Abstract
Deficits in self-regulation (SR) have been proposed as a potential contributor to child overweight/obesity, a public health concern that disproportionately affects children living in poverty. Although poverty is known to influence SR, SR has not been considered as a potential mechanism in the association between poverty and child obesity. The aim of the current paper was to systematically review the current literature to determine whether SR is a viable mechanism in the relationship between child exposure to poverty and later risk for overweight/obesity. We systematically review and summarize literature in three related areas with the aim of generating a developmentally informed model that accounts for the consistent association between poverty and child weight, specifically how: 1) poverty relates to child weight, 2) poverty relates to child SR, and 3) SR is associated with weight. To quantify the strength of associations for each pathway, effect sizes were collected and aggregated. Findings from the studies included suggest small but potentially meaningful associations between poverty and child SR and between SR and child weight. The conceptualization and measurement of SR, however, varied across literatures and made it difficult to determine whether SR can feasibly connect poverty to child obesity. Although SR may be a promising potential target for obesity intervention for low-income children, additional research on how SR affects risk for obesity is crucial, especially based on the lack of success of the limited number of SR-promoting interventions for improving children’s weight outcomes.
Keywords: poverty, obesity, BMI, self-regulation, food insecurity
Introduction
Pediatric obesity is a public health concern that affects children’s quality of life and their current and future health outcomes. Seventeen percent of U.S. children ages 2–19 are estimated to be obese, and an additional 15% overweight (Ogden, Carroll, Kit, & Flegal 2012), with these numbers reflecting a substantial increase over the past several decades (Ogden et al. 2016). Although the medical problems associated with overweight may not become apparent until adulthood (e.g., cardiovascular disease, metabolic syndrome), the risk of adult obesity is known to be greater for children who are overweight in childhood (Simmonds, Llewellyn, Owen, & Woolacott 2016). Furthermore, overweight and obese children report lower quality of life (Friedlander, Larkin, Rosen, Palermo, & Redline 2003) and social isolation (Strauss & Pollack 2003). Unfortunately, research on child obesity prevention and treatment has only recently started to include children from low-income families (Kimbro, Brooks-Gunn, & McLanahan 2007; Shrewsbury & Wardle 2008), who tend to be at greater risk for weight problems. Obesity prevention and treatment may be especially challenging for children living in poverty because of increased exposure to environmental stress and chaotic living conditions (Evans & English 2002).
There are many adverse psychosocial outcomes associated with exposure to poverty in childhood. Family income and other markers of financial hardship have been found to have detrimental effects on children’s academic achievement (Votruba-Drzal 2006), behavior (Eamon 2002), and mental (Dearing, McCartney, & Taylor 2006) and physical health (Lawlor, Ronalds, Macintyre, Clark, & Leon 2006). Poverty has also been established as a potent risk factor for child overweight and obesity (Alaimo, Olson, & Frongillo 2001; Cameron et al. 2015), an association that at first glance may appear paradoxical. Historically, poverty has been associated with inability to afford food, leading to malnutrition and underweight. Several mechanisms for this association have been proposed, with most focused on the premise that children living in poverty tend to eat more high calorie, low-nutrient foods and have less access to opportunities for physical activity (Drewnowski & Specter 2004; Sallis & Glanz 2006).
Although both family-based (Epstein, Valoski, Wing, & McCurley 1990) and community interventions (Bleich, Segal, Wu, Wilson, & Wang 2013) have been developed to address and prevent child overweight, few have been found to have lasting effects on child weight (Ebbeling, Pawlak, & Ludwig 2002). Most intervention efforts fall broadly in the category of “lifestyle interventions,” with a relatively narrow focus on decreasing calorie intake and increasing physical activity (T. Brown & Summerbell 2009; McCallum et al. 2007; Nemet et al. 2005); prevention efforts tend to focus on similar objectives (Economos et al. 2007; Hollar et al. 2010). However, targeting these areas has proven surprisingly and frustratingly resistant to long-term change. Theoretically, these behaviors may be even more challenging to modify in low-income children because of lack of access to nutritionally sound food and limited opportunities for physical activity.
Historically, child obesity treatment and prevention efforts have not taken into account differences in children’s developmental status. “Sensitive periods” during which excessive child weight gain is particularly strongly linked to later obesity have been identified (i.e., during middle childhood in a period known as “adiposity rebound,” and during adolescence when they go through puberty (Dietz 1994). However, knowledge about development has infrequently been incorporated into designing targeted treatment and prevention efforts for children at specific development stages, nor has it been systematically evaluated as a moderator of treatment efficacy in reviews or meta-analyses (Ho et al. 2012). In addition, few researchers have evaluated whether the effect of poverty on child weight varies depending on the timing and duration of poverty exposure at different developmental stages of childhood.
Because of the lack of success in reducing children’s weight by modifying their energy balance, it could prove valuable to investigate potential alternative mechanisms leading to child obesity as targets of prevention and/or intervention (i.e., focusing on nutrition and physical activity), targets that might be more malleable than diet or physical activity. Although addressing energy balance in children is the ultimate goal to promote and sustain healthy weight maintenance, it has become clear that addressing childhood obesity by focusing narrowly and primarily on children’s calorie intake and physical activity has shown limited success. Identifying broader behavioral styles that may underlie children’s tendencies to overeat and/or be physically inactive and exploring how such behavioral styles may exacerbate continued weight gain could prove helpful in improving obesity prevention efforts in particular. Such issues may be particularly critical for children living in poverty because of their greater exposure to contexts that promote obesity.
A critical attribute for children’s social and academic success that has been linked to poverty is self-regulation. Self-regulation (SR) encompasses one’s ability to modulate behavior and emotions in response to internal and external demands and is often conceptualized using a dual process model consisting of “hot,” reactive processes (e.g., impulsivity) and a “cool,” reasoned, cognitive system (Isasi & Wills 2011; Metcalfe & Mischel 1999). Children living in poverty have been postulated and found to show lower levels of SR because of their greater exposure to witnessing and experiencing violence and trauma, more frequent changes in residence, and both exposure to and genetic risk of mental health problems among family members (Evans & English 2002; Lengua, Honorado, & Bush 2007; Raver 2004). As SR is vital for helping children manage their emotions and behavior, it is not surprising that deficits in SR have been linked to a variety of adverse outcomes for children and adults, including peer rejection in middle childhood (Trentacosta & Shaw 2009), antisocial behavior in adolescence (Sitnick et al. 2017), and importantly, physical health in adulthood (Moffitt et al. 2011). As maintenance of healthy body weight involves appropriate SR of energy intake, it follows that SR has been found to be associated with child body mass index (BMI), overweight, and obesity in both cross-sectional studies (Miller, Rosenblum, Retzloff, & Lumeng 2016) and longitudinal ones (Francis & Susman 2009; Paulo A Graziano, Calkins, & Keane 2010; Seeyave et al. 2009).
As child weight and poverty have been associated with multiple components of SR, SR may be especially important in explaining how poverty affects child weight. In addition, as SR has been found to be malleable using school-, family-, and individual-based approaches during multiple developmental periods (Johnson 2000; Raver et al. 2011; Riggs, Greenberg, Kusché, & Pentz 2006; Shelleby et al. 2012), it represents a viable target for prevention and intervention. However, almost no studies have investigated the potential mediating role of SR in associations between poverty and child weight.
The current review summarizes literature in three related areas with the aim of generating a developmentally informed model that accounts for the consistent association between poverty and child weight, specifically how: 1) poverty relates to child weight, 2) poverty relates to child SR, and 3) SR is associated with weight. Although there is a relatively rich literature documenting each of these direct paths, extremely few empirical papers have attempted to integrate these literatures to investigate the possibility that SR might mediate associations between poverty and child weight. Further, a developmental approach to this literature can determine whether there are sensitive developmental periods during which child weight and SR are particularly vulnerable to the effects of poverty. In addition to summarizing and consolidating the evidence from studies across two separate literatures (i.e., obesity literature and SR literature), the goal of this paper was also to determine whether SR could be a viable target for obesity prevention for children living in poverty.
This review includes only longitudinal studies, which, in the absence of an experimental design, are necessary for establishing a case for the presence of causal mechanisms among variables of interest. Without a longitudinal design in which baseline levels of the variable of interest are included in the model, the possibility of other variables driving the association, or that variables simply cooccur without a causal relationship, is difficult to rule out.
Methods
Operational definitions of variables
Poverty/Financial Hardship.
Although poverty can be defined and operationalized in many ways, the current review focused specifically on studies that define poverty based on income and/or financial strain. Studies often use measures of poverty that aggregate multiple indicators of socioeconomic status (SES), including income but also variables such as parental education and occupation. This review included studies that used such composites as long as income or another proxy for financial strain was included. Although parental education and occupation may play some role in influencing children’s weight (Lamerz et al. 2005), there is a stronger rationale for focusing on income specifically, as it is more malleable and its measurement more straightforward than other aspects of SES.
This review also includes studies in which income/financial strain was incorporated into a cumulative risk index that included other risks and stressors. The use of cumulative risk indices has strong theoretical and empirical support, with the rationale being that although the effect of any single risk may be small, multiple risks in combination are particularly detrimental and more damaging than their individual additive effects (Forehand, Biggar, & Kotchick 1998). Children living in poverty are much more likely to be exposed to multiple, interrelated risks, such as exposure to violence, substandard housing, marital conflict, and maternal psychopathology (Evans & Kim 2007; Rutter et al. 1997).
Lastly, food insecurity (FI) was also considered a measure of poverty/financial strain, as a family’s FI status indicates the presence or absence of an important resource (food) that is closely tied to financial hardship. FI has been defined by the United States Department of Agriculture (USDA) as “reduced quality, variety, or desirability of diet,” with or without the presence of “disrupted eating patterns and reduced food intake” (i.e., with or without hunger) (ColemanJensen, Gregory, & Singh 2014). FI is most commonly measured using an 18-item scale developed by the USDA (Hamilton & Cook 1997).
When income or an income-to-needs ratio was used as the indicator of poverty, the word “income” is used to encompass both. The term “SES” is used when the study employed a measure that included not only income but also either parental education, occupational status, or both. The term “poverty” is used to refer broadly to all measures of poverty or poverty-related stressors included in this review, including income, SES, cumulative risk, and FI.
Self-Regulation.
The definition of SR and its various components varies greatly and is frequently inconsistent across studies. Conceptually, the construct of SR is quite broad and is thus frequently deconstructed into distinct but often closely related components. However, these components (e.g., effortful control, inhibitory control, emotion regulation) may be difficult to differentiate, in part because there are no tasks that “cleanly” measure one without involving the others. Furthermore, the language used to label and categorize SR and its components is quite variable, with different terms being used to describe the same processes, and vice versa, and different literatures tending to adopt divergent language for describing SR.
In spite of these issues, overarching themes to characterize SR have emerged across disparate literatures. For one, it is common for researchers to conceptualize SR processes using some kind of a dual process model. A particularly common and well-accepted model conceptualizes SR as consisting of two systems referred to as “hot” and “cool” (Metcalfe & Mischel 1999). Hot SR is thought to be engaged in emotionally arousing situations, including tasks with “appetitive demands,” whereas cool SR is deployed primarily in emotionally neutral contexts and involves more conscious, cognitive attentional processes and planful reactions (Eisenberg & Zhou 2016). Cool SR overlaps with the construct of executive functioning as it is typically conceptualized (Willoughby, Kupersmidt, VoeglerLee, & Bryant 2011).
In the current review, regardless of how authors referred to constructs and measures in their papers, behavioral measures were categorized as “hot” or “cool” based on the author’s evaluation of the SR domain each task intended to measure, with measures that involved regulation or inhibition with an emotional or appetitive component categorized as “hot,” and emotionally neutral tasks as “cool.” One commonly used measure of hot SR is delay of gratification (DoG). In a DoG task, children are presented with some desired object or food (for example, a cookie), and are told that they can either eat one cookie now, or have two cookies later. During the waiting period, children are usually left alone with the desired object/food with no other opportunities for entertainment or distraction and they can alert the experimenter at any time to indicate that they are unable to wait any longer. Refer to Table 1 for a summary of how additional common observed measures of SR were categorized as “hot” or “cool.”
Table 1.
Examples of observed self-regulation measures categorized as hot versus cool
| Hot | Cool |
|---|---|
| Delay of gratification (food/non-food) (e.g., Seeyave et al., 2009) | Stroop and Stroop-like tasks (e.g., Lengua et al., 2007) |
| Gift delay (e.g., Thompson et al., 2013) | Motor control tasks (e.g., Balance Beam task) (e.g., Bassett et al., 2012) |
| High chair frustration task (Graziano et al., 2010) | Opposite of Commands task (e.g., Head-to-Toes) (e.g., Wanless et al., 2011) |
| Continuous Performance Test (e.g., Bub et al., 2016) |
A variety of methodologies for the measurement of child SR is included in the current review, such as observed measures of child SR and parent or teacher reports on questionnaires. Nearly all questionnaire measures assessing child SR capture aspects of both hot and cool domains. For example, items from the inhibitory control subscale of the Child Behavior Questionnaire (Rothbart, Ahadi, Hershey, & Fisher 2001) measure both “hot” emotional, impulsive behaviors such as “has an easy time waiting to open a present,” and “cool,” measured behaviors or processes, as in “likes to plan carefully before doing something.” Therefore, in the current review, questionnaire measures are not categorized as “hot” or “cool.”
In her conceptualization of SR, Calkins (2007) adds a physiological component in addition to the systems she refers to as “emotional” and “attentional” (which map onto hot and cool SR, respectively). She highlights the importance of heart rate variability (HRV) as a measure of parasympathetic nervous system activation, which is crucial in modulating emotion regulation and reactivity (Calkins & Dedmon 2000; Porges 2007). Thus, measures of HRV such as respiratory sinus arrhythmia (RSA) are also considered a marker of SR in the current review and categorized as “physiological.” Physiological SR is subsumed under the category of hot SR, as it is thought to be more relevant in situations that require the regulation of emotional or behavioral arousal.
Studies that used both observed and questionnaire methods that specifically assessed eating or appetite components of SR (e.g., emotional overeating) were also included and considered as a category separate from hot and cool SR, as SR of appetite likely contains aspects of both hot and cool SR. For example, some children may overeat as a way to cope with and/or regulate negative emotions (Goossens, Braet, Van Vlierberghe, & Mels 2009), which would capture aspects of hot SR. Alternatively, features of cool SR may be employed when children consciously restrain themselves from eating large amounts of palatable but unhealthy foods, an eating behavior that has been observed in children as young as 5 years old (Carper, Fisher, & Birch 2000).
The aspects of SR featured in this review had to be viable candidates for mediating the association between poverty and weight. Although there are alternative models for understanding SR, the hot/cool distinction was selected to categorize SR measures because the SR of healthy weight maintenance likely involves both emotional and cognitive processes.
Child Weight.
Two ways of operationalizing weight were used in the studies included in this review. The first is using BMI, a continuous variable, as the outcome of interest, and the second is using weight status, a categorical outcome variable such as the presence or absence of overweight and/or obesity. The use of BMI has the advantage of allowing for trajectories of weight gain over time to be analyzed with respect to income or income changes, while weight status offers the ability to differentiate clinically significant from normal child weight.
There is some evidence to suggest that weight status measured after approximately age two is relatively stable throughout childhood. Findings from one study suggest that children categorized as normal weight or obese at as early as age 3 were likely to remain the same weight status at age 15 (Tran, Krueger, McCormick, Davidson, & Main 2016). However, some research indicates that early childhood BMI is a poor predictor of later childhood weight when it is measured prior to adiposity rebound, when normative increases in BMI start to occur in all children, usually by the age of 6 (Rolland-Cachera, Deheeger, Maillot, & Bellisle 2006). Therefore, it is important to consider the age that weight was measured before drawing conclusions about the effects (or lack thereof) of environmental (e.g., exposure to poverty) or child characteristics (e.g., SR) on child weight.
Age periods covered
This review focuses on longitudinal studies in which the final measurement of the independent variable (poverty or SR) was prior to age 10, as exposure to poverty during early and middle childhood was of primary interest because of the possible implications for obesity prevention. Additionally, the review excluded studies in which the last measurement of the dependent variable (weight or SR) was after age 18, as the scope of the review was limited to childhood and adolescence. Studies that measured weight prior to age 2 were also excluded, as some research suggests that this early in childhood, child overweight/obesity is a poor predictor of later excess weight (Whitaker, Wright, Pepe, Seidel, & Dietz 1997).
