Abstract
Purpose
Mindfulness based interventions (MBIs) are an emerging area of empirical study, not only in positive psychology, but also in clinical health care. This research aims to synthesize the evidence about whether MBIs reduce blood pressure (BP) in patients with non-communicable diseases (NCDs).
Methods
Relevant studies were identified via PubMed, the Cochrane Library, Embase and the CINAHL database between 2009 and 2019. The papers selected focused on mindfulness and the effect of these on the BP of patients with NCDs. The change in SBP and DBP were meta-analyzed, stratified by type of intervention (Breathing awareness meditation (BAM), Mindfulness Meditation (MM), and Mindfulness-based Stress Reduction (MBSR).
Results
Fourteen articles met eligibility criteria and were included in the final review. Among the studies using the type and duration of intervention, systolic BP was reduced after the mindfulness-based stress reduction for 8 weeks (-6.90 mmHg [95% CI: -10.82, -2.97], p < .050), followed by the breathing awareness meditation for 12 weeks (-4.10 mmHg [95% CI: -7.54, -0.66], p < .050) and the mindfulness-based intervention for 8 weeks (-2.69 mmHg [95% CI: -3.90, -1.49], p < .050) whereas diastolic BP was reduced after the mindfulness-based stress reduction for 8 weeks (-2.45 mmHg [95% CI: -3.74, -1.17], p < .050) and the mindfulness-based intervention for 8 weeks (-2.24 mmHg [95% CI: -3.22, -1.26], p < .050).
Conclusion
MBIs can provide effective alternative therapies to assist in blood pressure reduction for patients with NCDs.
Keywords: Public health, Health profession, Nursing, Blood pressure, Meta-analysis, Non-communicable diseases, Mindfulness, Systematic review
Public health; Health profession; Nursing; Blood pressure; Meta-analysis; Non-communicable diseases; Mindfulness; Systematic review.
1. Introduction
The World Health Organisation (2018) defines non-communicable diseases (NCDs) as, non-infectious diseases, caused by combinations of genetics, physiology, behavioural and environmental factors, that tend to be of long duration and to progress slowly [1]. They include cancers, cardiovascular diseases, respiratory diseases and diabetes. The United Nations has recognized the growing incidence of NCDs as constituting a global health crisis [2]. Each year, cardiovascular disease accounts for the deaths of 18 million people, with cancers killing 9 million, respiratory diseases 4 million, and diabetes 1.6 million worldwide [1]. It is suggested that the stress which these diseases put on the bodies of sufferers trigger physiological responses induced by the sympathetic nervous system, causing the body to release cortisol, which increases blood pressure (BP) [3]. Elevated BP is known as the ‘silent killer’ because it usually has no symptoms, so people are unaware of its presence unless BP is routinely measured. Even when individuals are aware of having high BP, they frequently still ignore it since they do not experience any symptoms and consequently they may face complications such as cerebral hemorrhage, stroke and ischemic heart disease [4]. These conditions causes suffering and economic loss to the individual, their family, society and country [4]. Reducing BP can reduce the risk of developing cardiovascular diseases as well as the risk of mortality [5]. Treatment for reducing BP includes medication and health-enhancing lifestyle changes. However, despite advances in BP treatment, there is still a high percentage of the population who with high BP and who are unable to control their BP level [6]. In addition, while antihypertensive drugs are effective, they can produce side effects such as insomnia, sedation, dry mouth, drowsiness and headaches and are quite expensive [7]. Many studies found that improved coping with stress can reduce BP by reducing the sympathetic nervous system's responses to stress [8].
Mindfulness was originally developed from Buddhist contemplative traditions integrated with meditation. It can help patients become more aware of changes in their cognitions and emotions and increase their levels of self-acceptance, thereby reducing worry and stress. Mindfulness within positive psychology was developed and used in treatment by Kabat-Zinn (1979). He defined mindfulness as non-judgmentally paying attention, on purpose, in the present moment [9]. Mindfulness interventions with patients have become increasingly popular. One pioneering example is the Mindfulness-based Stress Reduction (MBSR) program [10]. The program is made up of 8 sessions over 8 weeks with regular home practice. It includes sitting and walking meditation and yoga. In Grossman and colleagues'study, a meta-analysis of 20 studies utilizing MBSR for patients with diverse conditions such as cancer, sleep disorders, eating disorders, psoriasis, diabetes and heart diseases reported that MBSR can help individuals cope with physical, psychosomatic, psychiatric disorders to improve their well-being [10] and to reduce the arterial BP on the average 6 mmHg in patients with Type 2 diabetes mellitus [11]. Another program called Breathing Awareness Meditation (BAM) focuses on diaphragm movements while the patient breathes deeply and slowly with their eyes closed for 10 min. This helps calm the sympathetic nervous system and activates the parasympathetic nervous system simultaneously, leading to a relaxation response [12]. The program includes health education and requires practice at home. One study reported that a BAM program significantly reduced 24-hour SBP compared with an education and lifestyle modification program [13]. Another study found that BAM significantly reduced blood pressures and heart rates of 166 African American participants [14].
Despite the increasing popularity of Mindfulness Based Interventions (MBIs), there is a lack of consensual knowledge about their effectiveness in reducing BP in patients with NCDs. This present study aimed to address this by undertaking a systematic review and meta-analysis to evaluate the effectiveness of MBIs in BP reduction in patients with NCDs.
