Abstract
Background
The adverse association between income, health and survival is well documented, but little is known about how income trajectories influence health and survival for men and women. We aim to investigate sex differences in mortality and hospitalisations by income and income changes.
Methods
We performed a population-based, nationwide study including 1 063 787 Danes born 1935–1955 and residing in Denmark during 1980–2015. Income was calculated during two age intervals: 45–49 and 55–59 years. The average income was divided into quartiles for men and women separately, which formed the basis for the income trajectories. Individuals were followed up from age 60 until 2014/2015 for hospital admission and mortality, respectively.
Results
Men had higher mortality and were more hospitalised than women. Sex differences in mortality were most pronounced for people with stable low income (relative difference in hazard=1.93; 95% CI 1.89 to 1.98) and a downward income trajectory (1.91; 95% CI 1.85 to 1.98) with smaller sex differences for people with an upward trajectory (1.59; 95% CI 1.56 to 1.62) and stable high income (1.37; 95% CI 1.33 to 1.41). A similar pattern was found for family income. Regarding hospitalisations, similar results were found, though less pronounced. Investigation of mortality and hospitalisations by all possible trajectories demonstrated that income at ages 55–59 was an important predictor of mortality, with increasing mortality for decreasing income quartile.
Conclusion
Income trajectories as a proxy for change in social position have a larger influence on men’s than women’s health and mortality. Income in the late 50s is an important predictor of mortality, particularly for men.
INTRODUCTION
Although women in general live longer than men,1 they tend to report poorer self-rated health and worse physical functioning,2,3 they are more frail, have slightly more comorbidity4 and perform worse on physical tests.5,6 Despite increasing research on the male-female health survival paradox,7 we know little about the causes of sex differences or whether they can be reduced or eliminated.
Socioeconomic status (SES) is an important determinant of health,8 and differences in morbidity and mortality between SES groups are one of the most consistent epidemiological findings.9,10 In many populations, people with higher measures of SES such as income,11,12 education13,14 and occupational class15,16 are more likely to have longer life expectancy and reduced morbidity. Sex differences in the associations between income and health17 have received little attention, but SES gradients in mortality are generally weaker among women than men.11,12
SES has shown to be important for health and survival, but few studies have investigated the effects of income changes on health.18 A longitudinal study investigating income changes in relation to various self-assessed health measures19 found that income reduction over time resulted in poorer health compared with income increases or stable income, and that average income over a 5-year period had the strongest effects on health. Miething and Yngwe18 confirmed the higher risk of poor health following a substantial, downward income change, with stronger effects for men than women.
Research on the effect of changes in SES over the life course on sex differences in health and mortality has been limited. Using hospital admissions as indicator of population health,20 we investigated sex differences in health and mortality by income and income changes. We hypothesise that for women the loss of income and, thus, social status, is most strongly associated with health status and that for men it is most strongly associated with mortality.
METHODS
Setting and study population
This study is based on Danish register data that are linked through a 10-digit personal identification number.21-23 We used the Danish Civil Registration System (CPR) for information on gender, date of birth, migrations and mortality,21 the National Patient Register for information on hospitalisations, 24 the Income Statistics Register for information on income,22 the Population Education Register for information on education25 and the Employment Classification Module for information on employment.23 Family registration in the CPR was used for family income and to identify couples. Vital status was available until 31 December 2015, and data on hospitalisations were available until 31 December 2014.
The study population comprised persons born in 1935–1955 and residing in Denmark between 1 January 1980 and 31 December 2015. People alive at age 60 with available income measures at ages 45–49 and 55–59 were included in the study. To avoid reverse causation, that is, poor health causing low income,26 we excluded individuals retired before age 60, giving a total study population of 1 063 787 persons (online supplementary figure 1).
Income measures
Inhabitants in Denmark aged 15 and above are registered annually in the Income Statistics Register according to income.22 We used two income measures: individual disposable income (individual income after tax and interest expense) available from 1980 to 2014, and disposable household income (sum of income for all persons living in the family and liable to pay Danish taxes) available from 1990 to 2014. Income was calculated as an average income during 5 years investigated during two age periods: 45–49 and 55–59 years. The average income was divided into quartiles for men and women separately, which formed the basis for the four income trajectories: ‘stable high’ (income above median, but in the same quartile in both periods), ‘upward’ (an increase in income quartiles between periods), ‘downward’ (a decrease in income quartiles between periods) and ‘stable low’ (income below median, but in the same quartile in both periods). Because income was calculated as an average during 5 years, income values were corrected for inflation using the price index in Statistics Denmark, which was on average 3.1% per year for the period 1980–2014.
