Abstract
Background:
Alternate-day fasting (ADF) involves a ‘famine day’ (25% energy intake) and a ‘feast day’ (ad libitum intake). This secondary analysis examined changes in beverage intake in relation to energy intake and body weight during 12 months of ADF versus daily calorie restriction (CR).
Methods:
Obese subjects (n = 100 enrolled, n = 69 completers) were randomized to one of three groups for 12 months: (a) ADF; (b) CR; or (c) control.
Results:
At baseline, intakes of diet soda, caffeinated beverages, sugar-sweetened soda, alcohol, juice, and milk were similar between groups. There were no statistically significant changes in the intake of these beverages by month 6 or 12 between ADF (feast or famine day), CR, or control groups. Beverage intake was not related to energy intake or body weight at month 6 or 12 in any group.
Conclusion:
These pilot findings suggest that intermittent fasting does not impact beverage intake in a way that affects energy intake or body weight.
Keywords: Beverage intake, soda, caffeine, alcohol, body weight, alternate-day fasting, calorie restriction, obese adults
Introduction
Alternate-day fasting (ADF) is a form of intermittent fasting that has gained popularity over the past decade as weight-loss strategy (Tinsley and La Bounty, 2015). ADF involves a ‘famine day’ where one consumes approximately 25% of energy needs (~500 kcal) alternated with a ‘feast day’ where one consumes food ad libitum. While several clinical trials (Catenacci et al., 2016; Trepanowski et al., 2017; Varady et al., 2009; Klempel et al., 2013) have examined the weight-reducing efficacy of this diet, none have examined how fasting impacts the consumption of certain beverages. For instance, it has been speculated that subjects may increase consumption of caffeinated beverages (coffee, tea, energy drinks) and diet soda to manage appetite, reduce energy intake, and increase alertness (Brice and Smith, 2002; Gavrieli et al., 2013; Schubert et al., 2017). However, to date, no study has examined whether these assumptions are true. Accordingly, this study was undertaken to examine changes in beverage intake during 12 months of ADF, relative to a daily calorie restriction (CR) group and a no-intervention control group. We hypothesized that ADF subjects would increase intake of diet sodas and caffeinated beverages, relative to CR and controls, and that these increases would be related to reductions in energy intake and body weight.
Methods
Subjects and diets
This is a secondary analysis of a previous published trial (Trepanowski et al., 2017). Participants were recruited from the Chicago area by advertisements, and key inclusion criteria were as follows: age 18–65 y, BMI 25–40 kg/m2, weight stable, previously sedentary or lightly active, nondiabetic, no history of cardiovascular disease, and nonsmoker. Subjects were randomized to an ADF, CR, or control group for 12 months. The original goal of this study was to compare the ability of ADF versus CR to facilitate weight loss over 6 months. We were also interested in seeing if participants could maintain their weight loss with the ADF diet. Thus, the 12-month trial was divided into a 6-month weight-loss phase followed by a 6-month weight-maintenance phase. Baseline total energy expenditure was measured using doubly labeled water (Ravussin et al., 2015). Baseline measures were taken before the start of the diets and counseling sessions. From months 0 to 6 (weight-loss phase), ADF subjects were asked to consume 25% of energy needs on the famine day and 125% of energy needs on the feast day, whereas CR subjects were asked to consume 75% of energy needs every day. From months 7 to 12 (weight-maintenance phase), ADF subjects were instructed to consume 50% of energy needs on the famine day and 150% of energy needs on the feast day, whereas CR subjects were instructed to consume 100% of energy needs every day. Control participants were asked to maintain their weight throughout the trial. All groups were instructed not to change their physical activity habits. Body weight was measured in a hospital gown with a digital scale. Experimental protocols were approved by the Office for the Protection of Research Subjects at the University of Illinois, Chicago. All subjects gave written informed consent to participate in the study.
