Abstract
Objectives:
The objectives were 2-fold: (1) to examine how high school start times relate to adolescent sleep duration, and (2) to test associations between sleep duration and mental health– and substance use–related issues and behaviors in teens.
Design:
This study examines selected questions from survey data collected between 2010 and 2013 high school students.
Setting:
Respondents included more than 9000 students in grades 9 to 12 in 8 high schools in 5 school districts across the United States.
Measurements:
The survey instrument is the 97-item Teen Sleep Habits Survey. Logistic regression models were used to calculate adjusted odds ratios and 95% confidence intervals. Because of clustering within schools and the use of repeated measures, generalized estimating equations were used to account for variance inflation.
Results:
Greater sleep duration was associated with fewer reports of various mental health– and substance use–related issues and behaviors (all P values b.01). For instance, for each additional hour of sleep reported, there was a 28% reduction in the adjusted odds of a participant reporting that he or she felt “unhappy, sad, or depressed.” Later wake-up times were associated with a reduction in risk for some, but not all factors. Later start times were significantly associated with greater sleep duration.
Conclusions:
Given that later start times allow for greater sleep duration and that adequate sleep duration is associated with more favorable mental health– and substance use–related issues and behaviors, it is important that school districts prioritize exploring and implementing policies, such as delayed start times, that may increase the amount of sleep of adolescent students, which is needed for their optimal development.
Keywords: School start time, Adolescent health, Substance use, Adolescent mental health, Sleep duration, Start time policy
Introduction
Adolescent mental health concerns and risky behaviors including substance use (nicotine, alcohol, and other drug use) are immediate causes of substantial morbidity, mortality, and social problems for youth. In addition, these types of adolescent issues can set the stage for chronic lifelong health issues. Many of these risk factors are common among adolescents. For instance, in the 2015 Youth Risk Behavior Surveillance System, 32.3% of high school students reported ever trying a cigarette, 32.8% reported using alcohol in the past 30 days, and 21.7% reported using marijuana in the past 30 days.1 Mental health concerns are also prevalent among adolescents, with 8.3% of 12- to 17-year-olds reporting 14 or more mentally unhealthy days in the past month in the 2005–2010 National Health and Nutrition Examination Survey.2 In the National Survey of Children’s Health, 7.1% of parents reported that their child aged 12–17 years had ever received a diagnosis of depression2 which may be an underestimate of true prevalence, as some depression is undiagnosed.
In recent years, sleep deficiency has received increasing attention as being a potential component cause in the development of both substance use and mental/behavioral health concerns among youth. A likely pathway for this connection is that lack of sleep is known to diminish teens’ executive cognitive functioning and emotional regulation.3 In the area of substance use, a recent analysis from the cross-sectional Monitoring the Future study demonstrated that the frequency of obtaining 7 or more hours of sleep per night was associated with a reduced risk of using cigarettes, alcohol, marijuana, and amphetamines,4 which echoes other cross-sectional reports on sleep deficiencies and substance use.5–9
With regard to mental well-being, shorter sleep duration among adolescents is associated with lower self-esteem,10 a more negative attitude toward life,11 greater difficulty with emotional regulation,12 higher rates of mood disorders,8,9,13–16 and more thoughts of suicide.9,16–18 This association between sleep issues and mental health persists into young adulthood. Sleep disorders have been correlated with lower working memory capacity and poorer mental health among emerging adults.19,20 There is also evidence that weekday/weekend discrepancies in sleep duration and timing relate to poorer mental health and behavioral outcomes as well.8,9 Short sleep duration in adolescents has further been cross-sectionally correlated with unsafe behaviors that are expressions of mental health and substance use problems such as weapon carrying, fighting, and drunk driving.15,21,22
