Abstract
Background
Face mask usage by the healthy population in the community to reduce risk of transmission of respiratory viruses remains controversial. We assessed the effect of community-wide mask usage to control coronavirus disease 2019 (COVID-19) in Hong Kong Special Administrative Region (HKSAR).
Methods
Patients presenting with respiratory symptoms at outpatient clinics or hospital wards were screened for COVID-19 per protocol. Epidemiological analysis was performed for confirmed cases, especially persons acquiring COVID-19 during mask-off and mask-on settings. The incidence of COVID-19 per million population in HKSAR with community-wide masking was compared to that of non-mask-wearing countries which are comparable with HKSAR in terms of population density, healthcare system, BCG vaccination and social distancing measures but not community-wide masking. Compliance of face mask usage in the HKSAR community was monitored.
Findings
Within first 100 days (31 December 2019 to 8 April 2020), 961 COVID-19 patients were diagnosed in HKSAR. The COVID-19 incidence in HKSAR (129.0 per million population) was significantly lower (p<0.001) than that of Spain (2983.2), Italy (2250.8), Germany (1241.5), France (1151.6), U.S. (1102.8), U.K. (831.5), Singapore (259.8), and South Korea (200.5). The compliance of face mask usage by HKSAR general public was 96.6% (range: 95.7% to 97.2%). We observed 11 COVID-19 clusters in recreational ‘mask-off’ settings compared to only 3 in workplace ‘mask-on’ settings (p = 0.036 by Chi square test of goodness-of-fit).
Conclusion
Community-wide mask wearing may contribute to the control of COVID-19 by reducing the amount of emission of infected saliva and respiratory droplets from individuals with subclinical or mild COVID-19.
Keywords: Face mask, Community, Coronavirus, COVID-19, SARS-COV-2, Epidemic
Introduction
Coronavirus disease 2019 (COVID-19) due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is closely related to bat SARS related coronaviruses,1 is the second pandemic of the 21st century following the influenza A H1N1 pandemic of 2009. With the rapidly galloping epidemic due to globalization and international travel, World Health Organization (WHO) declared COVID-19 to be a pandemic on 11 March 2020,2 which is 72 days after the first official announcement of clusters of patients with community-acquired pneumonia in Wuhan, Hubei Province of China on 31 December 2019 (day 1).3 As of 8 April 2020 (day 100), over 1.35 million people have been infected worldwide with nearly 80,000 deaths.4 In response, proactive infection control measures have been implemented in hospital settings.5 , 6 In addition, non-pharmaceutical public health interventions including border control or closure, quarantine and testing of all incoming travelers or returnees, massive reverse-transcription polymerase chain reaction (RT-PCR) testing for case detection, rapid contact tracing and quarantine, frequent hand hygiene, and later social distancing measures including school closure, home office, cancelation of all mass gatherings, later stay-at-home order, and cessation of all socioeconomic activities except essential services, were also adopted to various degrees and at different time points in different geographical areas to reduce the risk of community transmission. Many of these measures had been used for the control of community transmission of severe acute respiratory syndrome (SARS) in 2003 and pandemic influenza A H1N1 in 2009 in Hong Kong Special Administrative Region of China (HKSAR) and other parts of the world.7 , 8 However, the efficacy of community-wide masking of the population during these past epidemics or the present COVID-19 pandemic has not been clearly investigated. Unlike 2003 SARS which was generally manifested with high fever and progressive pneumonia with a mortality of about 10%, COVID-19 can be associated with very mild symptoms and a mortality of less than 4%. Thus subclinical or asymptomatic SARS-CoV-2 shedders may play an important role in perpetuating the pandemic.9 , 10 We hypothesized that community-wide masking in HKSAR may break the chain of transmission of SARS-CoV-2 by reducing the infectiousness of the subclinical virus shedders while also offering some protection to the susceptible population.
In HKSAR, community-wide masking was practiced by the general population at an early stage of the local COVID-19 epidemic. Here, we described the comparative epidemiology of COVID-19 during the first 100 days. We also analyzed the incidence of COVID-19 in geographical areas with or without community-wide masking for most individuals, and also the number of COVID-19 clusters of COVID-19 in relation to workplace (mask-on setting) or non-workplace recreational settings (mask-off setting) of HKSAR.
Methods
Community control measures against COVID-19 in HKSAR
HKSAR is a cosmopolitan city of 7.45 million people in Southern China. Occupying only 1104 square-kilometers, it is the third most densely populated area in the world with around 6700 people per square-kilometer. Soon after the official announcement of a cluster of patients with community-acquired pneumonia in Wuhan by the National Health Commission of the People's Republic of China, on 31 December 2019 (day 1), the center for Health Protection (CHP) of the Department of Health, the HKSAR government alerted members of the public to maintain good personal and environmental hygiene, with specific emphasis on hand hygiene, refraining from work or attending class at school, avoiding crowded places, seek medical advice promptly and wear a surgical mask if they develop respiratory symptoms.3 Step-wise introduction of other community interventions later to control the spread of COVID-19 was described. As an objective parameter of community-wide preparedness, compliance of face mask usage by the general public monitored by staff working in Infection Control Unit, and Department of Microbiology, Queen Mary Hospital for three consecutive days from 6 April to 8 April 2020 (day 98 to day 100). Each staff member would count the number of persons not wearing a mask among the first 50 persons encountered in the street during their morning commute. The residential district of the staff was recorded.
