Abstract
Background
The pure soybean oil based lipid emulsions (S‐LE) conventionally used for parenteral nutrition (PN) in preterm infants have high polyunsaturated fatty acid (PUFA) content. The newer lipid emulsions (LE) from alternative lipid sources with reduced PUFA content may improve clinical outcomes in preterm infants.
Objectives
To determine the safety and efficacy of the newer alternative LE compared with the conventional S‐LE for PN in preterm infants.
Search methods
We used the standard search strategy of the Cochrane Neonatal Review Group (CNRG) to search the Cochrane Central Register of Controlled Trials (CENTRAL; Issue 7), MEDLINE (1946 to 31 July 2015), EMBASE (1947 to 31 July 2015), CINAHL (1982 to 31 July 2015), Web of Science (31 July 2015), conference proceedings, trial registries (clinicaltrials.gov, controlled‐trials.com, WHO's ICTRP), and the reference lists of retrieved articles for randomised controlled trials and quasi‐randomised trials.
Selection criteria
Randomised or quasi‐randomised controlled trials in preterm infants (< 37 weeks), comparing newer alternative LE with S‐LE.
Data collection and analysis
Data collection and analysis conformed to the methods of the CNRG. We assessed the quality of evidence for important outcomes using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, in addition to reporting the conventional statistical significance of results.
Main results
Fifteen studies (N = 979 infants) are included in this review. Alternative LE including medium chain triglycerides/long chain triglycerides (MCT/LCT) LE (3 studies; n = 108), MCT‐olive‐fish‐soy oil‐LE (MOFS‐LE; 7 studies; n = 469), MCT‐fish‐soy oil‐LE (MFS‐LE; 1 study; n = 60), olive‐soy oil‐LE (OS‐LE; 7 studies; n = 406), and borage‐soy oil‐LE (BS‐LE; 1 study; n = 34) were compared with S‐LE. The different LE were also considered together to compare ‘all fish oil containing‐LE’ versus S‐LE (7 studies; n = 499) and ‘all alternative LE’ versus S‐LE (15 studies; n = 979). Some studies had multiple intervention arms and were included in more than one comparison. No study compared pure fish oil‐LE or structured‐LE to S‐LE.
The GRADE quality of evidence (GRADE QoE) ranged from ‘low’ to ‘very low.’ Evidence came mostly from small single centre studies, many focusing on biochemical aspects as their primary outcomes, with optimal information size not achieved for the important clinical outcomes in any comparison.
In the primary outcomes of the review there was a pooled effect towards decreased bronchopulmonary dysplasia (BPD) in OS‐LE vs S‐LE (4 studies, n = 261) not reaching statistical significance (typical risk ratio (RR) 0.69, 95% confidence interval (CI) 0.46 to 1.04, I² = 32%; typical risk difference (RD) ‐0.08, 95% CI ‐0.17 to 0.00, I² = 76%; GRADE QoE: ‘very low’). No difference in BPD was observed in any other comparison. There were no statistically significant differences in the primary outcomes of death, growth rate (g/kg/day) or days to regain birth weight in any comparison.
Retinopathy of prematurity (ROP) stage 1‐2 was reported to be statistically significantly lower in one single centre study (n = 80) in the MOFS‐LE group compared with the S‐LE group (1/40 vs 12/40, respectively; RR 0.08, 95% CI 0.01 to 0.61; RD ‐0.27, 95% CI ‐0.43 to ‐0.12; number needed to benefit (NNTB) 4, 95% CI 2 to 8). However there were no statistically significant differences in the secondary outcome of ROP ≥ stage 3 in any of the individual studies or in any comparison (GRADE QoE: ‘low’ to ‘very low’). No other study reported on ROP stages 1 and 2 separately.
There were no statistically significant differences in the secondary outcomes of sepsis, PN associated liver disease (PNALD)/cholestasis, ventilation duration, necrotising enterocolitis (NEC) ≥ stage 2, jaundice requiring treatment, intraventricular haemorrhage grade III‐IV, periventricular leukomalacia (PVL), patent ductus arteriosus (PDA), hypertriglyceridaemia, and hyperglycaemia in any comparison.
No study reported on neurodevelopmental outcomes or essential fatty acid deficiency.
Authors' conclusions
All lipid emulsions in this review appeared to be safe and were well tolerated in preterm infants. Compared with the pure soy oil based LE, use of MOFS‐LE was associated with a decrease in the early stages (1‐2) of ROP in one study. However there were no statistically significant differences in clinically important outcomes including death, growth, BPD, sepsis, ROP ≥ stage 3, and PNALD with the use of newer alternative LE versus the conventional pure soy oil based LE (GRADE QoE ranged from ‘low’ to ‘very low’). Currently there is insufficient evidence to recommend any alternative LE over S‐LE or vice versa in preterm infants.
Larger randomised studies focusing on important clinical outcomes, targeting specific ‘at risk’ population subgroups (e.g. extreme prematurity, long term PN, etc), and exploring the effect of different proportions of lipid constituents are required to evaluate the effectiveness of newer lipid emulsions compared with the conventional pure soy based LE in preterm infants.
Plain language summary
Newer alternative fat emulsions versus the conventional pure soybean oil based fat emulsions for intravenous nutrition in preterm infants.
Review question: Are the newer alternative fat emulsions better than the conventional pure soybean oil based fat emulsions for improving outcomes in preterm infants?
Background: Preterm infants who need nutrition through intravenous lines have been conventionally given pure soy oil based fat emulsions. High polyunsaturated fatty acid (PUFA) content in pure soy oil based emulsions can, however, be harmful to preterm infants. The newer lipid emulsions (LE) from alternative lipid sources with reduced PUFA content may improve clinical outcomes in preterm infants.
Study characteristics: Review authors searched the medical literature and identified fifteen eligible studies (including 979 infants).
Key findings: All LE in this review appeared to be safe and were well tolerated in preterm infants. This review did not find any significant differences in the clinically important outcomes of death, growth, lung disease or severe eye disease (retinopathy of prematurity ≥ stage 3) with the use of newer alternative LE compared with the conventional pure soy oil based LE.
Conclusions: Based on this review, there is insufficient evidence to recommend any of the newer alternative LE over the conventional pure soy oil based LE or vice‐versa. Further studies are required to evaluate the effectiveness of newer LE compared with conventional pure soy based LE in preterm infants.
Summary of findings
Background
Description of the condition
Lipid emulsions (LE) have been a vital component of parenteral nutrition in preterm infants since their introduction in the 1960s. Preterm infants are vulnerable to postnatal growth failure, essential fatty acid (EFA) deficiency and intolerance to enteral feeds, requiring total or partial parenteral nutrition (PN) to provide all or part of their caloric requirements to ensure adequate growth.
Description of the intervention
LE serve as a source of high density energy and EFA, i.e. linoleic acid (LA; ω6) and α‐linolenic acid (ALA; ω3). These are precursors for eicosanoids active in numerous physiological mechanisms such as platelet function, immune response, inflammation, and early visual and neural development (Driscoll 2008; Koletzko 2001; Lapillonne 2013; SanGiovanni 2000;).
Pure soybean oil based lipid emulsions (S‐LE; for example Intralipid®, Ivelip®, Liposyn III®) have been the standard LE in the neonatal intensive care units (NICU) worldwide for the last few decades (de Meijer 2009). However there is evidence to suggest that S‐LE may have harmful effects due to excessive polyunsaturated fatty acid (PUFA) and LA content (Sala‐Vila 2007). Alternative LE aim to decrease the excessive ω6 content by using lipids from sources other than soybean oil.
Medium chain triglyceride (MCT) based LE (derived from coconut oil) decrease the ω6 content by adding MCT to lipid emulsions, for example Lipovenoes MCT® and 20% Lipofundin MCT/LCT® are a 1:1 mix of MCT and long chain triglycerides (LCT; Vanek 2012). Structured lipid emulsions (for example Structolipid®) are a modification of MCT‐LCT based LE and are formed by re‐esterification of medium and long chain fatty acids (Waitzberg 2006). Olive oil based LE, rich in the mono‐unsaturated fatty acid oleic acid (18:1; ω9), have been available since the 1990s. For example, ClinOleic® is an olive oil based LE with a 4:1 ratio of olive oil:soy oil and one‐third PUFA content compared with S‐LE (e.g. 20% Intralipid®). Fish oil based LE (e.g. Omegaven®) rich in ω3 fatty acids and with a low ω6:ω3 ratio have been developed (Wanten 2007).
More recently, LE derived from multiple sources have become available for clinical use. SMOFLipid® is one such LE which is a 30:30:25:15 mix of MCT, soybean oil, olive oil, and fish oil (Sala‐Vila 2007). Lipoplus®, also known as Lipidem® in some countries, is a mix of 50% MCT, 40% soybean oil, and 10% fish oil.
How the intervention might work
Currently available LE formulations differ in the source of lipid, fatty acid profile, anti‐oxidant levels, and presence of additional components (Wanten 2007; Appendix 1).
Soy oil based LE (S‐LE) have excessive amounts of PUFA (up to 60%) and LA (50%; Sala‐Vila 2007), exceeding the daily preterm LA requirement of 0.25 g/kg/day and adding to oxidative stress (Koletzko 2005; Pitkanen 1991). This may aggravate adverse outcomes including chronic lung disease (CLD; Schock 2001), as well as retinopathy of prematurity (ROP; Mylonas 1999).
Conventional S‐LE contribute to parenteral nutrition associated liver disease (PNALD) in preterm infants (de Meijer 2009); phytosterols present in soybean oil may have harmful effects on liver function (de Meijer 2009). High amounts of LA and ALA in S‐LE may lead to substrate inhibition of Δ6desaturase (Gobel 2003), resulting in decreased formation of arachidonic acid (AA) and docosahexaenoic acid (DHA) which are crucial for visual and cognitive development in premature infants (Heird 2005; Lehner 2006). S‐LE also leads to an increase in pro‐inflammatory prostaglandins and leukotrienes (Wanten 2007), may increase the risk of sepsis (Palmblad 1991), and may adversely affect phagocytic and lymphocytic functions (Gogos 1995).
MCT (coconut oil) and LCT (soybean oil) based LE (MS‐LE) may have advantages due to reduced ω6 content and the rapid metabolism of MCTs. Early data suggests good tolerance in preterm infants with increased eicosapentaenoic acid (EPA) levels and an equivalent EFA profile compared with S‐LE (Lehner 2006). However in vitro studies have raised concerns that MCTs may cause leucocyte activation, impair immune function, and decrease killing of Candida albicans (Waitzberg 2006; Wanten 2007). Use of MCT oil LE has also been associated with impaired lung function and aggravation of tissue inflammation in adults with acute respiratory distress syndrome (Lekka 2004), and may be ketogenic, limiting their utility in acidotic patients (Waitzberg 2006).
Structured LE have an even distribution of medium chain fatty acids in the lipid droplets, aimed at reducing the immunological adverse effects of MS‐LE. There is limited evidence to suggest that structured emulsions are well tolerated in critically ill patients, however unlike MS‐LE they may not affect phagocyte function (Wanten 2007).
Borage oil‐soy oil based LE (BS‐LE) substitute the soy content partially with borage oil which is the highest source of γ‐linolenic acid. The enzyme Δ6desaturase is essential in the conversion from LA to γ‐linolenic acid (GLA, 18:3 ω6) and is considered the rate‐limiting step in the metabolism from LA to AA. Borage oil based LE were developed to potentially circumvent this enzymatic step. PFE 4501® (Pharmacia, Sweden) was a combination of borage oil (15%) with soybean oil (85%) with increased amounts of carnitine to prevent carnitine deficiency in preterm infants (Magnusson 1997).
Olive oil‐soy oil based LE (OS‐LE) have generated interest due to the immune‐neutral nature of oleic acid (Reimund 2004), decreased PUFA content, higher α‐tocopherol content (Sala‐Vila 2007), and reduced peroxidability of low density lipoproteins, with an overall reduction in oxidative stress (Goulet 1999; Krohn 2006). OS‐LE (ClinOleic®) has been reported to have a fatty acid composition similar to that of breast milk, and to result in higher α‐tocopherol levels in preterm infants when compared with S‐LE (Intralipid®; Gobel 2003). Studies have reported decreased immunological disturbance, with lesser inhibition of T‐cell activation, lesser effect on interleukin (IL)‐2 production and decreased alteration in neutrophil responses with the use of OS‐LE compared with S‐LE (Buenestado 2006; Gawecka 2008a; Granato 2000). Olecanthol, a minor component in olive oil, has been shown to inhibit the cyclooxygenase pathway but not the 5‐lipoxygenase pathway, displaying "ibuprofen like" anti‐inflammatory activity (Beauchamp 2005). Use of OS‐LE may decrease the incidence of hyperglycaemia when compared with S‐LE (Intralipid®; Van Kempen 2006). Randomised controlled studies in critically ill neonates and preterm infants less than 32 weeks gestation have shown OS‐LE to be equally well tolerated as conventional S‐LE (Gawecka 2008a).
Fish oil based LE (F‐LE) have increased ω3 PUFAs, resulting in inhibition of the cyclooxygenase pathway and preferential use of the lipoxygenase pathway, which in turn decreases pro‐inflammatory prostaglandins (PGE2; Fürst 2000). EPA (C20:5; ω3), present in fish oil, activates the peroxisome proliferator‐activated receptors α and γ, which in turn antagonise the nuclear factor‐κB signalling pathway leading to reduced production of inflammatory mediators (Fürst 2000). Adult studies have indicated that, in sepsis, the use of F‐LE decreases the length of hospital stay, readmission rates, and rate of mechanical ventilation and improves survival (Wanten 2007). Recently an F‐LE (Omegaven®) was shown to decrease and even reverse PNALD in infants resulting in decreased mortality and lower levels of triglycerides (TG), conjugated bilirubin and liver enzymes compared with S‐LE (20% Intralipid®; de Meijer 2009; Puder 2009).
Multisource‐LE ‐ MCT‐fish‐soy based LE (MFS‐LE) and MCT‐olive‐fish‐soy based LE (MOFS‐LE) ‐ derive the advantages of lipids from multiple sources including MCTs (rapidly metabolised lipids), soybean oil (EFA source), olive oil (fewer immune effects), and fish oil (anti‐inflammatory effects). There is evidence of reduced hospital stay, better plasma elimination of TG, better α‐tocopherol levels, and good tolerance profile with a MOFS‐LE (SMOFlipid®) in adults (Grimm 2005; Wanten 2007). ClinOleic® and Omegaven® in 1:1 combination have been shown to decrease cholestasis and the incidence of ROP requiring laser therapy in preterm infants (Pawlik 2011). Decreased incidence of bronchopulmonary dysplasia (BPD) with SMOFlipid® has been reported in a prospective observational cohort study in preterm infants (Skouroliakou 2012).
The abbreviation scheme used for alternative LE is described in Appendix 2.
Why it is important to do this review
The introduction of life saving PN was a landmark in neonatology but it appears that the conventionally used S‐LE are far from ideal. Conventional S‐LE, despite their widespread use, may have harmful effects in preterm infants due to high PUFA content which may contribute to adverse outcomes including mortality, PNALD, ROP, BPD, and sepsis. The LE of choice in preterm infants would be one that is easy to metabolise, does not increase inflammatory or oxidative stress, is not immunosuppressive, has the least adverse effects, and has a proven safety profile in this population. Therefore, we undertook this review to compare the effectiveness of newer alternative LE to the conventionally used pure soybean oil based LE in preterm infants.
Objectives
Primary objectives
To determine the effectiveness and safety of newer alternative LE compared to S‐LE in parenterally fed preterm infants.
We considered the following individual comparisons:
MOFS‐LE (MCT‐olive‐fish‐soy oil) versus S‐LE.
MFS‐LE (MCT‐fish‐soy oil) versus S‐LE.
OS‐LE (olive‐soy oil) versus S‐LE.
MS‐LE (MCT‐soy oil) versus S‐LE.
F‐LE (pure fish oil) versus S‐LE.
BS‐LE (borage‐soy oil) versus S‐LE.
Structured lipids (structured MCT‐soy oil) versus S‐LE.
We considered the following combined intervention group comparisons:
All fish oil containing LE versus S‐LE.
All alternative LE versus S‐LE
Secondary objectives
To determine, using subgroup analyses, the effectiveness and safety of alternative LE compared with S‐LE in relation to gestational age (< 30 weeks; ≥ 30 weeks) and birth weight (≤ 1000 g; > 1000 g).
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled studies.
Types of participants
Preterm infants (< 37 weeks gestation) who received intravenous LE as a part of either total parenteral nutrition (TPN) or partial parenteral nutrition (PPN) within the first week of life and for a minimum of five days.
Types of interventions
Studies comparing newer alternative LE (lipids derived from olive oil, fish oil, and MCT, structured lipids, and multisource‐LE) versus the conventional pure soybean oil based LE in preterm infants were considered for the review.
Intervention group
Newer alternative lipid emulsions with partial or complete substitution of soy by lipids from alternative sources were considered in the intervention group. The following groups were considered.
MOFS‐LE, e.g. SMOFlipid®
MFS‐LE, e.g. Lipidem®
OS‐LE, e.g. ClinOleic®
MS‐LE, e.g. Lipovenoes MCT®
F‐LE, e.g. Omegaven®
BS‐LE, e.g. PFE 4501®
Structured LE, e.g. Structolipid®
Combined intervention groups:
All fish oil containing LE (MOFS‐LE, MFS‐LE, and F‐LE)
All alternative LE with partial or complete substitution of soybean oil from other sources (decreased LA content)
Control group: S‐LE
Lipid emulsions with 100% lipids derived from soybean oil (e.g. Intralipid®, Ivelip®, Liposyn III®, etc)
All infants within each group of the included studies received the same type of LE. We included studies using LE as a part of TPN or PPN within the first week of life and for a minimum of five days. There were no restrictions on minimum or maximum dose of LE. There were no restrictions on co‐interventions of amino acids, minerals, trace elements or vitamins for PN and expressed breast milk or formula feeds via a nasogastric tube for PPN. For this review we have not considered studies that did not have a pure S‐LE group and only compared one non‐pure soy LE to another (e.g. OS‐LE versus MOFS‐LE).
Types of outcome measures
Primary outcomes
Death before discharge or neonatal death (within the first 28 days of life).
Physical growth: a) days to regain birth weight; b) growth rate (g/kg/day) during study period and hospital stay.
BPD or CLD: a) oxygen requirement at 28 days; b) oxygen therapy or any form of respiratory support at 36 weeks postmenstrual age.
Neurodevelopmental outcome (neurodevelopmental outcome assessed by a standardised and validated assessment tool or a child developmental specialist) at any age reported (outcome data grouped at 12, 18, and 24 months if available).
Secondary outcomes
Duration of ventilation (days).
Duration of supplemental oxygen (days).
Need for home oxygen therapy.
Neonatal sepsis: (a) culture positive sepsis; (b) any sepsis including clinical/lab or culture positive sepsis.*
Necrotising enterocolitis (NEC) ≥ stage 2 on Bell's staging system (Bell 1978).
Significant jaundice: (a) requiring treatment with phototherapy or exchange transfusion, or both; b) duration of phototherapy.*
ROP (≥ stage 3) observed by direct or indirect ophthalmoscope, as defined by the International Classification of ROP (ICROP; ICROP 2005).
Intraventricular haemorrhage (IVH; grade III‐IV) on cranial ultrasound, as per Papile classification (Papile 1978).
PVL (any grade, on basis of ultrasound or magnetic resonance imaging; de Vries 1992).
PDA: a) any PDA*; b) significant PDA diagnosed clinically or by echocardiography, requiring treatment either conservatively by fluid restriction, diuretics, indomethacin or ibuprofen, or surgery.
Air leaks (pneumothorax, pneumomediastinum, pulmonary interstitial emphysema) reported individually or as a composite outcome.
Pulmonary haemorrhage needing alterations in respiratory care or causing haemodynamic instability.
Clinically significant thrombocytopenia requiring platelet transfusion.
PNALD (conjugated bilirubin > 2 g/dL or 34.2 µmol/L) with or without raised liver enzymes in the absence of other causes (Christensen 2007, Robinson 2008).
Hypertriglyceridaemia defined by serum TG levels > 200 mg/dL (2.25 mmol/L; Putet 2000).
Hyperglycaemia (blood sugar level > 8.3 mmol/L or > 150 mg/dL; Sinclair 2009) or hypoglycaemia (blood sugar level < 2.6 mmol/L or < 46 mg/dl).
EFA deficiency defined by triene/tetraene ratio > 0.05 (Cober 2010, Gura 2005).
Outcomes marked with asterisk (*) were not the in the original protocol and were added later. The definition of neurodevelopmental outcome was broadened to include neurodevelopmental outcomes reported at ‘any age’ and using different validated tools.
Search methods for identification of studies
Electronic searches
We used the standard search strategy of the Cochrane Neonatal Review Group (CNRG) and conducted test searches to refine the search strategy. The search included electronic searches of MEDLINE (PubMed, 1946 to 31 July 2015), Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 7, 2015), EMBASE (1947 to 31 July 2015), CINAHL (1982 to 31 July 2015), Ovid Nursing Database (1946 to September Week 4, 2014), and Maternity and Infant Care (1971 to August 2014). We also searched the reference lists of all included studies using Web of Science® Thomson Reuters. Abstracts were searched using Biological Abstracts (1985 to 2009), Pediatric Academic Societies (2002 to 2013; http://www.abstracts2view.com/pasall/), Pediatric Academic Societies 2014 abstracts (http://www.abstracts2view.com/pas/titleindex.php), and Web of Science (31 July 2015). We did not apply any language restrictions and limited the searches by filters to human studies and infant (birth to 23 months) where possible. The details of the search strategy for each database is described in Appendix 3.
From the search results, randomised controlled trials and quasi‐randomised controlled trials that fulfilled the inclusion criteria were selected. All the electronically searched studies were imported into EndNote 2014 citation manager to remove duplicates. The search process and flow of information through the different phases of this systematic review have been outlined in the PRISMA flow diagram (Figure 1).
1.
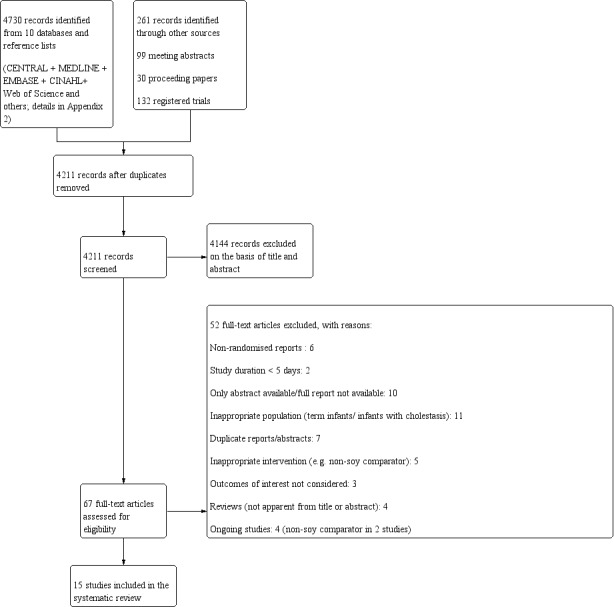
PRISMA flow diagram.
Searching other resources
We searched trial registries at www.clinicaltrials.gov, www.controlled‐trials.com, and the WHO International Clinical Trials Registry Platform (ICTRP; http://apps.who.int/trialsearch/) for ongoing trials. We sought unpublished data and further clarifications from the corresponding authors of included studies.
Data collection and analysis
We used the standard methods of the CNRG for data collection and analysis. Data extraction forms were specifically designed for this review, tested on two studies, further refined and then used to collect and collate data. For each included study, we recorded details regarding the method of randomisation, allocation concealment, blinding, intervention, stratification, and whether the study was single or multi‐centre. We extracted data regarding participants, PN details, and reported outcomes.
Selection of studies
Two review authors (VK, MM) independently searched the databases to identify articles eligible for inclusion in the review. Methodology was assessed with regard to blinding of randomisation, allocation concealment, intervention and outcome measurements, and completeness of follow up.
Data extraction and management
Two review authors (VK, MM) separately extracted the data for each study on data extraction forms. One review author (VK) entered data into Review Manager (RevMan 2011) and the other review author (MM) cross‐checked the printout against his own data extraction forms. At each stage, any difference in opinion was resolved by discussion.
Assessment of risk of bias in included studies
We followed the standard methods of the CNRG to assess the risk of bias. We performed methodological quality assessment of the included studies with consideration of major sources of potential bias and methods of avoidance of bias, as follows:
Selection bias ‐ randomisation and allocation concealment.
Performance bias ‐ blinding of intervention.
Attrition bias ‐ complete follow up.
Detection bias ‐ blinding of outcome assessment.
The following criteria were evaluated to estimate risk of bias in the included studies:
1) Random sequence generation
We assigned a rating of ‘low risk’ when the investigators described a random component in the sequence generation (random number table, computer based, etc), ‘high risk’ when the investigators described a non‐random component (alternation, date of admission, etc), and ‘unclear risk’ when the exact process for randomisation was not described.
2) Allocation concealment
We assigned a rating of ‘low risk’ if appropriate measures were described to conceal the allocation (central allocation, opaque sealed envelopes, etc) and ‘high risk’ when the allocation assignment could be foreseen. We assigned ‘unclear risk’ when the details were not available.
3) Blinding
We evaluated blinding for the participants, personnel, and outcome assessment. We assigned a ‘low risk’ rating if blinding was described and appropriate, 'unclear risk’ if methods or steps taken to achieve blinding were not described but the study was reported as a blinded trial, and ‘high risk’ if the study was not blinded.
4) Incomplete outcome data
We assessed incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, or protocol deviations). We assigned a rating of ‘low risk’ if all of the following were present: missing outcome data were less than 10% and were balanced in both groups and were unlikely to affect the estimation of true effect size and the reason for the missing data was unlikely to be related to the outcome. We assigned a ‘high risk’ rating if missing data were > 10% or unbalanced in comparison groups, or were balanced but reasons for attrition were different between groups (based on percentage difference in reasons for withdrawal), or were likely to be related to the outcome. We assigned a rating of ‘unclear risk’ if there were insufficient data or information provided.
5) Selective reporting bias
We considered selective reporting as ‘low risk’ if the study protocol was available and all the outcomes were reported in a pre‐specified manner. We assigned ‘high risk’ if not all of the pre‐specified outcomes were reported or pre‐specified outcomes were not reported in a manner that was specified a priori. A study was adjudged to have an ‘unclear risk of bias’ if there was insufficient information to permit judgement of 'low risk' or ‘high risk.’ If a study did not report specific data for a particular outcome of interest (mentioned only as ‘not significantly different’ or reported in a manner that could not be used in the meta‐analysis) then we took this into account while grading the quality of evidence (using GRADE working group recommendations; Guyatt 2011) in the ‘Summary of findings’ tables.
6) Other sources of bias
We judged the study to be at ‘low risk of other biases’ if we did not identify any other source of bias, ‘high risk’ if we identified some other potential sources of bias in the study (e.g. study stopped early after interim analysis), and ‘unclear risk’ if the risk was not clear.
Two review authors (VK, MM) independently judged from the publication of each study whether each criterion for method of avoidance of bias was met; any disagreements were resolved by discussion. For each criterion, we entered rating of ‘low risk,’ ‘unclear risk’ or ‘high risk’ in the ‘Risk of bias’ table (part of ‘Characteristics of included studies’ tables).The assessments were also based on the risk of material bias rather than any bias. Besides assessing overall risk of bias in the studies, we focused on the risk of bias for specific outcomes and this is reflected in the results for important outcomes in the ‘Summary of findings’ tables. We ensured that double counting of a risk of bias in multiple bias categories was avoided.
Measures of treatment effect
We followed the recommendations of the CNRG, using a fixed‐effect model for meta‐analysis. The treatment effects for categorical outcomes were estimated using the typical relative risk (RR) and typical risk difference (RD) with 95% confidence intervals (CI). The numbers needed to treat for benefit or harm (NNTB or NNTH, respectively) were estimated if RD was statistically significant. For the continuous outcomes, the mean difference (MD) with 95% CI was used to describe the data.
Unit of analysis issues
We ensured that there were no unit of analysis issues with double counting of controls when studies with multiple intervention arms were used in the meta‐analyses.
Dealing with missing data
We contacted the authors of included studies if clarifications were required or to obtain additional information. The publication authors were provided with open ended requests as well as a partially filled data extraction form (with data extracted from their study). In the case of missing data, the number of participants with missing data have been described in the results section and in the ‘Characteristics of included studies’ table.
Assessment of heterogeneity
We used the I2 statistic for heterogeneity to assess the appropriateness of pooling the data (Higgins 2003); results were interpreted as follows:
< 25%: no heterogeneity.
25% to 49%: low heterogeneity.
50% to 74%: moderate heterogeneity.
75% to 100%: high heterogeneity.
Assessment of reporting biases
Due to the paucity of eligible studies (less than 10 studies) for any outcome in any comparison, funnel plots could not be reliably used to assess publication bias (Sterne 2011). Multiple reports of a single study (multiple publication bias) were identified and evaluated by comparing the reported baseline characteristics and the author details, with clarifications requested from authors if required to avoid double counting.
Data synthesis
Meta‐analyses were performed using Review Manager (RevMan 2011) supplied by The Cochrane Collaboration. For estimates of typical RR and typical RD, we used the Mantel‐Haenszel method. The inverse variance method was used for measured quantities. All primary meta‐analyses were carried out and reported using the fixed‐effect model as per the recommendations of the CNRG.
Details of calculations and imputations
Any standard error of mean was replaced by the corresponding standard deviation (SD). If the data were described in medians and interquartile ranges (IQ), medians were substituted for means and the corresponding SDs were imputed by dividing IQ ranges by 1.35. If the data were described in medians and ranges then we used the formulae proposed by Hozo 2005 to impute the SD. For the outcome of growth rate, the SD had to be imputed for some studies. The means and SDs of weekly observations in a group of study participants were pooled using the formulae for pooling means and variances (McNaught 1997). For combining multiple groups' means and SDs, the formulae used were as described for pooling means and SDs in the Cochrane Handbook (Higgins 2011; Furukawa 2006).
Where meta‐analyses could not be performed, we planned to present qualitative inferences as systematically as possible with an explanation of why meta‐analyses could not be performed. The results for important outcomes are presented in the ‘Summary of findings’ tables.
Quality of evidence and 'Summary of findings' tables
In addition to reporting the conventional statistical significance of outcomes, we also assessed the quality of evidence for selected outcomes using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach. This methodological approach considers randomised controlled trials to be high quality evidence that may be ‘down’ rated due to limitations in any of five areas: design (risk of bias), inconsistency, imprecision, indirectness, and publication bias (Guyatt 2011a; Guyatt 2011b). Inconsistency was evaluated by similarity of point estimates, extent of overlap of CIs, and statistical criteria including the test for heterogeneity (I²). The quality of evidence was downgraded when inconsistency was large and unexplained (i.e. some studies suggest important benefit and others no effect or harm without a clinical explanation; Guyatt 2011). Imprecision was assessed in accordance with the 95% CI around the pooled estimation (Guyatt 2011c). A brief description of the GRADE approach used in this review is provided in Appendix 4. When trials were conducted in populations other than the target population, the GRADE framework suggests downgrading the quality of evidence because of indirectness (Guyatt 2011d), however we only included studies done in preterm infants (< 37 weeks) as per the review protocol.
We selected the following outcomes for inclusion in the ‘Summary of findings’ tables: death before discharge; days to regain birth weight; rate of weight gain (g/kg/day); BPD/CLD; any sepsis (clinical or culture positive); ROP (≥ stage 3) and PNALD/cholestasis.
The following grades of evidence have been used to qualify the effect estimates in the 'Summary of findings' tables (Guyatt 2008):
High quality: further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
The following ‘Summary of findings’ tables were created using the GRADE profiler (GradePro 2008) for each comparison; a summary of the risk estimates and the grading of the evidence are provided in the ‘Summary of findings’ tables:
MOFS‐LE versus S‐LE for parenterally fed preterm infants: death before discharge; days to regain birth weight; rate of weight gain (g/kg/day); BPD/CLD; any sepsis (clinical or culture positive); ROP (≥ stage 3); PNALD/cholestasis (Table 1).
MFS‐LE versus S‐LE for parenterally fed preterm infants: death before discharge; days to regain birth weight; rate of weight gain (g/kg/day); BPD/CLD; any sepsis (clinical or culture positive); PNALD/ cholestasis (Table 2).
OS‐LE versus S‐LE for parenterally fed preterm infants: death before discharge; days to regain birth weight; rate of weight gain (g/kg/day); BPD/CLD; BPD/CLD sensitivity analysis; duration of ventilation; any sepsis (clinical or culture positive (Table 3).
MS‐LE versus S‐LE for parenterally fed preterm infants: death before discharge; days to regain birth weight; rate of weight gain (g/kg/day); BPD/CLD; any sepsis (clinical or culture positive); PNALD/cholestasis; hypertriglyceridaemia (Table 4).
‘All fish oil containing LE’ versus S‐LE for parenterally fed preterm infants: death before discharge; days to regain birth weight; rate of weight gain (g/kg/day); BPD/CLD; any sepsis (clinical or culture positive); ROP (≥ stage 3); PNALD/cholestasis (Table 5).
‘All alternative LE’ versus S‐LE for parenterally fed preterm infants: death before discharge; days to regain birth weight; rate of weight gain (g/kg/day); BPD/CLD; any sepsis (clinical or culture positive); ROP (≥ stage 3); PNALD/cholestasis (Table 6).
Summary of findings 1. MOFS‐LE versus S‐LE for parenterally fed preterm infants.
| MOFS‐LE versus S‐LE for parenterally fed preterm infants(comparison 1) | ||||||
|
Population: Parenterally fed preterm infants
Intervention: MOFS‐LE Comparison: S‐LE | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| S‐LE (control) | MOFS‐LE | |||||
| Death before discharge | Study population | RR 1.26 (0.68 to 2.31) | 369 (5 studies) |
⊕⊕⊝⊝ low | Downgraded 2 levels for imprecision | |
| 86 per 1000 | 108 per 1000 (58 to 199) | |||||
| Days to regain birth weight Follow‐up: birth until discharge | The mean days to regain birth weight in the control groups was 9.6 days1 | The mean days to regain birth weight in the intervention groups was 1.12 days higher (0.17 lower to 2.41 higher) | 234 (3 studies) | ⊕⊕⊝⊝ low2,3,4 | Not downgraded for inconsistency but downgraded 2 levels for imprecision | |
|
Rate of weight gain (g/kg/day) Follow‐up: reported for variable time periods in different studies |
The mean rate of weight gain (g/kg/day) ranged across control groups from 5.42 g/kg/day to 24.5 g/kg/day | The mean rate of weight gain (g/kg/day) in the intervention groups was 0.71 g/kg/day higher (0.17 lower to 1.6 higher) | 347 (5 studies) |
⊕⊝⊝⊝ very low,2,3,4 | Downgraded 2 levels for imprecision and 1 level for possible bias: as very heterogenous outcome with growth rate reported for different time periods by different studies and Imputed values were used | |
|
Bronchopulmonary dysplasia/chronic lung disease Follow‐up: birth until discharge |
Study population | RR 1.02 (0.7 to 1.49) | 314 (4 studies) | ⊕⊕⊝⊝ low2,5 | Downgraded 2 levels for imprecision | |
| 245 per 1000 | 250 per 1000 (172 to 365) | |||||
|
Any sepsis (clinical and/or culture positive) Follow‐up: birth until discharge |
Study population | RR 0.94 (0.62 to 1.42) | 346 (5 studies) |
⊕⊕⊝⊝ low2,4,5 | Downgraded 2 levels for imprecision | |
| 198 per 1000 | 186 per 1000 (123 to 281) | |||||
| Retinopathy of prematurity (≥ stage 3) Follow‐up: birth until discharge | Study population | RR 0.43 (0.06 to 2.85) | 256 (3 studies) | ⊕⊕⊝⊝ low2,5,6,7 | Downgraded 2 levels for imprecision | |
| 23 per 1000 | 10 per 1000 (1 to 66) | |||||
| Parenteral nutrition‐associated liver disease/cholestasis Follow‐up: birth until discharge | Study population | RR 0.78 (0.29 to 2.13) | 314 (4 studies) | ⊕⊕⊝⊝ low2,5,8 | Downgraded 2 levels for imprecision | |
| 50 per 1000 | 39 per 1000 (15 to 107) | |||||
| *The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). MOFS‐LE: medium chain triglycerides‐olive‐fish‐soy lipid emulsion; S‐LE: soy lipid emulsion; CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Mean days to regain birth weight in the control group (calculated value). 2 Optimal information size not achieved. 3 Wide confidence intervals crossing appreciable harm or benefit. 4 Too few studies to make a reliable funnel plot. 5 Confidence intervals cross 0.75 or 1.25. 6 Possibility of outcome reporting bias as some studies did not provide data on ROP. 7 How blinding was achieved is not described in one study. 8 Objective outcome: less likely to be affected by problems in blinding.
