To the Editor:
Since December 2019, the outbreak of the novel coronavirus SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) that originated in Wuhan, Hubei province has spread rapidly across China. Many hospitals in Wuhan are the epicenter of the outbreak. The first 14 staff members who were infected with SARS-Cov-2 were from our department. All of them recovered. In such an urgent and unexpected situation, our department began immediate and effective prevention and control strategies to stop the spread of the epidemic in the department. We believe that clinical departments, especially those related to non-infectious diseases in geographic areas of high risk for virus transmission, should take appropriate management and control measures to improve safety during this epidemic. For this purpose, we summarize and share our experiences which should help medical staff prepare in advance for a similar situation. These include the characteristics of SARS-Cov-2 infection, principles of prevention and control of infection, management of infected patients, and epidemic prevention in the outpatient department, ward, operating room, and medical staff.
At the end of December 2019, several cases of pneumonia in Wuhan, China caused by an unknown virus were reported to the World Health Organization (WHO). The novel virus was initially identified as a coronavirus on January 7, 2020, and named “severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)” by WHO on February 11, 2020. The disease caused by SARS-CoV-2 is now known as coronavirus disease 2019 (COVID-19). According to the latest retrospective analysis, the median (range) incubation period of COVID-19 is 3 d, but incubation can be as long as 24 d.1 The median age of patients is 47 yr, and adults are more susceptible than children and adolescents.
There is no specific identifying symptom during the early stage of COVID-19 infection. Infected individuals may display weakness, cough, fever, or even no symptom, and yet they are already infectious. The accuracy of early diagnosis based on combined chest computed tomography and nucleic acid test can reach 97%. Expiratory dyspnea occurs in the late stages of infection, and respiratory distress syndrome, acute circulatory failure, or renal failure in severe cases. No specific effective therapeutic protocol in known. The current treatment methods are empiric based on symptoms, and consist of respiratory support (eg, oxygen, mechanical ventilation, or artificial lung technology), antibiotics, and antiviral drugs supplemented by immunoglobulin infusion.1,2
The outbreak of COVID-19 in Wuhan occurred on the eve of the Chinese New Year (January 12, 2020). However, due to lack of awareness and prevention measures taken at that time, the epidemic spread rapidly as people returned home for the Chinese New Year. Despite the government's closure and traffic control of Wuhan since January 23, 2020, COVID-19 had been spread into other provinces of China and even other countries. On January 30, 2020 the outbreak in China was announced as a public health emergency of international concern at a meeting of the WHO Emergency Committee in Geneva, in an effort to suppress global spread of the disease.
So far (from January 23, 2020 to February 24, 2020) as of this writing, there were 3019 medical professionals were infected with SARS-CoV-2; 1716 were diagnosed with COVID-19 and 9 unfortunately died.3 In the very early stage of the epidemic, the first 14 of these infected medical staff were from the Department of Neurosurgery, which was located in the epidemic center of the COVID-19 outbreak. In such an urgent and unexpected situation, the department took immediate and effective prevention and control strategies. These staff was now completely recovered and there were now new infected cases in the department. Here, we would like to summarize and share our successful experiences in the prevention and control of SARS-CoV-2 infection in medical staff of hospital departments, especially those devoted to non-infection diseases.
AN EXPERIENCE IN WUHAN UNION HOSPITAL
On December 25, 2019, a patient with pituitary adenoma was hospitalized for a surgery in the Department of Neurosurgery. Prior to the hospitalization, the patient showed no COVID-19 symptom. But 1 d after the neurosurgical operation, the patient showed low fever and decreased lymphocyte on January 7, 2020, and was admitted to isolation ward on January 11. However, he was diagnosed as COVID-19 and transferred to the designated hospital for the treatments that assigned by the government on January 19, 2020. At that time, the medical community experienced an initial delay in understanding that COVID-19 has a long incubation period prior to diagnosis, and protective measures at the onset were not at the current level III (Table 1). In the Department of Neurosurgery, 14 of the medical staff, including 11 nurses and 3 doctors, were infected after January 11, 2020. Fortunately, by February 5, 2020, all the 14 medical personnel had recovered and been discharged after active treatment.
TABLE 1.
Three-Level Standards Ffor Prevention and Control of Infectious Diseases
| Risk | Protection | Specific content | |
|---|---|---|---|
| I | Low | Basic | First-layer work clothes (eg, scrubs), disposable working caps, surgical masks |
| II | Medium | Increased | Work clothing, shoe covers, disposable working caps, N95 masks, goggles, protective clothing or isolation clothes, latex gloves |
| III | High | Stricta | Work clothing, protective boot covers, disposable working caps, N95 masks, goggles, medical protective masks (or positive pressure head covers), protective clothing, double-layer latex gloves |
aIncludes surgical theater.
