Abstract
Aim
The aim of this study is to evaluate the efficacy of sodium bicarbonate as an additive alkalizing agent to local anesthetic solutions in inflamed and infected pulpal and periapical tissues.
Type of Study
A prospective, randomized crossover double-blinded study was carried out in a university-affiliated hospital in Chennai.
Materials and Methods
A randomized crossover double-blinded study was designed wherein ninety-six patients were enrolled for the study. 1.8 ml of 2% lignocaine with 1:200,000 adrenaline was administered. The latency time period was found to be 5–10 min and extraction was attempted. During extraction, if the patient experienced pain, 0.5 ml of 8.4% sodium bicarbonate was injected into the previously injected local anesthesia site. A time period of 3 min was allowed for the alkalinization to occur. Extraction was carried out only when the patient did not complain of pain. Pain score was assessed before and after administration of 8.4% sodium bicarbonate using visual analog scale. Pulse rate at the baseline, before and after administration of 8.4% sodium bicarbonate, was recorded and the pain scale values were correlated with pulse rate.
Results
It was found that there was a significant decrease in pain after injecting buffered local anesthetics (p < 0.1). Pain score before injecting sodium bicarbonate was higher when compared to post-injection of sodium bicarbonate. There was also significant reduction in pulse rate following the administration of sodium bicarbonate.
Conclusion
Buffered 2% lignocaine with 1:200,000 epinephrine had early onset of anesthesia when compared to unbuffered form. Injecting 2% buffered lignocaine pain was significantly reduced during extraction in the teeth.
Keywords: Buffered local anesthesia, Local anesthesia, Pain, Sodium bicarbonate, Visual analog scale
Introduction
In this modern era, for many people, the fear of pain and anxiety prevents the patients seeking dental care. Local anesthetic solutions in many instances provide effective anesthesia through the dental treatment [1]. Local anesthetic forms the effective drug for the management of pain in dentistry. Painful stimuli are detected by the nociceptor. The signal is carried from the nociceptors in the form of action potential. Pain is perceived once the signal reaches the cerebral cortex [1, 2].
Depolarization occurs when local anesthesia is administered near the nociceptors which eventually prevent the signal from the central nervous system [3]. Local anesthetics are unstable; weakly basic compounds that are least soluble in water combine with acid to produce local anesthetic salt which becomes stable and soluble in water. Local anesthetics without epinephrine have a pH of about 6.5 and with epinephrine has the pH of about 3.5 [3].
The normal tissue has the pH of 7.4. When local anesthesia is injected because of the alkalinity of the tissue, it liberates free base, thereby the local anesthetic molecule penetrates into the lipid-rich nerve. In case of inflammation where there is acidic pH (5–6), the amount of free base liberated from the tissues is less thereby minimal local anesthetic molecules penetrate into the nerve membrane. This is the reason for local anesthetics do not work efficiently in infected and inflamed pulp and periapical tissues [1, 3].
However, local anesthetics have a number of drawbacks such as relatively slow onset, decreased latency period of anesthesia, produces sting on injection. The advent of using 8.4% sodium bicarbonate has addressed the drawback [3].
pH value of the anesthetic solution determines the ratio of RN and RNH. According to Henderson–Hasselbalch equation which states that when the acid dissociation constant pka matches the ph of the solution, there exists equal amount of half-charged and half-uncharged molecule [4]. Local anesthetic solution in a cartridge contains both charged (RNH) and uncharged molecule (RN) existing in equilibrium. Deionized lipid soluble (RH) form crosses the nerve membrane, within the nerve it picks up H+ resulting in RNH+ which enters the sodium channel and resulting in conduction blockade. The body buffers the pH-injected anesthetic solution to the physiological pH to produce anesthesia. The time taken for this transformation is the important factor for the latency [4].
The aim of this study is to enhance and evaluate the efficacy of sodium bicarbonate as an additive alkalizing agent to local anesthetic solutions in inflamed and infected pulpal and periapical tissues.
The null hypothesis tested was that there is no difference between buffered and unbuffered local anesthesia.
