1. Summary, 7
2. Introduction, 7
3. The burden of viral infection, 8
3.1 Gastrointestinal infections, 8
3.2 Respiratory infections, 9
4. Dispersal, persistence and spread of viruses in domestic homes and community settings, 10
4.1 Gastrointestinal viruses, 11
4.1.1 Rotavirus, 11
4.1.2 Norwalk‐like viruses, 11
4.1.3 Hepatitis A virus, 12
4.2 Respiratory viruses, 12
4.3 Herpes simplex virus, 13
4.4 Varicella virus, 13
4.5 The infectious dose, 13
5. Evidence that hygiene can play a part in preventing transmission of viral infections, 13
6. Development of effective hygiene policies for prevention of transmission of viral infections, 16
7. Conclusions, 17
8. References, 18
1. SUMMARY
Viruses are probably the most common cause of infectious disease acquired within indoor environments and have considerable impact on human health, ranging from severe life‐threatening illnesses to relatively mild and self‐limiting or asymptomatic diseases. In particular, viruses causing gastrointestinal and respiratory diseases spread rapidly in the community and cause considerable morbidity. Increasing numbers of people who have impaired immunity, for whom the consequences of infection can be much more serious, are now cared for in ‘out of hospital’ settings. This review examines the dispersal, persistence and control of some common viruses in the domestic home and in community facilities. There is growing evidence that person‐to‐person transmission via the hands and contaminated fomites plays a key role in the spread of viral infections and there is a need for wider understanding of the potential for contaminated surfaces to act as unidentified vectors of pathogens in the transmission cycle. Intervention studies have shown that improved standards of education, personal hygiene (particularly handwashing) and targeted environmental hygiene have considerable impact in the control and prevention of infectious organisms.
2. INTRODUCTION
Nearly one thousand different types of viruses are known to infect humans and it is estimated that they account for approximately 60% of all human infections (Horsfall 1965).
Viruses are spread easily through closed environments such as the home, schools, workplaces, transport systems, etc. Although many of the respiratory and gastrointestinal infections caused by viruses can be asymptomatic or relatively mild and self‐limiting (coughs and colds, etc.), they still represent a significant economic burden. Increasing numbers of people who have reduced immunity to infection, for whom the consequences of infection can be much more serious, are now cared for at home. At risk groups include not only the immunocompromised but also the elderly, neonates, pregnant women, hospital patients discharged into the community, individuals using immunosuppressive drugs and also those using invasive systems (indwelling catheters) or inhalation systems or devices. Otherwise healthy family members with asthma or allergies also have increased susceptibility to infection. In the UK it is estimated that one in six people in the community belong to an ‘at risk’ group (Bloomfield 2001). World Health Organisation estimates suggest that, by 2025, there will be more than 800 million people over 65 years old in the world, two‐thirds of them in developing countries (Anon. 1998).
Viruses are probably the most common cause of infectious disease acquired within indoor environments. Close personal contact within the home and community settings, such as daycare centres and schools, makes them ideal places for the spread of viral infections. Infected individuals can shed up to 1012 virus particles per ml of faeces with the possibility of transfer of the virus by contaminated hands to surfaces in the bathroom or toilet. Viruses that cause tonsillitis, colds, croup, bronchiolitis, influenza, pneumonia and other respiratory tract infections can be spread in aerosolized droplets. Aerosols produced by coughing, sneezing and talking can be inhaled directly by a susceptible host or may settle onto surfaces. Touching hands or fomites, such as eating utensils, towels or doorknobs, inadvertently contaminated with fresh secretions or vomit, etc. from an infected person and then transferring the virus from the hands to the eyes, nose or mouth, are further routes of spread. Infants are especially vulnerable to such infections because they frequently place objects, such as toys, into their mouths. Transfer of viruses to food during handling and preparation via hands and food contact surfaces is an important route of spread of viral gastroenteritis.
Amongst health care professionals there is growing awareness that improved standards of hand, surface and air hygiene in community settings could do much to prevent the spread of viral infections within these environments. The purpose of this paper is to review the evidence base for this assumption. Since viral infections are not easily treated, prevention of infection is still the main route of control. Assessment of the impact of hygiene is made difficult by the general lack of quantitative epidemiological data and, even where evidence for cross‐contamination as a causative factor in an outbreak exists, it is always circumstantial. A further problem in assessing whether contamination found on hands or other surfaces might represent a hazard is that the infectious dose can vary significantly according to the pathogenicity of the organism and the immune status of the host. Thus the case for practising good hygiene in these settings rests largely on evidence showing that cross‐contamination can occur in these environments coupled with laboratory data demonstrating the efficacy of hygiene procedures in minimizing microbiological contamination.
3. THE BURDEN OF VIRAL INFECTION
3.1 Gastrointestinal infections
In developed countries it is estimated that 30–40% of infectious gastroenteritis cases are attributable to viruses (Thompson 1994). Surveillance data from the UK show that reported outbreaks of viral intestinal infection have increased rapidly over the last 10 years; epidemiological data for 1995 and 1996 (Evans et al. 1998) show that rotavirus, astrovirus, Norwalk‐like viruses (NLVs; also known as small round structured viruses) and other caliciviruses were responsible for 48% of all reported outbreaks of infectious intestinal disease (IID). Other data indicate that NLVs and rotavirus are the commonest pathogens causing outbreaks of gastroenteritis in homes for the elderly (Djuretic et al. 1996; Ryan et al. 1997; Dedman et al. 1998).
Over the period 1993–96 a UK study involving some 460 000 participants was carried out to evaluate rates of IID in the community and presenting to general practice which has given valuable insights into the epidemiology of viral infections in the community (Wheeler et al. 1999). The study indicated that as many as one in five people in the general UK population develop IID each year with an estimated 9·4 million cases occurring annually. It has long been recognized that, since cases and outbreaks related to viral agents are often unreported, the impact of viral intestinal infections may be much greater than national surveillance suggests. The findings of the community study confirmed the validity of this assumption. Wheeler and co‐workers estimated that for every one case of rotavirus and NLV reported to national surveillance a further 35 cases of rotavirus and 1562 cases of NLV occur in the community.
UK surveillance covering 1995–96 showed NLV as a significant cause of epidemic gastroenteritis in community residential and nursing homes, accounting for 43% of all reported general gastroenteritis outbreaks (Evans et al. 1998). The rate of reported NLV infection reaches a peak in children under 5 years and again in the elderly. Foodborne outbreaks can arise from contaminated raw food such as shellfish and also through secondary contamination from food handlers carrying the virus. Foods implicated in outbreaks are mainly those eaten raw, or those not cooked after handling, e.g. salads, cold meats and fruit.
Worldwide, rotavirus is probably the most important viral pathogen causing diarrhoeal disease in infants, infecting virtually all children aged 3–5 years (Parashar et al. 1998a). However, a recent study by Pang et al. (2000) of children between 2 months and 2 years of age with acute gastroenteritis, has shown that human caliciviruses are found as commonly as rotaviruses. In developing countries rotavirus accounts for approximately 6% of all diarrhoeal episodes and 20% of all diarrhoea‐associated deaths of children under 5 years of age, resulting in an estimated 800 000 childhood deaths each year. It is second only to upper respiratory infections in infants under 2 years old as a major cause of death in the developing world (Glass et al. 1997). Each year in the US, 2·7 million children under 5 years old are affected by rotavirus diarrhoea, resulting in 500 000 visits to the doctor and 50 000 hospitalizations (Parashar et al. 1998b). A large proportion of hospital admissions due to gastroenteritis in children under 5 years old were caused by rotavirus in both the UK and Hong Kong (Ryan et al. 1996; Chan et al. 1998). In older children 51% of hospital admissions for acute diarrhoea were associated with rotavirus (Lewis et al. 1979). A study by Isaacs et al. (1986) showed that 20% of children under 14 years old who visited their doctor with diarrhoea had a rotavirus infection. Indications are that hospital admissions only represent a small percentage of rotavirus infections; the majority will be treated by general practitioners.
Rotavirus infections are highly seasonal, peaking in the winter months (Brandt et al. 1982; Ryan et al. 1996; Dedman et al. 1998). It has been suggested that low humidity and people spending more time indoors contribute to the spread of rotavirus infections (Anon. 1995). Such conditions may make it possible for the virus to be spread by the airborne route through environmental contamination (Brandt et al. 1982). A study in the US revealed that rotaviruses infected one or more members in 51% of families, including 28% of children and 13% of adults (Rodriguez et al. 1987). Within infected families rotavirus infection was found in 57% of children and 25% of adults. Some adults acquired rotavirus infections a few days after their children’s illnesses, suggesting that the children rather than the parents brought infection into the home. Rodriguez et al. (1979) also found rotavirus infection in 55% of adult family contacts of children hospitalized with gastroenteritis. In a community study in New Zealand, in families with an index case of rotavirus infection, children were more frequently infected than adults. Once a family member became infected there was a high probability of cross‐infection (Grimwood et al. 1983).
Among children with diarrhoea attending daycare centres, Lew et al. (1991) detected astroviruses and adenoviruses. Astrovirus was significantly more common in children with diarrhoea than those without diarrhoea. Enteric adenoviruses were detected in an equal percentage in children with and without diarrhoea. Children can excrete astrovirus before the onset of diarrhoea and up to 20 d after the diarrhoea has stopped (Mitchell et al. 1993). Although astrovirus primarily infects the young, the elderly can also be affected, with reported outbreaks in care homes and hospital wards for the elderly (Gray et al. 1987; Lewis et al. 1989). Enteric adenoviruses (generally serotypes 40 and 41) are also associated with outbreaks of gastroenteritis in schools, paediatric hospital wards and nursing homes (LeBaron et al. 1990). They may be second to rotavirus as a cause of gastroenteritis in young children (Blacklow and Greenberg 1991).