Epidemiology of COVID-19 in HKSAR
A multi-pronged screening strategy to identify patients infected with SARS-CoV-2 was implemented.5 , 6 The epidemiology of newly confirmed cases was announced in the daily press conference jointly held by CHP and Hospital Authority. Major clusters arising from mask-on (workplace) and mask-off (recreational) settings were analyzed to evaluate the efficacy of wearing face masks.
Comparing the epidemiology of COVID-19 in HKSAR and other parts of the world
The epidemiology of COVID-19 of HKSAR was compared to that of the representative countries in North America, Europe, and Asia using publicly accessible information from the website of WHO to understand the overall effect of our control measures used in HKSAR. Countries with well-established healthcare system, where face mask usage was not universally adopted in the community, and having over 100 confirmed cases at day 72 when WHO declared a pandemic were selected for comparison.
Laboratory diagnosis of SARS-CoV-2
Clinical specimens including nasopharyngeal aspirates, nasopharyngeal swabs, throat swab, saliva, sputum, endotracheal aspirates, or bronchoalveolar lavage were subjected to nucleic acid extraction by the eMAG extraction system (bioMérieux, Marcy-l’Étoile France) as we previously described.5 , 6 The presence of SARS-CoV-2 RNA in specimens was first determined by the LightMix Modular SebeccoV E-gene commercial kit (TIB Molbiol, Berlin, Germany) at all public hospitals under the Hospital Authority and the Public Health Laboratory Service of the Department of Health, and further confirmed by in-house real-time RT-PCR assay targeting the SARS-CoV-2 RNA-dependent RNA polymerase/helicase gene as described.11
Statistical analysis
Incidence rates were compared using the exact Poisson test using R software. Proportions were compared using the chi-squared test. A p value of <0.05 was considered statistically significant.
Results
Community response to COVID-19 in HKSAR
Due to the prior experience of the SARS outbreak in 2003, the general public of HKSAR was on high alert after the official announcement of a cluster of pneumonia cases of unknown etiology in Wuhan on 31 December 2019 (day 1), because a total of 1755 infected persons with 299 (17.0%) deaths over 133 days (11 February 2003 to 23 June 2003) was recorded during this past SARS epidemic. When the causative agent of COVID-19 was identified on 9 January 2020 (day 10), and named as SARS-CoV-2 on 12 February 2020 (day 44), this emerging pathogen was perceived to be as detrimental as 2003 SARS-CoV by the HKSAR general public. Even though initially HKSAR government only advocated people with respiratory symptoms to wear a surgical mask according to the recommendations of WHO and Centers for Disease Control and Prevention (CDC) of the United States, the general public volunteered to wear face mask quite compliantly from the pre-pandemic to pandemic phase of COVID-19.
Sixty-seven staff members (9 from Infection Control Unit, and 58 from Department of Microbiology), residing in all 18 administrative districts in HKSAR, recorded the number of persons not wearing face mask among the first 50 people they encountered during their morning commute to Queen Mary Hospital (located in Southern district) between 7:00am to 9:00am over three consecutive days from 6 April to 8 April 2020 (day 98 to day 100). A total of 10,050 persons were observed. Only 337 (3.4%) persons did not wear face mask. The daily compliance of face mask usage was 97.2%, 97.1%, and 95.7% over three consecutive days in all 18 administrative districts in HKSAR.
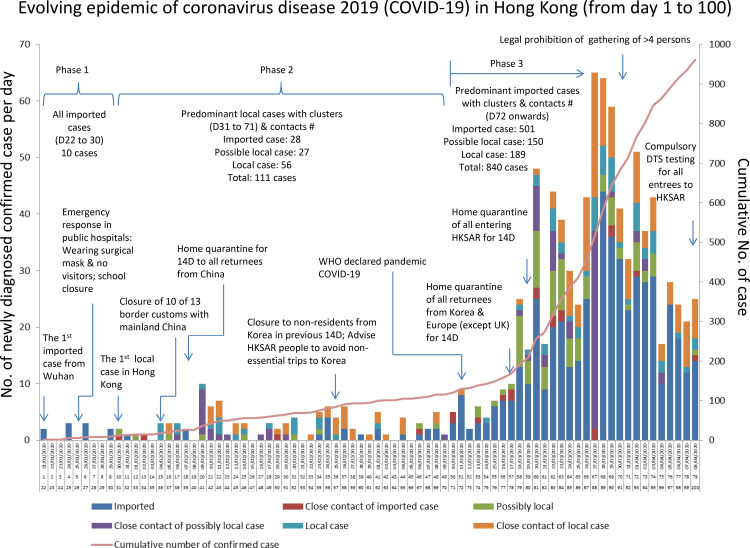
Besides proactive infection control measures implemented by public hospitals under the governance of Hospital Authority,5 , 6 step-wise introduction of epidemiological measures by the HKSAR government were enforced. They included border controls to reduce imported SARS-CoV-2 cases from mainland China on 4 February 2020 (day 36). This was followed by imposing home quarantine order for 14 days to all entrees from mainland China on 8 February 2020 (day 40). Subsequently, the quarantine order was progressively imposed to all entrees into HKSAR on and after 19 March 2020 (day 80) (Fig. 1 ). All entrees were compulsorily tested for SARS-CoV-2 by collecting their posterior oropharyngeal saliva with effect from 8 April 2020 (day 100). As in other localities, isolation of confirmed case, contact tracing and quarantine, closure of affected or high risk premises, and social distancing measures such as home-office and school closure were instituted.
