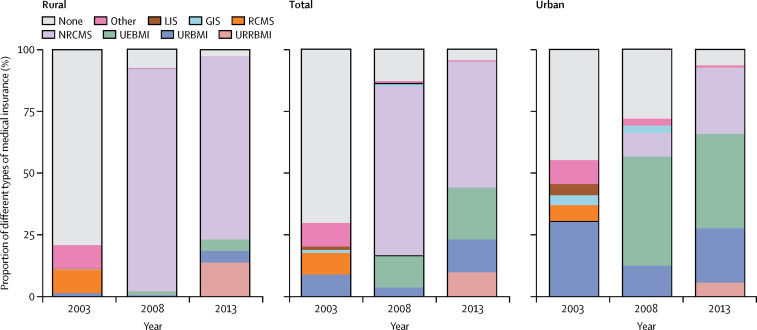
Health inequity
Health equity refers to the attainment of the highest level of health for all people. In the 1970s, China was a model of health equity for the rest of the world for its provision of universal health care. However, the first health reform, which stretched from the mid-1980s to the end of the 1990s, changed China's health-care system permanently. The reform successfully introduced market mechanisms but undermined universal access to health care. In 1981, 70% of the population was covered by three insurance schemes: the Government Insurance Scheme, the Labor Insurance Scheme for urban residents, and the Co-operative Medical System for rural residents. Preventive care was provided by the government at nearly zero cost to recipients. During the reform, many people lost their insurance coverage when state-owned enterprises were shut down and when collective farms were dismantled. Coverage under all insurance schemes dropped to 20% in 1993.184 Because of these and other factors, health inequity across sex, age groups, and geographic locations is increasing in terms of disease burdens and life expectancy. For example, life expectancy for men in Tibet in 1990 was 18·9 years (95% uncertainty interval 16·0–21·8) shorter than their counterparts in Shanghai; life expectancy for women was 21·4 years (18·7–24·3) shorter. Less developed regions also had higher burdens of infectious disease (eg, tuberculosis) than did developed regions.56
Equity in the health-care system deteriorated so rapidly that, in 2000, the WHO considered China one of the least equitable systems in the world; fairness of financial contributions to health care in China were ranked 188th of 191 countries and regions.185 The Chinese Government started the second stage of reform in 1998 but health inequity was not a central focus. Health inequity was still ubiquitous; for example, life expectancy in different regions still varied by as much as 11·8 years (95% uncertainty interval 9·3–14·5) for men and 12·8 years (10·7–15·0) for women in 2013.56 The difference in height between urban boys in east and west China actually increased during 1985–2010, highlighting the disparity in child development in different regions.186 Among Chinese adults, the values of the Apouey index of health inequality increased by 126·8% between 1997 and 2009 in urban areas.5
Professional, income, sex, and age distinctions have an ever-greater role in Chinese society, with social and economic inequalities contributing to increased health inequity. Widened income inequality is one reason why economic growth since the second stage of health reform did not improve health equity in China. The Gini coefficient of family income in urban areas of China was 0·51 in 2012,187 significantly higher than the national value of 0·40 for the USA and the average value of 0·32 for Organization for Economic Co-operation and Development countries in the same year.188 Between 1991 and 2006, income changes in urban areas accounted for 7·1% of rising inequality of urban health.189 In 2013, economic status was estimated to account for 13–14% of health inequality in urban populations.190
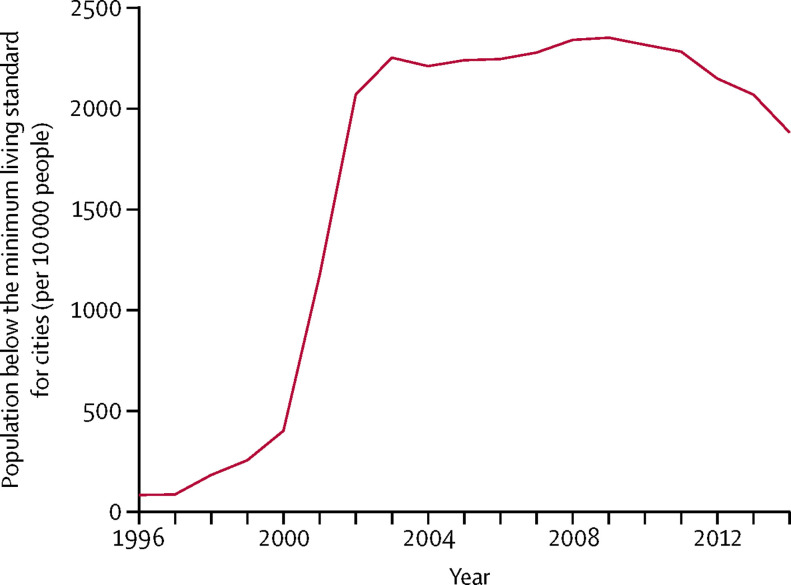
Urban residents can be divided into groups of poor, lower middle, upper middle, and rich based on household income and regional characteristics.191 The minimum living standard for urban residents set by local governments is used as an urban poverty line for the practical purposes of providing social relief or assistance to poor urban households. With the expansion of rural-to-urban migration and the extensive urban economic reforms of the late 1990s, the population of the urban poor substantially increased, only levelling off since 2010 (figure 10 ).
Figure 10.
Population below the minimum living standard for cities, 1996–2014
Source: China Civil Affairs' Statistical Yearbook 2015: Statistics of China Social Services.176
Several paths can lead residents into urban poverty. In addition to the traditional urban poor who have lived on low-income social security welfare, a new class of urban poor includes those who were unable to reap the benefits of rapid urbanisation and economic development. These include the unemployed and those underemployed because they do not have the skills required for emerging jobs or they lack the mobility needed to seek job opportunities.192 Another group consists of those whose rural Hukou (mandatory system of residence registration) changed to urban as a result of government reclassification of their land (ie, from rural to urban). Without the proper skills and necessary social capital to help them to adapt to new urban life, these individuals tend to work in poorly paid, labour-intensive jobs without job security. Despite their access to urban Hukou and qualification for social security welfare, many of them have substandard living conditions. The new urban poor also tend to be spatially segregated and confined to certain old neighbourhoods (eg, urban villages) in cities.193
Access to urban public services is another contributing factor to social segregation and poverty among migrants.194 Although many migrants have established long-term de facto residences in places far from their Hukou registration, because the Hukou system is the basis for access to essential supplies and services, urban immigrants without a local Hukou are often unable to access these resources, including public schools and public health services.195 In Beijing, Shenzhen, Guangzhou and Hangzhou, migrants do not qualify for public housing rentals; even in cities where they do qualify—such as Shanghai and Chongqing—strict rules apply. In Shanghai, about 70% of total housing poverty involves rural migrants.196 Many urban villages are populated with migrant workers. Although these are not officially recognised as slums, they often have inferior environmental and housing conditions than other urban neighbourhoods.193 In addition, the Hukou system also restricts migrant employment opportunities and increases commuter times because affordable local housing is scarce.197 A new policy is expected to relax the Hukou system in medium-sized and small-sized cities but continue to strictly control it in the large cities where most migrants congregate.198
The existence of different types of health insurance in urban China also adds to health inequity. The two major state-run medical insurance programmes—Urban Employee Basic Medical Insurance and Urban Resident Basic Medical Insurance—increase inequalities in outpatient utilisation but reduce pro-rich inequities in inpatient utilisation.199 In addition, subscriptions to less generous programmes, such as the Urban Resident Basic Medical Insurance scheme, are associated with decreased utilisation of general physical examinations.200
Inequity in access to health services for urban China is another major contributor to health inequities. Given that most of China's health service resources are located in urban areas, uneven urbanisation across the country is responsible for unequal availability of and access to various health services.201 Among prefecture-level cities, there is inequity in the health service (table ). The number of health-care personnel per 10 000 people based on populations in administrative areas or populations in urban districts both show that the divergence between the top-ranked cities and the bottom-ranked ones is substantial. Given that most of the bottom-ranked cities are third-tier cities located in the south and southwest of China, appropriate policies are needed to address this disparity. The National Plan for New Urbanization 2014–20 emphasises urbanisation in China should be focused on small-sized and mid-sized cities and towns, therefore these health service inequities need to be acted upon in a timely manner.
Table.
Numbers of registered doctors and doctor assistants per 10 000 people in cities at prefecture-level and above in 2014181
| Top five | Bottom five | |
|---|---|---|
| Based on populations in administrative areas | ||
| 1 | Shenzhen (84) | Xinyang (ten) |
| 2 | Dongguan (79) | Anshun (ten) |
| 3 | Daqing (73) | Shaoyang (nine) |
| 4 | Beijing (68) | Longyan (nine) |
| 5 | Taiyuan (52) | Dazhou (nine) |
| Based on populations in urban districts | ||
| 1 | Daqing (108) | Baoshan (15) |
| 2 | Ordos (100) | Suqian (15) |
| 3 | Kaifeng (92) | Dazhou (13) |
| 4 | Henyang (88) | Guigang (12) |
| 5 | Shenzhen (84) | Yichun (12) |
Section 3. Management of health challenges in urban China
Cities have taken actions to address urban health challenges. Most notable among these actions are controlling environmental pollution, improving livability of urban environments, enhancing disease prevention and control, advancing universal health coverage, and testing new methods in urban health management. Evidence summarised in this section show that substantial health improvements have been achieved. Nevertheless, there are still gaps that need to be addressed.
Environmental pollution
Cities in China have taken widespread actions to control pollution in urban areas. China recently added PM2·5 to its national Ambient Air Quality Standards and issued a major policy in 2013—the Action Plan on Prevention and Control of Air Pollution—to target reductions in PM2·5 through control of industrial emissions, promotion of clean energy, reduction in emissions from road traffic, and other measures. During the 5-year period covered by the plan (2013–17), the Beijing–Tianjin–Hebei region committed to reduce annual average PM2·5 by 25%, Yangtze River Delta by 20%, Pearl River Delta by 15%, and other major cities by 10%.202 Similar action was taken to address water pollution. In the Action Plan for Water Pollution Control issued in 2015, the focus was on the reduction of highly polluted urban water bodies in urban areas and the improvement of quality of drinking water sources for cities. According to the plan, by 2030 all highly polluted water bodies will have been remedied and 95% of drinking water sources for cities at prefecture-level and higher will have level 3 national water quality standards (ie, safe for drinking, fishing, and swimming).203
China is also taking actions to transform energy intensive industry, which is considered the root of many environmental pollution problems. For example, in 2014, China accounted for 23% of global primary energy consumption; of this energy, 69% was used in the industrial sector (figure 11 ). The manufacturing industry contributed most to total industrial output and its energy intensity ranked second among all sectors.37 In 2015, the State Council published Made in China 2025, a plan designed to improve the quality of China's manufacturing industry.205 The plan provides policy guidance for the replacement of energy intensive industries with service-oriented industries and is expected to lead to reduced industrial pollution. Beyond direct measures for pollution control, more than 200 cities have adopted low-carbon development goals, including a reduction in the intensity of CO2 emissions and energy consumption for buildings and for the transportation and industrial sectors.206
Figure 11.
Final energy consumption, 2000–14
Source: China Energy Statistical Yearbook 2014204 and China Statistical Yearbook 2015.37 TCE=tonne of coal equivalent.
The government is also working to improve transparency in environmental governance. The Open Government Information Regulations and the Environmental Information Disclosure Measures were passed in 2008. Accordingly, the number of environmental information queries received and answered by the Ministry of Environmental Protection increased from 68 in 2008 to 1076 in 2013.207 In 2008, the Institute of Public & Environmental Affairs began tracking the transparency of pollution information in China; the number of cities achieving a passing grade increased from just 4 (3·5%) of 113 in 2008 to 21 (17·5%) of 120 in 2015.208
Substantial progress has been made in some heavily polluted cities. Annual PM10 concentrations in 86 major cities decreased from 116 μg m−3 in 2001 to 85·3 μg m−3 in 2011. The number of days with a PM10 concentration above Chinese ambient air quality standards (24 h mean 150 μg m−3) also decreased, from 66 in 2001 to 28 in 2011. The number of days with a PM10 concentration that exceeded WHO guidelines (24 h mean 50 μg m−3) decreased from 294 in 2001 to 250 in 2011. Premature deaths caused by PM10 pollution as a fraction of all deaths decreased from 13·5% in 2001 to 11·6% in 2011.209 The mean annual concentration of PM10 in 2017 for cities at prefecture-level and above was 22·7% lower than that in in 2013. Between 2013 and 2017, PM2·5 concentrations declined by 39·6% in Beijing–Tianjin–Hebei, by 34·3% in Yangtze River Delta, and by 27·7% in Pearl River Delta. All cities achieved the targets for the reduction of PM2·5 specified in the Action Plan on Prevention and Control of Air Pollution.210
The reduction of environmental pollution has resulted in positive changes for health. In Taiyuan city, improvements in air quality between 2001 and 2010 are estimated to have prevented 2810 premature deaths and reduced the total disability-adjusted life-years associated with air pollution from 52 937 to 22 807.211 The exposure of children to lead in urban China is also declining. Between 1990 and 2009, mean blood lead concentration in urban children at 0–6 years of age decreased from 7–10 μg dL−1 to 2·5–6·0 μg dL−1 and the prevalence of children with increased blood lead concentration (≥10 μg dL−1) decreased from 30–50% to 1·5–15·0%. This decline can be attributed to the phase-out of leaded gasoline, use of clean energy, and relocation of heavy polluters.212
Despite many achievements, environmental governance in urban China needs to be strengthened. Current practices are largely top-down, relying heavily on enforcement by governments. Efforts to use market mechanisms to regulate pollution, such as through compulsory pollution insurance, have had mixed success to date. The compulsory pollution insurance programme is unpopular because of its weak legal basis, poor technical support, unattractive coverage and premium rates, and low demand among industrial companies.213 Although environmental policies often target large industrial companies, the polluters that cause the highest intensity of damage to population health are medium-sized facilities; larger facilities generally have more effective pollutant control technologies or are located farther away from densely populated areas, or both.214 Given that it will take time to substantially reduce ambient air pollution in major cities in China and that most exposure to air pollution occurs indoors, the control of indoor pollutants (of both outdoor and indoor origin) is a feasible interim solution for the reduction of overall exposure and corresponding health risks.
Programmes such as those devoted to the achievement of low carbon cities could help to avoid characteristic urban environmental harms, but the resources and long-term commitments needed for their success in China are still absent.206 Furthermore, the public is largely at the receiving end of environmental management, having at best a restricted participatory role. The government remains cautious about such participation; people are encouraged to reduce personal emissions and to monitor sources of pollution but citizens and NGOs are restricted in terms of the actions they can take to confront environmental pollution. For example, environmental NGOs' access to state institutions are intentionally restricted.215
Livability of urban environments
Cities in China have made considerable progress in the improvement of urban living conditions over the past four decades, particularly in terms of basic infrastructure and sanitation. Large-scale government investment has resulted in mass construction of basic infrastructure in cities. In 1978, fixed-asset investment in urban service facilities was ¥1·2 billion (about $2·7 billion when adjusted for inflation) nationwide, but this figure reached ¥1·6 trillion ($257·8 billion) in 2015.216 This investment has helped to improve water and gas supplies, heating, road and rail transit systems, sewerage and wastewater treatment, waste management, and flood control, while improving the design and aesthetics of the urban landscape. One key example is the improved water services that have expanded across cities in China, achieving coverage of 98·1% of urban residents in 2015 from just 53·7% in 1981.216 This improvement might contribute to the lower mortality rate of oesophageal cancer in urban areas (89·1 per 100 000 people) than in rural areas (285·9 per 100 000 people) in 2015,64 because the consumption of untreated water from polluted sources has been positively associated with oesophageal cancer in rural areas.217 Greenspace and open space, including greenways, parks, and other urban conservation lands, has increased in 97% of prefecture-level cities because of its known benefits for urban quality of life, public health, and climate change adaptation.218 Governments at various levels have used large-scale urban development projects to target specific aspects of urban infrastructure. For example, between 2000 and 2010 in China, massive inner-city renewal and urban expansion projects progressively removed slum-like residences, replacing them with high-rise modern residential blocks.219
The Hygienic Cities movement is a hallmark of urban development in China that resulted in an unprecedented level of improvement in urban sanitation across China's cities (panel 3 ). The policies aimed to create better living environments for urban residents through the improvement of waste management and personal hygiene habits and the elimination of urban decay.220 Municipal governments launched major initiatives focusing on sanitation, urban infrastructure, and environmental protection. For a city, city district, or town to attain the title of National Hygienic City (or District or Town), it has to meet more than 100 criteria and pass an initial 3-year period of scrutiny and periodic unannounced inspections.6 As of March, 2015, 216 cities and 42 urban districts met these stringent criteria (appendix). There are also 679 National Hygienic Towns. Hygienic cities and districts performed better, on average, with respect to waste treatment, air pollution control, urban greening, infrastructure construction, and health promotion than did non-designated cities and districts.221
Panel 3. Weihai—the first National Hygienic City.
Weihai, a coastal city in Shandong province, was the first to be certified a National Hygienic City in 1990. The improvements to the urban environment made during and after the certification campaign have brought substantial health benefits to its 2·8 million residents.
To meet the stringent requirements, Weihai invested heavily in various urban environmental improvements. It has built facilities to process waste, achieved a 100% processing rate, and formed a partnership with New York City, NY, USA in 2016 to deal with ocean waste. Given its coastal location, coastline restoration and environmental management were prioritised. Weihai has controlled pollution in all urban rivers and grounded 66 000 cars that failed to meet emissions standards. It has also closed the door to companies with high energy consumption and pollution, turning down US$2 billion in foreign direct investment and ¥20 billion ($3·2 billion) in domestic investment between 1989 and 2012.
As a result of these efforts, the water qualities of all city seashores in Weihai now meet national standards and Weihai ranks best in the country on this measure. Its air quality is consistently ranked the best in Shandong province. In 1997, Weihai was one of the first six cities to be certified as a National Model City for Environmental Protection. Life expectancy increased from 72·0 years in 1985 to 81·1 years in 2015, substantially exceeding the national average of 76·34 years.11
The success of the National Hygienic City programme in Weihai is a result of the realisation by its leaders that efforts to achieve this status would help them protect the natural environment, which is a unique resource of the city. The title helps the city stand out from larger, more prominent Chinese cities and provides credibility in attracting both domestic and foreign direct investments. Weihai's example shows that tightly aligning a health programme with local government development pathways guarantees its success.
These improvements were associated with important health gains. For example, the incidence of infectious gastrointestinal diseases in National Hygienic Cities was reduced by an average of 2·8% 4 years after certification and the incidence rates of other infections, including vector-borne, zoonotic, blood-borne, and sexually transmitted diseases, were lower than in control cities. Health literacy of people living in National Hygienic Cities is higher than that in control cities and poor sanitary habits, such as public spitting and littering, declined, while physical activity increased.6
China established a national emergency management platform to reduce the health, social, and economic effects of natural disasters, environmental and industrial incidents, public health events, and security challenges. The platform integrates multiple functions, such as daily emergency management, risk analysis, monitoring and control, risk forecasting and early warning, integrated coordination, decision-making assistance, command and dispatch, simulation, and training. The platform has greatly improved the capability and efficiency of the government when dealing with emergencies.222 For climate-mediated risks in particular, the central government released the Action Plan for Urban Adaptation to Climate Change in 2016223 and selected 28 cities in 2017 to be involved in a pilot programme to build climate-adaptive cities. These cities will use a comprehensive approach to adapt to future climate change; for example, through modifying urban planning and design, improving monitoring and early warning systems, adopting engineering and nature-based methods to increase cities' resilience, and working together with the international community.224
In addition to government-led programmes, the private sector has used innovative ways to improve health in cities.111 For example, China's dockless bike-sharing programme, which launched in Beijing on Sept 1, 2016, has expanded to more than 200 cities by the end of 2017. More than 25 million bikes have been made available to the public and 300 million people have registered as users.225, 226 The rapid development of bike-sharing programmes has been facilitated by mobile technologies whereby users can access any available bike immediately and can park bikes in any public space after use, with the entire process of renting, returning, and paying completed via an application on users' mobile phones. The bike-sharing programme has reduced car use, alleviated traffic jams, and reduced emissions in cities, while satisfying urban residents' transportation needs in Chinese cities. Nationwide, the programme has saved users 760 million hours in commuting time. In addition, 1·4 million tonnes of gasoline has been saved because of reduced car use; 4·2 million tonnes of carbon and 3·2 million tonnes of PM2·5 emissions have been avoided.226 Bike sharing programmes are expected to continue to expand and become more popular. However, although this programme should be credited for making urban transportation greener, the traffic safety and parking issues associated with the explosive growth of bikes in cities have caused concern. City governments and the private sector should work together to solve these emerging problems.