Summary of findings 2. MFS‐LE versus S‐LE for parenterally fed preterm infants.
| MFS‐LE versus S‐LE for parenterally fed preterm infants(comparison 2) | ||||||
|
Population: Parenterally fed preterm infants
Intervention: MFS‐LE Comparison: S‐LE | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| S‐LE (control) | MFS‐LE | |||||
| Death before discharge Follow‐up: birth until discharge |
Moderate risk^ (based on median control risk in S‐LE group in all studies) |
RR 5 (0.25 to 99.95) | 60 (1 study) | ⊕⊕⊝⊝ low1,2 | Downgraded 2 levels for imprecision | |
| 73 per 1000# | 365 per 1000 (18 to 1000) | |||||
| Days to regain birth weight Follow‐up: birth until discharge | The mean days to regain birth weight in the control group was 11 days | The mean days to regain birth weight in the intervention groups was 1 day lower (3.6 lower to 1.6 higher) | 57 (1 study) | ⊕⊕⊝⊝ low1,3 | Downgraded 2 levels for imprecision | |
|
Rate of weight gain (g/kg/day) Follow‐up: birth until 3 weeks |
The mean rate of weight gain (g/kg/day) in the control group was 5.6 g/kg/day | The mean rate of weight gain (g/kg/day) in the intervention groups was 1.67 g/kg/day lower (7.01 lower to 3.67 higher) |
57 (1 study) | ⊕⊕⊝⊝ low1,3 | Downgraded 2 levels for imprecision |
|
| Bronchopulmonary dysplasia/chronic lung disease Follow‐up: birth until discharge | Study population | RR 1.39 (0.42 to 4.65) | 57 (1 study) | ⊕⊕⊝⊝ low1,2 | Downgraded 2 levels for imprecision |
|
| 133 per 1000 | 185 per 1000 (56 to 620) | |||||
| Any sepsis (clinical and/or culture positive) Follow‐up: birth until discharge | Study population | RR 1.11 (0.31 to 4.02) | 57 (1 study) | ⊕⊕⊝⊝ low1,2 | Downgraded 2 levels for imprecision |
|
| 133 per 1000 | 148 per 1000 (41 to 536) | |||||
| Parenteral nutrition‐associated liver disease/cholestasis Follow‐up: birth until discharge | Moderate risk (based on median control risk in S‐LE group in all studies)^ | RR 3.32 (0.14 to 78.25) | 57 (1 study) | ⊕⊕⊝⊝ low1,2 | Downgraded 2 levels for imprecision |
|
| 42 per 1000 | 139 per 1000 (6 to 1000) | |||||
| *The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ^The control rate was 0 for this outcome therefore the 'median control group risk' in all infants treated with S‐LE in all included studies (‘all alternative LE’) was used for calculating the corresponding risk . MFS‐LE: medium chain triglycerides‐fish‐soy lipid emulsion; S‐LE: soy lipid emulsion; CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Optimal information size (OIS) not achieved. 2 Confidence intervals cross 0.75 or 1.25. 3 Wide confidence intervals crossing appreciable harm and benefit.
Summary of findings 3. OS‐LE versus S‐LE for parenterally fed preterm infants.
| OS‐LE versus S‐LE for parenterally fed preterm infants(comparison 3) | ||||||
| Population: Parenterally fed preterm infants Intervention: OS‐LE Comparison: S‐LE | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| S‐LE | OS‐LE | |||||
| Death before discharge (incidence) Follow‐up: birth until discharge | Study population | RR 1 (0.21 to 4.82) | 224 (3 studies) | ⊕⊕⊝⊝ low1,2,3,4 | Downgraded 2 levels for imprecision |
|
| 27 per 1000 | 27 per 1000 (6 to 129) | |||||
|
Days to regain birth weight (days) Follow‐up: birth until discharge |
The mean days to regain birth weight in the control groups was 11.69 days | The mean days to regain birth weight in the intervention groups was 0.19 days lower (2 lower to 1.62 higher) | 223 (3 studies) | ⊕⊕⊝⊝ low1,2,4,5 | Downgraded 2 levels for imprecision |
|
|
Rate of weight gain (g/kg/day) Follow‐up: variable |
The mean rate of weight gain (g/kg/day) ranged across control groups from 5.67 to 17.8 g/kg/day | The mean rate of weight gain (g/kg/day) in the intervention groups was 0.42 g/kg/day lower (5.15 lower to 4.3 higher) | 123 (2 studies) | ⊕⊕⊝⊝ low1,2,4,5 | Duration for which the data were presented was variable in different studies; imputed values were used Downgraded 2 levels for imprecision. |
|
|
Bronchopulmonary dysplasia/chronic lung disease (incidence ‐ variable definition) Follow‐up: birth until discharge |
Study population | RR 0.69 (0.46 to 1.04) | 261 (4 studies) | ⊕⊝⊝⊝ very low1,2,3,4,6 | Downgraded 2 levels for imprecision and 1 level for heterogeneity in risk difference Unexplained large difference in duration of ventilation in one study. |
|
| 265 per 1000 | 183 per 1000 (195 to 444) | |||||
|
Bronchopulmonary dysplasia/chronic lung disease (sensitivity analysis) Follow‐up: birth until discharge |
Study population | RR 1.01 (0.57 to 1.79) | 197 (3 studies) | ⊕⊕⊝⊝ low1,2,3,4 | Downgraded 2 levels for imprecision No heterogeneity in sensitivity analysis |
|
| 150 per 1000 | 152 per 1000 (171 to 543) | |||||
|
Duration of ventilation (days) Follow‐up: birth until discharge |
The mean duration of ventilation (days) in the control groups was 16.4 days |
The mean duration of ventilation (days) in the intervention groups was 0.2 days lower (1.67 lower to 1.26 higher) | 202 (3 studies) | ⊕⊝⊝⊝ very low6 | Downgraded 2 levels for imprecision and 1 level for heterogeneity Imputed values used for 1 study |
|
|
Any sepsis (clinical and/or culture positive) Follow‐up: birth until discharge |
Study population | RR 0.87 (0.56 to 1.36) | 301 (5 studies) | ⊕⊝⊝⊝ very low2,3,4,7 | Downgraded 2 levels for imprecision and 1 level for risk of bias | |
| 217 per 1000 | 189 per 1000 (122 to 295) | |||||
| *The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). OS‐LE: olive‐soy lipid emulsion; S‐LE: soy lipid emulsion; CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Objective outcome unlikely to be affected by blinding. 2 Optimal information size not achieved. 3 Confidence intervals cross 0.75 and 1.25. 4 Too few studies to make a funnel plot. 5 Wide confidence intervals crossing appreciable harm and benefit. 6 Heterogeneity > 40% and opposite direction of point estimates. 7 One study was not blinded; method of blinding was not described in two studies.
Summary of findings 4. MS‐LE versus S‐LE for parenterally fed preterm infants.
| MS‐LE versus S‐LE for parenterally fed preterm infants(comparison 4) | ||||||
|
Population: Parenterally fed preterm infants
Intervention: MS‐LE Comparison: S‐LE | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| S‐LE (control) | MS‐LE | |||||
| Death before discharge Follow‐up: birth until discharge | See comment | See comment | Not estimable | 60 (1 study) | Only one study included There were no deaths in either group, therefore RR and illustrative comparative risks were not estimable. |
|
| Days to regain birth weight Follow‐up: birth until discharge | The mean days to regain birth weight in the control group was 11 days |
The mean days to regain birth weight in the intervention groups was 1 day higher (1.53 lower to 3.53 higher) | 60 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | Downgraded 2 levels for imprecision and 1 level for outcome reporting issues as the other studies did not contribute data to this outcome | |
|
Rate of weight gain (g/kg/day) Follow‐up: birth until 3 weeks |
The mean rate of weight gain (g/kg/day) in the control group was 5.6 g/kg/day | The mean rate of weight gain (g/kg/day) in the intervention groups was 2.67 g/kg/day lower (8.2 lower to 2.86 higher) | 60 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | Downgraded 2 levels for imprecision and 1 level for outcome reporting issues as the other studies did not contribute data to this outcome. | |
| Bronchopulmonary dysplasia/chronic lung disease Follow‐up: birth until discharge | 133 per 1000 | 133 per 1000 (37 to 484) | RR 1 (0.28 to 3.63) | 60 (1 study) | ⊕⊝⊝⊝ very low1,2,4 | Downgraded 2 levels for imprecision and 1 level for outcome reporting issues |
|
Any sepsis (clinical and/or culture positive) Follow‐up: birth until discharge |
133 per 1000 | 267 per 1000 (89 to 792) | RR 2 (0.67 to 5.94) | 60 (1 study) | ⊕⊝⊝⊝ very low1,2,4 | Downgraded 2 levels for imprecision and 1 level for outcome reporting issues |
| Parenteral nutrition‐associated liver disease/cholestasis Follow‐up: birth until discharge | Moderate risk (based on median control risk in S‐LE group in all studies)^ | RR 3 (0.13 to 70.83) | 60 (1 study) | ⊕⊝⊝⊝ very low1,2,4 | Downgraded 2 levels for imprecision and 1 level for outcome reporting issues There was only 1 episode of cholestasis which occurred in the OS‐LE group | |
| 42 per 1000 | 126 per 1000 (5 to 1000) | |||||
| Hypertriglyceridaemia Follow‐up: birth to 8 days | See comment | See comment | Not estimable | 12 (1 study) | Only one study included There were no deaths in either group, therefore RR and illustrative comparative risks were not estimable |
|
| *The corresponding risk (and its 95% CI is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ^The control event rate was 0 for this outcome therefore the 'median control group risk' in all infants treated with S‐LE in all included studies (‘all alternative LE’) was used for calculating the corresponding risk. MS‐LE: medium chain triglycerides‐soy lipid emulsion; S‐LE: soy lipid emulsion; CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Outcome reporting issues: the other studies in this comparison did not provide data for this outcome. 2 Optimal information size not achieved. 3 Wide confidence intervals crossing appreciable harm and benefit. 4 Confidence intervals cross 0.75 or 1.25.
Summary of findings 5. All fish oil containing LE versus S‐LE for parenterally fed preterm infants.
| All fish oil containing LE versus S‐LE for parenterally fed preterm infants(comparison 8) | ||||||
|
Population: Parenterally fed preterm infants
Intervention: All fish oil containing LE Comparison: S‐LE | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| S‐LE (control) | All fish oil containing LE | |||||
| Death before discharge Follow‐up: birth until discharge | Study population | RR 1.28 (0.69 to 2.35) | 399 (5 studies) | ⊕⊕⊝⊝ low1,2,3 | Downgraded 2 levels for imprecision | |
| 86 per 1000 | 110 per 1000 (59 to 202) | |||||
|
Days to regain birth weight Follow‐up: birth until discharge |
The mean days to regain birth weight in the control groups was 9.6 days |
The mean days to regain birth weight in the intervention groups was 0.81 days higher (0.43 lower to 2.05 higher) | 261 (3 studies) | ⊕⊕⊝⊝ low2,4,5 | Downgraded 2 levels for imprecision | |
|
Rate of weight gain (g/kg/day) Follow‐up: reported for variable time periods in different studies |
The mean rate of weight gain (g/kg/day) ranged across control groups from 5.42 g/kg/day to 24.5 g/kg/day | The mean rate of weight gain (g/kg/day) in the intervention groups was 0.69 g/kg/day higher (0.19 lower to 1.57 higher) |
374 (5 studies) |
⊕⊝⊝⊝ very low,2,4,5,6 | Downgraded 2 levels for imprecision and 1 level for possible bias: very heterogenous outcome with growth rate reported for different time periods by different studies and Imputed values used |
|
|
Bronchopulmonary dysplasia/chronic lung disease Follow‐up: birth until discharge |
Study population | RR 1.02 (0.7 to 1.5) | 341 (4 studies) | ⊕⊕⊝⊝ low2,3,5 | Downgraded 2 levels for imprecision | |
| 245 per 1000 | 250 per 1000 (172 to 368) | |||||
|
Any sepsis (clinical and/or culture positive) Follow‐up: birth until discharge |
Study population | RR 0.92 (0.61 to 1.39) | 373 (5 studies) | ⊕⊕⊝⊝ low2,3,5 | Downgraded 2 levels for imprecision | |
| 198 per 1000 | 182 per 1000 (121 to 275) | |||||
| Retinopathy of prematurity (≥ stage 3) Follow‐up: birth until discharge | Study population | RR 0.43 (0.06 to 2.85) | 256 (3 studies) | ⊕⊕⊝⊝ low2,3 | Downgraded 2 levels for imprecision | |
| 23 per 1000 | 10 per 1000 (1 to 66) | |||||
| Parenteral nutrition‐associated liver disease/cholestasis Follow‐up: birth until discharge | Study population | RR 0.8 (0.29 to 2.16) | 341 (4 studies) | ⊕⊕⊝⊝ low2,3,5 | Downgraded 2 levels for imprecision | |
| 50 per 1000 | 40 per 1000 (15 to 109) | |||||
| The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). S‐LE: soy lipid emulsion; CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Two studies did not report on death before discharge, however we did not downgrade for bias as most studies reported on this outcome. 2 Optimal information size not achieved. 3 Confidence intervals cross 0.75 or 1.25. 4 Wide confidence intervals crossing appreciable harm and benefit. 5 Not enough studies to make a reliable funnel plot.
6 Bias due to different studies reporting growth rate for different time periods.
Summary of findings 6. All alternative LE versus S‐LE for parenterally fed preterm infants.
| All alternative LE versus S‐LE for parenterally fed preterm infants(comparison 9) | ||||||
| Population: Parenterally fed preterm infants Intervention: All alternative LE Comparison: S‐LE | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk* | |||||
| S‐LE (control) | All alternative LE | |||||
| Death before discharge Follow‐up: birth until discharge | Study population | RR 1.17 (0.66 to 2.07) | 623 (7 studies) | ⊕⊕⊝⊝ low1,2,3 | Downgraded 2 levels for imprecision |
|
| 71 per 1000 | 83 per 1000 (47 to 147) | |||||
| Days to regain birth weight Follow‐up: birth until discharge | The mean days to regain birth weight in the control groups was 10.56 days | The mean days to regain birth weight in the intervention groups was 0.53 days higher (0.52 lower to 1.58 higher) | 484 (5 studies) | ⊕⊝⊝⊝ verylow1,2,4,5 | Downgraded 2 levels for imprecision and 1 level for inconsistency |
|
|
Rate of weight gain (g/kg/day) Follow‐up: reported for variable time periods in different studies |
The mean rate of weight gain (g/kg/day) ranged across control groups from 5.42 g/kg/day to 24.5 g/kg/day | The mean rate of weight gain (g/kg/day) in the intervention groups was 0.68 g/kg/day higher (0.19 lower to 1.55 higher) | 497 (6 studies) |
⊕⊝⊝⊝ very low2,4,7 | Downgraded 2 levels for imprecision and 1 level for possible bias: very heterogenous outcome with growth rate reported for different time periods by different studies and imputed values used Not all studies reported on this outcome |
|
|
Bronchopulmonary dysplasia/chronic lung disease Follow‐up: birth until discharge |
Study population | RR 0.84 (0.63 to 1.12) | 602 (7 studies) | ⊕⊝⊝⊝ very low1,2,3,5 | Downgraded 2 levels for imprecision and 1 level for inconsistency |
|
| 268 per 1000 | 225 per 1000 (169 to 300) | |||||
|
Any sepsis (clinical and/or culture positive) Follow‐up: birth until discharge |
Study population | RR 0.9 (0.66 to 1.23) | 674 (9 studies) | ⊕⊝⊝⊝ very low2,3,6 | Downgraded 1 level for bias and 2 levels for imprecision | |
| 214 per 1000 | 193 per 1000 (141 to 263) | |||||
| Retinopathy of prematurity (≥ stage 3) Follow‐up: birth until discharge | Study population | RR 0.43 (0.06 to 2.85) | 256 (3 studies) | ⊕⊝⊝⊝ very low2,3,7 | Downgraded 1 level for risk of selective reporting bias as some studies did not report on ROP and 2 level for imprecision |
|
| 23 per 1000 | 10 per 1000 (1 to 66) | |||||
| Parenteral nutrition‐associated liver disease/cholestasis Follow‐up: birth until discharge | Study population | RR 0.83 (0.37 to 1.86) | 602 (7 studies) | ⊕⊕⊝⊝ low1,2,3 | Downgraded 2 levels for imprecision |
|
| 46 per 1000 | 38 per 1000 (17 to 86) | |||||
| *The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). S‐LE: soy lipid emulsion; CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Not graded down for potential problems with blinding as it is an objective outcome. 2 Optimal information size not achieved. 3 Confidence intervals cross 0.75 or 1.25. 4 Wide confidence intervals crossing appreciable harm and benefit. 5 Heterogeneity > 40% with opposite direction of point estimates. 6 Possibility of issues with blinding (clinical sepsis included). 7 Possibility of selective reporting bias.
Subgroup analysis and investigation of heterogeneity
We explored high statistical heterogeneity in the outcomes by visually inspecting the forest plots and by removing the outlying studies in the sensitivity analysis (Deeks 2011).The results of meta‐analyses where statistical heterogeneity was significant were interpreted accordingly and the quality of evidence was downgraded in the ‘Summary of findings’ tables as per the GRADE recommendations (Appendix 4). Subgroup analyses based on the gestational age or gender would have been undertaken if the stratified data were available.
Sensitivity analysis
Results of the sensitivity analyses are presented only if these were significantly different from the primary results. We decided to perform sensitivity analyses in the following situations:
Retrospective analysis of unexplained moderate to high heterogeneity by removing the outlying study/studies causing heterogeneity (if feasible).
If a study with high risk of (material) bias was included in the meta‐analysis of an outcome with the other studies having low risk of bias.
Results
Description of studies
We included 15 eligible studies (N = 979) in this review (Characteristics of included studies; Characteristics of excluded studies).
Results of the search
The flow of information and the search results are summarised in the PRISMA flow diagram (Figure 1).
Included studies
Out of the fifteen studies included in this review; seven studies (n = 469) compared MOFS‐LE to S‐LE, seven studies (n = 406) compared OS‐LE to S‐LE, and three studies (n = 108) compared MS‐LE to S‐LE. There was one study each comparing MFS‐LE (n = 60) to S‐LE and BS‐LE (n = 34) to S‐LE. One study had three intervention arms (Rubin 1994), while another study had five intervention arms with different LE in each arm (Savini 2013). One study used two different LE in two different doses resulting in four intervention arms (D'ascenzo 2014). Data from studies using more than two types of LE were used in multiple comparison groups in the meta‐analyses. We did not find any eligible studies comparing pure F‐LE or structured LE with S‐LE. Information on the baseline characteristics and the outcomes reported in the included studies are presented in Table 7 and Table 8, respectively.
1. Baseline characteristics of included studies.
| Study | Intervention: alternative lipid emulsion | Control: conventional pure soy lipid emulsion | ||||||||
| Lipid emulsion# | n | Males |
Gestation in weeks* |
Birth weight in grams* |
Lipid emulsion | n | Males |
Gestation in weeks* |
Birth weight in grams* |
|
| Beken 2014 | 20% SMOFlipid | 40 | 24 | 30 (28‐31)** | 1092 (224) | 20% Intralipid | 40 | 22 | 30 (27‐31)** | 1160 (251) |
| D'ascenzo 2014 | 20% SMOFlipid | 39 | 24 | 27.5 (3.4) | 898.5 (309.4) | 20% Intralipid | 41 | 23 | 28.1 (3.1) | 941 (299) |
| Demirel 2011 | ClinOleic | 20 | 9 | 30.3 (2.5) | 1300.2 (480) | 20% Intralipid | 20 | 12 | 29.2 (3.5) | 1252.5 (458) |
| Deshpande 2009 | ClinOleic | 24 | 14 | 26.1 (1.3) | 848.2 (184.2) | 20% Intralipid | 21 | 10 | 25.9 (1.2) | 801.2 (210.9) |
| Gawecka 2008 | ClinOleic | 18 | 9 | 27 (1) | 936 (218) | 20% Intralipid | 20 | 9 | 27 (2) | 924 (221) |
| Gobel 2003 | ClinOleic | 24 | 18 | 31.4 (2.4) | 1577 (378) | 20% Intralipid | 21 | 11 | 32 (1.8) | 1694 (475) |
| Koksal 2011 | ClinOleic | 32 | 14 | 30.2 (1.3) | 1520 (420) | 20% Intralipid | 32 | 16 | 30.4 (1.6) | 1460 (280) |
| Lehner 2006 | 20% Lipofundin (MCT) | 6 | 6 | 31.4 (1.6) | 1573.3(169.8) | 20% Lipofundin N | 6 | 3 | 33.2 (1.0) | 1781.7 (290.3) |
| Rayyan 2012 | 20% SMOFlipid | 26 | 8 | 29.9 (1.9) | 1335.6 (408.8) | 20% Intralipid | 27 | 16 | 30.4 (1.8) | 1364.1 (339.7) |
| Rubin 1994 | 20% Lipofundin (MCT) | 15 | 11 | 31.6 (2.3) | 1570 (400) | 20% Intralipid | 18 | 11 | 31.4 (2.1) | 1420 (400) |
| Rubin 1994 | PFE 4501 | 16 | 9 | 30.5 (2.7) | 1390 (500) | |||||
| Savini 2013 | Lipofundin (MCT) | 30 | 14 | 27.7 (1.8) | 937 (222) | 20% Intralipid | 30 | 13 | 28.3 (2.1) | 955 (202) |
| Savini 2013 | Lipidem (MFS) | 27 | 14 | 28.3 ( 2.3) | 935 (202) | |||||
| Savini 2013 | ClinOleic | 29 | 13 | 27.7 (2.4) | 905 (160) | |||||
| Savini 2013 | SMOFlipid | 28 | 12 | 27.6 (2) | 898 (199) | |||||
| Skouroliakou 2010 | 20% SMOFlipid | 14 | NA | 28.21 (2.9) | 1140 (260) | 20% Intralipid | 18 | NA | 30.3 (1.5) | 1210 (170) |
| Tomsits 2010 | 20% SMOFlipid | 30 | NA | 31.7 (1.90) | 1661.7 (418) | 20% Intralipid | 30 | NA | 31.9 (1.8) | 1676.7 (411.5) |
| Vlaardingerbroek 2014 | 20% SMOFlipid | 48 | 23 | 27.1 (2.3) | 855 (226) | 20% Intralipid | 48 | 18 | 27.2 (1.9) | 888 (204) |
| Wang 2015 | ClinOleic | 50 | 26 | 32.20 (1.7) | 1486.6 (253.8) | 20% Intralipid | 50 | 31 | 30.8 (4.9) | 1469.8 (250.5) |
# Please refer to Appendix 1 for details of the constituents of lipid emulsions NA: not available * gestation and birth weight are presented as mean (SD) ** median (range) Rubin 1994 had 3 intervention arms and Savini 2013 had 5 intervention arms; total enrolled infants (n = 979) were more than the total number of infants for which the baseline characteristics and results were available (due to withdrawals) n: number of infants for whom the baseline characteristics were known
2. Outcome measures reported in studies comparing alternative LE versus pure soy oil based LE.
| Study | LE | N |
Death before D/C |
Growth rate (g/kg/d) |
Days to regain bw |
BPD |
Vent durn (d) |
O2 (d) |
Any sepsis |
NEC | IVH | HB |
PTx (d) |
HG | HTG | PNALD | PDA | ROP |
| Beken 2014 | MOFS | 80 | Y | ‐ | ‐ | Y | Y | Y | Y | Y | Y | ‐ | ‐ | Y | ‐ | Y | ‐ | Y |
| D'ascenzo 2014 | MOFS | 80 | Y | Y | Y | Y | ‐ | ‐ | Y | Y | Y | ‐ | ‐ | ‐ | NU | Y | Y | Y |
| Demirel 2011 | OS | 40 | ‐ | NU | ‐ | NU | ‐ | ‐ | Y | NU | Y | ‐ | ‐ | ‐ | Y | ‐ | ‐ | NU |
| Deshpande 2009 | OS | 50 | ‐ | NU | ‐ | ‐ | ‐ | ‐ | NU | ‐ | NU | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Gawecka 2008 | OS | 44 | ‐ | ‐ | ‐ | Y | Y | Y | Y | Y | NU | ‐ | Y | ‐ | ‐ | Y | ‐ | NU |
| Gobel 2003 | OS | 45 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | Y | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Koksal 2011 | OS | 64 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | ‐ | Y | Y | Y | ‐ | NU |
| Lehner 2006 | MS | 15 | ‐ | NU | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | Y | ‐ | ‐ | ‐ |
| Rayyan 2012 | MOFS | 53 | Y | Y | ‐ | NU | ‐ | NU* | ‐ | ‐ | NU | ‐ | NU | NU | NU | ‐ | ‐ | |
| Rubin 1994 | MS | 59 | ‐ | NU | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | NU | ‐ | ‐ | ‐ | ‐ |
| Savini 2013 | OS/MS/ MFS/MOFS |
150 | Y | Y | Y | Y | ‐ | ‐ | Y | Y | ‐ | ‐ | ‐ | ‐ | ‐ | Y | Y | ‐ |
| Skouroliakou 2010 | MOFS | 38 | ‐ | NU | ‐ | ‐ | Y | ‐ | Y | ‐ | ‐ | ‐ | Y | Y | ‐ | ‐ | ‐ | ‐ |
| Tomsits 2010 | MOFS | 60 | ‐ | Y | ‐ | ‐ | Y* | Y* | NU* | ‐ | ‐ | ‐ | ‐ | NU | NU | ‐ | ‐ | ‐ |
| Vlaardingerbroek 2014 | MOFS | 98 | Y | Y | Y | Y | Y | ‐ | Y | Y | Y | ‐ | ‐ | ‐ | Y | Y | Y | Y |
| Wang 2015 | OS | 103 | Y | NU | Y | Y | Y | ‐ | Y | NU | ‐ | ‐ | ‐ | ‐ | ‐ | Y | ‐ | ‐ |
LE: lipid emulsion N: total enrolled infants in the study FU: follow‐up D/C: discharge bw: birth weight BPD: bronchopulmonary dysplasia Vent durn: ventilation duration d: days 02: duration of supplemental oxygen NEC: necrotising enterocolitis > stage 2 IVH: intraventricular haemorrhage stage III/IV HB: hyperbilirubinaemia PTx: phototherapy HG: hyperglycaemia HTG: hypertriglyceridaemia PNALD: parenteral nutrition associated liver disease PDA: any patent ductus arteriosus ROP: retinopathy of prematurity MOFS: medium chain triglycerides‐olive‐fish‐soy OS: olive‐soy MS: medium chain triglycerides‐soy MFS: medium chain triglycerides‐fish‐soy Y: data reported and used in the meta‐analysis ‐: outcome not reported NU: data provided in a format not usable in meta‐analysis or reported as “no difference between groups” * composite outcomes reported Not all outcomes could be presented due to space constraints.
MOFS‐LE versus S‐LE
This comparison was reported by Beken 2014, D'ascenzo 2014, Rayyan 2012, Savini 2013, Skouroliakou 2010, Tomsits 2010, and Vlaardingerbroek 2014.
Beken 2014 was a single centre randomised controlled study done in the NICU at Dr Sami Ulus Maternity and Children Research Centre in Ankara, Turkey.
Population: Preterm infants < 1500 g and < 32 weeks gestation were considered to be eligible. Exclusion criteria were major congential abnormalities, congential infections, and inborn errors of metabolism.
Objective: To compare the effect of 20% SMOFlipid® (MOFS‐LE; 30% MCT, 25% olive oil, 15% fish oil, 30% soybean oil) versus 20% Intralipid® (S‐LE) on the development of ROP in very low birth weight infants.
Interventions: Infants were randomised to receive either MOFS‐LE (n = 40) or S‐LE (n = 40) starting at 0.5 g/kg/day in infants weighing < 1000 g and 1 g/kg/day for infants weighing > 1000 g, infused over 24 hours. Lipids were increased by 0.5‐1 g/kg/day to a maximum of 3 g/kg/day. Infants received dextrose and amino acids 1 g/kg/day starting on day one of life. Both groups received enteral feeds of breast milk and/or DHA enriched formula (Prematil‐LCP®, Milupa, GmbH, Friedrichsdorf, Germany). Thirty‐two infants in the MOFS‐LE group and thirty infants in the S‐LE group received their own mothers' breast milk. The intravenous lipid infusion as a component of TPN was progressively replaced with enteral intake so as to maintain 3 g/kg/day of lipid intake. Oxygen saturation was targeted at 90‐95%.
Outcomes: Primary outcomes were the development of ROP and the need for laser photocoagulation. Secondary outcomes included cholestasis, nosocomial infections, NEC, IVH, and CLD. The initial ROP examinations were performed at corrected age of 31 weeks in infants born at ≤ 27 weeks gestation and fourth to fifth week in infants born at ≥28 weeks gestation. The authors reported that "all fundus examinations were performed by the same paediatric ophthalmologist who was blinded to the group assignment." The follow‐up examinations were performed once a fortnight in patients with low‐risk pre‐threshold disease and at least once a week for those with high‐risk pre‐threshold disease.
D'ascenzo 2014 was a single centre, four arm randomised controlled study on premature newborns in the NICU at the Salesi Children's Hospital, Italy between January 2008 and December 2012.
Population: Premature infants (birth weight 500 to 1249 g) were randomised in 1:1:1:1 ratio to receive either SMOFlipid® or Intralipid® at rate of either 3.5 g/kg/day or 2.5 g/kg/day in 4 groups. Exclusion criteria were severe malformations, inborn errors of metabolism, and severe congenital sepsis.
Objective: The objective of this study was to compare the plasma fatty acids and lipid tolerance in preterm infants receiving different doses of MOFS‐LE versus pure S‐LE.
Interventions: Infants (n = 80) were randomised to receive PN with SMOFlipid® (30% MCT, 30% soybean oil, 25% olive oil, 15% fish oil) or Intralipid® (100% soybean oil) at two levels of fat intake: 2.5 or 3.5 g/kg/day in 1:1:1:1 ratio. All infants were started on PN within the first hour of life. Lipids were infused at 1.0, 1.5, 2.0, and 2.5 g/kg/day from birth to postnatal day four and then kept at 2.5 g/kg/day until day seven in the 2.5 g/kg fat groups. The lipids were increased to a maximum of 3.5 g/kg/day in the 3.5 g/kg fat groups. The enteral feeds were allowed at a rate of 8 ml/kg/day from day one to day four, and 16 ml/kg/day from day five to day eight. The lipids were decreased by 1 g/kg/day if the TG were between 250 and 350 mg/dl (2.82 to 3.38 mmol/L) and decreased by 2 g/kg/day if the TG were between 350 and 450 mg/dl (3.95 to 4.5 mmol/L). If TG levels were > 450 mg/dl (4.5 mmol/L) then the lipids were stopped for 24 hours and restarted at half dose. All patients had routine biochemistry, TG levels, blood urea, and creatinine on day three, five, and seven, or more frequently as necessary.
Outcomes: The primary outcome was plasma phospholipid and DHA measured on postnatal day seven, and other plasma lipid components measured at day seven and day 14. Clinical outcomes including death, growth, BPD, ROP (stage 3 and 4), IVH, sepsis, NEC, and cholestasis were also reported.
Rayyan 2012 was a single centre study done at the Department of Neonatology, University Hospitals, Leuven, Belgium between November 2004 and February 2006.
Population: Preterm infants < 34 weeks gestation with weight between 500 and 2000 g and expected to receive PN for seven or more days were included in the study. Exclusion criteria were severe congenital malformations, congenital heart failure, organ damage including anuria, liver disease, haemolytic disease, thrombocytopenia, SaO2 < 80% for over two hours, severe acidosis, use of catecholamines, hypoxic ischaemic encephalopathy, and multi‐organ failure.
Objective: To compare the safety and tolerability of 20% SMOFlipid® (MOFS‐LE; 30% MCT, 30% soybean oil, 25% olive oil, 15% fish oil) versus 20% Intralipid® (S‐LE) with regard to TG levels, haematological and clinical parameters, adverse events, growth, and fatty acid profile.
Interventions: 20% SMOF lipid® (n = 26) versus 20% Intralipid® (n = 27). Lipid emulsions were given for at least seven days either peripherally or centrally. Enteral intake was allowed at less than 30% of the total lipid intake on days one to three, less than 50% on days four to seven, and < 70% on days eight to 14. The daily target dosage of fat started at 1.0 g/kg/day on days one to three and was increased to 2 g/kg/day on day four, 3 g/kg/day on day five, and 3.5 g/kg/day from day six onwards. Other components of PN were given as standardized solutions at the discretion of the clinician.
Outcomes: The primary safety parameter was change in TG levels from baseline by day eight. The primary efficacy outcome was change in weight at day eight from baseline and change in body length from birth to the last observation. Secondary outcomes were blood counts and biochemical parameters. Clinical assessments (heart rate, temperature, blood pressure, weight, oxygen therapy) were performed daily from the pre study visit until study termination, either on day 15 or following the last infusion of study treatment (post‐treatment). The authors reported on death, growth rate, duration of ventilation, hypertriglyceridaemia, composite outcomes of infections and infestations (including conjunctivitis, chorioamnionitis, sepsis), hepatobiliary adverse effects (including conjugated and unconjugated bilirubinaemia), and metabolic and nutrition disorders (including acid‐base abnormalities and hyperglycaemia).
Savini 2013 was a single‐centre, five arm randomised controlled study conducted at the NICU of “G. Salesi” Children’s Hospital, Ancona, Italy, with 20% SMOFlipid® and 20% Intralipid® in two out of 5 intervention arms.
Population: Preterm infants weighing 500 to 1249 g, who received PN from the first hour of life were included. Infants with severe malformations, metabolic disease, and severe congenital sepsis were excluded.
Objective: To compare the effect of different LE on plasma phytosterol concentrations (and the possible association with PNALD).
Interventions: There were five intervention arms; 150 preterm infants were randomly assigned to receive one of the following five lipid formulations: Intralipid® (S‐LE; n = 30), Lipofundin® (50% MCT, 50% soybean oil; n = 30), Lipidem® (50% MCT, 40% soybean oil, 10% fish oil; n = 30), ClinOleic® (80% olive oil, 20% soybean oil; n = 30), SMOFlipid® (30% MCT, 30% soybean oil, 25% olive oil, 15% fish oil; n = 30).
