Highlights
-
•
The current practices of smart technology applications to mobile health care are reviewed.
-
•
The fuzzy geometric mean and fuzzy analytic hierarchy process approach is proposed to assess the relative importance of critical factors.
-
•
The most important critical factors were the relaxation of laws, unobtrusiveness, and the correct identification of the need.
Keywords: Mobile, Health care, Smart technology, Fuzzy geometric mean, Fuzzy analytic hierarchy process
Abstract
Smart technologies present numerous opportunities for enhancing mobile health care. However, some concerns regarding the viability of smart technology applications must be addressed. This study investigated these concerns by reviewing the current practices of smart technology applications to mobile health care. As a result, five factors critical to the applicability of a smart technology to mobile health care are identified, and the fuzzy geometric mean-fuzzy analytic hierarchy process (FGM-FAHP) approach is proposed to assess the relative importance levels of the identified factors. The experimental results showed that the three most critical factors identified include: (a) the relaxation of the related medical laws; (b) unobtrusiveness; and (c) the precise need and situation of a user. Accordingly, approximately 44%, 26%, and 15% of the budget should be allocated to the realization of the three critical factors, respectively. In addition, the challenges involved and opportunities for enhancing the effectiveness of existing applications are discussed.
Introduction
Smart technologies enable a mobile user to apply intelligent sensors and actuators to detect and respond to ambient conditions unobtrusively, and the results of the detection can be transmitted wirelessly to a backend service center [1]. Today, smart technology applications have become more and more prevalent in mobile health care [2, 3]. For example, Baek et al. [4] designed a smart diagnostic chair that could measure unconstrained heart rate and blood pressure without the direct contact between embedded instruments and bare skin of the users. According to the survey by Baig and Gholamhosseini [5], no less than fifty smart health monitoring systems have since been invented at the time of their survey. These smart health monitoring systems automate patient monitoring tasks and facilitate workflow management. A smart surveillance system to detect abnormal motions of a user in emergency situations has been devised by Jung and Chung [6]. As noted by Natarajan et al. [7], smart sensors adopted by a mobile health care system could be connected via an Internet of things (IoT), thereby facilitating the aggregation of various information sources to judge the health problem of a user accurately.
Some smart technologies are dedicated to specific groups or situations. For example, an app was designed in Kaewkungwal te al. [8] to plan the schedule for providing antenatal care (ANC) and expanded program on immunization (EPI) services to mothers and children in an under-served region. Hirata et al. [9] and Mutiara et al. [10] equipped a smart cane with proximity sensors to detect the fall of an elderly person. The sudden movement of such an individual or an increasing distance detected between the user of a smart cane and the cane could be interpreted as a possible fall.
Purportedly, three major drivers of mobile health care in today's era of digital health transformation include: (a) the high expenditure on health care and the need for disruptive solutions; (b) the rapid and ongoing growth of wireless connectivity; and (c) the need for more precise and individualized health care [11]. So far, most applications of smart technologies to mobile health care have been intended to improve disease management (such as monitoring the health/disease status, adjusting the medication dosage, and increasing adherence to prescribed medication) and to change health behaviors [3, 12]. For a mobile health care service to be successful, five tasks need to be fulfilled, including allocation concealment, allocation sequence determination, blinding, complete follow-up, and the measurement of effects [3].
This study aims to identify factors critical to the applicability of a smart technology application to mobile health care. This is an urgent and critical topic for the following reasons. First, the worldwide market for mobile health care is predicted to grow from an estimated 134 billion in 2016 to 280 billion by 2021 [13]. The market scale is large with numerous opportunities for related industries and companies. Additionally, the Affordable Care Act (ACA) and related efforts in the United States are moving health services from fee-for-service (FFS) models to managed care, value-added payment or value-based (VB) models that may be built on smart technology applications [14]. More recently, advances in cloud computing and big data analytics [15] have enabled the analysis of massive data collected from mobile users via smart technologies in real time. With use of earlier technological applications quickly becoming obsolete, this is a critical step to achieve more precise recommendations for individualized care services.
This study also compares the relative importance levels of the identified critical factors. To this end, the fuzzy geometric mean-fuzzy analytic hierarchy process (FGM-FAHP) approach is proposed. The FGM-FAHP approach aggregates multiple experts’ judgments on the relative importance levels of critical factors and derives the weight for each. These weights provide valuable information to manage activities on the realization of the critical factors under limited resources [16]. In addition, a judgment modification mechanism is also incorporated in the FGM-FAHP approach, so that an expert can modify his/her judgment subjectively if that deviates considerably from the consensus, which was not considered in [17]. Further, experts can be of unequal authority levels, so that the decision-making process can be led by an authoritative professional, which is another novelty of this study when compared to earlier studies [17], [18], [19].
The remainder of this paper is organized as follows. The next section introduces and categorizes smart technologies and discusses how they can be applied to mobile health care. Various factors critical to the applicability of a smart technology to mobile health care are then identified. The third section details the FGM-FAHP approach to assess the relative importance levels of the identified critical factors. The fourth section presents the results of applying the FGM-FAHP approach to assisting the government of a region in allocating its budget among smart technologies for mobile health care. The fifth section discusses the challenges involved and opportunities for enhancing the effectiveness of existing smart technology applications to mobile health care. The last section makes concluding remarks.
Literature review
A scoping literature review has been performed with relevant citations sourced from Google Scholar from published works over the last ten years being reviewed and clustered into three themes: (a) smart technologies; (b) smart technology applications to mobile health care; and (c) the digital transformation of health care using smart technologies.
Classification of smart technologies
Van Doorn [20] classified smart technologies and systems into four categories, as shown in Table 1 .
Table 1.
Classification of smart technologies and systems.
| Category | Smart Technologies and Systems |
|---|---|
| Wirelessly connected smart systems | Internet of things, smart TV, smart baby monitors, smart phones, smart watches, smart wallets, smart motion sensors, smart smoke alarms, smart glasses, spectacles, and contact lenses, smart body analyzers, smart thermostats, smart cities |
| Interactive smart systems | Smart tables, smart boards, smart burglar alarms, smart fridges, smart cookers, smart washing machines, smart light bulbs, smart meters, smart plugs |
| Predictive smart systems | Smart hard drives, smart connected vehicles, smart buildings, smart traffic lights, smart surveillance cameras, smart toilets, smart wigs, smart farms, smart grids, smart shelves |
| Intelligent smart systems | Smart WiFi, smart mobile services, smart restart, smart defense, smart pajamas, smart vacuum cleaners, smart travel cards, smart wheelchairs, sleep-monitoring systems |
Obviously, not all of existing smart technologies are applicable in a mobile setting. Wu et al. [21] applied the technology acceptance model (TAM) and the theory of planned behavior (TPB) to sort out key factors influencing the adoption of smart technologies for mobile health by care professionals. They concluded from a questionnaire survey that perceived service availability (PSA) and personal innovativeness in information technology (PIIT) were the most critical factors. Other researchers such as Demirkan [22], Chen & Chiu [23], and Chen [17] have similarly encouraged using smart technology applications for mobile environments, all of which has been summarized in Table 2 .
Table 2.