Sociodemographic variables
Measures of sociodemographic and SES characteristics included sex, age groups (60–64, 65–69, 70–74 and 75–81), birth cohorts (1935–1939, 1940–1944, 1945–1949 and 1950–1955) and highest attained education measured according to the International Standard Classification of Education (ISCED)27 grouped into low (ISCED 1–2), medium (ISCED 3) (ISCED 4 was not included because there were no observations in this category) and high (ISCED 5–8), and employment status containing employed (including self-employed, earners and assisting spouse), unemployed and others (including students and unknown). Education and employment were identified at age 45, if possible, or at the earliest age thereafter.
Statistical analyses
Survival analyses were used, with age as the timescale, to investigate all-cause mortality by individual and family income trajectories. Because family income was only available from 1990, analyses were restricted to the 1945–1955 birth cohorts. Due to differences in the income–health associations for singles and couples, particularly a higher mortality among single men with stable low income (online supplementary figure 2), analyses of family income were restricted to contain couples only. Follow-up started at age 60 and continued until death, emigration or end of follow-up in 2015, whichever came first. Using a Cox proportional hazards analysis, we calculated HRs with 95% CIs for mortality among men and women with an upward trajectory, a downward trajectory and stable low income, respectively, relative to people with stable high income. Furthermore, we estimated the relative difference in hazard between men and women by income trajectories. Hospitalisation was measured at each age from age 60 to 80 as admission to a hospital for any reason as an inpatient at this specific age. Using Poisson regressions stratified by birth cohort, we estimated incidence rate ratios (IRR) with 95% CIs, comparing all-cause hospitalisations for the different income trajectories with stable high income as the reference group. Also, we calculated IRRs for the differences between men and women. The Cox proportional hazards assumption was checked using the log-log plot of the Kaplan-Meier survival function, while the assumptions of the Poisson regressions were checked by plotting estimated log hazard functions.
Analyses were performed for the total study population and stratified by age groups. All mortality analyses were adjusted for birth cohorts, and the analyses combining all age groups were further adjusted for education and employment, respectively. Moreover, within a subsample of people with partners in the study population, we investigated mortality and hospitalisations by income trajectories for spouses/partners adjusted for birth cohorts and income quartiles for the index person at ages 45–49. Partners were defined as the spouse/partner at the age range 45–59 years or, if not available, the partner at the age closest to 45 years outside the interval. To examine a more detailed pattern of the income–health associations, we also investigated mortality and hospitalisations for all 16 possible income trajectories. All analyses were performed using Stata V.14.2.
RESULTS
A total of 115 008 (10.8%) deaths were observed in 1 063 787 persons during the 21-year follow-up period: 72 629 (13.3%) men and 42 379 (8.2%) women. Hospitalisation rates were 150/1000 person-years for men and 124/1000 person-years for women (table 1). Individual disposable income was on average higher among people aged 55–59 than peopled aged 45–49, and in both periods, income was higher for men than for women; however, more men than women (47.2% vs 41.9%) had an upward income trajectory, and slightly more men than women had a downward trajectory (8.8% vs 8.5%). Fewer men than women had stable low (17.0% vs 19.8%) and stable high income (27.0% vs 29.8%) (table 1).
Table 1.
Baseline characteristics of men and women born 1935–1955 and resident in Denmark after age 60 during 1980–2015
| Men | Women | Total study population | |
|---|---|---|---|
| Study population, n (%) | 544 696 (51.2) | 519 091 (48.8) | 1 063 787 |
| Birth cohorts | |||
| 1935–1939 | 100 088 (18.4) | 88 152 (17.0) | 188 240 (17.7) |
| 1940–1944 | 126 613 (23.3) | 115 516 (22.3) | 242 129 (22.8) |
| 1945–1949 | 154 079 (28.3) | 149 724 (28.8) | 303 803 (28.6) |
| 1950–1955 | 163 916 (30.1) | 165 699 (31.9) | 329 615 (31.0) |
| Emigrated after age 60 | 2799 (0.5) | 1718 (0.3) | 4517 (0.4) |