Outcomes: Primary outcomes were plasma phytosterol concentrations at birth (cord), on day seven (on full TPN), and on day 14 (on 50% enteral calories). Secondary outcomes included clinical data such as death, growth rate, time to regain birth weight, BPD, sepsis, NEC, PNALD, and PDA.
Skouroliakou 2010 was a single centre study done in the NICU of ‘IASO’ Maternity Hospital in Athens, Greece.
Population: Preterm infants < 32 week gestation and birth weight < 1500 g requiring admission to NICU within 12 hours of birth with estimated > 80% energy intake from PN in the first eight days of life and requiring PN for at least seven days were included in the study. Exclusion criteria were inherited metabolic disorders, congenital malformations, transfusion of blood/fresh frozen plasma > 15 ml/kg and participation in another study.
Objective: To compare the effect of a parenteral fat emulsion rich in ω‐3 fatty acids on the antioxidant markers of preterm infants, when compared with a standard fat emulsion.
Interventions: 20% SMOFlipid® (MOFS‐LE; 30% MCT, 30% soybean oil, 25% olive oil, 15% fish oil; n = 14) versus 20% Intralipid® (n=18). Four different TPN protocols were created based on gestational age, weight, and clinical condition. Lipids were started on day one or two of life (based on gestational age) with a maximum of 3 g/kg/day in both groups. Enteral feeds were allowed at ≤ 20% of total energy intake and started as soon as feasible.
Outcomes: Primary outcomes were oxidation potential (vitamin A, E, and total anti‐oxidant potential). Secondary outcome were growth parameters, blood count, clinical condition, duration of ventilation, duration of phototherapy, hyperglycaemia, sepsis, and length of stay (parameters were recorded on day zero, day 14, and at discharge).
Tomsits 2010 was a single centre study done at the Department of Pediatrics, Semmelweis University, Budapest, Hungary.
Population: Sixty preterm infants < 34 weeks gestation, aged three to seven days, who were expected to receive TPN for at least seven days were randomised in this study. Exclusion criteria were not mentioned.
Objective: To evaluate the safety, tolerability, and efficacy of a MOFS‐LE (20% SMOFlipid®) compared with S‐LE (20% Intralipid®).
Interventions: 20% MOFS‐LE (n = 30) versus 20% S‐LE (n = 30). The LE was started at 0.5 g/kg/day on day one and was increased by increments of 0.5 g/kg/day daily up to a maximum of 2 g/kg/day on days four to 14. Additional oral/enteral intake comprising < 20% at baseline, < 30% on days one to three, and < 50% on days four to 14 of the total energy intake was permitted if appropriate. Other components of PN were given at the discretion of the investigator.
Outcomes: Outcomes were evaluated on day zero, eight, and 15. The primary efficacy outcome was change in weight from day one to day eight. Secondary efficacy variables included red blood cell (RBC) fatty acid profile, duration of mechanical ventilation, and oxygen therapy. Serum TG levels were used as a primary safety outcome. Secondary safety variables were vital signs, hematological variables, coagulation profile, and liver enzymes. The authors also reported on sepsis in two groups.
Vlaardingerbroek 2014 was a single centre randomised controlled study done in preterm very low birth weight (VLBW) infants at the NICU, Division of Neonatology, Department of Pediatrics, Erasmus MC, Sophia Children’s Hospital, Rotterdam, the Netherlands. Study enrolment occurred between December 2008 and January 2012. This study looked at the effect of different LE and included data from a larger trial (Vlaardingerbroek 2013) which was reported as a three arm study. In the previous study report (Vlaardingerbroek 2013), the infants were randomised into three intervention arms, i.e. standard amino acids or early lipids plus standard amino acids or early lipids plus high‐dose amino acids. Within the two early lipid intervention arms of the 2013 study (Vlaardingerbroek 2013), the infants were randomly assigned to receive two different lipid types. The effect of receiving two different lipid types is reported in Vlaardingerbroek 2014.
Population: Inborn VLBW infants (birth weight < 1500 g) with a central venous catheter for clinical purposes were eligible for the study. Exclusion criteria were congenital anomalies, chromosome defects, metabolic diseases, and endocrine, renal, or hepatic disorders.
Objective: To evaluate the safety and efficacy of a multi‐component LE containing 30% soybean oil, 30% medium‐chain triacylglycerol, 25% olive oil, and 15% fish oil compared with a conventional pure soybean oil based LE in VLBW infants.
Interventions: The study group (n = 49) received MOFS‐LE (SMOFlipid 20%®) and the control group (n = 49) received S‐LE (Intralipid 20%®). Minimal enteral feeding was initiated on day one and local feeding protocols were followed. The parenteral lipid intake was decreased by 25% to 50% if TG concentrations were between 265 and 442 mg/dL (3‐5 mmol/L) and temporarily stopped if plasma TG were more than 442 mg/dL (> 5 mmol/L). Parenteral amino acids were decreased by 25% to 50% if the plasma urea was more than 10 mmol/L (28 mg/dl) and stopped temporarily if the urea was more than 14 mmol/L (39 mg/dl). According to the local protocol, repeated blood glucose concentrations > 10 mmol/L (180 mg/dL) were treated with continuous intravenous insulin (starting dose 0.1 U/kg/hr) if reducing the glucose infusion rate to a minimal intake of 4 mg/kg/min was not effective in lowering the blood sugar. Minimal enteral feeding was initiated on the day of birth and after day three of life the nutritional regimen was left to the discretion of the attending physician.
Outcomes: Primary outcomes included fatty acid concentration in plasma TGs and phospholipids. Safety was evaluated by measuring hematological and bio‐chemical parameters, phytosterol concentrations, and clinical outcomes. Clinical outcomes included survival, duration of hospital stay, symptomatic PDA, respiratory distress syndrome (RDS), BPD, NEC, late‐onset sepsis, IVH, PVL, and ROP. Cholestasis was defined as direct bilirubin concentration > 20% of the total bilirubin concentration.
MFS‐LE versus S‐LE
Only one eligible study was available for this comparison. Savini 2013 was a single‐centre, five arm randomised controlled study done at the NICU, “G. Salesi” Children’s Hospital, Ancona, Italy, with MFS‐LE (Lipidem®) and S‐LE (20% Intralipid®) in two out of the five intervention arms. Meta‐analysis could not be performed for this comparison as no other eligible studies were identified. Details of this study are described under the MOFS‐LE versus S‐LE comparison.
OS‐LE versus S‐LE
This comparison was reported by Demirel 2011, Deshpande 2009, Gawecka 2008, Gobel 2003, Koksal 2011, Savini 2013, and Wang 2015.
Demirel 2011 was a single centre study done at the NICU, Zekai Tahir Burak Maternity Teaching Hospital, Turkey.
Population: Preterm infants ≤ 32 weeks gestation and receiving ≥ 40% parenteral calories at 14th day of life were included in the study.
Objective: To compare S‐LE (Intralipid®) and OS‐LE (ClinOleic®) in terms of plasma lipids and acyl carnitine profile.
Interventions: OS‐LE (ClinOleic®, n = 20) versus S‐LE (Intralipid®, n = 20). TPN protocol: Lipid emulsions were started on the second day of life at a rate of 1 g/kg/day and increased by 1 g/kg/day up to 3 g/kg/day and given over 24 hours. Enteral feeding was started on the second day.
Outcomes: Plasma lipid concentrations and acyl carnitine profile were compared between the groups. Other outcomes were weight on day 14, RDS, ROP, and sepsis. Data values were not provided for NEC and BPD. Liver function tests (alanine aminotransferase, aspartate aminotransferase, gamma‐glutamyl transferase) were reported.
Deshpande 2009 was a single centre study done at the Department of Neonatal Paediatrics at KEM Hospital in Perth, Western Australia.
Population: Preterm infants less than 28 weeks gestation who were less than seven days old at recruitment, with parenteral nutrition accounting for > 75% of energy intake. Exclusion criteria were major congenital malformations, inborn errors of metabolism, transfusion before baseline bloods could be taken, and exchange transfusion for hyperbilirubinaemia and lipid emulsion given before enrolment. Withdrawal criteria were enteral nutrition exceeding 25% at any time.
Objective: To compare the anti‐oxidant status and long chain polyunsaturated fatty acid (LC‐PUFA) status of infants receiving OS‐LE versus S‐LE and to evaluate the effect of the two different lipid emulsions on clinical outcomes.
Interventions: OS‐LE (ClinOleic®, n = 24) versus S‐LE (20% Intralipid®, n = 21). The amino acids were added on day one and lipids were added on day two with increments of 0.5, 1, 2, and 3 g/kg/day everyday for the first four consecutive days.
Outcomes: The primary outcomes of the study were plasma F2‐isoprostane levels as indicators of lipid peroxidation, levels of LC‐PUFA in plasma and in RBC membrane. The secondary outcomes were liver and renal function tests, blood culture positive sepsis, blood cell counts, and anthropometry at the study entry and exit.
Gawecka 2008 was a single centre study done at the NICU, Medical Academy Neonatology Department, Warsaw, Poland. The data from this study appear to be reported in two different publications ‐ data on immunological properties and clinical outcomes were published in the Journal of Pediatric Gastroenterology and Nutrition (Gawecka 2008a), while data on TG, cholesterol, bilirubin, and cholestasis appear in a polish journal (Gawecka 2008b). The baseline characteristics were identical for the participants in both published reports; we extracted data from both sources.
Population: Preterm infants < 32 weeks gestation with a birth weight <1500 g, admitted to the NICU on day one and requiring PN were eligible for inclusion in the study. Exclusion criteria were severe malformations, metabolic disease, congenital culture positive sepsis, and enteral calories < 25% of total calories.
Objective: To compare immune effects and clinical outcomes of OS‐LE versus S‐LE.
Interventions: OS‐LE (20% ClinOleic®; n = 18) versus S‐LE (20% Ivelip®; n = 20). PN was started on day one with amino acids. The LE were started within 72 hours of life at a dose of 1 g/kg/day and increased to a maximum dose of 3‐3.5 g/kg/day. Lipids were infused continuously over 24 hours.
Outcomes: Primary outcomes were tumour necrosis factor–α, IL‐6, and IL‐10 synthesis in un‐stimulated and anti‐CD3 induced peripheral blood mononuclear cells of parenterally fed premature infants. Secondary outcomes were incidence of BPD, ROP, NEC, IVH, and nosocomial infections.
Gobel 2003 was a multi‐centre study done at two neonatal intensive care units in Munich (Klinikum Rechts der Isar, Klinikum Schwabing), Germany.
Population: Inclusion criteria were 28 weeks to under 37 weeks gestation preterm infants, admitted to the NICU within 24 hours after birth with TPN requirement expected to be ≥ 80% of total energy intake. Exclusion criteria were severe malformations, hyperlipidaemia, metabolic disease, bacterial infection before study inclusion, enteral nutrition > 20 ml/kg/day and blood transfusion of more than 15 ml/kg before baseline blood sampling.
Objective: To evaluate a new parenteral LE based on olive and soybean oils (ratio 4:1), with less PUFA and more α‐tocopherol than the standard soybean oil emulsion in preterm infants.
Interventions: OS‐LE (ClinOleic®, n = 24) versus S‐LE (20% Intralipid®, n = 21). LE was started within 72 hours of birth as a 24 hour infusion at a dose of 0.5, 1.0, and 2.0 g/kg/day on the first three consecutive study days and 2 g/kg/day for next four days. Other co‐interventions were the same in the two groups. No vitamin E was given and minimal enteral nutrition was allowed. The infants were excluded if the enteral calories increased to more than 20% at any time.
Outcomes: Primary efficacy outcome variables were plasma fatty acids, α‐tocopherol, and urinary malondialdehyde. Safety outcomes included TG, cholesterol, phospholipids, hyperbilirubinaemia, and apnoea. The study reported no serious adverse events in either group. Efficacy outcomes were evaluated (per protocol) in patients on day of birth and day eight.
Koksal 2011 was a single centre study done at the NICU, Division of Neonatology, Görükle, Bursa, Turkey
Population: Preterm infants ≤ 34 weeks gestation, admitted to the NICU within 24 hours after birth with TPN requirement expected to be ≥ 80% of the total energy intake were eligible for study inclusion. Exclusion criteria were severe malformations, hyperlipidaemia, metabolic disease, enteral nutrition > 20 ml/kg/day, and blood transfusion > 15 ml/kg/day.
Objective: To compare OS‐LE versus S‐LE in terms of the effects on oxidative stress and safety of use in terms of biochemical indices.
Intervention: OS‐LE (ClinOleic®, n = 32) versus S‐LE (20% Intralipid®, n = 32). LE was started within 72 hours after the baseline blood samples were obtained. LE was infused at 1, 2, and 3 g/kg/day on the first three days and 3 g/kg/day over the next four days in both groups. After seven days of LE, infusion was stopped and blood samples were taken six hours later. Co‐interventions related to parenteral nutrition were the same in both groups. Glucose, 6% amino acid solution, trace elements, and water‐soluble vitamins except vitamin E were given to both groups.
Outcomes: The primary outcome was total anti‐oxidant capacity at day seven. Secondary outcomes were neonatal morbidity and biochemical indices after LE administration. Biochemical indices were compared at day seven, however neonatal morbidities have been reported until discharge (including ROP, BPD etc). The study reported results for continuous variables as ‘mean ± data’ values. We contacted the study authors who confirmed that the values presented in the study report were ‘mean ± standard error.' The authors also provided unpublished data on other clinical outcomes including growth rate, days to regain birth weight, IVH, and PVL.
Savini 2013 was a single‐centre, five arm randomised controlled study done at the NICU of “G. Salesi” Children’s Hospital, Ancona, Italy, with OS‐LE (ClinOleic®) and S‐LE (Intralipid®) in two out of the five intervention arms. Details of the study are described under the MOFS‐LE vs S‐LE comparison.
Wang 2015 was a double blind randomised study done at the NICU of Xin Hua Hospital and Shanghai Children's Medical Center in Shanghai, China
Population: Preterm infants with birth weight < 2000 g, admission within 72 hours after birth, and administration of parenteral nutrition for 14 days or more. Two infants from the OS‐LE arm and one infant from the S‐LE arm were excluded from analysis as they did not complete 14 days of parenteral nutrition. The exclusion criteria were administration of PN before screening, calorie intake from enteral nutrition > 10%, obstructive jaundice, suspected biliary atresia, neonatal hepatitis, liver or kidney markers increased to twice normal values, congenital abnormalities, major chromosomal diseases, cytomegalovirus infection, viral hepatitis, and suspected immunodeficiency.
Objective: To compare the effect of parenteral olive oil and soy oil based LE on liver chemistry and bile acid composition in preterm infants.
Interventions: Infants were randomised to receive either S‐LE (Intralipid®; n = 51) or OS‐LE (Clinoleic®; n = 52) for 14 days. The two LE looked identical and were started at 1 g/kg/day and increased by 0.5‐1 g/kg/day up to 3 g/kg/day. Amino acids were started at a dose of 1.5–2.0 g/kg/day and increased up to 3.5–4.0 g/kg/day. PN was decreased as enteral intake increased and withheld if enteral calorie intake was > 80% of total intake. ‘All‐in‐one’ solutions were infused continuously over 24 hours with all other co‐interventions being the same. Preterm formula was used for enteral nutrition for all infants as feasible.
Outcomes: The primary end point was liver chemistry. The secondary end point was plasma bile acid composition. Serum direct bilirubin was reported to be higher after seven days in the S‐LE group. The study reported on mortality, weight gain, days to regain birth weight, duration of ventilation, BPD, NEC, and culture positive sepsis. Clinical outcomes including ROP, IVH, and PVL were not reported in this trial.
MS‐LE versus S‐LE
This comparison was reported by Lehner 2006, Rubin 1994, and Savini 2013.
Lehner 2006 was a single centre study done at the Division of Neonatology, University of Pécs, Hungary.
Population: 25 to 37 weeks gestation preterm infants with birth weight less than 3000 g were eligible for inclusion.
Objective: To compare the effects of a MCT‐LCT emulsion (MS‐LE) and LCT emulsion (S‐LE) on the fatty acid composition of plasma phospholipids and TG.
Interventions: MS‐LE (20% Lipofundin®, n = 6) compared with S‐LE (20% Lipofundin N®, n = 6). Details of the TPN protocol were not available. Co‐interventions with 10% glucose, amino acids, electrolytes (sodium chloride, potassium chloride, calcium gluconate), trace elements (Pedel®, Pharmacia, Budapest, Hungary) and water‐soluble vitamins (Soluvit®, Baxter, Deerfield, IL) were the same in both groups.
Outcomes: Intended outcomes of the study were plasma fatty acid profile, plasma cholesterol level, hypertriglyceridaemia, and weight on day eight. Some other clinical and biochemical parameters were recorded but not reported.
Rubin 1994 was a single centre study done at the Beilinson Medical Center, Petach‐Tiqva, Israel and the results from the study were published in the Journal of Pediatrics. Results from this study regarding the fatty acid profiles appear to have been published in the Journal of Pediatric Gastroenterology and Nutrition the following year (Rubin 1995). The baseline characteristics were identical for the participants in both the published reports.
Population: Fifty‐nine preterm infants under 35 weeks gestation who received TPN for at least six days were included.
Objective: To study the effects of three different LE ‐ borage soybean LE, S‐LE, or MS‐LE ‐ on the lipid status and bilirubin levels in preterm infants.
Interventions: Infants were randomised to receive one of: a) PFE 4501® (20% LCT, 15% borage oil, L‐carnitine; n = 16); b) Intralipid® (LCT 20%; n = 18); or c) Lipofundin® (MCT‐LCT mix; n = 15). Lipid emulsion was started on day one at a dose of 0.5 g/kg/day, increased to 1.5 g/kg/day on day two to a maximum of 2.5 g/kg/day on day three, and continued till the end of the study period. Co‐interventions with amino acid solution (Vamin®) and electrolytes were the same in the two groups. Outcomes considered included weight gain, clinical variables, acid‐base balance, blood counts, glucose levels, and TG.
Savini 2013 was a single‐centre, five arm randomised controlled study done at the NICU of ‘G. Salesi’ Children’s Hospital, Ancona, Italy with MS‐LE (Lipidem®) and S‐LE (20% Intralipid®) in two out of the five intervention arms. Details of the study are described under the MOFS‐LE vs S‐LE comparison.
F‐LE versus S‐LE
No eligible studies were identified.
BS‐LE versus S‐LE
This comparison was reported by Rubin 1994.
Rubin 1994 was a single centre study done at Beilinson Medical Center, Petach‐Tiqva, Israel and was published in Journal of Pediatrics. Results from this study regarding the fatty acid profiles appear to have been published in the Journal of Pediatric Gastroenterology and Nutrition in 1995 (Rubin 1995). Borage oil‐soy oil combination LE was one of the three intervention arms in this study. Details of this study have been described under the comparison of MS‐LE versus S‐LE.
Structured LE versus S‐LE
No eligible studies were identified.
Excluded studies
Five randomised studies were excluded as the participants included term infants (Angsten 2002; Lima 1988; Magnusson 1997; Nehra 2014; Webb 2008). Some of these studies focused only on infants with surgical conditions (Angsten 2002; Magnusson 1997; Nehra 2014). One study focused on infants with cholestasis (Lam 2014). One study (Wilson 1997) compared aggressive parenteral nutrition with conventional nutrition (as per the TPN protocols in the 1990s), which was the main objective of the study, besides comparing the LE in the two groups. The details about the excluded studies have been provided in the ‘Characteristics of excluded studies’ table. Some other studies, where pure S‐LE were not included as a comparator, have been documented in the PRISMA flow diagram (Figure 1).
Risk of bias in included studies
The authors (VK, MM) assessed the quality of included studies using the criteria of the CNRG. Assessment of bias was predominantly based on allocation concealment, blinding of intervention, blinding of outcome assessment and completeness of follow up. Details of assessment are provided in ‘Risk of bias’ tables (‘Characteristics of included studies’).
Random sequence generation (selection bias)
All included studies were described as randomised. However the method of the random sequence generation was adequately described in only six studies (Demirel 2011; Deshpande 2009; Koksal 2011; Rayyan 2012; Skouroliakou 2010; Vlaardingerbroek 2014). Two studies were considered to be at a low risk for selection bias (by consensus between VK and MM) based on the description of random sequence generation in previous study reports by the same authors (D'ascenzo 2014; Savini 2013). Low risk was assigned in another study (Wang 2015) by consensus between review authors (VK, MM).
Allocation
Allocation concealment was described using the pharmacy/central allocation in eight studies (Beken 2014; D'ascenzo 2014; Deshpande 2009; Koksal 2011; Rayyan 2012; Savini 2013; Skouroliakou 2010; Vlaardingerbroek 2014) and using sealed envelopes containing cards in two studies (Gawecka 2008a; Wang 2015). In five studies there was insufficient information regarding concealment of allocation (Demirel 2011; Gobel 2003; Lehner 2006; Tomsits 2010; Rubin 1994).
Blinding
Blinding of intervention
Blinding of intervention was adequately described with both the intervention and control LE described as being identical in six studies (D'ascenzo 2014; Deshpande 2009; Rayyan 2012; Savini 2013; Skouroliakou 2010; Wang 2015). Eight studies were described as blinded but how blinding was achieved was not mentioned (Beken 2014; Gawecka 2008; Gobel 2003; Koksal 2011; Lehner 2006; Rubin 1994; Tomsits 2010; Vlaardingerbroek 2014). One study (Demirel 2011) was not described as a blinded study.
Blinding of outcome assessment
Blinding of outcome assessment was possibly achieved in six studies (D'ascenzo 2014; Deshpande 2009; Rayyan 2012; Savini 2013; Skouroliakou 2010; Wang 2015). One study (Beken 2014) was assigned low risk for detection bias by consensus between the authors (VK, MM). The risk was unclear due to absence of details on how blinding was achieved in seven studies (Gawecka 2008; Gobel 2003; Koksal 2011; Lehner 2006; Rubin 1994; Tomsits 2010; Vlaardingerbroek 2014). One study (Demirel 2011) was not described as a blinded study.
Incomplete outcome data
Demirel 2011 excluded infants who died. Rubin 1994 excluded infants who later developed sepsis, hyperbilirubinaemia, or thrombocytopenia and performed per protocol analysis (10 patients, amounting to 16% of the study sample). Gobel 2003 had 12 withdrawals (out of 45) and the data were provided only for the per protocol patients. The other studies reported outcomes for all patients with smaller numbers of withdrawals, for which the reasons were provided or intention to treat analysis was performed, and were therefore assessed to be at low risk of attrition bias. We contacted corresponding authors of eight studies by email for further information/clarification; four authors provided further information and one author provided further information including unpublished data which were included in the meta‐analyses (Koksal 2011).
Selective reporting
Study protocols were available for three studies (Beken 2014; Vlaardingerbroek 2014; Wang 2015). In the absence of study protocols the risk of bias was categorised as ‘unclear.’ The data values for some outcomes in the studies were not available (mentioned as "not significantly different") or presented as a composite outcomes and therefore could not be included in the meta‐analyses. Data values were not available for NEC and BPD/CLD in one study (Demirel 2011), sepsis in one study (Deshpande 2009), IVH in one study (Gawecka 2008), and hyperglycaemia in one study (Rubin 1994). Two studies (Rayyan 2012, Tomsits 2010) reported sepsis as a composite outcome ("infections and infestations"). One study (Rayyan 2012) reported composite outcomes of "hepatobiliary disorder" (included jaundice and cholestasis) and "metabolic and nutrition disorders" (including hyperglycaemia). Data values on growth rate were not provided in some short duration studies focusing on biochemical aspects.
For some outcomes, e.g. ROP and IVH, it was not clear from some of the study reports whether the reported outcomes were for all stages or only more advanced stages. The ROP results from such studies were mentioned in the results section if significantly different between the groups, however the data on ROP from these studies could not be used in the meta‐analyses.
Other potential sources of bias
In Demirel 2011, only the infants who were receiving 40% calories by parenteral route by the 14th day of life were included in the study, and this is likely to introduce bias and issues with randomisation. Koksal 2011 reported high rates of ventilation duration and BPD in the S‐LE intervention arm which was a cause of unexplained heterogeneity in these outcomes. Some studies did not provide data on gender distribution (Skouroliakou 2010; Tomsits 2010) or the level of sickness of the infants in the two groups (e.g. Koksal 2011) which may be a source of prognostic imbalance. The risk of bias in included studies is summarised in Figure 2.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6
We included 15 studies enrolling 979 preterm infants in the review. The authors agreed regarding inclusion and exclusion of the studies, quality assessment, and data extraction. We could not perform the planned subgroup analyses based on birthweight and gender due to lack of stratified data.
MOFS‐LE versus S‐LE (comparison 1)
Seven studies (n = 469) compared MOFS‐LE to S‐LE. A summary of the risk estimates and the grading of the evidence are provided in Table 1.
Primary outcome measures
Death before discharge (outcome 1.1)
Five studies (n = 369) reported on this outcome (Beken 2014; D'ascenzo 2014; Rayyan 2012; Savini 2013; Vlaardingerbroek 2014). None of the five studies reported any significant differences between the two groups in deaths before discharge. In the meta‐analysis, there was no statistically significant difference between groups: typical RR 1.26 (95% CI 0.68 to 2.31); typical RD 0.02 (95% CI ‐0.04 to 0.08). There was no significant heterogeneity among the studies (I² = 0% for both RR and RD).
Days to regain birth weight (outcome 1.2)
Three studies (n = 234) reported on this outcome. D'ascenzo 2014 reported significantly faster weight gain in the S‐LE group compared to the MOFS‐LE group with MD: 2.9 days (95% CI 0.55 to 5.25). In another study there was faster weight gain in the S‐LE group which did not reach statistical significance (Savini 2013). The third study reported no significant difference between the two groups (Vlaardingerbroek 2014).
In the meta‐analysis, there was a trend towards faster return to birth weight in the S‐LE group compared to the MOFS‐LE group: MD 1.12 days (95% CI ‐0.17 to 2.41; Figure 3). There was low heterogeneity among the studies (I² = 43 %).
3.

Forest plot of comparison: MOFS‐LE versus S‐LE, outcome: 1.2 Days to regain birth weight.
Rate of weight gain (g/kg/day; outcome 1.3)
Five studies (n = 347) provided data in a format that could be used for the meta‐analysis of rate of weight gain (g/kg/day). There was significant variation in the presentation of growth data and the duration for which the data were presented, making this a clinically heterogenous outcome.
Vlaardingerbroek 2014 reported weight gain (g/kg/day) as mean ± SD. Rayyan 2012 reported weight gain as mean ± SD until day eight. D'ascenzo 2014 provided growth rates only after the birth weight had been regained. Savini 2013 provided weekly mean growth rates with SDs for the first three weeks which were pooled by ‘lipid type’ to give the mean growth rate and SD over three weeks. Tomsits 2010 presented the percentage change in mean ± SD of weight at day eight and at the end of the study (14 days). Skouroliakou 2010 only reported mean ± SD of initial weight and weight on day 14. Only one study reported a statistically significant difference in growth rate, with a higher growth rate in the MOFS‐LE group compared to the S‐LE group: MD 3.10 g/kg/day (95% CI 0.6 to 5.60; Vlaardingerbroek 2014).
In the meta‐analysis there was no statistically significant difference between groups: MD 0.71 g/kg/day (95% CI ‐0.17 to 1.60). There was low statistical heterogeneity among the studies (I² = 30%).
BPD/CLD (outcome 1.4)
Four studies (n = 314) reported on this outcome. There was diversity in the definitions used for BPD and CLD in studies reporting this outcome. Beken 2014 defined CLD as oxygen dependency beyond 36 weeks of corrected age with diuretic or steroid use. Three studies defined BPD using the definition provided by Walsh 2004 (D'ascenzo 2014; Savini 2013; Vlaardingerbroek 2014). Vlaardingerbroek 2014 specified that BPD was diagnosed at 36 weeks with an oxygen reduction test performed if indicated.
There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 1.02 (95% CI 0.70 to 1.49); typical RD 0.00 (95% CI ‐0.09 to 0.10). There was low heterogeneity among the studies (I² = 31% for RR and 34% for RD).
Secondary outcome measures
Duration of ventilation (days; outcome 1.5)
Three studies (n = 208) reported on this outcome (Beken 2014; Skouroliakou 2010; Vlaardingerbroek 2014). None of the three studies individually reported any difference in the duration of ventilation in days between the two groups. Tomsits 2010 reported use of supportive/artificial ventilation and oxygen therapy as a combined outcome which could not be used in meta‐analysis. Rayyan 2012 reported that the median time to end supportive or artificial ventilation was two days in the MOFS‐LE group compared to three days in the S‐LE group (intention to treat (ITT) analysis), however did not provide IQ ranges therefore the means and SD could not be imputed.
In the meta‐analysis, there was no statistically significant difference between the groups: MD ‐0.59 days (95% CI ‐3.79 to 2.60). There was low heterogeneity among the studies (I² = 42%).
Duration of supplemental oxygen (days; outcome 1.6)
Two studies (n = 140) reported on this outcome (Beken 2014; Tomsits 2010). One study (Tomsits 2010) reported supportive/artificial ventilation and oxygen therapy as a combined outcome. There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: MD 0.47 days (95% CI ‐2.01 to 2.95). There was no heterogeneity for this outcome (I² = 0%).
Culture positive sepsis (outcome 1.7)
One study (n = 80) reported on culture positive sepsis with no statistically significant difference between the MOFS‐LE and S‐LE groups: RR 0.67 (95% CI 0.12 to 3.78); RD ‐0.02 (95% CI ‐0.13 to 0.08; Beken 2014). The test for heterogeneity was not applicable.
Any sepsis (clinical and/or culture positive; outcome 1.8)
Five studies (n = 346) reported on this outcome. Three studies used the criteria described by Stoll 2002, including Vlaardingerbroek 2014 which reported late‐onset septicaemia during the first 28 days, and two other studies reporting neonatal sepsis as positive blood culture or clinical syndrome with systemic signs and symptoms of infection and abnormalities of laboratory findings (D'ascenzo 2014; Savini 2013). Skouroliakou 2010 did not provide a definition of sepsis. Two studies reported on infections and infestations as a combined outcome and therefore the data could not be used in the meta‐analysis (Rayyan 2012; Tomsits 2010). Beken 2014 reported data on culture positive sepsis.
Vlaardingerbroek 2014 reported decreased sepsis episodes in the MOFS‐LE group compared with the S‐LE group (13/48 vs 20/48), however the difference was not statistically significant. There were no statistically significant differences between the MOFS‐LE and the S‐LE groups in the individual studies or in the meta‐analysis: typical RR 0.94 (95% CI 0.62 to 1.42); typical RD ‐0.01 (95% CI ‐0.09 to 0.07). There was low heterogeneity for this outcome (I² = 22% for RR and 6% for RD).
NEC (≥ stage 2; outcome 1.9)
Four studies (n = 314) reported on NEC. Three studies defined and reported NEC Bell stage 2 or 3 (D'ascenzo 2014; Savini 2013; Vlaardingerbroek 2014). Beken 2014 reported NEC ≥ stage 2 (exact classification not mentioned).
There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 1.35 (95% CI 0.68 to 2.67); typical RD 0.03 (95% CI ‐0.03 to 0.09). There was no heterogeneity for this outcome (I² = 0% for RR and RD).
Duration of phototherapy (days; outcome 1.10)
Skouroliakou 2010 (n = 32) reported no statistically significant difference between the MOFS‐LE and S‐LE groups: MD 0.00 days (95% CI ‐2.57 to 2.57). The test for heterogeneity was not applicable.
ROP (≥ stage 3; outcome 1.11)
Three studies (n = 256) reported on ROP (≥ stage 3; Beken 2014; D'ascenzo 2014; Vlaardingerbroek 2014); all three studies used the ICROP. One single centre study reported significantly lower rates in ROP stage 1‐2 in the MOFS‐LE group compared with the S‐LE group (1/40 vs 12/40, respectively; P value = 0.001); RR 0.08 (95% CI 0.01 to 0.61); RD ‐0.27 (95% CI ‐0.43 to ‐0.12); NNTB 4 (95% CI 2 to 8), however there was no difference in ROP stage 3 and above (Beken 2014). Only three out of seven studies comparing MOFS‐LE and S‐LE reported on ROP ≥ stage 3, which may indicate the possibility of a reporting bias for this outcome.
There were no statistically significant differences in ROP (≥ stage 3) between the MOFS‐LE and S‐LE groups in any individual study or in the meta‐analysis: typical RR 0.43 (95% CI 0.06 to 2.85); typical RD ‐0.02 (95% CI ‐0.05 to 0.02). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
IVH (grade III‐IV; outcome 1.12)
Three studies (n = 256) provided data for this outcome (though seven studies mentioned this outcome in their study report). Vlaardingerbroek 2014 reported using Papile classification, D'ascenzo 2014 mentioned using the "international classification", and Beken 2014 did not report the classification used. There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 1.02 (95% CI 0.51 to 2.04); typical RD 0.00 (95% CI ‐0.07 to 0.08). There was no heterogeneity among the studies (I² = 2% for RR and 13% for RD).
PVL (outcome 1.13)
Two studies (n = 176) provided data on PVL. Vlaardingerbroek 2014 mentioned the use of classification described by de Vries 1992, and D'ascenzo 2014 mentioned the use of "international classification". There were no infants with PVL in either study. There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR was not estimable; typical RD 0.00 (95% CI ‐0.03 to 0.03). The test for heterogeneity was not applicable for RR and there was no heterogeneity between the studies for RD (I² = 0%).
Any PDA (outcome 1.14)
Three studies (n = 234) reported on PDA. Vlaardingerbroek 2014 reported on significant PDA requiring treatment. Two studies reported the number of infants with PDA in each of the intervention arms but did not report how many of these infants required treatment (Savini 2013; D'ascenzo 2014). There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 0.93 (95% CI 0.70 to 1.22); typical RD ‐0.03 (95% CI ‐0.16 to 0.09). There was no significant heterogeneity among the studies (I² = 0% for RR and RD).
Significant PDA requiring treatment (outcome 1.15)
Vlaardingerbroek 2014 (n = 96) reported on significant PDA requiring treatment. There was no significant difference between the MOFS‐LE and S‐LE groups: typical RR 0.83 (95% CI 0.52 to 1.31); typical RD ‐0.08 (95% CI ‐0.28 to 0.11). The test for heterogeneity was not applicable.
PNALD/cholestasis (outcome 1.16)
Four studies (n = 314) provided data on this outcome (though seven studies mentioned this outcome in their reports). Two studies defined cholestasis as direct bilirubin > 20% of the total bilirubin (Beken 2014; Vlaardingerbroek 2014). D'ascenzo 2014 defined cholestasis as direct bilirubin > 2 mg/dl (> 34.2 micromoles/L). Savini 2013 defined cholestasis as direct bilirubin > 2 mg/dl (> 34.2 micromoles/L) at the age of six weeks.
There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 0.78 (95% CI 0.29 to 2.13); typical RD ‐0.01 (95% CI ‐0.06 to 0.04). There was no statistical heterogeneity for this outcome (I² = 0% for both RR and RD).
Hypertriglyceridaemia (outcome 1.17)
One study (n = 96) provided data that could be used in the meta‐analysis (although four studies reported this outcome). Two studies defined hypertriglyceridaemia as > 250 mg/dl (2.82 mmol/L; D'ascenzo 2014; Vlaardingerbroek 2014). Two studies only reported the mean TG levels (Rayyan 2012; Tomsits 2010). Two studies reported the percentage of infants with hypertriglyceridaemia (D'ascenzo 2014; Vlaardingerbroek 2014). Percentages from one of these studies could be used by converting them to the rounded off proportions (Vlaardingerbroek 2014). The (rounded) percentages reported by D'ascenzo 2014 could not be converted to equivalent proportions due to very small numbers in the groups. No study reported any significant difference in hypertriglyceridaemia between the two groups.