Globally, hepatitis A virus (HAV) is the most common cause of hepatitis in man (Melnick 1995). Contaminated water or food, particularly filter‐feeding shellfish, frequently transmit hepatitis A but other foods are occasionally implicated (raw milk, dairy products and cold meats). The virus is excreted in high numbers in faeces and is spread from person to person primarily by the faecal–oral route. When personal hygiene is not observed, food handlers may unintentionally transfer the virus to food during the incubation period of the disease (Sundkvist et al. 2000). Outbreaks of viral hepatitis occur in institutions such as daycare centres, hospitals, nurseries and schools (Bern et al. 1992; Dickinson 1992). These outbreaks may lead to secondary cases in the general community (Hadler et al. 1980).
3.2 Respiratory infections
Infections caused by influenza viruses, rhinoviruses, coronaviruses and respiratory syncytial viruses (RSVs) are a major health burden. Estimates suggest that adults suffer two to five colds per year and infants and preschool children have about four to eight colds per year (Sperber 1994). Although such infections are often regarded as trivial, taking into account lost days from work and school, hospital admissions and mortality rates in infants and the elderly, the health and economic costs are considerable. Although the common cold can be caused by a number of viruses, rhinoviruses and coronaviruses predominate. Rhinoviruses are responsible for outbreaks of the common cold in the general community such as schools, daycare centres and hospitals (Denny et al. 1986; Krilov et al. 1986; Kellner et al. 1988). Rhinoviruses and coronaviruses have been found to cause a greater disease burden in elderly people living at home, compared with influenza virus or RSV (Nicholson et al. 1997). Influenza affects all age groups, but it is the elderly and persons with underlying health problems who are at particular risk from complications of influenza and are more likely to require hospitalization.
Respiratory syncytial virus infections occur all over the world and outbreaks are common in the cold season in temperate climates and in the rainy season in tropical climates. Respiratory syncytial virus is a major cause of respiratory illness in young children, affecting about 90% of children by the age of 2 years (Crowcroft et al. 1999; Simoes 1999). School‐aged children often carry RSV to their homes and spread infection to younger siblings. Attack rates within families are high, with about 40% of family members, including adults, becoming infected. In most family outbreaks although more than 95% of infections are symptomatic they are not usually severe (Berglund 1967; Hall et al. 1976a). Infants admitted to hospital with RSV bronchiolitis or pneumonia tend to shed the virus abundantly and for prolonged periods allowing ample opportunity for spread (Hall et al. 1976b). In adults RSV infection generally results in a ‘common cold’ type illness although it can sometimes produce a ‘flu‐like’ syndrome indistinguishable from influenza. Antibodies resulting from an early childhood RSV infection do not prevent further RSV infections later in life. Respiratory syncytial virus is known to cause a high incidence of pneumonia and death in the elderly. In England and Wales it is estimated that RSV causes 60–80% more deaths than influenza, causing about 23 000 deaths each winter (Nicholson 1996).
Parainfluenza viruses (PIVs) are a further major group of respiratory pathogens. They cause severe colds, croup, bronchitis and pneumonia in children and adults and in infants the virus can cause life‐threatening disease (Hall 1987). Infection is probably spread by aerosols in addition to direct contact with contaminated surfaces (Hall et al. 1980). Brady et al. (1990) noted that the persistence of PIV on hospital surfaces contaminated with patients’ secretions was a potential source of transmission.
4. DISPERSAL, PERSISTENCE AND SPREAD OF VIRUSES IN DOMESTIC HOMES AND COMMUNITY SETTINGS
Cross infection from an infected person to a new host depends on a number of factors, including the number of virus particles shed by the infected person, their stability in the environment, in aerosols or on surfaces and the potential for spread within a closed environment (Valenti 1998). Viruses that increase fluid secretions or irritate the respiratory epithelium induce coughing and sneezing, which in turn increases the shedding and transmission of the virus. Although diarrhoea eliminates organisms from the gut, it increases the potential for contamination of the environment and spread of the virus infection. The more particles shed the greater their survival and the greater the chance of reaching a new host. Equally important, the likelihood of cross infection depends on the number of particles that reach the new host, the immune status of that host and the route by which they become infected.
Virus particles can be shed in large numbers in various body fluids from an infected person or a carrier, including blood, faeces, saliva, urine and nasal secretions. The non‐enveloped viruses have greater resistance to drying and thus spread more easily than enveloped viruses, which are less stable in the environment. Laboratory studies show that rotavirus, adenovirus, poliovirus, herpes simplex virus and HAV can survive for significant periods on dry surfaces (Nerurkar et al. 1983; Abad et al. 1994). Although few studies have been carried out in domestic homes, studies in children’s daycare centres (Lew et al. 1991; Keswick et al. 1983b; Butz et al. 1993) and in hospitals (Samadi et al. 1983; Akhter et al. 1995) show that viruses can survive on surfaces and that virus transfer and survival on hands play a part in the transmission of infections.
Bellamy et al. (1998) investigated the domestic environment for the presence of viruses and body fluids that may contain viruses. Haemoglobin was found on 2% of surfaces (taps, washbasins, toilet bowls and seats), indicating the presence of blood and possible contamination with bloodborne viruses. Amylase (an indicator of saliva, sweat and urine) was found on 29% of surfaces, which were frequently handled or in contact with urine. This highlights that surfaces may remain soiled for some time and may not be thoroughly cleaned. Bellamy et al. (1998) also detected enteroviral RNA in three of 448 environmental samples (tap handle, telephone handpiece and toilet bowl). A previous study has shown that enteric viruses can survive on environmental surfaces for up to 60 d (Abad et al. 1994).
Virus transmission in childcare facilities was studied using modified cauliflower virus DNA as an environmental marker (Jiang et al. 1998). The viral DNA, introduced through treated toy balls, spread within a few hours of handling. Although the marker treated objects were removed after 1 d, the viral DNA continued circulating in the facilities for up to 2 weeks. Hand contact with contaminated surfaces played an important part in transmission. The markers were also detected in the children’s homes, on the hands of family members and environmental surfaces, including toys.
Transmission of viruses in a household setting has been recently studied, using bacteriophage φX174 as a model virus with resistance properties similar to polio‐ or parvoviruses (Rheinbaben et al. 2000). Contaminated door handles and skin surfaces were found to be efficient vectors of contamination. At least 14 persons could be contaminated one after another by touching a contaminated door handle. Successive transmission from one person to another could be followed up to the sixth contact person. Transfer from contaminated door handles to other surfaces was also confirmed under everyday life conditions in a flat shared by four students.
Studies focusing on home and community settings are providing a better understanding of how infectious disease is spread in these environments. Such studies suggest that the airborne route is by no means the sole route of transmission of respiratory infections caused by rhinovirus and RSV and that IID, particularly that of viral origin, can arise from various sources of which food is only one. Evans et al. (1998) reported that, whereas 174 of 233 outbreaks of infection attributed to Salmonella were ‘mainly foodborne’ and 15 regarded as ‘mainly person to person’, for 680 reported outbreaks of NLV infection 607 were attributed to person‐to‐person transfer and only 21 were reported as foodborne.
Although epidemiological and surveillance studies provide vital information on modes of infection transmission during outbreaks, they give only a limited picture of how sporadic person‐to‐person transmission actually occurs within community and home environments. Although such data are limited, it is generally acknowledged that person‐to‐person transmission is associated not only with poor hand hygiene but also airborne or surface‐to‐surface transmission. What cannot be deduced from current data is the relative importance of these different modes of person‐to‐person transmission and how it may differ for different viral agents and different communities (home, daycare, etc.). In particular, it is difficult to assess the importance of environmental contamination as a source of secondary cases, but recent data show that this can be a significant factor, particularly in the transmission of NLVs (Anon. 1993). Although direct evidence is lacking, outbreaks in hotels and cruise ships in which recurrent waves of infection occurred in successive cohorts of guests strongly suggests transmission of NLV via environmental sites and surfaces (Ho et al. 1989; Gellert et al. 1994; McEvoy et al. 1996; Cheesbrough et al. 2000). These and other studies which can be used to assess the routes of transmission of viral infections in community and home settings are discussed in the following sections.
4.1 Gastrointestinal viruses
4.1.1 Rotavirus.
Rotavirus is shed in large numbers from an infected person, with faeces often containing> 1012 particles per gram. Children and adults can be asymptomatic excreters of rotavirus (Ansari et al. 1991a) and rotavirus excretion can persist for up to 34 d after diarrhoea has stopped in symptomatic patients (Pickering et al. 1988). More recently, a hospital study showed that 30% of the immunocompetent children excreted rotavirus particles for more than 21 d and as long as 57 d after the onset of diarrhoea (Richardson et al. 1998).
Rotavirus can survive on human hands and transfer of infectious virus to animate and non‐porous inanimate surfaces has been demonstrated (Sattar et al. 1986; Ansari et al. 1988). Ward et al. (1991) examined the transfer of rotavirus from contaminated surfaces to the mouth and from surfaces to hands to the mouth. All of the volunteers who licked rotavirus‐contaminated plates became infected whereas, of those individuals touching the virus‐contaminated plates with their fingers and then their mouths, only about half became infected.
A number of studies in child daycare centres have shown that rotavirus can be widely disseminated when outbreaks occur. In one such centre faecal contamination of hands and the environment was demonstrated during an outbreak of rotavirus diarrhoea (Keswick et al. 1983a). Other studies in daycare centres have shown that 16–30% of surfaces sampled can be contaminated with rotavirus. In particular, hand contact surfaces (e.g. refrigerator handle, toilet handles, telephone receivers and toys) and moist surfaces such as sinks, water fountains and water‐play tables were contaminated with the virus (Keswick et al. 1983a; Wilde et al. 1992; Butz et al. 1993).
