Abstract
Introduction
Regular physical activity (PA) participation has many important physical and psychological health benefits, managing and preventing over 25 chronic conditions. Being more physically active as a child is associated with being more active as an adult, but less than 10% of Canadian children are achieving the recommended PA guidelines of 60 minutes per day of moderate to vigorous PA. Parental support is a predictor of child PA, but parent intention to support child PA does not always predict enacted support. Targeting factors that assist in the sustainability of parent support behaviour of child PA may have an impact on child PA. The purpose of this study is to evaluate an intervention designed to promote habit formation of parental support (HABIT, independent variable) on child PA (dependant variable) compared with a planning and education group (PLANNING) and an education only group (EDUCATION).
Methods and analysis
The three conditions will be compared using a 6-month longitudinal randomised trial. Eligible families have at least one child aged 6–12 years who is not meeting the 2011 Canadian PA Guidelines. Intervention materials are delivered at baseline, with check-in sessions at 6 weeks and 3 months. Child’s moderate-to-vigorous PA, measured by accelerometry, is assessed at baseline, 6 weeks, 3 months and 6 months as the primary outcome. At baseline and 6 months, children perform fitness testing. Parents and children complete questionnaires at all timepoints. So far, 123 families have been recruited from the Greater Victoria and surrounding area. Recruitment will be continuing through 2020 with a target of 240 families.
Ethics and dissemination
This protocol has been approved by the University of Victoria Human Research Ethics Board (Victoria, Canada). Results will be shared at conferences as presentations and as published manuscripts. Study findings will be made available to interested participants.
Trial registration number
Keywords: public health, preventive medicine, sports medicine
Strengths and limitations of this study.
This randomised trial will build on family-based physical activity (PA) research evaluating whether building parent support habit for child PA is an effective strategy to promote child PA.
The findings of this study can inform health policy and programmes designed to improve health outcomes in children through increasing PA.
It is possible that results may be affected by participants unconsciously adopting techniques from different conditions (eg, the EDUCATION participant employs planning technique and PLANNING participant employs habit forming techniques).
Inclusion of quantitative and qualitative manipulation checks will be useful for assessing intervention fidelity.
Introduction
Physical activity (PA) has the potential to reduce the risk of at least 25 chronic medical conditions by 20%–30%,1 yet Canadian adults and children are not meeting recommended guidelines to optimise these benefits.2 3 Children are recommended to achieve 60 minutes (min) per day of moderate to vigorous physical activity (MVPA).4 For adults, 150 min of MVPA per week is recommended.5 While many complications and diseases present in adulthood, there is compelling evidence showing the positive impact of increased PA among children on health. PA can help to guard against high blood pressure, high cholesterol, metabolic syndrome, low bone density, depression and obesity; also, there is evidence demonstrating a relationship between increased MVPA and reduced psychological distress, improved peer relations and improved quality of life/well-being.6–8 Unfortunately, according to the Canadian Health Measures Survey, only 9% of boys and 4% of girls are achieving the recommended amount of PA.3 9 Understanding the factors that influence child PA is therefore important for promoting long-term population health.
Parental influence is one such factor; a review of family-based interventions to increase PA found that parent support was a consistent determinant of child PA.10 Parent support refers to the ways in which parents knowingly influence their child’s PA and includes both tangible (eg, transportation) and intangible (eg, encouragement) behaviours.11 Interventions focused on parent support to change child PA have been generally unsuccessful, however, as reported in several reviews.12–15 More recent intervention research has shown some positive effects,16–18 but these are still balanced by several null results.19–21 A recent study found that while most parents have positive intentions to support child health behaviours, few substantively enact this support.22 Furthermore, this intention–behaviour gap does not appear to be successfully bridged by current interventions targeting parents. For example, a review10 found that the majority of interventions focus on educating parents on the benefits of PA, which does not appear to drive subsequent PA change (among parents and their children). This is likely because parents are already aware of the health benefits of PA for their children,23–25 in addition to already having the intention to support behaviour.22 Therefore, focusing on what parenting support can be harnessed (ie, malleable through intervention) to promote child physical activity represents an important avenue of enquiry.
Several recent theoretical approaches have advanced beyond merely building intention to perform behaviour and suggest that building self-regulatory tactics such as planning is critical to bridge the intention–behaviour gap.26–28 This approach has been used in family interventions,10 yet it may not be sufficient to sustain behaviour changes over longer durations. For example, the Family Physical Activity Planning study22 compared an intervention group focused on family PA planning (goal setting, action planning and coping planning) to an education only group and found increased child PA at 3 months in the family planning group. This effect was not observed at 6 months, however, demonstrating a need to target behavioural strategies beyond mere planning for successful maintenance of PA.
The Multi-Process Action Control (M-PAC) Framework29 30 may assist in sustaining health behaviours such as parental support of child PA. This framework suggests that self-regulatory skills and tactics assist in translating intentions into behaviour during the initial adoption of physical activity, but sustainability is also determined by the development of habit across time to ease the burden of continual volitional motivation and self-regulation. Habits represent impulses to perform behaviour initiated via stimulus–response bonds,31 and contribute to PA largely via repeated consistency in behavioural practices, salient cues associated with behavioural initiation and affectively rewarding behaviour.32–34 Consistent with M-PAC theory, habit formation has seen promising results in PA research31 35 36; habits may sustain PA behaviour over time partially independent of goals (or intentions)35 37 and through helping turn intentions into actual behaviour.30 Of particular relevance to the current trial, a recent study evaluating parent support of child PA with M-PAC found parent habit to be the largest independent correlate with the translation of intention into behaviour compared with planning and motivational constructs.38
Study objectives and hypotheses
The primary objective of this study is to implement a theory-based intervention targeting parental support of child MVPA comparing the effect of a PA habit formation+PA planning+PA education (HABIT) condition to a PA planning+PA education (PLANNING) condition and a PA education only group (EDUCATION) on child MVPA (dependant variable). The primary end-point of this trial is 6 months, with additional secondary time points of 6 weeks and 3 months. Based on previous research,38 39 it is hypothesised that children of families in the HABIT condition will demonstrate a greater increase MVPA measured by accelerometry at 6 months compared with those in the PLANNING group and the EDUCATION group. As per the results of Rhodes et al’s family PA planning intervention,22 we expect children of families in the PLANNING group will demonstrate a greater increase in MVPA compared with the EDUCATION group; however, this effect may diminish over time.
Secondary objectives include evaluating child fitness at baseline and 6 months. It is hypothesised that child fitness will be greater for the HABIT condition compared with the PLANNING and EDUCATION conditions at 6 months because of the resulting increased PA hypothesised above. Tertiary objectives include evaluating parent PA and quality of life. While parent and child coparticipation in PA is not mandatory, parent support of child PA may include coparticipation (such as a family walk), and therefore, it is expected that parents in the HABIT condition will report higher PA via some activities being performed with their children in comparison with the other conditions. Finally, no differences in gender or season are hypothesised. The climate in Victoria is relatively mild, and outdoor activities continue throughout the year. Seasonal effects (eg, potentially less outdoor physical activity participation during winter months or less structured sport participation during summer months) are also expected to be balanced to a certain extent by the selected recruitment method. Rolling recruitment ensures that participants are at all stages of participation during all seasons. Finally, there is not sufficient evidence at this point to support that boys and girls will respond differently to a habit-based physical activity intervention.
