Summary
Rabies is one of the most deadly infectious diseases, with a case-fatality rate approaching 100%. The disease is established on all continents apart from Antarctica; most cases are reported in Africa and Asia, with thousands of deaths recorded annually. However, the estimated annual figure of almost 60 000 human rabies fatalities is probably an underestimate. Almost all cases of human rabies result from bites from infected dogs. Therefore, the most cost-effective approach to elimination of the global burden of human rabies is to control canine rabies rather than expansion of the availability of human prophylaxis. Mass vaccination campaigns with parenteral vaccines, and advances in oral vaccines for wildlife, have allowed the elimination of rabies in terrestrial carnivores in several countries worldwide. The subsequent reduction in cases of human rabies in such regions advocates the multidisciplinary One Health approach to rabies control through the mass vaccination of dogs and control of canine populations.
Introduction
In the 21st century, rabies remains as one of the most feared and important threats to public health. The untreated disease presents as a progressive encephalomyelitis, which is invariably fatal, and is caused by neurotropic viruses of the genus lyssavirus. As a neglected zoonotic disease, rabies is present throughout much of the world (figure 1 ), with many deaths in human beings occurring in Africa and Asia in children younger than 15 years. Rabies is regarded as under-reported in many regions,1 due in part to a lack of surveillance and laboratory infrastructure, confounded by cultural or social taboos.2, 3, 4 The absence of accurate data on disease incidence in turn tends to reduce rabies as a priority for policy makers and public health professionals.5, 6 Estimates of the global burden, based on models of incidence of dog bites, have been updated and augmented to include country-specific data from published studies and online surveys, giving a more comprehensive global estimate.7 Preliminary data suggest that almost 60 000 human deaths occur from rabies globally per year, which is more than that attributed to any other single zoonotic disease (table 1 ).8, 9 The large number of children among these fatalities means that rabies is estimated to cause more than 2 million disability-adjusted life-years (DALYs) lost per year, with an annual economic cost of more than US$4 billion per year.7 Other models have used estimates of values of statistical life to predict the economic impact of rabies. These values range from $1·8 to $2·2 million per human death—a value that does not take into account post-exposure treatments, livestock losses, and costs associated with diagnostic testing and vaccination.10 The total annual global costs of canine rabies alone are estimated to be of the order of tens of billions of dollars.10
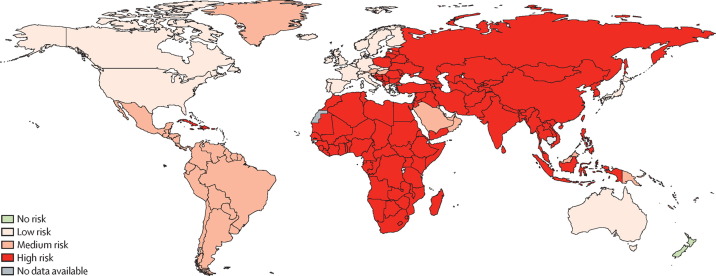
Figure 1.
WHO rabies risk map
Data from WHO. Most of the cases of human rabies occur in Africa and Asia. Attempts to accurately map the distribution of rabies risk or incidence show the absence of quantitative data and the irrelevance of political boundaries in the control of a disease with animal reservoirs. In low-risk areas, pre-exposure immunisation is recommended for individuals who will come into contacts with bats. In medium risk areas, pre-exposure immunisation is recommended for individuals who will come into contact with bats and other wildlife. In high-risk areas, pre-exposure immunisation is recommended for individuals who will come into contact with domestic animals such as dogs, and other rabies vectors.
Table 1.
Global morbidity and mortality from zoonotic diseases
|
Morbidity |
Mortality |
|||
|---|---|---|---|---|
| Cumulated | Annual | Cumulated | Annual | |
| SARS coronavirus | 8273 | .. | .. | .. |
| Highly pathogenic avian influenza | 610 | .. | 360 | .. |
| Ebola virus | 2288 | .. | 1531 | .. |
| Japanese encephalitis virus | .. | 50 000 | .. | 10 000 |
| Rabies | .. | 20 million receiving PEP | .. | 59 000 |
Dogs are the principal vector for human rabies, and are responsible for more than 99% of human cases. Hence controlling rabies in dogs, and especially free-roaming (stray) dogs, is the first priority for prevention of human rabies.11, 12, 13 The disease causes a severe and long-lasting societal and economic burden and the implications are especially apparent in poverty-stricken developing countries. Shortage of resources and a limited public health infrastructure in many rabies-endemic countries precludes data collection and analysis. Rabies has been successfully controlled in dog populations throughout the Americas, and rabies in both dog and terrestrial wildlife populations has been successfully eliminated from western Europe. Thus, rabies can be controlled with sufficient resources. Alongside the burden of rabies in terrestrial animals, many novel lyssaviruses causing clinically indistinguishable disease have been detected. Most virus species identified have been detected in bats, and include species that are antigenically distinct from current vaccine strains.
The aim of this Seminar is to review available information on rabies, including the causative lyssaviruses, and disease transmission, management, and prevention. We will also discuss new developments in rabies research including advances in the epidemiology of new lyssavirus species and the threat they pose to human health, methods for detecting rabies virus in human tissue samples, advances in the management of patients with rabies, and the development of new biologicals to potentially replace human rabies immunoglobulin with cost-effective alternatives. These developments enhance the efforts made towards the overall goal of human rabies elimination.
Rabies virus
The causes of rabies are RNA viruses belonging to the genus lyssavirus within the family Rhabdoviridae, order Mononegavirales. Rabies virus (RABV) is the type species and is responsible for most cases in human beings and animals. However, cases of rabies involving human infection with the other lyssaviruses have also been reported and, from these cases, it seems most lyssaviruses cause indistinguishable fatal encephalitis in humans.14 Fatal cases of encephalitis caused by lyssavirus species other than RABV are extremely rare. However, surveillance capable of distinguishing different lyssaviruses in many endemic regions is not comprehensive. The International Committee on Taxonomy of Viruses delineates the lyssavirus genus into 12 different virus species and two tentative virus species based on genetic distance, antigenic profiles, geographic distribution, and host range.15 Genetic evidence for an additional lyssavirus has been reported in Spain16 (figure 2 , appendix).
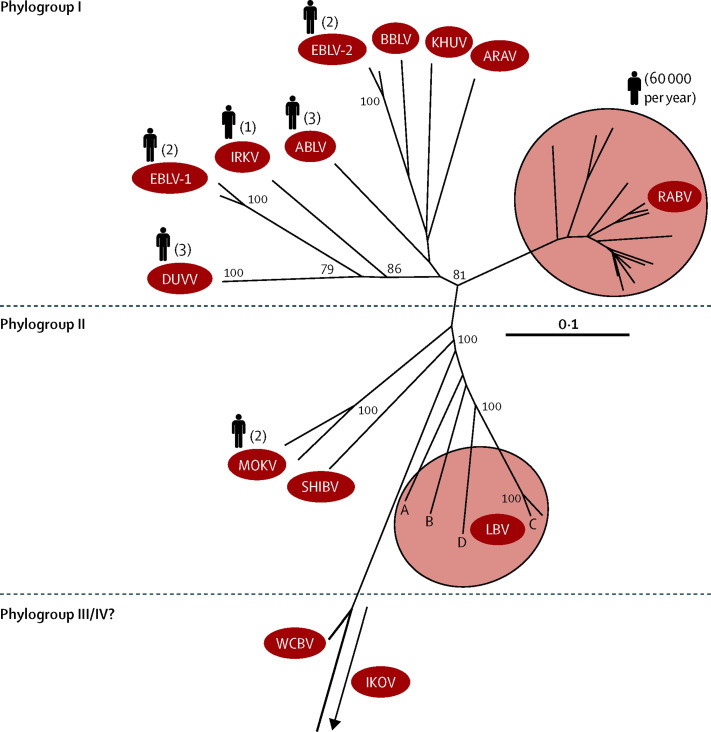
Figure 2.
Phylogenetic tree of the lyssavirus phylogroups and their respective species
Nucleoprotein sequences (405 nucleotides) were aligned with ClustalW and the phylogenetic tree was visualised using TreeView version 3.2. Bootstrap values at relevant nodes are shown. According to the proposed antigenicity of each group of isolates, the viruses are divided into different phylogroups. Where available, accession numbers for sequences are rabies virus (RABV AY102999, AY062068, AY103008, AY062069, AY102993,AY352514, AY330735, AY062090, AY062070, AY062047), Lagos bat virus (LBV EF547459, EF547449, EF547447, GU170202), West Caucasian bat virus (WCBV EF614258), Shimoni bat virus (SHIBV GU170201), Mokola virus (MOKV AY062074,AY062077), Duvenhage virus (DUVV AY062079), European bat lyssavirus type 1 (EBLV-1 AY062088, EF157976), Irkut virus (IRKV EF614260), Australian bat lyssavirus (ABLV AF418014), European bat lyssavirus type 2 (EBLV-2AY062091, AY062089), Bokeloh bat lyssavirus (BBLV JF311903), Khujand virus (KHUV EF614261), Aravan virus (ARAV EF614259), and Ikoma lyssavirus (IKOV JX193798). Several sequences within the phylogeny are unpublished and as such do not have accession numbers. The scale bar represents 0·1 substitutions per nucleotide site. The number of human cases are shown next to silhouettes where reported.