Materials and Methods
The Ethics Committee approved the protocol of the study, and written informed consent was obtained from each patient. Ninety-six patients aged 20–70 presented to the department of oral and maxillofacial surgery in a university-affiliated hospital with a complaint of pain and had been diagnosed to have a periapical infection for which extraction was planned. Maxillary teeth which clinically had tenderness on percussion along with acute abscess accompanied by localized or generalized swelling was included in the study. Patients who were under 20 years of age, who had a history of significant medical conditions, allergic to local anesthesia or sulfites, pregnant and who were taking medications that might influence anesthetic assessment or were unable to give informed consent were excluded. Patients were explained about the procedure, and informed consent was obtained before the start of intervention.
The sample size of ninety-six patients was calculated with a power of 80% and α error of 0.05. Crossover study design was performed where the subjects served as his/her own control. In order to eliminate the selection bias, simple randomization was done. Ninety-six random numbers were obtained using computer-generated random number. The operator who recruited the participants for the study and who performed the treatment was not blinded. To begin with the treatment, the operator administered approximately 1.8 ml 2% lignocaine with 1:200,000 adrenaline. The latency time period was found to be 5–10 min and extraction was attempted. During extraction, if the patient experienced pain, 0.5 ml of 8.4% sodium bicarbonate was injected into the previously injected LA site. A time period of 3 min was allowed for the alkalinization to occur. Extraction was carried out only when the patient did not complaint of pain. The blinded assessor evaluated the pain score before and after administration of 8.4% sodium bicarbonate using visual analog scale (VAS). Pulse rate was noted using pulse oximeter. Pulse rate at the baseline, before and after administration of 8.4% sodium bicarbonate, was recorded, and the pain scale values were correlated with pulse rate.
Statistical Analysis
The collected data were analyzed with IBM SPSS statistics software 23.0 Version. Wilcoxon signed-rank test was used to assess the bivariate sample. T test was used to calculate the difference between the pulse rate before and after sodium bicarbonate injection.
Results
Out of the ninety-six patients who participated in this study, 61% were female and 39% were male (Fig. 1).
Fig. 1.
Gender distribution
Based on visual analog scale (VAS), pain score was assessed before and after administration of sodium bicarbonate. The difference in pain score was calculated. The value obtained ranged from 0 to 10. Patient who experienced mild decrease in pain was categorized from score 1 to 4, moderate decrease in pain from 5 to 7, drastic decrease in pain from 8 to 10. Patients who did not experience any significant difference were assigned score 0. Out of the ninety-six participants in the study, 61 patients experienced mild decrease in pain after injecting sodium bicarbonate. 27 patients experienced moderate decrease in pain, whereas five patients experienced drastic decrease in pain. Three patients did not find any significant difference before and after administration bicarbonate.
Wilcoxon signed-rank test showed that, there was a significant decrease in pain after injecting buffered local anesthetics (p < 0.1) (Table 1). The mean value of pain score before injecting sodium bicarbonate was 7, whereas the pain score was reduced to 3 following the administration of after injecting sodium bicarbonate as shown in Fig. 2.
Table 3.
Wilcoxon signed-rank test
| After bicarbonate—before bicarbonate | |
|---|---|
| Z | − 8.409 |
| Asymp. sig. (2-tailed) | 0.000 |
Fig. 2.

VAS pain score
Figure 3 denotes that there is a significant decrease in pain after injecting buffered lignocaine to the patients with infected and inflamed pulp and periapical tissues.
Fig. 3.
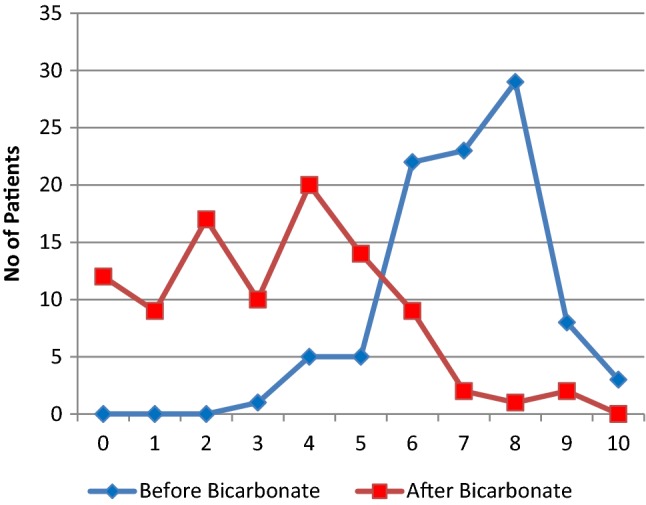
Comparison—before and after bicarbonate
T test was used to calculate the difference in pulse rate with respect to lignocaine and buffered lignocaine (Fig. 4). Pulse rate before and after injecting sodium bicarbonate was correlated with pain. The results revealed that the mean pulse rate score before administration of sodium bicarbonate was 90/min, whereas following the administration of sodium bicarbonate was found to be significantly reduced to 82/min.
