Abstract
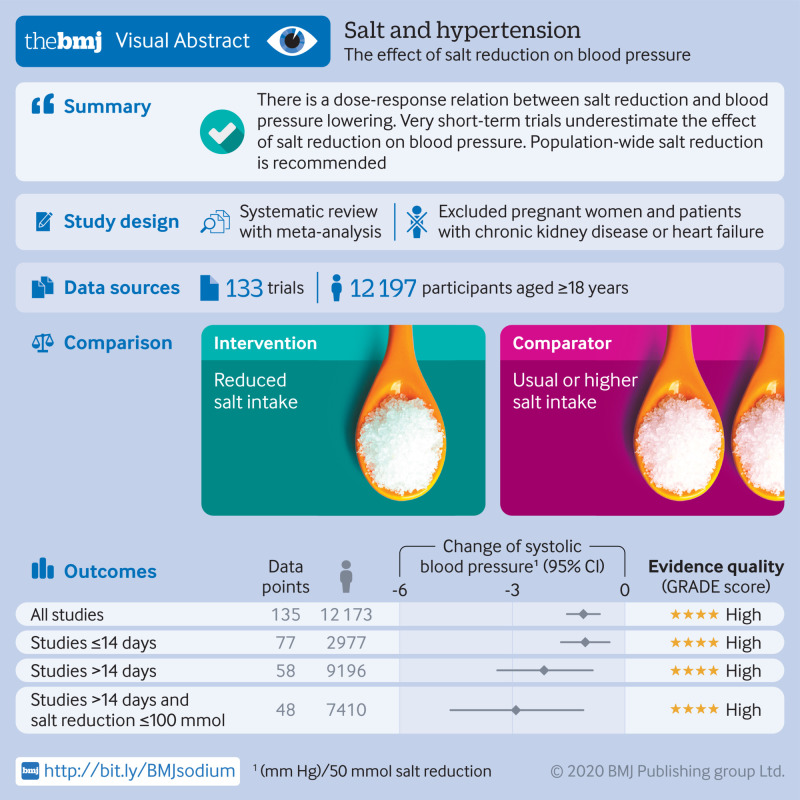
Objective
To examine the dose-response relation between reduction in dietary sodium and blood pressure change and to explore the impact of intervention duration.
Design
Systematic review and meta-analysis following PRISMA guidelines.
Data sources
Ovid MEDLINE(R), EMBASE, and Cochrane Central Register of Controlled Trials (Wiley) and reference lists of relevant articles up to 21 January 2019.
Inclusion criteria
Randomised trials comparing different levels of sodium intake undertaken among adult populations with estimates of intake made using 24 hour urinary sodium excretion.
Data extraction and analysis
Two of three reviewers screened the records independently for eligibility. One reviewer extracted all data and the other two reviewed the data for accuracy. Reviewers performed random effects meta-analyses, subgroup analyses, and meta-regression.
Results
133 studies with 12 197 participants were included. The mean reductions (reduced sodium v usual sodium) of 24 hour urinary sodium, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were 130 mmol (95% confidence interval 115 to 145, P<0.001), 4.26 mm Hg (3.62 to 4.89, P<0.001), and 2.07 mm Hg (1.67 to 2.48, P<0.001), respectively. Each 50 mmol reduction in 24 hour sodium excretion was associated with a 1.10 mm Hg (0.66 to 1.54; P<0.001) reduction in SBP and a 0.33 mm Hg (0.04 to 0.63; P=0.03) reduction in DBP. Reductions in blood pressure were observed in diverse population subsets examined, including hypertensive and non-hypertensive individuals. For the same reduction in 24 hour urinary sodium there was greater SBP reduction in older people, non-white populations, and those with higher baseline SBP levels. In trials of less than 15 days’ duration, each 50 mmol reduction in 24 hour urinary sodium excretion was associated with a 1.05 mm Hg (0.40 to 1.70; P=0.002) SBP fall, less than half the effect observed in studies of longer duration (2.13 mm Hg; 0.85 to 3.40; P=0.002). Otherwise, there was no association between trial duration and SBP reduction.
Conclusions
The magnitude of blood pressure lowering achieved with sodium reduction showed a dose-response relation and was greater for older populations, non-white populations, and those with higher blood pressure. Short term studies underestimate the effect of sodium reduction on blood pressure.
Systematic review registration
PROSPERO CRD42019140812.
Introduction
High blood pressure is a leading modifiable risk factor for cardiovascular disease, which caused at least 17.8 million deaths worldwide in 2017.1 A higher intake of dietary sodium is associated with a higher level of blood pressure in animals and humans.2 3 4 The physiological requirement for sodium in humans is less than 1 g a day,5 but currently most populations consume a much higher level.6 The maximum daily intake of dietary sodium recommended by the World Health Organisation (WHO) is 2 g (5 g salt) for adults,7 and most countries recommend reducing intake to less than 2.4 g a day8 9 as part of a dietary approach to prevent high blood pressure and cardiovascular disease.
The effect of sodium reduction on blood pressure and the risk of cardiovascular disease has been examined in numerous studies. Although there is a consensus among health and scientific organisations to reduce intake of dietary sodium in the general population,8 9 10 a few scientists have claimed that the benefit of sodium restriction for populations with normal blood pressure is small11 12 and could increase blood lipid levels and the risk of mortality.12 13 14 Others suggest that a higher risk of mortality at low sodium intake levels is an artefact attributable to factors such as reverse causation and biased estimation of sodium intake.15 16
The nature of the association between change in sodium intake and blood pressure is key to understanding the potential for health interventions based on sodium reduction. Previous overviews of the data were limited because a definitive dose-response relation could not be determined, especially for participants with normal blood pressure.12 17 18 19 A specific issue in previous meta-analyses was the inclusion of studies with sodium intake estimated from fractional urine samples.11 12 19 Fractional urine samples can produce overestimates of sodium intake when true intake is low but underestimates when true intake is high.20 Studies of short duration might also confound estimates of the average effect of change in sodium intake on blood pressure because large, short term reductions in sodium could elicit a different type of blood pressure response.21 A previous analysis that included 15 studies with measurements made at multiple time points was unable to determine whether effects of sodium reduction on blood pressure were sustained, declined, or increased with greater duration of intervention.22 The objective of this systematic review and meta-analysis was to examine the dose-response relation between dietary sodium reduction and blood pressure change, and to explore the impact of intervention duration, by applying more restricted inclusion criteria compared with previous reviews. The review was conducted with the support of the TRUE consortium.23
Methods
Search strategy
We carried out a search following a strategy developed for a previous meta-analysis21 that used keyword searches based on “sodium chloride, dietary,” “sodium, dietary,” or “diet, sodium-restricted” and “randomized controlled trial,” “controlled clinical trial,” or “randomized” (supplementary file 1). The databases searched included Ovid MEDLINE(R), EMBASE, and Cochrane Central Register of Controlled Trials (Wiley). The search date was from the start date of the databases to 21 January 2019. Additionally, we reviewed the references of pertinent original studies and review articles to identify additional studies. We imposed no language restriction on our search.
Inclusion and exclusion criteria
Two of three reviewers (LH, KT, and SY) independently assessed records identified from the search for eligibility. We resolved any discrepancies by consensus. We included only trials with random allocation of participants to reduced dietary sodium intake and usual/higher dietary sodium intake (that is, control). Trials with concomitant interventions (eg, non-pharmacological interventions, antihypertensive or other drugs) were included only if the other interventions were applied equally to all randomised groups of interest. We included only studies with sodium intake estimated by 24 hour urine collection that also had data on systolic blood pressure or diastolic blood pressure measurements. Studies with only mean arterial blood pressure reported were not included unless we could retrieve relevant data from the authors. We excluded studies conducted in children (age <18 years), pregnant women, or individuals with confounding chronic conditions such as chronic kidney disease or heart failure.
Study quality
Study quality was assessed independently by two reviewers based on the five domains defined by the Cochrane Collaboration’s tool for assessing risk of bias version 5.0.124; namely, random sequence generation, allocation concealment, blinding of participants, personnel and outcome assessors, incomplete outcome data, and selective outcome reporting.
Data extraction
One author (LH) extracted all data and two authors (KT and SY) reviewed the data for accuracy. Data sought for extraction included: characteristics of the study; demographics of the participants (race, mean age, percentage of female sex, percentage hypertension); study design (parallel group or crossover trial); risk of bias; duration of the intervention (calculated as the period from randomisation to the last follow-up measurement in parallel group studies and as the duration of each period of intervention, excluding run-in and washout, in crossover studies); 24 hour urinary sodium and blood pressure at baseline; and intervention effect on 24 hour urinary sodium and blood pressure.
For studies that only reported results as subgroups (eg, male and female subgroups), we obtained overall estimates as weighted averages based on the size of the subgroups for the primary analysis, following the Cochrane Handbook for Systematic Reviews of Interventions.24
Where available, data were extracted for subgroups defined by age, sex, ethnic group, and presence or absence of hypertension. We used casual blood pressure measurements rather than 24 hour ambulatory blood pressure if both were reported, and supine blood pressure was used ahead of standing blood pressure. In crossover studies, the last measurement of 24 hour urinary sodium and blood pressure at the highest sodium intake period was taken as the baseline.
The intervention effects on the 24 hour urinary sodium, systolic blood pressure, and diastolic blood pressure, were extracted directly from the studies, if reported. If not, we calculated them in crossover studies as the differences between the end of lowest sodium intake period (intervention) and the end of the highest sodium intake (control) period. For parallel studies, we calculated these as the differences between groups in the change from baseline to the last follow-up measurement.
Corresponding standard errors of each outcome were either extracted directly or calculated from standard deviations, confidence intervals, or exact P values following the Cochrane Handbook for Systematic Reviews of Interventions.24 If we could not derive the exact variance of the paired difference, we imputed it by assuming a correlation coefficient of 0.5 between the initial and final measurement following the same method used in a previous meta-analysis.21 We applied sensitivity analyses using different levels of correlation coefficients from 0.1 to 0.9 with 0.1 increments to check sensitivity to the assumption of a 0.5 correlation.
Statistical analysis
We used random effects meta-analysis, based on the DerSimonian and Laird method, to generate pooled estimates of the intervention effect on 24 hour urinary sodium excretion, systolic blood pressure, and diastolic blood pressure. We used the I2 statistic to examine the heterogeneity between trial results and used funnel plots and Egger’s regression test to detect potential publication bias.
To explore the dose-response relation, we summarised the changes in systolic and diastolic blood pressure by categorising trials into five equal groups (quintiles) based on the change in 24 hour urinary sodium excretion. We plotted studies with more than two levels of dietary sodium intake in a connected line graph.
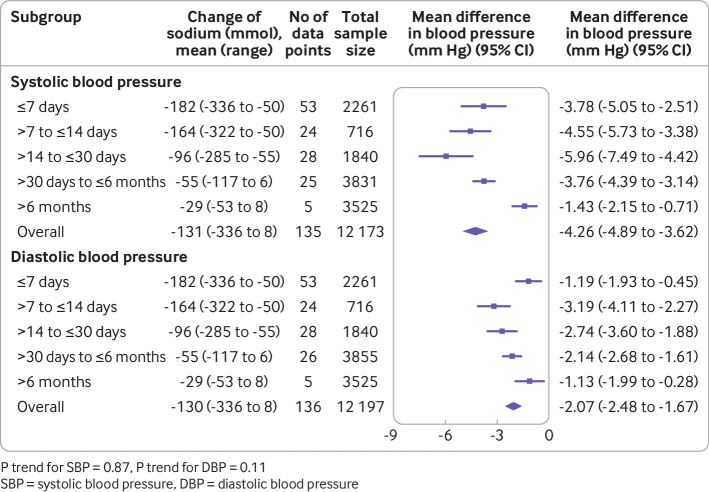
We assessed the effect of intervention duration on changes in blood pressure by grouping trials into five categories (≤7 days; >7 days to ≤14 days; >14 days to ≤30 days; >30 days to ≤6 months; >6 months). In addition, for studies with multiple follow-up measurements, we plotted the effects on blood pressure standardised to 50 mmol reduction of 24 hour urinary sodium against the duration of intervention in a connected line graph.
