Abstract
The emerging infection of COVID-19 was initiated from Wuhan, China, have been spread to more than 210 countries around the globe including India. The clinical symptoms of COVID-19 are very similar to other respiratory viruses. The number of laboratory-confirmed cases and associated deaths are increasing regularly in various parts of the World. Seven coronaviruses (229E, NL63, OC43, HKU1, SARS, MERS and, COVID-19) can naturally infect human beings. Out of these four (229E-CoV, NL63-CoV, OC43-CoV, HKU1-CoV) are responsible for mild upper respiratory infections, while SARS-CoV, MERS-CoV, and COVID-19 are well known for their high mortality. Few mild strains of coronaviruses are circulating in India but there is no evidence of SARS and MERS outbreaks. The COVID-19 is an emerging viral infection responsible for pandemics. Fortunately, the mortality of COVID-19 is low as compared with SARS and MERS, the majority of its cases are recovered. The death toll of COVID-19 is high even after its low mortality because COVID-19 causes a pandemic while SARS-CoV and MERS-CoV cause epidemics only. COVID-19 influenced the large segments of the world population, which led to a public health emergency of international concern, putting all health organizations on high alert. COVID-19 is the first coronavirus after Spanish Flu 1918–1919, who has extremely influenced the health system, economy, and psychology of India. The present study review is on the general continent, virology, pathogenesis, global epidemiology, clinical presentation, diagnosis, treatment and control of COVID-19 with the reference to India.
Keywords: Emerging viral infection, Coronavirus, COVID-19, Middle east respiratory syndrome coronavirus, SARS coronavirus, India
Introduction
Our health and wealth are highly influenced by various emerging viral diseases. The viral outbreaks like Crimean Congo hemorrhagic fever, Ebola, Lassa fever, Marburg virus, SARS- CoV, MERS-CoV, Nipah, Zika virus, Rift Valley fever virus and COVID-19 are some evidence of our disaster. Some of these outbreaks are highly influenced global life, WHO declared them as a public health emergency of international concern, H1N1 (2009), Polio (2014), Ebola in West Africa (2014), Zika (2016) and Ebola in Congo (2019). Just recently, in December 2019, a novel coronavirus (2019- nCoV), now COVID-19 has emerged in Wuhan, China and spread its wing over the whole globe [18]. A large segment of the world population can be affected by it. Therefore, the WHO declared the COVID-19 pandemics on 30 January 2020. Adaptations to human infection, easy way of transmission, and absence of immunity make the COVID-19 highly contagious in nature. Modern transport systems, convert the world into a global village is helpful for the quick spreading of any contagious agents like COVID-19 viruses. The COVID-19 was successful to spread the infection in more than 210 countries and responsible for 15, 21, 966 laboratory-confirmed cases with 88, 659 deaths up to 09 April, 2020. Fortunately, the death rate of COVID-19 (5.82%) is low as compared with SARS-CoV (10%), MERS-CoV (37.1%). (https://www.worldometers.info/coronavirus/seen on 09 April 2020). The COVID-19 was also entered in Indian boundaries through the various international travels and they handover it to the local population. The first laboratory-confirmed case of COVID-19 was a student returning from Wuhan, China on 30 January 2020. She was studying in Wuhan, return to her home in Kerala, admitted in the hospital for cure and quarantine, discharge after proper recovery. According to the Ministry of Health and Family Welfare, a total of 5734 laboratory-confirmed cases of COVID-19, out of which 473 (8.25%) recovered, while 166 (2.9%) deaths are in the India (https://www.mohfw.gov.in/seen on 09 April 2020). The mortality rate of COVID-19 in India is almost half of the global rate. Now, COVID-19 spread in almost every part of India. Therefore, health workers, governments and the public are needed to co-operate national as well as globally to prevent it from further spread [38].