The dominant role of government in China has allowed for urban environmental improvements of unprecedented speed and magnitude. However, there are inherent limitations in this centralised approach. Most environmental policies and management efforts were designed to address immediate environmental crises rather than the long-term health of the urban environment. This approach has also failed to address social equity concerns.227 For example, residents of old city districts often reap little reward from urban regeneration efforts; they are often inadequately compensated and are frequently relocated to the urban fringe.228 Environmental governance in cities in China is characterised by multi-sectoral administration, conflicting responsibility, scarcity of public participation, and local interest-centred frameworks, which, together, result in heterogeneous efforts and resources for environmental management.229 Since public participation is still restricted, more flexible and pragmatic policies are needed to facilitate this input in complex political contexts.228
Disease prevention and control
As in most of the developed world, prevention is the cornerstone of infectious disease management in China. Major initiatives include mass immunisation, timely detection and reporting of and response to infectious disease outbreaks, and measures to control transmission. The widespread improvement of urban infrastructure since the economic reform, particularly the construction of central water supply systems, public toilets, and wastewater treatment facilities, has helped to limit the transmission of many infectious diseases. By 2015, it was estimated that less than 10% of fecal coliform from human sources in Chinese waters were from urban areas.230 The Hygienic City movement has played an important role in controlling the transmission of infectious diseases, with its strong focus on controlling vectors and cultivating good habits for personal heath.6
In 1982, nationwide immunisation for children was started to vaccinate children against six communicable diseases: measles, poliomyelitis, tuberculosis, pertussis, diphtheria, and tetanus.231 Over the years, new vaccines have been successively added to this list; the Instruction and Procedure for National Immunization Program for Children, passed in 2016, now includes 14 vaccines covering 15 diseases.232 The latest National Health Survey on Health Service showed that more than 90% of urban children younger than 5 years old had received all required vaccines.233 The central government has also organised frequent large-scale vaccination campaigns for migrant children. In one such campaign in Guangdong province in 2009, more than 1 million migrant children were vaccinated.234 These immunisation programmes have led to significant decreases in incidence of infectious disease in urban populations. For example, the incidence of measles in Beijing has decreased from 593·5 per 100 000 people in 1951 to 0·5 per 100 000 people, which is mostly attributed to vaccination coverage rates of 95–99%.235
China has learnt from previous epidemics of infectious disease. One important lesson from the management of the 2003 pandemic of severe acute respiratory syndrome was the value of an effective disease monitoring and early-warning system at national level. Incomplete and delayed reporting of cases during the outbreak greatly weakened control efforts. To tackle this issue, the National Notifiable Diseases Reporting System was set up in 2004 with a mandate to monitor the occurrence of 37 infectious diseases, as laid out in the Law on Controlling Infectious Disease. By 2009, two more diseases were added to the reporting list. The national network reduces the average time between the identification of a disease case and its report to the Chinese Center for Disease Control from 29 days to under 24 h.236 Other national disease surveillance systems, such as the Disease Surveillance Points System, also track the occurrence of diseases and causes. Sentinel surveillance systems for specific diseases, such as malaria, have been set up at national and regional level to support the information collected by the standard systems.
The enhanced disease surveillance system has led to better control of infectious diseases in China. In 2016 alone, around 7 million cases and 18 000 deaths resulting from infectious disease were reported through the network.237 The national surveillance system for malaria, established in 2012, has provided data on epidemics, vectors, and other relevant factors to the national malaria elimination programme, which allows the programme to investigate and verify individual cases, screen surrounding populations, and start relevant vector control strategies.238 The surveillance system has also been useful at detecting emergent infectious disease. For example, the National Notifiable Diseases Reporting System helped the health administration in Dongguan (a manufacturing city in Guangdong province with 8 million residents) to detect an outbreak of dengue and trace its source to a patient just 1 month after the patient was infected during an oversea trip.239
Infectious disease prevention has expanded to areas that have historically been stigmatised in China, such as HIV/AIDS prevention in commercial sex workers. In Wuhan, the 100% Condom Use Program helped to increase condom use rates in commercial sex workers by 94·5% in 15 months.240 The central government started a national HIV/AIDS treatment programme in 2003, through which 157 050 people received antiretroviral therapy by 2011. This programme led to a 26% relative reduction in HIV transmission in 38 862 treated serodiscordant couples, indicating that this treatment-as-prevention approach is working in China, although further studies are needed to assess durability.241
Infectious disease control in urban China still faces many challenges. Although disease surveillance networks have proven indispensable, they face the common issues of poor accessibility, poor data quality, under-reporting, and inadequate staffing and funding.242, 243 For example, a field survey of 161 Disease Surveillance Points System sites in 2009–11 found that the crude under-reporting rate for mortality was 10·7% in urban areas.244 Some issues require creative solutions, such as the vaccination of migrant children whilst on the move with their parents.234 Other issues face cultural barriers, such as controlling male-to-male transmission of HIV/AIDS.245
Management of non-communicable diseases in China has shifted from disease treatment to prevention in the past decade. The promotion of healthy lifestyles has been prioritised and people in urban China are encouraged by governments to exercise more. Two national regulations, the Community Service System Construction Plan (2011–2015) issued in 2011 and the Urban Community Sports Facilities Construction Land Index issued in 2005, require that any new residential units must include spaces (including green spaces, open spaces, and yards) and exercise equipment, and specify the size and types of equipment for residential units of different sizes. Governments also provide incentives for people to participate in physical exercise, such as competitions and small awards. More recently, cities have experimented with allowing residents to charge the fee of using sports facilities to their medical insurance cards as a stimulus.246 The participation rate in moderate or vigorous physical activity outside of work among urban adults (≥18 years) was as low as 7·9% in 2001 but increased to 21·6% in 2013.73 Cities are also getting serious about the control of tobacco use. By the end of 2016, more than 30 cities in China have passed or are in the process of passing regional regulations and laws that ban smoking in public indoor spaces. Among them, Beijing passed the strictest regulation on banning smoking in public spaces (panel 4 ). The move, once successfully implemented, will protect 20% of the country's population from second-hand smoking.247
Panel 4. Tobacco control in Beijing—the strictest tobacco control policy in China.
The Beijing Smoking Control Ordinance, which was passed by the Beijing Municipal People's Congress in November, 2014 and came into effect on June 1, 2015, is one of the toughest tobacco control laws adopted in China to date.
Under the law, smoking is prohibited in all indoor public places and many outdoor public places, such as kindergartens, schools, and child and maternal health centres. The law includes strong penalties for violations; for example, owners or managers of premises—not just individual smokers—are liable for fines if they fail to comply. In addition, the law bans tobacco advertising on mass media, in public places, outdoors, and on public transport.
The capital's decision to adopt such a strong smoke-free law is important because other cities across China will seek to emulate Beijing's example. Both Shenzhen and Shanghai have since passed strong comprehensive smoke-free laws, thereby protecting well over 60 million Chinese citizens and residents from harmful exposure to second-hand smoke. More importantly, these cities have now set the benchmark for smoke-free policies for China.
Successful enforcement of a smoke-free law in a city the size of Beijing—with its myriad of offices, restaurants, bars, shops, and hotels—is a colossal task. It requires a visible and ongoing enforcement effort, rigorous application of penalties for offending smokers and businesses, and substantial investment of resources in public education and awareness. The Beijing Government has worked hard to enforce the law since it came into effect. Health inspectors are out in large numbers around the city, checking venues and ensuring compliance with the law, supported by thousands of community volunteers. Beijing's residents are actively engaging in the enforcement effort through complaints to the 12320 hotline or through the hugely popular WeChat social media platform. The Beijing Tobacco Control Association has an interactive virtual map at its premises, which shows in real-time the movement of the tobacco control volunteers around the city and highlights venues or establishments that are being reported for their non-compliance. This use of integrated innovative technology is impressive and helps to support enforcement efforts.
The effect the law has had is even more encouraging. Between May, and August, 2016, the Health Education Centre of Beijing Center for Disease Control and Prevention did a survey of 10 000 households from 16 districts in Beijing. The results showed a reduction in adult smoking rates (from 23·4% in 2014 to 22·3% in 2016); a reduction in exposure to second-hand smoke in various venues; an increase in the quitting rate among adults (from 14·9% in 2014 to 16·8% in 2016); an increase in public awareness of the harms of smoking; and a decrease in the number of adults who noticed tobacco advertisements at point-of-sale. Recent surveys have also shown that there is strong public support for 100% smoke-free laws.
The Beijing smoke-free law is a major step forward in the battle against tobacco in China and the people of Beijing are now breathing easier as a result. The success of the law so far is owed to dedicated enforcement by the government and the high proportion of well educated people living in Beijing, which tend to be more supportive of smoking bans. In less developed regions, the implementation of the smoke-free law will probably face more resistance.
Governments at various levels are trying to increase the health literacy of urban residents. Three major channels have been used to reach urban residents, including mass media, community organisations, and the education system. Mass media has a central role in disseminating health knowledge and information in China because more than half of Chinese people get their health knowledge from television.248 Community organisations are another effective way to improve health knowledge. The centralised government structure allows health information to be passed from the central government to the smallest communities in China. Cities are also offering health education classes through primary schools to high schools.249 In addition to these formal channels, cities in China came up with creative ways to disseminate health knowledge. For example, the Shanghai municipal government has given a free health package to 8 million households annually since 2010. The package contains publications on health, spoons to measure salt, an oil dispenser with measuring marks to reduce oil use in cooking, and tapes to measuring one's waistline. These small gifts have been very effective in communicating the concept of healthy lifestyle choices to a large population.250 These efforts have led to positive changes. For example, according to a 2015 survey of 10 000 urban residents in 44 cities, compared with 2013, consumption of carbonated soft drinks decreased by 21%, chewing gum by 15%, and western fast food by 16%. Further, 73% of survey participants participated in sports activities, which is simliar to the 70% reported in US cities.251
Disease screening is another important component of the prevention strategy. In 2011, the government started a national programme for stroke prevention and screening. The programme provides free screening to permanent urban residents aged 40 years or older and more than 4·6 million people have been screened so far. About 0·69 million high-risk people identified in the initial screening tests had further examinations, and those diagnosed received advice on treatment. The programme helps the health department to identify an increasing trend of stroke risk among people aged 40 years or older.252 Cancer screening services are now increasingly made available to at-risk populations through health insurance. For example, the proportion of women who had cervical cancer screening services reached 29·1%, with a higher percentage seen in women with urban insurance coverage than in those without or with rural health insurance.253 Some cities even offer free physical examinations for all residents (panel 5 ).
Panel 5. Luzhou–free physical examination for all residents.
Luzhou city is located in Sichuan province and is formed of 5 million people living in a mountainous area of about 12 000 km2 in size. In June, 2016, the city started a project to offer free physical examination to all residents. The entire population of permanent residents was divided into five age groups: 0–6 years, 7–17 years, 18–34 years, 35–64 years, and 65 years or older. People in the 0–6 years, 7–17 years, and 65 years or older groups were entitled to free annual physical examinations. The rest were entitled to free biannual physical examinations. The physical examination includes routine tests, such as blood tests and liver function tests, and specific tests that were decided by each district (such as digital radiography of the chest). Examinations are done in health facilities or onsite for people who are handicapped or living in remote areas.
1·8 million residents were checked in 2016, of which 500 000 had never had a physical examination. The examinations showed that around 306 000 people had high blood pressure, 99 000 people had diabetes, and 40 000 people had another chronic disease. The results of each examination were electronically archived and grouped by families, villages, and communities before storage in community health centres. The archives are updated dynamically with information on subsequent examinations, treatments, and insurance reimbursement. Residents can look up their health information via an application on their mobile device. The examination results were also used to separate people into three groups: people who need routine health management, people who need specific attention, and people who need precise health management. The latter two groups include people with diabetes, high blood pressure, or severe mental health problems, high-risk pregnant women, and people at high risk of chronic disease. Each individual is assigned to a management team, which includes a physician and a local government staff. The team tracks the health status of the person and advises them on how they can manage their personal health.
Two factors might have contributed to the successful implementation of the free-for-all physical examination in Luzhou. First, the population size of the city is relatively small by Chinese standards which keeps the expense at an acceptable level. Second, Southwest Medical University has been located in Luzhou since 1951. The medical university and its many associated medical agencies not only provide the human resources necessary for such a project but they also increase the health awareness of the residents in general.
Cities in China are using a comprehensive approach to deal with non-communicable diseases. China started a campaign for the control of chronic diseases in 2010 aimed at four main types of chronic disease: cardiovascular disease, malignant tumour, chronic respiratory disease, and diabetes. The campaign integrates disease surveillance, prevention, and treatment to form a comprehensive strategy. By the end of 2015, 265 counties, city districts, and county-level cities had been selected as national demonstration sites to receive this comprehensive approach.254 The management of mental disorders in cities also requires an increasingly comprehensive strategy. A grid model has been used in many cities to manage patients with mental disorder. The model is built on collaboration between public health service agencies and neighbourhood committees and involves measures that allows for discovering and treating patients in the community. These measures include health education, physical examination, regular doctor visits and reports of cases, patient registations, free treatments, and dealing with emergencies at the community level. The effectiveness of this model relies on the joint effort of patients' families, communities, and various government agencies.255 Results show that this comprehensive management is effective. A meta-analysis256 of studies between 2004 and 2015 showed that the recurrence rate of severe mental problems under comprehensive management is 32% of the rate in the control group.
New approaches like patient empowerment, which enables people to take control of their health, wellbeing, and disease management and to participate in decisions affecting their care, are being tested for chronic disease management. Self-management of chronic diseases in Shanghai has shown that identification of responsibilities, integration of multiple resources, and an emphasis on evaluation can make patient empowerment an efficient and effective mechanism for the prevention and control of non-communicable diseases and the achievement of improved health outcomes in patients suffering from these diseases, especially elderly people (panel 6 ).257 China has also participated in the community-based safety programme initiated by WHO since 2006 to prevent injury, violence and suicide. By November, 2011, China had 46 designated international safe communities and 244 designated national-level safe communities.147
Panel 6. Self-management of chronic disease in Shanghai.
In 2002, a randomised controlled trial of the Chronic Disease Self-Management Programme started in Shanghai. Initial results showed that the generic self-management education programme improved participants' health behaviour, self-efficacy, and aspects of their health status, and resulted in fewer visits to the emergency room and fewer admittances to hospital after 6 months. These successes were achieved through locally-based delivery models and the integration of routines of community government and community health services.
In 2007, the Health Promotion Committee of Shanghai adopted the recommendation from the School of Public Health at Fudan University to disseminate chronic disease self-management through the network of the healthy city in Shanghai. Powerful policy support, defined responsibilities for the different actors, and active participation from the relevant population characterised Chronic Disease Self-Management Programme as a tool for the prevention and control of chronic illness. As of 2016, 420 000 people (most of whom were elderly) had been organised into 26 000 groups and participated in these activities. Guided by the principles of doctor–patient cooperation, mutual aid, and self-management, the programme succeeded in creating a supportive environment for the prevention and control of chronic disease. Based on an evaluation of the programme in 2011, 63·6% of group members had sufficient interactive health literacy, 34·6% increased their physical activity significantly (45·1% increased slightly); 32·5% increased their vegetable and fruit intake significantly (46·0%increased slightly); 24·9% decreased their salt intake significantly (58·0% decreased slightly), and 28·3% decreased their oil intake significantly (55·4% decreased slightly). In this analysis, women tended to be better at improving their lifestyle behaviours than men were.
The qualitative analysis showed that members listed information exchange, shared experiences, and an improvement in mood as the biggest gains from participating in the self-management group. 58·8% of members did voluntary activities, 50·6% did activities organised by residential committees, and 47·8% did activities organised by various interest groups.
The Chronic Disease Self-Management Programme in Shanghai has been remarkably effective to date; it has empowered patients to make decisions on self-care and broader collective actions regarding chronic disease control. Its success in Shanghai can be attributed to the collaboration between Fudan university and the government. Given that Shanghai is the most developed region in China, the area's financial resources and well educated population contributed to the programme's success. Other large cities—such as Beijing, Guangzhou, and Shenzhen—could adopt the same programme.
Even with the enhanced efforts, there are still gaps in the control of non-communicable diseases in urban China. Prevention programmes in China often adopt a top-down approach and, although this method is able to generate positive results quickly, it might not be enough to address the increasingly complex health issues. For example, an investigation of health education in six provinces in 2013 found that only 36·1% of the urban residents aged 18–60 years had adequate health literacy.258 Multi-sectoral strategies that target the underlying causes of chronic diseases are nonexistent in most cities. Interventions that are evidence-based, low cost, simple, sustainable, and scalable need to be developed.259 The desire and actions of individual urban residents might be the key to success, rather than more government-sponsored programmes. Without the whole-hearted involvement of residents, effects from any health promotion programmes will be superficial and short-lived.
Reformed universal health coverage
Faced with the undesirable consequences of serious health inequity in China, the government started the third stage of reform in 2009 with recognition that access to health care is a basic right of citizens and its provision rests with the state. A major goal of the reform is to implement universal health coverage.184 Cities in China are acting to expand the health-care sector and make it more efficient, streamline the health insurance system, and improve affordability of health care, and make health services increasingly available to underserved groups, such as migrants.
The Chinese Government invested heavily to expand its health-care system and, as a result, the number of doctors (including assistant doctors), registered nurses, and hospitable beds increased substantially in urban areas in China. For 2010–15, the number of medical practitioners increased from 2·97 to 3·72 per 1000 people, registered nurses from 3·09 to 4·58 per 1000 people, and hospital beds from 5·94 to 8·27 per 1000 people.51, 260 The most notable example is Hong Kong, where government spending on health service is linked with economic growth and guaranteed by laws (panel 7 ).
Panel 7. Hong Kong—guarantee health services with laws.
Hong Kong Special Administrative Region is a coastal city in the south of China that has one of the highest life expectancies in the world. In 2015, life expectancy at birth was 81·2 years for men and 87·3 years for women, which is above China's national average of 74·6 years for men and 77·6 years for women and the USA's average life expectancy of 76·9 years for men and 81·69 years for women.261 The city is unique because it is one of the few cities in China where the health-care system is not managed by the central government's National Health and Family Planning Commission or its subsidiary local health bureaus. Instead, the health-care system is modelled on the National Health Service in the UK because of Hong Kong's history as a British colony.262
The laws and legislations of this system help to ensure access to quality medical care for its residents. According to the Basic Laws of Hong Kong (article 107), the government's expenditure needs to be consistent with the city's GDP growth.263 Article 138 states that the government should develop policies for the development of western medicine and traditional Chinese medicine and the improvement of medical and health services. Furthermore, under the provisions of Section 4d of the Hospital Authority Ordinance (chapter 113), the hospital authority recommends fees for the use of hospital services by the public based on the principle that no person should be prevented, through an absence of means, from obtaining adequate medical treatment. Section 8 of the same ordinance states that the hospital authority might also borrow money, if needed, to meet its obligations or perform its functions.
