Abstract
Background
We investigated the potential of proteomic fingerprinting with mass spectrometric serum profiling, coupled with pattern recognition methods, to identify biomarkers that could improve diagnosis of tuberculosis.
Methods
We obtained serum proteomic profiles from patients with active tuberculosis and controls by surface-enhanced laser desorption ionisation time of flight mass spectrometry. A supervised machine-learning approach based on the support vector machine (SVM) was used to obtain a classifier that distinguished between the groups in two independent test sets. We used k-fold cross validation and random sampling of the SVM classifier to assess the classifier further. Relevant mass peaks were selected by correlational analysis and assessed with SVM. We tested the diagnostic potential of candidate biomarkers, identified by peptide mass fingerprinting, by conventional immunoassays and SVM classifiers trained on these data.
Findings
Our SVM classifier discriminated the proteomic profile of patients with active tuberculosis from that of controls with overlapping clinical features. Diagnostic accuracy was 94% (sensitivity 93·5%, specificity 94·9%) for patients with tuberculosis and was unaffected by HIV status. A classifier trained on the 20 most informative peaks achieved diagnostic accuracy of 90%. From these peaks, two peptides (serum amyloid A protein and transthyretin) were identified and quantitated by immunoassay. Because these peptides reflect inflammatory states, we also quantitated neopterin and C reactive protein. Application of an SVM classifier using combinations of these values gave diagnostic accuracies of up to 84% for tuberculosis. Validation on a second, prospectively collected testing set gave similar accuracies using the whole proteomic signature and the 20 selected peaks. Using combinations of the four biomarkers, we achieved diagnostic accuracies of up to 78%.
Interpretation
The potential biomarkers for tuberculosis that we identified through proteomic fingerprinting and pattern recognition have a plausible biological connection with the disease and could be used to develop new diagnostic tests.
Introduction
Latent tuberculosis is present in a third of the world's population, with the prevalence of active tuberculosis in many areas exceeding 700 cases per 100 000 of the population.1 This global epidemic is fuelled by synergy with HIV, which is found in 40–70% of African patients with active tuberculosis.1 Most deaths from tuberculosis are preventable by early diagnosis and treatment.2 In areas of high prevalence, sputum smear microscopy is often the only available and affordable test, but at best achieves a sensitivity of 50–70%. Culture of Mycobacterium tuberculosis, the diagnostic gold standard, is sensitive and specific in cases of smear-positive tuberculosis, but takes 2–6 weeks to yield a result and is not routinely used in countries with high prevalences of tuberculosis. In these areas, tuberculin skin tests are often insufficiently accurate to aid diagnosis,3 and do not readily distinguish between contained infection and disease. Serological tests for tuberculosis have focused on detection of mycobacterial antigens and, like skin tests, can be confounded by crossreactivity with non-pathogenic mycobacteria or previous immunisation with BCG.4 Recently developed tests based on DNA amplification or interferon γ release are expensive and need particular expertise.5 A cheap, accurate, and rapid diagnostic test for tuberculosis will have immense impact on the control of this disease. For example, a test yielding results within a few hours but with a sensitivity similar to that of existing tests such as sputum microscopy (which requires two or more clinic visits) would be a great advance because it would enable initiation of treatment at a single clinic visit.
Proteomic fingerprinting is a diagnostic concept based on the idea that disease states are sometimes associated with distinctive configurations of circulating proteins. Because the biological complexity of most diseases means that individual biomarkers have limited diagnostic sensitivities and specificities, analysis of combinations of several biomarkers offers the possibility of enhanced diagnostic accuracy. High throughput proteomic profiling of serum has been revolutionised by recent advances in mass spectrometry, such as surface-enhanced laser desorption ionisation time of flight (SELDI-ToF) mass spectrometry.6 The application of approaches based on machine learning to the problem of pattern recognition7 makes it possible to identify diagnostic combinations of proteins (diagnostic signatures) embedded within such profiles.8 Analysis of serum proteomic fingerprints has improved diagnostic accuracy for some cancers6, 9, 10 and infections such as human African trypanosomiasis.11 This approach has also been used in the search for novel biomarkers for severe acute respiratory syndrome12 and intra-amniotic infections.13 We assessed the potential of proteomic fingerprinting as a basis for diagnosis of pulmonary tuberculosis.
Methods
Patients and controls
For the first phase of the study, 179 serum samples were obtained from patients with retrospectively confirmed culture-positive tuberculosis. Banked serum samples collected in Uganda and The Gambia were obtained from the WHO TB specimen bank.14 These samples had been taken at the time of first presentation to designated outpatient clinics, before initiation of chemotherapy for tuberculosis. Other samples were obtained prospectively from patients presenting with tuberculosis to the inpatient and outpatient facilities at St George's Hospital, London, UK. We restricted ourselves mainly to patients with tuberculosis who presented with typical manifestations of pulmonary disease,15 because this is the commonest presentation of tuberculosis in adults in all geographical areas.
170 serum samples from controls were collected at four separate sites: St George's Hospital, UK; Angola; The Gambia; and Uganda. Those from The Gambia and Uganda were taken from the WHO specimen bank. We recruited controls with a range of inflammatory conditions (confirmed by standard diagnostic criteria) with clinical features that can overlap with those of tuberculosis. For example, we included patients with sarcoidosis, which is frequently included in the differential diagnosis of pulmonary tuberculosis, and other severe respiratory infections representing patients who have non-tuberculous destructive pulmonary pathology. To allow for systemic inflammatory processes that can mimic tuberculosis, we recruited patients with other systemic infections, and patients with inflammatory bowel and autoimmune diseases. 21 healthy volunteers were also included among the controls. The distribution of cases and controls was not intended to reflect a particular population or epidemiological setting, but to encompass a broad range of symptomatically overlapping clinical presentations.
Because this first dataset relied heavily on archived samples, we subsequently collected a second dataset entirely from the UK to validate further our classifiers. These samples, from patients with tuberculosis and controls, were obtained prospectively from consecutive patients with predominantly respiratory symptoms attending the Hammersmith Hospital and St George's Hospital, London. Serum was collected within 2 days of first presentation and before initiation of treatment for tuberculosis. Most patients presented through the accident and emergency department, as is typical for cases of tuberculosis in these hospitals. Controls were symptomatic and underwent full diagnostic assessment to exclude tuberculosis.
For both datasets, fully informed consent was obtained from every patient, in accordance with local research ethics committee policy. Clinical information was archived in a linked, anonymised database.
Procedures
Serum was separated from 5 mL blood by centrifugation, and samples were allowed to clot for 30 min at room temperature in sterile glass tubes. 100-μL aliquots were frozen at −80°C within 1 h of collection, and underwent no more than two freeze-thaw cycles before mass spectrum analysis.
Samples were applied to CM10 protein chip arrays (Ciphergen, Fremont, CA, USA) as described previously,11 and a saturated solution of sinapinic acid in 50% acetonitrile, 0·5% trifluoroacetic acid was applied twice to each spot on the array, with air drying between each application. To minimise bias, serum samples from patients with tuberculosis and controls were assayed on the same chips.
