Abstract
Objectives
To evaluate whether a newly developed care pathway, Treatment and Recovery In PsycHosis (TRIumPH), is feasible, acceptable and effective in meeting National Institute of Health and Care Excellence (NICE) quality standards in a timely manner.
Methods
This is a pragmatic, non-randomised, prospective, mixed methods study comparing an implementation (TRIumPH) and comparator site (not implementing TRIumPH) across three cohorts to assess feasibility, acceptability and effectiveness of the integrated pathway.
Setting
Early intervention in psychosis (EIP) services at two National Health Service organisations in South of England.
Participants
All patients accepted into EIP services between 1 June 2014 and 31 May 2017 were each followed up for 1 year within their respective cohorts.
Methodology
Quantitative data consisted of routinely collected clinical data retrieved from patient records to assess whether the implementation of TRIumPH achieved better concordance to NICE standards. These included time to access services, physical health assessments, clinical outcomes based timeliness of delivery and acute data. The controlled trial has evaluated the effect of TRIumPH (Intervention) with Care As Usual (Comparator). Qualitative measures consisted of questionnaires, interviews and focus groups to assess acceptability and satisfaction. Outcome measures were compared within the baseline, year 1 and year 2 cohorts and between the two sites. Quantitative data were statistically analysed by comparing means and proportions.
Results
Time to assessment improved in the implementation site and remained within the target in comparator site. Meeting of quality standards increased substantially in the implementation site but was more variable and reached lower levels in the comparator site especially for physical health standards. Cognitive therapy for psychosis, family intervention and carer and employment support were all offered to a greater extent in the implementation site and uptake increased over the period.
Conclusions
Pathway implementation generally led to greater improvements in achievement of access and quality standards compared with comparator site.
Trial registration number
UK Clinical Research Network Portfolio (19187)
Keywords: adult psychiatry, early intervention, integrated care pathways, schizophrenia & psychotic disorders
Strengths and limitations of this study.
This is the only evaluation of a psychosis care pathway and results will be generalisable to NHS and managed care organisations.
Baseline differences between the sites could potentially affect interpretation of the results and conclusions that need to be interpreted in this light.
Two additional sites initially planned to participate but withdrew during the course of the study due to inability to provide required data.
Routine data were used to evaluate implementation which had the disadvantage of leading to significant amounts of missing data in some areas.
Financial and human resource limitations may have had an impact on results.
Background
Schizophrenia is listed as the eighth leading cause of DALYs worldwide in the age group 15–44 years in the World Health Report.1 In addition to the direct cost, there is a considerable burden on the relatives2 and life expectancy is reduced by approximately 15–20 years, mostly because of physical health problems.3
A primary factor contributing to the impact of schizophrenia is that the longer the duration of untreated psychosis (DUP) the worse the outlook especially for social functioning and recovery.4 5 DUP has been found to be the strongest predictor of symptom severity and prognosis.6 A meta-analysis showed a mean DUP of 61.3 weeks7 and further evidence from transcultural and international research suggests that DUP ranges between 364 and 721 days5 6 and so reducing DUP is of individual, national and international importance.7
In order to address both the impact of schizophrenia and the length of DUP the UK government strategy ‘No Health Without Mental Health’8 acknowledged that more must be done to address the disparity in care for people experiencing psychosis. It highlighted the importance of prevention, early detection and support for evidence-based models such as early intervention in psychosis (EIP) services. The national access and waiting time standard (AWTS) for psychosis9 announced in England from 1 April 2016 required that more than 50% of people experiencing a first episode psychosis should commence a National Institute of Health and Care Excellence (NICE) recommended package of care10 within 2 weeks of referral to secondary care services. This action was specifically introduced to reduce DUP and ensure people access services and start treatment in a timely manner.
In addition to the introduction of care standards the Five Year Forward View (NHS England)11 recommended development of standardised care pathways for every major mental health condition. Evidenced-based integrated pathways provide a standardised framework for good clinical practice, reduce variation in care and improving outcomes for patients through providing timely access and intervention.12 Standardised pathways improve quality by improving multidisciplinary communication with different care agencies using care planning and improve patient satisfaction.13 NICE has formulated quality standards for treatment of schizophrenia and psychosis10 but does not prescribe time frames.
Treatment and Recovery In PsycHosis (TRIumPH) is a codeveloped, integrated care pathway for psychosis that prescribes time frames around access and clinical interventions as developed in England.14–16 The work has used a similar approach to that taken to improve care in other health areas like acute stroke care13 and has produced a demonstrable improvement in outcomes for patients and carers. This new psychosis pathway aims to reduce the impact of disease and promote recovery by ensuring that every individual gets the best evidence-based care at the right time and in the right place.
In developing the pathway, a multipronged approach has been used, using (1) intelligence from information, (2) coproduction with individuals with lived experience of mental illness and their carers and (3) engagement with clinicians and other stakeholders including commissioners, primary care and third sector organisations. The development of TRIumPH used a robust methodology, outlined in previous publications by this group, which can be adapted and adopted nationally and internationally.14–16
Therefore, the pathway goals are to treat the symptoms as early as possible, provide skills to patients and their families, maintain the improvement over a period, prevent relapses and reintegrate the individuals into the community so that they can lead as normal a life as possible.
Study objectives
The objective of this study was to assess the feasibility, acceptability and effectiveness of the TRIumPH psychosis care pathway.
Does implementation of TRIumPH improve standards in line with the NICE quality standards as measured by: time taken to access services and waiting times, lengths of hospital stay, clinical outcomes based on Health of the Nation Outcome Scales (HoNOS scores),17 treatment options offered and how timely the delivery of these were?
How did staff members, service users and carers experience the implementation of the pathway? Was it feasibile and acceptable?
Methods
Study design
This is a prospective, mixed methods, pragmatic18 and non-randomised study comparing the intervention implementation (TRIumPH pathway) and comparison site that had treatment as usual (TAU) to evaluate feasibility, acceptability and effectiveness of an integrated care pathway, TRIumPH. Both qualitative and quantitative data were collected and analysed.
Setting
The study originally had four NHS sites: EIP teams from two pathway implementation and two comparator organisations. However, one pathway and one comparator site withdrew in the early stages due to an inability to provide necessary data. The remaining two NHS sites had pre-existing EIP teams who were working according to principles originally set out in the NHS Plan (2000).
Implementation site
The implementation site was an NHS Trust in the south of England implementing the pathway and covers a population of 1.3 million. This site had four EIP service teams. The Trust was predicted to have an incidence of psychosis of 100 patients (psymaptic.org).
Comparator site
The comparator was an NHS Trust in the south of England and covers a population of 780 000. This site had two EIP teams at the start of the study. Due to the needs of the service these two teams were amalgamated into one team during the study period. This Trust was predicted to have an incidence of psychosis of 54 patients (psymaptic.org).
Intervention
TRIumPH is an integrated care pathway for psychosis that emphasises the importance of timely access and interventions (see figure 1). The development, design and details of this pathway have been described in detail in the protocol paper15 and in other publications.14 16
Figure 1.