Fig. 1.
Evolving epidemic of coronavirus disease 2019 (COVID-19) in Hong Kong (from day 1 to 100).
Note. #including their close contacts
COVID-19, coronavirus disease 2019; DTS, deep throat saliva; WHO, World Health Organization.
Epidemiology of COVID-19 in HKSAR
Up to day 100 of the epidemic, a total of 961 cases of COVID-19 were confirmed in HKSAR. Transmission of COVID-19 was divisible into four phases: phase 0 (from day 1 to 21) with no confirmed cases of COVID-19 in HKSAR; phase 1 (from day 22 to 30) with 10 imported cases; phase 2 (from day 31 to 71) with 111 cases (predominantly local cases) and; phase 3 (from day 72, WHO declared COVID-19 pandemic, onwards) with 840 cases (predominantly imported cases with local clusters of cases) (Fig. 1). Among the 961 confirmed cases, there were 11 clusters of 113 persons that were directly engaged in mask-off activities such as dining and drinking in restaurant or bar, singing at karaoke, and exercise in fitness clubs. There were only three clusters involving 11 persons engaged in mask-on settings at the workplace. Using the chi-square test of goodness-of-fit with Williams’ continuity correction, there were significantly more COVID-19 clusters involving mask-off settings than might be expected assuming that the null hypothesis of equal number of clusters involving mask-on and mask-off settings was true (p = 0.036).
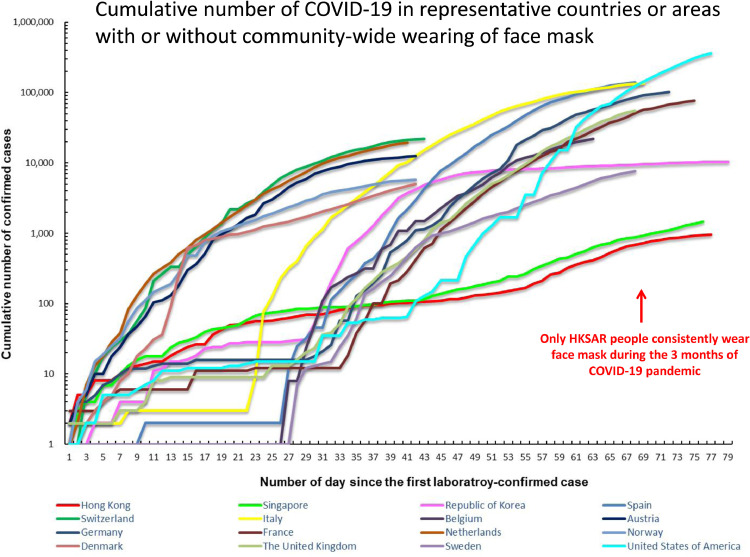
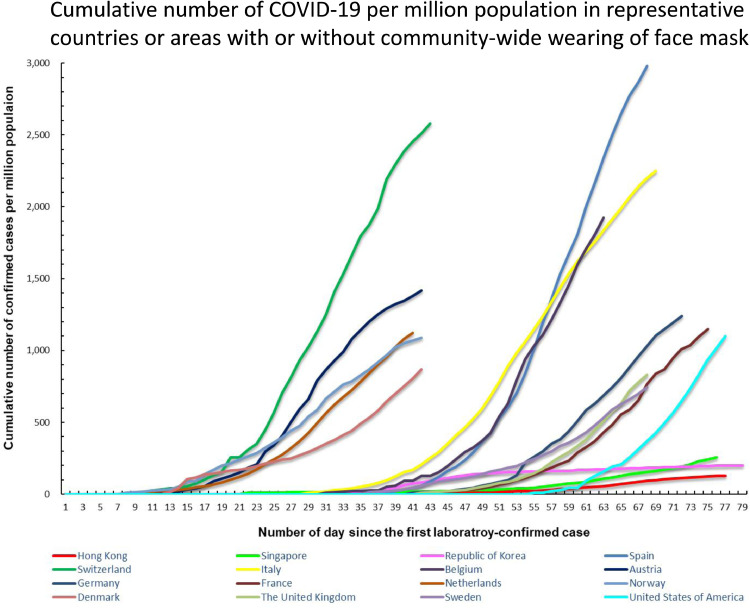
Comparing the epidemic progression of COVID-19 in HKSAR with other parts of the world
The incidence and cumulative number of COVID-19 cases in HKSAR and the representative countries or areas since the first laboratory-confirmed case of SARS-CoV-2 are illustrated in Fig. 2a & 2b . The incidence of COVID-19 in HKSAR was significantly less than that of the selected countries (with well-established healthcare system and having over 100 confirmed cases at day 72 when WHO declared a pandemic) in Asia, Europe, and North America, where face mask usage was not universally adopted in the community (Table 1 ). Singapore's land area and population density are comparable to HKSAR.4 On day 100 (8 April 2020), the incidence of COVID-19 per million population in Singapore was significantly higher than that in HKSAR (259.8 per million population vs 129.0 per million population, p <0.001) (Table 2 ). In South Korea, the number of molecular diagnostic tests per million population was comparable to HKSAR. The proportion of local cases in South Korea related to mask-off settings was significantly higher than that in HKSAR [5150/10,384 (49.6%) vs 113 / 961 (11.8%), p<0.001] because of super-spreading events at a church which was also a mask-off setting (Table 2).