Time-of-flight spectra were generated using a PBS-II mass spectrometer (Ciphergen, Freemont, CA, USA) at laser intensities of 200, 220, and 240, high mass 100 kDa, detector sensitivity 8, and focus mass 10 kDa. Each spot on the array was analysed from position 20 to 80, delta 4, with seven shots per position, preceded by two warming shots at laser intensities of 205, 225, or 245. Every protein chip array included a universal control sample (aliquoted from a single sample from one individual and stored at −80°C). Both groups of spectra (tuberculosis and controls) comprised samples run on different occasions over a 6-month period. The instrument was calibrated weekly using the Ciphergen all-in-one protein and peptide calibrants.
To identify peaks, spectra were normalised to the total ion current in the m/z range over 2000–100 000 after baseline subtraction. For each patient a single spectrum generated at a laser intensity of 200, 220, or 240 was selected to minimise deviation of the total ion current to within 2 SD from the mean of all patients, as described previously.11 Biomarker Wizard version 3.1 was used to identify corresponding peaks in each spectrum (peak clusters) within 0·6% of the molecular mass. Signal-to-noise ratio was set at 10 for the first pass and 2 for the second pass.
To identify proteins, 20 μL serum was incubated on ice for 20 min with 30 μL denaturation buffer, diluted in 50 μL binding buffer (denaturation buffer diluted 1:9 in 50 mM Tris-HCl pH 9) followed by a further 30 min incubation on ice. Samples were applied to Q Ceramic HyperD spin columns (Ciphergen, 20 minutes), pre-equilibrated first in Tris (50 mM, pH 9), followed by binding buffer. The 11·5 kDa and 13·7 kDa biomarkers were eluted from the spin column in elution buffer (50 mM sodium citrate, 0·1% octyl glucopyranoside, pH 3) and selective enrichment was confirmed by SELDI-ToF MS. The biomarkers were resolved by one-dimensional SDS-PAGE (NuPAGE, 4–12% Bis-Tris, Invitrogen, Carlsbad, CA, USA), stained with Coomassie blue, and excised from the gel. Gel pieces were washed three times in a mixture of ammonium bicarbonate (50 mM) and acetonitrile (50%), dehydrated in acetonitrile (100%) and dried. Proteins were subjected to in-gel tryptic digestion (15 min, room temperature) by the addition of trypsin (20 ng/μL) in acetonitrile (10%) and ammonium bicarbonate (25 mM), followed by incubation in ammonium bicarbonate (25 mM) for 4 h. Peptide mass fingerprints16 of the digests were analysed by matrix-assisted laser desorption/ionisation time-of-flight (MALDI-ToF) mass spectrometry using 20% α-cyano-4-hydroxy-cinnamic acid as matrix. The results of the in-gel tryptic digest were corroborated by tryptic digestion after passive elution of the protein from the gel. The peptide mass fingerprints were used to interrogate public databases with the MASCOT search engine.17
The four selected biomarkers were measured in a regional protein reference laboratory at St George's Hospital with commercially available kits validated for clinical use. Neopterin was measured by competitive ELISA with a kit (ELItest Neopterin, BRAHMS Aktiengesellschaft, Hennigsdorf, Germany) in a Triturus analyser (Diagnostics Grifols SA, Barcelona, Spain). Rate nephelemetry was used for measurement of C-reactive protein, transthyretin (Beckmann Immage 800 analyser, Beckman Coulter, Fullerton, CA, USA) and serum amyloid A (N latex SAA, BN II analyser, Dade-Behring, Marburg, Germany). In each case, kits were used according to the manufacturers' instructions. The antibody used in the serum amyloid A assay detects total serum amyloid A.
In supervised machine learning, a supervised learning algorithm is tasked to find a decision function capable of assigning the correct label for a set of input/output pairs of examples, called the training data. The ability of the decision function to predict correct labels for unseen samples (test data) is known as its generalisation. Current machine learning methods, such as support vector machines (SVM), aim to optimise this property (webappendix).18 The generalisation of a classifier is dependent on a set of parameters (model) that must be chosen to optimise performance. For this purpose we adopted a grid search strategy in which a range of parameter values were used and tested using cross-validation.
We used two cross-validation schemes. In k-fold cross-validation the training set is randomly split in k groups of equally distributed positive and negative cases. A classifier is trained on k–1 of the groups and its generalisation performance is validated on the remaining group. This process is repeated k times, each time holding out a different validation subset and the average represents the overall generalisation. In the second scheme, k-fold cross-validation with test, the data are first randomly split into training and testing sets. A k-fold cross-validation is performed on the training set and the generalisation is obtained on the unseen testing set.
The generalisation performance of the classifiers was assessed by considering the number of correctly classified (true positives, TP, and true negatives, TN) and incorrectly classified (false positives, FP, and false negatives, FN) cases in the testing set. Sensitivity (se) was defined as the conditional probability of a true positive, se=TP/(TP+FN); specificity (sp) as the conditional probability of a true negative, sp=TN/(TN+FP); and accuracy (ac) as the proportion of correct classifications, ac=(TP+TN)/(TP+FP+TN+FN). The performance (positive diagnostic likelihood ratio) of a classifier expressed by its true positive rate (se) and false positive rate (1–sp) was plotted in a receiver operator curve (ROC) space.
We created independent training and testing sets, with similar numbers of patients with tuberculosis and controls and similar representation of age and sex in each set. Using these sets we evaluated the generalisation performance of several supervised machine learning methods, such as single layer perceptron (SLP),19 multilayered perceptron (MLP),20 tree classifiers,21, 22, 23 and SVMs.
To provide robust estimates of the generalisation capability of the classifier we did ten-fold cross-validation with test. First, we generated 100 80:20 train:test sets by random sampling without replacement in the entire dataset. For each 80:20 train:test set a ten-fold cross-validation is done on the training set and the parameter with the best performance is chosen. The SVM is retrained with the best parameter over all ten subsets and the final performance is assessed on the testing set. In these experiments each ROC curve is smoothed, sampled, and averaged to show the mean curve with SD.
For further validation in the second independent testing set, the classifier was refined by training in the entire first dataset and then applied to the second set.
We used the Pearson correlation coefficient to rank peaks for their discriminatory power (webappendix). It can be used as a test statistic to assess the significance of a variable and it is linked to the t test. We estimated the Pearson correlation coefficient between values of each mass cluster and corresponding class labels across the training set. We then used this estimate to rank positively and negatively correlated mass clusters. We selected ten mass clusters with the highest positive, and ten with the highest negative, correlation coefficients.
We used a chunking and decomposition implementation of the support vector machine, SVMlight.24 We used Waikato Environment for Knowledge Analysis25 for decision tree algorithms, boosting, and MLP. The experimentation framework was coded in Matlab and Java. A custom and reusable object-oriented database was created using ObjectDB and interfaced with the experimentation framework. The Matlab interface to SVMlight was obtained online.26 The SPIDER Matlab object-oriented machine learning library was obtained online27 and was modified to use SVMlight version 6.