Age, sex, ethnic group, baseline sodium intake, and baseline blood pressure have been previously identified as potential modifiers of the effect of sodium reduction on blood pressure.21 We therefore summarised the effects on blood pressure for subgroups of trials (or subgroups within trials) defined by: mean age bands (≤35; >35 to ≤45; >45 to ≤55; >55 to ≤65; >65 years; unknown); sex (male; female; mixed; unknown); ethnicity (white; black; Asian; mixed race; unknown); mean baseline 24 hour sodium excretion (lowest <109 mmol; middle ≥109 to ≤209 mmol; highest >209 mmol)25; blood pressure status (normotensive; hypertensive; mixed; unknown); and mean baseline systolic blood pressure groups (<120; ≥120 to <130; ≥130 to <140; ≥140 to <150; ≥150 to <160, ≥160 mm Hg; unknown). The effects were standardised to a 50 mmol difference in 24 hour urinary sodium with variance estimated using the Taylor expansion.
To further explore the effects of these variables on blood pressure response to sodium reduction, we conducted unadjusted meta-regression for change in 24 hour urinary sodium, duration of intervention, mean age, percentage of white ethnicity, percentage of female sex, mean baseline blood pressure, and mean baseline 24 hour sodium excretion. We also did multivariable meta-regression including all covariates except for baseline 24 hour sodium excretion, which showed strong collinearity with the change in 24 hour urinary sodium (r=0.83). The following steps were undertaken to minimise missing data in the meta-regression analyses: if the studies did not report the participants’ race, this was imputed based on the study country (66 data points); if the percentage of female participants was not reported, the mean percentage of female of all other studies was used (8 data points); if only the age range was reported, the mean age was estimated as the mean of the minimum and maximum (12 data points); if neither mean age nor age range were reported, the mean age of all other studies was used (3 data points); and if baseline blood pressure was not reported, the mean value of all other studies was used (2 data points).
Short term studies are usually done using very restricted diets and could result in sudden large reductions in sodium intake that do not reflect medium or long term effects of sodium reduction on blood pressure.21 26 Accordingly, we conducted stratified analyses for studies with intervention duration of 14 days or less versus more than 14 days. For the same reason, we also did an analysis restricted to trials longer than 14 days with a 100 mmol or smaller reduction in 24 hour urinary sodium. All analyses were done using Stata (version 15.1, StataCorp, TX).
Patient and public involvement
Patients and the public were not involved in the design and conduct of this review.
Results
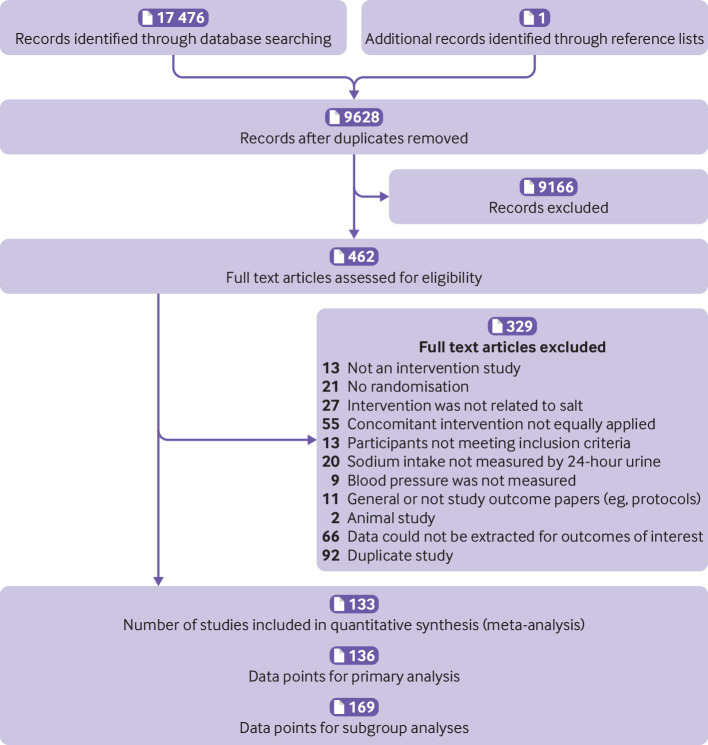
The search identified 17 477 records. After screening titles and abstracts, we selected 462 publications for full text review, of which 329 were excluded for the reasons summarised in figure 1. One hundred and thirty three studies27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 150 151 152 153 154 155 156 157 158 159 met our inclusion criteria, with 136 data points extracted for primary analyses involving 12 197 participants (fig 1) and 169 data points for various subgroup analyses. The characteristics of the included studies are presented in supplementary file 2. Fifty seven per cent (77/136) data points had intervention durations of up to 14 days, 21% (28/136) had intervention durations between 15 days and 30 days, 19% (26/136) had intervention durations longer than 30 days but within six months, and 4% (5/136) had intervention durations longer than six months.
Fig 1.
Flowchart for inclusion criteria
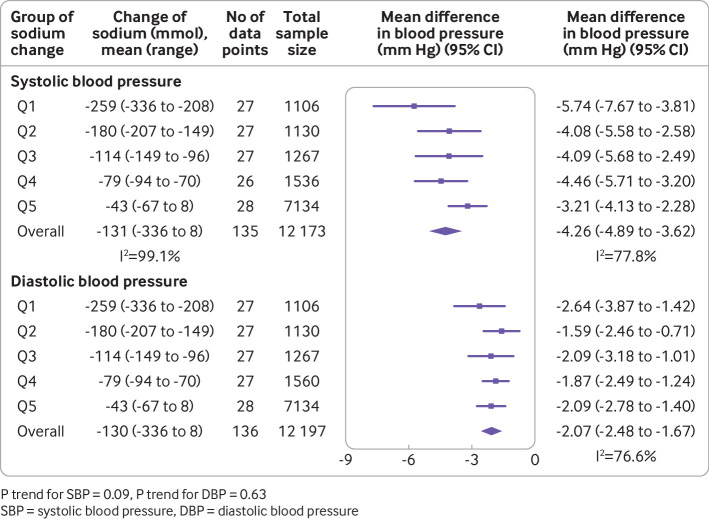
Overall, we saw a mean change of −130 mmol (95% confidence interval −145 to −115, P<0.001, I2=99.1%) in 24 hour urinary sodium, −4.26 mm Hg (−4.89 to −3.62, P<0.001, I2=77.8%) in systolic blood pressure, and −2.07 mm Hg (−2.48 to −1.67, P<0.001, I2=76.6%) in diastolic blood pressure (fig 2). We used different correlation coefficients to calculate the variance, which yielded similar pooled estimates of difference in systolic blood pressure (ranging from −4.59 mm Hg (−5.27 to −3.91) to −4.18 mm Hg (−4.59 to −3.51)) and diastolic blood pressure (ranging from −2.04 mm Hg (−2.46 to −1.63) to −2.13 mm Hg (−2.58 to −1.67)). Sodium reduction was associated with separately statistically significant reductions in blood pressure for most subgroups studied. As reflected by the I2 values, the magnitude of effect varied substantially between contributing trials, as well as between many of the subgroups (fig 3).
Fig 2.
Association of magnitude of sodium reduction (mmol) with size of blood pressure reduction (mm Hg)
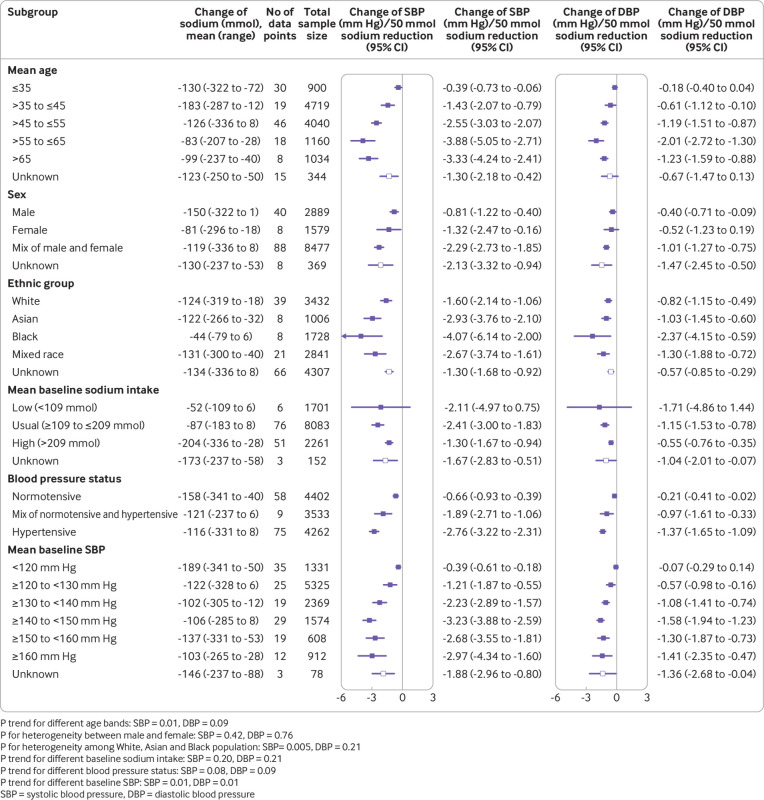
Fig 3.
Effects of age, sex, ethnicity, baseline sodium intake, baseline blood pressure, and blood pressure status on the size of blood pressure reduction (mm Hg) achieved with a 50 mmol reduction in sodium excretion
Association of magnitude of sodium reduction with size of blood pressure reduction
The meta-analysis of trials by group of achieved sodium reduction (fig 2) identified no clear association between the magnitude of sodium reduction and magnitude of either the systolic blood pressure reduction (P trend=0.09) or the diastolic blood pressure reduction (P trend=0.63). Likewise, the univariable meta-regression analyses including all studies (table 1) showed no association of blood pressure effect with magnitude of sodium reduction. However, the magnitude of the change in 24 hour urinary sodium excretion was positively associated with the change in blood pressure after adjusting for intervention duration, mean age, percentage of female sex, percentage of white ethnicity, and baseline blood pressure in the multivariable meta-regression. In these analyses, each 50 mmol reduction in 24 hour urinary sodium was associated with a 1.10 mm Hg (0.66 to 1.54) decrease in systolic blood pressure and a 0.33 mm Hg (0.04 to 0.63) decrease in diastolic blood pressure. Sensitivity analyses excluding studies with missing data other than ethnicity (18 studies) did not change the results substantially. We did not exclude studies missing only ethnicity data because this could be estimated with high confidence based on the study country. The analysis of studies with more than two levels of dietary sodium intake provided further support for a dose-response association between magnitude of sodium reduction and magnitude of systolic blood pressure response (supplementary fig 1). Findings in the subsidiary analyses for DBP were less clear.