Fig. 4.
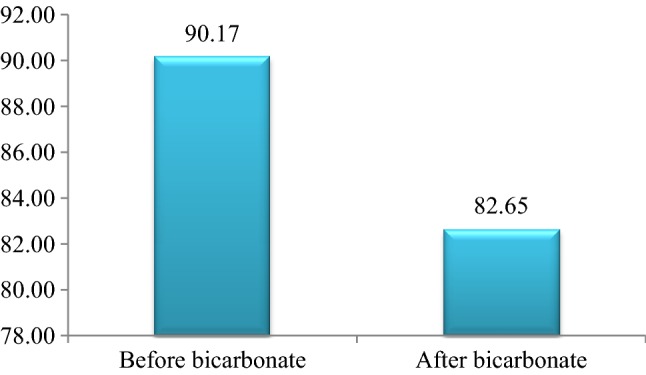
Pulse Rate
Discussion
The concept of alkalinization is well known in the literature. Though many studies using buffered LA have been done in ophthalmology [5], ears, nose and throat [6], dermatology [7], its use is not been practiced in dentistry.
The maximum recommended dose of sodium bicarbonate is 50 mEq. 2 ml of 8.4% sodium bicarbonate was added to 20 ml of 1 or 2% lignocaine. For effective results, the ratio of lignocaine to bicarbonate is from 5:1 to 10:1. Some studies have been reported that 10:1 ratio is said to produce profound anesthesia. Precipitation can occur if the bicarbonate level is more than this ratio. Sodium bicarbonate is contraindicated in patients with metabolic acidosis, hypocalemia, excessive vomiting and dehydrated patients [8].
Accidental extravasation of hypertonic solutions of sodium bicarbonate into the surrounding tissues has been reported to cause chemical cellulitis, with tissue necrosis, tissue calcification, ulceration or sloughing at the site of infiltration being the complications of sodium bicarbonate in an inexperienced hands. In such conditions, prompt elevation of the part, warmth and local injection of lignocaine or hyaluronidase are recommended to prevent sloughing.
Sodium bicarbonate has the pH ranging from 7 to 8.5; when combined with lignocaine hydrochloride, it reacts to form sodium chloride, water and carbon dioxide [9]. Sodium chloride further reduced to sodium and chlorine which enter the circulation. According to Catchlove [10], carbon dioxide produces an independent anesthetic effect by (1) a change in the charge of the local anesthetic inside the nerve (2) direct depressant effect of carbon dioxide on the nerve axon [3].
Acidic pH with the mean of 6.68 was reported to be evident in acutely inflamed periapical tissues [11]. In this study it was found that adding 8.4% of sodium bicarbonate to an already local anesthesia-injected site has reduced the sting on injection, reduced latency period, effective anesthetic effect, decreased pain and reduced post-injection tissue necrosis.
The onset of anesthesia occurred immediately after maxillary infiltration with buffered local anesthetics [12]. Kanna et al. [13] stated that the onset of anesthesia was within 46.9 s after infiltration with buffered LA. Batista da silva et al. [14] reported that comparing buffered and unbuffered solutions, buffered local anesthetics had a faster onset of anesthesia within 2 min.
Previous reports concluded that addition of sodium bicarbonate speeds the onset of action but not the duration [15–18]. The present study was in corroboration with the previous reports, which concluded that buffered anesthesia had a rapid onset of action within 2 min.
Previous study showed that there was no or least changes with the onset of anesthesia between 1% lignocaine with ph of 5, 1% lignocaine with ph of 6 and 1% of lignocaine with sodium bicarbonate to a ph of 7.35 [19, 20].
On comparing buffered and unbuffered local anesthetics in inferior alveolar nerve block, the previous reports revealed that there was no significant difference in pain reduction [20, 21]. However, same results were found with the use of 4% articaine buffered with sodium bicarbonate. [22].