Smart technology applications suitable for mobile environments.
| Reference | Suitable Smart Technology Applications |
|---|---|
| Chen [17] | Smart mobile services, smart phones, smart watches, smart connected vehicles, smart smoke alarms, smart motion sensors |
| Demirkan [22] | Biosensors, wearable devices, intelligent software agents. |
| Chen and Chiu [23] | Smart watches, smart motion sensors, smart body analyzers, smart connected vehicles, smart wigs, smart mobile services, smart defense technologies, smart wheelchairs |
Based on the scoping review of recent publications, not only should a smart mobile health care technology be interconnected, unobtrusive, and adaptable, but it also must be characterized as dynamic, embedded, and intelligent [24]. Table 3 shows how these various requirements are being met by a selection of existing smart technologies that are beginning to be diffused in developed and developing countries.
Table 3.
The checking results.
| Smart Technology | Requirement |
|||||
|---|---|---|---|---|---|---|
| Unobtrusive | Interconnected | Adaptable | Dynamic | Embedded | Intelligent | |
| Smart clothes | No | Yes | No | Yes | Yes | Yes |
| Smart glasses | No | Yes | Yes | Yes | No | Yes |
| Smart watches | Yes | Yes | Yes | Yes | No | Yes |
| Smart phones | Yes | Yes | Yes | Yes | No | Yes |
| Smart motion sensors | Yes | Yes | No | No | No | Yes |
| Smart smoke alarms | Yes | Yes | No | No | No | Yes |
| Smart body analyzers | Yes | Yes | No | Yes | No | Yes |
| Smart connected vehicles | Yes | Yes | Yes | Yes | No | Yes |
| Smart toilets | Yes | Yes | No | No | No | Yes |
| Smart wigs | Yes | Yes | No | Yes | No | Yes |
| Smart mobile services | Yes | Yes | Yes | Yes | Yes | Yes |
| Smart defense technologies | Yes | Yes | No | Yes | No | Yes |
| Smart wheelchairs | Yes | Yes | No | Yes | No | Yes |
Among them, smart mobile services meet all the requirements. Smart phones, smart watches, and smart connected vehicles also meet most of the requirements. Such results explain why smart phones and smart watches are the most widely applied smart technologies to mobile health care, and why the interest in smart connected vehicles is increasing. Conversely, the interest in smart glasses is decreasing, mostly because smart glasses are obtrusive. Smart clothes are also facing a decline in interest owing to the same reason.
Smart technologies applications to mobile health care
Among smart technological devices widely adopted for mobile health care services, smart phones are clearly the most prevent [25]. The sensors on a smart phone assist the mobile health care of users in a variety of ways [26]:
-
•
Single sensor function, for example, the GPS receiver may be used to inform the location of a user [27], and the camera to transmit a visual of the injured part, or to enable video-conferencing with a distant doctor.
-
•
Multi-sensor collaboration, for example, whether an individual has fallen may be ascertained by jointly applying the accelerometer, compass, and gyroscope on one's smart phone. Even so, the data collected by various sensors may be multifaceted with the ongoing challenge of aggregating them [28].
-
•
Multi-device collaboration, for example, a smart phone may be coupled with another smart device, typically a smart watch [29, 30], smart glasses [31], or smart clothing [32], to compensate for the inability to measure some health conditions.
Altogether, a mobile health care app supports a wide variety of useful and meaningful functions. Table 4 presents a taxonomy of such functions as noted in previous research.
Table 4.
The classification of functions supported by mobile health care apps.
| Target Population | Functions | References |
|---|---|---|
| Consumers or patients | ● Medication compliance ● Mobile and home monitoring ● Home care ● Managing conditions ● Wellness/fitness |
Chen [27], Sarasohn-Kahn [33], Brusse et al. [37], Chiou et al. [38], Boulos et al. [39] |
| Health care professionals | ● Alerts ● Medical reference tools ● Diagnostic tools ● Health record maintenance and access ● Information and time management ● Communications and consulting ● Patient management and monitoring ● Medical education and training |
Sarasohn-Kahn [33], Ventola [34] |
| System designer or administrator | ● Resource and communication abstraction ● Biomedical data acquisition ● Health knowledge extraction ● Persistent data storage ● Adaptive visualization ● System management ● Value-added services (e.g., intelligent alerts, recommendations, and guidelines) |
Amin et al. [28], Banos et al. [35] |
Generally speaking, the majority of people who use mobile health care apps are patients and consumers. In contrast, health care professionals rarely use such apps that may be considered to be inaccurate and unsafe for providers to rely upon in administering care [33, 34]. As of June 2017, approximately 250 free health-care-related apps with four stars or higher ratings by their users on Google Play [36]. The apps may be classified into five major types:
-
•
Apps that use smart phone devices to monitor, measure, track, or calculate the health conditions (such as blood pressure, heart rate, and blood oxygen) of mobile users.
-
•
Apps that introduce or recommend healthy habits, activities, sports, food, nutrition, stores, clinics, and others to users [27]. Such apps are usually coupled with a navigation service like Google Maps.
-
•
Apps that provide health-related tips, knowledge, Q&A, guides, advice, reports, and other services to users.
-
•
Apps that help users to book a clinic or order medicine. This type pf apps are always accompanied with a navigation service.
-
•
Others.
The percentages of the five types of apps are compared in Fig. 1 .
Fig. 1.
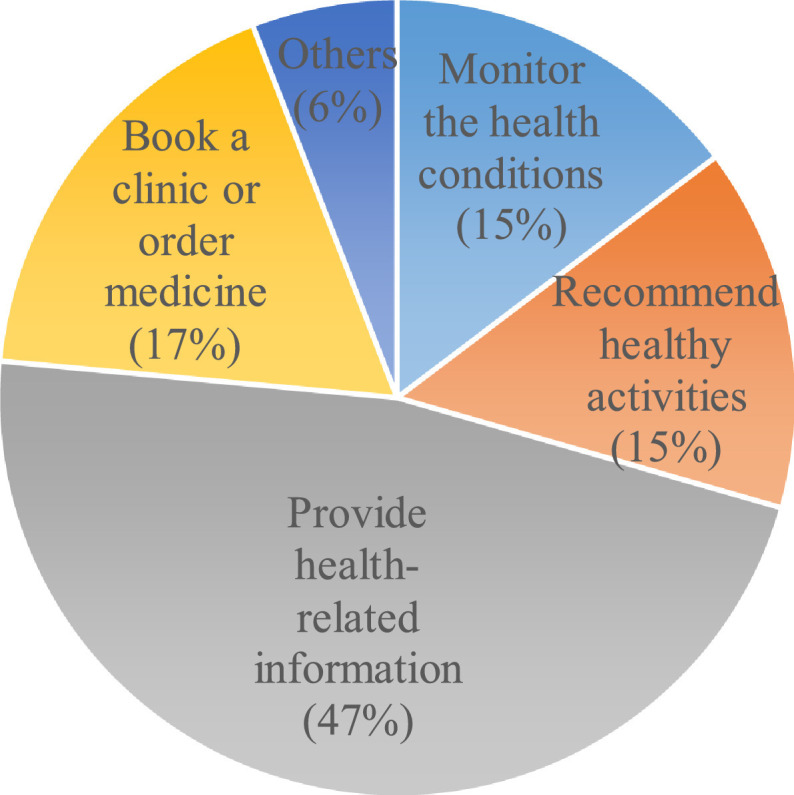
The percentages of the five types of apps.