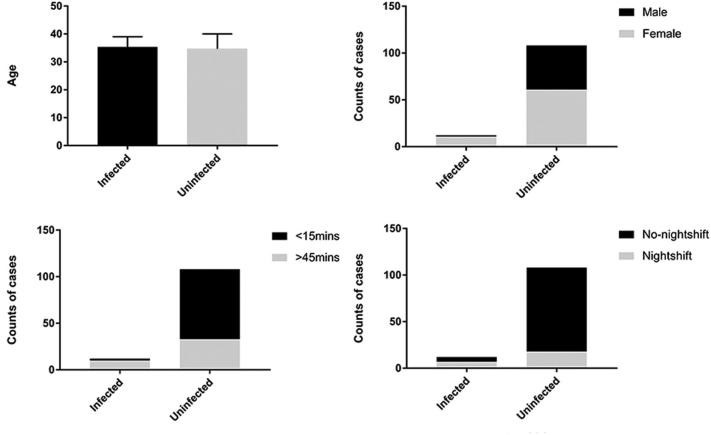
An immediate retrospective analysis was conducted of the differences between infected and uninfected workers in the department. The investigated factors included age, gender, duration of contact with the infected, and night shift experience (Figure 1). The results of binary logistic regression showed that, after adjustment for the remaining 3 variables, the risk of infection in the medical staff with longer exposure to an infected patient (>45 min) was 6 (1.1-32.8) times higher than that of those with shorter exposure (<15 min). Furthermore, the risk of infection was 3.9 (1.0-15.3) times higher for those who had worked a night shift, compared with those who had not.
FIGURE 1.
Differences between infected and uninfected medical staff with regard to age, gender, duration of contact with the infected, and shift work.
With the awareness of the high rate of infection in the medical staff, combined with the statistical results, we drew up strategies for emergency management and daily protection for medical staff in departments of non-infection disease during this severe epidemic. After the implementation of these measures in our department, there has been no further infection among patients or medical staff.
Patient Consent Statement
The study was done after agreement from the local ethics committee and informed consent was provided by participating patients.
PRINCIPLES OF EPIDEMIC PREVENTION AND CONTROL IN CLINICAL DEPARTMENTS
Reduce non-urgent and non-necessary medical activities, and assist diagnosis and treatment via the Internet.
Effectively manage all patients at different levels and categories, that is, patients are categorized as with or without fever, and each group further stratified as emergency or non-emergency, as appropriate.
Reduce direct contact between medical staff and patients, and avoid mutual contact between patients.
Aim for early detection, early isolation, and early treatment of all infected individuals.4
Implement continuous disinfection of the departmental environment.
RECOMMENDATIONS
Emergency Management Paths for Outpatient and Inpatient Patients During the Outbreak
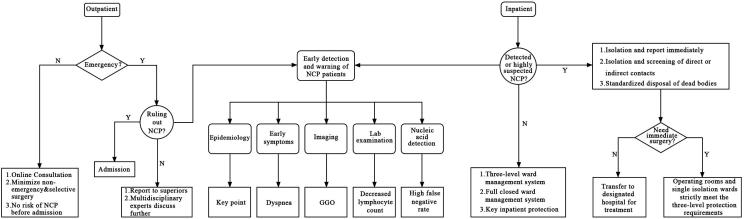
In a scenario of epidemic and shortage of medical resources, the medical staff should triage outpatients and inpatients, to achieve early detection and warning of COVID-19 infection (Figure 2).
FIGURE 2.
Flow chart of effective triage and classification management for outpatients and inpatients.
Protect High-Risk Inpatients
Elderly patients and those with serious underlying diseases. Elderly patients and those with underlying diseases of the heart, lung, liver, and renal system are susceptible to higher pathogenicity and mortality in response to COVID-19 infection.1 The risk of infection varies with the clinical department. For example, patients in the neurosurgery department are at high risk of COVID-19 infection. Therefore, the hospital should be committed to a strict 3-level ward management system (Table 1). Patients suspected of infection should be partitioned from other patients, and each ward should employ different sets of medical staff to avoid cross-contamination.
Patients with systemic abnormalities beyond the respiratory system. Among patients with COVID-19 there are reports of 12%, 7%, and 3% rates of acute cardiac impairment, acute renal impairment, and diarrhea, respectively. Liver injury has also been reported.1 These concomitant conditions are aggravated in COVID-19, and even present a major threat of mortality. Therefore, it is especially important during this epidemic that the basic vital signs and dysfunctional organs of such vulnerable patients are safeguarded. The effect of possible infection should be minimized, with early detection and intervention.5
Patients with associated mental stress. Because COVID-19 is highly contagious, can quickly progress in severe cases, and there is no specific effective treatment, hospitalized patients often experience anxiety, mania, insomnia, or other psychological problems. Patients should be reassured that, although the number of infected persons has rapidly increased, the prognosis is better than for SARS (severe acute respiratory syndrome), and the fatality rate is much lower.6 The medical staff should inform inpatients that the epidemic will subside if scientific prevention, control, and treatment measures are adhered to.