The antigenic and genetic profiles of the lyssavirus genus allow further segregation into phylogroups (figure 2).15, 17 Antibodies raised experimentally in mice against inactivated virus from one phylogroup neutralise viruses within that phylogroup but not others. Antibodies raised against West Caucasian bat virus do not cross-react with any members of the two main phylogroups.1, 18 The degree of cross-neutralisation predicts the likely efficacy of RABV-derived post-exposure prophylaxis. Protection mediated by the vaccine is inversely related to the genetic distance between the infecting virus isolate and rabies vaccine strain.17, 19, 20, 21
From a pathogenesis perspective, RABV, when experimentally injected in mice intracranially or when delivered via peripheral routes (eg, intramuscularly or subcutaneously) will cause fatal encephalitis. By contrast, although lyssaviruses are regarded as neurotropic agents, experimental studies with two lyssaviruses, Lagos bat virus and Mokola virus (MOKV), showed that no disease was evident when the viruses were injected via peripheral routes. This phenomenon was explained by aminoacid substitution Arg/Lys to Asp in the glycoprotein ectodomains.22 This generalisation has recently been challenged in further studies that suggest that pathogenic properties vary between virus strains within lyssavirus species.23, 24
Bats are thought to be the reservoir for lyssaviruses, with the exceptions of MOKV and Ikoma lyssavirus, for which the reservoir species have yet to be identified.25 RABV is detected extensively in bat species throughout the New World (the Americas) but not in bats elsewhere, whereas the non-RABV lyssaviruses have only been detected in Old World bat species (in Africa, Europe, and Asia).26 Furthermore, RABV is present extensively in terrestrial carnivore species across the globe26 whereas the remaining lyssaviruses are rarely detected in non-flying species. All mammals are susceptible to infection but few are capable of acting as long-term reservoirs for disease. RABV might have evolved in the order Chiroptera (ie, bats) and then later crossed into the order Carnivora (ie, terrestrial carnivorous mammals).22
Lyssaviruses are enveloped with a host-derived membrane and have a bullet-like or bacilliform shape that contains a non-segmented negative sense RNA genome (appendix). This genome is about 12 kilobase pairs in length and encodes genes for five proteins: N (nucleoprotein), P (phosphoprotein), M (matrix protein), G (glycoprotein), and L (RNA dependent RNA polymerase). The N, P, and L proteins, with the viral RNA, form the ribonucleoprotein complex, which is surrounded by the lipid envelope associated with M and G proteins. The G protein forms trimers and is the primary surface antigen to which neutralising antibodies bind. The nucleoprotein protects the viral RNA from innate immune recognition but also contains several antigenic sites that act as a major target for T helper cells (adaptive immune response).27, 28 The negative polarity of the RNA genome means that by itself it is non-infectious because it must first be transcribed to produce complementary positive sense mRNAs that are then translated by host cell machinery into the five proteins.29
Binding of lyssaviruses to host cells is dependent on the glycoprotein, which binds to one of several proposed receptors that facilitate virus entry.30 In vitro, lyssaviruses seem able to infect a diverse range of cell lines of different lineages, although the mechanisms of entry into various cells that do not express recognised receptors is unclear.31 However, carbohydrate moieties, phospholipids, sialylated gangliosides, and various undefined proteins associated with the membrane are thought to act as potential binding ports.32, 33, 34
After entry via the endocytic pathway, virus replication and transcription take place in neuronal cells in cytoplasmic inclusions termed Negri bodies,35, 36, 37 previously thought to be dumping grounds for excess viral proteins.35, 38, 39 Lyssavirus genomes seem to have evolved to produce optimum levels of each viral protein as evidenced by conserved gene order and the presence of intergenic regions that contain signals for transcriptional initiation, termination, and polyadenylation. For lyssaviruses, the intergenic regions vary in composition and length, and the application of reverse genetics to the study of these viruses has shown that individual intergenic regions have a specific role in gene expression.40 The M protein also has an important role in regulation of gene expression by inhibition of transcription and enhancement of replication, although the mechanisms and regulatory sequences involved in this model of transcription need further study.41, 42 Virus budding from the host cell is largely facilitated by the M protein.41, 42
Rabies virus is most commonly transmitted by the bite of a rabid animal (appendix). This mechanism enables the virus to transverse the dermal barrier and deposit the virus into tissues in which it can initiate infection (figure 3 ).43 Hosts that do not contribute to onward transmission, including human beings, are termed dead-end hosts. Transmission between human beings has only occurred in exceptional circumstances, including corneal and organ transplantation.44, 45 Transmission of rabies virus by aerosol exposures46, 47 or transplantation of tissues or organs is rare, but has been reported.
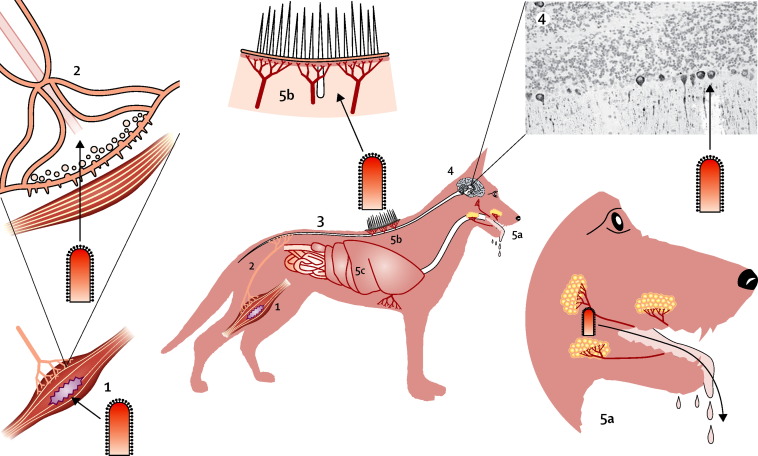
Figure 3.
Pathogenesis of rabies virus
Reproduced from Singh and Ruzek,43 by permission of Taylor & Francis. 1) Virus enters muscle tissue of host through bite wound, then 2) enters the peripheral nervous system (PNS) via neuromuscular junction, and then 3) travels from PNS to spinal cord and brain. 4) Virus enters brain and undergoes extensive replication leading to neuronal dysfunction (slide shows virus in Purkinje cells of cerebellum 40x magnification). 5a) The virus replicates in salivary glands and is excreted in saliva, 5b) enters peripheral nerves of skin and Purkinje cells, and 5c) spreads from the brain to infect many tissues and organs in the host.
Pathogenesis
Once infection is established within neuronal cells the virus usurps host cell machinery to reach cell bodies in the spinal cord or brainstem or in sensory ganglia (eg, dorsal root ganglia) where replication occurs. The motility of RABV along neuronal processes has been exploited to map neuronal circuitry.48, 49 The virus is transported by fast axonal transport through the spinal cord to the brain. Until this stage the patient shows no clinical signs. Host detection of virus intracellularly occurs through the retinoic acid-inducible gene 1 pathway50 through the detection of cap structures on the virus mRNAs and through Toll-like receptors.51 This detection stimulates an early interferon response that is antagonised by the virus phosphoprotein.52, 53 The mechanism of interferon antagonism seems to be conserved between many of the lyssaviruses.54, 55 Once in the CNS, the virus replicates extensively and clinical disease develops. Notably, fatal encephalitic rabies might not necessarily be accompanied by substantial inflammation and this feature could, in part, be due to the genetics of the infecting virus. This variability in inflammatory response is also seen in cases of dog rabies. Furthermore, neuronophagia can vary substantially and neuronal apoptosis does not seem to have an important role in rabies encephalitis in human beings.56 Nonetheless, extensive infection of the brain leads to centrifugal dissemination of virus through neurons to distant sites throughout the body. Of particular importance in reservoir species is the spread of the virus to peripheral sites that release the virus into the oral cavity via the salivary glands. Rabies virus antigen staining of the taste buds has also been observed.57, 58, 59 The salivary glands are innervated from the parasympathetic nervous system via the submandibular ganglion and glossopharyngeal nerves, by sympathetic innervation via the superior cervical ganglion, and by afferent innervation.60, 61 Ultrastructural studies suggested that the virus is able to travel from the brain to peripheral sites by budding on synaptic or adjacent plasma membranes of dendrites with budding also occurring, albeit less often, from the plasma membrane of the perikaryon.62 Detection of virus particles engulfed by an invaginated membrane of an adjacent axonal terminus suggested transneuronal dendroaxonal movement. However, alongside this finding, virus has also been reported to bud directly into the intercellular space, which along with hypersalivation and the aggressive behaviour often associated with infection, promotes onward transmission of the virus to new hosts (figure 3).
