Abstract
There is a need to optimize the fit between psychosocial interventions with known efficacy and the demands of real-word service delivery settings. However, adaptation of evidence-based interventions (EBI) raises questions about whether effectiveness can be retained. This randomized controlled trial (RCT) evaluated a streamlined package of cognitive, behavioral, and social skills training strategies known to prevent and reduce anxiety symptom and disorder escalation in youth. A total of 109 youth (Mage = 9.72; 68% girls; 54% Latinx) at risk based on high anxiety were randomized to the streamlined prevention and early intervention (SPEI) (n = 59) or control (n = 50) and were assessed at pretest, posttest, and 1-year follow-up. A main objective was to determine whether our redesign could be delivered by community providers, with acceptable levels of fidelity, quality, and impact. In terms of process evaluation results, there was high protocol fidelity, excellent clinical process skills, few protocol adaptations, and high satisfaction with the streamlined prevention and early intervention (SPEI). In terms of outcomes, there were no significant main or moderated effects of the SPEI at the immediate posttest. However, at the follow-up, youth in the SPEI reported greater self-efficacy for managing anxiety-provoking situations, greater social skills, and fewer negative cognitive errors relative to controls. Collectively, findings suggest that the redesigned SPEI might be an attractive and efficient solution for service delivery settings.
Keywords: Prevention, Anxiety, Children, Latinx, Hybrid-1 Effectiveness
Pediatric anxiety disorders are preventable, yet evidence-based interventions (EBIs) are not reaching U.S. youth (National Academies of Sciences, Engineering, and Medicine, 2017). Children with anxiety problems, for example, are the least likely to receive any services (40% for anxiety versus 72% for disruptive disorders, Kohn, 2014), despite anxiety disorders being the most prevalent mental illness in this segment of the population (~31.9%; Merikangas et al., 2010) and schools being staffed to respond as the primary source of care (80% of schools staff mental health and/or wellness personnel and anxiety is covered under the Individuals with Disabilities Education Act [2004]; Stockings et al., 2016).
Why are schools not offering EBIs for child anxiety? We collaborated with a school advisory board and various school districts to identify gaps between the provision of EBIs and school mental health practice. We surveyed stakeholders serving students with social and emotional difficulties and conducted focus groups. Our research showed that, in part, school mental health providers rarely offer EBIs for youth anxiety because the length of sessions exceeds class periods (60- to 90-minute sessions), the number and continuity of sessions are incompatible with school calendars (12 to 18 consecutive lessons), manuals are too lengthy and overly scripted (60 to 90 pages), and there is too much required training plus in-depth supervision (2 to 3 full-day trainings with about 1 hour of weekly supervision over the course of delivery) (Pina, Holly, Wynne, Zerr, & Stoll, 2012). These findings are generally consistent with Forman et al. (2009) and Langley et al. (2010) who also have identified additional barriers to the provision of EBIs in school settings (e.g., cost, parent engagement, competing responsibilities). Thus, we believe that one initial step to facilitate adoption and sustainability of school-based EBIs for youth anxiety is to redesign for intervention-setting fit.
School stakeholders have taught us that targeting youth anxiety in elementary school contexts fits best as a small group intervention for students with similar social and emotional learning needs (tier-2 or targeted efforts) (Sulkowski, Joyce, & Storch, 2012). Stakeholders explained traits they believe would make tier-2 EBIs for youth anxiety suitable for school mental health practice, including desirable program length (e.g., six or seven short sessions), broad targets/skills (e.g., for various types of anxiety), enabling strategies (e.g., brief training for school staff members serving as providers), and collaborative game-based learning (active learning strategies; Kapp, 2012). Armed with this knowledge, we searched the empirical literature to identify tier-2, brief anxiety programs, delivered at school, by school mental health providers, and via collaborative game-based learning strategies. No such program was found.
The literature on EBIs shows gaps between the architecture of programs for youth anxiety and school mental health practice. Brief anxiety programs tend to focus on single problems (e.g., 5 sessions for test anxiety, Weems et al., 2015) but schools desire EBIs that cut across various types of anxiety (Chiu et al., 2013). Programs focusing on multiple types of anxiety are not brief; instead, those EBIs have as many as 12 to 18 sessions, lessons longer than typical class periods (e.g., 60 to 90 minutes), manuals ranging from 46–85 pages in length, and 8–16 hours of provider training (1–1.5 hours/week for 8–10 weeks). Lastly, although not available during the initial stages of our research, four recent school-based programs, implemented by teachers exist at the time of this writing. But, these four programs have shown discouraging results. Specifically, Mindlight and Dojo do not produce significant effects compared to control, MoodGYM shows significant effects on one child self-report measure of anxiety and leads to poor engagement (only completed by 33% of youth), and e-Couch has no significant effects on any anxiety measure, even when highly trained providers are involved (Calear et al., 2016; Calear, Christensen, Mackinnon, Griffiths, & O’Kearney, 2009: Scholten, Malmberg, Lobel, Engels, & Granic, 2016; Schoneveld et al., 2016). Given this evidence, we redesigned a set of well-established intervention strategies for youth anxiety disorders, including those validated in our published trials (RCTs; Pina, Silverman, Fuentes, Kurtines, & Weems, 2003; Pina, Zerr, Villalta, & Gonzales, 2012; Silverman, Kurtines, Jaccard, & Pina, 2008).
To derive a brief anxiety program, meant to be delivered at school, by school mental health providers, and via collaborative game-based learning, we relied on the “small-theory” approach, a commonly used prevention framework attributed to Lipsey (1990). We relied on robust anxiety development theory (Barlow, 2000; Lang, 1961) and recent calls for EBIs that can be optimized for broad dissemination (MacKinnon, 2011; Rotheram-Borus, Swendeman, & Chorpita, 2012). Our use of the small-theory approach translated into defining multiple factors to target for change via intervention, with the intention of maximizing impact on the outcomes as well as specifying the directionality of change hypothesized to prevent or reduce behavior problems (Rothman, Greenland, & Walker, 1980; West & Aiken, 1997).