Virus, and pathogenesis
Coronaviruses are a large group of viruses that causes respiratory and enteric infections in both animals and humans. The virions are large in size (100–160 nm), spherical in shape and have an envelope. There is a capsid of 27–32 kb, which contained a single-stranded RNA genome with positive polarity protected by the envelope [13]. Coronaviruses contain four types of spikes; many long (20 nm) glycoprotein S-spikes in all the coronaviruses, small hemagglutinin-esterase (HE) spikes in some viruses, few transmembrane glycoproteins and envelope protein spikes [8, 16]. The Coronaviruses can be classified into three serogroups on the basis of their genome structure. Serogroups 1 and 2 viruses can infect mammalian and seven of them (229E-CoV, NL63-CoV, OC43-CoV, HKU1-CoV, SARS-CoV, MERS-CoV and, COVID-19) can infect man while serogroups 3 contains avian viruses only. The 229E-CoV, NL63-CoV, OC43-CoV, HKU1-CoV are responsible for 30% or more mild upper respiratory tract illnesses in human, while SARS-CoV, MERS-CoV and, COVID-19 are well known for serious humans infection. Recently, adapted animal coronaviruses causes a more fatal infection in humans [32, 33]. The majority of coronavirus are species-specific. They can expand their genetic diversity by nurturing recombination and mutation during peridomestic animal infections and sometimes a virus can jump a species barrier and start an infection in humans also [22]. The COVID-19 may be animal originated virus as majorities of its initial cases were associated with local fish and wild animal market of Wuhan, China. Some early local studies suggested the possibility of human-to-human transmission via droplets or direct contact and nosocomial infection [2, 3, 15, 34]. The incidences of COVID-19 infections are rapidly increasing, due to transmission from symptomatic/asymptomatic carriers, high mobility rate and rapid expansion through the world travel system. High transmission power and considerable mortality rate are responsible for the high potential of COVID-19 to become a pandemic agent [1, 20, 39]. In India, the majority of COVID-19 cases have travel history in the infected parts or close contact with an infected person, community transmission is doubtful till now.
After entry into a suitable host, the first step of the viral replication cycle is the binding of the virion to the receptors on the target cells in the human respiratory tract. The genomic analysis suggests that COVID-19 will utilize similar receptors that were used by SARS-CoV [19]. The COVID-19 will be attached to the angiotensin-converting enzyme 2 (ACE-2) receptor, which is expressed in the lungs, heart, kidney, small intestine and other tissues, while MERS-CoV uses the dipeptidyl peptidase 4 (DPP4), a transmembrane glycoprotein as a receptor [14, 17, 25, 26]. After binding with a specific receptor, it will enter into host cells via fusion of viral envelope with the plasma membrane or endosomal membranes. After entry, the viral genome RNA is released in the cytoplasm and translates into, pp1a and pp1ab polyproteins [6]. The translation produced the non-structural proteins and form replication-transcription complex (RTC) in double-membrane vesicles [28]. The RTC replicates continuously and synthesizes a nested set of sub-genomic RNAs that encode accessory and structural proteins [11, 23]. The newly formed genomic RNA, nucleocapsid proteins and envelope glycol-proteins assemble and form viral particle buds. At last, the virion-containing vesicles fuse with the plasma membrane to release the virus. Coronavirus infections were responsible for a variety of cytopathic effects (CPE), which depend upon the viral strains and host cells. The mechanism of CPE attributed to a variety of causes; interfere with signal pathway, derangement of cellular function, enhanced cytokine/chemokine expression, inhibition of transcription and translation of cellular proteins. Some coronaviruses cause cell fusion while many others induced apoptosis.