To gain an understanding of which developmental stages have been most studied with regard to the pathways of interest and whether there were differences in the strength of associations depending on stage, age periods were categorized as follows: Early Childhood (0–5), Middle Childhood (6–11), and Adolescence (12–18).
Inclusion of Studies
Articles for the current review were identified through searches using the databases PsycINFO and PubMed. Separate searches were conducted for each of the three pathways. 1) SES search terms (appearing in title and/or abstract) were as follows: socioeconomic, poverty, income, cumulative risk, adversity, and food insecurity. 2) SR keywords, also in the title or abstract, consisted of the following: regulat* (the asterisk denotes that a word stem was searched), executive function, inhibitory control, executive control, effortful control, delay of gratification, eating in the absence of hunger, overeat*, appetit*, impulsiv*, and attent*. 3) Weight search terms appearing in the title or abstract were: body mass index, BMI, overweight, obes*, weight. For all, the term child*, boy, or girl had to appear in the abstract.
As an example, for the poverty→weight pathway, PsycINFO was searched first using the terms “socioeconomic” and “body mass index.” The search was repeated until every combination of the “poverty” and “weight” search terms had been entered. The citation for every article that resulted from each search was downloaded to a file for review. This search was then repeated in an identical fashion using the PubMed database. This procedure was then repeated for the poverty→SR (using the “poverty” and “SR” keywords) and SR→weight (using the “SR” and “weight” search terms) searches.
Next, some studies were identified using reference lists of the initial articles, and also searching for papers that cited them. Only longitudinal studies, where the dependent variable was measured after the independent variable, were included in the formal review. Experimental studies where poverty or SR was manipulated as part of an intervention were also included. Although many child weight loss interventions involve some aspect of SR (Braet, Tanghe, Decaluwé, Moens, & Rosseel 2004; Epstein, Wing, Koeske, Andrasik, & Ossip 1981), only studies that specifically measured SR pre- and post-intervention were included in the review on the SR to weight pathway.
Upon completion of the searches in PsycINFO and PubMed, the results for each pathway were compiled and duplicates were removed. Each article was reviewed to determine its appropriateness for inclusion in the systematic review. Inclusion criteria were as follows: a) published in a peer-reviewed journal, b) published or available in English, c) normative sample (i.e., excluded studies that tested associations with specific populations like very low birth weight infants or children prenatally exposed to substances, d) longitudinal, with at least 6 months between assessments (several studies used assessments at the beginning and end of school years). Studies were excluded if they were part of an intervention study (e.g., an early childhood intervention that tested SR as an outcome and included family income as a covariate), unless it was a weight loss intervention that specifically targeted SR. There were several other exclusion criteria that were unique to one of the pathways; these are described in the section specific to that pathway.
For the two pathways in which poverty was the independent variable, in some cases the poverty variable was measured when mothers were pregnant with the target child -- these studies were included in the review. In addition, it was frequently the case that poverty (usually income) was operationalized using an average of family income across multiple years of assessment. For example, one study averaged income over three years of assessment (when children were 5, 7, and 9 years old), with the outcome for BMI at age 9 (Tiberio et al. 2014). These studies were included as long as there were at least two other assessment points included in the SES variable in addition to the concurrent assessment (i.e., the age 9 assessment in this example). However, studies were excluded if they tested trajectories of family income or chronicity of poverty over a period of more than five years, as such analyses are not directly comparable to those testing poverty exposure at a single assessment point. Similarly, studies that tested growth in child weight or children’s weight trajectories over time were also excluded.
The review was primarily concerned with the relationship between poverty and obesity in the United States, although this phenomenon has been well documented in many other high-income countries. Therefore, studies with non-U.S. samples were included if the World Bank defined the country as a “high-income economy,” as the U.S. is categorized. This classification is based on gross national income per capita; those with a GNI of $12,056 per capita are considered high-income. As the pattern of the relationship between poverty and weight for individuals living in low-income countries may differ compared to high-income countries, and the relationship for individuals in middle-income countries appears to be inconsistent (Dinsa, Goryakin, Fumagalli, & Suhrcke 2012), the attention of the current review was focused on high-income countries.
Effect size aggregation
Articles that met criteria for the review were searched to locate the unadjusted relationship between the two variables of interest (e.g., bivariate, zero-order correlation, unadjusted odds ratio). In addition to effect size, the following information was also extracted from each paper that met inclusion criteria: age that the independent variable was measured, age(s) that the dependent variable was measured, how poverty was operationalized, type of SR (if applicable), and information about the sample, including the country where the study took place and whether it was described in the paper as predominantly low-income.
For the poverty→weight pathway, an overall total aggregated effect size was calculated for each pathway, along with three different effect sizes stratified by developmental stage (i.e., early childhood, middle childhood, adolescence), as one goal of the study was to determine whether the relationship between poverty and weight differed depending on when weight was measured. Similarly, for the poverty→SR and SR→ weight pathways, three different effect sizes were calculated based on which type of SR was tested (hot, cool, or questionnaire). For the SR→ weight pathways, it would have been ideal to assess age of outcome in addition to SR type, but the cell sizes would have been too small to detect meaningful differences in effect sizes. In addition, a “total effect size” was calculated without consideration of developmental stage or SR type.
If an unadjusted measure of effect size was not included in the manuscript, the first and/or corresponding author of the paper was contacted by email to request the necessary information. Only studies with an effect size were retained for inclusion in the systematic review. After any one sample was represented in the effect size list for a given pathway, authors of other papers that used the same sample were no longer contacted if the effect size information was not included in the manuscript. If effect size information from the same sample was available from more than one paper, effect sizes were averaged into a single “entry” for that sample.
One exception to the above rule was that if the developmental stage during which BMI was measured (for the poverty→ weight pathway) or the type of SR measured (for the poverty→SR and SR→ weight pathways) differed across multiple papers that used the same sample, multiple effect sizes were retained. For example, for the poverty→weight pathway, three studies utilized the Fragile Families dataset (Assari, Thomas, Caldwell, & Mincy 2018; Burdette & Whitaker 2007; Starkey & Revenson 2014). Although in all three papers researchers used the same measure of poverty (income at birth), each assessed their outcome of obesity or weight at a different age, with Burdette and Whitaker (2007) using obesity at age 3 (early childhood), Starkey and Revenson (2014) using BMI at age 9 (middle childhood), and Assari and colleagues (2018) testing effects on BMI at age 15 (adolescence). Therefore, the effect sizes for all three papers were retained for the analysis by developmental stage, but not for a separate “total effect size” that was calculated without consideration of age of outcome.
Effect sizes were transformed such that all were consistently representing the relationship between poverty and weight. For example, if the variable for “poverty” used in the study was a continuous measure of family income, operationalized as dollars per year, the sign (+/−) was reversed so that it became an index of poverty rather than income (i.e., a positive r indicates that high poverty/low income is associated with higher BMI). Similarly, for the poverty→SR and SR→weight pathways, the way in which SR was operationalized was considered prior to aggregating effect sizes. When the variable of interest was operationalized in a study as a lack of SR (e.g., impulsivity, eating more in the absence of hunger), the sign was reversed to ensure consistency across studies.
Review of Literature
Longitudinal research linking poverty and food insecurity to childhood weight
Included in the review were studies in which the primary research aim was to assess the relationship between poverty and weight, and also studies in which the primary independent variable of interest was not poverty or SES, but some other variable (e.g., breastfeeding, parental smoking), with SES included as a covariate in analyses.
Results of aggregated effect size analysis for longitudinal associations between poverty exposure and weight.
Use of the search methodology described above resulted in the identification of 4,156 articles. Of those, 130 were found to meet criteria for inclusion in the review. Eighteen studies included effect size information in the paper. For 49 studies, authors were emailed. Of those, 17 provided effect size information. Twenty-five unique samples were represented in the analysis, with an additional five studies being from duplicate samples in which more than one paper included an effect size (in these cases, effect sizes were averaged across studies). Fifty-seven papers were from duplicate samples (e.g., ECLS-K, n =14; NICHD SECCYD, n = 9; NLSY79, n = 9) where the effect size was not available in the paper. As described above, authors were not emailed to obtain effect size information for studies that used duplicate samples (i.e., those samples for which an effect size had already been obtained via the paper itself or an email to the author).
Effect sizes were converted to r from odds ratios, risk ratios, spearman’s rho, and Cohen’s d (which was usually calculated by the first author using a table included in the paper) using an effect size calculation website (Lenhard & Lenhard 2016). Studies that had effect sizes of r ≥ .10 were enumerated, as r = .10 is generally considered to be the lower limit for what should be considered a “small” effect size (Cohen 1992). Out of the 25 effect sizes from the 25 unique samples, 14 exceeded that threshold with effect sizes of r ≥ .10 in the expected direction (i.e., greater poverty associated with higher weight) (see Tables 2 and 3). Two effect sizes were in the opposite direction, with correlation coefficients for the association between poverty and weight in the −.10 to −.20 range (i.e., higher poverty associated with lower weight) (Coley & Lombardi 2012; Tiberio et al. 2014). The total average effect size for the longitudinal association between poverty and weight was r = .09.
Table 2.
Studies with a positive relationship and effect size ≥ .10 for poverty-weight pathway
| Author | Sample | r (converted) |
|---|---|---|
| Bhargava (2008) | ECLS-K, N=7635 | 0.16 |
| Li (2007); Strauss (1999) | NLSY79; N=1739; 2913 | 0.24 |
| Williams (2018); Gibbs (2014) | ECLS-B; N=7022 | 0.12 |
| Evans (2012) | Community sample (NY); N=244 | 0.19 |
| Tandon (2015) | Community sample (WA); N=306 | 0.24 |
| Baldwin (2016) | E-Risk twins; N=2232 | 0.16 |
| Holm-Denoma (2014) | Community sample (OR); N=38 | 0.16 |
| Lee (2014); Lane (2013) | NICHD SECCYD; N=1150; 1238 | 0.11 |
| Hancock (2014) | Longitudinal Study of Australian Children (LSAC); N=2596 | 0.18 |
| Sen (2017) | Project VIVA; N=992 | 0.12 |
| Bush (2017) | Peers and Wellness Study; N=338 | 0.17 |
| Van Hulst (2015) | QUALITY Quebec; N=512 | 0.13 |
| Lim (2011) | Community sample (MI); N=317 | 0.39 |
| Strobino (2016) | Healthy Steps for Young Children National Evaluation; N = 4745 | 0.19 |
Table 3.
Studies with a negative relationship or effect size < .10 for poverty-weight pathway
| Author | Sample | r (converted) |
|---|---|---|
| Mészáros (2008) | Hungarian sample, N = 495 | −.04 |
| Janjua (2012) | Sample recruited from University of Alabama prenatal clinic, N = 740 | .06 |
| Slopen (2012) | Avon Longitudinal Study (UK), N = 3286 | .04 |
| Baptiste-Roberts (2012) | The National Collaborative Perinatal Project, N = 28358 | .05 |
| Carter (2012) | Longitudinal Study of Child Development in Quebec, N = 1566 | −.07 |
| Collings (2017) | Born in Bradford (UK); N = 1338 | −.03 |
| van Rossem (2010) | Generation R (Netherlands); N = 2954 | −.05 |
| Kwok (2010) | Children of 1997 (Hong Kong); N = 8237 | .04 |
| Bergmeier (2014) | Australian Research Council Discovery Grant Study; N = 201 | .03 |
Strength of associations by features of the sample.
Eight papers used predominantly low-income samples, with three from the Fragile Families study (Assari et al., 2018, Burdette & Whitaker, 2007; Starkey & Revenson, 2015) and five from other samples (Baptiste-Roberts, Nicholson, Wang, & Brancati 2012; Coley & Lombardi 2012; Collings et al. 2017; Janjua, Mahmood, Islam, & Goldenberg 2012; Lim, Zoellner, Ajrouch, & Ismail 2011). Of those, five studies found little to no association between poverty and weight (with r’s ranging from .06 to .03). For the sixth study, which used a low-income sample of 322 mother-child dyads from Boston, Chicago, and San Antonio, (Coley & Lombardi 2012), the effect size was in the small to moderate range (r =.19). However, the relationship was in the opposite direction of what was expected, with higher income in early childhood (age 0–2) associated with higher rates of child overweight/obesity at age 7.
Eleven of the 25 unique samples represented were comprised of non-U.S. participants (predominantly from the U.K., but also Canada, Hungary, Australia, Korea, and Hong Kong). Of the 11 studies that used non-U.S. samples, four found evidence for a small to moderate association between poverty and weight: one of the three studies from the U.K. (Baldwin et al. 2016), one of the two from Australia (Hancock, Lawrence, & Zubrick 2014), and one of the two studies from Canada (Van Hulst et al. 2015). As an example, Hancock and colleagues (2014) used a large longitudinal dataset from Australia (N = 2596) to address their primary research question of whether maternal protectiveness was associated with greater risk of child overweight/obesity. The study, which started when children were 4–5 years old, with follow-up assessments 2, 4, and 6 years later, included income quartile as a covariate in their analyses. At each follow-up visit, the group with the lowest income at baseline was consistently found to have greater risk of overweight/obesity compared to the highest income group, with odds ratios ranging from 1.7 (at the age 8–9 visit) to 2.3 (at the age 10–11 assessment). Of the other six studies in which the association between poverty and weight was minimal, samples were drawn from the Netherlands (van Rossem et al. 2010), Hungary (Mészáros et al. 2008), Korea (I. Lee, Bang, Moon, & Kim 2016), and Hong Kong (Kwok, Schooling, Lam, & Leung 2010). When the 11 non-U.S. samples were removed from the aggregated effect size calculation, the new aggregated effect size (n = 15) was r = .12.
Food Insecurity and Child Weight.
Upon review of the literature, a separate aggregated effect size was calculated for food insecurity (FI), as the evidence of an association between FI and child weight outcomes is generally weaker than for income and SES-based measures of poverty (Gundersen, Lohman, Eisenmann, Garasky, & Stewart 2008). Five effect sizes from five different samples were included in the FI→weight pathway, all but one of which overlapped with the samples included in the poverty→weight pathway (i.e., five studies tested the associations between both income and weight and FI and weight separately). Of the five studies that tested relationships between exposure to FI and child weight, the average effect size was .07 (with r’s ranging from −.15 − .16). One study (Coley & Lombardi 2012, described above) found that early childhood FI was associated with lower rates of overweight and obesity in middle childhood (r = −.15). Three other studies found that FI was associated with higher weight in early childhood with an association of r ≥ .10. For the studies that also tested the association between poverty and weight (Bhargava, Jolliffe, & Howard 2008; Coley & Lombardi 2012), the direction and strength of the association between FI and weight were quite similar as they were for the association between poverty and weight.
Timing of exposure to poverty and weight outcome by developmental period.
In estimating effect sizes by age at which the weight outcome was measured, poverty was most strongly related to weight when weight was measured in adolescence (r = .15, n = 5), versus weight in early (r = .04, n = 7) and middle childhood (r = .07, n =14). However, none of the differences between the magnitudes of the correlation coefficients were statistically significant (z = .08, ns and z = .15, ns, for adolescence versus early childhood and adolescence versus middle childhood, respectively).
Two samples out of the seven that tested the association between poverty exposure and BMI measured in early childhood found an effect size where r ≥ .10 for the association between the two variables. Two studies used the ECLS-B, a large, representative U.S. dataset . Researchers assessed risk for overweight/obesity at age 2 (Gibbs & Forste 2014) and age 4–5 (Williams et al. 2018) by SES at birth, both finding effect sizes of small magnitude; averaged across the two studies, the effect size for this sample was r = .12. Although Gibbs and Forste found that family SES at 9 months was associated with obesity at age 2, infant feeding practices (i.e., being formula-fed and early introduction to solid foods) were a powerful mediator in this relationship. Another study using a very large sample of children across the U.S. found that lower income tertile measured when infants were 2–4 months was associated with higher risk of being in the 90th or 95th percentile of weight-for-length (a measure similar to BMI that is appropriate for infants from birth to age 2) at age 2 (Strobino et al. 2016).
It should be noted that for a majority of studies that tested exposure to poverty in early childhood (n = 20), it was not possible to assess differences in the strength of associations depending on when exposure to poverty occurred.
Summary of literature testing associations between poverty and child weight.