Dietary counseling
Subjects were provided with all meals from months 0 to 3, received one-on-one weekly dietary counseling from months 3 to 6, and one-on-one monthly behavioral counseling from months 7 to 12. The goal of the dietary counseling was primarily to teach subjects how to read food labels, monitor portion sizes, reduce the consumption of processed foods, and increase intake of fruits and vegetables. There were 12 dietary counseling sessions in total, and one session focused specifically on decreasing intake of sugar-sweetened beverages, and another session focused on monitoring alcohol intake. Diet soda and caffeinated beverage intake was permitted ad libitum. Control subjects received no dietary counseling.
Dietary intake
Each subject completed a 7-day food record at baseline, month 6, and 12. Participants were provided with instruction on how to record food items and beverages in sufficient detail to obtain accurate estimates of intake. The investigators judged the diet record data to be, on average, ‘moderately’ to ‘very’ detailed with regards to foods and beverages. However, consumption of water was rarely recorded as we neglected to instruct subjects to record water intake in detail. Thus, water intake is not reported in this manuscript. Dietary information from the food records was analyzed by Nutritionist Pro (Axxya Systems). Consumption of diet soda, caffeinated beverages excluding sodas (caffeinated coffee, caffeinated tea, energy drinks), sugar-sweetened sodas, alcohol (beer, wine, liquor), fruit juices (including fruit drinks), and milk (including milk with cereal) are presented as mean intakes by volume (ml/d).
Statistics
All data are presented as mean ± standard error of the mean (SEM). Statistical analyses were performed using SPSS 25.0 for Mac (SPSS Inc., Chicago, IL). A two-tailed p < 0.05 was considered statistically significant. Tests for normality were included in the model, and all data were found to be normally distributed. Repeated-measures analysis of variance was used to compare changes in dependent variables between the groups over time. Pearson correlations were performed to assess relationships between beverage intake, energy intake, and body weight.
Results
Subjects, energy intake, and weight loss
One hundred subjects began the study, and 69 completed the 12-month trial (ADF n = 21, CR n = 25, control n = 23). Subjects were primarily female (86%), middle aged (44 ± 1 y), and obese (BMI 35 ± 1 kg/m2). Energy intake in the ADF group was as follows: baseline: 1699 ± 159 kcal/d; month 6: 1430 ± 79 kcal/d (feast day), 985 ± 97 kcal/d (famine day); month 12: 1651 ± 149 kcal/d (feast day), 1107 ± 86 kcal/d (famine day). Energy intake in the CR group was as follows: baseline: 1971 ± 133 kcal/d; month 6: 1612 ± 123 kcal/d; month 12: 1690 ± 132 kcal/d. Body weight was reduced (p < 0.001) similarly in the intervention groups by month 6 (ADF: −6.8 ± 1.0%; CR: −6.8 ± 1.1%) and month 12 (ADF: −6.0 ± 0.7%; CR: −5.3 ± 0.6%), relative to controls. Fat mass also decreased (p < 0.01) similarly in the intervention groups by month 6 (ADF: −4.2 ± 0.6 kg; CR: −5.1 ± 0.7 kg), but did not change relative to controls by month 12 (ADF: −2.0 ± 0.6 kg; CR: −2.0 ± 0.7 kg). Lean mass remained unchanged in the ADF and CR groups, relative to controls, by month 12.
Diet soda and caffeinated beverage intake
At baseline, diet soda and caffeinated beverage intake was similar between the ADF, CR, and control groups (Figure 1). There were no statistically significant changes in diet soda intake by month 6 (p = 0.55) or 12 (p = 0.53) between ADF, CR, or control groups. Moreover, there were no statistically significant changes in caffeinated beverage intake by month 6 (p = 0.23) or 12 (p = 0.31) between ADF, CR or control groups. Intake of diet soda and caffeinated beverages was not related to energy intake or body weight at month 6 or 12 in any group.
Figure 1.