There was no significant difference in hypertriglyceridaemia between the MOFS‐LE and S‐LE groups: RR 1.00 (95% CI 0.61 to 1.64); RD 0.00 (95% CI ‐0.20 to 0.20). The test for heterogeneity was not applicable.
Hyperglycaemia (outcome 1.18)
Two studies (n = 112) reported data on hyperglycaemia (though this outcome was mentioned in three study reports). The cutoff for hyperglycaemia was not mentioned in Beken 2014 and described as 200 mg/dl (11.1 mmol/L) in Skouroliakou 2010. Rayyan 2012 presented data as a composite outcome with other metabolic problems and therefore could not be included in the meta‐analysis. There were no statistically significant differences between the MOFS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 0.92 (95% CI 0.27 to 3.11), typical RD ‐0.01 (95% CI ‐0.11 to 0.09). There was low heterogeneity between the studies (I² = 37% for RR and 33% for RD).
Hypoglycaemia (outcome 1.19)
Beken 2014 (n = 80) reported on this outcome, however did not provide the definition or timing of the hypoglycaemia episodes. The study report mentioned a significant difference between the groups (0/40 in MOFS‐LE vs 3/40 in S‐LE) with a P value of 0.03, however there was no statistically significant difference between the groups using the Mantel‐Haenszel method: RR 0.14 (95% CI 0.01 to 2.68), RD ‐0.07 (95% CI ‐0.17 to 0.02). The test for heterogeneity was not applicable.
No studies in this comparison reported on the outcomes of neonatal deaths (within the first 28 days of life), neuro‐developmental outcomes, pulmonary haemorrhage, thrombocytopenia requiring platelet transfusion, hypoglycaemia, or EFA deficiency (triene/tetraene or T/T ratio > 0.5).
MFS‐LE versus S‐LE (comparison 2)
Data were available only from Savini 2013 (n = 60) for this comparison group. As there was only one study in this comparison therefore the heterogeneity tests were not applicable for any of the outcomes. All outcomes for the comparison of MFS‐LE to S‐LE refer to this study. A summary of the risk estimates and the grading of the evidence are provided in Table 2.
Primary outcome measures
Death before discharge (outcome 2.1)
There was no statistically significant difference between the MFS‐LE and S‐LE groups (n = 60): RR 5.00 (95% CI 0.25 to 99.95); RD 0.07 (95% CI ‐0.04 to 0.17).
Days to regain birth weight (outcome 2.2)
There was no statistically significant difference between the MFS‐LE and S‐LE groups (n = 57): MD ‐1.00 days (95% CI ‐3.60 to 1.60).
Rate of weight gain (g/kg/day; outcome 2.3)
There was no statistically significant difference between the MFS‐LE and S‐LE groups (n = 57): MD ‐1.67 g/kg/day (95% CI ‐7.01 to 3.67).
BPD/CLD (outcome 2.4)
Savini 2013 used the definition of BPD provided by Walsh 2004. There was no statistically significant difference between the MFS‐LE and S‐LE groups (n = 57): RR 1.39 (95% CI 0.42 to 4.65); RD 0.05 (95% CI ‐0.14 to 0.24).
Secondary outcome measures
Any sepsis (clinical and/or culture positive; outcome 2.5)
Savini 2013 reported neonatal sepsis as positive blood culture or as clinical syndrome with systemic signs and symptoms of infection and abnormalities of laboratory findings. There was no statistically significant difference between the MFS‐LE and S‐LE groups in sepsis episodes (n = 57): RR 1.11 (95% CI 0.31 to 4.02); RD 0.01 (95% CI ‐0.17 to 0.20).
NEC (≥ stage 2; outcome 2.6)
Savini 2013 defined and reported NEC Bell stage 2 or 3. There was no statistically significant difference between the MFS‐LE and S‐LE groups (n = 57): RR not estimable; typical RD 0.00 (95% CI ‐0.07 to 0.07).
Any PDA (outcome 2.7)
There was no statistically significant difference between the MFS‐LE and S‐LE groups (n = 57): RR 0.96 (95% CI 0.57 to 1.64); RD ‐0.02 (95% CI ‐0.28 to 0.24).
PNALD/cholestasis (outcome 2.8)
Savini 2013 defined cholestasis as direct bilirubin > 2 mg/dl (> 34.2 micromoles/L) at the age of six weeks. There was no statistically significant difference between the MFS‐LE and S‐LE groups in the incidence of cholestasis (n = 57): RR 3.32 (95% CI 0.14 to 78.25); RD 0.04 (95% CI ‐0.06 to 0.13).
OS‐LE versus S‐LE (comparison 3)
Seven studies (n = 406) compared OS‐LE to S‐LE. A summary of the risk estimates and the grading of the evidence are provided in Table 3.
Primary outcome measures
Death before discharge (outcome 3.1)
Three studies (n = 224) reported data on death before discharge (Koksal 2011; Savini 2013; Wang 2015). Another study reported two deaths in each of the OS‐LE and S‐LE groups, however this data could not be used as the authors did not provide the number of infants originally randomised to the two groups (Gawecka 2008). There were no statistically significant differences between the OS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 1.00 (95% CI 0.21 to 4.82); typical RD 0.00 (95% CI ‐0.05 to 0.05). There was no statistical heterogeneity among the studies (I² = 0% for RR and RD).
Days to regain birth weight (outcome 3.2)
Three studies (n = 223) reported data on this outcome (Koksal 2011 (unpublished data); Savini 2013; Wang 2015). There were no statistically significant differences between the OS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: MD ‐0.19 days (95% CI ‐2.00 to 1.62). There was low statistical heterogeneity among the studies (I² = 46%).
Rate of weight gain (g/kg/day; outcome 3.3)
Two studies (n = 123) reported data that could be used in meta‐analysis (Savini 2013, Koksal 2011 (unpublished data)). Savini 2013 provided weekly mean growth rates with SDs for the first three weeks which was pooled by ‘lipid type’ to give the mean growth rate over three weeks. Demirel 2011 reported mean ± SD of the initial weight and the weight on day 14, however the data on growth rate (g/kg/day) was not available. Wang 2015 provided the mean growth rate in g/day and mean birth weight, however the SD of the growth rate in g/kg/day could not be imputed due to lack of data on covariance.
There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: MD ‐0.42 g/kg/day (95% CI ‐5.15 to 4.30). There was no statistical heterogeneity between the studies (I² = 0%).
BPD/CLD (outcome 3.4)
Four studies (n = 261) reported data on this outcome. Savini 2013 defined BPD using the definition provided by Walsh 2004. Two studies did not provide a specific definition (Gawecka 2008a; Wang 2015). Koksal 2011 defined BPD as oxygen dependency at 36 weeks postconceptional age for those infants born at < 32 weeks gestational age or at 28 days of age for those infants born at > 32 weeks gestational age. Koksal 2011 reported a significant decrease in the incidence of BPD in the OS‐LE group compared with the S‐LE group: RR 0.45 (95% CI 0.24 to 0.83). Other studies did not report any statistically significant difference between the groups.
In the meta‐analysis, combining data from three studies for 161 preterm infants, there was an effect towards a decrease in BPD in the OS‐LE group compared with the S‐LE group: typical RR 0.69 (95% CI 0.46 to 1.04); typical RD ‐0.08 (95% CI ‐0.17 to 0.00) which did not reach statistical significance (Gawecka 2008; Koksal 2011; Savini 2013). The statistical heterogeneity among the studies was low for RR and high for RD (I² = 32% for RR and 76% for RD).
Sensitivity analysis was performed to explore statistical heterogeneity in this outcome.
BPD/CLD sensitivity analysis (outcome 3.5)
Three studies (n = 197) were included in the sensitivity analysis (Gawecka 2008; Savini 2013; Wang 2015). The heterogeneity in the outcome of BPD/CLD appeared to be due to Koksal 2011; the results of this study revealed an outlying higher incidence of BPD in the S‐LE group (20/32) compared with the OS‐LE (9/32) group. This study also appeared to have unusually high duration of ventilation in the S‐LE group. After removing this study in the sensitivity analysis, the observed effect of BPD reduction in OS‐LE compared to S‐LE disappeared with typical RR 1.01 (95% CI 0.57 to 1.79) and typical RD 0.00 (95% CI ‐0.09 to 0.09), and the I² statistic reduced to 0% for RR and RD.
Secondary outcome measures
Duration of ventilation (days; outcome 3.6)
Data from three studies (n = 202) were available for this outcome (Gawecka 2008; Koksal 2011; Wang 2015). Koksal 2011 reported a statistically significant difference between the groups, with longer duration of ventilation in the S‐LE group (mean ± SD: 34.6 ± 29.9 days) compared with the OS‐LE group (mean ± SD: 12.4 ± 26.6 days). Gawecka 2008 did not find any statistically significant difference between the two groups, with the direction of effect opposite to that seen in Koksal 2011. The largest study in this group did not report any significant difference in the median ventilation duration in the two groups (we imputed means and SDs from medians and interquartile ranges; Wang 2015).
In the meta‐analysis, there was no statistically significant difference in ventilation duration between the two groups: MD ‐0.20 days (95% CI ‐1.67 to 1.26; Figure 4). There was high heterogeneity among the studies (I² = 80%), opposite direction of the mean effect, and little overlap in the confidence intervals of one study (Koksal 2011).
4.

Forest plot of comparison: OS‐LE versus S‐LE, outcome: 3.6 Duration of ventilation (days).
Duration of supplemental oxygen (days; outcome 3.7)
Two studies (n = 102) reported data on this outcome (Savini 2013; Koksal 2011 (unpublished data)).
There were no statistically significant differences between the OS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: MD ‐0.76 days (95% CI ‐16.99 to 15.47). There was moderate heterogeneity between the studies (I² = 52%). Sensitivity analysis for high heterogeneity (by excluding studies) was not possible as there are only two studies in this outcome.
Need for home oxygen therapy (outcome 3.8)
Only unpublished data provided by the authors of one study (n = 64) was available for this outcome (Koksal 2011). There was no requirement of home oxygen in either of the groups: RR not estimable; RD 0.00 (95% CI ‐0.06 to 0.06). The test for heterogeneity was not applicable.
Culture positive sepsis (outcome 3.9)
Two studies (n = 164) provided data (unpublished data) for culture positive sepsis (Koksal 2011; Wang 2015). There was no statistically significant difference between the two groups: RR 1.22 (95% CI 0.54 to 2.78); RD 0.02 (95% CI ‐0.08 to 0.12). There was no statistical heterogeneity between the studies (I² = 0% for RR and RD).
Any sepsis (clinical and/or culture positive; outcome 3.10)
Five studies (n = 301) reported data on sepsis and nosocomial infections (Demirel 2011; Gawecka 2008; Koksal 2011; Savini 2013; Wang 2015). Koksal 2011 used the criteria described by Gitto 2001 and categorized sepsis as high probable, probable, and possible sepsis. Demirel 2011 described the outcome of sepsis on the basis of clinical and laboratory parameters. Savini 2013 used criteria described by Stoll 2002, reporting neonatal sepsis as positive blood culture or as clinical syndrome with systemic signs and symptoms of infection and abnormalities in laboratory investigations. Wang 2015 defined sepsis as positive blood or cerebrospinal culture in the presence of compatible clinical signs. One study provided data on nosocomial infections (Gawecka 2008).
There were no statistically significant differences between the OS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 0.87 (95% CI 0.56 to 1.36); typical RD ‐0.03 (95% CI ‐0.12 to 0.06). There was no statistical heterogeneity among the studies (I² = 0% for RR and RD).
NEC (≥ stage 2; outcome 3.11)
One study (n = 59) defined and reported NEC Bell stage 2 or 3 (Savini 2013), while two studies used the Bell classification but did not specify the stage of NEC and therefore data from these studies could not be used in the meta‐analysis (Gawecka 2008; Koksal 2011). One study reported no difference between the groups but did not provide data (Demirel 2011). One study did not provide the definition used and did not report the stage of NEC, therefore the data from this study could not be used in meta‐analyses (Wang 2015). None of the studies reported any statistically significant difference in NEC rates between the groups.
There was no statistically significant difference between the OS‐LE and S‐LE groups: RR 3.10 (95% CI 0.13 to 73.14); RD 0.03 (95% CI ‐0.06 to 0.12). The test for heterogeneity was not applicable.
Significant jaundice requiring treatment (outcome 3.12)
Two studies (n = 109) reported data on this outcome (Gobel 2003; Koksal 2011 (unpublished data)). There were no statistically significant differences between the OS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 1.04 (95% CI 0.52 to 2.07); typical RD 0.01 (95% CI ‐0.15 to 0.16). There was no statistical heterogeneity between the studies (I² = 0% for RR and RD).
Duration of phototherapy (days; outcome 3.13)
One study (n = 38) reported on the duration of phototherapy (Gawecka 2008). There was no difference between the groups: MD ‐0.10 days (95% CI ‐1.08 to 0.88). The test for heterogeneity was not applicable.
IVH (grade III‐IV; outcome 3.14)
Two studies (n = 104) reported data for this outcome (Demirel 2011; Koksal 2011(unpublished data)). Koksal 2011 reported using Papile classification. Demirel 2011 did not provide information on the classification used. One study reported no difference between the groups (grades not mentioned) however no data were provided in the study report (Gawecka 2008). Deshpande 2009 reported that one infant who died in the OS‐LE group had grade IV IVH, however data on IVH in the two groups was not available. There were no statistically significant differences between the OS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 0.50 (95% CI 0.10 to 2.61); typical RD ‐0.04 (95% CI ‐0.13 to 0.05). There was no statistical heterogeneity between the studies (I² = 0% for both RR and RD).
PVL (outcome 3.15)
One study (n = 64) recorded this outcome (unpublished data provided by Koksal 2011). There was no statistically significant difference between the OS‐LE and S‐LE groups: RR 0.33 (95% CI 0.01 to 7.89); RD ‐0.03 (95% CI ‐0.11 to 0.05).
Any PDA (outcome 3.16)
One study (n = 59) reported on this outcome (Savini 2013). There was no statistically significant difference between the OS‐LE and S‐LE groups: RR 1.03 (95% CI 0.63 to 1.71); RD 0.02 (95% CI ‐0.24 to 0.27). The test for heterogeneity was not applicable. No study reported on significant PDA requiring treatment.
Air leaks (outcome 3.17)
Data were available from one study (n = 64; Koksal 2011 (unpublished data)). There was no statistically significant difference between the OS‐LE and S‐LE groups for air leaks: RR 0.50 (95% CI 0.05 to 5.24); RD ‐0.03 (95% CI ‐0.13 to 0.07). The test for heterogeneity was not applicable.
PNALD/cholestasis (outcome 3.18)
Four studies (n = 261) reported data on cholestasis. One study defined cholestasis as direct bilirubin > 2 mg/dl (34.2 mmol/L) at the age of six weeks (Savini 2013). One study defined cholestasis as direct bilirubin fraction greater than 20% of the total bilirubin after fourteen days of life (Koksal 2011 (unpublished data provided by the authors)). Two studies did not provide definition for cholestasis (Gawecka 2008; Wang 2015). Only mean values for liver functions tests and conjugated bilirubin were available from one study (Deshpande 2009).
There were no statistically significant differences between the OS‐LE and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 1.00 (95% CI 0.26 to 3.86); typical RD 0.00 (95% CI ‐0.05 to 0.05). There was no heterogeneity among the studies (I² = 0% for RR and RD).
Hypertriglyceridaemia (outcome 3.19)
Two studies (n = 104) reported on this outcome. Demirel 2011 used the definition of TG > 200 mg/dl (2.25 mmol/L) and Koksal 2011 did not provide any definition.
There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 0.67 (95% CI 0.12 to 3.73); typical RD ‐0.02 (95% CI ‐0.11 to 0.07). There was no heterogeneity for RD (I² = 0%). The test of heterogeneity for RR was not applicable.
Hyperglycaemia (outcome 3.20)
One study (n = 64) provided data on this outcome (Koksal 2011 (unpublished data)). There was no statistically significant difference between the OS‐LE and S‐LE groups: RR 1.00 (95% CI 0.22 to 4.59); RD 0.00 (95% CI ‐0.14 to 0.14). The test for heterogeneity was not applicable.
No studies in this comparison group reported on the outcomes of neonatal deaths (within the first 28 days of life), neuro‐developmental outcomes, pulmonary haemorrhage, thrombocytopenia requiring platelet transfusion, hypoglycaemia or essential fatty acid deficiency (triene/tetraene or T/T ratio) > 0.5. ROP was reported by three studies in this comparison, however data from these studies could not be used for meta‐analysis because none of the studies clarified whether they were reporting on all stages of ROP or ROP stages 3 and 4. Two studies mentioned using the ICROP (Gawecka 2008; Koksal 2011). One study did not provide the definition of ROP (Demirel 2011). None of the studies reported any difference in the incidence of ROP between the groups.
MS‐LE versus S‐LE (comparison 4)
Three studies (n = 108) compared MS‐LE to S‐LE (Lehner 2006; Rubin 1994; Savini 2013). The heterogeneity tests were not applicable as none of the outcomes had data from more than one study. A summary of the risk estimates and the grading of the evidence are provided in Table 4.
Primary outcome measures
Death before discharge (outcome 4.1)
One study (n = 60) reported on this outcome (Savini 2013). There were no deaths in either group: RR not estimable; RD 0.00 (95% CI ‐0.06 to 0.06).
Days to regain birth weight (outcome 4.2)
One study (n = 60) reported data on this outcome (Savini 2013). There was no difference between groups: MD 1.00 days (95% CI ‐1.53 to 3.53).
Rate of weight gain (g/kg/day; outcome 4.3)
Only one study (n = 60) reported data on this outcome (Savini 2013). Another study reported no difference in growth between the two groups however the data values were not provided (Rubin 1994). There was no significant difference between the groups: MD ‐2.67 g/kg/day (95% CI ‐8.2 to 2.86).
BPD/CLD (outcome 4.4)
One study (n = 60) reported on this outcome and defined BPD using the criteria of Walsh 2004 (Savini 2013). There was no difference between the groups: RR 1.00 (95% CI 0.28 to 3.63); RD 0.00 (95% CI ‐0.17 to 0.17).
Secondary outcome measures
Any sepsis (clinical and/or culture positive; outcome 4.5)
One study (n = 60) reported on this outcome (Savini 2013). This study used the criteria by Stoll 2002, reporting neonatal sepsis as positive blood culture or as clinical syndrome with systemic signs and symptoms of infection and abnormalities of laboratory findings. There was no significant difference between the groups: RR 2.00 (95% CI 0.67 to 5.94); RD 0.13 (95% CI ‐0.07 to 0.33).
NEC (≥ stage 2; outcome 4.6)
One study (n = 60) reported on this outcome using Bell staging (stage 2 or 3; Savini 2013). There was no difference between the groups: RR 5.00 (95% CI 0.25 to 99.95); RD 0.07 (95% CI ‐0.04 to 0.17).
Any PDA (outcome 4.7)
One study (n = 60) reported on PDA but did not provide any details regarding whether treatment was required for PDA (Savini 2013). No study reported on significant PDA requiring treatment. There was no significant difference between the groups: RR 1.13 (95% CI 0.70 to 1.82); RD 0.07 (95% CI ‐0.19 to 0.32).
PNALD/cholestasis (outcome 4.8)
One study (n = 60) reported on this outcome and defined cholestasis as direct bilirubin > 2 mg/dl (> 34.2 micromol/L) at age of six weeks (Savini 2013). There was no statistically significant difference between the groups: RR 3.00 (95% CI 0.13 to 70.83); RD 0.03 (95% CI ‐0.05 to 0.12).
Hypertriglyceridaemia (outcome 4.9)
Only one study (n = 12) reported on this outcome and used a definition of TG > 200 mg/dl (> 2.25 mmol/L) for hypertriglyceridaemia (Lehner 2006). No infant in either group developed hypertriglyceridaemia: RR was not estimable; RD 0.00 (95% CI ‐0.27 to 0.27).
No study reported on neonatal deaths (within the first 28 days of life), neurodevelopmental outcomes, duration of ventilation, duration of supplemental oxygen, need for home oxygen, culture positive sepsis, PDA requiring treatment, jaundice requiring treatment, duration of phototherapy, ROP, IVH and PVL. No study reported data on episodes of hypoglycaemia or hyperglycaemia, though one study reported glucose within normal limits in both groups (only mean values provided; Rubin 1994).
F‐LE versus S‐LE (comparison 5)
We did not identify any eligible studies for this comparison.
BS‐LE versus S‐LE (comparison 6)
One study (n = 34) compared borage oil emulsion (PFE 4501) enriched in GLA and carnitine to S‐LE (20% Intralipid; Rubin 1994). In this study, both LE appeared to be safe and well tolerated in preterm infants. No data were available for any of our outcomes of interest.
Primary outcome measures
Physical growth
One study (Rubin 1994) reported no difference in the weights of infants in the BS‐LE and S‐LE groups during the study, however no data values were provided.
Secondary outcome measures
Hyperglycaemia
Rubin 1994 reported glucose (mean) within normal limits in all groups, but no data on the incidence of hyperglycaemia were provided.
Structured LE versus S‐LE (comparison 7)
We did not identify any eligible studies for this comparison.
All fish oil containing LE versus S‐LE (comparison 8)
This is a combined intervention comparison of ‘all fish oil containing LE’ versus S‐LE (7 studies; n = 499). This comparison includes the study data from comparison 1 (MOFS‐LE vs S‐LE) and comparison 2 (MFS‐LE vs S‐LE). There were no studies comparing F‐LE (i.e. Omegaven®) to S‐LE. A summary of the risk estimates and the grading of the evidence are provided in Table 5.
Primary outcome measures
Death before discharge (outcome 8.1)
Five studies (n = 399) reported on this outcome (Beken 2014; D'ascenzo 2014; Rayyan 2012; Savini 2013; Vlaardingerbroek 2014). There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 1.28 (95% CI 0.69 to 2.35); typical RD 0.03 (95% CI ‐0.03 to 0.08). There was no statistical heterogeneity among the studies (I² = 0% for both RR and RD).
Days to regain birth weight (outcome 8.2)
Three studies (n = 261) reported on this outcome. Two studies did not report any statistically significant difference between the groups (Vlaardingerbroek 2014, Savini 2013). D'ascenzo 2014 reported significantly faster weight gain in the S‐LE group compared to the MOFS‐LE group: MD 2.9 days (95% CI 0.55 to 5.25).
In the meta‐analysis, there was no statistically significant difference in days to regain birth weight between the fish oil containing LE and S‐LE groups: MD 0.81 days (95% CI ‐0.43 to 2.05). There was moderate heterogeneity among the studies (I² = 52 %).
Rate of weight gain (g/kg/day; outcome 8.3)
Five studies (n = 374) provided data in a format that could be used for the meta‐analysis. There was significant variation in the presentation of growth data and the duration for which the data were presented, making this a clinically heterogenous outcome.
Vlaardingerbroek 2014 reported weight gain (g/kg/day) as mean ± SD. Rayyan 2012 reported weight gain as mean ± SD until day eight. D'ascenzo 2014 provided growth rates only after the birth weight had been regained. Savini 2013 provided weekly mean growth rates with SDs for first three weeks which were pooled by ‘lipid type’ to give mean growth rates and SDs over three weeks. Tomsits 2010 presented percentage change in mean ± SD of weight at day eight and at the end of the study (14 days), and mean ± SD of rate of weight gain was imputed. Skouroliakou 2010 reported mean ± SD of initial weight and weight on day 14, however the data on growth rate were not available. Only Vlaardingerbroek 2014 reported a statistically significant difference in growth rate, with a higher rate in the MOFS‐LE group compared to the S‐LE group: MD 3.10 g/kg/day (95% CI 0.6 to 5.60).
In the meta‐analysis, there was no statistically significant difference between the groups: MD 0.69 g/kg/day (95% CI ‐0.19 to 1.57). There was low statistical heterogeneity among the studies (I² = 30%).
BPD/CLD (outcome 8.4)
Four studies (n = 341) reported on this outcome. There was diversity in the definitions used in the studies reporting this outcome. Beken 2014 defined CLD as oxygen dependency beyond 36 weeks of corrected age with diuretic or steroid use. Three studies defined BPD using the criteria provided by Walsh 2004 (D'ascenzo 2014; Savini 2013; Vlaardingerbroek 2014). Vlaardingerbroek 2014 specified that BPD was diagnosed at 36 weeks with an oxygen reduction test performed if indicated.
There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 1.02 (95% CI 0.70 to 1.50); typical RD 0.01 (95% CI ‐0.08 to 0.10). There was low heterogeneity among the studies (I² = 30 % for RR and 33% for RD).
Secondary outcome measures
Duration of ventilation (days; outcome 8.5)
Three studies (n = 208) reported on this outcome (Beken 2014; Skouroliakou 2010; Vlaardingerbroek 2014). None of the three studies individually reported any difference in the duration of ventilation between the two groups. One study reported the use of supportive/artificial ventilation and oxygen therapy as a combined outcome which could not be used in meta‐analysis (Tomsits 2010). One study did not report IQ ranges therefore the SD could not be imputed for meta‐analysis (Rayyan 2012).
In the meta‐analysis, there was no statistically significant difference between the groups: MD ‐0.59 days (95% CI ‐3.79 to 2.60). There was low heterogeneity among the studies (I² = 42%).
Duration of supplemental oxygen (days; outcome 8.6)
Two studies (n = 140) reported on this outcome (Tomsits 2010, Beken 2014). One study reported supportive/artificial ventilation and oxygen therapy as a combined outcome (Tomsits 2010).
There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: MD 0.47 days (95% CI ‐2.01 to 2.95). There was no heterogeneity among the studies (I² = 0%).
Culture positive sepsis (outcome 8.7)
One study (n = 80) reported on culture positive sepsis with no statistically significant difference between the groups: RR 0.67 (95% CI 0.12 to 3.78); RD ‐0.02 (95% CI ‐0.13 to 0.08; Beken 2014). The test for heterogeneity was not applicable.
Any sepsis (clinical and/or culture positive; outcome 8.8)
Five studies (n = 373) reported data on this outcome that could be used in the meta‐analysis. Three studies used criteria described by Stoll 2002, with Vlaardingerbroek 2014 reporting late‐onset septicaemia during the first 28 days, and two studies reporting neonatal sepsis as positive blood culture or as clinical syndrome with systemic signs and symptoms of infection and abnormalities of laboratory findings (D'ascenzo 2014; Savini 2013). One study did not provide definition of sepsis (Skouroliakou 2010). Two studies reported on infections and infestations as a combined outcome and therefore their data could not be used in the meta‐analysis (Rayyan 2012, Tomsits 2010). One study reported data on culture positive sepsis (Beken 2014).
Vlaardingerbroek 2014 reported decreased sepsis episodes in the MOFS‐LE group compared with the S‐LE group (13/48 vs 20/48), however the difference was not statistically significant. There were no statistically significant differences between the ‘all fish oil containing‐LE’ and S‐LE groups in the individual studies or in the meta‐analysis: typical RR 0.92 (95% CI 0.61 to 1.39); typical RD ‐0.02 (95% CI ‐0.09 to 0.06). There was no heterogeneity among the studies (I² = 3% for RR and 0% for RD).
NEC (≥ stage 2; outcome 8.9)
Four studies (n = 341) reported on NEC ≥ stage 2. Three studies defined and reported NEC Bell stage 2 or 3 (D'ascenzo 2014; Savini 2013; Vlaardingerbroek 2014). One study reported NEC ≥ stage 2 but did not mention the exact classification (Beken 2014).
There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 1.29 (95% CI 0.65 to 2.57); typical RD 0.02 (95% CI ‐0.03 to 0.08). There was no heterogeneity among the studies (I² = 0% for RR and RD).
Duration of phototherapy (outcome 8.10)
One study (n = 32) reported this outcome (Skouroliakou 2010). There was no statistically significant difference between the groups: MD 0.0 days (95% CI ‐2.57 to 2.57). The test for heterogeneity was not applicable.
ROP (≥ stage 3; outcome 8.11)
Three studies (n = 256) reported on ROP ≥ stage 3 (Beken 2014; D'ascenzo 2014; Vlaardingerbroek 2014). All three studies compared MOFS‐LE to S‐LE. There were no statistically significant differences in ROP ≥ stage 3 between the groups in the individual studies or in the meta‐analysis: typical RR 0.43 (95% CI 0.06 to 2.85); typical RD ‐0.02 (95% CI ‐0.05 to 0.02). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
IVH (grade III‐IV; outcome 8.12)
Three studies (n = 256) provided data for this outcome (though seven studies mentioned this outcome in their study reports). One study reported using Papile classification (Vlaardingerbroek 2014), one study mentioned using the "international classification" (D'ascenzo 2014), and a third did not report the classification used (Beken 2014). There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 1.02 (95% CI 0.51 to 2.04); typical RD 0.00 (95% CI ‐0.07 to 0.08). There was no heterogeneity among the studies (I² = 2% for RR and 13% for RD).
PVL (outcome 8.13)
Two studies (n = 176) provided data on PVL. Vlaardingerbroek 2014 mentioned the use of classification described by de Vries 1992; D'ascenzo 2014 mentioned the use of "international classification". There were no infants with PVL in either of the groups in both the studies. There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR not estimable; typical RD 0.00 (95% CI ‐0.03 to 0.03). The test for heterogeneity was not applicable for RR and there was no heterogeneity among the studies for RD (I² = 0%).
Any PDA (outcome 8.14)
Three studies (n = 261) reported on PDA. One study reported on significant PDA requiring treatment (Vlaardingerbroek 2014). Two studies reported the number of infants with PDA in each of the intervention arms but did not report how many of these infants required treatment (Savini 2013; D'ascenzo 2014). There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 0.93 (95% CI 0.72 to 1.21); typical RD ‐0.03 (95% CI ‐0.15 to 0.09). There was no heterogeneity among the studies (I² = 0% for RR and RD).
Significant PDA requiring treatment (outcome 8.15)
One study (n = 96) reported on significant PDA requiring treatment (Vlaardingerbroek 2014). There was no significant difference between the groups: RR 0.83 (95% CI 0.52 to 1.31); RD ‐0.08 (95% CI ‐0.28 to 0.11). The test for heterogeneity was not applicable.
PNALD/cholestasis (outcome 8.16)
Four studies (n = 341) provided data on this outcome (seven studies mentioned this outcome in their study report). Two studies defined cholestasis as direct bilirubin > 20% of the total bilirubin (Beken 2014; Vlaardingerbroek 2014). One study defined cholestasis as direct bilirubin > 2 mg/dl (> 34.2 micromoles/L; D'ascenzo 2014). One study defined cholestasis as direct bilirubin > 2 mg/dl (> 34.2 micromoles/L) at the age of six weeks (Savini 2013).
There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 0.80 (95% CI 0.29 to 2.16); typical RD ‐0.01 (95% CI ‐0.05 to 0.04). There was no statistical heterogeneity among the studies (I² = 0% for RR and 3% for RD).
Hypertriglyceridaemia (outcome 8.17)
One study (n = 96) provided data for this outcome (though four studies reported this outcome). Two studies used a definition of TG > 250 mg/dl (2.82 mmol/L; D'ascenzo 2014; Vlaardingerbroek 2014). Two studies only reported the mean TG levels (Rayyan 2012; Tomsits 2010). Two studies reported the percentage of infants with hypertriglyceridaemia (D'ascenzo 2014; Vlaardingerbroek 2014). Percentages from one of these studies was used by converting it to the rounded off proportions (Vlaardingerbroek 2014). The (rounded) percentages reported by D'ascenzo 2014 could not be converted to equivalent proportions due to very small numbers in the groups. No study reported any significant difference in hypertriglyceridaemia between the two groups.
There was no statistically significant difference between the MOFS‐LE and S‐LE groups in Vlaardingerbroek 2014: RR 1.00 (95% CI 0.61 to 1.64); RD 0.00 (95% CI ‐0.20 to 0.20). The test for heterogeneity was not applicable.
Hyperglycaemia (outcome 8.18)
Two studies (n = 112) reported data on hyperglycaemia (though this outcome was mentioned in three study reports). The cutoff for hyperglycaemia was not mentioned in one study report (Beken 2014), and described as 200 mg/dl (11.1 mmol/L) in one study (Skouroliakou 2010). In a third study, data were presented as a composite outcome with other metabolic problems and therefore data could not be used in meta‐analysis (Rayyan 2012). There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 0.92 (95% CI 0.27 to 3.11); typical RD ‐0.01 (95% CI ‐0.11 to 0.09). There was no heterogeneity among the studies (I² = 37% for RR and 33% for RD).
Hypoglycaemia (outcome 8.19)
One study (n = 80) comparing MOFS‐LE to S‐LE reported on this outcome, however did not provide the definition used (Beken 2014). The study report mentioned a significant difference between the groups (0/40 in MOFS‐LE vs 3/40 in S‐LE), with a P value of 0.03. However there was no statistically significant difference between the groups using the Mantel‐Haenszel method: RR 0.14 (95% CI 0.01 to 2.68); RD ‐0.07 (95% CI ‐0.17 to 0.02). The test for heterogeneity was not applicable.
No studies in this comparison group reported on the outcomes of neonatal deaths (within the first 28 days of life), neurodevelopmental outcomes, pulmonary haemorrhage, thrombocytopenia requiring platelet transfusion, or essential fatty acid deficiency.
All alternative LE vs S‐LE (comparison 9)
This comparison is a combined intervention comparison of ‘all alternative LE’ versus S‐LE (15 studies; n = 979) to evaluate the effect of decreased PUFA content in the alternative LE on the clinical outcomes in preterm infants. A summary of the risk estimates and the grading of the evidence are provided in Table 6.
Primary outcome measures
Death before discharge (outcome 9.1)
Seven studies (n = 623) reported on this outcome (Beken 2014; D'ascenzo 2014; Koksal 2011 (unpublished data); Rayyan 2012; Savini 2013; Vlaardingerbroek 2014; Wang 2015). None of the studies reported significant differences in comparison groups for death before discharge. In the meta‐analysis there was no difference between the ‘all alternative LE’ and S‐LE groups for this outcome: typical RR 1.17 (95% CI 0.66 to 2.07); typical RD 0.01 (95% CI ‐0.03 to 0.06). There was no heterogeneity among the studies (I² = 0% for RR and RD).
Days to regain birth weight (outcome 9.2)
Five studies (n = 484) reported on this outcome. Three studies reported no significant difference in days to regain birth weight (Savini 2013; Vlaardingerbroek 2014; Wang 2015). D'ascenzo 2014 reported a longer time to regain birth weight in the MOFS‐LE group compared to the S‐LE group (13.4 ± 5.6 days versus 10.5 ± 5.1 days, P value = 0.021; MD: 2.9 days (95% CI 0.55 to 5.25)). In the meta‐analysis, there was no statistically significant difference between the ‘all alternative LE’ and S‐LE groups: MD 0.53 days (95% CI ‐0.52 to 1.58). There was low heterogeneity among the studies (I² = 43%).
Rate of weight gain (g/kg/day; outcome 9.3)
Six studies (n = 497) provided data on growth that could be used for meta‐analysis out of the eleven studies that reported on this outcome.The presentation of growth data and the duration for which these data were presented varied greatly across studies.
