Abstract
Background
Patients with unicompartmental osteoarthritis of the knee can be treated with an osteotomy. The goal of an osteotomy is to unload the diseased compartment of the knee. This is the second update of the original review published in The Cochrane Library, Issue 1, 2005.
Objectives
To assess the benefits and harms of an osteotomy for treating patients with knee osteoarthritis, including the following main outcomes scores: treatment failure, pain and function scores, health‐related quality of life, serious adverse events, mortality and reoperation rate.
Search methods
The Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and EMBASE (Current Contents, HealthSTAR) were searched until November 2013 for this second update.
Selection criteria
Randomised and controlled clinical trials comparing an osteotomy with other treatments for patients with unicompartmental osteoarthritis of the knee.
Data collection and analysis
Two review authors independently selected trials, extracted data and assessed risk of bias using the domains recommended in the 'Risk of bias' tool of The Cochrane Collaboration. The quality of the results was analysed by performing overall grading of evidence by outcome using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach.
Main results
Eight new studies were included in this update, for a total of 21 included studies involving 1065 people.
In four studies, the randomised sequence was adequately generated and clearly described. In eight studies, allocation concealment was adequately generated and described. In four studies, the blinding procedures were sufficient. In six studies, incomplete outcome data were not adequately addressed. Furthermore, in 11 studies, the selective outcome reporting item was unclear because no study protocol was provided.
Follow‐up of studies comparing different osteotomy techniques was too short to measure treatment failure, which implicates revision to a knee arthroplasty.
Four studies evaluated a closing wedge high tibial osteotomy (CW‐HTO) with another high tibial osteotomy (aHTO). Based on these studies, the CW‐HTO group had 1.8% (95% confidence interval (CI) ‐7.7% to 4.2%; low‐quality evidence) more pain compared with the aHTO group; this finding was not statistically significant. Pooled function in the CW‐HTO group was 0.5% (95% CI ‐3.8% to 2.8%; low‐quality evidence) higher compared with the aHTO group; this finding was not statistically significant. No data on health‐related quality of life and mortality were presented.
Serious adverse events were reported in only four studies and were not significantly different (low‐quality evidence) between groups. The reoperation rate were scored as early hardware removal because of pain and pin track infection due to the external fixator. Risk of reoperation was 2.6 (95% CI 1.5 to 4.5; low‐quality evidence) times higher in the aHTO group compared with the CW‐HTO group, and this finding was statistically significant.
The quality of evidence for most outcomes comparing different osteotomy techniques was downgraded to low because of the numbers of available studies, the numbers of participants and limitations in design.
Two studies compared high tibial osteotomy versus unicompartmental knee replacement. Treatment failure and pain and function scores were not different between groups after a mean follow‐up of 7.5 years. The osteotomy group reported more adverse events when compared with the unicompartmental knee replacement group, but the difference was not statistically significant. No data on health‐related quality of life and mortality were presented.
No study compared an osteotomy versus conservative treatment.
Ten included studies compared differences in perioperative or postoperative conditions after high tibial osteotomy. In most of these studies, no statistically significant differences in outcomes were noted between groups.
Authors' conclusions
The conclusion of this update did not change: Valgus high tibial osteotomy reduces pain and improves knee function in patients with medial compartmental osteoarthritis of the knee. However, this conclusion is based on within‐group comparisons, not on non‐operative controls. No evidence suggests differences between different osteotomy techniques. No evidence shows whether an osteotomy is more effective than alternative surgical treatment such as unicompartmental knee replacement or non‐operative treatment. So far, the results of this updated review do not justify a conclusion on benefit of specific high tibial osteotomy technique for knee osteoarthritis.
Keywords: Humans; Arthroplasty, Replacement, Knee; Osteoarthritis, Knee; Osteoarthritis, Knee/surgery; Osteotomy; Osteotomy/adverse effects; Osteotomy/methods; Randomized Controlled Trials as Topic
Plain language summary
Osteotomy for treating knee osteoarthritis
Researchers from The Cochrane Collaboration conducted a review of the effects of an osteotomy in people with osteoarthritis of the knee. Upon searching for all relevant studies until November 2013, they found 21 studies that included up to 1065 people. Their findings are summarised below.
This review shows that in people with osteoarthritis of the knee:
• osteotomy can improve pain and function, but this is based on changes within a treatment group. No studies compared osteotomy versus conservative treatment; and • no evidence can be found for a preferred osteotomy technique.
What is osteoarthritis of the knee, and what is an osteotomy? Osteoarthritis (OA) is a disease of the joints, such as the knee or the hip. When the joint loses cartilage, the bone grows to try to repair the damage. Instead of making things better, however, the bone grows abnormally and makes things worse. For example, the bone can become misshapen, and this can make the joint painful and unstable. This can affect physical function or ability to use the knee. Two main types of surgery are used to treat patients with osteoarthritis of the knee: knee replacement and osteotomy.
Osteotomy is surgery in which the bones are cut and realigned. Osteotomy around the knee changes the alignment of the knee. Weight bearing will be shifted from the diseased part to a healthy part of the knee. By 'unloading' the damaged cartilage of the knee, osteotomy may decrease pain, improve function, slow knee deterioration and possibly delay the need for (partial or) total knee replacement surgery.
What happens to people after an osteotomy for knee osteoarthritis? Follow‐up of all studies was too short to allow scoring of treatment failure; this refers to a revision to a knee replacement.
In all studies, people reported less pain and improved knee function and quality of life after any type of high tibial osteotomy. However this comparison is based on differences before and after an osteotomy, not on comparison with non‐operative treatment. Probably no differences in pain and function scores are noted between different osteotomy techniques.
Rare complications may include thromboembolism and lesions to nerves and vascular structures.
The most important reasons for reoperation include hardware removal resulting from pain and pin track infection due to the external fixator. This reoperation rate may be higher in patients undergoing another high tibial osteotomy technique compared with those treated with the closing wedge technique.
Two studies compared high tibial osteotomy versus partial knee replacement. Benefits did not differ between these types of surgery.
Summary of findings
Summary of findings for the main comparison. Other types of high tibial osteotomy (aHTO) compared with closing wedge high tibial osteotomy (CW‐HTO) for people with knee osteoarthritis.
| Other types of HTO (aHTO) compared with closing wedge high tibial osteotomy (CW‐HTO) for people with knee osteoarthritis | ||||||
| Patient or population: people with knee osteoarthritis Settings: orthopaedic departments Intervention: another type of HTO (aHTO) Comparison: closing wedge high tibial osteotomy (CW‐HTO) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| CW‐HTO | aHTO | |||||
| Treatment failure rate | See comment | See comment | Not estimablea | ‐ | See comment | Outcome not reported in included studies |
|
Pain Follow‐up: 12 to 30 months Scale: 0 to 10 |
Mean pain score in control groups was 3.1 | Mean pain in intervention groups was 0.18 lower (0.77 lower to 0.42 higher) |
216 (4 studies) | ⊕⊝⊝⊝ Lowb,C | Scores estimated using SMD of ‐0.13 (95% CI ‐0.55 to 0.29) Absolute percentage change 1.8% (95% CI ‐7.7% to 4.2%) Relative percentage change 0.58% (95% CI ‐2.5% to 1.4%) |
|
|
Function Follow‐up: 12 to 30 months Scale: 0 to 100 |
Mean function score in control groups was 79.4 | Mean function in intervention groups was 0.48 lower (3.72 lower to 2.76 higher) | 216 (4 studies) | ⊕⊝⊝⊝ Lowb,C | Scores estimated using SMD of ‐0.10 (95% CI ‐0.57 to 0.36) Absolute percentage change 0.5% (95% CI ‐3.7% to 2.8%) Relative percentage change 0.01% (95% CI ‐0.05% to 0.03%) |
|
| Health‐related quality of life measures | See comment | See comment | Not estimablea | Outcome not reported in included studies | ||
| Serious adverse events Follow‐up: 12 to 28 months | Study population | RR 2.49 (0.64 to 9.75) | 265 (4 studies) | ⊕⊝⊝⊝ Lowb,C | Absolute percentage change 3% (95% CI ‐3% to 9%) Relative percentage change 149% (95% CI ‐36% to 875%) NNH not applicable |
|
| 15 per 1000 | 44 per 1000 | |||||
| Mortality | See comment | See comment | Not estimablea | ‐ | See comment | Outcome not reported in included studies |
| Reoperation rate Follow‐up: 12 to 28 months | Study population | RR 2.58 (1.49 to 4.45) | 224 (4 studies) | ⊕⊝⊝⊝ Lowb,C | Absolute percentage change 19% (95% CI ‐8% to 47%) Relative percentage change 158% (95% CI 49% to 345%) NNH 6 (95% CI 17 to 3) |
|
| 125 per 1000 | 340 per 1000 | |||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aNo useful data available.
bUnblinded studies.
cImprecise estimate due to low event rates.
dNot statistically significant.
Summary of findings 2. Closing wedge high tibial osteotomy (CW‐HTO) compared with unicompartmental knee arthroplasty for people with knee osteoarthritis.
| Closing wedge high tibial osteotomy (CW‐HTO) compared with unicompartmental knee arthroplasty for people with knee osteoarthritis | ||||||
| Patient or population: people with knee osteoarthritis Settings: orthopaedic departments Intervention: unicompartmental knee arthroplasty Comparison: CW‐HTO | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| CW‐HTO | Unicompartmental knee arthroplasty | |||||
|
Treatment failure rate Follow‐up: 7.5 (6.6 to 10) years |
Study population | RR 1.32 (0.94 to 1.87) | 60 (1 study) |
⊝⊝⊝⊝ Very lowa,b | Absolute percentage change 132% (94% CI 94% to 187%) Relative percentage change 32% (95% CI ‐6% to 87%) NNH 4 (95% CI 3.2 to 4.1) |
|
| 786 per 1000 | 594 per 1000 | |||||
| Pain | See comment | See comment | Not estimablec | ‐ | See comment | Outcome not reported in included studies |
| Function | See comment | See comment | Not estimablec | ‐ | See comment | Outcome not reported in included studies |
|
Health‐related quality of life measures Participant opinion: improvement Follow‐up: 5 years |
Study population | |||||
| 955 per 1000 | 1000 per 1000 | RR 0.96 (0.84 to 1.09) | 40 (1 study) |
⊝⊝⊝⊝ Very lowa,b | Absolute percentage change ‐5% (95% CI ‐17% to 8%) Relative percentage change 4% (95% CI ‐16% to 9%) NNT 23 (95% CI 17.3 to 31.1) |
|
| Adverse events Follow‐up: 7.5 (6.6 to 10) years | Study population | RR 0.25 (0.06 to 1.08) | 60 (1 study) |
⊝⊝⊝⊝ Very lowa,b | Absolute percentage change ‐21% (95% CI ‐39% to ‐3%) Relative percentage change 75% (95% CI ‐94% to 8%) NNH 5 (95% CI 4.3 to 5.9) |
|
| 71 per 1000 | 281 per 1000 | |||||
| Mortality | See comment | See comment | Not estimablec | ‐ | See comment | Outcome not reported in included studies |
| Reoperation rate | See comment | See comment | Not estimablec | ‐ | See comment | Outcome not reported in included studies |
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aUnblinded studies.
bImprecise estimate due to low event rates.
cNo useful data available.
Background
Description of the condition
Osteoarthritis has a major impact on functioning and independence and ranks among the top 10 causes of disability worldwide (Badley 1995; Murray 1996). Knee osteoarthritis is the most common joint disorder, and symptomatic disease occurs in 10% of men and 13% of women older than 60 years of age (Zhang 2010). The lifetime risk of developing symptomatic knee osteoarthritis has been estimated to be around 45% (Murphy 2008). Osteoarthritis of the knee is defined as a multi‐factorial disease that may result from both biological and mechanical events.
The knee joint can be divided into three compartments:
Medial compartment, consisting of the medial femur condyle and the medial tibial plateau;
Lateral compartment, consisting of the lateral femur condyle and the lateral tibial plateau; and
Patellofemoral compartment.
Osteoarthritis of the entire knee is distinguished from osteoarthritis of one compartment (Grelsamer 1995), which generally is caused by a mechanical problem (Tetsworth 1994). The mechanical axis of a straight leg is a line passing from the centre of the hip, through the centre of the knee, to the centre of the ankle (Phillips 1998). Patients with osteoarthritis of the medial compartment often have varus alignment, and the mechanical axis and load bearing pass through the medial compartment. Patients with osteoarthritis of the lateral compartment often have a valgus alignment, and the mechanical axis and load bearing pass through the lateral compartment. The medial compartment is almost 10 times more frequently involved than the lateral compartment. Moreover, varus but not valgus alignment increases the risk of incident tibiofemoral osteoarthritis (Brouwer 2007; Sharma 2010). Both varus malalignment and valgus malalignment increase the progression of knee osteoarthritis and predict declines in physical function (Sharma 2001).
Patients with unicompartmental osteoarthritis of the knee not reacting to non‐active interventions such as standard care including physiotherapy (Anandacoomarasamy 2013; Fransen 2008; Knoop 2013; Wang 2012), or to active non‐operative control interventions such as corrective insoles and braces (Brouwer (2) 2005), intra‐articular injection of hyaluronic acid (Berenbaum 2012; Strand 2012) or autologous platelet‐rich plasma (Cerza 2012), or both, can be treated with a correction osteotomy (Aglietti 2000; Coventry 1993; Edgerton 1993; Naudie 1999).
Alternative surgical treatment for patients with unicompartmental knee osteoarthritis in the standard orthopaedic clinic depends on the degree of osteoarthritis. In cases of early‐stage osteoarthritis, arthroscopic debridement of the knee is frequently performed (Feeley 2010; Steadman 2013). In cases of moderate or severe osteoarthritis, unicompartmental or total knee replacement is the preferred treatment option. Cartilage repair surgery such as autologous cartilage implementation, microfracture and an osteochondral autograft transfer system nowadays is possible only when a focal cartilage defect is present in one of the knee compartments, especially on the femoral site (Vasiliadis 2011; Vavken 2010).
Description of the intervention
An osteotomy is a surgical procedure, which implies that the bone is cut. A correction osteotomy at the knee is used to realign the leg and to transfer the weight‐bearing axis from the pathological compartment to the healthy compartment. Patients with osteoarthritis of the medial compartment and varus alignment can be treated with a valgus osteotomy, and those with osteoarthritis of the lateral compartment and valgus alignment with varus osteotomy.
Several correction osteotomy techniques are available for unicompartmental knee osteoarthritis such as the closing wedge technique with removal of a wedge of bone, the opening wedge technique with creation of a wedge, a combined (opening and closing wedge) technique and techniques that are performed without creating a wedge in the bone, including dome osteotomy and hemicallotasis osteotomy with an external fixator (Brouwer 2006; Gaasbeek 2010; Magyar 1999a; Nakamura 2001; Papp 2009). The correction osteotomy for knee osteoarthritis is performed at the proximal tibia or the distal femur. The choice of osteotomy technique and the level of the osteotomy depend on the degree and location of malalignment and the experience of the surgeon in performing one or more of these techniques.
How the intervention might work
A correction osteotomy will change the alignment of the affected leg with unloading of the osteoarthritic compartment of the knee. Unloading will result in slowing down of the osteoarthritis process. In retrospective studies, this procedure resulted in pain relief, improved function and postponement of knee arthroplasty for seven to 20 years, depending on participant selection, stage of osteoarthritis and achievement and maintenance of adequate operative correction (Berman 1991; Brouwer (2) 2005; Cameron 1997; Finkelstein 1996; Hernigou 1987; Mathews 1998; Naudie 1999; Raaij 2008; Rudan 1990).