The overall average effect size for the pathway from poverty to child weight was small (r = .09). However, for 14 studies using 14 independent samples, the effect size was greater than r = .10, compared with nine studies where r < .10. None of the studies using a predominantly low-income sample (n = 6) found evidence for an association between poverty and weight in the expected direction. Of the studies that used a non-U.S. sample, a slight majority did not find evidence for an association between poverty and child weight. The average effect size was the strongest (r = .15) for studies that tested the relationship between poverty and weight when weight was measured in adolescence. There was no evidence that the relationship between FI and weight differed from the relationship between poverty and weight.
Longitudinal research linking poverty to childhood self-regulation
SR as a mediator in the poverty to obesity pathway.
Although other potential mechanisms are certainly involved in the pathway from poverty to child weight, SR was selected as the focus of this review because there are relatively rich literatures on 1) poverty predicting SR and 2) SR predicting child weight. In addition, SR may be more malleable than other mediators that have proven resistant to change in earlier trials (e.g., diet, physical activity) (Webster Stratton, Jamila Reid, & Stoolmiller 2008).
Similar to the poverty to weight pathway reviewed above, the review included studies in which authors primarily sought to test relationships between poverty and child SR. Also included were studies where the research question was not specifically about relations between poverty and SR, but about some other independent variable (e.g., maternal depression, family structure) and SR, with SES or family income included as a covariate in analyses.
Results of aggregated effect size analysis for longitudinal associations between poverty exposure and SR.
Searching PubMed and PsycINFO with the terms listed above for the poverty→SR pathway yielded 842 articles. Of those, 95 were found to meet criteria for inclusion in the review. Forty-one studies already reported effect size information in the paper. For 22 studies, authors were emailed to obtain this information. Of those, 15 provided data on effect sizes. Thirty-seven unique samples were represented in the effect size aggregation analysis; an additional 19 papers used an already included sample. Thus, for these already-included samples, effect sizes were averaged across these multiple studies. Twenty-four papers were from duplicate samples where the effect size was not available in the manuscript (e.g., the Family Life Project, n =10; ECLS-K, n = 2, the Early Head Start Research and Evaluation Project, n = 2).
Effect sizes for all but two of the studies in the poverty→SR pathway were already in the form of r and did not need to be converted. A total r for the association between poverty and SR was calculated. When a study tested hot, cool, and questionnaire-measured SR (or any combination of two or three of these), the highest of the r’s for any one measure was used to represent the total. The total average effect size for the longitudinal association between poverty and SR was r = −.16. As in the poverty→weight pathway, studies that had effect sizes of r ≥ .10 were tabulated. Out of the 37 effect sizes from the 37 unique samples, 28 exceeded that threshold with effect sizes of r ≥ .10 in the expected direction (i.e., greater poverty associated with lower SR) (see Tables 4 and 5).
Table 4.
Studies with a negative relationship and effect size ≥ .10 for poverty-self-regulation (SR) pathway
| Author | Sample | SR classification | r (total) |
|---|---|---|---|
| Wanless (2011) | Community sample, N = 95 | Cool | −.26 |
| McClelland (2012) | Community sample, N = 34 | Cool | −.29 |
| Brown (2013) | Sample from PA Head Start, N = 205 | Cool | −.11 |
| Nesbitt (2013) | Durham Child Heath & Development Study, N = 206 | Cool | −.23 |
| Sturge-Apple (2015) | Community sample, N = 140 | Hot | −.24 |
| Lengua (2007) | Community sample, N = 70 | Questionnaire | −.26 |
| Lengua (2006) | Community sample, N = 120 | Questionnaire | −.22 |
| Thompson (2013); Tandon (2015), Lengua (2013; 2014; 2015) | Community sample, N = 306 | Hot; Cool | −.24 |
| Doan (2012) | Community sample, N = 265 | Cool; Questionnaire | −.31 |
| Sektnan (2010); Crook (2014); Dilworth-Bart (2007); Nievar (2014); Blums (2017); Pratt (2016) | NICHD SECCYD, N’s range from 10091364 | Hot; Cool; Questionnaire | −.26 |
| Conradt (2014) | Maternal Lifestyle Study, N = 1121 | Physiological | −.10 |
| Moilanen (2010) | Early Steps Study, N = 731 | Questionnaire | −.13 |
| King (2013) | Community sample, N = 214 | Questionnaire | −.17 |
| Bernier (2010; 2015); Rochette (2014) | Canadian community sample, N’s range from 60–114 | Hot; Cool; Questionnaire | −.27 |
| Suor (2018) | Community sample, N = 160 | Hot; Cool; Questionnaire | −.21 |
| Berry (2014); Vernon-Feagans (2016); Gueron-Sela (2018); Sulik (2015) | Family Life Project, N’s range from 1037–1235 | Cool; Questionnaire | −.26 |
| Bockneck (2014); Mistry (2010); Brophy-Herb (2013) | Early Head Start Research & Evaluation Project, N’s range from 1258–1851 | Cool; Questionnaire | −.16 |
| Peredo (2015) | Community sample, N = 100 | Hot | −.19 |
| Kidwell (2007) | Community sample, N = 56 | Questionnaire | −.27 |
| Sabol (2018) | National Center for Research on Early Childhood Education study, N = 211 | Cool | −.15 |
| Wade (2018) | Healthy Babies Healthy Children (Canada), N = 501 | Cool | −.13 |
| Eisenberg (2010) | Community sample, N = 209 | Hot; Questionnaire | −.18 |
| Gartstein (2013) | Community sample, N = 147 | Cool | −.13 |
| Martoccio (2014) | Sample from MI Head Start, N = 127 | Cool | −.12 |
| Hartanto (2018) | ECLS-K | Cool; Questionnaire | −.19 |
| Bassett (2012) | Community sample, N = 261 | Hot; Cool | −.15 |
| Evans (2005) | Community sample, N = 329 | Questionnaire | −.29 |
| Abenavoli (2015) | Community sample N = 207 | Cool; Questionnaire | −.15 |
Table 5.
Studies with a negative relationship or effect size < .10 for poverty-SR pathway
| Author | Sample | SR classification | r (total) |
|---|---|---|---|
| Brown (2013) | Sample from PA Head Start; N = 205 | Questionnaire | .05 |
| Roy (2014a; 2014b); Raver (2013) | Chicago School Readiness Project; N’s range from 391–602 | Cool; Questionnaire | −.07 |
| Choi (2016) | Sample from OK Early Head Start/Head Start; N = 169 | Cool | −.03 |
| Marcovitch (2015) | Community sample; N = 226 | Cool | −.08 |
| Razza (2010) | Fragile Families; N = 1046 | Cool | −.07 |
| Degol (2015) | Community sample; N = 216 | Hot | −.06 |
| Pearce (2016) | UK Millenium Cohort Study; N = 5107 | Questionnaire | −.05 |
Association between exposure to poverty on hot, cool, and questionnaire-based measures of child SR.
Separate rs were then calculated to compare the effect sizes for the associations between poverty and each type of SR (hot, cool, questionnaire-based). When the SR variable used in a study was a composite of both observed and questionnaire measures, it was classified as questionnaire-based. In addition, if there was one sample that tested more than one type of SR in different studies or in the same study, effect sizes for each were included in this analysis. As an example, of the six studies that used the NICHD SECCYD sample and had an effect size included in the original paper, Crook and Evans (2014), Dilworth-Bart, Khurshid, and Vandell (2007), and Blums, Belsky, Grimm, and Chen (2017) all tested associations between poverty and cool SR, as measured by the Tower of Hanoi task (Blums et al. 2017; Crook & Evans 2014) and the Continuous Performance Test (Dilworth-Bart et al. 2007). The aggregated effect size for cool SR was calculated using an average of the rs from these three studies. Two of the studies (Blums et al. 2017; Nievar, Moske, Johnson, & Chen 2014) tested associations with hot SR using a delay task, and the hot SR aggregated effect size was calculated as the average from these two papers.
In comparing the magnitude of the aggregated effect sizes for the three types of SR, all were comparable to one another. For studies that tested the relationship between poverty and cool SR (n = 21), r = −.14; for poverty and hot SR (n = 11), r = −.13; and for poverty and questionnaire-based SR (n = 19), r = −.17. A Fisher’s z test indicated that none of the correlation coefficients were significantly different from one another. Although more studies used cool SR measures than hot, there was little evidence to indicate that the strength of the relationship between poverty and SR was weaker when hot SR measures were used.
Features of the sample and measurement of poverty.
Most studies used income-based measures of poverty. Of the eight studies from six independent samples that used a cumulative risk index that included a measure of poverty (Bocknek, Brophy-Herb, Fitzgerald, Schiffman, & Vogel 2014; Brophy-Herb, Zajicek-Farber, Bocknek, McKelvey, & Stansbury 2013; Chang, Shelleby, Cheong, & Shaw 2012; Conradt et al. 2014; Doan, Fuller-Rowell, & Evans 2012; Lengua, Honorado, & Bush 2007; Mistry, Benner, Biesanz, Clark, & Howes 2010; Wade et al. 2018), only Wade and colleagues used an observed measure of child SR, with the other studies using questionnaires. Using a relatively large Canadian sample, Wade and colleagues (2018) found that a cumulative risk index (including variables such as maternal depression and single parenthood along with low family income) in early infancy was associated with lower children’s cool SR (as measured by tasks that tested inhibitory control—the Bear/Dragon and cognitive flexibility—the Dimensional Change Card Sort) at age 3 (r = −.13).
Fifteen studies (not including duplicate samples) used predominantly low-income samples. The Family Life Project, a longitudinal study of children born in low-income, rural counties in North Carolina and Pennsylvania, was one such sample that was used in four different studies included in the aggregated effect size analysis. Using this sample, researchers consistently found an association between early childhood income (when children were 0−3 years) and SR, also measured in early childhood. The observed SR battery included multiple tasks assessing several aspects of cool SR, including working memory, attention shifting, and inhibitory control (Berry et al. 2014; Gueron-Sela et al. 2018; Sulik et al. 2015; Vernon-Feagans, Willoughby, & Garrett-Peters 2016); teachers also reported on children’s “behavioral regulation” in kindergarten (Vernon-Feagans et al. 2016). To determine whether the magnitude of effect sizes was comparable, an aggregated effect size was calculated for the association between poverty and SR for low-income (n = 15) versus representative samples (n = 22). The magnitude was stronger for representative samples (r = .18 versus r = .13), but not significantly so (z = .14, ns).
Child age.
The majority of studies (n = 27) tested the outcome of SR in early childhood, usually starting at preschool-age (i.e., age 3–4), with just three studies using SR measured in adolescence as a final outcome (Doan, Fuller-Rowell, & Evans 2012; Evans, Gonnella, Marcynyszyn, Gentile, & Salpekar 2005; King, Lengua & Monahan 2013). The study that used the earliest outcome measure for SR, at age 18 months, was the only one of all 37 studies in the analysis for which the effect size was in the opposite of the expected direction (i.e., higher poverty associated with higher SR, r = .13). In this study, Gartstein, Bridgett, Young, Panksepp, and Power (2013) found that income in early infancy was negatively associated with parent-reported SR at 18 months using the effortful control subscale from a measure of early childhood temperament; maternal parenting stress was positively associated with effortful control.
Many studies, however, found significant associations for the association between poverty and child SR when children were as young as 3 and 4 years old (e.g., Lengua et al. 2007; Sektnan, McClelland, Acock, & Morrison 2010; Sturge-Apple et al. 2016). As an example, Thompson and colleagues (2013), Tandon, Thompson, Moran, and Lengua (2015), and Lengua in three different studies (Lengua et al. 2014; Lengua et al. 2015; Lengua, Zalewski, Fisher, & Moran 2013) all used the same economically representative community sample to test associations between age 3 income and both hot and cool measures of child SR assessed four times at nine-month intervals. In all studies, researchers found significant associations between income and both hot and cool SR, with hot SR measured with a gift delay task and cool SR measured using a battery that included verbal inhibitory control and cognitive flexibility tasks. Importantly, Lengua and colleagues (2014) found that the effect of income on both types of SR was primarily explained by parenting variables (e.g., scaffolding, limit-setting).
Effect of poverty on physiological SR.
Very few studies examined direct effects of poverty or poverty-related stressors on children’s parasympathetic nervous system functioning, often assessed using respiratory sinus arrhythmia (RSA). Baseline RSA is thought to provide an indication of physiological SR while at rest, and higher RSA is usually associated with more optimal health and behavior outcomes (Propper 2012). Children’s RSA is known to be vulnerable to several types of environmental stressors, such as adolescents’ exposure to early life adverse events (Daches et al. 2017). Only one study was found that assessed the longitudinal relation between poverty and/or cumulative risk and RSA. Researchers found that a cumulative risk index (which included poverty) from birth to age 3 was associated with less RSA reactivity and less growth in reactivity from ages 3 to 6 (Conradt et al., 2014). This finding is opposite of what was expected, as greater RSA reactivity is typically associated with negative outcomes. However, by age 6, researchers found that there was a significant, positive association between early cumulative risk and RSA reactivity in the expected direction, indicating that perhaps there is a “latent” effect of early adversity on physiological regulation.
Effect of food insecurity on SR.
Only one study was found that tested the association between child FI and SR longitudinally. Using the ECLS-K dataset, Grineski, Morales, Collins, and Rubio (2018) found evidence for a small, negative association between FI in kindergarten and SR one year later, as measured by teacher report (r = −.07) and observed cool SR (using a working memory test and the Dimensional Change Card Sort test, which tests cognitive flexibility, r = −.10).
Summary of research linking poverty exposure to child SR.
Overall, exposure to poverty and poverty-related risk was associated with lower SR, with several studies indicating that the association between poverty and diminished SR may be detected at as early as age 3 or 4. The majority of the literature focused on cool rather than hot SR as an outcome, but there was no evidence that the association with poverty was stronger for cool SR. More research is needed to understand more about the effect of poverty on physiological SR and the effect of food insecurity on SR in general.
Longitudinal research linking self-regulation to childhood weight
The final pathway in the proposed model focuses on SR as a predictor of child weight. In this model, SR is thought to mediate the effects of poverty on child weight, and thus in the following section SR is discussed specifically as a variable that predicts child weight outcomes.
Longitudinal research on SR to child weight: Measurement and Overview.
Measures of SR in relation to weight tended to resemble those used in studies unrelated to eating or weight. However, there are some domain-specific measures used to measure SR specifically related to food intake. One example is the Eating in the Absence of Hunger (EAH) paradigm. In EAH tasks, children are usually first provided with a standardized meal. When children report that they are full, they begin a “free-access” session in which they are allowed to eat as much as they would like from an assortment of palatable sweet and savory snacks. The amount of snacks that they eat is then recorded, with children who consume fewer calories in the absence of hunger assumed to be better at self-regulating their caloric intake. In addition to the EAH protocol, there are also some questionnaire measures that assess child SR regarding eating behaviors (e.g., Children’s Eating Behavior Questionnaire (CEBQ); Wardle, Guthrie, Sanderson & Rapoport 2001).
The extent to which domain-specific eating SR tasks are associated with more global measures of SR remains unclear, with some studies finding associations between EAH and traditional SR measures (Tan & Holub 2010) and others not finding evidence of this association (Leung et al. 2014). Interestingly, Hughes and colleagues (2015) found a significant correlation between EAH and a food DoG task in low-income preschoolers in an unexpected direction, with greater SR in the food DoG task associated with more calories consumed in the absence of hunger. They also found that only eating-specific SR tasks or questionnaires (EAH, parent-reported satiety and food responsiveness on the CEBQ) were concurrently associated with BMI, while domain-general hot (food DoG, gift delay) and cool (tapping task, flexible item selection task) SR tasks having no significant relation. In addition, a cross-sectional study found that for preschoolers, eating more in the absence of hunger was associated with greater BMI, while waiting time on a food DoG task was not (Power et al. 2016). Together these studies suggest that domain-specific food SR tasks may measure different aspects of child SR in relation to eating behavior than traditional hot and cool SR tasks.
Results of aggregated effect size analysis for longitudinal associations between SR and weight.
Searching PubMed and PsycINFO with the terms listed above for the poverty→weight pathway yielded 1131 articles. Of those, 33 were found to meet criteria for inclusion in the review. Twelve studies already included effect size information in the paper. For 13 studies, authors were emailed to obtain this information. Of those, six provided effect size information. Seventeen unique samples were represented in the effect size aggregation analysis. Two additional papers that reported a correlation coefficient used a duplicate sample (in both cases, the sample was drawn from the NICHD study). Five other papers were from duplicate samples where the effect size did not appear in the manuscript.