Fig. 2a.
Cumulative number of COVID-19 in representative countries or areas with or without community-wide wearing of face mask
Note. The x-axis denotes the number of days since the first laboratory-confirmed case in the representative countries or areas.
The date of first laboratory-confirmed case in Hong Kong (21 January 2020), Singapore (24 January 2020), South Korea (21 January 2020), Spain (1 February 2020), Switzerland (26 February 2020), Italy (31 January 2020), Belgium (06 February 2020), Austria (27 February 2020), Germany (28 January 2020), France (25 January 2020), Netherlands (28 February 2020), Norway (27 February 2020), Denmark (27 February 2020), The United Kingdom (1 February 2020), Sweden (01 February 2020) and United States of America (23 January 2020).
Fig. 2b.
Cumulative number of COVID-19 per million population in representative countries or areas with or without community-wide wearing of face mask
Note. The x-axis denotes the number of day since the first laboratory-confirmed case in the representative countries or areas.
The date of first laboratory-confirmed case in Hong Kong (21 January 2020), Singapore (24 January 2020), South Korea (21 January 2020), Spain (1 February 2020), Switzerland (26 February 2020), Italy (31 January 2020), Belgium (06 February 2020), Austria (27 February 2020), Germany (28 January 2020), France (25 January 2020), Netherlands (28 February 2020), Norway (27 February 2020), Denmark (27 February 2020), The United Kingdom (1 February 2020), Sweden (01 February 2020) and United States of America (23 January 2020).
Table 1.
Incidence of coronavirus disease 2019 (COVID-19) infection in Hong Kong Special Administrative Region (HKSAR) as compared with that of selected countries as of 8 April 2020 (at day 100 after official announcement of pneumonia outbreak in Wuhan, Hubei Province, China)a.
| Countries or city | Population (million)b | Cumulative number of confirmed casec | Number (percentage) of death | Incidence per million populationd | P value (incidence compared with HKSAR) | Population density: population per km2 (rank in the world)e |
|---|---|---|---|---|---|---|
| Hong Kong SARf | 7.45 | 961 | 4 (0.4%) | 129.0 | Not applicable | 6782 (3rd) |
| Western Pacific Region | ||||||
| Singapore | 5.70 | 1,481 | 6 (0.4%) | 259.8 | P<0.001 | 7894 (2nd) |
| South Korea | 51.78 | 10,384 | 200 (1.9%) | 200.5 | P<0.001 | 517 (13th) |
| European Region | ||||||
| Spain | 47.10 | 140,510 | 13,798 (9.8%) | 2,983.2 | P<0.001 | 93 (89th) |
| Switzerland | 8.59 | 22,164 | 641 (2.9%) | 2,580.2 | P<0.001 | 208 (48th) |
| Italy | 60.24 | 135,586 | 17,129 (12.6%) | 2,250.8 | P<0.001 | 200 (51st) |
| Belgium | 11.52 | 22,194 | 2,035 (9.2%) | 1,926.6 | P<0.001 | 376 (22nd) |
| Austria | 8.90 | 12,640 | 243 (1.9%) | 1,420.2 | P<0.001 | 106 (76th) |
| Germany | 83.15 | 103,228 | 1,861 (1.8%) | 1,241.5 | P<0.001 | 233 (41st) |
| France | 67.06 | 77,226 | 10,313 (13.4%) | 1,151.6 | P<0.001 | 123 (68th) |
| Netherlands | 17.44 | 19,580 | 2,101 (10.7%) | 1,122.7 | P<0.001 | 420 (16th) |
| Norway | 5.37 | 5,863 | 69 (1.7%) | 1,091.8 | P<0.001 | 17 (171st) |
| Denmark | 5.82 | 5,071 | 203 (4.0%) | 871.3 | P<0.001 | 135 (64th) |
| The United Kingdom | 66.44 | 55,246 | 6,159 (11.1%) | 831.5 | P<0.001 | 274 (32nd) |
| Sweden | 10.33 | 7,693 | 591 (7.7%) | 744.7 | P<0.001 | 23 (159th) |
| Region of Americas | ||||||
| United States of America | 329.45 | 363,321 | 10,845 (3.0%) | 1,102.8 | P<0.001 | 34 (145th) |
Developed countries with well-established healthcare system and reached more than 100 confirmed cases at day 72 (WHO declare pandemic COVID-19) were selected for comparison.