These legal protections have created a relatively equitable system such that health services for most residents in all communities are rarely more than 30 min away from their homes and access to essential health care is given regardless of their ability to pay. To provide an average of 5·2 beds per 1000 residents and other health services, the government owns 42 public hospitals and institutions and employs 6287 doctors and 20 057 registered nurses. However, the maintenance of these standards over the past decade has more than doubled government expenditure on health, with HK$67 430 million being spent in 2016 compared with $30 176 million in 2006. This rise led to a 4% increase in total government expenditure from 14·6% in 2006 to 18·6% in 2016.
Hong Kong's strong economy and independent law system are key to the level of health services provided in the city. Given that many cities in China now have a strong economy, other cities should try to secure support for health services through local laws or regulations.
China has been working to improve the efficiency of its health-care system since 2009. The basic principle is to tilt resources to primary care and form a hierarchical health-care system.264 The government hopes to return non-acute patients back to their respective community health centres to relieve the burdens of tertiary hospitals, promote a favourable patient–doctor relationship, maintain the quality of local hospitals, and target limited resources at populations with greater needs. A series of actions have been implemented to realise these goals. These actions include making community health centres or town (or village) clinics the gatekeepers to specialists and other medical resources and forming a hierarchical structure in different levels of hospitals through strategies like the bi-directional referral system and health insurance policies.265 Another important task is to reduce patients' out-of-pocket expenditure by reforming the revenue system of hospitals and reimbursement procedures.266
These actions have started to change patterns of health-care use in urban China. Longitudinal data since 2002 showed that community health centres in urban areas could provide better health care, demonstrated by an increased breastfeeding rate and decreased prevalence of lower respiratory tract infection compared with hospital outpatient clinics.265 In Fuzhou, patients at community health centres are more likely to report better experiences with primary care attributes than patients visiting hospital facilities.267 In Shanghai, a survey of residents showed that they consider community health centres for convenience, good services, and low cost. On average, they paid ¥16·2 ($2·4) less for their first visit when using these centres between 2006 and 2010.268
However, community health centres in China are still not functioning as the first contact points and regular sources of care. There are still many problems in the development of these centres, including unsustainable governmental roles, inadequate human resources, laggard general physician practices, poorly designed payment schemes, and a crisis of trust.265 Additional policy efforts are needed to help community health centres to develop. Recent government investments in public health and primary care alone are not sufficient and might not be sustainable. It will not relieve an omnipotent government until long-term self-sustaining mechanisms are established, including a competent general practitioner system, supportive social insurance reimbursement, appropriate financial incentives to providers, better transparency and accountability, more regulations for the referral system, and a legitimate, sustainable, and quality community health system.269
Health insurance is an important means of achieving universal health coverage. The health reform that started in 2009 has a clear mandate to increase access to health care. To fulfil that mandate, the three types of state-sponsored insurance schemes (Urban Employee Basic Medical Insurance, Urban Resident Basic Medical Insurance, and new rural cooperative medical system) have been expanded dramatically in China. Findings from consecutive Chinese National Health Services Surveys270 showed that medical insurance coverage has increased from 29·7% of the total population in 2003, to 87·9% in 2008, and 95·7% in 2011 (figure 12 ). Only 17 million urban residents (4·1% of all urban residents at the time) enrolled into a medical insurance programme when they started in 1998.7 By 2016, the number of people enrolled in urban medical insurance programmes had already increased to 743·9 million (93·8% of all urban residents).8 This increased coverage is associated with a substantial increase in health service utilisation and decrease in economic burden; for example, the Urban Employee Basic Medical Insurance scheme reduced out-of-pocket inpatient expenditure by 64·5% and the Urban Resident Basic Medical Insurance scheme reduced it by 45·6%.272 As a result, the out-of-pocket expenditure as a percentage of private expenditure on health declined from 95·6% in 2000 to 72·3% in 2014.273 The national reimbursement ratio, which reflects the average reimbursement level of state-sponsored insurance, increased from 22·4% in 2009 to 26·4% in 2011.274
Figure 12.
Different types of health insurances held by people living in different parts of China, 2003, 2008, and 2013
LIS=labour insurance system. GIS=government insurance system. RCMS=rural cooperative medical system. NRCMS=new rural cooperative medical system. UEBMI=urban employee-based medical insurance. URBMI=urban resident basic medical insurance. URRBMI=urban and rural resident basic medical insurance. Sources: China Health Statistics Yearbook 2003–09180 and China Statistical Yearbook of Health and Family Planning 2014.271
However, the effect of health insurance in China is highly heterogeneous among different population subgroups. Overall, health insurance leads to greater reduction in economic burden in retired people but has a smaller effect on decreasing the burden for individuals with a low income and low levels of education.272 There is a discrepancy between the reimbursement rate estimated from health expenditure (26·4%) and the reported reimbursement rate for listed services (50–60%) in 2011. This discrepancy suggests that the services covered by state-sponsored health insurance were not sufficient to meet residents' demand.274 Furthermore, the current health insurance scheme offers weak protection against rare diseases. It was estimated that, at a national scale, 247 620 urban residents could be lowered into poverty because of the medical cost caused by seven rare diseases in 2014.275
The uneven results are mostly caused by the decentralised and incremental approach to universal health coverage in China. The varied financing capacity of local governments leads to high variability of benefit packages for health insurance. For example, a 2011–12 survey of people aged 60 years or older in Xi'an, Wuhan, and Shanghai showed that the inpatient reimbursement rate was 45·5–81·2%, and the outpatient reimbursement rate was 4·1–100%. Multiple insurance schemes reduce efficiency and increase abuse and barriers to access at the same time.276 The Chinese Government announced its plan to merge Urban Resident Basic Medical Insurance and new rural cooperative medical system in early 2016, which is a starting point for the ultimate consolidation of all state-sponsored health insurance schemes and for the achievement of equal benefits for all.277 Rural migrants, elderly people, and those with non-communicable diseases in cities will benefit the most from the consolidation of the existing health insurance schemes with extended funding pools.278
Health services to migrants have been strengthened. 98·2% of migrants are covered by at least one type of medical insurance and 97·9% of migrant children are covered by the national imunisation programme.279 Nevertheless, there is room for improvement. For example, in a comparative study280 done in eight cities in the Pearl River Delta, female migrants of reproductive age were less covered by health insurance schemes and had less free health care than women with permanent urban residence.
Build pilot Healthy Cities in China
10 years after the concept of a Healthy City was first introduced in Canada (panel 8 ), China started a small-scale trial of building healthy cities. In 1994, the Ministry of Health worked with WHO to establish a pilot programme that included two urban districts: Jiading district in Shanghai and Dongcheng district in Beijing. In 2007, ten cities and towns were chosen by the Ministry of Health for the expanded pilot programme.284 In 2015, the State Council of China called for building healthy cities in Opinions of the State Council on Further Strengthening the Patriotic Health Work During a New Period, which calls for building healthy cities with Chinese characteristics.285 Then in 2016, after the Healthy China 2030 plan was passed, the National Health and Family Planning Commission expanded the pilot programme and chose 38 cities as the first group to be included in the national programme.
Panel 8. The concept Healthy Cities.
WHO defines a healthy city as “one that is continually developing those public policies and creating those physical and social environments which enable its people to mutually support each other in carrying out all functions of life and achieving their full potential.”281
WHO's Europe Office suggests that a city can become a healthy city if it adopts a Healthy Cities approach. This approach seeks to improve health in cities through good urban governance that puts health high on the political and social agenda of cities. The Healthy Cities approach recognises the determinants of health and the need to engage all stakeholders to address them; this attitude is supported by a set of core values, including equity, social inclusion, intersectoral management, and community participation. These values explicitly imply that urban health development is everyone's business.282
In 2016, the National Patriotic Health Campaign Committee of China defined a healthy city as an upgraded version of a hygienic city, stating that “through the improvement of urban planning, construction and management, (the city) improves the natural environment, social environment, and health services and popularizes healthy lifestyles to meet residents' health needs and to achieve the coordinated development of urban construction and human health.”
The five main focuses of healthy cities in China are constructing healthy environments, building healthy society, optimising health services, fostering healthy people, and developing healthy culture. The six key tasks include constructing healthy cells (healthy schools, institutions, and communities), establishing health governance models, improving environmental and sanitary infrastructure, enhancing the safety management of drinking water, improving environmental quality, and improving public security systems.283
The Healthy Cities movement in its essence is a social movement that mobilises the entire society to work together to improve urban health. Both leaders and residents in urban China are not new to this type of social movement thanks to the success of the Hygienic Cities movement. The Healthy Cities project in China has unique features. The participating cities focus on five fields: health service, healthy environment, healthy society, healthy people, and health culture. Municipal governments serve as conveners while different government agencies organise and implement specific projects on the ground. Residents, NGOs, and other social enterprises actively participate in these projects. The Healthy Cities project has been pushed forward by its inclusion in governmental plans and implementation of specific projects. These measures are in contrast with the largely project-driven and non-governmental Healthy Cities project in developed countries.9 The difference is also clear in the evaluation methods of healthy cities. Overlaps on indicators for health and environment can be found by comparing the indicators used in China with those developed by the WHO Europe Healthy Cities Network (appendix); we found that half of the indicators had an overlap. The Chinese system has more comprehensive health indicators and the European system has more environmental indicators. However, the two indicator systems overlap very little on health service and social indicators. Overall, the indicator system used in China focuses more on measuring results and less on measuring actions, policies, and governance.286
So far, the pilot programme has increased integration of health into all policies and improved health awareness among urban residents in participating cities.9 Some innovative ways to promote health literacy in residents have been regarded highly by WHO, including Shanghai's actions to give every family a health guidance book and a ruler for measuring waist size as gifts from the city. The successful use of mass media in health promotion and education is a particular strength of the Healthy Cities project in China (panel 9 ). The pilot programme also helped to improve urban environments. In a paired comparison of 15 healthy cities with 15 non-healthy cities, the programme helped to increase the proportion of urban domestic sewage that was treated by 32%, the proportion of urban domestic garbage treated by 30%, and the proportion of qualified farmer's markets by 40%.287 Common reasons for successful projects include strong leadership of the government, availability of a mechanism for wide participation, and a genuine desire to seek collaboration. Projects that serve the wellbeing of local residents are more likely to succeed if they have the full support of the local governments and health-relevant policies based on local conditions.288 Although actions taken by cities in China are highly diversified and tailored to local conditions, actions are often quickly adopted at the national scale once they are proved effective. For example, free health packages have been given to every household as a way to promote health literacy in many pilot cities since its first use in Shanghai in 2010.
Panel 9. Wuxi—health education through mass media.
Wuxi, a city that is located in Jiangsu province and has 6·5 million people, used mass media effectively to promote health literacy among residents in its efforts to become a healthy city.
The city circulates a weekly newspaper that is entirely devoted to health and has 50 000 subscriptions. The city's television stations shot a 60-epsiode sitcom named Health 66 in 2010, which was broadcasted in Wuxi and 12 other cities in Jiangsu province. The Center for Disease Prevention and Control of Wuxi worked with a movie company to produce a six-episode three-dimensional cartoon on smoking control in 2012; the cartoon won the first prize in a national competition for education materials on public health and has been viewed nationwide. In 2016, Wuxi Radio Station broadcasted a 25-min section on healthy lifestyles every Saturday and Sunday. The radio also has a 2 h call-in programme on health knowledge every Sunday. Monday to Friday, the Wuxi television station has a 40-min quiz programme on medical knowledge and a 60-min show named Living up to 100 Years. On Saturday and Sunday, there is a 90-min programme named Zero Distance to Medical Experts. Famous experts from different hospitals are invited to discuss the prevention and treatment for different diseases and answer calls from patients. In addition to its use of mass media, Wuxi city set up a billboard of health information, built a library of at least 300 books about health in every community, and recruited 464 volunteers to promote health education in communities. These efforts have led to a health awareness rate of 85% among urban residents (measured through health administration surverys), which is the highest rate in Jiangsu province.
The success of Wuxi's use of mass media is a good example of how the Healthy Cities movement can improve health education and health promotion. The social services sector in the government (culture, propaganda, civil affairs, and sports) works closely with the health sector to share health information on mass media and in every community. The decision and investment by the municipal government to make Wuxi a healthy city provided the political motivation and resources needed for the two sectors to work together. This type of intersectoral collaboration has been widely applied in other Chinese cities.
However, there are also lessons that have been learned. First, although cross-sector collaboration has been emphasised in the pilot programme, projects are still primarily restricted to public health system. It is still a challenge to break down traditional barriers between different government agencies and between governments, NGOs, and private enterprises.288 For example, there are some general issues with health education in primary and secondary schools in general, such as a shortage of qualified teachers and materials. The situation is worse in less developed regions compared with more developed ones and is arguably caused by the current arrangement in which the National Health and Family Planning Commission is responsible for health education rather than the Ministry of Education because this arrangement means that health education in China is done primarily through informal education avenues.249 Furthermore, most projects take on soft targets (ie, health promotion) rather than difficult issues, such as improvement of infrastructure and equity. There is a huge discordance between the construction of Healthy Cities and urban planning and development. Finally, assessments on cities focus too much on results rather than progress.9
Section 4. Healthy cities as the way forward
Despite the great progress that has been made by Chinese cities to address urban health challenges, it has become increasingly clear that the the health sector alone, with its traditional piecemeal approach, cannot effectively resolve the modern challenges to urban health in China. These challenges will best be addressed through a systems approach—the Healthy Cities approach. There has never been a better time to develop healthy cities in China because of the favourable political and economic environments and the advancements in supporting technologies. However, critical barriers to the success of healthy cities in China need to be addressed. We make five recommendations to Chinese cities on how to address these barriers.
Why Healthy Cities?
The health challenges faced by Chinese cities today resemble problems that their European and North American counterparts had in previous decades. In these settings, urban sprawl and automobile-dominated transportation contributed to increases in air pollution, road injuries, sedentary lifestyles, and rising obesity and diabetes, among other issues.289 Simultaneously, public health management focused on proximate causes of ill health rather than underlying urban environments or living conditions, meaning that cities faced new and resurgent epidemics of infectious disease, increases in chronic diseases, and widening health disparities between social groups.290 Cities began to realise that the rising health problems created or exacerbated by economic growth and urbanisation cannot be resolved solely through the health sector. A population health approach that engages in the ethical and political dimensions of these challenges, recognising their inherent complexity and embracing new approaches to the production of scientific evidence and its translation into policy, will be required to address these problems.291 The Healthy Cities approach has been proposed as a framework that is capable of tackling the complex urban health issues of the 21st century.292
The European experience of Healthy Cities has shown that societal, economic, environmental, political, and technological forces can determine the success or failure of Healthy City approaches to urban development,293 and there are indications that social, political, policy and other conditions are right for China to successfully adopt the model. China's experience of adopting a blueprint for eco-civilisation—and the new directives calling for integration of health into all policies—provide a highly favourable precedent for the Healthy City policy. A key goal of China's eco-civilisation is to increase the wellbeing of Chinese people by balancing environmental protection and economic growth. This aim closely matches the core commitment of Healthy Cities to manage cities for people's physical, mental, and social wellbeing.294 Indeed, the emerging paradigm of planetary health underscores the close relationship between environmental protection and human health.295 Meanwhile, China's new health directives already embrace many of the central tenets of the Healthy Cities approach, including equity, health for all, Health in All Policies, and innovation in health management.11, 296 Never has there been a better opportunity for cities in China to serve as a vehicle for the implementation of new health policies, building on valuable experiences and management networks from the county's Hygienic City movement, which span from the central government down to townships and communities across the country.
The Healthy Cities approach demands that effective health interventions come from an effort to understand the constantly shifting dynamic relationship between the urban environment and human health and wellbeing. Relationships between variables that affect human health in urban areas are complex, often nonlinear, and might involve substantial time delays. They typically are involved in feedback loops, which can reinforce or reduce effects with beneficial or detrimental results.297 For example, dockless bike-sharing programmes can promote active lifestyles and mitigate air pollution but might also increase personal exposure to pollutants and injuries from road traffic accidents (figure 13 ).111 Urban health interventions should be supported by a conceptual and action framework that can accommodate the dynamics of multiple sectors and multiple scales. This framework has important implications for the activities of city governments, which will need to consider infrastructural, environmental, and sociocultural determinants, and to create capacity and transparent governance across spatiotemporal scales and sectors.298 Therefore, cities need to take transdisciplinary, interconnected, integrated and inclusive approaches—systems approaches—to deal with complex health challenges.294 The Healthy Cities approach intrinsically includes such a framework.
Figure 13.
Dockless bike-sharing programme
An optimal time to develop healthy cities in China
The timing is uniquely favourable to shift urbanisation strategies in China from a land-centred to a people-centred focus,299 broadening access to basic public services and improving the livability of cities through investment in social welfare and infrastructure. A massive docket of proposals exists for large-scale urban renovation and environmental improvement across China, offering a unique opportunity to construct healthy urban environments by embracing health as an essential element in urban planning and design. Continuing economic growth will enable China to make these key investments in healthy cities; the World Bank predicts that the national economy will grow at a rate of 5–7% between 2016 and 2030300 and current government expenditure on health is far behind those in developed countries. As investments in health increase and the engines of economic growth shift from investment and export-oriented manufacturing to internal consumption and service industries, a highly favourable economic environment will emerge for tackling the social and environmental roots of urban health challenges.301
Technological advancements are also newly positioned to support the development of healthy cities in China, including internet and mobile technologies. By the end of 2016, the number of internet users in China reached 731 million and internet penetration reached 53·2%, which is 3·1% above the global average.302 The attention paid to mobile health (including applications for mobile devices and wearable sensors) by capital markets is quickly rising, with large internet companies–such as Baidu and Tencent Groups–investing heavily.303 Mobile health applications and services potentially enable great flexibility in their response to public health needs and rapid growth in the utilisation of internet and mobile applications in health care will offer radically new models for the distribution of quality medical resources to China's diverse population.
The tremendous success of the Hygienic Cities movement has paved the way for another health movement that focuses on cities. Although the Hygienic Cities and Healthy Cities approaches both focus on urban environments, there are some fundamental differences between the two. The Healthy Cities project is focused on the population, emphasising the role of cities in the provision of public services and improved equity, and inherently embraces a systems approach that is geared towards the recognition of and response to complexity. The Hygienic Cities movement mostly focused on interventions in infrastructure management and urban sanitation. The Hygienic Cities movement started at a time when urbanisation in China had just began to accelerate and urgent environmental problems linked to rapid urban development were in conflict with the population's rising expectations for health and quality of life in cities.6 As China approaches a new phase of urban development, the comprehensive and population-centred Healthy Cities movement will respond effectively to the complex health challenges arising from this development and to evolving attitudes towards health in China.304 In doing so, it will help to address the gaps in equitable health and development that persist despite the successes of the Hygienic Cities project.
Gaps in the development of healthy cities in China
China's pilot programme for building healthy cities capitalised on national cultural priorities and competencies, emphasising the importance of strong government leadership and health services in the achievement of its notable successes. However, as the programme expands to the entire nation, important gaps needs to be addressed. We assessed current practice in China by surveying the approaches adopted by 36 cities (appendix). Indeed, cities in China are acting across multiple domains (panel 10 ) with key features that include a strong commitment to clean urban environments, diverse approaches to fostering cultures of health and healthy lifestyles, and a wide range of support for the urban poor and disadvantaged. Yet, several important gaps remain with respect to best practices for building global healthy cities, as highlighted by the WHO and UN Habitat.305
Panel 10. Major actions taken by the 36 cities in China to build healthy cities.
Actions are in decreasing order by the number of times they were reported.