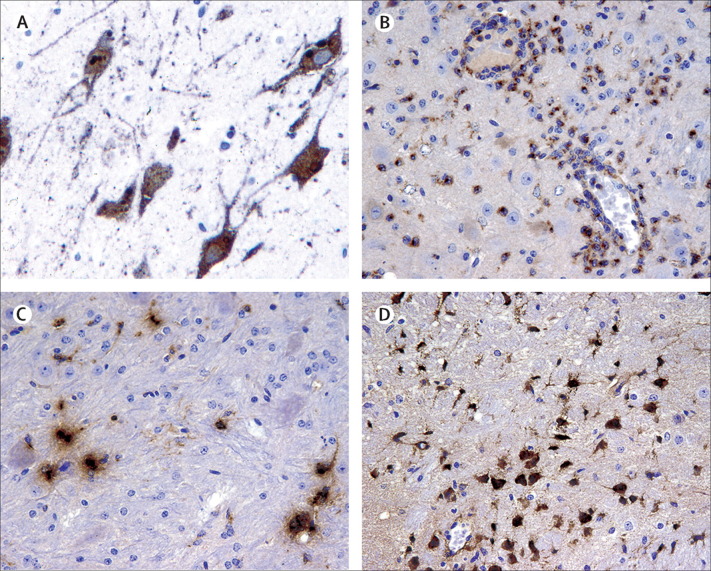
Cause of death as a result of infection with rabies virus has not been irrefutably established. Overwhelming virus replication in the nervous system leads to many systemic complications, including multiorgan failure. Experimental studies show strong evidence for upregulation of interferons, cytokines, and chemokines in the CNS in response to infection with rabies virus.63, 64 Transcriptomic studies have shown the upregulation of many interferon-inducible genes65, 66 and this upregulation has been supported by immunohistological demonstration of chemokine production in neurons. Such production drives an influx of immune cells into the CNS, particularly T cells. However, in the case of rabies virus infection, this influx does not control infection and the host invariably dies. In the absence of therapeutic options no mechanisms exist to ameliorate rabies virus replication once the virus reaches the brain. Evidence for an immune response is not detected until the virus has entered the CNS64, 67 (figure 4 ). How the virus avoids immune surveillance in the periphery is unknown, but might be attributable to the low level of replication early in the infection or activation of immune suppression in the periphery.55, 68
Figure 4.
Immunohistochemical detection of rabies virus nucleoprotein and chemokines in infected tissue
Immunohistochemical detection of rabies virus nucleoprotein (brown staining) in human neurons (A). Section prepared from a brain sample from a human case of rabies in the UK. Magnification, ×200. Immunohistochemical staining for chemokines within the brain of mice infected with rabies virus (B–D). Specific staining for CCL2 (B), CCL5 (C), and CXCL10 (D) are shown. Magnification ×200.
Clinical presentation
Two clinical forms of rabies disease are typically described: encephalitic (furious) and paralytic (dumb). The earliest neurological symptom in human beings is usually pain, paraesthesia, or pruritus at the site of infection because of viral replication in local dorsal root ganglia and associated ganglionitis.69 After the prodrome, either the encephalitic or paralytic forms of the disease might be observed. Encephalitic rabies often presents with hypersalivation, and periods of agitation alternating with lucidity will be observed—a key feature of the so-called “furious” type of rabies. Importantly, patients with hypersalivation have difficulty swallowing the excessive saliva produced (video 1). RABV nucleic acid might be detected in saliva samples taken at this stage. Hydrophobia is also often observed, and in developing countries water might be offered to suspected patients for diagnostic purposes (video 2). As hydrophobia progresses, the offer of water leads to pharyngeal spasms and involuntarily refusal of the water with excessive gagging being noted (video 3). Infection invariably leads to coma and death. The paralytic form of disease differs from the encephalitic form in that muscle weakness develops early (which is not observed in the so-called furious form of the disease), and progression to coma and death often takes longer than with the encephalitic form.69
Bat rabies is caused by RABV in the New World whereas across the Old World infection is caused by other lyssaviruses; in these regions, human infections with the bat lyssaviruses are reported rarely.1, 29 However, the true burden of human and animal cases caused by lyssaviruses other than RABV is unknown because the causative lyssavirus cannot be readily distinguished with standard diagnostic tests.14, 17, 70
Historically, Duvenhage virus (DUVV) was the first non-rabies lyssavirus associated with human infection, although earlier potential infections with European Bat Lyssavirus type 1 (EBLV-1) are unconfirmed.71 DUVV was first reported in the 1970s after diagnosis of rabies-like disease in an individual in South Africa who died after a bat bite.72 Since this initial isolation, two further cases of DUVV in people have been reported, both with a fatal outcome.73, 74 Of the other African lyssaviruses only Mokola virus has been associated a human fatality (reported in Nigeria).75 Infection with Eurasian lyssaviruses1 in human beings have also been reported, including confirmed fatalities from EBLV-1 infection,76, 77, 78 EBLV-2,79, 80 and Irkut virus.81 As well as these infections, Australian bat lyssavirus has caused three human fatalities.82, 83, 84 Although all of these infections have resulted in fatalities, several studies have reported the presence of neutralising antibodies in people who have not been vaccinated.85 Such findings suggest that natural immunisation can occur in human beings.86
Diagnosis
Infection with rabies virus can be difficult to diagnose ante-mortem.69 Although hydrophobia is highly suggestive, no clinical signs of disease are pathognomonic for rabies and differential diagnosis can involve many agents and syndromes (eg, other viral encephalitides, tetanus, listeriosis, and poisoning) and coinfections, such as malaria, can lead to misdiagnosis.87 Historical reliance on the detection of accumulations of Negri bodies is no longer regarded as suitable for diagnostic assessment because of low sensitivity, and alternative laboratory-based tests have been developed to conclusively confirm infection.
Most diagnostic tests for rabies virus in animals need brain material for diagnosis and as such are often only possible post mortem. Brain samples are most readily taken by breaching the skull and sampling directly. Brain smears or touch impressions are used for the detection of virus antigen with the fluorescent antibody test (FAT) for both human and animal samples. The FAT is recommended by WHO and the World Organisation for Animal Health (OIE) and, in 95–99% of cases, gives reliable results on fresh specimens within a few hours. To avoid the need for expensive fluorescently labelled antibodies and fluorescent microscopes, a histochemical test (direct rapid immunohistochemical test; dRIT) that allows the use of low-cost light microscopy has been developed. dRIT can detect rabies antigen in fresh brain impressions within 1 h.88 Development of dRIT will enable transfer of this diagnostic capability to endemic regions where cost precludes laboratory confirmation.89 Alongside FAT, the OIE recommends the use of a virus isolation test, particularly when FAT results are equivocal and for cases of human exposure. In-vitro isolation tests can be used to grow the virus from suspect samples with the added value of virus isolation for downstream characterisation and research activities. Molecular-based techniques are also becoming more widely accepted and accessible for the diagnosis of rabies,90 and PCR techniques have been used to confirm the origin of virus isolate. Such techniques are useful when cryptic cases occur, in which a clear history of exposure to rabies virus cannot be established despite extensive investigation. Confirmatory diagnosis with OIE-prescribed tests can only occur post mortem. For the future, the various conventional RT-PCR-based protocols and novel molecular protocols developed for the diagnostic amplification of lyssavirus genome fragments might overcome this obstacle,89 and offer an additional advantage in their ability to differentiate between species.
Ante-mortem diagnostic tests are reliant on widespread dissemination of the virus through the nervous system. Ante-mortem testing is not routinely applied to cases of animal infection. Antigen detection in skin biopsies can be used as a means of detecting infection when virus antigen can be detected in nerve fibres surrounding hair follicles.91 Rabies virus nucleic acid can also be detected in various biological fluids and samples (eg, saliva, cerebrospinal fluid and skin biopsies) by RT-PCR.92 Virus shedding in saliva is often used for ante-mortem testing; however, although saliva is a highly accessible sample, shedding is intermittent and can cease on seroconversion.67 Sensitivity with RT-PCR on single saliva samples has been reported as low as 70%, but similar tests on multiple successive saliva samples, or on nuchal skin biopsies have had a sensitivity of more than 98%.91 Cessation of viral shedding after seroconversion requires that a nuchal skin biopsy should also be taken when possible.67 For ante-mortem diagnostic assessment, all results should be carefully considered in combination rather than relying on individual diagnostic readouts.