The total average affect size was calculated in the same manner as for the poverty→SR pathway, with the highest of the rs for any one measure of SR (i.e., hot, cool, or questionnaire-based) used to represent the total. The total aggregated affect size for the SR→weight association was r = −.13, with greater SR associated with lower weight. Thirteen out of the 17 unique samples had an effect size of r ≥ .10 (see Tables 6 and 7).
Table 6.
Studies with a negative relationship and effect size ≺ .10 for self-regulation (SR)weight pathway
| Author | Sample | SR classification | r (total) |
|---|---|---|---|
| Graziano (2010) | Community sample; N = 57 | Cool; Hot | −.14 |
| Anzman (2009) | Community sample; N = 197 | Questionnaire | −.30 |
| Evans (2012) | Community sample; N = 244 | Hot (food) | −.21 |
| Mallan (2014) | Community sample; N = 37 | Questionnaire (appetite-specific) | −.38 |
| Graziano (2013) | Community sample; N = 195 | Hot | −.19 |
| Francis (2009); Seeyave (2009); Bub (2016) | NICHD; N’s range from 8051061 | Hot (food); Cool; Questionnaire | −.14 |
| Duckworth (2010) | Community sample; N = 105 | Questionnaire/Observed composite | −.22 |
| Tandon (2015) | Community sample; N = 306 | Hot; Cool | −.10 |
| Steinsbekk (2015) | Sample from Norway; N = 687 | Questionnaire (appetite-specific) | −.21 |
| Asta (2016) | Sample from MI Head Start; N = 209 | Eating in the Absence of Hunger task | −.11 |
| Parkinson (2010) | Gateshead Millenium Study (UK); N = 583 | Questionnaire (appetite-specific) | −.15 |
| Carter (2012) | Longitudinal Study of Child Development in Quebec, N = 1566 | Questionnaire (appetite-specific) | −.41 |
Table 7.
Studies with a negative relationship and effect size < .10 for self-regulation (SR)weight pathway
| Author | Sample | SR classification | r (total) |
|---|---|---|---|
| Anderson (2017) | Millenium Cohort Study; UK, N = 10,955 | Questionnaire | .05 |
| Piche (2012) | Longitudinal Study of Child Development in Quebec; N = 966 | Questionnaire | .04 |
| Stautz (2016) | Avon Longitudinal Study (UK); N = 6069 | Cool; Questionnaire | −.02 |
| Fogel (2018) | Growing up in Singapore Towards Healthy Outcomes; N = 158 | Eating in the Absence of Hunger task | −.05 |
| Bergmeier (2014) | Australian Research Council Discovery Grant Study; N = 201 | Questionnaire | .05 |
| Datar (2018) | ECLS-K; N = 7070 | Questionnaire | −.07 |
Type of self-regulation and longitudinal associations with weight.
Again, a correlation coefficient for the association between each type of SR (cool, hot, questionnaire) and later weight was calculated. Of the four studies that tested the relationship between cool SR and child weight, the average r = −.04, with just one study finding an association in which r ≥ .10. Of the studies that evaluated associations between hot SR and child weight, all seven r’s were ≥ 10 and the average effect size was r = −.14. In one study that tested multiple types of SR (hot, cool, and questionnaire-based) within the same large sample (NICHD), researchers used a single SR factor comprised of five indicators (hot, cool, and questionnaire-based, all measured at age 4) and found that higher SR predicted lower BMI at three different ages (8, 11, and 15) (Bub, Robinson, & Curtis 2016). In addition, researchers found that SR accounted for more of the variance in BMI when children were older. However, in considering the bivariate correlations between each SR indicator and BMI averaged across the three ages, the strongest relations were for hot SR (measured with a food DoG task) and the questionnaire measure (parent report of inhibitory control and attention focusing), r = −.10 and r = −.09, respectively, while the association between cool SR (measured with a Stroop and Continuous Performance Test) and average BMI was relatively lower (r = −.03).
A total of 11 studies analyzed questionnaire-based measures of SR in relation to child weight, with an aggregated effect size of r = −.14. Of those, eight used questionnaires that reported on general aspects of child SR (e.g., Children’s Behavior Questionnaire; Rothbart et al., 2001), and three used eating-specific questionnaires. The average effect size for questionnaires that assessed eating-specific behaviors was r = −.25, whereas for questionnaires that assessed SR broadly, r = −.07. All three of the studies that used eating-specific questionnaires used the CEBQ: some, but not all of the eight scales that comprise the CEBQ assess children’s SR of eating (e.g., emotional over-eating, satiety responsiveness).
Of the two studies that used an EAH task to predict later BMI, one study found some evidence for an association (Asta et al. 2016), while the other did not (Fogel et al. 2018). Asta and colleagues (2016), using a predominantly low-income sample, tested EAH twice in very early childhood (21 and 27 months) and BMI when children were 33 months. The association between 33-month BMI and EAH at 27 months was much stronger than for EAH at 21 months. Asta and colleagues note that in their study the number of calories consumed in the absence of hunger increased with age, particularly for sweet foods, supporting some prior research indicating that children’s eating SR declines with age (Johnson & Taylor-Holloway 2006). However, Fogel and colleagues’ (2018) study focused on a group of children in Singapore who were slightly older, with an EAH task at age 4 used to predict age 6 BMI, and did not find an association between EAH and BMI.
Developmental Timing.
In estimating effect sizes by age at which the weight outcome was measured, overall SR (i.e., not separated by SR type) was most strongly related to weight when measured in adolescence (r = −.18, n = 5), versus measuring weight in early (r = −.10, n = 6) and middle childhood (r = −.11, n =6). None of the differences between the magnitudes of the correlation coefficients were statistically significant (z = .09, ns and z = .08, ns, for adolescence versus early childhood and adolescence versus middle childhood, respectively).
Most studies (n = 13) measured SR beginning in early childhood. Six studies measured weight through adolescence and found significant effects for the relation between SR measured in early/middle childhood and adolescent weight. The association between SR measured in early childhood on adolescent weight was established using both observed (Francis & Susman 2009) and questionnaire measures of SR (Anzman & Birch 2009).
Effects of SR-Promoting Interventions on Child Weight.
Three studies were reviewed that used a weight loss intervention that included an SR component and measured SR pre- and post-treatment (see Table 8). One evaluated the effect of a general SR-building intervention as part of an obesity prevention program for low-income preschoolers (Lumeng et al. 2017) and two tested a weight loss intervention for obese children ages 8–13 (Israel, Guile, Baker, & Silverman 1994) and 8–14 (Verbeken, Braet, Goossens, & Van der Oord 2013).
Table 8.
SR-Promoting Weight Intervention Studies
| Author | Sample | Intervention | Intervention effects on SR | Intervention effects on weight |
|---|---|---|---|---|
| Lumeng (2017) | N=697 Head Start preschoolers | Preschool Obesity Prevention Series (POPS) vs. POPS + Incredible Years Series (IYS) vs. Head Start (HS) only | HS+POPS+IYS group had improvements in teacher-reported SR compared to both other groups (r = .21 for HS+POPS+IYS vs. HS+POPS) | No effect of intervention on obesity at the end of academic year (r = .01) |
| Israel (1994) | N=34 obese children age 9–13 | Standard treatment (ST) vs. Enhanced Child Involvement (ECI), including training in self-management skills | ECI associated with lower parent and teacher-reported SR (average r = −.19) but higher child-reported SR (r = .16) | At 3-year follow-up, ECI associated with lower % of overweight children compared to ST (r = .30) |
| Verbeken (2013) | N=44 obese Dutch children age 8–14 in an inpatient treatment program | Executive Functioning (EF) training vs. care as usual | Better weight loss maintenance in EF-training group 8 weeks post-intervention, but not maintained through 12-week f/u (r = .05 for 12-week f/u) | Improvements in cool SR (Corsi Block Tapping task) associated with EF-training group (r = .20). Increased deficits in working memory and metacognition subscales of teacher-reported BRIEF for the control group while EF-training group remained stable (r = .27) |
An effect size (d) for the effect of each intervention on SR and weight was calculated and then converted to r to be consistent with the effect size measures used for the other associations. The total aggregated effect size for the effect of the interventions (N = 3) on SR was r = .13 in favor of the SR intervention. For two of the three intervention studies (Lumeng et al. 2017; Verbeken et al. 2013), there was some evidence that the intervention promoted children’s SR, as measured by questionnaires. Only Verbeken and colleagues (2013) used an observed SR measure to investigate changes in SR during the intervention period, finding that the intervention was associated with increases in cool SR (r = .20). Israel and colleagues (1994), using parent, teacher, and child report of SR, did not find consistent associations between the intervention, which included training in child self-management and SR, and improvements in child SR; in fact, averaging across parent, teacher, and child reports, greater SR improvements were demonstrated in the comparison group (average r = −.10, ns).
For calculating the aggregated effect size for the effect of the interventions on child weight, if there were multiple follow-up assessments of weight, the final outcome for weight was used. The average r was .12 for the effect of the interventions on child weight compared to the control group, with one study finding an effect on weight and the other two studies having no or minimal effect on weight change. Israel and colleagues (1994) found that their “enhanced child involvement” intervention was associated with a lower proportion of children who were overweight at three years post-treatment compared to the standard treatment group (r = .30). Interestingly, as noted above, Israel and colleagues (1994) did not find any effect of the intervention on SR, suggesting that the effects of the intervention on child weight at follow-up were operating through a mechanism other than improvements to children’s SR. For the other two intervention studies, there was no evidence to suggest a meaningful effect of SR training on weight loss or weight loss maintenance.
Summary.
The aggregated average effect size from SR to child weight was in the “small” range (r = −.13) and comparable to the magnitude of the correlation coefficients for the other two pathways. There was some evidence that hot SR is a stronger predictor of later weight than cool SR, with hot SR more commonly tested. Of the different measures of SR, there was also some evidence that eating-specific questionnaires were more predictive of later weight than domain-specific SR questionnaires, but only three studies used this measure. There was little evidence that SR-focused obesity prevention or intervention programs help reduce child weight, but only three studies were found that tested a child weight intervention and also measured SR.
Discussion
Synthesis of Literature and Presentation of Updated Model
At the outset of this review, it was proposed that child SR might be one explanatory mechanism by which poverty influences children’s weight outcomes. In each of the pathways of interest, effect sizes were in expected direction, albeit in the “small” range, with r = .09 (poverty→weight), r = −.16 (poverty→SR), and r = −.13 (SR→weight).
Although the aggregated effect size for the pathway from poverty to weight was particularly small, it is comparable to the effect sizes that previous systematic reviews and/or meta-analyses have established for other risk factors of child obesity. Examples include the following: maternal smoking during pregnancy and child overweight: OR = 1.5 (equivalent to r = .11) (Oken, Levitan, & Gillman 2008); breast-feeding and child obesity: OR = .78 equivalent to r = .07 (Arenz, Rückerl, Koletzko, & von Kries 2004); and TV viewing and child body fat: r = .07 (Marshall, Biddle, Gorely, Cameron, & Murdey 2004).
For the pathway from poverty to SR, the effect size found in the current review (r = −.16) was identical to one found in a recent meta-analysis on the association between SES and behavioral executive functioning tasks (i.e., observed cool SR) (Lawson, Hook, & Farah 2018). There was minimal overlap of the studies include in both analyses -- of the 25 unique samples in their meta-analysis and the 37 in the effect size analysis in the current review, only four samples overlapped. Lawson, Hook, and Farah’s meta-analysis also included education and occupation-based measures of SES and was not limited to longitudinal studies.
Although to our knowledge no other systematic reviews or meta-analyses have been conducted on the relationship between SR and weight in children, a recent meta-analysis of the association between behavioral task and questionnaire measures of impulsivity and adult BMI also found evidence for a small but significant effect size (r = .07) (Emery & Levine 2017).
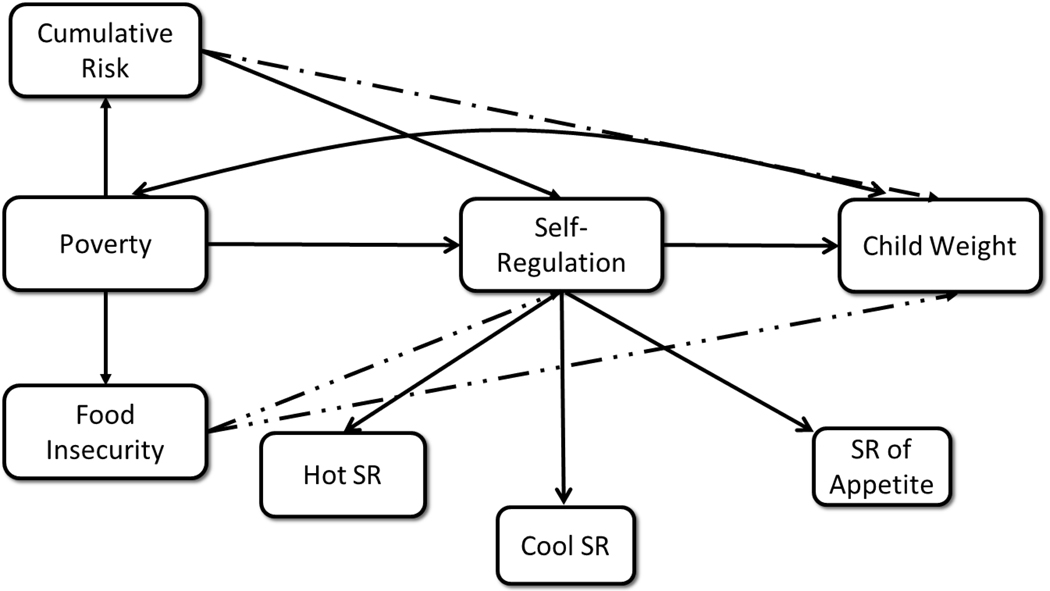
Based on the literature reviewed, Figure 1 represents a theoretical model depicting relationships among the variables of interest. The model includes both food insecurity and cumulative risk as variables related to poverty that may influence child weight. The dotted lines from FI to SR and child weight and from cumulative risk to child weight reflect that there is not yet enough evidence to suggest an association for these pathways and the need for more research examining these paths.
Figure 1.
Theoretical model of associations between poverty, SR, and child weight. * Dotted lines indicate that there is not yet enough evidence to suggest an association for these pathways and the need for more research examining these paths
Limitations of the Current Literature
Poverty to Weight.
The majority of studies reviewed in this pathway measured exposure to poverty during early childhood. Although there are compelling reasons to suspect that exposure to poverty in early childhood may be particularly harmful, such as early adversity impacting reactivity to stress (Shonkoff et al. 2012), it remains necessary to specifically test this assumption by comparing children’s exposure to poverty at various points in development in relation to later weight. It would be important to isolate the effects of poverty exposure during different developmental stages on child weight to determine the extent to which early poverty has unique effects on child BMI. Alternatively, more prospectively ascertained data are also needed to examine the cumulative effects of experiencing poverty across multiple developmental periods (e.g., early and middle childhood vs. early childhood through adolescence).
Poverty to SR.
A major limitation of the poverty to SR literature was that only three studies tested SR in adolescence. Moreover, few studies spanned multiple developmental periods. Therefore, it remains unclear whether early exposure to poverty continues to predict SR later in childhood and adolescence.
Prior research suggests that early exposure to poverty may be particularly detrimental for outcomes much later in development such as academic achievement and employment (Duncan & Magnuson 2013), but there is not yet enough evidence to indicate that this is also the case for SR.
Only one study evaluated the longitudinal relationship between FI and SR, using both teacher report and cool SR measures (Grineski et al. 2018). For developing a better understanding of the relationship between poverty and weight outcomes, it would be particularly interesting and important to test the relationship between FI and SR as measured by DoG tasks. When children are food insecure, they may not know exactly when their next meal might be, which could affect whether they are willing to wait for a bigger reward. Additionally, no studies were found that tested the longitudinal relationship between poverty or FI and eating-specific child SR, although a cross-sectional study found that children living in homeless shelters reported overeating as a coping strategy for FI (C. Smith & Richards 2008).
SR to Weight.