The population of country or city were retrieved from the website of World Health Organization.
Infection retrieved from situation report - 79 of World Health Organization issued on 8 April 2020 (day 100 after the official announcement of clusters of community-acquired pneumonia in Wuhan, Hubei Province, China.
The sequence of countries was listed as descending order in accordance with the incidence of COVID-19 per million population.
Information retrieved from Wikipedia - List of countries and dependencies by population density. https://en.wikipedia.org/wiki/List_of_countries_and_dependencies_by_population_density (Accessed 12 April 2020).
The number of confirmed case was based on the official announcement daily by HKSAR, China.
Table 2.
Comparison of the epidemiology and community responses against coronavirus disease 2019 (COVID-19) in Hong Kong SAR, Singapore, and South Korea.
| Epidemiology parameter as of 8 April 2020 | Hong Kong SAR | Singapore | South Korea |
| Total number of confirmed case | 961 | 1,481 | 10,384 |
| Number of imported cases | 517 (53.8%) | 567 (38.3%)a | NM |
| Number of RT-PCR performed per million population | ∼15,000 | ∼12,800b | ∼9,900c |
| Number of local cases related to mask-off setting (i.e. religious activities, dining and drinking in restaurant or bar, singing at karaoke, and exercise in gymnasium) | 113 (11.8%) | NM | 5150 (49.6%)c,d |
| Number of local cases related to family (other than mask-off setting described above) | 41 (4.3%) | NM | NM |
| Number of local cases related to mask-on setting (i.e. workplace) | 11 (1.4%) | NM | NM |
| Date of border restrictions | 25 March 2020e | 23 March 2020, 2359f | 1 April 2020g |
| Average of ambient temperature range in the first 100 days of COVID-19 transmission | 18 °C to 22 °Ch | 24 °C to 31 °Ci | 1 °C to 9 °Cj |
| Routine childhood BCG immunization programk | Yes | Yes | Yes |
Note. NM, not mentioned.
Daily report on COVID-19. Minister of Health, Singapore. https://www.moh.gov.sg/docs/librariesprovider5/local-situation-report/situation-report-1-apr-2020.pdf. Accessed 12 April 2020.
Information obtained from Minister of Health, Singapore. https://www.moh.gov.sg/covid-19. Accessed 12 April 2020.
Information obtained from Coronavirus Disease-19, Republic of Korea. http://ncov.mohw.go.kr/en/. Accessed 12 April 2020.
These patients were all related to a cohort of participants involving in religious activities - wearing face masks was discouraged. These were the believer of Olive Tree, a Christian new religious movement, originally known as Jesus Christ Congregation Revival Association of Korea, founded in Republic of Korea by Park Tae Son. https://en.wikipedia.org/wiki/Olive_Tree_(religious_movement). Accessed 12 April 2020.
Deny entry of non-Hong Kong resident.
All short-term visitors (from anywhere in the world) will not be allowed to enter or transit through Singapore.
All passengers are subject to mandatory self-quarantine for 14 days, except for airline crew. https://en.wikipedia.org/wiki/Travel_restrictions_related_to_the_2019%E2%80%9320_coronavirus_pandemic. Accessed 12 April 2020.
https://www.hko.gov.hk/en/wxinfo/pastwx/mws/mws.htm. Accessed 12 April 2020.
https://www.climatestotravel.com/climate/singapore. Accessed 12 April 2020.
https://www.climatestotravel.com/climate/south-korea. Accessed 12 April 2020.
There is postulation of countries with BCG vaccination program tends to have lower incidence and death due to COVID-1919.