There is an epidemic of short sleep duration among American adolescents.23 High school students often seem to stay up too late at night and then have difficulty getting out of bed the next morning. Although an estimated 9 hours 15 minutes of sleep may be optimal for adolescents,24 results from many studies have found that, on average, most adolescents report sleeping less than 8 hours on school nights.25–28 Although there are social and environmental factors that influence adolescents’ sleep behavior, such as peer pressure, homework, and screenuse, research on the sleep-wake cycle of teens over the past 30 years has identified changes in specific biological processes that occur with the onset of puberty. These biological changes unique to adolescents cause them to feel sleepy at a later time in the evening, as compared with the sleep-wake patterns of younger children.29 Given this biological obstacle to adolescents being able to successfully fall asleep at earlier hours, having an inflexible early wake-up time, such as the time that school starts each morning, limits teens’ sleep duration. Thus, early-start high schools have been identified as an important external condition that likely affects the amount of sleep teens obtain on school nights.30,31 The accumulation of evidence showing the detrimental effects of early high school start times on adolescents’ sleep duration, performance in school, and safety led the American Academy of Pediatrics to issue a policy statement in 2014 recommending that all high schools start no earlier than 8:30 AM.32 However, as recently as 2011/2012 (the most recent year for which national data are available), fewer than 15% of US high schools were in line with this recommendation.33,34
Given previous research on outcomes for students attending high schools with later start times,25,29,30 in this study we sought to test how school start times related to both adolescent sleep duration and wake-up times. We also aimed to test how these 2 factors of sleep duration and wake-up times related to mental health– and substance use–related behaviors. We hypothesized that later start times would be associated with greater sleep and later wake-up times. Furthermore, we posited that more sleep would be associated with fewer mental health and substance use risks.
Participants and methods
Participants
From 2010 to 2013, 9089 attendees in grades 9 to 12 of 8 comprehensive high schools in 5 school districts across the United States were invited to take a paper-and-pencil survey, administered in school, on sleep and selected health, academic, and behavioral issues. Table 1 displays the 8 schools that were included in this study, their start times, and when the data were collected. Students in Jackson Hole (WY) High School were surveyed twice, once in 2012, and a second time in 2013 after the school had made a start time change. All other schools were surveyed just once, during the 2010/2011 school year. Detailed methodology of this study has been previously reported.30
Table 1.
High schools, start times, and study timing
| Start time | High schools | Location | School year surveyed | Response proportion |
|---|---|---|---|---|
| 7:35 AM | Jackson Hole High School | Jackson Hole, WY | 2011/2012 | 88% |
| 8:00 AM | Boulder High School | Boulder, CO | 2010/2011 | 78% |
| Mahtomedi High School | Mahtomedi, MN | 80% | ||
| 8:05 AM | Fairview High School | Boulder, CO | 2010/2011 | 66% |
| 8:20 AM | St Louis Park High School | St Louis Park, MN | 2010/2011 | 76% |
| 8:35 AM | East Ridge High School | South Washington County, MN | 2010/2011 | 65% |
| Park High School | South Washington County, MN | 85% | ||
| Woodbury High School | South Washington County, MN | 77% | ||
| 8:55 AM | Jackson Hole High School | Jackson Hole, WY | 2012/13 | 88% |
Measures
Participants were administered the 97-item Teen Sleep Habits Survey, which was based on the School Sleep Habits Survey.35 The survey asked participants to write in their usual school-night bedtime and school-day wake-up time. For this analysis, “sleep duration” was calculated by counting the number of hours between self-reported school-night bedtime and self-reported wake-up time. Given that participants may fall asleep somewhat after their bedtime and/or may wake once or more during the night, and/or may “snooze” even after their school day wake-up time, our measure of sleep duration is an estimate, with some likely inherent error. A study by Wolfson et al36 found that subjective data using student self-report of sleep and wake times on a survey are sufficiently aligned with objective measures of sleep using actigraphy. Hence, we are confident that the sleep duration data we obtained are a valid measure for this large population.