Soule et al. (1999) found that there was an increase in the number of environmental surfaces contaminated with rotavirus in a hospital paediatric unit when there was an increase in the number of children suffering from rotavirus gastroenteritis. Of the surfaces in direct contact with children (thermometers, play mats and toys) rotavirus was detected in 63% of samples compared with 36% for surfaces without direct contact (telephones, door handles and washbasins). These findings were similar to those of Akhter et al. (1995) who showed that widespread rotavirus contamination of a paediatric ward and playroom correlated with the presence of patients infected with rotavirus.
In a treatment centre in Bangladesh, handwashings from 78% of the attendants of patients with diarrhoea (children under 5 years) were positive for rotavirus antigens (Samadi et al. 1983). Rotavirus was also found in handwashings of 19% of attendants of patients with non‐rotavirus diarrhoea, indicating that they may have come into contact with other attendants and patients in adjacent beds. This highlights the potential for contaminated hands to spread the infection.
4.1.2 Norwalk‐like viruses.
Projectile vomiting associated with NLVs is probably a major source of cross‐infection because it is estimated that 3 × 107 particles are distributed as an aerosol into the environment during a vomiting attack (Caul 1994). A recent report (Anon. 1993) showed how aerosols produced by vomiting can be inhaled or can contaminate hands or work surfaces, with the potential for subsequent transfer to foods or direct hand‐to‐mouth transfer. The importance of airborne transmission was demonstrated in a recent outbreak in a restaurant where no food source was detected but an analysis of the attack rate showed an inverse correlation with the distance from a person who had vomited (Marks et al. 2000). The potential for secondary transmission via environmental surfaces in semiclosed communities was demonstrated following a wedding reception, where an outbreak of NLV gastroenteritis affected 50% of guests (Patterson et al. 1997). The previous day, a kitchen assistant had vomited in a sink that was subsequently used for preparing vegetables eaten by the wedding guests. Further evidence for transmission of NLV via aerosols and environmental surfaces comes from reports of recurrent waves of NLV gastroenteritis occuring in successive cohorts of guests on a cruise ship over a 2‐year period (Ho et al. 1989). It was found that the risk of gastroenteritis amongst passengers who shared toilet facilities was twice that of those who had a private bathroom. Nosocomial spread is also a major concern. Norwalk‐like virus gastroenteritis in an elderly care unit in a hospital spread rapidly within and between wards, affecting both patients and staff. Analysis of risk exposure showed areas where patients had vomited to be the most significant factor for the spread of NLVs to staff (Chadwick and McCann 1994). A study by Cheesbrough et al. (1997) showed that carpets can also harbour NLVs and serve as reservoirs of infection. Two carpet fitters became ill after removing a carpet from a hospital ward 13 d after the last case in a NLV outbreak. Routine vacuuming every day since the outbreak had not removed the virus. During an outbreak of vomiting and diarrhoea due to NLV in a long‐stay ward for the mentally ill, 36 environmental samples were collected on the affected ward of which 11 (30%) were positive by reverse transcriptase‐polymerase chain reaction. Positive swabs were from lockers, curtains and commodes and were confined to the immediate environment of the affected patients (Green et al. 1998). Most recently the potential for environmental spread of NLVs was demonstrated in a prolonged hotel outbreak in successive cohorts of guests (Cheesbrough et al. 2000). Environmental sampling demonstrated widespread dissemination of the virus on hand contact and other surfaces. From the patterns of infection it was concluded that, although infectious aerosols were probably the main route of dissemination of infection within a particular cohort of guests, contact with contaminated fomites was the most likely factor responsible for maintaining the outbreak by forming the link between successive cohorts.
4.1.3 Hepatitis A virus.
As with other enteric viruses HAV is shed from an infected person in large numbers and is able to survive on environmental surfaces (Mbithi et al. 1991) and be readily transferred to hands (Mbithi et al. 1992). Fomites are potential risk factors in the spread of the virus, especially in hospital wards, daycare centres or restaurants (Cliver 1983). A recent outbreak of HAV was associated with a public house whose barman had chronic diarrhoea and had served drinks while incubating hepatitis A himself (Sundkvist et al. 2000). Fomite transmission by contamination of glasses was the likely route of spread. Assessments of community outbreaks of HAV have shown that persons involved in nappy‐changing in daycare centres often handle food and that this is a potential risk for transmission (Hadler and McFarland 1986). Hepatitis A virus may be acquired from children who are excreting HAV, the majority of whom are asymptomatic (Fox et al. 1974). A significant percentage (23–52%) of susceptible household contacts of index cases with acute HAV infection are at risk of acquiring acute HAV infection from the index case (Minuk et al. 1994). A higher rate of HAV infection amongst children (71–80%) compared with the parents (29%) suggests that play activity among children is a significant factor for HAV transmission in households.
4.2 Respiratory viruses
It is generally accepted that respiratory viruses, such as those which cause the common cold and flu, are spread from person to person by aerosol transmission due to sneezing and coughing. Nevertheless, there is growing evidence that a significant proportion of flu and particularly cold viruses are spread via hands and surfaces such as handkerchiefs and tissues, tap and door handles, telephones or other surfaces touched by an infected person (Eccles 2000; Goldman 2000). Cross infection can occur either by handshaking or by touching the contaminated surface. Rubbing either the nasal mucosa or the eyes with virus‐contaminated hands can cause infection.
Sattar et al. (1993) have shown that rhinoviruses can survive on environmental surfaces for several hours. Infectious viruses have been recovered from naturally contaminated objects in the surroundings of persons with rhinovirus colds (Reed 1975). Clean hands can readily pick up the virus by touching or handling such objects (Ansari et al. 1991b). As much as 70% of infectious rhinovirus on contaminated hands has been shown to transfer to a recipient’s fingers after contact of only 10 s (Gwaltney et al. 1978). After handling contaminated coffee cup handles and other objects, more than 50% of subjects developed an infection (Gwaltney and Hendley 1982). Hendley et al. (1973) and Reed (1975) have demonstrated that rhinoviruses can survive for several hours on the hands and self‐inoculation by rubbing of the nasal mucosa or conjunctivae via virus‐contaminated fingers can lead to infection.
Influenza virus can be shed before the onset of symptoms and for up to 7 d after onset and individuals with influenza can be infectious before they develop symptoms and for up to a week afterwards. Both influenza A and B virus have been shown to survive on hard surfaces such as stainless steel and plastic for 24–48 h and on absorbent surfaces such as cloth, paper and tissues for up to 12 h (Bean et al. 1982). It was shown that influenza A virus could be transferred from contaminated surfaces to hands for up to 24 h after the surface was inoculated. Epidemiological evidence supports the laboratory data because an influenza outbreak in a nursing home suggested that the virus was spread by staff, through hands contaminated directly with body fluids, or by touching contaminated fomites (Morens and Rash 1995).
There is similar evidence for the environmental survival and spread of PIV and RSV. Ansari et al. (1991b) demonstrated the transfer of PIV from stainless steel surfaces to clean fingers, which suggests that fomites have a role as a reservoir for the spread of the virus. Further, PIV could be recovered from non‐absorbent surfaces for as long as 10 h when the surface remained moist. However, Brady et al. (1990) found that, when material containing PIV was spread and allowed to dry, virus was only recoverable for up to 2 h. These workers also showed that PIV persisted on the skin for at least 1 h after contamination, which reinforces the need to perform vigorous handwashing before and after contact with patients and their environment. Likewise, Hall et al. (1980) showed that RSV was recovered from hands touching surfaces contaminated with fresh secretions from RSV‐infected infants. Evidence showing that direct and indirect contact is a key factor in transmission of RSV infection is further reviewed by Goldmann 2000).
4.3 Herpes simplex virus
Humans are the only known reservoir of herpes simplex virus 1 (HSV). The virus is most commonly spread by oral secretions and can be shed by persons with or without symptoms. Herpes simplex virus can be recovered from the skin for up to 2 h after inoculation of the hands with the virus (Bardell 1989). The virus was more readily transmitted from moist drops than from drops which had been allowed to dry, although touching dried virus‐containing droplets on the skin with a moistened finger resulted in transmission of the virus. Infectious HSV has also been recovered from environmental surfaces such as doorknobs and toilet seats, although it is not clear what role fomites play in the spread of herpes viruses (Larson and Bryson 1982; Bardell 1990; Bardell 1993).
4.4 Varicella virus
A recent study demonstrated the rapid and broad contamination of the environment with varicella‐zoster virus (VZV) when a family member acquired the disease (Asano et al. 1999). Eight days after onset of the index case VZV DNA was detected in both samples from the patient and on the surfaces of an air‐conditioning filter, a table, television channel push‐buttons and a door handle. The virus was also detected on the hands of the parents and children. Two siblings developed the disease 18 d after onset of the index case.
4.5 The infectious dose
The problem in assessing whether contamination in the environment might be a hazard is that the infectious dose can vary significantly according to the immune status of the individual. It is clear that increasingly the variability in immune status of individuals is becoming a significant factor in community and domestic settings as well as in the hospital environment. Although some viruses survive relatively poorly in the environment, the low infectious dose of many viral pathogens, even for individuals regarded as ‘healthy’, suggests that, where body fluids naturally contaminate objects with a high viral load, the virus can persist in sufficient numbers to act as sources of infection for several hours, weeks or even months (Sattar and Springthorpe 1999). The infective dose for NLVs may be as low as 10–100 particles, indicating that both aerosol and surface contamination could be a route of transfer of infection (Caul 1994). Likewise, the infective dose for rotavirus may be as few as 10 particles and person‐to‐person transmission probably perpetuates endemic disease (Ward et al. 1986). A minimal infective dose of less than 10 plaque‐forming units has been demonstrated for poliovirus (Minor et al. 1981). Respiratory viruses also have low infective doses. For rhinoviruses, the infective dose via the nasal route may be less than 1 TCID50 (Couch 1990), i.e. the tissue culture infective dose infecting 50% of the cells. Conversely, PIVs have an infective dose via the intranasal route of 80 TCID50 (Smith et al. 1966).