2. Methods
The first step involved conducting a preliminary literature review to determine definitions and get an overview of the research procedures being used. From this a conceptual framework for the meta-analysis was obtained that allowed a research synthesis framework to be developed. The third stage involved undertaking a systematic literature review from the PubMed, Cochrane Library, Embase, and CINAHL to identify papers with sufficient information for the research synthesis. To ensure standardization in the data collection, a data collection form was developed and piloted using data from 10 published experimental research studies. After modification it was utilized to record details of the selected research papers. Next a preliminary data analysis was performed to calculate descriptive statistics by analyzing the variables related to a) the research papers b) the researchers and c) the research methodologies. Finally, the meta-analysis was conducted. To ensure a rigorous approach to reporting the procedure the PRISMA guidance was followed. Ethical approval was obtained from the Institutional Review Board of Srinakharinwirot University, approval no. SWUEC-264/60.
2.1. Search strategy
We searched the PubMed, Cochrane Library, Embase, and CINAHL databases for articles published from January 2009 to April 2019. The search was conducted using the following terms: Population: patients with NCDs; Intervention: mindfulness; Comparator: standard care OR usual care OR attention control; Outcome: blood pressure; Study type: randomized controlled trial OR RCT OR clinical trial and NOT review.
2.2. Selection criteria
The studies had to be published in peer reviewed journals in English and be accessible and use experimental designs. Mindfulness interventions were defined as involving the following: the practice of paying attention, moment-to-moment to promote coping with stress, illness, and pain with the aim of improving patient health. Studies had to include quantitative assessment of the effectiveness of the mindfulness interventions with measurable BP relevant to NCDs with sufficient statistical information to allow for meta-analysis.
2.3. Data collection and analysis
Study Selection. The PubMed, Cochrane Library, Embase, and CINAHL databases were selected as they are the largest data bases for international peer-reviewed research providing comprehensive coverage of science, medicine, and social sciences which are all relevant inter-disciplinary areas. The focus was on identifying mindfulness interventions in patients with NCDs published between 2009 and 2019. The terms included: 1) Mindfulness interventions; 2) BP reported as a measure; 3) Randomized controlled studies; 4) The most recent studies (2009–2019); and 5) Publication in English and in a peer-reviewed journal. Once papers meeting these criteria had been identified, the authors checked the references in these papers for other papers that might be relevant. They also used their own knowledge of the literature.
Data Extraction and Quality Assessment. Data extraction and study quality assessment were performed by two independent reviewers. Disagreements between the reviewers were resolved by discussion. Data were collected on the patient characteristics, study design, control group, intervention characteristics, BP measurement, and results.
To assess the methodological quality of the studies the seven criteria outlined in the Cochrane Handbook [15], were utilized. These criteria are assessed as "high", "moderate" or "low" in quality. The seven criteria are: (1) control of quality: intervention standardization via a manual or published guidance; (2) adequate randomization occurring (3) baseline comparability: similarities in the baseline characteristics of intervention and control groups; (4) completeness of follow-up data; (5) reporting of dropout rates and their acceptability; (6) blind assessment of outcomes; (7) an intention-to-treat analysis for handling missing data. Each criterion was rated as 0 when it was not met or 1 when it is met. Research was evaluated independently by two reviewers and scores summated for each. The methodological quality of study was assessed as being high when six or seven criteria were met with a follow-up rate of 90%, medium when four to five criteria were met and low when three or less were met. Any differences were discussed till agreement was reached.
Data Synthesis. In this research, Statistical analyses were conducted using the Stata statistical software package (version 12, Stata Corporation, College Station, Tex). Data were presented as standardized mean differences (SMDs) and 95% confidence interval. The standardized mean differences were calculated for each comparison and referred to intervention results compared to control results after intervention. They were performed by Metan-meta-analysis command. When interpreting the standardized effect size, a negative effect size represents better results for intervention than for control group [16].
Identical analysis was used for each condition and outcome. A random-effects model was used to pool the effect size of all the studies and an associated 95% confidence intervals (CIs) was estimated. Sensitivity analyses and subgroup analyses were performed. A chi-square test of heterogeneity p value was used to evaluate the heterogeneity between the studies. Cochrane's Q test and Higgins' I2 statistics investigated heterogeneity. The differences between studies could be seen as the proportion of total variation rather than a sampling error. A heterogeneous meta-analysis is I2 > 75%, and for this a random-effects model was used. A I2 value of 0% indicates an absence of dispersion, and larger values show increasing levels of heterogeneity where 25% can be considered as low, 50% as moderate and 75% as a high level of heterogeneity, respectively. We conducted funnel plots and tested their symmetry to examined publication bias.