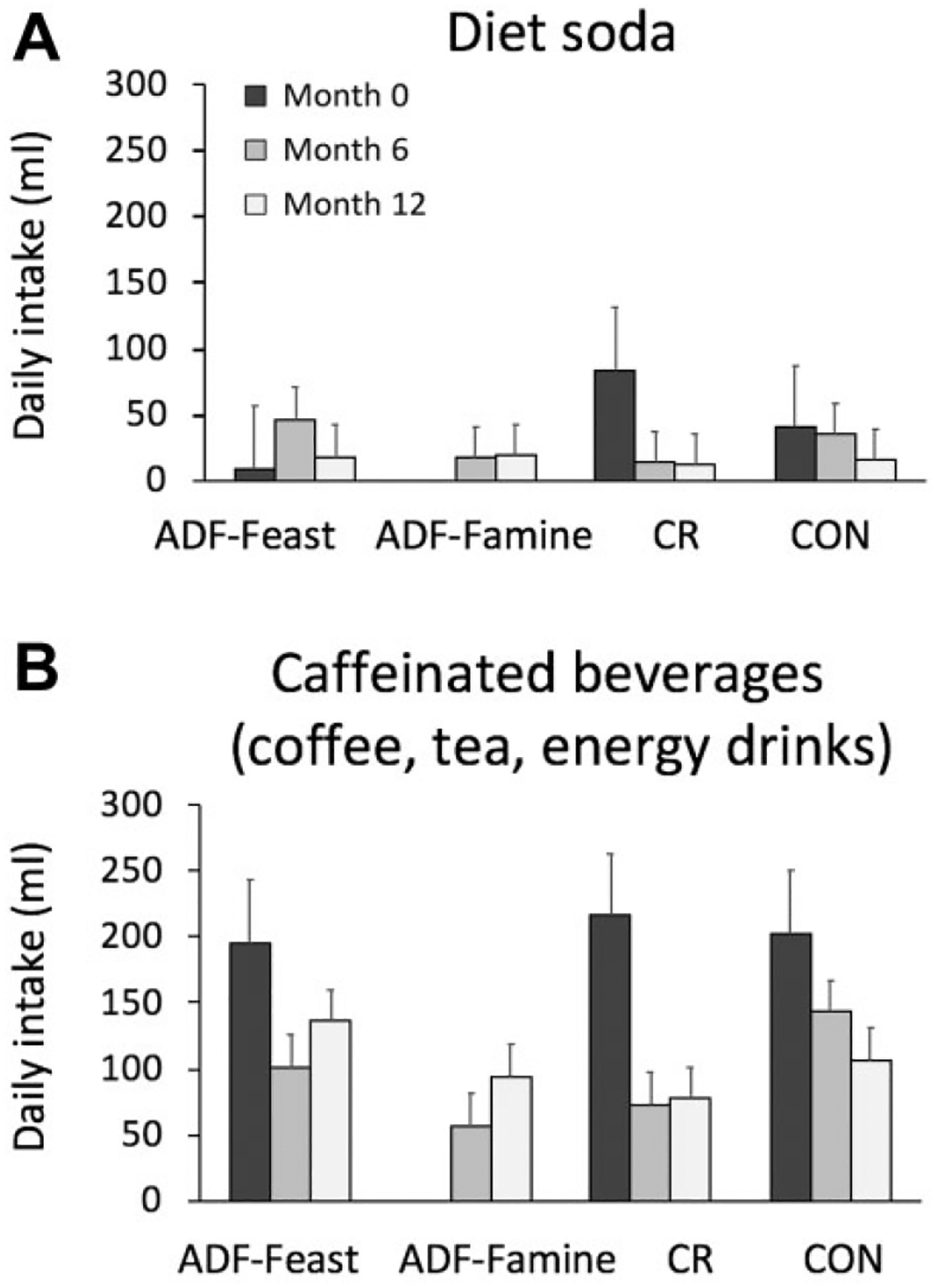
Diet soda and caffeinated beverage intake during 12 months of alternate-day fasting (ADF) or daily calorie restriction (CR).