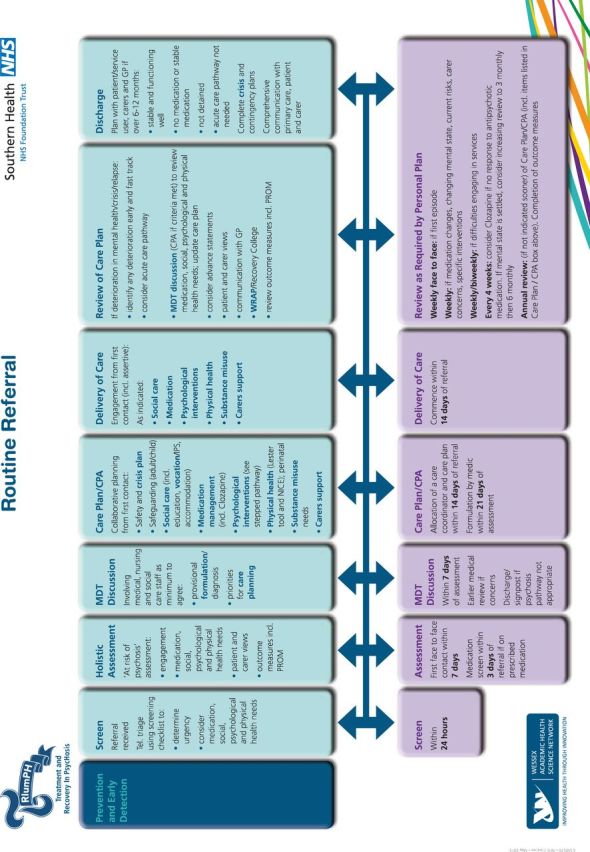
TRIumPH pathway. CPA, Care Programme Approach; GP, General Practitioner; MDT, multidisciplinary team; PROM, Patient related outcome measure; TRIumPH, Treatment and Recovery in PsycHosis.
Treatment as usual
Participants in the comparator site received TAU. This usually consisted of care coordination and outpatient appointments when needed. Access to psychological treatments and physical health interventions had been variable. The AWTS target was launched in April 2016, 1 year after the study started, and has influenced access to treatment in both the implementation and comparator site, as a national standard for seeing referrals within 2 weeks was established. Other requirements for the standard included physical health assessments and availability of treatments.
Research ethics approval and safety assessments
Ethics approval was obtained from East of Scotland Research Ethics Service (REC Ref no: LR/15/ES/0091). Written consent was taken for all those providing data for the questionnaires, focus groups and interviews. Quantitative data used for the study were limited to that routinely collected as part of clinical care and consent to access for research purposes was not sought by individual but approved via NHS Ethics Service. No adverse events were identified as a direct result of implementation of the pathway.
Patient and public involvement
Coproduction workshops were held with patients, carers and clinicians to develop the pathway and key outcome areas and a service user researcher was present in the study team. For further details see the previously published protocol.15
Outcome measures
Feasibility and acceptability were assessed through both qualitative and quantitative data collection regarding recruitment, retention and adherence to the process. These measures were defined based on TRIumPH pathway15 16 and NICE recommendations.10
Quantitative measures
Timeliness of access: waiting times from EIP referral and central triage points (CTPs), time to allocation and engagement with a care coordinator, time to multidisciplinary team (MDT) discussion, time to medical formulation, time to care planning approach (Care Programme Approach (CPA) meeting), time to risk assessment completion (see figure 1).
NICE-recommended interventions offered: medication, physical health assessment (within 3 months in accordance with NICE quality standard), psychological intervention (offered within 6 months), carers support, family intervention and employment support.
Clinical outcomes: severity of symptoms (HoNOS scores,17 number of acute admissions during referral, length of hospital stay, Mental Health Act (MHA) sections during referral, A&E (Accident and Emergency Department) attendance and contact with acute mental health services post EIP referral.
-
Reason for discharge to assess appropriateness of referrals.
These measures were collected for each cohort of participants from the time of their referral for 1 year. The HoNOS17 were the source of clinical outcome data collected routinely in the NHS including in EIP. It comprises 12 scales covering health and social care using a severity measure from 0 to 4 with 2–4 signifying clinically significant disorder.
Qualitative measures
Satisfaction and acceptability were assessed using questionnaires, interviews and focus groups. The later two were only conducted at the intervention site to enable a process evaluation of the implementation of the pathway at this site. Measures consisted of the following: patient experience (using specifically designed patient experience focus groups/interviews), staff experience (staff questionnaires and focus groups designed to measure the impact of the pathway on staff experience) and carer experience (using carer focus groups/interviews). Staff experience was assessed at baseline and after 12 and 24 months, carer and service user experience was assessed at 12 and 24 months.
Sample size
As this was a prospective and pragmatic study, no a priori power and sample size calculations were performed or required as routinely collected and available data for all patients and staff during the study period was used.
Data collection
Baseline data were collected for the period 1 June 2014 to 31 May 2015. The pathway was launched on 1 June 2015 and disseminated to four EIP teams in the implementation site. Data were collected over the subsequent 2-year period on every patient who was referred to and accepted by the EIP teams in participant organisations. This led to the following cohorts who were all followed up for 1 year:
Baseline (referral received 1 June 2014 to 31 May 2015).
Year 1 (referral received 1 June 2015 to 31 May 2016).
Year 2 (referral received 1 June 2016 to 31 May 2017).
Qualitative methods
Staff, patients and carers were approached via the mental health teams they were currently engaged with. Patients and carers showed a preference to semistructured interviews rather than attending offered focus groups. All focus groups and interviews were audio recorded, transcribed and then coded and analysed using thematic analysis.19 Thematic analysis was inductive using themes developed from the data produced by the structured scripts and remained at a semantic level to allow for a description of the views reported. Staff were also invited to complete a questionnaire to explore the impact of the pathway on staff experience and enable comparisons across the three time points (baseline, 12 and 24 months).
Statistical analysis
Continuous normal data were summarised by mean and SD, with comparisons to baseline made using t-tests. Continuous data that are non-normal, as tested by Kolmogorov-Smirnov or Shapiro-Wilk tests, were presented by median and IQR and compared using Mann-Whitney U test. Categorical variables were presented as n (%) and compared using χ2 or Fisher’s exact test as appropriate. However, no statistical comparisons were undertaken when the event rates in most groups were <5. P value <0.05 was assumed to indicate statistical significance. Missing data were excluded on a case-by-case basis. Statistical analyses were undertaken using IBM SPSS Statistics V.19 and R V.3.4.2. It was planned that in addition to analysing data by comparing means (or ranks) or proportions (depending on the data), regression analyses would be used to compare groups (for effect sizes and predictive models). However the extent of the missing data for many outcome variables meant that the validity and reliability would have been compromised. Thus, analysis was restricted to exploratory analysis rather than measuring effects and developing models using regression approach.
Results
The participants information and demographic data are presented in table 1. The demographic characteristics of individuals in both comparator and pathway site were broadly similar throughout the study period, with around 3 of 5 subjects being male, and the majority being of Caucasian ethnicity (88%–93%), unemployed (26%–54%) and residing in mainstream housing (76%–88%).
Table 1.