Governance
-
•
Form a working team in the municipal government
-
•
Integrate health into the development plan
-
•
Evaluate performance of participants
-
•
Enforce existing laws and regulations
-
•
Set aside budgets for building healthy cities
-
•
Conduct baseline survey of health in the city
-
•
Set up a special office dedicated to the building of the healthy city
-
•
Assess progress regularly
Healthy environment
-
•
Control emissions of air pollutants
-
•
Control water pollution
-
•
Improve infrastructure and facilities
-
•
Afforestation and greening
-
•
Garbage collection, recycling, sorting, and burning
-
•
Industry transition to low-emission technology
-
•
Expand public transit systems
-
•
Use clean energy
-
•
Enhance environmental monitoring
-
•
Introduce the market mechanism into pollution control
-
•
Optimise urban planning and design
Healthy society
-
•
Expand health insurance coverage and improve reimbursement rates
-
•
Increase the number of people eligible for social welfare and provide financial assistance to people in need (people who are poor, handicapped, mentally diseased, homeless, or have lost their only child)
-
•
Strengthen care for elderly people
-
•
Increase education equity
-
•
Encourage social groups and volunteers to get involved
-
•
Enhance public safety of the city
-
•
Create jobs
-
•
Provide housing assistance to low-income families
-
•
Mediate interpersonal conflicts
Health service
-
•
Build a hierarchical structure for the health-care system
-
•
Invest in health-care facilities and personnel
-
•
Reduce medical costs and out-of-pocket expenditure for patients
-
•
Strengthen primary health care (family doctors, general practitioners, and community health centers)
-
•
Enhance public health management
-
•
Control chronic diseases
-
•
Control infectious diseases
-
•
Control mental diseases
-
•
Provide health services to migrants
-
•
Adopt modern technologies in health management, such as electronic health archives, telemedicine, mobile health, smart medicine, big data, telemedicine, and health information data centers
-
•
Increase the use of traditional Chinese medicine
-
•
Encourage investment in health care from private sectors
-
•
Develop health industry (medical centers, pharmaceutical industry, and nursing homes)
Healthy people
-
•
Promote an active lifestyle
-
•
Strengthen health services for women and children
-
•
Monitor physical status of the general public
-
•
Cultivate health culture: controlled smoking and drinking and healthy diet
Health culture
-
•
Health education through mass media
-
•
Health education through the school system
-
•
Health information through internet and mobile platforms
-
•
Produce publications of health information
-
•
Health promotion in public spaces (advertisements and billboards)
-
•
Build health information centres in communities
-
•
Organise events and competitions to promote health literacy
-
•
Disseminate health information through doctors and experts
-
•
Engage private sectors to cultivate a healthy culture
First, among the practices identified as most important for developing healthy cities globally is a strong emphasis on urban planning and design, including transit-oriented development, mixed land use, and pedestrian-friendly design, an emphasis that is echoed by leading international scholars.306, 307, 308, 309 In China, however, few cities explicitly state an intent to incorporate health into planning. A wealth of evidence suggests that poor urban planning and design are root causes for many urban health problems in China, including risks associated with the separation of living and work places, road injuries caused by pedestrian-unfriendly environments, and increased vulnerability to natural hazards. This situation represents a substantial gap in China's efforts to build healthy cities.
Second, healthy city development requires the involvement and empowerment of the private sector, NGOs and community groups, public–private partnerships, and citizens themselves, not only in decision making but at the start of projects. By contrast, cities in China have mostly taken a top-down approach in which the public is relegated to a secondary role. This situation reflects the historical cultural and governance context of urban China, where highly centralised decision making is emphasised and there is a reluctance to empower non-government decision makers. Although this means that city governments in China can rapidly adopt and disseminate policies, it also complicates the implementation of the broad engagement that is essential to good outcomes.
Third, best global practices require intersectoral cooperation and joint action as prerequisites for dealing with complex urban health issues and recommend working across sectors in the city government and engaging different levels of government agencies. Place-based intersectoral action for health has the highest potential to successfully implement Health in All Policies. Although the importance of intersectoral collaboration is widely recognised in China, a large proportion of practices that are used by cities to improve health still focus on health care, health promotion, and health management, which are all traditional health sector approaches. This situation reflects weak intersectoral collaboration in the development of action plans.
Fourth, best practices generally emphasise reduction of health inequity as a central target for all actions and suggest using tools—such as the Urban Health Index and Urban Health Equity Assessment and Response Tool (HEART)—to establish a baseline to monitor and evaluate progress. Although most cities in China specify various goals and metrics (eg, targets for pollution control, urban renewal, social welfare, and health care), the overall effect of these practices on urban health is rarely assessed and equity analysis is rarer still. Only a small number of surveyed cities had conducted a baseline population health survey; the absence of such activities will make it more difficult to assess the overall progress of urban development policies and programmes. Moreover, the survey also shows that uneven development is constraining progress. Although highly developed cities (such as Beijing, Shanghai, and Hangzhou) can address individual health needs and the social roots of health problems, cities in less developed zones (such as central and west China) still struggle to provide basic public services, such as garbage collection, public toilets, and basic medical services. It is very unlikely that these two types of cities can be fruitfully assessed with the same set of indicators.
Section 5. Recommendations
Together, these gaps represent a crucial barrier to the achievement of healthy cities in China. We make the following five recommendations, with full consideration of the unique character and structure of urban China and of experiences from diverse international settings.
Integrate health in all policies
Health in All Policies was proposed in China as early as 2013 and has since been reaffirmed in the Healthy China 2030 plan. The concept is considered fundamental to the future of health management in China; however, there are major barriers to its effective use in cities. Although there is a consensus that urban planning is an important way to facilitate healthy urbanisation and respond to global health challenges,310 the implementation of Health in All Policies will require the replacement of traditional modes of urban planning with more sophisticated planning architectures that are capable of achieving multiple health outcomes, capturing development co-benefits, and supporting policy development and implementation with indicators and evidence.311 Although recent changes in China's urbanisation strategy have allowed some integration of health into urban and regional planning, and thus support the implementation of Health in All Policies, specific changes are still needed in current planning guidance and methods.
In particular, the guiding principles of traditional urban planning need to be revised at national and city levels. At the national level, urban and regional planning can no longer operate as an isolated sector; it needs to be incorporated into an intersectoral policy framework that involves the entire society. This change will require collaboration between the government, civil society, and private sector to develop laws, regulations, and financial incentives that address the basic tenets of sustainable development, such as quality of life, health advancement, economic development, and environmental protection, in complementary and synergistic ways. Innovation and coordination needs to be promoted through the chain of national policy making, planning, and implementation. At the city level, urban planning needs to evolve from isolating and tackling individual elements of the urban system to addressing the whole system.306 Through urban and regional planning and design, a city needs to achieve horizontal coordination across sectors and with other cities and vertical coordination in the administrative hierarchy from the central government to regional and local governments.
To build healthy cities, the traditional urban planning system needs reformation. First, healthy city planning and assessments of health effects should become fundamental elements of urban planning. Consistent with the Healthy China 2030 plan, indicator systems and local standards for healthy city and town planning should be established. City and town plans need to incorporate sections dedicated to healthy city planning, which should specify goals and overall action plans through field investigations and analysis of archived materials. The healthy city planning indicator system should guide urban land use planning and regulatory plans. The goals should be included in new development and redevelopment projects, guiding the urban site plan, site design, building design, and landscape design; such considerations will underpin the legal basis for issuing planning permits.
Second, to truly implement Health in All Policies, the planning and design of healthy cities should favour urban development projects that reduce human exposure to pollution, facilitate physical activity, and incorporate clear measures of health and environmental effects.312 Wherever possible, the spatial layout of cities should be compact, open, and with small gridded blocks,313 with mixed use and multiple functions that help to reduce rush-hour traffic jams and reduce commute times.309 Urban environments should be designed in response to the local climate with abundant and well designed public spaces, walkways, and playgrounds that match the needs of neighbourhoods and cities. Site selection, planning, and construction of urban development projects should comply with environmental effect assessments and green building evaluations, and the health components of projects should be evaluated via the latest science and technology, through a mandatory, comprehensive process that assesses the effects on human health. Residential communities should accommodate people at different income levels, which in turn can promote employment and services across diverse communities, help to reduce social separation, and contribute to community care for elderly people.314
Third, the planning and design of healthy cities should contribute to improved urban resilience for public health emergencies, including through strengthened capacity for emergency preparation, response, mitigation, and recovery. Identification of the characteristics of potential public health emergencies in specific cities would facilitate the development of public health event scenarios that can be assessed formally through vulnerability analysis, allowing for estimates of the degree of expected damage, affected area, and spatiotemporal dynamics of the hazard and health effects. Management plans and strategies should be based on such assessments and resources should be allocated to reduce the public health burden of emergencies. With the rapid development of information technologies for health risk communication in urban environments, vulnerable subgroups should be identified and targeted communications protocols should be developed to ensure that information reaches these groups during an emergency.
Increase participation
A basic element of the Healthy Cities approach is broad public participation. Cities in China generally follow a model in which programmes and projects are led by government with participation by the public. Nevertheless, analysis of current practices suggests that the public passively receives all information on project planning and implementation. Channels need to be established to allow individuals, NGOs, and other social enterprises to voice their opinions and advocate for their priorities with respect to the health (and other) dimensions of urban projects, programmes, and their management. Strengthening bottom-up approaches in China would complement China's traditional top-down approach to governance and would encourage individuals to act more proactively to improve their health and the health of their communities. Increased public participation in health management is a high priority task in the Healthy China 2030 plan, laying the foundation for a more inclusive Healthy Cities project in China. Without an inclusive, broadly participatory approach that embraces and builds on local knowledge about health and environment, interventions for healthy, sustainable urban development are ultimately likely to fail.315
In practice, the achievement of broad participation will require substantial changes in procedures and fora for public participation. For example, community participation in the planning and selection of sites for health-care and service facilities should be encouraged, and planning and design processes for the redevelopment of urban communities should involve the public in decisions about land use and transportation. Representatives of a full set of stakeholders should be involved, rather than merely the subset whose views and interests match the government's views. Furthermore, the degree of participation should be enhanced, aiming for a standard of consensus building rather than coercive approaches that involve manipulation and therapy participation. Finally, a multiple-channel approach based on trust and transparency should replace the strict reliance on formal, top-down formulae for participation and early-stage public involvement should be required of developers and decision makers.316
Invest in community capacity building
Community participation is closely tied to community capacity building, which is defined as “the interaction of human capital, organisational resources, and social capital existing within a given community that can be leveraged to solve collective problems, and improve or maintain the wellbeing of that community”.317 Since the launch of economic reform, there has been a steady growth in registered NGOs, citizen groups, and private foundations in China. These represent potential partners in the coproduction of knowledge and codesign of interventions and policy, as intended in systems approaches for healthy cities. However, the participation of such communities in decision making is scarce and such an absence of transparency in decision-making processes has strong repercussions for health. The establishment of favourable policy and legal environments for and encouragement of investments toward community capacity building should be high priorities.
Community capacity building has been both a means and an end for health promotion in general318 and for the development of healthy cities in particular.319 Such capacity building should emphasise development of the community assets that are essential to allow urban dwellers to understand the complexities they face in pursuing healthy lives; in particular, risks and opportunities for physical and mental health across different urban population groups and cities. The improvement of health literacy is a central goal, particularly with respect to health education and communication, disease monitoring and reporting, health-care service evaluation, and healthy lifestyle promotion. This approach is essentially bottom-up with institutional support because the actions that are needed should be rooted in the communities of concern.
Community capacity building will lead to community empowerment, through which urban dwellers from different population groups and across different cities share the responsibilities and benefits related to healthy city programmes and policies. Public participation needs to be a part of health-care system reform and should be supported through urban planning and economic development. This aspect of community capacity building needs definite and consistent top-down institutional support so that applicable regulations, practices, and systems can be established. The community-centred nature of community capacity building for healthy cities in China requires various components to interact, including citizens, government and health management institutions, health service agencies, and actors (NGOs, private enterprises, and other social organisations) within the broader social and political environment.
Engage the private sector
In the 1980s in China, almost all urban workers were employed by state-owned or collectively-owned enterprises. By 2016, 80% of urban residents worked in the private sector, which also generates 60% of national GDP.30 The private sector has an enormous influence on the health of employees and communities and a responsibility to address its effect on urban health and the environment. Moreover, there is emerging evidence that corporate involvement and investment in public health can create valuable opportunities for business.320
In line with WHO recommendations,305 healthy cities in China should use the private sector's potential to provide health-related services, support the adoption of health-promoting behaviours, and contribute to initiatives that are relevant to public health. To date, private sector involvement in health care in China is still small. Just 20% of urban hospitals in 2008 were privately owned and the market share of private health insurance was not substantial.321 Just 12·3% of all medical treatment visits between January, and November, 2016 were to private sector facilities.322 New policies are needed to encourage the private sector to invest more in health facilities and provide health services, especially to serve marginalised populations. At the same time, relevant regulatory and supervisory mechanisms need to be strengthened to improve the quality and consistency of private sector health care.323 The private sector also has great potential for new investment in health technologies (eg, internet health and mobile health). For example, WeChat, which is the most popular messaging app in China, has been shown to be effective in health promotion, patient care, monitoring, diagnosis, and public health communication.324
The private sector should also invest more in employee health and occupational safety. This situation is win-win because improvements in health can benefit businesses through reduced health-care expenditures, increased revenue, and improved reputation. Although, in some cities, privately-owned businesses have been involved in health promotion campaigns, the scale of such programmes is limited and is essentially based on voluntary participation. Therefore, there is substantial room for expansion. The private sector can also contribute to promoting healthy behaviour among customers or consumers more broadly. For example, a recent collaboration between the public health agency and a restaurant chain in Beijing aimed to cut salt content in food, benefiting customers and boosting the image of the company as health-conscious (panel 11 ).
Panel 11. Xicheng district, Beijing—engage the private sector to promote healthy diet.
Qingfeng Steamed Stuffed Buns Restaurant is a restaurant chain that is famous for its Beijing local food, especially steamed stuffed buns. The restaurant became even more popular after President Xi Jinping paid an unexpected visit to one of its stores and ordered a plate of famous buns for lunch in 2013. The Center for Disease Control and Prevention in Xicheng district started to work with the Qingfeng restaurant chain to reduce the use of salt in its buns in 2013. After experiments to find a recipe that decreased salt content by 10% but did not compromise the taste, Qingfeng began to sell a low-salt version of steamed buns stuffed with shredded seafood in 2013. In 2015, Qingfeng added another low-salt version of steamed buns stuffed with bamboo shoots and sauced pork. Both dishes have sold better than the regular versions. In 2015, 235 Qingfeng stores in Beijing started to offer free low-salt buns to selected elderly people. Qingfeng also use in-store advertisements, WeChat, and the company website to promote reduced salt consumption to their customers.
To build on the success of Qingfeng, Huatian Catering Group—which owns Qingfeng—now works with public health specialists to promote low-salt, low-oil, and low-sugar food in all its restaurants. The Center for Disease Control and Prevention in Xicheng joined forces with the Association of Catering Business in Xicheng to promote healthy restaurant foods. So far, 35 restaurants and cafeterias have been certified for their provision of healthy foods.
Collaborations between restaurants and public health agencies in China are facilitated by the power of public agencies to issue health permits to restaurants. However, in this case, the public health agency in Xicheng district went beyond its role as an administrator and helped restaurants to develop healthy food. There are many other ways in which public health agencies in China can use upstream preventions and interventions rather than focusing on downstream interventions.
The private sector should also be accorded more responsibility for environmental management and harm reduction. Under the 13th 5-year plan, Chinese businesses will be required to cut water and energy consumption, air pollutants, and carbon dioxide emissions. Industries that generate a disproportionate amount of pollution relative to output need to increase efficiency. Increased accountability in the private sector will lead to improved urban health.
The motivation of private sector involvement in building healthy cities will require effort from government, business owners, and employees and customers. City governments can apply financial and policy tools, such as tax credits, favourable loan and land policies, and purchase of services, to encourage the private sector to invest in health care and the health industry and to participate in health promotion. Employees and customers, once equipped with better knowledge on occupational health and product safety, can become a driving force for improved health. Business owners should embrace the opportunities that accompany actions to improve the health of employees, customers, and the environment. Third-party assessment reports that rank the engagement of businesses in urban health can be good incentives in this effort.
Promote intersectoral actions
One of the most serious challenges to the assurance of urban health is the formal segregation of design and management tasks within cities. The complexity of causal feedbacks across sectoral boundaries can lead to ineffective responses and unintended consequences if actions address only isolated parts of a larger problem. Further, health is often narrowly conceptualised in terms of access to medical or public health services and quality of care, rather than as the result of interacting social, environmental and economic systems that act in a particular context. This characterisation contributes to misunderstanding of the health consequences of actions in other sectors. A short-term vision for decision making can add to this problem. Decisions about urban design or management based on short-term considerations can fix features of the built environment but might continue to generate health problems in the long term.
All of these situations have been observed in Chinese cities. Health is often not a priority for municipal leaders. There are scarce incentives for non-health sector agencies to contribute and changes in leadership often make it difficult to maintain intersectoral actions on health. To be successful in the pursuit of intersectoral actions health, cities in China need to recognise the necessity of whole-of-government and whole-of-society approaches.325 For example, cites need to break the barrier of information sharing among different government sectors (panel 12 ). This recognition then needs to cause institutional changes to facilitate intersectoral collaboration, including formal mechanisms to ensure their long-term sustainability. Finally, cities should provide incentives for intersectoral collaboration.
Panel 12. Yichang—break the barrier to information sharing among different sectors.
Yichang is a city in Hubei province. As of 2015, there are 1·28 million registered residents in its urban districts. The city started to manage its five urban districts using a grid system in December, 2010. The 112 urban neighbourhoods were divided into 1421 grids, with each grid containing about 200–300 households. Grids are monitored by full-time staff who are responsible for reporting anything that happens in their grid directly to the city information hub through a specialised mobile application. The information hub is linked to different databases in more than 30 departments and offices in the municipal government. All relevant databases are updated once new information comes in.
The Health Management Analysis Center is a component of the hub that started to collect health data in 2015. It has connections to 173 health-care facilities and 368 pharmacies. So far, the centre has built 1·3 million copies of electronic archives that, in real-time, collect patients' health information, including physical exam records, X-ray images, prescriptions, and other health and medical information. Because the centre is linked to databases managed by the Public Security Department and the Urban Housing and Construction Department through the hub, it can trace each person to his or her home. This feature has been very helpful in the prevention and control of diseases and the allocation of medical resources. The 1421 grid monitor staff help the centre to collect health information (such as mental disorders and emergencies) as it occurs in the grid on a real-time basis and conduct specific surveys on topics, such as health insurance coverage.
The successful information sharing among different sectors in Yichang can be attributed to the commitment of city leaders to information technology, its centralised political system, and its relatively small population size. The grid system and the real-time information sharing from health-care facilities and pharmacies ensures that there are no gaps in health information at sub-city levels. Although this approach has merits, there are concerns about privacy issues and the safety of personal information. There is an urgent need for laws and regulations that clearly define the boundary and responsibility of the government, health services, and any other third-party entities on the collection and use of personal health information in China.
In addition, a mechanism is urgently needed to allow the health effects of urban management to be assessed and controlled, which will require changes in governance structures and management procedures. Currently, each city's Patriotic Health Campaign Committee is responsible for activities related to the Healthy Cities movement. The committee consists of members from different municipal departments and is led by a vice mayor or mayor, but its actions are often run by the local health family and planning commission. This arrangement makes sense when health is narrowly defined as access to medical or public health services and quality of care, since the local health family and planning commission is responsible for these functions. However, the need for intersectoral actions in building healthy cities renders such arrangements obsolete; the Patriotic Health Campaign Committee office, when subsumed within the health family and planning commission, does not have the required authority to coordinate multi-sectoral action for health. To resolve this, responsibility for the administration of the Patriotic Health Campaign Committee should be transferred from the local health family and planning commission to the mayor's office. More importantly, the committee should review major policies and plans for urban development and management, conduct formal assessments of the health effects where appropriate, and decide whether candidate policies and projects should be revised to reduce long-term negative effects on health.