Management
Medical care of patients with rabies is challenging for all physicians, especially in regions where there is little experience of the disease or the complex treatment issues.93 Critical care should be used as required pending confirmation of a laboratory diagnosis of rabies and when an aggressive approach is deemed necessary, although the chance of a successful outcome is very low. A palliative approach should include liberal use of sedatives and analgesics as needed to achieve comfort. Unfortunately, no effective therapy exists for rabies after the development of clinical disease. Clinical management of rabies has included a combination of therapies, rabies vaccine, immunotherapies, and ketamine.93 Ten people have survived rabies, including one who received pre-exposure immunisation and eight who received one or more doses of post-exposure prophylaxis before the onset of rabies; all but one of these individuals had neurological deficits and two died within a few years.94, 95 One individual who survived without post-exposure prophylaxis did so after the administration of an aggressive combination of medical treatments including the induction of a therapeutic coma, combined with ribavirin, ketamine, and amantadine treatment.96 This approach, dubbed the Milwaukee protocol, gave initial promise as a novel treatment to combat clinical rabies.97 However, attempts to repeat this first success have failed in at least 26 subsequent cases, suggesting that the protocol is ineffective.98
Excellent medical care in a critical care unit is important, but no specific therapeutic drug is known to effect a positive outcome. There are several factors that should be regarded as favourable in the decision to initiate an aggressive therapeutic approach: therapy with doses of rabies vaccine before the onset of illness, young age, previously healthy and immunocompetent individual, mild neurological disease at the time of initiation of therapy, rabies due to a New World bat rabies variant (eg, by contrast with a canine variant or Old World bat variant), and the early detection of neutralising antirabies virus antibodies in serum and cerebrospinal fluid.98 An effective therapy for rabies is unlikely to be developed in the future with a trial and error approach, especially because numerous neuroprotective drug studies have failed to show efficacy for any one drug.99 To develop a therapy for rabies a much better understanding of basic mechanisms involved in the pathogenesis of the disease is needed.61, 69, 98 Such knowledge might help in the development of an effective therapeutic intervention. Cooling of the brain (hypothermia) has also been considered a potential therapy.98
Vaccination of human beings
Pre-exposure prophylaxis vaccination
Early rabies vaccines were based on crude preparations of animal neuronal tissues that were poorly immunogenic and needed several doses to induce immunity. In the 1940s, these nerve tissue vaccines were replaced with more immunogenic and safer cell-culture-derived vaccines (CCVs).100 Despite official recommendations to discontinue use of nerve tissue vaccines some countries still produce and administer these vaccines. For CCVs, clinical trials have enabled a reduction in the numbers of doses administered, in turn increasing patient compliance with the treatment, as well as enabling alternative routes of administration to be adopted.100 WHO and the Advisory Committee on Immunization Practices recommend a single pre-exposure prophylaxis (PrEP) regimen (table 2 ). PrEP is also strongly recommended for travellers to endemic countries,101 and, because of waning antibody titres after PrEP, pre-exposure booster vaccine doses are also recommended. Booster vaccinations need to be administered in accordance with the vaccine manufacturer's recommendations.102 Pre-exposure vaccination is given as a three-dose schedule of intramuscular or intradermal injections on days 0, 7, and 21 or 28, where day 0 is the day of the first dose.103 For individuals at risk of exposure, booster doses could be administered dependent on individual maintenance of neutralising antibody titres, and the relative risk.100 Often, travellers fail to obtain PrEP because they do not understand the level of risk of rabies at their destination.102
Table 2.
Pre-exposure and post-exposure rabies vaccination regimens recommended by the WHO and the Advisory Committee on Immunization Practices by regimen
| Number of vaccine doses/number of clinic visits | Administration route | Schedule of injections | |
|---|---|---|---|
| Pre-exposure | |||
| Routine intramuscular | 3/3 | Intramuscular | Days 0, 7, and 21 or 28 (one dose each) |
| Routine intradermal | 3/3 | Intradermal | Days 0, 7, and 21 or 28 (one dose each) |
| Post-exposure | |||
| Essen | 5/5 | Intramuscular | Days 0, 3, 7, 14, 28 (one dose each) |
| Zagreb | 4/3 | Intramuscular | Days 0 (two doses), 7, 21 (one dose each) |
| Reduced four dose | 4/4 | Intramuscular | Days 0, 3, 7, 14 (one dose each) |
| Modified Thai Red Cross | 8/4 | Intradermal | Days 0, 3, 7, 28 (two doses each) |
| Post-exposure for previously vaccinated people | |||
| Two-dose intramuscular | 2/2 | Intramuscular | Days 0, 3 (one dose each) |
| Four-dose intradermal | 4/1 | Intradermal | Day 0 (four doses) |
The development and mass production of inactivated CCVs in the 1960s allowed a new approach to rabies control.100, 104 For the first time, human rabies vaccines were readily available for use before exposure to protect vulnerable individuals, rather than being exclusively employed for post-exposure prophylaxis. Although adults and children are equally susceptible to rabies and the prevention does not vary with age, rabies should be considered in the catalogue of paediatric diseases in endemic regions since about 40–50% of the annual death toll are children younger than 15 years.7, 105 To prevent rabies, PrEP could be given to children in these endemic regions in early childhood but this strategy is rare in low-income countries. A cost-benefit analysis of adoption of rabies vaccination in paediatric regimes concluded that for economic viability a novel formulation that induces immunity after a single inoculation is needed.106 Importantly, all licensed rabies vaccines have a good safety record with only rare adverse events, which do not differ according to age group.107
After vaccination, the present standard correlate of immunity is the development of neutralising antibodies.108 Memory and recall responses have been poorly studied in response to vaccination, despite the consistent waning of antibody responses in long-term follow-up studies of vaccine recipients.64 This waning might relate to the use of inactivated virus in current rabies vaccines.
Post-exposure prophylaxis
Every year, the application of post-exposure prophylaxis provides more than 20 million treatments and has been an effective counter-measure to rabies virus infection for more than 100 years.109 Rabies is preventable via several approved post-exposure prophylaxis recommendations, which consist of thorough wound-cleansing and prompt administration of rabies immune globulin (RIG), together with a full course of rabies vaccination (table 2). Wounds should be cleansed with soap or a virucidal antiseptic (eg, povidone iodine) with copious irrigation and should not be sutured unless absolutely necessary.
Post-exposure prophylaxis should be started as soon as possible after a recognised exposure110 and includes a series of injections of rabies vaccine. Four different post-exposure prophylaxis vaccine regimens are currently approved for individuals not previously vaccinated against rabies (table 2); three are given intramuscularly and one is given intradermally. RIG is also an important component of post-exposure prophylaxis to inhibit viral spread in the interval before sufficient immunity is developed in response to vaccination. It should be injected into and around the wound site, ideally on the day of exposure or up to 7 days after the initial dose of vaccine.100 Two WHO-approved regimens also exist for previously vaccinated individuals (table 2). In such cases RIG should not be given.100, 110
An animal bite is the most common exposure to rabies infection (appendix), and exposure of open wounds or mucosal membranes to saliva, nasopharyngeal fluids, or CNS tissues from infected animals is less common. Irrespective of the source of exposure, post-exposure prophylaxis should be started promptly and the suspect animal monitored for a period of 10–14 days. If the animal remains healthy after this period of observation, then post-exposure prophylaxis can be discontinued. If the suspect animal becomes ill during the observation period then full PEP should be continued following WHO guidelines. In other animals that are potential vectors, rabies can be excluded with a negative laboratory examination of the brain by FAT or, if the animal cannot be tested (eg, if it escaped or is valuable), then post-exposure prophylaxis should be started unless information from local public health officials suggests that it is unnecessary.
The availability of RIG is low in some rabies-endemic regions. Even when available, a lack of medical awareness of the importance of RIG in post-exposure prophylaxis means that its use is often not considered.111 The expense and scarcity of RIG has driven the search for alternative prophylactic methods that could be made available to rabies endemic areas. The manufacture of a cocktail of selected rabies monoclonal antibodies, which is capable of neutralising a broad range of RABV isolates from across the globe, to replace RIG, might further promote the use of passive immunity in rabies endemic areas where it is most needed.112 These preparations are undergoing clinical trials.113, 114 Application of the monoclonal antibody principle to the plant biotechnology sector offers a further promising direction for novel preparations where monoclonal antibody cocktails generated in plants enables ease of increased production and are economically advantageous.115, 116
Development of recombinant rabies vaccines has been proposed through the application of reverse genetics to generate rabies viruses with modified properties.108 Ideally, to generate more robust memory responses, vaccine preparations could involve live-attenuated virus to elicit a strong memory response, although use as either a pre-exposure or post-exposure option requires extensive development.117 Most progress in this area has been made with post-exposure treatment of experimental rabies in animals, rather than post-exposure prophylaxis in the manner of licensed vaccines. Prominent among these new prototype vaccines that may be licensed in the future for treating rabies is the so-called TriGAS construct that contains three copies of the glycoprotein gene.118 Overexpression of the glycoprotein gene by this construct stimulates a strong immune response and simultaneously seems to attenuate the infection.119 In the near future, such viruses will probably gain acceptance in veterinary vaccination. Oral vaccination with attenuated strains is commonplace in Europe although often, the cause of attenuation has not been deduced, and as such reversion to virulence is a concern. Molecular manipulation of vaccine strains with reverse genetics enables the mechanisms of attenuation to be investigated, which can then be applied to safely attenuate RABV, preventing possible reversion to virulence.120
Future challenges
A high proportion of cases of rabies involve childhood fatalities, and therefore rabies should be considered an important paediatric disease.121 The combination of an existing rabies human vaccine with a standard childhood vaccine regimen should be a priority to ensure global vaccination against rabies of children living in low-income countries. This strategy would involve the incorporation of rabies vaccination into the existing childhood Expanded Programme on Immunization (EPI) schedule.103 The addition of rabies vaccine into an existing multivalent paediatric vaccine as part of a childhood EPI schedule should ideally include a single-dose vaccine, preferably by a non-injectable route of administration.122 Unlike other viruses targeted for elimination, rabies will never be eradicated because of the presence of lyssaviruses in bats.26, 123 The realistic aim in the 21st century is to enhance efforts towards the elimination of rabies in dogs with the resultant reduction of human mortality,2, 11 a goal that has already been achieved in several regions.124, 125, 126, 127 The strategic approach for programmes aimed at the elimination of canine rabies should focus on a multidisciplinary core of disparate groups, including representatives from public and private sectors (ie, vaccine manufacturers, policy makers, scientists, veterinarians, and clinicians) with the overall vision of elimination of human rabies.128 This collaborative multidisciplinary initiative, often termed the One Health approach, is a step towards combating rabies through the mass vaccination of dogs and humane management of dog populations.129 Financial support for these initiatives will be needed. Such programmes are at present paid for by charitable foundations, sponsors, and financial donors working in partnership with global institutions.10 Alongside these measures the OIE have developed an animal vaccine repository that it uses to supply various regions with vaccine.126, 130, 131 The Food and Agriculture Organization of the United Nations has proposed a Progressive Control Pathway towards rabies elimination, with the final stage of the pathway being the maintenance of a freedom from rabies in humans and animals. This support should transgress community, district, national, and international levels. The development of novel diagnostic techniques for both ante-mortem and post-mortem diagnostic confirmation in endemic regions is essential to enable epidemiological assessment and assess treatment options when possible.2, 90 The pathway required by the veterinary services for the control of rabies in dogs was proposed by the OIE to sustainably improve the compliance of veterinary services. Its key components are performance, vision, and strategy.131 With this in mind WHO, OIE, and the Food and Agricultural Organisation have proposed a strategy for the elimination of human rabies transmitted by dogs in rabies-endemic countries; recommending this should be a realistic goal by 2030.