We examined mental health and substance use factors in relation to sleep. Mental health–related issues were assessed using 8 items, each of which questioned participants how frequently in the previous 2 weeks they were “bothered or troubled” by (1) feeling too tired to do things; (2) having trouble going to sleep or staying asleep; (3) feeling unhappy, sad, or depressed; (4) feeling hopeless about the future; (5) feeling nervous or tense; (6) worrying too much about things; (7) gad nightmares or bad dreams during the night; and (8) done dangerous things without thinking. Response options for each of these outcomes were “never,” “once,” “twice,” “several times,” and “every day/night.” We dichotomized participant responses for each question into those who reported “twice” or less vs those who responded “several times” or more.
Substance use was assessed through participant self-report. Five separate questions about a range of substances were asked, using the same response set for each question. Participants were asked if they had done the following in the past 2 weeks: (1) drank a beverage with caffeine (Coke, Pepsi, Monster, Mountain Dew, Red Bull), (2) drank coffee or tea with caffeine, (3) used tobacco (cigarettes, cigars, chewing tobacco, etc), (4) drank alcohol, and (5) used drugs. Response options for each question were “never,” “once or twice a week,” “once a day,” and “several times a day.” For purposes of analysis, for the tobacco, alcohol, and drugs items, we dichotomized the responses, such that only participants who reported “never” were categorized as nonusers; those reporting “once or twice a week” or more were categorized as users. For the analysis of caffeine use, we combined the 2 caffeinated beverage items and dichotomized persons into those who reported drinking any caffeine beverage “never” or “once or twice a week” vs “once a day” or more.
Statistical analysis
Logistic regression models were used to compute the association and 95% confidence intervals between the school start time that participants experienced and their school-day wake-up time, as well as school-night sleep duration. We also tested and quantified the association between sleep variables (sleep duration and wake-up time) and the mental health– and substance use–related items. To address variance inflation due to clustering by school, school district, and repeated measures on some individual students (specifically Jackson Hole High, the one high school surveyed in 2 consecutive years), we used generalized estimating equations. All models were adjusted for the following individual-level confounders: grade level, gender, racial/ethnic background, usual academic letter grades, and use of medication to help with concentration or a learning disability. We also adjusted for the potential school-level confounder: percentage of students eligible for free and reduced lunch. Analyses were conducted with SAS, version 9.4 (SAS Institute Inc, Cary, NC).
Results
Participant demographics are shown in Table 2; we controlled for these demographic factors in our analyses. Roughly 27% of the sample reported being a racial/ethnic minority and approximately 51% were female. There was a slight overrepresentation in the younger high school grades, with 28% of the sample being in the 9th grade and 20.3% were in the 12th grade. More than 63% of the sample reported that their typical grades were A’s and B’s. Fewer than 10% of the sample reported taking medication to help with concentration or a learning disability. Because many medications for concentration or learning disabilities are stimulant drugs, they could be associated with both reduced sleep duration and differences in mental health or substance use.
Table 2.