Role of the funding source
The sponsor of the study had no direct role in study design, data collection, data analysis, data interpretation, or writing of the report. A proportion of the serum samples from patients with tuberculosis were made available through the WHO TB databank. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Details of patients and controls from the first phase of the study are given in Table 1, Table 2 . Most patients had advanced pulmonary disease, presenting with cough, fever, and weight loss, and the majority had smear positive cavitary disease.
Table 1.
Characteristics of patients with tuberculosis and controls
| Train | Test | Total | ||
|---|---|---|---|---|
| Tuberculosis | ||||
| Total number of patients | 102 | 77 | 179 | |
| Symptomatic | 100 (98%) | 74 (96%) | 174 (97%) | |
| Persistent cough | 98 (96%) | 74 (96%) | 171 (96%) | |
| Haemoptysis | 5 (5%) | 1 (1%) | 6 (3%) | |
| Night sweats/fever | 68 (67%) | 53 (67%) | 121 (68%) | |
| Weight loss ≥5% | 86 (84%) | 60 (78%) | 146 (82%) | |
| Weight loss <5% | 11 (11%) | 15 (19%) | 26 (15%) | |
| Mean (range) symptom duration before recruitment in days | 122·6 (13–449) | 129·5 (12–754) | 126 (12–754) | |
| Smear positive | 89 (87%) | 66 (86%) | 155 (87%) | |
| Pulmonary disease | 77 (75%) | 64 (83%) | 141 (79%) | |
| Extrapulmonary disease | 2 (2%) | 2 (3%) | 4 (2%) | |
| Pulmonary and extrapulmonary | 22 (22%) | 11 (14%) | 33 (18%) | |
| Abnormal chest radiograph | 95 (93%) | 67 (87%) | 162 (91%) | |
| Cavitary disease | 66 (65%) | 49 (64%) | 115 (64%) | |
| Previous BCG vaccination* | 36 (35%) | 26 (34%) | 62 (35%) | |
| Skin test positive† | 56 (55%) | 36 (47%) | 92 (51%) | |
| Controls‡ | ||||
| Total number of patients | 91 | 79 | 170 | |
| Inflammatory bowel disease | 10 (11%) | 6 (8%) | 16 (9%) | |
| Sarcoidosis | 6 (7%) | 7 (9%) | 13 (8%) | |
| Respiratory infections§ | 27 (30%) | 24 (30%) | 51 (30%) | |
| Other Infections | ||||
| Malaria (Plasmodium falciparum) | 4 (4%) | 3 (4%) | 7 (4%) | |
| HAT (Trypanosoma brucei gambiense)¶ | 10 (11%) | 9 (11%) | 19 (11%) | |
| Others‖ | 1 (1%) | 2 (3%) | 3 (2%) | |
| Neurological disease** | 13 (14%) | 13 (16%) | 26 (15%) | |
| Autoimmune disease†† | 6 (7%) | 3 (4%) | 9 (5%) | |
| Myeloma/monoclonal gammopathy | 2 (2%) | 3 (4%) | 5 (3%) | |
| Healthy volunteers | 12 (13%) | 9 (11%) | 21 (12%) | |
Data are number (%) unless otherwise specified. HAT=human African trypanosomiasis.
Definite history of BCG vaccination, presence of scar, or both. Data missing for 38 patients.
Mantoux reaction ≥15 mm greatest diameter of induration or Heaf grade ≥3. Data missing for 46 patients.
12 controls were taking high-dose systemic steroids (prednisolone ≥60 mg per day or dexamethasone ≥12 mg per day). BCG history and skin-test data unavailable for most control patients; tuberculin skin testing was only done on small minority.
Majority pyogenic respiratory infections (based on presence of consolidation on CXR and prompt clinical response to antibacterial therapy. One patient with pulmonary infarction rather than infection is included in the test set.
Nine patients with HAT had advanced (neurological disease) based on detection of parasites and/or >5 white cells per mm3 in CSF.
Visceral leishmaniasis (1), meningococcal septicaemia (1), staphylococcal cellulitis (1).
Cerebral neoplasia (12), cerebral abscess in association with infective endocarditis (1), myasthenia gravis (2), multiple sclerosis (5) and lumbar disc prolapse (6).
Rheumatoid arthritis (3) systemic lupus erythematosis (4), systemic sclerosis (1), overlap syndrome (1).
Table 2.
Participant demographics
|
Tuberculosis* |
Controls |
Total | ||||||
|---|---|---|---|---|---|---|---|---|
| Train | Test | Total | Train | Test | Total | |||
| Total number of patients | 102 | 77 | 179 | 91 | 79 | 170 | 349 | |
| Mean (range) age in years | 31 (16–86) | 33 (19–84) | 32 (16–86) | 44 (16–88) | 46 (14–84) | 45 (16–84) | 38 (14–88) | |
| Sex (male:female) | 65:37 | 47:30 | 112:67 | 52:39 | 42:37 | 94:76 | 206:143 | |
| Ethnic origin | ||||||||
| Sub-Saharan African | 81 (79%) | 60 (78%) | 141 (79%) | 29 (32%) | 29 (37%) | 58 (34%) | 199 | |
| African, not specified | 3 (3%) | 1 (1%) | 4 (2%) | 5 (6%) | 4 (5%) | 9 (5%) | 13 | |
| Asian | 13 (13%) | 9 (12%) | 22 (12%) | 6 (7%) | 3 (4%) | 9 (5%) | 31 | |
| White | 5 (5%) | 7 (9%) | 12 (7%) | 49(54%) | 39 (49%) | 88 (51%) | 100 | |
| Not recorded | .. | .. | .. | 2 (2%) | 4 (5%) | 6 (4%) | 6 | |
| Collection site | ||||||||
| Sub-Saharan Africa | 81 (79%) | 60 (78%) | 141 (79%) | 21 (23%) | 19 (24%) | 40 (24%) | 181 | |
| UK | 21 (21%) | 17 (22%) | 38 (21%) | 70 (77%) | 60 (76%) | 130 (76%) | 168 | |
| HIV serology | ||||||||
| HIV positive† | 35 (34%) | 24 (31%) | 59 (33%) | 2 (2%) | 3 (4%) | 5 (3%) | 64 | |
| CD4 count ≥200×106 per mL | 19 | 13 | 32 | .. | .. | .. | .. | |
| CD4 count <200×106 per mL | 15 | 11 | 26 | .. | .. | .. | .. | |
| HIV negative | 60 (59%) | 45 (58%) | 105 (59%) | 12 (13%) | 8 (10%) | 20 (12%) | 125 | |
| Not determined | 7 (7%) | 8 (10%) | 15 (8%) | 77 (85%) | 68 (86%) | 145 (85%) | 160 | |
Percentages refer to proportion of patients in the training and testing set for each demographic category.
12 patients with tuberculosis had received 1–7 days of chemotherapy at time of recruitment.
CD4 counts were available for HIV-seropositive patients; no value was available for six seropositive patients.