The program’s theory for the redesign integrates Lang’s (1961) taxonomy of the fear response system and Barlow’s (2000) emotion model of anxiety. Briefly, when it comes to anxiety disorder development, cues demanding performance or arousal awareness can become anxiety provoking for some vulnerable youth. This occurs, in part, with a shift in attention from the cues to a self-evaluation of coping ability (or rather lack of) and even a realization of uncontrollability. The perceived lack of coping ability increases negative affect and somatic arousal, setting the stage for distortions in information processing and apprehension. When that occurs, pathological anxiety manifests itself as avoidance (subtle, gross) and persistent central nervous system arousal. Accordingly, our approach to disrupt anxiety disorder development is to increase youths’ capacity to cope with the cues outlined in the theory. This is consistent with child anxiety research showing that increases in coping self-efficacy, in general, and in direct problem solving and positive cognitive restructuring precede decreases in anxiety symptoms (Kendall et al., 2016). In fact, one study showed that self-efficacy mediated school attendance and decreases in fear about attending school the next day (Maric et al., 2012). Thus, our tier-2 intervention aimed to improve self-efficacy and social competence for managing anxiety provoking situations while also reducing physiological hyperarousal and distortions in information processing. To achieve this goal, and from the distillation of EBIs by Chorpita, Daleiden, and Weisz (2005), the specific component in the tier-2, brief anxiety program is in-vivo exposures to feared situations, facilitated by relaxation, cognitive self-control, and social skills training. These procedures are based on the formative work of Silverman and Kurtines (1996), and Beidel, Turner, and Morris (2004).
Regarding implementation, we worked with school stakeholders to derive a streamlined protocol that reduced the number of sessions from 12 to 6 group sessions and from 60-minute to 20–30-minute sessions. Lessons were redesigned into collaborative game-based learning strategies, handouts were modified into game-based scoring cards, the original manual was simplified from 40 to 12 pages. Training for school staff providers was packaged to fit with desired training practices, including: one continuing education credit for a one-day/5-hour training at the school district site, two weeks before implementation, with no financial compensation from the researchers, followed by no supervision from the researchers but support from trained peers implementing at other schools. In addition, for caregivers, teachers, and principals, educational materials were developed to explain that anxiety interferes with academics (e.g., less in-class learning and participation, lower test scores, less instructional time; Ingul, Klockner, Silverman, & Nordhahl, 2012). For caregivers, the educational brochure explained that anxiety is highly prevalent, has been linked to depression, illegal substance use, and unemployment in adulthood, and often fails to remit without intervention (Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012). Lastly, every brochure highlighted that, when ignored, youth anxiety problems can cost as much as 21 times more than the cost of caring for typically developing youth (Kilian, Losert, Park, McDaid, & Knapp, 2010).
Thus, we conducted an initial evaluation of our SPEI against an active control arm, using a hybrid-1 design (pretest, posttest, 12-month follow-up [FU]). The hybrid-1 is defined by essential efficacy (randomization, a comparison arm, manual, independent outcome evaluation, and fidelity evaluation) and effectiveness (various school sites, typical training, minimal inclusion criteria, community providers as implementers, implementation and satisfaction evaluations) traits relevant to empirically establishing interventions in their intended practice settings (Curran et al., 2012). Accordingly, we report process evaluation data (e.g., fidelity, engagement) albeit our basic goal was to gain some sense about the promise of our redesign by having school staff implement the protocol under natural conditions. We, therefore, report on the hybrid-1 effectiveness of the SPEI in terms of changes in self-efficacy for managing anxiety provoking situations, social competence, physiological hyperarousal, and distortions in information processing. We also report on the effectiveness of our streamlined program in terms of alleviating youth anxiety symptoms (clinically and statistically). Altogether, our hypothesis was that youth in the SPEI would show better outcomes than those in the control arm at the immediate posttest as well as continual improvements at the 12-month follow-up. This is plausible and consistent with our past pediatric anxiety intervention research (Pina, Silverman, Fuentes, Weems, & Kurtines, 2003).We also expected youth with higher baseline anxiety to show significant decreases in anxiety symptoms, which would be consistent with broad prevention research showing that those at most risk show benefits prior to their less severe counterparts (Spoth, Trudeau, Redmond, & Shin, 2014). More specifically, we investigated whether the effects of the SPEI on anxiety were moderated by baseline status on youth and caregiver report of the MASC, separately.
Methods
Participants
A total of 859 children in general education (Mage = 9.64, SD = 0.69; girls = 52%; White = 37%, Latinx = 45%, other = 18%) in Maricopa County, Arizona were screened at school. Of the 142 eligible children, 109 (77%) were randomized to the SPEI (n = 59) or control (n = 50). There were no significant differences along sociodemographic characteristics between identified and non-identified children, except for sex. As in past anxiety research (Lewinsohn, Gotlib, Lewinsohn, Seeley, & Allen, 1998), more girls than boys were identified (SCAS scores ≥ 42), χ2(1) = 23.62, p < .001.
Process Evaluation Measures
Fidelity, clinical process skills, adaptations, content knowledge, and program usability were rated using a measure developed by Fagan, Hanson, Briney, and Hawkins (2012). Providers reported on usability. Independent observer ratings of videotaped sessions and interventionists’ reports were aggregated to assess fidelity, clinical process skills, adaptations, and content knowledge. Interrater reliability between observers for fidelity, clinical process skills, and adaptations was achieved by using independent raters who watched 20% of the videos and reached 100% agreement, after discussing discrepancies with the researchers. Implementation was measured weekly, for every session, with scores summed across dimensions and then across sessions for each group receiving the SPEI. Youth active participation during sessions were coded by observers (0=not at all; 5=very, very much) with 100% interrater reliability, after discussing discrepancies with the researchers. Satisfaction and stigma were measured using child self-reports, as done in Rapee et al. (2006) (satisfaction and stigma α = .62 in this sample).
Anxiety and Program Target Measures
Total scores were computed for all scales by taking the sum of the items. To measure child anxiety, we used child and parent self-reports via the Spence Children’s Anxiety Scale (SCAS; Spence, 1998) and the Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997). The SCAS and MASC predict a child anxiety diagnosis derived from the Anxiety Disorders Interview Schedule for Children (ADIS-C/P; Silverman & Albano, 1996; Nauta et al., 2004). Cronbach’s α ranged from .77 to .94 for child report and from .92 to .95 for parent report. The MASC was the primary outcome measure as it assesses DSM pediatric anxiety symptoms while the SCAS focuses on typical anxiety levels. To measure program targets associated with the fear-emotion theories named, we used youth reports via the Children’s Self-Efficacy Questionnaire for Handling School Situations (SEQSS; Heyne et al., 1998), Physiological Hyperarousal Scale for Children (PHSC; Laurent, Catanzaro, & Joiner, 2004), and Children’s Negative Cognitive Error Questionnaire (CNCEQ; Leitenberg, Yost, & Carroll-Wilson, 1986) as well as parent reports on the Social Skills Improvement Rating System (SSIS-RS; Gresham & Elliott, 2008). Cronbach’s α ranged from .67 to .90 for child report and from .92 to .93 for parent report. No additional outcome variables were assessed.
