Abstract
Purpose of Review
The purpose of this review will be to provide both a historical and recent review of the role of the kinetic chain for the overhead athlete. The kinetic chain concept will then be applied to clinical exercise modifications and integrations for prevention and treatment of shoulder injury.
Recent Findings
The primary conclusion reached through this review is the important role the lower extremity, trunk, and scapular region play in the development of optimal terminal segment acceleration in the overhead throwing and serving motion. Failure of any links in the kinetic chain has implications for shoulder and elbow injury in the overhead athlete. Modifications of traditional shoulder exercises emphasizing activation of the scapular stabilizers and core musculature alongside concomitant rotator cuff activation are recommended and supported in EMG research.
Summary
Future research is needed to further identify risk factors and rehabilitation and prevention strategies and key clinical tests for the overhead athlete. The goal is to elucidate the important role the kinetic chain plays in both performance enhancement and injury prevention for the overhead athlete. Understanding the key role all segments of the kinetic chain play in the complex biomechanical segmental rotations required for high-level throwing and serving will assist clinicians who work with overhead athletes.
Keywords: Kinetic chain, Upper extremity, Shoulder, Rehabilitation
Introduction
This article will briefly review some of the initial historical concepts of the kinetic chain to provide an overview of more specific discussion of the relevancy of the kinetic chain biomechanical studies in throwing and the tennis serve. This will be followed by discussion regarding the application of the kinetic chain in first evaluation of the throwing athlete, as well as in designing and integrating concepts of the kinetic chain in the design and implementation of rehab programs for the overhead athlete with shoulder and elbow injury.
Relevant Historical Concepts of the Kinetic Chain
The kinetic chain or kinetic link principle provides both the framework for understanding and analyzing human movement patterns as well as the rationale for the utilization of exercise conditioning and rehabilitation programs that emphasize the entire body, despite a target joint or anatomical structure being injured. The kinetic link principle describes how the human body can be considered in terms of a series of interrelated links or segments. Movement of one segment affects segments both proximal and distal to the first segment. Kibler [1] refers to the kinetic link system as a series of sequentially activated body segments. The kinetic link principle is predicated on a concept developed and described initially by Hanavan [2], who constructed a computerized form of the adult human body. This computerized form comprises conical links that include the lower extremities, torso, and upper extremities. In reference to upper extremity skill performance, work in the upper extremity segments is transmitted to the trunk and spine via a large musculoskeletal surface. There is an exchange of forces across this musculoskeletal surface, which results in the generation of massive amounts of energy [2].
Davies [3] described how the upper extremity can be viewed as a series of links. The links proposed by Davies [3] include the trunk, scapulothoracic articulation, scapulohumeral or glenohumeral joints, and distal arm regions. Each of these links can be considered independent anatomically and biomechanically, but with reference to human function must be considered a unit.
Similar to the descriptions of the kinetic link by Hanavan [2] and Davies [3], the literature has described the concept of proximal-to-distal sequencing [4, 5]. While ultimately utilized in the biomechanical analysis of human movement, the proximal-to-distal sequencing model has relevance in exercise both for rehabilitation and performance enhancement. The terms kinetic link, proximal-to-distal sequencing, summation of speed principle [4], and Plagenhof’s [5] concept of acceleration-deceleration all attempt to describe the complex interaction of the body’s independent segments working together to form a sequence or unit of functional segments.
The goal of nearly all sport-related activities such as throwing, serving, and kicking a ball is to achieve maximal acceleration and the largest possible speed at the end of the linked segments [4]. The concept ideally states that motion should be initiated with the more proximal segments, and proceeds to the more distal segments, with the more distal segment initiating its motion at the time of the maximum speed of the proximal segment. Each succeeding segment would generate larger endpoint speeds than the proximal segment. This proximal-to-distal sequencing has been demonstrated in research by examining the linear speeds of segment endpoints, joint angular velocities, and resultant joint moments [6].
Biomechanics of the Kinetic Chain in the Throwing Motion
The overhead throwing motion is developed and controlled through a sequential body position and motion, involving sequential activation, both in onset timing and peak activation transferring from the lower extremities to upper extremities [7, 8]. Although the throwing motion is an extremely rapid movement occurring within only 0.145 s, the effective synchronous sequencing of the body segments is vital to maximize the efficiency of the kinetic chain [9]. Sciascia et al. [8] suggested that the kinetic chain is influenced by multiple factors including core strength, hip strength and range of motion (ROM), scapular kinematics, shoulder strength and ROM, knee, and ankle mobility, and efficient kinetic chains have been shown to demonstrate decreased joint loads, maximum velocity, and maximal force production during throwing. Dysfunction of kinetic chain during throwing increases stress placed on distal segments and can result in shoulder and elbow pathologies.