| Death after age 60* | 72 629 (13.3) | 42 379 (8.2) | 115 008 (10.8) |
| Hospitalisation rates per 1000 person-years after age† | 150 | 124 | 137 |
| Education‡ | |||
| Low | 141 228 (25.9) | 180 747 (34.8) | 321 975 (30.3) |
| Medium | 257 757 (47.3) | 194 500 (37.5) | 452 257 (42.5) |
| High | 136 777 (25.1) | 136 380 (26.3) | 273 157 (25.7) |
| Unknown/missing | 8934 (1.6) | 7464 (1.4) | 16 398 (1.5) |
| Employment | |||
| Employed | 507 235 (93.1) | 456 467 (87.9) | 963 702 (90.6) |
| Unemployed | 23 888 (4.4) | 28 331 (5.5) | 52 219 (4.9) |
| Others§ | 13 573 (2.5) | 34 293 (6.6) | 47 866 (4.5) |
| Individual disposable income | |||
| Median (IQR) ages 45–49 | 207 070 (172 243–253 000) | 170 718 (137 006–207 436) | 189 203 (152 889–230 788) |
| Median (IQR) ages 55–59 | 245 265 (196 161–312 090) | 196 289 (154 592–247 245) | 220 700 (172 343–280 730) |
| Change in individual disposable income¶ | |||
| Stable low | 92 785 (17.0) | 102 636 (19.8) | 195 421 (18.4) |
| Downward | 47 778 (8.8) | 44 021 (8.5) | 91 799 (8.6) |
| Upward | 257 069 (47.2) | 217 582 (41.9) | 474 651 (44.6) |
| Stable high | 147 064 (27.0) | 154 852 (29.8) | 301 916 (28.4) |
| Family disposable income | |||
| Median (IQR) ages 45–49 | 415 660 (324 453–500 631) | 413 046 (316 072–505 312) | 414 438 (320 105–502 949) |
| Median (IQR) ages 55–59 | 460 817 (347 056–577 331) | 432 038 (312 494–552 613) | 446 937 (328 864–565 584) |
| Change in family disposable income¶ | |||
| Stable low | 70 321 (22.3) | 67 328 (21.5) | 137 642 (21.9) |
| Downward | 42 686 (13.5) | 60 366 (19.3) | 103 052 (16.4) |
| Upward | 115 129 (36.5) | 92 262 (29.4) | 207 391 (33.0) |
| Stable high | 87 526 (27.7) | 93 877 (29.9) | 181 403 (28.8) |
Values are numbers (percentages) unless stated otherwise.
Before age 81 or 31 December 2015.
Before age 80 or 31 December 2014.
Highest completed education during 1980–2015. Low education refers to primary or lower secondary education, medium refers to upper secondary education and high refers to short-cycle tertiary education, bachelor’s level, master’s level, doctoral or equivalent level.
Contains students and missing.
Stable low: income below median, but in the same quartile in both periods. Downward: a decrease in income quartiles between periods. Upward: an increase in income quartiles between periods. Stable high: income above median, but in the same quartile in both periods.
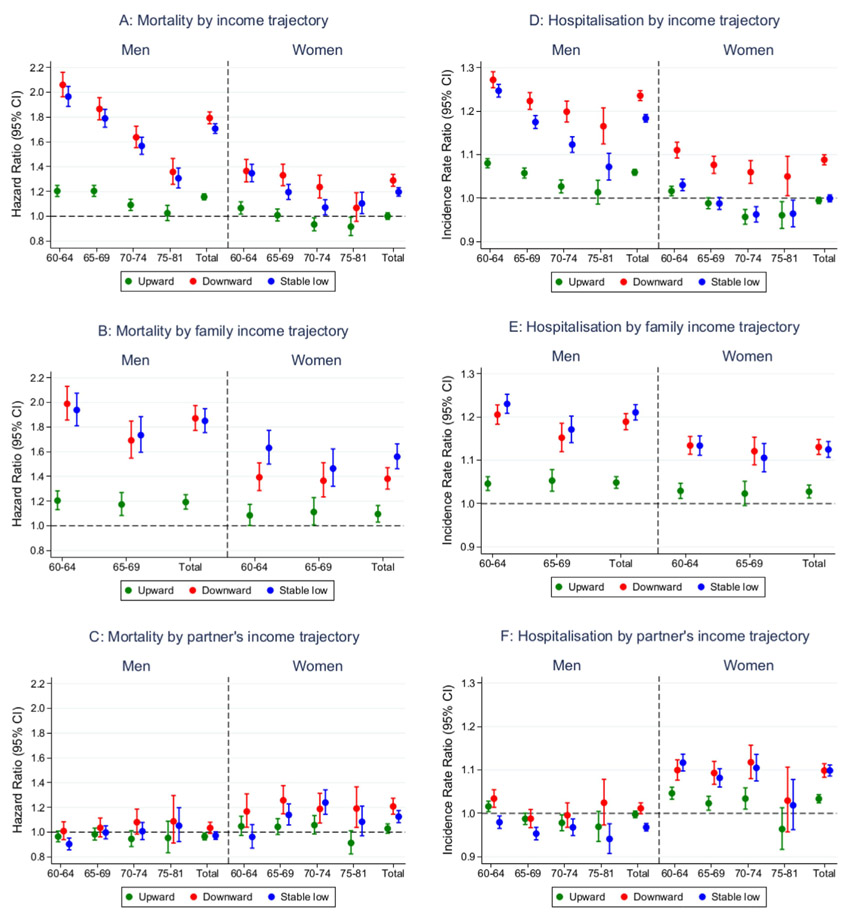
When investigating the income–health associations, we found the highest mortality among men with a downward income trajectory (HR=1.79; 95% CI 1.75 to 1.84) and stable low income (HR=1.71; 95% CI 1.67 to 1.75), but also men with an upward income trajectory (HR=1.16; 95% CI 1.13 to 1.18) had higher mortality than men with stable high income (figure 1A). A similar pattern was found for hospitalisations, though less pronounced (figure 1D). Women with a downward income trajectory (HR=1.29; 95% CI 1.24 to 1.34) and a stable low income (HR=1.20; 95% CI 1.16 to 1.23) had higher mortality than women with stable high income, whereas no difference was found for women with an upward income trajectory (figure 1A). Women with a downward income trajectory were more hospitalised than women with stable high income, whereas no overall differences were found for stable low income and an upward income trajectory (figure 1D). For family income, the highest mortality was found for people in families with stable low income and a downward income trajectory, but also people in families with an upward income trajectory had slightly higher mortality than people in families with stable high income, though most pronounced for men (figure 1B). A similar pattern was found for hospitalisations (figure 1E). However, the association between income and mortality depended on age, with the strongest association at ages 60–64, but with a decreasing effect with advancing age (figure 1A,B). For hospitalisations, a similar pattern was indicated, though less pronounced (figure 1D,E). Regarding mortality and hospitalisations by partner’s income trajectory, we found that women with partners having a downward income trajectory and a stable low income had higher mortality and were more often hospitalised than women with partners having a stable high income. Contrarily, only small differences were found for men in relation to their partners’ income trajectory (figure 1C,F). Generally, the patterns remained similar after further adjustments for education and employment, respectively (online supplementary table 1).
