Abstract
It has been a decade since smartphone application stores started allowing developers to post their own applications. This paper presents a narrative review on the state-of-the-art and the future of technology used by researchers in the field of mobile health promotion. Researchers build high cost, complex systems with the purpose of promoting health and collecting data. These systems promote health by using a feedback component that “educates” the subject. Other researchers instead use platforms which provide them with data collected by others, which allows for no communication with subjects, but may be cheaper than building a system to collect the data. This second type of systems cannot be used directly for health promotion. However, both types of systems are relevant to the field of health promotion, because they are precursors to a third type of systems that are emerging, the gig economy systems for mobile health data collection, which are low cost, globally available, and provide limited communication with subjects. If such systems evolve to include more channels for communication with the data-generating subjects, and also bring developers into the economy, they may eventually revolutionize the field of mobile health promotion and data collection by giving researchers new capabilities, such as the ability to replicate existing health promotion campaigns with the click of a button and the appropriate licenses. In this paper we present a review of state-of-the-art systems for mobile health promotion and data collection and a model for what these systems may look like in the future.
Keywords: Health promotion, Gig economy, Mobile health
1. Introduction
A successful health system may be described as one with healthy people, superior care, and fairness. A sustainable health system, on the other hand, can be described as one that is affordable to patients and government, acceptable to constituents, and adaptable to circumstances [1]. In order to achieve a successful and sustainable health system, one of the key aims should be to reduce financial, geographical, and cultural barriers to service access. Another key aim should be to develop information technology (IT) for both, patient and caregiver, which adapt across remote and rural areas [2]. Mobile phones can contribute to achieving a successful and sustainable health system, since they can eliminate some of the geographical, financial, and even cultural barriers that may be encountered when trying to access health resources.
In the year 2000 there were 109 M wireless subscribers in the US [3]. They were all using cell phones that could not perform the tasks of a mobile PC. In 2002, however, news broke out that the wireless handheld organizer Blackberry would now be able to place wireless phone calls [4]. This meant that a cell phone could now be used also to send emails and surf the web, capabilities which could be used for medical or health-related purposes if so desired. Later on, iPhone and Android were introduced in 2007 and 2008, respectively. The Apple iTunes Appstore and the Google Play Store were both introduced in 2008, allowing developers to launch their own software on the smartphones [5]. By 2012, the number of health-related apps was estimated to be 40,000 [6]. Currently there are 400 M subscribers in America, which corresponds to 1.2 subscribed cellphones per person, and the use of health and fitness apps has grown by 330% in the last three years [3].
Mobile technology ownership has increased substantially over the past decade, providing an extraordinary opportunity for innovation in the delivery of tailored health promotion interventions launched by health institutions, with the added advantage that it can be used by individuals in their natural environment [19]. It has been shown that certain minorities, such as African Americans have high eHealth literacy, are high users of mobile technology, and can therefore be receptive of mHealth interventions [20].
Recruiting participants for a health promotion study is typically done through dedicated campaigns to enroll eligible subjects and asking them to follow intervention protocols related to the study. Recruitment can be a slow and expensive process. In some cases, researchers advertise on social networks, send emails, or post flyers on different venues, while offering rewards such as coupons, gift cards, or nothing in exchange to whoever participates in a study. In mHealth studies, once a subject is recruited, he or she may be asked to download a mobile application, wear a tracker for a certain period of time, answer survey questions during certain phases of the study, take feedback from the application, take short online courses, and in some cases even play games as part of the study.
Many research studies have shown that mHealth tools are feasible, usable, acceptable, and satisfactory to the end-user. However, it is important to admit that in many cases there is still a need to study the effectiveness of the mHealth tool, not just its feasibility and approval by the subject [21,22,23,6]. This must be done carefully especially before implementing a specific mHealth application as part of a medical health care program. A study of melanoma detection apps from 2014 found that 3 out of 4 applications incorrectly detected 30% of melanomas as unconcerning [24]. When taken seriously by a user, the results can have disastrous consequences. Many studies, however, have shown encouraging results when it comes to the effectiveness of specific mHealth tools in improving education, the ability to communicate with an expert, and monitoring [25,26]. But mHealth is not for everyone. There are certain socioeconomic factors which can make or break the adoption of an mHealth tool by a given population. These factors include access to technology, age, and cost and implications for health insurance [27].
The use of mobile technology for health applications is greatly growing. In general, mobile health (mHealth) nowadays addresses an array of issues such as improving the convenience, speed, and accuracy of diagnostic tests [28]; monitoring chronic conditions, medication adherence, smoking cessation, physical activity promotion and recognition [29], appointment keeping and medical test result delivery; as well as improving patient-provider communication, health information communication and education, data collection and access to health records. mHealth services typically involve backend structures of servers and/or teams of medical staff which monitor and consult healthcare interested individuals [30,31]. Mobile technology also offers the possibility of moral support during an intervention. The technology has also been used for managing and monitoring mental health symptoms in persons with people with several mental disorder (SMD) [32].
In this paper, we review the typical systems for capturing health data and promoting health via mobile interfaces. Most importantly, we analyze current trends and predict that gig economy-based systems will revolutionize the field of health promotion and health data capture. We also present a detailed model for what we think these systems may look like in the future. Section II explains why data collection is relevant in the field of technology-based health promotion. Section III presents the scope of this review. Section IV explains the type of data analysis that is done with health-related data. Section V introduces technology-based health promotion from the perspective of the researcher. Section VI introduces systems that collect data which are based on a gig economy. Section VII presents a model for gig economies that can be used for both, data collection and health promotion. Sections VIII presents strengths and weaknesses of the model. Section IX presents a conclusion.
2. Relationship between health promotion and data collection
The focus of this paper is on reviewing existing technology used for health promotion research studies, and to describe trends that this technology may follow in the future. In order to understand this technology, however, we must first acknowledge that it is also used as a tool to collect data from the subjects. Collected data may be used as feedback for the health promotion task and is often also used in published scientific analysis. As such, collection of health-related data and the health promotion component are both present in most health promotion systems.
A survey was performed in Ref. [33], which evidenced the willingness of many participants to profit from selling anonymous personal data. The survey, which was done in 2014, included 400 participants from 59 countries from different continents (40% from Asia, 35% from Europe, 17% from North America, and 9% from the remaining continents). Most respondents attended college for at least 4 years, with 39% having Master’s education. Gender percentages were 61.5% female and the remaining percentage were males. The survey included respondents from 18 to 90+ years old. Table 1 shows survey results from Ref. [33] in a tabulated format, displaying the willingness of participants to sell their health data if identifying information such as name and age are removed.
Table 1 –
Tabulated results from Ref. [33].
| Data | Willing to sell (%) |
|---|---|
| Medications | 47 |
| Diseases and conditions | 45 |
| Exercise | 42 |
| Diet | 41 |
| Traits (i.e., eye color) | 37 |
| Electronic medical records | 35 |
| Genomic (DNA) | 32 |
| None | 18 |
| Other | 1 |
3. Scope of this narrative review
3.1. Inclusion criteria
As part of this review, several systems were studied which were published in the last decade, and systems which are expected to be launched in the next few years. The focus was on both, academic and industry systems. For academic work, the research was focused mostly on health-related studies which use technology to gather data from subjects. For inclusion, the technology in the study had to have at least one of the following components: sensor input, self-reporting via mobile or web application, education via mobile or web application, and/or gaming. A study on the feasibility of wearing a tracker was also included in the review.
For industry work, the review included health data marketplaces which are used by researchers or health institutions to acquire data for analysis. In the industry case, the systems which were studied only collect and distribute health-related data but are not directly used for health promotion. Such systems are also relevant to the review because they are a precursor to enterprise systems that can also be used to promote data, if only they had a feedback component. Therefore, the scope for this review encompasses health promotion systems which are published in academic work and also enterprise systems which are used by researchers for finding any type of health-related data. A pattern emerges which suggests that such enterprise systems may eventually include a feedback component.
3.2. Taxonomy of the scope
Systems that were studied were classified into one of two categories: systems created by researchers to promote health, and third-party solutions that sell data to the researcher. This duality stems from the type of analysis that researchers perform: primary data analysis vs. secondary data analysis, which are explained in detail in this paper. Third-party solutions were further classified into solutions which buy datasets from institutions and sell them to researchers, and solutions which obtain data directly from the subject in exchange for a reward and then sell the data to the researcher. We believe this second duality, on the other hand, stems from the ability of health institutions to own, handle, and profit from patient data efficiently vs. the desire of later generations to make a living in a way that is more independent, flexible, and varied than the typical so-called 9-to-5 job, which may have translated into a high acceptance of applications that allow users to earn something in exchange for short-term engagements, such as Uber [34], Airbnb [35], and TaskRabbit [36]. Whether such applications are a good model for the future economy or not is out of the scope of this paper. Nevertheless, we discuss how such a trend in the field of health promotion is also possible.
4. Health data analysis
In general, two types of data analysis are done in the research community: primary data analysis and secondary data analysis. Primary data analysis is when the same team that collected the data analyzes the data [37]. Secondary data analysis is when the data collected by one team is used by another team for a different analysis. mHealth studies that perform primary data analysis usually go beyond the tasks of collecting and analyzing data as done in most research fields. They actually provide a feedback component to educate, or enhance the health of the study participant. In the case of secondary data analysis of mHealth data, however, such task cannot be done. We have outlined the differences between primary data analysis and secondary analysis in Table 2.