Over the years, the rapid proliferation of smart technological apps has resulted in several bundles of such apps trending towards new ways of delivering mobile health care services. In the past, apps and online social networks were disjointed ways to support mobile heath care [37]. Recently, a number of mobile health care apps have supported the forming of online social networks [38]. Some of these apps are based on the co-work of participants, while others are peer-led (i.e., led by people who have more experience or professional knowledge). In contrast, some apps for online social networking, such as Facebook and Line, have been applied to support mobile health care. People share health care related information and discuss with each other in such online social networks. In addition, rich multimedia, virtual reality, and augmented reality are also incorporated into a mobile health care app to provide vivid experiences of distant health care delivery [39]. In the past, it was pads or smart glasses that were usually adopted to support such functions [40, 41]. However, advances in smart phone technologies and the several advantages of a smart phone (e.g., light weight, unobtrusiveness, etc.) have made it a more suitable alternative in recent years.
Users with visual impairments usually rely on voice-based instructions. However, this is not possible in some situations such as meetings, crowded places, and noisy environments. To overcome this challenge, Porzi et al. [42] combined the use of a smart watch and a smart phone to develop a gesture recognition system for visual impaired users. When the smart watch detects a gesture made by the user, it will then transmit a signal to the smart phone to activate certain devices such as the screen or a camera. Where the camera is used to capture an image, the image could then be compared with several predefined images, representing certain risk, a specific location, or a facility. After that, the result is transmitted to the user via smart phone vibrations.
Another innovative means of applying smart technologies for mobile health care delivery is the work of Doukas et al. [43], which emphasizes on affording caregivers with enhanced accessibility and availability of a mobile healthcare information management system. Here, the authors established a system in which the health records and medical images of a patient may be placed on a cloud so that the patient data can now be ubiquitously accessed by the patient's attending doctor via a smart phone.
Applications of other smart technologies
Wile et al. [40] used the accelerometer on a smart watch to record the re-emergent postural tremors (4–6 Hz) of a patient with Parkinson's disease and differentiate them from essential tremors (5–8 Hz). Several decision rules have been established for one to make meaningful use of the wave forms of the recorded results. Reasoning, or more specifically, pattern analysis [40] and/or pattern recognition [42], plays a key role in the continuing use and successful adoption of a smart watch application.
Linner et al. [44] identified an increasing shortage of caregivers in highly industrialized countries, particularly for elderly people. This problem can be overcome by using service robots. For example, Care-O-bot 4 is a service robot composed of a transportation unit, a telepresence unit, a telemanipulation system, and a two-armed structure. The robot can deliver food or drinks, assist with cooking, and clean [45]. Instead of developing a more sophisticated service robot, Linner et al. [44] employed multiple cooperating service robots (i.e., a service robot system). Various types of service robots were selected to fit the layout and furniture of a room and to compensate for each other. Moreover, sensors were installed throughout the room to detect signals for activating these service robots. Advantages of applying robotic technologies to health care in serving as flexible physical assistant substitutes have been summarized in Linner et al. [44]. Importantly, their work showed how robotic technologies can extend human intelligence, improve situation awareness, and offer novel methods of intuitive man–machine interaction.
However, according to the review results by Kumar et al. [46], although the applications of smart technologies to mobile health care were innovative and appealing, their efficacy still lacked sufficient evidence. In addition, a major barrier hampering the existing applications of smart technologies is the related laws that restrict the possibility of distant medical care [47].
Smart technologies for the digital transformation of health care services
Mobile health care relies heavily on long-distance data transmission. The digital nature of smart technologies confers an advantage in this regard. For example, a traditional electromyogram (EMG) sensor for monitoring muscle and neural activities is usually analog [48], which is not suitable for long-distance data transmission. To address this issue, a number of digital EMG sensors have been invented [49].
A digital sensor can achieve a high accuracy. For example, Wile et al. [40] used a smart watch to detect the re-emergent postural tremors of a patient with Parkinson's disease. The experimental results obtained using a smart watch were comparable to those obtained using an attached analog accelerometer. In addition, the use of a smart watch increased the ease and portability of routine measurement, as well as patients’ willingness to perform it.
In telehealth (or telemedicine), smart technologies can often aid in digitalizing the physician-patient interactions, so that many routine encounters such as contact, care, advice, reminders, education, intervention, monitoring, and remote admissions may be done more efficiently and at much lower costs even when the two parties are distant apart. Telehealth applications are particularly useful when an epidemic is highly infectious. For example, in the current China-led coronavirus situations [50], it would be much safer for would-be “quarantined” or “potentially infected” patients to interact with their doctors virtually than face-to-face [51].
In addition, advances in three-dimensional (3D) printing (or additive manufacturing) technologies are also conducive to the digital transformation of medical services such as transplantation. Traditionally, the organ required by a patient has to be prepared and transported to the hospital where the patient is. Now, the 3D file of the required organ can be transmitted via the Internet to the 3D printer of the hospital to print without transportation [52].
The prevalence of the Internet has raised many opportunities for the digitization of health care services. Without the Internet, digital medical records must be transported physically. By contrast, placing medical information on a cloud makes it easier to share such information across regions [43]. Today, cross-border transportation has become more and more convenient. As a result, the global spread of disease has become faster. Easily and quickly sharing the medical information at hand is a viable way for different regions to cooperate in fighting the same disease.
The fgm-fahp approach
To determine the relative importance levels of critical factors, the FGM-FAHP approach is proposed in this study. This approach comprises two phases: FGM for aggregating the pairwise comparison results by all experts (Phase 1), and FAHP for deriving the weights of critical factors (Phase 2), as described below.
FGM (Phase 1)
In Phase 1 of the proposed methodology, we first gather P experts from the related fields are gathered. In the extant literature, the value of P ranges from 3 to 30 [53]. With more experts, more diversified judgments may be sourced. However, it also becomes difficult for experts to reach a consensus. Smart technology applications for mobile health care is a relative new issue. It is not easy to gather a number of qualified experts for this issue. In addition, involving many experts may not be conducive to reaching a consensus.
Each expert compares the importance levels of critical factors in pairs. Only positive comparisons are accepted, i.e., a critical factor is more important than another to some degree. The accepted ratio is 0.5. Assuming the relative importance of critical factor i over critical factor j compared by domain expert p is indicated with ; i, j = 1–9; i ≠ j; p = 1–P. The following linguistic terms are provided to the experts to choose from [54]:
As important as:
Slightly more important than:
Considerably more important than:
Extremely more important than:
Absolutely more important than:
All parameters and variables in the proposed methodology are given in or approximated with triangular fuzzy numbers (TFNs). In addition, after is chosen, its counterpart is set as
| (1) |
to be consistent with the following FAHP operation and avoid the unnecessary increase in the uncertainty. Then, the comparison results by the experts are aggregated using FGM:
| (2) |
where is the aggregation result of the relative importance of critical factor i over critical factor j. ωp is the authority level of expert p; ωp ∈ R +. is no longer a TFN, but can be approximated with a TFN as
| (3) |
where
| (4) |
| (5) |
| (6) |
Subsequently, the fuzzy pairwise comparison matrix can be constructed based on the values of {}.
Finally, experts whose judgments are too far away from the aggregated result will be asked to modify their judgments. The authority level of an expert who refuses to modify his/her assessment will be adjusted until the distance between each expert's judgment and the aggregated result is small enough.
FAHP (Phase 2)
FAHP [55] is subsequently applied to derive the weight of each critical factor. Let be the fuzzy pairwise comparison matrix
| (7) |
The fuzzy maximal eigenvalue () and the corresponding fuzzy eigenvector () of satisfy the following equation:
| (8) |
where (–) and (×) denote fuzzy subtraction and multiplication, respectively; I is the identity matrix.
