Highlights
-
•
The entry of SARS-CoV-2 to brain via olfactory nerves.
-
•
The entry of SARS-CoV-2 to brain via ACE-2.
-
•
The entry of SARS-CoV-2 via cytokine storms.
Introduction
In December 2019, an outbreak of novel Corona Virus Disease 2019 (COVID-19) emerged in the Huanan Seafood Market, which is located in Wuhan city, China. In the past few months, COVID-19 cases have accelerated all over the world. As of Apr 21st, 2020, a total of 2,397,217 confirmed cases and 162,956 deaths have been announced. Nowadays, it has been declared as a global public health threat by WHO due to a high rate of morbidity and mortality worldwide.
COVID-19 is produced by a new virus which belongs to the Group 2 of beta-coronavirus that contains Severe Acute Respiratory Syndrome Coronavirus, namely, SARS-CoV-2. In parallel with this knowledge, COVID-19 patients commonly manifest respiratory complications, such as cough, respiratory insufficiency and fever. Recently, increasing evidence shows that the novel coronavirus not only attacks respiratory system, but also likely invades the central nervous system (CNS), developing neurological symptoms. In a retrospective analysis, it was documented that 36.4% (78/214) of SARS-CoV-2-infected patients possessed neurological manifestations including acute cerebrovascular diseases, disturbed consciousness and paresthesia (Mao et al., 2020). Severely infected patients are particularly more vulnerable to occurrence of neurological symptoms than patients who succumb to mild disease. The evidence supporting neuroinfection also arises from a case of viral encephalitis caused by SARS-CoV-2 in Beijing Ditan Hospital on Mar 4th, 2020 (Moriguchi et al., 2020). The researchers firstly reported that the cerebrospinal fluid tested positive for SARS-CoV-2 RNA by genome sequencing (Moriguchi et al., 2020), suggesting the neuroinvasive potential for the virus.
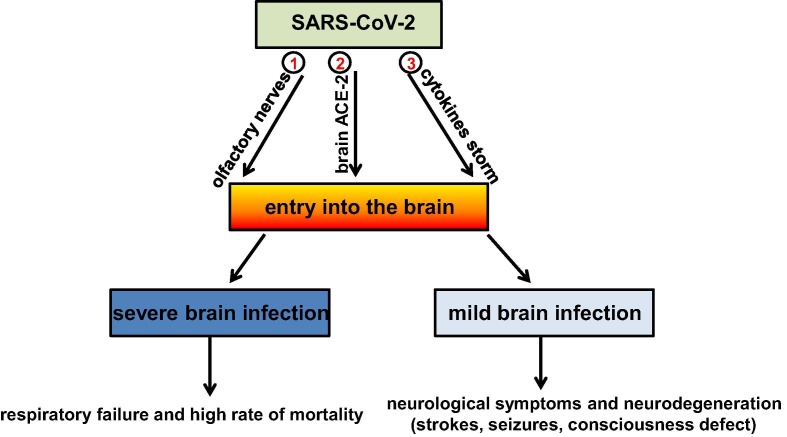
Mechanistically, SARS-CoV-2 has developed an ability to enter host cells through interacting directly with angiotensin-converting enzyme-2 (ACE-2), which is widely expressed in various tissues including brain (Gheblawi et al., 2020). In this case, we consider the virus infects central nervous system due to the abundant expression of ACE-2 target throughout the brain. Indeed, SARS-CoV-2 could interact with ACE-2 in the capillary endothelium and caused blood–brain-barrier destruction, finally promoting virus entry into CNS. Besides, there is compelling evidence showing that the presence of mRNA from closely related SARS virus including SARS-CoV, which also interacts with ACE-2, is present in the brain of infected patients (Inoue et al., 2007). In light of the high similarity between SARS-CoV and SARS-CoV-2, it is quite likely that ACE-2 abundance in brain tissues promotes the entry of SARS-CoV-2 into CNS and subsequently causes neuroinfection. Additionally, it is also noteworthy that SARS-CoV-2 may enter the brain via the olfactory nerves through the nasal cavity and infect neurons that control breathing. This evidence arises from a recent investigation showing that nearly 89% of SARS-CoV-2-infected patients in need of intensive care could not breathe spontaneously and many had neurological manifestations including headache, nausea, and vomiting (Li et al., 2020). Almost half of the patients became seriously sick in a short period of time and died as a result of respiratory failure. It is although not definitively demonstrated that neurons controlling breathing are likely to be infected. Another, under-investigated pathogenic factor that possibly triggers infection in the brain involves a cytokines storm. It is likely that proinflammatory factors released in large quantities promote neuroinflammation following viral infection. Further investigation is essential to clarify this issue. The mechanistic explanations are summarized in Fig. 1 .
Fig. 1.
Summarization of three possible ways by which SARS-CoV-2 enters the brain and causes neuroinfection. We propose three possible patterns about the entry of SARS-CoV-2 into brain, namely, via the olfactory nerves in the nasal cavity (①), interaction with angiotensin-converting enzyme-2 (ACE-2) in the brain (②) and a cytokine storm-induced blood brain barrier disruption (③).
In summary, the COVID-19 pandemic can result in neuroinfection. However, the reason why the infected patients have neurological manifestations remains elusive. A possible explanation arises after considering two aspects. On the one hand, SARS-CoV-2 itself attacks CNS and provokes neurological symptoms via binding ACE-2 target as mentioned above. On the other hand, as there is no vaccine or effective treatment to prevent SARS-CoV-2 infection, current therapeutic approaches such as antiviral drugs and traditional Chinese medicine merely alleviates the symptoms caused by this virus. And also these therapeutic strategies may cause side effects in CNS. In any case, COVID-19 patients should be assessed early for neurological conditions, especially cerebrovascular diseases, consciousness and paresthesia. Awareness and management of infection-associated neuro-complications may be critical for improvement of clinical prognosis. And it is also indispensible for higher surveillance and analysis of neurological complications in infected individuals.
Acknowledgments
Acknowledgements
The authors apologize to all the investigators whose work could not be cited in this paper due to space constraint. This work is finacially supported by National Natural Science Foundation of China (Nos. 81671293 and 81974502).
Competing interest
The authors declare no potential competing interests.
Contributor Information
Xiao-Yuan Mao, Email: xiaoyuanm@csu.edu.cn.
Wei-Lin Jin, Email: weilinjin@sjtu.edu.cn.
References
- Gheblawi M., Wang K., Viveiros A., Nguyen Q., Zhong J.C., Turner A.J., Raizada M.K., Grant M.B., Oudit G.Y. Angiotensin converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system. Circ Res. 2020 doi: 10.1161/CIRCRESAHA.120.317015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue Y., Tanaka N., Tanaka Y., Inoue S., Morita K., Zhuang M., Hattori T., Sugamura K. Clathrin-dependent entry of severe acute respiratory syndrome coronavirus into target cells expressing ACE2 with the cytoplasmic tail deleted. J Virol. 2007;81:8722–8729. doi: 10.1128/JVI.00253-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y.C., Bai W.Z., Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., Miao X., Li Y., Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriguchi T., Harii N., Goto J., Harada D., Sugawara H., Takamino J., Ueno M., Sakata H., Kondo K., Myose N., Nakao A., Takeda M., Haro H., Inoue O., Suzuki-Inoue K., Kubokawa K., Ogihara S., Sasaki T., Kinouchi H., Kojin H., Ito M., Onishi H., Shimizu T., Sasaki Y., Enomoto N., Ishihara H., Furuya S., Yamamoto T., Shimada S. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]