Trial design
This study is a three-arm parallel design single-blinded randomised trial. After baseline assessment (MVPA, fitness testing and questionnaire), families are randomised to one of three groups: (1) family PA habit formation+planning+education (HABIT); (2) family PA planning+education (PLANNING); and (3) standard PA education (EDUCATION). The trial is testing the superiority of the HABIT condition. Randomisation is performed by the project coordinator using Excel Sheet Randomization with an allocation ratio of 1:1:1. Participants are blind to their condition until their participation in the study is complete, at which point they are informed of their group by the project coordinator and/or research assistant. Under no circumstance will participants be informed of their condition while they are still enrolled in the study. Fitness testers are blind to each family’s condition, but the intervention delivery team is aware of the condition to allow for correct delivery of intervention materials.
Methods
The study has been approved by the University of Victoria Human Research Ethics Board (HREB). The design, conduct and reporting of the trial has and continues to follow the Standard Protocol Items: Recommendations for Interventional Trials guidelines.40 The trial is registered with the Clinical Trials Registry at the National Library of Medicine at the National Institutes of Health (ClinicalTrials.gov). See table 1 for WHO Trial Registration Data Set items.
Table 1.
WHO trial registration data set items
| Data category | Information |
| Primary registry and trial identifying number | ClinicalTrials.gov # NCT03145688. |
| Date of registration in primary registry | Submitted 27 January 2017, version 1 finalised and released 4 May 2017. |
| Secondary identifying numbers | Unique Protocol ID: 35941 51 350. |
| Source(s) of monetary or material support | Heart and Stroke Foundation of Canada. |
| Primary sponsor | Heart and Stroke Foundation of Canada. |
| Secondary sponsor(s) | n/a |
| Contact for public queries | EM, MSc. ermedd@uvic.ca, 250-721-8384. |
| Contact for scientific queries |
EM, MSc. Behavioural Medicine Lab, Victoria, Canada. |
| Public title | Family habit physical activity study. |
| Scientific title | Promoting habit formation in family physical activity. |
| Countries of recruitment | Canada. |
| Health condition(s) or problem(s) studied | Child physical activity. |
| Intervention(s) | Family based education, planning and habit formation. |
| Key inclusion and exclusion criteria | Ages eligible for study: families with children 6–12 years. Accepts healthy volunteers: yes. Inclusion criteria: child achieving less than 60 min of moderate to vigorous physical activity per day. Exclusion criteria: child achieving more than 60 min of moderate to vigorous physical activity per day. |
| Study type | Interventional. Allocation: randomised. Intervention model: parallel assignment. Masking: single blind (participants). Primary purpose: evaluate intervention designed to improve child physical activity through promoting parent support habit. |
| Date of first enrolment | February 2017. |
| Target sample size | 240 families. |
| Recruitment status | Recruiting. |
| Primary outcome(s) | Child moderate to vigorous physical activity. |
| Key secondary outcomes | Child fitness, parent support habit. |
In the case of protocol modifications or amendments, the project coordinator submits the appropriate documentation to the HREB at the University of Victoria. Once approved, the project coordinator then updates the trial information on the Clinical Trials Registry.
Patient and public involvement
No funds or time were allocated for patient (participant) and public involvement in this study. Participants were not invited to comment on the study design and were not consulted to develop participant relevant outcomes or interpret the results. Participants will not be invited to contribute to the writing or editing of this document for readability or accuracy. Participants are given the opportunity to share their experience in the wrap up interview providing information that will help inform future research.
Participants
Single or common law/married adult(s), with at least one child between the ages of 6 and 12 years, living in greater Victoria (including the Capital Regional District, Westshore Communities and Sooke) British Columbia, Canada, are being recruited for this study. If more than one child is eligible in this range, one child is randomly (computer randomiser) designated as the target for analysis, yet all willing children are included in the study. Families are included if the child participant is achieving less than the recommended 2011 Canadian PA guidelines of 60 min of MVPA daily.5
The age group of 6–12 years was selected from our earlier pilot work.18 Specifically, children under 6 years of age engage in physical activity that is quite sporadic and thus very different than children 6 years and older.41 Our decision to limit the age of children to 12 years was more practical; 12-year-old children represent the upper bound of the ‘tweens’, where parents are still very influential in PA decisions and PA interventions at the level of the parent would be still effective.12 42
Recruitment
Recruitment is being conducted by the Behavioural Medicine Lab at the University of Victoria in British Columbia, Canada. Parents with one or more children aged 6–12 years are the primary target for recruitment. Victoria’s population is representative of Canada: according to data from the 2016 Canadian census, the age distribution, family structure and income of Victoria residents are similar to those of Canada.43
Participants are being recruited through the social media platforms Facebook and Instagram, posters at community facilities, in person at local markets and festivals and through word of mouth. Facebook and Instagram posts are made bimonthly by the Behavioural Medicine Lab recruitment officer on the Behavioural Medicine Lab Facebook page (https://www.facebook.com/UVicBMED/) and Instagram account (@uvicbmed), which are linked, meaning a post made on Facebook is simultaneously shared on Instagram and vice versa. Posts are limited to 100 words or less and briefly describe the intent of the study and those eligible to partake, asking those interested to contact the Behavioural Medicine Lab through email or phone information provided in the post. Facebook posts are also shared to relevant Facebook groups (eg, neighbourhood groups and young parent groups). Facebook posts are ‘boosted’ by paying a small fee to have the post appear as an ad in a target demographic’s news feed. This increases the reach of the Facebook post with the goal of increasing recruitment. The target demographic is specified by selecting variables of age, location of residence and other filters such as ‘parents’, and the ads typically run for 7 days. The Recruitment officer also sets up a recruitment booth twice per month at local markets and festival events during the summer and at community and recreation centres in the winter to engage with potential participants, answer questions and collect contact information for interested families. Posters are put up every 3–4 months by a research assistant and/or recruitment officer in all major recreation centres in the area, as well as shopping centres, healthcare centres and schools. Word of mouth is also used as a recruitment strategy by asking participants to share information about the study with acquaintances. Since participants self-select, application of the results will be limited to families already interested in supporting their child’s PA.
Enrolment
When interested parents contact the lab, the recruitment officer(s) follows up with an email to schedule a phone conversation. If initial contact is a message through Instagram or Facebook, the recruitment officer replies asking the person to call/email or provide their contact information to be contacted by phone or email. An initial recruitment phone interview is set up with the recruitment officer. Participant families are screened by parent report of average child PA per day as well as the ParQ+ Health Screening Questionnaire.44 If screened in, then the recruitment officer books the baseline fitness test and advises the project coordinator who follows up with the family and schedules a fitness tester for the baseline session. Fitness testers are all certified personal trainers or clinical exercise physiologists registered with the Canadian Society for Exercise Physiology.
During the baseline session, the fitness tester obtains written consent from parents and verbal consent from children (see online supplementary appendix 1). Participants are asked not to participate in any other research studies while enrolled in the present study. After the baseline session, children wear an accelerometer for 7 days. The intervention delivery session is scheduled after the week of accelerometer wear; once scheduled, the project coordinator randomly assigns the family to one of the three conditions and prepares the appropriate materials for the research assistant to take with them to the participants’ home. The research assistants are kinesiology and psychology undergraduate and graduate students. These are paid positions that involve thorough training in the lab and in the field. Training involves review of a training manual and the research study materials, shadowing sessions with experienced research assistants, and practising delivering sessions with other research assistants. Research Assistants must successfully demonstrate all participant appointments to the project coordinator to confirm that they are ready to take the lead on these deliveries and check ins with participants on their own.
bmjopen-2019-033732supp001.pdf (1.1MB, pdf)
Participating families receive an honorarium at baseline ($25), 6 weeks ($30), 3 months ($35) and 6 months ($40) for a total of $130. Families only receive honorariums if they complete all the measures for the check in (accelerometers, logbooks and questionnaires).