Global epidemiology
COVID-19 has a capacity for human-to-human transmission, the public has no hard immunity against it, a high mortality rate, which makes it suitable agents for pandemic potential and the modern transport system also helps in its rapid expansion. Easy mode of transmission, nature of the virus, population density, environmental condition, social culture (like handshaking, etc.) are major contributors to its rapid spreading. Therefore, COVID-19 turned into a global health concern since its inception from Wuhan, China. Like other respiratory viruses, coronavirus is also contagious and easily spread from one person to another. Many viruses produced similar clinical symptoms; therefore COVID-19 cannot be differentiating on the basis of their clinical symptoms, for its accurate diagnosis a sensitive and specific assay always required. Unfortunately, only a few countries have a capacity for proper viral diagnosis or surveillance by laboratory assays. Without laboratory-confirmed assay or under the capacity of viral diagnosis or surveillance system can decreases the authenticity and accuracy of data. The Basic Reproductive Number (R0) can be utilized to calculate averaging the number of infections produced by infected individuals in susceptible populations. Basic Reproductive Number (R0) is for the SARS-CoV (1.4–5.5), MERS–CoV (< 1), COVID-19 (2.2–2.6) and Influenza viruses (5–25). The members of the coronaviridae are less contagious than influenza viruses [24, 27]. Although, COVID-19 is a slow virus than influenza viruses, but even then spread in the 210 countries within 120 days and caused a large number of infections. In these hundred days, COVID-19 causes the 15, 21, 966 laboratories confirmed cases and 88, 659 (5.82%) deaths worldwide till 09 April 2020. The USA (4, 35, 160), Spain (1, 48, 220), Italy (1, 39, 422), Germany (1, 13, 296) and France (1, 12, 950) are top five infected countries have 9, 49, 048 (62.35%) of total laboratories confirmed cases of COVID-19. Italy (17, 669), USA (14, 797), Spain (14,792), France (10, 869) and United Kingdom (7097) are the top five affected countries have 65, 224 (73.56%) of total deaths due to COVID-19. The mortality rate (%) of top ten countries on the basis of their laboratory-confirmed cases are Italy (12.67%), UK (11.68%), Spain (9.98%), France (9.62%), Belgium (9.57%), Iran (6.18%), China (4.07), USA (3.40%), Turkey (2.12%), and Germany (2.07%) (https://www.worldometers.info/coronavirus/seen on 09 April 2020).
Indian perspective
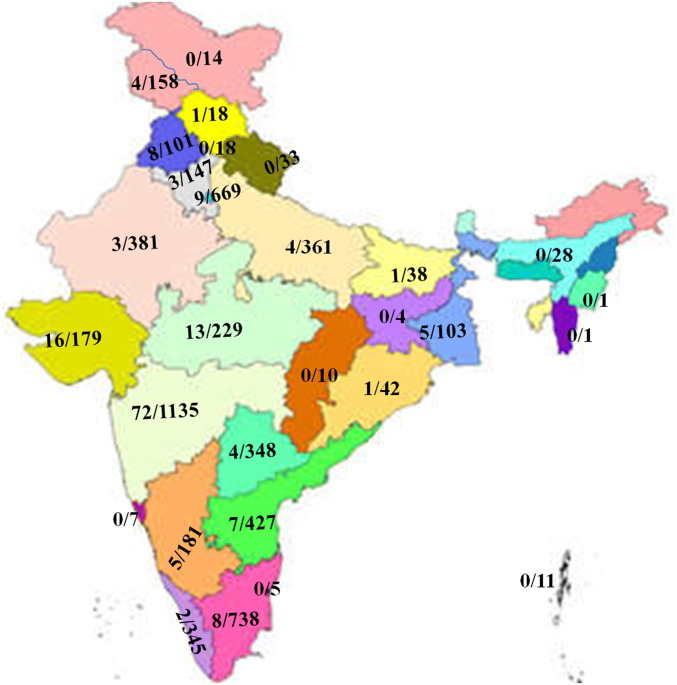
The COVID-19 was started in India from Kerala through the three students who returned from Wuhan, China. Up to 09 April 2020, more than a hundred confirmed cases of COVID-19 were identified from various parts of India; the majority of them have travel history to affected regions. Meanwhile, the first death was reported on 12 March 2020. The first victim was a 76-year-old man, who had returned from Saudi Arabia. COVID-19 accelerates its speed of infections, 1000 on 28 March and 1834 with death toll crossed 41 on 1 April, 2020. The numbers of cases are very less as compared to other countries, as India is the second-largest populated, developing country of the world with insufficient medical facilities. More than two million persons were screen, out of which 5734 are positive for COVID-19 by laboratory-confirmed assays, from which 166 (2.9%) die, 473 (8.25%) recovered included one migrated, while 5095 active cases are admitted in various hospitals shown in Fig. 1(https://www.mohfw.gov.in/seen on 09th April, 2020). Maharashtra (1135), Tamil Nadu (738), Delhi (669), Telangana (427), Rajasthan (381), Uttar Pradesh (361), Andhra Pradesh (348), Kerala (345), Madhya Pradesh (229), Karnataka (181) Gujarat (179) and Jammu, and Kashmir (158) are most affected sates contained 5151 out of 5734 (90%) of total laboratory-confirmed cases of COVID-19. The Distribution of deaths and laboratory-confirmed cases of COVID-19 in various Indian states and union territories as on 09th April, 2020 is shown in Fig. 2. (https://www.mohfw.nic.in/seen on 01 April 2020).
