Abstract
Purpose:
The purpose of this study was to measure the feasibility of an alternative and augmentative communication (AAC) application and an iPad (a customized tablet) to facilitate communication in post-operative patients with head and neck cancer.
Design:
A prospective feasibility study.
Methods:
The study was conducted in the main postanesthesia care unit at an urban comprehensive cancer center in the northeast United States between January 2014 and September 2014. The participants included patients with head and neck cancer who underwent surgery that resulted in altered communication. Patient questionnaires were developed and administered to measure feasibility and patient satisfaction at different time points (preoperative, postoperative, one to four days postoperatively).
Findings:
Of 38 patients consented to the study, 25 (66%) were able to use the customized tablet. Of these 25 patients, 15 (60%) were satisfied or somewhat satisfied with it. In addition, 84% found the customized tablet to be very or somewhat helpful for communication following surgery.
Conclusions:
Patients were satisfied with the customized tablet and the study found that using technology such as this was feasible in the immediate postoperative period.
Keywords: communication, technology, augmentative and alternative communication (AAC), mobile device, postoperative, patient satisfaction
Introduction
Nurses are often faced with difficult challenges in trying to assist patients toward optimal recovery1. Patients who are scheduled for a procedure that impacts communication (such as a tracheostomy or laryngectomy) encounter obstacles during their recovery period that vary in degree of emotional, psychological and physical demands on their bodies2. An iPad (computer tablet) is a tool that may be able to bridge communication between these patients and staff in the immediate postoperative period, with the ultimate goal of providing a safe environment for patients who are recovering from anesthesia.
Background
Communication between patients and health care providers in the immediate postoperative period can be challenging. Nurses routinely provide dry erase boards with markers, try to interpret patient’s facial/hand gestures, use verbal yes and no questions to solicit responses, and use a translator (if applicable) as their primary methods of communication. Unfortunately, these forms of communication are not very effective. The inability to verbally communicate has been associated with psychological distress, fear, and anger among patients with temporary or permanent speech impairment during their postoperative care1,3,4. Although health care institutions are increasingly adopting technology to improve patient care, our literature review for this study identified a gap in the utilization of technology for this patient population. The investigators of this study came together to research available technology to bridge this gap.
One of the most terrifying situations for a patient emerging from anesthesia after surgery is to be mechanically ventilated and unable to communicate. Head and neck surgery may often lead to compromised communication. Various types of surgeries result in the need to provide alternative ways for patients to communicate. For instance, a total laryngectomy, which may lead to immediate and permanent loss of the ability to speak, can be psychologically devastating to the patient and family2. What methods do patients have to communicate after surgery if they are unable to speak? During the early postoperative period, writing and mouthing are the usual methods of communication, but the latter is not always readily understood, and written communication can be difficult following anesthesia.
A patient’s initial recovery period can be complicated by pre-existing factors such as age, visual, hearing and language barriers5. Leveraging a customized tablet as an effective communication tool could alleviate some of the difficulties in trying to assist a patient unable to speak during recovery. A customized tablet has the benefit of offering a patient an alternate way for them to express themselves, creating an enhanced outcome, and adding value to PACU care services6.
The study team used the Systems Development Life Cycle (SDLC) model as a path to discovering the iPad and mobile device application as a potential solution7. The SDLC model is often used within Nursing Informatics and is comprised of several phases. Different variations of the model exist, but all essentially proceed through common stages including: planning, analysis, design, development, testing, implementation and maintenance. Following this framework allowed for a thorough understanding of the problem and how best to implement the proposed solution without negatively impacting nursing workflow or patient experience6.
Augmentative and Alternative Communication (AAC) is a broad term that encircles the communication technique used to replace speech or writing for those with impairments in the production or understanding of spoken or written language8. This intervention can serve as a temporary means of compensating for a lack of verbal communication and can enhance a patient’s quality of care during their stay in a PACU4. AssistiveWare is a leader in innovative assistive technology software and the first company to release a full-featured AAC solution for iPads. Their application, Proloquo2Go™, provides assistance to people who have impaired communication and could be a useful tool in hospital and rehabilitation settings. The iPad was first released in 2010 and has grown in popularity as a mobile device9. The use of the iPad and Proloquo2Go™ (i.e., customized tablet) will make it possible for patients to express their needs with ease, provides naturally sounding text-to-speech voices, and the ability to fully customize vocabularies for users along a broad continuum of abilities10.