Figure 1.
Associations between all-cause mortality (A–C) and hospitalisations (D–F) by individual income, family income and partner’s income trajectories for men and women, respectively.
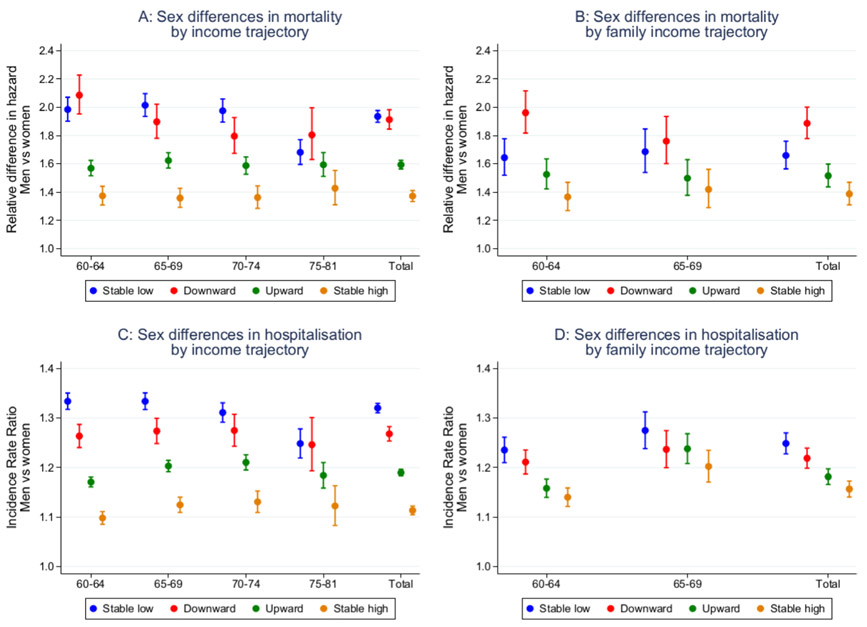
When examining sex differences, we found that men had higher mortality and were more hospitalised than women. Sex differences in mortality and hospitalisations were most pronounced for people with a stable low income (relative difference in hazard=1.93; 95% CI 1.89 to 1.98; IRR=1.32; 95% CI 1.31 to 1.33) and a downward income trajectory (1.91; 95% CI 1.85 to 1.98; IRR=1.27; 95% CI 1.25 to 1.28) with smaller sex differences for people with an upward trajectory (1.59; 95% CI 1.56 to 1.62; IRR=1.19; 95% CI 1.18 to 1.20) and a stable high income (1.37; 95% CI 1.33 to 1.41; IRR=1.11; 95% CI 1.10 to 1.12) (figure 2A,C). Identical patterns were found for family income, although slightly lower sex differences in mortality and hospitalisations were found for people in families with a stable low income and regarding hospitalisations also for people with a downward income trajectory (figure 2B,D). This was also the case after further adjustments for education and employment, respectively (online supplementary table 2). Sex differences were relatively stable over age groups except from a slight decrease in stable low income at ages 75–81 (figure 2A,C).
Figure 2.
Sex differences in all-cause mortality (A, B) and hospitalisations (C, D) by individual and family income trajectories.
Examination of mortality by all possible income trajectories demonstrated that the association with mortality for the upward and downward income trajectories was more influenced by the income quartile at ages 55–59 compared with the income quartile at ages 45–49. For instance, for people having an upward income trajectory ending at the highest quartile in their late 50s, the mortality was more similar to those with stable incomes at the highest quartile compared with those from the income quartile that they originally belonged to. This pattern was also observed for hospitalisations among men, whereas no clear pattern was found for women (table 2).