Fig. 1.
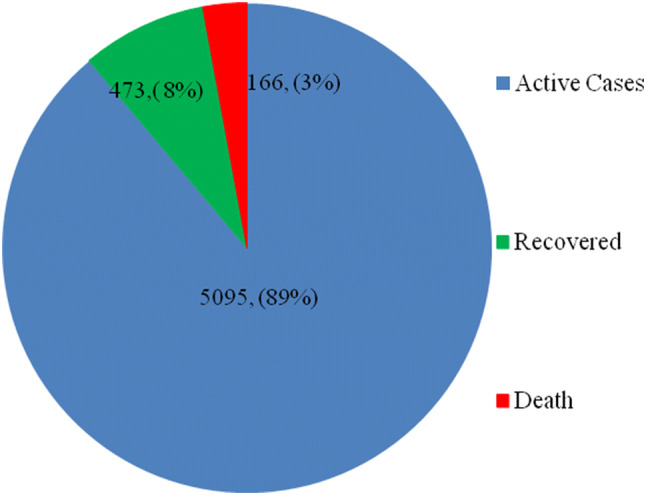
Distribution pattern of total active cases, recovered and number of deaths due to COVID-19 in India as on 09th April, 2020.
Source: https://www.mohfw.gov.in/seen on 09th April, 2020
Fig. 2.
Distribution of deaths and laboratory-confirmed cases of COVID-19 in various Indian states and union territories as on 09th April, 2020.
Source: https://www.mohfw.gov.in/seen on 09th April, 2020
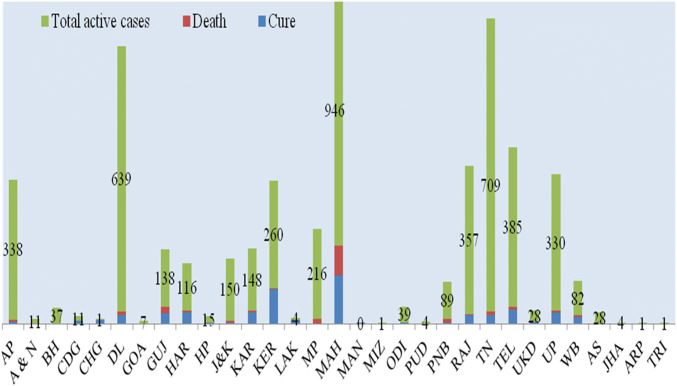
Some persons recovered from COVID-19, the distribution pattern of recover, deaths and active cases in various Indian states as of 01 April 2020 given in Fig. 3 (https://www.mohfw.gov.in/seen on 09th April, 2020). A total of 166 persons died, out of which 126 (75.90%) were from Maharashtra (72), Gujarat (16), Madhya Pradesh (13), Delhi (9), Tamil Nadu (8) and Punjab (8). Forty persons were died from the Telangana (7), Karnataka (5), West Bengal (5), Andhra Pradesh (4), J & K Kashmir (4), Uttar Pradesh (4), Haryana (3) Rajasthan (3), Kerala (2), Bihar (1), Himachal Pradesh (1) and Odisha (1) are shown in Fig. 4. (https://www.mohfw.gov.in/seen on 09th April, 2020)
Fig. 3.
