Recent estimates indicate that several million Americans are at risk of contracting COVID-19 and many fatalities will likely result. Implicit in these numbers is the risk involved for uninfected patients with COVID-19 seeking medical care in an emergency situation. Allergists/immunologists may need to modify recommendations for the acute management of anaphylaxis during these unprecedented times to ensure optimal outcomes of anaphylaxis while weighing the infectious risk and health care burdens associated with the COVID-19 pandemic.1 The following recommendations reinforce and expand on the recent expert opinion to assist allergists/immunologists in considering how to adjust their practice under these unique circumstances.1 , 2 Decision-making will vary based on local contexts and resources as rates of COVID-19 and access to health care differ geographically. Moreover, there will be cases of severe anaphylaxis where we would not deviate from the usual plan of contacting emergency services immediately after using epinephrine (Figure 1 ). Patients should be empowered to activate emergency medical services (EMS) if they feel concerns or feel urgent care is needed after epinephrine use, and EMS should be activated if severe symptoms do not completely resolve or if they recur. We recommend using telemedicine to proactively discuss the modified management of anaphylaxis and communicate thresholds for activating EMS, per individual patient's profile, local COVID-19 burden, and careful assessment of the risk-to-benefit ratio.
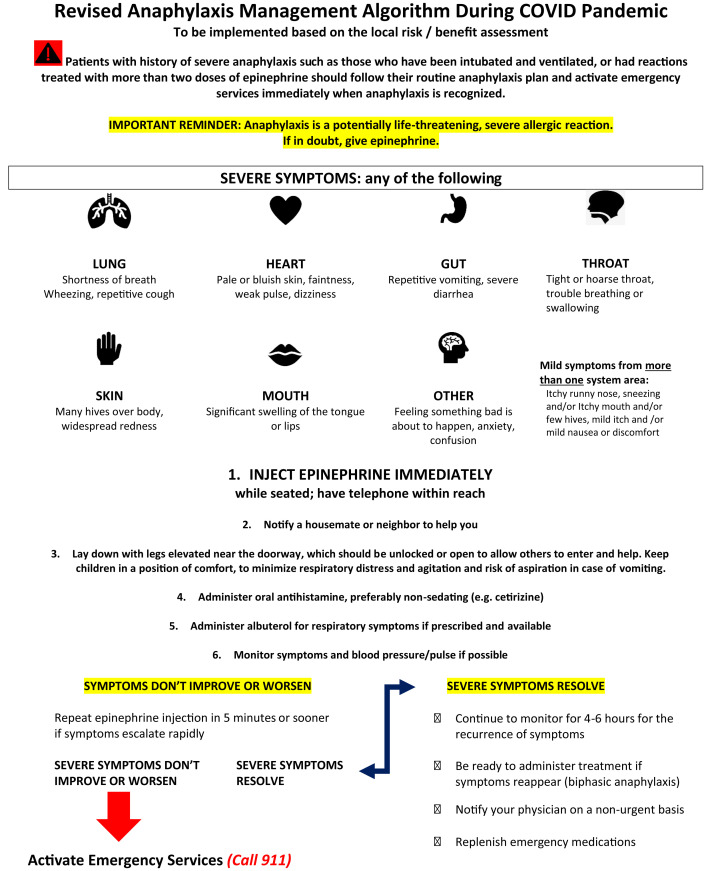
Figure 1.
Revised anaphylaxis algorithm replacing the standard management protocol during the COVID-19 pandemic.
Patients with specific disorders that require the immediate administration of epinephrine (Table I ) to treat acute immediate hypersensitivity reactions are typically advised to immediately use their epinephrine autoinjector and activate emergency services to be evaluated at an emergency department (ED).1, 2, 3, 4, 5, 6
Table I.
Disorders commonly treated with epinephrine
| Food-induced anaphylaxis, including reactions during food oral immunotherapy |
| Medication/drug-induced anaphylaxis |
| Venom-induced anaphylaxis |
| Idiopathic anaphylaxis |
| Physical urticarias resulting in anaphylaxis |
| Mast cell disorders |
| Home-administered allergen immunotherapy |
In view of the risk of contracting COVID-19 at overburdened ED facilities, such as New York City, it may be advisable for patients to follow a revised management algorithm (Figure 1). Successful implementation of at home management of an acute anaphylactic event requires capable and adherent patients and caregivers who have a clear understanding of the risk and benefits.7 It is critical for patients to have at least 2 epinephrine autoinjectors available for management. Patients who were treated with multiple doses of epinephrine in the past should have additional epinephrine auto-injectors available. Patients should inspect the epinephrine injectable devices to determine an expiration date and to identify any potential issues associated with malfunction (see recent Food and Drug Administration communication).8 The expired and otherwise “suspicious” epinephrine devices should be replaced as soon as possible; however, if a patient has access to only a recently expired autoinjector, he or she should be informed that use of that device is preferable to nontreatment if a severe reaction were to occur.8 Patients with underlying asthma should take prescribed asthma medications and maintain optimal asthma control. Having access to a home blood pressure and pulse monitor can also be helpful.