Table 2.
All-cause mortality and hospitalisations for Danish men and women aged 60 and above for the 16 possible income trajectories by individual income
| Mortality |
Hospitalisation |
||||
|---|---|---|---|---|---|
| HR (95% CI) |
IRR (95% CI) |
||||
| Men | Women | Men | Women | ||
| Income quartiles (ages 45–49) |
Income quartiles (ages 55–59) |
||||
| 4 | 4 (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 3 | 4 | 1.10 (1.06 to 1.13) | 1.04 (1.00 to 1.09) | 1.03 (1.02 to 1.04) | 1.02 (1.01 to 1.04) |
| 2 | 4 | 1.14 (1.08 to 1.19) | 1.02 (0.96 to 1.09) | 1.09 (1.07 to 1.10) | 1.03 (1.01 to 1.05) |
| 1 | 4 | 1.22 (1.14 to 1.30) | 1.05 (0.96 to 1.15) | 1.09 (1.07 to 1.11) | 1.03 (1.01 to 1.05) |
| 4 | 3 | 1.52 (1.42 to 1.62) | 1.23 (1.12 to 1.34) | 1.15 (1.13 to 1.18) | 1.12 (1.09 to 1.14) |
| 3 | 3 | 1.45 (1.40 to 1.50) | 1.26 (1.21 to 1.32) | 1.13 (1.12 to 1.14) | 1.09 (1.07 to 1.10) |
| 2 | 3 | 1.42 (1.38 to 1.47) | 1.21 (1.16 to 1.27) | 1.12 (1.11 to 1.13) | 1.06 (1.05 to 1.08) |
| 1 | 3 | 1.55 (1.48 to 1.62) | 1.15 (1.08 to 1.22) | 1.19 (1.18 to 1.21) | 1.03 (1.02 to 1.05) |
| 4 | 2 | 1.85 (1.68 to 2.04) | 1.52 (1.34 to 1.73) | 1.26 (1.21 to 1.30) | 1.11 (1.07 to 1.15) |
| 3 | 2 | 1.88 (1.79 to 1.97) | 1.51 (1.42 to 1.59) | 1.28 (1.26 to 1.30) | 1.16 (1.15 to 1.18) |
| 2 | 2 | 1.91 (1.85 to 1.97) | 1.40 (1.34 to 1.46) | 1.23 (1.22 to 1.25) | 1.11 (1.09 to 1.12) |
| 1 | 2 | 1.83 (1.76 to 1.89) | 1.22 (1.16 to 1.28) | 1.24 (1.23 to 1.25) | 1.03 (1.01 to 1.04) |
| 4 | 1 | 2.04 (1.84 to 2.27) | 1.26 (1.03 to 1.55) | 1.29 (1.24 to 1.34) | 1.07 (1.01 to 1.13) |
| 3 | 1 | 2.46 (2.30 to 2.62) | 1.55 (1.40 to 1.72) | 1.32 (1.29 to 1.35) | 1.14 (1.11 to 1.18) |
| 2 | 1 | 2.65 (2.54 to 2.75) | 1.54 (1.44 to 1.64) | 1.41 (1.39 to 1.43) | 1.11 (1.09 to 1.13) |
| 1 | 1 | 2.30 (2.22 to 2.37) | 1.35 (1.29 to 1.40) | 1.28 (1.27 to 1.29) | 0.99 (0.98 to 1.00) |
IRR, incidence rate ratio.
Sex differences for all income trajectories confirmed the pattern from the main trajectories with the most pronounced sex differences for people with a downward income trajectory and a stable low income. Nevertheless, income in the late 50s was also important for sex differences, with the smallest differences in mortality between men and women with incomes in the highest quartile at ages 55–59 and the largest differences for people with incomes in the lowest quartile. A similar pattern was found for hospitalisations, though less clear (table 3).
Table 3.