Table 2 –
Primary data analysis vs. secondary data analysis.
| Data analysis types | |
|---|---|
| Primary | Secondary |
| Data collected for target study | Data collected for another study but reused in target study |
| Interaction with participant possible (e.g., intervention) | Interaction not possible while data is being collected |
| Full control over data collection process parameters | No control over data collection process parameters |
| Takes resources to implement data collection process | Data is simply received as files from another entity |
In primary data analysis, the researcher has full control over how and what data is collected. In secondary data analysis, on the other hand, the researcher has no control, but acquiring the data in this case is generally less expensive and much less time-consuming [38]. Depending on the type of analysis to be executed, different systems have been built to deliver data to the researcher. Both types of data analysis are relevant in the field of health promotion.
Besides the control and cost aspects of the data acquisition process, there is another aspect that makes a difference in these systems: the level of interaction that the researcher may have with the subject. It is precisely this aspect which enables a system for primary data collection to also serve as a health promotion tool. Systems built by researchers for collecting data for primary data analysis often let the researcher have a high level of interaction with the subject via different channels. Systems that offer data for secondary data analysis, on the other hand, are typically repositories which provide no interaction channels at all. If there is any interaction at all, it will be with the business that owns the data, and not with the subject that generated it.
To summarize, systems built for delivering mHealth data to the hands of the researcher usually fall at one end of the spectrum (i.e., full control over data collection process, increased interaction with the subject, high cost), or the other (i.e., absolutely no control over data collection process, no interaction with the subject, low cost). There is a type of system, however, which provides a limited level of interaction with the subject at a cost much lower than that of a system for primary data capture. This type of system follows a gig economy approach in which the data-generating subject gets a reward from the researcher.
Systems based on a gig economy entail short-term engagements between the subject and the researcher in which data is uploaded in exchange for a reward. In the future, gig economy systems may add more channels for interaction between subject and researcher, which would make them an out-of-the-box tool for low cost health promotion. The fact that these gig economy-like systems are available to all researchers and subjects, as opposed to the typical system for primary data collection, may also bring in a new interesting feature, which is the ability to instantly replicate a health promotion campaign from a different research team with the click of a button (after obtaining a file that serves as the model for the campaign, and the appropriate licenses to run the file on the platform).
5. Technology-based health promotion
Currently, most health promotion studies follow a primary data collection paradigm. In this paper we use the compound word primary data system to refer to a system used by a researcher to collect primary data. These systems are usually tailor-made for a specific study and enable the researcher to interact with the subject in different ways. A feature breakdown of previous health-related studies which use primary data systems is shown in Table 3. These studies may collect data or promote a behavior in a variety of health data domains, such as physical activity (PA) or diet. Some studies attempt to collect data to study the feasibility of using the tracker itself. Many of these studies gather data from the participant via sensors. In some cases, sensor input is complemented with self-reporting as well [39,41,46,54,49,51,47,56,40], although some studies focus on the self-reporting aspect only [48,52,53,58]. Some studies execute an intervention by providing an educational component to the participants as a course or as feedback [39,59,42,41,43,44,46,49,50,57,56,40,53,52]. There are also studies that include a gaming component [44,46,49]. The gaming component may be video game that engages the user in order to collect data and/or promote a behavior.
Table 3 –
Mobile health study.
| Study | Domain(s) | # Subjects | Sensor Input | Self reporting | Education or feedback | Gamification |
|---|---|---|---|---|---|---|
| [39] | PA | 200 | * | * | * | |
| [40] | PA | 87 | * | * | * | |
| [17] | PA, blood glucose | 12 | * | * | ||
| [41] | PA | 41 | * | * | * | |
| [42] | PA, dietary | 12 | * | * | ||
| [43] | PA | 165 | * | * | ||
| [44] | PA | 54 | * | * | * | |
| [45] | Gait analysis | 22 | * | |||
| [46] | PA, weight, blood pressure | 40 | * | * | * | * |
| [47] | PA, feasibility of tracker | 34 | * | * | ||
| [48] | PA, behavior | 40 | * | |||
| [49] | PA, fitness | 51 | * | * | * | * |
| [50] | PA, feasibility of tracker | 16 | * | * | ||
| [51] | PA | 28 | * | * | ||
| [52] | Blood glucose | 15 | * | * | ||
| [53] | PA, behavior, weight | 13 | * | * | ||
| [54] | Feasibility of tracker | 24 | * | * | ||
| [55] | PA | 25 | * | |||
| [56] | PA | 35 | * | * | * | |
| [57] | PA | 3 | * | * | ||
| [58] | Feasibility of tracker | 14 | * |
As an example of such systems, we describe the data collection system used in the Healthy Frio intervention study that promotes healthy lifestyles in rural Latino families in Frio County, Texas [61]. The study aims to address obesity by using mobile and social technologies to educate, motivate, and change behaviors that support weight loss and healthy weight control. It integrates several technologies. It uses Fitbit Flex2 activity trackers [62], Withings Scale [63], Verizon Android-based tablets, and the Moodle learning management system (LMS) [64].
The technical characteristics of the study are shown in Table 4. Healthy Frio follows the same modular trend followed by the studies in Table 3. In other words, interactions with the participant can be broken down into sensor data collection, messaging, education, gaming, and the act of recruiting the participant. In some instances, a dashboard is also created to enable researchers to look at the resulting data in a meaningful way. In the case of Healthy Frio, data was collected from three different systems: Fitbit, Withings weighting scale, and a learning management system called Moodle. After collection, the data is transferred to Amazon servers. A dashboard is used to access the data from the servers and present it on REDCap cloud [65] to the research team. Messaging software was also created to communicate with the participants.
Table 4 –
Technical characteristics of Healthy Frio study [61].
| Campaign components | Deployment technologies used | Description |
|---|---|---|
| Activity& Diet Tracking | Fitbit Flex2 | Flex2 tracks steps, activity, nutrition & sleep |
| Weight Tracking | Withings Scale | Withings Scale tracks body weight and composition |
| eLearning Environment | Articulate RISE & Moodle LMS | Health Education lessons are developed in Articulate RISE and Storyline for deployment via Moodle Learning Management System |
| Access Control | Access & Refresh Tokens using Authorization Code Grant Flow | Fitbit, Withings and Moodle data of all the subjects involved in the campaign is retrieved with initial consent from them and further data retrieval using refresh tokens with automatic renewal daily |
| Backend Data Retrieval and Monitoring | Amazon Elastic Cloud Instance | The complete protocol and logic for Fitbit, Withings and Moodle data variables storage and retrieval resides here |
| Health Records Mode of Delivery to Researchers | REDCap | User friendly data dashboard view, surveys and analyses of collected data from different components of the campaign for scientists and researchers |
Software was implemented to integrate participant’s heterogeneous health data, wellness and health education data. REDCap was used as a dashboard in the project. The data collected from Fitbit, Nokia Weighing Scale, and Moodle LMS are stored as CSV files in a database and pre-processed before displayed in REDCap. In this case, Amazon servers which store the wearable and smart scale sensor data and health education data, act as the marketplace database of the system.
There are also commercially available systems for collection of primary data, which can be used by researchers to reduce development time. An example of such systems is Fitabase [66]. This system allows researchers to create a project, send invitation to participants, view incoming data through a dashboard, create participant profiles, and export data. The system also has an API which allows the researcher to do certain tasks such as deliver text messages automatically based on data metrics, and to create applications which process or transfer the data to other systems. Researchers who use Fitabase still follow the primary data collection paradigm, since they still control the data collection process. Fitabase is only a tool to make things easier.
Current approaches have the following limitations:
Extremely high cost (typically funded by governments).
Resulting data is often not available to other researchers.
Hard to replicate by other researchers.
The reason current health promotion studies are hard to replicate is that the same cost would need to be incurred by the team attempting to replicate a study. Additionally, there is no standard way of sharing the technology, or the configuration built for a health promotion campaign. There are no platforms for modelling a health promotion campaign and sharing the model or its components with other researchers. For example, ideally a researcher would take the model for a successful smoking cessation campaign executed by a research team in one university and deploy it somewhere else with the click of a button. Being able to replicate a successful health promotion campaign in such a way would be a formidable capability, since it would allow a given health promotion goal to have a more global effect, with each deploying team paying for the cost of their own replica of the campaign. This process, and the technology that could make it possible is described in more detail later in this paper.
6. Data sharing in a gig economy
In this section we discuss platforms that are used to share mHealth data. These platforms are data-centric and are not used for health promotion, since they currently offer limited, or inexistent interaction with the subjects who generate the data, or control over the data collection process. They are only used by researchers to find mHealth data for secondary data analysis. Nevertheless, the discussion of these platforms is relevant, given that some of these systems are evolving in their capabilities and paving the way to the future of health promotion. We start by describing secondary data systems, which are the more primitive way of sharing mHealth data, given that they provide no control over data collection and no interaction with subjects. The discussion then shifts to gig economy data systems, which will be relevant to the future of health promotion, given that they already offer a limited degree of interaction with the subjects.
6.1. Secondary data systems
We use the compound word secondary data system to refer to a system used by researchers to acquire secondary data. Depending on the research goal, researchers may choose to bypass the time and expenses associated with developing a study from scratch by acquiring existing data instead. There are websites which provide health-related datasets free of charge [67,68,69,70]. Sometimes the only requirement for using this data is to cite the study that generated the data. There are platforms, however, which are not necessarily free of charge but provide other datasets via licensing. In some cases, they even allow for limited interaction with subjects from who the data may be extracted. In this section, we review such platforms.
The typical health data marketplace allows for the sale of patient data between businesses, which is useful for finding secondary data. The data typically comes from service providers (i.e., health institutions, laboratories) who are willing to sell de-identified patient data. The parties interested in acquiring the data are usually pharmaceutical manufacturers, service providers, researchers, hospitals, and retail pharmacies. A representative list of existing marketplaces for personal physiological data is shown in Table 5.