Why it is important to do this review
Literature suggests that a correction osteotomy for unicompartmental knee osteoarthritis leads to good results, but many surgical techniques are available. Moreover, a few important surgical alternatives such as intra‐articular cartilage repair techniques for early‐stage osteoarthritis and unicompartmental knee arthroplasty for end‐stage osteoarthritis may be selected (Bouwmeester 2002; Broughton 1986; Stukenborg 2001). It is unclear which of these treatment options is superior.
Objectives
To assess the benefits and harms of an osteotomy for treating patients with knee osteoarthritis, including the following main outcomes scores: treatment failure, pain and function scores, health‐related quality of life, serious adverse events, mortality and reoperation rate.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and controlled clinical trials (CCTs) investigating all types of osteotomy for treatment of osteoarthritis of the knee compared with other surgical and non‐operative treatment modalities.
Types of participants
Adult patients (> 18 years) with unicompartmental osteoarthritis of the medial or lateral compartment of the knee confirmed by radiographic or arthroscopic investigation.
Types of interventions
All types of osteotomy around the knee for patients with unicompartmental osteoarthritis of the knee were compared with inactive control interventions (i.e. standard care including physiotherapy); with active non‐operative control interventions (e.g. corrective insoles and braces, intra‐articular injection of hyaluronic acid and/or autologous platelet‐rich plasma); and with operative control interventions including different osteotomy techniques, arthroscopic interventions, knee replacements (unicompartmental and total knee arthroplasties (TKAs)) and other types of surgery. Studies comparing one technique of osteotomy versus different perioperative conditions or versus different types of postoperative treatment were also included.
Types of outcome measures
Major outcomes
Treatment failure rate (i.e. incidence to TKA and time to revision).
Pain.
Function.
Health‐related quality of life measures.
Serious adverse events, neurovascular complications (e.g. bleeding, thromboembolism, neuropathy).
Mortality.
Reoperation rate (e.g. early or late hardware removal resulting from pain and pin track infection due to the external fixator).
Minor outcomes
Performance‐based outcome.
Adverse effects resulting from anatomical changes after high tibial osteotomy, including patellar descent and tibial plateau slope change, which may influence results of future total knee arthroplasty, and adverse effects resulting from use of an external fixator, including local pin track infection.
Other minor outcomes, including visual analogue scale (VAS) score satisfaction, Patient Global Assessment, joint imaging, walking distance, range of motion (ROM), collateral laxity and walking distance.
Search methods for identification of studies
The search strategy (search date, 5 November 2013) yielded a total of 633 records from the following databases: Ovid MEDLINE 1946 to 2013, Ovid EMBASE 1947 to 2013, the Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 10 of 12) (all databases) and clinicaltrials.gov, in accordance with the Methodological Expectations of Cochrane Intervention Reviews (MECIR) standards (http://www.editorial‐unit.cochrane.org/mecir Clinicaltrials.gov). After duplicates were removed, 491 records remained.
We used the sensitivity maximising RCT filter from Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions [version 5.1.0] (Lefebvre 2011). We applied no language restrictions. The search was developed in Ovid MEDLINE and was modified for use in other databases. (See Appendix 1: Search strategies.) Furthermore, the International Clinical Trials Registry Platform (ICTRP) of the World Health Organization (WHO) was checked for ongoing or recently completed studies (http://www.who.int/ictrp/en/).
Data collection and analysis
Selection of studies
Two review authors selected the trials, initially on the basis of title and abstract. Title, keywords and abstract were assessed to establish whether the study met the inclusion criteria regarding diagnosis, design and intervention. For each selected study, the full article was retrieved for final assessment. Next, two review authors independently performed a final selection of trials for inclusion in the review, using a pretested standardised form. Disagreements on inclusion were resolved by discussion, and the final decision of a third review author was not necessary.
Data extraction and management
Three review authors independently extracted data on the intervention, types of outcome measures, follow‐up, loss to follow‐up and outcomes, using a pretested standardised form. Various outcome measures are presented separately.
Assessment of risk of bias in included studies
The Cochrane Collaboration recommends a specific tool for assessing risk of bias in each included study. This comprises a judgement and a support for each judgement in a 'Risk of bias' table, in which each entry addresses a specific feature of the study. Judgement for each entry involves assessing risk of bias as 'low risk,' 'high risk' or 'unclear risk' of bias, with the last category indicating lack of information or uncertainty over the potential for bias.
Different entries for assessing risk of bias include the following.
-
Random sequence generation (selection bias).
Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence.
-
Allocation concealment (selection bias).
Selection bias (biased allocation to interventions) due to inadequate concealment of allocations before assignment.
-
Blinding (performance bias and detection bias).
Performance bias or detection bias due to knowledge of allocated interventions after assignment.
-
Blinding of participants and personnel (performance bias).
Performance bias due to knowledge of allocated interventions by participants and personnel during the study.
-
Blinding of outcome assessment (detection bias).
Detection bias due to knowledge of allocated interventions by outcome assessors.
-
Incomplete outcome data (attrition bias).
Attrition bias due to amount, nature or handling of incomplete outcome data.
-
Selective reporting (reporting bias).
Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence.
Other bias due to problems not covered elsewhere in the table such as recruitment bias, baseline imbalance, loss of clusters and incorrect analysis.
Two review authors independently assessed the risk of bias of included studies. Disagreements were resolved in a consensus meeting, and, when necessary, an independent third person was consulted.
Risk of bias items for each study are presented in the 'Risk of bias' tables, and a plot of the distribution of judgements across studies for each risk of bias item is presented in 'Risk of bias graphs' as figures.
Measures of treatment effect
For dichotomous outcomes, we calculated risk ratios (RRs) with corresponding 95% confidence intervals (CIs). For continuous outcomes, mean differences (MDs) or standardised mean differences (SMDs) with 95% confidence intervals were calculated.
Dealing with missing data
For continuous data, when dropouts were identified, we used available data. However, for dichotomous data, we performed an intention‐to‐treat analysis, whereby all missing people were considered to have a bad outcome. We refrained from imputing values for standard deviations unless missing standard deviations could be derived from confidence intervals, standard errors or presented P values in the same study.
Assessment of heterogeneity
Clinicians on the review team assessed clinical heterogeneity on the basis of information on the study population (age), interventions (type of osteotomy), control interventions (osteotomy and arthroplasty), outcomes (pain, function, etc) and timing of follow‐up (number of years). We assessed statistical heterogeneity between pooled trials using a combination of visual inspection of the graphs and consideration of the I2 statistic (Higgins 2011). We defined an I2 value less than 40% as indicating heterogeneity that is unimportant, 30% to 60% as indicating a moderate degree of heterogeneity, between 50% and 90% as showing substantial heterogeneity and 75% to 100% indicating considerable heterogeneity.
Data synthesis
RevMan 5.2 software was used to analyse these data, and the various outcomes are presented in the Analyses graphs. Pooling was implemented for the outcome complication only after a closing wedge high tibial osteotomy compared with another high tibial osteotomy technique, as trials were considered clinically heterogeneous in terms of study population, interventions and outcomes. Results of comparable groups of trials were pooled using a random‐effects model and 95% confidence intervals.
Analysis was set up to identify three study groups
Operative versus conservative treatment.
-
Different operative treatments.
Different high tibial osteotomy techniques.
High tibial osteotomy versus unicompartmental joint replacement.
Differences in perioperative conditions.
Different treatment post surgery.
'Summary of findings' table
'Summary of findings' tables were created using GRADEpro software (http://www.cc‐ims.net/gradepro) for the comparison of other type of high tibial osteotomy versus closing wedge high tibial osteotomy and for the comparison of closing wedge high tibial osteotomy versus unicompartmental knee arthroplasty, including the outcomes of treatment failure rate, pain, function, health‐related measures, adverse events, mortality and reoperation rate. See Table 1 and Table 2.
The quality of the presenting results was analysed through an overall grading of evidence by outcome using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach (Guyatt 2008a; Guyatt 2008b; Schünemann 2008). The highest quality rating is assigned for randomised trial evidence.
The GRADE approach specifies four levels of quality.
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
Trial evidence can be downsized to moderate, low or very low quality depending on the presence of five factors.
Limitations in design and implementation of available studies, suggesting high likelihood of bias.
Indirectness of evidence (indirect population, intervention, control, outcomes).
Unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses).
Imprecision of results (wide confidence intervals).
High probability of publications bias.
Quality will be reduced by one level for each factor, up to a maximum of three levels for all factors. If very severe problems are identified for any one factor (e.g. when limitations in design and implementation are assessed, all studies were unconcealed and unblinded and lost more than 50% of participants to follow‐up), randomised trial evidence may be reduced by two levels because of that factor alone.
If pooling of study results is not possible, a single study and by definition low‐quality evidence is evaluated; the quality of this study can be downgraded according to risk of bias items.
Results
Description of studies
A total of 21 studies involving 1065 people were included; 11 were included in the first version, two studies and one longer follow‐up study were included in the first update and eight additional studies were included in this second update.
Results of the search
The search strategy (up to 2013) yielded a total of 633 records from the following databases: Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and EMBASE (Current Contents, HealthSTAR).
A total of 491 reports of potentially eligible studies were found, from which 30 full reports were obtained. After the full reports were read, a total of 21 studies were included and nine were excluded from this review. No ongoing studies and no studies awaiting classification were identified (Figure 1, PRISMA diagram).
1.

Study flow diagram.
For further details on results of the search, see Appendix 1, 'Search strategies and results summary.'
Included studies
The mean number of included participants in the 21 studies was 52 (range 30 to 100). Mean participant age was 60 years (42 to 67 years). Interventions included different techniques of high tibial osteotomy, high tibial osteotomy versus unicompartmental joint replacement, different perioperative conditions and different types of postoperative treatment regimens.
Nine studies compared two techniques of high tibial osteotomy (HTO). Most of these studies concerned a valgus high tibial osteotomy for medial compartment osteoarthritis of the knee. In only two studies, participants with lateral compartment osteoarthritis were also included.
Two studies compared the high tibial osteotomy versus unicompartmental joint replacement.
Ten studies compared the same type of HTO versus different perioperative conditions (seven studies) or different types of postoperative treatment (three studies). Two studies compared high tibial osteotomy versus unicompartmental joint replacement. No study compared osteotomy versus conservative treatment. Follow‐up in most studies was relatively short (mean 1.8 years, range 0.2 to 7.5 years).
Outcomes
Pain, function, adverse events, reoperation rate, performance‐based outcomes and adverse effects of an osteotomy were the most frequently reported outcomes. Performance‐based outcome was focused principally on accuracy of postoperative correction. Because of the relatively short follow‐up time of most studies, joint imaging was focused on anatomical changes after high tibial osteotomy, not on the degree of progression of osteoarthritis.
Major outcomes
Failure of treatment rate (incidence to TKA and time to revision): In all included studies comparing different techniques of HTO, follow‐up was too short for scoring of this outcome. Only one longer follow‐up study (Stukenborg 2001) comparing high tibial osteotomy versus unicompartmental knee replacement scored treatment failure.
Pain: VAS and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain subscore were used to measure pain. In all studies, participants reported pain reduction after high tibial osteotomy.
Function: Knee injury and Osteoarthritis Outcome Score (KOOS) and WOMAC were the most important scores for measuring function. Lysholm score, Hospital for Special Surgery (HSS) knee score, American Knee Society Score (KSS), British Orthopaedic Association (BOA) knee score, Japanese Orthopaedic Association (JOA) knee score and gait analysis were less frequently used scores for measuring function.
In all studies, participant knee function scores improved after high tibial osteotomy.
Health‐related quality of life measure: Nottingham Health Profile (NHP) score and EuroQol were used to measure this outcome, which improved after high tibial osteotomy.
Serious adverse events: These events, including thromboembolism, neurovascular pathology, intra‐articular fracture, deep infection and non‐union of the osteotomy, were rarely reported.
Mortality: This event was not reported in all included studies.
Reoperation rate: This was scored as early hardware removal resulting from pain and pin track infection due to the external fixator. These adverse events were significantly more numerous in participants undergoing another high tibial osteotomy technique compared with those treated with the closing wedge technique.
Minor outcomes
Performance‐based outcome: This was scored as achievement of postoperative correction, surgery time, hospital stay, time to healing of the osteotomy and inferior limb length.
Adverse effects based on anatomical changes: These imply difficulties in performing total knee arthroplasty after high tibial osteotomy. Excessive valgus alignment, patellar descent and change in inclination angle of the tibial plateau were measured side effects in these studies. Alignment was scored according to the hip‐knee‐ankle (HKA) angle or the femoral tibial angle (FTA). For change in patellar height, the Insall Salvati, Blackburne Peel and Caton methods were used. The inclination angle of the tibial plateau was measured according to the Moore and Harvey and Brazier et al methods. The mechanical medial proximal tibial angle (mMPTA) and the mechanical lateral distal femoral angle (mLDFA) are anatomical changes that may cause difficulties when total knee arthroplasty is performed after high tibial osteotomy. Patellar descent and increased tibial slope were significantly greater after opening wedge high tibial osteotomy.
Patient Global Assessment: Wallgren‐Tegner and the Modified Cincinnati Rating System Questionnaire were used and showed improvement after high tibial osteotomy without statistical significance in between‐group differences.
Other minor outcomes: Joint imaging was measured in only one study (Odenbring 1992); degree of osteoarthritis was measured before and one year after high tibial osteotomy. This study demonstrated no progression of osteoarthritis within one year after osteotomy. VAS satisfaction was measured in one study (Gaasbeek 2010) and was improved after high tibial osteotomy. Collateral laxity was more improved after opening wedge compared with closing wedge high tibial osteotomy (Gaasbeek 2010). Walking distance, which is an indirect measurement of function, was assessed and showed improvement after osteotomy treatment (Brouwer 2006).
Included studies
These studies are described in detail in the Characteristics of included studies table.
Adili 2002 described a matched comparative analysis of two techniques: the osteotomy with the Ilizarov apparatus versus the Coventry‐type closing wedge osteotomy. Inclusion criteria were varus alignment and symptomatic medial compartment osteoarthritis (OA). Both groups consisted of 15 participants, but they were not randomly assigned. The study included 20 men and 10 women. The mean age of participants was 52, and the body mass index was 32.8. The mean degree of varus was three degrees (FTA). Follow‐up was different: 25.4 months in the Ilizarov group and 30.9 months in the Coventry group. The funding source was not reported.
Akizuki 1997 described an RCT of 79 participants (88 knees). A total of 45 participants (51 knees) were treated by osteotomy with arthroscopic abrasion arthroplasty, and 34 participants (37 knees) were treated by osteotomy alone. The inclusion criterion was medial compartment OA. The study included 9 men and 70 women. The mean age of participants was 64 years. The mean degree of varus was five degrees (FTA). Follow‐up was 4.8 years in the osteotomy with abrasion group and 3.5 years in the osteotomy group. The funding source was not reported.
Brouwer 2005 presented an RCT in which two techniques were evaluated: the opening wedge high tibial osteotomy versus the closing wedge high tibial osteotomy. Criteria for inclusion were OA of the medial compartment with medial pain and varus malalignment of the mechanical axis measured on long‐standing radiographs. Outcome measures were factors that may cause difficulties in conversion to total knee arthroplasty and were scored as side effects. A total of 51 participants (33 men and 18 women) were randomly assigned (opening wedge HTO; n = 26/closing wedge HTO; n = 24). The mean age of participants was 50. The mean degree of varus was seven degrees (HKA angle). Follow‐up was one year, and one participant was lost. No benefits or funding in any form was received.