AAC applications such as Proloquo2Go™ can help to reduce stress both prior to and after surgery for patients and caregivers. This tool may be used for pre- and postoperative patients to communicate information that will help nurses and other health care professionals to continue to deliver quality care6. Due to the popularity of the technology and the availability of AAC applications it was hypothesized that an iPad and application could circumvent challenges in communicating with these patients in the PACU. However, we were not sure that patients would accept the iPad and application, or be awake and alert enough to use them in the immediate postoperative period. For that reason, we proposed a feasibility study as a first step towards investigating this technology for patients immediately following head and neck surgery.
The primary objective of this pilot study was to test the feasibility of using a customized tablet as a communication tool with patients in the immediate postoperative setting. The secondary objectives were to evaluate the use of the customized tablet as a communication tool for patients following surgery for head and neck cancer and to assess patient satisfaction
Design
A prospective pre and post intervention design was used in this feasibility study. A convenience sample of patients with head and neck cancer, scheduled for a procedure that results in altered communication, were eligible to participate.
Method
An IRB approved prospective clinical research study was conducted, between January and September 2014, to measure the feasibility of using a customized tablet as a tool to bridge the communication gap in the head and neck surgical patient population.
A sample of 38 patients with head and neck cancer who were scheduled for a surgical procedure that resulted in impaired verbal communication participated. Informed written consent was obtained at the time of surgical consent, or in the pre-surgical area the morning of surgery, and participants could withdraw from the study at any time. The inclusion criteria for this study were as follows: age 18 years or older, able to understand written and/or oral English, and not requiring isolation precautions.
Procedure
Application choice and customization
After we identified the need for an alternative communication method, we conducted an extensive literature review to see if there were existing methods being used in other institutions for communication in a PACU setting. We found only limited research available on this topic. We then focused our attention towards finding a mobile application that would support patients with impaired communication following surgery. During this selection process we identified the iPad and Proloquo2go ™ as the best choice for our patients.
With assistance from our medical librarians, a needs assessment was conducted with staff to measure their technology literacy levels and obtain their input on prioritizing patient needs. The needs assessment method was developed and conducted by two medical librarians and consisted of a first-pass design of the Proloquo2Go app (based on initial feedback from the Smart Communication Committee), one-on-one participative and interactive card sort sessions with a select number of front-line nurses, followed by individual formal usability sessions with twelve night shift nurses (using a survey containing targeted tasks for participants to complete). The needs assessment was instrumental in customizing the application for our patient population. The feedback collected from these sessions, along with domain knowledge by the study investigators, helped to inform the initial iteration of the app interface, hierarchy, and design. Tiles were prioritized and hierarchically configured to meet most of the suggestions from staff during the card sorts. With the use of Proloquo2Go™, we were able to customize the user friendly application to meet the needs in our patient population. Predefined phrases were created, in the form of tiles (see Figure 1) that addressed basic needs such as pain, breathing, emotions and general questions related to their surgical procedure. In order to communicate participants had to select a tile for the application to speak. Certain tiles allowed for the construction of sentences that would speak out loud as they were chosen. In addition, this application provided a free text to speech feature.