Dysfunction of the kinetic chain will reduce efficiency of throwing and will increase the risk of injury in shoulder and elbow [7, 8, 10, 11•]. The hip/trunk area contributes approximately 50% of the kinetic energy and force to the entire throwing motion; thus, the force and power generation in this area is compromised by altered kinematic in this area, resulting in increased stress in distal segments. Robb et al. [12] found that decreased hip ROM in the dominant side hip compared with non-dominant side is highly correlated with shoulder injury and poor throwing mechanics. Kibler et al. [7] proposed that inadequate hip ROM and poor balance may significantly affect an athlete’s ability to transfer energy along the kinetic chain, resulting in dysfunctional movement and increased stresses on the shoulder and elbow, and several studies have shown a correlation between poor lower extremity balance and overhead injuries including UCL tear [7, 10, 13•, 14•, 15•].
The trunk is the vital structure to deliver the force produced by the lower limbs to the upper limbs. Proper trunk movement is important during throwing, as it is integral to the transfer of energy to distal body segments during the throwing motion. Previous studies using mathematical modeling showed that a reduction in trunk kinetic energy development increased the demand in the distal segment to maintain the same energy ball release, resulting in increased stress placed in the shoulder and elbow joints [11•, 16•, 17•, 18•].
The scapula and glenohumeral joints are the key in facilitating energy transfer produced by lower limbs and trunk. Kibler et al. [19] calculated that a 20% decrease in kinetic energy delivered from the hip and trunk to the arm requires a 34% increase in the rotational velocity of the shoulder to generate the same amount of force to the hand. Deficits of strength and mobility in these areas can negatively impact shoulder kinematics which would increase injury risk in the shoulder and elbow [10, 19].
Biomechanics of the Kinetic Chain in the Tennis Serve
Proximal-to-distal sequencing has been reported in the historical literature on the tennis serve [5, 20–22]. Closely analyzing the literature in upper extremity throwing or striking sports shows a modification of the proximal-to-distal pattern. This modification occurs when the human body exploits the benefits of long-axis rotation of the humerus (internal rotation) and forearm (forearm pronation) to maximize endpoint speed [6]. Research has demonstrated consistently that peak internal rotation of the shoulder (humerus) follows the movement of the wrist and hand [6, 21, 22]. Additionally, the peak speed of pronation has been found to occur immediately prior to ball contact on the tennis serve and forehand groundstroke suggesting that this long-axis rotation does not conform to traditional explanations of proximal-to-distal sequencing (Marshall & Elliot, 2000).
Additionally, Kibler [19] provided an objective analysis of force generation during a tennis serve. Fifty-four percent of the force development during the tennis serve comes from the legs and trunk, with only 25% coming from the elbow and wrist. Non-optimal performance and increased risk of injury occur in tennis and other sport activities when individual’s attempt to utilize the smaller muscles and distal arm segments as a primary source for power generation [1, 20].
Finally, research from the Sydney Olympics, where the highest level tennis players from around the world competed and were analyzed in competition, revealed some very clinically applicable information relative to the tennis serve and the kinetic chain. Servers were broken down into two categories based on the amount of leg drive (knee flexion) utilized during the loading or cocking phase of the tennis serve [23, 24]. Minimal “leg drive” servers had 7.6° of knee flexion compared with those with more optimal “leg drive” (14.7°) and had significantly larger anterior shoulder forces and elbow varus torques measured at the stage of maximal external rotation during the cocking phase of the tennis serve. Values for anterior shoulder force (shoulder internal rotation torque) and elbow varus torque at MER in the serving motion were shown to be greatly increased when the lower body contribution to the serving motion was decreased. Similar to the mathematical modeling research from Kibler [19], this study shows how non-optimal contribution from the lower body kinetic chain segments creates concomitant increases in shoulder and elbow loading which would potentially increase injury risk.
Application of the Kinetic Chain to Evaluation of the Overhead Athlete
Application of the kinetic link system in a clinical or rehabilitative way has led to the development of the total arm strength (TAS) concept [25, 26]. This concept is predicated on the kinetic link system as well as demonstrated by the close clinical relationship between shoulder and elbow injuries in sport. Classic research by Priest and Nagel [27] studied 84 world class tennis players and reported that 74% of men and 60% of women had a history of shoulder or elbow injury in the dominant arm that affected tennis play. Injuries to both the shoulder and elbow of the dominant arm were reported by 21% and 23% of the men and women, respectively. Another study by Priest et al. [28] surveyed 2633 recreational tennis players and found an incidence of tennis elbow of 31%. Additionally, there is a 63% greater incidence of shoulder injury in this population, as compared with those players who did not have a history of tennis elbow.