Primosch et al. reported the use of buffered lidocaine for maxillary infiltration and concluded that there was no significant difference in pain and onset of anesthesia [9, 23]. This result was found to be in contradiction with previous reports [20, 24–26], whereas the present study, based on the objective and subjective sign of local anesthesia latency period, was found to be faster after injecting sodium bicarbonate. The mean was approximately 1–2 min, thereby explaining the early onset of anesthesia.
Although many studies have been highlighted the relation between increase in blood pressure and anxiety of the patients toward dental treatment, very few studies reported on the correlation between pain and pulse rate. This study also aims to compare the pulse rate and pain experienced by the patient during extraction.
A previous study stated that there was increase in pulse rate and blood pressure after injecting local anesthesia. This was due to endogenous release of adrenaline as a result of emotional stress and anxiety [27]. Takuya et al. reported significant increase in pulse rate and blood pressure during extraction. He stated that pain-related stress was the factor for the hemodynamic changes in the patients [28].
The results of the present study revealed increase in pulse rate when extreme pain was experienced by the patient. It was concluded that the injection of buffered local anesthesia proved to decrease the pain and pulse rate.
Conclusion
Buffered 2% lignocaine with 1:200,000 epinephrine had early onset of anesthesia when compared to unbuffered form. Injecting 2% buffered lignocaine pain was significantly reduced during extraction in the teeth.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Pandian Senthoor, Email: senthoorster@gmail.com.
Krishnamachari Janani, Email: jananikchari@gmail.com.
References
- 1.Hutchins HS, Young FA, Lackland DT, Fishburne CP. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44(3):87–89. [PMC free article] [PubMed] [Google Scholar]
- 2.Tu Y, Piascik M, Abel PW, Yagiela JA, Dowd FJ, Johnson BS, Mariotti AJ, Neidle EA, editors. Pharmacology and therapeutics for dentistry. 6. St. Louis: Mosby Elsevier; 2011. pp. 91–105. [Google Scholar]
- 3.Malamed S (2011) Buffering local anesthetics in dentisry. In: The Pulse of the Montana State Nurses' Association, Vol 44(1)
- 4.Malamed S. Handbook of local anesthesia. 6. St. Louis: Mosby; 2012. [Google Scholar]
- 5.Metzinger SE, Rigby PL, Bailey DJ. Local anesthesia in blepharoplasty: a new look? South Med J. 1994;87:225–227. doi: 10.1097/00007611-199402000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Metzinger SE, Bailey DJ, Boyce RG. Local anesthesia in rhinoplasty: a new twist? Ear Nose Throat J. 1992;71:405–406. doi: 10.1177/014556139207100910. [DOI] [PubMed] [Google Scholar]
- 7.Stewart JH, Chinn SE, Cole GW. Neutralized lidocaine with epinephrine for local anesthesia, part II. J Derm Surg Oncol. 1990;16:842–845. doi: 10.1111/j.1524-4725.1990.tb01570.x. [DOI] [PubMed] [Google Scholar]
- 8.McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesth Analg. 1987;66(6):572–574. doi: 10.1213/00000539-198706000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Primosch RE, Robinson I. Pain elicited during intraoral infiltration with buffered lidocaine. Am J Dent. 1996;9(1):5. [PubMed] [Google Scholar]
- 10.Catchlove RFH. Potentiation of two different local anaesthetics by carbon dioxide. Brit J Anaesth. 1973;45:471–473. doi: 10.1093/bja/45.5.471. [DOI] [PubMed] [Google Scholar]
- 11.Nekoofar MH, Namazikhah MS, Sheykhrezae MS, Mohammadi MM, Kazemi A, Aseeley Z, Dummer PMH. pH of pus collected from periapical abscesses. Int End J. 2009;42:534–538. doi: 10.1111/j.1365-2591.2009.01550.x. [DOI] [PubMed] [Google Scholar]