Descriptive statistics of 8261 respondents: Teen Sleep Habits Survey, 2010–2013
| n | % | |
|---|---|---|
| Age (y), mean ± SE | 6.0 ± 0.01 | |
| Female | 4223 | 51.1 |
| Race/ethnicity | ||
| White | 6047 | 73.2 |
| Hispanic | 730 | 8.8 |
| Asian | 489 | 5.9 |
| Black | 344 | 4.2 |
| Other | 229 | 2.8 |
| Multiracial | 422 | 5.1 |
| Grade level | ||
| 9 | 2313 | 28 |
| 10 | 2271 | 27.5 |
| 11 | 1999 | 24.2 |
| 12 | 1678 | 20.3 |
| School district | ||
| South Washington County, MN | 3547 | 42.9 |
| Boulder, CO | 2250 | 27.2 |
| Teton County, WY | 905 | 11.0 |
| Saint Louis Park, MN | 845 | 10.2 |
| Mahtomedi, MN | 714 | 8.6 |
| Usual academic grades | ||
| A’s and B’s or higher | 5249 | 63.5 |
| B’s or lower | 3012 | 36.5 |
| Use of medication to help with concentration or a learning disability | ||
| No | 7507 | 90.9 |
| Yes | 754 | 9.1 |
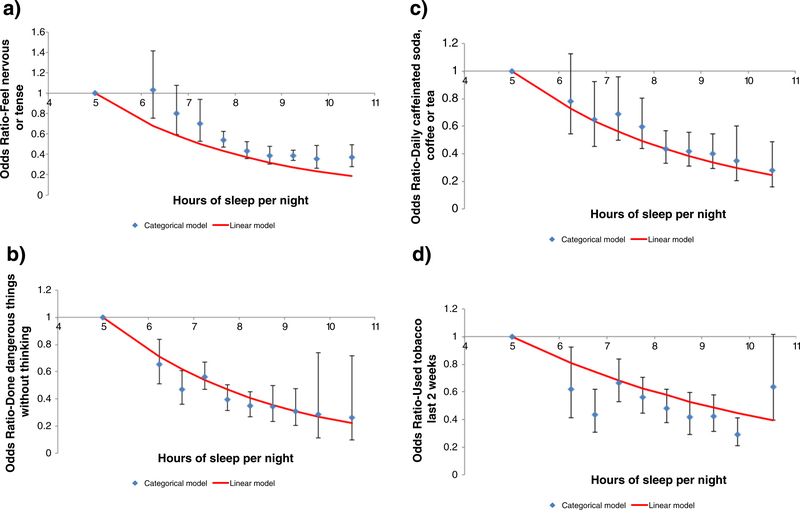
Table 3 displays adjusted associations (odds ratios) between both wake-up time and sleep duration and the mental health– and substance use–related factors. Greater reported sleep duration was significantly associated with a lesser risk of all of the mental health and substance use factors. For instance, for each additional hour of sleep reported, there was a 28% reduction in the adjusted odds of a participant reporting that he or she felt “unhappy, sad, or depressed.” Fig. 1A–D shows the associations between sleep duration and select mental health and behavior issues when sleep duration is modeled both categorically and linearly. Later wake-up times were significantly inversely associated with feeling “unhappy, sad or depressed,” “feeling hopeless about the future,” “feeling nervous or tense,” and “worrying about things.” However, later wake-up time was associated with greater risk for reporting tobacco, alcohol, or drug use in the past week.
Table 3.
Mental health– and substance use–related behaviors in relation to sleep duration and wake-up time on school days
| Wake-up time |
Sleep duration |
|||||||
|---|---|---|---|---|---|---|---|---|
| aORa | 95% CI | P | aORa | 95% CI | P | |||
| Feeling unhappy, sad, or depressedb | 0.87 | 0.78 | 0.96 | .006 | 0.72 | 0.68 | 0.75 | <.0001 |
| Trouble going to sleep or staying asleepb | 0.97 | 0.92 | 1.02 | .214 | 0.77 | 0.71 | 0.84 | <.0001 |
| Feel too tired to do thingsb | 0.94 | 0.83 | 1.06 | .308 | 0.68 | 0.67 | 0.70 | <.0001 |
| Feel hopeless about the futureb | 0.85 | 0.78 | 0.92 | <.0001 | 0.74 | 0.70 | 0.78 | < .0001 |
| Feel nervous or tenseb | 0.79 | 0.68 | 0.93 | .006 | 0.74 | 0.70 | 0.78 | <.0001 |
| Worry too much about thingsb | 0.78 | 0.70 | 0.88 | <.0001 | 0.72 | 0.69 | 0.76 | <.0001 |
| Does dangerous things without thinkingb | 0.97 | 0.74 | 1.26 | .800 | 0.76 | 0.67 | 0.86 | <.0001 |
| Has nightmares or bad dreamsb | 0.84 | 0.72 | 0.98 | .028 | 0.83 | 0.77 | 0.91 | <.0001 |
| Daily caffeinated drinksc | 0.93 | 0.87 | 0.99 | .030 | 0.77 | 0.73 | 0.82 | <.0001 |
| Tobacco used | 1.37 | 1.03 | 1.81 | .029 | 0.84 | 0.78 | 0.92 | <.0001 |
| Alcohol used | 1.51 | 1.28 | 1.78 | <.0001 | 0.92 | 0.87 | 0.98 | .008 |
| Drug used | 1.45 | 1.24 | 1.70 | <.0001 | 0.88 | 0.80 | 0.96 | .006 |
AOR, adjusted odds ratio; CI, confidence interval.