Two studies did not report any statistically significant difference in growth between the alternative lipid emulsion and S‐LE groups, but data values were not available for meta‐analysis. Vlaardingerbroek 2014 reported weight gain (g/kg/day) as mean ± SD. Rayyan 2012 reported weight gain (mean ± SD until day eight in ITT analysis). One study provided growth rates only after birth weight had been regained (D'ascenzo 2014). One study provided the weekly mean growth rate with SDs for each ‘lipid type’ for the first three weeks, which was pooled to give mean growth rates over three weeks for each ‘lipid type,’ which were further pooled together in a single group (for ‘all alternative LE’; Savini 2013). One study presented ‘the percentage change’ in mean ± SD of weight at day eight and at day 14 (from the initial weight) and mean ± SD of the rate of weight gain was imputed (Tomsits 2010). Two studies reported the mean ± SD of initial weight and weight on day 14, however the data on growth rate were not available (Skouroliakou 2010; Demirel 2011). Data from one study (provided as mean ± SD at the beginning and at the end of the study) could not be used as baseline weight was not available for 50% of the infants (Lehner 2006). Wang 2015 provided the mean growth rate in g/day and mean birth weight, however the SD of the growth rate in g/kg/day could not be imputed due to lack of data on covariance. Gawecka 2008a did not provide specific data on growth rate. Only Vlaardingerbroek 2014 reported a statistically significant difference in this outcome, with higher growth rate in the MOFS‐LE group compared to the S‐LE group: MD 3.10 g/kg/day (95% CI 0.6 to 5.60).
In the meta‐analysis, there was no statistically significant difference between the groups in the rate of growth: MD 0.68 g/kg/day (95% CI ‐0.19 to 1.55). There was no heterogeneity among the studies (I² = 17%).
BPD/CLD (outcome 9.4)
Seven studies (n = 602) reported data that could be used in the meta‐analysis for this outcome (although nine studies reported on this outcome). There was variation in the definition used for BPD and CLD. Beken 2014 defined CLD as oxygen dependency beyond 36 weeks of corrected age with diuretic or steroid use. Three studies defined BPD using the definition provided by Walsh 2004 (D'ascenzo 2014; Savini 2013; Vlaardingerbroek 2014). Vlaardingerbroek 2014 specified that BPD was diagnosed at 36 weeks with an oxygen reduction test performed if indicated. Koksal 2011 defined BPD as oxygen dependency at 36 weeks postconceptional age for those infants born at < 32 weeks gestational age or at 28 days of age for those infants born at > 32 weeks gestational age. Three studies did not provide a definition for BPD (Demirel 2011; Gawecka 2008a; Wang 2015). Demirel 2011 reported no statistically significant difference between the groups but did not provide any values.
Koksal 2011 reported a significant decrease in the incidence of BPD in infants treated with OS‐LE: RR 0.45 (95% CI 0.24 to 0.83). There was no statistically significant difference between the groups in any other study.
In the meta‐analysis, there was no statistically significant difference between the groups: typical RR 0.84 (95% CI 0.63 to 1.12), typical RD ‐0.04 (95% CI ‐0.11 to 0.02). There was low heterogeneity among the studies for RR (I² = 34%) and moderate heterogeneity for RD (I² = 55%).
Secondary outcome measures
Duration of ventilation (days; outcome 9.5)
Six studies (n = 410) reported data on this outcome in a format that could be used in the meta‐analysis. Three studies reported no difference in the duration of ventilation in the intervention or control groups (Gawecka 2008; Skouroliakou 2010; Wang 2015). One study reported use of supportive/artificial ventilation and oxygen therapy as a combined outcome which could not be used in meta‐analysis (Tomsits 2010). One study reported that the median time to end supportive or artificial ventilation was two versus three days (MOFS‐LE versus S‐LE, respectively; ITT), however did not provide IQ ranges, therefore the means and SD could not be imputed (Rayyan 2012). Koksal 2011 reported a statistically significant difference between the groups with a longer duration of ventilation in the S‐LE group (mean ± SD: 34.6 ± 29.9 days) compared with the OS‐LE group (mean ± SD: 12.4 ± 26.6 days).
In the meta‐analysis, there was no statistically significant difference between the groups: MD ‐0.27 days (95% CI ‐1.60 to 1.06). There was moderate heterogeneity among the studies (I² = 63%).
Duration of supplemental oxygen (days; outcome 9.6)
Four studies (n = 242) reported data on the duration of supplemental oxygen. Three studies reported duration of oxygen use (days; Beken 2014; Gawecka 2008a; Tomsits 2010). Tomsits 2010 reported use of supportive/artificial ventilation and oxygen therapy as a combined outcome.
In the meta‐analysis, there was no statistically significant difference between the groups: MD 0.44 days (95% CI ‐2.01 to 2.89). There was no heterogeneity among the studies (I² = 0%).
Need for home oxygen therapy (outcome 9.7)
Data from one study (n = 64) was available for this outcome (Koksal 2011 (unpublished data provided by the authors)). There was no requirement of home oxygen in either of the groups: RR not estimable; RD 0.00 (95% CI ‐0.06 to 0.06). The test for heterogeneity was not applicable.
Culture positive sepsis (outcome 9.8)
Three studies (n = 244) (Beken 2014; Koksal 2011; Wang 2015) reported on this outcome. Koksal and co‐workers (Koksal 2011) provided (unpublished) data on the number of infants with culture positive sepsis. There were no statistically significant differences between the groups in the individual studies or in the meta‐analysis: typical RR 1.08 (95% CI 0.52 to 2.26), typical RD 0.01 (‐0.07 to 0.08). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
Any sepsis (clinical and/or culture positive; outcome 9.9)
Nine studies (n = 674) provided data in a format that could be used in the meta‐analysis (although twelve studies reported on sepsis and infections). Three studies used criteria described by Stoll 2002, with Vlaardingerbroek 2014 reporting late‐onset septicaemia during the first 28 days and two studies reporting neonatal sepsis as positive blood culture or as clinical syndrome with systemic signs and symptoms of infection and abnormalities of laboratory findings (D'ascenzo 2014; Savini 2013). Study by Koksal 2011 used the criteria described by Gitto 2001 and categorized sepsis as high probable, probable, or possible sepsis. Demirel 2011 described the outcome of sepsis on the basis of clinical and laboratory parameters. Wang 2015 defined sepsis as positive blood or cerebrospinal culture in the presence of compatible clinical signs. One study did not provide definition of sepsis (Skouroliakou 2010). One study provided data for the outcome of nosocomial infections (Gawecka 2008a). Two studies reported on infections and infestations as a combined outcome (Rayyan 2012; Tomsits 2010). One study reported no difference in sepsis between the groups, however data values were not provided (Deshpande 2009). Three studies reported on culture positive sepsis (Beken 2014; Koksal 2011 (unpublished data); Wang 2015). No study reported a statistically significant difference between the groups for this outcome.
In the meta‐analysis, there was no difference between the groups: typical RR 0.90 (95% CI 0.66 to 1.23); typical RD ‐0.02 (95% CI ‐0.08 to 0.04; Figure 5). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
5.

Forest plot of comparison: All alternative LE vs S‐LE, outcome: 9.9 Any sepsis (clinical and/or culture positive).
NEC (≥ stage 2; outcome 9.10)
Four studies (n = 400) reported on NEC (≥ stage 2), however eight studies reported on NEC. Three studies defined and reported NEC Bell stage 2 or 3 (D'ascenzo 2014; Savini 2013; Vlaardingerbroek 2014). One study reported NEC ≥ stage 2 (classification not mentioned; Beken 2014). Two studies used Bell classification but did not report the stage of NEC (Gawecka 2008; Koksal 2011). One study did not provide the definition used and did not report the stage of NEC, therefore the data from this study could not be used in meta‐analyses (Wang 2015). One study reported no difference between the groups, but did not report data values (Demirel 2011). There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 1.34 (95% CI 0.67 to 2.67); typical RD 0.03 (95% CI ‐0.03 to 0.08). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
Significant jaundice requiring treatment (outcome 9.11)
Two studies (n = 109) provided data for this outcome which were used in the meta‐analysis. Gobel 2003 reported on the number of infants with hyperbilirubinaemia (the definition was not reported); Koksal 2011 provided unpublished data about the infants requiring phototherapy.
There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 1.04 (95% CI 0.52 to 2.07); typical RD 0.01 (95% CI ‐0.15 to 0.16). There was no heterogeneity between the studies (I² = 0% for both RR and RD).
Duration of phototherapy (days; outcome 9.12)
Two studies (n = 70) reported on the duration of phototherapy (days; Gawecka 2008a; Skouroliakou 2010). There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: MD ‐0.09 days (95% CI ‐1.00 to 0.83). There was no heterogeneity between the studies (I² = 0%).
ROP (≥ stage 3; outcome 9.13)
Only three studies (n = 256) reported on ROP ≥ stage 3 (Beken 2014; D'ascenzo 2014; Vlaardingerbroek 2014). All three studies compared MOFS‐LE to S‐LE and used the ICROP. One single centre study reported significantly lower ROP rates (stage 1‐2) in the MOFS‐LE group compared with the S‐LE group (1/40 vs 12/40, respectively; P value = 0.001): RR 0.08 (95% CI 0.01 to 0.61); RD ‐0.27 (95% CI ‐0.43 to ‐0.12); NNTB 4 (95% CI 2 to 8), however there was no difference in rates of ROP stage 3 and above in this study (Beken 2014).
There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 0.43 (95% CI 0.06, 2.85); typical RD ‐0.02 (95% CI ‐0.05, 0.02). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
IVH (grade III‐IV; outcome 9.14)
Five studies (n = 360) reported data on IVH grade III‐IV (although seven studies mentioned the outcome in their study report). Two studies reported using Papile classification (Koksal 2011; Vlaardingerbroek 2014), one study mentioned using the "international classification" (D'ascenzo 2014), and the other studies did not report the classification used. One study reported no difference between the groups (grades not mentioned), but no data were provided in the publication (Gawecka 2008). Deshpande 2009 reported that one infant who died in the OS‐LE group had grade IV IVH, however data on IVH in the two groups was not available. There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 0.90 (95% CI 0.48 to 1.70); typical RD ‐0.01 (95% CI ‐0.07 to 0.05). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
PVL (outcome 9.15)
Three studies (n = 240) reported data on PVL, however only two studies specified the classification. One study used the classification described by de Vries 1992 (Vlaardingerbroek 2014), while the other study mentioned the use of "international classification" (D'ascenzo 2014). Unpublished data regarding PVL were provided by Koksal 2011. There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 0.33 (95% CI 0.01 to 7.89); typical RD ‐0.01 (95% CI ‐0.04 to 0.02). There was no heterogeneity among the studies for RD (I² = 0% ). The test for heterogeneity was not applicable for RR.
Any PDA (outcome 9.16)
Three studies (n = 320) reported on PDA. One study reported on significant PDA requiring treatment (Vlaardingerbroek 2014). Two studies reported on the number of infants with PDA in each of the intervention arms but did not report how many of these infants required treatment (D'ascenzo 2014; Savini 2013). There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 0.96 (95% CI 0.75 to 1.23); typical RD ‐0.02 (95% CI ‐0.14 to 0.10). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
Significant PDA requiring treatment (outcome 9.17)
One study (n = 96) reported on significant PDA requiring treatment (Vlaardingerbroek 2014). There was no significant difference between the groups: RR 0.83 (95% CI 0.52 to 1.31); RD ‐0.08 (95% CI ‐0.28 to 0.11). The test of heterogeneity was not applicable.
Air leaks (outcome 9.18)
The authors of one study (n = 64) provided unpublished data on air leaks (Koksal 2011). There was no statistically significant difference between the groups: RR 0.50 (95% CI 0.05 to 5.24); RD ‐0.03 (95% CI ‐0.13 to 0.07). The test of heterogeneity was not applicable.
PNALD/cholestasis (outcome 9.19)
Seven studies (n = 602) provided data on this outcome (although eight studies mentioned this outcome in their study reports). Two studies defined cholestasis as direct bilirubin > 20% of the total bilirubin (Beken 2014; Vlaardingerbroek 2014), one defined it as direct bilirubin > 20% of total bilirubin after 14 days of life (Koksal 2011), another defined it as direct bilirubin > 2 mg/dl (> 34.2 micromoles/L; D'ascenzo 2014), and Savini 2013 defined it as direct bilirubin > 2 mg/dl (>34.2 micromoles/L) at the age of six weeks. Two studies did not provide a definition for cholestasis (Gawecka 2008; Wang 2015). Only mean values of liver function and conjugated bilirubin were available from one study (Deshpande 2009).
There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 0.83 (95% CI 0.37 to 1.86); typical RD ‐0.01 (95% CI ‐0.04 to 0.03). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
Hypertriglyceridaemia (outcome 9.20)
Four studies (n = 212) provided data that could be used in the meta‐analysis (though eight studies reported on this outcome). Two studies used the definition of TG > 200 mg/dl (2.25 mmol/L; Demirel 2011; Lehner 2006), while two studies used > 250 mg/dl (2.82 mmol/L; D'ascenzo 2014; Vlaardingerbroek 2014). Other studies did not provide the definition used. Three studies only reported the mean TG levels (Rubin 1994; Rayyan 2012; Tomsits 2010). Rubin 1994 reported that one infant with hypertriglyceridaemia was withdrawn from the study, but it was unclear to which group this infant belonged. Two studies reported the percentage of infants with hypertriglyceridaemia (D'ascenzo 2014; Vlaardingerbroek 2014). Percentages from one of these studies were converted to rounded off proportions (Vlaardingerbroek 2014). The (rounded) percentages reported by D'ascenzo 2014 could not be converted to equivalent proportions due to very small numbers in the groups.
There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 0.95 (95% CI 0.59 to 1.54); typical RD ‐0.01 (95% CI ‐0.11 to 0.09). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
Hyperglycaemia (outcome 9.21)
Three studies (n = 176) reported data on hyperglycaemia (although this outcome was mentioned in four studies). The definition for hyperglycaemia was not reported by three studies (Beken 2014; Koksal 2011; Rubin 1994). The hyperglycaemia cutoff was described as 200 mg/dl (11.1 mmol/L) in one study (Skouroliakou 2010). One study provided unpublished data on this outcome (Koksal 2011). Rubin 1994 reported glucose within normal limits (mean values) in all groups and did not provide any data values which could be used in meta‐analysis. In one study, data were presented as a composite outcome with other metabolic problems and therefore data could not be used in meta‐analysis (Rayyan 2012). There were no statistically significant differences between the groups in any of the individual studies or in the meta‐analysis: typical RR 0.95 (95% CI 0.37 to 2.46); typical RD ‐0.00 (95% CI ‐0.09 to 0.08). There was no heterogeneity among the studies (I² = 0% for both RR and RD).
Hypoglycaemia (outcome 9.22)
One study (n = 80), comparing MOFS‐LE to S‐LE, reported on this outcome but did not provide the definition of hypoglycaemia (Beken 2014). The study report mentioned a significant difference between the groups (0/40 in MOFS‐LE versus 3/40 in S‐LE) with a P value of 0.03. However there was no statistically significant difference between the groups using the Mantel‐Haenszel method: RR 0.14 (95% CI 0.01 to 2.68); RD ‐0.07 (95% CI ‐0.17 to 0.02). The test of heterogeneity was not applicable.
No studies in this comparison group reported on the outcomes of neonatal death (within the first 28 days of life), neurodevelopmental outcomes, pulmonary haemorrhage, thrombocytopenia requiring platelet transfusion, or essential fatty acid deficiency.
Discussion
Fifteen randomised controlled studies enrolling 979 preterm infants were included in this review comparing the newer alternative LE to the conventional pure soybean oil based LE. The included studies varied considerably in PN protocols, mostly reflecting the change in TPN practices over time as the review includes studies published over two decades from 1994 to 2015. The type of LE compared in the studies is also reflective of the evolution of lipid emulsions with the MCT‐LCT emulsions in the earlier studies, olive‐soy combinations in the later studies and multi‐source lipid emulsions containing fish oil in the more recent years.
Summary of main results
Out of the 15 studies included in this review, seven studies (n = 469) compared MOFS‐LE to S‐LE, seven studies (n = 406) compared OS‐LE to S‐LE, three studies (n = 108) compared MS‐LE to S‐LE, one study (n = 34) compared BS‐LE to S‐LE, and one study (n = 60) reported data comparing MFS‐LE to S‐LE. Besides performing individual comparisons between different types of alternative LE and S‐LE, we performed two comparisons of ‘all fish oil containing LE’ and ‘all alternative LE’ with S‐LE. Excessive PUFA content exposes preterm infants to the effects of oxidation (Sala‐Vila 2007), and may contribute to adverse outcomes including BPD, ROP, and mortality. We felt that the beneficial effects of substituting soybean oil, and thereby reducing high PUFA and ω‐6 content and achieving a better ω‐6/ω‐3 ratio, may become more obvious by pooling all studies using alternative LE. Similarly, we pooled all studies using LE containing fish oil to explore the beneficial effects of fish oil along with the reduced PUFA content.
Included studies were conducted in 11 different countries: three in Turkey, two studies each in Hungary and Italy, and one each in Poland, Israel, Australia, Germany, Belgium, Greece, China, and the Netherlands.
The GRADE QoE ranged from ‘low’ to ‘very low,’ as included studies were mostly small, single centre studies, and the OIS was not achieved for the important clinical outcomes in any comparison.
Meta‐analysis could not be performed for MS‐LE versus S‐LE, MFS versus S‐LE, or BS‐LE versus S‐LE due to a paucity of studies or reported data. There were no eligible studies comparing structured LE (e.g. Structolipid®) to S‐LE or F‐LE (e.g. Omegaven®) to S‐LE.
All LE used in the studies included in this review were reported to be well tolerated with no reports of any significant side effects.
In the primary outcomes of death, growth rate (g/kg/day), days to regain birth weight, and CLD or BPD, there were no statistically significant differences between any of the newer alternative LE and the pure soy based LE in any comparison. Most of the studies focused on biochemical parameters as their primary outcomes and therefore may not have been powered to detect differences in critical clinical outcomes. One study focused on ROP as the primary outcome (Beken 2014).
In preterm infants, the growth rate (g/kg/day) in the initial weeks is likely to be different than that in the later weeks, with different clinical factors impacting on the weight gain. The presentation of data on growth rate (g/kg/day) and the time period for which these data were presented varied greatly across the included studies making the results of the meta‐analysis for this outcome difficult to interpret.
Days to regain birth weight was more consistently reported among the studies. There was an effect towards more days to regain birth weight in the MOFS‐LE group compared to the S‐LE group which did not reach statistical significance. Some studies have reported lower AA levels in infants receiving MOFS‐LE (D'ascenzo 2014). The role of AA in growth potential and its possible beneficial effects for intrauterine and extrauterine growth in preterm infants has been suggested previously in the literature (Koletzko 2003). Interestingly, the effect towards delay in regaining birth weight was less obvious in the combined comparison of ‘all fish oil containing LE’ versus S‐LE. ‘All fish oil containing LE’ included the data from the MFS‐LE group, which received a higher soy content compared with the MOFS‐LE group (40% soy in MFS‐LE versus 30% soy in MOFS‐LE). However the GRADE QoE was ‘low’ and currently it is not clear whether a 10% difference in soy content between MFS‐LE and MOFS‐LE has a significant effect on AA status and growth in preterm infants. Further studies are required to evaluate the effect of AA and different lipid constituents in LE on growth in preterm infants.
Reduced oxidative stress with alternative LE may have a beneficial effect on the incidence of BPD and respiratory morbidity (Koletzko 2010). Additionally, OS‐LE have been shown to improve α‐tocopherol content, potentially decreasing oxidative stress (Gobel 2003). There was an effect towards decreased BPD in OS‐LE versus S‐LE not reaching statistical significance. There was high statistical heterogeneity for RD among the studies. The heterogeneity in this outcome and the observed effect appeared to be due to one single centre study, which reported significantly higher BPD incidence and ventilation duration in the S‐LE group compared with OS‐LE group (Koksal 2011). Studies with small sample size may be vulnerable to prognostic imbalance. After removing this study in the sensitivity analysis, the observed effect of BPD reduction in OS‐LE compared to S‐LE disappeared, as did the heterogeneity.
Alternative LE may have improved immunological effects due to the immune neutral properties of olive oil in OS‐LE (Sala‐Vila 2007) and due to the decreased cyclooxygenase products in fish oil based LE. Some included studies reported higher incidence of sepsis (statistically non‐significant) in the S‐LE group compared with OS‐LE group (Demirel 2011; Gawecka 2008). Demirel 2011 reported significantly higher levels of hexanoyl carnitine in the S‐LE group compared with the OS‐LE group and proposed that higher hexanoyl carnitine levels in patients receiving S‐LE may cause immunosuppression, leading to higher sepsis risk. In a previous meta‐analysis of three studies (n = 197), risk of sepsis was reported to be decreased with use of LE that were not purely soybean oil based compared with pure soybean oil LE (RR 0.75; 95% CI 0.56 to 1.00) (Vlaardingerbroek 2012). In the present, larger meta‐analysis of nine studies (n = 674), we did not find any statistically significant difference in sepsis between ‘all alternative LE’ and S‐LE, or in any of the other comparisons.
DHA is a major structural lipid in the sensory and vascular retina (Smithers 2008; Lapillonne 2013), and is considered important for neuro‐development (Henriksen 2008; Lapillonne 2013). Preterm infants are prone to DHA deficiency (Lapillonne 2013). DHA levels are shown to be higher with LE containing fish oil (Pawlik 2013). In the current review there was no statistically significant difference in the incidence of ROP (≥ stage 3) in any individual study or in any of the comparisons. One single centre study reported a significant lower incidence of ROP (stage 1‐2) in the MOFS‐LE group compared with the S‐LE group, however there was no difference in ROP stage 3 and above in this study (Beken 2014). It is noteworthy that only three out of seven studies comparing MOFS‐LE to S‐LE reported on ROP (≥ stage 3), which may indicate the possibility of an outcome reporting bias.
A previous randomised study in 130 preterm infants (<32 weeks gestation; birth weight < 1250 grams) (Pawlik 2013), comparing combination of Omegaven® (100% fish oil‐LE) and ClinOleic® (OS‐LE) in 1:1 ratio to ClinOleic® (OS‐LE), reported significant decrease in the requirement of laser therapy for ROP with RR 0.48 (95% CI 0.24 to 0.96) in the infants receiving fish‐olive‐soy combination. In this study, preterm infants had high incidence of ROP requiring surgery (22/70; 31.4 %) in the comparison (OS‐LE) group whereas the studies included in the current systematic review had much lower mean incidence of ROP stage 3 and above (2.3%) in the control (S‐LE) group. This study reported seven withdrawals (all in the fish oil group) and these infants were excluded from the analysis. Pawlik 2013 was not included in the present review due to the absence of pure soy based LE comparison arm. Further studies with larger sample sizes, especially focusing on higher risk groups including extremely low birth weight infants, are required to explore the effect of fish oil containing LE on ROP compared with S‐LE.
Improved liver function, reversal of cholestasis, and prevention of PNALD have been reported in the paediatric population, surgical patients, and preterm infants with the use of fish oil containing LE (Koletzko 2010; Nandiwada 2013; Pawlik 2011; Puder 2009). A recent randomised controlled study in preterm infants reported a statistically significant decrease in the incidence of cholestasis in the fish‐olive‐soy LE group (3/60) compared with the OS‐LE group (20/70; Pawlik 2013). The comparison group (OS‐LE) in this study had a high incidence of cholestasis (28.5%), whereas the studies included in the current systematic review had much lower mean incidence of cholestasis in the control (S‐LE) group (4.6%). We found no statistically significant differences in the incidence of cholestasis in any of the comparisons. It is possible that the potential beneficial effects of fish oil based LE on liver disease and the cholestatic adverse effects of S‐LE may be more evident with longer term TPN or in those clinical settings where the incidence of PNALD and cholestasis is high.
There were no statistically significant differences in the other secondary outcomes: ventilation duration, duration of supplemental oxygen, NEC (≥ stage 2), significant jaundice requiring treatment, IVH (grade III‐IV), PVL, PDA, hypertriglyceridaemia, hyperglycaemia or hypoglycaemia in any of the comparisons.
No study reported on long term neurodevelopmental outcomes, thrombocytopenia requiring treatment, pulmonary haemorrhage or infants with essential fatty acid deficiency.
Based on this review, there is need for further research to evaluate the effectiveness of newer LE compared with pure soy based LE in preterm infants.
Overall completeness and applicability of evidence
The evidence presented in this review is limited due to a paucity of large randomised studies reporting on clinically important outcomes on this topic. The low number of participants especially affects the individual comparisons of different LE versus S‐LE. Long term neurodevelopmental outcomes were not reported by any study.
Gender distribution was not available for two out of 15 studies and therefore total gender distribution in the review is unknown. No subgroup analysis based on gender or gestational cutoffs were possible due to the non‐availability of such data.
Quality of the evidence
The quality of evidence in this review ranged from ‘low’ to ‘very low’ for most of the outcomes (GRADE Working Group recommendations; Guyatt 2011a). This was primarily due to OIS not being achieved, with wide confidence intervals for most of the outcomes (Appendix 4). There was high statistical heterogeneity in some outcomes. Publication bias was difficult to evaluate using funnel plots as there were less than ten studies (usually less than five studies) in most comparisons.
Potential biases in the review process
The small number of studies, methodological diversity, heterogeneous reporting, and outcomes reported in a format that could not be used in meta‐analyses are some of the limitations of the review. For some outcomes (e.g. growth rate) we have used imputed values for means and SD to be able to use the available data in the meta‐analyses. Further, investigations of heterogeneity and sensitivity analyses where there are very few studies are unreliable. We have used the fixed‐effect model throughout the review as per the CNRG recommendations. For some situations with high heterogeneity and for an intrinsically heterogeneous intervention group, such as all alternative LE, random‐effects analyses may also be appropriate.
Authors' conclusions
Implications for practice.
In this review, all LE appeared to be well tolerated in preterm infants with the alternative LE appearing to have a similar safety profile compared with the conventional pure soy oil based LE. Although the use of MOFS‐LE was associated with lower rates of the early stages (1‐2) of ROP in one study, there were no statistically significant differences in the clinically important outcomes including death, growth, BPD, sepsis, ROP ≥ stage 3, and PNALD between newer alternative LE and conventional pure soy oil based LE. The GRADE QoE ranged from ‘low’ to ‘very low.’ Based on this review, there is insufficient evidence to recommend any alternative LE over S‐LE or vice versa in preterm infants.
Implications for research.
Large randomised studies focusing on clinically important outcomes such as death, growth, BPD, neurodevelopment, ROP, and PNALD as their primary outcomes are required to evaluate the effectiveness of newer LE compared with the conventional pure soy oil based LE in preterm infants. Studies aiming to explore the effect of fish oil based LE on ROP should be adequately powered to detect a difference in the clinically important outcome of ROP ≥ stage 3 in light of reports of decreases in early stages of ROP with fish oil based LE. Future studies should also focus on specific ‘at risk’ population subgroups (e.g. extreme prematurity, preterm infants on long term PN, etc) and aim to explore the effect of different proportions of lipid constituents including fish oil and olive oil on morbidity and mortality in preterm infants.
What's new
| Date | Event | Description |
|---|---|---|
| 28 April 2020 | Review declared as stable | This review will no longer be updated. This is because it has been replaced by the following Cochrane review: "Lipid emulsions for parenterally fed preterm infants" (Kapoor 2019). |
History
Protocol first published: Issue 6, 2011 Review first published: Issue 12, 2015
Acknowledgements
Editorial support of the CNRG has been funded with federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN267200603418C.
We would like to thank Professor Julian Higgins, Professor of Evidence Synthesis, School of Social and Community Medicine, University of Bristol and Centre for Reviews and Dissemination, University of York and Orestis Efthimiou, Co‐ordinator of the Cochrane Statistical Methodology Group, for giving advise regarding the imputed values of SD. We would like to thank to Dr Merih Cetinkaya (Koksal 2011), Uludag University, Division of Neonatology, Görükle, Bursa, Turkey for data clarifications and providing unpublished data regarding the study participants.
Appendices
Appendix 1. Constituents of lipid emulsions used in the studies included in the review.
| Constituents |
20% Intralipid (Fresenius Kabi) |
Lipoven2 (Fresenius Kabi) |
Liposyn III (Hospira) |
PFE 4501 Pharmacia Sweden* |
Lipofundin‐ MCT/LCT 20% (B Braun) |
Structolipid 20% (Fresenius Kabi) |
Lipovenoes ‐MCT (Fresenius Kabi) |
ClinOleic 20% (Baxter) |
Omegaven (Fresenius Kabi) |
Lipoplus3 (B Braun) |
20% SMOFlipid (Fresenius Kabi) |
| Oil source (%) | |||||||||||
| Soybean oil | 100 | 100 | 100 | 85 | 50 | 64 | 50 | 20 | ‐ | 40 | 30 |
| Coconut (MCT) oil | ‐ | ‐ | ‐ | 50 | 36 | 50 | ‐ | ‐ | 50 | 30 | |
| Olive oil | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 80 | ‐ | ‐ | 25 | |
| Fish oil | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 100 | 10 | 15 | |
| Borage oil | 15 | ||||||||||
|
Composition of major fatty acids: % by weight of total fatty acids MCTs | |||||||||||
| Caproic acid (6:0) | ‐ | ‐ | ‐ | 0.5 | 0.1 | 0.2 | ‐ | ‐ | ‐ | Trace | |
| Caprylic acid (8:0) | ‐ | ‐ | ‐ | 29 | 26 | 30 | ‐ | ‐ | 30 | 17 | |
| Capric acid (10:0) | ‐ | ‐ | ‐ | 20 | 10 | 17 | ‐ | ‐ | 19 | 12 | |
| Lauric acid (12:0) | ‐ | ‐ | ‐ | 1 | 0.2 | 0.2 | ‐ | ‐ | ‐ | 0.2 | |
| Long‐chain triacylglycerols | |||||||||||
| Myristic acid (14:0) | 0.2 | ‐ | Trace | ‐ | ‐ | Trace | 0.2 | 5 | 0.5 | 1 | |
| Palmitic acid (16:0) | 10.8 | 12 | 11 | 11.2 | 7 | 7 | 7 | 12 | 12 | 6 | 9 |
| Palmitoleic acid (16:1 ω‐7) | ‐ | ‐ | Trace | ‐ | ‐ | 0.2 | 1.5 | 9 | 0.6 | 2 | |
| Stearic acid (18:0) | 4.2 | 5 | 4 | 4.1 | 2 | 3 | 3 | 2 | 4 | 2 | 3 |
| Oleic acid (18:1 ω‐9) | 24 | 24 | 23 | 11 | 14 | 13 | 62 | 15 | 8 | 29 | |
| ω‐6/ω‐3 ratio | 7:1 | 7:1 | 7:1 | ‐ | 7:1 | 7:1 | 7:1 | 9:1 | 1:8 | 2.7:1 | 2.5:1 |
| ω‐6 long‐chain triacylglycerols | |||||||||||
| Linoleic acid (18:2 ω‐6) | 53 | 53 | 53 | 50.8 | 29 | 35 | 27 | 19 | 4.4 | 24 | 19 |
| Arachidonic acid (20:4 ω‐6) | 0.1 | ‐ | ‐ | 0.2 | ‐ | ‐ | 0.5 | 2 | ‐ | 0.5 | |
| ω‐3 long‐chain triacylglycerols | |||||||||||
| α‐linolenic acid (18:3 ω‐3) | 7 | 8 | 8.3 | 5.9 | 4 | 5 | 4 | 2 | 1.8 | 3 | 2 |
| EPA (20:5 ω‐3) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 19 | 3 | 3 | |
| DHA (22:6 ω‐3) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.5 | 12 | 2 | 2 | |
| α‐tocopherol (mg/L) | 38 | ‐ | ‐ | ‐ | 180 | 6.9 | ‐ | 32 | 150‐296 | 190 | 200 |
| Other constituents | |||||||||||
| Phytosterols (mg/L) | 348 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 327 | ‐ | ‐ | 47.6 |
| γ‐linolenic acid (GLA; 18:3 ω‐6) | 3.2 | ||||||||||
| L‐Carnitine | 0.4 | ||||||||||
Data collated from multiple sources including Vanek 2012; Vlaardingerbroek 2012; Wanten 2007 and other references in the review. MCT: medium‐chain triacylglycerol, NP: not provided. Lipoven® is also known as Lipovenoes®; Lipoplus® is also known as Lipidem®. * Pharmacia group merged with Pfizer in 2002. No recent trials with PFE4501® were identified and the current status of manufacturing could not be confirmed at the time of this review.
Appendix 2. Abbreviations for lipid emulsions
Specific lipid components have been denoted by the following letters: soy by ‘S’; MCT (from coconut oil) by ‘M’; fish oil by ‘F’; olive oil by ‘O’; borage oil by ‘B’. The abbreviations for the ‘alternative LE’ end in the letter ‘S’ (if containing soy oil) for consistency in nomenclature and to indicate the common theme of substitution of soy oil by lipids from alternative sources (e.g. olive‐soy is abbreviated as ‘OS‐LE’; MCT‐soy as ‘MS‐LE’; MCT‐olive‐fish‐soy as ‘MOFS‐LE’). Further, except the letter ‘S’ (which is always the last letter in the LE abbreviations), the sequence of letters denoting the other lipid components are in the decreasing order of lipid percentage (as found in commonly available preparations) e.g. in MFS‐LE (e.g. Lipidem®), the percentage of MCT > percentage of fish oil; and in MOFS‐LE (e.g. SMOFlipid®) the percentage of MCT (30%) > percentage of olive oil (25%) > percentage of fish oil (15%).