Distribution of Recover, Deaths and Active cases (label) of Coronavirus (COVID-19) in various Indian states as of 01 April 2020. AP Andhra Pradesh, A&N Andaman and Nicobar Islands, BH Bihar, CDG Chandigarh, CHG Chhattisgarh, DL Delhi, GOA Goa, GUJ Gujarat, HAR Haryana, HP Himachal Pradesh, J&K Jammu and Kashmir, KAR Karnataka, KER Kerala, LAK Ladakh, MP Madhya Pradesh, MAH Maharashtra, MAN Manipur, MIZ Mizoram, ODI Odisha, PUD Puducherry, PNB Punjab, RAJ Rajasthan, TN Tamil Nadu, TEL Telangana, UKD Uttarakhand, UP Uttar Pradesh, WB West Bengal, AS Assam, JHA Jharkhand, ARP Arunachal Pradesh, TRI Tripura.
Source: https://www.mohfw.gov.in/seen on 09th April, 2020
Fig. 4.

Distribution of deaths and laboratory-confirmed cases of COVID-19 in various Indian states and union territories as on 09th April, 2020.
Source: https://www.mohfw.gov.in/seen on 09th April, 2020
The distribute pattern COVID-19 other respiratory depends upon the various factor like their basic reproductive number (R0), nature of the virus, environmental condition, trade/travel with the affected area, population density and social culture. The basic reproductive number (R0) and nature of the virus are similar for the whole world; therefore the difference of outbreak potential depends on other factors. The WHO data is clearly suggested that colder and humid regions are more affected than warmer and dry regions (https://www.worldometers.info/coronavirus). In India, initial outbreaks started in the regions, which are directly linked to the affected area via trade/travel. In expert opinion, the number of COVID-19 cases could be more but diagnostic rates of India are very low as compared with other countries. The majority of the confirmed cases were linked to other countries; therefore all tourist visas were suspended and ban the entry from effected parts to reduce the chance of infections (https://mea.gov.in/covid-19-updates.htm). To hamper the virus spread in the community, educational institutions and many other commercial activities have been shut down. To reduce the COVID-19 spread, a 14-hour voluntary public curfew was observed in the whole country at the request of Prime Minister, Modi. The government followed it up with lockdowns in COVID-19 affected parts and major cities. The Prime minister ordered a national lockdown for 21 days on 24 March 2020 (https://www.independent.co.uk). Some person does not follow the instruction; become the super spreader of COVID-19. A Sikh preacher has a travel history of the infected area (Italy and Germany) attending a Sikh festival in Anandpur Sahib on 7 March. As a result, twenty-seven positive cases of COVID-19 were identified and more than 40,000 people belong to 20 villages of Punjab needed to be quarantined. In another case, more than 2000 people including 281 foreigners attending Tablighi Jamaat religious congregation event was organized in Delhi and staying at the mosque since 8 March. About 200 people have shown symptoms, out of which, 24 people were positive for COVID-19 so far. A large number of COVID-19 cases across the country were found to be linked to the event (https://www.mohfw.gov.in). Michael Ryan, chief executive director of WHO seems to be happy with Indian efforts to control COVID-19. The COVID-19 not only dangerous for our health but the Indian economy is highly affected due to the lockdown. A large segment of the Indian population, lose their livelihood due to shut down of trades, commercial, tourist and other business activities during the lockdown.
Clinical symptoms
The clinical symptoms of COVID-19 are very similar to influenza and other respiratory viruses. The clinical symptoms and severity of COVID-19 may be variable. Three relatively large-scale studies done on 278 pooled patients in Wuhan, China suggesting that COVID-19 causes viral pneumonia. All of the patients were adults with more than 18 years of age, consist of 172 (61.9%) males and 106 (38.1%) females [4, 10, 35]. A recent study in Beijing reported that 2 of the 13 patients with COVID-19 pneumonia were children aged 2–15 years [3]. Co-morbidity like cardiovascular, hypertension, diabetes and age of patients also plays a crucial role in disease output. An adult person without any serious co-morbidity was recovered easily while aged person co-morbidity with required intensive care and a ventilator [3, 35]. Similar observations were noted in Indian patients also. The patients come with unexplained upper respiratory viral infection. The majority of patients have symptoms of fever, cough, sore throat, nasal congestion, malaise, and headache. The elderly and other immunocompromised patients have more and severe atypical symptoms. Although, dehydration, sepsis or shortness of breath are absent in these patients [12].