Table 1.
Coefficient statistics of unadjusted and multivariable meta-regression on the association between blood pressure change and 24 hour urinary sodium change and other covariates
| Dependent variables and studies | Independent variables | Unadjusted | Multivariable | ||
|---|---|---|---|---|---|
| Coefficient* (95% CI) | P value | Coefficient* (95% CI) | P value | ||
| Change in SBP (mm Hg) | |||||
| All studies (135 data points) | Change of 24 hour urinary sodium (mmol) | 0.007 (−0.002 to 0.016) | 0.106 | 0.022 (0.013 to 0.031) | <0.001 |
| Duration of intervention (days) | −0.003 (−0.006 to 0.001) | 0.124 | 0.000 (−0.003 to 0.003) | 0.849 | |
| Mean age (years) | 0.121 (0.073 to 0.169) | <0.001 | 0.111 (0.046 to 0.177) | 0.001 | |
| Percentage of female sex | 2.258 (−0.794 to 5.309) | 0.146 | −0.412 (−3.170 to 2.346) | 0.768 | |
| Percentage of white ethnicity | −3.039 (−5.397 to −0.680) | 0.012 | −2.957 (−5.000 to −0.913) | 0.005 | |
| Mean baseline SBP (mm Hg) | 0.102 (0.065 to 0.138) | <0.001 | 0.074 (0.030 to 0.118) | 0.001 | |
| Studies with ≤14 days' intervention (77 data points) | Change of 24 hour urinary sodium (mmol) | 0.015 (−0.001 to 0.030) | 0.064 | 0.021 (0.008 to 0.034) | 0.002 |
| Duration of intervention (days) | 0.208 (−0.084 to 0.500) | 0.160 | 0.071 (−0.182 to 0.324) | 0.577 | |
| Mean age (years) | 0.180 (0.106 to 0.254) | <0.001 | 0.105 (−0.006 to 0.217) | 0.064 | |
| Percentage of female sex | 2.701 (−1.438 to 6.841) | 0.198 | −0.233 (−4.031 to 3.566) | 0.903 | |
| Percentage of white ethnicity | −5.061 (−8.923 to −1.199) | 0.011 | −2.787 (−6.343 to 0.770) | 0.123 | |
| Mean baseline SBP (mm Hg) | 0.132 (0.080 to 0.185) | <0.001 | 0.076 (0.002 to 0.150) | 0.044 | |
| Studies with >14 days' intervention (58 data points) | Change of 24 hour urinary sodium (mmol) | 0.043 (0.019 to 0.067) | 0.001 | 0.043 (0.017 to 0.068) | 0.002 |
| Duration of intervention (days) | −0.003 (−0.006 to −0.001) | 0.016 | 0.000 (−0.002 to 0.003) | 0.813 | |
| Mean age (years) | 0.107 (0.013 to 0.201) | 0.027 | 0.107 (0.012 to 0.203) | 0.028 | |
| Percentage of female sex | 0.523 (−4.924 to 5.970) | 0.848 | −0.421 (−5.337 to 4.496) | 0.864 | |
| Percentage of white ethnicity | −1.251 (−3.973 to 1.471) | 0.361 | −3.342 (−6.071 to −0.614) | 0.017 | |
| Mean baseline SBP (mm Hg) | 0.067 (0.004 to 0.129) | 0.036 | 0.058 (−0.003 to 0.120) | 0.062 | |
| Studies with duration >14 days and sodium reduction <=100 mmol (48 data points) | Change of 24 hour urinary sodium (mmol) | 0.059 (0.023 to 0.094) | 0.002 | 0.058 (0.022 to 0.093) | 0.002 |
| Duration of intervention (days) | −0.003 (−0.005 to −0.001) | 0.007 | 0.001 (−0.001 to 0.003) | 0.410 | |
| Mean age (years) | 0.113 (0.029 to 0.198) | 0.010 | 0.110 (0.032 to 0.188) | 0.007 | |
| Percentage of female sex | 0.945 (−4.278 to 6.169) | 0.717 | 0.155 (−3.854 to 4.164) | 0.938 | |
| Percentage of white ethnicity | −1.302 (−3.943 to 1.340) | 0.326 | −3.497 (−5.724 to −1.271) | 0.003 | |
| Mean baseline SBP (mm Hg) | 0.083 (0.025 to 0.141) | 0.006 | 0.087 (0.035 to 0.140) | 0.002 | |
| Change in DBP (mm Hg) | |||||
| All studies (136 data points) | Change of 24 hour urinary sodium (mmol) | 0.000 (−0.006 to 0.006) | 0.972 | 0.007 (0.001 to 0.013) | 0.028 |
| Duration of intervention (days) | −0.001 (−0.003 to 0.001) | 0.555 | 0.000 (−0.002 to 0.002) | 0.980 | |
| Mean age (years) | 0.068 (0.036 to 0.100) | <0.001 | 0.041 (−0.002 to 0.084) | 0.062 | |
| Percentage of female sex | −0.373 (−2.327 to 1.582) | 0.707 | −1.480 (−3.343 to 0.383) | 0.118 | |
| Percentage of white ethnicity | −1.102 (−2.569 to 0.366) | 0.140 | −0.909 (−2.249 to 0.430) | 0.182 | |
| Mean baseline DBP (mm Hg) | 0.102 (0.071 to 0.133) | <0.001 | 0.088 (0.049 to 0.127) | <0.001 | |
| Studies with ≤14 days' intervention (77 data points) | Change of 24 hour urinary sodium (mmol) | 0.003 (−0.007 to 0.014) | 0.531 | 0.007 (−0.002 to 0.015) | 0.134 |
| Duration of intervention (days) | 0.302 (0.127 to 0.478) | 0.001 | 0.174 (0.006 to 0.343) | 0.043 | |
| Mean age (years) | 0.104 (0.055 to 0.154) | <0.001 | 0.021 (−0.054 to 0.095) | 0.586 | |
| Percentage of female sex | −0.381 (−3.011 to 2.249) | 0.774 | −1.357 (−3.722 to 1.007) | 0.256 | |
| Percentage of white ethnicity | −1.230 (−3.590 to 1.130) | 0.302 | −0.570 (−2.701 to 1.561) | 0.596 | |
| Mean baseline DBP (mm Hg) | 0.126 (0.086 to 0.166) | <0.001 | 0.099 (0.036 to 0.162) | 0.003 | |
| Studies with >14 days' intervention (59 data points) | Change of 24 hour urinary sodium (mmol) | 0.015 (0.001 to 0.029) | 0.035 | 0.013 (−0.002 to 0.029) | 0.094 |
| Duration of intervention (days) | −0.001 (−0.003 to 0.000) | 0.157 | 0.000 (−0.002 to 0.002) | 0.983 | |
| Mean age (years) | 0.022 (−0.039 to 0.083) | 0.472 | 0.035 (−0.033 to 0.103) | 0.308 | |
| Percentage of female sex | −1.213 (−4.464 to 2.039) | 0.458 | −1.263 (−4.617 to 2.091) | 0.453 | |
| Percentage of white ethnicity | −0.780 (−2.472 to 0.911) | 0.359 | −1.493 (−3.353 to 0.368) | 0.113 | |
| Mean baseline DBP (mm Hg) | 0.049 (−0.011 to 0.109) | 0.110 | 0.048 (−0.015 to 0.110) | 0.134 | |
| Studies with duration >14 days and sodium reduction ≤100 mmol (49 data points) | Change of 24 hour urinary sodium (mmol) | 0.018 (−0.002 to 0.037) | 0.081 | 0.013 (−0.010 to 0.035) | 0.258 |
| Duration of intervention (days) | −0.001 (−0.002 to 0.000) | 0.049 | 0.000 (−0.002 to 0.001) | 0.810 | |
| Mean age (years) | 0.032 (−0.019 to 0.082) | 0.210 | 0.041 (−0.017 to 0.099) | 0.162 | |
| Percentage of female sex | −1.343 (−4.122 to 1.437) | 0.336 | −0.753 (−3.557 to 2.050) | 0.591 | |
| Percentage of white ethnicity | −0.370 (−1.848 to 1.109) | 0.617 | −0.979 (−2.544 to 0.586) | 0.214 | |
| Mean baseline DBP (mm Hg) | 0.059 (0.006 to 0.111) | 0.029 | 0.058 (0.003 to 0.113) | 0.040 | |
SBP=systolic blood pressure; DBP=diastolic blood pressure.
The coefficient means the change of the dependent variable (change in SBP or DBP) with each unit increase of the independent variables.
Association of duration of sodium reduction intervention with size of blood pressure reduction
The meta-analysis of trials by intervention duration (fig 4) identified no overall association between the duration of the sodium reduction intervention and the magnitude of either the systolic blood pressure reduction (P trend=0.87) or the diastolic blood pressure reduction (P trend=0.11). Likewise, the univariable meta-regression analyses of all trials showed no association of blood pressure effect with duration of sodium reduction and neither did the multivariable meta-regressions. The six studies that recorded multiple measurements at different time points showed no apparent difference in the pattern of blood pressure lowering over time (supplementary fig 2), which corresponded to the meta-regression analyses. In the subsidiary analysis of studies with intervention duration >14 days compared with ≤14 days, the effect of each 50 mmol reduction in 24 hour urinary sodium excretion on systolic blood pressure reduction was approximately twice as large in the studies of longer intervention duration (2.13 mm Hg; 0.85 to 3.40 v 1.05 mm Hg; 0.40 to 1.70). The univariable meta-regression analyses restricted to longer trials and trials with smaller reductions in sodium excretion showed inverse associations between intervention duration and magnitude of systolic blood pressure reduction but these were not apparent in the corresponding multivariable meta-regression analyses (table 1) with I2 reduced to 24.9%. There was no consistent pattern of association between intervention duration and reduction in diastolic blood pressure.
Fig 4.
Association of duration of sodium reduction intervention with size of blood pressure reduction (mm Hg)
Association of age, sex, race, baseline sodium intake, and baseline blood pressure with the size of blood pressure fall with 50 mmol sodium reduction
The analysis of trial subgroups standardised to a 50 mmol sodium reduction (fig 3) identified positive associations between the magnitude of systolic blood pressure reduction and baseline age and baseline systolic blood pressure (both P trend=0.01), and statistically significant heterogeneity by race (P=0.005). We observed no association for baseline sodium intake (P trend=0.20) or blood pressure status (P trend=0.08) and there was no detectable heterogeneity by sex (P=0.42). The meta-regression analyses (table 1) provided support for independent effects of age, ethnicity, and baseline blood pressure as modifiers of the effect of sodium reduction on blood pressure.
Study quality and publication bias
Most studies did not report whether there was random sequence generation (80.1%, 109/136) or appropriate allocation concealment (83.8%, 114/136). Only 41.9% (57/136) studies were double blinded and 52.9% (72/136) had inadequate blinding (open studies, or with only participants or outcome observers blinded). Most studies had low rates of loss to follow-up and there was low risk of selective outcome reporting (supplementary figure 3, supplementary file 3). Although the information for assessing individual study quality was limited, the overall evidence should be considered of fairly high quality since only randomised trials were included and only a small proportion of studies had significant missing data.
Egger’s regression test suggested asymmetry of funnel plots for both systolic blood pressure change (P<0.001) and diastolic blood pressure change (P=0.005) (supplementary figure 4). Use of the trim and fill method did not change the results and the contour enhanced funnel plots did not suggest under-reporting of studies with less statistical significance (supplementary figure 5). Asymmetry of the funnel plots is more likely to arise from other differences in study characteristics.