5. EVIDENCE THAT HYGIENE CAN PLAY A PART IN PREVENTING TRANSMISSION OF VIRAL INFECTIONS
Although studies about the survival characteristics of viruses represent an important component in understanding the infection potential and the preventive role of hygiene, much of our knowledge comes from reports of infection outbreaks where hygiene procedures have been defective or from case control studies. Fifteen such reports have been examined in which viral contamination was directly implicated or for which viral agents were likely to have been the cause of the infections. The effects of the hygiene intervention procedures are summarized in Table 1, 1 and relate to daycare and other community centres where the concentration of people and activity provides the most cost‐effective setting for evaluation of the impact of hygiene procedures. Although opportunities for cross‐contamination and cross‐infection may occur less frequently in the home it could be argued that, since the ratio of homes to daycare centres is very large, the impact of these environments on the overall infection rates across a community may not be so dissimilar, even though daycare centres bring more people together. None of the investigations cited relate specifically to the home but Fornasini et al. (1992) and Osterholm et al. (1992) report studies of disease transmission from daycare centres to the home where it is transferred among family members.
Table 1.
The effects of hygiene measures in the control of infection in homes and community settings

Table 1.
(continued)
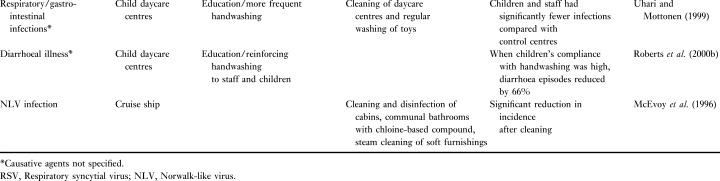
In eight of the 15 studies only the impact of handwashing was evaluated. In a 36‐week handwashing education programme in child daycare centres, Black et al. (1981) showed that the incidence of diarrhoea in children was significantly reduced compared with two control centres. Kilgore et al. (1996) studied the prevalence of neonatal rotavirus infection in Bangladesh. They found an increased risk for neonatal rotavirus infection among infants whose mothers reported no handwashing during care of the neonate.
In a study carried out during the cold and flu season at two daycare centres, fewer colds were reported in the test group of 3–5‐year‐olds using proper and frequent handwashing techniques than in the control group. In the test centre the proportion of colds remained fairly constant at 18·9% whilst in the control group the proportion of colds increased from 12·7% to 27·8% (Niffenegger 1997). Carter et al. (1980) demonstrated that families who used an iodine‐based hand disinfectant, known to kill rhinoviruses, had lower rates of infection than families using an inactive handwash. To decrease respiratory infections in senior daycare centres, staff were educated on viral transmission and the value of handwashing (Falsey et al. 1999). In the intervention year, the infection rate among those attending the centres was significantly lower than in the previous 3 years, with an almost 50% decrease in the infection rate. Roberts et al. (2000a) carried out a randomized controlled trial of the effect of infection control measures on the frequency of upper respiratory infection in childcare. The intervention measures were training of childcare staff about transmission of infection, handwashing and aseptic nose‐wiping technique. When compliance with infection control practice was high, the incidence of colds was reduced by 17%. A similar study by these workers also examined the effects of infection control measures on the frequency of diarrhoeal episodes in childcare using a randomized controlled trial (Roberts et al. 2000b). They found that, for those centres in which children’s compliance with handwashing was high, diarrhoeal episodes were reduced by 66%. In the US, an outbreak of aseptic meningitis due to echovirus 30 was reported amongst parents with children attending a childcare centre. It was found that more frequent handwashing among the teachers compared with the parents of young children was associated with significantly lower rates of infection (Helfand et al. 1994).
In six of the 15 studies handwashing combined with environmental decontamination or other control measures was considered, whilst one study which related to NLV infection highlighted only the importance of environmental disinfection. In a preschool daycare centre, respiratory and gastrointestinal infections decreased following implementation of measures which included reinforcing existing handwashing procedures and education of staff and families on issues of infection control including environmental surface cleaning and disinfection and disinfection of toys (Krilov et al. 1996). Uhari and Mottonen (1999) evaluated an infection prevention programme for reducing the transmission of infections in child daycare centres. It was evident that most of the infections that did occur were viral. The programme included increased handwashing, cleaning of the daycare centres and regular washing of toys. Both the children and staff had significantly fewer infections that those in control centres.
St. Sauver et al. (1998) studied hygienic practices and the prevalence of respiratory illness in children attending daycare homes. Never or rarely washing hands by both children and carers was associated with a higher frequency of respiratory illness in both family and group daycare homes. Using shared cloth towels rather than individual paper towels and washing of sleeping mats less than once a week were also associated with a higher frequency of upper respiratory infection.
Isaacs et al. (1991) reported a sevenfold reduction in the incidence of RSV in a hospital when patients and staff were educated about the importance of handwashing and infected babies were segregated. Before intervention 4·2% of children under 2 years old developed nosocomial RSV, whilst after intervention only 0·6% developed infection. Following implementation of a hygiene intervention programme that included handwashing education, use of gloves, disposable nappy pads and an alcohol‐based hand rinse the incidence of enteric illness was lowered in intervention child daycare homes as compared with control homes (Butz et al. 1990).
As stated previously, contamination of the environment may be considerable during an outbreak of NLV. Following outbreaks of viral gastroenteritis on consecutive cruises, a ship was cleared and disinfected at the end of the fourth cruise in order to interrupt transmission of NLV (McEvoy et al. 1996). Fewer than 10 cases presented in each of the fifth and sixth cruises compared with 195 cases during the fourth cruise. Control measures included cleaning and disinfection of cabins, crew and staff quarters and communal bathrooms and steam cleaning of soft furnishings. Hygiene measures were also introduced into the kitchen. The contamination of soft furnishing in areas where individuals have vomited presents a difficult cleaning problem and steam cleaning has been recommended by McEvoy et al. (1996).
During a hospital gastroenteritis outbreak caused by NLV, the attack rate among patients decreased in several wards following the implementation of environmental hygiene procedures (Chadwick and McCann 1994). Infection control measures implemented included cleaning and chemical disinfection (ward floors, toilet areas, toilet seats, taps and spillages of vomit and faeces) to reduce environmental contamination. Hypochlorite solution (1%) was used for disinfection of places contaminated with vomit or faeces and 0·1% hypochlorite for general disinfection of ward floors and toilet areas.
Since the studies highlighted in Table 1, 1 involved the implementation of infection control programmes involving several steps, it is difficult to attribute the effectiveness of the hygiene procedures to one specific aspect because they were inherently multifaceted. Indeed, the results do not prove that the various interventions had a direct effect in decreasing infection rates. It could be argued that the reduced rates were due to variations in individual susceptibility to infection or to a lower incidence of the pathogen amongst the case control groups. Nevertheless, overall, there is convincing circumstantial evidence to suggest that improved standards of hygiene can have a significant impact in reducing the rates of respiratory, intestinal and other viral infections in childcare facilities, domestic homes, hospitals and adult care centres and the circulation of infections between these communities.
6. DEVELOPMENT OF EFFECTIVE HYGIENE POLICIES FOR PREVENTION OF VIRAL INFECTIONS
The data reviewed show how improved standards of education and integrated hygiene measures, including hand and environmental hygiene, could have a significant impact in reducing infectious diseases within community and home environments. In recent years the concept of risk assessment or Hazard Analysis Critical Control Point (HACCP) has successfully controlled microbial risks in food and other manufacturing environments. Traditionally, the public has tended to regard good hygiene as creating an environment free of germs. To devise a hygiene policy that has real public health benefits, it is now accepted that a risk‐based approach should also be adopted (Bloomfield and Scott 1997; Jones 1998; Scott 1999).
A risk assessment approach to hygiene starts from the premise that homes and other settings always contain potentially harmful microbes (people, pets, food, etc.) and that good hygiene is not about eradication but about targeting measures in the places and at the times that matter, in order to limit risks of exposure. For both the hands and for environmental surfaces hygiene can be achieved by physical removal of organisms from the surface. Alternatively, organisms can be inactivated in situ by a disinfection process or a combination of both physical removal and disinfection. In many situations such as the hands, and cooking and eating utensils, appropriate risk reduction can be achieved using detergent and hot water. However, since, in this situation, hygiene is achieved by removal of the microbes from the surface, if it is to be effective it must be applied in conjunction with a thorough rinsing process with clean water and must take account of the strength of attachment of the microbes to the surface (Eginton et al. 1995). Stevens and Holah (1993) showed that wiping of contaminated abraded surfaces using a sponge followed by a 10‐s rinse produced a 3‐log reduction in bacterial contamination of stainless steel surfaces but only a 1–1·5‐log reduction on enamelled steel, mineral resin and polycarbonate surfaces. Scanning electron microscope studies showed that bacteria were typically retained in surface imperfections, such that surfaces which sustained the most extensive damage retained higher numbers of bacteria.
Studies by Schurmann and Eggers (1985) showed that enteric viruses may be more strongly bound to the skin surface and that the inclusion of an abrasive substance, such as sand or aluminium hydroxide, in the handwash preparation is advisable to achieve effective virus removal. Recent studies of the transmission of viruses in a household setting using bacteriophage φX174 as a model showed that virus spread was not prevented by the usual standards of hand hygiene as practised in the household (Rheinbaben et al. 2000). The virus was reisolated after 24 h from the hands of all persons tested even after normal use and cleaning of the hands.