Sex differences in all-cause mortality and hospitalisation for the 16 possible income trajectories by individual income among Danish men and women aged 60 and above
| Income quartiles (ages 45–49) |
Income quartiles (ages 55–59) |
Mortality HR (95% CI) |
Hospitalisation IRR (95% CI) |
|---|---|---|---|
| 4 | 4 | 1.29 (1.24 to 1.35) | 1.10 (1.09 to 1.11) |
| 3 | 4 | 1.39 (1.33 to 1.44) | 1.11 (1.10 to 1.12) |
| 2 | 4 | 1.46 (1.36 to 1.57) | 1.17 (1.15 to 1.19) |
| 1 | 4 | 1.51 (1.36 to 1.58) | 1.17 (1.13 to 1.20) |
| 4 | 3 | 1.61 (1.45 to 1.78) | 1.13 (1.10 to 1.17) |
| 3 | 3 | 1.50 (1.44 to 1.56) | 1.14 (1.13 to 1.16) |
| 2 | 3 | 1.54 (1.49 to 1.60) | 1.16 (1.15 to 1.17) |
| 1 | 3 | 1.74 (1.64 to 1.85) | 1.27 (1.25 to 1.29) |
| 4 | 2 | 1.60 (1.37 to 1.87) | 1.27 (1.25 to 1.29) |
| 3 | 2 | 1.62 (1.52 to 1.72) | 1.25 (1.19 to 1.32) |
| 2 | 2 | 1.77 (1.71 to 1.82) | 1.21 (1.19 to 1.23) |
| 1 | 2 | 1.92 (1.85 to 1.99) | 1.23 (1.22 to 1.24) |
| 4 | 1 | 2.10 (1.67 to 2.63) | 1.32 (1.31 to 1.34) |
| 3 | 1 | 2.08 (1.85 to 2.33) | 1.27 (1.22 to 1.32) |
| 2 | 1 | 2.23 (2.09 to 2.37) | 1.39 (1.36 to 1.42) |
| 1 | 1 | 2.15 (2.09 to 2.22) | 1.41 (1.40 to 1.43) |
IRR, incidence rate ratio.
DISCUSSION
The present study examined sex differences in mortality and hospitalisation after age 60 by income changes between 45–49 and 55–59 years. Overall, we found that income differentiates men more than women regarding mortality and hospitalisations. Sex differences were most pronounced for people with a stable low income and a downward income trajectory, with smaller sex differences for people with an upward income trajectory and a stable high income. Investigation of mortality and hospitalisations by all possible income trajectories showed that a main predictor of mortality was income in the late 50s, particularly for men.
We hypothesised that, for women, loss of income would be most strongly associated with health status, whereas for men we expected the association to be strongest with mortality. For all income trajectories, we found that men had higher mortality than women. Thus, it seems that men are more vulnerable than women towards income loss, and that men do not benefit as much as women from an increase in income, which may contribute to the shorter survival among men. Furthermore, the pattern of hospitalisations by income trajectories was in the same direction as that of mortality, lending no support to the notion that changes in income over the life course can explain the poorer health of women compared with men; nevertheless, we found that the health and survival of women were slightly negatively influenced by the income of their partner when the partner had a downward income trajectory or a stable low income. Few studies have examined the effects of partner's income,28 but a study comparing the relative importance of spouses’ SES indicators to mortality found that both education, occupational class and income were slightly associated with women’s mortality, whereas in men, only wife’s education had an impact on mortality.28 Similarly, McDonough et al found that elevated spousal income lowered the odds of dying for women, whereas the opposite was found for men.29
Similar to previous studies on income–health associations (eg, ref 8-10 30) we found that SES is a powerful determinant of health and that being disadvantaged during a period in mid-life has a significant impact on health and mortality particularly for men. Social mobility theories hypothesise that SES mobility across the life course impacts adult health. The ‘health constraint’ hypothesis posits that socially mobile individuals have the health characteristics of both the SES groups that they leave and of their new social group.31 There is growing evidence that life course SES is associated with cardiovascular disease risk.32,33 Findings from the British Women’s Heart and Health Study suggest that women aged 60–79 for whom SES improved or decreased over the life course adopt the eating and exercising habits of their new social group.34 In this study, the effects on mortality of a downward trajectory were overall at the same level as the effects of stable low income. Fowever, people in families with an upward income trajectory had higher risk of mortality than people with a stable high income, lending support for the ‘health constraint’ hypothesis, placing socially mobile individuals at an intermediate risk.31
In line with earlier studies,35-37 we found smaller relative associations between individual income and mortality with advancing age, indicating that income best predicts differences in health and mortality among the youngest elderly. The reason may be that the elderly population represents a selected group38 or that income in middle age does not accurately reflect the true socioeconomic conditions to which individuals are exposed in large portions of their adulthood. Fowever, importantly, this study demonstrates that income at ages 55–59 is an important predictor of mortality after age 60, suggesting that income in the late 50s may compensate, at least partly, for a lower income in middle age.
Previous studies have highlighted the importance of using both household and individual income measures,17,39 showing that household income is more strongly and consistently associated with health than individual income.17 This study demonstrated that the way in which income was measured appeared to make little difference for sex differences in mortality and hospitalisations except from a slightly lower sex difference for stable low income when using family income. Also, we found overall similar results when adjusting for education and employment, suggesting that, in Denmark, income has an independent effect on health and mortality.