3. Results
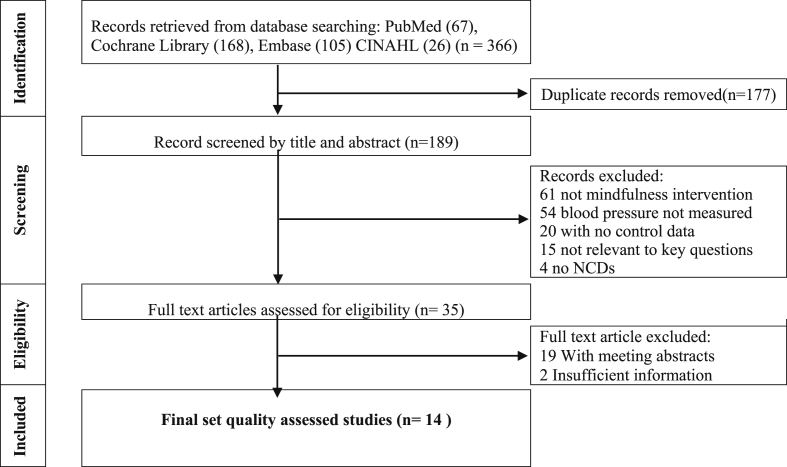
We identified 366 publications in the PubMed, Cochrane Library, Embase, and CINAHL database between 2009 and 2019. Following this, the titles and abstracts with duplicates were removed, 189 articles were identified as being potentially eligible for inclusion. From these, 154 were removed because they were found to have no mindfulness intervention, no NCDs, no appropriate outcomes, no control group and/or not relevant to the key questions. This left 35 articles potentially eligible for inclusion. Finally, 21 were removed because they were found to be conference abstracts and/or to have insufficient information to calculate the effect sizes. Therefore, 14 articles were included in the meta-analysis. All of the selected papers reported experimental research that studied independent variables related to mindfulness interventions and dependent variables including BP in patients with NCDs as given in Figure 1.
Figure 1.
Flow diagram of article selection.
3.1. Characteristics of included studies
The characteristics of the 14 studies, including the population, intervention, and outcomes are described in Table 1.
Table 1.
Characteristics of the studies.
| Authors (year) | Patient character-istic | Design | Control group | N | Ni | Nc | Intervention (the number of sessions, duration of intervention) | BP measure-ment | Results of Blood Pressure Reduction | Quality assess-ment |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Blom et al. (2014) [17] | Patients with unmedicated stage 1 hypertension | Randomized controlled trial | Wait-list control | 87 | 46 | 41 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) |
24-hour ABP | No significant group differences were found for all ambulatory BP parameters after the intervention | High |
| 2. Campbell et al. (2012) [18] | Patients with cancer | Quasi-experimental, pre- and posttest control group design | Wait-list control | 70 | 39 | 31 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) |
24-hour ABP | No significant group differences were found for BP parameters after the intervention | Medium |
| 3. Gotink et al. (2017) [19] | Patients with heart disease | Single blinded, pragmatic RCT | Usual care | 324 | 215 | 109 | Mindfulness-Based Stress Reduction, (12 sessions, 12 months) |
Clinic BP |
Significant group differences were found for changes in SBP after the intervention | High |
| 4. Hartmann et al. (2012) [20] | Patients at high risk of diabetes complications | Randomized controlled trial | Treatment-as-usual group (TAU) | 110 | 53 | 57 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) | 24-hour ABP | Significant group differences were found for changes in DBP after the intervention | High |
| 5. Hughes et al. (2013) [21] | Patients with unmedicated prehypertension | Randomized controlled trial | Progressive muscle relaxation training (PMR). | 56 | 28 | 28 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) | 24-hour ABP | Significant group differences were found for changes in SBP and DBP after the intervention | High |
| 6. Kumar et al. (2017) [22] | Patients with type-2 diabetes | Randomized Pilot Study | Control group | 40 | 20 | 20 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) | Clinic BP | Significant group differences were found for changes in SBP after the intervention No significant group differences for changes in DBP |
Medium |
| 7. Momeni et al. (2016) [23] | Patients with cardiovascular disease | Single-blind randomized controlled trial | Control group | 60 | 30 | 30 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) | Clinic BP | Significant group differences were found for changes in SBP after the intervention | High |
| 8. Nejati et al. (2015) [24] | Patients with hypertension | Quasi-experimental study with a control group | Yoga training | 30 | 15 | 15 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) | Clinic BP | Significant group differences were found for changes in SBP DBP after the intervention | Medium |
| 9.Ng et al. (2016) [25] | Patients with cancer | Randomized controlled trial | The normal listening group | 60 | 30 | 30 | Breathing awareness meditation (1 sessions, 1 day) | Clinic BP | Significant group differences were found for changes in SBP and DBP after the intervention | Medium |
| 10. Palta et al. (2012) [26] | Low-Income African-American Older Adults with cardiovascular disease | Prospective randomized controlled trial | Social support | 20 | 12 | 8 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) | Clinic BP | Significant group differences were found for changes in SBP and DBP after the intervention | Medium |
| 11. Parswani et al. (2013) [27] | Patients with cardiovascular disease | Randomized controlled trial | Treatment-as-usual group (TAU) | 30 | 15 | 15 | Mindfulness-Based Stress Reduction, (8 sessions, 8 weeks) | Clinic BP | Significant group differences were found for all BP parameters after the intervention | Medium |
| 12. Pearson et al. (2018) [28] | Patients with diabetes | Randomized controlled trial | Usual care | 67 | 31 | 36 | Mindfulness-based intervention (8 sessions, 8 weeks) | Clinic BP | Significant group differences were found for changes in SBP after the intervention | Medium |
| 13. Ponte Marquez et al. (2019) [29] | Patients with arterial hypertension | Randomized controlled trial | Health education | 42 | 24 | 18 | Mindfulness-based intervention (8 sessions, 8 weeks) | 24-hour ABP | Significant group differences were found for changes in SBP and DBP after the intervention | High |
| 14. Wright et al. (2011) [30] | African American Adolescents with hypertension | Randomized single-blind | Health education | 121 | 35 | 44 | Breathing awareness meditation, (12 sessions, 12 weeks) | 24-hour ABP | Significant group differences were found for changes in SBP after the intervention | Medium |
Design (RCT, randomized controlled trial; QE, quasi experimental design); N, total number of subjects in this study; Ni, number of subjects in the intervention group; Nc, number of subjects in the control group; BP measurement (24-h ABP, 24-h ambulatory blood pressure; Clinic BP, clinic blood pressure).