Demographic information for all individuals referred to EIP service. numbers represent either median (IQR) for continuous variables or proportions for categorical variables
| Implementation site | Comparator site | |||||
| Baseline (n=123) | Year 1 (n=416) | Year 2 (n=463) | Baseline (n=237) | Year 1 (n=271) | Year 2 (n=252) | |
| Age (years) | 22.4 (19.3 to 28.2) | 21.4 (19.0 to 26.1) | 21.6 (19.0 to 25.9) | 19.4 (16.7 to 24.9) | 19.7 (17.1 to 24.8) | 21.8 (17.9 to 30.3) |
| Gender | ||||||
| Female | 35% | 40% | 39% | 43% | 40% | 38% |
| Male | 65% | 60% | 61% | 57% | 60% | 62% |
| Ethnicity | ||||||
| White | 88% | 89% | 93% | 92% | 93% | 92% |
| Black or Black British | 5% | 3% | 3% | 1% | 3% | 1% |
| Asian or Asian British | 0% | 2% | 0% | 1% | 1% | 1% |
| Mixed race | 3% | 3% | 2% | 3% | 1% | 4% |
| Other | 5% | 2% | 1% | 3% | 3% | 2% |
| Accommodation status | ||||||
| Accommodation with MH care support | 3% | 1% | 0% | 0% | 2% | 0% |
| Accommodation with other support | 3% | 4% | 7% | 4% | 5% | 2% |
| Acute/long stay healthcare residential facility/hospital | 0% | 0% | 1% | 3% | 8% | 13% |
| Homeless | 7% | 9% | 13% | 10% | 8% | 7% |
| Mainstream housing | 88% | 86% | 80% | 79% | 76% | 76% |
| Bail/probation hostel | 0% | 0% | 0% | 2% | 0% | 0% |
| Other | 0% | 0% | 0% | 2% | 1% | 3% |
| Employment status | ||||||
| Employed | 38% | 20% | 29% | 24% | 26% | 20% |
| Unemployed | 26% | 38% | 40% | 48% | 40% | 54% |
| Homemaker | 1% | 2% | 1% | 4% | 3% | 1% |
| Student | 16% | 15% | 14% | 11% | 12% | 11% |
| Long-term sickness/disability benefit | 15% | 16% | 12% | 9% | 5% | 5% |
| Statutory sick pay | 0% | 3% | 0% | 5% | 9% | 3% |
| Retired | 0% | 0% | 0% | 0% | 0% | 1% |
| Other | 3% | 6% | 4% | 0% | 4% | 4% |
| Change in employment status during EIP | ||||||
| No reported change | 58 (84%) | 107 (91%) | 124 (100%) | 128 (88%) | 163 (97%) | 88 (86%) |
| Became employed | 0 (0%) | 4 (3%) | 0 (0%) | 13 (9%) | 2 (1%) | 5 (5%) |
| Left employment/became unemployed | 10 (14%) | 4 (3%) | 0 (0%) | 4 (3%) | 2 (1%) | 3 (3%) |
| Other | 1 (1%) | 3 (3%) | 0 (0%) | 0 (0%) | 1 (1%) | 6 (6%) |
| Referral source | ||||||
| Primary care | 75 (62%) | 256 (63%) | 283 (62%) | 143 (60%) | 172 (63%) | 139 (55%) |
| Community mental health service | 19 (16%) | 66 (16%) | 104 (23%) | 14 (6%) | 26 (10%) | 14 (6%) |
| Inpatient mental health service | 1 (1%) | 21 (5%) | 15 (3%) | 12 (5%) | 16 (6%) | 4 (2%) |
| A&E department | 11 (9%) | 20 (5%) | 21 (5%) | 5 (2%) | 13 (5%) | 23 (9%) |
| Physical healthcare service | 0 (0%) | 13 (3%) | 8 (2%) | 4 (2%) | 8 (3%) | 2 (1%) |
| Caring and social services | 0 (0%) | 0 (0%) | 5 (1%) | 10 (4%) | 5 (2%) | 11 (4%) |
| Education service | 0 (0%) | 6 (1%) | 4 (1%) | 12 (5%) | 7 (3%) | 8 (3%) |
| Police/prison/probation | 9 (7%) | 8 (2%) | 11 (2%) | 14 (6%) | 11 (4%) | 25 (10%) |
| Self-referral | 1 (1%) | 2 (0%) | 2 (0%) | 12 (5%) | 6 (2%) | 17 (7%) |
| Other | 5 (4%) | 16 (4%) | 4 (1%) | 11 (5%) | 8 (3%) | 9 (4%) |
| CTP | ||||||
| EIP | 22 (18%) | 107 (26%) | 120 (26%) | 33 (14%) | 24 (9%) | 27 (11%) |
| Community mental health service | 98 (80%) | 281 (69%) | 325 (71%) | 183 (78%) | 217 (81%) | 184 (73%) |
| Inpatient mental health service | 2 (2%) | 21 (5%) | 14 (3%) | 17 (7%) | 26 (10%) | 27 (11%) |
| Physical healthcare service | 0 (0%) | 1 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Police/prison/probation | 0 (0%) | 0 (0%) | 0 (0%) | 3 (1%) | 2 (1%) | 14 (6%) |
Data exclude EIP to EIP transfers.
A&E, accident and emergency department; CTP, central triage point; EIP, early intervention in psychosis; MH, mental health.
In both sites, the most common source of referral to EIP services was primary care, making up between 55% to 63% of referrals, followed by other mental health services (6%–23%) and then emergency departments (EDs, 2%–9%).
Quantitative results
Timeliness of access
Waiting times (shown in table 2) for EIP assessment from both EIP referral and CTPs (teams where referrals received) reduced significantly compared with baseline, from median 11 to 7 days and from 20 to 11 days, respectively (p<0.0001 for both) in the implementation site. Conversely, in the comparator site the median waiting time from EIP referral to assessment increased significantly from 7 to 12 days (p<0.0001) and was unchanged from central triage to assessment at 33 days (p=0.56). This suggests an improvement in assessment speed following referral to services in the implementation site.
Table 2.