Intervention
The intervention is conducted in-person with a research assistant and the family at the family home and includes take away material for the families to use later on. The material is a condition-specific PA workbook and serves as a template for the dialogue between the research assistant and families during the intervention delivery. The research assistant explains each section of the book to families as per the intervention delivery script from the training manual, answering questions as needed and ensuring that families are comfortable to complete the workbook in the coming weeks. Families are asked not to share any information with any acquaintances who happen to be participating in the same study. Intervention delivery sessions range from 25 min to 40 min in length depending on the condition and the family.
The workbook is designed for families with information directed at the parent to review with the child, sections for parents and children to complete together and some sections for the parent to complete on their own. The material incorporates established behaviour change techniques to promote child PA. The full list of behaviour change techniques employed in each condition are summarised in table 2 as per Michie et al’s45 Behaviour Change Taxonomy (BCT). These techniques are incorporated in the workbook and reinforced by the discussion between the research assistant and the family.
Table 2.
Description of intervention components and associated behaviour change techniques
| Intervention condition | Resources included in booklet | Physical activity behaviour change techniques | BCT taxonomy construct |
| Education | Canadian 24-hour Movement Guidelines: included list of benefits of physical activity. | Instruction on how to perform a behaviour. | 4.1 |
| Information about health consequences. | 5.1 | ||
| Salience of consequences. | 5.2 | ||
| Information about social and environmental consequences. | 5.3 | ||
| Information about emotional consequences. | 5.6 | ||
| Planning (includes education condition resources) |
Goal setting materials. Explanation of SMART goals (specific, manageable, achievable, realistic, timely), self-monitoring. Family physical activity planning worksheets: included brainstorming worksheets for where to be active, new modes for being active, how to plan activity, how to incorporate rewards and journaling and tracking worksheets. |
Goal setting (behaviour). | 1.1 |
| Problem solving. | 1.2 | ||
| Action planning. | 1.4 | ||
| Self-monitoring of behaviour. | 2.3 | ||
| Self-monitoring of outcome(s) of behaviour. | 2.4 | ||
| Social support (practical). | 3.2 | ||
| Social support (emotional). | 3.3 | ||
| Non-specific reward. | 10.3 | ||
| Self-incentive. | 10.7 | ||
| Restructure physical environment. | 12.1 | ||
| Restructure social environment. | 12.2 | ||
| Habit (includes education and planning group resources) |
Habit building resources. Explanation and examples of habits, introduction to cues and anchoring, brainstorming and planning worksheets. |
Prompts/cues. | 7.1 |
| Behavioural practice/rehearsal. | 8.1 | ||
| Habit formation. | 8.3 |
Behaviour change techniques are coded as outlined by the Behaviour Change Technique (BCT) Taxonomy Version 1.45
The three intervention conditions follow and advance the prior work conducted in our successful habit formation pilot trial32 and feasibility study, but now tested in comparison with our work on family physical activity planning.18 22 46 The condition of key interest (HABIT) is focused on the behaviour change technique of habit formation with the goal of impacting initiation of parental physical activity support and not the actual execution of child physical activity or execution of support behaviour, which may be quite mindful.47 Contemporary research has shown that habits in the PA domain can be discerned into habitual instigation—whereby, in this instance, a parent non-consciously ‘decides’ to provide PA activity support—and habitual execution, whereby a parent non-consciously performs the actions involved in providing PA support.48 49 The HABIT condition is focused on encouraging the formation of instigation habits, such that parents are automatically ‘reminded’ to select PA support (from available alternatives). We are not attempting to promote non-conscious engagement in child PA support (ie, execution habit).
Six-week and 3-month check-ins, or ‘booster’ sessions, are scheduled by the project coordinator with families in all conditions. This involves a 10–15 min house visit by a research assistant to discuss the families’ experience so far. Research assistants follow a check in script included in the training manual and review the intervention delivery materials as needed to support family problem solving (BCT construct 1.2) and promote adherence to the intervention. Based on what the family expresses as personal challenges or barriers, the research assistant will re-emphasise strategies in the workbook that address that concern. For example, if a family expresses difficulty with planning PA, the research assistant will go through the intervention materials again to help the family identify what techniques they can focus on (such as rewards or tracking) and help to brainstorm strategies.
Education condition (EDUCATION)
The standard EDUCATION package consists of the Canadian 24-hour Movement Guidelines for children recommending at least 60 min of MVPA per day and vigorous intensity activities at least three times per week (BCT construct 5.1).4 The guide also contains information about the benefits of PA for children (BCT construct 5.2, 5.3 and 5.6), explanations of what moderate and vigorous intensity activities are, and ideas for physical activities including structured (eg, play a sport) and unstructured (eg, go to the playground) examples (BCT construct 4.1). The research assistant reviews this information with families.
Planning+education group (PLANNING)
Participants in the PA planning intervention condition receive the same guidelines and information as the EDUCATION condition but are also provided with family PA planning material for parents and children to complete together. Goal setting and self monitoring are explained by the research assistant followed by a skill training component, which is a section on how to plan for family PA. The workbook includes a brainstorming exercise for families where they list PAs that they have found fun in the past, as well as activities that they would find enjoyable to do as a family. This brainstormed list helps create the template for PA planning by contextualising what the participants would like to do and the subsequent necessary support behaviours for parents (BCT construct 3.2, 3.3, 12.1 and 12.2). Research assistants explain the exercise and support brainstorming with families as needed.
The skill training material is based on our previous family-based PA interventions that have demonstrated the effectiveness of targeting family based self-regulatory processes such as planning, goal setting, problem solving and self-monitoring for increasing PA outcomes in children.18 22 46 The workbook facilitates goal setting and problem solving (BCT constructs 1.1 and 1.2). Families are instructed to plan for ‘when’, ‘where’, ‘how’ and ‘what’ PA will be performed commensurate with the creation of action planning (BCT construct 1.4) and implementation intentions (eg, refs 50 51). This section is followed by a page on rewards (BCT constructs 10.3 and 10.7) with space for children to brainstorm activities other than PA that they would like to do and that can function as a reward for when children engage in their planned PA. The final page is a journal and tracking sheet for families to log child PA (when, what, where and outcomes, eg, how the child felt and what happened right after) (BCT construct 2.3 and 2.4). The design of all material was created for prior research18 22 46 and features graphic design and colour images that represent family PA. The research assistant reviews each section with families, explains how to complete them and informs them that their participation in the study includes completing the workbook.