α-cut operations can be applied to solve for and ,
| (9) |
and
| (10) |
α = 0–1. If they are approximated with TFNs, then
| (11) |
and
| (12) |
Theorem 1
can be approximated as [ 55 ]
(13)
determines the importance (weight) of critical factor i.
Theorem 2
(14)
Proof
(13) is a fuzzy weighted average (FWA) problem that can be solved by applying α-cut operations:
(15)
Therefore,
| (16) |
where
| (17) |
| (18) |
| (19) |
Theorem 2 is proved.
The fuzzy consistency ratio () can be used to assess whether there is enough consensus among the experts:
| (20) |
where RI is the random consistency index (see Table 5 ) [56]. It is expected that ≤ 0.1 [56].
Table 5.
The random index.
| n | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RI | 0 | 0 | 0.58 | 0.9 | 1.12 | 1.24 | 1.32 | 1.41 | 1.45 | 1.49 | 1.51 | 1.48 | 1.56 | 1.57 | 1.59 |
An experiment
The FGM-FAHP approach has been applied to assist the government of a region in allocating its budget for developing smart technologies for mobile health care. To this end, six experts (including a professor researching smart technology management, two health care professionals, an assistant professor of health policy and management, and two professors of technology management) were asked to perform pairwise comparisons of factors critical to the applicability of a smart technology to mobile health care. From the scoping review, five critical factors have been identified as relevant in deploying smart technologies within a mobile health context:
-
•
Unobtrusiveness.
-
•
Supporting online social networking.
-
•
The relaxation of the related medical laws.
-
•
The size of the health care market.
-
•
The correct identification of the need and situation of a user.
The pairwise comparison results by the experts are summarized in Table 6 .
Table 6.
The results of pairwise comparisons.
| p | Pairwise Comparison Results |
|---|---|
| 1 | (i) “Unobtrusiveness” is considerably more important than “supporting online social networking”. (ii) “The relaxation of the related medical laws” is slightly more important than “unobtrusiveness”. (iii) “Unobtrusiveness” is extremely more important than “the size of the health care market”. (iv) “Unobtrusiveness” is considerably more important than “the correct identification of a user's need and situation”. (v) “The relaxation of the related medical laws” is considerably more important than “supporting online social networking”. (vi) “Supporting online social networking” is considerably more important than “the size of the health care market”. (vii) “The correct identification of a user's need and situation” is slightly more important than “supporting online social networking”. (viii) “The relaxation of the related medical laws” is considerably more important than “the size of the health care market”. (ix) “The relaxation of the related medical laws” is slightly more important than “the correct identification of a user's need and situation”. (x) “The correct identification of a user's need and situation” is extremely more important than “the size of the health care market”. |
| 2 | (i) “Unobtrusiveness” is slightly more important than “supporting online social networking”. (ii) “The relaxation of the related medical laws” is considerably more important than “unobtrusiveness”. (iii) “Unobtrusiveness” is considerably more important than “the size of the health care market”. (iv) “Unobtrusiveness” is slightly more important than “the correct identification of a user's need and situation”. (v) “The relaxation of the related medical laws” is considerably more important than “supporting online social networking”. (vi) “Supporting online social networking” is considerably more important than “the size of the health care market”. (vii) “The correct identification of a user's need and situation” is considerably more important than “supporting online social networking”. (viii) “The relaxation of the related medical laws” is extremely more important than “the size of the health care market”. (ix) “The relaxation of the related medical laws” is slightly more important than “the correct identification of a user's need and situation”. (x) “The correct identification of a user's need and situation” is considerably more important than “the size of the health care market”. |
| 3 | (i) “Unobtrusiveness” is extremely more important than “supporting online social networking”. (ii) “The relaxation of the related medical laws” is slightly more important than “unobtrusiveness”. (iii) “Unobtrusiveness” is considerably more important than “the size of the health care market”. (iv) “Unobtrusiveness” is slightly more important than “the correct identification of a user's need and situation”. (v) “The relaxation of the related medical laws” is considerably more important than “supporting online social networking”. (vi) “Supporting online social networking” is slightly more important than “the size of the health care market”. (vii) “Supporting online social networking” is slightly more important than “the correct identification of a user's need and situation”. (viii) “The relaxation of the related medical laws” is considerably more important than “the size of the health care market”. (ix) “The relaxation of the related medical laws” is slightly more important than “the correct identification of a user's need and situation”. (x) “The correct identification of a user's need and situation” is extremely more important than “the size of the health care market”. |
| 4 | (i) “Supporting online social networking” is as important as “unobtrusiveness”. (ii) “The relaxation of the related medical laws” is slightly more important than “unobtrusiveness”. (iii) “Unobtrusiveness” is extremely more important than “the size of the health care market”. (iv) “Unobtrusiveness” is slightly more important than “the correct identification of a user's need and situation”. (v) “The relaxation of the related medical laws” is slightly more important than “supporting online social networking”. (vi) “Supporting online social networking” is considerably more important than “the size of the health care market”. (vii) “Supporting online social networking” is as important as “the correct identification of a user's need and situation”. (viii) “The relaxation of the related medical laws” is considerably more important than “the size of the health care market”. (ix) “The relaxation of the related medical laws” is slightly more important than “the correct identification of a user's need and situation”. (x) “The correct identification of a user's need and situation” is extremely more important than “the size of the health care market”. |
| 5 | (i) “Unobtrusiveness” is slightly more important than “supporting online social networking”. (ii) “Unobtrusiveness” is considerably more important than “the relaxation of the related medical laws”. (iii) “Unobtrusiveness” is slightly more important than “the size of the health care market”. (iv) “The correct identification of a user's need and situation” is slightly more important than “unobtrusiveness”. (v) “Supporting online social networking” is slightly more important than “the relaxation of the related medical laws”. (vi) “Supporting online social networking” is considerably more important than “the size of the health care market”. (vii) “Supporting online social networking” is slightly more important than “the correct identification of a user's need and situation”. (viii) “The relaxation of the related medical laws” is slightly more important than “the size of the health care market”. (ix) “The correct identification of a user's need and situation” is considerably more important than “the relaxation of the related medical laws”. (x) “The correct identification of a user's need and situation” is considerably more important than “the size of the health care market”. |
| 6 | (i) “Unobtrusiveness” is slightly more important than “supporting online social networking”. (ii) “The relaxation of the related medical laws” is slightly more important than “unobtrusiveness”. (iii) “Unobtrusiveness” is extremely more important than “the size of the health care market”. (iv) “Unobtrusiveness” is slightly more important than “the correct identification of a user's need and situation”. (v) “Supporting online social networking” is slightly more important than “the relaxation of the related medical laws”. (vi) “Supporting online social networking” is slightly more important than “the size of the health care market”. (vii) “The correct identification of a user's need and situation” is considerably more important than “supporting online social networking”. (viii) “The relaxation of the related medical laws” is slightly more important than “the size of the health care market”. (ix) “The relaxation of the related medical laws” is slightly more important than “the correct identification of a user's need and situation”. (x) “The correct identification of a user's need and situation” is extremely more important than “the size of the health care market”. |
The pairwise comparison results were mapped to the corresponding TFNs that were then aggregated using FGM. The authority levels of the experts were 1.0, 1.25, 1.25, 1.25, 1.0, and 1.0, respectively. The results are summarized in Table 7 .
Table 7.