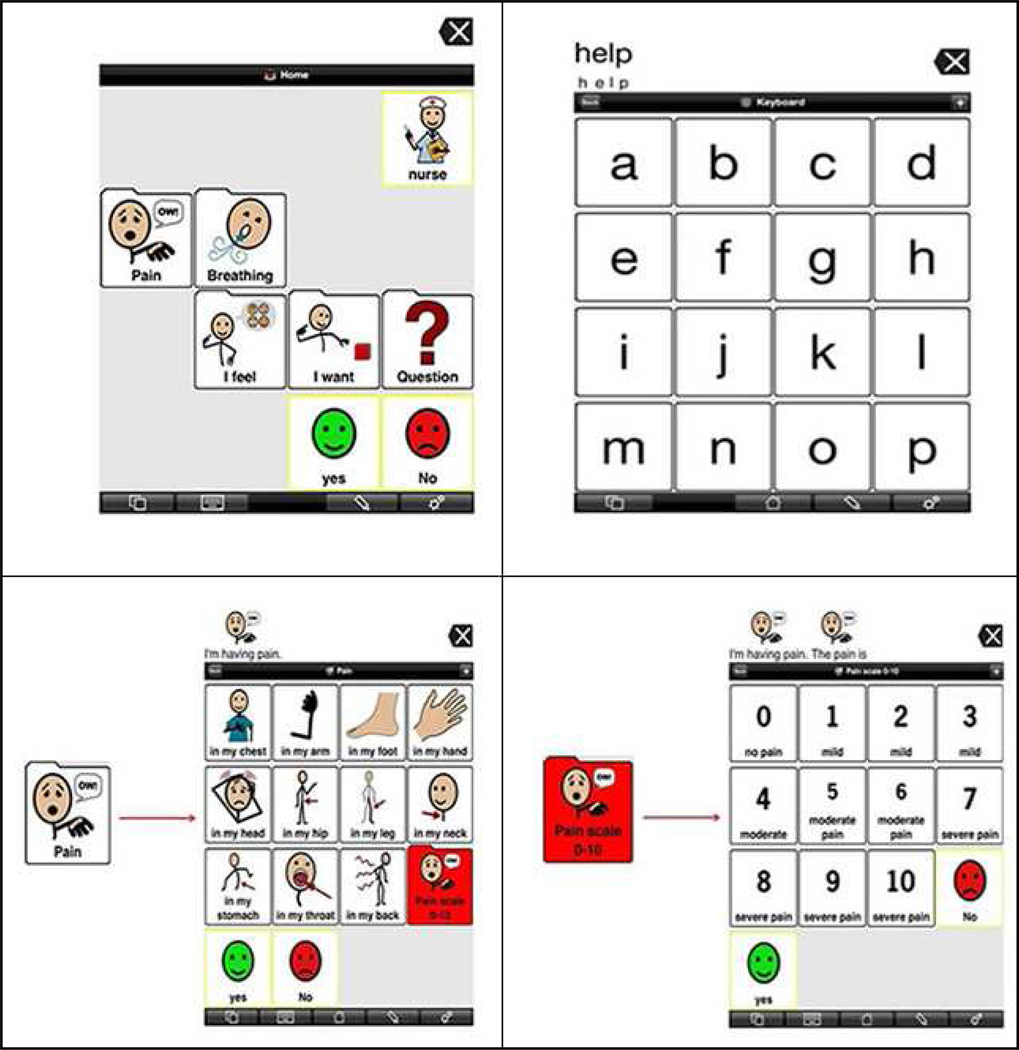
Figure 1.
Screenshots of the app home screen (top left), manual keyboard (top right), first-level pain folder (lower left), and second-level pain folder (lower right). Proloquo2go™ is an AssistiveWare product. Image(s) used with permission.
In order to gather information during the formal usability sessions, a list of four general questions was presented to each participant regarding first impressions of the application customization. Immediately following the general questions, a set of five tasks was asked of each participant. Each usability session had one moderator and a note taker during each card sort (both medical librarians).
In order to communicate participants had to select a tile for the application to speak. Certain tiles allowed for the construction of sentences that would speak out loud as they were chosen. In addition, this application provided a free text to speech feature. Inservice training also took place immediately following the formal usability sessions. Training documentation was developed as a take-away for participants which was used to either train other staff or introduce patients to the Proloquo2Go™ app. Results of the usability sessions were analyzed and combined into a two-page summary which was shared with the group of study investigators. Additional changes and updates were made to the Proloquo2Go™ app interface to deliver the most relevant design for the PACU patient population.
Patient procedure
Patients were informed about the study and shown the customized tablet at the time of surgical consent or on the morning of surgery. Following consent, patients and their families were educated on the basic functionality of the customized tablet. Patients were able to use the customized tablet to communicate with staff and family. For security and privacy reasons patients were not given Internet access. The only application that patients were able to access was the Proloquo2Go™ software. Following surgery, postoperative patients were given the customized tablet which was placed on a bedside stand to ensure easy access and they were encouraged to use the customized tablet to communicate during their PACU stay. Re-education was provided on an as needed basis.
