Abstract
Background
Growth hormone (GH) treatment is currently recommended in Prader-Willi syndrome (PWS) patients.
Objectives
To evaluate the impact (efficacy and safety) of the use of recombinant human GH (rhGH) as a treatment for PWS.
Method
We performed a systematic review and, where possible, meta-analysis for the following outcomes: growth, body mass index, body composition, cognitive function, quality of life, head circumference, motor development/strength, behaviour and adverse effects. We included all PWS patients, with all types of genetic defects and with or without GH deficiency, who participated in rhGH studies performed in infancy, childhood and adolescence, that were either randomised controlled trials (RCTs) (double-blinded or not) or non-randomised controlled trials (NRCTs) (cohort and before and after studies). The databases used were MEDLINE, Embase and Cochrane Central.
Results
In 16 RCTs and 20 NRCTs selected, the treated group had an improvement in height (1.67 SD scores (SDS); 1.54 to 1.81); body mass index z-scores (−0.67 SDS; −0.87 to −0.47) and fat mass proportion (−6.5% SDS; −8.46 to −4.54) compared with the control group. Data about cognition could not be aggregated.
Conclusion
Based on high quality evidence, rhGH treatment favoured an improvement of stature, body composition and body mass index, modifying the disease’s natural history; rhGH treatment may also be implicated in improved cognition and motor development in PWS patients at a young age.
Ethics and dissemination
The current review was approved by the ethical committee of our institution. The results will be disseminated through conference presentations and publications in peer-reviewed journals.
PROSPERO registration number
CRD42019140295
Keywords: Prader-Willi Syndrome, meta-analysis, growth hormone, endocrinology, growth, syndrome, obesity, genetics
What is known about the subject?
Wide systematic search considering the effect of growth hormone treatment in Prader-Willi syndrome (PWS), including randomised controlled trials and observational studies.
PWS patients treated by growth hormone had an improvement of stature, growth velocity and head circumference.
Growth hormone treatment impacts in body composition decreasing the fat mass and increasing the lean mass. Body mass index could be decreased in short-term follow-up and could be controlled in the long-term treatment in these patients.
What this study adds.
The impact of recombinant human growth hormone in cognition and motor development was not possible to be aggregate but show positive effects in treated patients, especially at a young age. No effect was found regarding behaviour.
The number of reported adverse events indicated few complications during long-term follow-up in studies.
Introduction
Prader-Willi syndrome (PWS) is a rare genetic disorder resulting from the loss of imprinted gene expression within the paternal chromosome 15q11-q13. It has a prevalence rate of 1/10 000 to 30 000 and is characterised by endocrine abnormalities due to hypothalamic-pituitary insufficiency and complex physical, behavioural and intellectual impairment. PWS is the main genetic cause of severe obesity in children. An early team approach to patient management allows improved quality of care and provides these individuals with a better quality of life.1
During early childhood, delayed motor and language development are observed; average milestones are achieved at approximately double the expected age. Intellectual and learning disabilities are variable and generally evident by the time the child reaches school age. Children with PWS can also develop psychiatric disorders throughout their lives.2
Growth hormone (GH) deficiency can occur in 40% to 100% of PWS patients, depending on GH stimulated test.3 The Pfizer International Growth Study (KIGS), with a cohort of 424 children with PWS, showed a prevalence for growth hormone deficiency of 74%.4 In the absence of GH replacement, patients with PWS usually present with short stature from the second decade of life, but it may be noticed earlier in childhood. It has been shown that insulin-like growth factor 1 and insulin-like growth factor binding protein 3 serum levels are low in patients with PWS.4 5 The association of GH deficiency, severe obesity and high fat mass indexes served as the foundation for the first studies to introduce the treatment with somatropin/recombinant human GH (rhGH) in these patients. Several studies trying to understand the real impact of the treatment with rhGH in PWS have since emerged.5–9
The use of rhGH is currently recommended in PWS patients with and without GH deficiency to improve short stature and metabolism;8–10 its use may also have beneficial effects on reducing weight gain and possibly on appetite regulation.9 10 GH acts as an anabolic agent that increases lean body mass and reduces fat mass.7 11 Once the natural history of PWS and its association with the progressive increase of fat mass with age was established, the positive effect of rhGH on body composition motivated its use in PWS patients as well as its approval by the US Food and Drug Administration since 2000.8 12
Another very important aspect of the use of rhGH therapy in PWS patients concerns the improvement in cognitive function, such as verbal intelligent quotients (IQs), adaptive communication, cognition abilities and language.13–15 Moreover, rhGH therapy may improve motor development, since hypotonia is a major problem in infants with PWS, may improve behaviours, since there is a high incidence of psychiatric problems, and may result in a better quality of life.15–18 In addition, some concerns about the increased risk of death in these patients have emerged, especially regarding an increased incidence of sleep apnoea.19–22
The purpose of this systematic review is to provide a concise summary of the current knowledge regarding the use of rhGH treatment in patients with PWS, including recommendations, outcomes and implications for future research and clinical practice.
Objective
To evaluate the impact (efficacy and safety) of the use of rhGH as a treatment for PWS. We performed a systematic review followed where possible by meta-analysis for the following outcomes:
Primary outcomes: growth, body mass index, body composition, cognitive function.
Secondary outcomes: quality of life, head circumference, motor development/muscle strength, behaviour and adverse effects.
Methods
The systematic review and meta-analysis were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (online supplementary file 1) and it was registered with PROSPERO (International Prospective Register of Systematic Reviews). We included all PWS patients, with all types of genetic defects, with or without GH deficiency, who participated in GH studies performed in infancy, childhood and adolescence, that were either randomised controlled trials (RCTs)(double-blinded or not) or non-randomised controlled trials (NRCTs) (cohort and before and after studies). Narrative reviews, systematic review protocols, case reports, abstracts, data from unpublished research or incomplete articles were excluded. Studies with less than 1 year of rhGH use were also excluded.
bmjpo-2019-000630supp001.pdf (298.9KB, pdf)
The rhGH group was compared with a matching placebo group or patients that received no drugs during the 1 year follow-up in RCTs. For NRCTs we evaluated patients at the start and at the end of the treatment. All studies that had patients who received a subcutaneous application of rhGH at any dosage were included.
We analysed the following outcome measures:
Growth: Z-stature SD scores (SDS) according to WHO growth charts, Centers for Disease Control and Prevention (CDC) growth charts or by PWS curve; growth velocity: centimetres/year or growth velocity SDS.23–25
Body mass index (m2/kg): BMI-SDS according to WHO growth charts and CDC growth charts.23–25
Body composition (lean mass and fat mass): measure by dual-energy X-ray absorptiometry (DXA-type Lunar Prodigy, GE Healthcare-Chalfont St Giles, UK, or Madison, Wisconsin). We evaluated the proportion of total body/trunk fat mass (kilograms) or SDS of lean mass.
Cognitive function: all types of validated questionnaires.
Quality of life: evaluated by different validated instruments.
Behaviour: evaluated by different validated instruments.
Head circumference: Z-score according to CDC growth charts and Netherlands charts.26
Motor development/muscle strength: evaluated by different types of measures.
Adverse effects: sleep abnormalities, initial headache, peripheral oedema, scoliosis, diabetes and mortality.
Electronic searches
The search for evidence on the efficacy of somatropin (rhGH) on PWS was performed through a systematic review based on the PRISMA checklist. There were no restrictions on language or period. The databases used were MEDLINE (via PubMed), Embase and Cochrane Central with the following search strategies.