The aggregation results using FGM (only positive comparisons are shown).
| TFN | |
|---|---|
| (1.29, 3.09, 4.35) | |
| (3.26, 5.45, 7.52) | |
| (0.93, 2.34, 4.14) | |
| (2.08, 4.22, 6.26) | |
| (0.92, 2.21, 3.56) | |
| (1.10, 2.04, 3.70) | |
| (2.38, 4.57, 6.64) | |
| (0.75, 2.01, 3.35) | |
| (0.69, 1.40, 2.43) | |
| (4.22, 6.26, 8.28) |
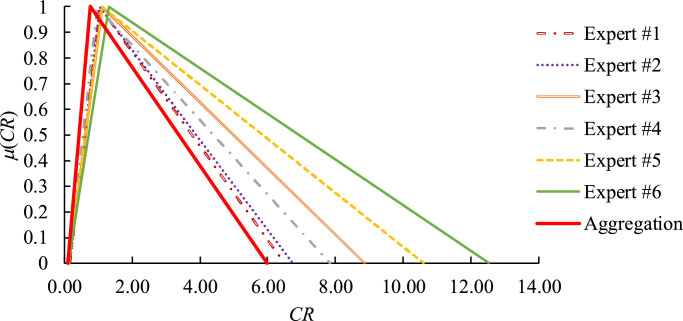
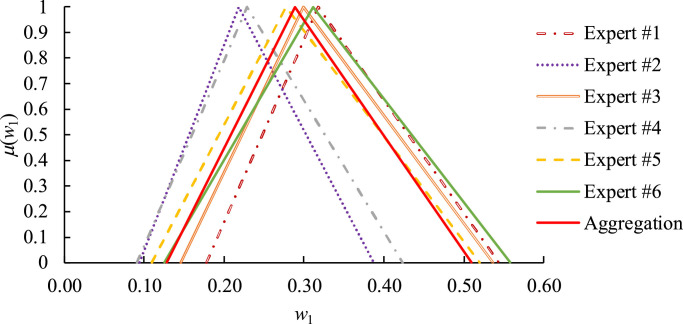
Consistency improved after aggregating these experts’ judgments, as illustrated in Fig. 2 . In addition, taking as an example, the aggregation results were compared with those derived by the experts in Fig. 3 . Obviously, the results derived by Expert #2 were farthest from the aggregation result. Therefore, Expert #2 was asked to modify his pairwise comparison results subjectively by considering the aggregation results (i.e. Table 7). After consideration, Expert #3 made the following modifications:
Fig. 2.
Consistency improved after aggregation.
Fig. 3.
Comparing the aggregation results with those derived by the experts.
The aggregation results after modification are shown in Table 8 . was improved from (0.09, 0.76, 6.0) to (0.08, 0.75, 6.1).
Table 8.
The aggregation results after modification.
| TFN | |
|---|---|
| (1.29, 3.09, 4.35) | |
| (3.02, 5.23, 7.30) | |
| (0.93, 2.34, 4.14) | |
| (2.08, 4.22, 6.26) | |
| (0.75, 2.01, 3.35) | |
| (1.10, 2.04, 3.70) | |
| (2.38, 4.57, 6.64) | |
| (0.75, 2.01, 3.35) | |
| (0.69, 1.40, 2.43) | |
| (4.22, 6.26, 8.28) |
The fuzzy maximal eigenvalue () and the corresponding fuzzy eigenvector () of were derived using α-cut operations as
| (21) |
| (22) |
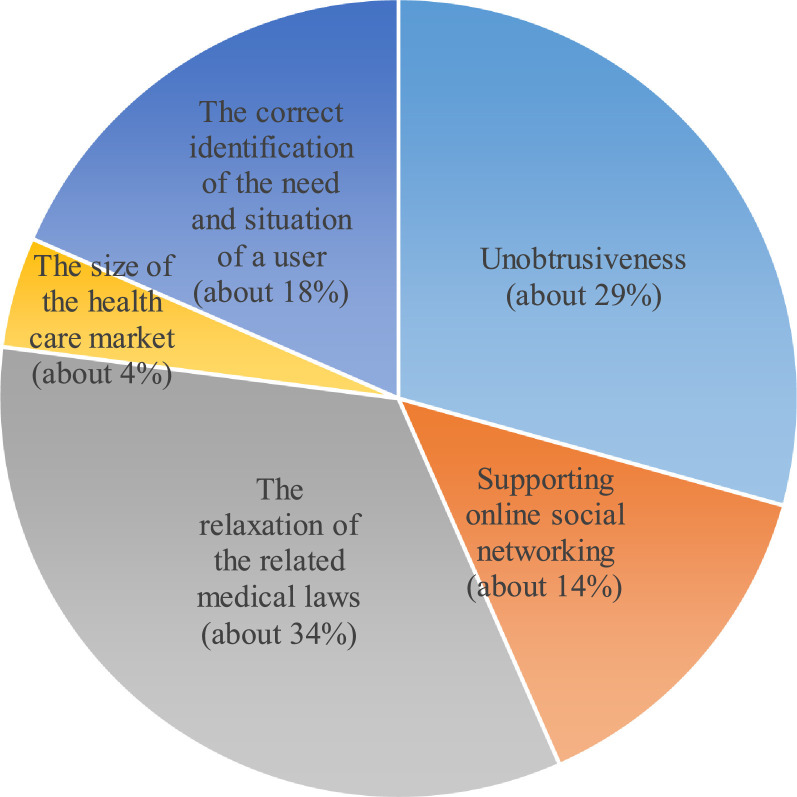
Based on the experimental results, the following observations can be made:
-
•
The relaxation of the related medical laws may be considered the most important factor, followed by unobtrusiveness, and then the correct identification of the need and situation of a user.
-
•
The derived fuzzy weights could be used to guide the government of a region in allocating its budget, as shown in Fig. 4 . It is noted that the values shown in this figure are flexible, since all weights are given in TFNs.
-
•The fuzzy consistency ratio was
which revealed that there was some consensus among experts since could be less than 0.1. However, the upper bound of the fuzzy consistency index was high, showing that there was considerable uncertainty behind such a judgement. Given that smart technology applications to mobile health care are still in their infancy, this finding was not surprising.(23) -
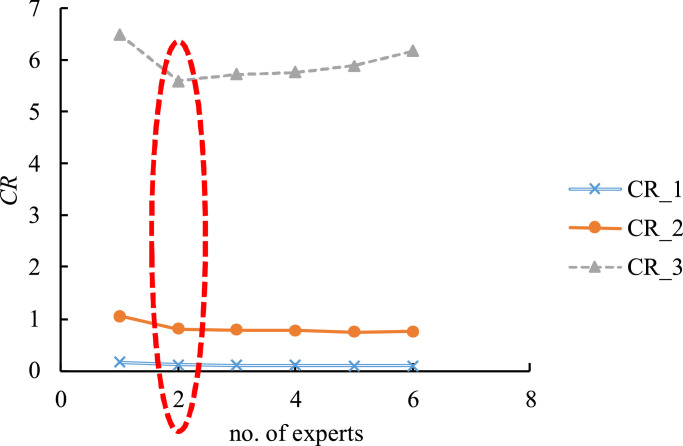
•
A parametric analysis was conducted to assess the effect of the number of experts (P) on the fuzzy consistency ratio (). The results are shown in Fig. 5 . In this experiment, two experts were sufficient to minimize (or optimize) . However, such a conclusion was based on consistency only. Involving more experts, so as to consider diversified viewpoints, was also meaningful to the practice.