For this feasibility study questionnaires were developed by the investigators with assistance from staff in our Psychology and Behavioral Sciences department. Questions included concern about communicating, use of the customized tablet, perceptions of how helpful they were and how satisfied the patient was using them. Answers included standard responses, open ended feedback and a Likert scale for satisfaction. A baseline assessment prior to surgery included demographics, as well as concern about communicating postoperatively and past experience with technology. At the time of PACU discharge, the questionnaires addressed their ability to use the customized tablet, its usefulness, any additional needs that could have been communicated, and how satisfied they were using the customized tablet. A convenience sample of patients were visited once while on the inpatient unit (days 1–4 post-surgery) to complete another questionnaire. This assisted us in understanding where improvements could be made. After each use, the customized tablet was disinfected to adhere to our hospital infection control policy.
Data Analysis
Primary outcomes include the feasibility of using the customized tablet in a PACU setting. This was measured by the number of eligible patients who used the customized tablet post surgery and their responses to the first post-surgery questionnaire. A secondary outcome includes patient satisfaction related to communication. We designated a successful trial as one where 50% of patients are able to use the customized tablet in the postoperative setting and/or 50% are satisfied with using it in the postoperative setting. For this feasibility study we planned to accrue a convenience sample of 25 patients with complete data. Descriptive statistics were used to summarize the categorical data. Open ended questions were analyzed by members of the research team. Reviewers from the research team independently grouped comments into themes related to communication. A consensus approach was used to verify the final group of themes.
Results
Thirty-eight patients were consented to this study. Of the 38 patients, 13 were not evaluated as they were unable to use the customized tablet after surgery. Reasons for nonuse of the iPad included six for medical reasons (blurry vision/eye swelling, sedation, postoperative nausea and vomiting, hand swelling and difficulty emerging from anesthesia), four patients unwilling to use it, one patient for technical reasons (the tablet malfunctioned and was not able to be fixed in time) and patient preparedness (two patients wanted to use the customized tablet but did not have their glasses and they could not see well enough). Of the 38 patients consented, 66% (25/38) were able to use the customized tablet in the immediate postoperative setting and remained in the study. The patients in the study included 22 males and three females with an age range of 25 to 80 years of age (median age 57). The age of the patients who were not able to use the iPad was slightly older than our study group, with a range of 45 – 88 (median age 69).
The primary study outcome was feasibility, and a successful trial was defined as one when at least 50% of patients are able to use the customized tablet in the postoperative setting and/or at least 50% are satisfied with using the customized tablet. Of the 38 patients consented to the study 25 (n=66%) were able to use the customized tablet. Of the 25 patients who used it, 15 were somewhat satisfied or satisfied and ten were neutral, somewhat satisfied or not satisfied. Thus, 60% (15/25) of patients expressed satisfaction with the customized tablet as a communication tool after surgery. Of note, we did not include neutral patients in our positive outcomes to set the bar higher to reach our study goals. Based on these results, both requirements for feasibility were met.
Preoperatively, 92% (n=23) of patients stated they were very concerned or somewhat concerned about communicating postoperatively. Only the 25 patients in the study completed the satisfaction questionnaires which asked how satisfied they were with the customized tablet and how helpful they thought it was. Of the patients who reported preoperatively that they were ‘very concerned’ about communication postoperatively, 61% (N=8) rated they were ‘satisfied’ using the customized tablet. Patients who reported they were ‘somewhat concerned’ about communication found the customized tablet somewhat or very helpful 70% (n=7) of the time. Two patients reported preoperatively they were not concerned with communication and both post peratively reported that they were satisfied with the customized tablet.
When asked how helpful the customized tablet was, 84% of patients (n=21) reported it was very or somewhat helpful. Patients who were very concerned about communication (92%; n=23) found the customized tablet helpful while 100% of patients who were not concerned about communication reported that it was helpful. Only 70% of patients who were somewhat concerned about communication found the customized application to be helpful, mirroring the results we found for satisfaction. (See Table 1)
Table 1.
