Abstract
Background
Aorta-right atrial tunnel (ARAT) is a rare congenital anomaly whose aetiology and incidence are unknown. It might represent a diagnostic and therapeutic challenge requiring a combination of imaging modalities and an integrated teamwork.
Case summary
We report a case of a 23-year-old man with an asymptomatic ARAT complicated by infective endocarditis, diagnosed with non-invasive multimodality imaging, and successfully treated with a catheter-based approach.
Discussion
Aorta-right atrial tunnel closure in asymptomatic patients is still a matter of debate. Considering the risk of serious complications surgical treatment might be recommended soon after diagnosis. In selected cases, catheter-based closure might represent a safe, effective, and less invasive alternative to traditional surgical approach.
Keywords: Aorto-right atrial tunnel, Transcatheter closure, Transoesophageal echocardiography, Multidetector computed tomography angiography, Endocarditis, Coronary vessel anomalie
Learning points
Aorta-right atrial tunnel (ARAT) is a rare congenital anomaly that may have serious complications.
The ARAT cases described in the literature were managed predominantly with surgical treatment.
In our case, the combination of different imaging modalities (transoesophageal echocardiography, Three-dimensional multidetector computed tomography angiography, aortography, and coronary angiography) provided useful anatomical and functional information of the rare anomaly and played a key role in planning a successful interventional procedure.
Introduction
Aorta-right atrial tunnel (ARAT), firstly described in 1980 by Coto et al.,1 is a rare congenital anomaly consisting of an extracardiac tunnel-like vascular communication arising from any one of the aortic sinuses and emptying into the right atrium (RA).2–8
The aetiology and exact incidence of the condition are unknown. This anomaly can be associated with coronary artery anomalies. Clinical presentation ranges from asymptomatic precordial murmur to congenital heart failure.9 We report a case of an asymptomatic ARAT complicated by infective endocarditis (IE), diagnosed with non-invasive multimodality imaging, and successfully treated with a catheter-based approach.
Timeline
| Day 1 | Patient admitted for a month-long fever, weight loss, mild cough, and dyspnoea; auscultatory findings confirmed the presence of a continuous murmur. |
| Day 2 | Patient found to be septic, blood cultures positive for a multi-sensitive Streptococcus mitis strain, antibiotic therapy with ceftriaxone started. |
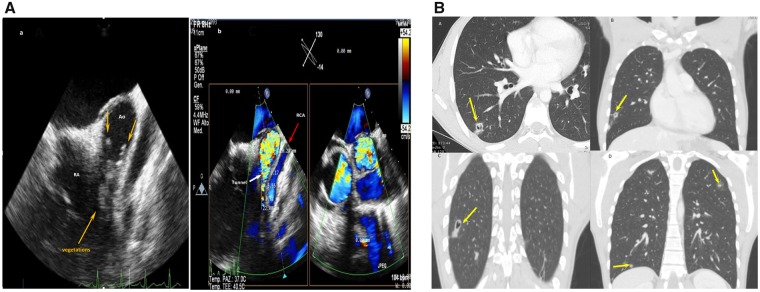
| Day 3 | A chest computed tomography scan highlighted multiple pseudo-nodular cavitations, bilateral pneumonia, hilar adenopathy, and pronounced right atrial profile. |
| Day 4 | Transoesophageal echocardiography colour Doppler showed right atrial dilation and bacterial vegetations inside a tunnel-like structure originating from the right coronary sinus and connected to the right atrium. |
