Abstract
Background
We systematically reviewed implementation research targeting depression interventions in low- and middle-income countries (LMICs) to assess gaps in methodological coverage.
Methods
PubMed, CINAHL, PsycINFO, and EMBASE were searched for evaluations of depression interventions in LMICs reporting at least one implementation outcome published through March 2019.
Results
A total of 8714 studies were screened, 759 were assessed for eligibility, and 79 studies met inclusion criteria. Common implementation outcomes reported were acceptability (n = 50; 63.3%), feasibility (n = 28; 35.4%), and fidelity (n = 18; 22.8%). Only four studies (5.1%) reported adoption or penetration, and three (3.8%) reported sustainability. The Sub-Saharan Africa region (n = 29; 36.7%) had the most studies. The majority of studies (n = 59; 74.7%) reported outcomes for a depression intervention implemented in pilot researcher-controlled settings. Studies commonly focused on Hybrid Type-1 effectiveness-implementation designs (n = 53; 67.1), followed by Hybrid Type-3 (n = 16; 20.3%). Only 21 studies (26.6%) tested an implementation strategy, with the most common being revising professional roles (n = 10; 47.6%). The most common intervention modality was individual psychotherapy (n = 30; 38.0%). Common study designs were mixed methods (n = 27; 34.2%), quasi-experimental uncontrolled pre-post (n = 17; 21.5%), and individual randomized trials (n = 16; 20.3).
Conclusions
Existing research has focused on early-stage implementation outcomes. Most studies have utilized Hybrid Type-1 designs, with the primary aim to test intervention effectiveness delivered in researcher-controlled settings. Future research should focus on testing and optimizing implementation strategies to promote scale-up of evidence-based depression interventions in routine care. These studies should use high-quality pragmatic designs and focus on later-stage implementation outcomes such as cost, penetration, and sustainability.
Key words: Depression interventions, Implementation outcomes, Implementation science, Implementation strategies, Low- and middle-income countries
Introduction
For adults globally, mental, neurologic, and substance-use (MNS) disorders are the greatest contributor to years lived with disability (YLDs) – accounting for almost one-third of all YLDs [Institute for Health Metrics and Evaluation (IHME), 2017]. This finding is true in both high-income and low- and middle-income countries (LMICs). Depression alone accounts for 35% of all YLDs for mental disorders in countries with a low socio-demographic index, and over 6% of YLDs from any health condition (IHME, 2017). Yet, even with this widespread recognition of MNS disorders – and depression in particular – as key drivers of global disability, the gap between knowledge of evidence-based prevention and treatment approaches in the literature and its application in community settings is large. In high-income settings, only one in five patients with depression receive minimally-adequate treatment, with gaps increasing to one in nine in upper-middle-income countries and 1 in 27 for lower-middle-income countries (Thornicroft et al., 2017). Others have written that a comprehensive ‘mental health care gap’ would likely be much larger, as it would include the biomedical treatment gap, combined with the psychosocial care gap as well as the physical health care gap (Pathare et al., 2018). The recent landmark Lancet Commission on Global Mental Health and Sustainable Development (Patel et al., 2018) highlighted that even amongst high-income countries that have increased access to, and use of, evidence-based treatments for mood disorders from 1990 to 2015, the population-level prevalence of these conditions has not decreased. In fact, from 1991 to 2016, the disability burden of MNS disorders has steadily increased across both low- and high-income countries, although the largest increases (almost a doubling) have been seen in low-income countries (Patel et al., 2018).
To address the particularly large depression care gap in LMICs, the past decade has seen increased investment in pragmatic effectiveness trials to generate the evidence-base for mental health treatment in LMICs. The Disease Control Priorities, 3rd Edition, states that sufficient evidence exists for effectiveness and cost-effectiveness for preventative, drug, physical interventions, and psychosocial interventions for individuals with depressive disorders globally (Patel et al., 2016). Due to very limited trained mental health human resources in LMICs (Saxena et al., 2007; Kakuma et al., 2011), many interventions tested to date in LMICs have employed task-shifting, using lay health workers or peers to deliver low-intensity behavioral interventions, often in collaboration with primary care staff who can deliver psychopharmacological or other higher-intensity interventions as needed. In the past few years, this evidence base for depression treatment has matured, with numerous pragmatic effectiveness trials across LMICs showing effectiveness for trans-diagnostic delivered psychological therapies (Bolton et al., 2014; Murray et al., 2014; Weiss et al., 2015; Rahman et al., 2016; Bryant et al., 2017; Bonilla-Escobar et al., 2018; Murray et al., 2018; Khan et al., 2019), problem solving therapy (Chibanda et al., 2016b), interpersonal psychotherapy (Bolton et al., 2003, 2007; Bass et al., 2006), behavioral activation (Chowdhary et al., 2016; Patel et al., 2017; Weobong et al., 2017), cognitive behavioral therapy (Rahman et al., 2008; Maselko et al., 2015), cognitive processing therapy (Bass et al., 2013), family-based interventions (Jordans et al., 2013; Betancourt et al., 2014, 2017), and stepped-care multi-component interventions (Araya et al., 2003; Rojas et al., 2007; Patel et al., 2010, 2011; Adewuya et al., 2018; Jordans et al., 2019), among others. However, of these effective interventions, few have moved beyond the pilot phase of researcher-controlled implementation in LMICs to routine implementation at scale and with quality (Wainberg et al., 2017).
Almost a decade ago, four of the five highest-priority Grand Challenges in Global Health highlighted by Collins et al. (2011) focused on improving the implementation of existing treatments and expanding access to care – hallmarks of the field of implementation science. Recently, there have been calls by researchers and funders alike to increase the focus of the field of global mental health on implementation science, given the rapidly maturing evidence-base for effective treatments in LMICs (Betancourt and Chambers, 2016). The field of implementation science focuses on developing, testing, and utilizing implementation strategies to optimize the delivery of evidence-based interventions in routine practice (Eccles and Mittman, 2006). Implementation science is highly interdisciplinary, leveraging methods across traditional clinical research, the social sciences, public health, economics, political science, industrial engineering, and business to develop, test, and employ implementation strategies – methods to enhance implementation outcomes for evidence-based interventions in routine practice (Proctor et al., 2013). Recently, the field has adopted specific recommendations for specifying implementation strategies (Proctor et al., 2013), and Powell et al. (2015) have developed an initial compilation of 73 distinct implementation strategies through the Expert Recommendations for Implementing Change (ERIC) project (Powell et al., 2015). The success of an implementation strategy is most often measured through improvements in the implementation outcomes of acceptability, adoption, appropriateness, cost, feasibility, fidelity, penetration, and sustainability targeting a given evidence-based intervention (Proctor et al., 2011). Given the large burden of mental disorders in LMICs and the persistent care and treatment gaps, the field of implementation science has a critical role to play as evidence-based interventions are scaled-up and optimized for delivery across LMICs.
The aim of the current study was to systematically review the existing studies focused on implementation science for depression interventions in LMICs. Given the evolving and multi-disciplinary nature of the field of implementation science, the specific terms used define it are heterogeneous and mixed. Thus, the current review included all studies conducted in an LMIC that reported an implementation outcome (Proctor et al., 2011) tied to an intervention [a program, practice, principle, procedure, product, pill, or policy (Brown et al., 2017)] addressing depression as at least one of the primary outcomes of interest. Given the preeminence of implementation strategies to the field of implementation science, we also abstracted implementation strategy information and coded according to ERIC classifications (Powell et al., 2015). We chose to focus the current review on implementation science for interventions addressing depression given it represents the largest individual burden of MNS conditions in LMICs. We hope that this paper can provide a summary of the state of implementation research for depression interventions in LMICs, and aid stakeholders in identifying gaps and prioritizing future work in this area.
Methods
Protocol, registration, and reporting guidelines
This project is registered in the PROSPERO international prospective register of systematic reviews under record ID CRD42018084203 and title ‘Implementation science for depression interventions in low- and middle-income countries: a systematic review’. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines for systematic reviews (Liberati et al., 2009), which is available in online Supplementary Appendix 1.
Search strategy
The lead author (BHW) searched four electronic bibliographic databases (PubMed; PsycINFO; CINAHL; and EMBASE) for articles published through 20 March 2019. We searched for articles including all four general search concepts, including: (1) depression; (2) an intervention, program, impact, or implementation; (3) implementation outcomes as defined by Proctor et al. (2011); and (4) studies conducted in LMICs, as defined by the World Bank Country and Lending Groups (2018). We developed a list of terms for each concept in collaboration with an information scientist. The PsycINFO search excluded dissertations, while the CINAHL focused only on scholarly peer-reviewed journals. See online Supplementary Appendix 2 for the detailed search strategy used.
Study selection
Studies were included that: (1) were published in English; (2) were based in an LMIC according to the World Bank at the time of study data collection (including low-income; lower-middle-income; and upper-middle-income economies) (World Bank Country and Lending Groups, 2018); and (3) reported an implementation outcome as defined by Proctor et al. (2011) tied to an intervention [a program, practice, principle, procedure, product, pill, or policy (Brown et al., 2017)] targeting depression as at least one of the primary outcomes of interest (see Table 1 for specific implementation outcome definitions used). Unpublished and non-peer-reviewed research studies were excluded. We utilized Covidence to import bibliographic data and screen/review studies (Covidence Systematic Review Software, 2020). Two independent reviewers from a team of five (BHW; WHH; CJ; DLA; and JMB) independently reviewed each abstract at the title/abstract, full-text review, and the extraction phase. Studies passed the title/abstract phase if depression was mentioned and it was possible that the study had been conducted in an LMIC. Disagreements were resolved through discussion until consensus was reached. Articles were excluded if the full-text was unavailable after consulting with an information scientist at the University of Washington.
Table 1.
Implementation outcome definitions used for systematic review based on Proctor's implementation outcome framework (Proctor et al., 2011)
| Implementation outcome | Narrative definition | Population reporting | Stage of implementation reported | Type of data reporting | Specific study inclusion criteria | Exclusion criteria |
|---|---|---|---|---|---|---|
| Acceptability | Satisfaction with various aspects of intervention or implementation strategy | Consumer; Implementer | Pre-implementation; During implementation; Post-implementation | Qualitative; Quantitative | Must report formal analyses of quantitative or qualitative results of satisfaction with specific depression intervention or implementation strategy being tested | Excluded if general service satisfaction not linked to specific depression intervention or implementation strategy; Excluded if descriptive without formal analyses of client or consumer perceptions |
| Adoption | Initial implementation, utilization, or intention to try intervention or implementation strategy | Implementer; Organization; Setting | Pre-implementation; During implementation | Quantitative | Must be able to calculate numerator and denominator (no. of implementers, organizations, or settings adopting or intending to adopt/no. of eligible) | Excluded if qualitative results on use or intent to use not allowing calculation of proportion adopting |
| Appropriateness | Perceived fit, relevance, compatibility, usefulness, or practicability of intervention or implementation strategy | Consumer; Implementer; Organization; Setting | Pre-implementation | Qualitative; Quantitative | Must report formal qualitative or quantitative analyses of pre-implementation perceived fit of specific depression intervention or implementation strategy being tested | Excluded if general service appropriateness not focused on intervention or strategy of interest; Excluded if descriptive without formal analyses of client or consumer perceptions |
| Feasibility | Actual fit, relevance, compatibility, usefulness, or practicability of intervention or implementation strategy | Consumer; Implementer; Organization; Setting | During implementation; Post-implementation | Qualitative; Quantitative | Must report formal quantitative or qualitative analyses of post-implementation actual fit of specific depression intervention or implementation strategy being tested | Excluded if general service feasibility not focused on intervention or strategy of interest; Excluded if descriptive without formal analyses of client or consumer experiences |
| Fidelity | Degree to which an intervention or implementation strategy was implemented as intended | Implementer | During implementation | Quantitative | Must report formal analyses of fidelity to intervention or implementation strategy of interest; must be able to calculate numerator and denominator of (no. of implementers achieving fidelity/no. of implementing) | Excluded if general quality of care or delivery not focused on intervention or strategy of interest; Excluded if qualitative results on fidelity that do not allow calculation of proportion achieving fidelity |
| Cost | Cost of intervention or strategy delivery | Implementer; Organization; Setting | Post-implementation | Quantitative | Must report actual dollar amounts of implementation cost of intervention or implementation strategy of interest | Excluded if general costs of service delivery not tied to intervention or strategy of interest |
| Penetration | Degree of integration of intervention or implementation strategy within service setting and subsystems in non-controlled settings | Consumer; Implementer; Organization; Setting | During implementation; Post-implementation | Quantitative | Must be able to calculate numerator and denominator of either (no. of implementers, organizations, or settings delivering intervention or implementation strategy/no. of eligible) or (no. of consumers using a given intervention/no. of eligible); Depression intervention must be under routine institutional implementation, rather than controlled by researchers or external implementers | Excluded if results do not allow calculation of proportion utilizing intervention or implementation strategy with depression intervention delivered under routine conditions; Excluded if depression intervention under researcher-controlled implementation and not institutional implementation |
| Sustainability | Extent to which an intervention or implementation strategy is maintained within service setting's ongoing, stable operations | Organization; Setting | During implementation; Post-implementation | Qualitative; Quantitative | Defined as measurement of maintenance (either quantitative or qualitative) or ‘intent-to-continue use’ after initial pilot research-based funding has been rescinded and implementation is progressing under routine care conditions | Excluded if measurement only occurred during pilot research-based funding; Excluded if general sustainability not targeting intervention or implementation strategy of interest |
Data abstraction
Four authors (BHW; CJ; DLA; and JMB) independently piloted a structured abstraction form with five studies; all co-authors reviewed, critiqued, suggested improvements, and approved the final version. Two authors (BHW and WHH) independently abstracted study, intervention, and implementation strategy characteristics. After independently abstracting study information, the two authors (BHW and WHH) verified each abstraction, resolving any disagreement through discussion until consensus was reached. At the study level, we collected: (1) the year the study was published; (2) country and region of the study as defined by the World Bank in 2018 (World Bank Country and Lending Groups, 2018); (3) the primary research study design; (4) implementation outcomes reported; (5) detailed information on the depression intervention of interest; and (6) detailed information on implementation strategies tested (see Table 2 for categories of data abstraction).