The main strength of this study is the use of Danish registers with complete unselected information on mortality and hospital admissions. The study population provides nationwide coverage with 21 years of follow-up. Thus, there is little selection bias due to non-response or loss to follow-up. A central concern in income-health analyses is the possibility of confounding by reverse causation.26 Although reverse causation cannot be completely ruled out because of, for example, no control for baseline health measures, the longitudinal design with measures of income that precede the health outcomes and the exclusion of early retirees can help in the assessment of the direction of causality. A limitation was that mortality and hospital admissions before age 60 were not considered, and that only people with available income measures in the two investigated age periods were included. Furthermore, the study design did not allow us to examine whether the observed sex differences changed over time or across cohorts. In Denmark, hospital care is financed through taxes, and access to healthcare services is free and universally independent of sex and SES.40 Thus, the external validity in less egalitarian countries may be limited. Our study examined sex differences in mortality and hospitalisations by income changes, but the underlying reasons for these differences should be addressed in future studies.
In conclusion, this study demonstrated that, after age 60, income differentiation is more marked among men than women regarding mortality and hospitalisation. Sex differences were most pronounced for people with a stable low income and a downward income trajectory, with smaller differences between men and women with an upward income trajectory and a stable high income. Income in the late 50s was a main predictor of mortality, particularly among men. The study lends support for the notion that men are more vulnerable to income loss than women, possibly contributing to the shorter survival among men, whereas income change cannot explain why women’s health is generally poorer than men’s health.
Supplementary Material
What is already known on this subject.
Although socioeconomic status is an important determinant of health, there has been a lack of attention to sex differences in income–health associations, and very little is known about the degree to which changes in socioeconomic position over the life course can explain sex differences in health and mortality.
What this study adds.
Through a large sample of more than 1 million Danes, we demonstrate that income in middle age has a greater differentiating effect on men than women regarding mortality and hospitalisations after age 60.
Men had higher mortality and were more hospitalised than women, but sex differences were most pronounced for people with stable low income and a downward income trajectory, and sex differences were smaller among people with an upward income trajectory and a stable high income.
Income level in the age period 55–59 years was a main predictor of mortality for both sexes and of hospitalisations among men.
Acknowledgments
Funding This study was supported by research grants from the National Institute on Aging (NIA-PO1-AG08761, NIAP01-AG031719) and from the European Union’s Seventh Framework Programme (FP7/2007–2011) under grant agreement number 259679.
Footnotes
Competing interests None declared.
Patient consent for publication Not required.
Ethics approval The study involves secondary data analyses of existing register data approved by the Danish Data Protection Agency.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available.
REFERENCES
- 1.Barford A, Dorling D, Smith GD, et al. Life expectancy: women now on top everywhere. BMJ 2006;332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crimmins EM, Kim JK, Solé-Auró A. Gender differences in health: results from share, ELSA and Hrs. Eur J Public Health 2011;21:81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scheel-Hincke LL, Möller S, Lindahl-Jacobsen R, et al. Cross-National comparison of sex differences in ADL and IADL in Europe: findings from share. Eur J Ageing 2019;64:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahrenfeldt LJ, Möller S, Thinggaard M, et al. Sex differences in comorbidity and frailty in Europe. Int J Public Health 2019;64:1025–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahrenfeldt LJ, Scheel-Hincke LL, Kjærgaard S, et al. Gender differences in cognitive function and grip strength: a cross-national comparison of four European regions. Eur J Public Health 2019;29:667–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wheaton FV, Crimmins EM. Female disability disadvantage: a global perspective on sex differences in physical function and disability. Ageing Soc 2016;36:1136–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oksuzyan A, Juel K, Vaupel JW, et al. Men: good health and high mortality. sex differences in health and aging. Aging Clin Exp Res 2008;20:91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mackenbach JP, Valverde JR, Artnik B, et al. Trends in health inequalities in 27 European countries. Proc Natl Acad Sci U S A 2018;115:6440–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mackenbach JP, Valverde JR, Bopp M, et al. Determinants of inequalities in life expectancy: an international comparative study of eight risk factors. The Lancet Public Health 2019;4:e529–37. [DOI] [PubMed] [Google Scholar]
- 10.Kriegbaum M, Hougaard Charlotte Ørsted, Andersen I, et al. Life course analysis on income and incident AMI: a Danish register-based cohort study. J Epidemiol Community Health 2019;73:810–6. [DOI] [PubMed] [Google Scholar]