Habit+planning+education group (HABIT)
Participants in the habit formation condition receive the same content as the EDUCATION condition and PLANNING condition as well as additional material on creating parent support habits for child PA. As with the other conditions, the research assistant reviews the workbook with families and answers questions as needed. While parent support habit includes the child, this section of the workbook is directed more to the parent as the habit of interest is parental support of child PA. The material is taken from research on habit formation33 and our successful pilot study32 but adapted in our feasibility study to the same colourful style and format as the other information provided. The material includes a brief discussion of what habits are with some very straightforward non-PA related examples such as preparing for sleep routines or selecting the car to commute to work. A key component of the habit section is based on planning for context-dependent repetition (BCT constructs 8.1 and 8.3), with pointers on how to maintain repetition as habit forms. The use of script elicitation to understand/describe existing routines and spot points at which PA support can be inserted follows. This involves a worksheet for parents to brainstorm existing routines in their child’s life (eg, family brunch on Sundays) and then identify what PAs brainstormed in the planning section with the child that might be tagged on to the routine (eg, family walk after brunch every Sunday). This process has been successful in forming habits in other behavioural domains52 as it helps identify reliable and consistent behaviour patterns into which new behaviours may be inserted to optimise the likelihood of the context-dependent performance required for habit to form. Cues are then introduced as factors to support habit formation (BCT construct 7.1). Based on our previously successful trial,32 cues are described as those factors that prompt a behaviour with a discussion of temporal, social, mood and visual cues to support PA.53 Cues are considered factors that: (A) can reliably precede the support activity but (b) rarely be present when the activity is not to be performed. Examples of cues are provided such as a soccer gear bag that is put out in the morning before the family leaves for school and work, which prompts taking the child to soccer when it is seen on the family’s return to the house (visual cue). The soccer gear bag is then removed from sight until the next soccer day. Examples of temporal cues are also provided, such taking the children on a walk with the family dog after dinner, where dinner occurs once a day and can serve to pair well with the family’s new plan to walk. We suggest that cues that are repeatedly present during times when family PA is not performed—for example, a sign on a door that the family walks by all the time—should not be considered, as it reduces the salience of the cue and so its potential for activating the desired action at opportune moments. Parents are reminded of the importance of having consistent support practices for child PA. It is made clear that this does not necessarily mean the same activity all the time, but it means consistent protected time where support is performed so it links with support instigation habits. This could mean child soccer practice every Tuesday night, family PA every Sunday after dinner or encouraging the kids to play in the back yard each day after school. Parents are then asked to brainstorm and create a plan of consistency and cues with the workbooks provided. Parent support of child PA may include coparticipation in PA by the parent (such as the family walk after dinner) or not (such as driving the child to sport practice). The final pages of the HABIT materials are titled ‘Ten tips for turning exercise intentions into actions’ and summarises evidence-based PA promotion practices, presenting the information in an accessible way. The research assistant reviews all sections and worksheets with families, explains how to complete them and informs them that participation in the study includes completing the workbook.
The intervention is discontinued if participants choose to withdraw from the study.
Outcome measures
Differences between the HABIT condition are being tested relative to the PLANNING and EDUCATION conditions.
Primary outcome measure
Child MVPA is measured using 7-day accelerometery with the Actigraph wGT3X-BT Activity Monitor. Child MVPA will be evaluated as change from baseline at 6 weeks, 3 months and 6 months. Child MVPA will be determined using the Evenson54 cutpoints based off of recommendations from Trost et al.55 Evenson cutpoints define moderate activity as 2296–4011 counts per minute (CPM) and vigorous activity as ≥4012 CPM. Therefore, MVPA will be any activity ≥2296 CPM.
Children wear the accelerometer on an elastic belt secured snugly around the waist with the device on their left hip for a minimum of 10 hours per day for seven consecutive days. Participants are instructed to remove the accelerometers for water-based activities as they are not waterproof. A logbook is provided for participants to note when accelerometers were removed for water-based activity or any other reason, provide other details of each day (eg, if their routine was changed for any reason) and record the details of their accelerometer wear days. ActiLife software version 6.11.956 is used to initialise accelerometers and download data and will be used to analyse the data. The accelerometers are initialised to collect prefiltered data at a sample rate of 30 Hz for the children and are downloaded into 10 s epochs to capture the sporadic nature of child PA.57–59 For determining valid wear time, the Troiano algorithm is used, which defines non-wear time as a period of at least 60 consecutive minutes of zero counts, with an allowance for 1–2 min of counts between 0 and 100.60 A minimum of 4 days with at least 600 min per day including at least 1 weekend day of valid wear time will be included in our analyses based on recommended best practice.59 61
Secondary outcome measures
Child PA measures
Children are asked to complete a modified version of the Physical Activity Questionnaire for Children (PAQ-C)62 at baseline, 6 weeks, 3 months and 6 months. This measure is included in addition to accelerometry measured PA as they are not identical measures: including self-report PA will allow for assessment of volitional PA.63 These recall questionnaires were designed to assess regular MVPA in children and adolescents. Frequency of different types of activity as well as intensity are assessed. The PAQ-C was validated against questionnaires, teacher rating, uniaxial accelerometer counts (Caltrac), fitness test (step test) and interview-assisted recall (r=0.39–0.63).62 Questions on barriers to physical activity are also included in these questionnaires to determine PA capability.
Parent report of child PA and family PA are also assessed using a modified Godin Leisure-Time Exercise Questionnaire64 asking frequency and duration of structured versus unstructured PA performed individually (child) and as a family (family).
The baseline and 6-month questionnaires are completed in the lab and the 6-week and 3-month questionnaires are sent as a link in an email to the parent and completed at the participant’s home.
Child health-related fitness
Health-related fitness is assessed in the lab at baseline and 6 months as per the Canadian Assessment of Physical Literacy physical fitness testing protocol.65 The key components of body composition, cardiovascular fitness and musculoskeletal fitness are tested. Body mass (kg), height (cm), body mass index and waist circumference (cm) are measured according to standard procedures. Cardiovascular fitness is assessed by performance on the Leger 20 m shuttle run. Musculoskeletal fitness involves a test of grip strength, the sit and reach test and the plank hold test. All tests are conducted by qualified exercise professionals using specialised equipment. The total time required for the health-related physical fitness measurements is approximately 30 min per person.
Parent support and support habit
The Activity Support Scale for Multiple Groups66 is used to measure parent support of child physical activity.
Parental support habit for child physical activity is measured with an adapted Self-Reported Habit Strength Index,67 which provides the opportunity to use the self-reported behavioural automaticity index subscale68 as well. Parents respond on a five-point scale to questions in the following format: ‘Regular support of my child’s PA is something I do…. automatically, frequently, etc.’. The Self-Reported Habit Strength Index has been shown to map well to measuring instigation habit.69 Both measures show excellent reliability and validity in self-reported and objective PA assessment.70 These measures evaluate the construct of habit, which is a component of the M-PAC framework, and have been adapted to parental support habits.38 All measures are examined at all time points (baseline, 6 weeks, 3 months and 6 months).
Tertiary outcome measures
Parent PA
Parents self-report PA using the Godin Leisure-Time Exercise Questionnaire64 71 at all time points. This questionnaire assesses the frequency of mild, moderate and strenuous activity performed during free time in a typical week.
Other parent factors
The 12-item Short-Form Health Survey72 is used to determine parental quality of life, and the Family Environment Scale73 is used to assess family functioning at baseline, 6 weeks, 3 months and 6 months. At one time point during the study, personality (Revised NEO Personality Inventory74), parenting sense of competence (the Parenting Sense of Competence scale75) and PA availability (from the Home Environment Survey76) are assessed.
M-PAC constructs for parental support of PA
In addition to habit, other M-PAC constructs of affective attitude, instrumental attitude and perceived behavioural control are assessed using the constructs of the theory of planned behaviour.77 Intention is measured using two questions employed in previous work with the Theory of Planned Behavior,78 79 asking about commitment and intention to support child PA. Behavioural regulation is measured via the instrument from Sniehotta and colleagues80 and parent support identity (whether parents identify as being a supportive of their child’s physical activity) is measured via a modified exercise identity scale from Anderson and colleagues.81–83 Measures from these instruments have demonstrated excellent predictive validity and internal consistency in adults,84–86 parental PA support42 and child/adolescent populations.87 The instruments have displayed validity for both personal and family-based (ie, activities as a family collective) PA.38 88
Demographics
The baseline questionnaire includes questions to assesses characteristics including age, gender, marital status, ethnicity, level of education, income level, number, gender, and age of children and employment information.