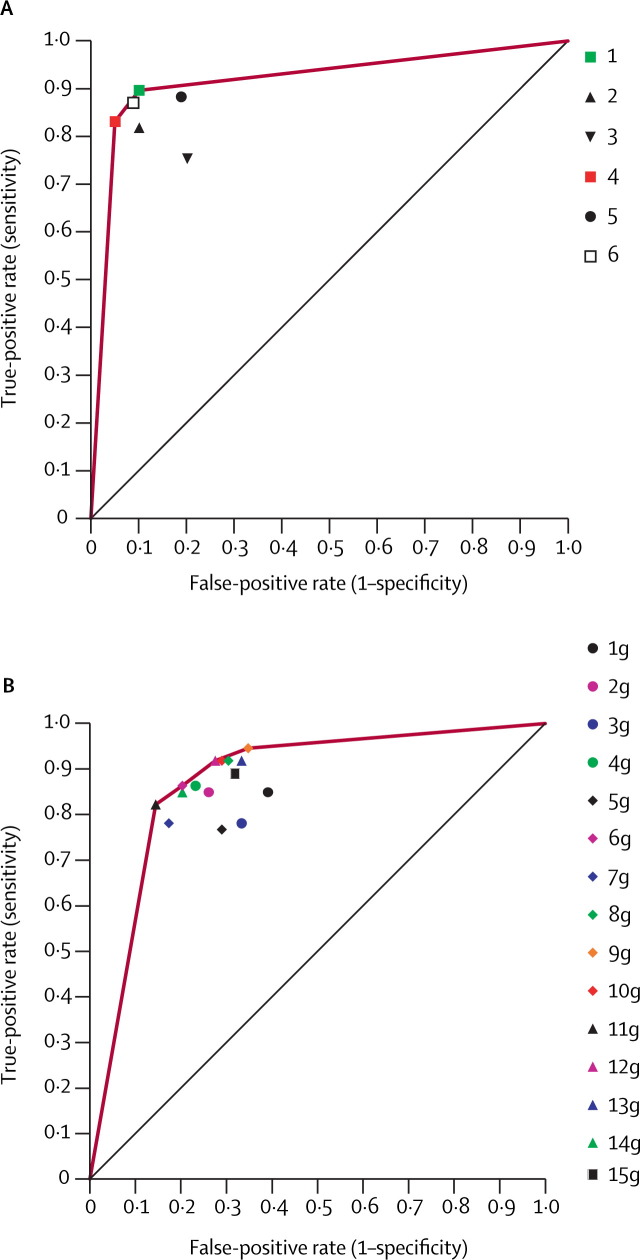
To generate diagnostic classifiers for tuberculosis, we first profiled 349 serum samples on weak cation exchange (CM10) protein chip arrays by SELDI-ToF MS,6, 28 and identified 219 peak clusters from m/z spectra in the range 2000–100 000. The choice of chip surface was based on our previous observation that the CM10 surface-chemistry yields particularly rich spectra from serum.11 Spectra were assigned randomly to a training and testing set and we then used supervised machine learning classification methods (table 3 , webappendix) to discriminate the proteomic spectra of patients with tuberculosis from the controls using the training and testing set approach (table 2). The ability of a classifier to discriminate data correctly in the testing set is known as its generalisation performance.18, 29 We compared the generalisation performance of a range of classifiers by plotting their performance on the testing set in ROC space (figure 1A ). A Gaussian kernel SVM16, 29, 30 (table 3 and figure 1A, red square) was the best discriminator between tuberculosis and control groups, with a sensitivity of 93·5% and specificity of 94·9% (overall accuracy 94·2%). This SVM classifier defines the convex hull of the ROC space (figure 1A, red line), achieving the best accuracy. Samples from five patients with tuberculosis and four controls in the testing set were misclassified (webtable 1). Notably, 21 of the 24 control patients with respiratory infection in the test set were correctly classified by the SVM, as were all seven patients with sarcoidosis. None of the African control patients with sleeping sickness or malaria were misclassified. Only one of the 11 smear-negative cases of tuberculosis was missed.
Table 3.
Diagnostic performance of classifiers
| Output |
Actual |
Accuracy | Sensitivity | Specificity | ||
|---|---|---|---|---|---|---|
| TB | C | |||||
| Support vector machine (SVM_1) | ||||||
| Kernel: Gaussian | TB | 72 | 4 | 94·23% | 93·50% | 94·93% |
| Soft margin=10 | C | 5 | 75 | |||
| ADTree+AdaBoost (ADT_2) | ||||||
| 100 iterations | TB | 72 | 7 | 92·30% | 93·50% | 91·13% |
| Weight threshold=100 | C | 5 | 72 | |||
| C4.5 Tree+AdaBoost (C4·5_2) | ||||||
| 100 iterations | TB | 71 | 8 | 91·02% | 92·20% | 89·87% |
| Weight threshold=100 | C | 6 | 71 | |||
| Tree classifier C5·0 (C5·0_1) | ||||||
| Boost=10 | TB | 72 | 10 | 90·38% | 93·51% | 87·34% |
| Global pruning 25% | C | 5 | 69 | |||
| Support vector machine (SVM_4) | ||||||
| Kernel=polynomial | TB | 71 | 9 | 88·46% | 92·20% | 84·81% |
| Soft margin=1 | C | 6 | 70 | |||
| SLP (SLP_3) | ||||||
| Normalised | TB | 68 | 12 | 86·54% | 88·31% | 84·81% |
| Shuffled presentation | C | 9 | 67 | |||
| MLP: 1 HL, 111 N (MLP) | ||||||
| Learning rate=0·3 | TB | 65 | 9 | 86·53% | 84·41% | 88·60% |
| Momentum=0·2 | C | 12 | 70 | |||
| Normalised 500 epochs | ||||||
Contingency table showing number of cases classified for each of the diagnostic classes. Codes in parentheses after classifier names refer to key of figure 1A. TB=tuberculosis; C=controls. ADTree=adaptive decision tree.22 C4·5 Tree.21 AdaBoost=adaptive boosting.23 SLP=single layer perceptron.19 MLP=multi layered perceptron.20 HL=hidden layers. N=neurons.
Figure 1.
Performance and validation of classifiers
(A) Classifier performance in ROC space. SVM_1, ADT_2, C4·5_2, C5·0_1, SVM_4, SLP_3, MLP: for names and parameters see table 3. ADT_1=Adaptive decision tree without AdaBoost. NCP_3=Non-conservative projection (normalised, random presentation). C5·0_2=C5·0 tree with winnowing. C4·5_1=C4·5 tree without AdaBoost. CP_2=conservative projection (normalised). NCP_2=non-conservative projection (normalised). Red line indicates convex hull. (B) Gaussian kernel Support Vector Machine performance (ten-fold crossvalidation). Each block of three bars shows the values for accuracy (red), sensitivity (green) and specificity (blue) obtained when the sigma Gaussian-kernel was optimised for each of these criteria. (C) Averaged ROC using ten-fold train crossvalidation with test. 100 randomly selected train and test sets with a train:test ratio [80:20]. Parameters were selected with a ten-fold crossvalidation on the train set and performance obtained in the test. Red line shows averaged ROC curve of classifiers obtained when kernel parameter is selected on accuracy criteria. Similar ROC curves were obtained when selecting on sensitivity and specificity (webfigure 1).