(A) There were no statistically significant changes in diet soda intake by month 6 or 12 between ADF (feast or famine day), CR, or control groups; (B) there were no statistically significant changes in caffeinated beverage intake by month 6 or 12 between ADF (feast or famine day), CR, or control groups.
Sugar-sweetened soda, alcohol, juice, and milk intake
At baseline, sugar-sweetened soda, alcohol, juice, and milk intake was similar between the ADF, CR, and controls (Figure 2). There were no statistically significant changes in sugar-sweetened soda intake by month 6 (p = 0.22) or 12 (p = 0.33) between ADF, CR, or control groups. Moreover, there were no significant changes in alcohol intake by month 6 (p = 0.78) or 12 (p = 0.29) between ADF, CR, or controls. Juice intake by month 6 (p = 0.63) or 12 (p = 0.47) also did not differ between groups. In addition, there were no significant changes in milk intake by month 6 (p = 0.37) or 12 (p = 0.29) between groups. Intakes of sugar-sweetened soda, alcohol, juice, and milk were not related to energy intake or body weight at month 6 or 12 in any group.
Figure 2.
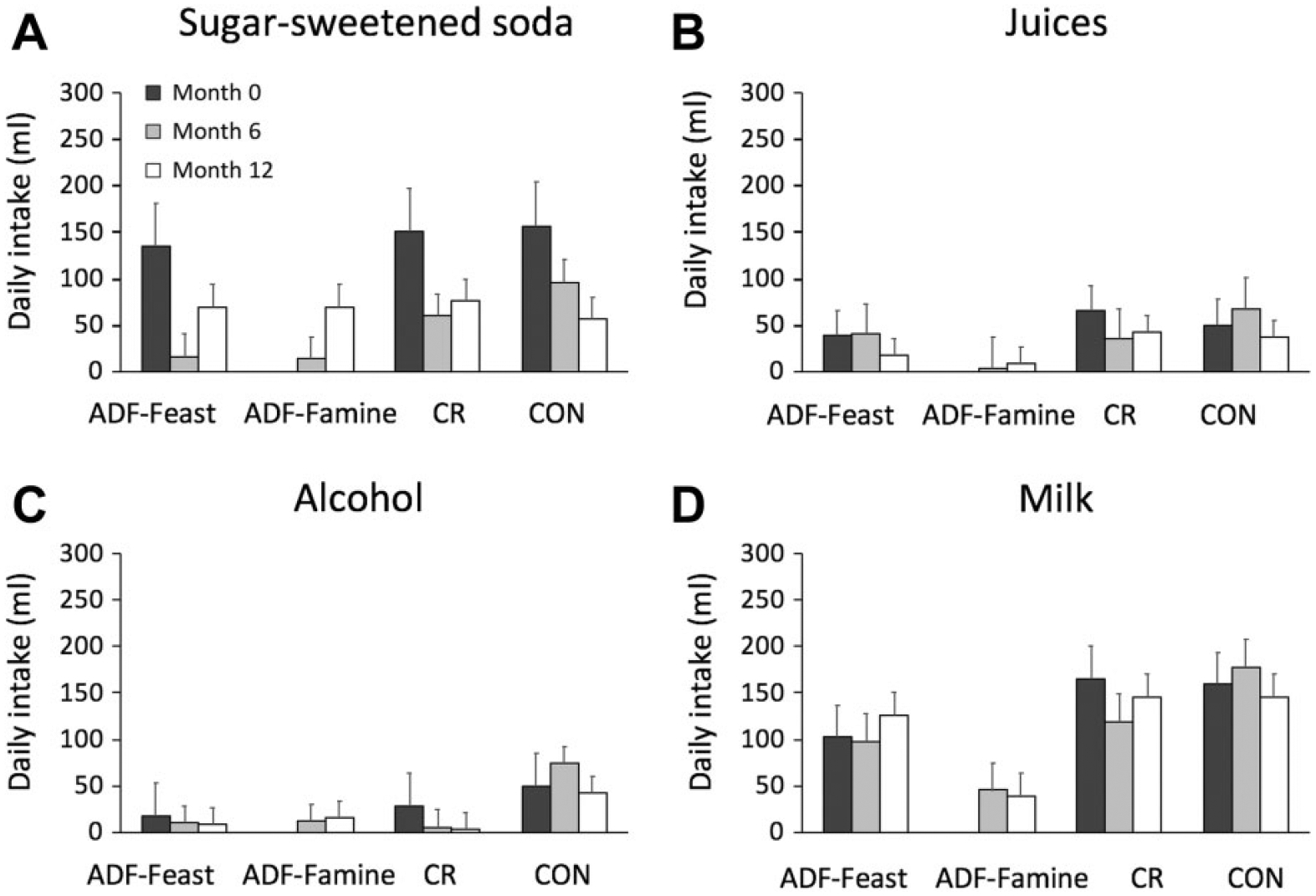
Sugar-sweetened soda, alcohol, juice, and milk intake during 12 months of alternate-day fasting (ADF) or daily calorie restriction (CR).
(A) There were no statistically significant changes in sugar-sweetened soda intake by month 6 or 12 between ADF (feast or famine day), CR, or control groups; (B) there were no statistically significant changes in alcohol intake by month 6 or 12 between ADF (feast or famine day), CR, or control groups; (C) there were no statistically significant changes in juice intake by month 6 or 12 between ADF (feast or famine day), CR, or control groups; (D) there were no statistically significant changes in milk intake by month 6 or 12 between ADF (feast or famine day), CR, or control groups.
Discussion
This study is the first to examine changes in beverage intake during intermittent fasting. We show here that consumption of diet soda, caffeinated beverages, sugar-sweetened soda, alcohol, juice, and milk did not change during 12 months of ADF. Moreover, we did not observe any associations between beverage intake, energy intake or body weight in any of the groups.