Table 5 –
Health data markets.
| Secondary data systems (institution gets paid in exchange for data) | |
|---|---|
| Healthverity | |
| Seller | Businesses who have data from patients and want to license it to others |
| Consumer | Pharmaceutical manufacturers, hospitals, payers, retail pharmacy, service providers, researchers |
| Data types | Medical claims, prescriptions, EMR, lab results, genomics, lab results, genomics, devices |
| Currency | USD |
| The health exchange market | |
| Seller | Businesses who have data from patients and want to license it to others |
| Consumer | Pharmaceutical manufacturers, hospitals, payers, retail pharmacy, service providers, researchers |
| Data types | Admin and billing, allergies, diagnosis, immunizations, lab and test results, medical histories, medications, patient demographics, progress notes, radiology images, vital signs |
| Currency | USD |
| Gig economy systems (subject gets rewarded for data) | |
| Healthwizz | |
| Seller | Mobile user who generates the data |
| Consumer | Physicians, personal trainer, researchers |
| Data types | Wearables, lab reports, doctor and hospital visits, data from other fitness and health apps |
| Currency | HealthCoins cryptocurrency |
| Coverus | |
| Seller | Mobile user who generates the data |
| Consumer | Health researchers, advertisers |
| Data types | Personal profile, physical, prescription, fitness data |
| Currency | CoverCoin cryptocurrency |
| Longenesis | |
| Seller | Patients and users who generate the data |
| Consumer | researchers and service providers |
| Data types | CT scans, MRIs, hair composition, high resolution pictures, transcriptome, genome, epigenome, clinical history, blood tests, urine tests, social networks feed, microbiome, electroencephalogram, electrocardiogram, video, voice |
| Currency | LifePound cryptocurrency |
As an example, Healthverity [71] system is a marketplace that contains de-identifiable healthcare data from 300 million individuals in the United States. The site sells data from more than 30 suppliers. The portal allows consumers to build their own datasets before performing the purchase. Healthverity offers four solutions, which together allow for the following: a marketplace in which users can find HIPAA compliant data, license data, and create cohorts, rapid and centralized access to permissions in order to ensure compliance, a data exploration tool, and a tool to consolidate patients across different datasets.
Another marketplace called the health exchange market (THEM) [28] for de-identified data asks consumers and data providers to fill out a questionnaire. Based on the questionnaire, consumers and data providers are matched. Performing a sale is free for data providers, but consumers must pay 11% of the data sale’s price in order to perform a transaction. The application guides the data seller and the consumer in the process of communicating, valuing, negotiating, and executing the exchange. Consumers and data providers have the ability to rate each other. It is mentioned in Ref. [72] that a blockchain will be used to determine the value of the data.
6.2. Gig economy data systems
We use the compound word gig economy data system to refer to a system that mediates short-term engagements between a subject and a researcher, with the purpose of delivering data in exchange for a reward. These platforms are not created by the researcher but may be configured by him/her. They essentially allow for a subject to upload and a researcher to download data, with a limited level of interaction between the two. These systems introduce the following aspects which are absent in the typical primary and secondary data systems:
More interaction between subject and researcher than in a typical secondary data system, but not as much as in a typical primary data system.
Subject has more control over the data than in typical primary or secondary data systems (e.g., can license data as many times as possible in exchange for a reward).
Data does not reside with a research team as in typical primary data system.
Data transactions are not centralized as in typical secondary data systems.
Consumer-to-business (C2B) health data marketplaces allow patients, health campaign participants or other users to share or sell their data to businesses. In some cases, these systems allow patients to profit from their data by selling it in the market in exchange for cryptocurrency. Users can then use the cryptocurrency to pay for services or items in the system’s marketplace. Data publishers may also benefit by channeling their data to their physicians or trainers, and by tracking their goals in the system.
Healthwizz [85] is an example of such system. It allows app users to sell data from wearables devices and media records. Users can sell their data to marketplace consumers, but they can also share it with physicians and trainers. The application can track the wellness of a family of users and deliver a health index. Users receive HealthTokens in exchange for their data. This system uses a blockchain for the transactions.
A detailed description of Healthwizz is given in their whitepaper [74]. The system is accessed through an online portal or a mobile web application. The application has an Ethereum client which connects it with the blockchain network. User data is stored in popular cloud storage services such as Dropbox, Google Drive, or Microsoft OneDrive. The user is able to upload biodata to his/her data storage by using the system’s web application. Data from health institutions can also be sold via the application. In this case, however, the Fast Healthcare Interoperability Resources (FHIR) standards framework is used to exchange data between involved parties (the health institution that collected the data, the marketplace, and the consumer). The blockchain does not store any user health data. It only stores references to the data.
In order to sell a piece of data, the user first uploads the data through the system’s application. The system transforms the data into an FHIR resource and stores it into the user’s personal storage. Additionally, the application uses an Ethereum client to store an ID (a hash) of the record and provenance data of the record into the blockchain, as a saleable entry for the user. A researcher can use the application to browse for records in the blockchain. The consumer then sends a request to the user who posted the data using the application. If the user approves the sale, the application makes an entry into the blockchain with the record ID, the consumer Ethereum address, and an access key, and sends the address of the contract to the consumer. The access key in the blockchain transaction can be used by the consumer as an authentication token in order to retrieve the data via an API that requires authentication. However, the access key is stored in the blockchain in an encrypted format using the consumer’s public key, so that only the consumer can perform the API call to retrieve the data. Once the consumer downloads the data, he can calculate the hash of the record and verify that this is the same hash as that of the record he browsed before making the purchase.
An alternative flow can be used in order to allow consumers to post requests for data. In this case, the application posts a “acquire contract” on behalf of the consumer, with specifications of the records that the consumer wants. The contract is funded with cryptocurrency. The application notifies users about the request for data. When a user is willing to fulfill the request, he indicates this through the application. The application then posts a transaction into a “share contract” with the record hash and an access key. The consumer is notified via the application and he can use the application to make FHIR API calls to retrieve a summary of the record. The access key does not allow for retrieving the actual record. It only allows for retrieval of the record’s summary. If the consumer is willing to acquire the record, he indicates that through the application. The application then transfers cryptocurrency from the “acquire contract” to the “share contract”, and it enables the access key to access the full record.
CoverUs is another emerging C2B company [75]. This application lets users connect their electronic health records and also input information manually. In exchange for the data, the application gives CoverCoins to the users, which the user may change for cash, lend, donate, or use to cover medical expenses (i.e., medical co-pays, transportation to an appointment). The system uses a blockchain for the transactions. The application benefits from a law in the 21st Century Cures Act which mandates that electronic health record systems should provide intuitive APIs so that patients can easily access their data, beginning in January 1st 2018. CoverCoins can be transferred to other users. The application is intuitive in the sense that it shows two buttons in a screen, one for earning coins, and one for redeeming coins. Coins can only be redeemed in a health-related expense, such as a trip to the doctor or a membership payment for the gym.
Longenesis is also a representative C2B company [76]. This application allows its users to upload de-identified data ranging from selfies to a blood sample file. The company claims that an AI will analyze the data and sell reports to pharmaceutical and drug development companies. The company will provide the exchange market for consumers and data providers to use along with the data validation. The research-related aspects of this platform are reported in Ref. [77]. Users can store and sell their biomedical data, and get health reports and tokens from the consumer in exchange for the data according to the system proposed in the paper. Data validators purchase and validate the data before it can be sold to anybody. They get a share of the revenue coming from data they have validated. Cloud storage is in AWS or Google Cloud Platform. The systems proposed in Refs. [76] and [77] both use a blockchain for the transactions. The system proposed in Ref. [77] allows users, data customers, and data validators to be rewarded. Data validators are the first to purchase the data to validate it before it is available to anyone else. The crypto-currency exchanged in reward is called LifePound. No personal data is stored in the blockchain, only hashes that are used to index data files. Data is stored in AWS or Google Cloud Platform in encrypted format. A threshold encryption scheme is used.
When uploading the data, the user first encrypts it with a symmetric cipher, and then splits the key using the secret sharing technique in Ref. [37]. The different parts of the key are sent to different key keepers. In order to decrypt the data, a minimum of K keys is needed. A transaction is posted in the blockchain, which contains the user’s public key, the data type, and a link to the data in the cloud storage. Validators are notified of the upload.
A data validator can create a transaction in the blockchain to acquire the data for a given amount of LifePounds. Once the purchase is made, key keepers deliver the keys to the consumer via an authenticated channel. The data validator downloads the data and decrypts it. Transactions are posted on the blockchain indicating validation results for each data hash corresponding to a piece of data. If the result of data validation is positive, its corresponding LifePounds are given to the data submitted. The validator will then get a share of LifePounds every time the data is purchased. On the other hand, if the validation result is negative, the validator gets his/her LifePounds back and the data is not available for sale. The process of acquiring the data once it has been validated is very similar.
7. Beyond data sharing: A model system for health promotion in a gig economy
In general, primary data systems have the drawback that they are costly to implement. Secondary data systems have the drawback that they impose limits in the types of data that can be acquired, and subject-researcher interaction is nonexistent. Gig economy data systems, on the other hand, attempt to bridge the gap, but they are still very limited in the types of interactions they allow. Ideally, the researcher would be able to have the flexibility of a primary data system at a low cost.