MEDLINE (via PubMed)
(Prader-Willi syndrome OR Prader-Labhart-Willi syndrome OR Labhart Willi Prader Fanconi syndrome OR Royer syndrome) AND (human growth hormone OR hGH OR somatotropin OR somatropin OR Serostim OR Zomacton OR Cryo-Tropin OR recombinant human growth hormone AND (mammalian) OR r-hGH-M OR r-hGH AND (m) OR Humatrope OR Umatrope OR Maxomat OR Norditropin OR Nutropin OR Omnitrope OR Saizen OR Genotropin OR Genotonorm)
Embase
(Prader-Willi Syndrome OR Prader-Labhart-Willi Syndrome OR Labhart Willi Prader Fanconi Syndrome OR Royer Syndrome) AND (human growth hormone OR hGH OR somatotropin OR somatropin OR Serostim OR Zomacton OR Cryo-Tropin OR recombinant human growth hormone AND (mammalian) OR r-hGH-M OR r-hGH AND (m) OR Humatrope OR Umatrope OR Maxomat OR Norditropin OR Nutropin OR Omnitrope OR Saizen OR Genotropin OR Genotonorm)
Cochrane
(Prader-Willi syndrome OR Prader-Labhart-Willi syndrome OR Labhart Willi Prader Fanconi syndrome OR Royer syndrome) AND (human growth hormone)
All PWS articles were evaluated independently by two reviewers. Following the eligibility criteria, studies were evaluated first by title and then by abstract. The full-text of selected articles was assessed for data extraction and bias evaluation. A characterisation matrix was constructed with the following variables: author, publication year, study design, country, age, period, dose and outcomes. When the data were not clear in the paper, we contacted the authors by email. Grey literature (thesis, book chapters) and references of selected articles were reviewed.
Selection of studies and data extraction
Identification, screening and eligibility assessments were performed independently in an unblinded, standardised manner by two reviewers. Disagreements between reviewers were discussed with a third researcher. Extraction of dichotomous (adverse effects) and continuous variables (all other outcomes) was independently performed.
Assessment of risk of bias in the included studies
Risk of bias was evaluated separately by two reviewers. The Cochrane Collaboration Risk of Bias tool was used for randomised trials, the New Castle Ottawa Scale was used for cohort studies and the Joanna Briggs Institute Instrument for used for before and after studies and for cohort studies when only one arm of the cohort was analysed.27 28
Measures of treatment effect and units of analyses
We performed separated meta-analyses of RCTs and NRCTs. Associations were demonstrated in relative and absolute risks, difference in means, SD, SEs and 95% CIs. Different follow-up lengths were standardised by using patient-years of follow-up. When different measures or instruments were used in the studies, SEs were used to estimate outcomes. P values lower p = 0.05 were considered statistically significant to evaluate treatment effect. Studies that did not report data in terms of means and their respective SD were recalculated or not included in the analysis. Studies that mentioned medians, 25th and 75th percentiles and CIs were included after transforming these statistics into SD by Hozo et al method.29 When the data were not clear in the paper or were missing, we contacted the authors by email.
Subjects were evaluated in two subgroups: infants (under 3.5 years old) and children and adolescents. We selected this younger group to look for differences in the early start of rhGH and the cut-off was based in the majority of articles found.
Assessment of heterogeneity and reporting bias
We measured the inconsistency (the proportion of total variation across studies due to heterogeneity) of effects across interventions using the I2. To obtain adequate CIs, we used a random-effects model if I2> 50% and a fixed-effect model if I2 ≤ 50%.
The software used was Cochrane Review Manager (V.5.3; The Nordic Cochrane Centre).30 The possibility of publication bias was assessed by evaluating a funnel plot (Egger test) for asymmetry. We used GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the data quality for each outcome and to draw conclusions about the quality of the evidence within the text of the review.31 32
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Results
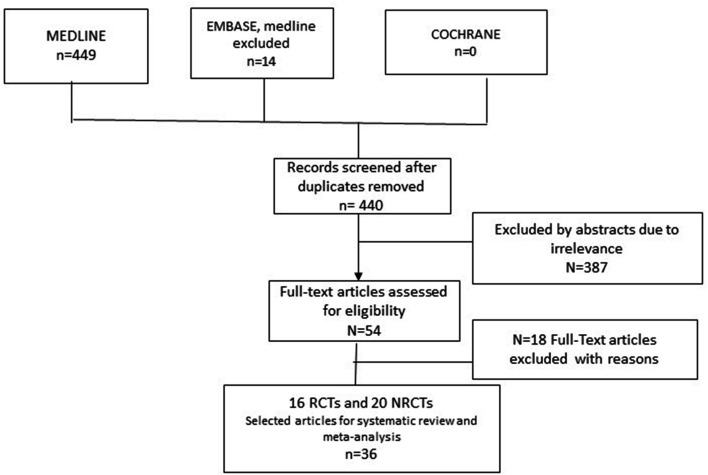
The electronic search yielded 463 titles from the databases until September 2019, and after text selection, this review included 16 completed RCTs and 20 NRCTs (figure 1). The excluded studies after full-text analysis (n=18) are presented in a separate table (see online supplementary file 2).
Figure 1.
PreferredReporting Items for Systematic Reviews and Meta-Analyses flow chart detailing selection of studies included in the meta-analysis. NRCTs; non-RCTs; RCTs, randomised controlled trials.
Randomised control studies
We performed the meta-analysis for the evaluation of growth hormone treatment versus no treatment in 9 of the 16 included RCT (table 1). No study used placebo due to ethical issues. The variables analysed were height z-scores (ZE), growth velocity (cm), BMI z-scores (Z-BMI), proportion of fat mass (%fat), lean mass z-scores (Z and kg) and head circumference z-scores (Z).
Table 1.
Characteristics of the randomised controlled trials studies that evaluated the use of growth hormone in patients with Prader-Willi syndrome
| Author/year | Age | N rhGH/control | Dose of rhGH | Period (years) | Country | Outcome |
| Bakker NE et al 45 | 6 months to 14 years | 12/16 | 1 mg/m2/day | 2 | Netherlands | Z-stature and body composition (%fat mass and LBM-SDS). |
| Bakker NE et al 18 | 6–14 years | 11/8 | 1 mg/m2/day | 2 | Netherlands | Quality of life (Dutch generic questionnaire-DUX25 and PWS-Dutch specific questionnaire-DUXPW questionnaires) |
| de Lind van Wijngaarden RFA et al 41 | 4, 9±3.0 years (<3 years and >3 years) | 29/21 | 1 mg/m2/day | 1;2 | Netherlands | Z-stature, BMI-SDS, body composition (%fat) |
| Böhm B et al 33 | 3–11 years | 19 | 0033 mg/kg/day | 2 | Sweden | Behaviour (specific test for the study) and cognition (Raven's Standard Progressive Matrices test, Arthur's adaptation of Leiter's Performance Scale; verbal comprehension test (SPIQ test), Terman’s Scale of Intelligence, Bender Gestalt test, Harris Draw-a-Man) |
| Lo ST et al 34 | 3, 5–14 years | 24/18 | 1 mg/m2/day | 1;2 | Netherlands | Behaviour (Developmental Behaviour Checklist of Children with intellectual disability and Children Social Behaviour Questionnaire) |
| Lo ST et al 36 | 3, 5–14 years | 41/34 | 1 mg/m2/day | 1;2 | Netherlands | VABS-II, cognitive function: Bayley Scales of Infants II- NL (BSID II), Weschsler Preschool and Primary Scale of Inteligence-Revised Dutch version |
| Reus L et al 37 | 12.9±7.1 months | 10/12 | 1 mg/m2/day | 2 | Netherlands | Muscular thickness with ultrasound, muscle strength (Infant Muscle Strength metre) and motor performance (Gross Motor Function Measure) |
| Reus L et al 35 | 12.9±7.1 months | 10/12 | 1 mg/m2/day | 2 | Netherlands | Cognition (BSID-II) and motor function (Gross Motor Function) |
| Siemensma EPC et al 14 | 3, 5–14 (mean 7,4 years) | 29/21 | 1 mg/m2/day | 2 | Netherlands | WISC-R (vocabulary, similarities, block design and picture arrangement) and Wechsler Preschool and Primary Scale of Intelligence-Revised Dutch version |
| Festen DAM et al 7 | 3–14 years | 25/25 | 1 mg/m2/day | 2 | Netherlands | Z-stature, body composition (%fat, LBM-SDS), head circumference (Z) |
| Festen DAM et al 16 | Grupo I: 2–3 years C: 1–5 years | 20/22 | 1 mg/m2/day | 1 | Netherlands | Motor and mental development (BSID-II). |
| Myers SE et al 44 | 4–37 months | 12/11 | 1 mg/m2/day | 1 | USA | Z-stature, head circumference, body composition (%fat, LBM-kg), language/cognition (age of first spoken word and Capute scales of infant’s language), motor development (age of walking and Toddler and Infant Motor Evaluation) |
| Carrel AL et al 38 | 4–37 months | 15/14 | 1 mg/m2/day | 1 | USA | Growth velocity, body composition and motor development (Toddler Infant Motor Evaluation) |
| Whitman BY et al 17 | 4–16 years | 35/19 | 1 mg/m2/day | 2 | USA | Behaviour (Offord Survey Diagnostic Instrument and Family Inventory of Life Events) |
| Carrel AL et al 5 | 4–16 years | 35/19 | 1 mg/m2/day | 1 | USA | Body composition (%fat, LBM-kg), growth velocity, BMI-kg, muscular strength and agility (agility run, broad jump, sit-ups in 20 secs and upper extremity strength) |
| Lindgren AC et al 6 | 3–12 years | 15/12 | 0.1 IU/kg/day | 1 | Sweden Denmark |
Z-stature, BMI-SDS, body composition (%fat, LBM-kg), growth velocity. |
BMI, body mass index; LBM, lean body mass; rhGH, recombinant human GH; SDS, SD scores.