Another classic foundational study of the total arm strength concept is that by Strizak et al. [29]. These researchers incorporated the isometric strength of the forearm (pronation and supination), wrist (radial, ulnar deviation, and flexion and extension), and metacarpal phalangeal (MCP) joints (flexion and extension) to create a total arm strength index. This index was compared among three groups: (1) a normal, uninjured, non-tennis-playing control population, (2) healthy recreational tennis players, and (3) recreational tennis players with tennis elbow. Results of this study showed significantly greater dominant-arm total arm strength relative to body weight in the control group and tennis-playing group, but no significant difference in the tennis elbow study population [29]. The finding of greater “total arm strength”: in both the control population and in healthy tennis players and lack of this finding in the injured group supports the use of “whole extremity” or in this application “total arm strength” rehabilitation and conditioning programs.
More recently, Alizadehkhaiyat et al. [30] measured EMG activity and fatigue response in a population of 16 patients with tennis elbow and 16 control subjects. Similar to the older study by Strizak et al. [29], five forearm muscles and two shoulder muscles were measured bilaterally. All control subjects showed a dominance difference effect in all muscles tested; however, the tennis elbow patients did not show a dominance effect for any muscle tested. In fact, deficits of 25 to 35% in strength were documented in the patients with tennis elbow compared with the control subjects. Similar findings were reported by Lucado et al. [31] in a group of female tennis players with lateral epicondylitis. Players in their study with lateral epicondylitis had significantly decreased lower trapezius strength compared with a control population that was asymptomatic. Day et al. [32] also reported unilateral weakness of the scapular musculature (middle trap, lower trap, and serratus anterior) in patients with lateral epicondylitis. The decrease in local and proximal muscle strength found in these studies shows the important of a kinetic chain “total arm strength” approach to rehabilitation in patients with upper extremity injury. This concept is prevalent today in upper extremity rehabilitation and is reflected in the large emphasis in both shoulder and elbow rehabilitation in trunk and scapular stabilization exercise and evaluation inclusion for the overhead athlete.
Extensive evaluation of the scapulothoracic joint is indicated as an essential part of the kinetic chain in the overhead athlete. Kibler [33, 34] has provided the early foundational emphasis regarding the role of the scapula in the overhead athlete as well as provided an evaluation scheme to identify scapular dyskinesis [34]. The use of repeated shoulder elevation with or without loading is an essential part in any evaluation of the overhead athlete and can identify unilateral scapular pathology for both preventative screening and clinical evaluation. Despite the recent study by Plummer et al. [35•], where similar incidences of scapular pathology were visually identified in patients with shoulder pathology (67% in flexion, 67% in abduction) and in controls (61% in flexion and 52% in abduction), scapular evaluation has been found to be a valuable inclusion in the evaluation of patients with upper extremity dysfunction. In fact, a recent systematic review and meta-analysis by Hickey et al. [36•] concluded that athletes with scapular dysfunction are 43% more likely to develop shoulder pain than athletes without scapular dysfunction. The use of the Kibler scapular dyskinesis test alongside tests like the scapular assistance [37] and scapular retraction test provides a battery of examination methods to screen this important articulation in the overhead athlete [38•].
Evaluation of the elite-level tennis player for prevention of injury and recognition of injury risk has resulted in the development and implementation of an instrument called the High Performance Profile (HPP) by the US Tennis Association [39], as well as the ATP Performance and Injury Prevention Screening PIPS tool [40]. This instrument has been utilized to screen elite-level tennis players resulting in published descriptive profiles showing the identification of core and lower body weakness on tests like the one-leg stability test (Fig. 1), and abdominal bracing and bridging core tests in elite players [40, 41, 42•]. Surprisingly, among healthy, uninjured competing tennis players, the number of failed one-leg stability tests indicating hip weakness has been reported to range between 45 and 55% and can serve to facilitate preventative hip and core training programs to improve hip and core stability [40, 41, 42•].
Fig. 1.