All of the papers aimed to assess the effectiveness of mindfulness interventions and 10 (71.4%) adopted randomized controlled trial designs. The 14 studies assessed 1,117 patients, of which 593 were in intervention groups and 482 were in control groups and all studied the effects of mindfulness interventions on BP. Nine papers (62.3%) were on patients with cardiovascular disease, followed by three (21.4%) on diabetes mellitus, and two (14.3%) on cancer. The inter-rater correlation for the quality assessment of the studies was considered to be moderate agreement (kappa = 0.73, Standard Error: 0.15, p ≤ .001) [31]. The quality scores shown are those agreed upon after discussion. The quality scoring ranged from 1 to 7. Eight studies were rated as medium quality and six were high quality.
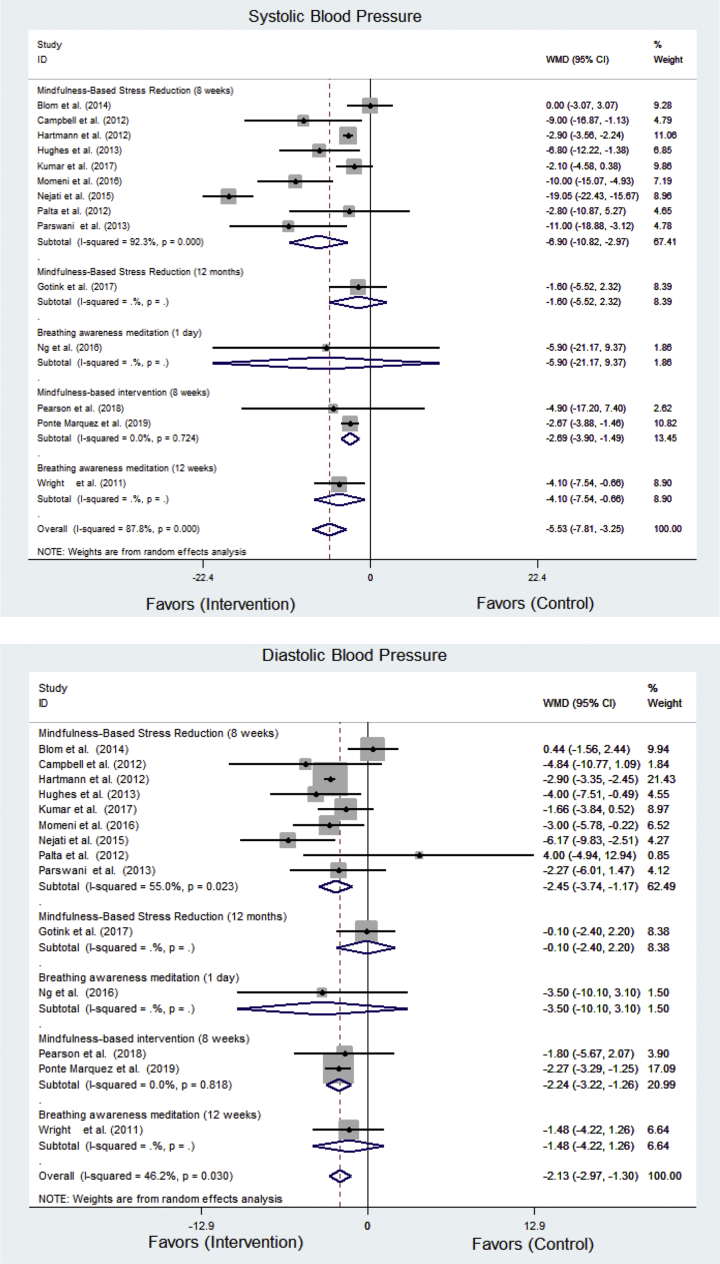
With random effects meta-analyses, the pooled estimate of the mean intervention effect on BP was high with significant effects in comparison to the control groups for SBP (-5.53 mmHg [95% CI: -7.81, -3.25]) and DBP (-2.13 mmHg [95% CI: -2.97, -1.30]) Heterogeneity was high for SBP (Q = 106.46; p < .001; I2 = 87.8%) and DBP (Q = 24.17; p < .001; I2 = 46.2%).
3.2. Subgroup analyses
Comparisons between the intervention and control groups, resulted in negative effect sizes indicating that BP levels were lower in the intervention groups compared with the control groups. The detailed results are presented in Figure 2.
Figure 2.
Forest plot showing effects of mindfulness intervention on blood pressure.