The seven meta-analysis excluded studies contain outcomes related to cognitive function, behaviour, quality of life and motor development. For the evaluation of cognitive function in patients with PWS, different questionnaires were used; therefore, meta-analysis was not possible.33–35 The same occurred with the behaviour outcome.17 33 36 Regarding quality of life, only one study was found.18 Five studies with different measures were found for muscular strength/motor development.5 16 35 37 38 All these studies are described in table 1 and analysed at the end of results section
Non-randomised studies
Regarding the non-randomised studies, 20 were selected: 11 before and after studies and 9 cohort studies (table 2). Of these, only 14 could be evaluated regarding the following outcomes: height z-scores (ZE), Z-BMI, proportion of fat mass (%) and adverse effects. The patient-year (number of patients x years of follow-up) unit was used for long-term follow-up studies.
Table 2.
Characteristics of the non-randomised studies that evaluated the use of growth hormone in patients with Prader-Willi syndrome
| Author | Type | Age | N rhGH | Dose of rhGH | Period (years) | Country | Outcome |
| Donze SH et al 15 | BEFORE AND AFTER | 6 months-3 years | 29 | 1 mg/m2/day | 3 | Netherlands | Psychomotor development (BSID-II - mental and motor development), head circumference |
| Dykens EM et al 13 | COHORT (three separated studies) |
4–21 years | 96; 127; 168 |
1 mg/m2/day | 6, 2 | USA | BMI-SDS. Cognition: KBIT-2 (verbal IQ, non-verbal IQ, composite IQ) VABS-II (communication and daily live skills, socialisation, adaptive composite). Hyperphagia Questionnaire; Repetitive Behaviour Scale |
| Bakker NE et al 10 |
BEFORE AND AFTER | 6±4.3 years | 1566 | 0.23 mg/kg/week | 3 | KIGS database -worldwide | Z-stature, BMI-SDS, adverse effects |
| Bakker NE et al 18 | BEFORE AND AFTER | 6–14 years | 76 | 1 mg/m2/day | 11 | Netherlands | Quality of life (DUX25 and DUXPW questionnaires) |
| Scheermeyer E et al 47 | BEFORE AND AFTER | 13–24 months 2–12 years | 72 | 1 mg/m2/day | 3 | Australia | Z-stature, BMI-SDS and adverse effects |
| Lo ST 201534 | COHORT | 3.5–14 years | 24 | 1 mg/m2/day | 2;8 | Netherlands | Behaviour. Developmental Behaviour Checklist of Children with intellectual disability (DBC) and Children's Social Behaviour Questionnaire (CSBQ) |
| Lo ST et al 36 | COHORT | 3.5–14 years | 53 | 1 mg/m2/day | 2;7 | Netherlands | VABS-II, Cognitive function: Bayley Scales of Infants II- NL (BSID-II), Wechsler Preschool and Primary Scale of Intelligence-Revised Dutch version |
| Bakker NE et al 12 | BEFORE AND AFTER | 3–7 years (mean: 5.49) | 60 | 1 mg/m2/day | 8 | Netherlands | Z-stature, BMI-SDS, lean body mass-SDS, % fat mass-SDS, head circumference |
| Meinhardt U et al 42 | COHORT | 0.4–12.2 years (mean:3.8) | 41 | 0.03 mg/kg/day | 1; 6 | Switzerland, Denmark, Germany | Z-stature, body composition and adverse effects |
| Siemensma EPC et al 14 | COHORT | 3.5–14 years | 29 | 1 mg/m2/day | 2; 4 | Netherlands | WISC-R (vocabulary, similarities, block design and picture arrangement) and Wechsler Preschool and Primary Scale of Intelligence-Revised Dutch version - less 7 years old |
| Colmenares A et al 48 | COHORT | 1–15 years (mean: 6±3.7) | 36 | 0.03 mg/kg/day | 3 | France | Z-stature, BMI-SDS and body composition- lean mass (kg)/ %fat mass |
| Sipilä I et al 39 | BEFORE AND AFTER | 2.0–10.3 years (mean: 6.6) | 20 | 0.033 mg⁄kg⁄ day | 1; 10 | Finland | Z-stature, BMI-SDS, body composition (%fat), and quality of life (HRQOL) |
| Carrel AL et al 8 | COHORT | 4–32 months/. 6–9 years | 46 | 1 mg/m2/day | 6 | USA | Z-stature, body composition and muscular strength |
| de Lind van Wijngaarden RFA et al 9 | BEFORE AND AFTER | 5.9±3.2 years | 55 | 1 mg/m2/day | 4 | Netherlands | Z-stature, BMI-SDS, body composition (%fat-SDS and lean body mass- SDS), head circumference |
| Nyunt O et al 49 | COHORT | <3 years and >3 years | 54 | 0,6 mg/m2/day | 4 | Australia | Z-stature and BMI-SDS |
| Lindgren AC et al 50 | BEFORE AND AFTER | 4.9–11.3 years (mean 6.9) | 22 | 0.03 mg/kg/day | 10 | Sweden | Z-stature, BMI-SDS and body composition |
| Lin H-Y et al 51 | BEFORE AND AFTER | 1.3–13.5 years | 46 | 0.01 U/kg/day | 5 | Taiwan | Z-stature, BMI-SDS and adverse effects |
| Angulo MA et al 43 | COHORT | 8.3±2.7 years | 21 | 0.25 mg/kg/week | 7.9 | USA | Z-stature and BMI-SDS |
| Carrel AL et al 40 | BEFORE AND AFTER | 12 years | 48 | 1 mg/m2/day | 4 | USA | Z-stature, body composition, muscular strength, adverse effects |
| Tauber M et al 52 | BEFORE AND AFTER | 8.4±3.2 years | 14 | 0.5 U/kg/week | 3.6 | France | Z- stature SDS, BMI-SDS, growth velocity |
BMI, body mass index; rhGH, recombinant human GH; SDS, SD scores.
There were only two studies that evaluated quality of life,18 39 two that evaluated behaviour with different questionnaires13 36 and four that evaluated cognitive function, also with different evaluation methods (table 2).13–15 34 We found two studies for muscular strength/motor development.15 40They are analysed at the end of results section. For the meta-analysis process and for a better approach to all data, we transformed all cohort studies into before and after studies. Therefore, the study of Carrel 2010 was excluded from all analysis because it had no baseline data.
For all the studies included, the obtained results are reported according to each outcome.