Biocides that have activity against both enveloped and non‐enveloped viruses include chlorine‐ and iodine–releasing agents, peracids and ozone (Rotter 1997; Sattar and Springthorpe 1999). Biocide effectiveness depends on the nature of the virus, the surface carrier, the presence of interfering substances such as organic soil and hard water salts and the contact time. Although these compounds can be used for disinfection of environmental surfaces they are generally too toxic and irritant for use on the skin. In achieving decontamination of hands, although handrub and handwash products currently available may have good activity against bacterial pathogens, activity against viral contamination is variable and depends on the type of virus. Rotter (1997) suggested that, although alcoholic handrubs are effective against enveloped viruses such as influenza, PIV, herpes and RSV, activity against non‐enveloped viruses such as rotaviruses, rhinovirus, poliovirus, adenovirus, NLV and hepatitis virus is limited unless extended contact times (up to 10 min) are used. Similarly, agents such as triclosan and chorhexidine have some activity against enveloped virus but are not considered effective against non‐enveloped viruses.
7. CONCLUSIONS
It is well established that viruses are shed in large numbers and can survive for long periods on surfaces or fomites commonly found in many environments and this emphasizes the possible role of surfaces in the transmission of viruses. Faeces can contain up to 1012 virus particles per gram and vomit up to 107 per millilitre so the potential for hand and environmental contamination is considerable. Viral shedding may begin before the onset of symptoms and may continue for several days or even weeks after the symptoms have ceased. Virus transfer from surfaces to hands, fingers and food has been demonstrated. Other studies have shown a high rate of spread once a viral infection is introduced into a family home or institution. Improved handwashing and surface hygiene procedures have been shown to interrupt the transmission of viral infections via hands, surfaces or fomites.
Although the importance of hygiene and most particularly handwashing cannot be over‐emphasized as a means of reducing infections it can be difficult to enforce even in healthcare facilities where staff should be aware of the infection risks. Studies have shown that handwashing compliance amongst healthcare workers is variable (Daniels and Rees 1999; McGuckin et al. 1999; Nishimura et al. 1999; Pittet et al. 1999). In a department of surgery, clinicians washed their hands between examinations in only 41% of cases (Daniels and Rees 1999). In continuous video‐camera surveillance of an intensive care unit personnel complied with handwashing in 71% of entries, whereas visitors of patients complied in 94% of entries (Nishimura et al. 1999). A recent survey of beliefs and attitudes towards hygiene in domestic homes showed that over 74% recognized handwashing as a key preventative measure in ensuring food safety and 66% believed that surface cleaning was also important. However, the respondents admitted that they would not carry out these procedures as frequently as they thought they should (Mathias 1999).
The importance of hands in the transmission of virus infections is well recognized and many of the studies cited in this review relate specifically to handwashing interventions. Increasingly however, there is evidence that cross contamination via surfaces is a significant contributory factor. Most particularly hand contact with contaminated surfaces is likely to be the cause of such cross contamination. Sattar and Springthorpe (1999) and Lieberman (1994) emphasized that, if hygiene programmes are to be effective, hand hygiene education must be integrated with education about the importance of surface and air hygiene in prevention of infection transmission.
To motivate changes in attitude to hygiene it will be necessary to gain acceptance that homes and other community settings will always contain potentially harmful microbes and that good hygiene is not about eradication but about targeting the correct measures at the times that matter, in order to reduce infection risks. There is a need for wider understanding of the potential for contaminated surfaces to act as unidentified vectors of pathogens, in the recontamination of hands, during the infection transmission cycle. The epidemiological evidence to date shows that raising awareness about the importance of key procedures, such as through handwashing and surface hygiene (particularly hand and food contact surfaces), will have a considerable impact in the control and prevention of infectious organisms.
References
- 1. Abad, F.X. , Pinto, R.M. , Bosch, A. (1994) Survival of enteric viruses on environmental fomites. Applied and Environmental Microbiology 60 , 3704–3710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Akhter, J. , Al‐Hajjar, S. , Myint, S. , Hussain Qadri, S.M. (1995) Viral contamination of environmental surfaces on a general paediatric ward and playroom in a major referral centre in Riyadh. European Journal of Epidemiology 11 , 587–590. [DOI] [PubMed] [Google Scholar]
- 3. Anon . (1993) Outbreaks of viral gastroenteritis associated with SRSVs. PHLS Microbiology Digest 10 , 2–8. [Google Scholar]
- 4. Anon . (1995) A working party of the Public Health Laboratory service Salmonella Committee. The prevention of human transmission of gastro‐intestinal infections, infestations and bacterial intoxications. Communicable Disease Report Review 5 , R158–R172. [PubMed] [Google Scholar]
- 5. Anon . (1998) The World Health Report 1998 Life in the 21st Century, a Vision for All Geneva: World Health Organisation.
- 6. Ansari, S.A. , Sattar, S.A. , Springthorpe, G.A. , Wells, G.A. , Tostowaryk, W. (1988) Rotavirus survival on human hands and transfer of infectious virus to animate and non‐porous inanimate surfaces. Journal of Clinical Microbiology 26 , 1513–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ansari, S.A. , Springthorpe, V.S. , Sattar, S.A. (1991a) Survival and vehicular spread of human rotaviruses — possible relation to seasonality of outbreaks. Reviews of Infectious Diseases 13 , 448–461. [DOI] [PubMed] [Google Scholar]
- 8. Ansari, S.A. , Springthorpe, V.S. , Sattar, S.A. , Rivard, S. , Rahman, M. (1991b) Potential role of hands in the spread of respiratory viral infections — studies with human parainfluenza virus 3 and rhinovirus 14. Journal of Clinical Microbiology 29 , 2115–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Asano, Y. , Yoshikawa, T. , Ihira, M. , Furukawa, M. , Suzuki, K. , Suga, S. (1999) Spread of varicella‐zoster virus DNA to family members and environments from siblings with varicella in a household. Paediatrics 103 , E611–E613. [DOI] [PubMed] [Google Scholar]
- 10. Bardell, D. (1989) Hand‐to‐hand transmission of herpes simplex virus type 1. Microbios 59 , 93–100. [PubMed] [Google Scholar]
- 11. Bardell, D. (1990) Survival of herpes simplex virus type 1 on some frequently touched objects in the home and public buildings. Microbios 63 , 145–150. [PubMed] [Google Scholar]
- 12. Bardell, D. (1993) Survival of herpes simplex virus type 1 in saliva and tap water contaminating some common objects. Microbios 74 , 81–87. [PubMed] [Google Scholar]
- 13. Bean, B. , Moore, B.M. , Peterson, L.R. , Gerding, D.N. , Balfour, H.H. (1982) Survival of influenza viruses on environmental surfaces . Journal of Infectious Diseases 146 , 47–51. [DOI] [PubMed] [Google Scholar]
- 14. Bellamy, K. , Laban, K.L. , Barrett, K.E. , Talbot, D.C.S. (1998) Detection of viruses and body fluids which may contain viruses in the domestic environment . Epidemiology and Infection 121 , 673–680.DOI: 10.1017/s0950268898001678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Berglund, B. (1967) Respiratory syncytical virus infections in families. Acta Paediatrica Scandinavica 56 , 395–404. [DOI] [PubMed] [Google Scholar]
- 16. Bern, C. , Martines, J. , De Zoysa, I. , Glass, R.I. (1992) The magnitude of the global problem of diarrhoeal disease: a ten year update. WHO Bulletin 70 , 705–714. [PMC free article] [PubMed] [Google Scholar]
- 17. Black, R.E. , Dykes, A.C. , Anderson, K.E. , Wells, J.G. , Sinclair, S.P. , Gary, G.W. Jr , Hatch, M.H. , Gangarosa, E.J. (1981) Handwashing to prevent diarrhoea in day‐care centres. American Journal of Epidemiology 113 , 445–451. [DOI] [PubMed] [Google Scholar]
- 18. Blacklow, N.R. & Greenberg, H.B. (1991) Viral gastroenteritis. New England Journal of Medicine 325 , 252–264. [DOI] [PubMed] [Google Scholar]
- 19. Bloomfield, S.F. (2001) How hygienic should our homes be? Professional Care of Mother and Child 11, 3–4.