Brouwer 2006 published a second RCT study comparing the opening wedge high tibial osteotomy versus the closing wedge high tibial osteotomy. Criteria for inclusion were OA of the medial compartment with medial pain and varus malalignment of the mechanical axis measured on long‐standing radiographs. A total of 92 participants (59 men and 33 women) were randomly assigned (opening wedge high tibial osteotomy; n = 45/closing wedge high tibial osteotomy; n = 47). The mean age of participants was 50. The mean degree of varus was six degrees (HKA angle). Outcome measures were accuracy of the operative correction, pain severity (VAS), knee function score (HSS) and walking distance. Follow‐up was one year. One participant was lost to follow‐up, and for another participant the follow‐up data were incomplete. No benefits or funding in any form was received.
Gaasbeek 2010 published an RCT comparing the opening wedge high tibial osteotomy versus the closing wedge high tibial osteotomy. Criteria for inclusion were active, between 18 and 70 years of age, symptomatic medial OA of the knee with a hip‐knee‐ankle (HKA) varus alignment. A total of 50 participants (30 men and 20 women) were randomly assigned (opening wedge HTO; n = 25/closing wedge HTO; n = 25).The mean age of participants was 49 years.The mean degree of varus was 4.1 degrees (HKA angle). Outcome measures were postoperative alignment, collateral laxity, WOMAC, KSS, VAS (pain and satisfaction), Caton Index, surgery time and hospital stay. Follow‐up was one year, and no participant was lost to follow‐up. The funding source was not reported.
Harding 2011 evaluated in an RCT the effect of a single infusion of bisphosphonate (zoledronic acid) on fracture healing four weeks post hemicallotasis osteotomy (HCO) compared with placebo (an infusion of sodium chloride). Inclusion criteria were age between 35 and 65 years and OA or deformity of the knee requiring an HCO. A total of 46 participants (36 men) with a mean age of 49 (37 to 63) years were included: 25 participants in the zoledronic group and 21 in the sodium chloride control group. The mean preoperative varus angle was seven degrees (HKA angle). A total of 41 participants had medial compartment OA, and five had lateral compartment OA. Outcome measures were time to bone healing, KOOS, evaluation of densitometry, evaluation of retention of surgically achieved correction and safety/side effects. Follow‐up was from eight weeks to 1.5 years. The funding source was reported.
Iori 2011 described an RCT of 24 participants (27 knees). A total of 13 participants (14 knees) were treated by opening wedge osteotomy with navigation, and 11 (13 knees) were treated by opening wedge osteotomy without navigation. Inclusion criteria were age < 65 years, Kellgren‐Lawrence symptomatic grade III or lower, isolated medial compartment knee OA, failed conservative treatment, absence of additional cartilage treatment and concomitant ligamentous lesions. The study included 14 men and 10 women. The mean age of participants was 55 years. The mean degree of varus was 6.8 degrees (HKA angle). Follow‐up time was 39 months (12 to 72). Outcome measures were alignment (HKA angle), proximal medial tibia angle (mMPTA), lateral distal femoral angle (mLDFA), tibial slope (Brazier methods), patellar height (Insall‐Salvati Index), inferior limb length, American KSS, Modified Cincinnati Rating System Questionnaire, VAS (pain: 0 = unbearable pain and 10 = no pain). The funding source was not reported.
Luites 2009 published an RCT of 42 participants (27 men and 15 women) comparing the opening wedge (n = 23) versus the closing wedge high tibial osteotomy (n = 19). Inclusion criteria were OA of the medial compartment and a varus mechanical axis deformity less than 12 degrees. Futhermore, the body mass index had to be less than 30 kg/m2. The mean age of participants was 53 years. Outcome measures were stability of the osteotomy and retention of the operative correction using radiostereometry (RSA). RSA is a method that uses tantalum markers in the bone to determine three‐dimensional changes in the osseous correction. Other outcomes were Lysholm function score and VAS pain score. No participant was lost to follow‐up; however one participant in the closing wedge group did not receive the allocated intervention and was subsequently included in the analysis for the opening wedge group. The funding source was reported.
Magyar 1999a presented an RCT of two techniques: the hemicallotasis opening wedge osteotomy (HCO; 24 participants/25 knees) versus the closing wedge high tibial osteotomy (22 participants/25 knees). Inclusion criteria were medial knee OA and younger, active patients. The study included 32 men and 14 women. The mean age of participants was 55 years. The mean degree of varus was nine degrees (HKA angle). Follow‐up was two years. Two dropouts (one in each group) were reported for the NHP assessment. No commercial funding was received.
Magyar 1999b published a second RCT study with RSA. This study is probably linked with the study Magyar 1999a because the participants and the interventions (hemicallotasis opening wedge osteotomy vs closing wedge high tibial osteotomy) are identical. The inclusion criterion was medial gonarthrosis grade I to III. A total of 33 participants (22 men and 11 women) were studied: hemicallotasis opening wedge osteotomy 18 participants/19 knees versus high tibial osteotomy 15 participants/16 knees with a baseline grade I to III. The mean age of participants was 54 years, and the mean body mass index was 29.5. The mean degree of varus was nine degrees (HKA angle). Follow‐up was one year. The funding source was not reported.
Mammi 1993 described a double‐blind study of 40 participants. In this study, the high tibial osteotomy technique was the same, but postoperatively, participants were randomly assigned to the intervention group (long plaster cast with an electromagnetic field stimulation; n = 20) or the control group (a long plaster cast with a dummy stimulator; n = 20). Randomisation was performed according to the order of admission of participants to the hospital. Inclusion criteria were maximum age of 80 years, good health and requiring tibial reduction osteotomy. The study included nine men and 31 women. The mean age of participants was 62 years. Follow‐up was 60 days. Two dropouts were reported in the intervention group versus one dropout in the control group. The funding source was not reported.
Motycka 2000 published an RCT of 65 participants to look at the side effects of high tibial osteotomy. He studied the incidence of thrombosis in high tibial osteotomy with (n = 37) and without (n = 28) the use of a tourniquet. A Dimer test and phlebography were used to confirm the diagnosis. The inclusion criterion was varus OA. The study included 30 men and 35 women. The mean age of participants was 61 years. Follow‐up was nine weeks. Dropout of 15 participants caused inequality in numbers in the groups. The funding source was not reported.
In the RCT of Myrnerts 1980, the closing wedge high tibial osteotomy technique was the same in both groups, but the 77 participants were allocated at random to the normal correction group (n = 40) or the five‐degree overcorrection group (n = 37). The inclusion criterion was varus alignment. The study included 32 men and 45 women. The mean age of participants was 61 years. All participants had a follow‐up of one year, and "most" were examined 24 months postoperatively. The funding source was not reported.
Nakamura 2001 presented an RCT wherein 46 participants were randomly allocated to a hemicallotasis opening wedge osteotomy (HCO; 23 participants/25 knees) or a dome osteotomy (DMO; 23 participants/25 knees). The inclusion criterion was medial OA of the knee. This study included nine men and 37 women. The mean age of participants was 63 years. The mean degree of varus was two degrees (FT angle). Investigtors studied changes in FTA, patellar tendon length, inclination angle of the tibial plateau and condylar offset at one year postoperatively. Follow‐up was one year. No commercial funding was received.
Odenbring 1992 published an RCT study with 32 participants randomly assigned to a cylinder plaster cast (n = 17) or a hinged cast brace (n = 14) after HTO. Because of a complication, one participant in the brace group was excluded and was not included in the analysis. Inclusion criteria were stages I to III medial gonarthrosis. Follow‐up was one year. The funding source was not reported.
Papp 2009 published an RCT comparing the closing wedge high tibial osteotomy versus the combined osteotomy (CO), which is a combination of an opening and a closing wedge high tibial osteotomy (CWO). Criteria for inclusion were pain on the medial side of the knee, varus malalignment involving the tibia and narrowing of the medial joint space that did not exceed 50% on a standing anteroposterior radiograph. A total of 91 participants (52 men and 49 women) were randomly assigned (CWO; n = 46/CO; n = 45). The mean age of participants was 52 years. Outcome measures were inclination of the tibial plateau and patellar height. Follow‐up was one year; three participants were excluded for analysis, and six (three in each group) were lost to follow‐up. The funding source was not reported.
Stukenborg 2001 published an RCT of 60 participants. The study compared HTO (HTO; n = 32) versus unicompartmental joint replacement (unicompartmental knee arthroplasty (UKA); n = 28). Inclusion criteria were medial unicompartmental OA, varus < 10 degrees, flexion contracture < 15 degrees, age > 60 years, ligament instability < grade II. This study included 25 men and 35 women. The mean age of participants was 67 years. The mean degree of varus was nine degrees (HKA angle). Follow‐up was 7.5 (6.6 to 10) years. The funding source was not reported.
Toksvig‐Larsen 2008 published an RCT comparing the strength of different types of pin fixation in hemicallotasis opening wedge osteotomy. A total of 50 participants (37 men and 13 woman) with a mean age of 51 years were included. Participants were randomly allocated to standard pins or XCaliber pins, both of which are hydroxyapatite (HA) coated. XCaliber pins are self‐drilling and are less conical than standard pins. Inclusion criteria were not specifically described, but participants with medial OA and a varus alignment (n = 42), as well as those with lateral compartment and a valgus alignment (n = 8), were included. Outcome measures were insertion/extraction torque forces, pin site infections and other complications. Follow‐up was less than six months. The funding source was not reported.
Toksvig‐Larsen 2013 published a second RCT comparing removal torque of different types of pin fixation in hemicallotasis opening wedge osteotomy. A total of 20 participants were included. Participants were randomly allocated to bisphosphonate‐coated pins and hydroxyapatite‐coated pins. Inclusion criteria are not specifically described: Patients treated by hemicallotasis osteotomy technique for medial or lateral OA of the knee were included. The outcome measure was removal torque force. Follow‐up was eight to 15 weeks. The funding source was reported.
Weidenhielm 1993 published the one‐year results of an ongoing RCT. This RCT started with 100 participants, but during the one‐year follow‐up, 41 participants were lost and were not included in the analysis. The reason for loss to follow‐up of a large number of participants was not described. In 59 participants, a high tibial osteotomy (n = 23) was compared with unicompartmental knee arthroplasty (UKA; n = 36). Inclusion criteria were medial osteoarthritis grade I to II and 55 to 70 years of age. This study included 28 men and 31 women. The mean age of participants was 64 years. The mean body mass index was 28.5. The mean degree of varus was nine degree (HKA angle). Five‐year follow‐up results were published in 2005 (Borjesson 2005 in Weidenhielm 1993). At five‐year follow‐up, 40 participants were left: high tibial osteotomy, n = 18; unicompartmental knee arthroplasty, n = 22. The funding source was not reported.
Zorzi 2011 published an RCT comparing opening wedge high tibial osteotomy with and without autologous bone iliac bone graft. Inclusion criteria were varus alignment of the limb that could be corrected by a plate with at least a 12.5‐mm spacer, associated with OA, and pain limited to the medial side that did not improve with conservative management. A total of 46 participants were included (43 men and three women): 23 in each group. The mean age of participants was 42 years, and BMI was 27.6. In 33 participants, knee instability was present in addition to varus OA. Follow‐up was at least one year, and no participants were lost to follow‐up. The funding source was not reported.
Excluded studies
After the full texts were retrieved for final assessment, nine studies were excluded (Bae 2009; Bekerom 2008; Cho 2013; Dallari 2012; Gouin 2010; Maffulli 2013; Odenbring 1992b; Pape 2013; Yim 2013). Four studies (Bae 2009; Bekerom 2008; Cho 2013; Yim 2013) were excluded because of a retrospective design. Dallari 2012 was excluded because participants with traumatic cartilage lesions were included. Maffulli 2013 was excluded because in addition to differences in augmentation of the gap after opening wedge high tibial osteotomy, fixation of the osteotomy was different between groups. Pape 2013 was excluded because of the design of the study and the primary outcome: fixation stability of high tibial osteotomy implants as determined by radiostereometric analysis.
Odenbring 1992b did not report the aimed outcome measure. Gouin 2010 was excluded because patients with lateral instability or post‐traumatic genu varum without OA were included. Moreover, investigators discontinued the study after 40 inclusions because of undesirable events in the intervention group (loss of correction).
Risk of bias in included studies
Random sequence generation
In two controlled clinical studies, no randomisation was performed (Adili 2002; Akizuki 1997). In only four studies, the randomised sequence was adequately generated and clearly described (Brouwer 2005; Brouwer 2006; Luites 2009; Mammi 1993).
Allocation concealment
In only eight studies, allocation concealment before assignment was adequately generated and described (Brouwer 2005; Brouwer 2006; Gaasbeek 2010; Luites 2009; Magyar 1999b; Papp 2009; Toksvig‐Larsen 2008; Toksvig‐Larsen 2013).
Blinding
In many studies, the blinding procedures of treatment providers, participants and outcome assessors were insufficient. However, blinding to surgical procedures frequently is not possible. In six studies, at least one of the blinding items was scored as low risk (Harding 2011; Iori 2011; Magyar 1999a; Mammi 1993; Papp 2009; Zorzi 2011); in two studies, both participants and outcome assessors were blinded (Harding 2011; Zorzi 2011); and in only two studies, the treatment provider, the participant and the outcome assessor were blinded (Mammi 1993; Toksvig‐Larsen 2013).
Incomplete outcome data
In six studies, incomplete outcome data were not adequately addressed (Mammi 1993; Motycka 2000; Odenbring 1992; Papp 2009; Toksvig‐Larsen 2008; Weidenhielm 1993). These studies with dropouts did not include an intention‐to‐treat analysis. In one of these studies (Motycka 2000), remarkable and inexplicably more dropouts were reported in the control group compared with the intervention group. In Luites 2009, one participant did not received the allocated intervention, but this participant was not excluded.
Selective reporting
In most studies, the selective outcome reporting item was unclear because no study protocol was provided.
Other potential sources of bias
In seven studies, bias was caused by different follow‐up times (Adili 2002; Akizuki 1997), imbalance of intervention groups without correction (Akizuki 1997; Harding 2011; Zorzi 2011) or incorrect analysis (Magyar 1999a; Odenbring 1992). These sources of bias were not described in the table and were scored as "other potential sources of bias."
Further details on risk in each study are available in Figure 2, Figure 3 and the 'Risk of bias' tables.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
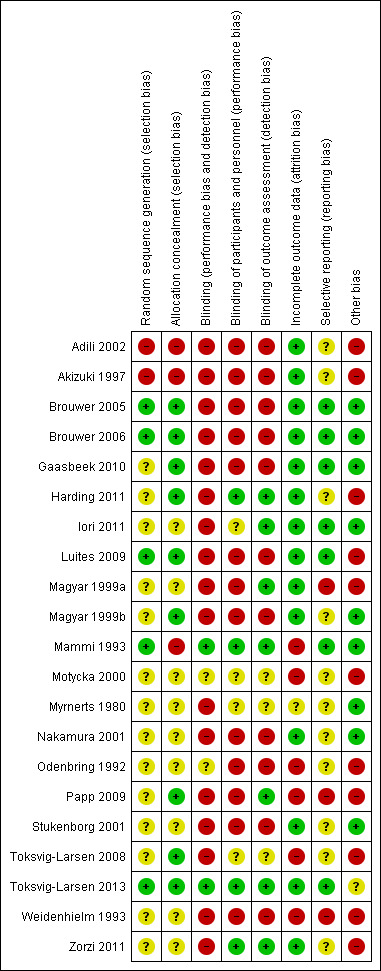
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Heterogeneity of included studies
Nine studies comparing different osteotomy techniques showed no clinical heterogeneity in terms of the study population because the indication for an osteotomy for knee OA is well defined. In eight of these nine studies, another type of osteotomy (aHTO) was compared with the closing wedge high tibial osteotomy. In only one study, other types of osteotomy techniques were compared, and in this study, major outcomes were not scored. Four of these nine studies scored major outcomes, and these data have been pooled. No clinical heterogeneity was noted in duration of follow‐up, which in all of these studies was one to two years. Two studies compared the closing wedge high tibial osteotomy versus unicompartmental knee replacement. Because of longer follow‐up and higher mean age of included participants, these data have not been pooled with those of studies comparing other types of osteotomy with the closing wedge technique. Statistical heterogeneity was considerable for the major outcome of pain (76.3%) and was substantial for the major outcome of function (62.9%). Unimportant heterogeneity was observed for the major outcomes of serious adverse events and reoperation rate.