Manipulation check outcomes
The manipulation check outcomes of the study are examined via parent self-report of cue use and consistency on the questionnaires at 6 weeks, 3 months and 6 months,32 as well as a short process evaluation of the intervention at 6 months. The consistency item asks parents ‘over the past 6 weeks/3 months, how consistently did you support your child to be physically active at the same time each day?’ on a five-point scale from not consistent (random) to very consistent. For cue consistency, parents rank statements from ‘Not true at all’ to ‘very true’ on a seven-point scale related to the question ‘over the last 6 weeks/3 months each time I supported my child to be physically active…’. Statements refer to different types of cues such as temporal (‘it was the same time of day, I was doing the same type of activity’), visual (‘I was in the same place’), social (‘I was around the same people’) and mood (‘I was in the same mood’).
The process evaluation procedures involve a brief quantitative questionnaire included on the final 6-month parent questionnaire to assess use of the intervention material and overall satisfaction of the study.89 Second, semistructured interviews are conducted with families during the 6-month lab session, allowing for more in-depth examination of intervention material use and satisfaction of the study. All parents complete the interview and children have the option to participate alongside their parent. Some straightforward quantitative questions (eg, did you use the intervention materials, how often) are included in this interview as these have proved useful in our prior evaluations.22 Participants have the opportunity to elaborate on their response to each question, providing more context. Key open-ended questions include family PA type and frequency, barriers and changes. The PLANNING and HABIT group participants are also asked if they used the material, found it useful in promoting PA and why/why not. All participants have the opportunity to provide any other feedback as well.
Statistical power and sample size
Given the hierarchical nature of the data (ie, the four measurement occasions at level-1 were considered to be nested within the participant at level-2), the OpDes Program for power estimation of hierarchical linear models90 was used. With a frequency of four measurement occasions, three conditions, a duration of 6 months as the primary end-point, within-person variance of 1.0, a growth rate of 1.0 and a small effect size (d=0.30–0.40), a minimum of 150 families with a goal of 240 families (ie, 50–80 children per condition) are needed to show significant difference in PA accelerometry (minutes of MVPA primary outcome) by condition over time. The effect size represents the findings from our prior intervention research with this demographic18 22 and considering our pilot study on habit formation,36 yet it is clearly in the range for the detection of differences between the PLANNING and HABIT conditions.91 92
Data management
Confidentiality procedures are outlined on the consent form. Each participant is given an ID#, all hardcopy data (fitness test records and accelerometer logbooks) is kept in locked cabinets in a locked lab at the University of Victoria, data entered on the computer (accelerometer data and fitness test data) are stored on secure servers. Questionnaire data are stored on SurveyMonkey servers in Canada. Only the research team has access to the data. The details of data confidentiality and storage are included in the consent form and explained to participants by the research assistant during the baseline lab session. If a participant chooses to withdraw from the study, they are asked by the project coordinator if they would like their data to be destroyed or if the data that have been collected to that point can be used in the study. Participants receive a report of their data when they are complete with participation. A formal data monitoring committee has not been created for this intervention; however, the project coordinator provides monthly reports on participant numbers and trial progress to the principal investigator. The trial will be stopped when target participant numbers are achieved and/or at the grant deadline of June 2020. The final decision will be made by the principal investigator. The research team (including project coordinator, assistants and fitness testers) are trained to document and report any adverse events to the project coordinator and principal investigator. Depending on the nature of the event, action will be taken to ensure safety of all parties involved.
Analysis strategy
Missing data will be evaluated for pattern of missingness for each outcome at all time points using the dummy coding procedures of Allison.93 Depending on the outcome of these tests (eg, missing at random and missing completely at random), we will initiate the appropriate missing data handling strategy. Intention-to-treat (ITT) analyses will also be performed in addition to sensitivity analysis procedures. The first set of analyses will make preliminary demographic comparisons among adherers to the study versus drop-outs. These analyses will allow us to determine the representativeness of the sample. To determine whether minutes/day of MVPA change over time similarly for all three conditions, a level 1 model will be specified wherein the intercept (ie, minutes/day of MVPA at baseline) will be allowed to vary randomly (ie, vary across participants) and the slope for the linear trend will be constrained to be fixed (ie, the same across participants) controlling for important covariates (ie, demographics) at level 2. Additionally, dummy variables will be created for condition (HABIT: 1=yes or 2=no; PLANNING: 1=yes or 2=no; EDUCATION: 1=yes or 2=No) at level 2 with the HABIT and PLANNING condition variables being added to the model to predict the intercept and slope at level 1. In doing so, the EDUCATION group is compared against the other two groups to determine if baseline MVPA is similar across conditions and whether the change in MVPA is similar across conditions. Follow-up analyses will be conducted for the HABIT versus PLANNING condition comparison. The same analytical approach will be used to determine whether there are group differences in the health-related fitness outcomes and tertiary outcomes of parent physical activity and health-related quality of life. To determine whether the change in the underlying motives explain the potential change in MVPA during the intervention similarly for all three groups, a time-varying covariate mediation analysis approach will be used following the procedure outlined by Krull and MacKinnon94 for level 1 mediation. Briefly, the analyses needed to establish mediation will treat the underlying motives as time-varying covariates at level-1 of the model. Then, the dummy-coded condition variables will be entered at level 2 to determine if the mediation relationships are similar across groups. Finally, to determine whether there is a seasonal, intergenerational or gender difference across the primary and secondary outcomes, each variable will be entered into the various models at level 2 to predict the intercepts and slopes at level 1. Doing so will determine if they impact the change in the various outcomes across time.
The end of study process evaluation questions will be analysed using descriptive statistics. Qualitative data analysis will be overseen by the principal investigator but conducted by research assistants unconnected with the intervention activities.95 The responses to open-ended questions will be categorised and coded into common themes.96
Results
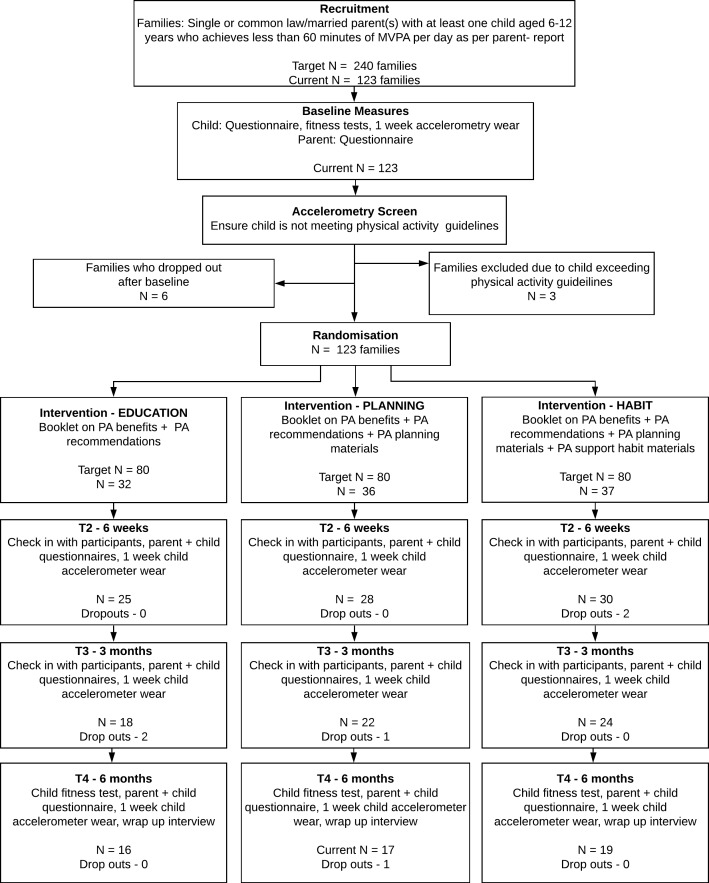
At time of submission (August 2019), we have obtained ethical approval, registered the trial and recruited 123 families. Recruitment is expected to be complete in December 2020. From the 123 families recruited, 22 have completed baseline measures, 19 have completed the 6-week measures, 12 have completed the 3-month measures, 52 have completed the study and 18 have dropped out. See figure 1 for the study procedures and participant flow chart.