Appendix 3. Details of search strategy
The searches were conducted in the following databases with database specific limits and syntax. The test searches were done in each database to fine tune strategy for each database and then search methodology was modified to maximise the balance between sensitivity and precision. We used truncation, wild cards and synonyms to maximise sensitivity. Test searches included searching for individual MeSH terms and EMTREE terms as applicable besides separately searching for the individual text terms before combining with "OR" in the final search. OvidSP Medline was used initially to build the search strategy (not shown here). The searches were initially performed for MEDLINE on 25.11.2014 and in all other databases till 25.9.2014. Further the searches were updated till 31 July, 2015 in the following databases: (CENTRAL 2015, Issue 7), MEDLINE, EMBASE, CINAHL and Web of Science. The details of the search strategy and results from the important databases have been described below for the initial searches:
MEDLINE: was searched using the PUBMED portal to ensure we captured the latest unindexed articles. Cochrane Neonatal Review Group's recommended ‘clinical queries filter’ (Haynes 2005) was used and search limited to "human" and "birth till 23 months". However search was repeated from 1.1. 2013 to 25.11.2014 without using any filters to ensure we did not miss any latest unindexed articles. Duplicates were removed using EndNote 2014.
| SN | MEDLINE Search strategy (accessed and searched via Pubmed 25.9.2014 and updated till 25.11.2014) | Hits |
| #1 | Search (infant, newborn[mesh:noexp]) OR ((((((((extreme* AND premat*[tw]) OR prematur*[tw]) OR low birth weight*[tw]) OR extreme* AND prematur*[tw]) OR lbw*[tw]) OR elbw*[tw]) OR preterm*[tw]) OR pre‐term*[tw]) |
591029 |
| #2 | Search ((((((((intravenous, infusions) OR emulsions) OR parenteral nutrition solutions) OR fat emulsions, intravenous) OR intraven*[tw]) OR parenter*[tw]) OR i.v.[tw]) OR infus*[tw]) OR le[tw] |
671357 |
| #3 | Search ((((((((((((((((((((((((((((((((((((((lipids[mesh:noexp]) OR glycerides) OR fatty acids) OR oils) OR soybean oil) OR soy*[tw]) OR coconut*[tw]) OR borage*[tw]) OR fish*[tw]) OR olive*[tw]) OR intralipid*[tw]) OR ivelip*[tw]) OR liposyn*[tw]) OR lipovenoes*[tw]) OR lipofundin*[tw]) OR SMOF*[tw]) OR omegaven*[tw]) OR clinoleic*[tw]) OR PFE4501*[tw]) OR MOFS*[tw]) OR MOFSLE*[tw]) OR lipoplus*[tw]) OR omega‐6*[tw]) OR omega‐3*[tw]) OR MCT*[tw]) OR LCT*[tw]) OR PUFA*[tw]) OR MUFA*[tw]) OR polyunsaturated*[tw]) OR monounsaturated*[tw]) OR linolenic*[tw]) OR linoleic*[tw]) OR docosahexaenoic acid*[tw]) OR eicosapentaenoic acid*[tw]) OR DHA[tw]) OR EPA[tw]) OR triacylgl*[tw]) OR triglyc*[tw]) OR arachidon*[tw] |
847844 |
| #4 | #1 AND #2 AND #3 (without any filters) | 1779 |
| #5 | Using Haynes filter AND (#1 AND #2 AND #3) Filters: Infant: birth‐23 months ; as shown below Search (Therapy/Broad[filter]) AND ((((((((((((intravenous, infusions) OR emulsions) OR parenteral nutrition solutions) OR fat emulsions, intravenous) OR intraven*[tw]) OR parenter*[tw]) OR i.v.[tw]) OR infus*[tw]) OR le[tw])) AND (((((((((((((((((((((((((((((((((((((((lipids[mesh:noexp]) OR glycerides) OR fatty acids) OR oils) OR soybean oil) OR soy*[tw]) OR coconut*[tw]) OR borage*[tw]) OR fish*[tw]) OR olive*[tw]) OR intralipid*[tw]) OR ivelip*[tw]) OR liposyn*[tw]) OR lipovenoes*[tw]) OR lipofundin*[tw]) OR SMOF*[tw]) OR omegaven*[tw]) OR clinoleic*[tw]) OR PFE4501*[tw]) OR MOFS*[tw]) OR MOFSLE*[tw]) OR lipoplus*[tw]) OR omega‐6*[tw]) OR omega‐3*[tw]) OR MCT*[tw]) OR LCT*[tw]) OR PUFA*[tw]) OR MUFA*[tw]) OR polyunsaturated*[tw]) OR monounsaturated*[tw]) OR linolenic*[tw]) OR linoleic*[tw]) OR docosahexaenoic acid*[tw]) OR eicosapentaenoic acid*[tw]) OR DHA[tw]) OR EPA[tw]) OR triacylgl*[tw]) OR triglyc*[tw]) OR arachidon*[tw])) AND ((infant, newborn[mesh:noexp]) OR ((((((((extreme* AND premat*[tw]) OR prematur*[tw]) OR low birth weight*[tw]) OR extreme* AND prematur*[tw]) OR lbw*[tw]) OR elbw*[tw]) OR preterm*[tw]) OR pre‐term*[tw]))) Filters: Infant: birth‐23 months |
1022 |
| #6 | (#1 AND #2 AND #3) Filters: Publication date from 2013/01/01 to 2014/11/25 (with no other filters) | 81 |
| Combining #5 (1022 results) + #6 (81 results) (after removing 38 duplicates) = | 1065 |
EMBASE was searched on 25.9.2014 via OvidSP using the database segment "emczd= Embase Classic+ Embase 1947 to 2014 september 25".
1. exp prematurity/ 2. (extrem$ adj prematur$).ab,ot,ti. 3. prematur$.mp. 4. (low adj birth adj weight$).ab,ot,ti. 5. (premature adj birth$).mp. 6. lbw.mp. 7. elbw.mp. 8. vlbw.mp. 9. preterm$1.mp. 10. pre‐term$1.mp. 11. or/1‐10 12. (intravenous adj infusion$).ab,ot,ti. 13. emuls$.mp. 14. (parenteral adj nutrition adj solution$).ab,ot,ti. 15. parenteral nutrition solution/ 16. intraven$.mp. 17. parenter$.mp. 18. iv.mp. 19. le.mp. 20. infus$.mp. 21. or/12‐20 22. exp lipid emulsion/ 23. exp fatty acids/ 24. fat$.mp. 25. exp oils/ 26. oil$.mp. 27. soy$.mp. 28. coconut$.mp. 29. borage$.mp. 30. fish$.mp. 31. olive$.mp. 32. intralipid$.mp. 33. ivelip$.mp. 34. liposyn$.mp. 35. lipovenoes.mp. 36. lipofundin$.mp. 37. SMOF$.mp. 38. omegaven$.mp. 39. clin?oleic$.mp. 40. PFE4501.mp. 41. MOFS$.mp. 42. MOFS$LE$.mp. 43. lipoplus$.mp. 44. (omega adj2 "6").ab,ot,ti. 45. (omega adj2 "3").ab,ot,ti. 46. (LCT adj10 MCT).ab,ot,ti. 47. PUFA$.mp. 48. MUFA$.mp. 49. linolenic$.mp. 50. linoleic$.mp. 51. docosa?hexanoic$.mp. 52. DHA.mp. 53. EPA.mp. 54. eicosapent??noic$.mp. 55. arachidon$.mp. 56. triacyl$.mp. 57. triglyc$.mp. 58. or/22‐57 59. 11 and 21 and 58 60. limit 59 to human
Limits: Human
Total hits: 1986 (25.9.2014) (details of hits with each search word are not provided)
CENTRAL (Cochrane Central Register of Controlled Trials) searched on 25.9.14
#1preterm* #2premat* #3preterm* #4pre‐term* #5(#1 OR #2 OR #3 OR #4) #6emulsion* #7parenter* #8intraven* #9infus* #10parenter* nutrition #11 (#6 OR #7 OR #8 OR #9 OR #10) #12lipid* #13fat* #14oil* #15soy* #16(medium adj chain adj triglyceride*) #17(long adj chain adj triglyceride*) #18(LCT* adj MCT*) #19LCT* #20MCT* #21coconut* #22olive* #23fish* #24triglycer* #25triacylgl* #26omega adj2 "3" #27omega adj2 "6" #28"n" adj "6" #29"n" adj "3" #30borage* #31eicosapenta?noic* #32EPA #33DHA #34docosahexa?noic* #35arachidon* #36intralipid* #37clinoleic #38SMOF* #39PFE4501 #40omegaven* #41lipoplus* #42lipovenoes #43lipofundin* #44MOFS* #45LE #46#12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 #47#5 AND #11 AND #46
Limits: None applied
Total hits: 308
Web of Science (WoS; Thomson Reuters): (searched on 25.9.2014) was used for keyword search and also for citation search for each of the included study report (except D'ascenzo 2014 which was not available on WoS citation index at time of this search)
| Set | Web of Science search strategy | Total Hits |
| #1 | ts= (prematur* OR (extreme* AND premat*) OR prematur* OR low birth weight* OR lbw* OR elbw* OR preterm* OR pre‐term) DocType=All document types; Language=All languages; | 179, 838 |
| #2 | ts=(parenteral nutrition solutions OR fat emulsions OR intraven* OR parenter* OR i.v. OR infus* OR le) DocType=All document types; Language=All languages; | 566, 548 |
| #3 | ts=(lipids OR glycerides OR fatty acids OR oils OR soybean oil OR soy* OR coconut* OR borage* OR fish* OR olive* OR intralipid OR ivelip* OR liposyn* OR lipovenoes* OR lipofundin* OR SMOF* OR omegaven* OR clinoleic* OR PFE4501* OR MOFS* OR MOFSLE OR lipoplus* OR omega‐6 OR omega‐3* OR MCT* OR LCT* OR PUFA* OR MUFA* OR polyunsaturated* OR monounsaturated* OR linolenic* OR linoleic* OR docosahexaenoic acid* OR eicosapentaenoic acid* OR DHA OR EPA OR triacylgl* OR triglyc* OR arachidon*) DocType=All document types; Language=All languages; |
1,555,777 |
| #4 | #3 AND #2 AND #1 DocType=All document types; Language=All languages; | 872 |
| #5 | #3 AND #2 AND #1
Refined by: [excluding]:WEB OF SCIENCE CATEGORIES: (OBSTETRICS GYNECOLOGY OR MEDICINE GENERAL INTERNAL OR SURGERY OR REPRODUCTIVE BIOLOGY OR NEUROSCIENCES OR PERIPHERAL VASCULAR DISEASE OR TOXICOLOGY OR AGRICULTURE DAIRY ANIMAL SCIENCE OR CLINICAL NEUROLOGY OR VETERINARY SCIENCES OR ANESTHESIOLOGY OR RHEUMATOLOGY OR RADIOLOGY NUCLEAR MEDICINE MEDICAL IMAGING OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH OR PSYCHIATRY OR BIOTECHNOLOGY APPLIED MICROBIOLOGY OR ZOOLOGY OR UROLOGY NEPHROLOGY OR SPORT SCIENCES OR SPECTROSCOPY OR ORTHOPEDICS OR DERMATOLOGY OR CHEMISTRY ORGANIC OR TRANSPLANTATION OR OTORHINOLARYNGOLOGY OR MYCOLOGY OR GERONTOLOGY OR GERIATRICS GERONTOLOGY OR ENGINEERING BIOMEDICAL OR ECOLOGY OR CHEMISTRY MULTIDISCIPLINARY OR CHEMISTRY APPLIED OR CELL TISSUE ENGINEERING OR AUDIOLOGY SPEECH LANGUAGE PATHOLOGY OR ANTHROPOLOGY OR ACOUSTICS) DocType=All document types; Language=All languages; |
631 |
Limits: All irrelevant categories removed as above
Advanced Key word search results (631 hits) + Citation search (861 hits)
Total from WoS: 1086 (after removing duplicates).
CINAHL via EBSCO host (1982 to September 2014) accessed on 25.9.14
| SN | CINAHL Search strategy |
| S1 | TX (prematur* OR (extreme* AND premat*) OR prematur* OR low birth weight* OR lbw* OR elbw* OR preterm* OR pre‐term) |
| S2 | TX (parenteral nutrition solutions OR fat emulsions OR intraven* OR parenter* OR i.v. OR infus* OR le) |
| S3 | TX (lipids OR glycerides OR fatty acids OR oils OR soybean oil OR soy* OR coconut* OR borage* OR fish* OR olive* OR intralipid OR ivelip* OR liposyn* OR lipovenoes* OR lipofundin* OR SMOF* OR omegaven* OR clinoleic* OR PFE4501* OR MOFS* OR MOFSLE OR lipoplus* OR omega‐6 OR omega‐3* OR MCT* OR LCT* OR PUFA* OR MUFA* OR polyunsaturated* OR monounsaturated* OR linolenic* OR linoleic* OR docosahexaenoic acid* OR eicosapentaenoic acid* OR DHA OR EPA OR triacylgl* OR triglyc* OR arachidon*) OR (MM "Fat Emulsions, Intravenous") |
| S4 | S1 AND S2 AND S3 |
Limit: Newborns
Total hits: 24
Ovid Nursing Database 1946 to September Week 4 2014 (searched on 25.9.14 via OvidSP)
1. exp infant, newborn/ 2. extrem* prematur*.mp. 3. prematur*.mp. 4. low birth weight*1.mp. 5. premature birth*1.mp. 6. lbw.mp. 7. preterm*1.mp. 8. pre‐term*1.mp. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. lipids/ 11. exp glycerides/ or glyceride*1.mp. 12. exp fatty acids/ or fatty acid*1.mp. 13. exp oils/ or oil*1.mp. 14. exp soybean oil/ or soy* oil.mp. or soy*.mp. 15. (Intralipid*1 or Ivelip or Liposyn or Lipofundin N or omega‐3 or Omega‐6 or n‐6 or n‐3 or olive oil* or ClinOleic or fish oil* or Omegaven or medium chain triglyceride * or MCT oil* or MCT‐LCT oil*1 or LCT‐MCT or Lipovenoes or Lipofundin or Structured lipid* or Structolipid* or SMOF lipid* or multi‐combination lipid* or Lipoplus or Lipidem or borage oil or PFE4501 or triacylgl* or triglyc*).mp. 16. 10 or 11 or 12 or 13 or 14 or 15 17. exp intravenous, infusions/ or intravenous infusion*.mp. 18. exp emulsions/ or emulsion*1.mp. 19. exp parenteral nutrition solutions/ or parenteral nutrition solution*1.mp. 20. intravenous fat emulsion*1.mp. 21. intraven* emulsion*.mp. 22. intraven*.mp. 23. parenter*.mp. 24. infus*.mp. 25. emulsion*.mp. 26. intraven* lipid*.mp. 27. intraven* fat*.mp. 28. 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 29. (9 and 16 and 28) 30.limit 29 to (humans and "all infant (birth to 23 months)")
Limits: humans and "all infant (birth to 23 months)
Total Hits: 64
Maternity and Infant Care 1971 to August 2014 (searched on 25.9.14 via OvidSP)
1. extrem$ prematur$.mp. 2. prematur$.mp. 3. low birth weight$1.mp. 4. premature birth$1.mp. 5. lbw.mp. 6. elbw.mp. 7. preterm$1.mp. 8. pre‐term$1.mp. 9. or/1‐8 10. (intravenous adj infusion$).mp. 11. emuls$.mp. 12. (parenteral adj nutrition adj solution$).ab,ot,ti,kw. 13. intraven$.mp. 14. parenter$.mp. 15. iv.mp. 16. le.mp. 17. infus$.mp. 18. or/10‐17 19. glyceride$1.mp. 20. fat$.mp. 21. oil$.mp. 22. soy$.mp. 23. coconut$.mp. 24. borage$.mp. 25. fish$.mp. 26. olive$.mp. 27. intralipid$.mp. 28. ivelip$.mp. 29. liposyn$.mp. 30. lipovenoes.mp. 31. lipofundin$.mp. 32. SMOF$.mp. 33. omegaven$.mp. 34. clin?oleic$.mp. 35. PFE4501.mp. 36. MOFS$.mp. 37. MOFS$LE$.mp. 38. lipoplus$.mp. 39. (omega adj2 "6").mp. 40. (omega adj2 "3").mp. 41. (LCT adj10 MCT).mp. 42. PUFA$.mp. 43. MUFA$.mp. 44. poly?unsaturat$.mp. 45. mono?unsaturat$.mp. 46. linolenic$.mp. 47. linoleic$.mp. 48. docosa?hexa?noic$.mp. 49. DHA.mp. 50. EPA.mp. 51. eicosapent??noic$.mp. 52. arachidon$.mp. 53. triacylgl$.mp. 54. triglyc$.mp. 55. or/19‐54 56. 9 and 18 and 55 57. limit 56 to (neonatal care adverse outcome or neonatal care complications or "neonatal and infant care" or neonatal intensive care or neonatal care screening)
Limits: Neonatal and infant care
Total hits: 33 (25.9.2014)
International Pharmaceutical Index 1970 to September 2014 (searched on 25.9.14 via OvidSP)
1. extrem$ prematur$.mp. 2. prematur$.mp. 3. low birth weight$1.mp. 4. premature birth$1.mp. 5. lbw.mp. 6. elbw.mp. 7. preterm$1.mp. 8. pre‐term$1.mp. 9. or/1‐8 10. (intravenous adj infusion$).mp. 11. emuls$.mp. 12. (parenteral adj nutrition adj solution$).ab,ot,ti,kw. 13. intraven$.mp. 14. parenter$.mp. 15. iv.mp. 16. le.mp. 17. infus$.mp. 18. or/10‐17 19. glyceride$1.mp. 20. fat$.mp. 21. oil$.mp. 22. soy$.mp. 23. coconut$.mp. 24. borage$.mp. 25. fish$.mp. 26. olive$.mp. 27. intralipid$.mp. 28. ivelip$.mp. 29. liposyn$.mp. 30. lipovenoes.mp. 31. lipofundin$.mp. 32. SMOF$.mp. 33. omegaven$.mp. 34. clin?oleic$.mp. 35. PFE4501.mp. 36. MOFS$.mp. 37. MOFS$LE$.mp. 38. lipoplus$.mp. 39. (omega adj2 "6").mp. 40. (omega adj2 "3").mp. 41. (LCT adj10 MCT).mp. 42. PUFA$.mp. 43. MUFA$.mp. 44. poly?unsaturat$.mp. 45. mono?unsaturat$.mp. 46. linolenic$.mp. 47. linoleic$.mp. 48. docosa?hexa?noic$.mp. 49. DHA.mp. 50. EPA.mp. 51. eicosapent??noic$.mp. 52. arachidon$.mp. 53. triacylgl$.mp. 54. triglyc$.mp. 55. or/19‐54 56. 9 and 18 and 55 57. limit 56 to human
Limits: Human
Total hits: 66 (25.9.2014)
Biological Abstracts 1985 to 2009 (searched on 25.9.14 via OvidSP)
1. extrem$ prematur$.mp. 2. prematur$.mp. 3. low birth weight$1.mp. 4. premature birth$1.mp. 5. lbw.mp. 6. elbw.mp. 7. preterm$1.mp. 8. pre‐term$1.mp. 9. or/1‐8 10. (intravenous adj infusion$).mp. 11. emuls$.mp. 12. (parenteral adj nutrition adj solution$).ab,ot,ti,kw. 13. intraven$.mp. 14. parenter$.mp. 15. iv.mp. 16. le.mp. 17. infus$.mp. 18. or/10‐17 19. glyceride$1.mp. 20. fat$.mp. 21. oil$.mp. 22. soy$.mp. 23. coconut$.mp. 24. borage$.mp. 25. fish$.mp. 26. olive$.mp. 27. intralipid$.mp. 28. ivelip$.mp. 29. liposyn$.mp. 30. lipovenoes.mp. 31. lipofundin$.mp. 32. SMOF$.mp. 33. omegaven$.mp. 34. clin?oleic$.mp. 35. PFE4501.mp. 36. MOFS$.mp. 37. MOFS$LE$.mp. 38. lipoplus$.mp. 39. (omega adj2 "6").mp. 40. (omega adj2 "3").mp. 41. (LCT adj10 MCT).mp. 42. PUFA$.mp. 43. MUFA$.mp. 44. poly?unsaturat$.mp. 45. mono?unsaturat$.mp. 46. linolenic$.mp. 47. linoleic$.mp. 48. docosa?hexa?noic$.mp. 49. DHA.mp. 50. EPA.mp. 51. eicosapent??noic$.mp. 52. arachidon$.mp. 53. triacylgl$.mp. 54. triglyc$.mp. 55. or/19‐54 56. 9 and 18 and 55 57. limit 56 to (human and (neonate or newborn))
Limits: Human ; Newborn
Total Hits: 29
Appendix 4. Details of GRADE ‘Quality of Evidence’ decisions in the review and in the ‘Summary of findings’ tables
ASSESSMENT OF RISK OF BIAS IN A STUDY
| No risk of bias | No critical limitation in any criteria* |
| Moderate risk of bias | Critical limitation in 1 criteria or some limitations in > 1 criteria |
| High risk of bias | Critical limitation in > 1 criteria |
* Criteria for assessing risk of bias in a study: Lack of allocation concealment, lack of blinding, loss to follow up or intention to treat analysis not performed, selective outcome reporting or other limitations.
DECISION MATRIX TO DOWNGRADE FOR 'QUALITY OF STUDIES' IN AN OUTCOME
| Decision to downgrade | Risk of bias across studies for an outcome |
| Do not downgrade | Most information is from studies at low risk of bias |
| Downgrade 1 level | Most information is from studies at moderate risk of bias |
| Downgrade 2 levels | Most information is from studies at high risk of bias |
DECISION MATRIX TO DOWNGRADE FOR 'IMPRECISION' IN AN OUTCOME
|
Decision matrix for imprecision |
CI do not cross null effect |
CI cross null effect but not 0.75 or 1.25 |
CI cross null effect AND cross 0.75 or 1.25 |
| OIS adequate | Do not downgrade | Do not downgrade | Downgrade 1 level |
| OIS inadequate | Downgrade 1 level | Downgrade 1 level | Downgrade 2 levels |
Adequate optimal information size (OIS; empirical) for this review:
a) For categorical variables: "300 or more total events in both groups"
b) For continuous variables: "minimum sample size of 400 participants" as a general approximation
However specific OIS should be calculated if possible, e.g. OIS was calculated to be 500 in each group (total 1000 required) for ventilation duration in comparison of all alternative LE versus S‐LE (for alpha error of 0.05, beta error of 0.2 and decrease in mean ventilation duration by 30%).
CI: confidence interval
DECISION MATRIX TO DOWNGRADE FOR 'INCONSISTENCY' IN AN OUTCOME
|
Decision matrix for inconsistency |
Heterogeneity I2 > 40% (40%‐74%) |
Unexplained high heterogeneity with I2 > 75 % and very low P value |
|
Same direction of effect estimates in the studies |
May not downgrade 1 level if most of the studies have similar point estimates and overlapping CI AND all point estimates are pointing in the same direction. |
Downgrade 1 level |
|
Different direction of effect estimates in the studies |
Downgrade 1 level | Downgrade 2 levels |
(adapted from GRADE working group recommendations;Guyatt 2011)
Data and analyses
Comparison 1. MOFS‐LE versus S‐LE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Death before discharge | 5 | 369 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.68, 2.31] |
| 1.2 Days to regain birth weight | 3 | 234 | Mean Difference (IV, Fixed, 95% CI) | 1.12 [‐0.17, 2.41] |
| 1.3 Rate of weight gain (g/kg/day) | 5 | 347 | Mean Difference (IV, Fixed, 95% CI) | 0.71 [‐0.17, 1.60] |
| 1.4 Bronchopulmonary dysplasia/chronic lung disease | 4 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.70, 1.49] |
| 1.5 Duration of ventilation (days) | 3 | 208 | Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐3.79, 2.60] |
| 1.6 Duration of supplemental oxygen (days) | 2 | 140 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐2.01, 2.95] |
| 1.7 Culture positive sepsis | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.78] |
| 1.8 Any sepsis (clinical and/or culture positive) | 5 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.62, 1.42] |
| 1.9 Necrotising enterocolitis (≥ stage 2) | 4 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.68, 2.67] |
| 1.10 Duration of phototherapy (days) | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐2.57, 2.57] |
| 1.11 Retinopathy of prematurity (≥ stage 3 ) | 3 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.06, 2.85] |
| 1.12 Intraventricular haemorrhage (grade III‐IV) | 3 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.51, 2.04] |
| 1.13 Periventricular leukomalacia | 2 | 176 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.03, 0.03] |
| 1.14 Any patent ductus arteriosus | 3 | 234 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.70, 1.22] |
| 1.15 Significant patent ductus arteriosus requiring treatment | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.52, 1.31] |
| 1.16 Parenteral nutrition associated liver disease/cholestasis | 4 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.29, 2.13] |
| 1.17 Hypertriglyceridaemia | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.61, 1.64] |
| 1.18 Hyperglycaemia | 2 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.27, 3.11] |
| 1.19 Hypoglycaemia | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.68] |
1.1. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 1: Death before discharge
1.2. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 2: Days to regain birth weight
1.3. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 3: Rate of weight gain (g/kg/day)
1.4. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 4: Bronchopulmonary dysplasia/chronic lung disease
1.5. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 5: Duration of ventilation (days)
1.6. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 6: Duration of supplemental oxygen (days)
1.7. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 7: Culture positive sepsis
1.8. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 8: Any sepsis (clinical and/or culture positive)
1.9. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 9: Necrotising enterocolitis (≥ stage 2)
1.10. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 10: Duration of phototherapy (days)
1.11. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 11: Retinopathy of prematurity (≥ stage 3 )
1.12. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 12: Intraventricular haemorrhage (grade III‐IV)
1.13. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 13: Periventricular leukomalacia
1.14. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 14: Any patent ductus arteriosus
1.15. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 15: Significant patent ductus arteriosus requiring treatment
1.16. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 16: Parenteral nutrition associated liver disease/cholestasis
1.17. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 17: Hypertriglyceridaemia
1.18. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 18: Hyperglycaemia
1.19. Analysis.

Comparison 1: MOFS‐LE versus S‐LE, Outcome 19: Hypoglycaemia
Comparison 2. MFS‐LE versus S‐LE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Death before discharge | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.00 [0.25, 99.95] |
| 2.2 Days to regain birth weight | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐3.60, 1.60] |
| 2.3 Rate of weight gain (g/kg/day) | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | ‐1.67 [‐7.01, 3.67] |
| 2.4 Bronchopulmonary dysplasia/chronic lung disease | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [0.42, 4.65] |
| 2.5 Any sepsis (clinical and/or culture positive) | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.31, 4.02] |
| 2.6 Necrotising enterocolitis (≥ stage 2) | 1 | 57 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.07, 0.07] |
| 2.7 Any patent ductus arteriosus | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.57, 1.64] |
| 2.8 Parenteral nutrition associated liver disease/cholestasis | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.32 [0.14, 78.25] |
2.1. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 1: Death before discharge
2.2. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 2: Days to regain birth weight
2.3. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 3: Rate of weight gain (g/kg/day)
2.4. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 4: Bronchopulmonary dysplasia/chronic lung disease
2.5. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 5: Any sepsis (clinical and/or culture positive)
2.6. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 6: Necrotising enterocolitis (≥ stage 2)
2.7. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 7: Any patent ductus arteriosus
2.8. Analysis.

Comparison 2: MFS‐LE versus S‐LE, Outcome 8: Parenteral nutrition associated liver disease/cholestasis
Comparison 3. OS‐LE versus S‐LE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Death before discharge | 3 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.21, 4.82] |
| 3.2 Days to regain birth weight | 3 | 223 | Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐2.00, 1.62] |
| 3.3 Rate of weight gain (g/kg/day) | 2 | 123 | Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐5.15, 4.30] |
| 3.4 Bronchopulmonary dysplasia/chronic lung disease | 4 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.46, 1.04] |
| 3.5 Bronchopulmonary dysplasia/chronic lung disease (sensitivity analysis) | 3 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.57, 1.79] |
| 3.6 Duration of ventilation (days) | 3 | 202 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.67, 1.26] |
| 3.7 Duration of supplemental oxygen (days) | 2 | 102 | Mean Difference (IV, Fixed, 95% CI) | ‐0.76 [‐16.99, 15.47] |
| 3.8 Need for home oxygen therapy | 1 | 64 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.06, 0.06] |
| 3.9 Culture positive sepsis | 2 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.54, 2.78] |
| 3.10 Any sepsis (clinical and/or culture positive) | 5 | 301 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.56, 1.36] |
| 3.11 Necrotising enterocolitis (≥ stage 2) | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.10 [0.13, 73.14] |
| 3.12 Significant jaundice requiring treatment | 2 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.52, 2.07] |
| 3.13 Duration of phototherapy (days) | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐1.08, 0.88] |
| 3.14 Intraventricular haemorrhage (grade III‐IV) | 2 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.10, 2.61] |
| 3.15 Periventricular leukomalacia | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.89] |
| 3.16 Any patent ductus arteriosus | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.63, 1.71] |
| 3.17 Air leaks | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.05, 5.24] |
| 3.18 Parenteral nutrition associated liver disease/cholestasis | 4 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.26, 3.86] |
| 3.19 Hypertriglyceridaemia | 2 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.73] |
| 3.20 Hyperglycaemia | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.22, 4.59] |
3.1. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 1: Death before discharge
3.2. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 2: Days to regain birth weight
3.3. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 3: Rate of weight gain (g/kg/day)
3.4. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 4: Bronchopulmonary dysplasia/chronic lung disease
3.5. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 5: Bronchopulmonary dysplasia/chronic lung disease (sensitivity analysis)
3.6. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 6: Duration of ventilation (days)
3.7. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 7: Duration of supplemental oxygen (days)
3.8. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 8: Need for home oxygen therapy
3.9. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 9: Culture positive sepsis
3.10. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 10: Any sepsis (clinical and/or culture positive)
3.11. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 11: Necrotising enterocolitis (≥ stage 2)
3.12. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 12: Significant jaundice requiring treatment
3.13. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 13: Duration of phototherapy (days)
3.14. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 14: Intraventricular haemorrhage (grade III‐IV)
3.15. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 15: Periventricular leukomalacia
3.16. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 16: Any patent ductus arteriosus
3.17. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 17: Air leaks
3.18. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 18: Parenteral nutrition associated liver disease/cholestasis
3.19. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 19: Hypertriglyceridaemia
3.20. Analysis.

Comparison 3: OS‐LE versus S‐LE, Outcome 20: Hyperglycaemia
Comparison 4. MS‐LE versus S‐LE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Death before discharge | 1 | 60 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.06, 0.06] |
| 4.2 Days to regain birth weight | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [‐1.53, 3.53] |
| 4.3 Rate of weight gain (g/kg/day) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.67 [‐8.20, 2.86] |
| 4.4 Bronchopulmonary dysplasia/chronic lung disease | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.28, 3.63] |
| 4.5 Any sepsis (clinical and/or culture positive) | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.00 [0.67, 5.94] |
| 4.6 Necrotising enterocolitis (≥ stage 2) | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.00 [0.25, 99.95] |
| 4.7 Any patent ductus arteriosus | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.70, 1.82] |
| 4.8 Parenteral nutrition associated liver disease/cholestasis | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.00 [0.13, 70.83] |
| 4.9 Hypertriglyceridaemia | 1 | 12 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.27, 0.27] |
4.1. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 1: Death before discharge
4.2. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 2: Days to regain birth weight
4.3. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 3: Rate of weight gain (g/kg/day)
4.4. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 4: Bronchopulmonary dysplasia/chronic lung disease
4.5. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 5: Any sepsis (clinical and/or culture positive)
4.6. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 6: Necrotising enterocolitis (≥ stage 2)
4.7. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 7: Any patent ductus arteriosus
4.8. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 8: Parenteral nutrition associated liver disease/cholestasis
4.9. Analysis.

Comparison 4: MS‐LE versus S‐LE, Outcome 9: Hypertriglyceridaemia
Comparison 8. All fish oil containing LE versus S‐LE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Death before discharge | 5 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.69, 2.35] |
| 8.2 Days to regain birth weight | 3 | 261 | Mean Difference (IV, Fixed, 95% CI) | 0.81 [‐0.43, 2.05] |
| 8.3 Rate of weight gain (g/kg/day) | 5 | 374 | Mean Difference (IV, Fixed, 95% CI) | 0.69 [‐0.19, 1.57] |
| 8.4 Bronchopulmonary dysplasia/chronic lung disease | 4 | 341 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.70, 1.50] |
| 8.5 Duration of ventilation (days) | 3 | 208 | Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐3.79, 2.60] |
| 8.6 Duration of supplemental oxygen (days) | 2 | 140 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐2.01, 2.95] |
| 8.7 Culture positive sepsis | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.78] |
| 8.8 Any sepsis (clinical and/or culture positive) | 5 | 373 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.61, 1.39] |
| 8.9 Necrotising enterocolitis (≥ stage 2) | 4 | 341 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.65, 2.57] |
| 8.10 Duration of phototherapy (days) | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐2.57, 2.57] |
| 8.11 Retinopathy of prematurity (≥ stage 3) | 3 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.06, 2.85] |
| 8.12 Intraventricular haemorrhage (grade III‐IV) | 3 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.51, 2.04] |
| 8.13 Periventricular leukomalacia | 2 | 176 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.03, 0.03] |
| 8.14 Any patent ductus arteriosus | 3 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.72, 1.21] |
| 8.15 Significant patent ductus arteriosus requiring treatment | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.52, 1.31] |
| 8.16 Parenteral nutrition associated liver disease/cholestasis | 4 | 341 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.29, 2.16] |
| 8.17 Hypertriglyceridaemia | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.61, 1.64] |
| 8.18 Hyperglycaemia | 2 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.27, 3.11] |
| 8.19 Hypoglycaemia | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.68] |
8.1. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 1: Death before discharge
8.2. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 2: Days to regain birth weight
8.3. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 3: Rate of weight gain (g/kg/day)
8.4. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 4: Bronchopulmonary dysplasia/chronic lung disease
8.5. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 5: Duration of ventilation (days)
8.6. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 6: Duration of supplemental oxygen (days)
8.7. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 7: Culture positive sepsis
8.8. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 8: Any sepsis (clinical and/or culture positive)
8.9. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 9: Necrotising enterocolitis (≥ stage 2)
8.10. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 10: Duration of phototherapy (days)
8.11. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 11: Retinopathy of prematurity (≥ stage 3)
8.12. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 12: Intraventricular haemorrhage (grade III‐IV)
8.13. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 13: Periventricular leukomalacia
8.14. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 14: Any patent ductus arteriosus
8.15. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 15: Significant patent ductus arteriosus requiring treatment
8.16. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 16: Parenteral nutrition associated liver disease/cholestasis
8.17. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 17: Hypertriglyceridaemia
8.18. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 18: Hyperglycaemia
8.19. Analysis.

Comparison 8: All fish oil containing LE versus S‐LE, Outcome 19: Hypoglycaemia
Comparison 9. All alternative LE versus S‐LE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Death before discharge | 7 | 623 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.66, 2.07] |
| 9.2 Days to regain birth weight | 5 | 484 | Mean Difference (IV, Fixed, 95% CI) | 0.53 [‐0.52, 1.58] |
| 9.3 Rate of weight gain (g/kg/day) | 6 | 497 | Mean Difference (IV, Fixed, 95% CI) | 0.68 [‐0.19, 1.55] |
| 9.4 Bronchopulmonary dysplasia/chronic lung disease | 7 | 602 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.63, 1.12] |
| 9.5 Duration of ventilation (days) | 6 | 410 | Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐1.60, 1.06] |
| 9.6 Duration of supplemental oxygen (days) | 4 | 242 | Mean Difference (IV, Fixed, 95% CI) | 0.44 [‐2.01, 2.89] |
| 9.7 Need for home oxygen therapy | 1 | 64 | Risk Difference (M‐H, Fixed, 95% CI) | 0.00 [‐0.06, 0.06] |
| 9.8 Culture positive sepsis | 3 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.52, 2.26] |
| 9.9 Any sepsis (clinical and/or culture positive) | 9 | 674 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.66, 1.23] |
| 9.10 Necrotising enterocolitis (≥ stage 2) | 4 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.67, 2.67] |
| 9.11 Significant jaundice requiring treatment | 2 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.52, 2.07] |
| 9.12 Duration of phototherapy (days) | 2 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐1.00, 0.83] |
| 9.13 Retinopathy of prematurity (≥ stage 3) | 3 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.06, 2.85] |
| 9.14 Intraventricular haemorrhage (grade III‐IV) | 5 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.48, 1.70] |
| 9.15 Periventricular leukomalacia | 3 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.89] |
| 9.16 Any patent ductus arteriosus | 3 | 320 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.75, 1.23] |
| 9.17 Significant patent ductus arteriosus requiring treatment | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.52, 1.31] |
| 9.18 Air leaks | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.05, 5.24] |
| 9.19 Parenteral nutrition associated liver disease/cholestasis | 7 | 602 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.37, 1.86] |
| 9.20 Hypertriglyceridaemia | 4 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.59, 1.54] |
| 9.21 Hyperglycaemia | 3 | 176 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.37, 2.46] |
| 9.22 Hypoglycaemia | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.68] |
9.1. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 1: Death before discharge
9.2. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 2: Days to regain birth weight
9.3. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 3: Rate of weight gain (g/kg/day)
9.4. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 4: Bronchopulmonary dysplasia/chronic lung disease
9.5. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 5: Duration of ventilation (days)
9.6. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 6: Duration of supplemental oxygen (days)
9.7. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 7: Need for home oxygen therapy
9.8. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 8: Culture positive sepsis
9.9. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 9: Any sepsis (clinical and/or culture positive)
9.10. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 10: Necrotising enterocolitis (≥ stage 2)
9.11. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 11: Significant jaundice requiring treatment
9.12. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 12: Duration of phototherapy (days)
9.13. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 13: Retinopathy of prematurity (≥ stage 3)
9.14. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 14: Intraventricular haemorrhage (grade III‐IV)
9.15. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 15: Periventricular leukomalacia
9.16. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 16: Any patent ductus arteriosus
9.17. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 17: Significant patent ductus arteriosus requiring treatment
9.18. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 18: Air leaks
9.19. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 19: Parenteral nutrition associated liver disease/cholestasis
9.20. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 20: Hypertriglyceridaemia
9.21. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 21: Hyperglycaemia
9.22. Analysis.

Comparison 9: All alternative LE versus S‐LE, Outcome 22: Hypoglycaemia
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beken 2014.