Table 2.
Study, depression intervention, implementation strategy, and implementation outcome descriptive statistics (N = 79)
| Characteristic | N (%), unless noted |
|---|---|
| Study characteristics | |
| Published year, median (range) | 2016 (2003–2019) |
| Region | |
| East Asia and Pacific | 8 (10.1) |
| Europe and Central Asia | 2 (2.5) |
| Latin America and Caribbean | 13 (16.5) |
| Middle East and North Africa | 3 (3.8) |
| South Asia | 23 (29.1) |
| Sub-Saharan Africa | 39 (36.7) |
| Primary research study design | |
| Mixed-methods | 27 (34.2) |
| Qualitative | 9 (11.4) |
| Quasi-experimental – controlled pre-post | 3 (3.8) |
| Quasi-experimental – uncontrolled pre-post | 17 (21.5) |
| Quasi-experimental – uncontrolled interrupted time-series | 0 (0) |
| Quasi-experimental – controlled interrupted time-series | 0 (0) |
| Quasi-experimental – regression discontinuity | 0 (0) |
| Quasi-experimental – other | 0 (0) |
| Randomized controlled trial – cluster | 7 (8.9) |
| Randomized controlled trial – individual | 16 (20.3) |
| Phase of implementation researcha | |
| Pre-implementation assessment | 4 (5.1) |
| Hybrid Type-1 | 53 (67.1) |
| Hybrid Type-2 | 0 (0.0) |
| Hybrid Type-3 | 16 (20.3) |
| T3 | 2 (2.5) |
| T4-1 | 4 (5.1) |
| T4-2 | 0 (0.0) |
| De-implementation (any phase) | 0 (0.0) |
| Implementation outcome characteristicsb | |
| Proctorc implementation outcome reported | |
| Acceptability | 50 (63.3) |
| Adoption | 4 (5.1) |
| Appropriateness | 14 (17.7) |
| Feasibility | 28 (35.4) |
| Fidelity | 18 (22.8) |
| Cost | 14 (17.7) |
| Penetration | 4 (5.1) |
| Sustainability | 3 (3.8) |
| Depression intervention characteristics | |
| Stage of implementation of depression intervention | |
| Pilot researcher-controlled implementation | 59 (74.7) |
| Delivered in routine care | 20 (25.3) |
| Undergoing de-implementation | 0 (0.0) |
| Implementation location of depression intervention | |
| Community | 30 (38.0) |
| Health facility | 47 (59.5) |
| Multi-level | 2 (2.5) |
| Population implementing depression intervention | |
| Community members | 7 (8.9) |
| Non-specialist healthcare workers | 36 (45.6) |
| Nurses | 6 (7.6) |
| Primary care physicians | 8 (10.1) |
| Psychiatrists | 2 (2.5) |
| Psychologists | 3 (3.8) |
| Technology-based delivery | 8 (10.1) |
| Multiple implementers | 9 (11.4) |
| Modality of depression intervention | |
| Activity-based | 3 (3.7) |
| Counseling | 2 (2.5) |
| Education/information | 1 (1.2) |
| Group counseling | 1 (1.2) |
| Group psychotherapy | 14 (17.3) |
| Individual psychotherapy | 30 (38.0) |
| Medication | 3 (3.7) |
| Multicomponent | 27 (33.3) |
| Implementation strategy characteristics | |
| ERICd classification of implementation strategy | |
| Not testing implementation strategy – testing intervention | 58 (73.4) |
| Conduct ongoing training | 3 (3.8) |
| Create new clinical teams | 1 (1.3) |
| Develop a formal implementation blueprint | 1 (1.3) |
| Distribute educational materials | 1 (1.3) |
| Facilitate relay of clinical data to providers | 3 (3.8) |
| Increase demand | 1 (1.3) |
| Provide clinical supervision | 1 (1.3) |
| Revise professional roles | 10 (12.7) |
| Implementation location of implementation strategy | |
| Not testing implementation strategy – testing intervention | 58 (73.4) |
| Community | 6 (7.6) |
| Health facility | 14 (17.7) |
| District | 1 (1.3) |
| Focal population utilizing implementation strategy | |
| Not testing implementation strategy – testing intervention | 58 (73.4) |
| Community members | 1 (1.3) |
| Non-specialist healthcare workers | 11 (13.9) |
| Nurses | 3 (3.8) |
| Primary care physicians | 4 (5.1) |
| Policy makers | 1 (1.3) |
| Multiple | 1 (1.3) |
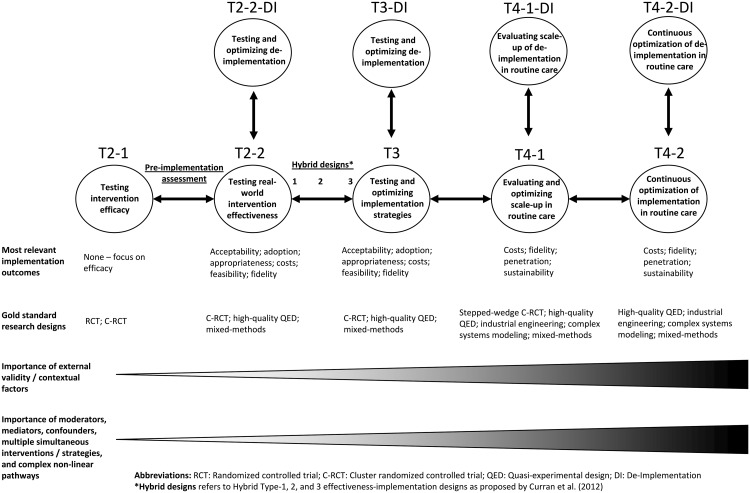
Phase of implementation research is defined as per Fig. 1.
More than one implementation outcome possible, thus, total percentages exceed 100%.
Implementation outcomes were defined as per Proctor's implementation outcome framework (Proctor et al., 2011).
ERIC classification refers to the Expert Recommendations for Implementing Change project and the list of 73 distinct implementation strategies (Powell et al., 2015).
We defined implementation outcomes using the Proctor implementation outcomes framework (Proctor et al., 2011) (see Table 1). All implementation outcomes required actual measurement and data reporting from target populations; for example, qualitative narrative descriptions of overall ‘lessons learned’ without explicit data reporting were excluded.
We defined the phase of implementation research for each study across a modified translational research continuum (see Fig. 1). Building on consensus definitions from systematic reviews (Fort et al., 2017) and recent efforts to situate implementation research in the traditional translational research continuum (Brown et al., 2017), we envision depression interventions progressing from studies testing depression interventions for efficacy in highly-controlled settings (T2-1), to pragmatic intervention effectiveness trials with increased focus on external validity (T2-2). These studies come before those focused on testing and optimizing of implementation strategies for a given depression intervention (T3). This T3 phase has been titled ‘pure implementation research’ by Curran et al. (2012) and most often occurs after clinical intervention effectiveness has been shown. Hybrid effectiveness-implementation trials aim to speed the transition from pragmatic effectiveness trials (T2-2) to pure implementation research (T3) and the eventual work to evaluate and optimize the scale-up of evidence-based interventions for population health impact in T4-1. Following Curran et al. (2012), we defined Hybrid Type-1 as those studies with a primary aim of assessing intervention effectiveness and a secondary aim to report implementation outcomes for a depression intervention. Process evaluations published separately from main trial outcomes but embedded in larger Hybrid Type-1 studies were coded as Hybrid Type-1. Studies were coded as a ‘pre-implementation assessment’ if they reported implementation outcomes prior to implementation of a given depression intervention or strategy. In Fig. 1 we situate these studies as occurring before T2-2, as in our review they most commonly occurred before depression intervention effectiveness testing. Hybrid Type-2 studies were coded as having dual primary aims of assessing intervention effectiveness and testing an implementation strategy. Hybrid Type-3 studies were coded as having the primary aim of testing an implementation strategy while reporting on intervention effectiveness or patient-level outcomes. We define phase T4-1 as studies focused on evaluating and optimizing the scale-up of interventions and strategies in routine care for population health impact. We anticipate that these studies will often make use of known evidence-based implementation strategies found effective in stage T3. The last stage of the translational research continuum (T4-2) is the continuous optimization and improvement of ongoing routine delivery of an intervention that is being delivered at scale. This phase could follow models being proposed of ‘embedded research’ (Churruca et al., 2019; Lieu and Madvig, 2019) and/or ‘learning evaluation’ (Balasubramanian et al., 2015) where implementation researchers and practitioners collaborate to continuously improve the delivery of ongoing evidence-based interventions in routine systems. We consider de-implementation as occurring at each phase of the implementation research continuum. For example, while testing real-world intervention effectiveness (T2-2), one could also nest simultaneous study of de-implementation of other ineffective, wasteful, or harmful interventions targeting the same population (T2-2-DI).
Fig. 1.
Situating implementation outcomes, research designs, and other key factors across the translational highway from efficacy research (T2-1) to continuous optimization of implementation in routine care (T4-2).
We defined the depression intervention as the specific proximal program, practice, principle, procedure, product, pill, or policy (Brown et al., 2017) that targeted depression symptoms. For depression intervention data abstraction, we coded the level of implementation as pilot researcher-controlled implementation, whether a given depression intervention was implemented in routine care, or whether the study was focused on de-implementation of a depression intervention. We also abstracted the implementation location of the depression intervention, the population implementing the intervention, and the modality of the depression intervention. Activity-based modalities were defined as depression interventions focused on a specific behavior for decreasing symptoms, such as running, yoga, or meditation. Counseling was defined as general one-on-one meetings not focused on a specific psychotherapy, such as general HIV or life-skills counseling. Education/information was defined as passive delivery of knowledge outside of a psychotherapy or counseling context, such as pamphlets or radio spots.
We coded implementation strategies only if the primary focus of the study was testing the effect of an implementation strategy, rather than testing the effects of a depression intervention. For studies meeting these criteria, we abstracted the implementation location of a given implementation strategy, the focal population utilizing the implementation strategy, and coded implementation strategy modalities according to the ERIC project's compilation of 73 distinct implementation strategies (Proctor et al., 2013; Powell et al., 2015).
Analysis
We imported our final reporting excel sheet into Stata 15 for analyses. Analyses focused on generating a qualitative summary of research aims, methods, approaches, implementation outcomes, implementation strategies, and depression interventions tested to date to inform future research. Descriptively, we calculated percentages for categorical variables and for our continuous variable, year study was published, we calculated the median and range. Quantitative meta-analyses of study findings were not an aim of the current study given the heterogeneity in research questions, depression interventions, implementation strategies, and outcomes reported. See online Supplementary File S1 for full data abstraction form and study data.
Results
Study selection
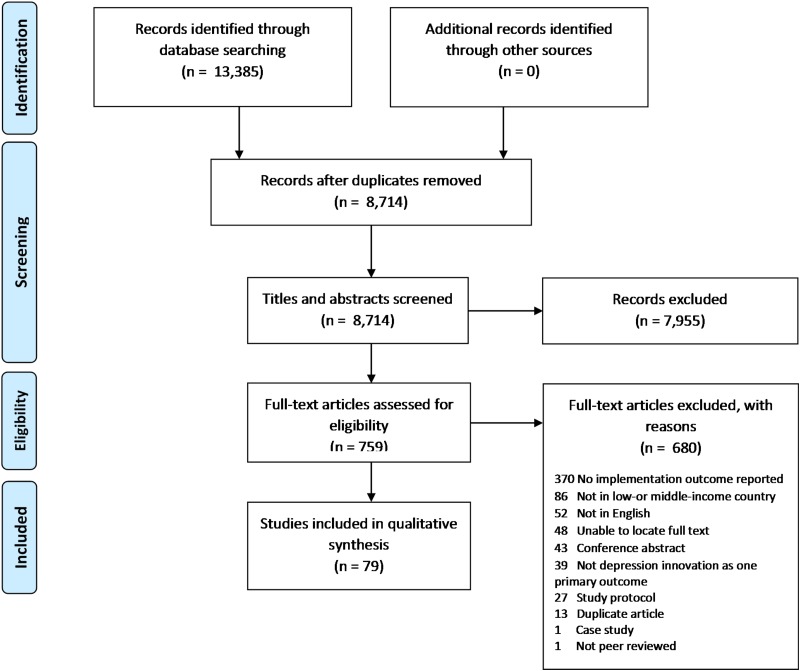
A total of 8714 unique studies were screened and 759 full-text articles were assessed for eligibility. Of these, 79 studies met our inclusion criteria (see Fig. 2 for PRISMA flow diagram). Of the 680 studies that were excluded at the full-text phase, the primary reason for exclusion was not reporting an implementation outcome (n = 370; 54.4%), not occurring in an LMIC (n = 86; 12.6%), not published in English (n = 52; 7.6%), and unable to locate the article full text (n = 48; 7.1%).
Fig. 2.
PRISMA flow diagram.