| Day 30 | Patient was treated for a total of 28 days with ceftriaxone with normalization of inflammatory markers and a consensual lung lesions improvement. |
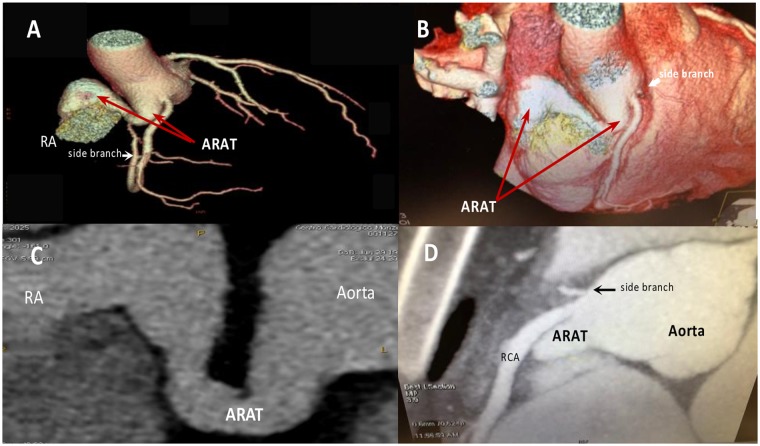
| Two months after discharge | Patient transferred to University hospital. Three-dimensional multidetector computed tomography angiography confirmed the presence of an aorta-right atrial tunnel (ARAT) and better defined its anatomy. After heart team discussion, catheter-based closure was decided. |
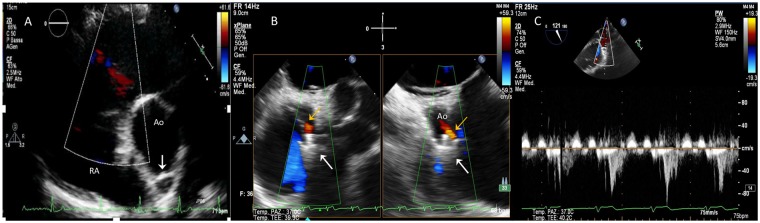
| Three months after procedure | Transoesophageal echocardiography colour Doppler showed correct device position with mild left-to-right shunt. |
| Six months after the procedure | Three-dimensional multidetector computed tomography angiography with volume rendering three-dimensional reconstruction showed correct position of the occlusion device and curved multiplanar reconstructions demonstrated the almost complete occlusion of the ARAT. |
Case presentation
A 23-year-old man was admitted for a month-long fever, weight loss, mild cough, and dyspnoea. Past medical history was unremarkable except for a continuous murmur heard since childhood.
Electrocardiogram and chest X-ray were normal. Blood tests showed increased inflammatory markers and mild normocytic anaemia. Blood cultures were positive for a multi-sensitive Streptococcus mitis strain. Different serology tests, oropharyngeal swab culture, bronchoalveolar lavage culture for mycobacterium tuberculosis, and autoimmune screening test were negative.
Antibiotic therapy with ceftriaxone was started and two-dimensional transthoracic echocardiography (TTE) did not show signs of IE. Chest computed tomography showed multiple pseudo-nodular bilateral pneumonia, hilar adenopathy, and pronounced right atrial profile that aroused the suspicion of IE, prompting transoesophageal echocardiography (TOE). The exam showed right atrial dilation and bacterial vegetations inside a tunnel-like structure (maximal diameter of 20 mm × 22 mm), originating from the right coronary sinus, running parallel to the right coronary artery and connected to the RA. Two-dimensional colour multiplanar reconstruction (MPR) images showed high-velocity flow within the tunnel (Figure 1). Pulmonary artery pressure was within normal limits, pulmonary/systemic blood flow ratio was 1.1:1 and left ventricle ejection fraction was 54% at TTE. Aortic root angiography showed a large and tortuous tunnel originating from the right coronary sinus and emptying into the RA. Coronary angiography demonstrated normal epicardial arteries. Three-dimensional multidetector computed tomography angiography (3D-MDCTA) confirmed the presence of an ARAT and better defined its anatomy (Figure 2). The patient was treated for 28 days with ceftriaxone achieving normalization of inflammatory markers and marked improvement of the lung lesions.
Figure 1.