As previously shown in Table 3, mHealth primary data systems usually have at least four components of interaction between the researcher and the subject: data collection, messaging, education, and gamification. These are custom-made by researchers to interact with study participants. Secondary data systems such as Healthverity and the Health Exchange Market do not allow for this type of interaction. These exchange systems typically acquire the data from businesses. In these cases, the researcher is restricted to the type of data that is available for sale. Modern systems such as HealthWizz, on the other hand, allows researchers to post a request for data of a specific type. However, although HealthWizz connects the data consumer directly with the supplier it is also restricted to the type of data that is available, and the type of interactions that can be made with the subject. CoverUs, which has not been launched, claims to let users post many different types of data (e.g., selfies, electronic health records, fill out forms). However, it is not clear whether researchers can interact directly with users through any of the study components shown in Table 3. Longenesis does not allow for a high level of subject-researcher interaction either.
7.1. Possible trends
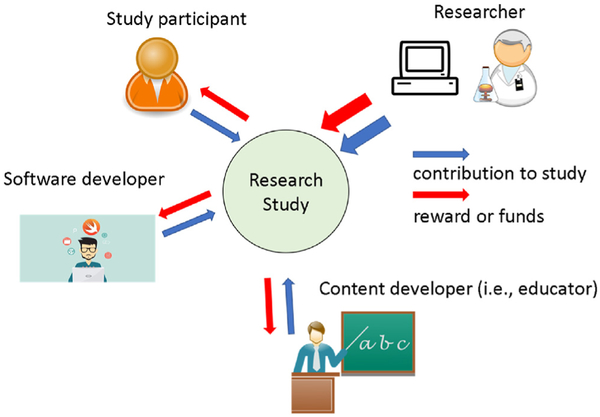
Upcoming systems might reduce the cost incurred by the health promotion research institution when developing a study, while also allowing researchers, developers, and participants to benefit by licensing any data, software, and content that results from a study. These interactions are depicted in Fig. 1. Currently, in a typical study the researcher must assemble and employ or somehow reward an entire team in order to recruit subjects and develop software to keep in touch with the subjects, collect data remotely, deliver online courses, and deliver educational games as needed. The approach is very time consuming, hard to replicate, and the infrastructure/data is often abandoned after the research is published. Upcoming systems, on the other hand, might bring together subjects, developers, and health promotion researchers through a single platform in which the researcher designs the entire study by creating a model. Subjects could get rewarded for participating in studies, developers could license software and course modules (i.e., messaging modules, game modules, course modules, data collection modules, and analysis modules), and researchers could implement their studies much faster by using such modules. Additionally, data owners (i.e., study participants and study researchers) could license data to other researchers through the platform.
Fig. 1 –
Future platforms may allow for other entities to collaborate in addition to study participant and researcher.
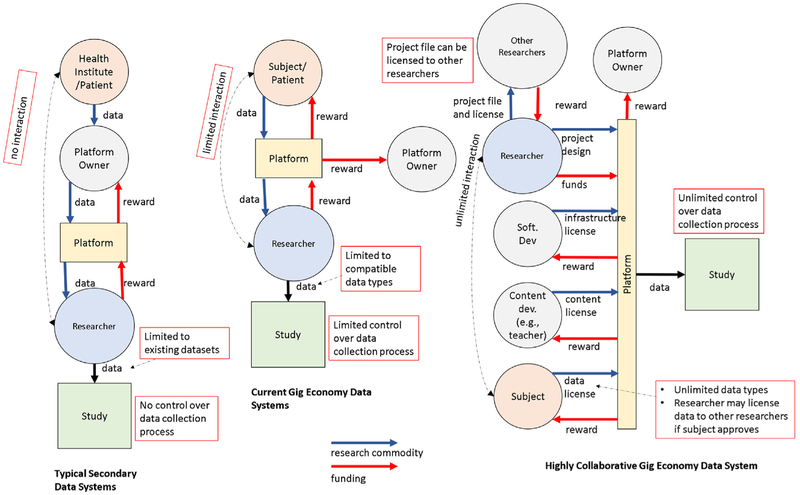
Gig economy data systems are bridging the gap between secondary data access and primary data collection by increasing interaction between the subject and the researcher via a platform, but this interaction is limited and most of the time does not allow for messaging, education, and gamification interactions. It only allows for sensorial input and in some cases self-reporting by the subject. Future systems, however, could make these interactions possible by bringing new collaborators besides the participant and the health promotion researcher. Entities such as software developers, content developers, and game developers could also license their creations as modules to researchers via these platforms. By bringing new entities into the picture, such platforms could eventually enable collaborations to go from exchanging data between a subject and a researcher to exchanging an entire intervention study defined in a single file which can be deployed to the masses via the platform. A comparison between typical secondary data systems, current gig economy data systems, and highly collaborative gig economy data systems is shown in Fig. 2. The figure shows how typical secondary data systems are limited in terms of interaction with the participants and the data that can be collected through them. Platforms that are more inclusive of other entities such as subject and developers, on the other hand, are able to provide much more interaction and richer data.
Fig. 2 –
Platforms for collecting mHealth data.
Collaborative platforms of the future might connect data consumers and data providers via a researcher, or developer application and a universal (i.e., same application used to join many studies) application for the participant. A potential participant could download the universal mobile application and use it to find and sign up for studies, track and license his/her data, and track rewards for participating in a study. To facilitate the recruiting process, such application could also perform the job of collecting profile data for the researcher, and delivering basic content (e.g., notifications) to the participant.
A health promotion researcher, on the other hand, could use the developer web application to design and deploy a study by dragging and dropping existing modules, and could also use it to track data, find potential participants, share modules, and license modules to other researchers. In essence, researchers could use a web application to create or replicate a health promotion study or intervention and launch in a matter of minutes, even when the study itself can last from days to several months. This can only be accomplished with platforms that make it easier for the researcher to acquire software infrastructure and content, and also enable him/her to assemble the intervention by choosing a configuration for such components. Such platforms could also be a marketplace for software and educational content developers. Software developers, for example, could use existing SDK and APIs for data collecting devices (e.g., Fitbit) to create data collection modules which can in turn be used by researchers as a ready-to-go module in a study creation. Licensing of such infrastructure would drastically save time and reduce cost incurred in studies such as Healthy Frio, which typically create this infrastructure from scratch, and in most cases abandon it later, as opposed to licensing it.
Collection of research data in the future could be done by recruiting data collection modules created by software developers and rented by study creators via a single platform. Health promotion researchers could use a study development platform to design a model of the study which they could deploy with the click of a button.
Newer systems might enhance collaboration by using licensing infrastructure. For example, a university might develop a messaging system that will communicate with participants via a bulk messaging platform. Researchers from another university can find and rent the messaging infrastructure as part of a study designed in a study development platform.
The ideal platform for developing a full-fledged data collection study for a study would allow for remote collaboration by letting each entity participate as follows:
Health promotion researchers can recruit participants, have access to data from previous studies, and can also design and deploy their own studies. They can also share study model files and data.
Participants can find studies they are interested in and get rewarded. They can also license their data to researchers.
Course creators can license their online courses.
Software developers can license data collection, messaging, and reporting subsystems or modules.
Game developers can license games.
Data collection modules created and licensed by software developers would essentially be pieces of software that use SDKs and APIs to retrieve data from third party systems and transfer it to the research platform database or to third party storage, with the ability to save the data in an encrypted format. Future platforms could also allow data owners (i.e., researchers and/or participants who generated the data) to license their previously generated data to other researchers in exchange for rewards. Reward transactions could be mediated by a blockchain and contracts funded with blockchain cryptocurrency. As participants progress through a study, for example, they could receive a reward while the study creator receives course assessment and progress data. Additionally, data could also be donated to other researchers.
Applications used to develop data collection studies in the future might be available on the web and also as mobile applications. The availability of particular modules such as educational modules, dashboards, messaging modules, or games, however, would depend on the developer’s implementation. Applications used by participants could be implemented in a way that they are accessible to people with special needs by following certain guidelines [78], such as the following:
Use of alt tags.
Use of transcripts on audio content.
Use of proper punctuation so that text can be converted to audio properly.
Use of smart color choices for the colorblind.
Use of simple language and small paragraphs for elderly audiences and people with disabilities.
Avoiding the use of extremely small clickable areas.
7.2. Technological aspects
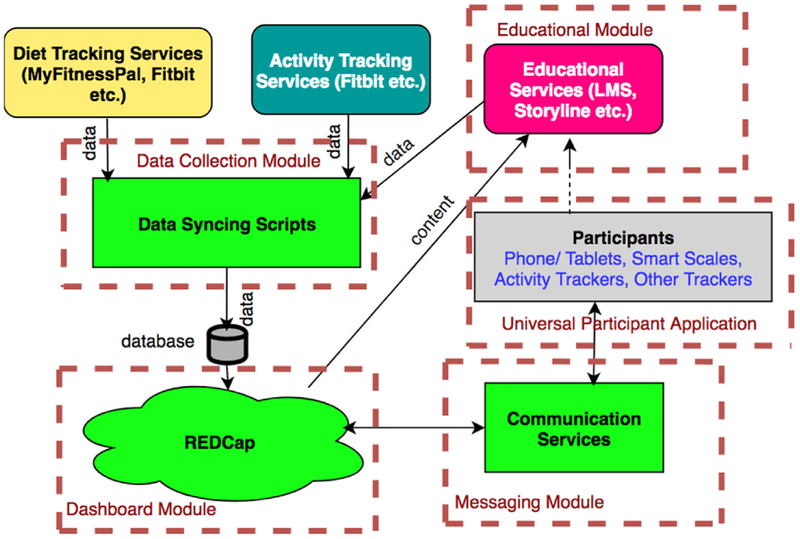
In this subsection we discuss how existing technologies and techniques could be leveraged in the future to create health promotion campaigns. We describe possible systems of the future in which a modular approach is used to increase collaboration between subject, researcher, and developers for executing a health promotion campaign. Fig. 3 shows a modular breakdown of the Healthy Frio project, which collected data for primary data analysis. The system can be divided into five different modules: data collection, education, a participant application, a messaging module, and a dashboard module. The data collection, education, and messaging modules could easily be reused by other researchers without major modifications. The data collection module could easily be adapted to take data from educational modules that have arbitrary content. The content of educational and messaging modules could easily be modified, given that there are applications available to change such content without having to modify the underlying software. The participant application, on the other hand, could be adapted to point the user to arbitrary educational content and messaging content. The dashboard, on the other hand, can be adapted to process different types of data and apply statistical analysis and visualization techniques in a generic way, or adapted to certain types of data.