Patient reported satisfaction and helpfulness results (N = 25)
| Level of concern about communication prior to surgery | Patient report of satisfaction with the customized tablet for communication | Patient report of how helpful the customized tablet was to communication |
|---|---|---|
| None (n=2) | 100% (n=2) were satisfied | 100% (n=2) found the customized tablet to be very helpful |
| Somewhat concerned (n=10) | 50% (n=5) were satisfied or somewhat satisfied
20% (n=2) were neutral 30% (n=3) were somewhat dissatisfied or not satisfied |
70% (n=7) found the customized tablet somewhat
or very helpful 30% (n=3) found the customized tablet not helpful |
| Very concerned (n=13) | 61% (n=8) were satisfied 31% (n=4) were somewhat dissatisfied 8% (n=1) did not answer |
92% (n= 12) found the customized tablet to be
somewhat or very helpful 8% (n=1) did not answer |
Open ended questions revealed information about patient education and experience in the postoperative setting. Information about communicating after surgery is a standard part of our preoperative education. When asked at the time of surgery what they recalled being told about communicating postoperatively only 36% of patients recalled a conversation about communication options. They recalled information about use of a white board, hand gestures, paper and pencil, use of the customized tablet as well as reassurance that staff would be present to assist them. Patients were also asked what concerned them most about communicating after surgery and the most common answer was communicating about pain followed by “making sure I’m understood” and that they would be able to communicate critical information to staff. Patients also expressed concern for communication stating they were “scared” about how they would communicate and that they were upset about “grandchildren not hearing my voice” again. Patients were approached on the inpatient floor 1–4 days after surgery for a final assessment. At that time they did not have the customized tablet as it was only used during their stay in the PACU. Patients were asked if they had any suggestions for improving communication with the health care team after surgery. The most common response related to the customized tablet – patients stated it was heavy and that the onscreen keyboard could be difficult to navigate with hands that were swollen following surgery. Several suggested that they customized tablet would be better used on the inpatient unit, when fully recovered from anesthesia. Several patients mentioned that using the white board worked well for communication.
Discussion
Impaired verbal communication and the inability to make their needs known can be stressful to the patient, family, and health care providers following surgery. This challenge creates increased anxiety and frustration which can impact patient outcome and satisfaction. In addition, nurses are faced with obstacles in meeting patients’ needs and the ability to provide patient care in a timely manner. This study was conducted based upon one simple question; how can we improve communication for this patient population? There is limited research to support the use of innovative technology in the post-operative setting. The research team of nurses collaborated with library staff to identify and then customize a communication application for the surgical population. The process was similar to needs assessments that are routinely conducted in clinical settings. Nursing and library staff who had experience with information technology were able to work with the vendor for the communication application to make the necessary changes and tailor the application to the needs of patients following surgery.
We were able to meet our primary objective in that a majority of patients were able to use the customized tablet and were also satisfied with using it in the immediate postoperative period. An interesting finding was that patients who were very concerned about communication and patients who were not concerned about communication reported the most benefit from using the customized tablet. Future research should explore the communication needs of this vulnerable population. The nursing staff who used the customized tablets with patients found them to be easy to use and intuitive. They were cleaned with standard cleaning wipes and were stored in a locked cabinet that the charge nurse had access to each shift. During the course of the study there were minimal technical difficulties and the tablets were easily incorporated into patient care. Following study completion the customized tablets were incorporated into routine patient care and continue to be used to assist with communication with positive responses from patients and staff.
In addition to our quantitative results we also learned that patients are primarily concerned with communicating about their pain after surgery and that less than half of patients recall being given information on communication during their surgical consent visit. This highlights the need to reinforce patient education at every clinical encounter as patients and families may be overwhelmed with the volume of information they are receiving when undergoing a complicated surgical procedure. Even though they were satisfied with the customized tablet patients did report several suggestions for improvements. Following surgery, patients may have swollen hands and larger buttons on the device would be easier to manipulate. They also reported that the computer tablet we used (an iPad) was heavy and at times difficult to position so that it could be easily used. Patients also reported that even though they were able to use the customized tablet and were satisfied, a white board and marker worked well to help communicate.