-
•
Two existing methods, FGM-fuzzy extent analysis (FEA) [57] and the FGM-alpha cut operations (ACO)-FWA method [17], were also applied to the collected data for comparison. In the FGM-FEA method, experts’ judgments were aggregated using FGM. Then, the weight of a critical factor was set to its minimal degree of being the maximum. As a result, the weight of a critical factor was estimated in a crisp value and did not need to be defuzzified. In the FGM-ACO-FWA method, experts’ judgments were also aggregated using FGM. Then, the weight of a critical factor was derived using ACO. The results of applying various methods are compared in Table 9 . The results using the FGM-ACO-FWA method were close to those using the proposed methodology. However, the FGM-ACO-FWA method was not able to consider experts’ unequal authority levels. In addition, it was possible to obtain weights with zero values using the FGM-FEA method.
-
•
The execution time of the proposed methodology using MATLAB on a personal computer (PC) with an i7-7700 CPU of 3.6 GHz and 8 GB RAM was less than 1 s, while that of the FGM-ACO-FWA method was up to 21 s, which showed the effectiveness of the proposed methodology. In addition, experts were allowed to modify their judgments in the proposed methodology, but were not allowed in the FGM-ACO-FWA method.
Fig. 4.
The optimal allocation of budget.
Fig. 5.
The effect of the number of experts on the fuzzy consistency ratio.
Table 9.
Results of applying various methods.
| FGM-FEA | FGM-ACO-FWA | The Proposed Methodology | |
|---|---|---|---|
| 0.30 | (0.15, 0.30, 0.43) | (0.13, 0.29, 0.52) | |
| 0.18 | (0.07, 0.14, 0.27) | (0.06, 0.14, 0.32) | |
| 0.28 | (0.16, 0.33, 0.47) | (0.14, 0.34, 0.55) | |
| 0.00 | (0.03, 0.05, 0.08) | (0.02, 0.04, 0.11) | |
| 0.25 | (0.10, 0.19, 0.36) | (0.09, 0.18, 0.41) |
Further discussion – challenges and opportunities
Existing smart technology applications to mobile health care face several challenges. First, a mobile health care system should support users in an unobtrusive, interconnected, adaptable, dynamic, embedded, and intelligent manner [24]. However, it is difficult to invisibly integrate smart technologies into our daily lives [58]. Another issue is the lack of dedicated tools. Although a number of smart technologies can be applied to assist mobile health care delivery, tools specifically devised for implementing mobile health care are still lacking [35]. In addition, the real-time availability information of a service facility is critical to the effectiveness of a mobile healthcare service. However, most service facilities are reluctant to share their scheduling commitments with each other.
There are a number of issues associated with smart phone applications. First, using a smart phone actively or passively (e.g., hearing an alert without picking up the smart phone) affects the concentration of a user and may cause safety problems while walking, driving, or working [59]. It is even more difficult for people with low or impaired vision to use smart phones, which prevents them from using the related applications [42]. This difficulty can be resolved by providing them with screen readers or allowing them to give voice or gesture commands (with the aid of a smart watch) [42]. Even when a smart phone is used safely, detecting the location of the user by using the GPS module on his/her smart phone is subject to imprecision [29], which affects the quality of inputs to a health care app. Existing health care apps are also subjected to several difficulties [60]. For example, answering numerous questions is not always convenient to a mobile user. To address this problem, a “short-form” survey is usually adopted to assess the functional health and well-being of a mobile user [59]. However, addressing all the concerns of a mobile user by applying this method is impossible. This leads to misjudgment by the system server [60]. Other problems include the breach of a user's confidentiality, the conflicts of interests, malfunction, the lack of business models, and privacy issues [33].
Reasoning is the most critical yet difficult step in a mobile health care service [62, 63]. Conventional reasoning methods include Petri nets, mathematical programming, simulation, and ordered weighted average (OWA). Rossetti et al. [64] applied simulation to assess the benefits of using robots for transportation in a hospital. Augusto and Xie [65] formulated and solved a mixed-integer linear programming problem for planning the transportation and replenishment of medicine for the pharmacy of a hospital. Alfonso et al. [66] constructed a Petri net for modeling the mobile behaviors of blood donors. However, a Petri net is based on numerous assumptions on probability distributions and parameter independence. Chen [27] solved a fuzzy integer nonlinear programming problem to determine the no-wait path to each nearby clinic for a patient. Then, he applied OWA to determine the clinic that was most suitable for the patient. However, the method was either too theoretical or not adequately efficient for real-time applications. To solve this problem, a recent study proposed a heuristic that could be easily implemented for online applications [67]. However, the heuristic could not guarantee the global optimality of the recommendation.
Notwithstanding, several opportunities may leverage on extending the applications of smart technologies to mobile health care. For example, mobile health care systems based on apps are expected to increase. Such a trend offers clinics and hospitals opportunities to advertise themselves, elevates the users’ accessibility to clinics and hospitals, and helps balance the loads on participating facilities [24]. To this end, Banos et al. [35] developed a framework named mHealthDroid that could be referred to in developing apps for assisting the delivery of mobile health care services.
Another opportunity comes from advances in cloud computing. For example, the system server of a mobile health care system can be easily developed using a platform-as-a-service (PaaS) cloud service. The most notable benefit of using cloud computing is that the system administrator does not need to acquire, set up, or maintain the system software and hardware. Some cloud service providers such as Google Cloud can help develop system servers that support mobile apps. In addition, new techniques for balancing the loads on health care facilities and resources have been proposed in the recent years. Health care facilities and resources in a mobile health care system are recommended and allocated to users through the intervention of the system server, which attempts to balance the loads on health care facilities and resources to prevent them from congestion or underuse, thereby providing opportunities to improve their performance. For example, the average waiting time in a crowded clinic can be reduced, whereas the utilization of an infrequently visited clinic can be improved. In light of this, users’ requirements can be more effectively mapped to the capabilities of clinics and hospitals.
In sum, innovative methods of applying smart technologies to mobile health care remain to be ingeniously developed [68]. For example, the face of a driver can be captured and recognized to determine whether the driver is tired or drunk to initiate automatic driving for the driver's safety.
Conclusions
Smart technologies have been universally applied to mobile health care. However, there are still a number of difficulties hampering the effectiveness and efficiency of existing smart applications technologies to mobile health care. Identifying key factors and methods that can inform on the perceived applicability and practical innovativeness of smart technologies in mobile health care delivery are clearly some of the paramount steps in breaking down such difficulties. To this end, this study reviews the current practices of smart technologies to mobile health care. As a result, five critical factors were identified as unobtrusiveness, supporting online social networking, the relaxation of the related medical laws, the size of the health care market, and the correct identification of the need and situation of a user. Importantly, the FGM-FAHP approach is proposed to assess the relative importance of the identified critical factors. Compared with existing methods in this field, the FGM-FAHP approach is able to consider unequal experts’ authority levels and incorporates a modification mechanism to enhance consistency.
Moreover, an experiment has been conducted to further examine the effectiveness of the FGM-FAHP approach. After analyzing the experimental results, the following conclusions may be drawn:
-
•
The three most critical factors are the relaxation of the related medical laws, unobtrusiveness, and the correct identification of the need and situation of a user.
-
•
Accordingly, approximately 44%, 26%, and 15% of the budget should be allocated respectively towards achieving these three critical factors.
Depending on the target population, specific smart technology applications for mobile health can be compared using the proposed methodology in a future study. In addition, more sophisticated mechanisms needs to be designed to facilitate the aggregation or modification of expert judgments. These constitute some directions for future research.
Author Statements
Funding
This study was sponsored by the Ministry of Science and Technology, Taiwan, Republic of China under Grant MOST 106–2221-E-035–063-MY3.