For systolic BP was reduced after the mindfulness-based stress reduction for 8 weeks (-6.90 mmHg [95% CI: -10.82, -2.97], p < .050), followed by the breathing awareness meditation for 12 weeks (-4.10 mmHg [95% CI: -7.54, -0.66], p < .050) and the mindfulness-based intervention for 8 weeks (-2.69 mmHg [95% CI: -3.90, -1.49], p < .050) but not after a 5-minute mindful breathing (-5.90 mmHg [95% CI: -21.17, 9.37], p > .050) and the online mindfulness-based stress reduction for 12 months (-1.60 mmHg [95% CI: -5.52, 2.32], p > .050). For diastolic BP was reduced after the mindfulness-based stress reduction for 8 weeks (-2.45 mmHg [95% CI: -3.74, -1.17], p < .050) and the mindfulness-based intervention for 8 weeks (-2.24 mmHg [95% CI: -3.22, -1.26], p < .050), but not after a 5-minute mindful breathing (-3.50 mmHg [95% CI: -10.11, 3.11], p > .050), the breathing awareness meditation for 12 weeks (-1.48 mmHg [95% CI: -4.22, -1.26], p > .050), the online mindfulness-based stress reduction for 12 months (-0.10 mmHg [95% CI: -2.40, 2.20], p > .050).
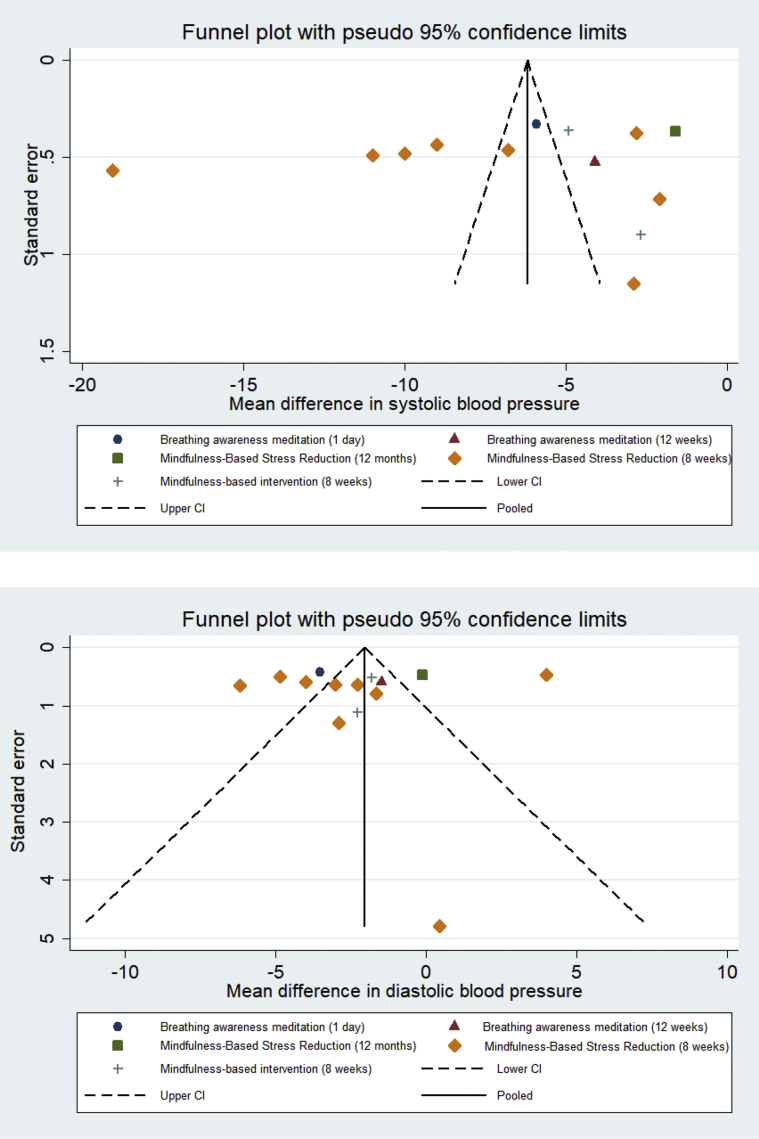
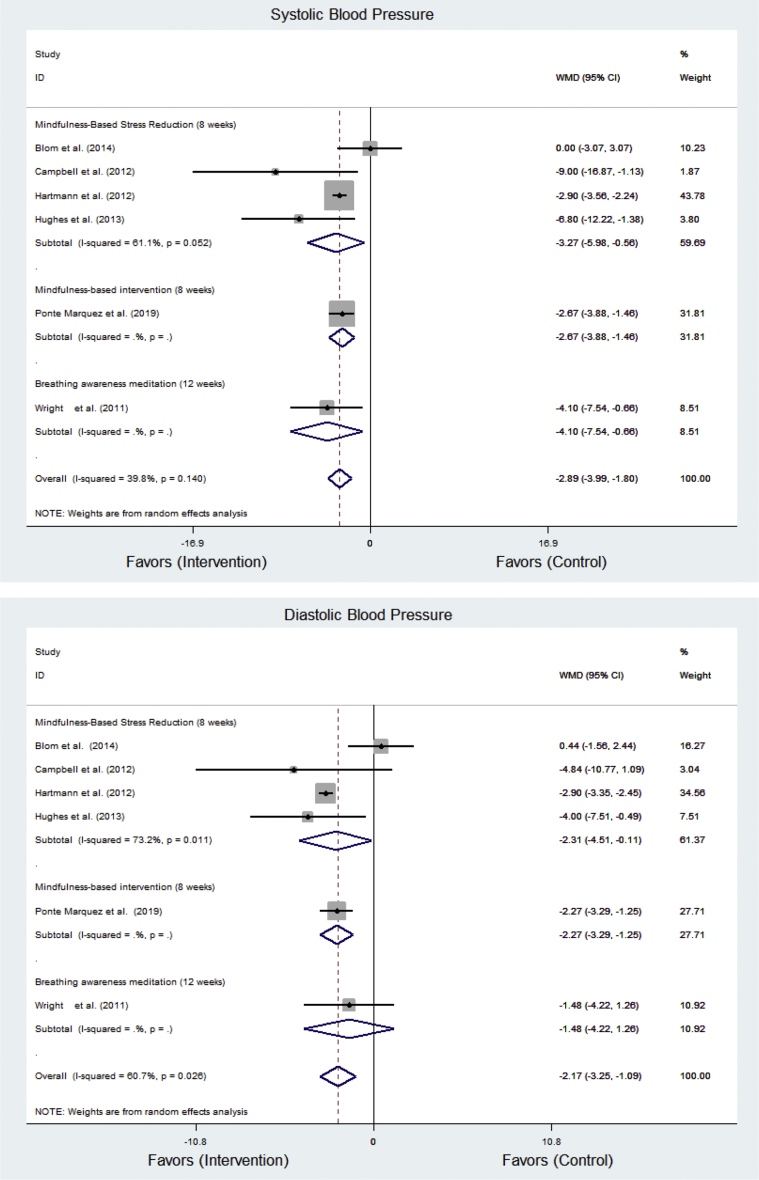
3.3. Publication bias
The Funnel plots were asymmetrically distributed for both systolic and diastolic BP in Figure 3. Egger's regression intercept suggests that publication bias is absent for the systolic BP (intercept = -0.45, t = -0.22, p > .050) and for the diastolic BP (intercept = 0.12, t = 0.46, p > .050). In a sensitivity analysis in which we excluded the eight trials that using office BP measurement from the meta-analyses, the overall effect size remained unchanged in Figure 4.
Figure 3.
Diagnosis of publication bias in the combined effect on blood pressure.
Figure 4.
Forest plot showing a sensitivity analysis a sensitivity analysis by removing studies based on office BP.
4. Discussion
There is increasing scientific evidence to support the mindfulness interventions on BP between 2009 and 2019, which is consistent with an increasing interest in the study of mindfulness interventions in clinical treatment in the last few years, both in research and practice. Moreover, various mindfulness interventions for hypertension have been developed and applied within the past few years. The rationale of applying the mindfulness for treatment on reducing BP level was sympathetic activities reduction, improving the brain function related to attention and memory, respiratory and circulatory system, and psychological health related to control of stress and emotions [32, 33]. In addition, research has consistently shown that the intervention most commonly used in the studies reviewed was MBSR. This intervention was also found to be associated with the greatest reductions in both diastolic and systolic BP. Delivery time for the intervention ranging from eight to twelve sessions although eight sessions delivered weekly