Odds ratios for difference in risk of selected mental health– and substance use–related behaviors for each additional hour of delayed wake-up or sleep duration time, adjusted for grade level, sex, race, medication for learning disability, usual grades in school, and school-level free and reduced lunch eligibility proportion.
Several times or more vs twice or less during the past 2 weeks.
Once a day or more vs less than once a day during the last 2 weeks.
Once or twice a week or more vs never during the last 2 weeks.
Fig. 1.
Associations between sleep duration and select mental health and behavior issues, adjusted for grade level, sex, race, medication for learning disability, usual grades in school, and school-level free, and reduced lunch eligibility proportion modeled both categorically and linearly. Bars represent 95% confidence intervals.
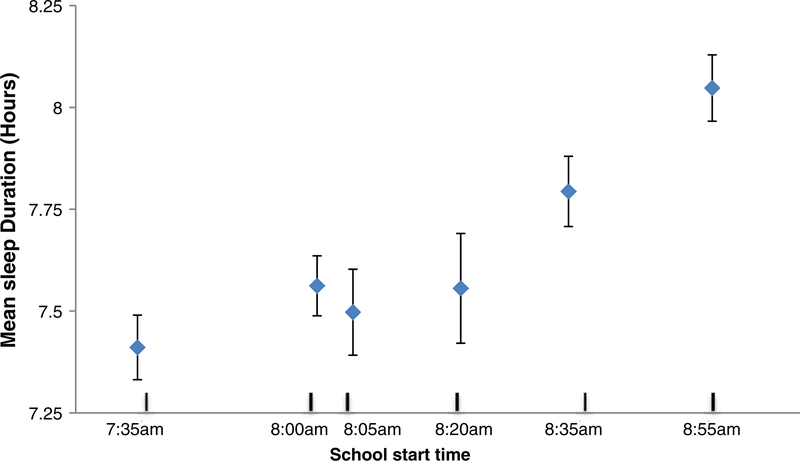
Fig. 2 shows that later school start times were associated with significantly greater sleep duration and later wake-ups. School-day wake-up time had moderate correlation with start time (r = 0.39, P < .001), whereas school-night sleep duration correlates weakly with start time (r = 0.14, P ˂ .001).
Fig. 2.
Associations between school start time and reported sleep duration, adjusted for grade level, sex, race, medication for learning disability, usual grades in school, and school-level free, and reduced lunch eligibility proportion. Bars represent 95% confidence intervals.
Discussion
In this study, we found that adolescents attending schools with later start times report greater sleep duration and later wake-up times. Confirming our hypotheses, we found that greater sleep duration was associated with students reporting fewer mental health– and substance use–related issues. Later wake-up times were associated with some, but not all, mental health concerns.
Our findings are consistent with results obtained in prior research. 37 Later starting times in this study were linked with students obtaining more sleep each school night. We found students who obtain more sleep are less likely to report mental health concerns, as has been substantiated by McKnight-Eily et al,6 Pasch et al,8Dahl and Lewin,12 Harvey et al,13 and Owens et al.31Also, the prevalence of use of alcohol, cigarettes, and other substances declines with students who obtain more sleep, confirming the findings of McKnight-Eily et al, who studied responses from more than 12,000 students across the United States using data from the Youth Risk Behavior Survey. Two of our findings—that greater sleep duration was associated with less tobacco, alcohol, and other drug use, and yet the latest wake up time revealed more tobacco, alcohol, and other drug use— at first appear contradictory. Although it is beyond the capacity of our data to examine this apparent discrepancy, we suspect that the finding that latest wake-up time associated with more substance use is driven by the fact that students who indicate on the survey that they awaken in the very latest of our wake categories may be those students who are struggling in multiple areas that also put them at risk for substance use.