Surprisingly little research has tested the extent to which eating-specific SR measures, particularly EAH, predict later child weight or weight gain over time, with only one observational EAH study evaluating this association in early to middle childhood and three studies using parent report. It would be helpful to learn more about relationships between different types of SR, including EAH and hot/cool observed measures, and child weight longitudinally across developmental stages.
Self-Regulation across Literatures
A challenge of the proposed model that future research should address is the extent to which each type of SR (hot, cool, appetite-specific) is a viable candidate to mediate the association between poverty and weight. The current review revealed that although there is some overlap in how SR is conceptualized in relation to the poverty to SR and the SR to weight pathways, there are also important differences. In the poverty to SR pathway, more of the literature has focused on cool SR. The relatively greater emphasis on cool SR in most studies may be because of a greater emphasis in the literature of identifying possible mechanisms for the relationship between poverty exposure and academic achievement. As an example, some research suggests that cool SR, rather than hot, is more strongly associated with academic performance (Willoughby et al. 2011). In line with this explanation, for many of the studies that used exclusively cool SR measures, authors emphasized the importance of SR in the context of academic achievement (McClelland & Wanless 2012; Nesbitt, Baker-Ward, & Willoughby 2013; Thompson, Lengua, Zalewski, & Moran 2013; Wanless, McClelland, Tominey, & Acock 2011).
Conversely, researchers investigating the pathway from SR to weight have primarily used hot SR measures, with relatively little evidence for an association between cool SR and child weight. It could be that hot and cool SR differentially affect various aspects of weight regulation or that the relative influence of each changes throughout development. For example, hot SR might be a better predictor of weight during early childhood, and cool SR might become more important later in childhood (Metcalfe & Mischel 1999) when children become more responsible for their own nutritional choices. More studies are needed that evaluate the effect of poverty and/or cumulative risk on hot SR, and especially studies that compare how poverty affects cool versus hot SR. Few researchers across both literatures used the same questionnaire measures of SR, which could simply reflect the multitude of SR-related questionnaires that are available rather than differences in their usage across literatures. Neither poverty nor obesity researchers have sufficiently tested physiological SR (e.g., RSA) as an outcome or predictor, and poverty researchers also have not evaluated eating-specific SR as a potential outcome of low SES or poverty-related stress.
Global versus domain-specific SR.
Eating-specific SR has been limited to use as a predictor of child weight. No studies tested the influence of poverty on SR specific to eating or appetite (e.g., observed EAH, parent-reported overeating or eating too quickly). However, there are some theoretical reasons why an association between poverty and SR of eating might be expected. Prior research suggests that general exposure to stress (not specific to poverty-related stressors) may affect children’s eating behaviors (Michels et al. 2012), and that cortisol output in response to a lab-based stressor is associated with eating more in the absence of hunger (Francis, Granger, & Susman 2013). This may be an interesting and important area for future investigation.
Prior research demonstrates that correlations between EAH and more global SR tasks, even DoG with food, are not as strong as might be expected (Hughes et al. 2015). It may be that EAH primarily measures reward responsiveness, and a child could be responsive to reward (i.e., enjoy the pleasurable taste of food) while still being able to successfully delay with the promise of a better reward. Another possibility is that SR of eating in the context of an EAH task is more of an involuntary process and is tapping a different aspect of SR than those that require volitional inhibition (e.g., DoG tasks). It would be important for longitudinal studies to further explore how different aspects and measures of SR are affected by poverty and affect weight, particularly because eating-specific SR tasks have infrequently been used as a predictor of later weight in methodologically rigorous, longitudinal studies.
Feasibility of model with respect to SR interventions
One goal of the current review was to evaluate the existing evidence for an explanatory mechanism in the pathway from poverty exposure to child risk for obesity with the intention of identifying a potential target of intervention. Findings from a recent meta-analysis indicate that not only do SR-promoting interventions have beneficial effects on child SR, but also on more distal outcomes, including academic achievement and behavior (Pandey et al. 2018). With respect to weight specifically as an outcome, prior research indicates that early childhood interventions that implicitly or explicitly promote SR skills may be associated with healthier BMIs later in childhood (Brotman et al. 2012; J. D. Smith, Montaño, Dishion, Shaw, & Wilson 2015). However, these studies did not directly measure children’s SR, so it is unclear whether the association between the intervention and improvements in children’s weight was driven by improvements in child SR or some other variable (e.g., perhaps the intervention influenced parental food purchases).
Unfortunately, the few studies that have tested SR-specific interventions and monitored SR have not found particularly compelling evidence to suggest that they help treat or prevent obesity. Researchers in one recent study included in the present analysis (Lumeng et al. 2017) tested an SR intervention in a manner closely aligned with the model proposed in this review, adding a general SR component (the Incredible Years Series) to an obesity prevention program for low-income preschoolers in Head Start. There are a variety of possible explanations for why Lumeng and colleagues did not find evidence for an effect of the SR intervention on child weight. One possibility is that although interventions that target children’s global SR may be beneficial for improving hot/cool SR, a component specific to eating SR may be necessary for obesity prevention. Another possibility could be that children in the study were too young to benefit from an SR intervention for obesity prevention, as some literature suggests that younger children are better at self-regulating their energy intake than older children (Cecil et al. 2005). A third explanation is that effects of the SR intervention might have latent effects on BMI that may not be evident until later in development during “sensitive” periods, such as adiposity rebound (~age 7) and puberty. Lastly, it could be that SR-promoting interventions are most effective for those children with the lowest levels of SR at baseline, and that SR interventions may fail to demonstrate main effects on weight for the whole sample while still having a moderate effect on specific subsamples (e.g., children with low SR). Interestingly, both Brotman and colleagues’ (2012) and Smith and colleagues’ (2015) studies focused on youth with high levels of conduct problems, and conduct problems are associated with diminished SR. Testing eating-specific versus general SR interventions for obesity treatment and prevention for children at a variety of stages of development, as well as potential moderators of treatment efficacy are areas of research that future studies should systematically address.
There is an ongoing treatment study testing the effects of an SR-promoting intervention for obese 8–16-year-old children (Warschburger 2015), but findings are not yet available. The intervention, which will be compared to a no-treatment control condition, involves a computer program where children are taught to “push” high-calorie snacks away while learning to “approach” nutritious foods (e.g., vegetables), with the Stroop test being used to measure changes in SR throughout the intervention period. This trial could add to the existing literature by testing the efficacy of appetite-specific SR training on child weight reduction, whereas the three other treatment studies tested more general SR interventions.
Research suggests that SR specific to energy intake is modifiable (Johnson 2000). In a study that was not a controlled trial and that did not test weight as an outcome, Johnson found that after six weeks of an SR-promoting intervention, normal weight preschool children were better able to regulate their eating in an EAH task, indicating that eating-specific SR behaviors may be malleable starting from an early age. Using doll play and skits, the intervention modeled appropriate SR of eating and focused on identifying physiological hunger and satiety cues. However, no studies were found that specifically incorporated eating-specific SR training into an intervention and measured effects on both SR and weight. One study addressing this issue is currently ongoing, testing an intervention that focuses on promoting parents’ knowledge of eating SR for their children (Eneli et al. 2015).
Developmental Considerations
One of the aims of the current review was to determine whether effects of poverty and SR on weight are visible in early childhood, prior to adiposity rebound. There was some evidence that perhaps the relationship between poverty and weight is weaker prior to adiposity rebound (~age 5–7), with only two studies out of seven finding an effect size of greater than r = .10 when weight was measured in early childhood. Additionally, some prior research suggests that younger children are better at self-regulating their energy intake than older children (Johnson & Taylor-Holloway 2006), with the beginning of middle childhood sometimes cited as a time in which children become less adept at modulating their energy intake (Tsukayama, Toomey, Faith, & Duckworth 2010). Therefore, timing of measurement of SR of eating/appetite may be particularly important, as EAH tasks administered prior to the age of 7 may be less effective in predicting later adiposity. However, none of the studies in the current review tested EAH in middle childhood or adolescence. Randomized or quasi-experimental studies where exogenous income is provided to low-income families at various child ages could prove especially useful for better understanding the effect of developmental timing of poverty on child weight outcomes.
Feasibility and limitations of proposed model
One important limitation is that the proposed model does not consider the effect of poverty or poverty-related stressors on specific child biological factors that may affect weight. For example, there is some evidence to suggest that children’s exposure to chronic stress has consequences for metabolism (Pervanidou & Chrousos 2011). It could be that poverty has both metabolic consequences and affects child SR, but that it is the adverse effects on metabolism that drives the association between poverty and weight.
Another possibility that few studies have accounted for in the relationship between SR and weight is a genetic pathway. Perhaps there may a relationship between low SR and risk for overweight, but it is not a causal one, and both traits are inherited. For example, when Seeyave and colleagues (2009) included a proxy for maternal weight in their model, the longitudinal association between SR and BMI was significantly attenuated, which they attribute to “inherited disinhibition.” Future studies should investigate the heritability of SR of eating behaviors.
Inherent in the proposed model and the studies reviewed in the SR to child weight path is that SR promotes healthy weight because of SR in relation to eating and appetite. However, eating is one of two major components of child weight maintenance, with the other being physical activity. Although the relationship between SR and physical activity has been previously evaluated, usually the focus is on the SR-promoting effects of physical activity rather than SR being a necessary component for maintaining regular physical activity.
Limitations of the Current Study
A limitation of the current review is its focus on financial aspects of poverty (e.g., income-based measures) rather than social class (e.g., parental education, occupation). Studies were excluded from the review if the measure of “poverty” did not include some aspect of income or deprivation at the family or neighborhood level. Future researchers should prioritize education or social class-based measures of SES in the relationship to child SR and weight outcomes, as this was outside of the scope of this review.
Another major limitation of the current systematic review and effect size analysis is that many studies were not able to be included because no effect size was available. Also, particularly for the poverty to weight and poverty to SR pathways, there was a great deal of variability in the definition and measurement of poverty, which resulted in the exclusion of some studies that may indeed have important implications for understanding the relationship between poverty and later outcomes. For example, as described in the Methods section, studies were excluded if they tested trajectories of family income or chronicity of poverty because it would be inappropriate to combine these effect sizes with those that tested poverty exposure at a single assessment point. However, studies that identify trajectories of family income over time (e.g., by categorizing families as “upwardly mobile” or “downwardly mobile”) could be very helpful for identifying whether there are sensitive developmental periods during which child weight and SR are particularly vulnerable or malleable.
Another limitation is that, although we report the results from Fisher’s z tests assessing differences in correlation coefficients across different aspects of the studies (e.g., hot versus cool SR in relation to child weight, differences in strength of association between poverty and weight in early childhood versus adolescence), there was little power to detect these differences. For example, for the z test to be significant with a difference between correlation coefficients of .30 (an effect size of medium magnitude), there would need to be 60 studies in each group.
Future Directions
Future research must first determine whether there is sufficient evidence across multiple studies with diverse samples that SR mediates the relationship between poverty and weight. If the model does indeed seem viable, a next step would be to explore the possible implications for intervention. That is, by improving child SR, can the impact of early exposure to poverty on overweight/obesity be attenuated?
Poverty and Food Insecurity.
Future research should take advantage of quasi-experimental study designs where income was increased for some families but not others. For example, the effect of the Earned Income Tax Credit (EITC) on BMI has been tested in adults (Schmeiser 2009), but has not yet been evaluated in children. A quasi-experimental study where researchers evaluated the effect of a conditional cash transfer program on Mexican children’s BMI found evidence for a beneficial effect of income increases in reducing the prevalence of child overweight (Fernald, Gertler, & Neufeld 2008), although this study was not longitudinal.
More research on the impact of FI on child weight is necessary, with quasi-experimental studies having the potential to be particularly informative. Programs exist that could theoretically reduce children’s exposure to FI by providing additional nutrition. In fact, the USDA states that the Supplemental Nutrition
Assistance Program (SNAP) is “designed to reduce food insecurity,” and there is indeed some evidence that it does (Bhattacharya & Currie 2001). However, there is mixed evidence for the effect of SNAP on child obesity, with some research suggesting that it may be associated with an increase in obesity among certain populations, such as girls in middle childhood (Gibson 2004). Research by Schmeiser (2012), however, suggests that a family’s participation in SNAP is associated with a reduction in BMI and overweight/obesity for boys 518 and girls 5–11, but not girls from 12–18. Yet another study found that Head Start children whose families participated in SNAP were no more or less likely to show increases in BMI over one year (Simmons, Alexander, Ewing, & Whetzel 2012). However, none of these studies directly measured FI, so there is no way to know whether reductions in FI attributed to SNAP participation are driving effects on child weight. Future studies should evaluate the hypothesis that the effect of SNAP on child weight operates through reducing FI, which could be informative for further exploring a causal relationship between FI and weight.
Parenting.
A promising mediator to explore in addition to or alongside child SR in relation to weight may be parenting, as parenting behaviors are known to be affected by poverty (Kiernan & Mensah 2011; McLeod & Shanahan 1993) explain some of the relationship between poverty and SR (Lengua et al. 2014), and are predictive of child weight (Kakinami, Barnett, Séguin, & Paradis 2015). Few studies have assessed the association between poverty and parents’ feeding practices, although one cross-sectional study found an association between FI and restrictive/pressuring feeding style (Gross, Mendelsohn, Fierman, Racine, & Messito 2012). Similar to SR, parenting may be a promising mediator to explore, as it is known to be malleable to intervention (Dishion et al. 2008). No longitudinal studies have previously tested whether SR mediates the relationship between parenting and child weight, which would be an important area for future research.
Gender.
Although child gender was not tested as a moderator in the relationship between poverty and weight in the current analysis, several studies that were included in the review found some evidence that the association between poverty and overweight/obesity may be more pronounced for female children. More studies should test the moderating effect of gender, as it could be that the stronger relationship between poverty and weight observed for girls is driving what appears to be a general effect of poverty on obesity for all children. Child gender would be particularly important to consider as a moderator when the outcome for weight is in adolescence, as puberty impacts boys and girls dissimilarly at different ages.
Specificity of Outcome of Child Weight in Relation to Poverty/SR.
As SR is known to be associated with a variety of child outcomes, it is unclear the extent to which the proposed model would be specific to child weight as an outcome, or whether one of several other outcomes (e.g., behavior problems, academic achievement, delinquency) could replace it. Future research should test this possibility.
Obesity is known to be comorbid with attention deficit hyperactivity disorder (ADHD) (Cortese et al. 2008; Cortese & Castellanos 2014), perhaps because of similar underlying mechanisms of difficulties with SR. One interesting question for future research might be to assess whether ADHD treatment, which should improve attention and impulsivity, also has a beneficial effect on child weight. Some research suggests that children medicated for ADHD have reduced risk of obesity compared with children with ADHD who are not taking medication (Kim, Mutyala, Agiovlasitis, & Fernhall 2011; Waring & Lapane 2008). However, it is important to note that another study failed to replicate this effect (Byrd, Curtin, & Anderson 2013), and in none of these studies were children randomly assigned to ADHD medication treatment. Another potential confound is that simulant medication is known to suppress appetite, so this could be driving the protective effects on weight rather than improvements to SR. The effect of psychosocial, nonstimulant ADHD treatment on child weight, potentially mediated by improvements to SR, would be an interesting area for further research.
Conclusions
Findings from the studies included in the current review suggest meaningful associations between poverty and child SR and between SR and child weight. However, more research is warranted to better understand specific factors that might underlie the association between poverty and child weight, especially based on the potential implications for prevention and treatment. Although SR may be a promising potential target for obesity intervention for low-income children, additional research on how SR affects risk for obesity is crucial, especially based on the lack of success of the limited number of SR-promoting interventions for improving children’s weight outcomes. In particular, aspects of SR that have traditionally been limited to the obesity literature (i.e., eating-specific SR) need to be tested in the context of poverty. Different aspects of SR (i.e., hot, cool, physiological, eating-specific) should be tested in additional studies as mediators in the relationship between poverty and child weight, which will allow the weaknesses and limitations of the current model to be tested systematically before being incorporated into interventions. In addition, a focus on developmental status should be incorporated into future research on associations between poverty, SR, and child weight.
Footnotes
Compliance with Ethical Standards
Ethical approval: This article does not contain any studies with human participants performed by any of the authors.