Process outcomes for all individuals referred to EIP service
| Implementation site | Comparator site | |||||||||||
| Baseline | Year 1 | Year 2 | P value | P value | Baseline | Year 1 | Year 2 | P value | P value | |||
| (n=123) | (n=416) | (n=463) | Y1 vs baseline | Y2 vs baseline | (n=237) | (n=271) | (n=252) | Y1 vs baseline | Y2 vs baseline | |||
| Accepted onto EIP pathway | 69 (56%) | 118 (28%) | 124 (27%) | <0.0001 | <0.0001 | 145 (61%) | 168 (62%) | 102 (40%) | 0.89 | <0.0001 | ||
| Time from EIP referral to EIP assessment (in days) | 11.0 (6.0 to 20.5) | 6.0 (3.0 to 12.0) | 7.0 (4.0 to 14.0) | <0.0001 | <0.0001 | 7.0 (3.0 to 12.0) | 7.0 (4.0 to 12.8) | 12.0 (7.0 to 21.0) | 0.24 | <0.0001 | ||
| Time from CTP referral to EIP assessment (in days) | 20.0 (11.8 to 55.3) | 15.0 (6.0 to 40.0) | 11.0 (6.0 to 23.0) | 0.0053 | <0.0001 | 33.0 (11.0 to 142.5) | 24.0 (9.3 to 130.5) | 33.0 (13.0 to 98.0) | 0.45 | 0.96 | ||
| DNAs prior to assessment | ||||||||||||
| 0 | 113 (92%) | 378 (91%) | 434 (94%) | 0.37 | 211 (89%) | 247 (91%) | 232 (92%) | 0.59 | ||||
| 1 | 7 (6%) | 28 (7%) | 17 (4%) | 17 (7%) | 19 (7%) | 12 (5%) | ||||||
| 2 or more | 3 (2%) | 10 (2%) | 12 (3%) | 9 (4%) | 6 (2%) | 9 (4%) | ||||||
| Time to allocation and engagement by care coordinator (in weeks) | 4.0 (0.0 to 11.0) | 1.0 (0.0 to 5.0) | 0.0 (0.0 to 3.0) | 0.0033 | <0.0001 | 0.0 (0.0 to 7.3) | 0.0 (0.0 to 7.0) | 0.0 (0.0 to 14.8) | 0.054 | 0.48 | ||
| Time to MDT discussion (in weeks) | 6.2 (1.7 to 20.0) | 1.9 (1.0 to 4.6) | 1.9 (0.9 to 3.0) | <0.0001 | <0.0001 | 1.8 (0.7 to 3.0) | 1.7 (1.0 to 2.7) | 4.9 (1.8 to 28.0) | 0.74 | <0.0001 | ||
| Time to medical formulation (in weeks) | 4.7 (2.3 to 8.4) | 3.9 (1.9 to 8.4) | 3.3 (1.9 to 6.0) | 0.45 | 0.11 | 6.5 (2.3 to 10.3) | 6.7 (2.4 to 11.0) | 8.3 (3.8 to 11.9) | 0.99 | 0.14 | ||
| Time to CPA /care plan (in weeks) | 2.4 (0.0 to 6.9) | 2.7 (0.8 to 5.4) | 2.0 (0.4 to 5.8) | 0.62 | 0.87 | 2.0 (0.7 to 5.6) | 3.0 (1.0 to 14.5) | 13.0 (4.3 to 34.0) | 0.080 | <0.0001 | ||
| Time to risk assessment completion (in weeks) | 50.3 (2.6 to 91.1) | 6.4 (1.0 to 15.3) | 4.7 (1.4 to 8.1) | <0.0001 | <0.0001 | 5.3 (1.4 to 15.0) | 3.6 (1.0 to 15.1) | 4.6 (1.1 to 13.4) | 0.38 | 0.60 | ||
| Reason for non-acceptance to EIP | ||||||||||||
| Does not fulfil EIP criteria | 29 (71%) | 202 (79%) | 280 (85%) | 0.0010 | 18 (20%) | 20 (19%) | 28 (19%) | 0.76 | ||||
| Discharged on professional advice | 4 (10%) | 14 (5%) | 2 (1%) | 62 (67%) | 65 (63%) | 100 (66%) | ||||||
| DNA/did not engage/declined treatment | 6 (15%) | 27 (11%) | 35 (11%) | 5 (5%) | 8 (8%) | 13 (9%) | ||||||
| Moved out of area | 0 (0%) | 11 (4%) | 10 (3%) | 6 (7%) | 7 (7%) | 9 (6%) | ||||||
| Other | 2 (5%) | 3 (1%) | 4 (1%) | 1 (1%) | 4 (4%) | 1 (1%) | ||||||
| Reason for discharge from EIP after acceptance | ||||||||||||
| Care completed | 4 (15%) | 4 (9%) | 0 (0%) | 0.076 | 0 (0%) | 0 (0%) | 0 (0%) | 0.40 | ||||
| Does not fulfil EIP criteria | 8 (31%) | 22 (48%) | 22 (50%) | 7 (6%) | 6 (5%) | 4 (9%) | ||||||
| Discharged on professional advice | 0 (0%) | 1 (2%) | 3 (7%) | 80 (72%) | 72 (61%) | 25 (54%) | ||||||
| DNA/did not engage/declined treatment | 6 (23%) | 8 (17%) | 8 (18%) | 16 (14%) | 25 (21%) | 11 (24%) | ||||||
| Moved out of area | 5 (19%) | 11 (24%) | 9 (20%) | 7 (6%) | 12 (10%) | 5 (11%) | ||||||
| Other | 3 (12%) | 0 (0%) | 2 (5%) | 1 (1%) | 4 (3%) | 1 (2%) | ||||||
| Change in accommodation status during EIP | ||||||||||||
| No reported change | 63 (91%) | 118 (100%) | 124 (100%) | <0.0001 | 136 (94%) | 157 (93%) | 78 (76%) | <0.0001 | ||||
| Moved to mainstream housing | 0 (0%) | 0 (0%) | 0 (0%) | 2 (1%) | 3 (2%) | 10 (10%) | ||||||
| Moved from acute/long stay/ hospital to supported accommodation | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1%) | 3 (2%) | 2 (2%) | ||||||
| Moved to acute/long stay/ hospital | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1%) | 4 (4%) | ||||||
| Committed to bail/probation hostel/prison | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1%) | ||||||
| No longer homeless | 1 (1%) | 0 (0%) | 0 (0%) | 3 (2%) | 2 (1%) | 1 (1%) | ||||||
| Became homeless | 1 (1%) | 0 (0%) | 0 (0%) | 1 (1%) | 2 (1%) | 1 (1%) | ||||||
| Other | 3 (4%) | 0 (0%) | 0 (0%) | 2 (1%) | 0 (0%) | 5 (5%) | ||||||
Numbers represent either N (%) for categorical variables or median (IQR) for continuous variables. Excludes EIP to EIP transfers. P values for categorical comparisons from χ2 test or Fisher's exact test as appropriate. P values for continuous data from Mann-Whitney U tests.
CPA, Care Programme Approach; EIP, early intervention in psychosis; MDT, multidisciplinary team.
The pathway implementation site also saw significantly reduced waiting times for allocation to and engagement by care coordinator, MDT discussions, risk assessment completion and discharge of service users found unsuitable for the service on assessment (p<0.0001 for all). There was no statistically significant difference in the time to medical formulation or CPA development. In the comparator site, time to allocation and engagement by the care coordinator remained unchanged at median 0 days throughout the study. Although not significantly different from baseline in year 1, by year 2 time to MDT discussion and to risk assessment completion had both increased significantly (p<0.0001 for both).
The numbers of patients accepted onto the EIP case load were much higher than expected in the comparator site, but this reduced to nearer the expected levels during the course of the project. The implementation site started below but rose to just above expected levels.
Reasons for discharge from EIP services remained similar in the comparator site throughout the study. However, in the implementation site there was a significant change, seemingly led by an increase in the number of unsuitable referrals to the service, which increased from 55% to 81%. Non-acceptance was also broadly similar as it was agreed with sites that ‘did not meet EIP criteria’ and ‘discharged on professional advice’ effectively meant the same thing.
NICE-recommended interventions offered
Physical health assessments
Both sites of the study saw significant improvements in the proportion of individuals receiving assessments of their general physical health, substance use, alcohol use and weight, having their bloods taken and given ECGs, but at much higher levels in the implementation site as seen in table 3. Assessment of smoking status increased significantly at the implementation site (p=0.00033). Measurements of pulse and blood pressure assessments increased significantly in the comparator site (p=0.010, p=0.0036). Assessment of waist measurement increased significantly in the pathway implementation site (p=0.011), while decreasing significantly in the comparator site (p=0.0037). Finally, neither site significantly increased the number of individuals receiving a full eight-point NICE-recommended health check within 8 weeks of EIP assessment.