- 20. Bloomfield, S.F. & Scott, E. (1997) Cross‐contamination and infection in the domestic environment and the role of chemical disinfectants. Journal of Applied Microbiology 83 , 1–9. [DOI] [PubMed] [Google Scholar]
- 21. Brady, M.T. , Evans, J. and , Cuartas, J. (1990) Survival and disinfection of parainfluenza viruses on environmental surfaces. American Journal of Infection Control 18 , 18–23. [DOI] [PubMed] [Google Scholar]
- 22. Brandt, C.D. , Kim, H.W. , Rodriguez, W.J. , Arrobio, J.O. , Jeffries, B.C. , Parrott, R.H. (1982) Rotavirus gastroenteritis and weather. Journal of Clinical Microbiology 16 , 478–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Butz, A.M. , Fosarelli, P. , Dick, J. , Cusack, T. , Yolken, R. (1993) Prevalence of rotavirus on high‐risk fomites in day care facilities. Paediatrics 92 , 202–205. [PubMed] [Google Scholar]
- 24. Butz, A.M. , Larson, E. , Fosarelli, P. , Yolken, R. (1990) Occurrence of infectious symptoms in children in day care homes. American Journal of Infection Control 18 , 347–353. [DOI] [PubMed] [Google Scholar]
- 25. Carter, C.H. , Hendley, J.O. , Mika, L.A. , Gwaltney, J.M. (1980) Rhinovirus inactivation by aqueous iodine in vitro and on skin . Proceedings of the Society for Experimental Biology and Medicine 165 , 380–383. [DOI] [PubMed] [Google Scholar]
- 26. Caul, E.O. (1994) Small round structured viruses — airborne transmission and hospital control. Lancet 343 , 1240–1242. [DOI] [PubMed] [Google Scholar]
- 27. Chadwick, P.R. & McCann, R. (1994) Transmission of a small round structured virus by vomiting during a hospital outbreak of gastroenteritis. Journal of Hospital Infection 26 , 251–259. [DOI] [PubMed] [Google Scholar]
- 28. Chan, P.K.S. , Tam, J.S. , Nelson, E.A.S. , Fung, K.S. , Adeyemi‐Doro, F.A.B. , Fok, T.F. , Cheng, A.F. (1998) Rotavirus infection in Hong Kong: epidemiology and estimates of disease burden. Epidemiology and Infection 120 , 21–325.DOI: 10.1017/s0950268897008364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cheesbrough, J.S. , Barkess‐Jones, L. , Brown, D.W. (1997) Possible prolonged environmental survival of small round structured viruses. Journal of Hospital Infection 35 , 325–326. [DOI] [PubMed] [Google Scholar]
- 30. Cheesbrough, J.S. , Green, J. , Gallimore, C.I. , Wright, P.A. , Brown, D.W.G. (2000) Widespread environmental contamination with Norwalk‐like viruses (NLV) detected in a prolonged hotel outbreak of gastroenteritis. Epidemiology and Infection 125 , 93–98.DOI: 10.1017/s095026889900432x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cliver, D.O. (1983) Manual on Food Virology. Publication No. VPH/83.46. Geneva: World Health Organisation.
- 32. Couch, R.B. (1990) Rhinoviruses. In Fields Virology eds. Fields, B.N., Knipe, D.M., Chanock, R.M., Hirsch, M.S., Melnick, J.L., Monath, T.P. and Roizman, B. pp. 607–629. New York: Raven Press.
- 33. Crowcroft, N.S. , Cutts, F. , Zambon, M.C. (1999) Respiratory syncytical virus: an underestimated cause of respiratory infection, with prospects for a vaccine. Communicable Disease and Public Health 2 , 234–241. [PubMed] [Google Scholar]
- 34. Daniels, I.R. & Rees, B.I. (1999) Handwashing: simple but effective. Annals of the Royal College of Surgeons of England 81 , 117–118. [PMC free article] [PubMed] [Google Scholar]
- 35. Dedman, D. , Laurichesse, H. , Caul, E.O. , Wall, P.G. (1998) Surveillance of small round structured virus infection in England and Wales, 1990–5. Epidemiology and Infection 121 , 139–149.DOI: 10.1017/s0950268898001095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Denny, F.W. , Collier, A.M. , Henderson, F.W. (1986) Acute respiratory infections in day care. Review of Infectious Diseases 8 , 527–532. [DOI] [PubMed] [Google Scholar]
- 37. Dickinson, C.J. (1992) Hepatitis A — new information on an old virus. Hepatology 16 , 1099–1101. [DOI] [PubMed] [Google Scholar]
- 38. Djuretic, T. , Ryan, M.J. , Fleming, D.M. , Wall, P.G. (1996) Infectious intestinal disease in elderly people. Communicable Disease Report Review 6 , R107–R112. [PubMed] [Google Scholar]
- 39. Eccles, R. (2000) International Scientific Forum on Home Hygiene. Spread of common colds and influenza. World Wide Web. Http://www.ifh-homehygiene.org/newspage/new05.htm.
- 40. Eginton, P.J. , Gibson, H. , Holah, J. , Handley, P.S. , Gilbert, P. (1995) Quantification of the ease of removal of bacteria from surfaces. Journal of Industrial Microbiology 15 , 305–310. [DOI] [PubMed] [Google Scholar]
- 41. Evans, H.S. , Madden, P. , Douglas, C. , Adak, G.K. , O'Brien, S.J. , Djuretic, T. , Wall, P.G. , Stanwell‐Smith, R. (1998) General outbreaks of infectious intestinal disease in England and Wales: 1995 and 1996. Communicable Disease and Public Health 1 , 165–171. [PubMed] [Google Scholar]
- 42. Falsey, A.R. , Criddle, M.M. , Kolassa, J.E. , McCann, R.M. , Brower, C.A. , Hall, W.J. (1999) Evaluation of a handwashing intervention to reduce respiratory illness rates in senior day‐care centers. Infection Control and Hospital Epidemiology 20 , 200–202. [DOI] [PubMed] [Google Scholar]
- 43. Fornasini, M. , Reves, R.R. , Murray, B.E. , Pickering, L.K. (1992) Trimethoprim‐resistant Escherichia coli in households of children attending day care centres. Journal of Infectious Diseases 166 , 326–330. [DOI] [PubMed] [Google Scholar]
- 44. Fox, M.K. , Langner, S.B. , Wells, R.W. (1974) How good is handwashing practice? American Journal of Nursing 74 , 1676–1678. [PubMed] [Google Scholar]
- 45. Gellert, G.A. , Waterman, S.H. , Ewert, D. (1994) An outbreak of gastro‐enteritis caused by small round structured virus in a geriatric convalescent facility. Infection Control and Hospital Epidemiology 11 , 459–464. [DOI] [PubMed] [Google Scholar]
- 46. Glass, R.I. , Bresee, J.S. , Parashar, U.D. , Miller, M.A. , Gentsch, J.R. (1997) Rotavirus vaccines at the threshold. Nature Medicine 3 , 10–11. [DOI] [PubMed] [Google Scholar]
- 47. Goldmann, D.A. (2000) Transmission of viral respiratory infections in the home. Paediatric Infectious Disease Journal 19 , S97–S102. [DOI] [PubMed] [Google Scholar]
- 48. Gray, J.J. , Wreghitt, T.G. , Cubitt, W.D. , Elliott, P.R. (1987) An outbreak of gastroenteritis in a home for the elderly associated with astrovirus type 1 and humans calicivirus . Journal of Medical Virology 23 , 377–381. [DOI] [PubMed] [Google Scholar]
- 49. Green, J. , Wright, P.A. , Gallimore, C.I. , Mitchell, O. , Morgan‐Capner, P. , Brown, D.W.G. (1998) The role of environmental contamination with small round structured viruses in a hospital outbreak investigated by reverse‐transcriptase polymerase chain reaction assay. Journal of Hospital Infection 39 , 39–45. [DOI] [PubMed] [Google Scholar]
- 50. Grimwood, K. , Abbott, G.D. , Fergusson, D.M. , Jennings, L.C. , Allan, J.M. (1983) Spread of rotavirus with families: a community‐based study. British Medical Journal 287 , 57–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gwaltney, J.M. & Hendley, J.O. (1982) Transmission of experimental rhinovirus infection by contaminated surfaces. American Journal of Epidemiology 116 , 828–833. [DOI] [PubMed] [Google Scholar]
- 52. Gwaltney, J.M. Jr , Moskalski, P.B. , Hendley, J.O. (1978) Hand‐ to‐hand transmission of rhinovirus colds. Annals of Internal Medicine 88 , 463–467. [DOI] [PubMed] [Google Scholar]
- 53. Hadler, S.C. & McFarland, L. (1986) Hepatitis in day care centers: epidemiology and prevention. Reviews of Infectious Diseases 8 , 548–557. [DOI] [PubMed] [Google Scholar]
- 54. Hadler, S.C. , Webster, H.M. , Erben, J.J. , Swanson, J.E. , Maynard, J.E. (1980) Hepatitis A in daycare centers — a community‐wide assessment. New England Journal of Medicine 302 , 1222–1227. [DOI] [PubMed] [Google Scholar]
- 55. Hall, C.B. (1987) Parainfluenza viruses. In Textbook of Paediatric Infectious Diseases eds Feigin, R.D. and Cherry, J.D. pp. 1632–1646. Philadelphia: W.B. Saunders.
- 56. Hall, C.B. , Douglas, R.G. Jr , Geiman, J.M. (1976b) Respiratory syncytical virus infections in infants: quantitation and duration of shedding. Journal of Paediatrics 89 , 11–15. [DOI] [PubMed] [Google Scholar]
- 57. Hall, C.B. , Douglas, R. Jr , Geiman, J.M. (1980) Possible transmission by fomites of respiratory syncytial virus. Journal of Infectious Diseases 141 , 98–102. [DOI] [PubMed] [Google Scholar]
- 58. Hall, C.B. , Geiman, J.M. , Biggar, R. , Kotok, D.I. , Kogan, P.M. , Douglas, R.G. (1976a) Respiratory syncytial virus infections within families. New England Journal of Medicine 294 , 414–419. [DOI] [PubMed] [Google Scholar]
- 59. Helfand, R.F. , Khan, A.S. , Pallansch, M.A. , Alexander, J.P. , Meyers, H.B. , DeSantis, R.A. , Schonberger, L.B. , Anderson, L.J. (1994) Echovirus 30 infection and aseptic meningitis in parents of children attending a child‐care centre. Journal of Infectious Diseases 169 , 1133–1137. [DOI] [PubMed] [Google Scholar]
- 60. Hendley, J.O. , Wenzel, R.P. , Gwaltney, J.M. (1973) Transmission of rhinovirus colds by self inoculation. New England Journal of Medicine 288 , 1361–1364. [DOI] [PubMed] [Google Scholar]
- 61. Ho, M.‐S. , Glass, R.I. , Monroe, S.S. , Madore, H.P. , Stine, S. , Pinsky, P.F. , Cubitt, D. , Ashley, C. , Caul, E.O. (1989) Viral gastroenteritis aboard a cruise ship. Lancet 2 , 961–965. [DOI] [PubMed] [Google Scholar]
- 62. Horsfall, F.L. (1965) General principles and historical aspects. In Viral and Rickettsial Infections of Man ed. Horsfall, F.L. Jr & Tamm, I. pp. 1–10. New York: Lippincott.