References
- Abenavoli RM, Greenberg MT, & Bierman KL. (2015). Parent support for learning at school entry: Benefits for aggressive children in high-risk urban contexts. Early childhood research quarterly, 31, 9–18. doi: 10.1016/j.ecresq.2014.12.003 [DOI] [Google Scholar]
- Alaimo K, Olson CM, & Frongillo EA. (2001). Low family income and food insufficiency in relation to overweight in US children: is there a paradox? Archives of pediatrics & adolescent medicine, 155(10), 1161–1167. [DOI] [PubMed] [Google Scholar]
- Anderson S, Sacker A, Whitaker R, & Kelly Y. (2017). Self-regulation and household routines at age three and obesity at age eleven: longitudinal analysis of the UK Millennium Cohort Study. International Journal of Obesity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anzman SL, & Birch LL. (2009). Low inhibitory control and restrictive feeding practices predict weight outcomes. The Journal of pediatrics, 155(5), 651–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arenz S, Rückerl R, Koletzko B, & von Kries R. (2004). Breast-feeding and childhood obesity—a systematic review. International Journal of Obesity, 28(10), 1247. [DOI] [PubMed] [Google Scholar]
- Assari S, Thomas A, Caldwell CH, & Mincy RB. (2018). Blacks’ diminished health return of family structure and socioeconomic status; 15 years of follow-up of a national urban sample of youth. Journal of Urban Health, 95(1), 21–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asta K, Miller AL, Retzloff L, Rosenblum K, Kaciroti NA, & Lumeng JC. (2016). Eating in the absence of hunger and weight gain in low-income toddlers. Pediatrics, 137(5), e20153786. doi: 10.1542/peds.2015-3786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin JR, Arseneault L, Odgers C, Belsky DW, Matthews T, Ambler A, … Danese A. (2016). Childhood bullying victimization and overweight in young adulthood: A cohort study. Psychosomatic medicine, 78(9), 1094–1103. doi: 10.1097/PSY.0000000000000388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baptiste-Roberts K, Nicholson WK, Wang N-Y, & Brancati FL. (2012). Gestational diabetes and subsequent growth patterns of offspring: The national collaborative perinatal project. Maternal and Child Health Journal, 16(1), 125–132. doi: 10.1007/s10995-011-0756-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassett HH, Denham S, Wyatt TM, & Warren-Khot HK. (2012). Refining the Preschool Self-Regulation Assessment for use in preschool classrooms. Infant and Child Development, 21(6), 596–616. doi: 10.1002/icd.1763 [DOI] [Google Scholar]
- Bergmeier H, Skouteris H, Horwood S, Hooley M, & Richardson B. (2014). Associations between child temperament, maternal feeding practices and child body mass index during the preschool years: A systematic review of the literature. Obesity Reviews, 15(1), 9–18. [DOI] [PubMed] [Google Scholar]
- Bernier A, Beauchamp MH, Carlson SM, & Lalonde G. (2015). A secure base from which to regulate: Attachment security in toddlerhood as a predictor of executive functioning at school entry. Developmental Psychology, 51(9), 1177–1189. doi: 10.1037/dev0000032 [DOI] [PubMed] [Google Scholar]
- Bernier A, Carlson SM, Bordeleau S, & Carrier J. (2010). Relations between physiological and cognitive regulatory systems: Infant sleep regulation and subsequent executive functioning. Child Development, 81(6), 1739–1752. doi: 10.1111/j.1467-8624.2010.01507.x [DOI] [PubMed] [Google Scholar]
- Berry D, Blair C, Ursache A, Willoughby MT, Granger DA, & Family Life Project Key, I. (2014). Early childcare, executive functioning, and the moderating role of early stress physiology. Developmental Psychology, 50(4), 1250–1261. doi: 10.1037/a0034700 [DOI] [PubMed] [Google Scholar]
- Bhargava A, Jolliffe D, & Howard LL. (2008). Socio-economic, behavioural and environmental factors predicted body weights and household food insecurity scores in the Early Childhood Longitudinal Study-Kindergarten. British Journal of Nutrition, 100(2), 438–444. doi: 10.1017/S0007114508894366 [DOI] [PubMed] [Google Scholar]
- Bhattacharya J, & Currie J. (2001). Youths at Nutrition Risk: Malnourished or Misnourished? In Risky behavior among youths: An economic analysis (pp. 483–522): University of Chicago Press. [Google Scholar]
- Bleich SN, Segal J, Wu Y, Wilson R, & Wang Y. (2013). Systematic review of community-based childhood obesity prevention studies. Pediatrics, 132(1), e201–e210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blums A, Belsky J, Grimm K, & Chen Z. (2017). Building links between early socioeconomic status, cognitive ability, and math and science achievement. Journal of Cognition and Development, 18(1), 16–40. doi: 10.1080/15248372.2016.1228652 [DOI] [Google Scholar]
- Bocknek EL, Brophy-Herb HE, Fitzgerald HE, Schiffman RF, & Vogel C. (2014). Stability of biological father presence as a proxy for family stability: Cross-racial associations with the longitudinal development of emotion regulation in toddlerhood. Infant Mental Health Journal, 35(4), 309–321. doi: 10.1002/imhj.21454 [DOI] [PubMed] [Google Scholar]
- Braet C, Tanghe A, Decaluwé V, Moens E, & Rosseel Y. (2004). Inpatient treatment for children with obesity: weight loss, psychological well-being, and eating behavior. Journal of pediatric psychology, 29(7), 519–529. [DOI] [PubMed] [Google Scholar]
- Brophy-Herb HE, Zajicek-Farber ML, Bocknek EL, McKelvey LM, & Stansbury K. (2013). Longitudinal connections of maternal supportiveness and early emotion regulation to children’s school readiness in low-income families. Journal of the Society for Social Work and Research, 4(1), 2–19. doi: 10.5243/jsswr.2013.1 [DOI] [Google Scholar]
- Brotman LM, Dawson-McClure S, Huang K-Y, Theise R, Kamboukos D, Wang J, … Ogedegbe G. (2012). Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics, 129(3), e621–e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown ED, Ackerman BP, & Moore CA. (2013). Family adversity and inhibitory control for economically disadvantaged children: Preschool relations and associations with school readiness. Journal of Family Psychology, 27(3), 443. [DOI] [PubMed] [Google Scholar]
- Brown ED, & Sax KL. (2013). Arts enrichment and preschool emotions for low-income children at risk. Early childhood research quarterly, 28(2), 337–346. doi: 10.1016/j.ecresq.2012.08.002 [DOI] [Google Scholar]
- Brown T, & Summerbell C. (2009). Systematic review of school based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obesity Reviews, 10(1), 110–141. [DOI] [PubMed] [Google Scholar]
- Bub KL, Robinson LE, & Curtis DS. (2016). Longitudinal associations between self-regulation and health across childhood and adolescence. Health Psychology, 35(11), 1235–1245. doi: 10.1037/hea0000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdette HL, & Whitaker RC. (2007). Differences by race and ethnicity in the relationship between breastfeeding and obesity in preschool children. Ethnicity and Disease, 17(3), 467. [PubMed] [Google Scholar]
- Bush NR, Allison AL, Miller AL, Deardorff J, Adler NE, & Boyce WT. (2017). Socioeconomic disparities in childhood obesity risk: Association with an oxytocin receptor polymorphism. JAMA Pediatrics, 171(1), 61–67. doi: 10.1001/jamapediatrics.2016.2332 [DOI] [PubMed] [Google Scholar]
- Byrd HM, Curtin C, & Anderson SE. (2013). Attention- deficit/hyperactivity disorder and obesity in US males and females, age 8–15 years: National Health and Nutrition Examination Survey 2001–2004. Pediatric obesity, 8(6), 445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins SD. (2007). The emergence of self-regulation: Biological and behavioral control mechanisms supporting toddler competencies. Socioemotional development in the toddler years: Transitions and transformations, 261–284. [Google Scholar]
- Calkins SD, & Dedmon SE. (2000). Physiological and behavioral regulation in two-year-old children with aggressive/destructive behavior problems. Journal of abnormal child psychology, 28(2), 103–118. [DOI] [PubMed] [Google Scholar]
- Cameron AJ, Spence AC, Laws R, Hesketh KD, Lioret S, & Campbell KJ. (2015). A review of the relationship between socioeconomic position and the early-life predictors of obesity. Current obesity reports, 4(3), 350362. [DOI] [PubMed] [Google Scholar]
- Carper J, Fisher JO, & Birch LL. (2000). Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite, 35(2), 121–129. [DOI] [PubMed] [Google Scholar]
- Carter M, Dubois L, Tremblay M, Taljaard M, & Jones B. (2012). Trajectories of childhood weight gain: The relative importance of local environment versus individual social and early life factors. PloS ONE, 7(10). doi: 10.1371/journal.pone.0047065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecil JE, Palmer CN, Wrieden W, Murrie I, Bolton-Smith C, Watt P, … Hetherington MM. (2005). Energy intakes of children after preloads: adjustment, not compensation. The American journal of clinical nutrition, 82(2), 302–308. [DOI] [PubMed] [Google Scholar]
- Chang H, Shelleby EC, Cheong J, & Shaw DS. (2012). Cumulative risk, negative emotionality, and emotion regulation as predictors of social competence in transition to school: A mediated moderation model. Social Development, 21(4), 780–800. doi: 10.1111/j.1467-9507.2011.00648.x [DOI] [Google Scholar]
- Choi JY, Castle S, Williamson AC, Young E, Worley L, Long M, & Horm DM. (2016). Teacher-child interactions and the development of executive function in preschool-age children attending Head Start. Early Education and Development, 27(6), 751–769. doi: 10.1080/10409289.2016.1129864 [DOI] [Google Scholar]
- Cohen J. (1992). A power primer. Psychological bulletin, 112(1), 155. [DOI] [PubMed] [Google Scholar]
- Coleman-Jensen A, Gregory C, & Singh A. (2014). Household food security in the United States in 2013. Washington, D.C.: Economic Research Service. [Google Scholar]
- Coley RL, & Lombardi CM. (2012). Early maternal employment and childhood obesity among economically disadvantaged families in the USA. Early Child Development and Care, 182(8), 983–998. doi: 10.1080/03004430.2012.678594 [DOI] [Google Scholar]
- Collings PJ, Ball HL, Santorelli G, West J, Barber SE, McEachan RR, & Wright J. (2017). Sleep duration and adiposity in early childhood: Evidence for bidirectional associations from the Born in Bradford Study. Sleep, 40(2). doi: 10.1093/sleep/zsw054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conradt E, Abar B, Sheinkopf S, Lester B, Lagasse L, Seifer R, … Higgins R. (2014). The role of prenatal substance exposure and early adversity on parasympathetic functioning from 3 to 6 years of age. Developmental Psychobiology, 56(4), 821–835. doi: 10.1002/dev.21155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortese S, Angriman M, Maffeis C, Isnard P, Konofal E, Lecendreux M, … Mouren M-C (2008). Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Critical reviews in food science and nutrition, 48(6), 524–537. [DOI] [PubMed] [Google Scholar]
- Cortese S, & Castellanos FX. (2014). The relationship between ADHD and obesity: implications for therapy. Expert review of neurotherapeutics, 14(5), 473–479. [DOI] [PubMed] [Google Scholar]
- Crook SR, & Evans GW. (2014). The role of planning skills in the income–achievement gap. Child Development, 85(2), 405–411. doi: 10.1111/cdev.12129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daches S, Kovacs M, George CJ, Yaroslavsky I, Kiss E, Vetró Á, … Halas K. (2017). Childhood adversity predicts reduced physiological flexibility during the processing of negative affect among adolescents with major depression histories. International Journal of Psychophysiology, 121, 22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datar A, & Chung PJ. (2018). Childhood self-control and adolescent obesity: Evidence from longitudinal data on a national cohort. Childhood Obesity, 14(4), 238–247. doi: 10.1089/chi.2017.0217 [DOI] [PubMed] [Google Scholar]
- Dearing E, McCartney K, & Taylor BA. (2006). Within-child associations between family income and externalizing and internalizing problems. Developmental Psychology, 42(2), 237. [DOI] [PubMed] [Google Scholar]
- Degol JL, & Bachman HJ. (2015). Preschool teachers’ classroom behavioral socialization practices and low-income children’s self-regulation skills. Early childhood research quarterly, 31, 89–100. doi: 10.1016/j.ecresq.2015.01.002 [DOI] [Google Scholar]
- Dietz WH. (1994). Critical periods in childhood for the development of obesity. The American journal of clinical nutrition, 59(5), 955–959. [DOI] [PubMed] [Google Scholar]
- Dilworth-Bart JE, Khurshid A, & Vandell DL. (2007). Do maternal stress and home environment mediate the relation between early income-to-need and 54-months attentional abilities? Infant and Child Development, 16(5), 525–552. doi: 10.1002/icd.528 [DOI] [Google Scholar]
- Dinsa GD, Goryakin Y, Fumagalli E, & Suhrcke M. (2012). Obesity and socioeconomic status in developing countries: a systematic review. Obesity Reviews, 13(11), 1067–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion T, Shaw DS, Connell AM, Gardner F, Weaver C, & Wilson M. (2008). The family check-up with high-risk indigent families: preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child development, 79, 1395–1414. doi: 10.1111/j.14678624.2008.01195.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doan SN, Fuller-Rowell TE, & Evans GW. (2012). Cumulative risk and adolescent’s internalizing and externalizing problems: the mediating roles of maternal responsiveness and self-regulation. Developmental Psychology, 48(6), 1529–1539. doi: 10.1037/a0027815 [DOI] [PubMed] [Google Scholar]
- Drewnowski A, & Specter S. (2004). Poverty and obesity: the role of energy density and energy costs. The American journal of clinical nutrition, 79(1), 6–16. [DOI] [PubMed] [Google Scholar]
- Duckworth AL, Tsukayama E, & Geier AB. (2010). Self-controlled children stay leaner in the transition to adolescence. Appetite, 54(2), 304–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, & Magnuson K. (2013). The long reach of early childhood poverty In Economic stress, human capital, and families in Asia (pp. 57–70): Springer. [Google Scholar]
- Eamon MK. (2002). Poverty, parenting, peer, and neighborhood influences on young adolescent antisocial behavior. Journal of Social Service Research, 28(1), 1–23. [Google Scholar]
- Ebbeling CB, Pawlak DB, & Ludwig DS. (2002). Childhood obesity: public-health crisis, common sense cure. The lancet, 360(9331), 473–482. [DOI] [PubMed] [Google Scholar]
- Economos CD, Hyatt RR, Goldberg JP, Must A, Naumova EN, Collins JJ, & Nelson ME. (2007). A community intervention reduces BMI z score in children: Shape Up Somerville first year results. Obesity, 15(5), 1325–1336. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Vidmar M, Spinrad TL, Eggum ND, Edwards A, Gaertner B, & Kupfer A. (2010). Mothers’ teaching strategies and children’s effortful control: A longitudinal study. Developmental Psychology, 46(5), 1294–1308. doi: 10.1037/a0020236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, & Zhou Q. (2016). Conceptions of executive function and regulation: When and to what degree do they overlap? In Griffin JA, McCardle P, & Freund LS. (Eds.), Executive function in preschool-age children: Integrating measurement, neurodevelopment, and translational research (pp. 115–136, Chapter xi, 362 Pages): American Psychological Association, Washington, DC. [Google Scholar]
- Emery RL, & Levine MD. (2017). Questionnaire and behavioral task measures of impulsivity are differentially associated with body mass index: A comprehensive meta-analysis. Psychological bulletin, 143(8), 868. [DOI] [PubMed] [Google Scholar]
- Eneli IU, Tylka TL, Hummel J, Watowicz RP, Perez SA, Kaciroti N, & Lumeng JC. (2015). Rationale and design of the Feeding Dynamic Intervention (FDI) study for self-regulation of energy intake in preschoolers. Contemporary clinical trials, 41, 325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Valoski A, Wing RR, & McCurley J. (1990). Ten-year follow-up of behavioral, family-based treatment for obese children. Jama, 264(19), 2519–2523. [PubMed] [Google Scholar]
- Epstein LH, Wing RR, Koeske R, Andrasik F, & Ossip DJ. (1981). Child and parent weight loss in family-based behavior modification programs. Journal of Consulting and Clinical Psychology, 49(5), 674. [DOI] [PubMed] [Google Scholar]
- Evans GW, & English K. (2002). The environment of poverty: Multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child development, 73(4), 1238–1248. [DOI] [PubMed] [Google Scholar]
- Evans GW, Fuller-Rowell TE, & Doan SN. (2012). Childhood cumulative risk and obesity: the mediating role of self-regulatory ability. Pediatrics, 129(1), e68–e73. [DOI] [PubMed] [Google Scholar]
- Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, & Salpekar N. (2005). The role of chaos in poverty and children’s socioemotional adjustment. Psychological Science, 16(7), 560–565. doi: 10.1111/j.09567976.2005.01575.x [DOI] [PubMed] [Google Scholar]
- Evans GW, & Kim P. (2007). Childhood poverty and health cumulative risk exposure and stress dysregulation. Psychological Science, 18(11), 953–957. [DOI] [PubMed] [Google Scholar]
- Fernald LC, Gertler PJ, & Neufeld LM. (2008). Role of cash in conditional cash transfer programmes for child health, growth, and development: an analysis of Mexico’s Oportunidades. The lancet, 371(9615), 828–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogel A, McCrickerd K, Fries LR, Goh AT, Quah PL, Chan MJ, … Forde CG. (2018). Eating in the absence of hunger: Stability over time and associations with eating behaviours and body composition in children. Physiology & Behavior, 192, 82–89. doi: 10.1016/j.physbeh.2018.03.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forehand R, Biggar H, & Kotchick BA. (1998). Cumulative risk across family stressors: Short-and long-term effects for adolescents. Journal of abnormal child psychology, 26(2), 119–128. [DOI] [PubMed] [Google Scholar]
- Francis LA, Granger D, & Susman EJ. (2013). Adrenocortical regulation, eating in the absence of hunger and BMI in young children. Appetite, 64, 3238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, & Susman EJ. (2009). Self-regulation and rapid weight gain in children from age 3 to 12 years. Archives of pediatrics & adolescent medicine, 163(4), 297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedlander SL, Larkin EK, Rosen CL, Palermo TM, & Redline S. (2003). Decreased quality of life associated with obesity in school-aged children. Archives of pediatrics & adolescent medicine, 157(12), 1206–1211. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Bridgett DJ, Young BN, Panksepp J, & Power T. (2013). Origins of effortful control: Infant and parent contributions. Infancy, 18(2), 149–183. doi: 10.1111/j.1532-7078.2012.00119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs BG, & Forste R. (2014). Socioeconomic status, infant feeding practices and early childhood obesity. Pediatric obesity, 9(2), 135–146. [DOI] [PubMed] [Google Scholar]
- Gibson D. (2004). Long-term food stamp program participation is differentially related to overweight in young girls and boys. The Journal of Nutrition, 134(2), 372–379. [DOI] [PubMed] [Google Scholar]
- Goossens L, Braet C, Van Vlierberghe L, & Mels S. (2009). Loss of control over eating in overweight youngsters: the role of anxiety, depression and emotional eating. European Eating Disorders Review, 17(1), 68–78. [DOI] [PubMed] [Google Scholar]
- Graziano PA, Calkins SD, & Keane SP. (2010). Toddler self-regulation skills predict risk for pediatric obesity. International Journal of Obesity, 34(4), 633–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graziano PA, Kelleher R, Calkins SD, Keane SP, & Brien MO. (2013). Predicting weight outcomes in preadolescence: the role of toddlers’ self-regulation skills and the temperament dimension of pleasure. International Journal of Obesity, 37(7), 937–942. doi: 10.1038/ijo.2012.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grineski SE, Morales DX, Collins TW, & Rubio R. (2018). Transitional dynamics of household food insecurity impact children’s developmental outcomes. Journal of Developmental and Behavioral Pediatrics, 39(9), 715–725. doi: 10.1097/DBP.0000000000000598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross RS, Mendelsohn AL, Fierman AH, Racine AD, & Messito MJ. (2012). Food insecurity and obesogenic maternal infant feeding styles and practices in low-income families. Pediatrics, 130(2), 254–261. [DOI] [PubMed] [Google Scholar]
- Gueron-Sela N, Camerota M, Willoughby MT, Vernon-Feagans L, Cox MJ, & Family Life Project Key, I. (2018). Maternal depressive symptoms, mother-child interactions, and children’s executive function. Developmental Psychology, 54(1), 71–82. doi: 10.1037/dev0000389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundersen C, Lohman BJ, Eisenmann JC, Garasky S, & Stewart SD. (2008). Child-specific food insecurity and overweight are not associated in a sample of 10-to 15-year-old low-income youth. The Journal of Nutrition, 138(2), 371–378. [DOI] [PubMed] [Google Scholar]
- Hamilton WL, & Cook JT. (1997). Household food security in the United States in 1995: technical report of the food security measurement project. [Google Scholar]
- Hancock KJ, Lawrence D, & Zubrick SR. (2014). Higher maternal protectiveness is associated with higher odds of child overweight and obesity: a longitudinal Australian study. PloS ONE, 9(6), e100686. doi: 10.1371/journal.pone.0100686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartanto A, Toh WX, & Yang H. (2018). Bilingualism narrows socioeconomic disparities in executive functions and self-regulatory behaviors during early childhood: Evidence from the Early Childhood Longitudinal Study. Child Development, 54(1), 71–82. doi: 10.1111/cdev.13032 [DOI] [PubMed] [Google Scholar]
- Ho M, Garnett SP, Baur L, Burrows T, Stewart L, Neve M, & Collins C. (2012). Effectiveness of lifestyle interventions in child obesity: systematic review with meta-analysis. Pediatrics, peds. 2012–1176. [DOI] [PubMed] [Google Scholar]
- Hollar D, Messiah SE, Lopez-Mitnik G, Hollar TL, Almon M, & Agatston AS. (2010). Effect of a two-year obesity prevention intervention on percentile changes in body mass index and academic performance in low-income elementary school children. American Journal of Public Health, 100(4), 646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm-Denoma JM, Smith A, Lewinsohn PM, & Pettit JW. (2014). Psychosocial predictors of body mass index at late childhood: A longitudinal investigation. Journal of Health Psychology, 19(6), 754–764. doi: 10.1177/1359105313479626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes SO, Power TG, O’Connor TM, & Fisher JO. (2015). Executive functioning, emotion regulation, eating self-regulation, and weight status in low-income preschool children: How do they relate? Appetite, 89, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isasi CR, & Wills TA. (2011). Behavioral self-regulation and weight-related behaviors in inner-city adolescents: a model of direct and indirect effects. Childhood Obesity, 7(4), 306–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel AC, Guile CA, Baker JE, & Silverman WK. (1994). An evaluation of enhanced self-regulation training in the treatment of childhood obesity. Journal of pediatric psychology, 19(6), 737–749. [DOI] [PubMed] [Google Scholar]
- Janjua NZ, Mahmood B, Islam MA, & Goldenberg RL. (2012). Maternal and early childhood risk factors for overweight and obesity among low-income predominantly black children at age five years: A prospective cohort study. Journal of Obesity, 2012, 457173–457179. doi: 10.1155/2012/457173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL. (2000). Improving preschoolers’ self-regulation of energy intake. Pediatrics, 106(6), 1429–1435. [DOI] [PubMed] [Google Scholar]
- Johnson SL, & Taylor-Holloway LA. (2006). Non-Hispanic white and Hispanic elementary school children’s self-regulation of energy intake. The American journal of clinical nutrition, 83(6), 1276–1282. [DOI] [PubMed] [Google Scholar]
- Kakinami L, Barnett TA, Séguin L, & Paradis G. (2015). Parenting style and obesity risk in children. Preventive medicine, 75, 18–22. [DOI] [PubMed] [Google Scholar]
- Kidwell SL, & Barnett D. (2007). Adaptive emotion regulation among low-income African American children. Merrill-Palmer Quarterly, 53(2), 155–183. doi: 10.1353/mpq.2007.0011 [DOI] [Google Scholar]
- Kiernan KE, & Mensah FK. (2011). Poverty, family resources and children’s early educational attainment: the mediating role of parenting. British Educational Research Journal, 37(2), 317–336. [Google Scholar]
- Kim J, Mutyala B, Agiovlasitis S, & Fernhall B. (2011). Health behaviors and obesity among US children with attention deficit hyperactivity disorder by gender and medication use. Preventive medicine, 52(3), 218–222. [DOI] [PubMed] [Google Scholar]
- Kimbro RT, Brooks-Gunn J, & McLanahan S. (2007). Racial and ethnic differentials in overweight and obesity among 3-year-old children. American Journal of Public Health, 97(2), 298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Lengua LJ, & Monahan KC. (2013). Individual differences in the development of self-regulation during pre-adolescence: Connections to context and adjustment. Journal of Abnormal Child Psychology, 41(1), 5769. doi: 10.1007/s10802-012-9665-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok MK, Schooling CM, Lam TH, & Leung GM. (2010). Paternal smoking and childhood overweight: evidence from the Hong Kong “Children of 1997”. Pediatrics, peds. 2009–2642. [DOI] [PubMed] [Google Scholar]
- Lamerz A, Kuepper-Nybelen J, Wehle C, Bruning N, Trost-Brinkhues G, Brenner H, … Herpertz-Dahlmann B. (2005). Social class, parental education, and obesity prevalence in a study of six-year-old children in Germany. International Journal of Obesity, 29(4), 373. [DOI] [PubMed] [Google Scholar]
- Lane SP, Bluestone C, & Burke CT. (2013). Trajectories of BMI from early childhood through early adolescence: SES and psychosocial predictors. British journal of health psychology, 18(1), 66–82. [DOI] [PubMed] [Google Scholar]
- Lawlor DA, Ronalds G, Macintyre S, Clark H, & Leon DA. (2006). Family socioeconomic position at birth and future cardiovascular disease risk: findings from the Aberdeen Children of the 1950s cohort study. American Journal of Public Health, 96(7), 1271–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson GM, Hook CJ, & Farah MJ. (2018). A meta analysis of the relationship between socioeconomic status and executive function performance among children. Developmental Science, 21(2), e12529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Andrew M, Gebremariam A, Lumeng JC, & Lee JM. (2014). Longitudinal associations between poverty and obesity from birth through adolescence. American Journal of Public Health, 104(5), e70–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee I, Bang K-S, Moon H, & Kim J. (2016). Comparison of obesity rates in early childhood (4 to 80 months) by parental socioeconomic status using national cohort dataset in Korea. Asian Nursing Research, 10(4), 305–311. doi: 10.1016/j.anr.2016.10.005 [DOI] [PubMed] [Google Scholar]
- Lengua LJ, Honorado E, & Bush NR. (2007). Contextual risk and parenting as predictors of effortful control and social competence in preschool children. Journal of Applied Developmental Psychology, 28(1), 40–55. doi: 10.1016/j.appdev.2006.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ, Kiff C, Moran L, Zalewski M, Thompson S, Cortes R, & Ruberry E. (2014). Parenting mediates the effects of income and cumulative risk on the development of effortful control. Social Development, 23(3), 631–649. doi: 10.1111/sode.12071 [DOI] [Google Scholar]
- Lengua LJ, Moran L, Zalewski M, Ruberry E, Kiff C, & Thompson S. (2015). Relations of growth in effortful control to family income, cumulative risk, and adjustment in preschool-age children. Journal of Abnormal Child Psychology, 43(4), 705–720. doi: 10.1007/s10802-014-9941-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ, Zalewski M, Fisher P, & Moran L. (2013). Does HPA-Axis dysregulation account for the effects of income on effortful control and adjustment in preschool children?: Income, HPA-Axis dysregulation and effortful control. Infant and Child Development, 22(5), 439–458. doi: 10.1002/icd.1805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhard W, & Lenhard A. (2016). Calculation of effect sizes. Bibergau: Psychometrica; Available online at: https://www.psychometrica.de/effect_size.html. [Google Scholar]
- Leung CY, Lumeng JC, Kaciroti NA, Chen YP, Rosenblum K, & Miller AL. (2014). Surgency and negative affectivity, but not effortful control, are uniquely associated with obesogenic eating behaviors among low-income preschoolers. Appetite, 78, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Goran MI, Kaur H, Nollen N, & Ahluwalia JS. (2007). Developmental trajectories of overweight during childhood: Role of early life factors. Obesity, 15(3), 760–771. doi: 10.1038/oby.2007.585 [DOI] [PubMed] [Google Scholar]
- Lim S, Zoellner JM, Ajrouch KJ, & Ismail AI. (2011). Overweight in childhood: the role of resilient parenting in African-American households. American Journal of Preventive Medicine, 40(3), 329–333. doi: 10.1016/j.amepre.2010.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumeng JC, Miller AL, Horodynski MA, Brophy-Herb HE, Contreras D, Lee H, … Peterson KE. (2017). Improving Self-regulation for Obesity Prevention in Head Start: A Randomized Controlled Trial. Pediatrics, e20162047. [DOI] [PubMed] [Google Scholar]
- Mallan KM, Nambiar S, Magarey AM, & Daniels LA. (2014). Satiety responsiveness in toddlerhood predicts energy intake and weight status at four years of age. Appetite, 74, 79–85. [DOI] [PubMed] [Google Scholar]
- Marcovitch S, O’Brien M, Calkins SD, Leerkes EM, Weaver JM, & Levine DW. (2015). A longitudinal assessment of the relation between executive function and theory of mind at 3, 4, and 5 years. Cognitive Development, 33, 40–55. doi: 10.1016/j.cogdev.2014.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall SJ, Biddle SJ, Gorely T, Cameron N, & Murdey I. (2004). Relationships between media use, body fatness and physical activity in children and youth: a meta-analysis. International Journal of Obesity, 28(10), 1238. [DOI] [PubMed] [Google Scholar]
- Martoccio TL, Brophy-Herb HE, & Onaga EE. (2014). Road to readiness: Pathways from low-income childrenʼs early interactions to school readiness skills. Infants & Young Children, 27(3), 193–206. doi: 10.1097/IYC.0000000000000014 [DOI] [Google Scholar]
- McCallum Z, Wake M, Gerner B, Baur L, Gibbons K, Gold L, … Riess C. (2007). Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. International Journal of Obesity, 31(4), 630–636. [DOI] [PubMed] [Google Scholar]
- McClelland MM, & Wanless SB. (2012). Growing up with assets and risks: The importance of self-regulation for academic achievement. Research in Human Development, 9(4), 278–297. doi: 10.1080/15427609.2012.729907 [DOI] [Google Scholar]
- McLeod JD, & Shanahan MJ. (1993). Poverty, parenting, and children’s mental health. American Sociological Review, 351–366. [Google Scholar]
- Mészáros Z, Mészáros J, Szmodis MB, Pampakas P, Osváth P, & Völgyi E. (2008). Primary school child development—Issues of socioeconomic status. Kinesiology, 40(2), 154–162. doi:https://hrcak.srce.hr/30815 [Google Scholar]
- Metcalfe J, & Mischel W. (1999). A hot/cool-system analysis of delay of gratification: dynamics of willpower. Psychological Review, 106(1), 3. [DOI] [PubMed] [Google Scholar]
- Michels N, Sioen I, Braet C, Eiben G, Hebestreit A, Huybrechts I, … De Henauw S. (2012). Stress, emotional eating behaviour and dietary patterns in children. Appetite, 59(3), 762–769. [DOI] [PubMed] [Google Scholar]
- Miller AL, Rosenblum KL, Retzloff LB, & Lumeng JC. (2016). Observed self-regulation is associated with weight in low-income toddlers. Appetite, 105, 705–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry RS, Benner AD, Biesanz JC, Clark SL, & Howes C. (2010). Family and social risk, and parental investments during the early childhood years as predictors of low-income children’s school readiness outcomes. Early childhood research quarterly, 25(4), 432–449. doi: 10.1016/j.ecresq.2010.01.002 [DOI] [Google Scholar]
- Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, … Ross S. (2011). A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences, 108(7), 2693–2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, & Eliakim A. (2005). Short-and long-term beneficial effects of a combined dietary– behavioral–physical activity intervention for the treatment of childhood obesity. Pediatrics, 115(4), e443–e449. [DOI] [PubMed] [Google Scholar]
- Nesbitt KT, Baker-Ward L, & Willoughby MT. (2013). Executive function mediates socio-economic and racial differences in early academic achievement. Early childhood research quarterly, 28(4), 774–783. doi: 10.1016/j.ecresq.2013.07.005 [DOI] [Google Scholar]