To maintain the sustainability of intersectoral efforts, municipal governments should integrate actions to build healthy cities into long-term governmental plans and legal and regulatory frameworks. Some cities have already begun such work, including the Beijing municipal government's Healthy Beijing People: 10-year action plan for promoting people's health (2009–2018) or Hangzhou's 13th 5-year plan for the construction of a Healthy City in Hangzhou in 2016. However, most cities do not have a long-term plan for the development of a healthy city.
It would be naive to assume that intersectoral actions will automatically emerge from the establishment of an institutional mechanism. Non-health sectors need to be motivated to address health issues. The success of the Hygienic Cities movement offers some valuable lessons. Among the keys to its success were the competitive campaigns organised by the National Patriotic Health Campaign Committee. Although the requirements for National Hygienic City status are stringent, cities are willing to invest substantial resources to compete for this recognition. In addition to reputational advantages for the city itself, attainment of the title is one factor recognised during the assessment and promotion of city officials, thus the project helps to motivate strong leadership.326 A well-organised competitive campaign is also linked to the breaking of intersectoral barriers and the enhancement of public awareness and involvement.327 Similarly, a reward system should be implemented to incentivise officials at various levels to seek intersectoral collaborations when building healthy cities. Most importantly, city performance in terms of health should be incorporated into the criteria used for the promotion of mayors, as assessed through the indicators discussed.
A lesson fromHealthy Cities projects in Europe is that strong local leadership and policy change can be driven by international collaboration. International recognition can be a strong motivating factor for cities and international linkages can provide insights to and generate innovation for all participants.328 Chinese cities should actively participate in the international network of healthy cities, taking leading roles where feasible.
Set local goals for 2030 and assess progress periodically
Building healthy cities in China serves to improve the health of people in participating cities and to achieve the goals specified in the Healthy China 2030 plan. As discussed, China's national health goals cannot be achieved without addressing the health of the 71% of the population that live in urban areas. Actions should therefore address both goals. Cities in China today vary widely in the extent to which they have taken actions towards the development of healthy cities and the degree to which they meet the health needs of their citizens. However, all cities will eventually need—at a minimum—to meet national targets by 2030, which will require short-term and mid-term goals and plans that are specific to each city.
To date, goals specified by cities in the pilot Healthy Cities project often reflect specific actions that address social and environmental determinants of urban health but not overall progress for health. For example, most cities set specific targets for the provision of sports facilities in cities, such as exercise facilities within a 15-min walk of residences. Although the attainment of this target certainly improves the likelihood that citizens will exercise, the numbers of people who actually exercise and meet fitness goals is generally unknown. Furthermore, too many specific targets will make it difficult for politicians and the public to easily gauge progress. Therefore, targets should be selected on the basis of an understanding of urban systems, prioritising variables that provide the most information about the city's ability to foster sustainable health outcomes.
Because all Chinese cities will ultimately need to meet the goals specified in the Healthy China 2030 plan, we suggest that these are used as the minimum long-term goals for building healthy cities. Some cities, like Shanghai and Suzhou, have already achieved some of these goals and can therefore specify higher targets. Baseline health surveys are needed to allow short-term and mid-term goals to be set on the basis of each cities' specific status and available resources. This process should be combined with a systematic analysis of existing strengths and gaps in health management to ensure action plans are tailored to local needs.
Regular assessments of progress should follow the adoption of goals and be based on a combination of self-evaluation and third-party evaluation. The indicator system for healthy cities developed by the National Patriotic Health Campaign Committee provides detailed data, allowing health experts to identify drivers of progress or hurdles. However, because the system is not easily understood by the public, a simplified indicator system is needed. As a starting point, we suggest a system based on three indicators: life expectancy, premature death rate from chronic diseases, and a composite index derived from the WHO HEART tool. The first two are included in the Healthy China 2030 targets and reflect the status of health and of the health-care system, respectively, in metrics that are easy to understand. Both indicators are monitored regularly by the Disease Surveillance Points System so no extra effort will be required. The third indicator reflects the status of health inequity. Since health for all is a guiding principle in the Healthy China 2030 plan and an international focus, it is key that progress in this area be measured. Most indicators in the WHO HEART tool are also used in the indicator system for healthy cities in China and should therefore be easy to attain. This simplified indicator system can be used to evaluate the performance of mayors and inform the public on progress made toward health goals.
High-quality data are a precondition for realistic goals and the measurement of progress. Although China has built strong surveillance networks to monitor diseases, risk factors, and the health history of citizens, data availability at city level is still poor and the quality of data generated by different networks is highly variable.243 Data at the sub-city level are also crucial,305 but have rarely been available in urban China. Monitoring networks are urgently needed in cities to provide timely and accurate information on the status of urban environments and resident health. Strengthened government-operated monitoring networks should be complemented by collaboration with private companies on big-data technologies. For example, diseases in cities can in some cases be tracked using internet query data, which was the case for hand, foot, and mouth disease in Chengdu (figure 14 , appendix). Data from governmental networks can be integrated with data from wearable sensors, mobile platforms, the internet, and remote sensing to establish an urban health monitoring network that is multi-scale, long lasting, and real time.
Figure 14.
Hand, foot, and mouth disease in Chengdu, 2013–16
Weekly number of cases reported to the Sichuan Center for Disease Control and Prevention.
Enhance research and education on healthy cities
The magnitude of the health challenges facing Chinese cities is much larger than in Europe and North America because of the relative size of its urban population and rate of socioeconomic change. New thinking and innovative ideas will be needed to successfully apply the Healthy Cities approach in this context; existing methods need to be rigorously assessed before large-scale adoption. In particular, research based on integrated monitoring through modern technologies, interdisciplinary studies, and quantitative modelling will need to be further advanced to support the development of healthy cities.
It will be extremely useful for cities to understand the health effects of management measures that have been or will be taken. However, the prediction of potential health effects or attribution of changes to particular policies and actions is rarely straightforward. In Europe, the realist evaluation framework has been proposed as a way to tackle the complex evaluation of the health effects and outcomes of the Healthy Cities movement.329 As discussed, we propose an interdisciplinary approach that is based on both qualitative and quantitative analyses of future scenarios and a consideration of demographical, socioeconomical, environmental, and political conditions. Individual environmental exposure and physiological indicators at the city level, effects of environmental factors on the morbidity and mortality of urban population, and risks of disease transmission via population migration networks on a global scale should be comprehensively analysed with the support of advanced models (eg, to integrate cities as a module into the Earth system simulator). A better understanding of the underlying mechanisms and causal systems that affect urban health will lead to improved policy making and forecasting of the health effects and outcomes of management measures. In addition, more systematic measurement and assessment of all dimensions of urban health on local, regional, and global scales would provide unbiased data for forecast models and support evidence-based policy making. The Chinese Government should increase investment in research and development and form partnerships with universities, research institutes, and the private sector to enhance research in these fields.
Finally, urban planners and public health practitioners are fundamental to the success of the Healthy Cities movement in China; traditional training in these fields needs to evolve to meet current needs. Curricula for urban planning programmes in higher education institutions should expand to include topics related to the interactions of society, environment, economy, and health. Urban planning elements as diverse as housing, transportation, information technology development, and land use can affect health through their influence on food access, physical activity, housing quality, health information, access to care, transport choice and affordability, school locations, social equity, clean air and water, and other factors.330 Therefore, a multi-scale, cross-sectoral vision of urban health should be built into city and regional planning programmes to ensure that urban planners are fully aware of the various elements required for a healthy city. If health cannot be given proper consideration in the design and planning of districts, communities, individual buildings, and urban infrastructural elements (such as roads), the healthy functioning of an entire city is unlikely to be achieved. A healthy city should also have the capacity to shield its citizens from potential health risks. Correspondingly, the curricula of public health programmes should provide the skills and knowledge needed to work together with urban planners to jointly develop strategies that address the root causes of poor health, rather than simply targeting specific diseases or individual behaviours.315
Looking forward
Urbanisation in China will continue to advance in years to come, sustained by policies that favour sustainable urban development and economic initiatives centred in cities. As long as the unprecedented pace and scale of urban growth continues, the health and wellbeing of millions of urban residents and the sustainability and livability of cities in China will depend on decisive action to secure and strengthen the Chinese Dream for future generations. Because of their dominant role in China's political, social, and economic systems and as the focus for scientific and technological innovation, cities are key to the successful control of health challenges both within and beyond city boundaries. In the words of Jaime Lerner, “cities are not the problem; cities are the solution”.329, 331 Four decades ago, as a result of health innovations like barefoot doctors and community health care centres, China improved the health of millions of rural dwellers, thus providing the world with a model for good health at low cost.332 Today, the drive to develop healthy cities in China and create the world's first ecocivilisation is set in the context of an unprecedented global push for sustainable development, in the form of the Sustainable Development Goals and the paradigm-shifting idea of planetary health. These powerful ideas reinforce and support one another and give us confidence that cities in China can face the aforementioned challenges and once again lead the world in securing sustainable health for all.
Acknowledgments
Acknowledgments
We thank WHO Beijing Office for arranging and providing meeting spaces. We thank staff from the Department of Earth System Sciences, Tsinghua University for providing logistical support for the first and third commission meetings in Tsinghua University. PG was supported by grants from the Cyrus Tang Foundation and the Cross-strait Tsinghua Research Institute. BX was supported by a grant from the Ministry of Science and Technology of China (2016YFA0600104). JY was supported by a grant from the Chinese Scholar Council (201706215005). JH was supported by research and development funds from the China National Engineering Research Center for Human Settlements. WCh was supported by a grant from the Ministry of Science and Technology of China (2014FY121100). M-PK was supported by a grant from the National Natural Science Foundation of China (41529101), a grant from the University of Illinois Research Board, and Grant 1-ZE24 (Project of Strategic Importance) from the Hong Kong Polytechnic University. PS was supported by the National Key Research and Development Program (2016YFA0602404). KKYC was supported by a grant from the Ministry of Science and Technology of China (2016YFA0600104). NC was supported by Cyrus Tang Foundation. YiZhang was supported by the Natural Science Foundation of China (51420105010 and 51521005). Finally, we thank the Office of National Patriotic Health Campaign Committee of China for their help in organising the survey and the 36 cities for participation.
Contributors
PG, JY, BX, and YoZhang conceived and led the preparation of the report. JY, QC, ZSu, KKYC, HZ, YZhao, NC, and XuL did the literature search. PG, BX, JY, QC, HZ, KKYC, ZSu, NC, WZ, YB, WCa, WCh, HH, PS, ZSh, XiaL, and YoZhang were involved in data collection, analysis, and interpretation. JY, QC, HZ, KKYC, YZhao, XM, WCh, QZ, and HH prepared the figures. JY, JGS, JVR, QC, HZ, KKYC, ZSu, JB, WCa, EYYC, WF, HF, JH, HH, JSJ, PJ, XJ, M-PK, TL, XigL, SL, LL, QL, YLu, YLuo, JSu, TW, CY, QZ, BS, YY, YiZhang, BX, and PG wrote and revsed this work. PG coordinated the Commission. All authors participated in study design and discussion.
Declaration of Interests
JSJ was the Asia editor of The Lancet between May and November, 2017. All other authors declare no competing interests.
Supplementary Material
References
- 1.Yang G, Liu S. Analysis on the average life expectancy in population of China based on Bayesian random-effect model. Stat Res. 2015;32:95–100. [Google Scholar]
- 2.Gong P, Liang S, Carlton EJ. Urbanisation and health in China. Lancet. 2012;379:843–852. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministry of Civil Affairs Results of the fourth national survey of urban and rural elderly in China. 2015. http://www.mca.gov.cn/article/zwgk/mzyw/201610/20161000001974.shtml (accessed Feb 8, 2018).
- 4.Wang H, Naghavi M, Allen C, the GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang H, Yu Y. Increasing health inequality in China: an empirical study with ordinal data. J Econ Inequal. 2016;14:41–61. [Google Scholar]
- 6.Meng Q, Yue D, Ruan S, Cheng G. Peking University China Center for Health Development Studies; Beijing: 2014. Report on comprehensive evaluation of National Hygienic Cities. [Google Scholar]
- 7.Ministry of Human Resources and Social Security Annual statistical bulletin on human resources and social security development in 1998. 2006. http://www.mohrss.gov.cn/SYrlzyhshbzb/zwgk/szrs/tjgb/200602/t20060207_69891.html (accessed Feb 8, 2018).
- 8.Ministry of Human Resources and Social Security Annual statistical bulletin on human resources and social security development in 2016. 2017. http://www.mohrss.gov.cn/SYrlzyhshbzb/zwgk/szrs/tjgb/201705/t20170531_271671.html (accessed Feb 8, 2018).
- 9.Wang Y, Wang H, Zhang X, Li J, Long Q. Analysis of the practice and development strategies of healthy cities in China. In: Wang H, Xie S, Sheng J, editors. Annual report on healthy city construction in China (2016) Social Science Academic Press; Beijing: 2016. [Google Scholar]
- 10.Chen Q, Dietzenbacher E, Los B. The effects of ageing and urbanisation on China's future rural and urban populations. Asian Popul Stud. 2017;13:172–197. [Google Scholar]
- 11.Central Committee of Chinese Communist Party. State Council . Government of the People's Republic of China; Beijing: 2016. The Plan for Healthy China 2030. [Google Scholar]
- 12.Bircher J, Kuruvilla S. Defining health by addressing individual, social, and environmental determinants: new opportunities for health care and public health. J Public Health Policy. 2014;35:363–386. doi: 10.1057/jphp.2014.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO Constitution of the World Health Organization. 1946. http://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf?ua=1 (accessed Feb 8, 2018).
- 14.United Nations Transforming our world: the 2030 agenda for sustainable development. 2015. https://sustainabledevelopment.un.org/post2015/transformingourworld (accessed Feb 8, 2018).
- 15.Watson B, Chuang T. Columbia University Press; New York, NY: 1996. Basic writings. [Google Scholar]
- 16.Luo X. 1st edn. China Press of Traditional Chinese Medicine; Beijing: 2009. Huangdi Neijing. [Google Scholar]
- 17.Wang CC, Lin JD, Chen LL. [Personal health maintenance: the perspective of traditional Chinese medicine] Hu Li Za Zhi. 2010;57:10–15. [PubMed] [Google Scholar]
- 18.Szreter S. Economic growth, disruption, deprivation, disease, and death: on the importance of the politics of public health for development. Popul Dev Rev. 1997;23:693–728. [Google Scholar]
- 19.Xia Y, Guan D, Jiang X, Peng L, Schroeder H, Zhang Q. Assessment of socioeconomic costs to China's air pollution. Atmos Environ. 2016;139:147–156. [Google Scholar]
- 20.Li L, Lei Y, Pan D, Yu C, Si C. Economic evaluation of the air pollution effect on public health in China's 74 cities. Springerplus. 2016;5:402. doi: 10.1186/s40064-016-2024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y, Zeng X, Liu J. Can China achieve a one-third reduction in premature mortality from non-communicable diseases by 2030? BMC Med. 2017;15:132. doi: 10.1186/s12916-017-0894-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bloom DE, Cafiero-Fonseca ET, McGovern ME. The macroeconomic impact of non-communicable diseases in China and India: Estimates, projections, and comparisons. J Econ Ageing. 2014;4:100–111. [Google Scholar]
- 23.Dataway Report on urban life quality indicators in China in 2015. Mark Res. 2016;3:10–12. [Google Scholar]
- 24.Liu X, Zhu H, Hu Y. Public's health risk awareness on urban air pollution in Chinese megacities: the cases of Shanghai, Wuhan and Nanchang. Int J Environ Res Public Health. 2016;13:E845. doi: 10.3390/ijerph13090845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bi J, Greene G, Ma Z. China's development and environmental risk management. In: Kasperson RE, editor. Risk conundrums. Routledge; London and New York: 2017. pp. 112–126. [Google Scholar]
- 26.Zheng S, Kahn ME, Sun W, Luo D. Incentives for China's urban mayors to mitigate pollution externalities: the role of the central government and public environmentalism. Reg Sci Urban Econ. 2014;47:61–71. [Google Scholar]
- 27.Central Committee of Chinese Communist Party. State Council . Government of the People's Republic of China; Beijing: 1997. The decision on reform and development in health. [Google Scholar]
- 28.National Bureau of Statistics Statistics data. 2016. http://www.stats.gov.cn/tjsj/ (accessed Feb 8, 2018).
- 29.National Bureau of Statistics Census data. 2016. http://www.stats.gov.cn/tjsj/pcsj/ (accessed Feb 8, 2018).
- 30.Li B, Chen C, Hu B. Governing urbanization and the New Urbanization Plan in China. Environ Urban. 2016;28:515–534. [Google Scholar]
- 31.Deng Y, Liu S, Cai J, Lu X, Nielsen CP. Spatial pattern and its evolution of Chinese provincial population: methods and empirical study. J Geogr Sci. 2015;25:1507–1520. [Google Scholar]
- 32.National Bureau of Statistics . China Statistics Press; Beijing: 2015. China statistical yearbook 2015. [Google Scholar]
- 33.National Bureau of Statistics Statistical method of defining urban and rural areas. 2008. http://www.stats.gov.cn/statsinfo/auto2073/201310/t20131031_450613.html (accessed Feb 8, 2018).
- 34.Fang C, Yu D. Urban agglomeration: an evolving concept of an emerging phenomenon. Landsc Urban Plan. 2017;162:126–136. [Google Scholar]
- 35.Ministry of Housing and Urban-Rural Development 2015 report on the statistics of urban and rural development. 2016. http://www.mohurd.gov.cn/xytj/tjzljsxytjgb/tjxxtjgb/201607/t20160713_228085.html (accessed Feb 8, 2018).