We applied a further test of generalisation performance of the SVM by ten-fold crossvalidation on the entire set of spectra (both training and testing), obtaining accuracy of 93·1% (SD 3·8), sensitivity of 94·4% (4·5), and specificity of 91·8% (8·8) when optimised for accuracy (figure 1B). We also evaluated the generalisation performance of the SVM by re-randomising the allocation of spectra to new training and testing sets, and varying the proportions of training to testing cases from 90:10 to 50:50. For 80:20 sets, we obtained values for accuracy, sensitivity, and specificity exceeding 90% (data not shown). The robustness of the SVM was further confirmed by its mean performance on 100 randomly generated 80:20 sets as shown in the ROC curve (figure 1C, webfigure 1), with an area under the curve of 0·96.
Coefficients of variation for peak intensity for spectra, derived from a single sample, run 25 times (six assays), were 15·6% (intra-assay) and 24·4% (interassay). These data were obtained by averaging values for nine of the highest amplitude peaks at the following m/z values: 5648, 6203, 6449, 6647, 8907, 9213, 9310, 9370, and 9419. As a further measure of reproducibility, 28 universal control spectra run at different times over a 6-month period were correctly classified as controls by the SVM classifier obtained in the ten-fold cross-validation.
We selected a subset of informative peak clusters for further evaluation by applying a correlation filter method to detect independently informative peaks.31 We ranked ten mass clusters with the highest positive, and ten with the highest negative, Pearson correlation coefficients. To study the discriminatory power of the selected 20 mass clusters we first paired each mass with every other (400 pairs) and trained SVM classifiers to diagnose tuberculosis cases. We ranked generalisation performance by accuracy and showed that 20 pairs (5%) of selected mass clusters gave accuracies greater than 80% and 17 of these combined negatively and positively correlated mass clusters (webfigure 2). No mass cluster pair achieved sensitivity of greater than 95% and specificity of greater than 85%, confirming that better generalisation relies on combinations of more than two mass peaks. Second, an SVM trained with just the 20 correlation-selected mass clusters achieved an accuracy of 89·7% on the independent test set, indicating that these clusters contain most relevant discriminatory information. Information in remaining peak clusters (n=199) retained an inferior, though acceptable, diagnostic accuracy (85·9%, figure 2A ), indicating that there was substantial residual diagnostic information in the remaining peak clusters. We summarised the generalisation performance of the SVMs in ROC space with different sets of mass clusters (figure 2A, webtable 1). The ROC convex hull (figure 2A, red line) is defined by two classifiers (figure 2A, red square and green square). The highest specificity (red square) was obtained with all peaks minus the ten that were positively correlated (209 in total), confirming information value in negatively correlated peaks. The other optimal classifier (figure 2A, green square) was obtained after using only ten positively and ten negatively correlated subsets of mass clusters.
Figure 2.
Performance of SVM classifiers based on subsets of peak clusters and combinations of identified biomarkers
SAA=serum amyloid A. CRP=C-reactive protein. Gaussian SVMs were trained with the initial train set (table 2) using the specified mass peak clusters or biomarker combination (ten-fold crossvalidation for parameter selection). Classifier performance was then assessed on initial test (table 2). (A) Classification performance of correlated mass clusters. 1=10 positively correlated and 10 negatively correlated; 2=remaining 199. 3=10 positively correlated; 4=remaining 209. 5=10 negatively correlated; 6=remaining 209. Raw values supplied in webtable 1. Red line represents convex hull defined by optimal classifiers (4 and 1). (B) Biomarkers. 1g=transthyretin. 2g=CRP. 3g=neopterin. 4g=SAA. 5g=neopterin-SAA. 6g=CRP-SAA. 7g=CRP-neopterin. 8g=transthyretin-SAA. 9g=transthyretin-neopterin. 10g=transthyretin-CRP. 11g=transthyretin-CRP-neopterin. 12g=transthyretin-CRP-SAA. 13g=transthyretin-neopterin-SAA. 14g=CRP-neopterin-SAA. 15g=transthyretin-CRP-neopterin-SAA. Raw values supplied in webtable 2. Red line represents convex hull defined by optimal classifiers (2g, 6g, 12g, 9g).
Using high-resolution mass-spectrometry after tryptic digestion, we identified an 11·5 kDa positive protein marker derived from serum amyloid A1 and a 13·7 kDa negative protein marker derived from transthyretin (webfigure 3). The molecular weight observed in the mass spectrum (13·7 kDa) for the protein identified as transthyretin corresponded closely to the theoretical value (13·76 kDa) for this protein. However, that observed for serum amyloid A1 (11·52 kDa) was 156 Da lower than its theoretical value (11·68 kDa) suggesting that the protein was a variant of serum amyloid A1. To investigate the nature of this variant, the tryptic digest was analysed in more detail and was found to include a peptide at m/z 1551 that did not correspond to a tryptic peptide predicted from the full amino acid sequence of serum amyloid A1. It did, however, correspond to the 2–15 peptide (SFFSFLGEAFDGAR) that would have resulted from loss of the N-terminal arginine.
To translate from proteomic signatures to conventional test formats, we measured serum amyloid A and transthyretin by immunoassay for all patients' serum. We also measured C-reactive protein and neopterin, which have previously been used to monitor disease activity in tuberculosis.32 We then selected the best polynomial and Gaussian kernel SVM parameters for these four markers. The best classifiers were obtained with Gaussian SVMs (figure 2B). The SVM classifier trained with transthyretin, C-reactive protein, and neopterin values discriminated patients with tuberculosis from controls with an accuracy of 84% (82% sensitivity, 86% specificity; figure 2B, black triangle). Other optimised classifiers were with serum amyloid A, C-reactive protein, and transthyretin (figure 2B, purple triangle; webtable 1) and C-reactive protein, neopterin, and serum amyloid A (figure 2B, green triangle; webtable 2).
To confirm our findings, we subsequently applied our classifiers to a second, independent test set, which was obtained by prospective collection of serum samples from patients attending two UK hospitals. Cases and controls were carefully matched for ethnic origin and a rigorous standardised protocol was followed for sample collection and processing. Most patients with tuberculosis had pulmonary disease, and the majority of controls had respiratory illnesses. Table 4 summarises the clinical data. A classifier trained on the spectra obtained in the first phase of the study discriminated cases of tuberculosis from controls in this completely new dataset, with a sensitivity of 88·9% and specificity of 77·2% (webtable 3). Moreover, the classifier trained on the 20 mass clusters highlighted in the correlation analysis achieved a sensitivity of 78% and specificity of 77%. A combination of the four immunoquantitated biomarkers achieved an accuracy of 81% (sensitivity 88%, specificity 74%; webtable 2).
Table 4.