Effects of interventions
All studies used different interventions or comparisons with a wide variety of outcome measures. Because of the heterogeneity of studies, pooling of results was possible only for pain, function, serious adverse events, reoperation rate and accuracy of the correction after a closing wedge high tibial osteotomy versus another high tibial osteotomy technique. Most studies showed improvement in patient‐reported outcomes (less pain and improved function scores) after high tibial osteotomy; however most studies also showed no statistically significant differences in comparison with other surgical treatments (other techniques of high tibial osteotomy/unicompartmental joint replacement).
Osteotomy versus non‐operative treatment
No studies compared osteotomy versus inactive control interventions (standard care including physiotherapy) or versus active non‐operative control interventions (corrective insoles and braces, intra‐articular injection of hyaluronic acid and/or autologous platelet‐rich plasma).
Osteotomy versus operative control interventions
A total of 11 studies compared osteotomy versus operative controls: Nine studies compared different osteotomy techniques, and two studies compared osteotomy versus unicompartmental knee replacement.
Different osteotomy techniques
Nine studies compared two techniques of high tibial osteotomy (Adili 2002; Brouwer 2005; Brouwer 2006; Gaasbeek 2010; Luites 2009; Magyar 1999a; Magyar 1999b; Nakamura 2001; Papp 2009). Four of these nine studies (Adili 2002; Brouwer 2006; Gaasbeek 2010; Luites 2009) compared another type of high tibial osteotomy (aHTO) with the closing wedge HTO (CW‐HTO) and scored the major outcomes of pain, function, serious adverse events and reoperation rate (see also Table 1).
Major outcomes
Treatment failure rate, which generally implicates revision to total knee prosthesis, was not an objective in all nine trials comparing different high tibial osteotomy techniques. The relatively short maximum follow‐up time of 2.5 years is the reason for lack of this important outcome.
Pain was measured in four studies (Adili 2002; Brouwer 2006; Gaasbeek 2010; Luites 2009). In these studies, including 216 participants, another type of high tibial osteotomy (aHTO) was compared with the closing wedge high tibial osteotomy (CW‐HTO). On the basis of these four studies, we found no differences in pain between the two interventions: standard mean difference (SMD) 0.13, 95% confidence interval (CI) ‐0.55 to 0.29. Because of the numbers of available studies, the numbers of participants and limitations in the design of one study (Adili 2002), the outcome was downgraded from high quality to low quality.
Function (knee score) was measured in four studies (Adili 2002; Brouwer 2006; Gaasbeek 2010; Luites 2009). All of these studies used different outcome measures. None reported a statistically significant difference between groups, except for the non‐randomised study ( Adili 2002 ) . Because of the numbers of available studies, the numbers of participants and limitations in the design of one study (Adili 2002), the outcome was downgraded from high quality to low quality.
Health‐related quality of life between the presented osteotomy techniques was not measured.
Serious adverse events were reported in four studies (Adili 2002; Brouwer 2006; Gaasbeek 2010; Papp 2009). Deep venous thrombosis was reported in three studies (Adili 2002; Gaasbeek 2010; Papp 2009). Deep infection was reported in one study (Gaasbeek 2010). Non‐union of an opening wedge osteotomy was reported in one study (Brouwer 2006). We found a pooled estimate that was not significantly different between groups (risk ratio (RR) 2.49, 95% confidence interval (CI) 0.64 to 9.75). Because of the numbers of available studies, the numbers of participants and limitations in the design of two studies (Adili 2002; Papp 2009), the outcome was dowgraded from high quality to low quality.
Mortality was not reported in the included studies.
Reoperation rate was scored as early hardware removal caused by pain and pin track infection due to the external fixator. Four studies (Adili 2002; Brouwer 2006; Gaasbeek 2010; Magyar 1999a) including 224 participants scored this outcome. Compared with the closing wedge high tibial osteotomy group, the reoperation rate was significantly higher in another high tibial osteotomy technique group. In particular, an opening wedge high tibial osteotomy with plate and screws on the medial side of the tibia caused complaints (Brouwer 2006; Gaasbeek 2010). Pooling of study results (reoperation rate after high tibial osteotomy) for Adili 2002, Brouwer 2006, Gaasbeek 2010 and Magyar 1999a was possible, and this rate was significantly higher in participants undergoing another high tibial osteotomy technique compared with the closing wedge technique (RR 2.58, 95% CI 1.49 to 4.45). Because of the numbers of available studies, the numbers of participants and limitations in the design of two studies (Adili 2002; Magyar 1999a), the outcome was downgraded from high quality to low quality.
Minor outcomes
Performance‐based outcome, namely, accuracy of postoperative correction scored by the hip‐knee‐ankle (HKA) angle, was determined in four studies (Brouwer 2006; Gaasbeek 2010; Luites 2009; Magyar 1999b), and in one study (Adili 2002) was scored by the femoral tibial angle (FTA). Three studies (Brouwer 2006; Gaasbeek 2010; Luites 2009) including 181 participants compared the opening wedge with the closing wedge high tibial osteotomy; no difference in mean postoperative correction between the closing wedge and other types of high tibial osteotomy was found in these studies (mean difference (MD) ‐0.05 degrees, 95% CI ‐2.61 to 2.51).
Side effects after high tibial osteotomy influencing total knee arthroplasty in the future, such as decreased patellar height and changes in tibial slope, were determined in four studies (Brouwer 2005; Gaasbeek 2010; Nakamura 2001; Papp 2009). In one study, these outcomes were presented as means with a range but without a standard deviation or 95% confidence intervals; this prevented any form of statistical analysis. According to the remaining three studies (Brouwer 2005; Gaasbeek 2010; Papp 2009), patellar height did not differ significantly between other types of high tibial osteotomy and the closing wedge high tibial osteotomy (MD ‐0.08, 95% CI ‐0.24 to 0.09). However, according to the two studies comparing the closing with the opening wedge high tibial osteotomy (Brouwer 2005; Gaasbeek 2010), patellar height was significantly lower in the opening wedge groups. Furthermore, according to two studies (Brouwer 2005; Papp 2009), the mean inclination of the tibial plateau was higher (MD 4.45 degrees, 95% CI 2.21 to 6.69) in the other type of high tibial osteotomy compared with the closing wedge group. Furthermore, in one study (Gaasbeek 2010), the opening wedge high tibial osteotomy group showed statistically significant reduction in medial collateral knee laxity compared with the closing wedge high tibial osteotomy group. Finally, in Papp 2009, combined osteotomy resulted in significantly smaller changes in tibial slope angle and patellar height values when compared with the closing wedge osteotomy.
Other minor outcomes
VAS satisfaction (0 to 10 scale) was measured in one trial (Gaasbeek 2010) and was improved after high tibial osteotomy. A small difference in favour of the closing wedge technique was measured (MD ‐0.9, 95% CI ‐1.79 to ‐0.01). Joint imaging was measured in only one study (Odenbring 1992); degree of OA was measured before and one year after high tibial osteotomy. This study demonstrated no progression of OA after osteotomy within one year. VAS satisfaction was measured in one study (Gaasbeek 2010) and was improved after high tibial osteotomy. Collateral laxity on the medial side was more improved after opening wedge compared with closing wedge high tibial osteotomy (Gaasbeek 2010). Walking distance, which is an indirect measurement of pain and function, improved after both opening and closing wedge high tibial osteotomy treatments (Brouwer 2006).
Osteotomy versus unicompartmental joint replacement
Only two studies (including 119 participants) were included (Stukenborg 2001; Weidenhielm 1993) (see also Table 2).
Treatment failure scored by revision to total knee arthroplasty was reported in one study (Stukenborg 2001) and was not significantly different after five years and 10 years (RR 1.32, 95% CI 0.94 to 1.87). According to both studies, participants improved after both types of surgical treatment, and pain, knee and function scores were not statistically significantly different. The high tibial osteotomy group had a greater number of complications (nine (28%) vs two (7%)) but no serious adverse events. These outcomes were downgraded from high quality to very low quality because only one study with a limitation in design was available.
Osteotomy with different perioperative conditions
Seven included studies (Akizuki 1997; Iori 2011; Motycka 2000; Myrnerts 1980; Toksvig‐Larsen 2008; Toksvig‐Larsen 2013; Zorzi 2011) compared perioperative conditions.
Akizuki 1997 found no differences in mean Japanese Orthopaedic Association (JOA) knee score at final follow‐up between the osteotomy with abrasion group and the osteotomy alone group. The one‐year postoperative FTA angle did not differ. Adverse events were not reported.
In Iori 2011, reproducibility in achieving a mechanical axis of 182 to 186 degrees valgus was significantly higher in the navigation group, the posterior tibial slope was significantly increased in the group without navigation and operative time was significantly shorter in the osteotomy group without navigation; however no statistically significant difference in patient‐reported outcomes was measured.
Motycka 2000 found that the average incidence of thrombosis was 10.8%, and that this event occurred five times with the use of a tourniquet and one time without the use of a tourniquet, but the difference was not statistically significant. No patient‐reported outcomes were reported.
In the Myrnerts 1980 RCT, no statistically significant difference in pain reduction between the normal group and an overcorrection group was noted after 12 months. However, the overcorrection group was significantly more satisfied with the results of the operation and reported significantly better walking ability. ROM and complications were described for the whole group with percentages and without numbers. This prevented any form of statistical analysis. Adverse events such as infection and thrombosis were reported for the whole group, not separately for the individual study groups.
In Toksvig‐Larsen 2008, the insertion torque was significantly higher for standard pins. The extraction torque was significantly higher for proximal HA‐coated standard pins. No differences in pin site infections were reported. Other complications were more present in the XCaliber pin group (four vs eight). No patient‐reported outcomes were reported.
In Toksvig‐Larsen 2013, the torque for removal of pins after hemicallotasis osteotomy was not different between bisphosphonate‐coated pins and hydroxyapatite‐coated pins. No patient‐reported outcomes were reported.
In Zorzi 2011, all opening wedge high tibial osteotomies achieved bone union, and no significant difference in mean time to clinical bone union was reported. Postoperative alignment (FT angle) was not significantly different, and loss of correction occurred in one participant with bone graft and in two without bone graft. No patient‐reported outcomes were reported.
Osteotomy with different postoperative treatment
Three included studies (Harding 2011; Mammi 1993; Odenbring 1992) compared different types of postoperative treatment. In Harding 2011, healing time of the osteotomy, functional outcome (KOOS) and loss of correction post surgery were not statistically different between the bisphosphonate (zoledronic) intervention group and the placebo (sodium chloride) control group.
In Mammi 1993, the intervention group with a long plaster cast with electromagnetic field stimulation had a significantly positive effect on rate of union of the high tibial osteotomy compared with the control group with a dummy stimulator. No patient‐reported outcomes were reported. For one participant in each study group, thrombophlebitis worsened in a pulmonary embolism.
After one year of follow‐up in the Odenbring 1992 study, significantly better range of motion was noted in the hinged cast brace group compared with the cylinder plaster cast group. Neither significant differences in the other clinical results (degree of pain, Lysholm knee score) nor changes in knee alignment or progression of OA were reported. No serious adverse events were described.
In all included studies, mortality due to surgical treatment was not reported.
Discussion
The purpose of this systematic review was to assess the benefits and harms of osteotomy for OA of the knee. All studies reported on valgus high tibial osteotomy for medial compartment OA of the knee. Twenty‐one studies were included in this updated review, and no studies compared osteotomy surgery versus non‐operative treatment. Two included studies (Harding 2011; Toksvig‐Larsen 2013) examined also the effects of an osteotomy for lateral compartment osteoarthritis of the knee.
Unfortunately the risk of bias of included studies was high: The randomisation procedure frequently was not described or was insufficient. In most studies, blinding procedures were insufficient. We realise that it is difficult to blind the treatment provider in trials of surgical procedures. Blinding of the participant is difficult mainly because of postoperative scars. Moreover, use of radiological outcome measurements makes it difficult to conceal the type of surgical procedure performed. Some studies did not provide full data on outcome measures; measures of variability (such as standard deviation) were especially lacking (Magyar 1999b; Myrnerts 1980; Nakamura 2001), which makes quantitative analysis impossible. Because of the heterogeneity of the studies, pooling of results was possible only for pain, function, serious adverse events and reoperation rate after a closing wedge high tibial osteotomy compared with another high tibial osteotomy technique.
Furthermore, for most trials, inclusion and exclusion criteria were briefly presented, and most did not have enough power to discern significant between‐group differences. At last, for treatment of chronic disease such as knee OA, follow‐up of most studies was relatively short: mean 1.8 years (range 0.2 to 7.5 years).
The primary goals of a high tibial osteotomy are to reduce pain and to improve function. Furthermore, this procedure may slow down the OA process, consequently postponing knee arthroplasty, although results seem to deteriorate over time, and an overall failure rate of 24% at 10 years has been reported (Virolainen 2004). Performing total knee arthroplasty after high tibial osteotomy can be difficult because of valgus alignment, scarring of soft tissue with patella baja and bone stock/anatomical changes in the proximal tibia. Three included studies (Brouwer 2006; Gaasbeek 2010; Nakamura 2001) estimated outcomes such as patellar height, inclination angle of the tibia and condylar offset; this may influence the outcome of a total knee arthroplasty performed after a high tibial osteotomy. The opening wedge high tibial osteotomy showed a greater number of side effects for revision to future total knee arthroplasty compared with the closing wedge high tibial osteotomy (Brouwer 2005; Gaasbeek 2010). A combined osteotomy (opening and closing wedge) and high tibial osteotomy showed fewer anatomical changes of the knee postoperatively when compared with the closing wedge technique. Futhermore, computer‐assisted surgery (CAS) can be used to produce more accurate correction of the osteotomy with less of an increase in the posterior tibial slope. This enhances anterior‐posterior stability without increasing posterior contact pressure, especially in anterior cruciate ligament (ACL)‐deficient knees (Iori 2011). The high tibial osteotomy technique with an external fixator showed fewer side effects for revision to future total knee arthroplasty (Nakamura 2001) but showed a significantly higher infection rate (pin track) (Adili 2002; Magyar 1999a).
One review showed that in spite of anatomical changes after high tibial osteotomy, subsequent total knee arthroplasty did not compromise clinical outcomes when compared with primary knee arthroplasty, but additional strong evidence is needed (Raaij 2009).
Timing of surgery and selection of a particular surgical procedure, especially high tibial osteotomy versus unicompartmental knee replacement, are interesting to study. The literature shows that varus alignment causes progression of knee osteoarthritis of the medial compartment, and a correction osteotomy may affect this process (Brouwer 2007; Sharma 2010). The high tibial osteotomy is probably more applicable for the younger patient, to delay the OA process. Unicompartmental knee arthroplasty represents more of a final solution for the osteoarthritic knee, comparable with total knee arthroplasty. This is probably the reason why these two surgical treatments for unicompartmental osteoarthritis have been compared with each other less in randomised controlled trials; only two studies (Stukenborg 2001; Weidenhielm 1993) are included in this review. At the moment, the tendency is for osteotomies to be performed less, and unicompartmental arthroplasties are gaining in popularity in the orthopaedic community. However, it is remarkable that this review shows no significant differences in pain scores and functional outcomes between these different surgical treatments, even in older patients, and orthopaedic surgeons must take care to avoid losing experience in this kind of treatment. Moreover so far, only one RCT (Newman 2009) has compared total versus unicompartmental knee arthroplasty. A recently published database study showed no differences in score changes preoperatively and postoperatively between total and unicompartmental knee arthroplasty (Lyons 2012), although survival of the total knee arthroplasty seems better (Koskinen 2008).