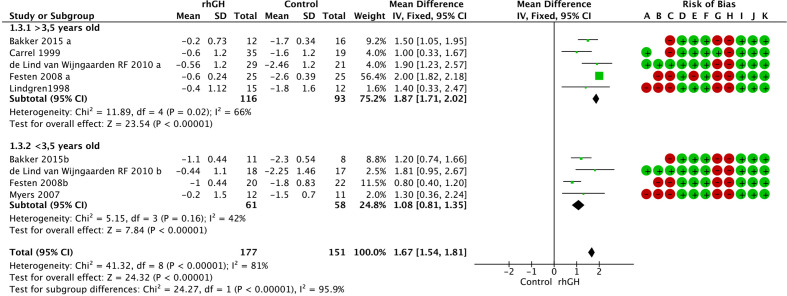
Growth: z-stature and growth velocity
Among the nine RCTs with a total of 328 patients, the treated group had an improvement in height of 1.67 (95% CI 1.54 to 1.81) SDS compared with that in the control group. In the younger group (under 3.5 years), the improvement was 1.08 (95% CI 0.81 to 0.35) SDS, and in the older group, it was 1.87 (95% CI 1.71 to 2.02) SDS. The Z-stature meta-analysis quality of evidence was moderate when all groups were included and high when the two age groups were analysed separately, due to decreased heterogenicity (figure 2, online supplementary file 3).
Figure 2.
Difference between rhGH treated group related to Z-stature in RCTs (RevMan 5.3). (A) Random sequence generation (selection bias). (B) Allocation concealment (selection bias). (C) Blinding of participants and personnel (performance bias). (D) Blinding of outcomes assessment (detection bias). (E) Incompleted outcome data (attrition bias), selective reporting (reporting bias). (G) Intention-to-treat. (H) Sample size determination. (I) Outcome. (J) Early interruption. (K) Prognostic characteristics. GH, growth hormone; RCTs, randomised controlled trials; rhGH, recombinant human GH.
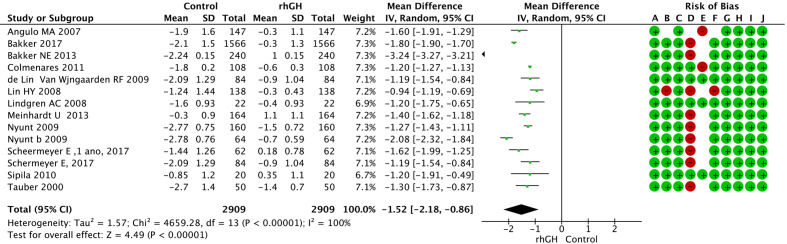
In the NRCT studies, the treated group had a significant improvement of stature (1.52 (95% CI 0.86 to 2.16) SDS) during the 2909 patients-years of follow-up (figure 3), this meta-analysis, however, was based in low quality evidence (online supplementary file 4).
Figure 3.
Association between rhGH treatment and Z-stature in the NRCTS (RevMan 5.3). (A) Inclusion criteria. (B) Condition and measure. (C) Diagnostic method. (D) Consecutive inclusion. (E) Loss of participants. (F) Group characteristics. (G) Clinical information. (H) Outcomes. (J) Demographics. NRCTs, non-randomised controlled trials; rhGH, recombinanthuman growth hormone.
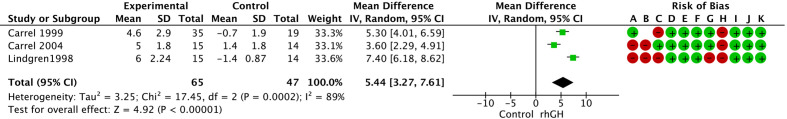
The group receiving rhGH treatment had a significant improvement in growth velocity of 5.44 cm (95% CI 3.27 to 7.61) compared with that in the control group among the three RCTs (figure 4), but the quality of evidence was also low (online supplementary file 3). We chose to report the growth velocity measure in centimetres and due to that one article that used only SDS measure was excluded.
Figure 4.
Association between rhGH-treated group and the no treatment group according to growth velocity in RCTs (RevMan 5.3). (A) Random sequence generation (selection bias). (B) Allocation concealment (selection bias). (C) Blinding of participants and personnel (performance bias). (D) Blinding of outcomes assessment (detection bias). (E) Incompleted outcome data (attrition bias). (F) Selective reporting (reporting bias). (G) Intention-to-treat. (H) Sample size determination. (I) Outcome. (J) Early interruption. (K) Prognostic characteristics. RCTs,randomised controlled trials; rhGH, recombinant human growth hormone.
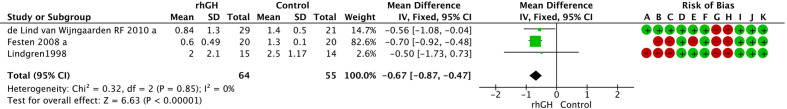
Z-BMI
The group receiving rhGH treatment had a Z-BMI decrease of −0.67 SDS (95% CI −0.87 to −0.47) compared with that in the control group among the three RCTs (figure 5). The quality of evidence was high (online supplementary file 3). The study of Bakker 2015 was excluded after examining the funnel plot.18
Figure 5.
Association between rhGH-treated group and the no treatment group related to Z-BMI in RCTs (RevMan 5.3). (A) Random sequence generation (selection bias). (B) Allocation concealment (selection bias). (C) Blinding of participants and personnel (performance bias). (D) Blinding of outcomes assessment (detection bias). (E) Incompleted outcome data (attrition bias). (F) Selective reporting (reporting bias). (G) Intention-to-treat. (H) Sample size determination. (I) Outcome. (J) Early interruption. (K) Prognostic characteristics. BMI,body mass index; RCTs, randomised controlled trials; rhGH, recombinant human growthhormone.
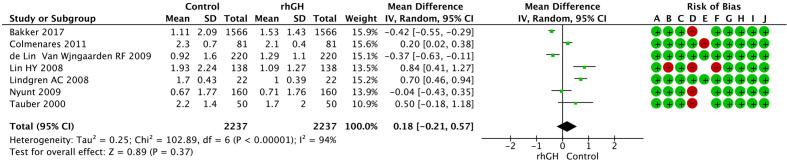
The NRCT studies showed no difference during the 2237 patients-years of follow-up after rhGH treatment (figure 6). It is important to note that no change in BMI during the follow-up of these patients was considered the opposite of the disease natural history. The quality of this evidence was very low (online supplementary file 4).
Figure 6.
Association between rhGH treatment and Z-BMI in the NRCTs (RevMan 5.3). (A) Inclusion criteria. (B) Condition and measure. (C) Diagnostic method. (D) Consecutive inclusion. (E) Loss of participants. (F) Group characteristics. (G) Clinical information. (H) Outcomes. (J) Demographics. (K) Statistical analysis. BMI,body mass index; NRCTs, non-randomisedcontrolled trials; rhGH, recombinant human growth hormone.
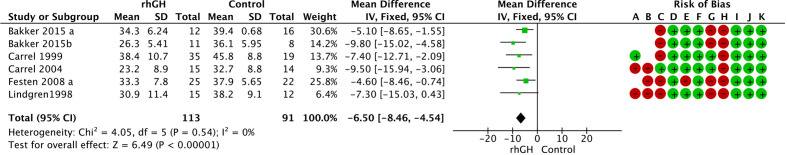
%Fat mass
In six of the included RCTs, which evaluated a total of 204 patients, the group treated with rhGH had a significant reduction in the fat mass proportion of −6.5 (95% CI −8.46 to −4.54) % compared with that in the control group. These data have high quality of evidence (figure 7) (online supplementary file 3). All studies used Lunar DXA. We excluded the de Lind van Wijngaarden RFA 2010 because they used a different type of measure for body fat mass (fat mass SDS according to Dutch patients).41
Figure 7.