Discussion
Principal findings
This meta-analysis shows that sodium reduction leads to a significant reduction in systolic blood pressure in adults, both female and male, all ethnic groups, and in both hypertensive and normotensive populations. Diastolic blood pressure also decreased significantly in most participant subgroups. There was a dose-response relation with a greater reduction in sodium intake producing a greater fall in blood pressure. Populations with older age and higher baseline blood pressure achieved greater blood pressure lowering from the same amount of sodium reduction and so did non-white compared with white populations.
Overall, the duration of the sodium reduction intervention was not associated with the size of the change in blood pressure, although short term studies of less than 15 days’ duration appear to underestimate the effect of sodium reduction on blood pressure. With few long term studies available, additional research is required to draw a definitive conclusion about whether prolonged sodium reduction influences the magnitude of the blood pressure lowering.
Strengths and limitations of the study
This meta-analysis represents a substantial update and enhancement compared with previous overviews. The selective inclusion of studies that used 24 hour urine collections to estimate intervention effect on sodium intake reduced the risk of bias, while the inclusion of studies with concomitant interventions applied in the same way to both intervention and control arms maximised the available data and the statistical power of the analyses. Likewise, the inclusion of studies regardless of the length of the duration of intervention enabled a robust and powerful examination of the effects of intervention duration on outcomes. The extensive sensitivity analyses provided for a full understanding of the strengths and weakness of the findings. There were, however, limitations in regard to our capacity to assess the quality of the studies. There was substantial heterogeneity across the included studies, but this was largely explained by some the of study characteristics in the meta-regression analyses. When the analyses were limited to studies with duration of more than 14 days and a sodium reduction of up to 100 mmol, the I2 statistics for heterogeneity reduced to 24.9%. The use of study level data rather than individual participant data greatly reduced the power of the analyses, although this limitation was somewhat offset by the large number of studies available. Different studies defined hypertension using different criteria and there was limited capacity to quantify the effects of pharmaceutical treatments on baseline diagnoses of hypertension or baseline blood pressure measurements. Finally, our use of random effects meta-analysis has resulted in wider confidence intervals but might better reflect uncertainty about the true constancy of effects across included trials.
Comparison with other studies
Effect of sodium reduction on blood pressure and the dose-response relation
The overall effect of sodium reduction on blood pressure has been observed in several previous meta-analyses, despite different trial selection criteria.12 21 160 161 We also observed strong associations of the magnitude of sodium reduction with the magnitude of the fall in systolic blood pressure,11 21 and interactions of age, race, and baseline blood pressure with size of the systolic blood pressure fall, as shown in previous reviews.162 163 However, the 2.2 mm Hg reduction in systolic blood pressure for each 100 mmol reduction in 24 hour urinary sodium observed in the current overview is substantially less compared with the 3.83 mm Hg reduction reported in a previous overview.164 The difference may be owing to the inclusion of studies with sodium intake estimated from fractional urine collections in the previous review.164 Another overview that included only studies with at least four weeks’ intervention and only moderate 24 hour urinary sodium reduction identified a 5.8 mm Hg reduction in SBP for each 100 mmol reduction in sodium,21 which is similar to the effect found in our subgroup analysis of studies longer than 14 days with a sodium reduction ≤100 mmol, further highlighting the sensitivity of the estimated strength of the dose-response association to the type of studies included in the analysis.
Previous overviews have generated uncertainty regarding the effects of sodium reduction among individuals with different levels of starting blood pressure. Some reports have suggested much larger effects in hypertensive individuals compared with non-hypertensive individuals,21 while others suggested that sodium reduction is of value only in those with hypertension.11 12 The conclusion that there is no value in non-hypertensive individuals is dependent upon the results from very short term studies in which sodium reduction had a limited effect on blood pressure and in which there were adverse effects on other markers of cardiovascular risk. The responses of the renin-angiotensin system and sympathetic nervous system as well as adverse metabolic effects associated with acute large falls in dietary sodium do not, however, appear to be present in longer term interventions21 165 and it is unlikely that short term unfavourable metabolic effects would override the long term benefits anticipated from sustained blood pressure lowering of moderate magnitude. Our review identifies an approximate doubling of the effect of sodium reduction on blood pressure in studies of longer than two weeks’ duration versus shorter studies, indicating that the full effects of dietary sodium reduction require several weeks to become apparent. Very short term studies of sodium reduction are not a sound basis for drawing conclusions about the effects of sodium reduction on blood pressure and are not helpful in formulating policy recommendations for public health.
Analyses that simply separate studies based upon those that included hypertensive, non-hypertensive, or mixed populations are weak because the definition of hypertension is arbitrary and there is a rationale for expecting a graded interaction between sodium reduction, blood pressure reduction, and starting blood pressure. In the present analysis, meta-regressions based on mean starting blood pressure levels of participants in each study provided for a much more nuanced evaluation of the effects of starting blood pressure on the size of the blood pressure fall achieved with sodium reduction. These analyses showed that sodium reduction produced a progressively greater reduction in blood pressure among those with higher starting blood pressure levels, but also that sodium reduction substantially lowered blood pressure, even among those with starting systolic blood pressure levels as low as 120 mm Hg. These findings indicate potentially important health benefits from sodium reduction among normotensive as well as hypertensive individuals. More importantly, sodium reduction among normotensive individuals could potentially avert or delay the development of hypertension with ageing as the association between sodium intake and blood pressure is greater at older age.3
The differential blood pressure lowering effect of sodium reduction across different ethnic groups has been observed in various studies and meta-analyses12 21 166; specifically, there was a greater blood pressure reduction in non-white populations compared with white populations for the same amount of sodium reduction. Some authors explained this phenomenon as caused by differential “salt sensitivity.”167 Others have shown that the difference in the responsiveness of the renin-angiotensin system to sodium reduction among various ethnic groups is at least partially responsible.166 Nonetheless, while population wide sodium reduction is recommended, the cost effectiveness for some particular populations is potentially greater. This has important public health implications, especially in regions where resources are constrained.
The findings from this overview of randomised trials conflict directly with findings from the Prospective Urban Rural Epidemiology (PURE)168 study, which reported that associations between sodium intake and systolic blood pressure are observed only among communities with very high sodium intake (>5.08 g or 221 mmol sodium/day, equivalent to 13 g/day salt). We observed very clear effects of sodium reduction on both systolic and diastolic blood pressure at levels of sodium intake far below this. Measurement errors and uncontrolled confounding in the PURE study have likely biased conclusions about the association of sodium intake and blood pressure.16 169
Impact of intervention duration of sodium reduction
The optimal method to assess the impact of duration of sodium reduction on the magnitude of blood pressure reduction would be to collate data from studies that measure change of sodium and change of blood pressure at multiple time points. In practice, however, most studies made measurements only once at completion of follow-up. Neither the univariable nor the multivariable meta-regressions identified an effect of intervention duration on the size of the blood pressure fall achieved with sodium reduction. The power of the analyses was strengthened by the wide range of intervention durations recorded (from three days to five years) but limited by the highly skewed distribution of the studies, with most being of short or very short duration. Among the 133 studies included, 77 were shorter than 15 days’ duration and only five extended beyond six months. The DASH sodium trial that assessed effects at four time points over one month showed with some rigour that blood pressure effects from sodium reduction were clearly greater at week 4 compared with earlier weeks.170
Conclusions and policy implications
Sodium reduction resulted in lower blood pressure among a very broad group of populations with a strong dose-response relation between the magnitude of the sodium reduction achieved and the magnitude of the fall in blood pressure. The effects of sodium reduction were more evident at higher starting blood pressure levels, older ages, and among non-white populations, but almost every population group examined achieved a reduction in blood pressure. In trials of more than two weeks’ duration, the dose-response relation between sodium reduction and blood pressure fall was greater than that in trials of shorter duration, but there was limited evidence that interventions of longer duration further increased the effects of sodium reduction on blood pressure. Longer term trials that achieve sustained sodium reduction and make multiple assessments of blood pressure are required to properly assess this issue.
What is already known on this topic.
An extensive body of evidence has shown that a higher level of dietary sodium intake is associated with a higher blood pressure
There are clear effects of sodium reduction on blood pressure in those with hypertension, but uncertainty persists about the comparability of effects in different population subsets. In addition, the impact of intervention duration is not fully understood
What this study adds
Evidence shows that sodium reduction lowers blood pressure in both hypertensive and non-hypertensive individuals, with greater effects in high risk subsets
The magnitude of blood pressure lowering achieved with sodium reduction showed a dose-response relation
Very short term trials could substantially underestimate the effect of sodium reduction on blood pressure
Contributors: Members of the TRUE Consortium conceived the review. LH undertook the search. LH, KT, and SY undertook the screening for eligibility in duplicate. LH extracted all relevant data from published papers. KT and SY checked all extracted data for accuracy. MW and QL provided advice on statistical analyses. LH analysed the data and drafted the manuscript. FH and BN provided overall guidance and editing of the manuscript. All authors in the author list provided comments and feedback on the manuscript, and GM and NC also provided some guidance during the conduct of the review. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. LH and FH are the guarantors of this manuscript.
Funding: This research received no funding support.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work. Outside this work, BN has received salt substitute for trials from Salt Manufacturing Company in China and Nutek; MW is supported by the National Health and Medical Research Foundation of Australia grants (1080206 and 1149987) and receives personal fees from Amgen, personal fees from Kirin; NRCC is an unpaid member of World Action on Salt and Health and an unpaid consultant on dietary sodium and hypertension control to numerous governmental and non-governmental organisations; AAL is funded by the Hypertension Canada New Investigator Award; FJH is a member of Consensus Action on Salt and Health (CASH) and World Action on Salt and Health (WASH). Both CASH and WASH are non-profit charitable organisations and FJH does not receive any financial support from CASH or WASH; GAM is the Chairman of Blood Pressure UK (BPUK), Chairman of Consensus Action on Salt and Health (CASH) and Chairman of World Action on Salt and Health (WASH). BPUK, CASH and WASH are non-profit charitable organisations and GAM does not receive any financial support from any of these organisations.
Ethical approval: Ethical approval was not required for this research.
Data sharing: Data used for analysis have been included in this manuscript. Additional data can be obtained upon request.
The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Following publication, the results of this review will be disseminated to appropriate audiences such as academia, clinicians, policy makers, and the general public, through various channels including engagement with collaborators and World Action on Salt and Health (WASH) members, press release, social media, e-newsletter, WHO Collaborating Centre on Salt Reduction website and monthly bulletin.
Web extra.
material supplied by authors
Web appendix: Supplementary figures 1-5
Web appendix: supplementary files 1-3
References
- 1. GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Denton D, Weisinger R, Mundy NI, et al. The effect of increased salt intake on blood pressure of chimpanzees. Nat Med 1995;1:1009-16. 10.1038/nm1095-1009 [DOI] [PubMed] [Google Scholar]
- 3. Intersalt Cooperative Research Group Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988;297:319-28. 10.1136/bmj.297.6644.319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Walkowska A, Kuczeriszka M, Sadowski J, et al. High salt intake increases blood pressure in normal rats: putative role of 20-HETE and no evidence on changes in renal vascular reactivity. Kidney Blood Press Res 2015;40:323-34. 10.1159/000368508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Michell AR. Physiological aspects of the requirement for sodium in mammals. Nutr Res Rev 1989;2:149-60. 10.1079/NRR19890012 [DOI] [PubMed] [Google Scholar]
- 6. Powles J, Fahimi S, Micha R, et al. Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE) Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3:e003733. 10.1136/bmjopen-2013-003733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization Guideline: Sodium intake for adults and children. World Health Organization, 2012. [PubMed] [Google Scholar]
- 8. Scientific Advisory Committee on Nutrition Salt and health. The Stationery Office, 2003. [Google Scholar]
- 9.US Department of Health and Human Services and US Department of Agriculture. 2015-2020 Dietary guidelines for Americans. 8th Ed. https://health.gov/dietaryguidelines/2015/guidelines.