Discussion
Evidence for using face masks to prevent transmission of respiratory viruses in the community remains limited to a few studies conducted in the household setting.12 , 13 Although there is no expert consensus on this issue, universal masking is voluntarily adopted by people in our HKSAR community soon after the first imported case of COVID-19 was reported. This public action was linked to the painful experience of the 2003 SARS outbreak (1755 cases with 299 deaths in 6.73 million population) when HKSAR people adopted universal masking in addition to other non-pharmaceutical interventions such as hand hygiene, social distancing and school closure.7 These community hygienic measures during the SARS outbreak resulted in a significant reduction of positive specimens of all circulating respiratory viruses including influenza viruses in 2003 compared with preceding periods.14 In a case-control study conducted in Beijing during 2003 SARS, consistent wearing of a face mask outdoors was associated with a 70% risk reduction, compared to those not wearing a face mask.15
HKSAR is the only area practicing universal masking despite the recommendation of WHO and CDC that mask should be reserved for those with symptoms and in healthcare settings. We therefore compared the number of COVID-19 clusters in mask-on settings at workplace with that of the mask-off settings such as dining and drinking in restaurant or bar, singing at karaoke, and exercising in gymnasium, where there was a large gathering of people sharing food, drinks, and instruments. In effect, these mask-off settings allowed the sharing of their saliva and respiratory droplets, which may contain a viral load of 100 million per ml, directly or indirectly.16 , 17 In HKSAR hospitals, wearing face masks is mandatory during the pandemic. It is also the practice among many community service providers and those who are working indoors. Since the supply of face mask was tight in the community as well as in the healthcare setting, it is the practice of our general public not to use more than one face mask per person per day. We observed that the overall compliance of face mask usage was 97% in all administrative districts in the morning. Thus we have the reason to believe that their compliance to face mask usage would remain high throughout the day at the workplace. It is therefore not surprising that the number of COVID-19 clusters was significantly higher in the mask-off recreational settings in HKSAR.
Universal masking in the community may mitigate the extent of transmission of COVID-19 and may be a necessary adjunctive public health measure in a densely populated city like HKSAR, with an average of 170,000 people entering HKSAR from Mainland and overseas per day.18 Our incidence of COVID-19 was also lower than that of other areas with local transmission, vindicating this approach. In particular, our incidence of COVID-19 was significantly lower than that of Singapore, a city comparable with HKSAR in terms of area, population density, healthcare infrastructure, BCG vaccination,19 as well as adopting social distancing strategies and SARS-CoV-2 testing infrastructure.20 Besides a lower ambient temperature and a higher risk of importation of COVID-19 cases from the mainland which are factors promoting COVID-19 transmission in HKSAR, the most important difference between the two cities is the community-wide usage of face masks in HKSAR but not in Singapore. Moreover, 50% of local transmission of COVID-19 in South Korea was attributed to religious activities where face mask usage was discouraged. Mask-off activities clearly have potential implications for COVID-19 transmission in the community.
However, the use of face mask in the community remains controversial.21 , 22 WHO issued an interim guideline regarding the use of masks in the context of COVID-19 on 6 April 2020, stating no evidence that wearing a mask by healthy persons in the wider community setting can prevent acquisition of COVID-19.23 European Centre for Disease Prevention and Control issued a technical report on 8 April 2020 that the use of face masks in the community could be considered, especially when visiting busy, closed spaces, despite not knowing how much the use of masks in the community can contribute to a decrease in transmission in addition to the other counter measures.24 On 3 April 2020, CDC recommended the use of cloth face coverings, especially in areas of significant community-based transmission.25 The shift of paradigm from not recommending to promoting the use of face masks was based on the rationale of pre-symptomatic shedding of SARS-Cov-2 and presence of asymptomatic patients with high viral load in the community.9 , 26 The use of face mask may serve as source control by preventing dispersal of droplets during talking, sneezing, and coughing,27 and also reduce the risk of environmental contamination by SARS-CoV-2. Despite some supporters of WHO recommendation speaking against universal masking in our local medical community, most opinion leaders in the clinical microbiology and infectious disease specialties of HKSAR openly championed this measure for the control of community transmission of COVID-19.28 Masking is a continuous form of protection to stop the spreading of saliva and respiratory droplets to others or from others, and to the environment or from the environment to the susceptible by hands through touching of nose, mouth and eye. Touching nose and mouth is a subconscious behavior.29 Hand hygiene is always the cornerstone to prevent transmission of COVID-19 but it is a one-off discontinuous process where hand contamination may occur easily between each alcoholic handrubbing or hand washing. Although we have successfully implemented directly observed hand hygiene (DOHH) by regular delivery of alcohol-based hand rub to conscious hospitalized patients and persons in residential care homes for the elderly before meal and medication rounds,30, 31, 32 it may be difficult to practice DOHH in the community. Studies have also shown that wearing a mask with frequent hand hygiene significantly reduced transmission of seasonal influenza virus in the community setting. But once the effect of the use of surgical mask was removed, the effect of hand hygiene became insignificant.33 With the understanding that the supply of face masks should primarily be reserved for usage in healthcare settings, we believe that it is still advisable to encourage people to wear face masks in the public based on the precautionary principles.34 Moreover, wearing a cloth mask with less filtration efficiency may still be better than no mask at all in communities of high transmission.