- 12.Brunetto PC, Ranali J, Ambrosano GMB, de Oliveira PC, Groppo FC, Meechan JG, Volpato MC. Anesthetic efficacy of 3 volumes of lidocaine with epinephrine in maxillary infiltration anesthesia. Anesth Prog. 2008;55:29–34. doi: 10.2344/0003-3006(2008)55[29:AEOVOL]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanaa MD, Whitworth JM, Corbett IP, Meechan JG. Articaine and lidocaine mandibular buccal infiltration anesthesia: a prospective randomized double-blind cross-over study. J Endod. 2006;32:296–298. doi: 10.1016/j.joen.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 14.Da Batista Silva C, Berto LA, Volpato MC, Ramacciato JC, Motta RHL, Ranali J. Groppo FC (2010) Anesthetic efficacy of articaine and lidocaine for incisive/mental nerve block. J Endod. 2010;36:438–441. doi: 10.1016/j.joen.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Christoph RA, Buchanan L, Begalia K, Schwartz S. Pain reduction in local anesthetic administration through pH buffering. Ann Emerg Med. 1998;17(2):117–120. doi: 10.1016/S0196-0644(88)80293-2. [DOI] [PubMed] [Google Scholar]
- 16.Sinnott CJ, Garfield JM, Thalhammer JG, Strichartz GR. Addition of sodium bicarbonate to lidocaine decreases the duration of peripheral nerve block in the rat. Anesth. 2000;93:1045–1052. doi: 10.1097/00000542-200010000-00028. [DOI] [PubMed] [Google Scholar]
- 17.Zahl K, Jordan A, McGroarty J, Sorensen B, Gotta AW. Peribulbar anesthesia effect of bicarbonate on mixtures of lidocaine, bupivacaine, and hyaluronidase with or without epinephrine. Ophthalmology. 1991;98:239–242. doi: 10.1016/S0161-6420(91)32311-X. [DOI] [PubMed] [Google Scholar]
- 18.Benson HT, Toleikis JR, Dixit P, Goodman I, Hill JA. Onset, intensity of blockade and somato sensory evoked potential changes of the lumbo sacral dermatomes after epidural anesthesia with alkalinized lidocaine. Anesth Analg. 1993;76:328–332. [PubMed] [Google Scholar]
- 19.McGlone R, Bodenham A. Reducing the pain of intradermal lignocaine injection by pH buffering. Arch Emerg Med. 1990;7(2):65–68. doi: 10.1136/emj.7.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whitcomb M, Drum M, Reader A, Nusstein J, Beck MA. A prospective, randomized, double-blind study of the anesthetic efficacy of sodium bicarbonate buffered with 2% lidocaine with 1:100,000 epinephrine in inferior alveolar nerve blocks. Anesth Prog. 2010;57(2):59–66. doi: 10.2344/0003-3006-57.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaney MA, Kerby R, Reader A, Beck FM, Meyers WJ, Weaver J. An evaluation of lidocaine hydrocarbonate compared with lidocaine hydrochloride for inferior alveolar nerve block. Anesth Prog. 1991;38:212–216. [PMC free article] [PubMed] [Google Scholar]
- 22.Shurtz R, Nusstein J, Reader A, Drum M, Fowler S, Beck M. Buffered 4% articaine as a primary buccal infiltration of the mandibular first molar: a prospective, randomized double-blind study. J Endod. 2015;41(9):1403–1407. doi: 10.1016/j.joen.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 23.Galindo A. pH-adjusted local anesthetics: clinical experience. Reg Anesth. 1983;8:35–36. [Google Scholar]
- 24.Rood JP. The use of buffered lignocaine solution in the presence of acute inflammation. J Dent. 1977;5:128–130. doi: 10.1016/0300-5712(77)90073-2. [DOI] [PubMed] [Google Scholar]
- 25.Younis I, Bhutiani RP. Taking the ‘ouch’ out—effect of buffering commercial xylocaine on infiltration and procedure pain—a prospective, randomized, double blind, controlled trial. Ann R Coll Surg Engl. 2004;86(3):213–217. doi: 10.1308/003588404323043382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruegg TA, Curran CR, Lamb T. Use of buffered lidocaine in bone marrow biopsies: a randomized, controlled trial. Oncol Nurs Forum. 2009;36:52–60. doi: 10.1188/09.ONF.52-60. [DOI] [PubMed] [Google Scholar]
- 27.Liau FL, Kok SH, Lee JJ, Kuo RC, Hwang CR, Yang PJ, et al. Cardiovascular influence of dental anxiety during local anesthesia for tooth extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:16–26. doi: 10.1016/j.tripleo.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 28.Tsuchihashi T, Takata Y, Kurokawa H, Miura K, Maruoka Y, Kajiyama M, Fujishima M. Blood pressure response during dental surgery. Hypertens Res. 1996;19:189–194. doi: 10.1291/hypres.19.189. [DOI] [PubMed] [Google Scholar]