Table 3.
Physical health assessments and interventions
| Implementation site | Comparator site | |||||||
| Baseline | Year 1 | Year 2 | P value | Baseline | Year 1 | Year 2 | P value | |
| (n=69) | (n=118) | (n=124) | (n=145) | (n=168) | (n=102) | |||
| Physical health assessments received within 12 weeks | ||||||||
| Physical health (general) | 33 (48%) | 81 (69%) | 86 (69%) | 0.0038 | 38 (26%) | 40 (24%) | 44 (43%) | 0.0019 |
| Smoking | 23 (33%) | 72 (61%) | 76 (61%) | 0.00033 | 38 (26%) | 42 (25%) | 34 (33%) | 0.30 |
| Substance use | 35 (51%) | 93 (79%) | 98 (79%) | <0.0001 | 71 (49%) | 63 (38%) | 66 (65%) | <0.0001 |
| Alcohol | 35 (51%) | 89 (75%) | 102 (82%) | <0.0001 | 60 (41%) | 60 (36%) | 61 (60%) | 0.00045 |
| Weight | 17 (25%) | 46 (39%) | 60 (48%) | 0.0065 | 46 (32%) | 39 (23%) | 39 (38%) | 0.027 |
| Waist | 4 (6%) | 16 (14%) | 27 (22%) | 0.011 | 18 (12%) | 9 (5%) | 2 (2%) | 0.0037 |
| Pulse | 20 (29%) | 48 (41%) | 47 (38%) | 0.30 | 25 (17%) | 32 (19%) | 33 (32%) | 0.010 |
| Blood pressure | 22 (32%) | 50 (42%) | 55 (44%) | 0.25 | 32 (22%) | 38 (23%) | 40 (39%) | 0.0036 |
| Bloods taken | 18 (26%) | 58 (49%) | 50 (40%) | 0.010 | 15 (10%) | 25 (15%) | 36 (35%) | <0.0001 |
| ECG | 10 (14%) | 49 (42%) | 27 (22%) | <0.0001 | 17 (12%) | 10 (6%) | 30 (29%) | <0.0001 |
| NICE health check in 12 weeks | 2 (3%) | 9 (8%) | 11 (9%) | 0.30 | 1 (1%) | 1 (1%) | 1 (1%) | 0.94 |
| Interventions offered at any time | ||||||||
| CBT | 43 (62%) | 68 (58%) | 84 (68%) | 0.26 | 1 (1%) | 23 (14%) | 22 (22%) | <0.0001 |
| Family intervention | 36 (52%) | 64 (54%) | 80 (65%) | 0.17 | 7 (5%) | 7 (4%) | 10 (10%) | 0.13 |
| Carer support | 50 (72%) | 82 (69%) | 90 (73%) | 0.86 | 34 (23%) | 29 (17%) | 25 (25%) | 0.26 |
| Employment support | 41 (59%) | 47 (40%) | 57 (46%) | 0.043 | 37 (26%) | 47 (28%) | 18 (18%) | 0.15 |
| Interventions taken up within 6 months | ||||||||
| Engagement | 52 (75%) | 103 (87%) | 111 (90%) | 0.039 | 82 (57%) | 74 (44%) | 80 (79%) | <0.0001 |
| CBT for psychosis | 3 (4%) | 10 (8%) | 8 (6%) | 0.56 | 0 (0%) | 7 (4%) | 7 (7%) | 0.010 |
| Carer support | 24 (35%) | 63 (53%) | 84 (68%) | <0.0001 | 17 (12%) | 22 (13%) | 16 (16%) | 0.66 |
| Medication | 37 (54%) | 80 (68%) | 91 (73%) | 0.027 | 25 (17%) | 37 (22%) | 28 (28%) | 0.16 |
| Collaborative care planning | 22 (32%) | 85 (72%) | 86 (69%) | <0.0001 | 45 (31%) | 38 (23%) | 1 (1%) | <0.0001 |
| Physical health | 2 (3%) | 4 (3%) | 7 (6%) | 0.58 | 37 (26%) | 9 (5%) | 15 (15%) | <0.0001 |
| Vocational | 14 (20%) | 79 (67%) | 89 (72%) | <0.0001 | 29 (20%) | 37 (22%) | 39 (39%) | 0.0023 |
| Family work for psychosis | 2 (3%) | 11 (9%) | 8 (6%) | 0.25 | 2 (1%) | 6 (4%) | 1 (1%) | 0.26 |
| Any of these | 57 (83%) | 113 (96%) | 117 (94%) | 0.0071 | 83 (57%) | 74 (44%) | 82 (81%) | <0.0001 |
N (%) individuals accepted onto the EIP pathway at each site, who received listed physical health checks within 12 weeks, were offered interventions or took up interventions within 6 months of EIP referral. Excludes EIP to EIP transfers. P values from χ2 test or Fisher's exact test as appropriate.
CBT, cognitive–behavioural therapy; EIP, early intervention in psychosis; NICE, National Institute of Health and Care Excellence.
Other interventions
The proportion of individuals being offered cognitive–behavioural therapy (CBT) increased significantly in the comparator site from 1% to 22% (p<0.0001) and was matched with a significant increase in taking up CBT intervention from 0% to 7% (p=0.010). The implementation site did not see any significant change in either of these factors. However throughout the period, CBT for psychosis and family work for psychosis were much more likely to be offered (table 3).
Prevalence of individuals receiving any of the listed interventions increased in both the pathway (83% to 94%, p=0.0071) and comparator sites (57% to 81%, p<0.0001), as did engagement (75% to 90%, p=0.039% and 57% to 79%, p<0.0001 respectively) from baseline to year 2.
The implementation site saw increases in the proportion of participants receiving carer support (35% to 68%, p<0.0001) and medication (54% to 73%, p=0.027), although neither of these changed significantly in the comparator site. Receipt of collaborative care planning increased significantly in the implementation site (32% to 69%, p<0.0001), while the comparator site saw a decrease (31% to 1%, p<0.0001). Prevalence of physical health interventions also decreased in the comparator site (26% to 15%, p<0.0001) but did not change significantly in the implementation site, remaining low (3% to 6%, p=0.58). Receipt of vocational support increased significantly in both the implementation site (20% to 72%, p<0.0001) and the comparator site (20% to 39%, p=0.0023). However subsequently, after 6 months, there was a much higher take-up rate with over 80% in the implementation and over 70% in the comparator site.
Clinical outcomes
Acute care
There was a substantial contrast in the numbers of patients who had been admitted to hospital at the point of referral, much higher in the implementation site compared with comparator but reducing over time (table 4). Further admissions were low across both sites with neither site seeing a significant change in the prevalence of acute mental health admissions, in the time to being admitted or in the time to discharge. Similarly, the number of EIP participants subject to MHA section did not change significantly, although there was a tendency towards a decrease in the implementation site (36% to 33% to 27%, p=0.58). In both sites, the number of EIP service users attending ED or general hospital within a year was low (7%–10%) and there were no significant changes over time.
Table 4.