(A) (a) Transoesophageal echocardiography showed right atrial dilation and bacterial vegetations (orange arrows) inside the tunnel-like structure; (b) two-dimensional colour multiplanar reconstruction images showing high-velocity flow within the tunnel (white arrowhead) originating from the right coronary sinus and running parallel to the right coronary artery (red arrow). (B) Chest computed tomography scans (A, axial plane; B–D, coronal planes) showing multiple pseudo-nodular cavitations (yellow arrows) and bilateral pneumonia, hilar adenopathy, and pronounced right atrial profile. Ao, aorta; CT, computed tomography; MPR, multiplanar reconstruction; RA, right atrium; RCA: right coronary artery.
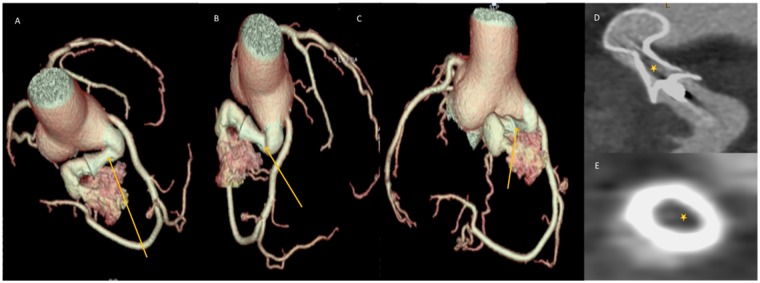
Figure 2.
Three-dimensional multidetector computed tomography angiography pre-operative assessment. (A and B) Volume-rendering three-dimensional reconstruction showing the aorta-right atrial tunnel (red arrows) arising from the right aortic sinus and emptying into the right atrium. Note the coronary side branch (white arrows) originating from the proximal right coronary artery. (C) Curved multiplanar reconstruction showing the entire path of the aorta-right atrial tunnel. (D) Maximum intensity projection reconstruction confirming the origin of the side branch (black arrow) from the proximal right coronary artery. 3D-MDCTA, three-dimensional multidetector computed tomography angiography; ARAT, aorta-right atrial tunnel; RCA, right coronary artery.
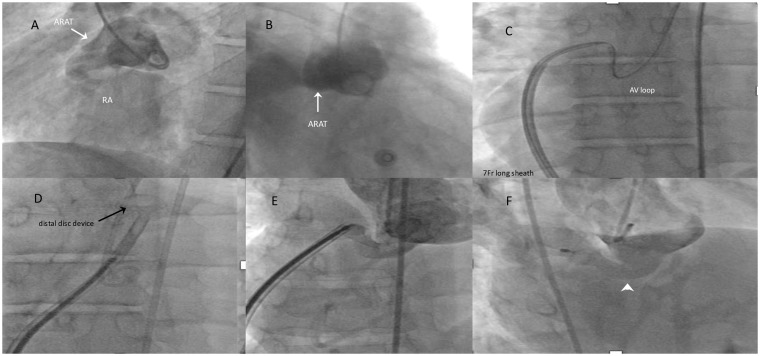
After heart team discussion, catheter-based closure was recommended and the procedure was performed under general anaesthesia with angiographic and TOE guidance. Using a right femoral vein and artery approach, an artero-venous loop was established across the ARAT and the fistulous communication was closed using a patent ductus arteriosus closure device (PDA Long Shank 10/8 mm, 10.5 mm in length, Occlutech International AB, Sweden) (Figure 3). Aortic angiography and TOE confirmed device stability at the entrance of the tunnel with moderate residual shunt. The patient was discharged 2 days after the procedure. At 3-month follow-up, TTE showed further device expansion and mild left-to-right residual shunt (Figure 4). At 6 months, 3D-MDCTA was performed. Volume rendering three-dimensional reconstruction showed correct position of the occluder device and curved MPR demonstrated almost total occlusion of the tunnel confirmed in cross-section reconstructions (Figure 5).
Figure 3.