SARS-CoV-2 is a highly transmissible respiratory virus which causes upper and lower respiratory tract infection leading to a high viral load in respiratory secretions and saliva as shown in clinical studies and transmission studies by close contact in animal models.35 Moreover, SARS-CoV-2 can suppress the host innate immune response in terms of interferon and cytokine response which in turn leads to a higher level of viral replication than that by the 2003 SARS-CoV in an ex vivo lung tissue explant model.10 These ex vivo findings supported the suggestion that an important proportion of COVID-19 patients may be pre-symptomatic or mildly symptomatic virus shedders. These groups of patients are unlikely to be tested or isolated and may contribute to the perpetuation of the pandemic. Therefore community-wide mask usage irrespective of symptoms may reduce the infectivity of these silent COVID-19 cases to the susceptible individuals.
There are several limitations in our study. First, we did not analyze the mask-off settings in the family because the modes of transmission among close household contacts can be more diverse. If the 15 family clusters were also counted within the mask-off settings, the difference would be even more significant (p<0.001). Second, the type of mask used in the community cannot be controlled. The compliance of wearing face mask in terms of not touching the external surface of mask or face, and hand hygiene before or after touching the mask cannot be assessed. Third, we cannot count the mask compliance directly for every community settings. Nevertheless, in the absence of effective antiviral and vaccines, the pandemic spread COVID-19 to many countries provide an unique opportunity to study the effectiveness of this non-pharmaceutical control measures. As of 27 February 2020 (day 38 since the first reported case in South Korea), South Korea government has started to distribute face masks to the public amid the outbreak of the COVID-19,36 which was associated with a flattening of the epidemic curve. As of 14 April 2020 (day 82 since the first reported case in Singapore), Singapore government has started to enforce a penalty of 300 Singapore dollar for anyone going out from home without a mask.37 Further studies on this important non-pharmaceutical control measure are warranted. In order to live with emerging infectious diseases and seasonal influenza epidemics, every individual should have personalized reusable mask, gown, and gloves made of self-disinfecting fabrics, and even reusable anti-fog face shield within their own set of Epidemic Combat Kit for their personal protection.
Financial support
This work was supported in part by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, the Ministry of Education of China.
Declaration of Competing Interest
All authors report no conflicts of interest relevant to this article.
Acknowledgments
Acknowledgement
We thank colleagues of Hospital Authority and Department of Health for facilitating this study.
References
- 1.Chan J.F., Kok K.H., Zhu Z., Chu H., To K.K., Yuan S. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020;9:221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020Accessed 10 April 2020.
- 3.The Centre for health protection closely monitors cluster of pneumonia cases on Mainland. Press release of the department of health, Hong Kong Special Administrative Region. 2019. https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htmAccessed 10 April 2020.
- 4.Coronavirus disease 2019 (COVID-19). Situation Report – 79. World Health Organization. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200408-sitrep-79-covid-19.pdf?sfvrsn=4796b143_6Accessed 10 April 2020.
- 5.Cheng V.C.C., Wong S.C., To K.K.W., Ho P.L., Yuen K.Y. Preparedness and proactive infection control measures against the emerging novel coronavirus in China. J Hosp Infect. 2020;104:254–255. doi: 10.1016/j.jhin.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020:1–6. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng V.C., Lau S.K., Woo P.C., Yuen K.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 2007;20:660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng V.C., To K.K., Tse H., Hung I.F., Yuen K.Y. Two years after pandemic influenza A/2009/H1N1: what have we learned? Clin Microbiol Rev. 2012;25:223–263. doi: 10.1128/CMR.05012-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chu H., Chan J.F., Wang Y., Yuen T.T., Chai Y., Hou Y. Comparative replication and immune activation profiles of SARS-CoV-2 and SARS-CoV in human lungs: an ex vivo study with implications for the pathogenesis of COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan J.F., Yip C.C., To K.K., Tang T.H., Wong S.C., Leung K.H. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J Clin Microbiol. 2020 doi: 10.1128/JCM.00310-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacIntyre C.R., Cauchemez S., Dwyer D.E., Seale H., Cheung P., Browne G. Face mask use and control of respiratory virus transmission in households. Emerg Infect Dis. 2009;15:233–241. doi: 10.3201/eid1502.081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowling B.J., Chan K.H., Fang V.J., Cheng C.K., Fung R.O., Wai W. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann Intern Med. 2009;151:437–446. doi: 10.7326/0003-4819-151-7-200910060-00142. [DOI] [PubMed] [Google Scholar]
- 14.Lo J.Y., Tsang T.H., Leung Y.H., Yeung E.Y., Wu T., Lim W.W. Respiratory infections during SARS outbreak, Hong Kong, 2003. Emerg Infect Dis. 2005;11:1738–1741. doi: 10.3201/eid1111.050729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu J., Xu F., Zhou W., Feikin D.R., Lin C.Y., He X. Risk factors for SARS among persons without known contact with SARS patients, Beijing, China. Emerg Infect Dis. 2004;10:210–216. doi: 10.3201/eid1002.030730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.To K.K., Tsang O.T., Chik-Yan Yip C., Chan K.H., Wu T.C., Chan J.M.C. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.To K.K., Tsang O.T., Leung W.S., Tam A.R., Wu T.C., Lung D.C. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong Kong in figures. Census and Statistics Department. Hong Kong Special Administrative Region. 2020. https://www.statistics.gov.hk/pub/B10100062020AN20B0100.pdf. Accessed 24 April 2020.