Prevention and Control Strategies in the Neurosurgery Clinic
For outpatients, prevention and control procedures for the new coronavirus can refer to the diagnosis and treatment plan for pneumonia of the National Health and Medical Commission (Trial sixth Edition). This includes a previewing triage system (Figure 2). Outpatient treatment should be arranged for patients with suspected infection or fever. In addition, the management and disinfection of outpatient clinics should be given priority. Patients should be instructed regarding how wear masks correctly, and to put them on before entering the waiting area.
Prevention and Control Strategies in the Neurosurgery Ward
Thorough cleaning and disinfection is essential after contact with each patient. Hands must be carefully washed for 2 to 3 min with disinfectant (75% ethanol or chlorine-containing disinfectant).
As far as practicable, the medical staff should remain 1.5 to 2 meters away from the patient during diagnosis and treatment, and time of contact should be minimized. If an atomizer, stethoscope, or other examination instrument must be used, the medical personnel should avoid contact with patients’ secretions, especially for patients with trachea intubation or tracheotomy. Medical personnel should note the color of phlegm when suctioning sputum, avoid the airway opening as much as possible, and wear a protective mask. Body fluids, secretions, excreta, and used articles collected from confirmed and suspected patients should be regarded as biological pollutants, and treated as clinical waste at the highest biosafety level.
Testing throat swabs for nucleic acid is important for diagnosing COVID-19 infection. However, the sampling process poses great risk to the healthcare worker. To protect the medical staff to the greatest extent, only designated, senior, and experienced medical staff should collect samples, and in accordance with a standardized protocol with level III protection measures.
Ward Management and Disinfection and Sterilization
Inpatients and accompanying persons should be instructed and required to wear masks in the ward. Warnings should be posted at the entrance of the ward, and information regarding protection against infection should be promoted and disseminated to increase public knowledge. Accompanying persons should not be permitted to take the inpatients outside the hospital without permission, or visit other wards or congregate.
All wards should institute a layered management system, with the wards strictly divided into 3 levels according to risk: common ward, isolation ward for suspected patients, and single isolation for the diagnosed patient. Free movement of persons among the 3 ward levels should be strictly limited to avoid cross contamination. Each level should deliver its own medical treatment.
Wards should be ventilated at least 2 to 3 times daily, for not less than half an hour each time. All objects in the ward that are frequently handled, such as door knobs, bed edges, window sills, and wall switches, should be cleaned regularly and disinfected with 500 mg/L chlorine-containing disinfectant twice per day.
As much as possible, individual items that are commonly used in departments should be designated for use in a single ward, including blood pressure meters, thermometers, and stethoscopes. If the number is insufficient or it is necessary to borrow in an emergency, the items must be thoroughly disinfected.
Prevention and Control Strategies for Medical Staff in Operating Rooms
For patients undergoing elective neurosurgery, stepwise preoperative screening for COVID-19 should be conducted based on the diagnostic criteria. The surgery should be performed only after no abnormality is detected. Due to the long incubation period, medical staff should take level II protection measures (Table 1).
In principle, no elective surgery should be scheduled for patients with suspected or confirmed COVID-19. If emergency craniotomy is needed, the medical staff must take the following level III precautions: strictly wearing disinfected first-layer work clothes (hospital scrubs) and additional gown with hood; double latex gloves; 2 layers of cap; goggles and other facial protection tools; and medical protective masks (N95). It is necessary to avoid or reduce endotracheal intubation, tracheostomy, and other procedures that aggravate infection. If possible, during surgery adequate and proper hemostasis should be maintained to prevent the need for blood transfusion. The spatter of body fluid should be avoided to lower the risk of infection.
A one-way path should be used to enter and exit the operating room. Suspected pollution areas should be avoided. The operating room should contain infrared thermometers to measure the body temperature of the medical staff and patients at any time to give early warning of acute illness.
After surgery, medical staff must use quick-drying hand disinfectant before and after removing protective clothing, after taking off googles and hat, after removing the inner gloves, and again after removing masks before donning new masks and immediately leaving the operating room.
Prevention and Control Strategies for Neurosurgery Office and Living Areas
In addition to operating rooms and wards, the offices and living areas of the medical staff are important potential areas of infection that are often overlooked. Therefore, the following 4 measures are necessary.
A safe distance should be maintained between the medical office and ward, with good ventilation. An electrostatic air purifier can be installed if feasible.