According to several recent publications, the opening wedge high tibial osteotomy is increasing in popularity. Fixation with a fixed‐angle device (plate with locking screws) is probably very important in opening wedge high tibial osteotomy. In one study, closing wedge high tibial osteotomy achieved significantly more accurate correction with less morbidity compared with the opening wedge technique using non‐angular stable implants (Brouwer 2006). Another study using angular stable implants showed the opposite result (Luites 2009). Moreover, the opening wedge high tibial osteotomy group showed a significant reduction in medial collateral knee laxity compared with the closing wedge high tibial osteotomy group (Gaasbeek 2010). In opening wedge high tibial osteotomy, there is no absolute necessity to use autologous bone graft to accelerate bone union (Zorzi 2011). Moreover, according to Harding 2011, a single bisphosphonate infusion provided four weeks post osteotomy does not accelerate bone union.
Finally, early mobilisation of the knee joint postoperatively seems of imminent importance: Postoperative treatment with a cylinder plaster showed a significant reduction in range of motion (Odenbring 1992).
Summary of main results
Treatment failure rate, which generally implicates revision to total knee prosthesis, was not an objective in all nine trials comparing different high tibial osteotomy techniques. In all included studies comparing different techniques of HTO, follow‐up was too short for scoring of this outcome. Participants reported reduced pain after a high tibial osteotomy. On the basis of four studies comparing another type of high tibial osteotomy technique versus the closing wedge high tibial osteotomy, the mean pain score did not differ significantly between groups. Function according to knee score was measured in four studies. All of these studies showed improved knee function, but no statistically significant differences between groups were noted. Health‐related quality of life outcomes improved after high tibial osteotomy, although this outcome was not measured in the included studies comparing different osteotomy techniques. Serious adverse events were rarely reported. Deep venous thrombosis was reported in three studies. Deep infection was reported in one study. Non‐union of an opening wedge osteotomy was reported in one study. The reoperation rate were scored as early hardware removal caused by pain and pin track infection due to the external fixator. These adverse events occurred significantly more often in participants undergoing another high tibial osteotomy technique compared with the closing wedge technique. Two studies compared high tibial osteotomy versus unicompartmental knee replacement. Treatment failure, pain and function scores were not different after a mean follow‐up of 7.5 years. More adverse events were described for the osteotomy group compared with the unicompartment knee replacement group. No studies compared osteotomy versus non‐operative treatment.
Overall completeness and applicability of evidence
The only robust conclusion regarding the objective of this review is that valgus high tibial osteotomy improves knee function and reduces pain. However, this conclusion is based on within‐group comparisons. Other unconditional statements cannot be made. The main reasons for this are the limited numbers and heterogeneity of included studies with different types of interventions and outcome measures. Furthermore, the methodological quality of the included studies was moderate, and risk of bias for most items was high. Finally, in most studies, follow‐up time was too short for treatment of a chronic disease such as knee osteoarthritis.
Quality of the evidence
Quality of the evidence for most outcomes comparing different osteotomy techniques was downgraded to low because of the numbers of available studies, the numbers of participants and limitations in design. According to four studies (Adili 2002; Brouwer 2006; Gaasbeek 2010; Luites 2009) comparing other types of high tibial osteotomy versus closing wedge high tibial osteotomy, the conclusion is that low‐quality evidence shows no difference in pain after closing wedge high tibial osteotomy and other types of osteotomy. Low‐quality evidence shows no difference in knee scores between different osteotomy techniques after one to two years of follow‐up. Furthermore, low‐quality evidence shows a higher reoperation rate after other types of high tibial osteotomy compared with the closing wedge technique (Adili 2002; Brouwer 2006; Gaasbeek 2010; Magyar 1999a). Four studies (Brouwer 2006; Gaasbeek 2010; Nakamura 2001; Papp 2009) described side effects after high tibial osteotomy influencing total knee arthroplasty in the future, such as changes in tibial slope and decreased patellar height. Acccording to two of these studies (Brouwer 2005; Gaasbeek 2010), low‐quality evidence shows greater patellar descent after opening wedge osteotomy compared with closing wedge osteotomy, and very low‐quality evidence shows less patellar descent with hemicallotasis opening wedge osteotomy compared with dome osteotomy (Nakamura 2001). According to three studies (Brouwer 2006; Gaasbeek 2010; Luites 2009) determining postoperative alignment, moderate‐quality evidence shows no differences between the closing and the opening wedge technique.
According to one study, very low‐quality evidence shows that opening wedge high tibial osteotomy with computer‐assisted navigation will result in more accurate correction and fewer side effects, such as increased tibial slope (Iori 2011).
Moreover, very low‐quality evidence shows more optimal one‐year postoperative correction after hemicallotasis osteotomy compared with closing wedge high tibial osteotomy (Magyar 1999a). In terms of medial collateral knee laxity, very low‐quality evidence indicates that opening wedge high tibial osteotomy shows a significant reduction in medial collateral knee laxity compared with closing high tibial osteotomy (Gaasbeek 2010).
According to one study (Zorzi 2011), very low‐quality evidence shows no additive effect of autologous bone graft in time to bone union for opening wedge high tibial osteotomy (Zorzi 2011). According to another study (Harding 2011), very low‐quality evidence shows no additive effect of bisphosphonate infusion post high tibial osteotomy in time to bone union.
When the closing wedge high tibial osteotomy is compared with unicompartmental knee arthroplasty, very low‐quality evidence shows no statistically significant differences in pain (Stukenborg 2001) and no differences in gait analysis between these two surgical treatments for medial compartmental knee osteoarthritis (Weidenhielm 1993). However, very low‐quality evidence indicates that high tibial osteotomy causes a greater number of complications compared with unicompartmental knee arthroplasty (Stukenborg 2001).
For differences in perioperative conditions, very low‐quality evidence shows no supplementary postoperative effects of abrasion arthroplasty during high tibial osteotomy (Akizuki 1997); very low‐quality evidence reveals no higher incidence of thrombosis with tourniquet during high tibial osteotomy (Motycka 2000); low‐quality evidence shows that electromagnetic field stimulation leads to high tibial osteotomy healing (Mammi 1993); and very low‐quality evidence shows that use of a hinged cast brace after closing wedge high tibial osteotomy results in better range of motion compared with use of a postoperative plaster cast (Odenbring 1992). Very low‐quality evidence indicates that computer‐assisted navigation in open wedge osteotomy produces a more accurate correction (Iori 2011). Finally, very low‐quality evidence shows that high tibial osteotomy with overcorrection results in better walking ability and greater patient satisfaction than are seen with normal correction (Myrnerts 1980).
Potential biases in the review process
The strength of this review is that it has been updated twice since 2005 with a systematic, comprehensive search. Limitations are that controlled clinical trials with high risk of bias have been included. Moreover, osteotomy studies performed under different perioperative conditions have been included, which leads to heterogeneity and makes pooling of most of the results impossible.
Agreements and disagreements with other studies or reviews
No disagreements with recently published systematic reviews and meta‐analyses (Smith 2011; Spahn 2011) concerning osteotomy for knee osteoarthritis have been reported.
Authors' conclusions
Implications for practice.
Based on the results of 21 studies included in this review, we conclude that valgus high tibial osteotomy improves knee function and reduces pain. However, this conclusion is based on within‐group comparisons, not on non‐operative controls. It is unclear which technique we have to use because few statistically significant differences have been reported between different high tibial osteotomy techniques. Low‐quality evidence shows no differences in the major outcomes of pain and function between closing wedge high tibial osteotomy and other types of osteotomy after one to two years of follow‐up. Furthermore, low‐quality evidence reveals a higher reoperation rate after other types of high tibial osteotomy compared with the closing wedge technique. The latest studies show that we probably have to use a fixed‐angle device (plate with locking screws) for fixation of the opening wedge high tibial osteotomy (this is associated with maintaining the correction).
When the closing wedge high tibial osteotomy is compared with the unicompartmental knee arthroplasty, very low‐quality evidence shows no statistically significant differences between these two surgical treatments for medial compartmental knee osteoarthritis.
A large number of complications after osteotomy were reported, and no comparative evidence shows whether an osteotomy is more effective than non‐operative therapy. However, significant postoperative improvement has been seen following osteotomy.
Implications for research.
Large, high‐quality studies are needed, with a focus on appropriate allocation concealment, blinding and adequate data presentation, including mean and standard deviation or 95% confidence intervals with risk of bias reduction analyses. The design and reports of future trials should comply with the CONSORT statement (Ross 1996). A single common international knee score should be agreed upon to make pooling of data possible.
Future research should examine the effects of treatments not only in trials comparing various interventions with each other, but also in more explanatory trials comparing interventions with conservative treatment.
Future research should focus on treating unicompartmental knee osteoarthritis. A broad variety of treatments are available; most are costly, and data on their benefits are not available.
Evaluation of study groups with longer follow‐up periods is necessary for treatment of a chronic disease such as knee osteoarthritis.
The literature shows that varus malalignment is a risk factor for osteoarthritis progression in the medial compartment of the knee. Correction osteotomy may affect this process. Future trials should measure delays in the osteoarthritis process and should determine the mechanisms.
Timing of surgery and choice of a particular surgical procedure, especially high tibial osteotomy versus unicompartmental knee replacement, are interesting to study.
We conclude that performing randomised studies of high methodological quality to examine the benefit of osteotomy compared with other frequently performed treatments for knee osteoarthritis is possible and necessary if high‐quality evidence is to be obtained.
What's new
| Date | Event | Description |
|---|---|---|
| 5 November 2014 | New citation required but conclusions have not changed | New review author added and 8 new studies included in this update New methods include different grading of evidence synthesis and risk of bias assessment, as well as changes in major outcomes as per the CMSG Editorial base |
| 5 November 2014 | New search has been performed | New search with 8 new studies |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 1, 2005
| Date | Event | Description |
|---|---|---|
| 1 May 2007 | New search has been performed | Substantive amendment. See published notes |
Notes
This is the second update of the original review, which was published in 2005, Issue 1. We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and EMBASE for controlled trials in the first update until May 2007, and in the second update until November 2013. As a result of the search strategy, two new studies and one longer follow‐up study were included in the first update, and eight new studies were included in the second update of this review. The two new studies in the first update compared two high tibial osteotomy techniques: the opening and the closing wedge during follow‐up of one year. Functional outcome scores were not different, but the closing wedge achieved a more accurate correction with less morbidity. The longer follow‐up study presented five‐year results when high tibial osteotomy was compared with unicompartmental knee arthroplasty. Both groups were improved after five years of follow‐up, but no differences were noted between the two groups. In this update, the conclusions of the original review have not changed.
Three studies included in the second update compared two types of high tibial osteotomy. Two studies compared the closing and the opening wedge high tibial osteotomy, and one study compared the closing wedge high tibial osteotomy versus a combined high tibial osteotomy, including an opening and a closing wedge. Functional outcome scores and pain scores were not different. In one study, no difference in achieved postoperative correction angles was reported, but a significant reduction in medial collateral knee laxity was described after opening wedge high tibial osteotomy. In another included study, which compared opening and closing wedge high tibial osteotomies, the opening wedge high tibial osteotomy showed significantly more accurate correction. After a combined (opening and closing wedge) high tibial osteotomy, significantly smaller changes in patellar height and tibial slope were noted. Another five included studies compared different types of pin fixation in the hemicallotasis high tibial osteotomy technique, the healing effects of a single infusion of bisphosphonate (zoledronic acid) four weeks post hemicallotasis osteotomy versus placebo, open‐wedge high tibial osteotomy with and without navigation and opening wedge high tibial osteotomy with and without filling of the opening wedge with autologous iliac bone graft.
Acknowledgements
The review authors thank Jessie McGowan from the Institute of Population Health University of Ottawa (Canada) for devising the search strategy, and Maria Judd and Lara Maxwell of the Cochrane Musculoskeletal Group for their support.
For the second update, the review authors thank Rachel Marshall, Editor of the Cochrane Group, for her support.
Appendices
Appendix 1. Appendix: Search strategies and results summary
| Database and coverage | Search date | Number of references retrieved | Number of references after de‐duplication |
| Ovid MEDLINE(R) 1946‐5 November 2013 | 5 November 2013 | 324 | 248 |
| EMBASE Classic + EMBASE 1947‐5 November 2013 | 5 November 2013 | 152 | 86 |
|
The Cochrane Library
October 2013, Issue 10 of 12
CDSR DARE Economic evaluations Health technology assessments CENTRAL (trials) |
5 November 2013 | 22 9 1 2 50 |
22 9 1 2 50 |
| Clinicaltrials.gov | 5 November 2013 | 73 | 73 |
| Totals | 633 | 491 |
Search strategies for all databases
Database: Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations and Ovid MEDLINE(R) <1946 to Present>
Search strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp Osteotomy/ (23621)
2 Osteotomy, Le Fort/ (1226)
3 gonarthrosis$.tw / (60)
4 osteotom$.tw. (20660)
5 or/1‐4 (30327)
6 exp osteoarthritis/ (38807)
7 osteoarthr$.tw. (36720)
8 (degenerative adj2 arthritis).tw. (1077)
9 or/6‐8 (52385)
10 randomized controlled trial.pt. (332056)
11 controlled clinical trial.pt. (84622)
12 randomized.ab. (247363)
13 placebo.ab. (137714)
14 drug therapy.fs. (1549552)
15 randomly.ab. (181327)
16 trial.ab. (256643)
17 groups.ab. (1182024)
18 or/10‐17 (2972545)
19 exp animals/ not humans.sh. (3752923)
20 18 not 19 (2538516)
21 5 and 9 and 20 (280)
Database: EMBASE Classic + EMBASE <1947 to 5 November 2013>
Search strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 exp osteotomy/ (32343)
2 osteotom$.tw. or gonarthrosis$.tw (27059)
3 1 or 2 (38166)
4 exp osteoarthritis/ (77468)
5 osteoarthr$.tw. (50633)
6 (degenerative adj2 arthritis).tw. (1567)
7 or/4‐6 (89892)
8 random$.tw. (761285)
9 factorial$.tw. (20041)
10 crossover$.tw. (45103)
11 cross over.tw. (20597)
12 cross‐over.tw. (20597)
13 placebo$.tw. (186288)
14 (doubl$ adj blind$).tw. (139005)
15 (singl$ adj blind$).tw. (12686)
16 assign$.tw. (212872)
17 allocat$.tw. (71540)
18 volunteer$.tw. (168996)
19 crossover procedure/ (34713)
20 double blind procedure/ (114378)
21 randomized controlled trial/ (327555)
22 single blind procedure/ (16135)
23 or/8‐22 (1272819)
24 3 and 7 and 23 (132)
The Cochrane Library: Search name: Osteotomy for OA
Save date: 2012‐07‐17 12:47:33.64
ID Search
#1 MeSH descriptor Osteoarthritis explode all trees
#2 osteoarthr*:ti,ab OR gonarthrosis*:ti,ab
#3 degenerative Near/2 arthritis:ti,ab
#4 osteotomy
#5 MeSH descriptor Osteotomy explode all trees
#6 osteotom*
#7 (#1 OR #2 OR #3)
#8 (#4 OR #5 OR #6)
#9 (#7 AND #8)
Clinicaltrials.gov Search date: 5 November 2013
Condition = osteoarthritis or arthritis
Intervention = osteotomy
Data and analyses
Comparison 1. Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 4 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.55, 0.29] |
| 2 Stiffness | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 WOMAC stiffness | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐1.20 [‐2.63, 0.23] |
| 3 Function | 4 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.57, 0.36] |
| 3.1 WOMAC function | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.67, ‐0.20] |
| 3.2 Knee Society Score | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.71, 0.40] |
| 3.3 Hospital for Special Surgery | 1 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.29, 0.53] |
| 3.4 Lysholm | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [‐0.24, 0.98] |
| 4 Walking distance (km) | 1 | 92 | Mean Difference (IV, Random, 95% CI) | 0.70 [‐0.95, 2.35] |
| 5 Valgus angle | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 HKA angle | 3 | 184 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.77, 0.85] |
| 5.2 FTA | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.32, 0.11] |
| 6 Participant satisfaction | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 VAS satisfaction | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.79, ‐0.01] |
| 7 Willingness to undergo surgery again | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [0.87, 4.31] |
| 8 Serious adverse events | 4 | 265 | Risk Difference (M‐H, Random, 95% CI) | 0.03 [‐0.03, 0.09] |
| 9 Reoperation rate | 4 | 224 | Risk Difference (M‐H, Random, 95% CI) | 0.19 [‐0.08, 0.47] |
| 10 Patellar height (Insall‐Salvati ratio) | 3 | 191 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.24, 0.09] |
| 11 Inclination of the tibial plateau (degrees) | 2 | 141 | Mean Difference (IV, Random, 95% CI) | 4.45 [2.21, 6.69] |
| 12 Medial laxity | 1 | 50 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐1.11, 1.31] |
| 13 Lateral laxity | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.78, 0.38] |
1.1. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 1 Pain.