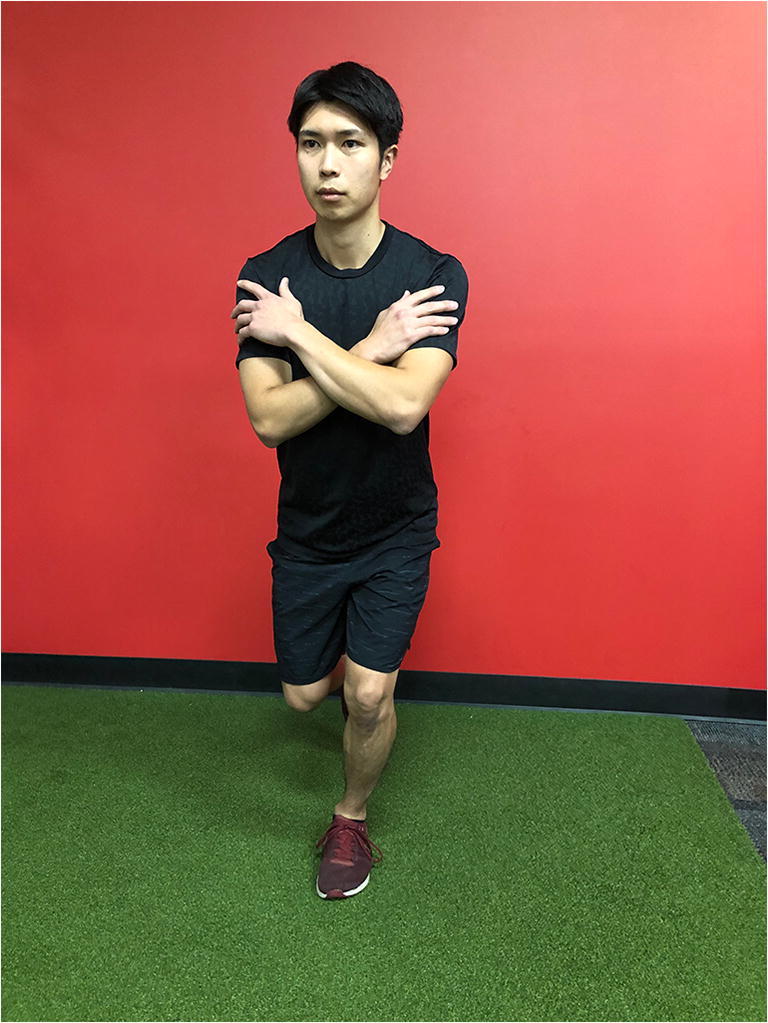
One-leg stability test to assess hip and core stabilization
Garrison et al. [10] found a decreased score on the Y balance test (Fig. 2) for both the stance and stride lower limb in baseball players with confirmed UCL tears. The Y balance score is reflective of lower extremity strength and neuromuscular control. Thus, a lower score on the Y balance test may indicate a deficit in balance, strength, and neuromuscular control in the lower extremities. In baseball, the deficit in neuromuscular control and strength at the trunk and lower extremities would negatively impact the ability to transfer energy into the upper extremities, resulting in increased stresses placed on the shoulder and elbow which would potentially increase in injury risk.
Fig. 2.

Y balance test
Another key measure for the kinetic chain in throwing athlete is hip rotation range of motion. Prior studies have established normative data for the key movements of hip internal and external rotation range of motion in elite-level tennis players [40, 41, 43] and in youth, collegiate, and professional baseball players [12, 43, 44•, 45•]. Limitation in hip rotation ROM can have consequences and affect upper extremity loading during the throwing motion and negatively impact performance and elevate injury risk. Therefore, a screen of prone hip internal rotation (IR) ROM has been reliably utilized to assess hip rotation range of motion in overhead athletes [43, 46] (Fig. 3).
Fig. 3.

Prone hip internal rotation range of motion measurement
The inclusion of lower body and core screening tests is an important part of the comprehensive evaluation of an overhead athlete. The key tests for inclusion recommended by these authors would include the one-leg stability test, Y balance, and core series including abdominal and extensor-based tests to determine competency in this important part of the kinetic chain. Failure of these kinetic chain tests can guide exercise prescription for both prevention and treatment of upper extremity injuries in the overhead athlete.
Application of the Kinetic Chain: Upper Extremity Rehabilitation Concepts for the Overhead Athlete
Following the use of a comprehensive evaluation of the upper extremity and other key components of the kinetic chain for the throwing athlete, several modifications to traditional exercise programs can be undertaken to provide greater activation of the kinetic chain and incorporate proprioceptive and core challenges to the athlete while performing upper body exercise.