Acute care and clinical outcomes
| Implementation site | Comparator site | |||||||||
| Baseline | Year 1 | Year 2 | P value | P value | Baseline | Year 1 | Year 2 | P value | P value | |
| (n=69) | (n=118) | (n=124) | Y1 vs baseline | Y2 vs baseline | (n=145) | (n=168) | (n=102) | Y1 vs baseline | Y2 vs baseline | |
| Acute MH admission within 1 year of EIP referral | 27 (39%) | 47 (40%) | 36 (29%) | 0.16 | 16 (11%) | 21 (13%) | 19 (19%) | 0.20 | ||
| Time to acute admission (where applicable) (weeks) |
0.0 (0.0 to 10.0) | 1.0 (0.0 to 7.0) | 0.0 (0.0 to 3.5) | 0.88 | 0.11 | 15.0 (3.0 to 41.0) | 11.0 (2.0 to 41.0) | 13.5 (3.0 to 34.0) | 0.82 | 0.92 |
| Time to acute MH/inpatient screening (hours) | ||||||||||
| 0–4 | 21 (91%) | 1 (100%) | 14 (67%) | – | 11 (73%) | 11 (58%) | 8 (53%) | 0.49 | ||
| 4–6 | 0 (0%) | 0 (0%) | 6 (29%) | 3 (20%) | 4 (21%) | 3 (20%) | ||||
| 6–8 | 1 (4%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (11%) | 1 (7%) | ||||
| 8–10 | 1 (4%) | 0 (0%) | 1 (5%) | 1 (7%) | 2 (11%) | 3 (20%) | ||||
| Time from acute admission to discharge (where applicable weeks) | 4.5 (2.0 to 10.3) | 4.0 (2.0 to 6.8) | 3.0 (1.0 to 5.3) | 0.42 | 0.56 | 3.0 (2.0 to 13.5) | 3.0 (2.0 to 5.0) | 3.0 (2.3 to 3.8) | 0.56 | 0.95 |
| Number of subsequent acute admissions | ||||||||||
| None | 18 (64%) | 41 (85%) | 25 (71%) | 0.091 | 14 (67%) | 15 (65%) | 13 (62%) | 0.95 | ||
| 1 | 6 (21%) | 4 (8%) | 9 (26%) | 5 (24%) | 2 (9%) | 8 (38%) | ||||
| More than 1 | 4 (14%) | 3 (6%) | 1 (3%) | 2 (10%) | 6 (26%) | 0 (0%) | ||||
| MHA section within 1 year of EIP referral | 25 (36%) | 39 (33%) | 34 (27%) | 0.58 | 16 (11%) | 21 (13%) | 18 (18%) | 0.18 | ||
| Contact acute MH services (post EIP) | 32 (46%) | 41 (35%) | 37 (30%) | <0.0001 | 25 (17%) | 30 (18%) | 22 (22%) | <0.0001 | ||
| Crisis plan completed | 35 (51%) | 59 (50%) | 44 (35%) | 0.032 | 71 (49%) | 69 (41%) | 68 (67%) | 0.00023 | ||
| Time to crisis plan completed (weeks) | 50.0 (15.0 to 79.0) | 22.5 (10.0 to 37.8) | 12.5 (6.0 to 22.8) | 0.0010 | <0.0001 | 8.0 (1.0 to 23.0) | 11.0 (1.0 to 39.0) | 12.0 (2.0 to 34.3) | 0.36 | 0.10 |
| A&E attendance within 1 year of EIP referral | 7 (10%) | 10 (8%) | 11 (9%) | 0.91 | 11 (8%) | 12 (7%) | 10 (10%) | 0.72 | ||
| Time to A&E attendance (weeks) | 21.0 (2.5 to 68.3) | 8.5 (0.0 to 17.0) | 13.0 (8.0 to 43.0) | 0.15 | 0.88 | 30.0 (25.0 to 41.0) | 44.0 (11.0 to 76.0) | 14.5 (7.3 to 31.5) | 0.87 | 0.11 |
| Reason for A&E attendance | ||||||||||
| Deterioration in mental state | 7 (41%) | 7 (50%) | 5 (42%) | – | 2 (15%) | 4 (24%) | 2 (20%) | – | ||
| Self harm/suicidal ideation/suicide attempt/overdose | 6 (35%) | 5 (36%) | 4 (33%) | 10 (77%) | 6 (35%) | 4 (40%) | ||||
| Alcohol/substance abuse | 1 (6%) | 1 (7%) | 2 (17%) | 0 (0%) | 1 (6%) | 0 (0%) | ||||
| Medication side effects | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (6%) | 1 (10%) | ||||
| Physical injury/illness (not apparently psychosis related) | 3 (18%) | 1 (7%) | 1 (8%) | 1 (8%) | 5 (29%) | 3 (30%) | ||||
| General hospital admission within 1 year of EIP referral | 1 (1%) | 4 (3%) | 3 (2%) | – | 2 (1%) | 0 (0%) | 4 (4%) | – | ||
| Contact with criminal justice system while in EIP pathway | 15 (22%) | 34 (29%) | 4 (3%) | <0.0001 | 20 (14%) | 20 (12%) | 21 (21%) | <0.0001 | ||
| Criminal conviction within 1 year of EIP referral | 1 (1%) | 0 (0%) | 0 (0%) | – | 4 (3%) | 4 (2%) | 1 (1%) | – | ||
| Deaths within 1 year of EIP referral | 0 (0%) | 0 (0%) | 0 (0%) | – | 0 (0%) | 0 (0%) | 1 (1%) | – | ||
Proportion of individuals accepted onto the EIP pathway at each trust experiencing acute care outcomes (n (%)) within 1 year of trust referral, and time to reach those outcomes, where applicable (median (IQR)). Excludes EIP to EIP transfers. P values for categorical comparisons from χ2 test or Fisher's exact test as appropriate. P values for continuous data from Mann-Whitney U tests.
EIP, early intervention in psychosis; MH, mental health; MHA, Mental Health Act.
Crisis planning
In the implementation site, the proportion of participants having a crisis plan completed reduced significantly (51% to 35%, p=0.032), occurring alongside a decrease in the time to crisis plan completion (50.0 to 12.5 weeks, p<0.0001) as seen in table 4. Conversely, in the comparator site the proportion of participants having a crisis plan completed increased significantly (49% to 67%, p=0.00023).
Clinical and social outcomes
These were assessed by extracting the data routinely collected using the HoNOS as seen in table 5. At the implementation site, there were significant reductions over the 2-year period in ‘problems with relationships’ (p=0.013) and ‘problems with occupation and activities’ (p=0.037). At the comparator site, there were significant reductions in ‘problems with activities of daily living’ (p=0.04). The comparator site however had substantial amounts of missing data. There was no significant difference in reductions in ‘problems with delusions and hallucinations’ between sites.
Table 5.