1.2. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 2 Stiffness.
1.3. Analysis.
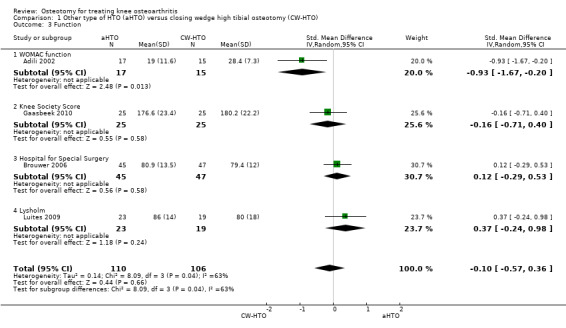
Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 3 Function.
1.4. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 4 Walking distance (km).
1.5. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 5 Valgus angle.
1.6. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 6 Participant satisfaction.
1.7. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 7 Willingness to undergo surgery again.
1.8. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 8 Serious adverse events.
1.9. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 9 Reoperation rate.
1.10. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 10 Patellar height (Insall‐Salvati ratio).
1.11. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 11 Inclination of the tibial plateau (degrees).
1.12. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 12 Medial laxity.
1.13. Analysis.

Comparison 1 Other type of HTO (aHTO) versus closing wedge high tibial osteotomy (CW‐HTO), Outcome 13 Lateral laxity.
Comparison 2. Closing wedge high tibial osteotomy (HTO) versus UKA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Survival (revision) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse events | 1 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Participant opinion: improvement at 5 years | 1 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Gait analysis: free walking speed at 5 years | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Gait analysis: step frequency at 5 years | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
2.1. Analysis.

Comparison 2 Closing wedge high tibial osteotomy (HTO) versus UKA, Outcome 1 Survival (revision).
2.2. Analysis.

Comparison 2 Closing wedge high tibial osteotomy (HTO) versus UKA, Outcome 2 Adverse events.
2.3. Analysis.

Comparison 2 Closing wedge high tibial osteotomy (HTO) versus UKA, Outcome 3 Participant opinion: improvement at 5 years.
2.4. Analysis.

Comparison 2 Closing wedge high tibial osteotomy (HTO) versus UKA, Outcome 4 Gait analysis: free walking speed at 5 years.
2.5. Analysis.

Comparison 2 Closing wedge high tibial osteotomy (HTO) versus UKA, Outcome 5 Gait analysis: step frequency at 5 years.
Comparison 3. Differences in perioperative conditions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 JOA score | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Valgus angle (FTA) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Complication (phlebography) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Time (weeks) to bony union | 1 | 46 | Mean Difference (IV, Random, 95% CI) | ‐1.30 [‐1.65, ‐0.95] |
| 5 KSS (American) | 1 | 24 | Mean Difference (IV, Random, 95% CI) | 5.70 [0.30, 11.10] |
| 6 Cincinnati Rating System Questionnaire | 1 | 24 | Mean Difference (IV, Random, 95% CI) | 16.90 [7.92, 25.88] |
3.1. Analysis.

Comparison 3 Differences in perioperative conditions, Outcome 1 JOA score.
3.2. Analysis.

Comparison 3 Differences in perioperative conditions, Outcome 2 Valgus angle (FTA).
3.3. Analysis.

Comparison 3 Differences in perioperative conditions, Outcome 3 Complication (phlebography).
3.4. Analysis.
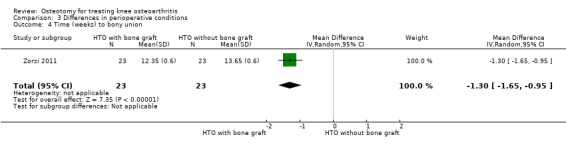
Comparison 3 Differences in perioperative conditions, Outcome 4 Time (weeks) to bony union.
3.5. Analysis.
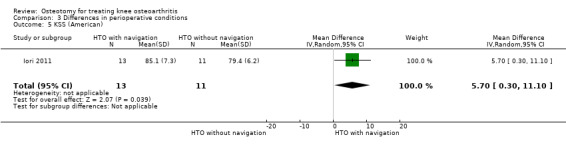
Comparison 3 Differences in perioperative conditions, Outcome 5 KSS (American).
3.6. Analysis.

Comparison 3 Differences in perioperative conditions, Outcome 6 Cincinnati Rating System Questionnaire.
Comparison 4. Differences in postoperative treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Less than 50% consolidation | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 More than 50% consolidation | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Complications | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Range of motion | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Pain‐free walking distance | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Pain at rest | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 Degree of osteoarthritis | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 Valgus angle (HKA angle) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
4.1. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 1 Less than 50% consolidation.
4.2. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 2 More than 50% consolidation.
4.3. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 3 Complications.
4.4. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 4 Range of motion.
4.5. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 5 Pain‐free walking distance.
4.6. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 6 Pain at rest.
4.7. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 7 Degree of osteoarthritis.
4.8. Analysis.

Comparison 4 Differences in postoperative treatment, Outcome 8 Valgus angle (HKA angle).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adili 2002.
| Methods | CCT; no randomisation Not blinded | |
| Participants | Varus alignment and symptomatic medial compartment osteoarthritis | |
| Interventions | I: high tibial osteotomy using an Ilizarov apparatus (n = 15) C: closed wedge high tibial osteotomy (n = 15) Follow‐up: I = 25.4 months C = 30.9 months No dropouts mentioned | |
| Outcomes | WOMAC scores FTA Complications | |
| Notes | Study funding source and any declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Depends on treatment provider |
| Allocation concealment (selection bias) | High risk | Matched compared analysis |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | High risk | Follow‐up period was different |
Akizuki 1997.
| Methods | CCT; no randomisation: Participants were assigned to both groups in turn Not blinded | |
| Participants | Medial compartment osteoarthritis | |
| Interventions | I: high tibial osteotomy with arthroscopic abrasion (n = 45)
C: high tibial osteotomy alone (n = 34)
Follow‐up:
I = 4.8 years
C = 3.5 years No dropouts |
|
| Outcomes | JOA knee score FTA | |
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were assigned to group A or B in turn" |
| Allocation concealment (selection bias) | High risk | Quote: "Patients were assigned to group A or B in turn" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Blinding procedure is not described" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | High risk | Follow‐up period and numbers of participants were different |
Brouwer 2005.
| Methods | RCT; computer blocked randomisation Not blinded | |
| Participants | Osteoarthritis of the medial compartment and varus malalignment | |
| Interventions | I: opening wedge high tibial osteotomy (n = 26)
C: closing wedge high tibial osteotomy (n = 24)
Follow‐up: 1 year C: 1 dropout |
|
| Outcomes | Patellar height Inclination of the tibial plateau | |
| Notes | Quote: "No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Consecutive patients were randomised according to a computer‐generated procedure" |
| Allocation concealment (selection bias) | Low risk | Quote: "using sealed envelopes" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not possible |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Study protocol available |
| Other bias | Low risk | Does not apply |
Brouwer 2006.
| Methods | RCT; computer blocked randomisation Not blinded | |
| Participants | Osteoarthritis of the medial compartment with medial joint pain and varus malalignment | |
| Interventions | I: opening wedge high tibial osteotomy (n = 45)
C: closing wedge high tibial osteotomy (n = 47)
Follow‐up: 1 year I: 1 dropout C: 1 dropout |
|
| Outcomes | Accuracy of postoperative correction VAS pain score HSS knee score Walking distance Complications | |
| Notes | Quote: "No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomised by a computer generated procedure in blocks of 16" |
| Allocation concealment (selection bias) | Low risk | Quote: "Sealed envelopes contained the group assignment" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Study protocol available |
| Other bias | Low risk | No issue |
Gaasbeek 2010.
| Methods | RCT; sealed envelope procedure Not blinded |
|
| Participants | Active patients between 18 and 70 years of age, suffering from medial osteoarthritis of the knee with a hip‐knee‐ankle (HKA) varus alignment | |
| Interventions | I: opening wedge high tibial osteotomy (n = 25)
C: closing wedge high tibial osteotomy (n = 25)
Follow‐up: 1 year No dropout |
|
| Outcomes | Accuracy of postoperative correction Medial and collateral laxity WOMAC Modified Knee Society Score (KSS) VAS knee pain VAS satisfaction Patellar height according to Caton Index (CI) Surgery time Hospital stay |
|
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised for their treatment" |
| Allocation concealment (selection bias) | Low risk | Quote: "according to a sealed envelope procedure" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned |
| Selective reporting (reporting bias) | Low risk | Study protocol available |
| Other bias | Low risk | No issue |
Harding 2011.
| Methods | RCT; randomisation using closed envelopes Double‐blinded |
|
| Participants | Age between 35 and 65 years and osteoarthritis or deformity if knee requires surgery | |
| Interventions | I: single infusion of zoledronic acid 4 weeks post hemicallotasis osteotomy (n = 25) C: sodium chloride infusion 4 weeks post hemicallotasis osteotomy (n = 21) |
|
| Outcomes | Time to bone healing KOOS Evaluation of densitometry Evaluation of retention of surgically achieved correction Safety/Side effects |
|
| Notes | Quote: "No competing interests declared. The study was carried out independently of the manufacturers of the pharmaceuticals used" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomizations was performed by one of the authors" |
| Allocation concealment (selection bias) | Low risk | Quote: "using closed envelopes" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "prepared by the unblinded nurse" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "the patient[s] were blinded regarding the type of infusion" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "evaluation of healing, blinded, on radiograph and ultrasound was done" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | CONSORT flow diagram |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | High risk | The intervention group included 4 smokers vs 7 in the control group |
Iori 2011.
| Methods | RCT; randomisation and allocation procedures not described | |
| Participants |
|
|
| Interventions | I: open wedge HTO with a navigation system (n = 13; 14 knees) C: open wedge HTO without navigation system (n = 11; 13 knees) |
|
| Outcomes | Alignment (HKA angle), mechanical medial proximal tibial angle (mMPTA), mechanical lateral distal femoral angle (mLDFA), tibial slope (Brazier methods), patellar height (Insall‐Salvati Index), inferior limb length, American KSS, Modified Cincinnati Rating System Questionnaire, VAS (pain: 0 = unbearable pain and 10 = no pain) | |
| Notes | Quote: "The authors declare that they have no conflict of interest with this study" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All the radiological evaluations were performed by a single blinded expert radiologist" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned |
| Selective reporting (reporting bias) | Low risk | All outcomes presented |
| Other bias | Low risk | No issue |
Luites 2009.
| Methods | RCT; computer blocked randomisation Not blinded | |
| Participants | Osteoarthritis of the medial compartment with a varus mechanical axis of less than 12 degrees and a body mass index (BMI) < 30 kg/m2 | |
| Interventions | I: opening wedge high tibial osteotomy (n = 19) C: closing wedge high tibial osteotomy (n = 23) Follow‐up: 12 months and 24 months | |
| Outcomes | Stability of HTO (measured with RSA) Alignment Lysholm score VAS |
|
| Notes | Quote: "No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "using a computer‐generated random allocation to both groups" |
| Allocation concealment (selection bias) | Low risk | Quote: "in blocks of four per participating surgeon" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned |
| Selective reporting (reporting bias) | Low risk | All outcomes presented |
| Other bias | High risk | In the opening wedge high tibial osteotomy group, 22 participants were allocated to this intervention, but 23 received this intervention and were also included in the analysis |
Magyar 1999a.
| Methods | RCT; randomisation procedure not described Follow‐up examination blinded | |
| Participants | Medial gonarthrosis and younger active patients | |
| Interventions | I: hemicallotasis open wedge osteotomy (HCO/n = 24)
C: closing wedge high tibial osteotomy (n = 22)
Follow‐up: 2 years Two dropouts for the NHP assessment: 1 in each group |
|
| Outcomes | VAS score ROM HSS knee score Lysholm score Wallgren‐Tegner activity score NHP score HKA angle Hospital stay Complications | |
| Notes | Only pre‐ and post analysis Quote: "No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We randomly allocated 46 patients" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Before examination, the relevant leg was covered to conceal the operative technique" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 2 dropouts for the NHP assessment: 1 in each group |
| Selective reporting (reporting bias) | High risk | Only subgroup scores of the NHP given No study protocol available |
| Other bias | High risk | In our opinion, the ROM of the HCO group on page 446 is not correct |
Magyar 1999b.
| Methods | RCT; randomisation using numbered closed envelopes Not blinded | |
| Participants | Medial gonarthrosis grade I to III | |
| Interventions | I: HCO (n = 18)
C: closing wedge high tibial osteotomy (n = 15)
Follow‐up: 1 year No dropout |
|
| Outcomes | Radiostereometry (RSA) HKA angle | |
| Notes | RSA measurement is not an outcome measurement in our protocol, but high tibial osteotomy was associated with greater translation Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The randomisation was made before the study started" |
| Allocation concealment (selection bias) | Low risk | Quote: "The results were put in closed and numbered envelopes" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Low risk | No issue |
Mammi 1993.
| Methods | RCT; randomisation according to order of admission to the hospital Double‐blind | |
| Participants | Maximum age of 80 years, good health, requiring tibial reduction osteotomy | |
| Interventions | I: high tibial osteotomy with electrical stimulation (n = 18)
C: high tibial osteotomy without electrical stimulation (n = 19)
Follow‐up: 60 days I: 2 dropouts C: 1 dropout |
|
| Outcomes | Rate of union (score 1t/m4) | |
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A random seed number was entered into the computer to generate a list that assigned equal numbers of active and control stimulators (block of four, two active and two control units)" |
| Allocation concealment (selection bias) | High risk | Quote: "The patients were placed either in a control or stimulated group according to their order of admission to the hospital" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Control (dummy) units did not differ from active stimulators, either in shape, weight, or by their operation" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Control (dummy) units did not differ from active stimulators, either in shape, weight, or by their operation" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The roentgenographs were independently evaluated on a double‐blind basis by four orthopedists" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No study protocol available |
| Other bias | Low risk | No issue |
Motycka 2000.