The data shown in Fig.1A–D are consistent with prior research studies that have documented the links between mental health and sleep duration,5,6,11,17 as well as caffeine use as a stimulant for persons who are otherwise sleep deprived.12,38 Prior research on sleep and tobacco use in teens have discovered similar findings.3,4 Sleep deprivation of less than 8 hours per night and sleeping longer than is considered normal at 9.25 hours for adolescents are similar in that both can be viewed as likely being symptomatic of other environmental and emotional issues that preclude or induce sleep.
Research on the effects or outcomes associated with school start time will always be inherently confounded with other school- and district-level factors, which affect all students in that particular school (such as community culture, other school policies, etc). Given this, we were unable to isolate associations that start time might have had on mental health and substance use variables due to inherent structural confounding. This is because mental health and substance use are determined by a universe of factors, many of which are unrelated to sleep, but closely related to other aspects of the school environment. For example, students whose schools have a high degree of pressure for academic achievement, coupled with great emphasis on participation in sports and clubs (some of which may require meeting before the school day starts), are often those same students who find it impossible to obtain adequate sleep due to extreme high-performance demands. Despite this, we could identify proxy characteristics that are consequences of varying effective school start times (school-day wake-up time and school-night sleep duration) and test their associations with substance use and mental health. Although both school-day wake-up time and school-night sleep duration are imperfect stand-ins for start time policy, they are the best possible option for the widest range of high school students as a mechanism through which start time is hypothesized to affect mental and physical health.
Our study’s strengths are in the large, geographically-diverse sample of responses from more than 9000 students and in the use of the Teen Sleep Habits Survey, an up-to-date instrument of 97 items that cover a wide variety of adolescent issues, including sleep, activities and homework, and physical and mental health. Most of the previous research on school start time impacts has been on single sites, restricting generalizability across a range of locations. Our research is limited by the fact that all student measures are self-reported. Furthermore, given that only 1 of the 8 schools was surveyed twice, we were not able to conduct a true longitudinal analysis for the cohort of schools enrolled in the study.
It is impossible to do true, multisite experimental, randomized-control trial research in the United States to assess the outcomes of later school start time, given that school districts in the United States have complete local autonomy as far as determining policies such as their schools’ start times. That said, future research could continue on the path of the research by Wahlstrom et al,30 to take advantage of natural experiments by studying, over time, those schools that are taking the initiative to implement changes. A longitudinal exploration of such natural experiments would allow for stronger causal inference as compared with cross-sectional studies. An additional goal for future search would be to incorporate more objective measurements, such as saliva cotinine to assess tobacco use and sleep actigraphy, to more accurately measure actual sleep. Furthermore, there is much to learn about how other school policies, such as limiting activities that occur before the start of the school day and banning hand-in deadlines for homework that are past a certain hour (eg, 10 PM), and so on, that might further enhance adolescent sleep. These potential policy actions by school districts would serve to complement later start times, or at least would provide sleep gains for students who attend a high school that cannot or will not move their start time later. Finally, although the American Academy of Pediatrics recommends that high schools start no earlier than 8:30 AM,32 it is not yet known what range of start times is truly optimal and/or realistic. This, too, is an area for additional research.
Conclusions
Despite the strong medical evidence of the need for adolescents to obtain at least 8, and preferably 9 or more, hours of sleep every night to maximize their neural development, a strong resistance to a delayed high school start time exists in many localities across the United States.38 School districts are very complex organisms that link bureaucratic structures with community norms and family life patterns, and where homeostasis or maintenance of the status quo is probably the strongest force against adopting a later start time for high schools. However, given the findings reported here that greater sleep duration is linked to improved mental health, as well as less substance use, it would appear important for school districts to place a priority on adolescents’ obtaining sufficient sleep. Having school policies that allow for greater sleep per school night can positively affect most adolescents, by enhancing their well-being, with the potential to serve their long-term health throughout their life-span.