Clinical outcomes (HoNOS)
| Implementation site | Comparator site | |||||||||
| Baseline | Year 1 | Year 2 | P value | P value | Baseline | Year 1 | Year 2 | P value | P value | |
| (n=52) | (n=77) | (n=53) | Y1 vs baseline | Y2 vs baseline | (n=28) | (n=16) | (n=11) | Y1 vs baseline | Y2 vs baseline | |
| Change in HoNOS scores (from referral to 1 year) | ||||||||||
| 1. Overactive, aggressive, disruptive or agitated behaviour | −0.56 (1.73) | −0.43 (1.72) | −0.69 (1.45) | 0.59 | 0.78 | −0.43 (1.55) | −1.06 (1.65) | −0.09 (1.14) | * | * |
| 2. Non-accidental self injury | −0.50 (1.38) | −0.22 (1.26) | −0.22 (1.15) | 0.18 | 0.21 | −0.25 (0.84) | −0.06 (1.29) | −0.36 (1.43) | * | * |
| 3. Problem drinking or drug taking | −0.40 (1.48) | −0.15 (1.87) | 0.04 (1.71) | 0.30 | 0.12 | 0.14 (1.04) | −0.31 (1.20) | −0.10 (1.52) | * | * |
| 4. Cognitive problems | −0.27 (1.34) | −0.15 (1.32) | −0.06 (1.32) | 0.48 | 0.33 | −0.29 (1.18) | −0.38 (0.96) | −0.50 (1.51) | * | * |
| 5. Physical illness or disability problems | −0.23 (1.10) | 0.03 (1.35) | 0.02 (1.08) | 0.19 | 0.17 | 0.11 (0.50) | −0.38 (1.02) | 0.45 (1.44) | * | * |
| 6. Problems associated with hallucinations and delusions | −0.56 (1.62) | −0.71 (1.70) | −0.11 (1.51) | 0.74 | 0.14 | −0.86 (1.46) | −1.81 (1.42) | −0.91 (1.76) | * | * |
| 7. Problems with depressed mood | −0.50 (1.59) | −0.19 (1.49) | −0.55 (1.12) | 0.24 | 0.94 | −0.46 (1.29) | −0.88 (1.41) | −0.55 (1.21) | * | * |
| 8. Other mental and behavioural problems | −0.45 (1.53) | −0.73 (1.81) | −0.27 (1.49) | 0.58 | 0.68 | −0.61 (1.26) | −0.75 (1.98) | −0.36 (1.69) | * | * |
| 9. Problems with relationships | −0.83 (1.32) | −0.41 (1.51) | −0.20 (1.25) | 0.07 | 0.013 | −0.21 (1.26) | −1.00 (1.41) | −0.10 (0.57) | * | * |
| 10. Problems with activities of daily living | −0.33 (1.57) | −0.32 (1.55) | −0.46 (1.47) | 0.85 | 0.68 | −0.64 (1.16) | −1.00 (1.55) | 0.18 (0.75) | * | * |
| 11. Problems with living conditions | −0.20 (1.51) | −0.33 (1.44) | 0.08 (1.21) | 0.69 | 0.28 | −0.36 (1.31) | −0.69 (1.20) | 0.45 (1.13) | * | * |
| 12. Problems with occupation and activities | −0.33 (1.64) | −0.19 (1.47) | 0.30 (1.45) | 0.54 | 0.037 | −0.25 (1.58) | −1.06 (1.57) | −0.09 (1.45) | * | * |
Mean (SD) change in HoNOS scores from referral to 1 year at each trust for patients accepted onto EIP pathway. Excludes EIP to EIP transfers. P values from paired t-tests.
*P values not calculated due to amount of missing data.
EIP, early intervention in psychosis; HoNOS, Health of the Nation Outcome Scales.
Criminal justice system contact
The number of participants having contact with the criminal justice system decreased significantly in the implementation site (22% to 3%, p<0.0001), while increasing significantly in the comparator site (14% to 21%, p<0.0001). Criminal convictions were rare in both sites (table 4).
Discharge and death
Discharge from services within a year of patients accepted by EIP teams (table 2) was relatively low, although disengagement remained a concern. It reduced in the implementation site (18% to 11%) and remained stable in comparator (10% to 12%). There was one death of a participant within a year of EIP assessment in the comparator site, year 2 cohort (table 4).
Qualitative results
Staff and patient interviews and focus groups
Across the 2 years, 64 staff in the implementation site took part in focus groups and reported that the psychosis pathway appeared to be beneficial, well embedded and a positive change with good team working within the teams and with other services. However, they found workload to be high and had some difficulties getting the right staff skills mix in teams to deliver all the needed interventions. They also noted that often interventions were offered but were not always completed due to patient’s ability to engage with them. Additionally, they worried about future changes being implemented in addition to their current workload. They felt that by year 2 they were more able to adapt the pathway to individuals’ needs which they saw as important rather than a prescriptive measure.
Patients (14 participants) in the implementation site reported that they were generally satisfied with being seen quickly and developed good relationships with the staff members. They found appointments helpful and felt they gained useful skills. However, they also reported that at times there was inconsistencies in the staff they saw and out of hours services could be improved. Carers views (7 participants) in the implementation site appeared to improve from year 1 to year 2 with more positive reports about the team and services than at year 1, however at both time points the sample was small.
Results from staff questionnaires
In total 1680 questionnaires were completed by staff members in the implementation and comparator site across the three time points. There was no notable change in staff experience across the time points or between the sites (online supplementary table 1). All staff members with adult mental health services were eligible to complete this questionnaire to capture the experience of staff referring into services and caring for service users with psychosis in services such as hospital settings.
bmjopen-2019-033711supp001.pdf (90KB, pdf)
Discussion
This comparison study provides evidence that the introduction of an integrated psychosis care pathway led to improvements in access to EIP and implementation of quality standards, especially for physical healthcare in comparison with a site which did not implement the pathway. In terms of acceptability and feasibility, staff, service user and carer attitudes to TRIumPH were found to be generally positive. However, there were pre-existing differences during the baseline period between the sites, which influenced the comparison as seen by access and waiting times, and level of interventions offered. Prior to the project, the implementation site had dismantled three out of four EIP teams and integrated them into community mental health teams, in contrast to the comparator site which had maintained specialist teams. At the beginning of the project, the implementation site reintroduced the four EIP teams. There was a marked difference in referrals in each site with movement in both sites towards predicted levels of patients accepted by EIP teams. This reflects the variations in service commissioning and provision landscape in the UK which can be geographically determined and can potentially impact on outcomes. There are other factors like staff skillset, recruitment and data quality among others. Due to the pragmatic nature of the study, it was not designed to explore these differences and their potential impact.
Time to assessment improved in the implementation site and remained within the AWTS in the comparator site. From a patient and carer perspective, a reduction in waiting times and DUP even of a few days, especially when acutely unwell, could be meaningful, for example the potential impact that being unwell could cause on relationships and employment. Referral from the CTP was relatively high especially in the comparator site, as was found by Birchwood and colleagues20 and this remains an important area for attention.
Compliance with quality standards increased substantially in the implementation site but was more variable and reached lower levels in the comparator site. This was especially noticeable for physical health standards, although the full set of NICE recommendations was only met in under 10% patients within 3 months of acceptance. In the implementation site, offering of CBT for psychosis was relatively high throughout, although uptake within 6 months was low. However, by 2 years, this was considerably higher. There was an increase in offering of CBT and family work in the comparator site from a very low baseline, attributed to a lack of fully trained therapists. This seems an area where implementation of the quality standards through a pathway process could be especially effective. Family intervention, carer and employment support were all offered to a greater extent in implementation site and uptake increased over the period. The findings also compare favourably with those of the National Clinical Audit of Psychosis.21
The changes in teams were reflected in the results as numbers of patients accepted onto case load were much higher than expected in the comparator site but reduced to nearer expected levels during the project. Referrals increased substantially in implementation site but then plateaued after introduction of the pathway.