Wilk et al. [47] have recommended a more advanced form of upper extremity exercises that are characterized by bilateral upper extremity activation and performance, and the application and use of unstable surfaces. These exercises create further challenge for the athlete performing the traditional glenohumeral and scapulothoracic exercise patterning with the added requirement of enhanced core activation through the unstable surface and bilateral extremity activation. Myers et al. [48] applied the advanced thrower’s ten exercises characterized by a sustained isometric contraction and bilateral extremity involvement in a randomized clinical trial. They found these exercises to improve strength and muscle endurance by 10–14% in a pre-/post-testing paradigm. While these exercises did not increase strength and endurance to a greater extent than traditional exercises, the bilateral activation and increased involvement of the core and lower extremity musculature during the performance of these exercises are clinically recommended.
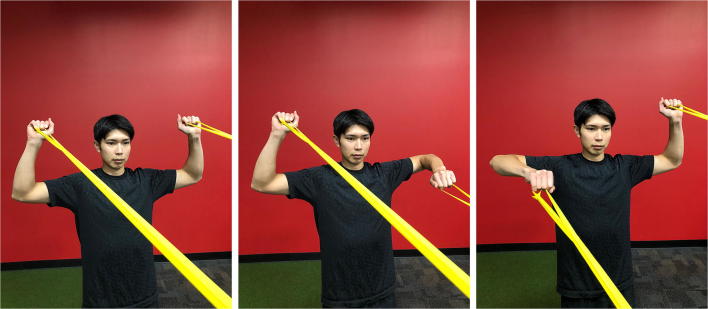
Figures 4 and 5 show two examples of the sustained hold bilateral exercises recommended by Wilk et al. [47]. The 90/90 external rotation exercise (Fig. 4a–c) starts with both arms in 90° of external rotation with resistance applied by an elastic band or tubing. While holding one extremity in an isometric external rotation position as pictured, the contralateral extremity performs 10–15 repetitions of slow controlled external rotation. Upon completion of those extremity repetitions of external rotation, the contralateral extremity is then moved through 10–15 repetitions of external rotation. Finally, one set of 10–15 repetitions is completed using a reciprocal activation pattern (one rep left with isometric hold right, then one rep right with isometric hold left) to provide greater endurance training. Figure 5 a, b, and c show how the same patterning can be used while the athlete is positioned over a physio ball using the movement of prone horizontal abduction.
Fig. 4.
Bilateral sustained isometric 90/90 external rotation exercise: each limb performs 90° abducted external rotation while the contralateral limb maintains an isometric 90/90 position with scapular retraction. a Sustained hold 90/90 START. b Sustained hold R shoulder isometric. c Sustained hold L shoulder isometric
Fig. 5.
Prone horizontal abduction sustained isometric exercise: each limb performs horizontal abduction while the contralateral limb maintains an isometric position with scapular retraction. a Sustained hold horiz ABD START. b Sustained hold R shoulder isometric. c Sustained hold L shoulder isometric
DeMay et al. [49] has demonstrated the effects of combining different weight-bearing postures and positions on lower trapezius muscle activity during upper extremity shoulder exercises. Their study has shown that unilateral stance and other postures have an effect (both unilateral stance and bilateral stance) on lower trapezius muscle activation. Figure 6 shows a unilateral stance external rotation exercise on a stability trainer that can be used to augment a traditional exercise for external shoulder rotation in the overhead athlete. The use of perturbation exercise is also added to provide additional challenger to the athlete. Figure 7 shows the application of a core challenge through the use of a side plank posture for the side lying external rotation ball drop plyometric. Elastic resistance is added to provide additional overpressure and challenge to the exercise where 30–45 s time intervals are applied to foster local muscular endurance.
Fig. 6.

90/90 external rotation exercise with unilateral stance and distal arm segment perturbation
Fig. 7.

Side lying plank plyometric ball drop with band loop external rotation loading
A final component worth discussing regarding the use of any kinetic chain exercise is the use of visual and tactile feedback to the athlete through clinical exercise supervision. Two studies [50, 51•] have both advocated conscious correction and use of visual and tactile feedback to enhance muscle activation of the scapular stabilizing musculature during shoulder rehabilitation exercise. These studies demonstrate the importance of using proper body positioning and especially scapular positions to enhance muscular activation of the important scapular stabilizers that are a critical part of the kinetic chain in the overhead athlete.
Summary
A review of the classic and more recent biomechanical studies on the throwing motion and tennis serve demonstrates the important interaction between segments of the kinetic chain for optimal performance and injury prevention. A comprehensive evaluation program for the overhead athlete that includes key tests and measures to assess hip and core function is advocated. Finally, the inclusion of evidence-based modifications to traditional shoulder rehabilitation exercises can be used to engage surrounding portions of the kinetic chain for the overhead athlete.