Fig. 3 –
Modular breakdown of Healthy Frio.
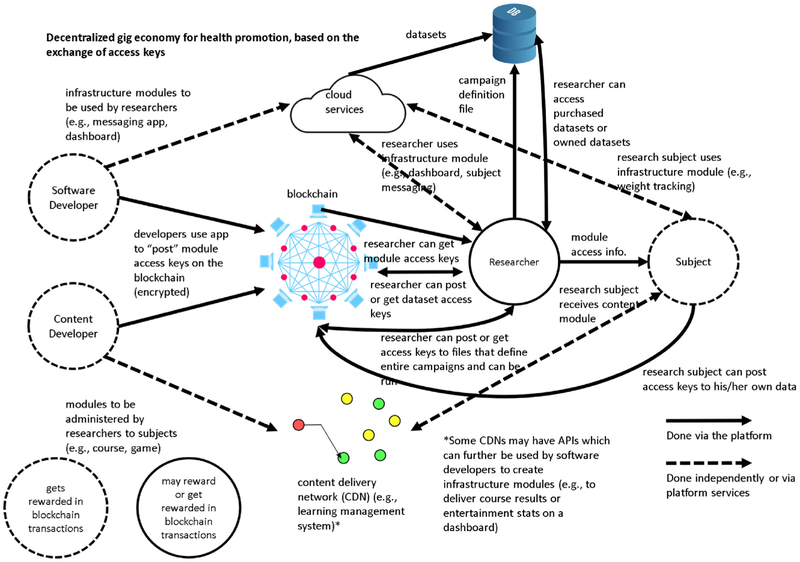
In the following subsections, we describe how advanced gig economy systems may use a modular approach to deliver the required functionality. A pictorial representation of a possible gig economy is shown in Fig. 4. This hypothetical, decentralized gig economy benefits all stakeholders (i.e., researchers, software developers, educational content developers, game developers, participants) and is powered by the purchase and selling of access keys. As seen in the figure, access keys are posted and purchased in the blockchain. The blockchain is not necessary, but it allows for a decentralized economy. The access keys are essentially licenses which provide access to items such as project infrastructure, content, datasets, among other assets. Once a stakeholder purchases an item listed on the blockchain, the seller posts an access key on the blockchain, encrypted with the buyer’s public key.
Fig. 4 –
A hypothetical platform for a decentralized gig economy for health promotion which is based on the exchange of access keys.
7.2.1. Matching participants to health promotion campaigns
In future gig economy systems, both participants and health promotion campaigns may have a profile. A participant could perform a search using a universal application that works as a hub for health promotion studies. The participant could search for a campaign that meets specific criteria (e.g., lasts for less than a month, gives reward, donates data) or follows under a given category (e.g., fitness). A search could also be performed by using keywords (e.g., quit smoking, lose weight). The user’s profile would also be used in campaign searches in order to show the user only studies that fit his/her profile. In search results, the participant could be able to look at the profile of a study and request to join the campaign. Participants should not be able join a study if specific criteria for the study is not met (e.g., minimum age). If there is any information missing from the potential participant’s profile which is part of the requirements for participating in a study (e.g., gender), the platform could ask the potential participant to specify this information and give him/her the choice to add this new information to his/her profile.
Health promotion researchers could use a developer web application to search for potential participants and send them an invitation to the study. To avoid spam, participants could have the choice to appear as potential participants only to studies that meet specific criteria (such as search criteria). Additionally, participants and health promotion researchers could have the ability to flag a study or participant as inappropriate.
7.2.2. Data collection
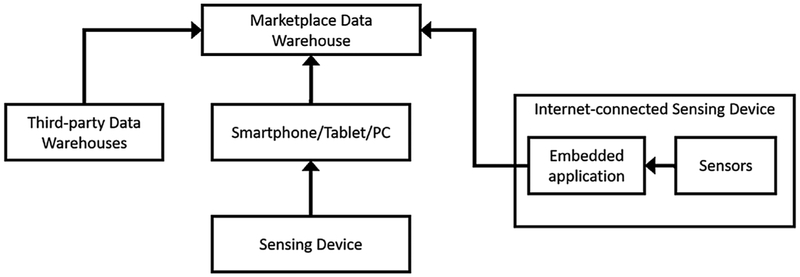
A health promotion researcher could assemble a promotion campaign using data collection modules. These modules could be created by software developers by using sensing devices SDKs and APIs. These modules would be rented for a study by the researchers. The study in Ref. [79] discusses the different approaches that developers use when collecting data from wearables into third-party servers. The data is extracted by a system on the cloud application and transferred to the marketplace database. In general, the data transferred by a data collecting application can come from several sources, as shown in Fig. 5, and it can also come in several formats (i.e., CSV files, JSON objects, XML files, HDF5 files). As shown in the figure, in cases in which the data is not directly available from a device, the data can often be collected from the device manufacturer’s servers and transferred to the target server. In other cases, the device connects to the smartphone or a PC, from which the data can be collected by using an SDK and transferred to the target server. In other cases in which the device connects directly to the internet, the data may be transferred directly to the target server if embedded applications can be written for the device. The purpose of a data collection module would be to take the data from a service and transfer it to the study development platform, where it can easily be downloaded by the participant, researchers, and dashboard modules. Data collection modules may also parse or process the data and save it in a different format. Data collection modules would make use of a study development platform API to store the data on the platform database. The API could allow modules to store data using server-side encryption if desired, which would be especially useful when storing identifiable data. Access to the marketplace database API would be secured by using state-of-the-art protocols such as OAuth [80].
Fig. 5 –
Data collection subsystem for heterogeneous data sources.
Manufacturers have already developed platforms that support collection of data from their own devices and those of partners. These platforms make the data available to the user as an app, and in some cases to third-party developers via SDKs and representational state transfer APIs (REST APIs). When the data is transferred directly from the collecting device to a third-party server, an SDK is used to access the data via an application in the collecting device. When the data is collected from a warehouse, an SDK or a REST API is typically used. SDKs to collect data from a warehouse must also be used in applications residing in the user’s device. REST APIs, on the other hand, may be used to access the warehouse data from a third-party application on the user’s device, or on the cloud [79].
Apple Health provides the Health Kit SDK, which enables access to warehouse data from apps residing on the user’s device [81]. Google Fit provides SDKs for Android and cloud applications, and also a REST API for cloud applications [82]. Samsung S-Health provides an app SDK, SDK-Warehouse, and a REST API [83]. Fitbit provides a REST API [84]. Transferring data from a warehouse may occur under different timing configurations and the data may be processed or aggregated in different ways by the collecting system. Data is typically stored as key-value pairs. Each system has its own data models with different sampling intervals, data types, and ways of representing the data. Current subsystems used as part of a research study may already collect data from the participant’s device via SDKs and also from servers using REST APIs.
The Healthy Frio study tracked diet and activity data via a Withings scale and a Fitbit. This type of data is typically synchronized using a Bluetooth wireless connection to the smartphone. Some devices have the option to connect to other third-party variable-specific (e.g. calorie counting or meal tracking app) tracking applications (e.g. MyFitnessPal [85]), that bring diet and nutrition aspects into the activity tracking picture. Fitbit, for example, offers the convenience of tracking user’s calorie intake; sleep duration, steps, miles, and activity minutes, etc. for the day. All this collected data can also be retrieved accurately using an API.
A data acquisition subsystem for a study may involve wearable sensors (such as Fitbit and Withings weighing scale [86]), a smartphone or tablet, study servers, and other cloud services. The workflow for the subsystem that delivers the data to the researchers is as follows:
Participant needs consent to the data collection application via a webpage in which he/she can also input information as desired.
Sensor data reaches third-party applications (i.e., Fitbit and Withings) after initial synchronization by the participant via Bluetooth.
The third-party applications transmit data to their respective servers via internet.
The da ta is retrieved by a middleware script from the third-party servers and saved to our system in comma-separated value (CSV) or excel format. These files consist of participant bio data, such as activity, sleep, steps, food logs, nutrients and body logs measured by the activity tracker and the smart scale.
These files are then stored in the database in encrypted format.
The backend of this data collection system resides on cloud server instances. APIs are used to implement data retrievals. The initial step in the data collecting application involves the participant authorizing the system to collect personal data. After this initial step, an automated process is used for data retrieval, collection and storage. Scalable hosting allows the system to increase the number of server instances depending on the number of participants in the study. The activity, nutrition and other lifestyle tracking sensor data from the participants is then collected automatically from their accounts based on the ID that is retrieved during the initial registration process.
7.2.3. Delivering educational content
Educational modules could be developed by online course creators and made available to health promotion researchers via licensing through platforms. Once purchased, these licenses which contain access information could be distributed by researchers to participants via the platform as part of the study. A similar type of licensing could also allow a researcher to access course progress data. Study subjects who finish a course successfully could also receive a reward through the platform.
With current technology, courses could first be designed in a third-party course authoring system. The course would then be uploaded to a third-party learning management system. The learning management system would be able to provide study researchers with a dashboard view of a participant’s progress. A data collection module could be used to extract progress data from the learning management system and upload it to the platform database. This workflow is described as follows.