Acknowledgments
The authors would like to thank Jason Johnson for database management.
This work was supported by the Centers for Disease Control and Prevention, Grant No. CDC 5U48DP001939 (SIP10-035), and the Teton County School District. The study sponsors had no role in the study design, data collection, analysis, interpretation of the data, writing, or decision to submit for publication.
References
- 1.Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance—United States, 2015. MMWR Surveill Summ. 2016;65(6):1–174. 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- 2.Perou R, Bitsko RH, Blumberg SJ, et al. Mental health surveillance among children —United States, 2005–2011. MMWR Suppl. 2013;62(2):1–35. [PubMed] [Google Scholar]
- 3.Edwards S, Reeves GM, Fishbein D. Integrative model of the relationship between sleep problems and risk for youth substance use. Curr Addict Rep. 2015;2(2): 130–140. 10.1007/s40429-015-0052-0. [DOI] [Google Scholar]
- 4.Terry-McElrath YM, Maslowsky J, O’Malley PM, Schulenberg JE, Johnston LD Sleep and substance use among US adolescents, 1991–2014. Am J Health Behav. 2016; 40(1):77–91. 10.5993/AJHB.40.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe M. Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use. J Youth Adolesc. 2015;44(2):362–378. 10.1007/s10964-014-0170-3. [DOI] [PubMed] [Google Scholar]
- 6.McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med. 2011;53(4–5):271–273. 10.1016/j.ypmed.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 7.Stea TH, Knutsen T, Torstveit MK Association between short time in bed, health-risk behaviors and poor academic achievement among Norwegian adolescents. Sleep Med. 2014;15(6):666–671. 10.1016/j.sleep.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Pasch KE, Laska MN, Lytle LA, Moe SG Adolescent sleep, risk behaviors, and depressive symptoms: are they linked? Am J Health Behav. 2010;34(2):237–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Paksarian D, Lamers F, Hickie IB, He J, Merikangas KR Sleep patterns and mental health correlates in US adolescents. J Pediatr. 2017;182:137–143. 10.1016/j.jpeds.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Fredriksen K, Rhodes J, Reddy R, Way N. Sleepless in Chicago: tracking the effects of adolescent sleep loss during the middle school years. Child Dev. 2004;75(1):84–95. [DOI] [PubMed] [Google Scholar]
- 11.Perkinson-Gloor N, Lemola S, Grob A. Sleep duration, positive attitude toward life, and academic achievement: the role of daytime tiredness, behavioral persistence, and school start times. J Adolesc. 2013;36(2):311–318. 10.1016/j.adolescence.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Dahl RE, Lewin DS Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6 Suppl):175–184. [DOI] [PubMed] [Google Scholar]
- 13.Harvey AG, Alfano CA, Clarke G. Mood disorders. In: Wolfson AR, Montgomery-Downs HE, editors. The Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. Ontario, Canada: Oxford University Press; 2013. p. 515–531. [Google Scholar]
- 14.Beebe DW Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin N Am. 2011;58(3):649–665. 10.1016/j.pcl.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18(1):75–87. 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Sarchiapone M, Mandelli L, Carli V, et al. Hours of sleep in adolescents and its association with anxiety, emotional concerns, and suicidal ideation. Sleep Med. 2014; 15(2):248–254. 10.1016/j.sleep.2013.11.780. [DOI] [PubMed] [Google Scholar]