| Methods | RCT; randomisation procedure not described | |
| Participants | Varus osteoarthritis | |
| Interventions | I: high tibial osteotomy with a tourniquet (n = 40)
C: high tibial osteotomy without a tourniquet (n = 40)
Follow‐up: 9 weeks I: 3 dropouts C: 15 dropouts |
|
| Outcomes | D‐Dimer test and phlebography | |
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "In a prospective randomised study" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding procedures not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding procedures not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding procedures not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | High risk | In the intervention group, 3 dropouts; in the control group, 15 dropouts |
Myrnerts 1980.
| Methods | RCT; randomisation procedure not clear Not blinded | |
| Participants | Varus alignment | |
| Interventions | I: high tibial osteotomy without overcorrection (n = 40)
C: high tibial osteotomy with 5 degrees overcorrection (n = 37)
Follow‐up: 1 year No dropout mentioned |
|
| Outcomes | Pain on weight bearing Participant's opinion HKA angle Complications | |
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were allocated at random to one of two groups" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding procedures not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding procedures not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study reports percentages, no numbers No dropouts mentioned |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Low risk | No issue |
Nakamura 2001.
| Methods | RCT; randomisation procedure not described | |
| Participants | Medial osteoarthritis of the knee | |
| Interventions | I: HCO (n = 23)
C: dome osteotomy (DMO; n = 23)
Follow‐up: 12 months No dropout |
|
| Outcomes | FTA Patellar height Inclination angle of tibial plateau Tibial condylar offset | |
| Notes | Quote: "No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "They were randomly allocated to either a DMO or [an] HCO" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Low risk | No issue |
Odenbring 1992.
| Methods | RCT; "randomisation code was opened" Not blinded | |
| Participants | Stages I to III medial gonarthrosis | |
| Interventions | I: high tibial osteotomy with a hinged cast brace postoperative (n = 14) C: high tibial osteotomy with a cylinder plaster cast postoperative (n = 17) Follow‐up: 1 year | |
| Outcomes | ROM Pain‐free walking distance Pain at rest Degree of OA HKA angle Lysholm score Complications | |
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomised into a brace group and a plaster group" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After wound closure, the randomisation code was opened" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding procedure not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | One participant in the brace group excluded and not included in the analysis |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | High risk | One participant with a complication was excluded |
Papp 2009.
| Methods | RCT; computer blocked randomisation Not blinded | |
| Participants | Pain on the medial side of the knee, varus malalignment involving the tibia, narrowing of the medial joint space that did not exceed 50% on a standing anteroposterior radiograph | |
| Interventions | I: combined osteotomy (CO), which is a combination of an opening and a closing wedge high tibial osteotomy (n = 45) C: closing wedge high tibial osteotomy (CWO; n = 46) Follow‐up: 1 year I: 4 dropouts (1 participant excluded for analysis and 3 lost to follow‐up) C: 5 dropouts (2 participants excluded for analysis and 3 lost to follow‐up) |
|
| Outcomes | Patellar height according to length of patellar tendon (LPT) Inclination of the tibial plateau/posterior tibial slope (TS) |
|
| Notes | Quote: "The authors report no conflict of interest" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "One was randomly assigned to CWO, the other to CO" |
| Allocation concealment (selection bias) | Low risk | Quote: "Pairs were created, and by use of sequentially numbered and sealed envelopes" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote "Preoperative and postoperative LPT and TS were measured by an experienced radiologist who, to avoid any potential bias, was blinded to the surgical technique" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | Postoperative alignment scores (FTA) not published; no study protocol available |
| Other bias | High risk | Three participants were excluded for analysis, and 6 were lost to follow‐up |
Stukenborg 2001.
| Methods | RCT; participants were randomly assigned by computer Not blinded | |
| Participants | Medial unicompartmental OA, varus < 10 degrees, flexion contracture < 15 degrees, age > 60 years, ligament instability < grade II | |
| Interventions | I: high tibial osteotomy (n = 32)
C: unicompartmental knee arthroplasty (UKA; n = 28)
Follow‐up: 7.5 years No dropouts |
|
| Outcomes | Knee score Functional score ROM HKA angle Survivorship Complications | |
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were computer‐randomised" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts mentioned. Quote: "all patients could be assessed" |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Low risk | No issue |
Toksvig‐Larsen 2008.
| Methods | RCT; sealed numbered envelopes | |
| Participants | Participants treated by hemicallotasis osteotomy technique for knee osteoarthritis | |
| Interventions | Two types of pins compared in hemicallotasis osteotomy | |
| Outcomes | Torque forces for insertion and extraction | |
| Notes | Quote: "No competing interests declared" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Quote: "Sealed numbered envelopes were used for the randomisation process" |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | High risk | Three participants were excluded from the analysis |
Toksvig‐Larsen 2013.
| Methods | RCT; sealed numbered envelopes | |
| Participants | Patients treated by hemicallotasis osteotomy technique for medial or lateral osteoarthritis of the knee | |
| Interventions | Two types of pins were compared in hemicallotasis osteotomy | |
| Outcomes | Removal torque of the pins | |
| Notes | Second study author reports conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "shuffling sealed envelopes in blocks" |
| Allocation concealment (selection bias) | Low risk | Quote: "numbered, sealed envelopes" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "The surgeon and all clinical staff were blinding regarding treatment" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The surgeon and all clinical staff were blinding regarding treatment" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not possible to discern differences between pins |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Study protocol available |
| Other bias | Unclear risk | The second study author reports conflicts of interest |
Weidenhielm 1993.
| Methods | RCT; randomisation procedure not described Not blinded | |
| Participants | Medial OA grade I to II, 55 to 70 years old | |
| Interventions | I: high tibial osteotomy (n = 23)
C: UKA (n = 36)
Follow‐up: 1 year I: high tibial osteotomy (n = 18) C: UKA (n = 22) Follow‐up: 5 years Dropouts: After 1‐year follow‐up: 41 After 5‐ year follow‐up: 60 |
|
| Outcomes | BOA knee score Pain during walking Passive ROM HKA angle Gait analysis Survivorship Complications | |
| Notes | One‐year and 5‐year results reported in 2 different publications
Original study started with 100 participants, including 50 in each group
After 1‐year follow‐up, 59 participants were left. In the first publications, the cause of this large number of losses has not been described
In the second publication, including 5‐year results, only 40 participants are left, because in the 5‐year analysis, "only patients with strictly unilateral osteoarthritis were included" Study funding source and declarations of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Before surgery, 50 patients were randomly selected to unicompartmental knee replacement and 50 to high tibial osteotomy" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Relevant leg not covered to conceal the operative technique |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | For 5‐year follow‐up, only participants with strictly unilateral osteoarthritis were analysed |
| Other bias | High risk | Dropouts: after 1‐year follow‐up: 41; after 5‐year follow‐up: 60 |
Zorzi 2011.
| Methods | RCT; randomisation procedure not described Blinded |
|
| Participants | Varus misalignment of the limb that could be corrected by a plate with at least a 12.5‐mm spacer, associated with osteoarthritis and pain limited to the medial side that did not improve with conservative management | |
| Interventions | I: medial opening wedge HTO with the gap filled with autologous iliac bone graft (n = 23) C: medial opening wedge HTO with the gap unfilled (n = 23) Follow‐up: 23.6 months (range 12 to 36 months) |
|
| Outcomes | Time to bone union Alignment (FTA) immediately postoperatively and loss of correction after 6 months |
|
| Notes | Study funding source and declarations of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Bone graft was harvested from the opposite iliac crest in all patients" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Time to bone union was assessed by two blinded investigators" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All patients completed 1‐year minimal follow‐up" |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | High risk | 3/23 smokers in the intervention group vs 8/23 smokers in the control group (p=0.084) |
Legend: BOA = British Orthopaedic Association. C = closed wedge high tibial osteotomy. CCT = controlled clinical trial. CI = Caton Index. CO = combined osteotomy. CWO = closing wedge high tibial osteotomy. DMO = dome osteotomy. FTA = femoral tibial angle. HCO = hemicallotasis osteotomy. HKA = hip‐knee‐ankle. HSS = Hospital for Special Surgery. HTO = high tibial osteotomy. I = high tibial osteotomy using an Ilizarov apparatus. JOA = Japanese Orthopaedic Association. KOOS = Knee Injury and Osteoarthritis Outcome Score. KSS = American Knee Society Scale. LPT = length of patellar tendon. mLDFA = mechanical lateral distal femoral angle. mMPTA = mechanical medial proximal tibial angle. NHP: Nottingham Health Profile. OA: osteoarthritis. RCT: randomised controlled trial. ROM = range of motion. RSA = radiostereometry. TS = tibial slope. UKA = unicompartmental knee arthroplasty. VAS = visual analogue scale. WOMAC = Western Ontario and McMaster Universities Arthritis Index.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bae 2009 | Control group retrospectively reviewed |
| Bekerom 2008 | Prospective cohort study; no baseline measurements |
| Cho 2013 | Design of the study |
| Dallari 2012 | Excluded because participants with traumatic cartilage lesions were included |
| Gouin 2010 | Participants with lateral instability or post‐traumatic genu varum were included; the study was discontinued after 40 inclusions because of undesirable events in the intervention group (loss of correction) |
| Maffulli 2013 | Design of the study |
| Odenbring 1992b | Design of the study |
| Pape 2013 | Design of the study and primary outcome |
| Yim 2013 | Design of the study |
Differences between protocol and review
In the protocol, outcome measures were based on core OMERACT measures for hip, knee and hand osteoarthritis, as suggested by the Third Conference on Outcome Measures in Rheumatology (OMERACT). For this update, these outcome measures have been changed to outcomes recommended by the Cochrane Musculoskeletal Group editors.
Contributions of authors
Reinoud Brouwer (RB) proposed the review. RB, Sita Bierma‐Zeinstra (SB) and Arianne Verhagen (AV) wrote the protocol. Jessie McGowan (JM) developed the search strategy. RB, Tijs Jakma (TS) and Tom van Raaij (TR) selected studies upon review of the abstracts. RB, TJ and TM performed final selection after reading the full articles. RB, SB and Jan Verhaar (JV) assessed the methodological quality of studies. RB, TJ and AV performed data extraction. With contributions from all review authors, RB wrote the original review.
In the first and second updates, RB and TR selected studies upon review of the abstracts. RB and TR performed the final selection after reading the full article. In the second update, RB and TR assessed the risk of bias of included studies. SB checked data extraction. AV checked data and analyses. Tijs Duivenvoorden (TD) prepared the 'Summary of findings' table. With contributions from all review authors, RB and MH wrote the second update of the review.
Sources of support
Internal sources
None, Other.
External sources
No sources of support supplied
Declarations of interest
Potential conflict of interest must be reported because two included studies were conducted by the author of the systematic review.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Adili 2002 {published data only}
- Adili A, Bhandari M, Giffin R, Whalely C, Kwok DC. Valgus high tibial osteotomy. Comparison between an Ilizarov and a Coventry wedge technique for the treatment of medial compartment osteoarthritis of the knee. Knee Surgery, Sports Traumatology, Arthroscopy 2002;10(3):169‐76. [DOI] [PubMed] [Google Scholar]
Akizuki 1997 {published data only}
- Akizuki S, Yasukawa Y, Takizawa T. Does arthroscopic abrasion arthroplasty promote cartilage regeneration in osteoarthritic knees with eburnation? A prospective study of high tibial osteotomy with abrasion arthroplasty versus high tibial osteotomy alone. Arthroscopy 1997;13(1):9‐17. [DOI] [PubMed] [Google Scholar]
Brouwer 2005 {published data only}
- Brouwer RW, Bierma‐Zeinstra SMA, Koeveringe AJ, Verhaar JAN. Patellar height and the inclination of the tibial plateau after high tibial osteotomy. Journal of Bone and Joint Surgery [British] 2005;87(9):1227‐32. [DOI] [PubMed] [Google Scholar]
Brouwer 2006 {published data only}
- Brouwer RW, Bierma‐Zeinstra SMA, Raaij TM, Verhaar JAN. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate. Journal of Bone and Joint Surgery [British] 2006;88(11):1454‐9. [DOI] [PubMed] [Google Scholar]
Gaasbeek 2010 {published data only}
- Gaasbeek RDA, Rijnberg LNWJ, Loon CJM, Kampen A. Correction accuracy and collateral laxity in open versus closed wedge high tibial osteotomy. A one‐year randomised controlled study. International Orthopedics 2010;34(2):201‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harding 2011 {published data only}
- Harding AK, W‐Dahl A, Geijer M, Toksvig‐Larsen S, Tagil M. A single bisphosphonate infusion does not accelerate fracture healing in high tibial osteotomies. Acta Orthopaedica 2011;82(4):465‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iori 2011 {published data only}
- Iorio R, Pagnottelli M, Vadala A, Giannetti S, Sette P, Papandrea P, et al. Open‐wedge high tibial osteotomy: comparison between manual and computer‐assisted techniques. Knee Surgery, Sports Traumatology, Arthroscopy 2011;21:113‐9. [DOI] [PubMed] [Google Scholar]
Luites 2009 {published data only}
- Luites JW, Brinkman JM, Wymenga AB, Heerwaarden RJ. Fixation stability of opening‐ versus closing‐wedge high tibial osteotomy: a randomised clinical trial using radiostereometry. Journal of Bone and Joint Surgery [British] 2009;91(11):1459‐65. [DOI] [PubMed] [Google Scholar]
Magyar 1999a {published data only}
- Magyar G, Ahl Tl, Toksvig‐Larsen S, Lindstrand A. Open‐wedge osteotomy by hemicallotasis or the closed‐wedge technique for osteoarthritis of the knee. A randomised study of 50 patients. Journal of Bone and Joint Surgery [British] 1999;81(3):444‐8. [DOI] [PubMed] [Google Scholar]
Magyar 1999b {published data only}
- Magyar G, Toksvig‐Larsen S, Lindstrand A. Changes in osseous correction after proximal tibial osteotomy. Radiosterometry of closed and open osteotomy in 33 patients. Acta Orthopaedica Scandinavica 1999;70(5):473‐7. [DOI] [PubMed] [Google Scholar]
Mammi 1993 {published data only}