Compliance with Ethical Standards
Conflict of Interest
Todd S. Ellenbecker & Ryoki Aoki declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Kibler WB. Clinical biomechanics of the elbow in tennis: implications for evaluation and diagnosis. Med Sci Sports Exerc. 1994;26(10):1203–1206. doi: 10.1249/00005768-199410000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Hanavan EP. A mathematical model of the human body: Wright-Patterson Air Force Base; 1964. (AMRL-TR-64–102) [PubMed]
- 3.Davies GJ. A compendium of isokinetics in clinical usage. LaCrosse: S & S Publishing; 1992. [Google Scholar]
- 4.Bunn J. Scientific principles of coaching. Englewood Cliffs: Prentice-Hall; 1972. [Google Scholar]
- 5.Plagenhoef S. Patterns of human movement. Englewood Cliffs: Prentice-Hall; 1971. [Google Scholar]
- 6.Marshall RN, Elliot BC. Long-axis rotation: the missing link in proximal-to-distal segmental sequencing. J Sports Sci. 2000;18:247–254. doi: 10.1080/026404100364983. [DOI] [PubMed] [Google Scholar]
- 7.Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implication of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med. 2013;47:877–885. doi: 10.1136/bjsports-2013-092425. [DOI] [PubMed] [Google Scholar]
- 8.Sciascia A, Thigpen C, Namdari S. Kinetic chain abnormalities in the athletic shoulder. Sports Med Arthrosc Rev. 2012;20:16–21. doi: 10.1097/JSA.0b013e31823a021f. [DOI] [PubMed] [Google Scholar]
- 9.Seroyer ST, Nho SJ, Bah BR et al. The kinetic chain in overhead pitching: its potential role for performance enhancement and injury prevention. [DOI] [PMC free article] [PubMed]
- 10.Garrison CJ, Arnold A, Macko MJ, Conway JE. Baseball players diagnosed with ulnar collateral ligament tears demonstrate decreased balance compared to healthy controls. J Orthop Sports Phys Ther. 2013;43:752–758. doi: 10.2519/jospt.2013.4680. [DOI] [PubMed] [Google Scholar]
- 11.Chalmers PN, Wimmer MA, Verma NN, Cole BJ, Romeo AA, Cvetanovich GL, Pearl ML. The relationship between pitching mechanics and injury: a review of current concepts. Sports Health. 2017;9:216–221. doi: 10.1177/1941738116686545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robb AJ, Fleisig G, Wilk KE, et al. Passive range of motion of the hips and their relationship with pitching biomechanics and ball velocity in professional baseball pitchers. Am J Sports Med. 2010;38(12). 10.1177/0363546510375535. [DOI] [PubMed]
- 13.Chu SK, Jayabalan P, Kibler WB. The kinetic chain revisited: new concept on throwing. PM R. 2016;8:S69–S77. doi: 10.1016/j.pmrj.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 14.• Kantrowitz DE, Trofa DP, Woode R, et al. Athletic hip injury in Major League Baseball pitchers associated with ulnar collateral ligament tear. Orthorp J Sports Med. 2018. 10.1177/2325967118800704The purpose of this study was to determine whether professional baseball pitchers who underwent UCL reconstruction (UCLR) had an increased incidence of hip or groin injuries 4 years before or after surgery. There were 247 subjects who are MLB players at the time of study and underwent UCLR between 2005 and 2017. As a result of this study, MLB pitchers who required UCLR sustained a higher frequency of proximal lower extremity injury both before and after surgery. Hip mobility and core strengthening may help reduce elbow injury in baseball players. Level of evidence: Cohort study, level 3.