The introduction of the AWTS target brought increased funding for EIP nationally. In the implementation site the local service commissioners remained well engaged with the pathway implementation and resulting outcomes and this enabled positive contract discussions for future investment. A formal cost-effectiveness analysis was not conducted due to limitations in data availability but the reduction in patients admitted to inpatient wards and the subsequent reduction in relapses to hospital suggest that the implementation of the pathway could be expected to have had a positive impact on cost in the implementation site.
However, not all outcomes for the intervention site were positive, for example the decrease in the recording of crisis plans, paralleled by the significant increase in the comparator site are worth to be note.
Study limitations
This is an observational prospective study based on manual audit of patients’ medical records. Therefore, causality cannot be assumed. We took steps to maintain data consistency by having one dedicated member of staff involved in the data audit throughout, and by performing post hoc data checks for consistency and outliers. However, data accuracy is naturally limited by the quality of mental health care providers’ original record keeping. This was additionally limited by the amount of analyses performed on the data. Furthermore, missing data were common, for example only 237 (33%) of participants had a HoNOS score recorded at both referral and 1 year later. The HoNOS data were lower in the comparator site which meant it was not meaningful to test for changes among cohorts at the comparator sites due to the fact that 90% had missing data.
Conclusion
This comparison of the implementation of a quality standard-based psychosis pathway with a comparator site which followed established guidelines for EIP teams suggests that the former was more effective at improving the level of evidence-based practice offered to patients and their carers. Integrated care pathways can offer a platform to inform gaps in services, implement good clinical practice and measure the impact.
Supplementary Material
Acknowledgments
The authors would like to thank everyone who have been involved at any stage of this study.
Footnotes
Twitter: @shanaya_rathod
Contributors: SR and DK are grant holders and contributed to the concept and design of the study. SR is the CI and led the development of the study protocol and study documentation and made a significant contribution to the manuscript. KT provided statistical expertise throughout the protocol development, data collection and analysis. CA provided PPI expertise throughout the protocol development and study delivery. AG supported the implementation of the TRIumPH development and delivery. EG, PP and TR supported the delivery of the study at their respective sites. All authors contributed to elaboration and refinement of the study protocol and approved the final manuscript.
Funding: This project has been funded by the NHS England (Regional Innovation Fund programme); Small grant from the Royal College of Psychiatrists General Adult Psychiatry Faculty.
Competing interests: The production of the pathway has been supported by the Wessex Academic Health Sciences Network (AHSN) and evaluation has been supported by the Wessex Clinical Research Network (CRN). The views and opinions expressed herein are those of the authors and do not necessarily reflect those of funders, NIHR, NHS or the RCPsych, AHSN or CRN. The study is sponsored by Southern Health NHS Foundation Trust.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Author note: Study Status: The study is complete.
References
- 1.World Health Organisation The world health report 2001. mental health: new understanding. Geneva, 2005. [Google Scholar]
- 2.Rössler W, Salize HJ, van Os J, et al. . Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol 2005;15:399–409. 10.1016/j.euroneuro.2005.04.009 [DOI] [PubMed] [Google Scholar]
- 3.Chang C-K, Hayes RD, Perera G, et al. . Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One 2011;6:e19590. 10.1371/journal.pone.0019590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drake RJ, Haley CJ, Akhtar S, et al. . Causes and consequences of duration of untreated psychosis in schizophrenia. Br J Psychiatry 2000;177:511–5. 10.1192/bjp.177.6.511 [DOI] [PubMed] [Google Scholar]
- 5.McGlashan TH. Duration of untreated psychosis in first-episode schizophrenia: marker or determinant of course? Biol Psychiatry 1999;46:899–907. 10.1016/S0006-3223(99)00084-0 [DOI] [PubMed] [Google Scholar]
- 6.Marshall M, Lewis S, Lockwood A, et al. . Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry 2005;62:975–83. 10.1001/archpsyc.62.9.975 [DOI] [PubMed] [Google Scholar]
- 7.Penttilä M, Jääskeläinen E, Hirvonen N, et al. . Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry 2014;205:88–94. 10.1192/bjp.bp.113.127753 [DOI] [PubMed] [Google Scholar]
- 8.Department of Health No health without mental health. UK: Department of Health, 2011. [Google Scholar]
- 9.England NHS Guidance to support the introduction of access and waiting time standards for mental health services in 2015/16. London: NHS England, 2015. [Google Scholar]
- 10.NICE Psychosis and schizophrenia in adults. Quality standard [QS80], 2015. Available: https://www.nice.org.uk/guidance/qs80 [Accessed 31 May 2019].
- 11.England NHS Mental health Task force. five year forward view. London: NHS England, 2016. [Google Scholar]
- 12.Campbell H, Hotchkiss R, Bradshaw N, et al. . Integrated care pathways. BMJ 1998;316:133–7. 10.1136/bmj.316.7125.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Excellence. NIfHaSC Stroke and transient ischaemic attack, 2019. Available: https://www.nice.org.uk/guidance/conditions-and-diseases/cardiovascular-conditions/stroke-and-transient-ischaemic-attack
- 14.Rathod S, Griffiths A, Kingdon D, et al. . Pathways to recovery: a case for adoption of systematic pathways in psychosis. London: Jointly produced by Imperial College Health Partners and Wessex Academic Health Science Network supported by the Royal College of Psychiatrists and Rethink Mental Illness, 2015. [Google Scholar]
- 15.Rathod S, Garner C, Griffiths A, et al. . Protocol for a multicentre study to assess feasibility, acceptability, effectiveness and direct costs of triumph (treatment and recovery in psychosis): integrated care pathway for psychosis. BMJ Open 2016;6:e012751. 10.1136/bmjopen-2016-012751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Network WAHS TRIumPH - Treatment and Recovery in Psychosis, 2015. Available: https://wessexahsn.org.uk/projects/59/triumph-treatment-and-recovery-in-psychosis
- 17.Preti A, Pisano A, Cascio MT, et al. . Validation of the health of the nation outcome scales as a routine measure of outcome in early intervention programmes. Early Interv Psychiatry 2012;6:423–31. 10.1111/j.1751-7893.2011.00329.x [DOI] [PubMed] [Google Scholar]
- 18.Bergman MM. Straw man of the Qualitative-Quantitative Divide : Advances in mixed methods research. London: Sage Publications, 2008. [Google Scholar]
- 19.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative research in psychology. 2006;3(2):77-101. Birchwood M, Connor C, Lester H, et al. Reducing duration of untreated psychosis: care pathways to early intervention in psychosis services. Br J Psychiatry 2013;203:58–64. [DOI] [PubMed] [Google Scholar]
- 20.Birchwood M, Connor C, Lester H, et al. . Reducing duration of untreated psychosis: care pathways to early intervention in psychosis services. Br J Psychiatry 2013;203:58–64. 10.1192/bjp.bp.112.125500 [DOI] [PubMed] [Google Scholar]
- 21.Royal College of Psychiatrists Report of the National audit of schizophrenia (nas) 2019. London: Royal College of Psychiatrists Healthcare Quality Improvement Partnership, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-033711supp001.pdf (90KB, pdf)