Competing interests
None declared.
Ethical approval
Not required.
Acknowledgements
The author would like to thank the valuable comments of guest editor and reviewers for improving the quality of this paper.
References
- 1.Curtis D.W., Pino E.J., Bailey J.M., Shih E.I., Waterman J., Vinterbo S.A., Stair T.O., Guttag J.V., Greenes R.A., Ohno-Machado L. SMART—an integrated wireless system for monitoring unattended patients. Journal of the American Medical Informatics Association. 2008;15(1):44–53. doi: 10.1197/jamia.M2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jordan, M. (2011) What is ‘smart’ technology?http://knowit.co.nz/2011/08/what-is-smart-technology.
- 3.Free C., Phillips G., Galli L., Watson L., Felix L., Edwards P. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1) doi: 10.1371/journal.pmed.1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baek H.J., Chung G.S., Kim K.K., Park K.S. A smart health monitoring chair for nonintrusive measurement of biological signals. IEEE Transactions on Information Technology in Biomedicine. 2011;16(1):150–158. doi: 10.1109/TITB.2011.2175742. [DOI] [PubMed] [Google Scholar]
- 5.Baig M.M., Gholamhosseini H. Smart health monitoring systems: an overview of design and modeling. J Med Syst. 2013;37(2):9898. doi: 10.1007/s10916-012-9898-z. [DOI] [PubMed] [Google Scholar]
- 6.Jung H., Chung K. Sequential pattern profiling based bio-detection for smart health service. Cluster Comput. 2015;18(1):209–219. [Google Scholar]
- 7.Natarajan K., Prasath B., Kokila P. Smart health care system using internet of things. Journal of Network Communications and Emerging Technologies. 2016;6(3):37–42. [Google Scholar]
- 8.Kaewkungwal J., Singhasivanon P., Khamsiriwatchara A., Sawang S., Meankaew P., Wechsart A. Application of smart phone in “Better border healthcare program”: a module for mother and child care. BMC Med Inform Decis Mak. 2010;10(1):69. doi: 10.1186/1472-6947-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirata Y., Komatsuda S., Kosuge K. 2008 IEEE/RSJ International Conference on Intelligent Robots and Systems. 2008. Fall prevention control of passive intelligent walker based on human model; pp. 1222–1228. [Google Scholar]
- 10.Mutiara G.A., Hapsari G.I., Rijalul R. 2016 4th International Conference on Information and Communication Technology. 2016. Smart guide extension for blind cane; pp. 1–6. [Google Scholar]
- 11.Steinhubl S.R., Muse E.D., Topol E.J. Can mobile health technologies transform health care? JAMA. 2013;310(22):2395–2396. doi: 10.1001/jama.2013.281078. [DOI] [PubMed] [Google Scholar]
- 12.Vodopivec-Jamsek V., de Jongh T., Gurol-Urganci I., Atun R., Car J. Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews. 2008:12. doi: 10.1002/14651858.CD007457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MarketsandMarkets Research (2011) Healthcare it market by product (EHR, RIS, PACS, VNA, CPOE, HIE, telehealth, healthcare analytics, population health management, supply chain management, CRM, fraud management, claims management) end user (provider, payer) - Global forecast to2021. http://marketsandmarkets.com/Market-Reports/healthcare-it-252.html
- 14.UIC (2016) Innovative strategies to address the mental health crisis. http://www.adjacentgovernment.co.uk/wp-content/uploads/2016/07/UIC-ebook-June-16-WEB.pdf
- 15.Bates D.W., Heitmueller A., Kakad M., Saria S. Why policymakers should care about “big data” in healthcare. Health Policy and Technology. 2018;7(2):211–216. [Google Scholar]
- 16.Mukherjee K. A smart framework for hta capability development: lessons from India. Health Policy and Technology. 2019:1–7. [Google Scholar]
- 17.Chen T.C.T. Evaluating the sustainability of a smart technology application to mobile health care: the FGM–ACO–FWA approach. Complex & Intelligent Systems. 2019:1–13. [Google Scholar]
- 18.Lin Y.C., Wang Y.C., Chen T.C.T., Lin H.F. Evaluating the suitability of a smart technology application for fall detection using a fuzzy collaborative intelligence approach. Mathematics. 2019;7(11):1097. [Google Scholar]
- 19.Chen T.C.T., Wang Y.C., Lin Y.C., Wu H.C., Lin H.F. A fuzzy collaborative approach for evaluating the suitability of a smart health practice. Mathematics. 2019;7(12):1180. [Google Scholar]
- 20.van Doorn, M. (2015) What does smart technology actually mean?http://labs.sogeti.com/wat-smart-technology-actually-mean/
- 21.Wu L., Li J.Y., Fu C.Y. The adoption of mobile healthcare by hospital’s professionals: an integrative perspective. Decis Support Syst. 2011;51(3):587–596. [Google Scholar]
- 22.Demirkan H. A smart healthcare systems framework. IT Prof. 2013;15(5):38–45. [Google Scholar]
- 23.Chen T., Chiu M.-C. Smart technologies for assisting the life quality of persons in a mobile environment - A review. J Ambient Intell Humaniz Comput. 2016 in press. [Google Scholar]
- 24.Ducatel, K., Bogdanowicz, M., Scapolo, F., Leijten, J., & Burgelman, J.-.C. (2001) Scenarios for ambient intelligence in 2010. IST Advisory Group Final Report, European Commission, Brussels.