-
1
A course creator designs the course and creates different modules using a course authoring system.
-
2The course is packaged into a zip file and converted to a standard format to make it compatible with a learning management system (LMS). While exporting the package, the authoring system offers ways we would like to track the course contents:
- Tracking based upon course completion.
- Tracking based upon quiz results.
The package is uploaded into a LMS.
-
3
The course creator adds an entry with the course details to the marketplace using the application.
-
4
A health promotion researcher purchases a given number of licenses for the course.
-
5
If a data collection module that is compatible with the LMS is available, the researcher may decide to use it in order to export the data into the marketplace.
-
6
The researcher gives the course licenses to the participants of the study. The license allows participants to create an account and take the course.
Study participants can access the course from the learning environment.
-
7
Course progress data is accessible to the researchers who purchased the licenses via the LMS and/or the marketplace application.
-
8
The participant receives tokens as he progresses through a course, or at the end of a course.
7.2.4. Educational entertainment content
Similar to educational modules, these types of modules could also be license-based and could be administered by health promotion researchers as part of a study. A researcher could purchase licenses for an educational game which contain access information and distribute them to study participants. These licenses could be used by participants to get access to the game. Games could collect data such as play times and player statistics and upload these data to the platform via an API or SDK, or made accessible to the researcher via an external platform.
7.2.5. Messaging with participants
In order to provide the messaging feature that many studies require, developers could create messaging components for health promotion researchers to use out-of-the-box as part of a study. This type of component could be used as a module that forms part of a study model created by a researcher on a study development platform. For example, an SMS or any other messenger chatbot module may be used by researchers to monitor participants that are trying to quit smoking, and to send them motivational messages [87]. Even though this type of component is already used in studies, the research team usually has to hire developers to create it. Additionally, the infrastructure is typically not reused, or licensed to other researchers. A much simpler example would be an email module which can be used by researchers to send an announcement to all participants in a study. In this case, a very simple software component with a user interface could be posted as a module on the platform and licensed for researchers to use in their studies.
7.2.6. Analytics
Throughout a study, health promotion researchers need to be able to observe the data in a way that is convenient. This includes looking at graphs, tables, and other aggregation methods for reporting, as opposed to looking at CSV files. By using APIs and SDKs, developers can create applications that access the data from a study and present it in a dashboard, graph, or aggregated form. Dashboard modules could also be licensed to researchers and function as clients that can be executed on the cloud, or as a web, desktop, or mobile application. Dashboard modules could perform online analysis and could also be interfaced with other modules for feedback purposes. This would enable researchers to trigger actions in other modules. For example, a dashboard module could be used to set a trigger so that a text message is sent from a messaging module to study participants who have finished taking a course. In this case, a data collection module could be used to extract course data and make it available in the platform. The ability to implement pre-processing schemes as part of a dashboard module (i.e., calculations such as moving average, or classifiers) would allow for complex analytics without the need to resort to outside tools.
7.2.7. Accessing data
In current data collection platforms, both participant and researcher can access the participant’s data. The data comes from data collection modules which gather data from internet-connected sensors and sensors (e.g., motion sensors) attached to personal computing devices such as tablets, smartphones, and computers [88,89]. However, in future platforms the data may also be extracted from educational, gaming, and messaging components. The data may also be stored in an encrypted format. For accessing the data, future systems may implement viewers for certain types of files such as HDF5 files, for example. An HDF5 file is a container that can include several dataset files, each with its own metadata. File directories can also be stored as groups in an HDF5 file. Storing data in HDF5 format also offers performance and storage efficiency benefits. This file format is portable to many platforms, and there are libraries and tools for manipulating HDF5 files. There are also tools for analyzing HDF5 data, which would facilitate development of dashboard modules.
Using file viewers, participant and researcher could both be able to look at the participant’s de-identified data records stored in the platform database and share the data (i.e., certified as belonging to a particular study) with other researchers in exchange for a reward (i.e., cryptocurrency) or as a donation. Researchers and institutions could acquire the data through the study development platform.
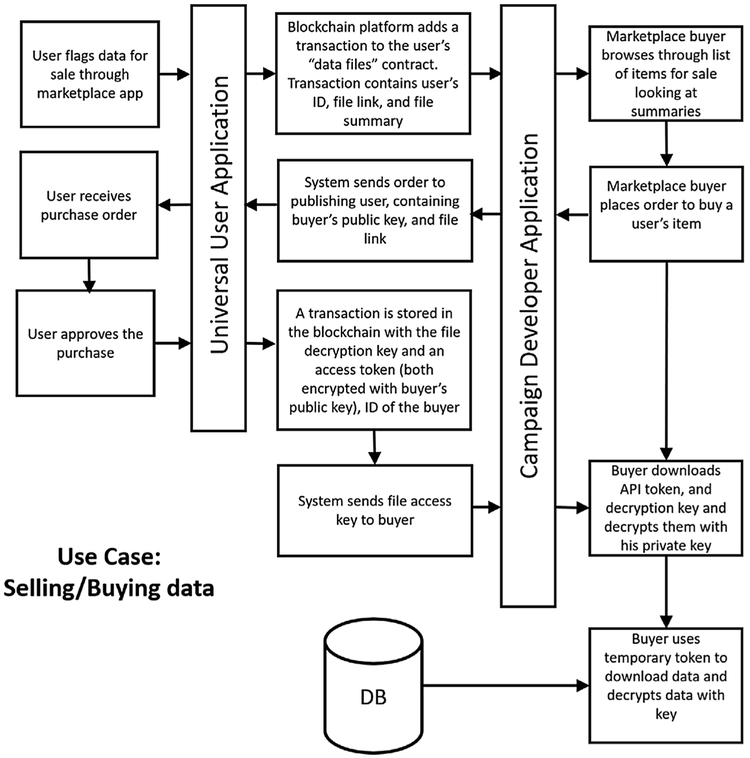
7.2.8. Sharing data
In newer platforms, blockchains are used to mediate market transactions, but do not store any identifiable data from the participant. An example flow for a health promotion researcher acquiring data from a user is shown in Fig. 6. In such flow, the following actions are performed:
Fig. 6 –
Example implementation that allows researcher to collect data from subject.
Data owner (i.e., participant and/or study researcher) flags data as available for other researchers through the developer application.
The application posts a transaction in the blockchain, which contains a user identifier, a link to the file, and a summary of the file.
A researcher uses the developer application to browse for data that is available for licensing.
The researcher places an order to acquire an item.
The developer application sends a notification to the data owner, containing the consumer’s public key and a link to the file summary.
The data owner approves the purchase.
A transaction is stored in the blockchain. The transaction has a file decryption key, and a temporary access token, which have both been encrypted with the researcher’s public key, and an identifier for the researcher.
The blockchain platform transfers the cryptocurrency funds from the researcher to the data owner.
The researcher downloads API temporary access token and decryption key and uses his private key to decrypt them.
The researcher uses temporary token to download data and decrypts data with decryption key.
The participant can also give access to his data to a trusted party, such as his/her doctor. In this case, the flow is as follows:
Data owner assigns access to a specific record to another user via the participant application or the developer application.
A transaction is stored in the blockchain. The transaction has a file decryption key, and a temporary access token, which have both been encrypted with the receiving party’s public key, and an identifier for the receiving user.
The receiving party gets a notification.
The receiving party downloads API temporary access token and decryption key and uses his private key to decrypt them.
The receiving party uses temporary token to download data and decrypts data with decryption key.
7.2.9. Compliance
Future platforms used for collaboration may use a regional compliance feature in order to help health promotion researchers make sure that their study complies with regulations at any region in which the study collects data, and also in regions in which the data or subsystems reside. Such regional compliance feature may be analogous to the digital rights management technique used in DVDs. This would enable researchers to abide to certain country regulations, such as the European Union’s General Data Protection Regulation. When using the regional compliance feature, the developer could select a country or region for the study and this would restrict and/or configures the modules which may be used as part of the study, and the users that may participate. Using this regional compliance feature would not guarantee that the deployed study complies with all regulations and as such, it would still remain the responsibility of the researcher to make sure that the study complies with all regulations in any country in which a participant, developer, or system gets involved as part of the study. The proposed compliance feature could also be implemented in a way similar to how permissions for mobile applications are handled by the Android OS. The developer requests for the user to enable permissions so that the application can have access to some of the native features of the OS. This ensures that the user of the application agrees to let the application use certain features of the device. In this case, certain reviewed modules or module features would not be available unless the team that runs the module(s) is notified and approves.
8. Critique of the trend model (SWOT analysis)
In previous sections we analyzed trends of state-of-the-art systems for mobile health promotion and data collection and used a model system to predict how these systems will look in the future. In this section we provide a SWOT (Strengths, Weaknesses, Opportunities, and Threats) analysis of such model system.
8.1. Strengths
The strengths of the model system have been discussed in detail in previous sections. The main strength of the predicted type of system is in the benefits it provides to each entity of the gig economy with a reduced overhead. Developers, subjects, and researchers all can easily participate in a study and obtain rewards. The researcher can create a study or campaign much faster by reusing modules and even license his/her own modules or entire campaigns to other institutions for a reward.
8.2. Weaknesses
The discussed model for future systems stems from looking at the mobile health promotion problem from a holistic perspective. As such, it may resemble a one-shoe-fits-all type of solution, which typically does not apply in domains that are so diverse in terms of data types. Typical systems that are built for mobile health data collection and promotion are usually tailor made to solve a specific problem. Even if a campaign such as Healthy Frio is written using a modular approach, the modules in the system are usually built to solve a specific problem. To make a module reusable for other problems, it needs to become flexible by allowing for different configurations in terms of parameterizing its behavior and allowing it to interface with different modules. However, flexibility comes at the expense of complexity for both, the developer and the user. As for the modules used in a campaign, not everything can be easily recycled or adapted for reuse by incurring a reasonable cost.