Characteristics of patients and controls in second dataset
| Tuberculosis | Control | Total | ||
|---|---|---|---|---|
| Total number of patients | 18 | 23 | 41 | |
| Mean (range) age in years | 35 (18–61) | 32 (18–60) | 34 (18–61) | |
| Sex (male:female) | 12:6 | 7:16 | 19:22 | |
| Ethnic origin | ||||
| African | 10 | 13 | 23 | |
| Asian | 6 | 4 | 10 | |
| White | 2 | 6 | 8 | |
| Collection site | ||||
| UK (St George's Hospital) | 9 | 7 | 16 | |
| UK (Hammersmith Hospital) | 9 | 16 | 25 | |
| Symptoms | ||||
| Persistent cough | 14 | 13 | 27 | |
| Haemoptysis | 5 | 2 | 7 | |
| Night sweats/fever | 11 | 11 | 22 | |
| Weight loss | 6 | 3 | 9 | |
| Tuberculosis smear-positive | 10 | N/A | 10 | |
| Tuberculosis site of disease | ||||
| Pulmonary | 16 | N/A | 16 | |
| Extrapulmonary | 1 | N/A | 1 | |
| Pulmonary and extrapulmonary | 1 | N/A | 1 | |
| Abnormal chest radiograph | 14 | 11 | 25 | |
| Cavitary disease | 4 | 0 | 4 | |
| Previous BCG vaccination* | 7 | 16 | 23 | |
| Controls with respiratory infections | N/A | 15 | 15 | |
| Controls with inflammatory bowel disease | N/A | 4 | 4 | |
| Healthy volunteers | N/A | 4 | 4 | |
| HIV-negative† | 8 | 3 | 11 | |
Controls: 20 undetermined.
Data missing for ten patients with tuberculosis and six controls.
Tuberculosis: one HIV positive, nine undetermined.
Discussion
We investigated new approaches for diagnosing tuberculosis using serum from patients with the disease and controls from several countries, representing at least four different ethnic backgrounds. Despite the heterogeneity of the control group, our SVM diagnostic classifier discriminated accurately between patients with tuberculosis (both smear-negative and smear-positive) and those with other infective and non-infective inflammatory conditions. These results provide proof-of-principle that a diagnostic approach based on a proteomic signature can be applied to tuberculosis. If our classifier retained a similar diagnostic performance after validation in a population in an African tuberculosis clinic, where the prevalence of tuberculosis in patients presenting with respiratory symptoms might be around 10%, the positive and negative predictive values for our best classifier would be 67% and 99%, respectively. This diagnostic accuracy would surpass that of other available immediate diagnostic options, and could yield a result much more rapidly than culture.
However, although SELDI technology can provide a diagnostic test for tuberculosis that makes no previous assumptions about the identities of proteins constituting an informative signature, cost and complexity preclude its general use. We therefore identified two of the 20 most discriminatory proteins to demonstrate the possibility of implementing more conventional diagnostic assays that are adaptable for field use. These proteins (serum amyloid A and transthyretin), selected by Pearson correlation analysis and confirmed by SVM classification of proteomic signatures, have already been independently associated with pathophysiological processes in tuberculosis. Serum amyloid A is an acute phase protein that is associated with circulating high-density lipoprotein33 and modulates lipid trafficking and immune responses. It is the precursor protein in reactive amyloidosis, which complicates chronic tuberculosis in some individuals, and is a marker of disease activity in several inflammatory states, including tuberculosis.34 The ELISA assay used a commercially available antibody that recognises total serum amyloid A rather than the des-arginine subtype identified in the signature. Specific detection of this variant might further enhance diagnostic discrimination. Transthyretin is a 55 kDa homotetramer in serum and a major transporter of thyroxine and tri-iodothyronine, as well as vitamin A (retinol or trans-retinoic acid) through association with retinol-binding protein.35 Retinoic acid stimulates monocyte differentiation and inhibits multiplication of M tuberculosis in human macrophages.36 Low levels of vitamin A, correlating with reduced transthyretin and raised concentrations of C-reactive protein, have been reported in patients with tuberculosis.37, 38 A truncated form of transthyretin is a negative marker in proteomic fingerprinting studies on ovarian cancer;39 serum amyloid A is a positive marker in severe acute respiratory syndrome (SARS),12 and indicates relapse in nasopharyngeal cancer.40
Artefacts associated with collection and handling of samples or spectrum generation could create spurious classifications. Although collection biases were difficult to control because we also used archived samples, we sought to minimise postcollection bias by interspersing the processing of samples from cases and controls over months and by using samples from four geographical sites and with varying HIV serostatus. Another possible source of bias is the predominance of African patients in the tuberculosis group and white people in the controls. However, at least 58 of 170 controls were of sub-Saharan African origin. It is possible, although unlikely, that our classifiers detect the presence of tuberculosis infection rather than active disease. Tuberculin skin-test reactivity (as a questionable marker of latent tuberculosis) was not available for most control patients, but a substantial minority of the African and Asian control patients were probably latently infected. Moreover, the effectiveness of the classifier on the basis of the four biomarkers (three of which are inflammatory markers), provides evidence against discrimination between the groups on the basis of quiescent tuberculosis. Notably, of the five patients with tuberculosis misclassified by the SVM, three were Ugandan, whereas of the four misclassified controls, two were white. The diverse pathologies in the control group are also likely to have made correct classification more difficult. Furthermore, the findings are unlikely to have been biased by systematic differences in concurrent drug treatment, because only 12 of the patients with tuberculosis had started chemotherapy at the time of recruitment.
Nevertheless, biases could have been introduced because of the predominance of archived samples in the tuberculosis group (collected in Africa and derived from the WHO databank), compared with the control set. We therefore applied our trained classifier to a second, independent dataset that was collected prospectively at a later date in the UK, over 4 months. Patients in this dataset were more closely matched for ethnic origin and included a greater proportion of controls with respiratory disease than in the training set. All samples in the test set were processed with precisely the same standard operating protocol. The fact that the diagnostic performance of the classifiers survived rigorous testing in this new set strengthens the conclusions of the first part of the study. The small decrease in diagnostic accuracy might be at least partly attributable to the small size of the second dataset, and might also reflect the existence of some biases in the first dataset. The limitations of the SELDI-ToF platform with respect to reproducibility in peak intensity might also have an effect. For example, although we found average interassay coefficients of variation of about 24% for nine universally present peaks in our quality control spectra, there may be larger variations in low intensity peaks residing closer to noise. This suggestion is consistent with maintenance of greater diagnostic accuracy across two datasets seen with inherently less variable immunological assays, and strengthens diagnostic approaches that use two independent assays. A key advantage of SELDI-ToF MS lies in the discovery phase, which can profile large numbers of samples in a high throughput fashion, and by using whole signatures, reduce problems with individual variability in peak detection.
Although single protein markers might have insufficient accuracy in the diagnosis of tuberculosis, the use of proteome-guided analysis combined with machine learning methods such as SVMs can achieve better accuracy than that of current standard methods. These findings suggest that markers with low individual diagnostic specificities can boost diagnostic yields when used in particular combinations. In some cases, truncated or fragmented derivatives of common plasma proteins might be more specific markers of some diseases and arise by proteolytic enzyme induction characteristic of defined disease states.41 For example, the des-arginine variant of serum amyloid A we identified might be more specific than other variants for tuberculosis. Similarly, truncated forms of another apparently non-specific acute-phase protein, α1-antitrypsin, have been reported as relatively specific markers in SARS.12 Thus, a possible explanation for the apparent paradox that seemingly non-specific acute-phase proteins could provide diagnostic specificity for particular infections, is the possibility of disease-specific modification of common proteins, as has been proposed for several cancers.8
Preservation of high diagnostic accuracy when translating from proteomic signatures to immunoassays, and the plausible disease-association of the identified biomarkers, establishes the value of SVM classifiers for diagnosis of tuberculosis and provides strong evidence to support the use of serological testing. Although we have shown reasonable diagnostic accuracies based on a subset of four biomarkers as an illustration of the principle, better classifiers might ultimately require use of a larger number of biomarkers. To adapt the test for field use, antibodies to panels of defined biomarkers could be incorporated into dipstick-type formats, and patterns analysed with trained SVM classifiers on personal computers. These tests can then be applied to longitudinal studies of tuberculosis and other difficult diagnostic categories, such as sputum-negative tuberculosis, extrapulmonary cases, and paediatric infections.