- 36.Wang L, Li C, Ying Q. China's urban expansion from 1990 to 2010 determined with satellite remote sensing. Chin Sci Bull. 2012;57:2802–2812. [Google Scholar]
- 37.National Bureau of Statistics . China Statistics Press; Beijing: 2015. China statistical yearbook 2015. [Google Scholar]
- 38.Qin B, Zhang Y. Note on urbanization in China: urban definitions and census data. China Econ Rev. 2014;30:495–502. [Google Scholar]
- 39.National Bureau of Statistics . National Statistics Bureau of the People's Republic of China; Beijing: 2016. Status of converting migrant workers into city residents: report of mornitoring the dynamic process of converting migrant workers into city residents in 2015. [Google Scholar]
- 40.Zhang J, Cai Y. Forecasting China's labor supply and demand and the unemployment structure in the 13th five-year-plan period. Popul Res. 2016;40:38–56. [Google Scholar]
- 41.Shi Y, Xu N. Analysis of influence of population aging on urban economic growth. Open Cybernetics Syst J. 2015;9:2847–2852. [Google Scholar]
- 42.Xie B, Zhou J, Luo X. Mapping spatial variation of population aging in China's mega cities. J Maps. 2016;12:181–192. [Google Scholar]
- 43.Cai Y. China's below-replacement fertility: government policy or socioeconomic development? Popul Dev Rev. 2010;36:419–440. doi: 10.1111/j.1728-4457.2010.00341.x. [DOI] [PubMed] [Google Scholar]
- 44.Zeng Y, Hesketh T. The effects of China's universal two-child policy. Lancet. 2016;388:1930–1938. doi: 10.1016/S0140-6736(16)31405-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiang Q, Yang S, Sánchez-Barricarte JJ. Can China afford rapid aging? Springerplus. 2016;5:1107. doi: 10.1186/s40064-016-2778-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fang C, Zhou C, Gu C, Chen L, Li S. A proposal for the theoretical analysis of the interactive coupled effects between urbanization and the eco-environment in mega-urban agglomerations. J Geogr Sci. 2017;27:1431–1449. [Google Scholar]
- 47.Li Y, Wu F. The transformation of regional governance in China: the rescaling of statehood. Prog Plann. 2012;78:55–99. [Google Scholar]
- 48.van der Kamp D, Lorentzen P, Mattingly D. Racing to the bottom or to the top? Decentralization, revenue pressures, and governance reform in China. World Dev. 2017;95:164–176. [Google Scholar]
- 49.Wu F. China's emergent city-region governance: a new form of state spatial selectivity through state-orchestrated rescaling. Int J Urban Reg Res. 2017;40:1134–1151. [Google Scholar]
- 50.Satterthwaite D, Mitlin D. Recognising the potential of cities. BMJ. 2011;343:d7979. doi: 10.1136/bmj.d7979. [DOI] [PubMed] [Google Scholar]
- 51.National Health and Family Planning Commission . Peiking Union Medical College Press; Beijing, China: 2016. China statistical yearbook of health and family planning 2016. [Google Scholar]
- 52.Zhou S, Deng L, Kwan MP, Yan R. Social and spatial differentiation of high and low income groups' out-of-home activities in Guangzhou, China. Cities. 2015;45:81–90. [Google Scholar]
- 53.Zhou S, Miao X, Kwan MP. Ageing in place and ageing with migration in the transitional context of urban China: a case study of ageing communities in Guanzhou. Habitat Int. 2015;49:177–186. [Google Scholar]
- 54.Li Y. Healthcare reform in urban China. World Health Popul. 2010;12:23–29. [PubMed] [Google Scholar]
- 55.Blumenthal D, Hsiao W. Lessons from the East—China's rapidly evolving health care system. N Engl J Med. 2015;372:1281–1285. doi: 10.1056/NEJMp1410425. [DOI] [PubMed] [Google Scholar]
- 56.Zhou M, Wang H, Zhu J. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 57.Wu M. Analysis of political factors affecting health policy making and implementation in China. Chin J Health Pol. 2008;1:54–57. [Google Scholar]
- 58.Zhou Q. Impact of urbanization on public health expenditure. J Guangzhou City Polytechnic. 2017;11:27–37. [Google Scholar]
- 59.Tobe RG, Xu L, Song P, Huang Y. The rural-to-urban migrant population in China: gloomy prospects for tuberculosis control. Biosci Trends. 2011;5:226–230. doi: 10.5582/bst.2011.v5.6.226. [DOI] [PubMed] [Google Scholar]
- 60.Muldavin J. Using cities to control the countryside: an alternative assessment of the China National Human Development Report 2013. Dev Change. 2015;46:993–1009. [Google Scholar]
- 61.Lozano R, Naghavi M, Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.National Center for Cardiovascular Diseases . National Center for Cardiovascular Diseases, People's Republic of China; Beijing: 2015. Report on cardiovascular diseases in China (2014) [Google Scholar]
- 64.Chen W, Zheng R, Baade PD. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 65.Chen WQ, Zheng RS, Zeng HM, Zhang SW, Zhao P, He J. Trend analysis and projection of cancer incidence in China between 1989 and 2008. Zhonghua Zhong Liu Za Zhi. 2012;34:517–524. doi: 10.3760/cma.j.issn.0253-3766.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 66.Bode AM, Dong Z, Wang H. Cancer prevention and control: alarming challenges in China. Natl Sci Rev. 2016;3:117–127. doi: 10.1093/nsr/nwv054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Guo P, Huang ZL, Yu P, Li K. Trends in cancer mortality in China: an update. Ann Oncol. 2012;23:2755–2762. doi: 10.1093/annonc/mds069. [DOI] [PubMed] [Google Scholar]
- 68.Ding B, DiBonaventura M, Karlsson N, Ling X. Asthma-chronic obstructive pulmonary disease overlap syndrome in the urban Chinese population: prevalence and disease burden using the 2010, 2012, and 2013 China National Health and Wellness Surveys. Int J Chron Obstruct Pulmon Dis. 2016;11:1139–1150. doi: 10.2147/COPD.S103873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sha L, Shao M, Liu C. The prevalence of asthma in children: a comparison between the year of 2010 and 2000 in urban China. Zhonghua Jie He He Hu Xi Za Zhi. 2015;38:664–668. [PubMed] [Google Scholar]
- 70.Dong GH, Qian Z, Fu Q. A Multiple Indicators Multiple Cause (MIMIC) model of respiratory health and household factors in Chinese children: the seven Northeastern cities (SNEC) study. Matern Child Health J. 2014;18:129–137. doi: 10.1007/s10995-013-1245-6. [DOI] [PubMed] [Google Scholar]
- 71.Pan C, Shang S, Kirch W, Thoenes M. Burden of diabetes in the adult Chinese population: A systematic literature review and future projections. Int J Gen Med. 2010;3:173–179. doi: 10.2147/ijgm.s6343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xu Y, Wang L, He J, the 2010 China Noncommunicable Disease Surveillance Group Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310:948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 73.Wang L, Wang L, Zhou M. Military Medical Science Press; Beijing: 2016. Report on chronic disease risk factor surveillance in China (2013) [Google Scholar]
- 74.Wang L, Gao P, Zhang M. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317:2515–2523. doi: 10.1001/jama.2017.7596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.WHO . World Health Organization; Geneva: 2016. Ambient air pollution: a global assessment of exposure and burden of disease. [Google Scholar]
- 76.Ministry of Environmental Protection 2016 report on the state of environment in China. 2017. http://english.mep.gov.cn/Resources/Reports/soe/ReportSOE/201709/P020170929573904364594.pdf (accessed Feb 8, 2018).
- 77.Mijling B, Ding J, Koukouli ME. Cleaning up the air: effectiveness of air quality policy for SO 2 and NOx emissions in China. Atmos Chem Phys. 2017;17:1775–1789. [Google Scholar]
- 78.Wang J, Zhao B, Wang S. Particulate matter pollution over China and the effects of control policies. Sci Total Environ. 2017;584–85:426–447. doi: 10.1016/j.scitotenv.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 79.Wang S, Xing J, Zhao B, Jang C, Hao J. Effectiveness of national air pollution control policies on the air quality in metropolitan areas of China. J Environ Sci (China) 2014;26:13–22. doi: 10.1016/s1001-0742(13)60381-2. [DOI] [PubMed] [Google Scholar]
- 80.Verstraeten WW, Neu JL, Williams JE, Bowman KW, Worden JR, Boersma KF. Rapid increases in tropospheric ozone production and export from China. Nat Geosci. 2015;8:690–695. [Google Scholar]
- 81.National Bureau of Statistics, Ministry of Environmental Protection . China Statistics Press; Beijing: 2003–2012. China statistical yearbook of environment (2003–2012) [Google Scholar]
- 82.Han L, Zhou W, Pickett STA, Li W, Li L. An optimum city size? The scaling relationship for urban population and fine particulate (PM(2.5)) concentration. Environ Pollut. 2016;208:96–101. doi: 10.1016/j.envpol.2015.08.039. [DOI] [PubMed] [Google Scholar]
- 83.Liu F, Zhang Q, Tong D. High-resolution inventory of technologies, activities, and emissions of coal-fired power plants in China from 1990 to 2010. Atmos Chem Phys. 2015;15:13299–13317. [Google Scholar]
- 84.Wang Q, Li R. Journey to burning half of global coal: trajectory and drivers of China's coal use. Renew Sustain Energy Rev. 2016;58:341–346. [Google Scholar]
- 85.Chen W, Xu R. Clean coal technology development in China. Energy Policy. 2010;38:2123–2130. [Google Scholar]
- 86.International Energy Agency . International Energy Agency; Paris: 2016. World energy outlook 2016 executive summary. [Google Scholar]
- 87.Wu X, Wu Y, Zhang S, Liu H, Fu L, Hao J. Assessment of vehicle emission programs in China during 1998-2013: Achievement, challenges and implications. Environ Pollut. 2016;214:556–567. doi: 10.1016/j.envpol.2016.04.042. [DOI] [PubMed] [Google Scholar]
- 88.Zhang Q, Streets DG, Carmichael GR. Asian emissions in 2006 for the NASA INTEX-B mission. Atmos Chem Phys. 2009;9:5131–5153. [Google Scholar]
- 89.Shi S, Chen C, Zhao B. Modifications of exposure to ambient particulate matter: Tackling bias in using ambient concentration as surrogate with particle infiltration factor and ambient exposure factor. Environ Pollut. 2017;220:337–347. doi: 10.1016/j.envpol.2016.09.069. [DOI] [PubMed] [Google Scholar]
- 90.Zhang Y, Mo J, Weschler CJ. Reducing health risks from indoor exposures in rapidly developing urban China. Environ Health Perspect. 2013;121:751–755. doi: 10.1289/ehp.1205983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Du Z, Mo J, Zhang Y. Risk assessment of population inhalation exposure to volatile organic compounds and carbonyls in urban China. Environ Int. 2014;73:33–45. doi: 10.1016/j.envint.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 92.Wang L, Zhao B, Liu C, Lin H, Yang X, Zhang Y. Indoor SVOC pollution in China: a review. Chin Sci Bull. 2010;55:1469–1478. [Google Scholar]
- 93.Li Q, Jiang J, Wang S. Impacts of household coal and biomass combustion on indoor and ambient air quality in China: Current status and implication. Sci Total Environ. 2017;576(suppl C):347–361. doi: 10.1016/j.scitotenv.2016.10.080. [DOI] [PubMed] [Google Scholar]
- 94.Chen W, Zheng R, Zeng H, Zhang S. Epidemiology of lung cancer in China. Thorac Cancer. 2015;6:209–215. doi: 10.1111/1759-7714.12169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chen R, Yin P, Meng X. Fine particulate air pollution and daily mortality: a nationwide analysis in 272 Chinese cities. Am J Respir Crit Care Med. 2017;196:73–81. doi: 10.1164/rccm.201609-1862OC. [DOI] [PubMed] [Google Scholar]
- 96.Chen X, Shao S, Tian Z, Xie Z, Yin P. Impacts of air pollution and its spatial spillover effect on public health based on China's big data sample. J Clean Prod. 2017;142:915–925. [Google Scholar]
- 97.Yang J. Heterogeneity analysis of the relationship between economic growth and water environmental pollution in Beijing, Tianjin and Zhengzhou of China. Nat Environ Pollut Technol. 2016;15:51–58. [Google Scholar]
- 98.Pal A, He Y, Jekel M, Reinhard M, Gin KY. Emerging contaminants of public health significance as water quality indicator compounds in the urban water cycle. Environ Int. 2014;71:46–62. doi: 10.1016/j.envint.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 99.Development Research Center of the State Council, The World Bank . World Bank Publications; Beijing: 2014. Urban China: toward efficient, inclusive, and sustainable urbanization. [Google Scholar]
- 100.Jiang Y. China's water security: current status, emerging challenges and future prospects. Environ Sci Policy. 2015;54:106–125. [Google Scholar]
- 101.Zhu D, Zhang J, Shi X, Liu Z. Security assessment of urban drinking water sources II. Security assessment for cities in China. J Hydraul Eng. 2010;41:914–920. [Google Scholar]
- 102.Peters M, Guo Q, Strauss H, Zhu G. Geochemical and multiple stable isotope (N, O, S) investigation on tap and bottled water from Beijing, China. J Geochem Explor. 2015;157:36–51. [Google Scholar]
- 103.Gan W, Guo W, Mo J. The occurrence of disinfection by-products in municipal drinking water in China's Pearl River Delta and a multipathway cancer risk assessment. Sci Total Environ. 2013;447:108–115. doi: 10.1016/j.scitotenv.2012.12.091. [DOI] [PubMed] [Google Scholar]
- 104.WHO . The World Health Organization; Geneva: 2011. Guidelines for drinking-water quality. [Google Scholar]
- 105.Chen P. Chinese city children and youth physical activity study: an introduction. Res Q Exerc Sport. 2013;84(suppl 2):S1–S3. doi: 10.1080/02701367.2013.851162. [DOI] [PubMed] [Google Scholar]
- 106.Zang J, Ng SW. Age, period and cohort effects on adult physical activity levels from 1991 to 2011 in China. Int J Behav Nutr Phys Act. 2016;13:40. doi: 10.1186/s12966-016-0364-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Muntner P, Gu D, Wildman RP. Prevalence of physical activity among Chinese adults: results from the International Collaborative Study of Cardiovascular Disease in Asia. Am J Public Health. 2005;95:1631–1636. doi: 10.2105/AJPH.2004.044743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Alfonzo M, Guo Z, Lin L, Day K. Walking, obesity and urban design in Chinese neighborhoods. Prev Med. 2014;69(suppl 1):S79–S85. doi: 10.1016/j.ypmed.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 109.Day K. Built environmental correlates of physical activity in China: A review. Prev Med Rep. 2016;3:303–316. doi: 10.1016/j.pmedr.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kwan M-P, Chai Y. Tana. Reflections on the similarities and differences between Chinese and US cities. Asian Geogr. 2014;31:167–174. [Google Scholar]
- 111.Jiang B, Liang S, Peng ZR. Transport and public health in China: the road to a healthy future. Lancet. 2017;390:1781–1791. doi: 10.1016/S0140-6736(17)31958-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yang Z, Jia P, Liu W, Yin H. Car ownership and urban development in Chinese cities: A panel data analysis. J Transp Geogr. 2017;58:127–134. [Google Scholar]
- 113.Zheng B, Zhang Q, Borken-Kleefeld J. How will greenhouse gas emissions from motor vehicles be constrained in China around 2030? Appl Energy. 2015;156:230–240. [Google Scholar]
- 114.Cao H, Qian Q, Weng T. Screen time, physical activity and mental health among urban adolescents in China. Prev Med. 2011;53:316–320. doi: 10.1016/j.ypmed.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 115.Li J, Shangguan Z. Food consumption patterns and per-capita calorie intake of China in the past three decades. J Food Agric Environ. 2012;10:201–206. [Google Scholar]
- 116.Zhai FY, Du SF, Wang ZH, Zhang JG, Du WW, Popkin BM. Dynamics of the Chinese diet and the role of urbanicity, 1991-2011. Obes Rev. 2014;15(suppl 1):16–26. doi: 10.1111/obr.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chinese Center for Disease Prevention and Control . Chinese Cener for Disease Prevention and Control; Beijing: 2016. China adult tobacco survey Report 2015. [Google Scholar]
- 118.Wang T, Wang Z, Wang L. Military Medical Science Press; Beijing: 2012. Report on chronic disease risk factor surveillance in China (2010) [Google Scholar]
- 119.Sun X, Li X, Phillips M. A cross-sectional survey of the awareness of common mental disorders among urban and rural residents in northern China. Chin Ment Health J. 2009;23:729–733. [Google Scholar]
- 120.Tang YL, Xiang XJ, Wang XY, Cubells JF, Babor TF, Hao W. Alcohol and alcohol-related harm in China: policy changes needed. Bull World Health Organ. 2013;91:270–276. doi: 10.2471/BLT.12.107318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Goggins WB, Chan EY, Ng E, Ren C, Chen L. Effect modification of the association between short-term meteorological factors and mortality by urban heat islands in Hong Kong. PLoS One. 2012;7:e38551. doi: 10.1371/journal.pone.0038551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Qin D. Science Press; Beijing: 2015. China national assessment report on risk managment and adaptation of climate extremes and diasters. [Google Scholar]
- 123.Li T, Horton RM, Bader DA. Aging will amplify the heat-related mortality risk under a changing climate: projection for the elderly in Beijing, China. Sci Rep. 2016;6:28161. doi: 10.1038/srep28161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Watts N, Adger WN, Agnolucci P. Health and climate change: policy responses to protect public health. Lancet. 2015;386:1861–1914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 125.Song QB, Zhao Y, Liu YQ, Zhang J, Xin SJ, Dong GH. Sex difference in the prevalence of metabolic syndrome and cardiovascular-related risk factors in urban adults from 33 communities of China: The CHPSNE study. Diab Vasc Dis Res. 2015;12:189–198. doi: 10.1177/1479164114562410. [DOI] [PubMed] [Google Scholar]
- 126.Jia P, Xue H, Zhang J, Wang Y. Time trend and demographic and geographic disparities in childhood obesity prevalence in China—evidence from 20 years of longitudinal data. Int J Environ Res Public Health. 2017;14:369. doi: 10.3390/ijerph14040369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ji CY, Chen TJ, the Working Group on Obesity in China (WGOC) Empirical changes in the prevalence of overweight and obesity among Chinese students from 1985 to 2010 and corresponding preventive strategies. Biomed Environ Sci. 2013;26:1–12. doi: 10.3967/0895-3988.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 128.Fan JG. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China. J Gastroenterol Hepatol. 2013;28(suppl 1):11–17. doi: 10.1111/jgh.12036. [DOI] [PubMed] [Google Scholar]
- 129.Dong GH, Wang J, Zeng XW. Interactions between air pollution and obesity on blood pressure and hypertension in Chinese children. Epidemiology. 2015;26:740–747. doi: 10.1097/EDE.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 130.Zhu YG, Ioannidis JPA, Li H, Jones KC, Martin FL. Understanding and harnessing the health effects of rapid urbanization in China. Environ Sci Technol. 2011;45:5099–5104. doi: 10.1021/es2004254. [DOI] [PubMed] [Google Scholar]
- 131.Li X, Liu J, Gibson V, Zhu Y. Urban sustainability and human health in China, East Asia and Southeast Asia. Curr Opin Environ Sustain. 2012;4:436–442. [Google Scholar]
- 132.Li Z, Wang P, Gao G, Xu C, Chen X. Age-period-cohort analysis of infectious disease mortality in urban-rural China, 1990–2010. Int J Equity Health. 2016;15:55. doi: 10.1186/s12939-016-0343-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Suk JE, Van Cangh T, Beauté J. The interconnected and cross-border nature of risks posed by infectious diseases. Glob Health Action. 2014;7:25287. doi: 10.3402/gha.v7.25287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mangili A, Gendreau MA. Transmission of infectious diseases during commercial air travel. Lancet. 2005;365:989–996. doi: 10.1016/S0140-6736(05)71089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Fang LQ, de Vlas SJ, Feng D. Geographical spread of SARS in mainland China. Trop Med Int Health. 2009;14(suppl 1):14–20. doi: 10.1111/j.1365-3156.2008.02189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Khan K, Arino J, Hu W. Spread of a novel influenza A (H1N1) virus via global airline transportation. N Engl J Med. 2009;361:212–214. doi: 10.1056/NEJMc0904559. [DOI] [PubMed] [Google Scholar]
- 137.Weng W, Ni S. Evaluation of containment and mitigation strategies for an influenza A pandemic in China. Simulation. 2015;91:407–416. [Google Scholar]