Association between rhGH-treated group and the no treatment group related to %fat mass in RCTs (RevMan 5.3). (A) Random sequence generation (selection bias). (B) Allocation concealment (selection bias). (C) Blinding of participants and personnel (performance bias). (D) Blinding of outcomes assessment (detection bias). (E) Incompleted outcome data (attrition bias). (F) Selective reporting (reporting bias). (G) Intention-to-treat. (H) Sample size determination. (I) Outcome. (J) Early interruption. (K) Prognostic characteristics. RCTs,randomised controlled trials; rhGH, recombinant human growth hormone.
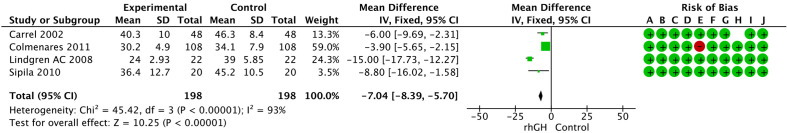
In the NRCT studies, we also found a significant reduction in the proportion of fat mass (−7.04%; 95% CI−8.39 to −5.7)) in 198 patients-year of follow-up with a low quality of evidence (figure 8) (online supplementary file 4). The data in the de Lind van Wijngaarden RFA 2009 study were reported in SDS-fat mass and were not included in the analysis.9
Figure 8.
Association between rhGH-treated group and the no treatment group related to %fat mass during follow-up in the NRCTs studies. (A) Inclusion criteria. (B) Condition and measure. (C) Diagnostic method. (D) Consecutive inclusion. (E) Loss of participants. (F) Group characteristics. (G) Clinical information. (H) Outcomes. (J) Demographics. (K) Statistical analysis. NRCTs, non-randomised controlled trials; rhGH,recombinant human growth hormone.
Lean mass
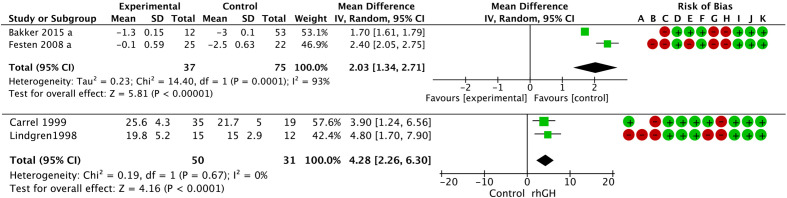
The group receiving rhGH treatment had an SDS-lean mass improvement of 2.03 (95% CI 1.34 to 2.71) SDS compared with that of the control group among two randomised controlled trials with moderate quality of evidence (figure 9. online supplementary file 3. The studies by Lindgren 1998 and Carrel 1999 used another variable and showed an increase of 4.28 (95% CI 2.26 to 6.30) kg of lean mass with high quality of evidence (online supplementary file 3).5 6
Figure 9.
Difference between rhGH treated group and the no treatment group related to lean mass-SDS and kg in RCTs (RevMan 5.3). (A) Random sequence generation (selection bias). (B) Allocation concealment (selection bias). (C) Blinding of participants and personnel (performance bias). (D) Blinding of outcomes assessment (detection bias). (E) Incompleted outcome data (attrition bias). (F) Selective reporting (reporting bias). (G) Intention-to-treat. (H) Sample size determination. (I) Outcome. (J) Early interruption. (K) Prognostic characteristics. RCTs,randomised controlled trials; rhGH, recombinant human growth hormone; SDS, SD scores.
Head circumference
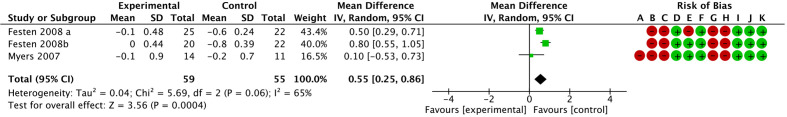
The group receiving rhGH treatment had a head circumference improvement of 0.55 (95% CI 0.25 to 0.86) cm compared with that of the control group among the three RCTs including a total of 114 patients. The quality of the evidence was moderate (figure 10, online supplementary file 3).
Figure 10.
Difference between rhGH treated group and the no treatment group according to head circumference in RCTs (RevMan 5.3). (A) Random sequence generation (selection bias). (B) Allocation concealment (selection bias). (C) Blinding of participants and personnel (performance bias). (D) Blinding of outcomes assessment (detection bias). (E) Incompleted outcome data (attrition bias). (F) Selective reporting (reporting bias). (G) Intention-to-treat. (H) Sample size determination. (I) Outcome. (J) Early interruption. (K) Prognostic characteristics. RCTs,randomised controlled trials; rhGH, recombinant human growth hormone.
Cognitive function, behaviour, motor development/muscular strength and quality of life
All the results from RCTs and NRCTs were described in table 3.
Table 3.
Results of cognitive function, behaviour, motor development and quality of life
| Author | Test type | Results |
| Cognitive function | ||
| Dykens EM et al 13 | Cognition: KBIT-2 (verbal IQ, non-verbal IQ, composite IQ) VABS-II (communication and daily live skills, socialisation, adaptive composite). | Children receiving GHT had significantly higher verbal and composite IQs, and adaptive communication and daily living skills. Those who started before 12 months of age had higher non-verbal and composite IQs. |
| Donze SH et al 15 | Psychomotor development (Bayley Scales of Infants II -BSID-II - mental and motor development) | During 3 years of GH, mental development increased from 58.1% (2.8) at baseline to 79.6% (3.7) (p<0.01). A lower baseline psychomotor development and a younger age at start of GH treatment were associated with a higher increase in mental development (p<0.01). No control group for this analysis. |
| Lo ST 201536 | VABS-II, cognitive function: BSID-II, Wechsler Preschool and Primary Scale of Intelligence-Revised Dutch version | Starting GH treatment at an earlier age during infancy led to better adaptive skills on the long-term. No effect in short-term. BSD-II already described in Festen 2008. |
| Siemensma EPC et al 14 | WISC-R (Vocabulary, similarities, block design and picture arrangement) and Wechsler Preschool and Primary Scale of Intelligence-Revised Dutch version | In short-term, rhGH prevented deterioration of certain cognitive skills (similarities and vocabulary domain) and significantly improved abstract reasoning and visuospatial skills during 4 years of GH treatment. Children with lower cognitive functioning at baseline, GH treatment had a greater effect on abstract verbal reasoning and visuospatial skills in comparison with control group. |
| Festen DAM et al 16 | Mental development Bayley Scales of Infant Development II (BSID-II) | Mental development improved significantly during the first year of study in the GH group versus the control group: median (IQR) change was +9.3% (-5.3 to 13.3) versus -2.9% (8.1 to 4.9) (p<0.05) in mental development. |
| Myers SE44 | Language/ cognition (age of first spoken word and Capute scales of Infants language) | GH-treated PWS group progressed significantly more during the first year in both language and cognitive development than the PWS control group; First words were spoken at 14 months, in 12 subjects treated before their first birthday and 17.2 in late-treated subjects, compared with reported data for global PWS of 21–23 months. |
| Böhm B et al 33 | Cognition (Raven's Standard, Progressive Matrices test, Arthur's adaptation of Leiter's Performance Scale; SPIQ test, Terman's Scale of intelligence, Bender Gestalt test, Harris Draw-a-Man) | No difference was found in these patients (mean age 6.3 years) regarding cognitive function. |
| Behaviour outcome | ||
| Dykens EM et al 13 | Repetitive Behaviour Scale and Adaptive Behaviour | rhGH treated versus treatment naïve 4 to 21 years old children with PWS had significantly higher adaptive behaviour standard scores, but no differences in repetitive behaviour scales. |
| Lo ST et al 34 | Behaviour (Developmental Behaviour Checklist of Children with intellectual disability and Children Social Behaviour Questionnaire) | No difference reported. |
| Whitman BY et al 17 | Behaviour (Offord Survey Diagnostic Instrument and Family Inventory of Life Events) | No differences between groups; however, a significant positive effect (reduction of depressive symptoms) was noted for the treated group |
| Böhm B et al 33 | Behaviour (specific test for this study) | No difference between groups. Successively worsened behaviour after discontinuing GH treatment. |
| Motor development/ muscle strength | ||
| Donze SH et al 15 | Psychomotor development (BSID-II - mental and motor development) | During 3 years of GH, mean motor development increased from 41.9% (2.9) to 78.2% (3.9) (p<0.01). A lower baseline psychomotor development and a younger age at start of GH treatment were associated with a higher increase in motor development (p<0.01). |
| Reus L et al 37 | Muscular thickness by ultrasound | GH has a positive effect on muscle thickness (biceps; forearm flexor, quadriceps and tibialis anterior) in PWS infants. |