- Nievar MA, Moske AK, Johnson DJ, & Chen Q. (2014). Parenting practices in preschool leading to later cognitive competence: A family stress model. Early Education and Development, 25(3), 318–337. doi: 10.1080/10409289.2013.788426 [DOI] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, & Flegal KM. (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. Jama, 307(5), 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, & Flegal KM. (2016). Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 20132014. Jama, 315(21), 2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken E, Levitan E, & Gillman M. (2008). Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. International Journal of Obesity, 32(2), 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey A, Hale D, Das S, Goddings A-L, Blakemore S-J, & Viner RM. (2018). Effectiveness of universal self-regulation–based interventions in children and adolescents: a systematic review and meta-analysis. JAMA pediatrics, 172(6), 566–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkinson KN, Drewett RF, Le Couteur AS, Adamson AJ, & Gateshead Milennium Study Core, T. (2010). Do maternal ratings of appetite in infants predict later Child Eating Behaviour Questionnaire scores and body mass index? Appetite, 54(1), 186–190. doi: 10.1016/j.appet.2009.10.007 [DOI] [PubMed] [Google Scholar]
- Pearce A, Sawyer ACP, Chittleborough CR, Mittinty MN, Law C, & Lynch JW. (2016). Do early life cognitive ability and self-regulation skills explain socio-economic inequalities in academic achievement? An effect decomposition analysis in UK and Australian cohorts. Social Science & Medicine, 165, 108–118. doi: 10.1016/j.socscimed.2016.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peredo TN, Owen MT, Rojas R, & Caughy MOB (2015). Child vocabulary, maternal behavior, and inhibitory control development among Spanish-speaking children. Early Education and Development, 26(5–6), 749–769. doi: 10.1080/10409289.2015.1009319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pervanidou P, & Chrousos GP. (2011). Stress and obesity/metabolic syndrome in childhood and adolescence. Pediatric obesity, 6(S1), 21–28. [DOI] [PubMed] [Google Scholar]
- Piché G, Fitzpatrick C, & Pagani LS. (2012). Kindergarten Self Regulation As a Predictor of Body Mass Index and Sports Participation in Fourth Grade Students. Mind, Brain, and Education, 6(1), 19–26. [Google Scholar]
- Porges SW. (2007). The polyvagal perspective. Biological Psychology, 74(2), 116–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power TG, Olivera YA, Hill RA, Beck AD, Hopwood V, Garcia KS, … Hughes SO. (2016). Emotion regulation strategies and childhood obesity in high risk preschoolers. Appetite, 107, 623–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt ME, McClelland MM, Swanson J, & Lipscomb ST. (2016). Family risk profiles and school readiness: A person-centered approach. Early childhood research quarterly, 36, 462–474. doi: 10.1016/j.ecresq.2016.01.017 [DOI] [Google Scholar]
- Propper C. (2012). The early development of vagal tone: Effects of poverty and elevated contextual risk. New York, New York: Oxford University Press. [Google Scholar]
- Raver CC. (2004). Placing emotional self regulation in sociocultural and socioeconomic contexts. Child development, 75(2), 346–353. [DOI] [PubMed] [Google Scholar]
- Raver CC, Jones SM, Li Grining C, Zhai F, Bub K, & Pressler E. (2011). CSRP’s impact on low income preschoolers’ preacademic skills: self regulation as a mediating mechanism. Child development, 82(1), 362378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raver CC, McCoy DC, Lowenstein AE, & Pess R. (2013). Predicting individual differences in low income children’s executive control from early to middle childhood. Developmental Science, 16(3), 394–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razza RA, Martin A, & Brooks-Gunn J. (2010). Associations among family environment, sustained attention, and school readiness for low-income children. Developmental Psychology, 46(6), 1528–1542. doi: 10.1037/a0020389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs NR, Greenberg MT, Kusché CA, & Pentz MA. (2006). The mediational role of neurocognition in the behavioral outcomes of a socialemotional prevention program in elementary school students: Effects of the PATHS curriculum. Prevention Science, 7(1), 91–102. [DOI] [PubMed] [Google Scholar]
- Rochette É, & Bernier A. (2014). Parenting, family socioeconomic status, and child executive functioning: A longitudinal study. Merrill-Palmer Quarterly, 60(4), 431–460. doi: 10.13110/merrpalmquar1982.60.4.0431 [DOI] [Google Scholar]
- Rolland-Cachera M, Deheeger M, Maillot M, & Bellisle F. (2006). Early adiposity rebound: causes and consequences for obesity in children and adults. International Journal of Obesity, 30, S11–S17. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, & Fisher P. (2001). Investigations of temperament at three to seven years: The Children’s Behavior Questionnaire. Child development, 72(5), 1394–1408. [DOI] [PubMed] [Google Scholar]
- Roy AL, McCoy DC, & Raver CC. (2014). Instability versus quality: residential mobility, neighborhood poverty, and children’s self-regulation. Developmental Psychology, 50(7), 1891–1896. doi:10.1037/a0036984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy AL, & Raver CC. (2014). Are all risks equal? Early experiences of poverty-related risk and children’s functioning. Journal of Family Psychology, 28(3), 391–400. doi: 10.1037/a0036683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Dunn J, Plomin R, Simonoff E, Pickles A, Maughan B, … Eaves L. (1997). Integrating nature and nurture: Implications of person–environment correlations and interactions for developmental psychopathology. Development and psychopathology, 9(02), 335–364. [DOI] [PubMed] [Google Scholar]
- Sabol TJ, Bohlmann NL, & Downer JT. (2018). Low income ethnically diverse children’s engagement as a predictor of school readiness above preschool classroom quality. Child Development, 89(2), 556–576. doi: 10.1111/cdev.12832 [DOI] [PubMed] [Google Scholar]
- Sallis JF, & Glanz K. (2006). The role of built environments in physical activity, eating, and obesity in childhood. The Future of Children, 89–108. [DOI] [PubMed] [Google Scholar]
- Schmeiser MD. (2009). Expanding wallets and waistlines: the impact of family income on the BMI of women and men eligible for the Earned Income Tax Credit. Health economics, 18(11), 1277–1294. [DOI] [PubMed] [Google Scholar]
- Schmeiser MD. (2012). The impact of long term participation in the supplemental nutrition assistance program on child obesity. Health economics, 21(4), 386–404. [DOI] [PubMed] [Google Scholar]
- Seeyave DM, Coleman S, Appugliese D, Corwyn RF, Bradley RH, Davidson NS, … Lumeng JC. (2009). Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Archives of pediatrics & adolescent medicine, 163(4), 303–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sektnan M, McClelland MM, Acock A, & Morrison FJ. (2010). Relations between early family risk, children’s behavioral regulation, and academic achievement. Early Childhood Research Quarterly, 25(4), 464–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen S, Rifas-Shiman SL, Shivappa N, Wirth MD, Hebert JR, Gold DR, … Oken E. (2017). Associations of prenatal and early life dietary inflammatory potential with childhood adiposity and cardiometabolic risk in Project Viva. Pediatric Obesity, 13(5), 292–300. doi: 10.1111/ijpo.12221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelleby EC, Shaw DS, Cheong J, Chang H, Gardner F, Dishion TJ, & Wilson MN. (2012). Behavioral control in at-risk toddlers: The influence of the Family Check-Up. Journal of Clinical Child & Adolescent Psychology, 41(3), 288–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, … Care D. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. [DOI] [PubMed] [Google Scholar]
- Shrewsbury V, & Wardle J. (2008). Socioeconomic status and adiposity in childhood: a systematic review of cross sectional studies 1990–2005. Obesity, 16(2), 275–284. [DOI] [PubMed] [Google Scholar]
- Simmonds M, Llewellyn A, Owen C, & Woolacott N. (2016). Predicting adult obesity from childhood obesity: a systematic review and meta analysis. Obesity Reviews, 17(2), 95–107. [DOI] [PubMed] [Google Scholar]
- Simmons S, Alexander JL, Ewing H, & Whetzel S. (2012). SNAP Participation in Preschool Aged Children and Prevalence of Overweight and Obesity. Journal of School Health, 82(12), 548–552. [DOI] [PubMed] [Google Scholar]
- Sitnick SL, Shaw DS, Weaver CM, Shelleby EC, Choe DE, Reuben JD, … Taraban L. (2017). Early Childhood Predictors of Severe Youth Violence in Low Income Male Adolescents. Child development, 88(1), 27–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Kubzansky LD, McLaughlin KA, & Koenen KC. (2012). Childhood adversity and inflammatory processes in youth: A prospective study. Psychoneuroendocrinology, 38(2), 188–200. doi: 10.1016/j.psyneuen.2012.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C, & Richards R. (2008). Dietary intake, overweight status, and perceptions of food insecurity among homeless Minnesotan youth. American Journal of Human Biology, 20(5), 550–563. [DOI] [PubMed] [Google Scholar]
- Smith JD, Montaño Z, Dishion TJ, Shaw DS, & Wilson MN. (2015). Preventing weight gain and obesity: Indirect effects of the family check-up in early childhood. Prevention Science, 16(3), 408–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starkey L, & Revenson TA. (2014). Early Changes in Socioeconomic Status Do Not Predict Changes in Body Mass in the First Decade of Life. Annals of Behavioral Medicine, 49(2), 212–220. [DOI] [PubMed] [Google Scholar]
- Stautz K, Pechey R, Couturier D-L, Deary IJ, & Marteau TM. (2016). Do executive function and impulsivity predict adolescent health behaviour after accounting for intelligence? Findings from the ALSPAC Cohort. PloS ONE, 11(8), e0160512. doi: 10.1371/journal.pone.0160512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinsbekk S, & Wichstrøm L. (2015). Predictors of change in BMI from the age of 4 to 8. Journal of pediatric psychology, 40(10), 1056–1064. [DOI] [PubMed] [Google Scholar]
- Strauss RS, & Knight J. (1999). Influence of the home environment on the development of obesity in children. Pediatrics, 103(6), e85–e85. [DOI] [PubMed] [Google Scholar]
- Strauss RS, & Pollack HA. (2003). Social marginalization of overweight children. Archives of pediatrics & adolescent medicine, 157(8), 746–752. [DOI] [PubMed] [Google Scholar]
- Strobino DM, Ahmed S, Mistry K, Wasserman E, Hossain MB, & Minkovitz C. (2016). Maternal depressive symptoms and attained size among children in the first 2 years of life. Academic pediatrics, 16(1), 75–81. [DOI] [PubMed] [Google Scholar]
- Sturge-Apple ML, Suor JH, Davies PT, Cicchetti D, Skibo MA, & Rogosch FA. (2016). Vagal tone and children’s delay of gratification: Differential sensitivity in resource-poor and resource-rich environments. Psychological Science, 27(6), 885–893. doi: 10.1177/0956797616640269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulik MJ, Blair C, Mills Koonce R, Berry D, Greenberg M, Vernon Feagans L, … The Family Life Project, I. (2015). Early parenting and the development of externalizing behavior problems: Longitudinal mediation through children’s executive function. Child Development, 86(5), 1588–1603. doi: 10.1111/cdev.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suor JH, Sturge-Apple ML, & Jones-Gordils HR. (2018). Parsing profiles of temperamental reactivity and differential routes to delay of gratification: A person-based approach. Development and Psychopathology, 1–20. doi: 10.1017/S0954579417001894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan CC, & Holub SC. (2010). Children’s self-regulation in eating: Associations with inhibitory control and parents’ feeding behavior. Journal of pediatric psychology, 36(3), 340–345. [DOI] [PubMed] [Google Scholar]
- Tandon P, Thompson S, Moran L, & Lengua LJ. (2015). Body mass index mediates the effects of low income on preschool children’s executive control, with implications for behavior and academics. Childhood Obesity, 11(5), 569–576. doi: 10.1089/chi.2014.0071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson SF, Lengua LJ, Zalewski M, & Moran L. (2013). Income and the development of effortful control as predictors of teacher reports of preschool adjustment. Early childhood research quarterly, 28(4), 784–793. doi: 10.1016/j.ecresq.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiberio SS, Kerr DCR, Capaldi DM, Pears KC, Kim HK, & Nowicka P. (2014). Parental monitoring of children’s media consumption: The long-term influences on body mass index in children. JAMA Pediatrics, 168(5), 414–421. doi: 10.1001/jamapediatrics.2013.5483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran MK, Krueger PM, McCormick E, Davidson A, & Main DS. (2016). Body mass transitions through childhood and early adolescence: a multistate life table approach. American journal of epidemiology, 183(7), 643–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trentacosta CJ, & Shaw DS. (2009). Emotional self-regulation, peer rejection, and antisocial behavior: Developmental associations from early childhood to early adolescence. Journal of Applied Developmental Psychology, 30(3), 356–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsukayama E, Toomey SL, Faith MS, & Duckworth AL. (2010). Selfcontrol as a protective factor against overweight status in the transition from childhood to adolescence. Archives of pediatrics & adolescent medicine, 164(7), 631–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hulst A, Roy-Gagnon M-H, Gauvin L, Kestens Y, Henderson M, & Barnett TA. (2015). Identifying risk profiles for childhood obesity using recursive partitioning based on individual, familial, and neighborhood environment factors. The International Journal of Behavioral Nutrition and Physical Activity, 12(1), 17–17. doi: 10.1186/s12966-015-0175-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rossem LM, Silva LMMDP, Hokken-Koelega AMDP, Arends LRP, Moll HAMDP, Jaddoe VWVMDP, … Raat HMDP (2010). Socioeconomic status is not inversely associated with overweight in preschool children. The Journal of Pediatrics, 157(6), 929–935.e921. doi: 10.1016/j.jpeds.2010.06.008 [DOI] [PubMed] [Google Scholar]
- Verbeken S, Braet C, Goossens L, & Van der Oord S. (2013). Executive function training with game elements for obese children: A novel treatment to enhance self-regulatory abilities for weight-control. Behaviour research and therapy, 51(6), 290–299. [DOI] [PubMed] [Google Scholar]
- Vernon-Feagans L, Willoughby M, & Garrett-Peters P. (2016). Predictors of behavioral regulation in kindergarten: Household chaos, parenting, and early executive functions. Developmental Psychology, 52(3), 430–441. doi: 10.1037/dev0000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Votruba-Drzal E. (2006). Economic disparities in middle childhood development: Does income matter? Developmental Psychology, 42(6), 1154. [DOI] [PubMed] [Google Scholar]
- Wade M, Madigan S, Plamondon A, Rodrigues M, Browne D, & Jenkins JM. (2018). Cumulative psychosocial risk, parental socialization, and child cognitive functioning: A longitudinal cascade model. Developmental Psychology, 54(6), 1038–1050. doi: 10.1037/dev0000493 [DOI] [PubMed] [Google Scholar]
- Wanless SB, McClelland MM, Tominey SL, & Acock AC. (2011). The influence of demographic risk factors on children’s behavioral regulation in prekindergarten and kindergarten. Early Education & Development, 22(3), 461–488. doi: 10.1080/10409289.2011.536132 [DOI] [Google Scholar]
- Wardle J, Guthrie CA, Sanderson S, & Rapoport L. (2001). Development of the children’s eating behaviour questionnaire. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 42(7), 963–970. [DOI] [PubMed] [Google Scholar]
- Waring ME, & Lapane KL. (2008). Overweight in children and adolescents in relation to attention-deficit/hyperactivity disorder: results from a national sample. Pediatrics, 122(1), e1–e6. [DOI] [PubMed] [Google Scholar]
- Warschburger P. (2015). SRT-Joy–computer-assisted self-regulation training for obese children and adolescents: study protocol for a randomized controlled trial. Trials, 16(1), 566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster Stratton C, Jamila Reid M, & Stoolmiller M. (2008). Preventing conduct problems and improving school readiness: evaluation of the incredible years teacher and child training programs in high risk schools. Journal of Child Psychology and Psychiatry, 49(5), 471–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, & Dietz WH. (1997). Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine, 337(13), 869–873. [DOI] [PubMed] [Google Scholar]
- Williams AS, Ge B, Petroski G, Kruse RL, McElroy JA, & Koopman RJ. (2018). Socioeconomic Status and Other Factors Associated with Childhood Obesity. The Journal of the American Board of Family Medicine, 31(4), 514–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby M, Kupersmidt J, Voegler-Lee M, & Bryant D. (2011). Contributions of hot and cool self-regulation to preschool disruptive behavior and academic achievement. Developmental neuropsychology, 36(2), 162–180. [DOI] [PMC free article] [PubMed] [Google Scholar]