Experimental Arms
The Streamlined Prevention and Early Intervention (SPEI) is 6 sessions/weeks (~20–30 min each), in group format (5 to 7 students), offered to youth during school hours, and tier-2. The SPEI is a cognitive, behavioral, and social skills training program (Pina et al., 2003; Pina et al., 2012). In the SPEI, parents and teachers are contacted weekly, via email or postcard, to describe the week’s skill and to encourage youth practice during the 6-weeks and beyond. Youth sessions 1–6 train for and include corrective feedback centered on skill generalization.
The Control consisted of three commercially available books: What to do When You’re Scared and Worried: A Guide for Kids (Crist, 2004), How to do Homework Without Throwing Up (Romain, 1997), and Getting Organized Without Losing It (Fox, 2006). This is an ecologically valid arm (Rohde, Stice, Shaw, & Gau, 2015); variants of it have been earmarked promising (Chavira et al., 2018). Books and instructions are mailed to each home, followed by a phone call to the caregiver to encourage home practice.
Procedures
First, districts identified staff members to serve as providers (social workers, school psychologists), teachers sent home 1,539 screening permission slips and the brochure to parents of those in regular classes, and 10 days later, 875 parents consented. Second, 859 children were screened using the SCAS (16 consented youth were absent from school on the screening day and thus were excluded) and those with scores ≥ 42 (Barret & Turner, 2001; Spence, 1997) were invited to participate. Simple randomization to arms occurred at the child level, using a true random number generator, by a blinded research member. Of note, 39 students were excluded because the teacher did not feel anxiety was a primary concern, instead the concern was comorbid oppositionality (20% of anxious youth meet criteria for a disruptive behavior disorder; Cunningham & Ollendick, 2010). Third, seven school psychologists and two school social workers, each serving one or two schools were trained in the SPEI. Training focused on delivering with fidelity and differentiating change components from program strategies. Training included content on working in the contexts of cultural diversity. No additional in-person or online support was provided by the researchers. Clinical data were collected at pretest, posttest (week 7), and FU (12 months) by research members, blinded to randomization and hypotheses.
Analytic Strategy
We assessed differences between youth randomized to the SPEI and those in the control arm on 16 demographic and baseline measures using t-tests and χ2 tests. Cook’s distance was used to identify influential data points (Cook, 1977). To assess the impact of attrition on internal and external validity, we compared the attrition rates across arms using Fisher’s exact test and performed 2 × 2 (arm × attrition status) analysis of variance or factorial logistic regression on each baseline measure (Jurs & Glass, 1971). Intent-to-treat analyses were conducted by regressing each youth- and caregiver-outcome on arm assignment and baseline status on the outcome. We investigated whether the effects of the SPEI on anxiety were moderated by baseline status on youth and caregiver report on the MASC, separately. We assessed whether the effects of the SPEI on anxiety were moderated by ethnicity (Non-Hispanic White versus Latinx). Significant and marginally significant moderated effects were probed via simple main effects, which were computed at the mean and at one standard deviation above/below the mean of the moderator (Aiken & West, 1991). Cohen’s d was calculated for all significant main effects and simple main effects using adjusted means based on the regression analysis (Cohen, 1988). All analyses were performed in Mplus 7.3 (Muthén & Muthén, 1998–2014) using full information maximum likelihood estimation, which does not exclude cases with missing scores. Because youth were recruited from nine schools, we used a sandwich estimator for the standard error computations to adjust for clustering by school (average number of children per school = 12.11; Yuan & Bentler, 2000). Intraclass correlations ranged from .00 to .12 for youth-reported outcomes (MICC = .02) and from .00 to .11 for caregiver-reported outcomes (MICC = .06).
Results
Preliminary Analyses
Figure 1 shows participant flow using the CONSORT. Table 1 shows sociodemographic characteristics for the total sample and by arm. When assessing differences between youth randomized to the SPEI versus control on demographic and baseline measures, no significant differences were found. No influential data points were identified based on Cook’s distance. Attrition rates did not significantly differ across arms at posttest (Fisher’s exact test p = .73 and .18 for youth and caregivers, respectively) or FU (Fisher’s exact test p = .80 and .26). No other attrition status main effects or attrition status by arm interaction effects were significant.
Figure 1.
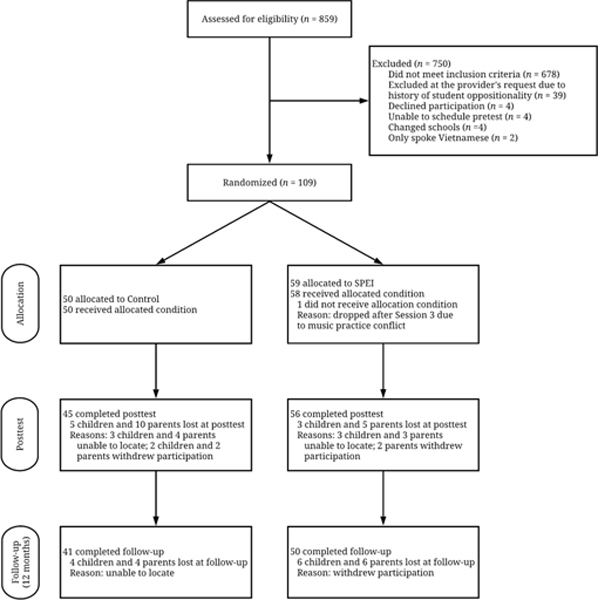
CONSORT Diagram
Table 1.