| Reus L et al 35 | Muscle strength (Infant Muscle Strength Meter - AIMS) and Motor function (Gross Motor Function Measure - GMFM); Bayley Scales of Infants II- BSD-II | The AIMS and GMFM clearly revealed a significant a positive effect of GH on motor development; the child’s maximum motor potential increased with GH treatment, thereby resulting in a clear functional improvement. BSID-II revealed no effect of GH on motor development. |
| Festen DAM et al 16 | Motor and mental development. Bayley Scales of Infant Development II (BSID-II) | Significant improvement in motor development (+11.2% vs −18.5%) at the first year of treatment in the treated group versus control group from the baseline. |
| Myers SE et al 44 | Motor development (age of walking and Toddler and Infant Motor Evaluation) | A trend towards improved mobility and stability percentile rankings was noted with GH therapy, however, wide variability among PWS subjects was seen at all time points. Eleven PWS subjects treated before their first birthday walked independently at a mean age of 23.5 months. Five late-treated PWS subjects walked independently at a mean age of 24.3 months. |
| Carrel AL et al 40 | Muscular strength | Documented changes in physical function (strength and agility testing) in PWS children treated with GH in first 2 years therapy, but no change in the following 2 years. |
| Carrel AL et al 5 | Muscular strength and agility (agility run, broad jump, sit-ups in 20 s and upper extremity strength) | Agility run (faster by 2.3±0.5 s), broad jump (farther by 3.3±1.9 inches), abdominal strength (an improvement of 3.0±2.1 sit-ups/20 s) and upper extremity strength (increase of 2.5±1.8 weight-lift repetitions/30 s); compared with baseline performance |
| Quality of life | ||
| Bakker NE et al 18 | DUX25 and DUXPW questionnaires for children and parents | GH-treated children showed a significant improvement in health -related quality of life during the 2-year RCT in the physical subdomain of the DUX25 and the DUXPW, compared with the untreated ones. During long-term GH treatment (11 year), questionnaires scores remained stable. Social subdomain was higher in children with a deletion than in children with an uniparental disomy or imprinting defect, according to parents |
| Sipilä I et al 39 | 16D (generic 16-dimension health-related quality of life) instrument for adolescents | The effect of rhGH therapy remains unclear because of a lack of untreated control group with PWS and lack of comparable baseline measurements for evaluating changes over time. |
GH, growth hormone; GHT, GH therapy; IQs, intelligent quotients; PWS, Prader-Willi syndrome; RCT, randomised controlled trial; rhGH, recombinant human GH.
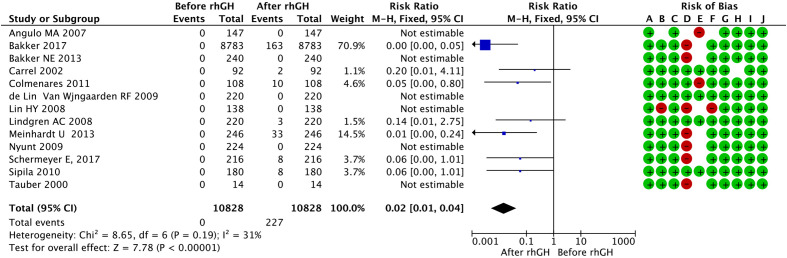
Adverse effects
In the RCT studies, there were few reports related to the adverse effects of rhGH use. Carrel 1999 reported one case of cerebral pseudotumour, and Myers reported one case of scoliosis.5 6 For a better analysis, we used ‘before and after studies’, which evaluated more patients and had a longer follow-up. Side effects related to rhGH in patients/year of follow-up were 227. We only included the following side effects for this analysis that are according the authors are related to the treatment: sleep apnoea (n=35), initial headache (n=9), peripheral oedema (n=7), type 2 diabetes mellitus (n=11), scoliosis (n=64). This last side effect is cited and counted, but it is difficult to establish a relationship between its rhGH progression and treatment. The quality of this evidence was moderate. Twelve deaths were reported in all these studies. (figure 11, online supplementary file 4).
Figure 11.
Adverse effects during the rhGH follow-up period in NRCTs (RevMan 5.3). (A) Inclusion criteria. (B) Condition and measure. (C) Diagnostic method. (D) Consecutive inclusion. (E) Loss of participants. (F) Group characteristics. (G) Clinical information. (H) Outcomes. (J) Demographics. NRCTs, non-randomised controlled trials; rhGH,recombinant human growth hormone.
Discussion
PWS is a challenging and rare disease with few treatment options. To the best of our knowledge, this is the first meta-analysis that evaluated the use of rhGH in a large number of PWS patients while assessing different domains, allowing an overall vision of the impact of rhGH treatment.
Our study showed that rhGH use during infancy promoted an improvement of stature, body composition (%fat mass and lean body mass) and growth velocity. Indeed, data about final height confirmed this evidence.3 24 42 43 The impact of +1.67 SD in stature and the decrease of 6.5% to 7.0% in fat mass is not negligible in PWS daily life and can contribute with their fight against obesity and their complications. The short-term impact on BMI, in association with diet, was good; in the long run, rhGH controlled the weight gain that is part of the natural history of PWS, but there was a great deal of variability among the studies.
The confidence level for each effect changed according to the quality of the evidence. We found a high quality of evidence for stature, BMI and %fat mass, and we found a moderate level for the other parameters in the RCT studies. Furthermore, a reasonable number of non-RCT studies confirmed our findings even with a low quality of evidence.
Although the effects of rhGH on growth and body composition were more objectively reported, cognitive function studies were quite difficult to evaluate. Most cognitive function studies reported improvements in the different measures used, especially in verbal and non-verbal IQ and vocabulary domain.13 14 44 Children that started the treatment at a young age (less than 1 year old) reported better adaptive communication skills in long-term studies.13 44 Indeed, in Bayley Scales for Infants two studies showed differences in mental development.15 16 Unfortunately, these data could not be aggregated.
The actions of rhGH on cognitive function could be explained by the presence of brain GH receptors, especially at a younger age, during which brain development is taking place at a more intense pace.14 Moreover, GH can increase the muscle tone, as we will discuss in reviewed articles, and stimulate physical activity. Therefore, it can promote articulation and motor control for optimal development of communication skills, which additionally promotes social interaction and physical tasks. These effects might be cumulative over time. Also, the largest effect of GH treatment on adaptive functioning was reached if GH treatment was started at a younger age during infancy.45
Muscular strength and motor development seemed to improve in treated patients according to selected articles.5 15 16 35 37 40 44 Multilevel regression models controlled for age and baseline muscle thickness identified a statistically significant rhGH dependency in the Reus article.37 The authors discuss a major response in the first years of treatment and at a young age.16 40
The impact on behaviour in patients with PWS was not clear. Most of the articles did not show any difference. Positive results are cited in Böhm et al that found worse behaviour in PWS patients, as evaluated by a parental questionnaire, after cessation of hGH treatment and in Dykens et al that showed better adaptive behaviour scores.13 27Regarding quality of life, there is only one study with a specific PWS questionnaire that showed an improvement at the start of the treatment, but not in the long run.18
The low number of adverse effects in RCTs are generally poorly reported in literature, as we found in our analysis.46 In NRCTs, the number of reported adverse events indicated a low risk of mortality and few complications during long-term follow-up in studies with moderate quality of evidence. Sleep apnoea still needs to be evaluated with polysomnography. Even in cohort studies, we have some difficulties to access all information regarding adverse effects, so we cannot fully comment on safety.