Accumulating evidence suggests that ADF is an effective diet strategy for moderate weight loss (3–7% over 3–12 months) (Catenacci et al., 2016; Trepanowski et al., 2017; Varady et al., 2009; Klempel et al., 2013). What remains unknown, however, is whether subjects change their beverage intake behaviors during fasting. More specifically, it has been speculated that fasting participants increase the intake of diet soda and caffeinated beverages to manage appetite, reduce energy intake and increase alertness (Brice and Smith, 2002; Gavrieli et al., 2013; Schubert et al., 2017). Contrary to this hypothesis, the present study shows that these compensatory behaviors (i.e. increasing diet soda and caffeinate beverage intake on famine days) do not occur during 12 months of intermittent fasting. We also show no association between diet soda/caffeinated beverage intake, energy intake, and body weight. Thus, the degree of weight loss observed with intermittent fasting does not appear to be related to changes in beverage intake.
Regular consumption of sugar-sweetened soda, juice, and alcohol is associated with weight gain (Malik et al., 2006; Hu, 2013). Thus, we provided our subjects with dietary advice to reduce the consumption of these beverages in order to help with weight management. Despite receiving nutrition education, consumption of sugar-sweetened beverage and alcohol remained unchanged over the course of the trial in both the ADF and CR groups. Other clinical trials that have examined this relationship generally show reductions in sugar-sweetened beverage and alcohol consumption with counseling (Kim et al., 2017; Metzgar and Nickols-Richardson, 2016; Ostovan et al., 2013). However, it should be noted that intake of sugar-sweetened beverages and alcohol were not excessive in this population at baseline. As such, reducing the consumption of these beverages even further would most likely have little impact on energy intake and body weight. It will be of interest for future trials to examine the impact of intermittent fasting on beverage intake in populations that consume higher amounts of sugar-sweetened beverages and alcohol upon starting the diet.