- 10. World Health Organization Global action plan for the prevention and control of noncommunicable diseases 2013-2020: World Health Organization. WHO, 2013. [Google Scholar]
- 11. Graudal N, Hubeck-Graudal T, Jürgens G, Taylor RS. Dose-response relation between dietary sodium and blood pressure: a meta-regression analysis of 133 randomized controlled trials. Am J Clin Nutr 2019;109:1273-8. 10.1093/ajcn/nqy384 [DOI] [PubMed] [Google Scholar]
- 12. Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev 2017;4:CD004022. 10.1002/14651858.CD004022.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Graudal N, Jürgens G, Baslund B, Alderman MH. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a meta-analysis. Am J Hypertens 2014;27:1129-37. 10.1093/ajh/hpu028 [DOI] [PubMed] [Google Scholar]
- 14. Zhu Y, Zhang J, Li Z, et al. Association of sodium intake and major cardiovascular outcomes: a dose-response meta-analysis of prospective cohort studies. BMC Cardiovasc Disord 2018;18:192. 10.1186/s12872-018-0927-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cappuccio FP, Beer M, Strazzullo P, European Salt Action Network Population dietary salt reduction and the risk of cardiovascular disease. A scientific statement from the European Salt Action Network. Nutr Metab Cardiovasc Dis 2018;29:107-14. 10.1016/j.numecd.2018.11.010 [DOI] [PubMed] [Google Scholar]
- 16. He FJ, Campbell NRC, Ma Y, MacGregor GA, Cogswell ME, Cook NR. Errors in estimating usual sodium intake by the Kawasaki formula alter its relationship with mortality: implications for public health. Int J Epidemiol 2018;47:1784-95. 10.1093/ije/dyy114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang M, Moran AE, Liu J, et al. A meta-analysis of effect of dietary salt restriction on blood pressure in Chinese adults. Glob Heart 2015;10:291-299.e6. 10.1016/j.gheart.2014.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newberry SJ, Chung M, Anderson CAM, et al. Sodium and potassium intake: effects on chronic disease outcomes and risks. Rockville (MD) Agency for Healthcare Research and Quality (US) 2018 [PubMed] [Google Scholar]
- 19. Midgley JP, Matthew AG, Greenwood CM, Logan AG. Effect of reduced dietary sodium on blood pressure: a meta-analysis of randomized controlled trials. JAMA 1996;275:1590-7. 10.1001/jama.1996.03530440070039 [DOI] [PubMed] [Google Scholar]
- 20. Huang L, Crino M, Wu JH, et al. Mean population salt intake estimated from 24-h urine samples and spot urine samples: a systematic review and meta-analysis. Int J Epidemiol 2016;45:239-50. 10.1093/ije/dyv313 [DOI] [PubMed] [Google Scholar]
- 21. He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013;346:f1325. 10.1136/bmj.f1325 [DOI] [PubMed] [Google Scholar]
- 22. Graudal N, Hubeck-Graudal T, Jürgens G, McCarron DA. The significance of duration and amount of sodium reduction intervention in normotensive and hypertensive individuals: a meta-analysis. Adv Nutr 2015;6:169-77. 10.3945/an.114.007708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. TRUE Consortium (inTernational consoRtium for qUality resEarch on dietary sodium/salt) Recommended standards for assessing blood pressure in human research where blood pressure or hypertension is a major focus. J Clin Hypertens (Greenwich) 2017;19:108-13. 10.1111/jch.12948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions 2008. https://www.radioterapiaitalia.it/wp-content/uploads/2017/01/cochrane-handbook-for-systematic-reviews-of-interventions.pdf
- 25. McCarron DA, Kazaks AG, Geerling JC, Stern JS, Graudal NA. Normal range of human dietary sodium intake: a perspective based on 24-hour urinary sodium excretion worldwide. Am J Hypertens 2013;26:1218-23. 10.1093/ajh/hpt139 [DOI] [PubMed] [Google Scholar]
- 26. He FJ, MacGregor GA. Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat Rev Cardiol 2018;15:371-7. 10.1038/s41569-018-0004-1 [DOI] [PubMed] [Google Scholar]
- 27. Parijs J, Joossens JV, Van der Linden L, Verstreken G, Amery AK. Moderate sodium restriction and diuretics in the treatment of hypertension. Am Heart J 1973;85:22-34. 10.1016/0002-8703(73)90522-X [DOI] [PubMed] [Google Scholar]
- 28. Mark AL, Lawton WJ, Abboud FM, Fitz AE, Connor WE, Heistad DD. Effects of high and low sodium intake on arterial pressure and forearm vasular resistance in borderline hypertension. A preliminary report. Circ Res 1975;36(Suppl 1):194-8. 10.1161/01.RES.36.6.194 [DOI] [PubMed] [Google Scholar]
- 29. Morgan TO, Myers JB. Hypertension treated by sodium restriction. Med J Aust 1981;2:396-7. 10.5694/j.1326-5377.1981.tb101026.x [DOI] [PubMed] [Google Scholar]
- 30. Skrabal F, Auböck J, Hörtnagl H. Low sodium/high potassium diet for prevention of hypertension: probable mechanisms of action. Lancet 1981;2:895-900. 10.1016/S0140-6736(81)91392-1 [DOI] [PubMed] [Google Scholar]
- 31. MacGregor GA, Markandu ND, Best FE, et al. Double-blind randomised crossover trial of moderate sodium restriction in essential hypertension. Lancet 1982;1:351-5. 10.1016/S0140-6736(82)91389-7 [DOI] [PubMed] [Google Scholar]
- 32. Puska P, Iacono JM, Nissinen A, et al. Controlled, randomised trial of the effect of dietary fat on blood pressure. Lancet 1983;1:1-5. 10.1016/S0140-6736(83)91556-8 [DOI] [PubMed] [Google Scholar]
- 33. Silman AJ, Locke C, Mitchell P, Humpherson P. Evaluation of the effectiveness of a low sodium diet in the treatment of mild to moderate hypertension. Lancet 1983;1:1179-82. 10.1016/S0140-6736(83)92463-7 [DOI] [PubMed] [Google Scholar]
- 34. Watt GCM, Edwards C, Hart JT, Hart M, Walton P, Foy CJ. Dietary sodium restriction for mild hypertension in general practice. Br Med J (Clin Res Ed) 1983;286:432-6. 10.1136/bmj.286.6363.432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Erwteman TM, Nagelkerke N, Lubsen J, Koster M, Dunning AJ. Beta blockade, diuretics, and salt restriction for the management of mild hypertension: a randomised double blind trial. Br Med J (Clin Res Ed) 1984;289:406-9. 10.1136/bmj.289.6442.406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gillies AH, Carney SL, Smith AJ, Waga SM. Adjunctive effect of salt restriction on antihypertensive efficacy. Clin Exp Pharmacol Physiol 1984;11:395-8. 10.1111/j.1440-1681.1984.tb00286.x [DOI] [PubMed] [Google Scholar]
- 37. Koolen MI, van Brummelen P. Sodium sensitivity in essential hypertension: role of the renin-angiotensin-aldosterone system and predictive value of an intravenous frusemide test. J Hypertens 1984;2:55-9. 10.1097/00004872-198402000-00010 [DOI] [PubMed] [Google Scholar]
- 38. Koolen MI, van Brummelen P. Adrenergic activity and peripheral hemodynamics in relation to sodium sensitivity in patients with essential hypertension. Hypertension 1984;6:820-5. 10.1161/01.HYP.6.6.820 [DOI] [PubMed] [Google Scholar]
- 39. Maxwell MH, Kushiro T, Dornfeld LP, Tuck ML, Waks AU. BP changes in obese hypertensive subjects during rapid weight loss. Comparison of restricted v unchanged salt intake. Arch Intern Med 1984;144:1581-4. 10.1001/archinte.1984.00350200073012 [DOI] [PubMed] [Google Scholar]
- 40. Myers JB, Morgan TO. Effect of alteration in sodium chloride intake on blood pressure of normotensive subjects. J Cardiovasc Pharmacol 1984;6(Suppl 1):S204-9. 10.1097/00005344-198400061-00032 [DOI] [PubMed] [Google Scholar]
- 41. Richards AM, Nicholls MG, Espiner EA, et al. Blood-pressure response to moderate sodium restriction and to potassium supplementation in mild essential hypertension. Lancet 1984;1:757-61. 10.1016/S0140-6736(84)91276-5 [DOI] [PubMed] [Google Scholar]
- 42. Skrabal F, Herholz H, Neumayr M, et al. Salt sensitivity in humans is linked to enhanced sympathetic responsiveness and to enhanced proximal tubular reabsorption. Hypertension 1984;6:152-8. 10.1161/01.HYP.6.2.152 [DOI] [PubMed] [Google Scholar]
- 43. Resnick LM, Nicholson JP, Laragh JH. Alterations in calcium metabolism mediate dietary salt sensitivity in essential hypertension. Trans Assoc Am Physicians 1985;98:313-21. [PubMed] [Google Scholar]
- 44. Skrabal F, Hamberger L, Cerny E. Salt sensitivity in normotensives with and salt resistance in normotensives without heredity of hypertension. Scand J Clin Lab Invest Suppl 1985;176(suppl. 176):47-57. [PubMed] [Google Scholar]
- 45. Ashry A, Heagerty AM, Alton SM, Bing RF, Swales JD, Thurston H. Effects of manipulation of sodium balance on erythrocyte sodium transport. J Hum Hypertens 1987;1:105-11. [PubMed] [Google Scholar]
- 46. Grobbee DE, Hofman A, Roelandt JT, Boomsma F, Schalekamp MA, Valkenburg HA. Sodium restriction and potassium supplementation in young people with mildly elevated blood pressure. J Hypertens 1987;5:115-9. 10.1097/00004872-198702000-00016 [DOI] [PubMed] [Google Scholar]
- 47. MacGregor GA, Markandu ND, Singer DRJ, Cappuccio FP, Shore AC, Sagnella GA. Moderate sodium restriction with angiotensin converting enzyme inhibitor in essential hypertension: a double blind study. Br Med J (Clin Res Ed) 1987;294:531-4. 10.1136/bmj.294.6571.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Morgan T, Anderson A. Sodium restriction can delay the return of hypertension in patients previously well-controlled on drug therapy. Can J Physiol Pharmacol 1987;65:1752-5. 10.1139/y87-274 [DOI] [PubMed] [Google Scholar]
- 49. Lawton WJ, Sinkey CA, Fitz AE, Mark AL. Dietary salt produces abnormal renal vasoconstrictor responses to upright posture in borderline hypertensive subjects. Hypertension 1988;11:529-36. 10.1161/01.HYP.11.6.529 [DOI] [PubMed] [Google Scholar]
- 50. Morgan T, Anderson A. Interaction in hypertensive man between sodium intake, converting enzyme inhibitor (enalapril), plasma renin and blood pressure control. J Hum Hypertens 1988;1:311-5. [PubMed] [Google Scholar]