- 17.Fitzgerald CT, Messias E, Buysse DJ Teen sleep and suicidality: results from the youth risk behavior surveys of 2007 and 2009. J Clin Sleep Med. 2011;7(4): 351–356. 10.5664/JCSM.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee YJ, Cho S-J, Cho IH, Kim SJ Insufficient sleep and suicidality in adolescents. Sleep. 2012;35(4):455–460. 10.5665/sleep.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor DJ,Gardner CE,Bramoweth AD,et al. Insomniaandmentalhealthincollegestudents.Behav Sleep Med. 2011;9(2):107–116. 10.1080/15402002.2011.557992. [DOI] [PubMed] [Google Scholar]
- 20.Petrov ME, Lichstein KL, Baldwin CM Prevalence of sleep disorders by sex and ethnicity among older adolescents and emerging adults: relations to daytime functioning, working memory and mental health. J Adolesc. 2014;37(5):587–597. 10.1016/j.adolescence.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Meldrum RC, Restivo E. The behavioral and health consequences of sleep deprivation among U.S. high school students: relative deprivation matters. Prev Med. 2014;63:24–28. 10.1016/j.ypmed.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Clinkinbeard SS, Simi P, Evans MK, Anderson AL Sleep and delinquency: does the amount of sleep matter? J Youth Adolesc. 2011;40(7):916–930. 10.1007/s10964-010-9594-6. [DOI] [PubMed] [Google Scholar]
- 23.Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics. 2015; 135(3):460–468. 10.1542/peds.2014-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carskadon MA Optimal sleep habits in adolescents. In: Van Dongen HPA, Kerkhof GA, editors. Encyclopedia of sleep, 190; 2013. p. 86–87. [Google Scholar]
- 25.Carskadon MA Sleep in adolescents: the perfect storm. Pediatr Clin N Am. 2011; 58(3):637–647. 10.1016/j.pcl.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wahistrom K. Changing times: findings from the first longitudinal study of later high school start times. NASSP Bull. 2002;86(633):3–21. 10.1177/019263650208663302. [DOI] [Google Scholar]
- 27.Dexter D, Bijwadia J, Schilling D, Applebaugh G. Sleep, sleepiness and school start times: a preliminary study. WMJ. 2003;102(1):44–46. [PubMed] [Google Scholar]
- 28.2006. Teens and sleep—National Sleep Foundation. https://sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/28.-teens-and-sleep.[Accessed February 8, 2017].
- 29.Crowley SJ, Acebo C, Carskadon MA Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8(6):602–612. 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 30.Wahlstrom K, Dretzke B, Gordon M, Peterson K, Edwards K, Gdula J. Examining the Impact of Later High School Start Times on the Health and Academic Performance of High School Students: A Multi-Site Study. http://conservancy.umn.edu/handle/11299/162769; 2014. [Accessed March 16, 2015].
- 31.Owens JA, Belon K, Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch Pediatr Adolesc Med. 2010;164(7):608–614. 10.1001/archpediatrics.2010.96. [DOI] [PubMed] [Google Scholar]
- 32.Group ASW, Committee on Adolescence AC on SH. School start times for adolescents. Pediatrics. 2014. 10.1542/peds.2014-1697[peds.2014-1697]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schools and Staffing Survey (SASS). http://nces.ed.gov/surveys/sass/tables/sass1112_201381_s1n.asp. [Accessed March 16, 2015].
- 34.Wheaton AG, Ferro GA, Croft JB School start times for middle school and high school students—United States, 2011–12 school year. MMWR Morb Mortal Wkly Rep. 2015;64(30):809–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolfson AR, Carskadon MA Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69(4):875–887. [PubMed] [Google Scholar]
- 36.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–216. [DOI] [PubMed] [Google Scholar]
- 37.Boergers J, Gable CJ, Owens JA Later school start time is associated with improved sleep and daytime functioning in adolescents. J Dev Behav Pediatr. 2014;35(1): 11–17. 10.1097/DBP.0000000000000018. [DOI] [PubMed] [Google Scholar]
- 38.Wahlstrom KL The prickly politics of school starting times. Phi Delta Kappan. 1999;80(5):344–347. [Google Scholar]