Sociodemographic Characteristics for the Total Sample and by Arm
| Total | Control | IPEI | ||||
|---|---|---|---|---|---|---|
| (N = 109) | (n = 50) | (n = 59) | ||||
| n (%) | M (SD) | n (%) | M (SD) | n (%) | M (SD) | |
| Child Age (years) | 9.72 (0.73) | 9.68 (0.68) | 9.76 (0.77) | |||
| Girls | 85 (78%) | 40 (80%) | 45 (76%) | |||
| Race/Ethnicity | ||||||
| White | 39 (36%) | 17 (34%) | 22 (37%) | |||
| Latinx | 59 (54%) | 27 (54%) | 32 (54%) | |||
| Native American | 4 (4%) | 1 (2%) | 3 (5%) | |||
| African American | 3 (3%) | 2 (4%) | 1 (2%) | |||
| Other | 4 (4%) | 3 (6%) | 1 (2%) | |||
| Caregiver Unmarried | 58 (53%) | 28 (56%) | 30 (51%) | |||
| Family Income | ||||||
| < $20,000 | 40 (37%) | 21 (42%) | 19 (32%) | |||
| $20,000 to 40,000 | 19 (17%) | 13 (26%) | 6 (10%) | |||
| > $40,000 | 48 (44%) | 15 (30%) | 33 (56%) | |||
| Not Reported | 2 (2%) | 1 (2%) | 1 (2%) | |||
| College Education | ||||||
| Mother | 30 (28%) | 12 (24%) | 18 (31%) | |||
| Father | 29 (27%) | 13 (26%) | 16 (27%) | |||
Note. For each arm, the number of participants listed was the number included in each analysis and analyses were conducted on the basis of original assignment to arms. Unmarried refers to single (n = 9), divorced (n = 26), or other (n = 23).
Process Evaluation
In the SPEI, all but one youth completed all sessions of the program (66% perfectly attended the regular sessions, 32% received make-up sessions, one youth discontinued participation due to a music practice scheduling conflict), and observers reported high child participation in the sessions (M = 4.40, SD = 0.25 on a 0 to 5 scale). For weekly out-of-session skill practice, 68% of youth used relaxation, 53% used cognitive self-control, 61% used assertiveness strategies, and 51% engaged in out-of-session exposures. Youth reported adequate satisfaction (M = 7.63, SD = 1.69 on a 1 to 10 scale) and low stigma (M = 2.03, SD = 1.22 on a 1 to 10 scale). SPEI interventionists and observers reported high fidelity (M = 3.46, SD = 0.36 on a 0 to 4 scale) and excellent clinical process skills (M = 4.50, SD = 0.33 on a 1 to 5 scale). Interventionists reported few adaptations (M = 1.35, SD = 0.78 on a 1 to 5 scale) and high satisfaction with the SPEI (M = 3.87, SD = 0.09 on a 0 to 4 scale). Observers reported that interventionists seemed knowledgeable about the SPEI (M = 4.32, SD = 0.70 on a 1 to 5 scale). In the control, 86% of caregivers read at least half of the handout outlining the content of each book, and 76% of youth completed at least two of the three books. About 14% of caregivers reported that the child spent no time reading the books, and 15% of youth said that they spent no time reading the books. No caregiver contacted the school provider for help with the child anxiety management skills prescribed by either arm. One interventionist sought within-district support from a trained peer after delivering the cognitive self-control lesson in session 2.
Outcome Evaluation
Table 2 presents means and standard deviations at each time point for the total sample and by arm. At posttest (Week 7), there were no significant main or moderated effects of the SPEI on the outcomes. However, at the FU, youth in the SPEI reported greater self-efficacy for managing anxiety-provoking situations (b = 3.61, SEb = 1.39, z = 2.60, p = .01, d = 0.50, 95% CI [0.12, 0.88]) relative to those in the control. Additionally, youth in the SPEI reported greater social skills (b = 5.14, SEb = 2.29, z = 2.25, p = .03, d = 0.44, 95% CI [0.05, 0.81]) and fewer negative cognitive errors (b = −4.02, SEb = 1.58, z = −2.55, p = .01, d = 0.49, 95% CI [−0.87, −0.11]) at FU relative to controls. No significant main effects on autonomic arousal were found.
Table 2.
Means (Standard Deviations), and Cohen’s d (p-value) for the Total Sample and by Arm at Pretest, Posttest, and Follow-Up
| Total | Control | IPEI | Cohen’s d (p-value) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretest | Posttest | FU | Pretest | Posttest | FU | Pretest | Posttest | FU | Pretest | Posttest | FU | |
| Child reported | ||||||||||||
| Hyperarousal | 2.15 (0.74) | 2.04 (0.74) | 1.90 (0.68) | 2.22 (0.82) | 2.11 (0.77) | 2.03 (0.66) | 2.10 (0.67) | 2.01 (0.72) | 1.78 (0.66) | −0.15 (.44) | 0.10 (.59) | 0.30 (.12) |
| Cognitive Errors | 36.72 (7.52) | 36.26 (9.05) | 35.84 (7.70) | 36.53 (8.44) | 37.44 (9.93) | 38.15 (7.91) | 36.88 (6.74) | 35.32 (8.26) | 33.94 (7.05) | 0.05 (.81) | 0.23 (.24) | 0.49 (.01) |
| Social Skills | 102.63 (17.76) | 101.92 (19.30) | 99.41 (17.28) | 100.87 (21.09) | 101.64 (23.85) | 95.81 (18.68) | 104.09 (14.45) | 102.15 (14.93) | 102.36 (15.61) | 0.18 (.51) | 0.15 (.43) | 0.44 (.03) |
| Self-Efficacy | 39.94 (7.15) | 40.45 (8.93) | 41.52 (8.54) | 40.87 (7.40) | 40.56 (9.76) | 40.46 (8.57) | 39.17 (6.92) | 40.37 (8.30) | 42.38 (8.51) | −0.14 (.33) | 0.16 (.41) | 0.50 (.01) |
| Anxiety Levels | 55.82 (12.16) | -- | 43.66 (19.20) | 56.93 (13.03) | -- | 46.07 (20.71) | 54.88 (11.40) | -- | 41.68 (17.83) | −0.17 (.15) | -- | 0.15 (.43) |
| Anxiety Symptoms | 62.53 (14.81) | 57.50 (17.14) | 55.22 (15.66) | 60.25 (17.87) | 55.55 (20.69) | 55.29 (17.21) | 64.43 (11.50) | 59.06 (13.67) | 55.16 (14.44) | 0.28 (.14) | 0.03 (.90) | 0.05 (.79) |
| Parent Reported | ||||||||||||
| Anxiety Levels | 26.16 (17.35) | 23.06 (16.99) | 23.71 (16.09) | 23.28 -(15.48) | 19.82 (12.80) | 19.42 (11.09) | 28.60 (18.57) | 25.45 (19.27) | 26.94 (18.47) | 0.31 (.15) | 0.04 (.79) | 0.28 (.15) |
| Anxiety Symptoms | 50.39 (17.65) | 46.40 (16.54) | 44.88 (15.50) | 47.24 (15.62) | 43.74 (15.32) | 41.36 (13.59) | 53.06 (18.92) | 48.35 (17.27) | 47.52 (16.43) | 0.33 (.07) | 0.01 (.98) | 0.13 (.50) |
Note. Cohen’s d is provided for all main effects at posttest and follow-up. The p-values are for the regression coefficient associated with treatment group. FU = 12-month follow-up; PHSC = Physiological Hyperarousal Scale for Children (Laurent et al., 2004); CNCEQ = Children’s Negative Cognitive Error Questionnaire (Leitenberg et al., 1986); SSIS-RS = Social Skills Improvement System—Rating Scales (Elliot et al., 2008); SEQSS = The Self-Efficacy Questionnaire for School Situations (Heyne et al., 1998); SCAS = Spence Children’s Anxiety Scale (Spence, 1997, 1998) (levels, child and parent versions); MASC = Multidimensional Anxiety Scale for Children (March et al., 1997) (symptoms) (child and parent versions). Child report of the SCAS was unintentionally excluded at posttest.