Study characteristics
The 79 studies in our sample were published between 2003 and 2019, with the median published in 2016 and the mean being published in late 2014 (see Table 2). The number of studies has increased since 2015, with less than 10 studies published every year from 2003 to 2015, compared to 12 studies in 2016, 10 studies in 2017, 15 studies in 2018, and 8 studies published through 20 March 2019. The first three studies, published between 2003 and 2006, reported: (1) adoption and cost for the implementation strategy of ongoing training of primary health care nurses for depression treatment in Zimbabwe (Abas et al., 2003); (2) acceptability and fidelity of a psycho-educational depression intervention in Mexico (Lara et al., 2004); and (3) the costs associated with a multi-component stepped-care depression program for treating women with depression in Chile (Araya et al., 2006).
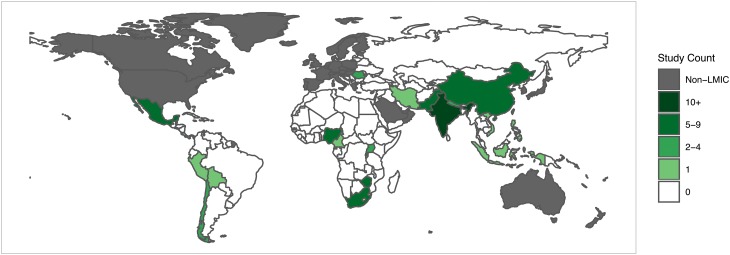
The majority of studies were from Sub-Saharan Africa (n = 39; 36.7%), although only eight total countries in this region were represented, with South Africa (n = 9; 31.0%), Zimbabwe (n = 6; 20.7%), and Nigeria (n = 6; 20.7%) accounting for more than half of all articles published in the region (see Fig. 3 for world map of included studies). South Asia had the second greatest representation with 23 studies (29.1%); however, these were from only three countries: India (n = 14; 60.1%), Pakistan (n = 6; 26.1%), and Nepal (n = 3; 13.0%). Thirteen studies (16.5%) were from Latin America and the Caribbean, with the majority of studies coming from Mexico (n = 5; 38.5%) and Chile (n = 4; 30.8%). East Asia and the Pacific had relatively poor representation with only eight total studies (10.1%). Only five total studies were conducted across Europe and Central Asia (n = 2; 2.5%) and Middle East and North Africa (n = 3; 3.8%).
Fig. 3.
Thematic world map for distribution of included studies (N = 79).
In terms of primary study designs, the most common design was mixed-methods (n = 27; 34.2%), using both qualitative and quantitative methods to address specific primary research questions. In terms of studies utilizing primary quantitative research study designs (n = 43; 54.4%), the most common design was quasi-experimental uncontrolled pre-post (n = 17; 21.5%), followed by individual randomized trials (n = 16, 20.3%), cluster randomized trials (n = 7; 8.9%), and quasi-experimental controlled pre-post designs (n = 3; 3.8%). No studies used quasi-experimental designs with the strongest causal inference, such as controlled interrupted time-series or regression discontinuity. Nine studies used pure qualitative research designs (11.4%).
In terms of phase of implementation research, the majority of studies were Hybrid Type-1 effectiveness-implementation designs (n = 53; 67.1), followed by Hybrid Type-3 designs (n = 16; 20.3), pre-implementation assessments (n = 4; 5.1%), T4-1 (n = 4; 5.1%), and T3 (n = 2; 2.5%). No studies assessed de-implementation at any phase, utilized Hybrid Type-2 designs, or targeted the last phase of T4-2. Three of the four studies targeting phase T4-1 were conducted in Chile (Vicente et al., 2007; Alvarado et al., 2012; Araya et al., 2012), with one study from Zimbabwe (Chibanda et al., 2016a). For example, Araya et al. (2012) conducted a mixed-methods study reporting on feasibility, cost, and sustainability to inform the optimization of implementation strategies for the National Depression Detection and Treatment Program which was in the process of scale-up across routine primary care in Chile. Similarly, Chibanda et al. (2016a) reported initial appropriateness and adoption of the ‘Friendship Bench’ program as it was in the process of being scaled-up across 60 primary care facilities in Zimbabwe.
Implementation outcome characteristics
The 79 studies in our sample focused primarily on reporting early-stage implementation outcomes of acceptability (n = 50; 63.3%), feasibility (n = 28; 35.4%), and appropriateness (n = 14; 17.7%). Fidelity was also commonly measured (n = 19; 22.8%), as was cost (n = 14; 17.7%). Very few studies reported adoption (n = 4; 5.1%) or the later-stage implementation outcomes of penetration (n = 4, 5.1%) or sustainability (n = 3, 3.8%). In terms of studies reporting less-commonly reported implementation outcomes, Adewuya et al. (2018) reported adoption as the percentage of trained nurses (95.2%) who actively were delivering a pilot multicomponent screening, psychoeducation, psychological therapy, and medication intervention in primary care settings in Nigeria. Chatterjee et al. (2008) reported penetration as the percentage of patients (53%) who tested positive for a common mental disorder – including depression – who received the first session of psycho-education in their project testing the revision of professional roles (task-shifting) for a multicomponent depression intervention in routine primary care in India. Abas et al. (2016) reported on the quantitative sustainability of ‘Friendship Bench’ project activities up to 8 years after the initial pilot project ended and the depression intervention was formally integrated into routine care settings in Zimbabwe.
Depression intervention characteristics
Seventy-five percent (n = 59) of depression interventions included in the studies occurred as part of pilot researcher-controlled implementation, rather than being implemented under routine care conditions. For example, in a Hybrid Type-1 study, Khan et al. (2019) reported the acceptability, feasibility, and initial clinical outcomes for patients attended by lay health workers randomized to implement group-based problem management plus (PM+) compared with enhanced usual care in Pakistan. Thus, the primary aim of this study was to test group PM+ as a novel depression intervention rather than testing an implementation strategy to enhance implementation outcomes for a depression intervention being delivered in routine implementation settings, as would occur in a Hybrid Type-3 or T3 study (see Table 3 for detailed study descriptions). By contrast, in a Hybrid Type-3 study, Shidhaye et al. (2017) reported the costs associated with an implementation strategy focused on increasing population-level demand for the existing routine depression care. The primary aim of their study was increase contact coverage of existing routinely-implemented depression interventions.
Table 3.
Included studies (N = 79) and associated detailed study, intervention, and implementation strategy information
| N | Author | Country | Research objectives | Description of primary depression intervention (implementing agent; where implemented; modality) | Description of primary implementation strategy (implementing agent; where implemented; ERIC classification) | Primary study design | Phase of implementation research | Depression intervention implementation stage | Implementation outcomes reported |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Abas et al. (2003) | Zimbabwe | Explore barriers and facilitators to care of those with common mental disorders using routinely available data and face-to-face interviews with primary care staff, in public primary care clinics Harare | Multicomponent intervention delivered to community members by nurses at the facility level | Ongoing training conducted by nurses at the facility level | Mixed Methods | T3 | Routine care | Adoption Cost |
| 2 | Abas et al. (2016) | Zimbabwe | Investigate acceptability and implementation of the ‘Friendship Bench Project’ using mixed-methods, 4-8 years after initial pilot study in Zimbabwe | Individual psychotherapy delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Routine care | Acceptability Feasibility Sustainability |
| 3 | Abas et al. (2018) | Zimbabwe | Pilot a task-shifted intervention to enhance adherence to HIV medication and improve depression outcomes in people living with HIV in Zimbabwe | Individual psychotherapy delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility Fidelity |
| 4 | Abi Ramia et al. (2018) | Lebanon | Conduct bottom-up, community-driven qualitative cognitive interviewing from a multi-stakeholder perspective to inform the cultural adaptation of an Internet-delivered mental health intervention in Lebanon | Individual psychotherapy intervention delivered to community members through technology at the community level | Primary focus is evaluating depression intervention | Qualitative | Pre-implementation assessment | Pilot researcher-controlled implementation | Appropriateness |
| 5 | Adams et al. (2012) | Tanzania | Investigate feasibility of nurse-led antidepressant medication management of depression in an HIV clinic in Tanzania | Medication delivered to community members by nurses at the facility level | Nurses revising professional roles at the facility level | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-3 | Routine care | Fidelity |
| 6 | Adewuya et al. (2018) | Nigeria | Develop and test the feasibility of a primary care worker-led psychological intervention as the main feature of a collaborative stepped care intervention for depression in Nigeria | Multicomponent intervention delivered to community members by multiple providers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Adoption Appropriateness Feasibility Fidelity |
| 7 | Alampay et al. (2019) | Philippines | Examine the feasibility and acceptability of a local adaptation of a mindfulness-based cognitive therapy (MBCT) program for Filipino school children, facilitated by trained public school teachers | Group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 8 | Alvarado et al. (2012) | Chile | Evaluate a depression intervention implemented in the primary care setting in Chile | Multicomponent intervention delivered to community members by primary care physicians at the facility level | Primary care physicians revising professional roles at the facility level | Quasi-Experimental – Uncontrolled Pre-Post | T4-1 | Routine care | Cost Sustainability |
| 9 | Andersen et al. (2016) | South Africa | Pilot a nurse-delivered cognitive behavioral therapy intervention (‘Ziphamandla’) to enhance adherence to HIV medication and improve depression in people living with HIV in South Africa | An individual psychotherapy intervention delivered to community members by nurses at the facility level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Fidelity |
| 10 | Araya et al. (2006) | Chile | Evaluate the cost-effectiveness of a pilot depression treatment program for low-income women in the primary care setting in Santiago, Chile | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 11 | Araya et al. (2012) | Chile | Evaluate the scale-up of a depression treatment program in the primary care setting in Chile | A multicomponent intervention delivered to community members by primary care physicians at the facility level | Primary care physicians revising professional roles at the facility level | Mixed Methods | T4-1 | Routine care | Feasibility Cost Sustainability |
| 12 | Asunción Lara et al. (2014) | Mexico | Describe a 4-year study monitoring the use of HDep, (‘Help for Depression’ or ADep, ‘Ayuda Para Depression’), an open access/free web-based, psycho-education, cognitive-behavioral intervention program in Mexico | An individual psychotherapy intervention delivered to community members by community members at the community level | Community members using mass media at the national level | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-3 | Pilot researcher-controlled implementation | Acceptability |
| 13 | Lara et al. (2004) | Mexico | Investigate the degree of fidelity with which a psycho-educational intervention for women with depressive symptoms was delivered in Mexico | A group psychotherapy intervention delivered to community members by psychologists at the facility level | Primary focus is evaluating depression intervention | Qualitative | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Fidelity |
| 14 | Atif et al. (2016) | Pakistan | Identify barriers and facilitators to delivering the ‘Barefoot Therapists’ maternal mental health intervention through peer volunteers in Pakistan | Individual psychotherapy intervention delivered to community members by non-specialist healthcare workers in the community setting | Primary focus is evaluating depression intervention | Qualitative | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 15 | Atif et al. (2017) | Pakistan | Evaluate the adaptation and feasibility of the ‘Mother to Mother’ implementation of the therapy intervention ‘The Thinking Healthy Programme’ among mothers in India and Pakistan | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers in the community setting | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 16 | Beardslee et al. (2011) | Costa Rica | Describe the adaptation of an evidence-based preventive depression-focused intervention for eventual widespread use in Costa Rica | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Qualitative | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 17 | Bella-Awusah et al. (2016) | Nigeria | Determine the effectiveness of a school-based cognitive behavioral therapy program (CBT) on adolescents with depression in southwestern Nigeria | A group psychotherapy intervention delivered to community members by psychiatrists at the community level | Primary focus is evaluating depression intervention | Cluster Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 18 | Betancourt et al. (2014) | Rwanda | Assess the feasibility and acceptability of an intervention to reduce mental health problems and bolster resilience among children in households affected by caregiver HIV in Rwanda | A multicomponent intervention delivered to community members by psychologists at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Fidelity |
| 19 | Betancourt et al. (2017) | Rwanda | Pilot the ‘Family Strengthening Intervention’, a family home-visit intervention designed to promote mental health and improve parent-child relationships in families with caregivers living with HIV in Rwanda | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 20 | Burton et al. (2016) | Romania | Conduct a pilot RCT of Help4Mood, an interactive system with an embodied virtual agent (avatar) to assist in self-monitoring of patients receiving treatment for depression in Romania, Spain, and Scotland and the UK and evaluate the system use and acceptability of the pilot | A multicomponent intervention delivered to community members by technology at the community level | Primary focus is evaluating depression intervention | Cluster Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 21 | Buttorff et al. (2012) | India | To carry out an economic evaluation of a task-shifting intervention for the treatment of depressive and anxiety disorders in primary-care settings in Goa, India | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the facility level | Non-specialist healthcare workers revising professional roles at the facility level | Randomized Controlled Trial | Hybrid Type-3 | Routine care | Cost Penetration |
| 22 | Chatterjee et al. (2008) | India | Integrate the MANAS intervention, an evidence-based treatment for common mental disorders, into routine primary care in Goa, India | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the facility level | Non-specialist healthcare workers revising professional roles at the facility level | Mixed Methods | Hybrid Type-3 | Routine care | Acceptability Appropriateness Feasibility Penetration |
| 23 | Chibanda et al. (2011) | Zimbabwe | Pilot a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV in Zimbabwe | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Feasibility |
| 24 | Chibanda et al. (2016a) | Zimbabwe | Scale-up a depression intervention delivered by lay health workers in primary care facilities in Zimbabwe | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | T4-1 | Routine care | Appropriateness Adoption |
| 25 | Chowdhary et al. (2016) | India | Evaluate The Healthy Activity Program, a lay counselor-delivered treatment for severe depression in India | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Appropriateness Feasibility |
| 26 | Diez-Canseco et al. (2018) | Peru | Design, develop, and test a strategy to promote early detection, optimize referral, and access to treatment of patients with mental disorders attending public primary health care services in Lima, Peru | A multicomponent intervention delivered to community members by primary care physicians at the facility level | Primary care physicians revising professional roles at the facility level | Mixed Methods | Hybrid Type-3 | Routine care | Appropriateness Feasibility Penetration |
| 27 | Doumit et al. (2018) | Lebanon | Assess the feasibility, acceptability, and preliminary effects of a cognitive-behavioral intervention [Creating Opportunities for Patient Empowerment (COPE)] on depression, anxiety, and quality of life (QOL) in a sample of adolescent refugees in Lebanon | A group psychotherapy intervention delivered to community members by multiple providers at the community level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 28 | Duffy et al. (2017) | Zimbabwe | Pilot a nurse-led integration of mental health and HIV services in Zimbabwe | A multicomponent intervention delivered to community members by nurses at the facility level | Non-specialist healthcare workers revising professional roles at the facility level | Mixed Methods | Hybrid Type-3 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 29 | Dwommoh et al. (2018) | South Africa | Investigate the cost-effectiveness of a brief motivational interviewing (MI) intervention v. a combined intervention of MI and problem-solving therapy (MI-PST) for reducing substance use and depression among patients presenting to emergency departments in South Africa | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 30 | Fisher et al. (2014) | Vietnam | Adapt and field-test the Thinking Healthy Program (THP) for perinatal depression and anxiety treatment in Vietnam | A group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Appropriateness |
| 31 | Fuhr et al. (2019) | India | Assess the effectiveness and cost-effectiveness of the Thinking Healthy Programme (THP) when peer-delivered in Goa, India | An individual psychotherapy intervention delivered to community members by community members at the community level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 32 | Gallegos et al. (2012) | Mexico | Evaluate the effectiveness of the FRIENDS for Life program, a social and emotional skills program implemented in an orphanage in Mexico | A group psychotherapy intervention delivered to community members by community members at the community level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 33 | Guo et al. (2018) | China | Implement an mHealth intervention program for people living with HIV in China via the popular social media app WeChat | An education/information intervention delivered to community members through technology at the community level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 34 | Gureje et al. (2015) | Nigeria | Pilot a program integrating mental health into primary care in Osun State, Nigeria | A multicomponent intervention delivered to community members by multiple providers at the facility level | Multiple providers conducting ongoing training at the facility level | Quasi-Experimental – Uncontrolled Pre-Post | T3 | Routine care | Fidelity |