Mobile phones, landline phones, keyboards, cups, medical records, and other items that are used frequently should be regularly disinfected.
Meals should be eaten away from crowds, sitting face-to-face, and without talking if possible.
To reduce direct physical contact between colleagues, as far as possible communication should be made by telephone or WeChat.
Improve the Awareness of the Medical Staff About the Epidemic
COVID-19 differs from any other known infectious disease, and information regarding adequate protection is lacking. In addition, a high incidence of infectious disease in a department of neurosurgery is unusual. The neurosurgery staff must be instructed regarding what is known about infections of this disease. In addition to basic hospital training, our department has improved education regarding important guidelines and procedures related to COVID-19 infection (Table 2). The great importance of early detection and isolation of suspected cases must be emphasized, and safety measures strictly implemented. The staff must receive both theoretical and practical knowledge about COVID-19 infection and medical protection to enhance vigilance and the ability to confront emergencies.
TABLE 2.
Guidelines, Manuals, and SOPs for Responding to NCP Infection.
| Content | Source | |
|---|---|---|
| Guideline | Diagnosis and treatment of pneumonia caused by novel coronavirus (Trial 5th Edition) | NHC |
| Handbook | Handbook for the prevention of NCP | Hubei Science & Technology Press |
| SOP | Guidelines for the use of common medical protective equipment in the prevention and control of NCP | NHC |
| SOP | Flow chart of patients with fever during NCP | Wuhan Union Hospital |
NCP, novel coronavirus-infected pneumonia; NHC, National Health Commission of the People's Republic of China; SOP, standard operating procedure
Safeguard the Mental Health of Medical Staff
Under the pressures imposed by the severe epidemic and intense clinical work, medical staff may experience negative emotions that can reduce daily work efficiency and have long-term adverse effects on the entire medical team. Negative emotions may manifest as anxiety, depression, or insomnia, among others. Appropriate mental health education and positive encouragement are crucial for protecting the staff against these stressful conditions.7
CONCLUSION
The number of infected persons and the rapid spread of COVID-19 are unprecedented as a public health emergency. This epidemic is a serious challenge to China's medical system and its ability to cope. The nation cannot afford further misjudgments regarding the need for information, prevention, and protection against COVID-19 infection. Herein, we have summarized the experience of our neurosurgery department and the protection measures we have implemented. Because of these new preventive protocols, there have been no further cases of infection among our medical staff. Coping with this emergency will require better understanding of infection characteristics and route of transmission, and achieving early detection, isolation, and treatment. With adequate upgrades in protective protocols and training, medical personnel in departments not related to infectious diseases can face this outbreak in a scientific, effective, and easy manner, and ensure the normal procedures of diagnosis and treatment.
According to Tedros Ghebreyesus, the director-general of WHO, “No single country or organization can stop this outbreak alone. Our greatest and only hope is to work together.” To this end, we share with our colleagues around the world our practical experience in dealing with the outbreak, and we hope to contribute to the world health system.
Disclosures
This project was supported by the Medjaden Academy & Research Foundation for Young Scientists (Grant No. nCoV_MJA20200221). The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Acknowledgments
This project was supported by the Medjaden Academy & Research Foundation for Young Scientists (Grant No. nCoV_MJA20200221).
REFERENCES
- 1. Guan W-j, Ni Z-y, Hu Y et al.. Clinical characteristics of 2019 novel coronavirus infection in china. N Engl J Med. published online: February 28, 2020(doi:10.1056/NEJMoa2002032). [Google Scholar]
- 2. Wang D, Hu B, Hu C et al.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in wuhan, china. JAMA. 2020;323(11):1061-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Read JM, Bridgen JRE, Cummings DAT, Ho A, Jewell CP. Novel coronavirus 2019-nCoV: early estimation of epidemiological parameters and epidemic predictions. Centre for Health Informatics, Computing and Statistics, Lancaster Medical School, Lancaster University, Lancaster, United Kingdom ( 10.1101/2020.01.23.20018549). [DOI] [Google Scholar]
- 4. Shao P, Shan Y. Beware of asymptomatic transmission: study on 2019-nCoV prevention and control measures based on extended SEIR model. bioRxiv 2020( 10.1101/2020.01.28.923169). [DOI] [Google Scholar]
- 5. Huang C, Wang Y, Li X et al.. Clinical features of patients infected with 2019 novel coronavirus in wuhan, china. Lancet. 2020;395(10223):497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Benvenuto D, Giovanetti M, Salemi M et al.. The global spread of 2019-nCoV: a molecular evolutionary analysis. Pathog Glob Health. 2020:1-4 ( 10.1080/20477724.2020.1725339). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kang L, Li Y, Hu S et al.. The mental health of medical workers in wuhan, china dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]