The 109 youths reported high anxiety at pretest based on the SCAS (cutoff score ≥ 42), yet 48% of children in the SPEI and 39% in the control scored below the cutoff at FU. In the SPEI, 7% deteriorated at FU compared to 22% in the control (p= .07, Fisher’s exact test, odds ratio = 0.28, 95% CI [0.08 to 0.98], risk difference = .15, 95% CI [.00 to .29]). Based on the MASC, 25% in the SPEI returned to normal levels (defined as below T-score of 65) compared to 15% in the control at FU. On the parent MASC, 18% in the SPEI moved from clinical to normal levels at FU compared to 6% in the control. These changes were not statistically significant.
Levels of child-reported MASC anxiety symptoms at baseline moderated the effect of the SPEI on child-reported MASC anxiety symptoms (b = −0.50, SEb = 0.18, z = −2.85, p < .01) and SCAS anxiety levels (b = −0.66, SEb = 0.35, z = −1.88, p = .06) at the FU. Relative to those in the control, higher risk children in the SPEI reported fewer anxiety symptoms at the FU based on the MASC (b = −8.32, SEb = 3.95, z = −2.11, p = .04, d+1SD = 0.41) and lower anxiety levels based on the SCAS (b = −14.57, SEb = 4.25, z = −3.43, p < .01, d+1SD = 0.67). Comparisons at the mean and at −1SD were not significant. Caregiver-reported youth MASC anxiety symptoms at baseline moderated the effect of the SPEI on caregiver-reported youth SCAS anxiety levels at the FU (b = 0.25, SEb = 0.09, z = 2.83, p = .01). However, relative to those in the control, caregivers of youth in the SPEI reported lower SCAS anxiety levels at the FU for lower risk children (b = −2.69, SEb = 1.26, z = −2.12, p = .03, d-1SD = 0.41) but greater anxiety levels for higher risk children (b = 5.98, SEb = 2.55, z = 2.35, p = .02, d+1SD = 0.46). Lastly, ethnicity moderated the effect of the SPEI on caregiver-reported anxiety about the child at FU using the SCAS (b = 6.02, SEb = 2.67, z = 2.25, p = .02) such that caregivers of Latinx (Lx) youth in the control reported fewer anxiety symptoms than caregivers of Lx youth in the SPEI (b = 4.45, SEb = 1.65, z = 2.70, p = .01). The difference for the Non-Hispanic White youth was not significant.
Discussion
With known gaps between the architecture of psychosocial interventions with efficacy and the parameters for service delivery in real world settings, such as school mental health, there is a pressing need for EBIs redesign to optimize intervention-setting fit. Improved fit by redesign may support adoption at-scale to achieve broad population-level impact, but pragmatic adaptations to EBIs raise questions about whether effectiveness can be retained. In this study, we redesigned several well-established cognitive, behavior, and social skills strategies known to prevent and reduce anxiety symptom and disorders in youth (Silverman, Pina, & Viswesvaran, 2008). Both the process and outcome evaluations suggest that the redesign might have achieved the intended goals of creating an efficient and attractive intervention for schools.
In this study, school provider’s implementation was outstanding (high fidelity, excellent clinical process skills, few adaptations). Providers not only implemented the SPEI well but were knowledgeable about the SPEI, reported high satisfaction with the SPEI, and engaged the students in the SPEI. These findings are important because implementation problems are common when research-developed interventions are delivered in service settings, like schools (McLeod, Southam-Gerow, Tully, Rodriguez, & Smith, 2013). In this research, high quality of implementation probably emerged for several reasons. First, consistent with Diffusion of Innovations Theory (Rogers, 2003), the high fidelity observed might be related to the SPEI having few core elements, with each element being relatively easy to implement and differentiate. Second, we feel the SPEI was delivered with excellent clinical process skills because our providers had experience delivering school-based interventions and because, as explained by Carroll et al. (2007), our use of representative stakeholders to design the SPEI probably resulted in a program responsive to the typical clinical skill set of school mental health staff (rather than the highly trained and supervised research staff in most efficacy trials). Third, implementation deviations or adaptations were minimal (and trivial) because the SPEI relied on gamification theory (Kapp, 2012; Pretti-Frotczak & Bricker, 2004) and game-based elements (storytelling, visualizations, problem solving) familiar to youth, which are staples in academic instruction. Nonetheless, we know that our findings need replication because monitoring of implementation can influence interventionist behavior, such that the combination of direct and indirect quality assuring measures used might have prompted higher than typical quality (e.g., monitoring and videotaping each session; Breitenstein, Gross, & Gavey, 2010).