Diagnosis
All coronavirus infections need not be diagnosed as they are self-limited and cause mild upper respiratory infection only. Clinical symptoms of coronavirus and other respiratory viruses are very mimic. Their accurate diagnosis is possible by laboratory-based assays. Initially, coronavirus can be diagnosis by virus-isolation, electron microscopy, serological methods and in later stages (after genomic sequences), molecular assays are priority. Virus isolation is a gold standard but time-consuming and high containment level required. Virus isolation is not a good method of diagnosis but produced a good amount of viruses at the end, which can be utilized for further antigenic and molecular characterizations. Electrons microscopy is costly and highly expert persons required for viral identification. Serological methods are good but pair serum required for confirmation. In the modern era of time, molecular diagnosis assays are more rapid, sensitive, specific and cost-effective for viral diagnosis [7, 29]. COVID-19 was diagnosis by Real-time RT-PCR after the availability of the full genomic sequence of the viruses [5, 37]. In India, the suspected patients are select as per country and/or WHO guidelines; the appropriate samples should be collected in the early phase of infection. The samples should collect after proper wearing of personal protective equipment (PPE) [36]. The collected samples should be transported in the virology laboratory in cold conditions. In the virology laboratory, the sample will be processed and standardized assay will be applied for the diagnosis. In India, All the COVID-19 diagnoses done in more than a hundred NABL accredits virology laboratories. COVID-19 is diagnosis by the Real-time RT-PCR by following the WHO protocol and ICMR guidelines.
Prevention and treatment
A reliable vaccine or antiviral could be the best answer for any virus. In the absence of these, prevention is only the choice. The outbreaks of MERS, SARS, Nipah [30], Zika [31], give a lesson to us that social distance, frequent hand-washing, avoiding contact of animals and infected persons will protect us. The COVID-19 is similar to other respiratory viruses, can be transmissions from infected to susceptible persons, via droplets, contaminated body parts, and objectives. A susceptible person got the infection through these contaminated objectives, amplify the virus and spread to other persons. The infected or suspected person should follow the cough etiquette, maintain distance, cover coughs/sneezes via tissues or clothing, frequently wash their hands and safe dispose-off infected material to a reduced viral transmission. The hospital, diagnostic laboratory, emergency departments, and other health care facilities should follow standard infection prevention and control practices to avoid nosocomial infections [21]. In India, COVID Care Centres (CCC) is set up in public or private hostels, hotels, schools, stadiums, lodges etc. COVID suspected patients can be divided into three; Groups a): These are suspect cases with mild fever and upper respiratory tract infection. They may be admitted and screen for COVID-19. Negative patients should discharge after the symptomatic management while COVID-19 positive patients need to be admitted to CCC. Their health monitor regularly and symptomatic treatment will be given. Group b): Suspect pneumonia with respiratory rate 15–30/min and SpO2 90–94% come under moderate categories. They will be admitted as suspect cases in section of dedicate COVID-19 health centre and screen for infections of COVID-19. Negative patients transfer to Non-COVID hospital/block and manage according to clinical assessment and discharge as per clinical assessment. While COVID-19 positive need to shift into the confirmed case section of CCC. Monitor for clinical severity can be shift to COVID-19 dedicated hospital. Their health monitor regularly and symptomatic treatment will be given. Group c): COVID-19 suspect patient with pneumonia and respiratory rate more than 30/minute and SpO2 more than 94% come under severe categories. They will be admitted to dedicating COVID-19 health centres with ICU facilities and screen for infections of COVID-19. Negative patients should be a shift to Non-COVID hospital/block. While COVID-19 positive patients should be remain in ICU and their management will be done according to clinical assessment. They can be discharged as per clinical assessment after their negative reports (https://www.mohfw.gov.in). In case of absence treatment, quarantine and supportive care (oxygen therapy, fluid management, antimicrobials antibiotic, etc. can be given to the patients. Some antiviral like Remdesivir, lopinavir-ritonavir and interferon-α 2b and other drug was tried to control the 2019-nCoV but expecting results were not obtained. There is no specific antiviral available against CVID-19. Hydroxychloroquine (Dose 400 mg BD for 1 day followed by 200 mg BD for 4 days) with the combination of Azithromycin (500 mg OD for 5 days) can be given under the close medical supervision (https://www.mohfw.gov.in). The government should do continuous surveillance, screening the traveler comes from infected areas; develop timely diagnostics, therapeutics, vaccines [9].