| 35 | Gureje et al. (2019) | Nigeria | Compare high-intensity treatment (HIT) with low-intensity treatment (LIT) for perinatal depression in Nigeria | An individual psychotherapy intervention delivered to community members by nurses at the facility level | Primary focus is evaluating depression intervention | Cluster Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 36 | Hashemi et al. (2012) | Iran | Compare the efficacy of nortriptyline with that of fluoxetine in the treatment of patients with major depressive disorder in Iran | A medication intervention delivered to community members by primary care physicians at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Control Trial | Hybrid Type-1 | Routine care | Acceptability |
| 37 | Isa et al. (2018) | Nigeria | Investigate the effects of a psychological intervention that includes psycho-education and basic elements of cognitive behavioral therapy (CBT) on medication-treated adolescents with depression in Nigeria | A group psychotherapy intervention delivered to community members by psychiatrists at the facility level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 38 | Janevic et al. (2016) | Bolivia | Evaluate the feasibility of an automated telephonic interactive voice response (IVR) depression self-care service among Bolivian primary care patients | A counseling intervention delivered to community members through technology at the community level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 39 | Jordans et al. (2013) | Burundi | Evaluate the impact of a brief parenting psychoeducation intervention on children's mental health in Burundi | A group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Quasi-Experimental – Controlled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 40 | Jordans et al. (2019) | Nepal | Evaluate the impact of a district mental healthcare plan for depression, psychosis, alcohol use disorder, and epilepsy as part of the Programme for Improving Mental Health Care (PRIME) in Chitwan District, Nepal | A multicomponent intervention delivered to community members by multiple providers at the multiple levels | Policy-makers developing a formal implementation blueprint at the district level | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-3 | Pilot researcher-controlled implementation | Fidelity Penetration |
| 41 | Khan et al. (2019) | Pakistan | Evaluate the feasibility and acceptability of the locally adapted Group Problem Management Plus (PM+) intervention for women in the conflict-affected settings in Swat, Pakistan | A group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Cluster Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 42 | Maulik et al. (2016) | India | Implement an approach incorporating mobile-based electronic decision support systems (EDSS) to provide services for common mental disorders, combined with a community-based anti-stigma campaign, in Andhra Pradesh, India | A multicomponent intervention delivered to community members by primary care physicians at the facility level | Non-specialist healthcare workers at the community level facilitating the relay of clinical data to providers at the facility level | Mixed Methods | Hybrid Type-3 | Routine care | Acceptability Feasibility |
| 43 | McIntyre et al. (2018) | South Africa | Examine the application of Mindfulness Based Stress Reduction (MBSR) for HIV-infected individuals in South Africa | An activity-based intervention delivered to community members by primary care physicians at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 44 | Mehrotra et al. (2018) | India | Develop and pilot-test PUSH-D (Practice and Use Self-Help for Depression), a self-help intervention for depression, in an urban setting in India | An individual psychotherapy intervention delivered to community members by technology at the community level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 45 | Munodawafa et al. (2017) | South Africa | Explore the lay counselor experience of delivering a task-shared psycho-social intervention for perinatal depression in Khayelitsha, South Africa | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at multiple levels | Primary focus is evaluating depression intervention | Qualitative | Hybrid Type-1 | Pilot researcher-controlled implementation | Feasibility Fidelity |
| 46 | Murray et al. (2014) | Multiple (Iraq; Thailand) | Describe the Common Elements Treatment Approach (CETA) for adults presenting with mood or anxiety problems developed specifically for use with lay counselors in low- and middle-income countries | An individual psychotherapy intervention delivered to community members by community members at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Adoption Fidelity |
| 47 | Myers et al. (2019) | South Africa | Examine the feasibility and acceptability of integrating into chronic disease care two approaches to community health worker-delivered mental health counseling in South Africa | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Feasibility |
| 48 | Nakimuli-Mpungu et al. (2014) | Uganda | Assess the feasibility, acceptability and impact on depression, functioning, social support and self-esteem of a manualized culturally sensitive group support psychotherapeutic intervention for depressed HIV-affected Ugandan adults | A group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Quasi-Experimental – Controlled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 49 | Nakimuli-Mpungu et al. (2017) | Uganda | Evaluate the effectiveness of a group support psychotherapy for depression treatment among people with HIV/AIDS in northern Uganda | A group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility Fidelity |
| 50 | Naveen et al. (2013) | India | Develop and pilot a yoga therapy module for patients with depression in India | An activity-based intervention delivered to community members by community members at the community level | Primary focus is evaluating depression intervention | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Appropriateness |
| 51 | Oladeji et al. (2015) | Nigeria | Pilot a stepped care intervention package for depression in the primary care setting in Nigeria | A multi-component intervention delivered to community members by non-specialist healthcare workers at the facility level | Non-specialist healthcare workers revising professional roles at the facility level | Cluster Randomized Controlled Trial | Hybrid Type-3 | Routine care | Appropriateness Feasibility Fidelity |
| 52 | Patel et al. (2017) | India | Pilot The Healthy Activity Program (HAP), a lay counselor-delivered brief psychological treatment for severe depression, in primary care in India | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Fidelity Cost |
| 53 | Pence et al. (2014) | Cameroon | Adapt measurement-based care for depressed HIV-infected patients in Cameroon and completed a pilot study to assess feasibility, safety, acceptability, and preliminary efficacy | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the facility level | Non-specialist healthcare workers creating new clinical terms at the facility level | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-3 | Routine care | Acceptability Fidelity |
| 54 | Petersen et al. (2014) | South Africa | Assess the feasibility of a group-based counseling intervention for HIV-positive patients with depression in primary health care in South Africa using a task shifting approach | A group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 55 | Rahman, (2007) | Pakistan | Identify challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Pre-implementation assessment | Pilot researcher-controlled implementation | Acceptability Appropriateness |
| 56 | Ramaiya et al. (2018) | Nepal | Implement a dialectical behavioral therapy intervention among women with history of suicidality and evaluate its feasibility and acceptability | A group psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 57 | Sava et al. (2009) | Romania | Assess the cost-effectiveness and cost-utility of cognitive therapy (CT), rational emotive behavioral therapy (REBT), and fluoxetine (Prozac) for major depressive disorder (MDD) in Romania | A multicomponent intervention delivered to community members by multiple providers at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 58 | Seedat et al. (2008) | South Africa | Pilot a consumer psychoeducation program to improve antidepressant adherence in South Africa | A medication intervention delivered to community members by multiple providers at the facility level | Community members distributing education materials at the community level | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-3 | Routine care | Acceptability Feasibility |
| 59 | Shidhaye et al. (2017) | India | Assess whether implementation of the community mental health program VISHRAM was associated with an increase in the proportion of people with depression who sought treatment in India | A multicomponent intervention delivered to community members by multiple providers at the facility level | Non-specialist healthcare workers increasing demand at the community level | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-3 | Routine care | Cost |
| 60 | Shinde et al. (2013) | India | Perform a qualitative analysis of the intervention experience of the MANAS trial, a lay counselor led collaborative stepped care intervention in Goa, India | A multicomponent intervention delivered to community members by multiple providers at the facility level | Non-specialist healthcare workers revising professional roles at the facility level | Qualitative | Hybrid Type-3 | Routine care | Acceptability |
| 61 | Sikander et al. (2019) | Pakistan | Adapt the Thinking Healthy Programme (THP) for delivery by volunteer peers and assess its effectiveness and cost-effectiveness in Rawalpindi, Pakistan | An individual psychotherapy intervention delivered to community members by community members at the community level | Primary focus is evaluating depression intervention | Cluster Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 62 | Singla et al. (2014) | India | Evaluate a peer-led quality assessment of psychological treatments in Goa, India | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Non-specialist healthcare workers providing clinical supervision at the facility level | Mixed Methods | Hybrid Type-3 | Pilot researcher-controlled implementation | Acceptability Fidelity |
| 63 | Smith Fawzi et al. (2012) | Haiti | Examine the feasibility and assess the preliminary effectiveness of a psychosocial support group intervention for HIV-affected youth and their caregivers in central Haiti | A group counseling intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 64 | Sorsdahl et al. (2015) | South Africa | Evaluate feasibility and preliminary responses to a screening and brief intervention program for maternal mental disorders within the context of primary care in South Africa | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Feasibility |
| 65 | Sullivan et al. (2016) | Mexico | Describe the process of culturally adapting and disseminating the Community Advocacy Project to improve depression among survivors of intimate partner violence in Monterrey, Mexico | A counseling intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 66 | Surjaningrum et al. (2018) | Indonesia | Examine the feasibility of an integrated mental health task-sharing intervention focused on identifying perinatal depression in Surabaya, Indonesia | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the facility level | Non-specialist healthcare workers revising professional roles at the community level | Qualitative | Pre-implementation assessment | Routine care | Appropriateness |
| 67 | Tang et al. (2015) | China | Explore the advantages and challenges of implementing a village doctor-based cognitive behavioral therapy intervention in treating late-life depression in rural China | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Qualitative | Hybrid Type-1 | Pilot researcher-controlled implementation | Appropriateness Feasibility Fidelity |
| 68 | Tewari et al. (2017) | India | Implement a mental health services delivery model that leverages technology and task sharing to facilitate identification and treatment of common mental disorders in rural Andhra Pradesh, India | A multicomponent intervention delivered to community members by primary care physicians at the facility level | Non-specialist healthcare workers facilitating the relay of clinical data to providers at the community level | Mixed Methods | Hybrid Type-3 | Routine care | Acceptability Feasibility Fidelity |
| 69 | Tiburcio et al. (2016) | Mexico | Develop and evaluate the usability of the web-based Help Program for Drug Abuse and Depression in Mexico | An individual psychotherapy intervention delivered to community members through technology at the community level | Primary focus is evaluating depression intervention | Qualitative | Pre-implementation assessment | Pilot researcher-controlled implementation | Acceptability Appropriateness Feasibility |
| 70 | Tomita et al. (2016) | South Africa | Assess the feasibility of SMS-based methods to screen for depression risk among refugees in South Africa and to compare its reliability and acceptability with face-to-face consultation | A multicomponent intervention delivered to community members by multiple providers at the facility level | Technology facilitating relay of clinical data to nurses at the community level | Quasi-Experimental – Uncontrolled Pre-Post | Hybrid Type-3 | Pilot researcher-controlled implementation | Acceptability |
| 71 | Tripathy et al. (2010) | India | Assess the effects of participatory women's groups on birth outcomes and maternal depression in a largely tribal and rural population in three districts in eastern India | A multicomponent intervention delivered to community members by community members at the community level | Primary focus is evaluating depression intervention | Cluster Randomized Controlled Trial |
Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 72 | Vicente et al. (2007) | Chile | Evaluated the results of a brief 2-day educational training program for Chilean primary care physicians to improve diagnosis and treatment of depression | A multicomponent intervention delivered to community members by primary care physicians at the facility level | Primary care physicians conducting ongoing training at the facility level | Quasi-Experimental – Controlled Pre-Post | T4-1 | Routine care | Acceptability |
| 73 | Walker et al. (2018) | Nepal | Assess the feasibility and acceptability of a psychosocial support package for people receiving treatment for multidrug-resistant TB in Nepal | A multicomponent intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 74 | Watt et al. (2017) | Tanzania | Evaluate a psychological intervention for women receiving surgical care for obstetric fistula in Tanzania | An individual psychotherapy intervention delivered to community members by nurses at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Fidelity |
| 75 | Weobong et al. (2017) | India | Evaluate the sustained effectiveness and cost-effectiveness of the Healthy Activity Programme, a brief psychological treatment for depression delivered by lay counselors in primary care in India | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Cost |
| 76 | Yang et al. (2018) | China | Develop and test a culturally tailored, brief three-session CBT skills-based intervention for HIV+ men who have sex with men (MSM) integrated into primary care in China | An individual psychotherapy intervention delivered to community members by psychologists at the facility level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Feasibility |
| 77 | Yang et al. (2019) | China | Test the feasibility and acceptability of an 8-week online mindfulness intervention for pregnant women as an approach to reduce depressive and anxious symptoms in China | An individual psychotherapy intervention delivered to community members by technology at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 78 | Yeung et al. (2018) | China | Examine the feasibility, safety, and effectiveness of using an online computerized cognitive behavioral therapy (CBT) for treating patients with depression in China | An individual psychotherapy intervention delivered to community members by technology at the facility level | Primary focus is evaluating depression intervention | Individual-level Randomized Controlled Trial | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability |
| 79 | Zafar et al. (2014) | Pakistan | Develop and integrate a cognitive behavioral therapy-based maternal psychosocial well-being intervention (the five-pillars approach) into a child nutrition and development program in Pakistan | An individual psychotherapy intervention delivered to community members by non-specialist healthcare workers at the community level | Primary focus is evaluating depression intervention | Mixed Methods | Hybrid Type-1 | Pilot researcher-controlled implementation | Acceptability Appropriateness Feasibility Fidelity |
The depression interventions of interest were most often delivered at the health facility level (n = 47; 59.5), followed by the community level (n = 30; 38.0%), and multi-level programs (n = 2; 2.5%). Most depression interventions were delivered by non-specialist healthcare workers (n = 36; 45.6%) who did not have specific specialist mental health training and were not trained as a nurse or other clinical providers. Other common providers included team-based delivery (9, 11.4%); primary care physicians (8, 10.1%), and technology-based delivery (8, 10.1%). The modality for depression intervention was most commonly individual psychotherapy (n = 30, 38.0%), followed by multi-component interventions (n = 27; 33.3%) that commonly included both psychotherapy and psychotropic medication. Group psychotherapy was also common, with 14 studies (17.3%). Few studies focused on medication alone (n = 3; 3.7%), activity-based treatments (n = 3; 3.7%), or education/information (n = 1; 1.2%).