- 63. Isaacs, D. , Day, D. , Crook, S. (1986) Childhood gastroenteritis: a population study. British Medical Journal 293 , 545–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Isaacs, D. , Dickson, H. , O'Callaghan, C. , Sheaves, R. , Winter, A. , Moxon, E.R. (1991) Handwashing and cohorting in prevention of hospital acquired infections with respiratory syncytial virus. Archives of Disease in Childhood 66 , 227–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Jiang, X. , Dai, X. , Goldblatt, S. , Buescher, C. , Cusack, T.M. , Matson, D.O. , Pickering, L.K. (1998) Pathogen transmission in child care settings studied by using a cauliflower virus DNA as a surrogate marker. Journal of Infectious Diseases 177 , 881–888. [DOI] [PubMed] [Google Scholar]
- 66. Jones, M.V. (1998) Application of HACCP to identifying hygiene risks in the home. International Biodeterioration and Biodegradation 41 , 191–199. [Google Scholar]
- 67. Kellner, G. , Popow‐Kraupp, T. , Kundi, M. , Binder, C. , Wallner, H. , Kunz, C. (1988) Contribution of rhinoviruses to respiratory viral infections in childhood: a prospective study on a mentally hospitalized infant population. Journal of Medical Virology 25 , 455–469. [DOI] [PubMed] [Google Scholar]
- 68. Keswick, B.H. , Pickering, L.K. , DuPont, H.L. , Woodward, W.E. (1983a) Prevalence of rotavirus in children in day‐care centres. Journal of Paediatrics 103 , 85–86. [DOI] [PubMed] [Google Scholar]
- 69. Keswick, B.H. , Pickering, L.K. , DuPont, H.L. , Woodward, W.E. (1983b) Survival and detection of rotaviruses on environmental surfaces in day care centres. Applied and Environmental Microbiology 46 , 813–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kilgore, P.E. , Unicomb, L.E. , Gentsch, J.R. , Albert, M.J. , McElroy, C.A. , Glass, R.I. (1996) Neonatal rotavirus infection in Bangladesh: strain characterization and risk factors for nosocomial infection. Paediatric Infectious Diseases 15 , 672–677. [DOI] [PubMed] [Google Scholar]
- 71. Krilov, L.R. , Barone, S.R. , Mandel, F.S. , Cusack, T.M. , Gaber, D.J. , Rubino, J.R. (1996) Impact of an infection control program in a specialized preschool. American Journal of Infection Control 24 , 167–173. [DOI] [PubMed] [Google Scholar]
- 72. Krilov, L. , Pierik, L. , Keller, E. , Mahan, K. , Watson, D. , Hirsch, M. , Hamparian, V. , McIntosh, K. (1986) The association of rhinoviruses with lower respiratory tract diseases in hospitalized patients. Journal of Medical Virology 19 , 345–352. [DOI] [PubMed] [Google Scholar]
- 73. Larson, T. & Bryson, Y. (1982) Fomites and herpes simples virus: the toilet seat revisited. Paediatric Research 16 , 244–244, abstract no. 995. [Google Scholar]
- 74. LeBaron, C.W. , Furutan, N.P. , Lew, J.F. , Allen, J.R. , Gouvae, V. , Moe, C. , Monroe, S.S. (1990) Viral agents of gastroenteritis: public health importance and outbreak management. Morbidity and Mortality Weekly Report 39 , 1–24. [PubMed] [Google Scholar]
- 75. Lew, J.F. , Moe, C.L. , Monroe, S.S. , Allen, J.R. , Harrison, B.M. , Forrester, B.D. , Stine, S.E. , Woods, P.A. , Hierholzer, J.C. , Herrmann, J.E. , Blacklow, N.R. , Bartlett, A.V. , Glass, R.I. (1991) Astrovirus and adenovirus associated with diarrhoea in children in day care settings. Journal of Infectious Diseases 164 , 673–678. [DOI] [PubMed] [Google Scholar]
- 76. Lewis, D.C. , Lightfoot, N.F. , Cubitt, W.D. , Wilson, S.A. (1989) Outbreaks of astrovirus type 1 and rotavirus gastroenteritis in a geriatric inpatient population. Journal of Hospital Infection 14 , 9–14. [DOI] [PubMed] [Google Scholar]
- 77. Lewis, H.M. , Parry, J.V. , Davies, H.A. (1979) A year’s experience of the rotavirus syndrome and its association with respiratory illness. Archives of Disease in Childhood 54 , 125–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lieberman, J.M. (1994) Rotavirus and other viral causes of gastroenteritis. Paediatric Annals 23 , 529–535. [DOI] [PubMed] [Google Scholar]
- 79. Marks, P.J. , Vipond, I.B. , Carlisle, D. , Deakin, D. , Fey, R.E. , Caul, E.O. (2000) Evidence for airborne transmission of Norwalk‐like virus (NLV) in a hotel restaurant. Epidemiology and Infection 124 , 481–487.DOI: 10.1017/s0950268899003805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Mathias, K.A. (1999) The use of consumer knowledge, beliefs and attitudes in the development of a local authority strategy for domestic food hygiene education. MPhil Thesis. Open University.
- 81. Mbithi, J.N. , Springthorpe, V.S. , Boulet, J.R. , Sattar, S.A. (1992) Survival of hepatitis A virus on human hands and its transfer on contact with animate and inanimate surfaces. Journal of Clinical Microbiology 30 , 757–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Mbithi, J.N. , Springthorpe, V.S. , Sattar, S.A. (1991) Effect of relative humidity and air temperature on survival of Hepatitis A virus on environmental surfaces. Applied and Environmental Microbiology 57 , 1394–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. McEvoy, M. , Blake, W. , Brown, D. , Green, J. , Cartwright, R. (1996) An outbreak of viral gastroenteritis on a cruise ship. Communicable Disease Report Review 6 , R188–R192. [PubMed] [Google Scholar]
- 84. McGuckin, M. , Waterman, R. , Porten, L. , Bello, S. , Caruso, Juzaitis, B. , Krug, E. , Mazer, S. , Ostrawski, S. (1999) Patient education model for increasing handwashing compliance. American Journal of Infection Control 27 , 309–314. [DOI] [PubMed] [Google Scholar]
- 85. Melnick, J.L. (1995) History and epidemiology of Hepatitis A virus. Journal of Infectious Diseases 171 (Suppl. 1), S2–S8. [DOI] [PubMed] [Google Scholar]
- 86. Minor, T.E. , Allen, C.I. , Tsiatis, A.A. , Nelson, D.B. , Alessio, D.J. (1981) Human infective dose determinations for oral poliovirus type 1 vaccine in infants . Journal of Clinical Microbiology 13 , 388–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Minuk, G.Y. , Ding, L.X. , Hannon, C. , Sekla, L. (1994) The risks of transmission of acute hepatitis A and B virus infection in an urban centre. Journal of Hepatology 21 , 118–121. [DOI] [PubMed] [Google Scholar]
- 88. Mitchell, D.K. , Van R., Morrow, A.L. , Monroe, S.S. , Glass, R.I. , Pickering, L.K. (1993) Outbreaks of astrovirus gastroenterititis in day care centres. Journal of Paediatrics 123 , 725–732. [DOI] [PubMed] [Google Scholar]
- 89. Morens, D.M. & Rash, V.M. (1995) Lessons from a nursing home outbreak of influenza A. Infection Control and Hospital Epidemiology 16 , 275–280. [DOI] [PubMed] [Google Scholar]
- 90. Nerurkar, L.S. , West, F. , May, M. , Madden, D.L. , Sever, J.L. (1983) Survival of herpes simplex in water specimens collected from hot tubs in spa facilities and on plastic surfaces. Journal of the American Medical Association 22 , 3081–3083. [PubMed] [Google Scholar]
- 91. Nicholson, K.G. (1996) Impact of influenza and respiratory syncytial virus on mortality in England and Wales from January, 1975 to December, 1990 . Epidemiology and Infection 116 , 51–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Nicholson, K.G. , Kent, J. , Hammersley, V. , Cancio, E. (1997) Acute viral infections of upper respiratory tract in elderly people living in the community: comparative, prospective, populations based study of disease burden. British Medical Journal 315 , 1060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Niffenegger, J.P. (1997) Proper handwashing promotes wellness in child care. Journal of Paediatric Health Care 11 , 26–31. [DOI] [PubMed] [Google Scholar]
- 94. Nishimura, S. , Kagehira, M. , Kono, F. , Nishimura, M. , Taenaka, N. (1999) Handwashing before entering the intensive care unit: what we learned from continuous video‐camera surveillance. American Journal of Infection Control 27 , 367–369. [DOI] [PubMed] [Google Scholar]
- 95. Osterholm, M.T. , Reves, R.R. , Murph, J.R. , Pickering, L.K. (1992) Infectious diseases and child day care. Paediatric Infectious Diseases Journal 11 , S31–S41. [PubMed] [Google Scholar]
- 96. Pang, X.L. , Honma, S. , Nakata, S. , Verikari, T. (2000) Human caliciviruses in acute gastro‐enteritis of young children in the community. Journal of Infectious Diseases 181 , S288–S294. [DOI] [PubMed] [Google Scholar]
- 97. Parashar, U.D. , Bresee, J.S. , Gentsch, J.R. , Glass, R.I. (1998a) Rotavirus. Emerging Infectious Diseases 4 , 561–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Parashar, U.D. , Holman, R.C. , Clarke, M.J. , Bresee, J.S. , Glass, R.I. (1998b) Hospitalizations associated with rotavirus diarrhoea in the US, 1993 through 1995: surveillance based on the new ICD‐ 9‐CM rotavirus specific diagnostic code. Journal of Infectious Diseases 177 , 7–13. [DOI] [PubMed] [Google Scholar]