Acknowledgments
Acknowledgments
DA and MP were Wellcome Trust Clinical Fellows sponsored by SK. DF-R is a Medical Research Council Fellow in Bioinformatics. AS was a Wellcome International Fellow. This investigation received financial support from the UNDP/World Bank/WHO Special programme for Research and Training in Tropical Diseases (TDR) (Project ID A20536). We thank Mark Perkins, the WHO TB databank, and Derek Macallan for serum samples, Angotrip for collaboration, Diane Irving for immunoassays, Gurjinder Sandhu for help in sample processing and Nathan Harris (Ciphergen, UK) for assistance in identification of proteins.
Contributors
The study was designed by D Agranoff, D Fernandez-Reyes, and S Krishna. D Fernandez-Reyes and M Herbster developed the machine-learning and feature selection analyses. D Fernandez-Reyes and S Rojas did classification experiments and produced the diagnostic SVM classifiers. A Loosemore, R Pollock, and C Rayner recruited patients and obtained serum samples in the UK. A Schwenk provided some of the UK tuberculosis serum samples. D Agranoff, M Papadopoulos, D Fernandez-Reyes, and E Tarelli generated the mass spectra. Protein identification was undertaken by D Agranoff with help from E Tarelli. J Sheldon coordinated and advised on immunoassays. Writing was by D Agranoff, D Fernandez-Reyes, and S Krishna, with contributions from all authors. D Agranoff and D Fernandez-Reyes contributed equally to this work.
Conflict of interest statement
St George's, University of London has applied for a patent to diagnose tuberculosis.
Web Extra Material
Averaged ROC using ten-fold train crossvalidation with test
100 randomly selected train and test sets with a train:test ratio [80:20] were created. Parameters were selected using a ten-fold crossvalidation on the train set and performance obtained in the corresponding test set. (A) Green line shows averaged ROC curve of classifiers obtained when kernel parameter is selected on sensitivity criteria. (B) Blue line shows averaged ROC curve of classifiers obtained when kernel parameter is selected on specificity criteria.
Classification performance in two-dimensional feature space of selected mass clusters ranked by accuracy
Tuberculosis=red dots. Controls=blue dots. Green line: decision boundary found by the classifier in the feature space induced by the kernel. Each box provides a visual representation of the discriminatory power of mass cluster pairs with achieved sensitivity (se) and specificity (sp).
Representative spectra from patient with tuberculosis (top) and control with bacterial pneumonia (bottom) showing locations of peaks corresponding to transthyretin and truncated variant of serum amyloid A
Misclassified samples
SVM classifiers performance on selected mass cluster peaks and biomarkers
SVM classifiers performance on selected mass cluster peaks and biomarkers of second dataset
Supplementary methods
References
- 1.WHO Global tuberculosis control-surveillance, planning, financing. Annex 1: Profiles of high burden countries. http://www.who.int/tb/publications/global_report/2006/annex_1_download/en/index.html (accessed April 7, 2005)
- 2.Mwinga A, Fourie PB. Prospects for new tuberculosis treatment in Africa. Trop Med Int Health. 2004;9:827–832. doi: 10.1111/j.1365-3156.2004.01274.x. [DOI] [PubMed] [Google Scholar]
- 3.Perkins M, Kritski AL. Diagnostic testing in the control of tuberculosis. Bull WHO. 2002;80:512–513. [PMC free article] [PubMed] [Google Scholar]
- 4.Perkins MD, Conde MB, Martins M, Kritski AL. Serologic diagnosis of tuberculosis using a simple commercial multiantigen assay. Chest. 2003;123:107–112. doi: 10.1378/chest.123.1.107. [DOI] [PubMed] [Google Scholar]
- 5.Drobniewski FA, Caws M, Gibson A, You ng D. Modern laboratory diagnosis of tuberculosis. Lancet Infect Dis. 2003;3:141–147. doi: 10.1016/s1473-3099(03)00544-9. [DOI] [PubMed] [Google Scholar]
- 6.Issaq HJ, Veenstra TD, Conrads TP, Felschow D. The SELDI-TOF MS approach to proteomics: protein profiling and biomarker identification. Biochem Biophys Res Comm. 2002;292:587–592. doi: 10.1006/bbrc.2002.6678. [DOI] [PubMed] [Google Scholar]
- 7.Duda RO, Hart PE, Stork DG. Pattern classification. 2nd edn. John Wiley and Sons; New York: 2001. [Google Scholar]
- 8.Petricoin EF, Liotta LA. SELDI-TOF-based proteomic pattern diagnostics for early detection of cancer. Curr Opin Biotechnol. 2004;15:24–30. doi: 10.1016/j.copbio.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Adam BL, Qu Y, Davis JW. Serum protein fingerprinting coupled with a pattern-matching algorithm distinguishes prostate cancer from benign prostatic hyperplasia and healthy men. Cancer Res. 2002;62:3609–3614. [PubMed] [Google Scholar]
- 10.Petricoin EF, Ardekani AM, Hitt BA. Use of proteomic patterns in serum to identify ovarian cancer. Lancet. 2002;359:572–577. doi: 10.1016/S0140-6736(02)07746-2. [DOI] [PubMed] [Google Scholar]
- 11.Papadopoulos MC, Abel PM, Agranoff D. A novel and accurate test for human African trypanosomiasis. Lancet. 2004;363:1358–1363. doi: 10.1016/S0140-6736(04)16046-7. [DOI] [PubMed] [Google Scholar]
- 12.Ren Y, He QY, Fan J. The use of proteomics in the discovery of serum biomarkers from patients with severe acute respiratory syndrome. Proteomics. 2004;4:3477–3484. doi: 10.1002/pmic.200400897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buhimschi IA, Christner R, Buhimschi CS. Proteomic biomarker analysis of amniotic fluid for identification of intra-amniotic inflammation. Bjog. 2005;112:173–181. doi: 10.1111/j.1471-0528.2004.00340.x. [DOI] [PubMed] [Google Scholar]
- 14.Special Programme for Research and Training in Tropical Diseases WHO/TDR TB specimen bank. http://www.who.int/tdr/diseases/tb/specimen.htm (accessed April 5, 2003)
- 15.Rathman G, Sillah J, Hill PC. Clinical and radiological presentation of 340 adults with smear-positive tuberculosis in The Gambia. Int J Tuberc Lung Dis. 2003;7:942–947. [PubMed] [Google Scholar]