was the most frequently found pattern. In terms of quality six of the MBSR studies were judged to be of high quality using the Cochrane criteria and this adds to the confidence with which these results can be accepted. Two studies used BAM but intervention descriptions lacked some detail resulting in both studies being ranked as of medium quality. Despite this, the BAM interventions did produce significant reductions in BP in patients with NCDs. For systolic BP, the second highest reduction was reported, while for diastolic BP it reported the lowest reduction of the three interventions, although it was still statistically significant. Again two studies used MM as the intervention. One study was judged to be of high quality while one was of medium quality. For diastolic BP, the reduction reported was greater than for the BAM intervention but it was lowest for systolic BP although still statistically significant.
These results indicate that mindfulness interventions appear to be effective at reducing BP in patients suffering from a range of NCDs. Theoretically, it is suggested patients with NCDs may benefit from mindfulness practice through various pathways. Firstly, psychological symptoms may be modulated through the self-regulation of attention. Thus stress and anxiety may be better controlled. Secondly, mindfulness has been shown to promote body awareness, relaxation and cognitive coping processes that are associated with parasympathetic activation, that have been shown to reduce BP [34]. From this review it appears that effective interventions can be delivered individually or in groups and can help enhance wellbeing [34]. The resultant more positive attitudes reported by participants had positive effects on their wellbeing [35]. They also show that mindfulness interventions can help patients apply lifestyle modifications more effectively to reduce and maintain reductions in their BP [36].
There is physiological evidence demonstrating that regular mindfulness practice, especially deep meditation, activates the autonomic nervous system to release endorphins and serotonin which leads to norepinephrine and parasympathetic responses [37] and lowers cortisol levels which can help reduce the symptoms of NCDs and make our bodies and minds work more effectively [38].
While this review has identified and examined three different mindfulness interventions delivered in clinical settings, the findings in support of the effectiveness of mindfulness is in line with other views of different types of mediation or specific groups of patients [39]. One review examined the found transcendental and non-transcendental meditation to be effective in the reducing BP [14]. Another review reported that mindfulness-based intervention effectively reduced BP inpatients with vascular disease by reducing levels of albuminuria and stress homones [40].