Implementation strategy characteristics
Seventy-three percent of studies (n = 58) had the primary aim of testing the depression intervention of interest, rather than testing an implementation strategy to enhance implementation outcomes for a given depression intervention. Of the 21 studies (26.5%) testing an implementation strategy, the majority employed the strategy at the health facility level (n = 14; 66.6%), followed by the community (n = 6; 28.6%) and the district levels (n = 1; 4.8%). For example, in a Hybrid Type-3 study, Maulik et al. (2016) assessed the acceptability and feasibility of a community-based electronic decision-support implementation strategy to facilitate the relay of clinical data from non-specialist health workers in the community to primary care providers to improve routinely-provided public-sector depression care in India. Additionally, Jordans et al. (2019) reported fidelity and penetration resulting from an implementation strategy to work with policy-makers at the district level to develop a formal implementation blueprint focused on improving routinely-delivered depression care in Nepal.
Of the 21 studies testing implementation strategies, the majority employed non-specialist healthcare workers in strategy implementation (n = 11; 52%), followed by primary care physicians (n = 4; 19.0%) and nurses (n = 3; 14.2%). The ERIC classification of implementation strategies highlighted revising professional roles as the dominant strategy (n = 10; 47.6%). These studies primarily focused on testing task-sharing approaches to optimize implementation outcomes of depression interventions. For example, Alvarado et al. (2012) studied the cost and sustainability of revising the professional roles of primary care providers to implement a stepped-care multicomponent depression treatment program in routine care settings in Chile. Buttorff et al. (2012) reported the cost and penetration of testing the strategy of revising professional roles to have non-specialist workers deliver depression care in routine primary care settings in India.
Other implementation strategies commonly tested included facilitating the relay of clinical data to providers (n = 3; 14.3%) and conducting ongoing training (n = 3; 14.3%). For example, Tewari et al. (2017) reported the acceptability, feasibility, and fidelity of a community-based electronic decision-support implementation strategy to facilitate the relay of clinical depression data from the community to primary care providers in India. Gureje et al. (2015) reported fidelity associated with the conducting ongoing training of primary healthcare workers in the WHO Mental Health Gap Action Programme Intervention Guide to integrate depression treatment with primary care in Nigeria. Five of the eight distinct ERIC strategies tested were covered by only one study, including: (1) creating new clinical teams; (2) developing a formal implementation blueprint; (3) distributing educational materials; (4) increasing demand; and (5) providing clinical supervision. Sixty-five of the 73 distinct ERIC strategies were not represented by studies in our sample.
Discussion
Our systematic review found a relatively large body of implementation research targeting depression interventions in LMICs. Researchers are increasing their use of modern methods in implementation science, with a growing focus on reporting implementation outcomes, testing implementation strategies, and using pragmatic study designs to optimize the delivery of evidence-based interventions in routine settings. Nevertheless, our review identified significant gaps in the literature. The vast majority of existing implementation research focuses on early-stage implementation outcomes, such as acceptability, appropriateness, and feasibility, with a paucity of studies focusing on later-stage outcomes such as cost, penetration, and sustainability. In addition, only one quarter of studies had the primary aim of testing an implementation strategy. The majority of studies reported implementation outcomes as part of a ‘process evaluation’ complementary to a pragmatic trial or pilot study focused on evaluating clinical effectiveness for a depression intervention. Thus, the bulk of studies identified in our review were labeled as ‘Hybrid Type-1 effectiveness-implementation’ designs (Curran et al., 2012). With this continued focus on clinical effectiveness, it is no surprise that three quarters of included studies were studying a depression intervention delivered under pilot researcher-controlled implementation, rather than in routine care. Furthermore, we found only four studies that were focused on evaluating and optimizing the scale-up of depression interventions for population health impact in LMICs. We also found specific LMIC regions with few existing studies, including the Middle East and North Africa and Europe and Central Asia. Overall, our findings corroborate a recent systematic review focused on implementation science for stigma reduction interventions in LMICs (Kemp et al., 2019a) which found that the majority of studies utilized Hybrid Type-1 designs, qualitative research methods, and reported the implementation outcomes of acceptability and feasibility.
Assessing depression intervention effectiveness in a randomized controlled trial along with a mixed-methods process evaluation to assess early-stage implementation outcomes tied to depression intervention acceptability, appropriateness, feasibility, or initial fidelity is an optimal approach for a Hybrid Type-1 research design. Yet, even among the 57 studies at this stage, only two (Murray et al., 2014; Adewuya et al., 2018) reported the early-stage implementation outcome of adoption. This is not surprising since pilot researcher-controlled implementation projects often hire separate research staff as implementers and thus ‘non-participation’ (or lack of adoption) of these separate paid staff is not common. Nevertheless, the lack of reporting on adoption, paired with the dearth of studies reporting on penetration, means that little is known regarding the uptake, initial implementation, or potential routine institutionalization of depression interventions in LMICs – key implementation outcomes for effective and sustained scale-up of depression interventions. Future research, even at T2-2 and Hybrid Type-1 stages, could focus on approximating real-world routine implementation conditions to allow effective reporting of provider and organizational adoption and implementation costs. Where possible, these studies should also build in funding for assessment of later-stage penetration and sustainability (maintenance) once research-based implementation has ended as has been advocated by the RE-AIM evaluation framework for decades (Glasgow et al., 1999). Researchers working at this stage could also consider increased utilization of high-quality quasi-experimental designs with optimal design features for causal inference, rather than the current dominance of randomized trials and poor-quality uncontrolled pre-post quasi-experimental designs (Bärnighausen et al., 2017; Geldsetzer and Fawzi, 2017; Reeves et al., 2017). The highest-quality quasi-experimental designs for causal inference in routine implementation settings of controlled interrupted time-series (Bernal et al., 2017) and regression discontinuity (Bor et al., 2014) were not represented in our review.
Of the 21 studies testing implementation strategies, over 70% (n = 16) were Hybrid Type-3 designs, followed by studies at phases T3 (n = 2; 9.5%), and T4-1 (n = 3; 14.3%). Compared to Hybrid Type-1 studies, Hybrid Type-3 studies were more likely to use quasi-experimental designs (7 of 16; 43.8% v. 10 of 53; 18.9%) and less likely to use randomized designs (2 of 16; 12.5% v. 21 of 53; 39.6%). Furthermore, no study with a primary aim to test an implementation strategy used individual randomization, compared to 27.6% (17 of 58) of studies with a primary aim to test intervention effectiveness. This pattern is in line with the fact that pragmatic cluster randomized trials and high-quality quasi-experimental designs are the gold standard research designs for testing and optimizing implementation strategies for an intervention delivered in routine care. Using individual randomization at the later phases of the implementation research continuum is logistically difficult, and can potentially alter routine systems of implementation, decreasing both internal and external validity. As expected, implementation outcome distributions were similar across Hybrid Type-1 and Hybrid Type-3 studies. The six studies situated at T3 and T4-1 were more likely to focus on the later-stage implementation outcomes of cost (n = 3; 50.0%) and sustainability (n = 2; 33.3%); these studies were also more likely to report adoption (n = 2; 33.3%). As visualized in Fig. 1, we suggest that the most relevant implementation outcomes at the testing implementation strategy phase (T3) are similar at T2-2 or when using Hybrid designs. Although, at stage T3, implementation outcome reporting should target both the implementation strategy being tested along with the target depression intervention. For example, if testing an implementation strategy to improve the adoption of a depression intervention, researchers will also be interested in measuring, assessing, and optimizing the adoption of the implementation strategy.
Almost half of the 21 studies testing implementation strategies focused on assessing the effectiveness of revising professional roles, most often through task-sharing to provide depression care led by primary care providers or lay health workers in a stepped-care approach supervised by specialist providers. Only eight of the 73 distinct ERIC implementation strategies (Powell et al., 2015) had any representation in our review, with five strategies being tested in only one study. For efficient generation of evidence given the large number of potential distinct implementation strategies – not to mention multicomponent or blended groups of strategies – we suggest future implementation research considers increased use of adaptive trial designs, such as sequential multiple assignment randomized trials (SMART); (Lei et al., 2012) or multiphase optimization strategy trials (MOST) (Collins et al., 2007) which can allow testing multiple strategies across multiple doses in a single trial. Quasi-experimental designs, natural experiments, and descriptive analyses utilizing routine data systems and naturally-occurring heterogeneity in implementation strategies should also be prioritized to help rapidly identify, test, and optimize the scale-up of promising implementation strategies in LMICs (Wagenaar et al., 2016).
Overall, our findings that the majority of existing implementation studies on depression interventions in LMICs are utilizing Hybrid Type-1 designs could reflect three things. First, that researchers and implementers working in LMICs do not believe we have sufficient evidence for depression intervention effectiveness across diverse contexts to move to later implementation research phases. Second, few researchers and implementers have the necessary skills or knowledge to effectively extend past traditional clinical research designs focused on depression intervention effectiveness testing toward testing implementation strategies (T3), optimizing scale-up in routine systems settings (T4-1), or continuous optimization in routine systems settings (T4-2). Third, research funders have yet to fully embrace the field of implementation science and the value of moving beyond traditional clinical research paradigms.
To address the first point, we argue that with the publishing of the Disease Control Priorities, 3rd Edition in 2016 outlining that sufficient evidence exists for effectiveness and cost-effectiveness for depression interventions globally (Patel et al., 2016), the time is now for increased investments in implementation research and to move beyond testing intervention effectiveness and toward testing implementation strategies (T3), scale-up (T4-1), and continuous optimization of routine implementation (T4-2). The second point will require the development and re-training of a pipeline of researchers with expertise outside of traditional clinical research paradigms centered on highly-controlled randomized trials as the lone gold standard research design. As the field of global mental health progresses away from pragmatic clinical intervention studies and toward optimizing the scaling-up (T4-1) of best-evidence interventions and associated implementation strategies and continuous ‘embedded research’ and ‘learning evaluation’ of interventions and strategies already scaled-up (T4-1), we anticipate that a number of key evolutions will occur. Implementation outcome reporting will center on later stage costs, fidelity, penetration, and sustainability of both interventions and implementation strategies. Clinical researchers will have to be re-trained or partner with various disciplinary experts to implement analytical designs focused more on high-quality quasi-experimental approaches, continuous improvement and systems optimization borrowing from industrial engineering and business domains, along with novel systems modeling approaches (Royston, 2011; Sherr et al., 2014; Wagner et al., 2019). These methods will be of increasing importance due to the need to model, test, and continuously improve complex webs of multiple evidence-based interventions and implementation strategies for depression operating across contexts and in non-linear pathways (Galea et al., 2010; Kemp et al., 2019b). Studies operating at the level of entire districts, provinces, or nations in LMICs will have the necessary primary focus on external validity and will focus on continuous reporting of implementation outcomes using routine data systems (Victora et al., 2004; Wagenaar et al., 2016). To catalyze later phases of implementation research in LMICs, funding agencies, governments, and stakeholders will need to recognize their role in funding ongoing real-world implementation of depression interventions, not simply focusing on funding one-off research-based implementation projects.