- 16.Thiede B, Hohenwarter W, Krah A. Peptide mass fingerprinting. Methods. 2005;35:237–247. doi: 10.1016/j.ymeth.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 17.Perkins DN, Pappin DJ, Creasy DM, Cottrell JS. Probability-based protein identification by searching sequence databases using mass spectrometry data. Electrophoresis. 1999;20:3551–3567. doi: 10.1002/(SICI)1522-2683(19991201)20:18<3551::AID-ELPS3551>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 18.Cristianini N, Shawe-Taylor J. An introduction to support vector machines and other kernel-based learning methods. Cambridge University Press; Cambridge: 2000. [Google Scholar]
- 19.Rosenblatt F. Principles of neurodynamics. Spartan Books; New York: 1962. [Google Scholar]
- 20.McClelland JL, Rumelhart DE. Parallel and Distributed Processing. MIT Bradford Press; 1986. [Google Scholar]
- 21.Quinlan JR. C4.5: Programs for Machine Learning. Morgan Kaufmann; San Francisco: 1993. [Google Scholar]
- 22.Freund Y, Mason L. The alternating decision tree learning algorithm. In: Proceedings of the sixteenth international conference on machine learning. Morgan Kaufmann; San Francisco: 1999. pp. 124–133. [Google Scholar]
- 23.Freund Y, Schapire RE. Experiments with a new boosting algorithm. Thirteenth International Conference on Machine Learning; Bari: 1996. pp. 148–156. [Google Scholar]
- 24.Joachims T. Making large-scale SVM learning practical. Advances in kernel methods—support vector learning. MIT Press; Cambridge: 1999. [Google Scholar]
- 25.Witten IH, Frank E. Data mining: practical machine learning tools with Java implementations. Morgan Kaufmann; San Francisco: 2000. [Google Scholar]
- 26.Schweighofer A. Matlab interface to SVM light, Intelligent Data Analysis (IDA), Berlin, Germany. http://www.igi.tugraz.at/aschwaig/software.html (accessed January 2005)
- 27.Weston J, Elisseeff A, BakIr G. The spider. Department: Empirical Inference for Machine Learning and Perception, Max Planck Institute for Biological Cybernetics, Tübingen, Germany. http://www.kyb.tuebingen.mpg.de/bs/people/spider (accessed January, 2004)
- 28.von Eggeling F, Junker K, Fiedle W. Mass spectrometry meets chip technology: a new proteomic tool in cancer research? Electrophoresis. 2001;22:2898–2902. doi: 10.1002/1522-2683(200108)22:14<2898::AID-ELPS2898>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 29.Vapnik V. Statistical learning theory. John Wiley and Sons; New York: 1998. [Google Scholar]
- 30.Boser BE, Guyon IM, Vapnik VN. A training algorithm for optimal margin classifiers. Proceedings of the fifth annual workshop on computational learning theory; Pittsburgh: 1992. pp. 144–152. [Google Scholar]
- 31.Guyon I, Eliseeff A. An introduction to variable and feature selection. J Machine Learn Res. 2003;3:1157–1182. [Google Scholar]
- 32.Hosp M, Elliott AM, Raynes JG. Neopterin, beta 2-microglobulin and acute phase proteins in HIV-1-seropositive and -seronegative Zambian patients with tuberculosis. Lung. 1997;175:265–275. doi: 10.1007/pl00007573. [DOI] [PubMed] [Google Scholar]
- 33.Kiernan UA, Tubbs KA, Nedelkov D, Niederkofler EE, Nelson RW. Detection of novel truncated forms of human serum amyloid A protein in human plasma. FEBS Letts. 2003;537:166–170. doi: 10.1016/s0014-5793(03)00097-8. [DOI] [PubMed] [Google Scholar]
- 34.Salazar A, Pinto X, Mana J. Serum amyloid A and high-density lipoprotein cholesterol: serum markers of inflammation in sarcoidosis and other systemic disorders. Eur J Clin Invest. 2001;31:1070–1077. doi: 10.1046/j.1365-2362.2001.00913.x. [DOI] [PubMed] [Google Scholar]
- 35.Peterson PA. Characteristics of a vitamin A-transporting protein complex occuring in human serum. J Biol Chem. 1971;246:34–43. [PubMed] [Google Scholar]
- 36.Crowle AJ, Ross EJ. Inhibition by retinoic acid of multiplication of virulent tubercle bacilli in cultured macrophages. Infect Immun. 1989;57:840–844. doi: 10.1128/iai.57.3.840-844.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hanekom WA, Potgieter S, Hughes EJ, Malan H, Kessow G, Hussey GD. Vitamin A status and therapy in childhood pulmonary tuberculosis. J Pediatr. 1997;131:925–927. doi: 10.1016/s0022-3476(97)70046-5. [DOI] [PubMed] [Google Scholar]
- 38.Koyanagi A, Kuffo D, Gresely L, Shenkin A, Cuevas LE. Relationships between serum concentrations of C-reactive protein and micronutrients in patients with tuberculosis. Ann Trop Med Parasitol. 2004;98:391–399. doi: 10.1179/000349804225003424. [DOI] [PubMed] [Google Scholar]
- 39.Zhang Z, Bast RCJ, Yinhua Y. Three biomarkers identified from serum proteomic analysis for the detection of early stage ovarian cancer. Cancer Res. 2004;64:5882–5890. doi: 10.1158/0008-5472.CAN-04-0746. [DOI] [PubMed] [Google Scholar]
- 40.Cho WCS, Yip TTC, Yip C. Identification of serum Amyloid A protein as a potentially useful biomarker to monitor relapse of nasopharyngeal cancer by serum proteomic profiling. Clin Canc Res. 2004;10:43–52. doi: 10.1158/1078-0432.ccr-0413-3. [DOI] [PubMed] [Google Scholar]
- 41.Tolson J, Bogumil R, Brunst E. Serum protein profiling by SELDI mass spectrometry: detection of multiple variants of serum amyloid alpha in renal cancer patients. Lab Invest. 2004;84:845–856. doi: 10.1038/labinvest.3700097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Averaged ROC using ten-fold train crossvalidation with test
100 randomly selected train and test sets with a train:test ratio [80:20] were created. Parameters were selected using a ten-fold crossvalidation on the train set and performance obtained in the corresponding test set. (A) Green line shows averaged ROC curve of classifiers obtained when kernel parameter is selected on sensitivity criteria. (B) Blue line shows averaged ROC curve of classifiers obtained when kernel parameter is selected on specificity criteria.
Classification performance in two-dimensional feature space of selected mass clusters ranked by accuracy
Tuberculosis=red dots. Controls=blue dots. Green line: decision boundary found by the classifier in the feature space induced by the kernel. Each box provides a visual representation of the discriminatory power of mass cluster pairs with achieved sensitivity (se) and specificity (sp).
Representative spectra from patient with tuberculosis (top) and control with bacterial pneumonia (bottom) showing locations of peaks corresponding to transthyretin and truncated variant of serum amyloid A
Misclassified samples
SVM classifiers performance on selected mass cluster peaks and biomarkers
SVM classifiers performance on selected mass cluster peaks and biomarkers of second dataset
Supplementary methods