- 19.Gursel M., Gursel I. Is global BCG vaccination coverage relevant to the progression of SARS-CoV-2 pandemic? Med Hypothesis. 2020 doi: 10.1111/all.14345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Updates on COVID-19 (Coronavirus disease 2019) local situation. Ministry of Health, Singapore. 2020. https://www.moh.gov.sg/covid-19 Accessed 12 April 2020.
- 21.Chan K.H., Yuen K.Y. COVID-19 epidemic: disentangling the re-emerging controversy about medical facemasks from an epidemiological perspective. Int J Epidemiol. 2020 doi: 10.1093/ije/dyaa044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Advice on the use of masks in the context of COVID-19. Interim guidance (6 April 2020). https://apps.who.int/iris/bitstream/handle/10665/331693/WHO-2019-nCov-IPC_Masks-2020.3-eng.pdf?sequence=1&isAllowed=yAccessed 10 April 2020.
- 24.Using face masks in the community - Reducing COVID-19 transmission from potentially asymptomatic or pre-symptomatic people through the use of face masks. 2020. https://www.ecdc.europa.eu/en/publications-data/using-face-masks-community-reducing-covid-19-transmission Accessed 10 April 2020.
- 25.Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). Recommendation regarding the use of cloth face coverings, especially in areas of significant community-based transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.htmlAccessed 10 April 2020
- 26.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hui D.S., Chow B.K., Chu L., Ng S.S., Lee N., Gin T. Exhaled air dispersion during coughing with and without wearing a surgical or N95 mask. PLoS ONE. 2012;7:e50845. doi: 10.1371/journal.pone.0050845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan A.L.Y., Leung C.C., Lam T.H., Cheng K.K. To wear or not to wear: WHO’s confusing guidance on masks in the covid-19 pandemic. BMJ opinion. 2020 [Google Scholar]; https://blogs.bmj.com/bmj/2020/03/11/whos-confusing-guidance-masks-covid-19-epidemic/. Accessed 24 April 2020
- 29.Hendley J.O., Wenzel R.P., Gwaltney J.M., Jr. Transmission of rhinovirus colds by self-inoculation. N Engl J Med. 1973;288:1361–1364. doi: 10.1056/NEJM197306282882601. [DOI] [PubMed] [Google Scholar]
- 30.Cheng V.C., Tai J.W., Li W.S., Chau P.H., So S.Y., Wong L.M. Implementation of directly observed patient hand hygiene for hospitalized patients by hand hygiene ambassadors in Hong Kong. Am J Infect Control. 2016;44:621–624. doi: 10.1016/j.ajic.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 31.Cheng V.C.C., Wong S.C., Wong S.C.Y., Yuen K.Y. Directly observed hand hygiene - from healthcare workers to patients. J Hosp Infect. 2019;101:380–382. doi: 10.1016/j.jhin.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 32.Cheng V.C.C., Chen H., Wong S.C., Chen J.H.K., Ng W.C., So S.Y.C. Role of hand hygiene ambassador and implementation of directly observed hand hygiene among residents in residential care homes for the elderly in Hong Kong. Infect Control Hosp Epidemiol. 2018;39:571–577. doi: 10.1017/ice.2018.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong V.W., Cowling B.J., Aiello A.E. Hand hygiene and risk of influenza virus infections in the community: a systematic review and meta-analysis. Epidemiol Infect. 2014;142:922–932. doi: 10.1017/S095026881400003X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greenhalgh T., Schmid M.B., Czypionka T., Bassler D., Gruer L. Face masks for the public during the covid-19 crisis. BMJ. 2020;369:m1435. doi: 10.1136/bmj.m1435. [DOI] [PubMed] [Google Scholar]
- 35.Chan J.F., Zhang A.J., Yuan S., Poon V.K., Chan C.C., Lee A.C. Simulation of the clinical and pathological manifestations of coronavirus disease 2019 (COVID-19) in golden Syrian hamster model: implications for disease pathogenesis and transmissibility. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.South Korea takes new measures to have enough face masks domestically amid coronavirus. abc News. 2020. https://abcnews.go.com/International/south-korea-takes-measures-face-masks-domestically-amid/story?id=69254114Accessed 16 April 2020.
- 37.Mandatory for all in Singapore to wear mask when out, except for kids under 2 and those doing strenuous exercise. Straits Times. 2020. https://www.straitstimes.com/singapore/coronavirus-mandatory-for-all-to-wear-a-mask-when-out-with-exceptions-for-kids-under-2-andAccessed 16 April 2020.