Figure 1.
Study procedures and participant flow chart. MVPA, moderate to vigorous physical activity; PA, physical activity.
Discussion
This protocol paper outlines the implementation of a randomised trial employing parent supported physical activity habit formation strategies with their children. The guiding conceptual model is the M-PAC framework, and the overall goal is increased physical activity behaviour in children.
Ethics and dissemination
This protocol has been approved by the University of Victoria HREB (Victoria, Canada). Details on obtaining consent from participants and confidentiality is outlined in the Methods section. No harms are expected as a result of participation in this study; however, participants are provided with contact information for the project coordinator, principal investigator and HREB in the case they have something to report. Results from this trial will be shared at conferences as presentations and in scientific journals as published manuscripts. Participants who express interest in study results will be made aware of any relevant publications. Public access to the participant level dataset will not be granted. There are no current plans to grant public access to the full protocol or statistical code. All authors who have contributed to the protocol design are eligible for authorship on subsequent publications.
Supplementary Material
Footnotes
Twitter: @BeauchampDr, @ValLCarson, @drbengardner, @warburtonlab, @bmedlab
Contributors: RER, MRB, CMB, VC, BG and DERW all had input on conceptual model used and design of the study. ERM lead the writing of the protocol, and all authors approved the final manuscript. RER is responsible for project oversight.
Funding: This work was supported by the Heart and Stroke Foundation of Canada grantnumber G-16-00014050.
Disclaimer: The Heart and Stroke Foundation had no involvement in study design or data collection and analysis.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rhodes RE, Janssen I, Bredin SSD, et al. Physical activity: health impact, prevalence, correlates and interventions. Psychol Health 2017;32:942–75. 10.1080/08870446.2017.1325486 [DOI] [PubMed] [Google Scholar]
- 2.Colley RC, Garriguet D, Janssen I, et al. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian health measures survey. Health Rep 2011;22:7–14. [PubMed] [Google Scholar]
- 3.Colley RC, Garriguet D, Janssen I, et al. Physical activity of Canadian children and youth : Accelerometer results from the Survey. Stat Canada Heal Reports 2011;22:1–9. [PubMed] [Google Scholar]
- 4.Tremblay MS, Carson V, Chaput J-P. Introduction to the Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab 2016;41:iii–iv. 10.1139/apnm-2016-0203 [DOI] [PubMed] [Google Scholar]
- 5.Tremblay MS, Warburton DER, Janssen I, et al. New Canadian physical activity guidelines. Appl Physiol Nutr Metab 2011;36:36–46. 10.1139/H11-009 [DOI] [PubMed] [Google Scholar]
- 6.Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010;7:40 10.1186/1479-5868-7-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahn JV, Sera F, Cummins S, et al. Associations between objectively measured physical activity and later mental health outcomes in children: findings from the UK millennium cohort study. J Epidemiol Community Health 2018;72:94–100. 10.1136/jech-2017-209455 [DOI] [PubMed] [Google Scholar]
- 8.Poitras VJ, Gray CE, Borghese MM, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab 2016;41:S197–9. 10.1139/apnm-2015-0663 [DOI] [PubMed] [Google Scholar]
- 9.Colley RC, Carson V, Garriguet D, et al. Physical activity of Canadian children and youth, 2007 to 2015. Health Rep 2017;28:8–16. [PubMed] [Google Scholar]
- 10.Brown HE, Atkin AJ, Panter J, et al. Family-Based interventions to increase physical activity in children: a systematic review, meta-analysis and realist synthesis. Obes Rev 2016;17:345–60. 10.1111/obr.12362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beets MW, Cardinal BJ, Alderman BL. Parental social support and the physical activity-related behaviors of youth: a review. Health Educ Behav 2010;37:621–44. 10.1177/1090198110363884 [DOI] [PubMed] [Google Scholar]
- 12.O'Connor TM, Jago R, Baranowski T. Engaging parents to increase youth physical activity a systematic review. Am J Prev Med 2009;37:141–9. 10.1016/j.amepre.2009.04.020 [DOI] [PubMed] [Google Scholar]
- 13.Kitzman-Ulrich H, Wilson DK, St George SM, et al. The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clin Child Fam Psychol Rev 2010;13:231–53. 10.1007/s10567-010-0073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salmon J, Booth ML, Phongsavan P, et al. Promoting physical activity participation among children and adolescents. Epidemiol Rev 2007;29:144–59. 10.1093/epirev/mxm010 [DOI] [PubMed] [Google Scholar]
- 15.van Sluijs EMF, Kriemler S, McMinn AM. The effect of community and family interventions on young people's physical activity levels: a review of reviews and updated systematic review. Br J Sports Med 2011;45:914–22. 10.1136/bjsports-2011-090187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Dwyer MV, Fairclough SJ, Knowles Z, et al. Effect of a family focused active play intervention on sedentary time and physical activity in preschool children. Int J Behav Nutr Phys Act 2012;9:117 10.1186/1479-5868-9-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morgan PJ, Lubans DR, Callister R, et al. The ‘Healthy Dads, Healthy Kids’ randomized controlled trial: efficacy of a healthy lifestyle program for overweight fathers and their children. Int J Obes 2011;35:436–47. 10.1038/ijo.2010.151 [DOI] [PubMed] [Google Scholar]
- 18.Rhodes RE, Naylor P-J, McKay HA. Pilot study of a family physical activity planning intervention among parents and their children. J Behav Med 2010;33:91–100. 10.1007/s10865-009-9237-0 [DOI] [PubMed] [Google Scholar]
- 19.Ranucci C, Pippi R, Buratta L, et al. Effects of an intensive lifestyle intervention to treat overweight/obese children and adolescents. Biomed Res Int 2017;2017:1–11. 10.1155/2017/8573725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morrison R, Reilly JJ, Penpraze V, et al. Children, parents and pets exercising together (CPET): exploratory randomised controlled trial. BMC Public Health 2013;13:1096 10.1186/1471-2458-13-1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olvera NN. A healthy lifestyle program for Latino daughters and mothers: the bounce overview and process evaluation. Am J Heal Educ 2008;39:p283–95. [Google Scholar]
- 22.Rhodes RE, Blanchard CM, Quinlan A, et al. Family physical activity planning and child physical activity outcomes: a randomized trial. Am J Prev Med 2019;57:135–44. 10.1016/j.amepre.2019.03.007 [DOI] [PubMed] [Google Scholar]
- 23.Rhodes RE, Spence JC, Berry T, et al. Understanding action control of parental support behavior for child physical activity. Health Psychol 2016;35:131–40. 10.1037/hea0000233 [DOI] [PubMed] [Google Scholar]