Search strategy and selection criteria
We searched PubMed in February, 2013 with the terms “rabies” and “lyssavirus”. There were no restrictions on date or language. We identified 12 297 articles on rabies and 442 articles on lyssavirus, spanning 140 years since the earliest identified publications. We then undertook more specific searches with the terms “rabies vaccine”, “rabies epidemiology”, “rabies post-exposure prophylaxis”, and “rabies pathogenesis”. 1467 articles on rabies vaccine, 128 articles on rabies epidemiology, 74 articles on rabies post-exposure prophylaxis, and 245 articles on rabies pathogenesis were identified. We reviewed 131 articles identified in both the general and specific searches as relevant to this topic.
Acknowledgments
Acknowledgments
Financial support was received from the UK Department for Environment, Food and Rural Affairs (grants SV3500 and SE0426). We thank Daniel Hicks (Pathology Department, Animal Health and Veterinary Laboratories Agency) for providing figure 4 and Stephen Scholand (Rabies Free World, USA) for the supplementary videos and photographs used in the appendix. Part of the appendix was reproduced courtesy of ResearchGraphix, UK.
Contributors
ARF developed the outline of the report. ARF and ACB compiled the sections, and integrated the reviewers comments into the final version. ARF and ACB provided table 1 and NJ/LMM provided table 2. Figure 2 was prepared by ACB. The appendix was prepared by ARF. All authors contributed to the writing of the seminar and revision of the amended version.
Declaration of interests
We declare that we have no competing interests.
Supplementary Material
A young patient with rabies showing agitation and hypersalivation.
Hydrophobia in a young patient with rabies.
Hydrophobia and agitated behaviour in a rabies patient.
References
- 1.Fooks AR. Rabies remains a ‘neglected disease’. Euro Surveill. 2005;10:211–212. [PubMed] [Google Scholar]
- 2.Banyard AC, Horton DL, Freuling C, Müller T, Fooks AR. Control and prevention of canine rabies: the need for building laboratory-based surveillance capacity. Antiviral Res. 2013;98:357–364. doi: 10.1016/j.antiviral.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Horton DL, Ismail MZ, Siryan ES. Rabies in Iraq: trends in human cases 2001–2010 and characterisation of animal rabies strains from Baghdad. PLoS Negl Trop Dis. 2013;7:e2075. doi: 10.1371/journal.pntd.0002075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dodet B, Korejwo J, Briggs DJ. Eliminating the scourge of dog-transmitted rabies. Vaccine. 2013;31:1359. doi: 10.1016/j.vaccine.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 5.Lembo T, Hampson K, Kaare MT. The feasibility of canine rabies elimination in Africa: dispelling doubts with data. PLoS Negl Trop Dis. 2010;4:e626. doi: 10.1371/journal.pntd.0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sudarshan MK. The changing scenario of rabies in India: are we moving towards its prevention and control? Indian J Public Health. 2007;51:145–147. [PubMed] [Google Scholar]
- 7.Knobel DL, Cleaveland S, Coleman PG. Re-evaluating the burden of rabies in Africa and Asia. Bull World Health Organ. 2005;83:360–368. [PMC free article] [PubMed] [Google Scholar]
- 8.Hampson K, Cleaveland S, Briggs D. Evaluation of cost-effective strategies for rabies post-exposure vaccination in low-income countries. PLoS Negl Trop Dis. 2011;5:e982. doi: 10.1371/journal.pntd.0000982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dodet B, Adjogoua EV, Aguemon AR, the Africa Rabies Expert Bureau (AfroREB) Fighting rabies in Africa: the Africa Rabies Expert Bureau (AfroREB) Vaccine. 2008;26:6295–6298. doi: 10.1016/j.vaccine.2008.04.087. [DOI] [PubMed] [Google Scholar]
- 10.Shwiff S, Hampson K, Anderson A. Potential economic benefits of eliminating canine rabies. Antiviral Res. 2013;98:352–356. doi: 10.1016/j.antiviral.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meslin FX, Briggs DJ. Eliminating canine rabies, the principal source of human infection: what will it take? Antiviral Res. 2013;98:291–296. doi: 10.1016/j.antiviral.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Reece JF, Chawla SK. Control of rabies in Jaipur, India, by the sterilisation and vaccination of neighbourhood dogs. Vet Rec. 2006;159:379–383. doi: 10.1136/vr.159.12.379. [DOI] [PubMed] [Google Scholar]
- 13.Totton SC, Wandeler AI, Zinsstag J. Stray dog population demographics in Jodhpur, India following a population control/rabies vaccination program. Prev Vet Med. 2010;97:51–57. doi: 10.1016/j.prevetmed.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Johnson N, Vos A, Freuling C, Tordo N, Fooks AR, Müller T. Human rabies due to lyssavirus infection of bat origin. Vet Microbiol. 2010;142:151–159. doi: 10.1016/j.vetmic.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Dietzgen RG, Calisher CH, Kurath G. Family Rhabdoviridae. In: AMQ King MJA, E B Carstens EJL, editors. Virus Taxonomy: Ninth Report of the International Committee on Taxonomy of Viruses. Elsevier Academic Press; 2011. pp. 686–714. [Google Scholar]
- 16.Aréchiga Ceballos N, Vázquez Morón S, Berciano JM. Novel lyssavirus in bat, Spain. Emerg Infect Dis. 2013;19:793–795. doi: 10.3201/eid1905.121071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans JS, Horton DL, Easton AJ, Fooks AR, Banyard AC. Rabies virus vaccines: is there a need for a pan-lyssavirus vaccine? Vaccine. 2012;30:7447–7454. doi: 10.1016/j.vaccine.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 18.Kuzmin IV, Hughes GJ, Botvinkin AD, Orciari LA, Rupprecht CE. Phylogenetic relationships of Irkut and West Caucasian bat viruses within the Lyssavirus genus and suggested quantitative criteria based on the N gene sequence for lyssavirus genotype definition. Virus Res. 2005;111:28–43. doi: 10.1016/j.virusres.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Brookes SM, Parsons G, Johnson N, McElhinney LM, Fooks AR. Rabies human diploid cell vaccine elicits cross-neutralising and cross-protecting immune responses against European and Australian bat lyssaviruses. Vaccine. 2005;23:4101–4109. doi: 10.1016/j.vaccine.2005.03.037. [DOI] [PubMed] [Google Scholar]
- 20.Hanlon CA, Kuzmin IV, Blanton JD, Weldon WC, Manangan JS, Rupprecht CE. Efficacy of rabies biologics against new lyssaviruses from Eurasia. Virus Res. 2005;111:44–54. doi: 10.1016/j.virusres.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Horton DL, McElhinney LM, Marston DA. Quantifying antigenic relationships among the lyssaviruses. J Virol. 2010;84:11841–11848. doi: 10.1128/JVI.01153-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Badrane H, Tordo N. Host switching in Lyssavirus history from the Chiroptera to the Carnivora orders. J Virol. 2001;75:8096–8104. doi: 10.1128/JVI.75.17.8096-8104.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Markotter W, Kuzmin IV, Rupprecht CE, Nel LH. Lagos bat virus virulence in mice inoculated by the peripheral route. Epidemiol Infect. 2009;137:1155–1162. doi: 10.1017/S0950268808001945. [DOI] [PubMed] [Google Scholar]