The different measures adopted, especially regarding the body composition analysis (related to the Dutch SDS for all parameters) and the cognitive function evaluation, were a limitation for this study. Many articles could not be used. It was not possible to analyse the impact in mental development and IQ, an important initial endpoint for this study, due to the lack of universal questionnaires in this field. We are convinced that the elaboration of a specific questionnaire to evaluate the syndrome at each age would add great value for this analysis in future studies. Additionally, more studies evaluating cognitive function and quality of life are needed in PWS patients.
Another barrier was the difficulty in finding RCTs that studied the use of rhGH in patients with PWS. The main reason is that professionals who treat PWS feel uncomfortable and unethical withholding rhGH treatment in a group of their patients with PWS. At the same time, many countries still do not have access to rhGH treatment. Potential biasses could be related to exclusion criteria in clinical studies, where severe cases or adherence difficulties (social and economic problems) could be excluded. Therefore, larger registry is still important to evaluate long-term follow-up with specific emphasis on the covariates of PWS to extrapolate our results. The genetic variability of PWS, with different implicated genes, is a great challenge for patients’ comparison, especially regarding cognition. Differences according to the dose response and genetic subtypes could not be analysed in this review but may be very important to ascertain conclusive disease knowledge and its prognosis following treatment.
Conclusion
Growth hormone treatment can promote an improvement of stature, body composition and BMI, modifying the disease’s natural history; growth hormone treatment may also be implicated in improving cognition and motor development at a young age.
Supplementary Material
Acknowledgments
The authors are grateful to all associated professors and fellows from pediatric endocrinology unit at University of Sao Paulo.
Footnotes
Correction notice: This article has been corrected after publication. Due to a translation error, the term 'Beggar's test' was erroneously used in the Methods section instead of 'Egger test'.
Contributors: All authors contributed to the focus of the systematic review. CP and WB drafted the initial protocol, with guidance and feedback at all stages from SI, RF, ET, DD and MP. CP, SI and RF collected data from the articles. CP, WB, DD and MP interpreted the results. All authors have revised and reviewed the results and have approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: No, there are no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. Data from published studies were analysed.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Passone CBG, Pasqualucci PL, Franco RR, et al. Prader-willi syndrome: What is the general pediatrician supposed to do? - A review. Rev Paul Pediatr 2018;36:345–52. 10.1590/1984-0462/;2018;36;3;00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Miller JL. Approach to the child with Prader-Willi syndrome. J Clin Endocrinol Metab 2012;97:3837–44. 10.1210/jc.2012-2543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bridges N. What is the value of growth hormone therapy in Prader Willi syndrome? Arch Dis Child 2014;99:166–70. 10.1136/archdischild-2013-303760 [DOI] [PubMed] [Google Scholar]
- 4. Tauber M, Cutfield W. KIGS highlights: growth hormone treatment in Prader-Willi syndrome. Horm Res 2007;68:48–50. 10.1159/000110475 [DOI] [PubMed] [Google Scholar]
- 5. Carrel AL, Myers SE, Whitman BY, et al. Growth hormone improves body composition, fat utilization, physical strength and agility, and growth in Prader-Willi syndrome: a controlled study. J Pediatr 1999;134:215–21. 10.1016/S0022-3476(99)70418-X [DOI] [PubMed] [Google Scholar]
- 6. Lindgren AC, Hagenäs L, Müller J, et al. Growth hormone treatment of children with Prader-Willi syndrome affects linear growth and body composition favourably. Acta Paediatr 1998;87:28–31. 10.1111/j.1651-2227.1998.tb01380.x [DOI] [PubMed] [Google Scholar]
- 7. Festen DAM, de Lind van Wijngaarden R, van Eekelen M, et al. Randomized controlled GH trial: effects on anthropometry, body composition and body proportions in a large group of children with Prader-Willi syndrome. Clin Endocrinol 2008;69:443–51. 10.1111/j.1365-2265.2008.03228.x [DOI] [PubMed] [Google Scholar]
- 8. Carrel AL, Myers SE, Whitman BY, et al. Long-Term growth hormone therapy changes the natural history of body composition and motor function in children with Prader-Willi syndrome. J Clin Endocrinol Metab 2010;95:1131–6. 10.1210/jc.2009-1389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. de Lind van Wijngaarden RFA, Siemensma EPC, Festen DAM, et al. Efficacy and safety of long-term continuous growth hormone treatment in children with Prader-Willi syndrome. J Clin Endocrinol Metab 2009;94:4205–15. 10.1210/jc.2009-0454 [DOI] [PubMed] [Google Scholar]
- 10. Bakker NE, Lindberg A, Heissler J, et al. Growth hormone treatment in children with Prader-Willi syndrome: three years of longitudinal data in prepubertal children and adult height data from the KIGS database. J Clin Endocrinol Metab 2017;102:1702–11. 10.1210/jc.2016-2962 [DOI] [PubMed] [Google Scholar]
- 11. Colmenares A, Pinto G, Taupin P, et al. Effects on growth and metabolism of growth hormone treatment for 3 years in 36 children with Prader-Willi syndrome. Horm Res Paediatr 2011;75:123–30. 10.1159/000319709 [DOI] [PubMed] [Google Scholar]
- 12. Bakker NE, Kuppens RJ, Siemensma EPC, et al. Eight years of growth hormone treatment in children with Prader-Willi syndrome: maintaining the positive effects. J Clin Endocrinol Metab 2013;98:4013–22. 10.1210/jc.2013-2012 [DOI] [PubMed] [Google Scholar]
- 13. Dykens EM, Roof E, Hunt-Hawkins H. Cognitive and adaptive advantages of growth hormone treatment in children with Prader-Willi syndrome. J Child Psychol Psychiatry 2017;58:64–74. 10.1111/jcpp.12601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Siemensma EPC, Tummers-de Lind van Wijngaarden RFA, Festen DAM, et al. Beneficial effects of growth hormone treatment on cognition in children with Prader-Willi syndrome: a randomized controlled trial and longitudinal study. J Clin Endocrinol Metab 2012;97:2307–14. 10.1210/jc.2012-1182 [DOI] [PubMed] [Google Scholar]
- 15. Donze SH, Damen L, Mahabier EF, et al. Improved mental and motor development during 3 years of GH treatment in very young children with Prader-Willi syndrome. J Clin Endocrinol Metab 2018;103:3714–9. 10.1210/jc.2018-00687 [DOI] [PubMed] [Google Scholar]
- 16. Festen DAM, Wevers M, Lindgren AC, et al. Mental and motor development before and during growth hormone treatment in infants and toddlers with Prader-Willi syndrome. Clin Endocrinol 2008;68:919–25. 10.1111/j.1365-2265.2007.03126.x [DOI] [PubMed] [Google Scholar]
- 17. Whitman BY, Myers S, Carrel A, et al. The behavioral impact of growth hormone treatment for children and adolescents with Prader-Willi syndrome: a 2-year, controlled study. Pediatrics 2002;109:E35. 10.1542/peds.109.2.e35 [DOI] [PubMed] [Google Scholar]
- 18. Bakker NE, Siemensma EPC, van Rijn M, et al. Beneficial effect of growth hormone treatment on health-related quality of life in children with Prader-Willi syndrome: a randomized controlled trial and longitudinal study. Horm Res Paediatr 2015;84:231–9. 10.1159/000437141 [DOI] [PubMed] [Google Scholar]