- Mammi GI, Rocchi R, Cadossi R, Massari L, Traina GC. The electrical stimulation of tibial osteotomies. Double‐blind study. Clinical Orthopaedics and Related Research 1993;288:473‐7. [PubMed] [Google Scholar]
Motycka 2000 {published data only}
- Motycka T, Eggerth G, Landsiedl F. The incidence of thrombosis in high tibial osteotomies with and without the use of a tourniquet. Archives of Orthopaedic and Trauma Surgery 2000;120(3‐4):157‐9. [DOI] [PubMed] [Google Scholar]
Myrnerts 1980 {published data only}
- Myrnerts R. High tibial osteotomy with overcorrection of varus malalignment in medial gonarthrosis. Acta Orthopaedica Scandinavica 1980;51(3):557‐60. [DOI] [PubMed] [Google Scholar]
Nakamura 2001 {published data only}
- Nakamura E, Mizuta H, Kudo S, Takagi K, Sakamoto K. Open‐wedge osteotomy of the proximal tibia with hemicallotasis. Journal of Bone and Joint Surgery [British] 2001;83(8):1111‐5. [DOI] [PubMed] [Google Scholar]
Odenbring 1992 {published data only}
- Odenbring S, Lindstrand A, Egund N. Early knee mobilization after osteotomy for gonarthrosis. Acta Orthopaedica Scandinavica 1989;60(6):699‐702. [DOI] [PubMed] [Google Scholar]
Papp 2009 {published data only}
- Papp M, Szabo L, Lazar I, Takacs I, Karolyi Z, Nagy GG, Vereb G. Combined high tibial osteotomy decreases biomechanical changes radiologically detectable in the sagittal plane compared with closing‐wedge osteotomy. Arthroscopy 2009;25(4):355‐64. [DOI] [PubMed] [Google Scholar]
Stukenborg 2001 {published data only}
- Stukenborg‐Colsman C, Wirth CJ, Lazovic D, Wefer A. High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7‐10‐ year follow‐up prospective randomised study. Knee 2001;8:187‐94. [DOI] [PubMed] [Google Scholar]
Toksvig‐Larsen 2008 {published data only}
- Toksvig‐Larsen S, Dahl AW. Inferior fixation with a new pin design for external fixation. A randomized study in 50 patients operated on by the hemicallotasis technique. Acta Orthopaedica 2008;79(1):48‐52. [DOI] [PubMed] [Google Scholar]
Toksvig‐Larsen 2013 {published data only}
- Toksvig‐Larsen S, Aspenberg P. Bisphosphonate‐coated external fixation pins appear similar to hydroxyapatite‐coated pins in the tibial metaphysis and to uncoated pins in the shaft. Acta Orthopaedica 2013;84(3):14‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weidenhielm 1993 {published data only}
- Borjesson M, Weidenhielm L, Mattsson E, Olsson E. Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5‐year follow‐up study. Knee 2005;12:121‐7. [DOI] [PubMed] [Google Scholar]
- Weidenhielm L, Olssen E, Brostrom LA, Borjesson‐Henderstrom M, Mattsson E. Improvement in gait one year after surgery for knee osteoarthritis: a comparison between high tibial osteotomy and prosthetic replacement in a prospective randomised study. Scandinavian Journal of Rehabilitation Medicine 1993;25:25‐31. [PubMed] [Google Scholar]
Zorzi 2011 {published data only}
- Zorzi AR, Silva HG, Muszkat C, Marques LC, Cliquet A Jr, Miranda JB. Opening‐wedge high tibial osteotomy with and without bone graft. Artificial Organs 2011;35(3):301‐7. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bae 2009 {published data only}
- Bae DK, Song SJ, Yoon KH. Closed‐wedge high tibial osteotomy using computer‐assisted surgery compared to the conventional technique. Journal of Bone and Joint Surgery [British] 2009;91(9):1164‐74. [DOI] [PubMed] [Google Scholar]
Bekerom 2008 {published data only}
- Bekerom van den MPJ, Patt TW, Kleinhout MY, Vis HM, Albers GHR. Early complications after high tibial osteotomy. Journal of Knee Surgery 2008;21:68‐74. [DOI] [PubMed] [Google Scholar]
Cho 2013 {published data only}
- Cho SW, Kim DH, Lee GC, Lee SH, Park SH. Comparison between autogenous bone graft and allogenous cancellous bone graft in medial open wedge high tibial osteotomy with 2‐year follow‐up. Knee Surgery and Related Research 2013;25(3):117‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dallari 2012 {published data only}
- Dallari D, Savarino L, Albisinni U, Fornasari P, Ferruzzi A, Baldini N, et al. A prospective, randomised, controlled trial using a Mg‐hydroxyapatite‐demineralized bone matrix nanocomposite in tibial osteotomy. Biomaterials 2012;33(1):72‐9. [DOI] [PubMed] [Google Scholar]
Gouin 2010 {published data only}
- Gouin F, Yaouanc F, Waast D, Delecrin J, Passuti N. Open wedge high tibial osteotomies: calcium‐phospate ceramic spacers versus autologous bone graft. Orthopaedics & Traumatology: Surgery & Research 2010;96:637‐45. [DOI] [PubMed] [Google Scholar]
Maffulli 2013 {published data only}
- Maffulli N, Loppini M, Longo UG, Denaro V, Oliva F. Bovine xenograft locking Puddu plate versus tricalcium phosphate spacer non‐locking Puddu plate in opening‐wedge high tibial osteotomy: a prospective double‐cohort study. International Orthopaedics 2013;37(5):819‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Odenbring 1992b {published data only}
- Odenbring S, Egund N, Lindstrand A, Lohmander LS, Willen H. Cartilage regeneration after proximal tibial osteotomy for medial gonarthrosis. Clinical Orthopaedics and Related Research 1992;277:210‐6. [PubMed] [Google Scholar]
Pape 2013 {published data only}
- Pape D, Kohn D, Giffen N, Hoffmann A, Seil R, Lorbach O. Differences in fixation stability between spacer plate and plate fixator following high tibial osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy 2013;21(1):82‐9. [DOI] [PubMed] [Google Scholar]
Yim 2013 {published data only}
- Yim JH, Song EK, Seo HY, Kim MS, Seon JK. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty at a minimum follow‐up of 3 years. Journal of Arthroplasty 2013;28(2):243‐7. [DOI] [PubMed] [Google Scholar]
Additional references
Aglietti 2000
- Aglietti P, Menchetti PP. Distal femoral varus osteotomy in the valgus osteoarthritic knee. American Journal of Knee Surgery 2000;13(2):89‐95. [PubMed] [Google Scholar]
Anandacoomarasamy 2013
- Anandacoomarasamy A, Leibman S, Smith G, Caterson I, Giuffre B, Fransen M, et al. Weight loss in obese people has structure‐modifying effects on medial but not on lateral knee articular cartilage. Annals of the Rheumatic Diseases 2012;71(1):26‐32. [DOI] [PubMed] [Google Scholar]
Badley 1995
- Badley EM, Webster GK, Rasooly I. The impact of musculoskeletal disorders in the population: are they just aches and pains? Findings from the 1990 Ontario Health Survey. Journal of Rheumatology 1995;22(4):733‐9. [PubMed] [Google Scholar]
Berenbaum 2012
- Berenbaum F, Grifka J, Cazzaniga S, D'Amato M, Giacovelli G, Chevalier X, et al. A randomised, double‐blind, controlled trial comparing two intra‐articular hyaluronic acid preparations differing by their molecular weight in symptomatic knee osteoarthritis. Annals of the Rheumatic Diseases 2012;71(9):1454‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berman 1991
- Berman AT, Bosacco SJ, Kirshner S, Avolio A Jr. Factors influencing long term‐results in high tibial osteotomy. Clinical Orthopaedics 1991;272:192‐8. [PubMed] [Google Scholar]
Bouwmeester 2002
- Bouwmeester PS, Kuijer R, Homminga GN, Bulstra SK, Geesink RG. A retrospective analysis of two independent prospective cartilage repair studies: autogenous perichondrial grafting versus subchondral drilling 10 years postsurgery. Journal of Orthopaedic Research 2002;20(2):267‐73. [DOI] [PubMed] [Google Scholar]
Broughton 1986
- Broughton NS, Newman JH, Baily RA. Unicompartmental replacement and high tibial osteotomy for osteoarthritis of the knee. A comparative study after 5‐10 years' follow‐up. Journal of Bone and Joint Surgery [British] 1986;68(3):447‐52. [DOI] [PubMed] [Google Scholar]
Brouwer (2) 2005
- Brouwer RW, Jakma TS, Verhagen AP, Verhaar JA, Bierma‐Zeinstra SM. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2005;25(1):CD004020. [DOI] [PubMed] [Google Scholar]
Brouwer 2007
- Brouwer GM, Tol AW, Bergink AP, Belo JN, Bernsen RM, Reijman M, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis and Rheumatism 2007;56(4):1204‐11. [DOI] [PubMed] [Google Scholar]
Cameron 1997
- Cameron HU, Botsford DJ, Park YS. Prognostic factors in the outcome of supracondylar femoral osteotomy for lateral compartment osteoarthritis of the knee. Canadian Journal of Surgery 1997;40(2):114‐8. [PMC free article] [PubMed] [Google Scholar]
Cerza 2012
- Cerza F, Carnì S, Carcangiu A, Vavo I, Schiavilla V, Pecora A, et al. Comparison between hyaluronic acid and platelet‐rich plasma, intra‐articular infiltration in the treatment of gonarthrosis. American Journal of Sports Medicine 2012;40(12):2822‐7. [DOI] [PubMed] [Google Scholar]
Coventry 1993
- Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long‐term study of eighty‐seven cases. Journal of Bone and Joint Surgery [American] 1993;75(2):196‐201. [DOI] [PubMed] [Google Scholar]
Edgerton 1993
- Edgerton BC, Mariani EM, Morrey BF. Distal femoral varus osteotomy for painful genu valgum. A five‐to‐11 year follow‐up study. Clinical Orthopaedics and Related Research 1993;288:263‐9. [PubMed] [Google Scholar]
Feeley 2010
- Feeley BT, Gallo RA, Sherman S, Williams RJ. Management of osteoarthritis of the knee in the active patient. Journal of the American Academy of Orthopaedic Surgeons 2010;18(7):406‐16. [DOI] [PubMed] [Google Scholar]
Finkelstein 1996
- Finkelstein JA, Gross AE, Davis A. Varus osteotomy of the distal part of the femur. A survivorship analysis. Journal of Bone and Joint Surgery [American] 1996;78(9):1348‐52. [DOI] [PubMed] [Google Scholar]
Fransen 2008
- Fransen M, McConnell S. Exercise for osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2008;8(4):CD004376. [DOI] [PubMed] [Google Scholar]
Grelsamer 1995
- Grelsamer RP. Unicompartmental osteoarthrosis of the knee. Journal of Bone and Joint Surgery [American] 1995;77(2):278‐92. [DOI] [PubMed] [Google Scholar]
Guyatt 2008a
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2008b
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ. What is "quality of evidence" and why is it important to clinicians?. BMJ 2008;336(7651):995‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hernigou 1987
- Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen‐year follow‐up study. Journal of Bone and Joint Surgery [American] 1987;69(3):332‐54. [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Whitehead A, Simmonds M. Sequential methods for random‐effects meta‐analysis. Statistics in Medicine 2011;30(9):903‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Knoop 2013
- Knoop J, Dekker J, Leeden M, Esch M, Thorstensson CA, Gerritsen M, et al. Knee joint stabilization therapy in patients with osteoarthritis of the knee: a randomized, controlled trial. Osteoarthritis and Cartilage 2013;21(8):1025‐34. [DOI] [PubMed] [Google Scholar]
Koskinen 2008
- Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Comparison of survival and cost‐effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow‐up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthopaedica 2008;79(4):499‐507. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Lyons 2012
- Lyons MC, Macdonald SJ, Somerville LE, Naudie DD, McCalden RW. Unicompartmental versus total knee arthroplasty database analysis: is there a winner?. Clinical Orthopaedics and Related Research 2012;470(1):84‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mathews 1998
- Mathews J, Cobb AG, Richardson S, Bently G. Distal femoral osteotomy for lateral compartment osteoarthritis of the knee. Orthopedics 1998;21(4):437‐40. [DOI] [PubMed] [Google Scholar]
Murphy 2008
- Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis and Rheumatism 2008;59(9):1207‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 1996
- Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of the Mortality and Disability From Diseases and Risk Factors in 1990 and Projected to 2020. Boston: Harvard School of Public Health on behalf of the World Health Organization and the World Bank, 1996. [Google Scholar]
Naudie 1999
- Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. The Insall award. Survivorship of the high tibial valgus osteotomy. A 10‐ to 22‐year follow‐up study. Clinical Orthopaedics and Related Research 1999;367:18‐27. [PubMed] [Google Scholar]
Newman 2009
- Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15‐year results of a prospective randomised controlled trial. Journal of Bone and Joint Surgery [British] 2009;91(1):52‐7. [DOI] [PubMed] [Google Scholar]
Phillips 1998
- Phillips MJ, Krackow KA. High tibial osteotomy and distal femoral osteotomy for valgus or varus deformity around the knee. Instructional Course Lectures 1998;47:429‐36. [PubMed] [Google Scholar]
Raaij 2008
- Raaij T, Reijman M, Brouwer RW, Jakma TS, Verhaar JN. Survival of closing‐wedge high tibial osteotomy: good outcome in men with low‐grade osteoarthritis after 10‐16 years. Acta Orthopaedica 2008;79(2):230‐4. [DOI] [PubMed] [Google Scholar]
Raaij 2009
- Raaij van TM, Reijman M, Furlan AD, Verhaar JAN. Total knee arthroplasty after valgus high tibial osteotomy: a systematic review. BMC Musculoskeletal Disorders 2009;10(88):10.1186/1471‐2474‐10‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ross 1996
- Ross SD. The CONSORT statement. JAMA 1996;28(276(8)):637‐9. [DOI] [PubMed] [Google Scholar]
Rudan 1990
- Rudan JF, Simurda MA. High tibial osteotomy. A prospective clinical and roentgenographic review. Clinical Orthopaedics and Related Research 1990;255:251‐6. [PubMed] [Google Scholar]
Schünemann 2008
- Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008;336(7653):1106‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharma 2001
- Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001;11(286(2)):188‐95. [DOI] [PubMed] [Google Scholar]
Sharma 2010
- Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Annals of the Rheumatic Diseases 2010;69(11):1940‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2011
- Smith TO, Sexton D, Mitchell P, Hing CB. Opening‐ or closing‐wedged high tibial osteotomy: a meta‐analysis of clinical and radiological outcomes. Knee 2011;18(6):361‐8. [DOI] [PubMed] [Google Scholar]
Spahn 2011
- Spahn G, Hofmann GO, Engelhardt LV, Li M, Neubauer H, Klinger HM. The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: a meta‐analysis. Knee Surgery, Sports Traumatology, Arthroscopy 2013;21(1):96‐112. [DOI] [PubMed] [Google Scholar]
Steadman 2013
- Steadman JR, Briggs KK, Matheny LM, Ellis HB. Ten‐year survivorship after knee arthroscopy in patients with Kellgren‐Lawrence grade 3 and grade 4 osteoarthritis of the knee. Arthroscopy 2013;29(2):220‐5. [DOI] [PubMed] [Google Scholar]
Strand 2012
- Strand V, Baraf HS, Lavin PT, Lim S, Hosokawa H. A multicenter, randomized controlled trial comparing a single intra‐articular injection of Gel‐200, a new cross‐linked formulation of hyaluronic acid, to phosphate buffered saline for treatment of osteoarthritis of the knee. Osteoarthritis and Cartilage 2012;20(5):350‐6. [DOI] [PubMed] [Google Scholar]
Tetsworth 1994
- Tetswort K, Paley D. Malalingnment and degenerative arthropathy. Orthopedic Clinics of North America 1994;25(3):367‐77. [PubMed] [Google Scholar]
Vasiliadis 2011
- Vasiliadis HS, Wasiak J. Autologous chondrocyte implantation for full thickness articular cartilage defects of the knee. Cochrane Database of Systematic Reviews 2010;6(10):CD003323. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vavken 2010
- Vavken P, Samartzis D. Effectiveness of autologous chondrocyte implantation in cartilage repair of the knee: a systematic review of controlled trials. Osteoarthritis and Cartilage 2010;18(6):857‐63. [DOI] [PubMed] [Google Scholar]
Virolainen 2004
- Virolianen P, Aro HT. High tibial osteotomy for the treatment of osteoarthritis of the knee: a review of the literature and a meta‐analysis of follow‐up studies. Archives of Orthopaedic and Trauma Surgery 2004;124:258‐61. [DOI] [PubMed] [Google Scholar]
Wang 2012
- Wang SY, Olson‐Kellogg B, Shamliyan TA, Choi JY, Ramakrishnan R, Kane RL. Physical therapy interventions for knee pain secondary to osteoarthritis: a systematic review. Annals of Internal Medicine 2012;157(9):632‐44. [DOI] [PubMed] [Google Scholar]
Zhang 2010
- Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clinics in Geriatric Medicine 2010;26(3):355‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]