This review has several important limitations. First, given available resources, we were only available to review papers published in English, likely systematically excluding studies emanating from certain LMICs. Second, this review focused on peer-reviewed studies. Given the barriers to publishing in international peer-reviewed journals, especially for LMIC investigators, this likely biases our findings to papers published by internationally-connected and funded investigators. Third, given the heterogeneous language and terminology used in the burgeoning field of implementation science, making strict distinctions between ‘evidence-based depression interventions’ and ‘implementation strategies’ of interest, as well as coding implementation strategies into distinct ERIC classifications (Powell et al., 2015) is challenging. Similarly, coding the stage of implementation research is also difficult and somewhat qualitative in nature, as implementation researchers themselves have not adopted a comprehensive and common language to situate their studies along the implementation research continuum. Fourth, given the size of this review, we focused data abstraction on implementation outcomes and high-level coding of depression intervention characteristics. We did not abstract detailed information on implementation context, the use of implementation science frameworks, or on the diversity of specific depression interventions – areas that could be of interest for future systematic reviews. Last, we did not code the level of analysis for implementation outcomes which we suggest future researchers conduct. This is important to distinguish, for example, client-level adoption or sustainability (reach and maintenance, respectively in the RE-AIM framework, Glasgow et al., 1999) from provider- or organizational-level adoption or sustainability.
Conclusions
Our systematic review of implementation outcomes and strategies for depression interventions in LMICs found that existing research has focused largely on early-stage implementation outcomes. Most studies had the primary aim of testing the pragmatic effectiveness of a depression intervention in pilot researcher-controlled settings paired with a ‘process evaluation’ to collect information on implementation context. Thus, the majority of studies were Hybrid Type-1 effectiveness-implementation designs, with very few studies focused on evaluating and optimizing strategies for scale-up of depression interventions in routine care. Even though the ostensible focus of the field of implementation science is to test implementation strategies to optimize the real-world implementation of evidence-based interventions, only a quarter of studies had a primary aim to test implementation strategies for interventions implemented in routine care. Approximately half of these studies testing implementation strategies were focused on testing revised professional roles, or task-shifting, for depression intervention implementation. Only eight of the 73 distinct ERIC implementation strategies were represented in our systematic review. Future implementation research should focus on testing implementation strategies and optimizing the use of evidence-based strategies to scale-up and improve the quality of routine depression care. These studies should use high-quality pragmatic research designs such as controlled interrupted time-series, regression discontinuity, stepped-wedge randomized trials, and novel complex systems modeling approaches, as well as focus on later-stage implementation outcomes such as cost, penetration, and sustainability. Certain LMIC regions, such as Middle East and North Africa and Europe and Central Asia could be prioritized for investments given the paucity of existing studies.
Data
All data are available in online Supplementary File S1.
Author contributions
BHW conceived the idea. CGK provided assistance with the search strategy and systematic review methods. All authors contributed to article review, data extraction, and data interpretation. All authors read and approved the final manuscript.
Financial support
BHW was supported by grant number K01MH110599 from the U.S. National Institute of Mental Health. CGK was supported by grant number F31MH112397 from the U.S. National Institute of Mental Health. JMB was supported by a Postdoctoral Fellowship grant from the Canadian Institutes of Health Research (CIHR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or CIHR.
Conflict of interest
The authors report no conflict of interest.
Ethical standards
N/A, systematic review.
Consent for publication
N/A, systematic review.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/gmh.2020.1.
click here to view supplementary material
References
- Abas M, Bowers T, Manda E, Cooper S, Machando D, Verhey R, Lamech N, Araya R and Chibanda D (2016) ‘Opening up the mind’: problem-solving therapy delivered by female lay health workers to improve access to evidence-based care for depression and other common mental disorders through the Friendship Bench Project in Zimbabwe. International Journal of Mental Health Systems 10, 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abas M, Mbengeranwa OL, Chagwedera IVS, Maramba P and Broadhead J (2003) Primary care services for depression in Harare, Zimbabwe. Harvard Review of Psychiatry 11, 157–165. [DOI] [PubMed] [Google Scholar]
- Abas M, Nyamayaro P, Bere T, Saruchera E, Mothobi N, Simms V, Mangezi W, Macpherson K, Croome N, Magidson J, Makadzange A, Safren S, Chibanda D and O'Cleirigh C (2018) Feasibility and acceptability of a task-shifted intervention to enhance adherence to HIV medication and improve depression in people living with HIV in Zimbabwe, a Low income country in Sub-Saharan Africa. AIDS and Behavior 22, 86–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abi Ramia J, Harper Shehadeh M, Kheir W, Zoghbi E, Watts S, Heim E and El Chammay R (2018) Community cognitive interviewing to inform local adaptations of an e-mental health intervention in Lebanon. Global Mental Health (Cambridge, England) 5, e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams J, Almond M, Ringo E, Shangali W and Sikkema K (2012) Feasibility of nurse-led antidepressant medication management of depression in an HIV clinic in Tanzania. International Journal of Psychiatry in Medicine 43, 105–117. doi: 10.2190/PM.43.2.a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adewuya A, Adewumi T, Momodu O, Olibamoyo O, Adesoji O, Adegbokun A, Adeyemo S, Manuwa O and Adegbaju D (2018) Development and feasibility assessment of a collaborative stepped care intervention for management of depression in the mental health in primary care (MeHPriC) project, Lagos, Nigeria. Psychological Medicine 49(13), 1–9. doi: 10.1017/S0033291718002970. [DOI] [PubMed] [Google Scholar]
- Alampay LP, Galvez Tan LJT, Tuliao AP, Baranek P, Ofreneo MA, Lopez GD, Fernandez KG, Rockman P, Villasanta A, Angangco T, Freedman ML, Cerswell L and Guintu V (2019) A pilot randomized controlled trial of a mindfulness program for Filipino children. Mindfulness 11, 303–316. doi: 10.1007/s12671-019-01124-8. [DOI] [Google Scholar]
- Alvarado R, Rojas G, Minoletti A, Alvarado F and Domínguez C (2012) Depression program in primary health care. International Journal of Mental Health 41, 38–47. Available at http://offcampus.lib.washington.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=104419945&site=ehost-liveNS-. [Google Scholar]
- Andersen L, Magidson J, O'Cleirigh C, Remmert J, Kagee A, Leaver M, Stein D, Safren S and Joska J (2016) A pilot study of a nurse-delivered cognitive behavioral therapy intervention (Ziphamandla) for adherence and depression in HIV in South Africa. Journal of Health Psychology 23(6), 1359105316643375. doi: 10.1177/1359105316643375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araya R, Alvarado R, Sepúlveda R and Rojas G (2012) Lessons from scaling up a depression treatment program in primary care in Chile. Revista panamericana de salud publica = Pan American Journal of Public Health 32, 234–240. [DOI] [PubMed] [Google Scholar]
- Araya R, Flynn T, Rojas G, Fritsch R and Simon G (2006) Cost-effectiveness of a primary care treatment program for depression in low-income women in Santiago, Chile. The American Journal of Psychiatry 163, 1379–1387. [DOI] [PubMed] [Google Scholar]
- Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, Simon G and Peters TJ (2003) Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet 361, 995–1000. [DOI] [PubMed] [Google Scholar]
- Asunción Lara M, Tiburcio M, Aguilar Abrego A and Sánchez-Solís A (2014) A four-year experience with a Web-based self-help intervention for depressive symptoms in Mexico. Revista Panamericana de Salud Publica 36, 399–406. [PubMed] [Google Scholar]
- Atif N, Krishna R, Sikander S, Lazarus A, Nisar A, Ahmad I, Raman R, Fuhr D, Patel V and Rahman A (2017) Mother-to-mother therapy in India and Pakistan: adaptation and feasibility evaluation of the peer-delivered Thinking Healthy Programme. BMC Psychiatry 17, 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atif N, Lovell K, Husain N, Sikander S, Patel V and Rahman A (2016) Barefoot therapists: barriers and facilitators to delivering maternal mental health care through peer volunteers in Pakistan: a qualitative study. International Journal of Mental Health Systems 10, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramanian BA, Cohen DJ, Davis MM, Gunn R, Miriam Dickinson L, Miller WL, Crabtree BF and Stange KC (2015) Learning Evaluation: blending quality improvement and implementation research methods to study healthcare innovations. Implementation Science 10, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bärnighausen T, Tugwell P, Røttingen JA, Shemilt I, Rockers P, Geldsetzer P, Lavis J, Grimshaw J, Daniels K, Brown A, Bor J, Tanner J, Rashidian A, Barreto M, Vollmer S and Atun R (2017) Quasi-experimental study designs series – paper 4: uses and value. Journal of Clinical Epidemiology 89, 21–29. [DOI] [PubMed] [Google Scholar]
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, Cetinoglu T, Wachter K, Murray LK and Bolton PA (2013) Controlled trial of psychotherapy for Congolese survivors of sexual violence. New England Journal of Medicine 368, 2182–2191. [DOI] [PubMed] [Google Scholar]
- Bass J, Neugebauer R, Clougherty KF, Verdeli H, Wickramaratne P, Ndogoni L, Speelman L, Weissman M and Bolton P (2006) Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes. British Journal of Psychiatry 188, 567–573. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Paez-Soto A, Herrera-Amighetti LD, Montero F, Herrera HC, Llerena-Quinn R, Arenales GA and Alvarado MD (2011) Adaptation of a preventive intervention approach to strengthen families facing adversities, especially depression. Costa Rica: initial systems approaches and a case example. International Journal of Mental Health Promotion 13, 5–13. [Google Scholar]
- Bella-Awusah T, Ani C, Ajuwon A and Omigbodun O (2016) Effectiveness of brief school-based, group cognitive behavioural therapy for depressed adolescents in south west Nigeria. Child and Adolescent Mental Health 21, 44–50. [DOI] [PubMed] [Google Scholar]
- Bernal JL, Cummins S and Gasparrini A (2017) Interrupted time series regression for the evaluation of public health interventions: a tutorial. International Journal of Epidemiology 46, 348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt T, Ng L, Kirk C, Brennan R, Beardslee W, Stulac S, Mushashi C, Nduwimana E, Mukunzi S, Nyirandagijimana B, Kalisa G, Rwabukwisi C and Sezibera V (2017) Family-based promotion of mental health in children affected by HIV: a pilot randomized controlled trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines 58, 922–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Ng LC, Kirk CM, Munyanah M, Mushashi C, Ingabire C, Teta S, Beardslee WR, Brennan RT, Zahn I, Stulac S, Cyamatare FR and Sezibera V (2014) Family-based prevention of mental health problems in children affected by HIV and AIDS: an open trial. AIDS (London, England) 28, S359–S368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS and Chambers DA (2016) Optimizing an era of global mental health implementation science. JAMA Psychiatry 73, 99–100. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Betancourt T, Onyango G, Clougherty KF, Neugebauer R, Murray L and Verdeli H (2007) Interventions for depression symptoms among adolescent survivors of war and displacement in Northern Uganda. JAMA 298, 519–527. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Verdeli H, Clougherty KF and Ndogoni L (2003) Group interpersonal psychotherapy for depression in rural Uganda. JAMA 289, 3117–3124. [DOI] [PubMed] [Google Scholar]
- Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, Robinson C, Ugueto AM and Bass J (2014) A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Medicine 11. doi: 10.1371/journal.pmed.1001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Escobar F, Fandino-Losada A, Martinez-Buitrago D, Santaella-Tenorio J, Tobon-Garcia D, Munoz-Morales E, Escobar-Roldan I, Babcock L, Duarte-Davidson E, Bass J, Murray L, Dorsey S, Gutierrez-Martinez M and Bolton P (2018) A randomized controlled trial of a transdiagnostic cognitive-behavioral intervention for Afro-descendants’ survivors of systemic violence in Colombia’. PLoS ONE 13, e0208483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J, Moscoe E, Mutevedzi P, Newell M-L and Bärnighausen T (2014) Regression discontinuity designs in epidemiology. Epidemiology 25, 729–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CH, Curran G, Palinkas LA, Aarons GA, Wells KB, Jones L, Collins LM, Duan N, Mittman BS, Wallace A, Tabak RG, Ducharme L, Chambers DA, Neta G, Wiley T, Landsverk J and Cheung K (2017) An overview of research and evaluation designs for dissemination and implementation. Annual Review of Public Health 38, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Schafer A, Dawson KS, Anjuri D, Mulili C, Ndogoni L, Koyiet P, Sijbrandij M, Ulate J, Harper Shehadeh M, Hadzi-Pavlovic D and van Ommeren M (2017) Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: a randomised clinical trial. PLoS Medicine 14, e1002371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton C, Tatar AS, McKinstry B, Matheson C, Matu S, Moldovan R, Macnab M, Farrow E, David D, Pagliari C, Blanco AS and Wolters M (2016) Pilot randomised controlled trial of Help4Mood, an embodied virtual agent-based system to support treatment of depression. Journal of Telemedicine and Telecare 22, 348–355. [DOI] [PubMed] [Google Scholar]
- Buttorff C, Hock R, Weiss H, Naik S, Araya R, Kirkwood B, Chisholm D and Patel V (2012) Economic evaluation of a task-shifting intervention for common mental disorders in India. Bulletin of the World Health Organization 90, 813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee S, Chowdhary N, Pednekar S, Cohen A, Andrew G, Andrew G, Araya R, Simon G, King M, Telles S, Verdeli H, Clougherty K, Kirkwood B and Patel V (2008) Integrating evidence-based treatments for common mental disorders in routine primary care: feasibility and acceptability of the MANAS intervention in Goa, India. World Psychiatry 7, 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R and Abas M (2011) Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health 11, 828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibanda D, Verhey R, Munetsi E, Rusakaniko S, Cowan F and Lund C (2016a) Scaling up interventions for depression in sub-Saharan Africa: lessons from Zimbabwe. Global Mental Health 3, e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibanda D, Weiss HA, Verhey R and Simms V (2016b) Effect of a primary care-based psychological intervention on symptoms of common mental disorders in Zimbabwe: a randomized clinical trial. JAMA 316, 2618–2626. [DOI] [PubMed] [Google Scholar]
- Chowdhary N, Anand A, Dimidjian S, Shinde S, Weobong B, Balaji M, Hollon S, Rahman A, Wilson G, Verdeli H, Araya R, King M, Jordans M, Fairburn C, Kirkwood B and Patel V (2016) The Healthy Activity Program lay counsellor delivered treatment for severe depression in India: systematic development and randomised evaluation. The British Journal of Psychiatry: The Journal of Mental Science 208, 381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churruca K, Ludlow K, Taylor N, Long JC, Best S and Braithwaite J (2019) The time has come: embedded implementation research for health care improvement. Journal of Evaluation in Clinical Practice 25(3), 1–8. [DOI] [PubMed] [Google Scholar]
- Collins LM, Murphy SA and Strecher V (2007) The Multiphase Optimization Strategy (MOST) and the Sequential Multiple Assignment Randomized Trial (SMART). New Methods for More Potent eHealth Interventions. American Journal of Preventive Medicine 32(5 suppl.), 112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Patel V, Joestl SS, March D, Insel TR and Daar AS (2011) Grand challenges in global mental health. Nature 475, 27–30. doi: 10.1038/475027a.Grand. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covidence Systematic Review Software (2020). Available at: https://www.covidence.org.