- 19. Angulo MA, Butler MG, Cataletto ME. Prader-Willi syndrome: a review of clinical, genetic, and endocrine findings. J Endocrinol Invest 2015;38:1249–63. 10.1007/s40618-015-0312-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tauber M, Diene G, Molinas C. Sequelae of GH treatment in children with PWS. Pediatr Endocrinol Rev 2016;14:138–46. 10.17458/PER.2016.TDM.SequelaeofGH [DOI] [PubMed] [Google Scholar]
- 21. Al-Saleh S, Al-Naimi A, Hamilton J, et al. Longitudinal evaluation of sleep-disordered breathing in children with Prader-Willi syndrome during 2 years of growth hormone therapy. J Pediatr 2013;162:263–8. 10.1016/j.jpeds.2012.07.042 [DOI] [PubMed] [Google Scholar]
- 22. Nishi Y, Tanaka T. Growth hormone treatment and adverse events. Pediatr Endocrinol Rev 2017;14:235–9. 10.17458/per.vol14.2017.nt.growthhormonetreatment [DOI] [PubMed] [Google Scholar]
- 23. de Onis M, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7. 10.2471/BLT.07.043497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Butler MG, Lee J, Cox DM, et al. Growth charts for Prader-Willi syndrome during growth hormone treatment. Clin Pediatr 2016;55:957–74. 10.1177/0009922815617973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 2002;11:1–190. [PubMed] [Google Scholar]
- 26. Fredriks AM, van Buuren S, Burgmeijer RJ, et al. Continuing positive secular growth change in the Netherlands 1955-1997. Pediatr Res 2000;47:316–23. 10.1203/00006450-200003000-00006 [DOI] [PubMed] [Google Scholar]
- 27. Higgins J, Savović J, Page M, et al. Revised Cochrane risk of bias tool for randomized trials (rob 2.0). Version 20. Bristol: University of Bristol, 2016: 1–7. [Google Scholar]
- 28. Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 29. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13. 10.1186/1471-2288-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. The Nordic Cochrane Centre, The Cochrane Collaboration . Review manager (RevMan). version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. [Google Scholar]
- 31. Guyatt GH, Oxman AD, Vist GE, et al. Grade: an emerging consensus on rating quality of evidence and strength of recomendations. BMJ 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Böhm B, Ritzén EM, Lindgren AC. Growth hormone treatment improves vitality and behavioural issues in children with Prader-Willi syndrome. Acta Paediatr 2015;104:59–67. 10.1111/apa.12813 [DOI] [PubMed] [Google Scholar]
- 34. Lo ST, Siemensma EPC, Festen DAM, et al. Behavior in children with Prader-Willi syndrome before and during growth hormone treatment: a randomized controlled trial and 8-year longitudinal study. Eur Child Adolesc Psychiatry 2015;24:1091–101. 10.1007/s00787-014-0662-4 [DOI] [PubMed] [Google Scholar]
- 35. Reus L, Pelzer BJ, Otten BJ, et al. Growth hormone combined with child-specific motor training improves motor development in infants with Prader-Willi syndrome: a randomized controlled trial. Res Dev Disabil 2013;34:3092–103. 10.1016/j.ridd.2013.05.043 [DOI] [PubMed] [Google Scholar]
- 36. Lo ST, Festen DAM, Tummers-de Lind van Wijngaarden RFA, et al. Beneficial effects of long-term growth hormone treatment on adaptive functioning in infants with Prader-Willi syndrome. Am J Intellect Dev Disabil 2015;120:315–27. 10.1352/1944-7558-120.4.315 [DOI] [PubMed] [Google Scholar]
- 37. Reus L, Pillen S, Pelzer BJ, et al. Growth hormone therapy, muscle thickness, and motor development in Prader-Willi syndrome: an RCT. Pediatrics 2014;134:e1619–27. 10.1542/peds.2013-3607 [DOI] [PubMed] [Google Scholar]
- 38. Carrel AL, Moerchen V, Myers SE, et al. Growth hormone improves mobility and body composition in infants and toddlers with Prader-Willi syndrome. J Pediatr 2004;145:744–9. [DOI] [PubMed] [Google Scholar]
- 39. Sipilä I, Sintonen H, Hietanen H, et al. Long-Term effects of growth hormone therapy on patients with Prader-Willi syndrome. Acta Paediatr 2010;99:1712–8. 10.1111/j.1651-2227.2010.01904.x [DOI] [PubMed] [Google Scholar]
- 40. Carrel AL, Myers SE, Whitman BY, et al. Benefits of long-term GH therapy in Prader-Willi syndrome: a 4-year study. J Clin Endocrinol Metab 2002;87:1581–5. 10.1210/jcem.87.4.8414 [DOI] [PubMed] [Google Scholar]
- 41. de Lind van Wijngaarden RFA, Cianflone K, Gao Y, et al. Cardiovascular and metabolic risk profile and acylation-stimulating protein levels in children with Prader-Willi syndrome and effects of growth hormone treatment. J Clin Endocrinol Metab 2010;95:1758–66. 10.1210/jc.2009-0656 [DOI] [PubMed] [Google Scholar]
- 42. Meinhardt U, Christiansen JS, Farholt S, et al. Eiholzer U;The efficacy and safety of long-term Norditropin treatment in children with Prader-Willi syndrome. Horm Metab Res 2013;45:532–6. [DOI] [PubMed] [Google Scholar]
- 43. Angulo MA, Castro-Magana M, Lamerson M, et al. Final adult height in children with Prader-Willi syndrome with and without human growth hormone treatment. Am J Med Genet A 2007;143A:1456–61. 10.1002/ajmg.a.31824 [DOI] [PubMed] [Google Scholar]
- 44. Myers SE, Whitman BY, Carrel AL, et al. Two years of growth hormone therapy in young children with Prader-Willi syndrome: physical and neurodevelopmental benefits. Am J Med Genet A 2007;143A:443–8. 10.1002/ajmg.a.31468 [DOI] [PubMed] [Google Scholar]
- 45. Bakker NE, Siemensma EPC, Koopman C, et al. Dietary energy intake, body composition and resting energy expenditure in prepubertal children with Prader-Willi syndrome before and during growth hormone treatment: a randomized controlled trial. Horm Res Paediatr 2015;83:321–31. 10.1159/000374113 [DOI] [PubMed] [Google Scholar]
- 46. Anderson M, Choonara I. A systematic review of safety monitoring and drug toxicity in published randomised controlled trials of antiepileptic drugs in children over a 10-year period. Arch Dis Child 2010;95:731–8. 10.1136/adc.2009.165902 [DOI] [PubMed] [Google Scholar]
- 47. Scheermeyer E, Harris M, Hughes I, et al. Low dose growth hormone treatment in infants and toddlers with Prader-Willi syndrome is comparable to higher dosage regimens. Growth Horm IGF Res 2017;34:1–7. 10.1016/j.ghir.2017.03.001 [DOI] [PubMed] [Google Scholar]
- 48. Colmenares A, Pinto G, Taupin P, et al. Effects on growth and metabolism of growth hormone treatment for 3 years in 36 children with Prader-Willi syndrome. Horm Res Paediatr 2011;75:123–30. [DOI] [PubMed] [Google Scholar]
- 49. Nyunt O, Harris M, Hughes I, et al. Benefit of early commencement of growth hormone therapy in children with Prader-Willi syndrome. J Pediatr Endocrinol Metab 2009;22:1151–8. 10.1515/JPEM.2009.22.12.1151 [DOI] [PubMed] [Google Scholar]
- 50. Lindgren AC, Lindberg A. Growth hormone treatment completely normalizes adult height and improves body composition in Prader-Willi syndrome: experience from KIGS (pfizer international growth database). Horm Res 2008;70:182–7. 10.1159/000145019 [DOI] [PubMed] [Google Scholar]
- 51. Lin H-Y, Lin S-P, Tsai L-P, et al. Effects of growth hormone treatment on height, weight, and obesity in Taiwanese patients with Prader-Willi syndrome. J Chin Med Assoc 2008;71:305–9. 10.1016/S1726-4901(08)70127-8 [DOI] [PubMed] [Google Scholar]
- 52. Tauber M, Barbeau C, Jouret B, et al. Auxological and endocrine evolution of 28 children with Prader-Willi syndrome: effect of GH therapy in 14 children. Horm Res 2000;53:279–87. 10.1159/000053184 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2019-000630supp001.pdf (298.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. Data from published studies were analysed.