- 24.Kgaladi J, Nel LH, Markotter W. Comparison of pathogenic domains of rabies and African rabies-related lyssaviruses and pathogenicity observed in mice. Onderstepoort J Vet Res. 2013;80:E1–13. doi: 10.4102/ojvr.v80i1.511. [DOI] [PubMed] [Google Scholar]
- 25.Banyard AC, Hayman DTS, Freuling CF, Mueller T, Fooks AR, Johnson N. Bat rabies. In: Jackson ACJ, editor. Rabies: scientific basis of the disease and its management. 3rd edn. Elsevier Academic Press; Oxford, UK: 2013. pp. 215–267. [Google Scholar]
- 26.Banyard AC, Hayman D, Johnson N, McElhinney L, Fooks AR. Bats and lyssaviruses. Adv Virus Res. 2011;79:239–289. doi: 10.1016/B978-0-12-387040-7.00012-3. [DOI] [PubMed] [Google Scholar]
- 27.Albertini AA, Wernimont AK, Muziol T. Crystal structure of the rabies virus nucleoprotein-RNA complex. Science. 2006;313:360–363. doi: 10.1126/science.1125280. [DOI] [PubMed] [Google Scholar]
- 28.Drings A, Jallet C, Chambert B, Tordo N, Perrin P. Is there an advantage to including the nucleoprotein in a rabies glycoprotein subunit vaccine? Vaccine. 1999;17:1549–1557. doi: 10.1016/s0264-410x(98)00357-0. [DOI] [PubMed] [Google Scholar]
- 29.Albertini AA, Ruigrok RW, Blondel D. Rabies virus transcription and replication. Adv Virus Res. 2011;79:1–22. doi: 10.1016/B978-0-12-387040-7.00001-9. [DOI] [PubMed] [Google Scholar]
- 30.Lafon M. Rabies virus receptors. J Neurovirol. 2005;11:82–87. doi: 10.1080/13550280590900427. [DOI] [PubMed] [Google Scholar]
- 31.Reagan KJ, Wunner WH. Rabies virus interaction with various cell lines is independent of the acetylcholine receptor. Arch Virol. 1985;84:277–282. doi: 10.1007/BF01378980. [DOI] [PubMed] [Google Scholar]
- 32.Broughan JH, Wunner WH. Characterization of protein involvement in rabies virus binding to BHK-21 cells. Arch Virol. 1995;140:75–93. doi: 10.1007/BF01309725. [DOI] [PubMed] [Google Scholar]
- 33.Superti F, Derer M, Tsiang H. Mechanism of rabies virus entry into CER cells. J Gen Virol. 1984;65:781–789. doi: 10.1099/0022-1317-65-4-781. [DOI] [PubMed] [Google Scholar]
- 34.Superti F, Hauttecoeur B, Morelec MJ, Goldoni P, Bizzini B, Tsiang H. Involvement of gangliosides in rabies virus infection. J Gen Virol. 1986;67:47–56. doi: 10.1099/0022-1317-67-1-47. [DOI] [PubMed] [Google Scholar]
- 35.Lahaye X, Vidy A, Pomier C. Functional characterization of Negri bodies (NBs) in rabies virus-infected cells: Evidence that NBs are sites of viral transcription and replication. J Virol. 2009;83:7948–7958. doi: 10.1128/JVI.00554-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ménager P, Roux P, Mégret F. Toll-like receptor 3 (TLR3) plays a major role in the formation of rabies virus Negri Bodies. PLoS Pathog. 2009;5:e1000315. doi: 10.1371/journal.ppat.1000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Negri A. Contributo allow studio dell'eziologia dell rabia. Bollettino della Società Medico Chirurgica di Pavia. 1903;2:88–115. [Google Scholar]
- 38.Heinrich BS, Cureton DK, Rahmeh AA, Whelan SP. Protein expression redirects vesicular stomatitis virus RNA synthesis to cytoplasmic inclusions. PLoS Pathog. 2010;6:e1000958. doi: 10.1371/journal.ppat.1000958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Finke S, Brzózka K, Conzelmann KK. Tracking fluorescence-labeled rabies virus: enhanced green fluorescent protein-tagged phosphoprotein P supports virus gene expression and formation of infectious particles. J Virol. 2004;78:12333–12343. doi: 10.1128/JVI.78.22.12333-12343.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Finke S, Cox JH, Conzelmann KK. Differential transcription attenuation of rabies virus genes by intergenic regions: generation of recombinant viruses overexpressing the polymerase gene. J Virol. 2000;74:7261–7269. doi: 10.1128/jvi.74.16.7261-7269.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Finke S, Conzelmann KK. Dissociation of rabies virus matrix protein functions in regulation of viral RNA synthesis and virus assembly. J Virol. 2003;77:12074–12082. doi: 10.1128/JVI.77.22.12074-12082.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Finke S, Mueller-Waldeck R, Conzelmann KK. Rabies virus matrix protein regulates the balance of virus transcription and replication. J Gen Virol. 2003;84:1613–1621. doi: 10.1099/vir.0.19128-0. [DOI] [PubMed] [Google Scholar]
- 43.Singh SK, Ruzek D. Rabies Virus Neurovirulence. In: Singh SK, Ruzek D, editors. Neuroviral Infections. CRC press. Taylor & Francis Inc; 2013. p. 376. table 16–1. [Google Scholar]
- 44.Maier T, Schwarting A, Mauer D. Management and outcomes after multiple corneal and solid organ transplantations from a donor infected with rabies virus. Clin Infect Dis. 2010;50:1112–1119. doi: 10.1086/651267. [DOI] [PubMed] [Google Scholar]
- 45.Fekadu M, Endeshaw T, Alemu W, Bogale Y, Teshager T, Olson JG. Possible human-to-human transmission of rabies in Ethiopia. Ethiop Med J. 1996;34:123–127. [PubMed] [Google Scholar]
- 46.Winkler WG, Fashinell TR, Leffingwell L, Howard P, Conomy P. Airborne rabies transmission in a laboratory worker. JAMA. 1973;226:1219–1221. [PubMed] [Google Scholar]
- 47.Johnson N, Phillpotts R, Fooks AR. Airborne transmission of lyssaviruses. J Med Microbiol. 2006;55:785–790. doi: 10.1099/jmm.0.46370-0. [DOI] [PubMed] [Google Scholar]
- 48.Ginger M, Haberl M, Conzelmann KK, Schwarz MK, Frick A. Revealing the secrets of neuronal circuits with recombinant rabies virus technology. Front Neural Circuits. 2013;7:2. doi: 10.3389/fncir.2013.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ugolini G. Rabies virus as a transneuronal tracer of neuronal connections. Adv Virus Res. 2011;79:165–202. doi: 10.1016/B978-0-12-387040-7.00010-X. [DOI] [PubMed] [Google Scholar]
- 50.Hornung V, Ellegast J, Kim S. 5′-Triphosphate RNA is the ligand for RIG-I. Science. 2006;314:994–997. doi: 10.1126/science.1132505. [DOI] [PubMed] [Google Scholar]
- 51.Rieder M, Conzelmann KK. Interferon in rabies virus infection. Adv Virus Res. 2011;79:91–114. doi: 10.1016/B978-0-12-387040-7.00006-8. [DOI] [PubMed] [Google Scholar]
- 52.Chelbi-Alix MK, Vidy A, El Bougrini J, Blondel D. Rabies viral mechanisms to escape the IFN system: the viral protein P interferes with IRF-3, Stat1, and PML nuclear bodies. J Interferon Cytokine Res. 2006;26:271–280. doi: 10.1089/jir.2006.26.271. [DOI] [PubMed] [Google Scholar]
- 53.Brzózka K, Finke S, Conzelmann KK. Inhibition of interferon signaling by rabies virus phosphoprotein P: activation-dependent binding of STAT1 and STAT2. J Virol. 2006;80:2675–2683. doi: 10.1128/JVI.80.6.2675-2683.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oksayan S, Wiltzer L, Rowe CL, Blondel D, Jans DA, Moseley GW. A novel nuclear trafficking module regulates the nucleocytoplasmic localization of the rabies virus interferon antagonist, P protein. J Biol Chem. 2012;287:28112–28121. doi: 10.1074/jbc.M112.374694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wiltzer L, Larrous F, Oksayan S. Conservation of a unique mechanism of immune evasion across the Lyssavirus genus. J Virol. 2012;86:10194–10199. doi: 10.1128/JVI.01249-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jackson AC, Randle E, Lawrence G, Rossiter JP. Neuronal apoptosis does not play a important role in human rabies encephalitis. J Neurovirol. 2008;14:368–375. doi: 10.1080/13550280802216502. [DOI] [PubMed] [Google Scholar]