- 138.Cheng Q, Jing Q, Spear RC, Marshall JM, Yang Z, Gong P. The interplay of climate, intervention and imported cases as determinants of the 2014 dengue outbreak in Guangzhou. PLoS Negl Trop Dis. 2017;11:e0005701. doi: 10.1371/journal.pntd.0005701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Huang Y, Yi C. Invisible migrant enclaves in Chinese cities: underground living in Beijing, China. Urban Stud. 2015;52:2948–2973. [Google Scholar]
- 140.Hu Z, Liu H, Li X, Stanton B, Chen X. HIV-related sexual behaviour among migrants and non-migrants in a rural area of China: role of rural-to-urban migration. Public Health. 2006;120:339–345. doi: 10.1016/j.puhe.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 141.Ying L, Shaokai T, Xingdong Y. Awareness and knowledge of syphilis among different populations in Guangzhou, Guangdong Province, China. Sex Health. 2013;10:282–283. doi: 10.1071/SH12181. [DOI] [PubMed] [Google Scholar]
- 142.Nutbeam D, Padmadas SS, Maslovskaya O, Wu Z. A health promotion logic model to review progress in HIV prevention in China. Health Promot Int. 2015;30:270–280. doi: 10.1093/heapro/dat037. [DOI] [PubMed] [Google Scholar]
- 143.National Health and Family Planning Commission . National Health and Family Planning Commission, People's Republic of China; Beijing: 2015. China AIDS response progress report 2015. [Google Scholar]
- 144.Office of China National Narcotics Control Commission . China National Narcotics Control Commission; Beijing: 1999. Annual report on drug control in China 1998. [Google Scholar]
- 145.Office of China National Narcotics Control Commission . China National Narcotics Control Commission; Beijing: 2017. Annual report on drug control in China 2016. [Google Scholar]
- 146.Zhang L, Li Z, Li X. Study on the trend and disease burden of injury deaths in Chinese population, 2004–2010. PLoS One. 2014;9:e85319. doi: 10.1371/journal.pone.0085319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhao J, Tu EJC, McMurray C, Sleigh A. Rising mortality from injury in urban China: demographic burden, underlying causes and policy implications. Bull World Health Organ. 2012;90:461–467. doi: 10.2471/BLT.11.093849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Li YH, Wang CF, Song GX. Pedestrian injuries and the relevant burden in shanghai, china: implications for control. Biomed Environ Sci. 2015;28:127–135. doi: 10.3967/bes2015.015. [DOI] [PubMed] [Google Scholar]
- 149.Wang Y, Meng Q. China Science Press; Beijing: 2016. National disease surveilance system death surveilance data sets 2015. [Google Scholar]
- 150.Fang X, Jing R, Zeng G, Linnan HW, Zhu X, Linnan M. Socioeconomic status and the incidence of child injuries in China. Soc Sci Med. 2014;102:33–40. doi: 10.1016/j.socscimed.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 151.Yang T, Yang XY, Cottrell RR, Wu D, Jiang S, Anderson JG. Violent injuries and regional correlates among women in China: results from 21 cities study in China. Eur J Public Health. 2016;26:513–517. doi: 10.1093/eurpub/ckv193. [DOI] [PubMed] [Google Scholar]
- 152.Li SB. Analysis of present situation of peasant workers safety production in construction industry. Qual Civil Eng Construction. 2006;7:29–31. [Google Scholar]
- 153.Lin G, Zhang X, Dong H, Shen J, Li K, Zhou Q. Excessive fatal injury among migrant children in China: inequities in safety. Inj Prev. 2016;22:68–71. doi: 10.1136/injuryprev-2014-041270. [DOI] [PubMed] [Google Scholar]
- 154.Zhou N, Zhao S. Urbanization process and induced environmental geological hazards in China. Nat Hazards. 2013;67:797–810. [Google Scholar]
- 155.Yi L, Ge L, Zhao D, Zhou J, Gao Z. An analysis on disasters management system in China. Nat Hazards. 2012;60:295–309. [Google Scholar]
- 156.Shi P, Xu W, Ye T. Springer; Beijing: 2015. World atlas of natural disaster risk. [Google Scholar]
- 157.Xu W, Wang J, Shi P. Hazard degree assessment of urban earthquake disaster in China. J Nat Disasters. 2004;13:9–15. [Google Scholar]
- 158.Xiao H, Luo Z, Niu Q, Chang J. The 2010 Zhouqu mudflow disaster: possible causes, human contributions, and lessons learned. Nat Hazards. 2013;67:611–625. [Google Scholar]
- 159.Chen G. New trend of urban flooding. Inf China Constr. 2013;17:10–12. [Google Scholar]
- 160.Duan W, He B, Nover D. Floods and associated socioeconomic damages in China over the last century. Nat Hazards. 2016;82:401–413. [Google Scholar]
- 161.Wang J, Gao W, Xu S, Yu L. Evaluation of the combined risk of sea level rise, land subsidence, and storm surges on the coastal areas of Shanghai, China. Clim Change. 2012;115:537–558. [Google Scholar]
- 162.Gu L, Xie J, Long J. Epidemiology of major depressive disorder in mainland china: a systematic review. PLoS One. 2013;8:e65356. doi: 10.1371/journal.pone.0065356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Gupta S, Goren A, Dong P, Liu D. Prevalence, awareness, and burden of major depressive disorder in urban China. Expert Rev Pharmacoecon Outcomes Res. 2016;16:393–407. doi: 10.1586/14737167.2016.1102062. [DOI] [PubMed] [Google Scholar]
- 164.Chen J, Chen S, Landry PF. Urbanization and mental Health in China: Linking the 2010 population census with a cross-sectional survey. Int J Environ Res Public Health. 2015;12:9012–9024. doi: 10.3390/ijerph120809012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhong BL, Liu TB, Chan SSM. Common mental health problems in rural-to-urban migrant workers in Shenzhen, China: prevalence and risk factors. Epidemiol Psychiatr Sci. 2017:1–10. doi: 10.1017/S2045796016001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Xu J, Wang J, Wimo A, Qiu C. The economic burden of mental disorders in China, 2005-2013: implications for health policy. BMC Psychiatry. 2016;16:137. doi: 10.1186/s12888-016-0839-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Yu W, Chiu C. Growing pains: Changes in psychological well-being in urban China. Soc Indic Res. 2015;126:1349–1382. [Google Scholar]
- 168.Cheng Y, Li X, Lou C. The association between social support and mental health among vulnerable adolescents in five cities: findings from the study of the well-being of adolescents in vulnerable environments. J Adolesc Health. 2014;55(suppl):S31–S38. doi: 10.1016/j.jadohealth.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 169.Bao C, Mayila M, Ye Z. Forecasting and analyzing the disease burden of aged population in China, based on the 2010 Global Burden of Disease Study. Int J Environ Res Public Health. 2015;12:7172–7184. doi: 10.3390/ijerph120707172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jia J, Wang F, Wei C. The prevalence of dementia in urban and rural areas of China. Alzheimers Dement. 2014;10:1–9. doi: 10.1016/j.jalz.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 171.Zhang T, Tan H, Wu Y, Han B, Wang T. Urban older adults becoming unhealthier in modern China: a cross-temporal meta-analysis. Psychol Rep. 2016;118:737–747. doi: 10.1177/0033294116646160. [DOI] [PubMed] [Google Scholar]
- 172.Department of Policy Studies . Ministry of Human Resources and Social Security, People's Republic of China; Beijing, China: 2016. Advancements in human resources and social security in the fourth quarter of 2015 and the plan for further works. [Google Scholar]
- 173.Liu M, Sun LH, Liu G. Economic burden and economic risk of five major chronic diseases among Chinese urban residents. Beijing Da Xue Xue Bao. 2014;46:782–789. [PubMed] [Google Scholar]
- 174.Gao X, Liu X, Yan B. Planning response to older people's long-term care needs: Evidence from Beijing, China. Gerontechnology (Valkenswaard) 2016;14:210–217. [Google Scholar]
- 175.Wang G. Research on the total population, age structure and developing trend of the lost only child women by computer simulation. Population and Economics. 2016;5:1–11. [Google Scholar]
- 176.Ministry of Civil Affairs . China Statistics Press; Beijing: 2015. China Civil Affairs' Statistical Yearbook: Statistics of China Social Services 2015. [Google Scholar]
- 177.Shum MH, Lou VW, He KZ, Chen CC, Wang J. The “leap forward” in nursing home development in urban China: future policy directions. J Am Med Dir Assoc. 2015;16:784–789. doi: 10.1016/j.jamda.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 178.National Bureau of Statistics . China Statistics Press; Beijing: 2015. China social statistical yearbook 2015. [Google Scholar]
- 179.World Bank Health expenditure. 2017. http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS (accessed Feb 8, 2018).
- 180.Ministry of Health . Peiking Union Medical College Press; Beijing: 2003–2009. China health statistical yearbook (2003–2009) [Google Scholar]
- 181.National Health and Family Planning Commission of China . Peiking Union Medical College Press; Beijing: 2015. China statistical yearbook of health and family planning 2015. [Google Scholar]
- 182.Economics Department. OECD . Organization for Economic Operation and Development; Paris: 2013. What future for health spending? [Google Scholar]
- 183.Feng J, Yu Y, Lou P. Medical demand and growing medical costs in China-based on the gap between senior citizens' medical costs in urban and rural areas. J Soc Sci China. 2015;3:85–103. [Google Scholar]
- 184.Ramesh M, Wu X, He AJ. Health governance and healthcare reforms in China. Health Policy Plan. 2014;29:663–672. doi: 10.1093/heapol/czs109. [DOI] [PubMed] [Google Scholar]
- 185.WHO . World Health Organization; Geneva: 2000. The world health report 2000: health systems: improving performance. [Google Scholar]
- 186.Xu Y, Hang L. Height inequalities and their change trends in China during 1985-2010: results from 6 cross-sectional surveys on children and adolescents aged 7-18 years. BMC Public Health. 2017;17:473. doi: 10.1186/s12889-017-4402-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Xie Y, Zhang X, Xu Q, Zhang C. Short-term trends in China's income inequality and poverty: evidence from a longitudinal household survey. China Economic J. 2015;8:235–251. doi: 10.1080/17538963.2015.1108118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Center for Opportunity and Equality . Organisation for Economic Co-operation and Development; Paris: 2016. OECD inequality update 2016. “Income inequality remains high in the face of weak recovery”. [Google Scholar]
- 189.Xie E. Income-related inequalities of health and health care utilization. Front Econ China. 2011;6:131–156. [Google Scholar]
- 190.Zhou Z, Fang Y, Zhou Z. Assessing income-related health inequality and horizontal inequity in China. Soc Indic Res. 2017;132:241–256. [Google Scholar]
- 191.Anderson G, Farcomeni A, Pittau MG, Zelli R. A new approach to measuring and studying the characteristics of class membership: examining poverty, inequality and polarization in urban China. J Econom. 2016;191:348–359. [Google Scholar]
- 192.Liu Y, He S, Wu F. Urban pauperization under China's social exclusion: a case study of Nanjing. J Urban Aff. 2008;30:21–36. [Google Scholar]
- 193.Liu Y, He S, Wu F, Webster C. Urban villages under China's rapid urbanization: unregulated assets and transitional neighbourhoods. Habitat Int. 2010;34:135–144. [Google Scholar]
- 194.Herd R. The evolution of China's social policies. Econ Change Restruct. 2013;46:109–141. [Google Scholar]
- 195.Hu X, Cook S, Salazar MA. Internal migration and health in China. Lancet. 2008;372:1717–1719. doi: 10.1016/S0140-6736(08)61360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Zhang Y, Chen J. Housing poverty in post-reform Shanghai: Profiles in 2010 and decompositions. Open House Int. 2015;40:12–17. [Google Scholar]
- 197.Zhao P, Howden-Chapman P. Social inequalities in mobility: the impact of the hukou system on migrants' job accessibility and commuting costs in Beijing. Int Dev Plan Rev. 2010;32:363–384. [Google Scholar]
- 198.Li SM, Chan KW, He S. Migration, mobility, and community change in Chinese cities: introducing the special issue. Eurasian Geogr Econ. 2014;55:307–312. [Google Scholar]
- 199.Zhou Z, Zhu L, Zhou Z, Li Z, Gao J, Chen G. The effects of China's urban basic medical insurance schemes on the equity of health service utilisation: evidence from Shaanxi Province. Int J Equity Health. 2014;13:23. doi: 10.1186/1475-9276-13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Huang C, Liu CJ, Pan XF, Liu X, Li NX. Correlates of unequal access to preventive care in China: a multilevel analysis of national data from the 2011 China Health and Nutrition Survey. BMC Health Serv Res. 2016;16:177. doi: 10.1186/s12913-016-1426-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Brixi H, Mu Y, Targa B, Hipgrave D. Engaging sub-national governments in addressing health equities: challenges and opportunities in China's health system reform. Health Policy Plan. 2013;28:809–824. doi: 10.1093/heapol/czs120. [DOI] [PubMed] [Google Scholar]
- 202.State Council Air pollution prevention and control. 2013. http://www.gov.cn/zwgk/2013-09/12/content_2486773.htm (accessed Feb 8, 2018).
- 203.Ministry of Environmental Protection Action plan for water pollution control. 2015. http://zfs.mep.gov.cn/fg/gwyw/201504/t20150416_299146.htm (accessed Feb 8, 2018).
- 204.Department of Energy Statistics, National Bureau of Statistics . China Statistics Press; Beijing: 2015. China energy statistical yearbook 2014. [Google Scholar]
- 205.State Council Made in China 2025. 2015. http://www.gov.cn/zhengce/content/2015-05/19/content_9784.htm (accessed Feb 8, 2018).
- 206.Schroeder PM, Chapman RB. Renewable energy leapfrogging in China's urban development? Current status and outlook. Sustain Cities Soc. 2014;11(suppl C):31–39. [Google Scholar]
- 207.Zhang L, Mol APJ, He G. Transparency and information disclosure in China's environmental governance. Curr Opin Environ Sustain. 2016;18:17–24. [Google Scholar]
- 208.IPE. NRDC . Institute of Public & Environmental Affairs and Natural Resources Defense Council; Beijing: 2016. Assessment of pollution information transparency index (PITI) 2015–2016. [Google Scholar]
- 209.Cheng Z, Jiang J, Fajardo O, Wang S, Hao J. Characteristics and health impacts of particulate matter pollution in China (2001–2011) Atmos Environ. 2013;65:186–194. [Google Scholar]
- 210.Ministry of Environmental Protection Record of press conference in January. 2018. http://www.mep.gov.cn/gkml/hbb/qt/201801/t20180131_430706.htm (accessed Feb 8, 2018).
- 211.Tang D, Wang C, Nie J, the Taiyuan CDC Health benefits of improving air quality in Taiyuan, China. Environ Int. 2014;73:235–242. doi: 10.1016/j.envint.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 212.Yan CH, Xu J, Shen XM. Childhood lead poisoning in China: challenges and opportunities. Environ Health Perspect. 2013;121:A294–A295. doi: 10.1289/ehp.1307558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Feng Y, Mol APJ, Lu Y, He G, van Koppen CSA. Environmental pollution liability insurance in China: in need of strong government backing. Ambio. 2014;43:687–702. doi: 10.1007/s13280-013-0436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Cai B, Bo X, Zhang L, Boyce JK, Zhang Y, Lei Y. Gearing carbon trading towards environmental co-benefits in China: Measurement model and policy implications. Glob Environ Change. 2016;39:275–284. [Google Scholar]
- 215.Gaudreau M, Cao H. Political constraints on adaptive governance: environmental NGO networks in Nanjing, China. J Environ Dev. 2015;24:418–444. [Google Scholar]
- 216.Ministry of Housing and Urban-Rural Development . Chinese Statistics Press; Beijing: 2016. China urban construction statistical yearbook 2015. [Google Scholar]
- 217.Zhang X, Zhuang D, Ma X, Jiang D. Esophageal cancer spatial and correlation analyses: water pollution, mortality rates, and safe buffer distances in China. J Geogr Sci. 2013;24:46–58. [Google Scholar]
- 218.Song X, Chang KT, Yang L, Scheffran J. Change in environmental benefits of urban land use and its drivers in Chinese cities, 2000–2010. Int J Environ Res Public Health. 2016;13:535. doi: 10.3390/ijerph13060535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Wong TC. Developmental idealism: Building cities without slums in China. In: Wong T, Han S, Zhang H, editors. Population mobility, urban planning and management in China. Springer; Switzerland: 2015. [Google Scholar]
- 220.Zhou M, Li Y, Shi Z. Sanitary city and healthy city. J Environ Health. 2000;17:377–380. [Google Scholar]
- 221.National Health and Family Planning Commission Progress in disease prevention and control in China. Can J Public Health. 2015;9:97–101. [Google Scholar]
- 222.Zhang H, Tong X. Structural change in China's emergency management: theoretical generalizations. Soc Sci China. 2016;37:77–98. [Google Scholar]
- 223.National Development and Reform Commission. the Ministry of Housing and Urban-Rural Development Action plan for urban adaptation to climate change. 2016. http://www.mohurd.gov.cn/wjfb/201602/t20160224_226732.html (accessed Feb 8, 2018).
- 224.National Development and Reform Commission. the Ministry of Housing and Urban-Rural Development Note on pilot projects of builiding Climate Adaptative Cities. 2017. http://www.ndrc.gov.cn/gzdt/201702/W020170224631971736878.pdf (accessed Feb 8, 2018).
- 225.Urban Data Lab . Tsinghua Urban Planning and Design Institute; Beijing: 2017. 2017 White paper on bike sharing and urban development. [Google Scholar]
- 226.Policy and Economics Research Institute. China Academy of Information and Communications Technology Report on the socioeconomic impacts of bike sharing in 2017. 2018. http://www.caict.ac.cn/kxyj/caictgd/201802/t20180206_2238032.htm (accessed Feb 7, 2018).
- 227.Tu W, Shi C. Urban environmental management in Shanghai: achievements, problems, and prospects. Environ Manage. 2006;37:307–321. doi: 10.1007/s00267-003-0155-6. [DOI] [PubMed] [Google Scholar]
- 228.He G, Boas I, Mol APJ, Lu Y. E-participation for environmental sustainability in transitional urban China. Sustain Sci. 2017;12:187–202. [Google Scholar]
- 229.Li W. China's urban environmental governance in transition: a tale of two cities. In: Cheng Z, Wang M, Chen J, editors. Urban China in the new era: market reforms, current state, and the road forward. Springer; Berlin: 2014. pp. 103–124. [Google Scholar]
- 230.Tong Y, Yao R, He W. Impacts of sanitation upgrading to the decrease of fecal coliforms entering into the environment in China. Environ Res. 2016;149:57–65. doi: 10.1016/j.envres.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 231.Liu Y, Ling R, Yu X. The national immunization plan: China. Australas Med J. 2010;3:375–379. [Google Scholar]
- 232.Department for Disease Prevention and Control, National Health and Family Planning Commission Instruction and procedure for national immunization program for children. 2016. http://www.nhfpc.gov.cn/jkj/s3581/201701/a91fa2f3f9264cc186e1dee4b1f24084.shtml (accessed Feb 8, 2018).
- 233.Center for Health Statistics and Information . National Health and Family Planning Committee of the People's Rebublic of China; Beijing: 2016. An analysis report of National Health Services Survey in China 2013. [Google Scholar]
- 234.Peng ZQ, Chen WS, He Q. Evaluation of the mass measles vaccination campaign in Guangdong Province, China. Int J Infect Dis. 2012;16:e99–e103. doi: 10.1016/j.ijid.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 235.Li J, Lu L, Pang X. A 60-year review on the changing epidemiology of measles in capital Beijing, China, 1951–2011. BMC Public Health. 2013;13:986. doi: 10.1186/1471-2458-13-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Wan L, Cheng S, Chin D. A new disease reporting system increases TB case detection in China. Bull World Health Organ. 2007;85:401. [Google Scholar]
- 237.Department of Planning and Information. National Health and Family Planning Commission Statistical communique on the development of health and family planning in China in 2016. http://www.nhfpc.gov.cn/guihuaxxs/s10748/201708/d82fa7141696407abb4ef764f3edf095.shtml (accessed Feb 9, 2018).