Procedural steps of the catheter-based aorta-right atrial tunnel closure. (A and B) Aortic angiography showing the aorta-right atrial tunnel (white arrow) originating from the right coronary sinus and draining into the right atrium. (C) Advancement from the inferior vena cava of a 7-Fr long sheath over the artero-venous loop towards the ascending aorta. (D) Opening of the distal disc of the closure device (black arrow). (E) Control angiography before full device deployment. (F) Occlusion device correctly positioned inside the aorta-right atrial tunnel (white arrowhead). ARAT, aorta-right atrial tunnel; RA: right atrium.
Figure 4.
Transoesophageal echocardiography colour Doppler 3 months after the procedure. (A) Correct device position (white arrow). Note that the distal disc of the device is not protruding into the aorta. (B) Xplane transoesophageal echocardiography showing mild residual left-to-right shunt (orange arrows). White arrows indicate occlusion device position inside the tunnel. (C) Continuous-wave Doppler ultrasound showing early diastole flow with peak velocity of 80 cm/s inside the tunnel. Ao, aorta; CW, continuous-wave; RA, right atrium; TOE, transoesophageal echocardiography.
Figure 5.
Three-dimensional multidetector computed tomography angiography at 6-month follow-up. (A–C) Volume rendering three-dimensional reconstructions showing correct position of the occlusion device (orange arrows) inside the aorta-right atrial tunnel. (D and E) Curved multiplanar reconstructions showing an almost complete occlusion of the aorta-right atrial tunnel. Note the hypodense region (stars) inside the occluder device visible in the longitudinal (D) and cross-section views (E) indicating neo-intimal growth. 3D-MDCTA, three-dimensional multidetector computed tomography angiography; ARAT, aorta-right atrial tunnel.
Discussion
A continuous murmur has been reported in most cases of ARAT described in the literature.3 In our patient, this finding was not taken into consideration until he had multiple embolic focal pneumonia and bacterial vegetations prompting cardiology evaluation. While TTE was negative, TOE allowed to diagnose the rare anomaly. The diagnosis was confirmed by 3D-MDCTA that helped to differentiating ARAT from a ruptured sinus of Valsalva aneurysm and coronary fistula.2
The need for surgical closure in asymptomatic patients might be debated. However, as the continued patency of the tunnel may predispose patients to increasing risks of serious complications including ventricular overload, bacterial endocarditis, cardiac failure, aneurysm formation and rupture, ARAT obliteration might be recommended soon after diagnosis.3
Surgical options include external ligation of the tunnel under controlled hypotension or patch closure of aortic origin with direct closure of the atrial opening under cardiopulmonary bypass. In case a coronary artery takes off from the tunnel, it should be surgically reimplanted in the sinus of Valsalva.4
Catheter-based closure might be a less invasive alternative treatment option provided the opening of the right atrial end is small, the appropriate device according to the size is available, and there is a constriction in the course of the fistula.3 Sreedharan et al.10 were the first to report a case in which the tunnel was embolized using coils with transcatheter technique. The largest case study of nine patients was reported by Gajjar et al.6 Eight of them underwent surgical correction, while one patient was treated with coil embolization. Chandra et al.11 reported the case of a 12-year-old girl with effort dyspnoea and palpitations with a large fistula between the right aortic sinus and the RA successfully closed with an Amplatzer duct occluder. The case of a 3-year-old child whose ARAT was closed with a vascular plug four device has been described by Baykan et al.12
In our case, the multimodality imaging excluded that the small coronary branch originated from the tunnel and provided all measurements for choosing the right device size. This allowed to achieve a safe and effective ARAT closure.
Conclusions
Our case represented a diagnostic and therapeutic challenge requiring multimodality imaging and a multidisciplinary team approach. This is the first ARAT case successfully closed with a PDA long shank occluder that was used with an off-label indication.