- 57.Murphy FA, Harrison AK, Winn WC, Bauer SP. Comparative pathogenesis of rabies and rabies-like viruses: infection of the central nervous system and centrifugal spread of virus to peripheral tissues. Lab Invest. 1973;29:1–16. [PubMed] [Google Scholar]
- 58.Jackson AC, Ye H, Phelan CC. Extraneural organ involvement in human rabies. Lab Invest. 1999;79:945–951. [PubMed] [Google Scholar]
- 59.Freuling C, Vos A, Johnson N. Experimental infection of serotine bats (Eptesicus serotinus) with European bat lyssavirus type 1a. J Gen Virol. 2009;90:2493–2502. doi: 10.1099/vir.0.011510-0. [DOI] [PubMed] [Google Scholar]
- 60.Emmelin N. Nervous control of salivary glands. In: Code CF, editor. vol 2. American Phys Society; Washington DC: 1967. pp. 595–632. (Handbook of physiology). [Google Scholar]
- 61.Jackson AC, Fu ZF. Pathogenesis. In: Jackson AC, editor. Rabies: scientific basis of the disease and its management. 3rd edn. Elsevier Academic Press; Oxford, UK: 2013. pp. 299–349. [Google Scholar]
- 62.Charlton KM, Casey GA. Experimental oral and nasal transmission of rabies virus in mice. Can J Comp Med. 1979;43:10–15. [PMC free article] [PubMed] [Google Scholar]
- 63.Hicks DJ, Nuñez A, Healy DM, Brookes SM, Johnson N, Fooks AR. Comparative pathological study of the murine brain after experimental infection with classical rabies virus and European bat lyssaviruses. J Comp Pathol. 2009;140:113–126. doi: 10.1016/j.jcpa.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 64.Johnson N, Cunningham AF, Fooks AR. The immune response to rabies virus infection and vaccination. Vaccine. 2010;28:3896–3901. doi: 10.1016/j.vaccine.2010.03.039. [DOI] [PubMed] [Google Scholar]
- 65.Wang H, Zhang G, Wen Y, Yang S, Xia X, Fu ZF. Intracerebral administration of recombinant rabies virus expressing GM-CSF prevents the development of rabies after infection with street virus. PLoS One. 2011;6:e25414. doi: 10.1371/journal.pone.0025414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Johnson N, Mansfield KL, Hicks D. Inflammatory response in the nervous system of mice infected with a street isolate of rabies virus. Dev Biol (Basel) 2008;131:65–72. [PubMed] [Google Scholar]
- 67.Hunter M, Johnson N, Hedderwick S. Immunovirological correlates in human rabies treated with therapeutic coma. J Med Virol. 2010;82:1255–1265. doi: 10.1002/jmv.21785. [DOI] [PubMed] [Google Scholar]
- 68.Lafon M. Evasive strategies in rabies virus infection. Adv Virus Res. 2011;79:33–53. doi: 10.1016/B978-0-12-387040-7.00003-2. [DOI] [PubMed] [Google Scholar]
- 69.Hemachudha T, Ugolini G, Wacharapluesadee S, Sungkarat W, Shuangshoti S, Laothamatas J. Human rabies: neuropathogenesis, diagnosis, and management. Lancet Neurol. 2013;12:498–513. doi: 10.1016/S1474-4422(13)70038-3. [DOI] [PubMed] [Google Scholar]
- 70.Both L, Banyard AC, van Dolleweerd C, Horton DL, Ma JK, Fooks AR. Passive immunity in the prevention of rabies. Lancet Infect Dis. 2012;12:397–407. doi: 10.1016/S1473-3099(11)70340-1. [DOI] [PubMed] [Google Scholar]
- 71.Mohr W. Die Tollwut. Med Klin. 1957;52:1057–1060. [PubMed] [Google Scholar]
- 72.Meredith CD, Prossouw AP, Koch H. An unusual case of human rabies thought to be of chiropteran origin. S Afr Med J. 1971;45:767–769. [PubMed] [Google Scholar]
- 73.Paweska JT, Blumberg LH, Liebenberg C. Fatal human infection with rabies-related Duvenhage virus, South Africa. Emerg Infect Dis. 2006;12:1965–1967. doi: 10.3201/eid1212.060764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van Thiel PP, de Bie RM, Eftimov F. Fatal human rabies due to Duvenhage virus from a bat in Kenya: failure of treatment with coma-induction, ketamine, and antiviral drugs. PLoS Negl Trop Dis. 2009;3:e428. doi: 10.1371/journal.pntd.0000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Familusi JB, Osunkoya BO, Moore DL, Kemp GE, Fabiyi A. A fatal human infection with Mokola virus. Am J Trop Med Hyg. 1972;21:959–963. doi: 10.4269/ajtmh.1972.21.959. [DOI] [PubMed] [Google Scholar]
- 76.Roine RO, Hillbom M, Valle M. Fatal encephalitis caused by a bat-borne rabies-related virus. Clinical findings. Brain. 1988;111:1505–1516. doi: 10.1093/brain/111.6.1505. [DOI] [PubMed] [Google Scholar]
- 77.Selimov MA, Tatarov AG, Botvinkin AD, Klueva EV, Kulikova LG, Khismatullina NA. Rabies-related Yuli virus; identification with a panel of monoclonal antibodies. Acta Virol. 1989;33:542–546. [PubMed] [Google Scholar]
- 78.Botvinkin AD, Poleschuk EM, Kuzmin IV. Novel lyssaviruses isolated from bats in Russia. Emerg Infect Dis. 2003;9:1623–1625. doi: 10.3201/eid0912.030374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lumio J, Hillbom M, Roine R. Human rabies of bat origin in Europe. Lancet. 1986;1:378. doi: 10.1016/s0140-6736(86)92336-6. [DOI] [PubMed] [Google Scholar]
- 80.Fooks AR, McElhinney LM, Pounder DJ. Case report: isolation of a European bat lyssavirus type 2a from a fatal human case of rabies encephalitis. J Med Virol. 2003;71:281–289. doi: 10.1002/jmv.10481. [DOI] [PubMed] [Google Scholar]
- 81.Leonova GN, Belikov SI, Kondratov IG. A fatal case of bat lyssavirus infection in Primorskiy Territory of the Russian Far East. Rabies Bull Eur. 2009;33:5–7. [Google Scholar]
- 82.Allworth A, Murray K, Morgan J. A human case of encephalitis due to a lyssavirus recently identified in fruit bats. Commun Dis Intell. 1996;20:504. [Google Scholar]
- 83.Hanna JN, Carney IK, Smith GA. Australian bat lyssavirus infection: a second human case, with a long incubation period. Med J Aust. 2000;172:597–599. doi: 10.5694/j.1326-5377.2000.tb124126.x. [DOI] [PubMed] [Google Scholar]
- 84.Francis JR, Nourse C, Vaska VL. Australian bat lyssavirus in a child: the first reported case. Pediatrics. 2014;133:e1063–e1067. doi: 10.1542/peds.2013-1782. [DOI] [PubMed] [Google Scholar]
- 85.Gilbert AT, Petersen BW, Recuenco S. Evidence of rabies virus exposure among humans in the Peruvian Amazon. Am J Trop Med Hyg. 2012;87:206–215. doi: 10.4269/ajtmh.2012.11-0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Willoughby RE, Jr, Hammarin AL. Prophylaxis against rabies in children exposed to bats. Pediatr Infect Dis J. 2005;24:1109–1110. doi: 10.1097/01.inf.0000191443.48828.79. [DOI] [PubMed] [Google Scholar]
- 87.Mallewa M, Fooks AR, Banda D. Rabies encephalitis in malaria-endemic area, Malawi, Africa. Emerg Infect Dis. 2007;13:136–139. doi: 10.3201/eid1301.060810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lembo T, Niezgoda M, Velasco-Villa A, Cleaveland S, Ernest E, Rupprecht CE. Evaluation of a direct, rapid immunohistochemical test for rabies diagnosis. Emerg Infect Dis. 2006;12:310–313. doi: 10.3201/eid1202.050812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fooks AR, Johnson N, Freuling CM. Emerging technologies for the detection of rabies virus: challenges and hopes in the 21st century. PLoS Negl Trop Dis. 2009;3:e530. doi: 10.1371/journal.pntd.0000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fooks AR, McElhinney LM, Horton D, et al. Molecular tools for rabies diagnosis in animals. In: Fooks AR, Müller T, eds. OIE, Compendium of the OIE Global Conference on Rabies Control; 2012: 75–87.