- Curran G, Bauer M, Mittman B, Pyne J and Stetler C (2012) Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care 50, 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Canseco F, Toyama M, Ipince A, Perez-Leon S, Cavero V, Araya R and Miranda J (2018) Integration of a technology-based mental health screening program into routine practices of primary health care services in Peru (The Allillanchu Project): development and implementation. Journal of Medical Internet Research 20, e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doumit R, Kazandjian C and Militello L (2018) COPE for adolescent Syrian refugees in Lebanon: a brief cognitive-behavioral skill-building intervention to improve quality of life and promote positive mental health. Clinical Nursing Research, 1054773818808114. doi: 10.1177/1054773818808114. [DOI] [PubMed] [Google Scholar]
- Duffy M, Sharer M, Cornman H, Pearson J, Pitorak H and Fullem A (2017) Integrating mental health and HIV services in Zimbabwean communities: a nurse and community-led approach to reach the most vulnerable. The Journal of the Association of Nurses in AIDS Care: JANAC 28, 186–198. [DOI] [PubMed] [Google Scholar]
- Dwommoh R, Sorsdahl K, Myers B, Asante K, Naledi T, Stein D and Cleary S (2018) Brief interventions to address substance use among patients presenting to emergency departments in resource poor settings: a cost-effectiveness analysis. Cost Effectiveness and Resource Allocation: C/E 16, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles MP and Mittman BS (2006) Welcome to implementation science. Implementation Science 1, 1–3. [Google Scholar]
- Fisher J, Nguyen H, Mannava P, Tran H, Dam T, Tran H, Tran T, Durrant K, Rahman A and Luchters S (2014) Translation, cultural adaptation and field-testing of the Thinking Healthy Program for Vietnam. Globalization and Health 10, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fort DG, Herr TM, Shaw PL, Gutzman KE and Starren JB (2017) Mapping the evolving definitions of translational research. Journal of Clinical and Translational Science 1, 60–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuhr D, Weobong B, Lazarus A, Vanobberghen F, Weiss H, Singla D, Tabana H, Afonso E, De Sa A, D'Souza E, Joshi A, Korgaonkar P, Krishna R, Price L, Rahman A and Patel V (2019) Delivering the Thinking Healthy Programme for perinatal depression through peers: an individually randomised controlled trial in India. The Lancet. Psychiatry 6, 115–127. [DOI] [PubMed] [Google Scholar]
- Galea S, Riddle M and Kaplan GA (2010) Causal thinking and complex system approaches in epidemiology. International Journal of Epidemiology 39, 97–106. doi: 10.1093/ije/dyp296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallegos J, Rodríguez A, Gómez G, Rabelo M and Gutiérrez MF (2012) The FRIENDS for life program for Mexican girls living in an orphanage: a pilot study. Behaviour Change 29, 1–14. [Google Scholar]
- Geldsetzer P and Fawzi W (2017) Quasi-experimental study designs series – paper 2: complementary approaches to advancing global health knowledge. Journal of Clinical Epidemiology 89, 12–16. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM and Boles SM (1999) Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health 89, 1322-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Xu Z, Qiao J, Hong Y, Zhang H, Zeng C, Cai W, Li L and Liu C (2018) Development and feasibility testing of an mHealth (text message and WeChat) intervention to improve the medication adherence and quality of life of people living with HIV in China: pilot randomized controlled trial. JMIR mHealth and uHealth 6, e10274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gureje O, Abdulmalik J, Kola L, Musa E, Yasamy M and Adebayo K (2015) Integrating mental health into primary care in Nigeria: report of a demonstration project using the mental health gap action programme intervention guide. BMC Health Services Research 15, 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gureje O, Oladeji B, Montgomery A, Araya R, Bello T, Chisholm D, Groleau D, Kirmayer L, Kola L, Olley L, Tan W and Zelkowitz P (2019) High- versus low-intensity interventions for perinatal depression delivered by non-specialist primary maternal care providers in Nigeria: cluster randomised controlled trial (the EXPONATE trial). The British Journal of Psychiatry: the Journal of Mental Science 215(3), 1–8. doi: 10.1192/bjp.2019.4. [DOI] [PubMed] [Google Scholar]
- Hashemi S, Shirazi H, Mohammadi A, Zadeh-Bagheri G, Noorian K and Malekzadeh M (2012) Nortriptyline versus fluoxetine in the treatment of major depressive disorder: a six-month, double-blind clinical trial. Clinical Pharmacology: Advances and Applications 4, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation (IHME) (2017) GBD Compare Data Visualization: Global. Seattle, WA: University of Washington. [Google Scholar]
- Isa E, Ani C, Bella-Awusah T and Omigbodun O (2018) Effects of psycho-education plus basic cognitive behavioural therapy strategies on medication-treated adolescents with depressive disorder in Nigeria. Journal of Child and Adolescent Mental Health 30, 11–18. doi: 10.2989/17280583.2018.1424634 [DOI] [PubMed] [Google Scholar]
- Janevic M, Aruquipa Yujra A, Marinec N, Aguilar J, Aikens J, Tarrazona R and Piette J (2016) Feasibility of an interactive voice response system for monitoring depressive symptoms in a lower-middle income Latin American country. International Journal of Mental Health Systems 10, 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans M, Luitel N, Kohrt B, Rathod S, Garman E, De Silva M, Komproe I, Patel V and Lund C (2019) Community-, facility-, and individual-level outcomes of a district mental healthcare plan in a low-resource setting in Nepal: a population-based evaluation. PLoS Medicine 16, e1002748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans M, Tol W, Ndayisaba A and Komproe I (2013) A controlled evaluation of a brief parenting psychoeducation intervention in Burundi. Social Psychiatry and Psychiatric Epidemiology 48, 1851–1859. [DOI] [PubMed] [Google Scholar]
- Kakuma R, Minas H, van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, Saxena S and Scheffler RM (2011) Human resources for mental health care: current situation and strategies for action. Lancet 378, 1654–1663. [DOI] [PubMed] [Google Scholar]
- Kemp CG, Jarrett BA, Kwon CS, Song L, Jetté N, Sapag JC, Bass J, Murray L, Rao D and Baral S (2019a) Implementation science and stigma reduction interventions in low- and middle-income countries: a systematic review. BMC Medicine 17, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp CG, Wagenaar BH and Haroz EE (2019b) Expanding hybrid studies for implementation research: intervention, implementation strategy, and context. Frontiers in Public Health 7, 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan M, Hamdani S, Chiumento A, Dawson K, Bryant R, Sijbrandij M, Nazir H, Akhtar P, Masood A, Wang D, Wang E, Uddin I, van Ommeren M and Rahman A (2019) Evaluating feasibility and acceptability of a group WHO trans-diagnostic intervention for women with common mental disorders in rural Pakistan: a cluster randomised controlled feasibility trial. Epidemiology and Psychiatric Sciences 28, 77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara MA, Navarro C, Acevedo M, Berenzon S, Mondragón L and Rubí NA (2004) A psycho-educational intervention for depressed women: a qualitative analysis of the process. Psychology and Psychotherapy: Theory, Research and Practice 77, 429–447. [DOI] [PubMed] [Google Scholar]
- Lei H, Nahum-shani I, Lynch K, Oslin D and Murphy S (2012) A ‘SMART’ design for building individualized treatment sequences. Annual Review of Clinical Psychology 8, 21–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J and Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology 62, e1–34 [DOI] [PubMed] [Google Scholar]
- Lieu TA and Madvig PR (2019) Strategies for building delivery science in an integrated health care system. Journal of General Internal Medicine 34, 1043–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maselko J, Sikander S, Bhalotra S, Bangash O, Ganga N, Mukherjee S, Egger H, Franz L, Bibi A, Liaqat R, Kanwal M, Abbasi T, Noor M, Ameen N and Rahman A (2015) Effect of an early perinatal depression intervention on long-term child development outcomes: follow-up of the thinking healthy programme randomised controlled trial. The Lancet. Psychiatry 2, 609–617. [DOI] [PubMed] [Google Scholar]
- Maulik P, Tewari A, Devarapalli S, Kallakuri S and Patel A (2016) The Systematic Medical Appraisal, Referral and Treatment (SMART) mental health project: development and testing of electronic decision support system and formative research to understand perceptions about mental health in rural India. PLoS ONE 11, e0164404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre T, Elkonin D, de Kooker M and Magidson J (2018) The application of mindfulness for individuals living with HIV in South Africa: a hybrid effectiveness-implementation pilot study. Mindfulness 9, 871–883, Available at NS. [PMC free article] [PubMed] [Google Scholar]
- Mehrotra S, Sudhir P, Rao G, Thirthalli J and Srikanth T (2018) Development and pilot testing of an internet-based self-help intervention for depression for Indian users. Behavioral Sciences (Basel, Switzerland) 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munodawafa M, Lund C and Schneider M (2017) A process evaluation exploring the lay counsellor experience of delivering a task shared psycho-social intervention for perinatal depression in Khayelitsha, South Africa. BMC Psychiatry 17, 236. doi: 10.1186/s12888-017-1397-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, Haydary A, Weiss WM and Bolton P (2014) A common elements treatment approach for adult mental health problems in low- and middle-income countries. Cognitive and Behavioral Practice 21, 111–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Hall BJ, Dorsey S, Ugueto AM, Puffer ES, Sim A, Ismael A, Bass J, Akiba C, Lucid L, Harrison J, Erikson A and Bolton PA (2018) An evaluation of a common elements treatment approach for youth in Somali refugee camps. Global Mental Health 5, e16. doi: 10.1017/gmh.2018.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, Petersen-Williams P, van der Westhuizen C, Lund C, Lombard C, Joska J, Levitt N, Butler C, Naledi T, Milligan P, Stein D and Sorsdahl K (2019) Community health worker-delivered counselling for common mental disorders among chronic disease patients in South Africa: a feasibility study. BMJ Open 9, e024277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakimuli-Mpungu E, Wamala K, Okello J, Alderman S, Odokonyero R, Musisi S, Mojtabai R and Mills E (2014) Outcomes, feasibility and acceptability of a group support psychotherapeutic intervention for depressed HIV-affected Ugandan adults: a pilot study. Journal of Affective Disorders 166, 144–150. doi: 10.1016/j.jad.2014.05.005 [DOI] [PubMed] [Google Scholar]
- Nakimuli-Mpungu E, Wamala K, Okello J, Ndyanabangi S, Kanters S, Mojtabai R, Nachega J, Mills E and Musisi S (2017) Process evaluation of a randomized controlled trial of group support psychotherapy for depression treatment among people with HIV/AIDS in northern Uganda. Community Mental Health Journal 53, 991–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naveen G, Rao M, Vishal V, Thirthalli J, Varambally S and Gangadhar B (2013) Development and feasibility of yoga therapy module for out-patients with depression in India. Indian Journal of Psychiatry 55(suppl. 3), S350–S356. doi: 10.4103/0019-5545.116305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oladeji B, Kola L, Abiona T, Montgomery A, Araya R and Gureje O (2015) A pilot randomized controlled trial of a stepped care intervention package for depression in primary care in Nigeria. BMC Psychiatry 15, 96. doi: 10.1186/s12888-015-0483-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, Ferrari AJ, Hyman S, Laxminarayan R, Levin C, Lund C, Medina Mora ME, Petersen I, Scott J, Shidhaye R, Vijayakumar L, Thornicroft G and Whiteford H (2016) Addressing the burden of mental, neurological, and substance use disorders: key messages from disease control priorities, 3rd edition. The Lancet 387, 1672–1685. [DOI] [PubMed] [Google Scholar]
- Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, Herrman H, Herzallah MM, Huang Y, Jordans MJD, Kleinman A, Medina-Mora ME, Morgan E, Niaz U, Omigbodun O, Prince M, Rahman A, Saraceno B, Sarkar BK, De Silva M, Singh I, Stein DJ, Sunkel C and UnÜtzer J (2018) The Lancet Commission on global mental health and sustainable development. The Lancet 392, 1553–1598. [DOI] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, Bhat B, Araya R, King M, Simon G, Verdeli H and Kirkwood BR (2011) Lay health worker led intervention for depressive and anxiety disorders in India: impact on clinical and disability outcomes over 12 months. British Journal of Psychiatry 199, 459–466. doi: 10.1192/bjp.bp.111.092155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, De Silva MJ, Bhat B, Araya R, King M, Simon G, Verdeli H and Kirkwood BR (2010) Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet 376, 2086–2095. doi: 10.1016/S0140-6736(10)61508-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Weobong B, Weiss H, Anand A, Bhat B, Katti B, Dimidjian S, Araya R, Hollon S, King M, Vijayakumar L, Park A, McDaid D, Wilson T, Velleman R, Kirkwood B and Fairburn C (2017) The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. Lancet (London, England) 389, 176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathare S, Brazinova A and Levav I (2018) Care gap: a comprehensive measure to quantify unmet needs in mental health. Epidemiology and Psychiatric Sciences 27, 463–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pence B, Gaynes B, Atashili J, O'Donnell J, Kats D, Whetten K, Njamnshi A, Mbu T, Kefie C, Asanji S and Ndumbe P (2014) Feasibility, safety, acceptability, and preliminary efficacy of measurement-based care depression treatment for HIV patients in Bamenda, Cameroon. AIDS and behavior 18, 1142–1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen I, Hanass Hancock J, Bhana A and Govender K (2014) A group-based counselling intervention for depression comorbid with HIV/AIDS using a task shifting approach in South Africa: a randomized controlled pilot study. Journal of Affective Disorders 158, 78–84. [DOI] [PubMed] [Google Scholar]
- Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, Proctor EK and Kirchner JAE (2015) A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation Science 10, 1–14. doi: 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor EK, Powell BJ and McMillen JC (2013) Implementation strategies: recommendations for specifying and reporting. Implementation Science 8, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R and Hensley M (2011) Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research 38, 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A (2007) Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan – a multi-method study. Archives of Women's Mental Health 10, 211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Hamdani SU, Awan NR, Bryant RA, Dawson KS, Khan MF, Azeemi MMUH, Akhtar P, Nazir H, Chiumento A, Sijbrandij M, Wang D, Farooq S and Van Ommeren M (2016) Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. JAMA – Journal of the American Medical Association 316, 2609–2617. [DOI] [PubMed] [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C and Creed F (2008) Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. The Lancet 372, 902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaiya M, McLean C, Regmi U, Fiorillo D, Robins C and Kohrt B (2018) A dialectical behavior therapy skills intervention for women with suicidal behaviors in rural Nepal: a single-case experimental design series. Journal of Clinical Psychology 74, 1071–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves BC, Wells GA and Waddington H (2017) Quasi-experimental study designs series – paper 5: a checklist for classifying studies evaluating the effects on health interventions – a taxonomy without labels. Journal of Clinical Epidemiology 89, 30–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas G, Fritsch R, Solis J, Jadresic E, Castillo C, Gonzalez M, Guajardo V, Lewis G, Peters TJ and Araya R (2007) Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet (London, England) 370, 1629–1637. [DOI] [PubMed] [Google Scholar]
- Royston G (2011) Meeting global health challenges through operational research and management science. Bulletin of the World Health Organization 89, 683–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sava FA, Yates BT, Lupu V, Szentagotai A and David D (2009) Cost-effectiveness and cost-utility of cognitive therapy, rational emotive behavioral therapy, and fluoxetine (Prozac) in treating clinical depression: a randomized clinical trial. Journal of Clinical Psychology 65, 36–52. [DOI] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M and Whiteford H (2007) Resources for mental health: scarcity, inequity, and inefficiency. Lancet 370, 878–889. [DOI] [PubMed] [Google Scholar]
- Seedat S, Haskis A and Stein D (2008) Benefits of consumer psychoeducation: a pilot program in South Africa. International Journal of Psychiatry in Medicine 38, 31–42. [DOI] [PubMed] [Google Scholar]
- Sherr K, Gimbel S, Rustagi A, Nduati R, Cuembelo F, Farquhar C, Wasserheit J and Gloyd S (2014) Systems analysis and improvement to optimize pMTCT (SAIA): a cluster randomized trial. Implementation Science: IS 9, 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shidhaye R, Murhar V, Gangale S, Aldridge L, Shastri R, Parikh R, Shrivastava R, Damle S, Raja T, Nadkarni A and Patel V (2017) The effect of VISHRAM, a grass-roots community-based mental health programme, on the treatment gap for depression in rural communities in India: a population-based study. The Lancet. Psychiatry 4, 128–135. [DOI] [PubMed] [Google Scholar]
- Shinde S, Andrew G, Bangash O, Cohen A, Kirkwood B and Patel V (2013) The impact of a lay counselor led collaborative care intervention for common mental disorders in public and private primary care: a qualitative evaluation nested in the MANAS trial in Goa, India. Social Science & Medicine (1982) 88, 48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikander S, Ahmad I, Atif N, Zaidi A, Vanobberghen F, Weiss H, Nisar A, Tabana H, Ain Q, Bibi A, Bilal S, Bibi T, Liaqat R, Sharif M, Zulfiqar S, Fuhr D, Price L, Patel V and Rahman A (2019) Delivering the Thinking Healthy Programme for perinatal depression through volunteer peers: a cluster randomised controlled trial in Pakistan. The Lancet. Psychiatry 6, 128–139. [DOI] [PubMed] [Google Scholar]
- Singla DR, Weobong B, Nadkarni A, Chowdhary N, Shinde S, Anand A, Fairburn CG, Dimijdan S, Velleman R, Weiss H and Patel V (2014) Improving the scalability of psychological treatments in developing countries: an evaluation of peer-led therapy quality assessment in Goa, India. Behaviour Research and Therapy 60, 53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Fawzi M, Eustache E, Oswald C, Louis E, Surkan P, Scanlan F, Hook S, Mancuso A and Mukherjee J (2012) Psychosocial support intervention for HIV-affected families in Haiti: implications for programs and policies for orphans and vulnerable children. Social Science & Medicine (1982) 74, 1494–1503. [DOI] [PubMed] [Google Scholar]
- Sorsdahl K, Petersen Williams P, Everett-Murphy K, Vythilingum B, de Villiers P, Myers B and Stein D (2015) Feasibility and preliminary responses to a screening and brief intervention program for maternal mental disorders within the context of primary care. Community Mental Health Journal 51, 962–969. doi: 10.1007/s10597-015-9853-9 [DOI] [PubMed] [Google Scholar]
- Sullivan C, Aguilar E, López-Zerón G and Parra-Cardona J (2016) Disseminating the community advocacy project in Mexico: a feasibility study. Journal of Interpersonal Violence 34(14), 2920–2937. doi: 10.1177/0886260516663901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surjaningrum E, Minas H, Jorm A and Kakuma R (2018) The feasibility of a role for community health workers in integrated mental health care for perinatal depression: a qualitative study from Surabaya, Indonesia. International Journal of Mental Health Systems 12, 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang X, Yang F, Tang T, Yang X, Zhang W, Wang X, Ji L, Xiao Y, Ma K, Wang Y, Kong X, Wang J, Liu J, Xu Q, Tian D and Qu Z (2015) Advantages and challenges of a village doctor-based cognitive behavioral therapy for late-life depression in rural China: a qualitative study. PLoS ONE 10, e0137555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tewari A, Kallakuri S, Devarapalli S, Jha V, Patel A and Maulik P (2017) Process evaluation of the systematic medical appraisal, referral and treatment (SMART) mental health project in rural India. BMC Psychiatry 17, 385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Andrade L, Borges G, Bruffaerts R, Bunting B, De Almeida JMC, Florescu S, De Girolamo G, Gureje O, Haro JM, He Y, Hinkov H, Karam E, Kawakami N, Lee S, Navarro-Mateu F, Piazza M, Posada-Villa J, De Galvis YT and Kessler RC (2017) Undertreatment of people with major depressive disorder in 21 countries. British Journal of Psychiatry 210, 119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiburcio M, Lara M, Aguilar Abrego A, Fernández M, Martínez Vélez N and Sánchez A (2016) Web-based intervention to reduce substance abuse and depressive symptoms in Mexico: development and usability test. JMIR Mental Health 3, e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita A, Kandolo K, Susser E and Burns J (2016) Use of short messaging services to assess depressive symptoms among refugees in South Africa: implications for social services providing mental health care in resource-poor settings. Journal of Telemedicine and Telecare 22, 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, Rath S, Gope R, Mahto D, Sinha R, Lakshminarayana R, Patel V, Pagel C, Prost A and Costello A (2010) Effect of a participatory intervention with women's groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. The Lancet 375, 1182–1192. [DOI] [PubMed] [Google Scholar]
- Vicente B, Kohn R, Levav I, Espejo F, Saldivia S and Sartorius N (2007) Training primary care physicians in Chile in the diagnosis and treatment of depression. Journal of Affective Disorders 98, 121–127. [DOI] [PubMed] [Google Scholar]
- Victora CG, Habicht J and Bryce J (2004) Evidence-based public health: moving beyond randomized trials. American Journal of Public Health 94, 400–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagenaar BH, Sherr K, Fernandes Q and Wagenaar AC (2016) Using routine health information systems for well-designed health evaluations in low- and middle-income countries. Health Policy and Planning 31, 129–135. doi: 10.1093/heapol/czv029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner AD, Crocker J, Liu S, Cherutich P, Gimbel S, Fernandes Q, Mugambi M, Ásbjörnsdóttir K, Masyuko S, Wagenaar BH, Nduati R and Sherr K (2019) Making smarter decisions faster: systems engineering to improve the global public health response to HIV. Current HIV/AIDS Reports 16, 279–291. doi: 10.1007/s11904-019-00449-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, Neria Y, Bradford JME, Oquendo MA and Arbuckle MR (2017) Challenges and opportunities in global mental health: a research-to-practice perspective. Current Psychiatry Reports 19, 28. doi: 10.1007/s11920-017-0780-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker I, Khanal S, Hicks J, Lamichhane B, Thapa A, Elsey H, Baral S and Newell J (2018) Implementation of a psychosocial support package for people receiving treatment for multidrug-resistant tuberculosis in Nepal: a feasibility and acceptability study. PLoS ONE 13, e0201163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt M, Mosha M, Platt A, Sikkema K, Wilson S, Turner E and Masenga G (2017) A nurse-delivered mental health intervention for obstetric fistula patients in Tanzania: results of a pilot randomized controlled trial. Pilot and Feasibility Studies 3, 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss WM, Murray LK, Zangana GAS, Mahmooth Z, Kaysen D, Dorsey S, Lindgren K, Gross A, Murray SMI, Bass JK and Bolton P (2015) Community-based mental health treatments for survivors of torture and militant attacks in Southern Iraq: a randomized control trial. BMC Psychiatry 15, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weobong B, Weiss H, McDaid D, Singla D, Hollon S, Nadkarni A, Park A, Bhat B, Katti B, Anand A, Dimidjian S, Araya R, King M, Vijayakumar L, Wilson G, Velleman R, Kirkwood B, Fairburn C and Patel V (2017) Sustained effectiveness and cost-effectiveness of the Healthy Activity Programme, a brief psychological treatment for depression delivered by lay counsellors in primary care: 12-month follow-up of a randomised controlled trial. PLoS Medicine 14, e1002385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank Country and Lending Groups (2018) Available at https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (Accessed 20 March 2019).
- Yang M, Jia G, Sun S, Ye C, Zhang R and Yu X (2019) Effects of an online mindfulness intervention focusing on attention monitoring and acceptance in pregnant women: a randomized controlled trial. Journal of Midwifery & Women's Health 64, 68–77 [DOI] [PubMed] [Google Scholar]
- Yang JP, Simoni JM, Dorsey S, Lin Z, Sun M, Bao M and Lu H (2018) Reducing distress and promoting resilience: a preliminary trial of a CBT skills intervention among recently HIV-diagnosed MSM in China. AIDS Care – Psychological and Socio-Medical Aspects of AIDS/HIV 30(Supp5), S39–S48. doi: 10.1080/09540121.2018.1497768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung A, Wang F, Feng F, Zhang J, Cooper A, Hong L, Wang W, Griffiths K, Bennett K, Bennett A, Alpert J and Fava M (2018) Outcomes of an online computerized cognitive behavioral treatment program for treating Chinese patients with depression: a pilot study. Asian Journal of Psychiatry 38, 102–107. [DOI] [PubMed] [Google Scholar]
- Zafar S, Sikander S, Haq Z, Hill Z, Lingam R, Skordis-Worrall J, Hafeez A, Kirkwood B and Rahman A (2014) Integrating maternal psychosocial well-being into a child-development intervention: the five-pillars approach. Annals of the New York Academy of Sciences 1308, 107–117. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/gmh.2020.1.
click here to view supplementary material