- 99. Patterson, W. , Haswell, P. , Fryers, P.T. , Green, J. (1997) Outbreak of small round structured virus gastroenteritis arose after kitchen assistant vomited. Communicable Disease Report Review 7 , R101–R103. [PubMed] [Google Scholar]
- 100. Pickering, L.K. , Bartlett, A.V. , Reeves, R.R. , Morrow, A. (1988) Asymptomatic excretion of rotavirus before and after rotavirus diarrhoea in children in day care centres. Journal of Paediatrics 112 , 361–365. [DOI] [PubMed] [Google Scholar]
- 101. Pittet, D. , Mourouga, P. , Pereger, T.V. (1999) Compliance with handwashing in a teaching hospital. Annals of Internal Medicine 130 , 126–130. [DOI] [PubMed] [Google Scholar]
- 102. Reed, S.E. (1975) An investigation on the possible transmission of rhinovirus colds through indirect contact. Journal of Hygiene (Cambridge) 75 , 249–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Rheinbaben, F.V. , Schünemann, S. , Broß, T. , Wolff, M.H. (2000) Transmission of viruses via contact in a household setting: experiments using bacteriophage φX174 as a model virus. Journal of Hospital Infection 46 , 61–66.DOI: 10.1053/jhin.2000.0794 [DOI] [PubMed] [Google Scholar]
- 104. Richardson, S. , Grimwood, K. , Gorrell, R. , Palombo, E. , Barnes, G. , Bishop, R. (1998) Extended excretion of rotavirus after severe diarrhoea in young children. Lancet 351 , 1844–1848.DOI: 10.1016/s0140-6736(97)11257-0 [DOI] [PubMed] [Google Scholar]
- 105. Roberts, L. , Jorm, L. , Patel, M. , Smith, W. , Douglas, R.M. , McGilchrist, C. (2000a) Effect of infection control measures on the frequency of upper respiratory infection in child care: a randomised, controlled trial. Paediatrics 105 , 738–742. [DOI] [PubMed] [Google Scholar]
- 106. Roberts, L. , Jorm, L. , Patel, M. , Smith, W. , Douglas, R.M. , McGilchrist, C. (2000b) Effect of infection control measures on the frequency of diarrhoeal episodes in child are: a randomised, controlled trial. Paediatrics 105 , 743–746. [DOI] [PubMed] [Google Scholar]
- 107. Rodriguez, W.J. , Kim, H.W. , Brandt, C.D. , Schwartz, R.H. , Gardner, M.K. , Jeffries, B. , Parrott, R.H. , Kaslow, R.A. , Smith, J.L. , Kapikain, A.Z. (1987) Longitudinal study of rotavirus infection and gastroenteritis in families served by a paediatric medical practice: clinical and epidemiological observations. Paediatric Infectious Diseases 6 , 170–176. [DOI] [PubMed] [Google Scholar]
- 108. Rodriguez, W.J. , Kim, H.W. , Brandt, C.D. , Yolken, R. , Richard, M. , Arrobio, J.O. , Schwartz, R.H. , Kapikian, A.Z. , Chanock, R.M. , Parrott, R.H. (1979) Common exposure outbreak of gastroenteritis due to type 2 rotavirus with high secondary attack rates within families. Journal of Infectious Diseases 140 , 353–357. [DOI] [PubMed] [Google Scholar]
- 109. Rotter, M.L. (1997) Handwashing and hand disinfection. In Prevention and Control of Nosocomial Infections ed. Wenzel, R.P. pp. 1052–1068. Philadelphia: Lippincott Williams & Wilkins.
- 110. Ryan, M.J. , Ramsey, M.E. , Brown, D. , Gay, N.J. , Farrington, C.P. , Wall, P.G. (1996) Hospital admissions attributable to rotavirus infection in England and Wales. Journal of Infectious Diseases 174 , S12–S18. [DOI] [PubMed] [Google Scholar]
- 111. Ryan, M.J. , Wall, P.G. , Adak, G.K. , Evans, H.S. , Cowden, J.M. (1997) Outbreaks of infectious intestinal disease in residential institutions in England and Wales 1992–4 . Journal of Infection 34 , 49–54. [DOI] [PubMed] [Google Scholar]
- 112. Samadi, A.R. , Huq, M.I. , Ahmed, Q.S. (1983) Detection of rotavirus in handwashings of attendants of children with diarrhoea. British Medical Journal 286 , 188–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Sattar, S.A. , Jacobsen, H. , Springthorpe, S. , Cusack, T. , Rubino, J. (1993) Chemical disinfection to interrupt the transfer of Rhinovirus type 14 from environmental surfaces to hands. Applied and Environmental Microbiology 59 , 1579–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Sattar, S.A. , Lloyd‐Evans, N. , Springthorpe, V.S. (1986) Institutional outbreaks of rotavirus diarrhoea: potential role of fomites and environmental surfaces as vehicles for virus transmission. Journal of Hygiene 96 , 277–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Sattar, S.A. & Springthorpe, S. (1999) Viricidal activity of biocides. Activity against human viruses. In Principles and Practice of Disinfection, Preservation and Sterilization, 3rd edn. eds Russell, A.D., Hugo, W.B. and Ayliffe, G.A.J. pp. 168–186. Oxford: Blackwell Science.
- 116. Schurmann, W. & Eggers, H.J. (1985) An experimental study on the epidemiology of enteroviruses — water and soap washing of poliovirus 1 contaminated hands, its effectiveness and kinetics. Medical Microbiology and Immunology 174 , 221–236. [DOI] [PubMed] [Google Scholar]
- 117. Scott, E. (1999) Hygiene issues in the home. American Journal of Infection Control 27 , S22–S25. [DOI] [PubMed] [Google Scholar]
- 118. Simoes, E.A.F. (1999) Respiratory syncytial virus infection. Lancet 354 , 847–852.DOI: 10.1016/s0140-6736(98)10263-5 [DOI] [PubMed] [Google Scholar]
- 119. Smith, C.B. , Purcell, R.H. , Bellanti, J.A. , Chanock, R.M. (1966) Protective effect of antibody to parainfluenza type 1 virus. New England Journal of Medicine 275 , 1145–1149. [DOI] [PubMed] [Google Scholar]
- 120. Soule, H. , Genoulaz, O. , Gratacap‐Cavallier, B. , Mallaret, M.R. , Morand, P. , Francois, P. , Bin, D.L.D. , Charvier, A. , Bost‐Bru, C. , Seigneurin, J.‐M. (1999) Monitoring rotavirus environmental contamination in a paediatric unit using polymerase chain reaction. Infection Control and Hospital Epidemiology 20 , 432–434. [DOI] [PubMed] [Google Scholar]
- 121. Sperber, S.J. (1994) The common cold. Medicine 11 , 235–242. [Google Scholar]
- 122. St. Sauver, J. , Khurana, M. , Kao, A. , Foxman, B. (1998) Hygienic practices and acute respiratory illness in family and group day care homes. Public Health Reports 113 , 544–551. [PMC free article] [PubMed] [Google Scholar]
- 123. Stevens, R.A. & Holah, J.T. (1993) The effect of wiping and spray‐wash temperature on bacterial retention on abraded domestic sink surfaces . Journal of Applied Bacteriology 75 , 91–94. [Google Scholar]
- 124. Sundkvist, T. , Hamilton, G.R. , Hourihan, B.M. , Hart, I.J. (2000) Outbreak of hepatitis A spread by contaminated drinking glasses in a public house. Communicable Disease and Public Health 3 , 60–62. [PubMed] [Google Scholar]
- 125. Thompson, S.C. (1994) Infectious diarrhoea in children: controlling transmission in the child care setting. Journal of Paediatrics and Child Health 30 , 210–219. [DOI] [PubMed] [Google Scholar]
- 126. Uhari, M. & Mottonen, M. (1999) An open randomized controlled trail of infection prevention in child day‐care centres. Journal of Paediatrics and Infectious Diseases 18 , 672–677. [DOI] [PubMed] [Google Scholar]
- 127. Valenti, W.M. (1998) Selected viruses of nosocomial importance. In Hospital Infections, 4th edn. eds Bennett, J.V. and Brachman, P.S. pp. 637–664. Philadelphia: Lippincott‐Raven.
- 128. Ward, R. , Bernstein, D. , Knowlton, D. , Sherwood, J. , Yung, E. , Cusack, T. , Rubino, J. , Schiff, G. (1991) Prevention of surface‐to‐human transmission of rotavirus by treatment with disinfectant spray. Journal of Clinical Microbiology 29 , 1991–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Ward, R.L. , Bernstein, D.I. , Young, E.C. , Sherwood, J.R. , Knowlton, D.R. , Schiff, G.M. (1986) Human rotavirus studies in volunteers: determination of infectious dose and serological response to infection. Journal of Infectious Disease 154 , 871–880. [DOI] [PubMed] [Google Scholar]
- 130. Wheeler, J.G. , Sethi, D. , Cowden, J.M. , Wall, P.G. , Rodrigues, L.C. , Tompkins, D.S. , Hudson, M.J. , Roderick, P.J. (1999) Study of infectious intestinal disease in England: rates in the community, presenting to general practice and reported to national surveillance. British Medical Journal 318 , 1046–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Wilde, J.R. , Pickering, L. , Eiden, J. , Yolken, R. (1992) Detection of rotaviruses in the day care environment by reverse transcriptase polymerase chain reaction. Journal of Infectious Disease 166 , 507–511. [DOI] [PubMed] [Google Scholar]