5. Conclusion
The decision to include only research papers that were published in international research journals, did limit the size of data sources. The gray literature was not searched. This loss of data may bias the findings in that studies with non-significant results are less likely to be published, this increasing selection bias. It is of concern when reviewing literature such as this to observe that many experimental research studies do not present sufficient statistical detail to allow meta-analyses to be undertaken. Despite these limitations, clear support for the effectiveness of mindfulness interventions in reducing BP in patients suffering from NCDs is emerging.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This work was supported by the Newton fund via the British Academy (Grant No. AF170002/2017), UK. and Thailand Research Fund (DBG61/2561).
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: 2018. Noncommunicable Diseases.http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases [Internet] [cited 2019 Feb 22]. Available from: [Google Scholar]
- 2.Beaglehole R., Bonita R., Horton R., Adams C., Alleyne G., Asaria P. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal A., Garg M., Dixit N., Godara R. Evaluation and correlation of stress scores with blood pressure, endogenous cortisol levels, and homocysteine levels in patients with central serous chorioretinopathy and comparison with age-matched controls. Indian J. Ophthalmol. 2016;64(11):803–805. doi: 10.4103/0301-4738.195591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Heart Association . American Heart Association; Texas: 2017. Why High Blood Pressure Is a Silent Killer.https://www.heart.org/en/health-topics/high-blood-pressure/why-high-blood-pressure-is-a-silent-killer [Internet] [cited 2019 Feb 22]. Available from: [Google Scholar]
- 5.Ettehad D., Emdin C.A., Kiran A., Anderson S.G., Callender T., Emberson J. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 6.Ukpabi O.J., Ewelike I.D. The eighth joint national committee on the prevention, detection, evaluation, and treatment of high blood pressure (joint national committee-8) report: matter arising. Nig J Cardiol. 2017;14:15–18. [Google Scholar]
- 7.Ram C.V.S. Antihypertensive drugs: an overview. Am. J. Cardiovasc. Drugs. 2002;2(2):77–89. doi: 10.2165/00129784-200202020-00002. [DOI] [PubMed] [Google Scholar]
- 8.Chiesa A., Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol. Med. 2010;40(8):1239–1252. doi: 10.1017/S0033291709991747. [DOI] [PubMed] [Google Scholar]
- 9.Kabat-Zinn J. Hachette Books; New York: 1994. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life. [Google Scholar]
- 10.Grossman P., Niemann L., Schmidt S., Walach H. Mindfulness-based stress reduction and health benefits A meta-analysis. J. Psychosom. Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 11.Rosenzweig S., Reibel D.K., Greeson J.M., Edman J.S., Jasser S.A., McMearty K.D., Goldstein B.J. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Alternative Ther. Health Med. 2007;13(5):36–38. https://www.ncbi.nlm.nih.gov/pubmed/17900040 [PubMed] [Google Scholar]
- 12.Kabat-Zinn J. University of Massachusetts Medical CW, Stress Reduction Clinic; New York: 1990. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Delacorte Press. [Google Scholar]
- 13.Gregoski M.J., Barnes V.A., Tingen M., Harshfield G.A., Treiber F.A. Breathing awareness meditation and life skills training programs influence upon ambulatory blood pressure and sodium excretion among African American adolescents. J. Adolesc. Health. 2011;48(1):59–64. doi: 10.1016/j.jadohealth.2010.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi L., Zhang D., Wang L., Zhuang J., Cook R., Chen L. Meditation and blood pressure: a meta-analysis of randomized clinical trials. J. Hypertens. 2017;35(4):696–705. doi: 10.1097/HJH.0000000000001217. [DOI] [PubMed] [Google Scholar]
- 15.Higgins J.P.T., Green S. The Cochrane Collaboration; 2011. Cochrane Handbook for Systematic Reviews of Interventions.http://handbook.cochrane.org version 5.1.0[Internet] [cited 2019 Feb 22]. Available from: [Google Scholar]
- 16.Faraone S.V. Interpreting estimates of treatment effects: implications for managed care. P T. 2008;33(12):700–711. [PMC free article] [PubMed] [Google Scholar]
- 17.Blom K., Baker B., How M., Dai M., Irvine J., Abbey S. Hypertension analysis of stress reduction using mindfulness meditation and yoga: results from the harmony randomized controlled trial. Am. J. Hypertens. 2014;27(1):122–129. doi: 10.1093/ajh/hpt134. [DOI] [PubMed] [Google Scholar]
- 18.Campbell T.S., Labelle L.E., Bacon S.L., Faris P., Carlson L.E. Impact of mindfulness-based stress reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: a waitlist-controlled study. J. Behav. Med. 2012;35(3):262–271. doi: 10.1007/s10865-011-9357-1. [DOI] [PubMed] [Google Scholar]