- 51. Morgan T, Anderson A. Interaction of slow-channel calcium blocking drugs with sodium restriction, diuretics and angiotensin converting enzyme inhibitors. J Hypertens Suppl 1988;6(4):S652-4. 10.1097/00004872-198812040-00205 [DOI] [PubMed] [Google Scholar]
- 52. Nowson CA, Morgan TO. Change in blood pressure in relation to change in nutrients effected by manipulation of dietary sodium and potassium. Clin Exp Pharmacol Physiol 1988;15:225-42. 10.1111/j.1440-1681.1988.tb01065.x [DOI] [PubMed] [Google Scholar]
- 53. Staessen J, Bulpitt CJ, Fagard R, Joossens JV, Lijnen P, Amery A. Salt intake and blood pressure in the general population: a controlled intervention trial in two towns. J Hypertens 1988;6:965-73. 10.1097/00004872-198812000-00003 [DOI] [PubMed] [Google Scholar]
- 54. Chalmers JP, Doyle AE, Hopper JL, et al. Australian National Health and Medical Research Council Dietary Salt Study Management Committee Fall in blood pressure with modest reduction in dietary salt intake in mild hypertension. Lancet 1989;1:399-402. [PubMed] [Google Scholar]
- 55. Chalmers JP, Doyle AE, Hopper JL, et al. Effects of replacing sodium intake in subjects on a low sodium diet: a crossover study. Australian National Health & Medical Research Council Dietary Salt Study Management Committee. Clin Exp Hypertens A 1989;11:1011-24. 10.3109/10641968909035388 [DOI] [PubMed] [Google Scholar]
- 56. Dodson PM, Beevers M, Hallworth R, Webberley MJ, Fletcher RF, Taylor KG. Sodium restriction and blood pressure in hypertensive type II diabetics: randomised blind controlled and crossover studies of moderate sodium restriction and sodium supplementation. BMJ 1989;298:227-30. 10.1136/bmj.298.6668.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hargreaves M, Morgan TO, Snow R, Guerin M. Exercise tolerance in the heat on low and normal salt intakes. Clin Sci (Lond) 1989;76:553-7. 10.1042/cs0760553 [DOI] [PubMed] [Google Scholar]
- 58. MacGregor GA, Markandu ND, Sagnella GA, Singer DR, Cappuccio FP. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet 1989;2:1244-7. 10.1016/S0140-6736(89)91852-7 [DOI] [PubMed] [Google Scholar]
- 59. Bruun NE, Skøtt P, Damkjaer Nielsen M, et al. Normal renal tubular response to changes of sodium intake in hypertensive man. J Hypertens 1990;8:219-27. [PubMed] [Google Scholar]
- 60. Parker M, Puddey IB, Beilin LJ, Vandongen R. Two-way factorial study of alcohol and salt restriction in treated hypertensive men. Hypertension 1990;16:398-406. 10.1161/01.HYP.16.4.398 [DOI] [PubMed] [Google Scholar]
- 61. Del Río A, Rodríguez-Villamil JL, López-Campos JM, Carrera F. [Effect of moderate salt restriction on the antihypertensive action of nifedipine: a double blind study]. Rev Clin Esp 1990;186:5-10. [PubMed] [Google Scholar]
- 62. Sharma AM, Arntz HR, Kribben A, Schattenfroh S, Distler A. Dietary sodium restriction: adverse effect on plasma lipids. Klin Wochenschr 1990;68:664-8. 10.1007/BF01667013 [DOI] [PubMed] [Google Scholar]
- 63. Sharma AM, Kribben A, Schattenfroh S, Cetto C, Distler A. Salt sensitivity in humans is associated with abnormal acid-base regulation. Hypertension 1990;16:407-13. 10.1161/01.HYP.16.4.407 [DOI] [PubMed] [Google Scholar]
- 64. Carney SL, Gillies AH, Smith AJ, Smitham S. Increased dietary sodium chloride in patients treated with antihypertensive drugs. Clin Exp Hypertens A 1991;13:401-7. 10.3109/10641969109045059 [DOI] [PubMed] [Google Scholar]
- 65. Creager MA, Roddy MA, Holland KM, Hirsch AT, Dzau VJ. Sodium depresses arterial baroreceptor reflex function in normotensive humans. Hypertension 1991;17:989-96. 10.1161/01.HYP.17.6.989 [DOI] [PubMed] [Google Scholar]
- 66. Sharma AM, Ruland K, Spies KP, Distler A. Salt sensitivity in young normotensive subjects is associated with a hyperinsulinemic response to oral glucose. J Hypertens 1991;9:329-35. 10.1097/00004872-199104000-00004 [DOI] [PubMed] [Google Scholar]
- 67. Singer DRJ, Markandu ND, Sugden AL, Miller MA, MacGregor GA. Sodium restriction in hypertensive patients treated with a converting enzyme inhibitor and a thiazide. Hypertension 1991;17:798-803. 10.1161/01.HYP.17.6.798 [DOI] [PubMed] [Google Scholar]
- 68. Alli C, Avanzini F, Bettelli G, et al. Feasibility of a long-term low-sodium diet in mild hypertension. J Hum Hypertens 1992;6:281-6. [PubMed] [Google Scholar]
- 69.Arroll B. The Auckland blood pressure control study: a randomised controlled trial of physical activity and salt restriction in persons. Med Health Sci 1992;PhD. https://researchspace.auckland.ac.nz/handle/2292/2245
- 70. Benetos A, Xiao YY, Cuche JL, Hannaert P, Safar M. Arterial effects of salt restriction in hypertensive patients. A 9-week, randomized, double-blind, crossover study. J Hypertens 1992;10:355-60. 10.1097/00004872-199204000-00006 [DOI] [PubMed] [Google Scholar]
- 71. Cobiac L, Nestel PJ, Wing LMH, Howe PR. A low-sodium diet supplemented with fish oil lowers blood pressure in the elderly. J Hypertens 1992;10:87-92. 10.1097/00004872-199201000-00014 [DOI] [PubMed] [Google Scholar]
- 72. Cutler JA, Whelton PK, Appel L, et al. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. JAMA 1992;267:1213-20. 10.1001/jama.1992.03480090061028 [DOI] [PubMed] [Google Scholar]
- 73. Gow IF, Dockrell M, Edwards CR, et al. The sensitivity of human blood platelets to the aggregating agent ADP during different dietary sodium intakes in healthy men. Eur J Clin Pharmacol 1992;43:635-8. 10.1007/BF02284963 [DOI] [PubMed] [Google Scholar]
- 74. Huggins RL, Di Nicolantonio R, Morgan TO. Preferred salt levels and salt taste acuity in human subjects after ingestion of untasted salt. Appetite 1992;18:111-9. 10.1016/0195-6663(92)90188-C [DOI] [PubMed] [Google Scholar]
- 75. Fotherby MD, Potter JF. Effects of moderate sodium restriction on clinic and twenty-four-hour ambulatory blood pressure in elderly hypertensive subjects. J Hypertens 1993;11:657-63. 10.1097/00004872-199306000-00010 [DOI] [PubMed] [Google Scholar]
- 76. Nestel PJ, Clifton PM, Noakes M, McArthur R, Howe PR. Enhanced blood pressure response to dietary salt in elderly women, especially those with small waist: hip ratio. J Hypertens 1993;11:1387-94. 10.1097/00004872-199312000-00011 [DOI] [PubMed] [Google Scholar]
- 77. Redón-Más J, Abellán-Alemán J, Aranda-Lara P, et al. The VERSAL Study Group Antihypertensive activity of verapamil: impact of dietary sodium. J Hypertens 1993;11:665-71. 10.1097/00004872-199306000-00011 [DOI] [PubMed] [Google Scholar]
- 78. Del Río A, Rodríguez-Villamil JL. Metabolic effects of strict salt restriction in essential hypertensive patients. J Intern Med 1993;233:409-14. 10.1111/j.1365-2796.1993.tb00692.x [DOI] [PubMed] [Google Scholar]
- 79. Ruilope LM, Lahera V. Influence of salt intake on the antihypertensive effect of carvedilol. J Hypertens Suppl 1993;11(4):S17-9. 10.1097/00004872-199306003-00005 [DOI] [PubMed] [Google Scholar]
- 80. Ruppert M, Overlack A, Kolloch R, Kraft K, Göbel B, Stumpe KO. Neurohormonal and metabolic effects of severe and moderate salt restriction in non-obese normotensive adults. J Hypertens 1993;11:743-9. 10.1097/00004872-199307000-00010 [DOI] [PubMed] [Google Scholar]
- 81. Sharma AM, Schorr U, Oelkers W, Distler A. Effects of sodium salts on plasma renin activity and norepinephrine response to orthostasis in salt-sensitive normotensive subjects. Am J Hypertens 1993;6:780-5. 10.1093/ajh/6.9.780 [DOI] [PubMed] [Google Scholar]
- 82. Sharma AM, Schorr U, Distler A. Insulin resistance in young salt-sensitive normotensive subjects. Hypertension 1993;21:273-9. 10.1161/01.HYP.21.3.273 [DOI] [PubMed] [Google Scholar]
- 83. Sharma AM, Schorr U, Thiede HM, Distler A. Effect of dietary salt restriction on urinary serotonin and 5-hydroxyindoleacetic acid excretion in man. J Hypertens 1993;11:1381-6. 10.1097/00004872-199312000-00010 [DOI] [PubMed] [Google Scholar]
- 84. Zoccali C, Mallamaci F, Leonardis D, Romeo M. Randomly allocated crossover study of various levels of sodium intake in patients with mild hypertension. J Hypertens Suppl 1993;11(5):S326-7. 10.1097/00004872-199312050-00142 [DOI] [PubMed] [Google Scholar]
- 85. Howe PRC, Lungershausen YK, Cobiac L, Dandy G, Nestel PJ. Effect of sodium restriction and fish oil supplementation on BP and thrombotic risk factors in patients treated with ACE inhibitors. J Hum Hypertens 1994;8:43-9. [PubMed] [Google Scholar]
- 86. Iwaoka T, Umeda T, Inoue J, et al. Dietary NaCl restriction deteriorates oral glucose tolerance in hypertensive patients with impairment of glucose tolerance. Am J Hypertens 1994;7:460-3. 10.1093/ajh/7.5.460 [DOI] [PubMed] [Google Scholar]
- 87. MacFadyen RJ, Lees KR, Reid JL. Responses to low dose intravenous perindoprilat infusion in salt deplete/salt replete normotensive volunteers. Br J Clin Pharmacol 1994;38:329-34. 10.1111/j.1365-2125.1994.tb04362.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Zoccali C, Mallamaci F, Parlongo S. The influence of salt intake on plasma calcitonin gene-related peptide in subjects with mild essential hypertension. J Hypertens 1994;12:1249-53. 10.1097/00004872-199411000-00007 [DOI] [PubMed] [Google Scholar]
- 89. Doig JK, MacFadyen RJ, Sweet CS, Reid JL. Haemodynamic and renal responses to oral losartan potassium during salt depletion or salt repletion in normal human volunteers. J Cardiovasc Pharmacol 1995;25:511-7. 10.1097/00005344-199504000-00001 [DOI] [PubMed] [Google Scholar]
- 90. Draaijer P, de Leeuw P, Maessen J, van Hooff J, Leunissen K. Salt-sensitivity testing in patients with borderline hypertension: reproducibility and potential mechanisms. J Hum Hypertens 1995;9:263-9. [PubMed] [Google Scholar]
- 91. Stein CM, Nelson R, Brown M, He H, Wood M, Wood AJ. Dietary sodium intake modulates systemic but not forearm norepinephrine release. Clin Pharmacol Ther 1995;58:425-33. 10.1016/0009-9236(95)90056-X [DOI] [PubMed] [Google Scholar]