| Study characteristics | ||
| Methods | Single centre randomised controlled study done in neonatal intensive care unit of Dr Sami Ulus Maternity and Children Research Centre in Ankara, Turkey. Study enrolment: 1st January 2013 to 31st July 2013 I. Allocation concealment ‐ yes II. Blinding of intervention ‐ can't tell III. Blinding of outcome measurement(s) ‐ yes (for ROP) IV. Complete follow‐up ‐ yes |
|
| Participants | Inclusion criteria: < 1500 g and < 32 weeks gestation. Exclusion criteria: Major congential abnormalities, congential infections and metabolic errors. |
|
| Interventions | 80 infants were randomly assigned to two groups: 1) Group 1 (n = 40): 20% SMOFlipid 2) Group 2 (n = 40): 20% Intralipid® TPN was started with IV glucose and amino acid solution (1 g/kg) on the first day of life. The lipid emulsions were administered from day 1 as a continuous infusion for 24 hour per day. The initial lipid daily dose was 0.5 g/kg/day if the birth weight was < 1000 g and was 1 g/kg/day if the birth weight was > 1000 g. Lipids were increased by 0.5 to 1.0 g/kg every 24 hours to a maximum of 3 g/kg/day. Infants in both arms also received trace elements, water and lipid soluble vitamins as a standard part of the TPN protocol. Both groups were started on enteral feeds with DHA enriched preterm formula or breast milk. |
|
| Outcomes | Primary outcome: ROP Secondary outcomes: Cholestasis, nosocomial infections, NEC, CLD and mortality. Laboratory data including complete blood count, triglyceride levels, and liver and kidney function tests were recorded. |
|
| Notes | 1. Funding: None revealed. 2. DHA levels were not done in the two groups. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomly assigned to one of the two groups by balanced blocks using sealed envelopes. Stratification was not included in the block design." Comment: Method of random sequence generation is not described. |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomly assigned to one of the two groups by balanced blocks using sealed envelopes. Group assignment was made by the investigator (last author) who was not involved in the care of the infants." "A member of the TPN team who was blinded and not involved in the care of infants followed orders from the sealed envelope prepared by the investigators." Comment: The review authors decided by consensus that the risk was low. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Follow‐up was complete. |
| Selective reporting (reporting bias) | Low risk | Comment: The trial was registered with ClinicalTrials.gov under Identifier: NCT01875510 and there appears to be no deviation from the protocol. Study started on 1st January 2013, however the protocol was registered on May 31st 2013. The review authors decided by consensus that the risk was probably low for selective reporting. |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Nurses and doctors responsible for the infants were also blinded to the group assignment." Comment: How the blinding was achieved is not described, therefore the risk is unclear. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All fundus examinations were performed by the same paediatric ophthalmologist who was blinded to the group assignment" Comment: Probably done (decision by consensus between VK and MM). |
D'ascenzo 2014.
| Study characteristics | ||
| Methods | Premature neonates were recruited from the NICU at the Salesi Children’s Hospital, Rome, Italy, between January 2008 and December 2012. I. Allocation concealment ‐ yes II. Blinding of intervention ‐ yes III. Blinding of outcome measurement(s) ‐ yes IV. Complete follow‐up ‐ yes |
|
| Participants | Inclusion criteria: Preterm infants (birth weight 500‐1249 g). Exclusion criteria: Severe congenital malformations or no consent. |
|
| Interventions | 80 premature infants were randomised in 1:1:1:1 ratio to receive either SMOFlipid® or Intralipid® at rate of either 3.5 g/kg/day or 2.5 g/kg/day in 4 groups: 1) MOFS‐LE 2.5 (n = 21): MOFS‐LE (30% soybean oil, 30% medium‐chain triglycerides, 25% olive oil, 15% fish oil), SMOFlipid® Fresenius Kabi. 2) MOFS‐LE 3.5 (n = 18): MOFS‐LE (30% soybean oil, 30% medium‐chain triglycerides, 25% olive oil, 15% fish oil), SMOFlipid® Fresenius Kabi. 3) S‐LE 2.5 (n = 22): S‐LE (100% soybean oil), Intralipid® Fresenius Kabi. 4) S‐LE 3.5 (n = 19): S‐LE (100% soybean oil), Intralipid® Fresenius Kabi. |
|
| Outcomes | Primary outcome: Plasma phospholipid and DHA (mol%) on postnatal day 7. Secondary outcome: On postnatal day 7 and 14, levels of plasma fatty acids and plasma lipid concentration, triglyceride levels, free cholesterol and cholesterol esters. Other outcomes reported: Death and clinical outcomes. |
|
| Notes | Funding source: None revealed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "At birth, the caring neonatologist randomised the study infants by a simple randomisation method (sealed envelope system)." Comment: Probably done as the previous reports involving the same team has mentioned it in their previous report: "Randomization was obtained with sealed envelopes using a random permuted blocks within strata protocol" (decision by consensus between the review authors). |
| Allocation concealment (selection bias) | Low risk | Quote: "sealed envelope system." Comment: Low risk of bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Follow‐up was complete.. |
| Selective reporting (reporting bias) | Unclear risk | Quote: "The trial was conducted between January 2008 and December 2012 so we had not registered it in a public trials registry as it is now required for trials that started after July 2008." Comment: Study protocol was not available to us so we can not ascertain any deviation from the protocol. |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The PN bags containing the study lipid emulsion were of the same size and of identical appearance. Both the caregivers involved with data collection and the laboratory personnel were blind to group assignment." Comment: Probably done. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The PN bags containing the study lipid emulsion were of the same size and of identical appearance. Both the caregivers involved with data collection and the laboratory personnel were blind to group assignment." Comment: Probably done. |
Demirel 2011.
| Study characteristics | ||
| Methods | Randomised prospective study in VLBW preterms in a single centre conducted at NICU at Zekai Tahir Burak Maternity Teaching Hospital in Turkey. Study enrolment from January 2010 to October 2010. I. Allocation concealment ‐ cannot tell II. Blinding of intervention ‐ no III. Blinding of outcome measurement(s) ‐ no IV. Complete follow‐up ‐ yes (however deaths were excluded) |
|
| Participants | Inclusion criteria: preterm infants ≤ 32 weeks gestation and receiving ≥ 40% parenteral calories at 14th day of life. Exclusion criteria: metabolic disorders, congenital anomalies, severe unconjugated hyperbilirubinaemia, using medications in competition with bilirubin, birth asphyxia and death within 14 days of life. |
|
| Interventions | The infants were randomised to receive either: 1) ClinOleic® (n = 20) OR 2) Intralipid® (n = 20) TPN protocol: Lipid emulsion was started on day 2 of life at 1 g/kg/day and increased daily by 1g/kg/day to 3 g/kg/day (24 hour infusion). Amino acids were given as Primene® 10% besides glucose, electrolytes and vitamins. Enteral feeding started on day 2, lipids started on day 2. |
|
| Outcomes | Main outcome measures: Plasma lipid concentrations and acyl carnitine profile. Other outcomes: Gestational age, birth weight, sex, APGAR scores, day 14 weight, RDS, ROP and sepsis. No data provided for NEC and BPD. Liver function tests (ALT, AST, GGT), lipid profile, and carnitine levels were recorded. |
|
| Notes | Authors postulated that higher levels of hexanoyl carnitine reflecting defective mitochondrial transport of hexanoyl may lead to immunosuppression which may be the cause of higher sepsis risk in the Intralipid® group (hexanoyl carnitine levels 2.18 ± 2.10 in Group I (Intralipid®) and 0.38 ± 0.12 μM in Group II (ClinOleic®); P value 0.005). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using computer‐generated randomisation sequence." Comment: Probably done. |
| Allocation concealment (selection bias) | Unclear risk | Comment: The details of allocation concealment have not been mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Outcomes were reported for all included participants. |
| Selective reporting (reporting bias) | Unclear risk | Comment: Study protocol is not available to us so we can not ascertain any deviation from the protocol. Also, data were not provided for outcomes of NEC and BPD which have been reported as "statistically insignificant between the groups" (data for these outcomes could not be used in meta‐analyses). |
| Other bias | High risk | Quote: "The major limitation of our study was based on the randomisation method based on per protocol. We analysed the patients that fulfil the inclusion criteria at the 14th day of life." "Only patients who were receiving 40% of calories parenterally at Day 14 were included in the study. Those who died were also excluded from the study. This methodology can introduce problems with randomisation design and serious bias". Comment: Possibly high risk. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: Not a blinded study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: Not a blinded study. |
Deshpande 2009.
| Study characteristics | ||
| Methods | Double blind randomised controlled trial done at the department of neonatal paediatrics at KEM Hospital in Perth, Western Australia. Study enrolment from November 2006 to August 2007. I. Allocation Concealment ‐ yes II. Blinding of intervention ‐ yes III. Blinding of outcome measurement(s) ‐ yes IV. Complete follow‐up ‐ yes |
|
| Participants | Inclusion criteria: preterm infants < 28 weeks who were < 7 days at recruitment with parenteral nutrition accounting for > 75% of energy intake. Exclusion criteria: major congenital malformations, inborn errors of metabolism, transfusion before baseline bloods could be taken, exchange transfusion for hyperbilirubinaemia or lipid emulsion given before enrolment. Withdrawal: Enteral nutrition > 25% at any time. |
|
| Interventions | Total of 50 infants were randomised; the detailed results were available for 45 infants (24 infants in ClinOleic® group; 21 in Intralipid® group) OS‐LE vs S‐LE. 1) ClinOleic® (n = 25) 2) Intralipid® (n = 25) TPN protocol: The amino acids were added on day 1 and lipids added on day 2 in increments of 0.5, 1 , 2, 3 g/kg/day every day for 4 consecutive days. The lipid emulsion was in coded amber coloured syringes. The lipid infusion was given for 20 hours per day. The bloods were done 2 hours after stopping the lipid infusion. |
|
| Outcomes | The primary outcomes of the study were: a) Plasma F2‐isoprostane levels as indicators of lipid peroxidation. b) Levels of long chain polyunsaturated fatty acids in plasma and in RBC membrane. The secondary outcomes were: a) Safety outcomes ‐ liver and renal function tests, blood culture positive sepsis, blood cell counts. b) Total enteral nutrition and PN. c) Anthropometry |
|
| Notes | 1. Funding: Study was partly funded by research grant from Baxter Healthcare Australia and this funding was used for cost of laboratory assays and fat emulsions. Baxter health had no involvement in study design, data analysis or manuscript preparation. 2. One death on day 3 due to IVH in the olive oil group and shown in study diagram. Two more deaths occurred due to respiratory failure during the study period however information regarding which group these patients belonged to was not available. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"The coordinating pharmacist who was not directly involved in the management of patients performed block randomisation using a computer‐generated code." Comment: Probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "The coordinating pharmacist who was not directly involved in the management of patients performed block randomisation using computer‐generated code." "lipid emulsions were dispensed in coded and amber‐coloured (light protected) syringes." Comment: Probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "One participant in the OL group died on day 2 (grade IV IVH) but was included in the analysis on intention to treat basis; however, there was no blood sample on day 6 for the patient." Comment: Two more deaths occurred due to respiratory failure during the study period however information regarding which group these patients belonged to was not available. There was 1 patient in the ClinOleic® group and 4 patients in the Intralipid® group who were withdrawn from the study due to enteral energy intake > 25%. Their data is not available. Probably low risk. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we can not ascertain any deviation from the protocol. The data on outcomes of sepsis and weight were not available (could not be used in meta‐analysis). |
| Other bias | Low risk | Comment: No other biases identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The lipid emulsions were dispensed in coded and amber‐coloured (light protected) syringes." Comment: The blinding of participants and personnel is acceptable in this study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote:"The data were analysed without breaking the code to ensure masking of statistical analysers" Comment: Probably done. |
Gawecka 2008.
| Study characteristics | ||
| Methods | Single centre study done at NICU of Medical Academy Neonatology Department in Warsaw, Poland in 44 preterm infants. Study enrolment: March 2004 to September 2005. I. Allocation Concealment ‐ yes II. Blinding of intervention ‐ yes III. Blinding of outcome measurement(s) ‐ yes IV. Complete follow‐up ‐ yes |
|
| Participants | Inclusion criteria: preterm infants < 32 week gestation with a birth weight of < 1500 g, admitted to ICU on day 1 and requiring PN. Exclusion criteria: Severe malformations, metabolic disease, congenital infection with positive blood culture, enteral calories > 25%. |
|
| Interventions | Infants received either (initially 44 infants at the enrolment stage): 1) 20% ClinOleic® (n = 18) OR 2) soybean‐based LE, 20% Ivelip® (n = 20) PN protocol: PN started on day 1 with amino acids. The LE was started within 72 hours of life from a dose of 1 g/kg/day and was increased to the maximal dose of 3‐3.5 g/kg/day. Lipids were infused continuously over 24 hours. Blood sampling was done at baseline and after 14 days of lipid infusion. Follow up: All infants were followed up till discharge. |
|
| Outcomes | Primary outcome: Tumour necrosis factor–α, IL‐6, and IL‐10 synthesis in un‐stimulated and anti‐CD3 induced peripheral blood mononuclear cells of parenterally fed premature infants. Secondary outcomes: Incidence of BPD, ROP, NEC, IVH, and nosocomial infections in the two groups. | |
| Notes | Study showed no difference in the inflammatory cytokines or clinical parameters in the two groups. LDL cholesterol was significantly higher in olive oil group. No funding source has been mentioned. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The randomisation was done by a hospital pharmacist." Comment: Details of random sequence generation have not been provided. |
| Allocation concealment (selection bias) | Low risk | Quote: "Investigators, parents, and nursing staff were unaware of the treatment allocation," "The randomisation was done by a hospital pharmacist." Commnets: Probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Of the 44 recruited infants, 38 (87%) completed the study, 18 in the olive oil group and 20 in the soy oil group. 2 deaths occurred in each group due to pulmonary complications (balanced in two groups and for the same reason). Two more infants were excluded but the group allocation was not mentioned. Intention to treat analysis was not done. Authors' consensus was that material risk of bias was probably low. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we cannot ascertain any deviation from the protocol. The study report did not provide data on IVH (mentioned as not significantly different in the two groups). |
| Other bias | Low risk | None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "randomised with double‐blind method," "randomisation code was broken after the data analysis was performed." "The parenteral lipid emulsion was prepared by the pharmacist." "fat emulsion was administered in a syringe with 'lipids'" (from the article in Polish). Comment: Probably done. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "randomisation code was broken after the data analysis was performed" Comment: Probably done. |
Gobel 2003.
| Study characteristics | ||
| Methods | Double blind randomised study at two NICU in Munich The randomisation was stratified for study centre and birth weight (< 1,250 g and > 1,250 g). I. Allocation concealment ‐ cannot tell II. Blinding of intervention ‐ cannot tell III. Blinding of outcome measurement(s) ‐ cannot tell IV. Complete follow‐up ‐ no Safety analysis was performed on the intention‐to‐treat population (42 treated infants including dropouts), efficacy analysis was performed on the per‐protocol population (33 infants treated for 7 days). |
|
| Participants | Inclusion criteria: Preterm infants with gestation range of 28 weeks to < 37 weeks with admission to NICU within 24 hours of birth and PN providing ≥ 80% calories during the study. Exclusion criteria: Severe malformations, inborn error of metabolism, jaundice before randomisation, hyperlipidaemia, bacterial infection and transfusion of packed red blood cells and/or fresh frozen plasma of more than 15 mL/kg (cumulative volume) before baseline blood sampling. |
|
| Interventions | Randomised (n = 45) within 72 hours of life to receive: 1) OS‐LE (20% ClinOleic®) n = 24 2) S‐LE (Intralipid 20%®) n = 21 LE was started within 72 hours of birth, given as 24 hour infusions at doses of 0.5, 1.0, and 2.0 g/kg/day on the first 3 consecutive study days and 2 g/kg/day for the next 4 days. The rest of the TPN co‐interventions were the same in the two groups. Vitamin E was not given, minimal enteral nutrition was provided and infants were excluded if the enteral calories exceeded 20% at any time. |
|
| Outcomes | Outcomes included levels of triglycerides, cholesterol, phospholipids. Clinical outcomes included hyperbilirubinaemia, bradycardia, apnoea and gastro‐oesophageal reflux. The study reported no serious adverse events in any group. Efficacy outcomes were evaluated in per protocol patients on day 0 and day 8 which included proportions of plasma phospholipid fatty acids, alpha tocopherol levels, and urine malondialdehyde excretion. |
|
| Notes | The study was supported by Baxter. Some of authors were affiliated with Baxter research and development centre. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Method of random sequence generation is not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Details of allocation concealment are not provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Initially 45 infants were randomised; 3 infants did not fit inclusion criteria and 9 were excluded as enteral intake exceeded 20%. Intention to treat analysis was done for safety outcomes (including the excluded infants) for initially randomised patients. For this review, the only outcome of interest was hyperbilirubinaemia which was a safety variable. Overall taking all these factors into account, the study was graded as being at low risk of bias. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we can not ascertain any deviation from the protocol. |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "After the study was completed and the database locked, the blind code was opened." Comment: The authors have not mentioned how blinding was achieved. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "After the study was completed and the database locked, the blind code was opened." Comment: The authors have not mentioned how blinding was achieved. |
Koksal 2011.
| Study characteristics | ||
| Methods | Single centre blinded randomised trial in 64 preterm infants done at NICU in Division of Neonatology, Görükle, Bursa, Turkey. Study enrolment: September 2005‐December 2009 I. Allocation concealment ‐ yes II. Blinding of intervention ‐ cannot tell III. Blinding of outcome measurement(s) ‐ cannot tell IV. Complete follow‐up ‐ yes |
|
| Participants | Inclusion criteria: ≤ 34 weeks, admission to NICU within 24 h after birth, and TPN requirement expected to be ≥ 80% of the total energy intake during the study. Exclusion criteria: Severe malformations, hyperlipidaemia, metabolic disease, enteral nutrition > 20 ml/kg/day and transfusion > 15 ml/kg/day. |
|
| Interventions | Infants were randomised to receive either: 1) 20% ClinOleic® (OS‐LE) (n = 32) OR 2) 20% Intralipid® (S‐LE) (n = 32) LE was started within 72 h after the baseline blood sample was obtained. LE was infused at 1, 2, 3 g/kg/day on first 3 days and 3 g/kg/day over the next 4 days in both groups. After 7 days of LE, infusion was stopped and blood samples taken after 6 hours. Study endpoint was day 7 for total anti‐oxidant capacity (primary outcome). The secondary clinical outcomes have been reported until discharge. |
|
| Outcomes | Primary outcome: To evaluate the total anti‐oxidant capacity in both lipid emulsions at day 7 (not significantly different between groups) Secondary outcomes: To assess neonatal morbidity and the biochemical indices after LE administration. The biochemical indices were also compared at day 7. The neonatal morbidities have been reported till discharge (including ROP, BPD, IVH, NEC, RDS and sepsis). |
|
| Notes | 1. No source of funding has been stated. 2. No growth outcomes were provided in the study report, however these were provided by the study authors on request. 3. Unpublished data were provided by the authors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Block randomisation was performed using a computer‐generated code." Comment: Probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "The coded emulsion was prepared and labelled by the blinded clinical pharmacist." Comment: Probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Outcomes have been reported for all participants. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we cannot ascertain any deviation from the protocol. |
| Other bias | Unclear risk | Comment: This study contributed to high heterogeneity in the outcomes of ventilation duration and duration of oxygen therapy (standard deviation data were confirmed by authors). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Randomly assigned in a double‐blind manner," "The coded emulsion was prepared and labelled by the blinded clinical pharmacist." Comment: The authors have not provided details of how blinding was achieved. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "Parents, trial physicians and clinical staff were blinded to the lipid content of the TPN." Comment: The authors have not provided details of how blinding was achieved. |
Lehner 2006.
| Study characteristics | ||
| Methods | Single centre randomised controlled study in 12 preterm infants done (initially 15 infants enrolled) at the Division of Neonatology at the University of Pécs, Hungary. I. Allocation concealment ‐ can't tell II. Blinding of intervention ‐ can't tell III. Blinding of outcome measurement(s) ‐ can't tell IV. Complete follow‐up ‐ no |
|
| Participants | Inclusion criteria: 25‐37 week preterm infants with weight < 3 kg with requirement of LE within 48 hours with expected enteral calorie intake < 20%. Exclusion criteria: Known metabolic diseases. |
|
| Interventions | Infants were randomised to receive either S‐LE or MS‐LE. 15 infants were enrolled, with 3 withdrawals (all from the MS‐LE group) leaving 6 infants in each group. 1) S‐LE (Lipofundin N 20%®, n = 6 ) 2) MS‐LE emulsion (Lipofundin® MCT 20%, n = 6) Co‐interventions with 10% glucose, amino acids, electrolytes (sodium chloride, potassium chloride, calcium gluconate), trace elements (Pedel®; Pharmacia, Budapest, Hungary), and water‐soluble vitamins (Soluvit®; Baxter) were the same in both groups. |
|
| Outcomes | Intended outcomes of the study were plasma fatty acid profile, plasma cholesterol level and hypertriglyceridaemia. However the study reported some clinical outcomes, i.e. weight on day 8. The study reported faster regain of birth weight in the MS‐LE group, however no data were available. | |
| Notes | 1. No episodes of hypertriglyceridaemia in both groups. The outcomes are reported for 8 days. 2. Funding: The study was financially supported by B Braun besides financial support from Deutsche Forschungsgemeinschaft and Child Health Foundation (Munich, Germany). 3. The study is primarily a biochemical study with some clinical outcomes reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "randomised double blind trial." Comment: Method of random sequence generation not mentioned. Initially there were 9 infants in the MS‐LE group and 6 infants in the S‐LE group. One infant was reported to have the wrong randomisation. Details regarding the wrong randomisation have not been provided. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Method of allocation concealment is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Initially 15 infants were randomised with 3 infants excluded (all from the MS‐LE group; unbalanced exclusions; 33% in one group), giving 6 infants in each arm. Reasons for exclusion were provided (wrong randomisation, breaching of the study conditions, and contraindication to the feeding protocol ‐ one infant each). |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we cannot ascertain any deviation from the protocol. |
| Other bias | Unclear risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "randomised double blind trial." Comment: No details were provided regarding how blinding was achieved. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Mentioned "randomised double blind trial" Comment: No details were provided regarding how blinding was achieved. The study does not report whether there was blinding of the outcome. |
Rayyan 2012.
| Study characteristics | ||
| Methods | Double blind randomised controlled study done at a single centre at the Department of Neonatology, University Hospitals, Leuven, Belgium. Enrolment period: November 2004 to February 2006. I. Allocation concealment ‐ yes II. Blinding of intervention ‐ yes III. Blinding of outcome measurement(s) ‐ yes IV. Complete follow‐up ‐ yes Study duration: 15 days or until last IV infusion. The main study period was until day 7 of treatment; all subjects were followed up until discharge. For statistical analysis the last value was carried forward. Adverse events were reported until 6 days after the end of last infusion. |
|
| Participants | Inclusion criteria: Under 34 weeks gestation preterm infants with weight of 500‐2000 g, who received PN for at least 7 days. Exclusion criteria: Extremely premature infants, severe congenital malformations, heart failure, organ damage ‐ anuria, haemolytic disease, thrombocytopenia, oxygen saturations < 80% for more than 2 hours, severe acidosis, use of catecholamines, hypoxic‐ischemic encephalopathy, and multi‐organ failure. |
|
| Interventions | Preterm infants (n = 53) were randomised to receive either: 1) 20% SMOFlipid® (n = 26) 2) 20% Intralipid® (n = 27) LE were given for at least 7 days and up to 14 days, peripherally or centrally. Enteral intake was allowed as per protocol, i.e. < 30% of the total lipid intake on days 1‐3, < 50% on days 4‐7, and <70% on days 8‐14 of the total energy intake was permitted. The daily target dosage of fat started at 1.0 g/kg BW/d on days 1–3 and was increased to 2 g/kg/day on day 4, 3 g/kg BW/d on day 5, and 3.5 g/kg/day from day 6 on. Other components of PN were given as standardised solutions at the discretion of the investigator. |
|
| Outcomes | Primary safety outcome ‐ triglyceride levels, until day 8 Primary efficacy outcome ‐ change in body weight at day 8 from baseline. Secondary outcomes ‐ blood counts and biochemical parameters. Clinical assessments (heart rate, temperature, blood pressure, body weight, oxygen therapy) were performed daily from day 0 (pre‐study visit) until study termination, either on day 15 or following the last infusion of study treatment (post‐treatment). |
|
| Notes | Financial disclosure: The clinical research is supported by the Fund for Scientific Research, Flanders (Belgium) J a Fundamxntal Clinical Investigatorship (1 800209 N) and a research grant (1506409 N). The study was sponsored by Fresenius Kabi, Bad Homburg, Germany. Authors: Hugo Devlieger and Frank Jochum have received speaking honoraria and consulting fees from Fresenius Kabi. The publication of the supplement in which this article appears is sponsored by Nestlé Nutrition Institute. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "using the software RANCODE," "The randomisation was stratified by weight‐ 500‐1000, 1000‐1500, 1501‐2000 g" Comment: Probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization list was prepared prior to the study and lipid emulsion dispensed by pharmacy." Comment: Probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Protocol violations/premature discontinuation occurred only in 3 participants in the SMOFlipid® group and in 4 participants in the Intralipid® group (balanced in both groups). The trial profile and participant flow is well described. All outcome data are provided. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we can not ascertain any deviation from the protocol. Data could not be used for sepsis (it was reported as a combined outcome of infection and infestations). |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Double blind controlled," " ...the study and control infusions were of the same size and identical appearance," "Infusions were prepared in the hospital pharmacy identified only by the patient number on the outside of packaging." Comment: Probably done. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: Probably done. The review authors agreed that the risk is low. |
Rubin 1994.
| Study characteristics | ||
| Methods | Double blind randomised controlled study done at Beilinson Medical Center, Petach‐Tiqva, Israel. Results regarding fatty acid profile from this study were published in 1995 (Rubin 1995). Enrolment period: not mentioned. I. Allocation Concealment ‐ cannot say II. Blinding of intervention ‐ cannot say III. Blinding of outcome measurement(s) ‐ cannot say IV. Complete follow‐up ‐ no |
|
| Participants | Preterm infants < 35 weeks who received TPN for ≥ 6 days. A total of 59 infants were enrolled during the study period. | |
| Interventions | Preterm infants (initially 59 infants enrolled with 10 withdrawals) who were randomised to receive either: 1) 20% PFE 4501® (soy + borage oil in 8.5:1.5 ratio to increase GLA + added carnitine; n = 16) OR 2) 20% Intralipid® (S‐LE; n = 18) OR 3) 20% Lipofundin MCT® (MS‐LE; LCT from soy: MCT from coconut in 1:1 weight ratio; n = 15) Lipid emulsion: Day 1: 0.5 g/kg/day, day 2: 1.5 g/kg/day to a maximum of 2.5 g/kg/day on day 3, and this dose was maintained until the end of the study period. Co‐interventions with amino acid solution (Vamin) and electrolytes were similar in the two groups. |
|
| Outcomes | Similar weight gain, clinical variables, acid‐base, blood counts, glucose levels (remained normal) mentioned in all the groups. AST decreased significantly in groups 2 and 3 from baseline, however the values were only provided for triglyceride levels. The fatty acid profile is reported in detail from the same study in Rubin 1995. | |
| Notes | Triglycerides levels (mean ± SD) have been reported but authors have not reported the proportion of infants with hypertriglyceridaemia. Therefore we were not able to include any data in the quantitative synthesis for the clinical outcomes. It was a short study of 6 days duration. Authors demonstrated the safety of LE in jaundiced babies as the bilirubin levels fell in both groups despite the rise in free fatty acids as reported in Rubin 1995. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The infant were randomly assigned to..." Comment: No information on random sequence generation provided. |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information on allocation concealment was provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 10 withdrawals in the study equivalent to 16% of the study sample. Withdrawals were for varying reasons including sepsis (5), hyperbilirubinaemia (1), and thrombocytopenia (2). It is not reported which intervention arm these infants belonged to. Data from these patients is not available. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we can not ascertain any deviation from the protocol. |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "randomly assigned in a double blind manner" Comment: How blinding was achieved has not been described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "randomly assigned in a double blind manner" Comment: How blinding was achieved has not been described. |
Savini 2013.
| Study characteristics | ||
| Methods | Double blind single‐centre 5‐arm RCT in NICU of “G. Salesi” Children’s Hospital, Ancona, Italy. Study enrolment period: January 2007 to October 2011. I. Allocation Concealment ‐ yes II. Blinding of intervention ‐ yes III. Blinding of outcome measurement(s) ‐ yes IV. Complete follow‐up ‐ yes Study duration: Primary study criteria including phytosterol until day 21, but clinical outcomes have been reported beyond that period (e.g. liver enzymes and cholestasis at 6 weeks). Follow‐up: All study participants appear to have been followed until discharge. |
|
| Participants | Inclusion criteria: Preterm infants 500‐1249 g who received PN from 1st hr of life. Exlusion criteria: Severe malformations, metabolic disease and severe congenital sepsis. |
|
| Interventions | 150 consecutive admitted preterm infants were randomly assigned to receive five different LE (n = 30 in each group): 1) S‐LE: Intralipid® (100% soy based LE) 2) MS‐LE: Lipofundin® (MCT 50%/soy LCT 50%) 3) MFS‐LE: Lipidem® (MCT 50%/soy 40%/fish oil 10%) 4) OS‐LE: ClinOleic® (olive oil 80%/soy oil 20%) 5) MOFS‐LE: SMOFlipid® (MCT 30%/soy oil 30%/olive oil 25%/fish oil 15%) |
|
| Outcomes | Primary outcome: Plasma phytosterol concentrations (campesterol and β‐sitosterol levels) day 0 (cord), day 7 (full TPN), day 14 (50% enteral calories) Secondary outcomes: Clinical outcomes including mortality, growth outcomes, BPD, NEC, PDA, sepsis, and cholestasis. |
|
| Notes | No funding source mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly assigned in a 1:1:1:1:1 ratio to 1 of the 5 LEs studied following a simple randomisation procedure." Comment: How random sequence was generated is not mentioned. Authors mention "pharmacy received the enveloped randomisation list with the patient codes and provided the allocated interventions." Probably done. Previous reports involving the same team mentioned "Randomization was obtained with sealed envelopes using a random permuted blocks within strata protocol." |
| Allocation concealment (selection bias) | Low risk | Quote: "The pharmacy received the enveloped randomisation list with the patient codes and provided the allocated interventions. (sealed envelope system)" "They were identified only by the patient number according to the randomisation schedule." Comment: Probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Outcome data complete, attrition well explained and less than 10%. |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we can not ascertain any deviation from the protocol. |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "5 different LEs prepared in the hospital pharmacy were of the same size and identical appearance." Comment: Probaby done. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "5 different LEs prepared in the hospital pharmacy were of the same size and identical in appearance;" "The clinicians, the patient’s parents, and the individuals who assessed the study endpoints were blinded to the LEs." Comment: Probably done. |
Skouroliakou 2010.
| Study characteristics | ||
| Methods | Randomised controlled trial in preterm infants done in a single centre at the NICU of ‘IASO’ Maternity Hospital in Athens, Greece. Study enrolment: Nov 2008 to April 2009. I. Allocation Concealment ‐ yes II. Blinding of intervention ‐ yes III. Blinding of outcome measurement(s) ‐ yes IV. Complete follow‐up ‐ no |
|
| Participants | 38 infants were enrolled in the study. Inclusion criteria: Under 32 week gestation preterm infants with birth weight of < 1500 g requiring admission to ICU within 12 hours of birth and expected to receive > 80% of the energy intake by parenteral route in the first 8 days of life and requiring PN for at least 7 days. Exclusion criteria: Inherited metabolic disorders, congenital malformations, transfusion of blood/fresh frozen plasma > 15 ml/kg, and participation in another study. |
|
| Interventions | Infants were randomised to receive either: 1) MOFS‐LE: (SMOFlipid ®; n = 19) OR 2) S‐LE: (Inralipid ®; n = 19) 4 different TPN protocols were created based on gestational age/weight/clinical condition. Lipids were started on day 1 or 2 of life (based on gestational age) with a maximum of 3g/kg/day in both the groups. Enteral feeds were allowed at ≤ 20% of total energy intake and started as soon as feasible. Oral feeds were started after at least 14 days of parenteral nutrition for all infants in the study group. |
|
| Outcomes | Primary outcome: Oxidation potential (vitamin A, E and total anti‐oxidant potential) Hypothesis: A reduction in oxidative stress in the SMOFlipid® group? Secondary outcomes: Growth parameters, blood count, clinical condition and length of stay (parameters noted on day 0, day 14, and at discharge). |
|
| Notes | 1. SMOFlipid® was supplied by Freseniius Kabi. 2. Vitamin E and A levels were not affected by the intervention, however TAP level was increased in the SMOFlipid® group, indicating possible reduction in the oxidant stress. 3. Authors mention "none of the children in each group had any side effects related to parenteral nutrition or sepsis." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer generated randomisation." Comment: Probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "the pharmacist, who was responsible for the placement of each infant in a group (intervention vs control)..." Comment: Statistician and Pharmacist not involved in the trial. Probably done. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Out of 38 randomised infants there were 6 exclusions (16%) with 5 from the SMOFlipid® group (n = 2 transfusion > 15 ml/kg, n = 1 PN < 7 days, n = 1 transfer to another centre) and 1 from the 20% Intralipid® group (PN < 7 days). (unbalanced exclusions) |
| Selective reporting (reporting bias) | Unclear risk | Comment: The protocol for the study was not available to us so we cannot ascertain any deviation from the protocol. |
| Other bias | Low risk | None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "PN were in identical bags" Comment: Probably done. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "PN were in identical bags;" " All medical personnel and participants were blinded to treatment assignment during the whole course of the study" Comment: Probably done. |
Tomsits 2010.