This study is limited in that it did not measure water intake. We neglected to instruct subjects to record water consumption in detail in the food records throughout the study. For this reason, we did not include water, as it was rarely recorded, and the data are most likely very inaccurate. In addition, we were not able to tease apart the effects of the diets (ADF or CR) versus the dietary counseling, as these interventions were applied simultaneously. Future studies should examine if ADF alone (without any diet counseling) has any impact on beverage intake.
In summary, these pilot findings suggest intermittent fasting does not impact beverage consumption in a way that affects energy intake or body weight.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: National Institutes of Health (NHLBI) R01HL106228.
Footnotes
Consent for publication
All authors have approved the version of the manuscript submitted.
Ethical approval
Experimental protocols were approved by the Office for the Protection of Research Subjects at the University of Illinois, Chicago. All subjects gave written informed consent to participate in the study.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Krista Varady is the author of the book ‘The Every Other Day Diet’ published by the Hachette Book Group. The other authors have no competing interests to disclose.
Trial registration
ClinicalTrials.gov identifier: NCT00960505.
References
- Brice CF and Smith AP. (2002) Effects of caffeine on mood and performance: a study of realistic consumption. Psychopharmacology (Berl) 164: 188–192. [DOI] [PubMed] [Google Scholar]
- Catenacci VA, Pan Z, Ostendorf D, et al. (2016) A randomized pilot study comparing zero-calorie alternate-day fasting to daily caloric restriction in adults with obesity. Obesity (Silver Spring) 24: 1874–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavrieli A, Karfopoulou E, Kardatou E, et al. (2013) Effect of different amounts of coffee on dietary intake and appetite of normal-weight and overweight/obese individuals. Obesity (Silver Spring) 21: 1127–1132. [DOI] [PubMed] [Google Scholar]
- Hu FB. (2013) Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obesity Reviews: an official journal of the International Society of Obesity 14: 606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim BR, Seo SY, Oh NG, et al. (2017) Effect of nutrition counseling program on weight control in obese university students. Clinical Nutrition Research 6: 7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klempel MC, Kroeger CM and Varady KA. (2013) Alternate day fasting (ADF) with a high-fat diet produces similar weight loss and cardio-protection as ADF with a low-fat diet. Metabolism 62: 137–143. [DOI] [PubMed] [Google Scholar]
- Malik VS, Schulze MB and Hu FB. (2006) Intake of sugar-sweetened beverages and weight gain: a systematic review. American Journal of Clinical Nutrition 84: 274–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzgar CJ and Nickols-Richardson SM. (2016) Effects of nutrition education on weight gain prevention: a randomized controlled trial. Nutrition Journal 15: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostovan MA, Zibaeenezhad MJ, Keshmiri H, et al. (2013) The impact of education on weight loss in overweight and obese adults. International Cardiovascular Research Journal 7: 79–82. [PMC free article] [PubMed] [Google Scholar]
- Ravussin E, Redman LM, Rochon J, et al. (2015) A 2-year randomized controlled trial of human caloric restriction: feasibility and effects on predictors of health span and longevity. Journals of Gerontology Series A Biological Sciences and Medical Sciences 70: 1097–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert MM, Irwin C, Seay RF, et al. (2017) Caffeine, coffee, and appetite control: a review. International Journal of Food Science and Nutrition 68: 901–912. [DOI] [PubMed] [Google Scholar]
- Tinsley GM and La Bounty PM. (2015) Effects of intermittent fasting on body composition and clinical health markers in humans. Nutrition Reviews 73: 661–674. [DOI] [PubMed] [Google Scholar]
- Trepanowski JF, Kroeger CM, Barnosky A, et al. (2017) Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Internal Medicine 177: 930–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varady KA, Bhutani S, Church EC, et al. (2009) Shortterm modified alternate-day fasting: a novel dietary strategy for weight loss and cardioprotection in obese adults. American Journal of Clinical Nutrition 90: 1138–1143. [DOI] [PubMed] [Google Scholar]