- 11.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001-2014. JAMA 2016;315:1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bilal U, Cainzos-Achirica M, Cleries M, et al. Socioeconomic status, life expectancy and mortality in a universal healthcare setting: An individual-level analysis of >6 million Catalan residents. Prev Med 2019;123:91–4. [DOI] [PubMed] [Google Scholar]
- 13.Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health 2018;39:273–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brønnum-Hansen H, Eriksen ML, Andersen-Ranberg K, et al. Persistent social inequality in life expectancy and disability-free life expectancy: outlook for a differential pension age in Denmark? Scand J Public Health 2017;45:459–62. [DOI] [PubMed] [Google Scholar]
- 15.Toch-Marquardt M, Menvielle G, Eikemo TA, et al. Occupational class inequalities in all-cause and cause-specific mortality among middle-aged men in 14 European populations during the early 2000s. PLoS One 2014;9:e108072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanaka H, Nusselder WJ, Bopp M, et al. Mortality inequalities by occupational class among men in Japan, South Korea and eight European countries: a national register-based study, 1990–2015. J Epidemiol Community Health 2019;73:750–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rahkonen O, Arber S, Lahelma E, et al. Understanding income inequalities in health among men and women in Britain and Finland. Int J Health Serv 2000;30:27–47. [DOI] [PubMed] [Google Scholar]
- 18.Miething A, Yngwe MA. Stability and variability in income position over time: exploring their role in self-rated health in Swedish survey data. BMC Public Health 2014;14:1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benzeval M, Judge K. Income and health: the time dimension. Soc Sci Med 2001;52:1371–90. [DOI] [PubMed] [Google Scholar]
- 20.Höhn A, Larsen LA, Schneider DC, et al. Sex differences in the 1-year risk of dying following all-cause and cause-specific hospital admission after age 50 in comparison with a general and non-hospitalised population: a register-based cohort study of the Danish population. BMJ Open 2018;8:e021813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pedersen CB. The Danish civil registration system. Scand J Public Health 2011;39:22–5. [DOI] [PubMed] [Google Scholar]
- 22.Baadsgaard M, Quitzau J. Danish registers on personal income and transfer payments. Scand J Public Health 2011;39:103–5. [DOI] [PubMed] [Google Scholar]
- 23.Petersson F, Baadsgaard M, Thygesen LC. Danish registers on personal labour market affiliation. Scand J Public Health 2011;39:95–8. [DOI] [PubMed] [Google Scholar]
- 24.Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol 2015;7:449–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jensen VM, Rasmussen AW. Danish education registers. Scand J Public Health 2011;39:91–4. [DOI] [PubMed] [Google Scholar]
- 26.Elstad JI. Health-Related mobility, health inequalities and gradient constraint. discussion and results from a Norwegian study. Eur J Public Health 2001;11:135–40. [DOI] [PubMed] [Google Scholar]
- 27.UNESCO. International standard classification of education ISCED 2011, 2012. Available: http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf [Google Scholar]
- 28.Skalická V, Kunst AE. Effects of spouses’ socioeconomic characteristics on mortality among men and women in a Norwegian longitudinal study. Soc Sci Med 2008;66:2035–47. [DOI] [PubMed] [Google Scholar]
- 29.McDonough P, Williams DR, House JS, et al. Gender and the socioeconomic gradient in mortality. J Health Soc Behav 1999;40:17–31. [PubMed] [Google Scholar]
- 30.Padyab M, Malmberg G, Norberg M, et al. Life course socioeconomic position and mortality: a population register-based study from Sweden. Scand J Public Health 2013;41:785–91. [DOI] [PubMed] [Google Scholar]
- 31.Blane D, Smith GD, Bartley M. Social selection: what does it contribute to social class differences in health? Sociol Health Illness 1993;15:1–15. [Google Scholar]
- 32.Stringhini S, Zaninotto P, Kumari M, et al. Socio-Economic trajectories and cardiovascular disease mortality in older people: the English longitudinal study of ageing. Int J Epidemiol 2018;47:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lawlor DA, Ebrahim S, Davey Smith G. Adverse socioeconomic position across the lifecourse increases coronary heart disease risk cumulatively: findings from the British women’s heart and health study. J Epidemiol Community Health 2005;59:785–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Watt HC, Carson C, Lawlor DA, et al. Influence of life course socioeconomic position on older women’s health behaviors: findings from the British women’s heart and health study. Am J Public Health 2009;99:320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Illness HR. Not age, is the leveler of social mortality differences in old age. J Gerontol B Psychol Sci Soc Sci 2011;66:374–9. [DOI] [PubMed] [Google Scholar]
- 36.Mortensen LH, Rehnberg J, Dahl E, et al. Shape of the association between income and mortality: a cohort study of Denmark, Finland, Norway and Sweden in 1995 and 2003. BMJ Open 2016;6:e010974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rehnberg J, Fors S, Fritzell J. Divergence and convergence: how do income inequalities in mortality change over the life course? Gerontology 2019;65:313–22. [DOI] [PubMed] [Google Scholar]
- 38.Kaplan GA, Seeman TE, Cohen RD, et al. Mortality among the elderly in the Alameda County study: behavioral and demographic risk factors. Am J Public Health 1987;77:307–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fritzell J, Nermo M, Lundberg O. The impact of income: assessing the relationship between income and health in Sweden. Scand J Public Health 2004;32:6–16. [DOI] [PubMed] [Google Scholar]
- 40.Olesen F, Hansen RP, Vedsted P. Delay in diagnosis: the experience in Denmark. BrJ Cancer 2009;101:S5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.