A modified algorithm for the acute management of anaphylaxis is displayed in Figure 1. Patients should administer their epinephrine autoinjector as soon as there are symptoms of a severe allergic reaction. After the epinephrine autoinjector is used, patients should be monitored for response to treatment, and if severe symptoms resolve promptly (eg, wheezing, shortness of breathing, difficulty breathing, vomiting, throat swelling, faintness, hypotension), they should notify their doctor on a nonurgent basis. If severe symptoms persist or worsen, a second dose of epinephrine should be injected, and if prompt resolution of severe symptoms is not achieved, emergency services should be activated. If patients have questions regarding subsequent management, they might attempt to contact their physician urgently although during the COVID pandemic access might be limited. For patients with a prior history of severe anaphylaxis, it might be prudent to proactively discuss the modified management of anaphylaxis, if feasible, for example, via telemedicine. There should be clear, open communication regarding the risk/benefit assessment for ED evaluation, taking into account symptoms, prior history (ie, asthma and anaphylaxis history), access to EMS/ED if symptoms progress, patient/caregiver knowledge, and comfort as well as other factors that may influence decision-making.6 It is also important to emphasize that the recommendation for ED evaluation is based on the assessment of how likely there will be need for additional medical intervention to manage anaphylaxis, and not because epinephrine is a dangerous medication (this misconception should be dispelled). Telephone or telehealth video follow-up can be helpful to address any questions that may arise regarding avoidance of anaphylaxis triggers and management of future reactions.
Biphasic or prolonged anaphylaxis can occur.9 Patients need to be educated about this possibility and be ready to emergently manage a recurrence. If they have exhausted their supply of epinephrine autoinjectors managing the initial symptoms and symptoms have resolved or improved significantly, they should continue monitoring and obtain a refill of EAIs. If symptoms have persisted or escalated, they should call 911 and seek immediate medical assistance.
Open communications with patients and families regarding risks and benefits of ED evaluation after epinephrine administration for anaphylaxis are strongly encouraged.6 Patients should understand that these modifications reflect a shift in risk/benefit assessment as infectious risks and health care system burdens associated with ED visits during the COVID-19 pandemic are significantly higher than usual. The successful implementation of home management of an acute anaphylactic event requires patients to be calm, educated, and in possession of medications needed to treat an acute reaction. As with all anaphylactic reactions, the quicker epinephrine is administered the less likely a reaction will progress to a catastrophic event.6
Footnotes
No funding was received for this work.
Conflicts of interest: T. B. Casale receives research support from Aimmune and Regeneron. J. Wang receives research support from National Institute of Allergy and Infectious Diseases, Aimmune, DBV Technologies, and Regeneron, and consultancy fees from Aimmune, ALK Abello, and DBV Technologies. A. Nowak-Wegrzyn received research support from National Institute of Allergy and Infectious Diseases, DBV Technologies, Astellas Pharma, Danone, and Nestle, and consultancy fees from Regeneron and Gerber Institute; she serves as the Deputy Editor for the Annals of Allergy, Asthma and Immunology.
References
- 1.Shaker M.S., Oppenheimer J., Grayson M., Stukus D., Hartog N., Hsieh E.W.Y. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–1488. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaker M., Karaoke T., Feenan L., Greenhawt M. An economic evaluation of immediate vs non-immediate activation of emergency medical services after epinephrine use for peanut-induced anaphylaxis. Ann Allergy Asthma Immunol. 2019;122:79–85. doi: 10.1016/j.anai.2018.06.035. [DOI] [PubMed] [Google Scholar]
- 3.Shaker M.S., Wallace D.V., Golden D.B.K., Oppemheimer J., Bernstein J.A., Campbell R.L. Anaphylaxis-a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020;145:1082–1123. doi: 10.1016/j.jaci.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 4.Boyce J.A., Assa'ad A., Burks A.W., Jones S.M., Sampson H.A., Wood R.A. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(Suppl):S1–S58. doi: 10.1016/j.jaci.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carter M.C., Akin C., Castells M.C., Scott E.P., Lieberman P. Idiopathic anaphylaxis yardstick: practical recommendations for clinical practice. Ann Allergy Asthma Immunol. 2020;124:16–27. doi: 10.1016/j.anai.2019.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Shaker M.S., Oppenheimer J., Wallace D.V., Golden D.B.K., Lang D.M., Lang E.S. Making the GRADE in anaphylaxis management: towards recommendations integrating values, preferences, context, and shared decision-making. Ann Allergy Asthma Immunol. 2020;124:526–535. doi: 10.1016/j.anai.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 7.US Food and Drug Administration FDA alerts patients and health care professionals of EpiPen auto-injector errors related to device malfunctions and user administration. https://www.fda.gov/drugs/drug-safety-and-availability/fda-alerts-patients-and-health-care-professionals-epipen-auto-injector-errors-related-device Available from:
- 8.Cantrell F.L., Cantrell P., Wen A., Gerona R. Epinephrine concentrations in EpiPens after the expiration date. Ann Intern Med. 2017;166:918–919. doi: 10.7326/L16-0612. [DOI] [PubMed] [Google Scholar]
- 9.Shaker M., Wallace D., Golden D.B.K., Oppenheimer J., Greenhawt M. Simulation of health and economic benefits of extended observation of resolved anaphylaxis. JAMA Netw Open. 2019;2:e1913951. doi: 10.1001/jamanetworkopen.2019.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]