This study has several limitations. As a feasibility study the sample size was small and generalizability is limited. The application was only available in English so patients who did not speak English were not able to participate. The iPad was our tablet of choice for purposes of this study, but there are other options on the market that may also help to support patient communication via applications and custom programs. Some of the iPad alternatives vary in price and may offer less expensive options to an iPad.
This study tested an intervention to bridge the gap in communication for patients in the immediate postoperative period. The findings of our study provided us with positive feedback from our patients in regards to using the customized tablet as an alternative communication tool. This solution enabled us to provide our patients with a “voice”.
Conclusion
With the growing use of technology in health care the use of a computer tablet and application as a means to communicate has proven to be an effective tool in improving the patient experience and outcomes in the postoperative setting. Introducing a computer tablet with a customized AAC application can offer a temporary means of communication, reduce stress, and enhance the patient’s quality of life8. In addition, technology can act as a resource that assists healthcare professionals as they face the difficult challenges in trying to support patients with impaired communication6,11,12. This alternate innovative solution addresses the need for further research on integrating technology in health care to improve the patient experience.
Acknowledgements:
We would like to acknowledge the MSKCC PACU and PSC leadership and staff; Sarah Jewell, MLIS, Bonnie Monson, RN, Bhuvanesh Singh, MD Lyndsay West, BS, the outpatient head and neck nurses, and most importantly our patients who participated in this study.
This research was funded in part by the Geri & ME Nursing Fund, The Society of Memorial Sloan Kettering, and the NIH/NCI Cancer Center Support Grant P30 CA008748.
Footnotes
Conflicts of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.MacAulay F ICU-Talk, a communication aid for intubated intensive care patients. 2002:226. [Google Scholar]
- 2.Happ MB, Roesch T, Kagan SH. Communication needs, methods, and perceived voice quality following head and neck surgery: a literature review. Cancer nursing. Jan-Feb 2004;27(1):1–9. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez CF, Rowe M, Thomas L, Shuster J, Koeppel B, Cairns P Enhancing the Communication of Suddenly Speechless Critical Care Patients. Am J Crit Care. May 2016;25(3):e40–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miglietta MA, Bochicchio G, Scalea TM. Computer-assisted communication for critically ill patients: a pilot study. The Journal of trauma. September 2004;57(3):488–493. [DOI] [PubMed] [Google Scholar]
- 5.Menzel LK. Factors related to the emotional responses of intubated patients to being unable to speak. Heart & lung : the journal of critical care. Jul-Aug 1998;27(4):245–252. [DOI] [PubMed] [Google Scholar]
- 6.Flores M, Musgrove K, Renner S, et al. A comparison of communication using the Apple iPad and a picture-based system. Augmentative and alternative communication (Baltimore, Md. : 1985). June 2012;28(2):74–84. [DOI] [PubMed] [Google Scholar]
- 7.McGonigle D, Mastrian K. Nursing informatics and the foundation of knowledge. Jones & Bartlett Publishers; 2014. [Google Scholar]
- 8.Costello J AAC intervention in the intensive care unit: The children’s hospital Boston model. Augmentative and alternative communication. 01 2000;16(3):137–153. [Google Scholar]
- 9.iPad Available in US on April 3 [press release]. Cupertino, CA: Apple Inc., 03/05/10 2010.
- 10.Version 2.0 of Award-Winning Proloquo2Go App for iPhone, iPad & iPod touch Speeds Up Communication, Adds New Voices and Customization Options [press release]. Amsterdam: AssitiveWare Technologies, 06/19/12 2012. [Google Scholar]
- 11.Rodriguez C, Rowe M Use of a speech-generating device for hospitalized post operative patients with head and neck cancer experiencing speechlessness. Oncol Nurs Forum. Mar 2010;37(2):199–205 [DOI] [PubMed] [Google Scholar]
- 12.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P & T : a peer-reviewed journal for formulary management. May 2014;39(5):356–364. [PMC free article] [PubMed] [Google Scholar]