At the immediate posttest, no significant differences or differences between arms were found. It might be the case that youth in the SPEI needed more time to master the anxiety management skills. As suggested by Ost and Ollendick (2017), brief interventions like the SPEI are more likely to show robust effects after youth have had time to test anxiety-related catastrophic beliefs and assumptions. At FU, the SPEI effectively changed multiple factors targeted for change (i.e., improved self-efficacy, decreased cognitive interpretation biases, and strengthened social competence). No statistically significant reductions in autonomic arousal were found. Changes in autonomic arousal have been rarely examined in RCTs but have sometimes emerged (Ost et al., 2001). Allen, Allen, Austin, Waldron, and Ollendick (2015) explained that changes in arousal could be slower to emerge and detect because arousal habituation takes longer to occur. Variability on the effects of the SPEI on youth anxiety emerged when considering youth vs. caregiver reports. Relative to controls, higher risk children in the SPEI reported fewer anxiety symptoms at the FU. At FU, caregivers of youth in the SPEI reported greater anxiety levels for higher risk youth but lower anxiety levels for lower risk youth. Caregivers of Lx youth in the control reported lower anxiety levels than their counterparts in the SPEI. These findings should not be viewed as iatrogenic effects of the SPEI for several reasons. First, discrepancies between youth and caregivers are often found in the child anxiety literature (De Los Reyes, Bunnell, & Beidel, 2013). Discrepancies tend to signal areas within which youth experienced improvement versus those within which parent concerns remain (De Los Reyes, Alfano, & Beidel, 2010). Second, findings were based on the SCAS alone, with the higher scores corresponding to seven children in the SPEI (5 Lx) whose MASC scores also were 1SD above the mean at FU. Lastly, clinical improvements consistently favored the SPEI over the control.
This research is limited in several ways. First, the same score cutoff was used to screen all youth. Cutoffs for an important segment of our sampled population -- Lx -- were unavailable. During the course of this study, we found that higher cutoffs apply to Lx youth (Holly et al., 2015). Thus, we might have slightly overidentified Lx youth. Second, anxiety inclusion criterion was based on a single assessment point, such that the stability of anxiety prior to randomization is unknown. Third, findings of the main and moderation effects are limited by sample size, such that we can detect only the medium effect size (i.e., d ~ .50). Fourth, Lx ethnicity predicted poorer outcomes in the Child Anxiety Multisite Study (CAMS, Taylor et al., 2018; Walkup et al., 2008) and we found moderation by ethnicity on one parent measure about the child’s anxiety. These findings call for in-depth research to identify which parameters in cultural adaptations are necessary and for whom given that our past trials showed null moderation effects by Lx ethnicity (Pina et. El., 2008). Fifth, we accounted for clustering by school but we did not account for clustering by intervention group due to the partially nested design and small sample size. Lastly, the precise timing of SPEI effects could not be discerned but were detectable at 12-month FU. Earlier detection of changes in the program targets (as well as its cascading effects on the principal outcomes) could suggest avenues to accelerate prevention and recovery by increasing program dosage and thereby strengthen the provision of care in school mental health practice.
Acknowledgments
Note. This work was supported in part by grant number K01MH086687 awarded to A. Pina from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not represent the official views of the funding agency. The authors declare that they have no conflict of interest. All study procedures and measures were reviewed and approved by the Institutional Review Board. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA, US: Sage Publications, Inc. doi: 10.2307/2583960 [DOI] [Google Scholar]
- Allen KB, Allen B, Austin KE, Waldron JC, & Ollendick TH (2015). Synchrony–desynchrony in the tripartite model of fear: Predicting treatment outcome in clinically phobic children. Behaviour Research and Therapy, 71, 54–64. doi:10.1016/j.brat.2015.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH (2000). Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist, 55, 1247–1263. doi:10.1037/0003-066X.55.11.1247 [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, & Morris TL (2004). Social effectiveness therapy for children and adolescents (SET-C). Ontario, Toronto: Multi-Health Systems, Inc. [Google Scholar]
- Breitenstein SM, Gross D, Garvey CA, Hill C, Fogg L, & Resnick B (2010). Implementation fidelity in community-based interventions. Research in Nursing & Health, 33, 164–173. doi:10.1002/nur.20373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calear AL, Christensen H, Mackinnon A, Griffiths KM, & O’Kearney R (2009). The YouthMood Project: A cluster randomized controlled trial of an online cognitive behavioral program with adolescents. Journal of Consulting and Clinical Psychology, 77, 1021–1032. doi:10.1037/a0017391 [DOI] [PubMed] [Google Scholar]
- Calear AL, Batterham PJ, Poyser CT, Mackinnon AJ, Griffiths KM, & Christensen H (2016). Cluster randomised controlled trial of the e-couch Anxiety and Worry program in schools. Journal of Affective Disorders, 196, 210–217. doi:10.1016/j.jad.2016.02.049 [DOI] [PubMed] [Google Scholar]
- Carroll C, Patterson M, Wood S, Booth A, Rick J, & Balain S (2007). A conceptual framework for implementation fidelity. Implementation Science, 2, 275–282. doi:10.1186/1748-5908-2-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira DA, Bustos C, Garcia M, Reinosa Segovia F, Baig A, Ng B, & Camacho A (2018). Telephone-assisted, parent-mediated CBT for rural Latino youth with anxiety: A feasibility trial. Cultural Diversity and Ethnic Minority Psychology, 24, 429–441. doi:10.1037/cdp0000186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu AW, Langer DA, McLeod BD, Har K, Drahota A, Galla BM, ... & Wood JJ (2013). Effectiveness of modular CBT for child anxiety in elementary schools. School Psychology Quarterly, 28, 141–153. doi:10.1037/spq0000017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, & Weisz JR (2005). Identifying and selecting the common elements of evidence-based interventions: A distillation and matching model. Mental Health Services Research, 7, 5–20. doi:10.1007/s11020-005-1962-6 [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Earlbaum Associates. [Google Scholar]