Acknowledgement
Sulochana Kaushik and Yashika Sharma acknowledge their financial supports received from Maharshi Dayanand University, Rohtak for the award of University Research Scholarship to them.
Funding
For review article does not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Biscayart C, Angeleri P, Lloveras S, Chaves TD, Schlagenhauf P, Rodríguez-Morales AJ. The next big threat to global health? 2019 novel coronavirus (2019-nCoV): What advice can we give to travellers?-Interim recommendations January 2020, from the Latin-American society for Travel Medicine (SLAMVI) Travel Med Infectious Dis. 2020;33:101567. doi: 10.1016/j.tmaid.2020.101567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carlos WG, Cruz D, Cs CB, Pasnick S, Jamil S. Novel Wuhan (2019-nCoV) Coronavirus. Am J Respir Crit Care Med. 2020;2020(201):P7–P8. doi: 10.1164/rccm.2014P7. [DOI] [PubMed] [Google Scholar]
- 3.Chang D, Lin M, Wei L, Xie L, Zhu G, Cruz CS, Sharma L. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. JAMA. 2020;323:1092–1093. doi: 10.1001/jama.2020.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen J. Chinese researchers reveal draft genome of virus implicated in Wuhan pneumonia outbreak. Washington, DC: American Association for the Advancement of Science, 2020. https://www.sciencemag.org/news/2020/01/chinese-researchers-reveal-draft-genome-virus-implicated-wuhan-pneumonia-outbreak.
- 6.De Wilde AH, Snijder EJ, Kikkert M, van Hemert MJ. Host factors in coronavirus replication. In Roles of Host Gene and Non-coding RNA Expression in Virus Infection 2017 (pp. 1–42). Springer, Cham. https://link.springer.com/chapter/10.1007/82_2017_25. [DOI] [PMC free article] [PubMed]
- 7.Dhull D, Sharma V, Sharma Y, Kaushik S. Applicability of molecular assays for detection and typing of herpes simplex viruses in encephalitis cases. Virus Dis. 2019;30:504–510. doi: 10.1007/s13337-019-00558-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Escors D, Ortego J, Laude H, Enjuanes L. The membrane M protein carboxy terminus binds to transmissible gastroenteritis coronavirus core and contributes to core stability. J Virol. 2001;75:1312–1324. doi: 10.1128/JVI.75.3.1312-1324.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain S, Chen Y, Yang Y, Xu J, Peng Y, Wu Y, Li Z, Zhu Y, Tien P, Guo D. Identification of novel subgenomic RNAs and noncanonical transcription initiation signals of severe acute respiratory syndrome coronavirus. J Virol. 2005;79:5288–5295. doi: 10.1128/JVI.79.9.5288-5295.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kachroo V. Novel Coronavirus (COVID-19) in India. Curr Scenar. 2020;7(3):435–447. doi: 10.20944/preprints202003.0436.v1. [DOI] [Google Scholar]
- 13.Lai MM, Cavanagh D. The molecular biology of coronaviruses. Adv Virus Res. 1997;48:1–100. doi: 10.1016/S0065-3527(08)60286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC, Choe H. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Locker JK, Rose JK, Horzinek MC, Rottier PJ. Membrane assembly of the triple-spanning coronavirus M protein. Individual transmembrane domains show preferred orientation. J Biol Chem. 1992;267:21911–21918. doi: 10.1016/S0021-9258(19)36699-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu G, Hu Y, Wang Q, Qi J, Gao F, Li Y, Zhang Y, Zhang W, Yuan Y, Bao J, Zhang B. Molecular basis of binding between novel human coronavirus MERS-CoV and its receptor CD26. Nature. 2013;500:227–231. doi: 10.1038/nature12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020 doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel coronavirus emerging in China—key questions for impact assessment. N Engl J Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 21.Patel A, Jernigan DB. Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak—United States, December 31, 2019–February 4, 2020. Morb Mortal Wkly Rep. 2020;69:140. doi: 10.15585/mmwr.mm6905e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paules CI, Marston HD, Fauci AS. Coronavirus infections—more than just the common cold. JAMA. 2020;323:707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 23.Perrier A, Bonnin A, Desmarets L, Danneels A, Goffard A, Rouillé Y, Dubuisson J, Belouzard S. The C-terminal domain of the MERS coronavirus M protein contains a trans-Golgi network localization signal. J Biol Chem. 2019;294:14406–14421. doi: 10.1074/jbc.RA119.008964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38:1–9. doi: 10.12932/AP-200220-0772. [DOI] [PubMed] [Google Scholar]
- 25.Qian Z, Travanty EA, Oko L, Edeen K, Berglund A, Wang J, Ito Y, Holmes KV, Mason RJ. Innate immune response of human alveolar type ii cells infected with severe acute respiratory syndrome–coronavirus. Am J Resp Cell Mol. 2013;48:742–748. doi: 10.1165/rcmb.2012-0339OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raj VS, Mou H, Smits SL, Dekkers DH, Müller MA, Dijkman R, Muth D, Demmers JA, Zaki A, Fouchier RA, Thiel V. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251–254. doi: 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riley S, Fraser C, Donnelly CA, Ghani AC, Abu-Raddad LJ, Hedley AJ, Leung GM, Ho LM, Lam TH, Thach TQ, Chau P. Transmission dynamics of the etiological agent of SARS in Hong Kong: impact of public health interventions. Science. 2003;300:1961–1966. doi: 10.1126/science.1086478. [DOI] [PubMed] [Google Scholar]
- 28.Sawicki SG, Sawicki DL. Coronavirus transcription: a perspective. In Coronavirus replication and reverse genetics 2005 (pp. 31–55). Springer, Berlin, Heidelberg. https://link.springer.com/chapter/10.1007/3-540.
- 29.Sharma V, Chaudhry D, Kaushik S. Evaluation of clinical applicability of reverse transcription-loop-mediated isothermal amplification assay for detection and sub-typing of Influenza A viruses. J Virol Methods. 2018;253:18–25. doi: 10.1016/j.jviromet.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharma V, Kaushik S, Kumar R, Yadav JP, Kaushik S. Emerging trends of Nipah virus: a review. Rev Med Virol. 2019;29:e2010. doi: 10.1002/rmv.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharma V, Sharma M, Dhull D, Sharma Y, Kaushik S, Kaushik S. Zika virus: an emerging challenge to public health worldwide. Can J Microbiol. 2020;66:87–98. doi: 10.1139/cjm-2019-0331. [DOI] [PubMed] [Google Scholar]
- 32.Snijder EJ, Bredenbeek PJ, Dobbe JC, Thiel V, Ziebuhr J, Poon LL, Guan Y, Rozanov M, Spaan WJ, Gorbalenya AE. Unique and conserved features of genome and proteome of SARS-coronavirus, an early split-off from the coronavirus group 2 lineages. J Mol Biol. 2003;331:991–1004. doi: 10.1016/S0022-2836(03)00865-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Su S, Wong G, Shi W, Liu J, Lai AC, Zhou J, Liu W, Bi Y, Gao GF. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24:490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization (WHO). Novel coronavirus (2019-nCoV). Situation report. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200207-sitrep-18-ncov.pdf?sfvrsn=fa644293_2. Accessed on 9 Feb 2020.
- 37.World Health Organization. Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases: interim guidance. Geneva: WHO. 2020. https://apps.who.int/iris/handle/10665/330676. Accessed on 31 Jan 2020.
- 38.Yoo JH. The fight against the 2019-nCoV outbreak: an arduous march has just begun. J Korean Med Sci. 2019 doi: 10.3346/jkms.2020.35.e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W, Lou Y, Gao D, Yang L, He D, Wang MH. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214–217. doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]