- 91.Dacheux L, Reynes JM, Buchy P. A reliable diagnosis of human rabies based on analysis of skin biopsy specimens. Clin Infect Dis. 2008;47:1410–1417. doi: 10.1086/592969. [DOI] [PubMed] [Google Scholar]
- 92.Smith J, McElhinney L, Parsons G. Case report: rapid ante-mortem diagnosis of a human case of rabies imported into the UK from the Philippines. J Med Virol. 2003;69:150–155. doi: 10.1002/jmv.10253. [DOI] [PubMed] [Google Scholar]
- 93.Jackson AC, Warrell MJ, Rupprecht CE. Management of rabies in humans. Clin Infect Dis. 2003;36:60–63. doi: 10.1086/344905. [DOI] [PubMed] [Google Scholar]
- 94.Jackson AC. Therapy of human rabies. In: Jackson AC, editor. Rabies: scientific basis of the disease and its management. 3rd edn. Elsevier Academic Press; Oxford, UK: 2013. pp. 573–587. [Google Scholar]
- 95.Jackson AC. Recovery from rabies: a call to arms (editorial) J Neurol Sci. 2013;15:5–7. doi: 10.1016/j.jns.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 96.Willoughby RE, Jr, Tieves KS, Hoffman GM. Survival after treatment of rabies with induction of coma. N Engl J Med. 2005;352:2508–2514. doi: 10.1056/NEJMoa050382. [DOI] [PubMed] [Google Scholar]
- 97.Jackson AC. Recovery from rabies. N Engl J Med. 2005;352:2549–2550. doi: 10.1056/NEJMe058092. [DOI] [PubMed] [Google Scholar]
- 98.Jackson AC. Current and future approaches to the therapy of human rabies. Antiviral Res. 2013;99:61–67. doi: 10.1016/j.antiviral.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 99.Sutherland BA, Minnerup J, Balami JS, Arba F, Buchan AM, Kleinschnitz C. Neuroprotection for ischaemic stroke: translation from the bench to the bedside. Int J Stroke. 2012;7:407–418. doi: 10.1111/j.1747-4949.2012.00770.x. [DOI] [PubMed] [Google Scholar]
- 100.Warrell MJ. Current rabies vaccines and prophylaxis schedules: preventing rabies before and after exposure. Travel Med Infect Dis. 2012;10:1–15. doi: 10.1016/j.tmaid.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 101.Fooks AR, Johnson N, Brookes SM, Parsons G, McElhinney LM. Risk factors associated with travel to rabies endemic countries. J Appl Microbiol. 2003;94(suppl):31S–36S. doi: 10.1046/j.1365-2672.94.s1.4.x. [DOI] [PubMed] [Google Scholar]
- 102.Gautret P, Parola P. Rabies vaccination for international travelers. Vaccine. 2012;30:126–133. doi: 10.1016/j.vaccine.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 103.WHO Publication Rabies vaccines: WHO position paper-recommendations. Vaccine. 2010;28:7140–7142. doi: 10.1016/j.vaccine.2010.08.082. [DOI] [PubMed] [Google Scholar]
- 104.WHO Rabies vaccines. WHO position paper. Wkly Epidemiol Rec. 2007;82:425–435. [PubMed] [Google Scholar]
- 105.Suraweera W, Morris SK, Kumar R, Warrell DA, Warrell MJ, Jha P, the Million Death Study Collaborators Deaths from symptomatically identifiable furious rabies in India: a nationally representative mortality survey. PLoS Negl Trop Dis. 2012;6:e1847. doi: 10.1371/journal.pntd.0001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu Q, Ertl HC. Preventative childhood vaccination to rabies. Expert Opin Biol Ther. 2012;12:1067–1075. doi: 10.1517/14712598.2012.691162. [DOI] [PubMed] [Google Scholar]
- 107.Prasad R, Marothiya A, Mishra OP, Srivastava A. Encephalitis following purified chick embryo rabies vaccination. Paediatr Int Child Health. 2012;32:242–243. doi: 10.1179/2046905511Y.0000000012. [DOI] [PubMed] [Google Scholar]
- 108.Hicks DJ, Fooks AR, Johnson N. Developments in rabies vaccines. Clin Exp Immunol. 2012;169:199–204. doi: 10.1111/j.1365-2249.2012.04592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.WHO . WHO expert consultation on rabies—second report, 2013 and Technical Report Series 982. World Health Organization; Geneva: 2013. [PubMed] [Google Scholar]
- 110.Manning SE, Rupprecht CE, Fishbein D. Human rabies prevention–United States, 2008: recommendations of the Advisory Committee on Immunization Practices. Centers for Disease Control MMWR Recomm Rep. 2008;57(RR-3):1–28. [PubMed] [Google Scholar]
- 111.Meslin FM. The Louis Pasteur Oration. Kolkatta India Association for the Prevention of Rabies in India; 2012. [Google Scholar]
- 112.Müller T, Dietzschold B, Ertl H. Development of a murine monoclonal antibody cocktail for post-exposure rabies prophylaxis in humans. PLoS Negl Trop Dis. 2009;3:e542. doi: 10.1371/journal.pntd.0000542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bakker AB, Python C, Kissling CJ. First administration to humans of a monoclonal antibody cocktail against rabies virus: safety, tolerability, and neutralizing activity. Vaccine. 2008;26:5922–5927. doi: 10.1016/j.vaccine.2008.08.050. [DOI] [PubMed] [Google Scholar]
- 114.de Kruif J, Bakker AB, Marissen WE. A human monoclonal antibody cocktail as a novel component of rabies postexposure prophylaxis. Annu Rev Med. 2007;58:359–368. doi: 10.1146/annurev.med.58.061705.145053. [DOI] [PubMed] [Google Scholar]
- 115.Both L, van Dolleweerd C, Wright E. Production, characterization, and antigen specificity of recombinant 62-71-3, a candidate monoclonal antibody for rabies prophylaxis in humans. FASEB. 2013;27:2055–2065. doi: 10.1096/fj.12-219964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Both L, Banyard AC, van Dolleweerd C, Wright E, Ma JK, Fooks AR. Monoclonal antibodies for prophylactic and therapeutic use against viral infections. Vaccine. 2013;31:1553–1559. doi: 10.1016/j.vaccine.2013.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dorfmeier CL, Lytle AG, Dunkel AL, Gatt A, McGettigan JP. Protective vaccine-induced CD4(+) T cell-independent B cell responses against rabies infection. J Virol. 2012;86:11533–11540. doi: 10.1128/JVI.00615-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Faber M, Li J, Kean RB, Hooper DC, Alugupalli KR, Dietzschold B. Effective preexposure and postexposure prophylaxis of rabies with a highly attenuated recombinant rabies virus. Proc Natl Acad Sci USA. 2009;106:11300–11305. doi: 10.1073/pnas.0905640106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Schutsky K, Curtis D, Bongiorno EK. Intramuscular inoculation of mice with the live-attenuated recombinant rabies virus TriGAS results in a transient infection of the draining lymph nodes and a robust, long-lasting protective immune response against rabies. J Virol. 2013;87:1834–1841. doi: 10.1128/JVI.02589-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Vos A, Conzelmann KK, Finke S. Immunogenicity studies in carnivores using a rabies virus construct with a site-directed deletion in the phosphoprotein. Adv Prev Med. 2011;2011:898171. doi: 10.4061/2011/898171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Taylor LH, Costa P, Briggs DJ. Public health management of humans at risk. In: Jackson AC, editor. Rabies: scientific basis of the disease and its management. 3rd edn. Elsevier Academic Press; Oxford, UK: 2013. pp. 543–573. [Google Scholar]
- 122.Fooks AR. Rabies—the need for a ‘one medicine’ approach. Vet Rec. 2007;161:289–290. doi: 10.1136/vr.161.9.289. [DOI] [PubMed] [Google Scholar]
- 123.Rupprecht CE, Barrett J, Briggs D. Can rabies be eradicated? Dev Biol (Basel) 2008;131:95–121. [PubMed] [Google Scholar]
- 124.Schneider MC, Belotto A, Adé MP. Current status of human rabies transmitted by dogs in Latin America. Cad Saude Publica. 2007;23:2049–2063. doi: 10.1590/s0102-311x2007000900013. [DOI] [PubMed] [Google Scholar]
- 125.Belotto AJ. The Pan American Health Organization (PAHO) role in the control of rabies in Latin America. Dev Biol (Basel) 2004;119:213–216. [PubMed] [Google Scholar]
- 126.Vigilato MA, Clavijo A, Knobl T. Progress towards eliminating canine rabies: policies and perspectives from Latin America and the Caribbean. Philos Trans R Soc Lond B Biol Sci. 2013;368:20120143. doi: 10.1098/rstb.2012.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Vigilato MA, Cosivi O, Knöbl T, Clavijo A, Silva HM. Rabies update for Latin America and the Caribbean. Emerg Infect Dis. 2013;19:678–679. doi: 10.3201/eid1904.121482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Taylor L, the Partners for Rabies Prevention Eliminating canine rabies: the role of public-private partnerships. Antiviral Res. 2013;98:314–318. doi: 10.1016/j.antiviral.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 129.Lembo T, Attlan M, Bourhy H. Renewed global partnerships and redesigned roadmaps for rabies prevention and control. Vet Med Int. 2011;2011:1–18. doi: 10.4061/2011/923149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Franka R, Smith TG, Dyer JL, Wu X, Niezgoda M, Rupprecht CE. Current and future tools for global canine rabies elimination. Antiviral Res. 2013;100:220–225. doi: 10.1016/j.antiviral.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 131.Murray JG, Aviso SM. OIE activities to support sustainable rabies control: vaccine banks, OIE twinning and evaluation of the performance of veterinary services. In: Müller F, editor. Compendium of the OIE Global Conference on Rabies Control. OIE; Paris: 2012. pp. 197–205. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A young patient with rabies showing agitation and hypersalivation.
Hydrophobia in a young patient with rabies.
Hydrophobia and agitated behaviour in a rabies patient.