- 238.Feng XY, Xia ZG, Vong S, Yang WZ, Zhou SS. Surveillance and response to drive the national malaria elimination program. Adv Parasitol. 2014;86:81–108. doi: 10.1016/B978-0-12-800869-0.00004-4. [DOI] [PubMed] [Google Scholar]
- 239.Peng HJ, Lai HB, Zhang QL. A local outbreak of dengue caused by an imported case in Dongguan China. BMC Public Health. 2012;12:83. doi: 10.1186/1471-2458-12-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Zhongdan C, Schilling RF, Shanbo W, Caiyan C, Wang Z, Jianguo S. The 100% condom use program: a demonstration in Wuhan, China. Eval Program Plann. 2008;31:10–21. doi: 10.1016/j.evalprogplan.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 241.Jia Z, Mao Y, Zhang F. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003–11): a national observational cohort study. Lancet. 2013;382:1195–1203. doi: 10.1016/S0140-6736(12)61898-4. [DOI] [PubMed] [Google Scholar]
- 242.Xiong W, Lv J, Li L. A survey of core and support activities of communicable disease surveillance systems at operating-level CDCs in China. BMC Public Health. 2010;10:704. doi: 10.1186/1471-2458-10-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Liu S, Wu X, Lopez AD. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ. 2016;94:46–57. doi: 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Guo K, Yin P, Wang L. Propensity score weighting for addressing under-reporting in mortality surveillance: a proof-of-concept study using the nationally representative mortality data in China. Popul Health Metr. 2015;13:16. doi: 10.1186/s12963-015-0051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Zhang L, Chow EPF, Jing J. HIV prevalence in China: integration of surveillance data and a systematic review. Lancet Infect Dis. 2013;13:955–963. doi: 10.1016/S1473-3099(13)70245-7. [DOI] [PubMed] [Google Scholar]
- 246.Li H, Wang B. Feasibility study of sports consumption using by urban workers and staff medical insurance-example of Anhui province. Sports Sci Res. 2014;18:21–28. [Google Scholar]
- 247.ThinkTank Research Center for Health Development Tobacco control in China 2017: A civil society erspective. 2017. http://www.tcrc.org.cn/html/xwzx/3575.html (accessed Feb 6, 2018).
- 248.Hill S, Lowe DB, Liu C, Santesso N. Building health-literate societies. In: Hill S, editor. The knowledgeable patient: communication and participation in health—a Cochrane handbook. Wiley–Blackwell; Oxford: 2011. pp. 184–195. [Google Scholar]
- 249.Wang Y. Health education in China (1978–2010): challenges and reforms. In: Taylor N, Quinn F, Littledyke M, Coll RK, editors. Health education in context: an international perspective on health education in schools and local communities. Sense Publishers; Rotterdam: 2012. pp. 253–260. [Google Scholar]
- 250.Tang Q, Li Z, Li G, Xu Y. The practice and development of healthy cities movement in Shanghai. Shanghai J Prev Med. 2016;28:7–10. [Google Scholar]
- 251.Zipser D, Chen Y, Gong F. McKinsey & Company; Shanghai: 2016. The modernization of the Chinese consumer. [Google Scholar]
- 252.Yan F, Chao B, Zhao D. Exploration of Chinese style management for stroke prevention and treatment. Chin J Contemp Neurol Neurosurg. 2016;16:235–238. [Google Scholar]
- 253.Wang B, He M, Chao A. Cervical cancer screening among adult women in China, 2010. Oncologist. 2015;20:627–634. doi: 10.1634/theoncologist.2014-0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Department of Publicity, National Health and Family Planning Committee Construction of national chronic disease prevention and control demonstration zones. 2016. http://www.nhfpc.gov.cn/xcs/s3582/201611/67ea0c9fd996425ba9425b5dd1b2afb9.shtml (accessed Feb 8, 2018).
- 255.Zhang N, Li Y. Application of grid management model in managing patients with mental disorder in Huilong community. China Health Ind. 2016;21:58–60. [Google Scholar]
- 256.Li Y, Ding L, Bian X, Zhang Q. Effect of comprehensive community intervention on recurrence rate of severe mental patients in China: a meta-analysis. Chin J Public Health. 2016;26:398–401. [Google Scholar]
- 257.Fu D, Fu H, McGowan P. Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: randomized controlled trial. Bull World Health Organ. 2003;81:174–182. [PMC free article] [PubMed] [Google Scholar]
- 258.Nie X, Li Y, Li L, Huang X. A study on health information literacy among urban and suburban residents in six provinces in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2014;48:566–570. [PubMed] [Google Scholar]
- 259.Wu Y, Benjamin EJ, MacMahon S. Prevention and control of cardiovascular disease in the rapidly changing economy of China. Circulation. 2016;133:2545–2560. doi: 10.1161/CIRCULATIONAHA.115.008728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.National Healthy and Family Planning Commission . Peiking Union Medical College Press; Beijing: 2011. China statistical yearbook of health and family planning 2011. [Google Scholar]
- 261.Department of Health, Government of the Hong Kong Special Administrative Region Health facts of Hong Kong. 2016. http://www.dh.gov.hk/english/statistics/statistics_hs/files/Health_Statistics_pamphlet_E.pdf (accessed Feb 8, 2018).
- 262.Kong X, Yang Y, Gao J. Overview of the health care system in Hong Kong and its referential significance to mainland China. J Chin Med Assoc. 2015;78:569–573. doi: 10.1016/j.jcma.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 263.Government of the Hong Kong Special Administrative Region Basic law of the Hong Kong Special Administrative Region of the People's Republic of China. July 1, 1997. http://www.basiclaw.gov.hk/en/basiclawtext/ (accessed Feb 8, 2018).
- 264.Lin V. Transformations in the healthcare system in China. Curr Sociol. 2012;60:427–440. [Google Scholar]
- 265.Wang HHX, Wang JJ, Wong SYS, Wong MCS, Mercer SW, Griffiths SM. The development of urban community health centres for strengthening primary care in China: a systematic literature review. Br Med Bull. 2015;116:139–153. doi: 10.1093/bmb/ldv043. [DOI] [PubMed] [Google Scholar]
- 266.Gao C, Xu F, Liu GG. Payment reform and changes in health care in China. Soc Sci Med. 2014;111:10–16. doi: 10.1016/j.socscimed.2014.03.035. [DOI] [PubMed] [Google Scholar]
- 267.McCollum R, Chen L, ChenXiang T. Experiences with primary healthcare in Fuzhou, urban China, in the context of health sector reform: a mixed methods study. Int J Health Plann Manage. 2014;29:e107–e126. doi: 10.1002/hpm.2165. [DOI] [PubMed] [Google Scholar]
- 268.Chen Y, Zhen Y, Zhu W. Evaluation of the effect of comprehensive community health system reform in Jiading District, Shanghai. Chin Health Resour. 2011;14:201–203. [Google Scholar]
- 269.Wang H, Gusmano MK, Cao Q. An evaluation of the policy on community health organizations in China: will the priority of new healthcare reform in China be a success? Health Policy. 2011;99:37–43. doi: 10.1016/j.healthpol.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Meng Q, Xu L, Zhang Y. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379:805–814. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- 271.National Health and Family Planning Commission . Peiking Union Medical College Press; Beijing: 2014. China satistical yearbook of health and family planning 2014. [Google Scholar]
- 272.Zhou Q, Liu GG, Krumholz S. Is Chinese national health insurance effective in the face of severe illness? a perspective from health service utilization and economic burden. Soc Indic Res. 2016;132:1307–1329. [Google Scholar]
- 273.World Bank Out-of-pocket health expenditure (% of private expenditure on health) 2016. http://data.worldbank.org/indicator/SH.XPD.OOPC.ZS?display=default&locations=CN (accessed Feb 8, 2018).
- 274.Zhang Y, Tang W, Zhang X, Zhang Y, Zhang L. National health insurance development in China from 2004 to 2011: coverage versus benefits. PLoS One. 2015;10:e0124995. doi: 10.1371/journal.pone.0124995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Xin XX, Guan XD, Shi LW. Catastrophic expenditure and impoverishment of patients affected by 7 rare diseases in China. Orphanet J Rare Dis. 2016;11:74. doi: 10.1186/s13023-016-0454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Teng H, Cao Z, Liu J. Health status and burden of health care costs among urban elderly in China. Asia Pac J Public Health. 2015;27(suppl):61S–68S. doi: 10.1177/1010539515571579. [DOI] [PubMed] [Google Scholar]
- 277.He AJ, Wu S. Towards universal health coverage via social health insurance in China: systemic fragmentation, reform imperatives, and policy alternatives. Appl Health Econd Health Policy. 2016;15:1–10. doi: 10.1007/s40258-016-0254-1. [DOI] [PubMed] [Google Scholar]
- 278.Meng Q, Fang H, Liu X, Yuan B, Xu J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. 2015;386:1484–1492. doi: 10.1016/S0140-6736(15)00342-6. [DOI] [PubMed] [Google Scholar]
- 279.Department of Migrant Population. National Health and Family Planning Commission of the People's Republic of China . China Population Publishing House; Beijing: 2017. Development report on China's migrant population 2017. [Google Scholar]
- 280.Zhang L, Ma H, Hao A, Zhang X. Equality investigation of primary public health service for migrant reproductive women in the Pearl River Delta Area Region. Chin J Public Health Manage. 2016;32:150–152. [Google Scholar]
- 281.WHO Health promotion glossary. 1998. www.who.int/healthpromotion/about/HPR%20Glossary%201998.pdf (accessed Feb 8, 2018).
- 282.WHO Healthy cities. 2016. http://www.euro.who.int/en/health-topics/environment-and-health/urban-health/activities/healthy-cities (accessed Feb 8, 2018).
- 283.National Patriotic Health Campaign Committee Guidance regarding the development of healthy cities, townships, and villages. 2016. http://www.nhfpc.gov.cn/jkj/s5898/201608/3a61d95e1f8d49ffbb12202eb4833647.shtml (accessed Feb 8, 2018).
- 284.Luo Y. Current status, issues, and solutions of the development of Healthy Cities in China. Chin J Public Health. 2011;27:1229–1230. [Google Scholar]
- 285.State Council Opinions of the State Council on further strengthening the patriotic health work during a new period. 2015. http://www.gov.cn/zhengce/content/2015-01/13/content_9388.htm (accessed Feb 8, 2018).
- 286.Yu H, Cheng G, Xu J, Wang H, Chang J, Meng Q. Comparative analysis on indicator system of healthy cities in China. Chin J Health Policy. 2012;5:30–33. [Google Scholar]
- 287.Yue D, Ruan S, Xu J. Impact of the China Healthy Cities initiative on urban environment. J Urban Health. 2017;94:149–157. doi: 10.1007/s11524-016-0106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Huang J, Xin Y, Hu J, Xia G, Tao M, Lei Q. Discussion on some idea questions about health city construction in our country. Chin J Health Educ. 2008;24:389–391. [Google Scholar]
- 289.Vlahov D, Gibble E, Freudenberg N, Galea S. Cities and health: history, approaches, and key questions. Acad Med. 2004;79:1133–1138. doi: 10.1097/00001888-200412000-00003. [DOI] [PubMed] [Google Scholar]
- 290.Freudenberg N. Interventions to improve urban health. In: Freudenberg N, Galea S, Vlahov D, editors. Cities and the health of the public. Vanderbilt University Press; Vanderbilt, TN: 2006. pp. 294–326. [Google Scholar]
- 291.Szreter S. The population health approach in historical perspective. Am J Public Health. 2003;93:421–431. doi: 10.2105/ajph.93.3.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Hancock T. The evolution, impact and significance of the healthy cities/healthy communities movement. J Public Health Policy. 1993;14:5–18. [PubMed] [Google Scholar]
- 293.Bezold C, Hancock T. The futures of the Healthy Cities and communities movement. Natl Civ Rev. 2014;103:66–70. [Google Scholar]
- 294.Gatzweiler FW, Zhu Y, Diez Roux AV. Advancing health and wellbeing in the changing urban environment. In: Gatzweiler FW, Zhu Y, Diez Roux AV, editors. Advancing health and wellbeing in the changing urban environment: implementing a systems approach. Springer Singapore; Singapore: 2017. pp. 1–48. [Google Scholar]
- 295.Whitmee S, Haines A, Beyrer C. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet. 2015;386:1973–2028. doi: 10.1016/S0140-6736(15)60901-1. [DOI] [PubMed] [Google Scholar]
- 296.Li L, Fu H. China's health care system reform: Progress and prospects. Int J Health Plann Manage. 2017;32:240–253. doi: 10.1002/hpm.2424. [DOI] [PubMed] [Google Scholar]
- 297.Tozan Y, Ompad DC. Complexity and dynamism from an urban health perspective: a rationale for a system dynamics approach. J Urban Health. 2015;92:490–501. doi: 10.1007/s11524-015-9963-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Ramaswami A, Russell AG, Culligan PJ, Sharma KR, Kumar E. Meta-principles for developing smart, sustainable, and healthy cities. Science. 2016;352:940–943. doi: 10.1126/science.aaf7160. [DOI] [PubMed] [Google Scholar]
- 299.State Council National new-type urbanization plan (2014–2020) 2014. http://ghs.ndrc.gov.cn/zttp/xxczhjs/ghzc/201605/t20160505_800839.html (accessed Feb 8, 2018).
- 300.World Bank . World Bank; Washington, DC: 2013. China 2030: building a modern, harmonious, and creative society. [Google Scholar]
- 301.Bellos I, Ferguson M. Moving from a product-based economy to a service-based economy for a more sustainable future. In: Bouchery Y, Corbett CJ, Fransoo JC, Tan T, editors. Sustainable supply chains. Springer; Switzerland: 2017. pp. 355–373. [Google Scholar]
- 302.China Internet Network Information Center . China Internet Network Information Center; Beijing: 2017. China statistical report on internet development. [Google Scholar]
- 303.Hsu J, Liu D, Yu YM. The top Chinese mobile health apps: a systematic investigation. J Med Internet Res. 2016;18:e222. doi: 10.2196/jmir.5955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Ruan S, Yue D, Cheng G, Meng Q. Creating national hygienic cities under the view of healthy cities. J Environ Health. 2014;31:829–832. [Google Scholar]
- 305.Rosenberg P, Kano M, Ludford I, Prasad A, Thomson H. World Health Organization; Geneva: 2016. Global report on urban health: equitable, healthier cities for sustainable development. [Google Scholar]
- 306.Rydin Y, Bleahu A, Davies M. Shaping cities for health: complexity and the planning of urban environments in the 21st century. Lancet. 2012;379:2079–2108. doi: 10.1016/S0140-6736(12)60435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Giles-Corti B, Vernez-Moudon A, Reis R. City planning and population health: a global challenge. Lancet. 2016;388:2912–2924. doi: 10.1016/S0140-6736(16)30066-6. [DOI] [PubMed] [Google Scholar]
- 308.Stevenson M, Thompson J, de Sá TH. Land use, transport, and population health: estimating the health benefits of compact cities. Lancet. 2016;388:2925–2935. doi: 10.1016/S0140-6736(16)30067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Sallis JF, Bull F, Burdett R. Use of science to guide city planning policy and practice: how to achieve healthy and sustainable future cities. Lancet. 2016;388:2936–2947. doi: 10.1016/S0140-6736(16)30068-X. [DOI] [PubMed] [Google Scholar]
- 310.Kent JL, Thompson S. The three domains of urban planning for health and well-being. J Plann Lit. 2014;29:239–256. [Google Scholar]
- 311.Grant M. European Healthy City Network Phase V: patterns emerging for healthy urban planning. Health Promot Int. 2015;30(suppl 1):i54–i70. doi: 10.1093/heapro/dav033. [DOI] [PubMed] [Google Scholar]
- 312.Chen T, Hui ECM, Lang W, Tao L. People, recreational facility and physical activity: New-type urbanization planning for the healthy communities in China. Habitat Int. 2016;58:12–22. [Google Scholar]
- 313.Salat S, Labbé F, Nowacki C, Walker G. Hermann; Paris: 2011. Cities and forms: on sustainable urbanism. [Google Scholar]
- 314.Plochg T, Schmidt M, Klazinga NS, Stronks K. Health governance by collaboration: a case study on an area-based programme to tackle health inequalities in the Dutch city of the Hague. Eur J Public Health. 2013;23:939–946. doi: 10.1093/eurpub/ckt038. [DOI] [PubMed] [Google Scholar]
- 315.Corburn J. Equitable and healthy city planning: towards healthy urban governance in the century of the city. In: de Leeuw E, Simos J, editors. Healthy cities: the theory, policy, and practice of value-based urban planning. Springer–Verlag; New York, NY: 2017. pp. 31–41. [Google Scholar]
- 316.Sun L, Zhu D, Chan EHW. Public participation impact on environment NIMBY conflict and environmental conflict management: comparative analysis in Shanghai and Hong Kong. Land Use Policy. 2016;58:208–217. [Google Scholar]
- 317.Chaskin RJ. Building community capacity a definitional framework and case studies from a comprehensive community initiative. Urban Aff Rev. 2001;36:291–323. [Google Scholar]
- 318.Wendel ML, Burdine JN, McLeroy KR, Alaniz A, Norton B, Felix MR. Community capacity: theory and application. In: DiClemente RJ, Richard AC, Michelle CK, editors. Emerging theories in health promotion practice and research 2009. Jossey–Bass; San Francisco, CA: 2009. pp. 277–302. [Google Scholar]
- 319.Raeburn J, Akerman M, Chuengsatiansup K, Mejia F, Oladepo O. Community capacity building and health promotion in a globalized world. Health Promot Int. 2006;21(suppl 1):84–90. doi: 10.1093/heapro/dal055. [DOI] [PubMed] [Google Scholar]
- 320.Quelch JA, Boudreau EC. Building a culture of health. In: Quelch JA, Boudreau EC, editors. A new imperative for business. Springer; New York, NY: 2016. pp. 1–25. [Google Scholar]
- 321.Mackintosh M, Channon A, Karan A, Selvaraj S, Cavagnero E, Zhao H. What is the private sector? Understanding private provision in the health systems of low-income and middle-income countries. Lancet. 2016;388:596–605. doi: 10.1016/S0140-6736(16)00342-1. [DOI] [PubMed] [Google Scholar]
- 322.Information Center, National Health and Family Planning Committee Information on health services nationwide (01/2016-11/2016) 2017. http://www.nhfpc.gov.cn/mohwsbwstjxxzx/s7967/201702/79b6d9e3bf9e40e6a8efa1328b80ada9.shtml (accessed Feb 8, 2018).
- 323.Qian D, Lucas H, Chen J, Xu L, Zhang Y. Determinants of the use of different types of health care provider in urban China: a tracer illness study of URTI. Health Policy. 2010;98:227–235. doi: 10.1016/j.healthpol.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 324.Gandhi S, Chen S, Hong L. Effect of mobile health interventions on the secondary prevention of cardiovascular disease: systematic review and meta-analysis. Can J Cardiol. 2017;33:219–231. doi: 10.1016/j.cjca.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 325.Tsouros AD. Healthy cities: A political project designed to change how cities understand and deal with health. In: de Leeuw E, Simos J, editors. Healthy cities: the theory, policy, and practice of value-based urban planning. Springer–Verlag; New York, NY: 2017. pp. 489–504. [Google Scholar]
- 326.Zhang Y, Li B. Motivating service improvement with awards and competitions—hygienic city campaigns in China. Environ Urban. 2011;23:41–56. [Google Scholar]
- 327.Li B, Huikuri S, Zhang Y, Chen W. Motivating intersectoral collaboration with the Hygienic City Campaign in Jingchang, China. Environ Urban. 2015;27:285–302. [Google Scholar]
- 328.de Leeuw E, Green G, Spanswick L, Palmer N. Policymaking in European healthy cities. Health Promot Int. 2015;30(suppl 1):i18–i31. doi: 10.1093/heapro/dav035. [DOI] [PubMed] [Google Scholar]
- 329.de Leeuw E. Do healthy cities work? A logic of method for assessing impact and outcome of healthy cities. J Urban Health. 2012;89:217–231. doi: 10.1007/s11524-011-9617-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Hodgson K. American Planning Association; Washington, DC: 2011. Comprehensive planning for public health: results of the planning and community health research center survey. [Google Scholar]
- 331.Worldwatch Institute . Worldwatch Institute; Washington, DC: 2006. State of the World 2007: our urban future. [Google Scholar]
- 332.Thresia CU. Rising private sector and falling ‘good health at low cost’: health challenges in China, Sri Lanka, and Indian state of Kerala. Int J Health Serv. 2013;43:31–48. doi: 10.2190/HS.43.1.c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.