- 25.Rathod, R. (2012) Sensors used in smartphone. http://myphonefactor.in/2012/04/sensors-used-in-a-smartphone/
- 26.Android Developers (2017) Sensors overview. https://developer.android.com/guide/topics/sensors/sensors_overview.html
- 27.Chen T. Ubiquitous multicriteria clinic recommendation system. J Med Syst. 2016;40:113. doi: 10.1007/s10916-016-0469-6. [DOI] [PubMed] [Google Scholar]
- 28.Amin M.B., Banos O., Khan W.A., Muhammad Bilal H.S., Gong J., Bui D., Cho S.H., Hussain S., Ali T., Akhtar U., Chung T.C., Lee S. On curating multimodal sensory data for health and wellness platforms. Sensors. 2016;16(7):980. doi: 10.3390/s16070980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen T. A fuzzy parallel processing scheme for enhancing the effectiveness of a dynamic just-in-time location-aware service system. Entropy. 2014;16:2001–2022. [Google Scholar]
- 30.Shcherbina A., Mattsson C.M., Waggott D., Salisbury H., Christle J.W., Hastie T. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J Pers Med. 2017;7(2):3. doi: 10.3390/jpm7020003. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lv Z., Feng L., Li H., Feng S. SIGGRAPH Asia 2014 Mobile Graphics and Interactive Applications. 2014. Hand-free motion interaction on google glass. 21-21. [Google Scholar]
- 32.Ma Y.C., Chao Y.P., Tsai T.Y. IEEE Third International Conference on Consumer Electronics. 2013. Smart-clothes—Prototyping of a health monitoring platform; pp. 60–63. [Google Scholar]
- 33.Sarasohn-Kahn, J. (2010) How smartphones are changing health care for consumers and providers. http://www.chcf.org/publications/2010/04/how-smartphones-are-changing-health-care-for-consumers-and-providers
- 34.Ventola C.L. Mobile devices and apps for health care professionals: uses and benefits. Pharmacy and Therapeutics. 2014;39(5):356. [PMC free article] [PubMed] [Google Scholar]
- 35.Banos O., Villalonga C., Garcia R., Saez A., Damas M., Holgado-Terriza J.A. Design, implementation and validation of a novel open framework for agile development of mobile health applications. Biomed Eng Online. 2015;14(2):56. doi: 10.1186/1475-925X-14-S2-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Google Play (2017) https://play.google.com/store/search?q=health&c=apps&rating=1
- 37.Brusse C., Gardner K., McAullay D., Dowden M. Social media and mobile apps for health promotion in australian indigenous populations: scoping review. J. Med. Internet Res. 2014;16(12) doi: 10.2196/jmir.3614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chiou W.K., Kao C.Y., Lo L.M., Huang D.H., Wang M.H., Chen B.H. International Conference of Design, User Experience, and Usability. 2017. Feasibility of utilizing e-mental health with mobile app interface for social support enhancement: a conceptional solution for postpartum depression in taiwan; pp. 198–207. [Google Scholar]
- 39.Boulos M.N.K., Lu Z., Guerrero P., Jennett C., Steed A. From urban planning and emergency training to pokémon go: applications of virtual reality gis (VRGIS) and augmented reality gis (ARGIS) in personal, public and environmental health. Int J Health Geogr. 2017;16(1):7. doi: 10.1186/s12942-017-0081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wile D.J., Ranawaya R., Kiss Z.H. Smart watch accelerometry for analysis and diagnosis of tremor. J. Neurosci. Methods. 2014;230:1–4. doi: 10.1016/j.jneumeth.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 41.Pallavicini F., Pedroli E., Serino S., Dell’Isola A., Cipresso P., Cisari C. Assessing unilateral spatial neglect using advanced technologies: the potentiality of mobile virtual reality. Technology and Health Care. 2015;23(6):795–807. doi: 10.3233/THC-151039. [DOI] [PubMed] [Google Scholar]
- 42.Porzi L., Messelodi S., Modena C.M., Ricci E. Proceedings of the 3rd ACM International Workshop on Interactive Multimedia on Mobile & Portable Devices. 2013. A smart watch-based gesture recognition system for assisting people with visual impairments; pp. 19–24. [Google Scholar]
- 43.Doukas C., Pliakas T., Maglogiannis I. 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology. 2010. Mobile healthcare information management utilizing cloud computing and android os; pp. 1037–1040. [DOI] [PubMed] [Google Scholar]
- 44.Linner T., Pan W., Georgoulas C., Georgescu B., Güttler J., Bock T. Co-adaptation of robot systems, processes and in-house environments for professional care assistance in an ageing society. Procedia Eng. 2014;85:328–338. [Google Scholar]
- 45.Care-O-bot 4 (2015) http://www.care-o-bot-4.de/
- 46.Kumar S., Nilsen W.J., Abernethy A., Atienza A., Patrick K., Pavel M. Mobile health technology evaluation: the mHealth evidence workshop. Am J Prev Med. 2013;45(2):228–236. doi: 10.1016/j.amepre.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hamel M.B., Cortez N.G., Cohen I.G., Kesselheim A.S. FDA regulation of mobile health technologies. The New England Journal of Medicine. 2014;371(4):372. doi: 10.1056/NEJMhle1403384. [DOI] [PubMed] [Google Scholar]
- 48.Circuit.rocks (2019) EMG analog sensor OYMotion gravity. https://circuit.rocks/emg-analog-sensor-oymotion-gravity.html
- 49.Shimmer (2019) Shimmer3 EMG unit. http://www.shimmersensing.com/products/shimmer3-emg-sensor.
- 50.Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China—Key questions for impact assessment. New England Journal of Medicine. 2020 doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 51.Phelan A.L., Katz R., Gostin L.O. The novel coronavirus originating in wuhan, china: challenges for global health governance. JAMA. 2020 doi: 10.1001/jama.2020.1097. [DOI] [PubMed] [Google Scholar]
- 52.Wang Y.C., Chen T., Lin Y.C. A collaborative and ubiquitous system for fabricating dental parts using 3D printing technologies. Healthcare. 2019;7(3):103. doi: 10.3390/healthcare7030103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pan N.F. Fuzzy AHP approach for selecting the suitable bridge construction method. Automation in Construction. 2008;17(8):958–965. [Google Scholar]
- 54.Stefanini, L., Sorini, L., Guerra, M.L. (2008) Fuzzy numbers and fuzzy arithmetic. Handbook of granular computing, pp. 249–83.
- 55.Ruoning X., Xiaoyan Z. Fuzzy logarithmic least squares ranking method in analytic hierarchy process. Fuzzy Sets and Systems. 1996;77(2):175–190. [Google Scholar]
- 56.Satty T.L. McGraw-Hill; New York: 1980. The analytic hierarchy process. [Google Scholar]
- 57.Chang D.Y. Applications of the extent analysis method on fuzzy ahp. Eur J Oper Res. 1996;95(3):649–655. [Google Scholar]
- 58.Linner T., Pan W., Georgoulas C., Georgescu B., Güttler J., Bock T. Co-adaptation of robot systems, processes and in-house environments for professional care assistance in an ageing society. Procedia Eng. 2014;85:328–338. [Google Scholar]
- 59.Nield, D. (2015) Study says smartphone notifications are ruining our concentration. http://www.digitaltrends.com/mobile/how-smartphones-distract-us-even-when-were-not-using-them/
- 60.Buijink A.W.G., Visser B.J., Marshall L. Medical apps for smartphones: lack of evidence undermines quality and safety. BMJ Evidence-Based Medicine. 2013;18(3):90–92. doi: 10.1136/eb-2012-100885. [DOI] [PubMed] [Google Scholar]
- 62.Jagtenberg C.J., Bhulai S., van der Mei R.D. Dynamic ambulance dispatching: is the closest-idle policy always optimal? Health Care Manag Sci. 2017;20(4):517–531. doi: 10.1007/s10729-016-9368-0. [DOI] [PubMed] [Google Scholar]
- 63.Khodaparasti S., Maleki H.R., Jahedi S., Bruni M.E., Beraldi P. Enhancing community based health programs in iran: a multi-objective location-allocation model. Health Care Manag Sci. 2017;20(4):485–499. doi: 10.1007/s10729-016-9366-2. [DOI] [PubMed] [Google Scholar]
- 64.Rossetti M.D., Felder R.A., Kumar A. Simulation of robotic courier deliveries in hospital distribution services. Health Care Manag Sci. 2000;3(3):201–213. doi: 10.1023/a:1019049609350. [DOI] [PubMed] [Google Scholar]
- 65.Augusto V., Xie X. Redesigning pharmacy delivery processes of a health care complex. Health Care Manag Sci. 2009;12(2):166–178. doi: 10.1007/s10729-008-9086-3. [DOI] [PubMed] [Google Scholar]
- 66.Alfonso E., Xie X., Augusto V., Garraud O. Modeling and simulation of blood collection systems. Health Care Manag Sci. 2012;15(1):63–78. doi: 10.1007/s10729-011-9181-8. [DOI] [PubMed] [Google Scholar]
- 67.Chen T. Enhancing the performance of a ubiquitous location-aware service system using a fuzzy collaborative problem solving strategy. Computers & Industrial Engineering. 2015;87:296–307. [Google Scholar]
- 68.Nembhard I.M., Lee Y.S.H. Time for more creativity in health care management research and practice. Health Care Manage Rev. 2017;42(3):191. doi: 10.1097/HMR.0000000000000171. [DOI] [PubMed] [Google Scholar]