- 24.Rhodes RE, Berry T, Craig CL, et al. Understanding parental support of child physical activity behavior. Am J Health Behav 2013;37:469–77. 10.5993/AJHB.37.4.5 [DOI] [PubMed] [Google Scholar]
- 25.Rhodes RE, Spence JC, Berry T, et al. Predicting Changes Across 12 Months in Three Types of Parental Support Behaviors and Mothers’ Perceptions of Child Physical Activity. ann. behav. med. 2015;49:853–64. 10.1007/s12160-015-9721-4 [DOI] [PubMed] [Google Scholar]
- 26.Hagger MS, Chatzisarantis NLD. An integrated behavior change model for physical activity. Exerc Sport Sci Rev 2014;42:62–9. 10.1249/JES.0000000000000008 [DOI] [PubMed] [Google Scholar]
- 27.Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008;57:1–29. 10.1111/j.1464-0597.2007.00325.x [DOI] [Google Scholar]
- 28.Sheeran P, Webb TL. The Intention-Behavior gap. Soc Personal Psychol Compass 2016;10:503–18. 10.1111/spc3.12265 [DOI] [Google Scholar]
- 29.Rhodes RE. The evolving understanding of physical activity behavior: A multi-process action control approach : Elliot AJ, Advances in motivation science. Cambridge, MA: Elsevier Academic Press, 2017: 171–205. [Google Scholar]
- 30.Rhodes RE, de Bruijn G-J. What predicts intention-behavior discordance? A review of the action control framework. Exerc Sport Sci Rev 2013;41:201–7. 10.1097/JES.0b013e3182a4e6ed [DOI] [PubMed] [Google Scholar]
- 31.Gardner B. A review and analysis of the use of 'habit' in understanding, predicting and influencing health-related behaviour. Health Psychol Rev 2015;9:277–95. 10.1080/17437199.2013.876238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaushal N, Rhodes RE. Exercise habit formation in new gym members: a longitudinal study. J Behav Med 2015;38:652–63. 10.1007/s10865-015-9640-7 [DOI] [PubMed] [Google Scholar]
- 33.Lally P, Gardner B. Promoting habit formation. Health Psychol Rev 2013;7:S137–58. 10.1080/17437199.2011.603640 [DOI] [Google Scholar]
- 34.Rhodes RE, Rebar A. Physical activity habit: Complexities and controversies : Verplanken B, The psychology of habit. Cham. Switzerland: Springer, 2018: 91–109. [Google Scholar]
- 35.Gardner B, de Bruijn G-J, Lally P. A systematic review and meta-analysis of applications of the self-report habit index to nutrition and physical activity behaviours. Ann Behav Med 2011;42:174–87. 10.1007/s12160-011-9282-0 [DOI] [PubMed] [Google Scholar]
- 36.Kaushal N, Rhodes RE, Meldrum JT, et al. The role of habit in different phases of exercise. Br J Health Psychol 2017;22:429–48. 10.1111/bjhp.12237 [DOI] [PubMed] [Google Scholar]
- 37.Deutsch R, Strack F. Target article: duality models in social psychology: from dual processes to interacting systems. Psychol Inq 2006;17:166–72. 10.1207/s15327965pli1703_2 [DOI] [Google Scholar]
- 38.Rhodes RE, Berry T, Faulkner G, et al. Application of the Multi‐Process action control framework to understand parental support of child and youth physical activity, sleep, and screen time behaviours. Appl Psychol 2019;11:223–39. 10.1111/aphw.12150 [DOI] [PubMed] [Google Scholar]
- 39.Brown H, Hume C, Pearson N, et al. A systematic review of intervention effects on potential mediators of children's physical activity. BMC Public Health 2013;13:165 10.1186/1471-2458-13-165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan A-W, Tetzlaff JM, Altman DG, et al. Spirit 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Temple VA, Naylor P-J, Rhodes RE, et al. Physical activity of children in family child care. Appl Physiol Nutr Metab 2009;34:794–8. 10.1139/H09-061 [DOI] [PubMed] [Google Scholar]
- 42.Rhodes RE, Gustafson SL. Parental correlates of physical activity in children and early adolescents parental correlates of physical activity in children and early adolescents. Sport Med 2016;36:79–97. [DOI] [PubMed] [Google Scholar]
- 44. Statistics Canada. Victoria, British Columbia and Canada Census Profile. 2016 Census [Internet].. Ottawa; 2017. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E [Google Scholar]
- 44.Warburton DER, Jamnik VK, Bredin SSD, et al. The physical activity readiness questionnaire for everyone (PAR-Q+) and electronic physical activity medical examination (ePARmed-X). Heal Fit J Canada 2011;4:3–23. [Google Scholar]
- 45.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (V1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 46.Quinlan A, Rhodes RE, Blanchard CM, et al. Family planning to promote physical activity: a randomized controlled trial protocol. BMC Public Health 2015;15:1–9. 10.1186/s12889-015-2309-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Verplanken B, Melkevik O. Predicting habit : The case of physical exercise 2008;9:15–26. [Google Scholar]
- 48.Phillips LA, Gardner B. Habitual exercise instigation (vs. execution) predicts healthy adults’ exercise frequency. Health Psychology 2016;35:69–77. 10.1037/hea0000249 [DOI] [PubMed] [Google Scholar]
- 49.Gardner B, Rebar AL, Lally P. A matter of habit: recognizing the multiple roles of habit in health behaviour. Br J Health Psychol 2019;24:241–9. 10.1111/bjhp.12369 [DOI] [PubMed] [Google Scholar]
- 50.Milne S. Combining motivational and volitional interventions to promote exercise participation. Br J Health Psychol 2002;2:163–84. [DOI] [PubMed] [Google Scholar]
- 51.Prestwich A, Lawton R, Conner M. The use of implementation intentions and the decision balance sheet in promoting exercise behaviour. Psychol Health 2003;18:707–21. 10.1080/08870440310001594493 [DOI] [Google Scholar]
- 52.Judah G, Gardner B, Aunger R. Forming a flossing habit: an exploratory study of the psychological determinants of habit formation. Br J Health Psychol 2013;18:338–53. 10.1111/j.2044-8287.2012.02086.x [DOI] [PubMed] [Google Scholar]
- 53.Pimm R, Vandelanotte C, Rhodes RE, et al. Cue consistency associated with physical activity automaticity and behavior. Behav Med 2016;42:248–53. 10.1080/08964289.2015.1017549 [DOI] [PubMed] [Google Scholar]
- 54.Evenson KR, Catellier DJ, Gill K, et al. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557–65. 10.1080/02640410802334196 [DOI] [PubMed] [Google Scholar]
- 55.Trost SG, Loprinzi PD, Moore R, et al. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011;43:1360–8. 10.1249/MSS.0b013e318206476e [DOI] [PubMed] [Google Scholar]
- 56.Actilife Actigraph (version 6.11.9. Pensacola, FL, 2015. [Google Scholar]
- 57.Bailey RC, Olson J, Pepper SL, et al. The level and tempo of children's physical activities: an observational study. Med Sci Sports Exerc 1995;27:1033–41. 10.1249/00005768-199507000-00012 [DOI] [PubMed] [Google Scholar]
- 58.Cain KL, Sallis JF, Conway TL, et al. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health 2013;10:437–50. 10.1123/jpah.10.3.437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc 2005;37:S531–43. 10.1249/01.mss.0000185657.86065.98 [DOI] [PubMed] [Google Scholar]