8.3. Opportunities
The model in discussion attempts to use an inclusive approach by bringing entities which are out of the scope of current systems (content developers and software developers). Including these entities has proven to be advantageous in some sectors such as mobile application development and media sharing sites. It may also be advantageous to the scientific community, especially since such developers already participate, but are usually restricted to working in projects localized to a few institutions, and certain content such as datasets and papers is already shared in social networks. In general, the many studies that have been cited as primary data analysis studies for mobile health promotion show that much infrastructure has been developed already and more is constantly being developed for mobile health research. However, the infrastructure is not being shared because no platforms allow for it to be formally shared via licensing.
8.4. Threats
A drawback of the model is that compliance and security cannot be guaranteed by the system. Using a blockchain can protect the assets of each stake holder. However, the system on its own cannot guarantee that each asset is secure to whoever uses it, and that it complies with local law. This is the case because modules run on different platforms and the use of those platforms cannot be controlled by the system (as done in the case of Android, in which certain features are controlled by the system and applications can use them only if they have permissions). Additionally, even if control of those platforms was available, the developer in general cannot be trusted. For example, the system cannot guarantee that a module will not email private data to a third-party. As mentioned in the compliance subsection, only reviewed modules can be trusted to be safe (as in the case of iOS applications, in which applications are reviewed before becoming available). A possible solution to this problem is to allow reusable modules only from trusted entities (i.e., from accounts belonging to specific institutions), or by using some type of verification or review system.
9. Conclusion
In the last decade, the ubiquity of smartphones has presented an opportunity to deliver health solutions to the public. This paper analyzed trends in systems used for mobile health promotion and predicted a trend for future systems. The discussion of state-of-the-art included systems currently used by researchers for primary and secondary mobile health data analysis. These systems are relevant to the field of health promotion. Systems for primary data analysis are tailor-made by researchers to solve a specific research question, and allow for communication with the subjects, but they have a high cost and are usually not globally available. Systems made to exchange data for secondary data analysis, on the other hand, are usually industry solutions which are globally available, and have a low cost for the user. However, they do not allow for communication with data-generating subjects. As such, systems used to collect data for secondary data analysis cannot be used directly for health promotion. However, a new type of system has the potential to revolutionize the field. This new type of system follows a gig economy paradigm. Systems of the gig economy kind are typically globally available, low cost, and allow for limited interaction between subject and researcher. However, current implementations still do not allow for certain types of interaction such as messaging, self-reporting, and gaming. This drastically limits their ability to be used as health promotion tools. Future gig economy systems, however, may allow for these interactions to happen with a reduced effort from the researcher. Coupled with other features, such as licensable infrastructure, data, and campaign design files, these systems may eventually be used as efficient health promotion tools. For this to happen, however, new entities such as software, content, and game developers may need to be included into the gig economy framework.
Acknowledgement
Research reported in this publication was supported by the National Institute Of Nursing Research of the National Institutes of Health under Award Number R01NR016269. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- [1].Fineberg H. A successful and sustainable health system—how to get there from here. N Engl J Med 2012;366(11):1020–7. [DOI] [PubMed] [Google Scholar]
- [2].Lehoux P, Roncarolo F, Silva HP, Boivin A, Denis JL, Hébert R. What health system challenges should responsible innovation in health address? Insights from an international scoping review. Int J Health Policy Manage 2018;8(2):63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].CTIA, The Wireless Industry. Industry Data, 2019. [Online]. Available: https://www.ctia.org/the-wireless-industry/infographics-library. [Accessed 21 6 2019].
- [4].Hesseldahl A. Blackberry gets chatty. Forbes 2002;4(March) [Online]. Available: https://www.forbes.com/2002/03/04/0304tentech.html#adfb5f669f97. [Accessed 21 6 2019]. [Google Scholar]
- [5].Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T 2014;39(5):356–64. [PMC free article] [PubMed] [Google Scholar]
- [6].Boulos MN, Brewer AC, Karimkhani C, Buller DB, Dellavalle RP. Mobile medical and health apps: state of the art, concerns, regulatory control and certification. Online J Public Health Inform 2014;5(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Arsand E, Tatara N, Østengen G, Hartvigsen G. Mobile phone-based self-management tools for type 2 diabetes: the few touch application. J Diabetes Sci Technol 2010;4 (March (2)):328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Glynn LG, Hayes PS, Casey M, Glynn F, Alvarez-Iglesias A, Newell J, et al. Effectiveness of a smartphone application to promote physical activity in primary care: the SMART MOVE randomised controlled trial. Br J Gen 2014;64(624). e384–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Brewer LC, Jenkins S, Lackore K, Johnson J, Jones C, Cooper LA, et al. mHealth intervention promoting cardiovascular health among African-Americans: recruitment and baseline characteristics of a pilot study. JMIR Res Protoc 2018;7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Overdijkink SB, Velu AV, Rosman AN, van Beukering MD, Kok M, Steegers-Theunissen RP. The Usability and effectiveness of mobile health technology-based lifestyle and medical intervention apps supporting health care during pregnancy: systematic review. JMIR mHealth and uHealth 2018;6(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Armoiry X, Sturt J, Phelps EE, Walker CL, Court R, Taggart F, et al. Digital clinical communication for families and caregivers of children or young people with short- or long-term conditions: rapid review. J Med Internet Res 2018;20(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zan S, Agboola S, Moore SA, Parks KA, Kvedar JC, Jethwani K. Patient engagement with a mobile web-based telemonitoring system for heart failure self-management: a pilot study. JMIR mHealth and uHealth 2015;3(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wolf JA, Moreau JF, Akilov O, Patton T, English JC, Ho J, et al. Diagnostic inaccuracy of smartphone applications for melanoma detection. JAMA Dermatol 2013;149(4):422–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hurt K, Walker RJ, Campbell JA, Egede LE. mHealth interventions in low and middle-income countries: a systematic review. Global J Health Sci 2015;8(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ossebaard H, Gemert-Pijnen J. EHealth and quality in health care: implementation time. Int J Qual Health Care 2016;28(3):415–9. [DOI] [PubMed] [Google Scholar]
- [27].Tamura T, Maeno S, Hattori T, Kimura Y, Yoshida M, Minato K. Assessment of participant compliance with a web-based home healthcare system for promoting specific health checkups. Biocybernet Biomed Eng 2014;34(1):63–9. [Google Scholar]
- [28].Glowacz A, Glowacz Z. Recognition of images of finger skin with application of histogram, image filtration and K-NN classifier. Biocybernet Biomed Eng 2016;36(1):95–101. [Google Scholar]
- [29].Morales J, Akopian D. Physical activity recognition by smartphones, a survey. Biocybernet Biomed Eng 2017;37(no.3):388–400. [Google Scholar]
- [30].Istepanian RSH, Laxminarayn S, Pattichis CS. M-Health: emerging mobile health systems Topics in biomedical engineering. Int. Book Series; London, UK: Springer-Verlag; 2006. [Google Scholar]
- [31].Research2guidance. mHealth App Developer Economics 2014. Report. http://www.research2guidance.com/r2g/research2guidance-mHealth-App-Developer-Economics-2014.pdf. [Google Scholar]
- [32].Naslund JA, Aschbrenner KA. Digital technology for health promotion: opportunities to address excess mortality in persons living with severe mental disorders. Evid Based Mental Health 2019;22(1):17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Pickard KT. Exploring markets of data for personal health information. IEEE International Conference on Data Mining Workshop (ICDMW) 2014. [Google Scholar]
- [34].Uber Technologies Inc., “Uber,” 2019. [Online]. Available: https://www.uber.com/. [Accessed 20 6 2019]. [Google Scholar]
- [35].Airbnb, “Airbnb,” 2019. [Online]. Available: https://www.airbnb.com/. [Accessed 20 6 2019]. [Google Scholar]
- [36].TaskRabbit, “The convenient & affordable way to get things done around the home.,” 2019. [Online]. Available: https://www.taskrabbit.com. [Accessed 20 6 2019]. [Google Scholar]
- [37].Koziol N. Arthur A., An Introduction to Secondary Data Analysis, CYFS Statistics and Measurement. [Google Scholar]
- [38].Romano, Using secondary data, Department of Medicine and Pediatrics. University of California. [Google Scholar]