Lead author biography

Dr Eustaquio Maria Onorato is an active adult and paediatric interventional cardiologist. Currently, he is a senior consultant, congenital and structural heart diseases interventions at Centro Cardiologico Monzino, University School of Medicine, Milan, Italy. SCAI and ESC fellow. Honorary Membership of the Venezuelan Society of Invasive Cardiology and Russian Scientific Society of Interventional Endovascular Surgery. He has authored several original manuscripts and chapters of books in interventional cardiology and has published in Stroke, J Am Coll Cardiol, Catheter Cardiovasc Interv, Eur Heart J, and EuroIntervention. Peer Reviewer of Int J Cardiol, Am J Cardiol, J Cardiovasc Med, and Catheter Cardiovasc Interv.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Cesare Bolla, MD and Guido Chichino, Struttura Organizzativa Complessa di Malattie Infettive and Stefano Barbero, MD, SC Radiologia, Azienda Sanitaria SS. Antonio e Biagio e Cesare Arrigo, Alessandria for their assistance and valuable guidance in preparing this article.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: E.M.O. is a consultant for Occlutech. The remaining authors have no conflict of interest to declare.
References
- 1. Coto EO, Caffarena JM, Such M, Marques JL.. Aorto-right atrial communication. J Thorac Cardiovasc Surg 1980;80:941–944. [PubMed] [Google Scholar]
- 2. Rosenberg H, Williams WG, Trusler GA, Smallhorn J, Rowe RD, Moes CA, Freedom RM.. Congenital aortic-right atrial communications: the dilemma of differentiation from coronary-cameral fistula. J Thorac Cardiovasc Surg 1986;91:841–847. [PubMed] [Google Scholar]
- 3. Kalangos A, Beghetti M, Vala D, Chraibi S, Faidutti B.. Aorticoright atrial tunnel. Ann Thorac Surg 2000;69:635–637. [DOI] [PubMed] [Google Scholar]
- 4. Turkay C, Golbagi I, Bayezid O.. Aorta-right atrial tunnel. J Thorac Cardiovasc Surg 2003;125:1058–1060. [DOI] [PubMed] [Google Scholar]
- 5. Elwatidy AF, Galal AN, Rhydderch D, Ashmeg AK.. Aorto-right atrial fistula. Ann Thorac Surg 2003;76:929–931. [DOI] [PubMed] [Google Scholar]
- 6. Gajjar T, Voleti C, Matta R, Iyer R, Dash PK, Desai N.. Aorta-right atrial tunnel: clinical presentation, diagnostic criteria, and surgical options. J Thorac Cardiovasc Surg 2005;130:1287–1292. [DOI] [PubMed] [Google Scholar]
- 7. Sai Krishna C, Baruah DK, Reddy GV, Panigrahi NK, Suman K, Kumar PV.. Aorta-right atrial tunnel. Tex Heart Inst J 2010;37:480–482. [PMC free article] [PubMed] [Google Scholar]
- 8. Omeroglu SN, Goksedef D, Balkanay OO, Ipek G.. Aorta-right atrial tunnel in an adult. Eur J Cardiothorac Surg 2014;45:580–581. [DOI] [PubMed] [Google Scholar]
- 9. Jain J, Wani A, Kulkarni A, Yelne P.. Aorta-right atrial tunnel presenting with heart failure in an adult. Heart Views 2018;19:152–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sreedharan M, Baruah B, Dash PK.. Aorta-right atrial tunnel—a novel therapeutic option. Int J Cardiol 2006;107:410–412. [DOI] [PubMed] [Google Scholar]
- 11. Chandra S, Vijay S, Kaur D, Dwivedi S.. Congenital aorta right atrial fistula: successful transcatheter closure with the Amplatzer occluder. Pediatr Cardiol 2011;32:1057–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Baykan A, Narin N, Ozyurt A, Uzum K.. Aorta–right atrial tunnel closure using the transcatheter technique: a case of a 3-year-old child. Cardiol Young 2013;23:457–459. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.