- Cook RD (1977). Detection of influential observation in linear regression. Technometrics, 19, 15–18. doi:10.1080/00401706.1977.10489493 [Google Scholar]
- Crist JJ (2004). What to do when you’re scared & worried: A guide for kids. Minneapolis, MN: Free Spirit Publishing. [Google Scholar]
- Cunningham NR & Ollendick TH (2010). Comorbidity of anxiety and conduct problems in children: Implications for clinical research and practice. Clinical Child and Family Psychology Review, 13, 333–347. 10.1007/s10567-010-0077-9 [DOI] [PubMed] [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, & Stetler C (2012). Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50, 217–226. doi:10.1097/MLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Alfano CA, & Beidel DC (2010). The relations among measurements of informant discrepancies within a multisite trial of treatments for childhood social phobia. Journal of Abnormal Child Psychology, 38, 395–404. doi:10.1007/s10802-009-9373-6 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Bunnell BE, & Beidel DC (2013). Informant discrepancies in adult social anxiety disorder assessments: Links with contextual variations in observed behavior. Journal of Abnormal Psychology, 122, 376–386. doi:10.1037/a0031150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan AA, Hanson K, Briney JS, & Hawkins JD (2012). Sustaining the utilization and high quality implementation of tested and effective prevention programs using the Communities That Care prevention system. American Journal of Community Psychology, 49, 365–377. doi:10.1007/s10464-011-9463-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman SG, Olin SS, Hoagwood KE, Crowe M, & Saka N (2009). Evidence-based interventions in schools: Developers’ views of implementation barriers and facilitators. School Mental Health, 1, 26–36. doi:10.1007/s12310-008-9002-5 [Google Scholar]
- Fox JS (2006). Get organized without losing it. Minneapolis, MN: Free Spirit Publishing. [Google Scholar]
- Gresham FM, & Elliott SN, (2008). Social Skills Improvement System Rating Scales. Minneapolis, MN: NCS Pearson. [Google Scholar]
- Heyne D, King N, Tonge B, Rollings S, Pritchard M, Young D, & Myerson N (1998). The self-efficacy questionnaire for school situations: Development and psychometric evaluation. Behaviour Change, 15, 31–40. doi:10.1017/S081348390000588X [Google Scholar]
- Individuals with Disabilities Education Improvement Act 20, U.S.C. § 1400 (2004)
- Ingul JM, Klöckner CA, Silverman WK, & Nordahl HM (2012). Adolescent school absenteeism: Modeling social and individual risk factors. Child and Adolescent Mental Health, 17, 93–100. doi:10.1111/j.1475-3588.2011.00615.x [DOI] [PubMed] [Google Scholar]
- Jurs SG, & Glass GV (1971). The effect of experimental mortality on the internal and external validity of the randomized comparative experiment. The Journal of Experimental Education, 40, 62–66. doi:10.1080/00220973.1971.11011304 [Google Scholar]
- Kapp KM (2012). The gamification of learning and instruction: Game-based methods and strategies for training and education. John Wiley & Sons. [Google Scholar]
- Kendall PC, Cummings CM, Villabø MA, Narayanan MK, Treadwell K, Birmaher B, ... & Gosch E (2016). Mediators of change in the Child/Adolescent Anxiety Multimodal Treatment Study. Journal of Consulting and Clinical Psychology, 84, 1–14. doi:10.1037/a0039773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen HU (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21, 169–184. doi:10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilian R, Losert C, Park AL, McDaid D, & Knapp M (2010). Cost-effectiveness analysis in child and adolescent mental health problems: An updated review of literature. International Journal of Mental Health Promotion, 12, 45–57. doi:10.1080/14623730.2010.9721825 [Google Scholar]
- Kohn R (2014). Trends, gaps, and disparities in mental health In Okpaku SO (Ed.), Essentials of global mental health (pp. 27–38). New York: Cambridge University Press. doi:10.1017/CBO9781139136341.006 [Google Scholar]
- Langley AK, Nadeem E, Kataoka SH, Stein BD, & Jaycox LH (2010). Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health, 2, 105–113. doi:10.1007/s12310-010-9038-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, & Joiner TE Jr (2004). Development and preliminary validation of the physiological hyperarousal scale for children. Psychological Assessment, 16, 373–380. doi:10.1037/1040-3590.16.4.373 [DOI] [PubMed] [Google Scholar]
- Leitenberg H, Yost LW, & Carroll-Wilson M (1986). Negative cognitive errors in children: Questionnaire development, normative data, and comparisons between children with and without self-reported symptoms of depression, low self-esteem, and evaluation anxiety. Journal of Consulting and Clinical Psychology, 54, 528–536. doi:10.1037/0022-006X.54.4.528 [DOI] [PubMed] [Google Scholar]
- Lang PJ (1968). Fear reduction and fear behavior: Problems in treating a construct. In Research in Psychotherapy Conference, 3rd, May-Jun, 1966, Chicago, IL, US. American Psychological Association. [Google Scholar]
- Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, & Allen NB (1998). Gender differences in anxiety disorders and anxiety symptoms in adolescents. Journal of Abnormal Psychology, 107, 109–117. doi:10.1037/0021-843X.107.1.109 [DOI] [PubMed] [Google Scholar]
- Lipsey MW (1990). Theory as method: Small theories of treatments In Sechrest L, Perrin E, & Bunker J (Eds.), Research methodology: Strengthening causal interpretations of nonexperimental data (DHHS Publication No. 90–3454, pp. 33–51). Washington, DC: U.S. Department of Health and Human Services, Agency for Health Care Policy and Research. [Google Scholar]
- MacKinnon DP (2011). Integrating mediators and moderators in research design. Research on Social Work Practice, 21, 675–681. doi:10.1177/1049731511414148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, & Conners CK (1997). The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 554–565. doi:10.1097/00004583-199704000-00019 [DOI] [PubMed] [Google Scholar]
- Maric M, Heyne DA, MacKinnon DP, Van Widenfelt BM, & Westenberg PM (2012). Cognitive mediation of cognitive-behavioural therapy outcomes for anxiety-based school refusal. Behavioural and Cognitive Psychotherapy, 41, 549–564. doi:10.1017/S1352465812000756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod BD, Southam-Gerow MA, Tully CB, Rodriguez A, & Smith MM (2013). Making a case for treatment integrity as a psychosocial treatment quality indicator for youth mental health care. Clinical Psychology: Science and Practice, 20, 14–32. doi:10.1111/cpsp.12020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, ... & Swendsen J (2010). Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49, 980–989. doi:10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2014). Mplus User’s Guide. Seventh Edition. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2017). Advancing the science to improve population health: Proceedings of a workshop. National Academies Press. [PubMed] [Google Scholar]
- Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, & Waters A (2004). A parent-report measure of children’s anxiety: Psychometric properties and comparison with child-report in a clinic and normal sample. Behaviour Research and Therapy, 42, 813–839. doi: 10.1016/S0005-7967(03)00200-6 [DOI] [PubMed] [Google Scholar]
- Ost LG, Svensson L, Hellstrom K, & Lindwall R (2001). One-session treatment of specific phobias in youths: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 69(5), 814–824. doi:10.1037/0022-006X.69.5.814 [PubMed] [Google Scholar]
- Pina A, Holly LE, Wynne H, Zerr AA, & Stoll R (2012, May). A social network and qualitative data approach to assist transportability of a child anxiety prevention program into elementary school settings. Paper presented at the meeting of the Society for Prevention Research, Washington, DC. [Google Scholar]
- Pina AA, Silverman WK, Fuentes RM, Kurtines WM, & Weems CF (2003). Exposure-based cognitive-behavioral treatment for phobic and anxiety disorders: Treatment effects and maintenance for Hispanic/Latino relative to European-American youths. Journal of the American Academy of Child & Adolescent Psychiatry, 42, 1179–1187. doi:10.1097/00004583-200310000-00008 [DOI] [PubMed] [Google Scholar]
- Pina AA, Zerr AA, Villalta IK, & Gonzales NA (2012). Indicated prevention and early intervention for childhood anxiety: A Randomized trial with Caucasian and Hispanic/Latino youth. Journal of Consulting and Clinical Psychology, 80, 940–946. doi:10.1037/a0029460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Wignall A, Sheffield J, Kowalenko N, Davis A, McLoone J, & Spence SH (2006). Adolescents’ reactions to universal and indicated prevention programs for depression: Perceived stigma and consumer satisfaction. Prevention Science, 7, 167–177. doi:10.1007/s11121-006-0035-4 [DOI] [PubMed] [Google Scholar]
- Rogers EM (2003). Diffusion of Innovations Theory. New York: Free Press, 5th ed. doi:10.1111/j.1467-9523.1970.tb00071.x [Google Scholar]
- Rohde P, Stice E, Shaw H, & Gau JM (2015). Effectiveness trial of an indicated cognitive–behavioral group adolescent depression prevention program versus bibliotherapy and brochure control at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology, 83, 736–747. doi:10.1037/ccp0000022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romain T (1997). How to do homework without throwing up. Minneapolis, MN: Free Spirit Publishing. [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, & Chorpita BF (2012). Disruptive innovations for designing and diffusing evidence-based interventions. American Psychologist, 67, 463–476. doi:10.1037/a0028180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, & Walker AM (1980). Concepts of interaction. American Journal of Epidemiology, 112, 467–470. doi:10.1093/oxfordjournals.aje.a113015 [DOI] [PubMed] [Google Scholar]
- Scholten H, Malmberg M, Lobel A, Engels RC, & Granic I (2016). A randomized controlled trial to test the effectiveness of an immersive 3D video game for anxiety prevention among adolescents. PLOS One, 11, e0147763. doi:10.1371/journal.pone.0147763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoneveld EA, Malmberg M, Lichtwarck-Aschoff A, Verheijen GP, Engels RC, & Granic I (2016). A neurofeedback video game (MindLight) to prevent anxiety in children: A randomized controlled trial. Computers in Human Behavior, 63, 321–333. doi:10.1016/j.chb.2016.05.005 [Google Scholar]
- Silverman WK, & Albano AM (1996). Anxiety Disorders Interview Schedule for DSM-IV: Child interview schedule. Graywind Publications. [Google Scholar]
- Silverman WK, & Kurtines WM (1996). Anxiety and phobic disorders: A pragmatic approach. New York, NY, US: Plenum Press. doi:10.1007/978-1-4757-9212-6 [Google Scholar]
- Silverman WK, Kurtines WM, Jaccard J, & Pina AA (2009). Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology, 77, 474–485. doi: 10.1037/a0015761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, & Viswesvaran C (2008). Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 37, 105–130. doi:10.1080/15374410701817907 [DOI] [PubMed] [Google Scholar]
- Spence SH (1998). A measure of anxiety symptoms among children. Behaviour Research and Therapy, 36, 545–566. doi:10.1016/S0005-7967(98)00034-5 [DOI] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Redmond C, & Shin C (2014). Replication RCT of early universal prevention effects on young adult substance misuse. Journal of Consulting and Clinical Psychology, 82, 949–963. doi:10.1037/a0036840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockings EA, Degenhardt L, Dobbins T, Lee YY, Erskine HE, Whiteford HA, & Patton G (2016). Preventing depression and anxiety in young people: A review of the joint efficacy of universal, selective and indicated prevention. Psychological Medicine, 46, 11–26. doi:10.1017/S0033291715001725 [DOI] [PubMed] [Google Scholar]
- Sulkowski ML, Joyce DK, & Storch EA (2012). Treating childhood anxiety in schools: Service delivery in a response to intervention paradigm. Journal of Child and Family Studies, 21, 938–947. doi:10.1007/s10826-011-9553-1 [Google Scholar]
- Taylor JH, Lebowitz ER, Jakubovski E, Coughlin CG, Silverman WK, & Bloch MH (2018). Monotherapy insufficient in severe anxiety? Predictors and moderators in the Child/Adolescent Anxiety Multimodal Study. Journal of Clinical Child & Adolescent Psychology, 47, 266–281. doi:10.1080/15374416.2017.1371028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, ... & Iyengar S (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine, 359, 2753–2766. doi: 10.1056/NEJMoa0804633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weems CF, Scott BG, Graham RA, Banks DM, Russell JD, Taylor LK, ... & Marino RC (2015). Fitting anxious emotion-focused intervention into the ecology of schools: Results from a test anxiety program evaluation. Prevention Science, 16, 200–210. doi:10.1007/s11121-014-0491-1 [DOI] [PubMed] [Google Scholar]
- West SG, & Aiken LS (1997). Toward understanding individual effects in multicomponent prevention programs: Design and analysis strategies In Bryant KJ, Windle M, & West SG (Eds.), The science of prevention: Methodological advances from alcohol and substance abuse research (pp. 167–209). Washington, DC, US: American Psychological Association. [Google Scholar]
- Yuan KH, & Bentler PM (2000). Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology, 30, 165–200. doi:10.1111/0081-1750.00078 [Google Scholar]