- [39].Kirwan M, Duncan M, Vandelanotte C, Mummery W. Using smartphone technology to monitor physical activity in the 10,000 steps program: a matched case-control trial. JMIR 2012;14(2). p. e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Slootmaker S, Chinapaw M, Seidell J, van Mechelen W, Schuit A. Accelerometers and Internet for physical activity promotion in youth? Feasibility and effectiveness of a minimal intervention. Prev Med 2010;51(1):31–6. [DOI] [PubMed] [Google Scholar]
- [41].Fukuoka Y, Vittinghoff E, Jong S, Haskell W. Innovation to motivation: pilot study of a mobile phone intervention to increase physical activity among sedentary women. Prev Med 2010;51(3–4):287–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Seto E, Hua J, Wu L, Shia V, Eom S, Wang M, et al. Models of individual dietary behavior based on smartphone data: the influence of routine, physical activity, emotion, and food environment. PLoS ONE 2016;11(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Harries T, Eslambolchilar P, Rettie R, Stride C, Walton S, van Woerden H. Effectiveness of a smartphone app in increasing physical activity amongst male adults: a randomised controlled trial. BMC Public Health 2016;16 p. 925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Garde A, Umedaly A, Abulnaga S, Robertson L, Junker A, Chanoine J. Assessment of a mobile game (‘MobileKids Monster Manor’) to promote physical activity among children. Games Health 2015;4(2):149–58. [DOI] [PubMed] [Google Scholar]
- [45].Furrer M, Bichsel L, Niederer M, Baur H, Schmid S. Validation of a smartphone-based measurement tool for the quantification of level walking. Gait Posture 2015;42:289–94. [DOI] [PubMed] [Google Scholar]
- [46].Cowdery J, Majeske P, Frank R, Brown D. Exergame apps and physical activity: the results of the ZOMBIE trial. Am J Health Educ 2015;46:216–22. [Google Scholar]
- [47].Schaefer S, Van Loan M, German J. A feasibility study of wearable activity monitors for pre-adolescent school-age children. Prev Chronic Dis 2014;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Klein M, Mogles N, van Wissen A. Intelligent mobile support for therapy adherence and behavior change. J Biomed Inform 2014;51:137–51. [DOI] [PubMed] [Google Scholar]
- [49].Direito A, Jiang Y, Whittaker R, Maddison R. Apps for IMproving FITness and increasing physical activity among young people: the AIMFIT pragmatic randomized controlled trial. JMIR 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Hooke M, Gilchrist L, Tanner L, Hart N, Withycombe J. Use of a fitness tracker to promote physical activity in children with acute lymphoblastic leukemia. Pediatr Blood Cancer 2016;63(4):684–9. [DOI] [PubMed] [Google Scholar]
- [51].Vosa S, Janssena M, Goudsmita J, Lauwerijssenc C, Brombacherb A. From problem to solution: developing a personalized smartphone application for recreational runners following a three-step design approach. Procedia Eng 2016;147:799–805. [Google Scholar]
- [52].Nes A, van Dulmen S, Eide E. The development and feasibility of a web-based intervention with diaries and situational feedback via smartphone to support self-management in patients with diabetes type 2. Diabetes Res Clin Pract 2012;97(3):385–93. [DOI] [PubMed] [Google Scholar]
- [53].Morrison L, Hargood C, Lin S, Dennison L, Joseph J, Hughes S, et al. Understanding usage of a hybrid website and smartphone app for weight management: a mixed-methods study. J Med Internet Res 2014;16(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Schaefer S, Ching C, Breen H, German J. Wearing, thinking, and moving: testing the feasibility of fitness tracking with urban youth. Am J Health Educ 2016;47(1):8–16. [Google Scholar]
- [55].Nolan M, Mitchell J, Doyle-Baker P. Validity of the Apple iPhone® /iPod Touch® as an accelerometer-based physical activity monitor: a proof-of-concept study. J Phys Act Health 2014;11:759–69. [DOI] [PubMed] [Google Scholar]
- [56].Choi J, Lee J, Vittinghoff E, Fukuoka Y. mHealth physical activity intervention: a randomized pilot study in physically inactive pregnant women. Matern Child Health 2016;20:1091–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Hayes L, Van Camp C. Increasing physical activity of children during school recess. J Appl Behav Anal 2015;48(3):690–5. [DOI] [PubMed] [Google Scholar]
- [58].Nguyen N, Hadgraft N, Moore M, Rosenberg D, Lynch C, Reeves M, et al. A qualitative evaluation of breast cancer survivors’ acceptance of and preferences for consumer wearable technology activity trackers. Support Care Cancer 2017;25(11):3375–84. [DOI] [PubMed] [Google Scholar]
- [59].Årsand E, Tatara N, Hartvigsen G. Mobile phone-based self-management tools for type 2 diabetes: the Few Touch Application. J Diabetes Sci Technol 2010;4(2):328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].The University of Texas at Austin, “Healthy Frio,” 2018.. [Online]. Available: https://liberalarts.utexas.edu/lri/ResearchPrograms/index.php. [Accessed 4 7 2018]. [Google Scholar]
- [62].Fitbit, Inc, “Fitbit Flex 2,” 2018. [Online]. Available: https://www.fitbit.com/my/flex2. [Accessed 19 12 2018]. [Google Scholar]
- [63].Withings, “Scales,” 2018. [Online]. Available: https://www.withings.com/us/en/scales. [Accessed 19 12 2018]. [Google Scholar]
- [64].Moodle Community, “moodle,” [Online]. Available: https://moodle.org/. [Accessed 19 12 2018]. [Google Scholar]
- [65].nPhase, Inc, “REDCAP CLOUD,” 2018. [Online]. Available: https://www.redcapcloud.com/. [Accessed 19 12 2018]. [Google Scholar]
- [66].Small Steps Labs LLC, “fitabase,” 2018. [Online]. Available: https://www.fitabase.com/. [Accessed 19 12 2018]. [Google Scholar]
- [67].US Federal Government, “HealthData.gov,” U.S. Department of Health & Human Services, 30 November 2018. [Online]. Available: https://healthdata.gov. [Accessed 30 11 2018]. [Google Scholar]
- [68].US Government, “DATA.GOV,” US Government, [Online]. Available: https://www.data.gov/. [Accessed 30 11 2018]. [Google Scholar]
- [69].Kaggle Inc, “kaggle,” Kaggle Inc, 2018. [Online]. Available: https://www.kaggle.com/. [Accessed 30 11 2018]. [Google Scholar]
- [70].University of California, Irvine and Rexa.info, “UCI Machine Learning Repository,” University of California, Irvine and Rexa.info, [Online]. Available: https://archive.ics.uci.edu/ml/datasets.html. [Accessed 30 11 2018]. [Google Scholar]
- [71].HealthVerity, Inc., “Healthverity Marketplace,” Healthverity, 2018. [Online]. Available: http://healthverity.com/. [Accessed 21 May 2018]. [Google Scholar]
- [72].The Health Exchange Market, “The Health Exchange Market,” Website Design by Bigfoot Media, 2018. [Online]. Available: https://thehealthexchangemarket.com/. [Accessed 21 May 2018]. [Google Scholar]
- [73].Wizz Health, “Health Wizz,” Health Wizz, 2018. [Online]. Available: https://www.healthwizz.net/. [Accessed 21 May 2018]. [Google Scholar]
- [74].Health Wizz Inc., “MY HEALTHCARE IN MY HANDS, A user-centric approach to mak ing medical records accessible on blockcha in,” [Onl ine]. Available: https://daks2k3a4ib2z.cloudfront.net/586ebe41ba9f9499729002dc/5a4b017c7b791a00019e6fb1_Healthwizz_WhitePaper.pdf. [Accessed 21 May 2018]. [Google Scholar]
- [75].CoverUS, “CoverUs,” 2018. [Online]. Available: https://www.coverus.io/ [Accessed 21 May 2018]. [Google Scholar]
- [76].Longenesis, “Longenesis,” Longenesis Ltd, 2018. [Online]. Available: http://longenesis.com/. [Accessed 21 May 2018]. [Google Scholar]
- [77].Mamoshina P, Ojomoko L, Yanovich Y, Ostrovski A, Botezatu A, Prikhodko P, et al. Converging blockchain and next-generation artificial intelligence technologies to decentralize and accelerate biomedical research and healthcare. Oncotarget 2018;9(5):5665–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Desta Y. 9 simple tips for making your website disability-friendly. Mashable 2014;22(April) [Online]. Available: https://mashable.com/2014/04/22/website-disability-friendly/#g2mztd2RasqO. [Accessed 25 October 2018]. [Google Scholar]
- [79].de Arriba-Pérez F, Caeiro-Rodríguez M, Santos-Gago J. Collection and processing of data from wrist wearable devices in heterogeneous and multiple-user scenarios. Sensors (Basel) 2016;16(9). p. PMC5038811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].R. 6749, “The Oauth2.0 Authorization Framework,” 1 October 2012. [Online]. Available: https://tools.ietf.org/html/rfc6749. [Accessed 7 July 2018]. [Google Scholar]
- [81].Apple, Inc, “Apple Health,” Apple, Inc, 2018. [Online]. Available: https://www.apple.com/ios/health/. [Accessed 21 May 2018]. [Google Scholar]
- [82].Google, “The Google Fit SDK,” [Online]. Available: https://developers.google.com/fit/. [Accessed 21 May 2018]. [Google Scholar]
- [83].SAMSUNG, “Samsung Health: The Beginning of Smart Health Care,” 2018. [Online]. Available: https://health.apps.samsung.com/. [Accessed 21 May 2018]. [Google Scholar]
- [84].Fitbit, Inc., “Fitbit,” 2018. [Online]. Available: https://www.fitbit.com/home. [Accessed 21 May 2018]. [Google Scholar]
- [85].MyFitnessPal, Inc., “Lose Weight with MyFitnessPal,” 2018. [Online]. Available: https://www.myfitnesspal.com/. [Accessed 21 May 2018]. [Google Scholar]
- [86].Nokia, “Nokia Body, Weight & BMI Wi-Fi Scale,” 2018. [Online]. Available: https://health.nokia.com/uk/en/body. [Accessed 21 May 2018]. [Google Scholar]
- [87].Morales J, Escobar R, Kaghyan S, Natarajan G, Akopian D, Chalela P, et al. Two-tier state-machine programming for messaging applications Electronic imaging 2017; 2017. Burlingame, CA, USA. [Google Scholar]
- [88].Morales J, Akopian D, Agaian S. Human activity recognition by smartphones regardless of device orientation Proc. SPIE 9030, mobile devices and multimedia: enabling technologies, algorithms, and applications 2014; 2014. San Francisco, CA, USA. [Google Scholar]
- [89].Morales J, Akopian D. Human activity tracking by mobile phones through hebbian learning. Int J Artif Intell Appl 2016;7(6). [Google Scholar]