| Study characteristics | ||
| Methods | Single centre randomised controlled trial done at the Department of Paediatrics at Semmelweis University, Budapest, Hungary. Study enrolment: April 2004‐January 2006. I. Allocation concealment ‐ cannot tell II. Blinding of intervention ‐ cannot tell III. Blinding of outcome measurement(s) ‐ cannot tell IV. Complete follow‐up ‐ yes Both intention to treat and per protocol analysis were performed ‐ both with the last observation carried forward. Stratified study with the following strata: 1000‐1499 g, 1500‐1999 g and 2000 to 2500 g |
|
| Participants | Inclusion criteria: < 34 week gestation preterm infants aged 3 to 7 days expected to receive TPN for ≥ 7 days. Exclusion criteria: None mentioned. |
|
| Interventions | 60 infants born < 34 weeks gestation were randomised to receive either: 1) MOFS‐LE: (20% SMOF®; n = 30) 2) S‐LE: (20% Iintralipid®; n = 30) LE was started at 0.5 g/kg/day on day 1 and was increased by increments of 0.5 g/kg/day daily up to a maximum of 2 g/kg/day on days 4 to 14. Additional oral/enteral intake comprising < 20% at baseline, < 30% on days 1 to 3, and < 50% on days 4 to 14 of the total energy intake was permitted if appropriate. Other components of PN were given at the discretion of the investigator. |
|
| Outcomes | Outcomes were evaluated on day 0, 8 and 15. Primary efficacy outcome: Change in weight from day 1 to day 8. Secondary efficacy outcomes: Mechanical ventilation/oxygen therapy and RBC fatty acid profile. Primary safety outcome: Serum triglycerides. Secondary safety outcomes: Vital signs, hematology, coagulation profile, and liver enzymes. The study also reported on growth rate and sepsis. |
|
| Notes | 1. No funding source mentioned. 2. 57 adverse events ‐ all mild, some outcomes grouped into composite groups, sepsis was reported as infections and infestations. 3. Decreased GGT in the SMOFlipid® group (and increased GGT in the Iintralipid® group, P value < 0.05). 4. The SMOFlipid® group had lower GGT, higher ω‐3, RBC, eicosapentaenoic acid levels, and α‐tocopherol levels. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...randomised to receive PN..." Comment: Method of random sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Details are not provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9 infants (15% participants; 4 in the study group) terminated the study early and were included in the intention to treat analysis with last observation carried forward. Out of 9, in 7 "oral feeding reached exclusion criteria" and in 2 consent was withdrawn. Missing subjects are balanced in numbers across intervention groups, however it is not mentioned to which group the 2 infants where consent was withdrawn belonged. As the data is provided for the ITT set (all participants), the reviewers agreed to give a low risk rating. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available to us. Some side effects were grouped together (infections and infestations) and could not be used in the meta‐analysis for sepsis. Ventilation and oxygen duration appears to be a combined outcome. In the absence of the study protocol we have assigned the risk category as "unknown." |
| Other bias | Low risk | None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "were randomised to receive in a double blind manner..." Comment: Details of how blinding was achieved were not mentioned by the authors. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "were randomised to receive in a double blind manner..." Comment: Details of blinding were not mentioned by the authors. |
Vlaardingerbroek 2014.
| Study characteristics | ||
| Methods | Randomised prospective single centre study in VLBW preterm infants conducted at NICU of the Erasmus MC‐Sophia Children’s Hospital, Rotterdam, The Netherlands. Study enrolment: December 2008 to January 2012. I. Allocation concealment ‐ yes II. Blinding of intervention ‐ cannot tell III. Blinding of outcome measurement(s) ‐ cannot tell IV. Complete follow‐up ‐ yes (per protocol only) |
|
| Participants | Inclusion criteria: Inborn VLBW infants (birth weight < 1500 g) with a central venous catheter for clinical purposes were eligible for the study. Exclusion criteria: Congenital anomalies, chromosome defects, metabolic diseases, and endocrine, renal, or hepatic disorders. |
|
| Interventions | Ninety‐eight preterm infants were randomised to receive either: 1) MOFS‐LE: (n = 49; SMOFlipid® 20%, Fresenius Kabi, Germany) 2) S‐LE: (n = 49; Intralipid® 20%, Fresenius Kabi, Germany) There was one withdrawal from each arm (leaving 48 infants in each arm). |
|
| Outcomes | Primary outcomes were fatty acid concentration in plasma triglycerides and phospholipids. Secondary outcomes included hematological, biochemical parameters, phytosterol concentrations, and clinical outcomes including survival, duration of hospital stay, symptomatic PDA, RDS, BPD, NEC, late‐onset sepsis, IVH, PVL, ROP and cholestasis. Growth outcomes were reported as a part of efficacy parameters. | |
| Notes | Funding source: None disclosed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer generated block randomisation list with variable block sizes generated by a statistician" |
| Allocation concealment (selection bias) | Low risk | Quote: "sealed opaque randomisation envelope that was stratified by weight (< 1000 g and 1000–1499 g) and sex. The envelopes were made by a research pharmacist who was not involved in clinical care" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Clinical outcomes were reported for most infants. |
| Selective reporting (reporting bias) | Low risk | Comment: The study protocol was available at www.trialregister.nl.com, registration no. NTR1445 |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "randomisation to the lipid group remained double‐blinded throughout the study and the analyses;" "double‐blind randomised controlled trial." Comment: Details of how blinding was achieved were not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "randomisation to the lipid group remained double‐blinded throughout the study and the analyses;" "double‐blind randomised controlled trial." Comment: Details of how blinding was achieved were not described. |
Wang 2015.
| Study characteristics | ||
| Methods | Double‐blind, randomised study conducted at NICU of Xin Hua Hospital and Shanghai Children's Medical Center in Shanghai, China. Study enrolment from February 2012 to July 2013. I. Allocation concealment ‐ yes II. Blinding of intervention ‐ yes III. Blinding of outcome measurement(s) ‐ yes IV.Complete follow‐up ‐ yes (per protocol only) |
|
| Participants | 118 preterm infants (< 37 weeks) were eligible for inclusion. 103 infants (12 refused consent and 3 died in < 72 hrs before randomisation) were randomised to receive either: 1) S‐LE (Intralipid®; n = 51) 2) OS‐LE (ClinOleic®; n = 52) |
|
| Interventions | PN using either S‐LE, n = 51 or OS‐LE, n = 52. | |
| Outcomes | The primary end point was liver chemistry. The secondary end point was plasma bile acid composition. Serum direct bilirubin was reported to be higher after 7 days in the S‐LE group. The study reported on weight gain, days to regain birth weight, duration of ventilation, BPD, NEC, and culture positive sepsis. There were 3 deaths before randomisation and 3 deaths occurred during the study (2 in OS‐LE group and 1 in S‐LE group). ROP, IVH and PVL were not reported in this trial. | |
| Notes | Funding disclosure: Supported in part by grants from the National Natural Science Foundation of China (No. 81100631) and Shanghai Key Laboratory of Pediatric Gastroenterology and Nutrition (No. 11DZ2260500). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "cards were created with a unique randomisation code." Comment: Though the authors did not mention how the unique randomisation code was generated, the review authors agreed that the risk was low |
| Allocation concealment (selection bias) | Low risk | Quote: "...unique randomisation code and placed in sequentially numbered opaque envelopes" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Clinical outcomes were reported for most outcomes. 2 infants in the OS‐LE arm and 2 infant in the S‐LE arm were excluded from analysis as they had < 14 days of parenteral nutrition. Intention to treat analysis was done. |
| Selective reporting (reporting bias) | Low risk | Comment: The study protocol was available: NCT01786759. |
| Other bias | Low risk | Comment: None identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Investigators, parents, and all the physicians and nurses involved in patient care were blinded to the group assignment," "The 2 solutions looked identical to the clinicians" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Investigators, parents, and all the physicians and nurses involved in patient care were blinded to the group assignment," "The 2 solutions looked identical to the clinicians" Comment: Reviewers agreed about blinding of outcome assessment. |
ALT: alanine aminotransferase AST: aspartate aminotransferaseROP: retinopathy of prematurity BPD: bronchopulmonary dysplasia BW: birth weight CLD: chronic lung disease DHA: docosahexaenoic acid GGT: gamma‐glutamyl transferase IV: intravenous IVH: intraventricular haemorrhage LCT: long chain triglycerides LE: lipid emulsion(s) MCT: medium chain triglycerides MFS‐LE: medium chain triglycerides‐fish‐soy lipid emulsion MOFS‐LE: medium chain triglycerides‐olive‐fish‐soy lipid emulsion MS‐LE: medium chain triglycerides‐soy lipid emulsion NEC: necrotising enterocolitis NICU: neonatal intensive care unit OS‐LE: olive‐soy lipid emulsion PDA: patent ductus arteriosus PN: parenteral nutrition PVL: periventricular leukomalacia RBC: red blood cells RDS: respiratory distress syndrome S‐LE: soy lipid emulsion TPN: total parenteral nutrition VLBW: very low birth weight
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Angsten 2002 | The study included term infants. Population included 36 to 41 week newborns ≤ 4 days of age needing surgery and expected to require total parenteral nutrition for at least 5 days. |
| Ariyawangso | The study included newborns requiring surgery and included term infants. Infants were randomised to receive SMOFlipid® 20% (experimental group, n = 21) or Intralipid® 20% (control group, n = 21). |
| Lam 2014 | Infants with parenteral nutrition‐associated cholestasis (conjugated bilirubin concentration ≥ 34 µmol/l or 2 mg/dl) and expected to be parenteral nutrition‐dependent for > 2 weeks were randomised to receive either fish oil based lipid preparation or soy oil based lipid preparation at 1.5 g/kg/day. |
| Lima 1988 | The study included term infants up to 38 weeks gestation. |
| Magnusson 1997 | The population included newborn infants requiring surgery and included term infants. |
| Nehra 2014 | Inclusion criteria included newborn and infants < 3 months with gastrointestinal disease requiring surgery (included term infants). Fish oil LE (Omegaven®; n=9) versus soy LE (Intraplipid®; n=10). |
| Webb 2008 | The study included term babies with mean gestation of infants 37.0 ± 3.6 and 36.7± 3.0 weeks in the two arms of the study. |
| Wilson 1997 | This study aimed to compare "aggressive parenteral nutrition" in preterm infants versus "conventional parenteral nutrition." The "aggressive nutrition group" received a higher rate of lipids, proteins, dextrose and 33% of participants in this group received insulin besides getting medium chain and long chain triglyceride based LE (Lipofundin®). The conventional nutrition group received a lesser percentage of dextrose, lesser rate of lipids (S‐LE) and no insulin. The duration of LE was a median of 20 days (interquartile range 12‐28 days) in the aggressive nutrition (MS‐LE) group versus a median of 6 days (interquartile range 2‐15 days) in the conventional nutrition (S‐LE group). This study, done in 1997, reported advantages of the aggressive parenteral nutritional regimen versus conventional parenteral nutrition. |
LE: lipid emulsion
Characteristics of ongoing studies [ordered by study ID]
NCT01585935.
| Study name | Preventing cholestasis using SMOFLipid®. |
| Methods | Allocation: Randomised Endpoint Classification: Efficacy study Intervention model: Parallel assignment Masking: Double blind (subject, investigator, outcomes assessor) Primary purpose: Prevention |
| Participants | Birth weight ≤ 1000 g Admission to the neonatal ward in the first 24 hours of life Informed consent and randomisation in the first five days of life |
| Interventions | Experimental: SMOFLipid® (mixture of soy, fish, medium chain triglycerides, and olive oil); target dose: 3 g/kg/day Comparator: Intralipid® (soy bean oil); target dose: 3g/kg/d |
| Outcomes | Primary Outcome: parenteral nutrition‐associated cholestasis defined as two conjugated bilirubin > 1.5 mg/dl measurements on two consecutive occasions. Secondary Outcome: The most important secondary outcome is neurodevelopment at 12 and 24 months of corrected age. |
| Starting date | June 2012 |
| Contact information | Study Director: Andreas Repa, MD, Medical University Vienna. |
| Notes | None. |
NCT01683162.
| Study name | Effects of parenteral nutrition with different lipid emulsions in preterm infants. |
| Methods | Allocation: Randomised Endpoint classification: Safety/efficacy study Intervention model: Parallel assignment Masking: Double blind (subject, caregiver, investigator) Primary purpose: Supportive care |
| Participants | Birth weight ≤ 2000 g Preterm infants < 37 weeks admitted within 72 hours after birth |
| Interventions | MCT/LCT lipid emulsion OS‐LE (ClinOleic®) S‐LE (Intralipid®) |
| Outcomes | Primary outcome: Lipometabolism and change in fatty acid profile at day seven and 14. Secondary outcome: oxidative stress; Other outcomes: weight, growth parameters, days on ventilator, length of hospitalisation, sepsis and NEC. |
| Starting date | July 2012 |
| Contact information | Ying Wang PhD, Wei Cai PhD, Xin Hua Hospital, School of Medicine, Shanghai Jiao Tong University. |
| Notes | None. |
Differences between protocol and review
The ‘control (S‐LE) versus intervention’ format in the protocol was changed to the ‘intervention versus control’ format in the review. The background section was updated to reflect more recent evidence. Combined intervention comparisons between ‘all fish oil containing LE’ and ‘all alternative LE’ with S‐LE were added. A comparison between PFE450 (borage oil based LE) and S‐LE was also added. Secondary outcomes including duration of phototherapy, clinical and/or culture positive sepsis, and any PDA were added to the review. The sequence of the secondary outcomes was changed to bring the similar outcomes together. The search strategy was updated to include more databases and an increased number of search terms with the use of truncations and wild cards to increase sensitivity (details in Appendix 3). Abbreviations for lipid emulsions were changed to reflect the source of lipid and avoid confusion (details in Appendix 2).
The ‘GRADE Working Group Recommendations’ have been used for important clinical outcomes to grade the quality of evidence and help in decision making.
Contributions of authors
All review authors were involved in conceiving and designing the protocol and the review. Two review authors (VK, MM) performed study searches and data extraction. Data were entered into RevMan 2011 by one author (VK) and checked by another author (MM). All authors reviewed the manuscript and any differences in opinion between the authors at any stage were resolved by discussion.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services, USA
Editorial support of the Cochrane Neonatal Review Group has been funded with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN275201100016C
Declarations of interest
None.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Beken 2014 {published data only}
- Beken S, Dilli D, Fettah ND, Kabatas EU, Zenciroqlu A, Okumus N. The influence of fish-oil lipid emulsions on retinopathy of prematurity in very low birth weight infants: a randomized controlled trial. Early Human Development 2014;90(1):27-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
D'ascenzo 2014 {published data only}
- D'Ascenzo R, Savini S, Biagetti C, Bellagamba MP, Marchionni P, Pompilio A, et al. Higher Docosahexaenoic acid, lower Arachidonic acid and reduced lipid tolerance with high doses of a lipid emulsion containing 15% fish oil: A randomized clinical trial. Clinical Nutrition 2014;33(6):1002-9. [DOI] [PubMed] [Google Scholar]
Demirel 2011 {published data only (unpublished sought but not used)}
- Demirel G, Oguz SS, Celik IH, Erdeve O, Uras N, Dilmen U. The metabolic effects of two different lipid emulsions used in parenterally fed premature infants--a randomised comparative study. Early Human Development 2012;88(7):499-501. [PMID: ] [DOI] [PubMed] [Google Scholar]
Deshpande 2009 {published data only (unpublished sought but not used)}
- Deshpande GC, Simmer K, Mori T, Croft K. Parenteral lipid emulsions based on olive oil compared with soybean oil in preterm (<28 weeks' gestation) neonates: a randomised controlled trial. Journal of Pediatric Gastroenterology and Nutrition 2009;49(5):619-25. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gawecka 2008 {published data only (unpublished sought but not used)}
- Gawecka A, Michalkiewicz J, Kornacka MK, Luckiewicz B, Kubiszewska I. Immunologic properties differ in preterm infants fed olive oil vs soy-based lipid emulsions during parenteral nutrition. JPEN. Journal of Parenteral and Enteral Nutrition 2008;32(4):448-53. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gobel 2003 {published data only}
- Göbel Y, Koletzko B, Böhles HJ, Engelsberger I, Forget D, Le Brun A, et al. Parenteral fat emulsions based on olive and soybean oils: a randomised clinical trial in preterm infants. Journal of Pediatric Gastroenterology and Nutrition 2003;37(2):161-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Koksal 2011 {published and unpublished data}
- Köksal N, Kavurt AV, Cetinkaya M, Ozarda Y, Ozkan H. Comparison of lipid emulsions on antioxidant capacity in preterm infants receiving parenteral nutrition. Pediatrics International 2011;53(4):562-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lehner 2006 {published data only (unpublished sought but not used)}
- Lehner F, Demmelmair H, Röschinger W, Decsi T, Szász M, Adamovich K, et al. Metabolic effects of intravenous LCT or MCT/LCT lipid emulsions in preterm infants. Journal of Lipid Research 2006;47(2):404-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rayyan 2012 {published data only (unpublished sought but not used)}
- Rayyan M, Devlieger H, Jochum F, Allegaert K. Short-term use of parenteral nutrition with a lipid emulsion containing a mixture of soybean oil, olive oil, medium-chain triglycerides, and fish oil: a randomised double-blind study in preterm infants. Journal of Parenteral and Enteral Nutrition 2012;36(1 Suppl):81S-94S. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rubin 1994 {published data only}
- Rubin M, Moser A, Naor N, Merlob P, Pakula R, Sirota L. Effect of three intravenously administered fat emulsions containing different concentrations of fatty acids on the plasma fatty acid composition of premature infants. The Journal of Pediatrics 1994;125(4):596-602. [PMID: ] [DOI] [PubMed] [Google Scholar]
Savini 2013 {published data only (unpublished sought but not used)}
- Savini S, D'Ascenzo R, Biagetti C, Serpentini G, Pompilio A, Bartoli A, et al. The effect of 5 intravenous lipid emulsions on plasma phytosterols in preterm infants receiving parenteral nutrition: a randomised clinical trial. American Journal of Clinical Nutrition 2013;98(2):312-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Skouroliakou 2010 {published data only (unpublished sought but not used)}
- Skouroliakou M, Konstantinou D, Koutri K, Kakavelaki C, Stathopoulou M, Antoniadi M, et al. A double-blind, randomised clinical trial of the effect of omega-3 fatty acids on the oxidative stress of preterm neonates fed through parenteral nutrition. European Journal of Clinical Nutrition 2010;64(9):940-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tomsits 2010 {published data only (unpublished sought but not used)}
- Tomsits E, Pataki M, Tölgyesi A, Fekete G, Rischak K, Szollár L. Safety and efficacy of a lipid emulsion containing a mixture of soybean oil, medium-chain triglycerides, olive oil, and fish oil: a randomised, double-blind clinical trial in premature infants requiring parenteral nutrition. Journal of Pediatric Gastroenterology and Nutrition 2010;51(4):514-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vlaardingerbroek 2014 {published data only}
- Vlaardingerbroek H, Vermeulen MJ, Carnielli VP, Vaz FM, den Akker CH, Goudoever JB. Growth and fatty acid profiles of VLBW infants receiving a multicomponent lipid emulsion from birth. Journal of Pediatric Gastroenterology and Nutrition 2014;58(4):417-27. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wang 2015 {published data only}
- Wang Y, Zhou KJ, Tang QY, Hong L, Feng Y, Lu LN, et al. Effect of an Olive Oil-Based Lipid Emulsion Compared With a Soybean Oil-Based Lipid Emulsion on Liver Chemistry and Bile Acid Composition in Preterm Infants Receiving Parenteral Nutrition: A Double-Blind, Randomized Trial. Journal of Parenteral and Enteral Nutrition 2015 Jan 5 [Epub ahead of print]. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Angsten 2002 {published data only}
- Angsten G, Boberg M, Cederblad G, Meurling S, Stiernström H. Metabolic effects in neonates receiving intravenous medium-chain triglycerides. Acta Paediatrica 2002;91(2):188-97. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ariyawangso {published data only}
- Ariyawangso U, Puttilerpong C, Ratanachuek S, Anuntkosol M. Short-term safety and efficacy of fish-oil emulsions on the prevention of parenteral nutrition-associated liver disease in surgical neonates: a randomized controlled trial. Thai Journal of Pharmaceutical Sciences 2014;38(4):202-9. [Google Scholar]
Lam 2014 {published data only}
- Lam HS, Tam YH, Poon TC, Cheung HM, Yu X, Chan BP, et al. A double-blind randomised controlled trial of fish oil-based versus soy-based lipid preparations in the treatment of infants with parenteral nutrition-associated cholestasis. Neonatology 2014;105(4):290-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lima 1988 {published data only}
- Lima LA, Murphy JF, Stansbie D, Rowlandson P, Gray OP. Neonatal parenteral nutrition with a fat emulsion containing medium chain triglycerides. Acta Paediatrica Scandinavica 1988;77(3):332-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Magnusson 1997 {published data only}
- Magnusson G, Boberg M, Cederblad G, Meurling S. Plasma and tissue levels of lipids, fatty acids and plasma carnitine in neonates receiving a new fat emulsion. Acta Paediatrica 1997;86(6):638-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nehra 2014 {published data only}
- Nehra D, Fallon EM, Potemkin AK, Voss SD, Mitchell PD, Valim C, et al. A comparison of 2 intravenous lipid emulsions: interim analysis of a randomized controlled trial. Journal of Parenteral and Enteral Nutrition 2014;38(6):693-701. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Webb 2008 {published data only}
- Webb AN, Hardy P, Peterkin M, Lee O, Shalley H, Croft KD, et al. Tolerability and safety of olive oil-based lipid emulsion in critically ill neonates: a blinded randomised trial. Nutrition 2008;24(11-12):1057-64. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wilson 1997 {published data only}
- Wilson DC, Cairns P, Halliday HL, Reid M, McClure G, Dodge JA. Randomised controlled trial of an aggressive nutritional regimen in sick very low birthweight infants. Archives of Disease in Childhood. Fetal and Neonatal Edition 1997;77(1):F4-11. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
NCT01585935 {published data only}
- NCT01585935. Preventing Cholestasis Using SMOFLipid®. https://clinicaltrials.gov/ct2/show/NCT01585935 (accessed 17 August 2015). [Google Scholar]
NCT01683162 {published data only}
- NCT01683162. Effects of Parenteral Nutrition With Different Lipid Emulsions in Preterm Infants. https://clinicaltrials.gov/ct2/show/NCT01683162.
Additional references
Beauchamp 2005
- Beauchamp GK, Keast RS, Morel D, Lin J, Pika J, Han Q, et al. Phytochemistry: ibuprofen-like activity in extra-virgin olive oil. Nature 2005;437(7055):45-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bell 1978
- Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Annals of Surgery 1978;187(1):1-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buenestado 2006
- Buenestado A, Cortijo J, Sanz MJ, Naim-Abu-Nabah Y, Martinez-Losa M, Mata M, et al. Olive oil-based lipid emulsion's neutral effects on neutrophil functions and leukocyte-endothelial cell interactions. Journal of Parenteral and Enteral Nutrition 2006;30(4):286-96. [PMID: ] [DOI] [PubMed] [Google Scholar]
Christensen 2007
- Christensen RD, Henry E, Wiedmeier SE, Burnett J, Lambert DK. Identifying patients, on the first day of life, at high-risk of developing parenteral nutrition-associated liver disease. Journal of Perinatology 2007;27(5):284-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cober 2010
- Cober MP, Teitelbaum DH. Prevention of parenteral nutrition-associated liver disease: lipid minimization. Current Opinion in Organ Transplantation 2010;15(3):330-3. [PMID: ] [DOI] [PubMed] [Google Scholar]
de Meijer 2009
- Meijer VE, Gura KM, Le HD, Meisel JA, Puder M. Fish oil-based lipid emulsions prevent and reverse parenteral nutrition-associated liver disease: the Boston experience. Journal of Parenteral and Enteral Nutrition 2009;33(5):541-7. [DOI] [PubMed] [Google Scholar]
de Vries 1992
- Vries LS, Eken P, Dubowitz LM. The spectrum of leucomalacia using cranial ultrasound. Behavioural Brain Research 1992;49(1):1-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Driscoll 2008
- Driscoll DF, Bistrian BR, Demmelmair H, Koletzko B. Pharmaceutical and clinical aspects of parenteral lipid emulsions in neonatology. Clinical Nutrition 2008;27(4):497-503. [PMID: ] [DOI] [PubMed] [Google Scholar]
EndNote 2014 [Computer program]
- EndNote. Version 6.0.1. Thompson Reuters, 2014.
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59(1):7-10. [PMID: ] [DOI] [PubMed] [Google Scholar]
Fürst 2000
- Fürst P, Kuhn KS. Fish oil emulsions: what benefits can they bring? Clinical Nutrition 2000;19(1):7-14. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gawecka 2008a
- Gawecka A, Michalkiewicz J, Kornacka MK, Luckiewicz B, Kubiszewska I. Immunologic properties differ in preterm infants fed olive oil vs soy-based lipid emulsions during parenteral nutrition. Journal of Parenteral and Enteral Nutrition 2008;32(4):448-53. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gawecka 2008b
- Gawecka A, Kornacka MK, Luckiewicz B, Rudzinska I. Tolerance of two lipid emulsions used in parenterally-fed premature infants - a comparative study. Medycyna Wieku Rozwojowego 2008;12(3):782-8. [PMID: ] [PubMed] [Google Scholar]
Gitto 2001
- Gitto E, Karbownik M, Reiter RJ, Tan DX, Cuzzocrea S, Chiurazzi P, et al. Effects of melatonin treatment in septic newborns. Pediatric Research 2001;50(6):756-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gogos 1995
- Gogos CA, Kalfarentzos F. Total parenteral nutrition and immune system activity: a review. Nutrition 1995;11(4):339-44. [PMID: ] [PubMed] [Google Scholar]
Goulet 1999
- Goulet O, Potter S, Antebi H, Driss F, Colomb V, Bereziat G, et al. Long-term efficacy and safety of a new olive oil-based intravenous fat emulsion in paediatric patients: a double-blind randomised study. American Journal of Clinical Nutrition 1999;70(3):338-45. [PMID: ] [DOI] [PubMed] [Google Scholar]
GradePro 2008 [Computer program]
- McMaster University, 2008 GradePro Version 3.2. McMaster University, 2008.
Granato 2000
- Granato D, Blum S, Rossle C, Le Boucher J, Malnoe A, Dutot G. Effects of parenteral lipid emulsions with different fatty acid composition on immune cell functions in vitro. Journal of Parenteral and Enteral Nutrition 2000;24(2):113-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Grimm 2005
- Grimm H. A balanced lipid emulsion - a new concept in parenteral nutrition. Clinical Nutrition Supplements 2005;1(3):25-30. [Google Scholar]
Gura 2005
- Gura KM, Parsons SK, Bechard LJ, Henderson T, Dorsey M, Phipatanakul W, et al. Use of a fish oil-based lipid emulsion to treat essential fatty acid deficiency in a soy allergic patient receiving parenteral nutrition. Clinical nutrition 2005;24(5):839-47. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines: 6. Rating the quality of evidence--imprecision. Journal of Clinical Epidemiology 2011;64(12):1283-93. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383-94. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407-15. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011c
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294-302. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011d
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. Journal of Clinical Epidemiology 2011;64(12):1303-10. [PMID: ] [DOI] [PubMed] [Google Scholar]
Haynes 2005
- Haynes RB, McKibbon KA, Wilczynski NL, Walter SD, Werre SR. Optimal search strategies for retrieving scientifically strong studies of treatment from Medline: analytical survey. BMJ 2005;330(7501):1179. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heird 2005
- Heird WC, Lapillonne A. The role of essential fatty acids in development. Annual Review of Nutrition 2005;25:549-71. [PMID: ] [DOI] [PubMed] [Google Scholar]
Henriksen 2008
- Henriksen C, Haugholt K, Lindgren M, Aurvag AK, Ronnestad A, Gronn M, et al. Improved cognitive development among preterm infants attributable to early supplementation of human milk with docosahexaenoic acid and arachidonic acid. Pediatrics 2008;121(6):1137-45. [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Deeks JJ. Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Hozo 2005
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology 2005;5:13. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
ICROP 2005
- International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Archives of Ophthalmology 2005;123(7):991-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kapoor 2019
- Kapoor V, Malviya MN, Soll R. Lipid emulsions for parenterally fed preterm infants. Cochrane Database of Systematic Reviews 2019, Issue 6. [DOI: 10.1002/14651858.CD013163.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Koletzko 2001
- Koletzko B, Agostoni C, Carlson SE, Clandinin T, Hornstra G, Neuringer M, et al. Long chain polyunsaturated fatty acids (LC-PUFA) and perinatal development. Acta Paediatrica 2001;90(4):460-4. [PMID: ] [PubMed] [Google Scholar]
Koletzko 2003
- Koletzko B, Sauerwald U, Keicher U, Saule H, Wawatschek S, Bohles H, et al. Fatty acid profiles, antioxidant status, and growth of preterm infants fed diets without or with long-chain polyunsaturated fatty acids. A randomized clinical trial. European Journal of Nutrition 2003;42(5):243-53. [PMID: ] [DOI] [PubMed] [Google Scholar]
Koletzko 2005
- Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R. Guidelines on Paediatric Parenteral Nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), supported by the European Society of Paediatric Research (ESPR). Journal of Pediatric Gastroenterology and Nutrition 2005;41(Suppl 2):S1-87. [PMID: ] [DOI] [PubMed] [Google Scholar]
Koletzko 2010
- Koletzko B, Goulet O. Fish oil containing intravenous lipid emulsions in parenteral nutrition-associated cholestatic liver disease. Current Opinion in Clinical Nutrition and Metabolic Care 2010 May;13(3):321-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Krohn 2006
- Krohn K, Koletzko B. Parenteral lipid emulsions in paediatrics. Current Opinion in Clinical Nutrition and Metabolic Care 2006;9(3):319-23. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lapillonne 2013
- Lapillonne A, Groh-Wargo S, Gonzalez CH, Uauy R. Lipid needs of preterm infants: updated recommendations. The Journal of Pediatrics 2013;162(3 Suppl):S37-47. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lekka 2004
- Lekka ME, Liokatis S, Nathanail C, Galani V, Nakos G. The impact of intravenous fat emulsion administration in acute lung injury. American Journal of Respiratory and Critical Care Medicine 2004;169(5):638-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
McNaught 1997
- McNaught AD, Wilkinson A. IUPAC. Compendium of Chemical Terminology (the "Gold Book"); http://goldbook.iupac.org/P04758.html (2006-). 2nd edition. Oxford: Blackwell Scientific Publications, 1997. [Google Scholar]
Mylonas 1999
- Mylonas C, Kouretas D. Lipid peroxidation and tissue damage. In Vivo 1999;13(3):295-309. [PMID: ] [PubMed] [Google Scholar]
Nandiwada 2013
- Nandivada P, Carlson SJ, Cowan E, Chang MI, Gura KM, Puder M. Role of parenteral lipid emulsions in the preterm infant. Early Human Development 2013;89(Suppl 2):S45-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Palmblad 1991
- Palmblad J. Intravenous lipid emulsions and host defence - a critical review. Clinical Nutrition 1991;10(6):303-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Papile 1978
- Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular haemorrhage: a study of infants with birth weights less than 1,500 gm. Journal of Pediatrics 1978;92(4):529-34. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pawlik 2011
- Pawlik D, Lauterbach R, Turyk E. Fish-oil fat emulsion supplementation may reduce the risk of severe retinopathy in VLBW infants. Pediatrics 2011;127(2):223-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pawlik 2013
- Pawlik D, Lauterbach R, Walczak M, Hurkala J, Sherman MP. Fish-Oil Fat Emulsion Supplementation Reduces the Risk of Retinopathy in Very Low Birth Weight Infants: A Prospective, Randomized Study. Journal of Parenteral and Enteral Nutrition 2013;38(6):711-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pitkanen 1991
- Pitkanen O, Hallman M, Andersson S. Generation of free radicals in lipid emulsion used in parenteral nutrition. Pediatric Research 1991;29(1):56-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Puder 2009
- Puder M, Valim C, Meisel JA, Le HD, Meijer VE, Robinson EM, et al. Parenteral fish oil improves outcomes in patients with parenteral nutrition-associated liver injury. Annals of Surgery 2009;250(3):395-402. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Putet 2000
- Putet G. Lipid metabolism of the micropremie. Clinics in Perinatology 2000;27(1):57-69. [PMID: ] [DOI] [PubMed] [Google Scholar]
Reimund 2004
- Reimund JM, Scheer O, Muller CD, Pinna G, Duclos B, Baumann R. In vitro modulation of inflammatory cytokine production by three lipid emulsions with different fatty acid compositions. Clinical Nutrition 2004;23(6):1324-32. [PMID: ] [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version 5.0.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Robinson 2008
- Robinson DT, Ehrenkranz RA. Parenteral nutrition-associated cholestasis in small for gestational age infants. The Journal of Pediatrics 2008;152(1):59-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rubin 1995
- Rubin M, Naor N, Sirota L, Moser A, Pakula R, Harell D, et al. Are bilirubin and plasma lipid profiles of premature infants dependent on the lipid emulsion infused? Journal of Pediatric Gastroenterology and Nutrition 1995;21(1):25-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sala‐Vila 2007
- Sala-Vila A, Barbosa VM, Calder PC. Olive oil in parenteral nutrition. Current Opinion in Clinical Nutrition and Metabolic Care 2007;10(2):165-74. [DOI] [PubMed] [Google Scholar]
SanGiovanni 2000
- SanGiovanni JP, Berkey CS, Dwyer JT, Colditz GA. Dietary essential fatty acids, long-chain polyunsaturated fatty acids, and visual resolution acuity in healthy full term infants: a systematic review. Early Human Development 2000;57(3):165-88. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schock 2001
- Schock BC, Sweet DG, Halliday HL, Young IS, Ennis M. Oxidative stress in lavage fluid of preterm infants at risk of chronic lung disease. American Journal of Physiology. Lung Cellular and Molecular Physiology 2001;281(6):L1386-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sinclair 2009
- Sinclair JC, Bottino M, Cowett RM. Interventions for prevention of neonatal hyperglycemia in very low birth weight infants. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007615.pub2] [DOI] [PubMed] [Google Scholar]
Skouroliakou 2012
- Skouroliakou M, Konstantinou D, Agakidis C, Delikou N, Koutri K, Antoniadi M, et al. Cholestasis, bronchopulmonary dysplasia, and lipid profile in preterm infants receiving MCT/ω-3-PUFA-containing or soybean-based lipid emulsions. European Journal of Clinical Nutrition 2012 Dec;27(6):817-24. [DOI] [PubMed] [Google Scholar]
Smithers 2008
- Smithers LG, Gibson RA, McPhee A, Makrides M. Higher dose of docosahexaenoic acid in the neonatal period improves visual acuity of preterm infants: results of a randomized controlled trial. The American journal of clinical nutrition 2008;88(4):1049-56. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D. Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. In: Available from www.cochrane-handbook.org. [Google Scholar]
Stoll 2002
- Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 2002;110(2 Pt 1):285-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Kempen 2006
- Kempen AA, Crabben SN, Ackermans MT, Endert E, Kok JH, Sauerwein HP. Stimulation of gluconeogenesis by intravenous lipids in preterm infants: response depends on fatty acid profile. American Journal of Physiology, Endocrinology and Metabolism 2006;290(4):E723-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vanek 2012
- Vanek VW, Seidner DL, Allen P, Bistrian B, Collier S, Gura K, et al. A.S.P.E.N. position paper: Clinical role for alternative intravenous fat emulsions. Nutrition in Clinical Practice 2012;27(2):150-92. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vlaardingerbroek 2012
- Vlaardingerbroek H, Veldhorst MA, Spronk S, den Akker CH, Goudoever JB. Parenteral lipid administration to very-low-birth-weight infants--early introduction of lipids and use of new lipid emulsions: a systematic review and meta-analysis. American Journal of Clinical Nutrition 2012;96(2):255-68. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vlaardingerbroek 2013
- Vlaardingerbroek H, Vermeulen MJ, Rook D, den Akker CH, Dorst K, Wattimena JL, et al. Safety and efficacy of early parenteral lipid and high-dose amino acid administration to very low birth weight infants. The Journal of Pediatrics 2013;163(3):638-44.e1-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Waitzberg 2006
- Waitzberg DL, Torrinhas RS, Jacintho TM. New parenteral lipid emulsions for clinical use. JPEN. Journal of Parenteral and Enteral Nutrition 2006;30(4):351-67. [PMID: ] [DOI] [PubMed] [Google Scholar]
Walsh 2004
- Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics 2004;114(5):1305-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Wanten 2007
- Wanten GJ, Calder PC. Immune modulation by parenteral lipid emulsions. American Journal of Clinical Nutrition 2007;85(5):1171-84. [PMID: ] [DOI] [PubMed] [Google Scholar]