- 60.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40:181–8. 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 61.Ward DS, Evenson KR, Vaughn A, et al. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc 2005;37:S582–8. 10.1249/01.mss.0000185292.71933.91 [DOI] [PubMed] [Google Scholar]
- 62.Crocker PR, Bailey DA, Faulkner RA, et al. Measuring General levels of physical activity: preliminary evidence for the physical activity questionnaire for older children. Med Sci Sports Exerc 1997;29:1344–9. 10.1097/00005768-199710000-00011 [DOI] [PubMed] [Google Scholar]
- 63.Troiano RP, McClain JJ, Brychta RJ, et al. Evolution of accelerometer methods for physical activity research. Br J Sports Med 2014;48:1019–23. 10.1136/bjsports-2014-093546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 1985;10:141–6. [PubMed] [Google Scholar]
- 65.Longmuir PE, Boyer C, Lloyd M, et al. The Canadian Assessment of Physical Literacy: methods for children in grades 4 to 6 (8 to 12 years). BMC Public Health 2015;15:767 10.1186/s12889-015-2106-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Davison KK, Li K, Baskin ML, et al. Measuring parental support for children's physical activity in white and African American parents: the activity support scale for multiple groups (ACTS-MG). Prev Med 2011;52:39–43. 10.1016/j.ypmed.2010.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Verplanken B, Orbell S. Reflections on past behavior: a self-report index of habit Strength1. J Appl Soc Psychol 2003;33:1313–30. 10.1111/j.1559-1816.2003.tb01951.x [DOI] [Google Scholar]
- 68.Gardner B, Abraham C, Lally P, et al. Towards parsimony in habit measurement: testing the convergent and predictive validity of an automaticity subscale of the self-report habit index. Int J Behav Nutr Phys Act 2012;9:102 10.1186/1479-5868-9-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gardner B, Phillips LA, Judah G. Habitual instigation and habitual execution: definition, measurement, and effects on behaviour frequency. Br J Health Psychol 2016;21:613–30. 10.1111/bjhp.12189 [DOI] [PubMed] [Google Scholar]
- 70.Thurn J, Finne E, Brandes M, et al. Validation of physical activity habit strength with subjective and objective criterion measures. Psychol Sport Exerc 2014;15:65–71. 10.1016/j.psychsport.2013.09.009 [DOI] [Google Scholar]
- 71.Godin G, Jobin J, Bouillon J. Assessment of leisure time exercise behavior by self-report: a concurrent validity study. Can J Public Health 1986;77:285. [PubMed] [Google Scholar]
- 72.Ware J, Kosinski M, Keller SD. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:2–9. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 73.Moos RH, Moos BS. Family Environemtn scale manual. 3rd edn Palo Alto, CA: Consulting Psychologists Press, 1994. [Google Scholar]
- 74.Costa PT, McCrae RR. The Revised NEO Personality Inventory (NEO-PI-R) : Boyle GJ, Saklofske DH, The SAGE Handbook of personality theory and assessment. vol.2 Sage Publications Inc, 2008: 179–98. [Google Scholar]
- 75.Robinson CC, Mandleco B, Olsen SF, et al. Authoritative, authoritarian, and permissive parenting practices: development of a new measure.. Psychol Rep 1995;77:819–30. 10.2466/pr0.1995.77.3.819 [DOI] [Google Scholar]
- 76.Gattshall ML, Shoup JA, Marshall JA, et al. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. Int J Behav Nutr Phys Act 2008;5:3 10.1186/1479-5868-5-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 78.Courneya KS, McAuley E. Factors affecting the intention-physical activity relationship: intention versus expectation and scale correspondence. Res Q Exerc Sport 1994;65:280–5. 10.1080/02701367.1994.10607629 [DOI] [PubMed] [Google Scholar]
- 79.Rhodes RE, Blanchard CM, Hunt D, et al. Intention, and planning in the physical activity domain. Psychol Sport Exerc 2006;7:15–27. [Google Scholar]
- 80.Sniehotta FF, Schwarzer R, Scholz U, et al. Action planning and coping planning for long-term lifestyle change: theory and assessment. Eur J Soc Psychol 2005;35:565–76. 10.1002/ejsp.258 [DOI] [Google Scholar]
- 81.Anderson DF, Cychosz CM. Development of an exercise identity scale. Percept Mot Skills 1994;78:747–51. 10.1177/003151259407800313 [DOI] [PubMed] [Google Scholar]
- 82.Anderson DF, Cychosz CM. Exploration of the relationship between exercise behavior and exercise identity. J Sport Behav 1995;18. [Google Scholar]
- 83.Anderson DF, Cychosz CM, Franke WD. Association of exercise identity with measures of exercise commitment and physiological indicators of fitness in a law enforcement cohort. J Sport Behav 1998;21:233–41. [Google Scholar]
- 84.Rhodes RE, Lim C. Understanding action control of daily walking behavior among dog owners: a community survey. BMC Public Health 2016;16:1–10. 10.1186/s12889-016-3814-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rhodes RE, Plotnikoff RC. Can current physical activity act as a reasonable proxy measure of future physical activity? evaluating cross-sectional and passive prospective designs with the use of social cognition models. Prev Med 2005;40:547–55. 10.1016/j.ypmed.2004.07.016 [DOI] [PubMed] [Google Scholar]
- 86.Rhodes RE, Warburton DER, Bredin SSD. Predicting the effect of interactive video bikes on exercise adherence: an efficacy trial. Psychol Health Med 2009;14:631–40. 10.1080/13548500903281088 [DOI] [PubMed] [Google Scholar]
- 87.Rhodes RE, Macdonald HM, McKay HA. Predicting physical activity intention and behaviour among children in a longitudinal sample. Soc Sci Med 2006;62:3146–56. 10.1016/j.socscimed.2005.11.051 [DOI] [PubMed] [Google Scholar]
- 88.Casiro NS, Rhodes RE, Naylor PJ, et al. Correlates of intergenerational and personal physical activity of parents. Am J Health Behav 2011;35:81–91. 10.5993/AJHB.35.1.8 [DOI] [PubMed] [Google Scholar]
- 89.Carroll C, Patterson M, Wood S, et al. A conceptual framework for implementation fidelity. Implementation Sci 2007;2:1–9. 10.1186/1748-5908-2-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Raudenbush SW, Bryk TA. Hierarchical linear model: applications and data analysis. 2nd edn Thousand Oaks: Sage, 2002. [Google Scholar]
- 91.Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol 2009;40:532–8. 10.1037/a0015808 [DOI] [Google Scholar]
- 92.Cohen J. A power primer. Psychol Bull 1992;112:155–9. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- 92.Allison PD. Missing Data : Quantitative applications in the social sciences. Thousand Oaks: Sage, 2002. [Google Scholar]
- 94.Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behav Res 2001;36:249–77. 10.1207/S15327906MBR3602_06 [DOI] [PubMed] [Google Scholar]
- 95.Merrick E. An exploration of quality in qualitative research: Are “reliability” and “validity” relevant? : Kopala M, Suzuki LA, Using qualitative methods in psychology. Thousand Oaks: Sage, 1999: 25–36. [Google Scholar]
- 96.Patton MQ. Qualitative evaluation and research methods. 2nd edn Newbury Park, NJ: Sage, 1990. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-033732supp001.pdf (1.1MB, pdf)