- 19.Gotink R.A., Younge J.O., Wery M.F., Utens E., Michels M., Rizopoulos D. Online mindfulness as a promising method to improve exercise capacity in heart disease: 12-month follow-up of a randomized controlled trial. PloS One. 2017;12(5) doi: 10.1371/journal.pone.0175923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hartmann M., Kopf S., Kircher C., Faude-Lang V., Djuric Z., Augstein F. Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients. Diabetes Care. 2012;35(5):945–947. doi: 10.2337/dc11-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hughes J.W., Fresco D.M., Myerscough R., Dulmen M., Carlson J.R. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosom. Med. 2013;75(8):721–728. doi: 10.1097/PSY.0b013e3182a3e4e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar S., Lathif F., Raghavan V. Effects of mindfulness-based stress reduction on blood pressure (MBSR) among patients with type-2 diabetes- a randomized pilot study. Nursing. Nurs. J. India. 2017;108(2):61–63. [Google Scholar]
- 23.Momeni J., Omidi A., Raygan F., Akbari H. The effects of mindfulness-based stress reduction on cardiac patients' blood pressure, perceived stress, and anger: a single-blind randomized controlled trial. J. Am. Soc. Hypertens. 2016;10(10):763–771. doi: 10.1016/j.jash.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Nejati S., Zahiroddin A., Afrookhteh G., Rahmani S., Hoveida S. Effect of group mindfulness-based stress-reduction program and conscious yoga on lifestyle, coping strategies, and systolic and diastolic blood pressures in patients with hypertension. J. Tehran Heart Cent. 2015;10(3):140–148. [PMC free article] [PubMed] [Google Scholar]
- 25.Ng C.G., Lai K.T., Tan S.B., Sulaiman A.H., Zainal N.Z. The effect of 5 minutes of mindful breathing to the perception of distress and physiological responses in palliative care cancer patients: a randomized controlled study. J. Palliat. Med. 2016;19(9):917–924. doi: 10.1089/jpm.2016.0046. [DOI] [PubMed] [Google Scholar]
- 26.Palta P., Page G., Piferi R.L., Gill J.M., Hayat M.J., Connolly A.B. Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. J. Urban Health. 2012;89(2):308–316. doi: 10.1007/s11524-011-9654-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parswani M.J., Sharma M.P., Iyengar S. Mindfulness-based stress reduction program in coronary heart disease: a randomized control trial. Int. J. Yoga. 2013;6(2):111–117. doi: 10.4103/0973-6131.113405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pearson S., Wills K., Woods M., Warnecke E. Effects of mindfulness on psychological distress and HbA1c in people with diabetes. Mindfulness. 2018;9(5):1615–1626. [Google Scholar]
- 29.Ponte Marquez P.H., Feliu-Soler A., Sole-Villa M.J., Matas-Pericas L., Filella-Agullo D., Ruiz-Herrerias M. Benefits of mindfulness meditation in reducing blood pressure and stress in patients with arterial hypertension. J. Hum. Hypertens. 2019;33(3):237–247. doi: 10.1038/s41371-018-0130-6. [DOI] [PubMed] [Google Scholar]
- 30.Wright L.B., Gregoski M.J., Tingen M.S., Barnes V.A., Treiber F.A. Impact of stress reduction interventions on hostility and ambulatory systolic blood pressure in african American adolescents. J. Black Psychol. 2011;37(2):210–233. doi: 10.1177/0095798410380203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McHugh M.L. Interrater reliability: the kappa statistic. Biochem. Med. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- 32.Keng S.L., Smoski M.J., Robins C.J. Effects of mindfulness on psychological health: a review of empirical studies. Clin. Psychol. Rev. 2011;31(6):1041–1056. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hughes J.W., Fresco D.M., Myerscough R., van Dulmen M., Carlson L.E., Josephson R. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosom. Med. 2013;75(8):721–728. doi: 10.1097/PSY.0b013e3182a3e4e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Solano Lopez A.L. Effectiveness of the mindfulness-based stress reduction program on blood pressure: a systematic review of literature. Worldviews Evid. Based Nurs. 2018;15(5):344–352. doi: 10.1111/wvn.12319. [DOI] [PubMed] [Google Scholar]
- 35.Intarakamhang U., Macaskill A. Multi-group causal model of health literacy and behaviors on family well-being among Thai adults at risk of non- communicable diseases (NCDs) J. Res. Health Sci. 2018;18(4) [PMC free article] [PubMed] [Google Scholar]
- 36.Sutipan P., Intarakamhang U., Kittipichai W., Macaskill A. Effect of a self-management program on healthy lifestyle behaviors and health outcomes in the elderly with hypertension. IJBS. 2018;13(2):1–15. [Google Scholar]
- 37.Casellas Grau A., Font A., Vives J. Positive psychology interventions in breast cancer. A systematic review. Psycho Oncol. 2014;23(1):9–19. doi: 10.1002/pon.3353. [DOI] [PubMed] [Google Scholar]
- 38.Turakitwanakan W., Mekseepralard C., Busarakumtragul P. Effects of mindfulness meditation on serum cortisol of medical students. J. Med. Assoc. Thai. 2013;96(Suppl 1):S90–95. [PubMed] [Google Scholar]
- 39.Hilton L., Hempel S., Ewing B.A., Apaydin E., Xenakis L., Newberry S. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann. Behav. Med. 2017;51(2):199–213. doi: 10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abbott R.A., Whear R., Rodgers L.R., Bethel A., Thompson Coon J., Kuyken W. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta-analysis of randomised controlled trials. J. Psychosom. Res. 2014;76(5):341–351. doi: 10.1016/j.jpsychores.2014.02.012. [DOI] [PubMed] [Google Scholar]