- 15.Culiver A, Garrison CJ, Creed KM, et al. Correlation among Y-balance test-lower quarter composite scores, hip musculoskeletal characteristics, and pitching kinematics in NCAA division I baseball pitchers. J Sports Rehabil. 2019;28:432–437. doi: 10.1123/jsr.2017-0111. [DOI] [PubMed] [Google Scholar]
- 16.Tocci NX, Howell DR, Sugimoto D, Dawkins C, Whited A, Bae D. The effect of stride length and lateral pelvic tilt on elbow torque in youth baseball pitchers. J Appl Biomech. 2017;33:339–346. doi: 10.1123/jab.2016-0305. [DOI] [PubMed] [Google Scholar]
- 17.Laudner KG, Wong R, Mister K. The influence of lumbopelvic control on shoulder and elbow kinetic s in elite baseball pitchers. J Should Elbow Surg. 2019;28:330–224. doi: 10.1016/j.jse.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 18.Myrick KM, Pallone AS, Feinn RS. Trunk muscle endurance, flexibility, stride foot balance, and contralateral trunk lean in collegiate baseball pitchers. J Strength Cond Res. 2019;33(10):2641–2647. doi: 10.1519/JSC.0000000000003292. [DOI] [PubMed] [Google Scholar]
- 19.Kibler WB, Chandler J. Baseball and tennis. In: Griffin LY, editor. Rehabilitation of the injured knee. St. Louism MO: Mosby; 1995. pp. 219–226. [Google Scholar]
- 20.Groppel JL. High tech tennis. 2. Champaign: Human Kinetics; 1992. [Google Scholar]
- 21.Van Gheluwe B, Hebbelinck M. Muscle actions and ground reaction forces in tennis. Int J Sport Biomech. 1986;2:88–99. doi: 10.1123/ijsb.2.2.88. [DOI] [Google Scholar]
- 22.Elliott BC, Marshall RN, Noffal GJ. Contributions of upper limb segment rotations during the power serve in tennis. J Appl Biomech. 1995;11:433–442. doi: 10.1123/jab.11.4.433. [DOI] [Google Scholar]
- 23.Elliott B, Fleisig GS, Nicholls R, Escamilla R. Technique effects on upper limb loading in the tennis serve. J Sci Med Sport. 2003;6(1):76–87. doi: 10.1016/S1440-2440(03)80011-7. [DOI] [PubMed] [Google Scholar]
- 24.Kovacs M, Ellenbecker TS. An 8-stage model for evaluating the tennis serve: implications for performance enhancement and injury prevention. Sports Health. 2011;3(6):504–513. doi: 10.1177/1941738111414175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davies GJ, Ellenbecker TS. Scientific and clinical rationale for utilization of a total arm strength rehabilitation program for shoulder and elbow overuse injuries. LaCrosse: APTA Orthopaedic Section, Home Study Course; 1993. [Google Scholar]
- 26.Ellenbecker TS, Davies GJ. Closed kinetic chain exercise. A comprehensive guide to multiple joint exercises. Champaign: Human Kinetics Publishers; 2001. [Google Scholar]
- 27.Priest JD, Nagel DA. Tennis shoulder. Am J Sports Med. 1976;4(1):28–42. [PubMed] [Google Scholar]
- 28.Priest JD, Braden V, Gerberich SG. The elbow and tennis, part 1: an analysis of players with and without pain. Phys Sportsmed. 1980;8(4):80–91. doi: 10.1080/00913847.1980.11710917. [DOI] [PubMed] [Google Scholar]
- 29.Strizak AM, Gleim GW, Sapega A, Nicholas JA. Hand and forearm strength and its relation to tennis. Am J Sports Med. 1983;11(4):234–239. doi: 10.1177/036354658301100410. [DOI] [PubMed] [Google Scholar]
- 30.Alizadehkhaiyat O, Fisher AC, Kemp GJ, Vishwanathan K, Frostick SP. Upper limb muscle imbalance in tennis elbow: a functional and electromyographic assessment. J Orthop Res. 2007;25(12):1651–1657. doi: 10.1002/jor.20458. [DOI] [PubMed] [Google Scholar]
- 31.Lucado AM, Kolber KJ, Cheng MS, Echternach JL. Upper extremity strength characteristics in female recreational tennis players with and without lateral epicondylalgia. J Orthop Sports Phys Ther. 2012;42(12):1025–1031. doi: 10.2519/jospt.2012.4095. [DOI] [PubMed] [Google Scholar]
- 32.Day JM, Bush H, Nitz AJ, UHL TL. Scapular muscle performance in individuals with lateral epicondylalgia. J Orthop Sports Phy Ther. 2015;45(5):414–424. doi: 10.2519/jospt.2015.5290. [DOI] [PubMed] [Google Scholar]
- 33.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325–337. doi: 10.1177/03635465980260022801. [DOI] [PubMed] [Google Scholar]
- 34.Kibler WB, Uhl TL, Maddux JW, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elb Surg. 2002;11:550–556. doi: 10.1067/mse.2002.126766. [DOI] [PubMed] [Google Scholar]
- 35.Plummer HA, Sum JC, Pozzi F, Varghese R, Michener LA. Observational scapular dyskinesis: known-group validity in patients with and without shoulder pain. J Orthop Sports Phys Ther. 2017;47(8):530–537. doi: 10.2519/jospt.2017.7268. [DOI] [PubMed] [Google Scholar]
- 36.Hickey D, Solvig V, Cavalheri V, Harrold M, Mckenna L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br J Sports Med. 2018;52(2):102–110. doi: 10.1136/bjsports-2017-097559. [DOI] [PubMed] [Google Scholar]
- 37.Rabin A, Irrgang JJ, Fitzgerald KG, Eubanks A. The intertester reliability of the scapular assistance test. J Orthop Sports Phys Ther. 2006;36(9):653–660. doi: 10.2519/jospt.2006.2234. [DOI] [PubMed] [Google Scholar]
- 38.• Kibler WB, Sciascia AD. Disorders of the Scapula and their role in shoulder injury. Springer 2017. Level of evidence: Book, Author opinion; Level 5.