- 92. Weir MR, Dengel DR, Behrens MT, Goldberg AP. Salt-induced increases in systolic blood pressure affect renal hemodynamics and proteinuria. Hypertension 1995;25:1339-44. 10.1161/01.HYP.25.6.1339 [DOI] [PubMed] [Google Scholar]
- 93. Bellini C, Ferri C, Carlomagno A, et al. Impaired inactive to active kallikrein conversion in human salt-sensitive hypertension. J Am Soc Nephrol 1996;7:2565-77. [DOI] [PubMed] [Google Scholar]
- 94. Ferri C, Bellini C, Carlomagno A, Desideri G, Santucci A. Active kallikrein response to changes in sodium-chloride intake in essential hypertensive patients. J Am Soc Nephrol 1996;7:443-53. [DOI] [PubMed] [Google Scholar]
- 95. Grey A, Braatvedt G, Holdaway I. Moderate dietary salt restriction does not alter insulin resistance or serum lipids in normal men. Am J Hypertens 1996;9:317-22. 10.1016/0895-7061(95)00390-8 [DOI] [PubMed] [Google Scholar]
- 96. Inoue J, Cappuccio FP, Sagnella GA, et al. Glucose load and renal sodium handling in mild essential hypertension on different sodium intakes. J Hum Hypertens 1996;10:523-9. [PubMed] [Google Scholar]
- 97. Ishimitsu T, Nishikimi T, Matsuoka H, et al. Behaviour of adrenomedullin during acute and chronic salt loading in normotensive and hypertensive subjects. Clin Sci (Lond) 1996;91:293-8. 10.1042/cs0910293 [DOI] [PubMed] [Google Scholar]
- 98. Schorr U, Distler A, Sharma AM. Effect of sodium chloride- and sodium bicarbonate-rich mineral water on blood pressure and metabolic parameters in elderly normotensive individuals: a randomized double-blind crossover trial. J Hypertens 1996;14:131-5. [PubMed] [Google Scholar]
- 99. Zoccali C, Mallamaci F, Cuzzola F, Leonardis D. Reproducibility of the response to short-term low salt intake in essential hypertension. J Hypertens 1996;14:1455-9. 10.1097/00004872-199612000-00011 [DOI] [PubMed] [Google Scholar]
- 100. Cappuccio FP, Markandu ND, Carney C, Sagnella GA, MacGregor GA. Double-blind randomised trial of modest salt restriction in older people. Lancet 1997;350:850-4. 10.1016/S0140-6736(97)02264-2 [DOI] [PubMed] [Google Scholar]
- 101. The Trials of Hypertension Prevention Collaborative Research Group Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. Arch Intern Med 1997;157:657-67. 10.1001/archinte.1997.00440270105009 [DOI] [PubMed] [Google Scholar]
- 102. McCarron DA, Weder AB, Egan BM, et al. Blood pressure and metabolic responses to moderate sodium restriction in isradipine-treated hypertensive patients. Am J Hypertens 1997;10:68-76. 10.1016/S0895-7061(96)00295-6 [DOI] [PubMed] [Google Scholar]
- 103. Meland E, Laerum E, Aakvaag A, Ulvik RJ, Høstmark AT. Salt restriction: effects on lipids and insulin production in hypertensive patients. Scand J Clin Lab Invest 1997;57:501-5. 10.3109/00365519709084600 [DOI] [PubMed] [Google Scholar]
- 104. Schorr U, Turan S, Distler A, Sharma AM. Relationship between ambulatory and resting blood pressure responses to dietary salt restriction in normotensive men. J Hypertens 1997;15:845-9. 10.1097/00004872-199715080-00007 [DOI] [PubMed] [Google Scholar]
- 105. Yamamoto H. Randomized controlled trial of salt-restriction program for primary prevention of hypertension in the community. J Osaka City Med Center. 1997;46:255-67. [Google Scholar]
- 106. Foo M, Denver AE, Coppack SW, Yudkin JS. Effect of salt-loading on blood pressure, insulin sensitivity and limb blood flow in normal subjects. Clin Sci (Lond) 1998;95:157-64. 10.1042/cs0950157 [DOI] [PubMed] [Google Scholar]
- 107. Gomi T, Shibuya Y, Sakurai J, Hirawa N, Hasegawa K, Ikeda T. Strict dietary sodium reduction worsens insulin sensitivity by increasing sympathetic nervous activity in patients with primary hypertension. Am J Hypertens 1998;11:1048-55. 10.1016/S0895-7061(98)00126-5 [DOI] [PubMed] [Google Scholar]
- 108. Herlitz H, Dahlöf B, Jonsson O, Friberg P. Relationship between salt and blood pressure in hypertensive patients on chronic ACE-inhibition. Blood Press 1998;7:47-52. 10.1080/080370598437565 [DOI] [PubMed] [Google Scholar]
- 109. Wing LM, Arnolda LF, Harvey PJ, et al. Low-dose diuretic and/or dietary sodium restriction when blood pressure is resistant to ACE inhibitor. Blood Press 1998;7:299-307. 10.1080/080370598437169 [DOI] [PubMed] [Google Scholar]
- 110. Davrath LR, Gotshall RW, Tucker A, et al. Moderate sodium restriction does not alter lower body negative pressure tolerance. Aviat Space Environ Med 1999;70:577-82. [PubMed] [Google Scholar]
- 111. Schorr U, Blaschke K, Beige J, Distler A, Sharma AM. Angiotensinogen M235T variant and salt sensitivity in young normotensive Caucasians. J Hypertens 1999;17:475-9. 10.1097/00004872-199917040-00004 [DOI] [PubMed] [Google Scholar]
- 112. Uzu T, Fujii T, Nishimura M, et al. Determinants of circadian blood pressure rhythm in essential hypertension. Am J Hypertens 1999;12:35-9. 10.1016/S0895-7061(98)00182-4 [DOI] [PubMed] [Google Scholar]
- 113. Boero R, Pignataro A, Bancale E, et al. [Metabolic effects of changes in dietary sodium intake in patients with essential hypertension] [Italian]. Minerva Urol Nefrol 2000;52:13-6. [PubMed] [Google Scholar]
- 114. Ames RP. The effect of sodium supplementation on glucose tolerance and insulin concentrations in patients with hypertension and diabetes mellitus. Am J Hypertens 2001;14:653-9. 10.1016/S0895-7061(01)01310-3 [DOI] [PubMed] [Google Scholar]
- 115. Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE). Arch Intern Med 2001;161:685-93. 10.1001/archinte.161.5.685 [DOI] [PubMed] [Google Scholar]
- 116. Johnson AG, Nguyen TV, Davis D. Blood pressure is linked to salt intake and modulated by the angiotensinogen gene in normotensive and hypertensive elderly subjects. J Hypertens 2001;19:1053-60. 10.1097/00004872-200106000-00009 [DOI] [PubMed] [Google Scholar]
- 117. Akita S, Sacks FM, Svetkey LP, Conlin PR, Kimura G, DASH-Sodium Trial Collaborative Research Group Effects of the Dietary Approaches to Stop Hypertension (DASH) diet on the pressure-natriuresis relationship. Hypertension 2003;42:8-13. 10.1161/01.HYP.0000074668.08704.6E [DOI] [PubMed] [Google Scholar]
- 118. Dishy V, Sofowora GG, Imamura H, et al. Nitric oxide production decreases after salt loading but is not related to blood pressure changes or nitric oxide-mediated vascular responses. J Hypertens 2003;21:153-7. 10.1097/00004872-200301000-00025 [DOI] [PubMed] [Google Scholar]
- 119. Nowson CA, Morgan TO, Gibbons C. Decreasing dietary sodium while following a self-selected potassium-rich diet reduces blood pressure. J Nutr 2003;133:4118-23. 10.1093/jn/133.12.4118 [DOI] [PubMed] [Google Scholar]
- 120. Pechère-Bertschi A, Maillard M, Stalder H, et al. Renal hemodynamic and tubular responses to salt in women using oral contraceptives. Kidney Int 2003;64:1374-80. 10.1046/j.1523-1755.2003.00239.x [DOI] [PubMed] [Google Scholar]
- 121. Perry CG, Palmer T, Cleland SJ, et al. Decreased insulin sensitivity during dietary sodium restriction is not mediated by effects of angiotensin II on insulin action. Clin Sci (Lond) 2003;105:187-94. 10.1042/CS20020320 [DOI] [PubMed] [Google Scholar]
- 122. Beeks E, van der Klauw MM, Kroon AA, Spiering W, Fuss-Lejeune MJ, de Leeuw PW. Alpha-adducin Gly460Trp polymorphism and renal hemodynamics in essential hypertension. Hypertension 2004;44:419-23. 10.1161/01.HYP.0000141410.72537.fd [DOI] [PubMed] [Google Scholar]
- 123. van Berge-Landry H, James GD. Serum electrolyte, serum protein, serum fat and renal responses to a dietary sodium challenge: allostasis and allostatic load. Ann Hum Biol 2004;31:477-87. 10.1080/03014460412331281746 [DOI] [PubMed] [Google Scholar]
- 124. Gates PE, Tanaka H, Hiatt WR, Seals DR. Dietary sodium restriction rapidly improves large elastic artery compliance in older adults with systolic hypertension. Hypertension 2004;44:35-41. 10.1161/01.HYP.0000132767.74476.64 [DOI] [PubMed] [Google Scholar]
- 125. Forrester T, Adeyemo A, Soarres-Wynter S, et al. A randomized trial on sodium reduction in two developing countries. J Hum Hypertens 2005;19:55-60. 10.1038/sj.jhh.1001782 [DOI] [PubMed] [Google Scholar]
- 126. Swift PA, Markandu ND, Sagnella GA, He FJ, MacGregor GA. Modest salt reduction reduces blood pressure and urine protein excretion in black hypertensives: a randomized control trial. Hypertension 2005;46:308-12. 10.1161/01.HYP.0000172662.12480.7f [DOI] [PubMed] [Google Scholar]
- 127. Cappuccio FP, Kerry SM, Micah FB, Plange-Rhule J, Eastwood JB. A community programme to reduce salt intake and blood pressure in Ghana [ISRCTN88789643]. BMC Public Health 2006;6:13. 10.1186/1471-2458-6-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Ho JT, Keogh JB, Bornstein SR, et al. Moderate weight loss reduces renin and aldosterone but does not influence basal or stimulated pituitary-adrenal axis function. Horm Metab Res 2007;39:694-9. 10.1055/s-2007-985354 [DOI] [PubMed] [Google Scholar]
- 129. Melander O, von Wowern F, Frandsen E, et al. Moderate salt restriction effectively lowers blood pressure and degree of salt sensitivity is related to baseline concentration of renin and N-terminal atrial natriuretic peptide in plasma. J Hypertens 2007;25:619-27. 10.1097/HJH.0b013e328013cd50 [DOI] [PubMed] [Google Scholar]
- 130. Townsend RR, Kapoor S, McFadden CB. Salt intake and insulin sensitivity in healthy human volunteers. Clin Sci (Lond) 2007;113:141-8. 10.1042/CS20060361 [DOI] [PubMed] [Google Scholar]
- 131. Jessani S, Hatcher J, Chaturvedi N, Jafar TH. Effect of low vs. high dietary sodium on blood pressure levels in a normotensive Indo-Asian population. Am J Hypertens 2008;21:1238-44. 10.1038/ajh.2008.256 [DOI] [PubMed] [Google Scholar]