- 39.United States Tennis Association High Performance Profile. www.usta.com
- 40.Ellenbecker TS, Windler G, Dines D, Renstrom P. Musculoskeletal profile of tennis players on the ATP World Tour: results of a 9 year screening program. J Med Sci Tennis. 20(3):94–106.
- 41.Ellenbecker TS. Musculoskeletal testing of elite junior tennis players. Aspetar Sports Med J. 2014:548–56.
- 42.Rice RP, Roach KE, Waltz B, Kirk-Sanchez NJ, Ellenbecker TS, Raya M. Side to side asymmetries of the hip and core are associated with back injuries in elite and professional tennis players. J Orthop Sports Phys Ther. 2018;48(1):A-57. [Google Scholar]
- 43.Ellenbecker TS, Ellenbecker GA, et al. Descriptive profile of hip rotation range of motion in elite tennis players and professional baseball pitchers. Am J Sports Med. 2007;35(8):1371–1376. doi: 10.1177/0363546507300260. [DOI] [PubMed] [Google Scholar]
- 44.Cheatham SW, Shimamura, Kolber MJ. Difference in hip range of motion among collegiate pitchers when compared to youth and professional baseball pitcher data. J Can Chiropr Assoc. 2016;60(3):233–240. [PMC free article] [PubMed] [Google Scholar]
- 45.Oliver GD, Weimar WH. Hip and shoulder range of motion in youth baseball pitchers. J Strength Cond Res. 2016;30(10):2823–2827. doi: 10.1519/JSC.0000000000000796. [DOI] [PubMed] [Google Scholar]
- 46.McCulloch PC, Patel JK, Ramkumar PN. Asymmetric hip rotation in professional baseball pitchers. Orthop J Sports Med. 2014;2(2). 10.1177/2325967114521575. [DOI] [PMC free article] [PubMed]
- 47.Wilk KE, Yenchak AJ, et al. The advanced throwers ten exercise program: a new exercise series for enhanced dynamic shoulder control in the overhead throwing athlete. Phys Sports Med. 2011;39(2). 10.3810/psm.2011.11.1943. [DOI] [PubMed]
- 48.Myers NL, Toonstra JL, Smith JS, et al. Sustained isometric shoulder contraction on muscular strength and endurance: a randomized clinical trial. Int J Sports Phys Ther. 2015;10(7):1015–1025. [PMC free article] [PubMed] [Google Scholar]
- 49.DeMay K, Danneels L, Cagnie B, et al. Kinetic chain influences on upper and lower trapezius muscle activation during eight variations of a scapular retraction exercises in overhead athletes. J Sci Med Sport. 2013;16:65–70. doi: 10.1016/j.jsams.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 50.DeMay K, Danneels L, Cagnie B, et al. Conscious correction of scapular orientation in overhead athletes performing selected shoulder rehabilitation exercises: the effect on trapezius muscle activation measured by surface electromyography. J Orthop Sports Phys Ther. 2013;43(1):3–10. doi: 10.2519/jospt.2013.4283. [DOI] [PubMed] [Google Scholar]
- 51.• Staker JL, Evans AJ, Jacobs LE, et al. The effect of tactile and verbal guidance during scapulothoracic exercises: an EMG and kinematic investigation. J Electromyogr Kinesiol. 2019. 10.1016/j.jelekin.2019.07.004The purpose of this study was to determine if clinician guidance changes scapulothoracic muscle activity and kinematics compared with unguided shoulder exercises with electromyographic (EMG) sensors placed on serratus anterior, upper, and lower trapezius. The study found that verbal and tactile guidance during exercises significantly increases shoulder muscle activity and improves lower trapezius/upper trapezius muscle recruitment. Level of evidence: case-controlled study; Level 3.