- 132. Tzemos N, Lim PO, Wong S, Struthers AD, MacDonald TM. Adverse cardiovascular effects of acute salt loading in young normotensive individuals. Hypertension 2008;51:1525-30. 10.1161/HYPERTENSIONAHA.108.109868 [DOI] [PubMed] [Google Scholar]
- 133. Visser FW, Boonstra AH, Titia Lely A, Boomsma F, Navis G. Renal response to angiotensin II is blunted in sodium-sensitive normotensive men. Am J Hypertens 2008;21:323-8. 10.1038/ajh.2007.63 [DOI] [PubMed] [Google Scholar]
- 134. Dickinson KM, Keogh JB, Clifton PM. Effects of a low-salt diet on flow-mediated dilatation in humans. Am J Clin Nutr 2009;89:485-90. 10.3945/ajcn.2008.26856 [DOI] [PubMed] [Google Scholar]
- 135. He FJ, Marciniak M, Visagie E, et al. Effect of modest salt reduction on blood pressure, urinary albumin, and pulse wave velocity in white, black, and Asian mild hypertensives. Hypertension 2009;54:482-8. 10.1161/HYPERTENSIONAHA.109.133223 [DOI] [PubMed] [Google Scholar]
- 136. Meland E, Aamland A. Salt restriction among hypertensive patients: modest blood pressure effect and no adverse effects. Scand J Prim Health Care 2009;27:97-103. 10.1080/02813430802661795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Paulsen L, Holst LM, Bech JN, Starklint J, Pedersen EB. Glomerular filtration rate and blood pressure are unchanged by increased sodium intake in atorvastatin-treated healthy men. Scand J Clin Lab Invest 2009;69:323-9. 10.1080/00365510802571007 [DOI] [PubMed] [Google Scholar]
- 138. Pimenta E, Gaddam KK, Oparil S, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension 2009;54:475-81. 10.1161/HYPERTENSIONAHA.109.131235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Weir MR, Yadao AM, Purkayastha D, Charney AN. Effects of high- and low-sodium diets on ambulatory blood pressure in patients with hypertension receiving aliskiren. J Cardiovasc Pharmacol Ther 2010;15:356-63. 10.1177/1074248410377173 [DOI] [PubMed] [Google Scholar]
- 140. Zanchi A, Maillard M, Jornayvaz FR, et al. Effects of the peroxisome proliferator-activated receptor (PPAR)-gamma agonist pioglitazone on renal and hormonal responses to salt in diabetic and hypertensive individuals. Diabetologia 2010;53:1568-75. 10.1007/s00125-010-1756-2 [DOI] [PubMed] [Google Scholar]
- 141. Starmans-Kool MJ, Stanton AV, Xu YY, McG Thom SA, Parker KH, Hughes AD. High dietary salt intake increases carotid blood pressure and wave reflection in normotensive healthy young men. J Appl Physiol (1985) 2011;110:468-71. 10.1152/japplphysiol.00917.2010 [DOI] [PubMed] [Google Scholar]
- 142. Carey RM, Schoeffel CD, Gildea JJ, et al. Salt sensitivity of blood pressure is associated with polymorphisms in the sodium-bicarbonate cotransporter. Hypertension 2012;60:1359-66. 10.1161/HYPERTENSIONAHA.112.196071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Graffe CC, Bech JN, Pedersen EB. Effect of high and low sodium intake on urinary aquaporin-2 excretion in healthy humans. Am J Physiol Renal Physiol 2012;302:F264-75. 10.1152/ajprenal.00442.2010 [DOI] [PubMed] [Google Scholar]
- 144. Bonfils PK, Taskiran M, Damgaard M, et al. The influence of high versus low sodium intake on blood pressure and haemodynamics in patients with morbid obesity. J Hypertens 2013;31:2220-9, discussion 2229. 10.1097/HJH.0b013e328363c769 [DOI] [PubMed] [Google Scholar]
- 145. Mallamaci F, Leonardis D, Pizzini P, Cutrupi S, Tripepi G, Zoccali C. Procalcitonin and the inflammatory response to salt in essential hypertension: a randomized cross-over clinical trial. J Hypertens 2013;31:1424-30, discussion 1430. 10.1097/HJH.0b013e328360ddd5 [DOI] [PubMed] [Google Scholar]
- 146. Allen AR, Gullixson LR, Wolhart SC, Kost SL, Schroeder DR, Eisenach JH. Dietary sodium influences the effect of mental stress on heart rate variability: a randomized trial in healthy adults. J Hypertens 2014;32:374-82. 10.1097/HJH.0000000000000045 [DOI] [PubMed] [Google Scholar]
- 147. Cavka A, Cosic A, Jukic I, et al. The role of cyclo-oxygenase-1 in high-salt diet-induced microvascular dysfunction in humans. J Physiol 2015;593:5313-24. 10.1113/JP271631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Gijsbers L, Dower JI, Schalkwijk CG, et al. Effects of sodium and potassium supplementation on endothelial function: a fully controlled dietary intervention study. Br J Nutr 2015;114:1419-26. 10.1017/S0007114515002986 [DOI] [PubMed] [Google Scholar]
- 149. He FJ, Wu Y, Feng XX, et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ 2015;350:h770. 10.1136/bmj.h770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Matthews EL, Brian MS, Ramick MG, Lennon-Edwards S, Edwards DG, Farquhar WB. High dietary sodium reduces brachial artery flow-mediated dilation in humans with salt-sensitive and salt-resistant blood pressure. J Appl Physiol (1985) 2015;118:1510-5. 10.1152/japplphysiol.00023.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Pinjuh Markota N, Rumboldt M, Rumboldt Z. Emphasized warning reduces salt intake: a randomized controlled trial. J Am Soc Hypertens 2015;9:214-20. 10.1016/j.jash.2014.12.022 [DOI] [PubMed] [Google Scholar]
- 152. Riphagen IJ, Gijsbers L, van Gastel MD, et al. Effects of potassium supplementation on markers of osmoregulation and volume regulation: results of a fully controlled dietary intervention study. J Hypertens 2016;34:215-20. 10.1097/HJH.0000000000000786 [DOI] [PubMed] [Google Scholar]
- 153. Suckling RJ, He FJ, Markandu ND, MacGregor GA. Modest salt reduction lowers blood pressure and albumin excretion in impaired glucose tolerance and type 2 diabetes mellitus: A randomized double-blind trial. Hypertension 2016;67:1189-95. 10.1161/HYPERTENSIONAHA.115.06637 [DOI] [PubMed] [Google Scholar]
- 154. Brian MS, Dalpiaz A, Matthews EL, Lennon-Edwards S, Edwards DG, Farquhar WB. Dietary sodium and nocturnal blood pressure dipping in normotensive men and women. J Hum Hypertens 2017;31:145-50. 10.1038/jhh.2016.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Gefke M, Christensen NJ, Bech P, et al. Hemodynamic responses to mental stress during salt loading. Clin Physiol Funct Imaging 2017;37:688-94. 10.1111/cpf.12360 [DOI] [PubMed] [Google Scholar]
- 156. Babcock MC, Brian MS, Watso JC, et al. Alterations in dietary sodium intake affect cardiovagal baroreflex sensitivity. Am J Physiol Regul Integr Comp Physiol 2018;315:R688-95. 10.1152/ajpregu.00002.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Parvanova A, Trillini M, Podestà MA, et al. PROCEED Study Organization and the Scientific Writing Academy (SWA) 2016 Moderate salt restriction with or without paricalcitol in type 2 diabetes and losartan-resistant macroalbuminuria (PROCEED): a randomised, double-blind, placebo-controlled, crossover trial. Lancet Diabetes Endocrinol 2018;6:27-40. 10.1016/S2213-8587(17)30359-5 [DOI] [PubMed] [Google Scholar]
- 158. Rorije NMG, Olde Engberink RHG, Chahid Y, et al. Microvascular permeability after an acute and chronic salt load in healthy subjects: a randomized open-label crossover intervention study. Anesthesiology 2018;128:352-60. 10.1097/ALN.0000000000001989 [DOI] [PubMed] [Google Scholar]
- 159. Wang Y, Chu C, Wang KK, et al. Effect of salt intake on plasma and urinary uric acid levels in Chinese adults: an interventional trial. Sci Rep 2018;8:1434. 10.1038/s41598-018-20048-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Cutler JA, Follmann D, Allender PS. Randomized trials of sodium reduction: an overview. Am J Clin Nutr 1997;65(Suppl):643S-51S. 10.1093/ajcn/65.2.643S [DOI] [PubMed] [Google Scholar]
- 161. Ebrahim S, Smith GD. Lowering blood pressure: a systematic review of sustained effects of non-pharmacological interventions. J Public Health Med 1998;20:441-8. 10.1093/oxfordjournals.pubmed.a024800 [DOI] [PubMed] [Google Scholar]
- 162. Graudal NA, Galløe AM, Garred P. Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride: a meta-analysis. JAMA 1998;279:1383-91. 10.1001/jama.279.17.1383 [DOI] [PubMed] [Google Scholar]
- 163. Jürgens G, Graudal NA. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride. Cochrane Database Syst Rev 2004;(1):CD004022. 10.1002/14651858.CD004022.pub2 [DOI] [PubMed] [Google Scholar]
- 164. Mozaffarian D, Fahimi S, Singh GM, et al. Global Burden of Diseases Nutrition and Chronic Diseases Expert Group Global sodium consumption and death from cardiovascular causes. N Engl J Med 2014;371:624-34. 10.1056/NEJMoa1304127 [DOI] [PubMed] [Google Scholar]
- 165. Rhee OJ, Rhee MY, Oh SW, et al. Effect of sodium intake on renin level: Analysis of general population and meta-analysis of randomized controlled trials. Int J Cardiol 2016;215:120-6. 10.1016/j.ijcard.2016.04.109 [DOI] [PubMed] [Google Scholar]
- 166. He FJ, Markandu ND, Sagnella GA, MacGregor GA. Importance of the renin system in determining blood pressure fall with salt restriction in black and white hypertensives. Hypertension 1998;32:820-4. 10.1161/01.HYP.32.5.820 [DOI] [PubMed] [Google Scholar]
- 167. Peters RM, Flack JM. Salt sensitivity and hypertension in African Americans: implications for cardiovascular nurses. Prog Cardiovasc Nurs 2000;15:138-44. 10.1111/j.0889-7204.2000.080404.x [DOI] [PubMed] [Google Scholar]
- 168. Mente A, O’Donnell M, Rangarajan S, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet 2018;392:496-506. 10.1016/S0140-6736(18)31376-X [DOI] [PubMed] [Google Scholar]
- 169. Cogswell ME, Mugavero K, Bowman BA, Frieden TR. Dietary sodium and cardiovascular disease risk–measurement matters. N Engl J Med 2016;375:580-6. 10.1056/NEJMsb1607161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Juraschek SP, Woodward M, Sacks FM, Carey VJ, Miller ER, 3rd, Appel LJ. Time course of change in blood pressure from sodium reduction and the DASH diet. Hypertension 2017;70:923-9. 10.1161/HYPERTENSIONAHA.117.10017 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary figures 1-5
Web appendix: supplementary files 1-3