End-stage organ failure is estimated to affect more than six million people worldwide.1 In 2018, transplant systems across the world enabled around 150 000 patients to benefit from a kidney, heart, lung, liver, or other solid organ—a number far less than the demand. According to data from WHO, more than 1 500 000 people live with a transplanted organ worldwide. In the USA, approximately 40 000 patients receive an organ transplant every year, but 120 000 patients remain on a waiting list for transplantation, with 7600 individuals dying annually while waiting for an organ transplant. In Europe and many other countries, patients are affected by a similar scarcity of organs and high death rates while on the waiting list for transplantation.
As nations adjust to new realities driven by the coronavirus disease 2019 (COVID-19) pandemic, many health-care providers, institutions, and patients are concerned about the potential effect that COVID-19 will have on organ donation and transplantation. One concern is that transplant recipients might have greater susceptibility to infection and increased viral burden.2 A second concern is that hospitals will not have the resources in terms of staff and equipment to care for recipients after transplantation, who typically need intensive care and multispecialty management.
Because of the overwhelming health-care system burden of the COVID-19 pandemic, a pronounced negative effect on worldwide organ donation and transplantation is anticipated but has not been measured. Our objective was to quantify the contemporary effect of the COVID-19 pandemic on organ donation and transplantation in France and the USA.
We did nationwide analyses using data on COVID-19 diagnoses from Public Health France and the Center for System Science and Engineering.3 Organ procurement and transplantation data were obtained from two federal agencies, the National Organ Procurement Agency in France and the United Network for Organ Sharing in the USA.4 Organ transplantations were counted using mean 5 days moving averages, with stratified analyses done for kidney, liver, heart, and lung.
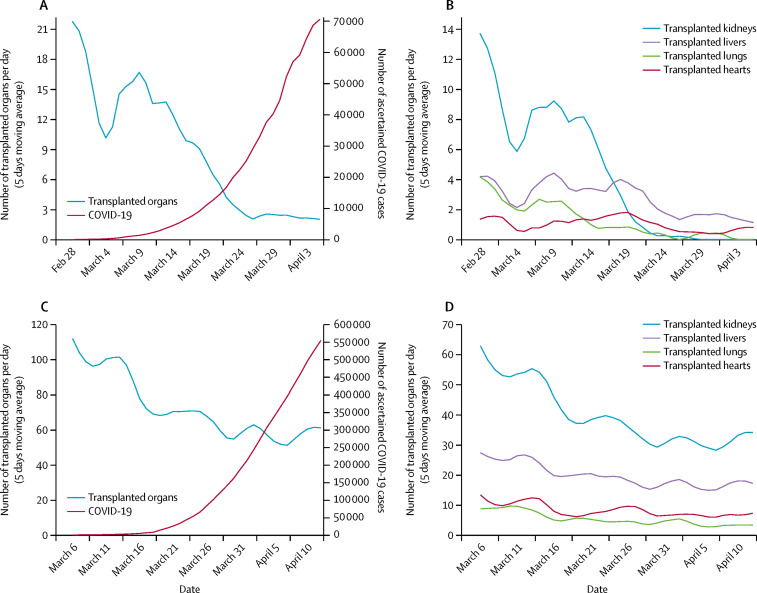
We noted a strong temporal association between the increase in COVID-19 infections and a striking reduction in overall solid-organ transplantation procedures (figure ). The effect was seen in France and confirmed in the USA. The overall reduction in deceased donor transplantations since the COVID-19 outbreak was 90·6% in France and 51·1% in the USA, respectively. In both France and the USA, this reduction was mostly driven by kidney transplantation, but a substantial effect was also seen for heart, lung, and liver transplants, all of which provide meaningful improvement in survival probability. In the appendix, the geographical association is shown between areas with COVID-19 clusters and the decrease in organ procurement, showing a significant reduction in transplantation rates even in regions where COVID-19 cases are low, suggesting a global and nationwide effect beyond the local COVID-19 infection prevalence.
Figure.
Trends in COVID-19 spread over time in France and the USA and recovery of organs and solid-organ transplantation procedures from deceased donors
(A, C) Number of COVID-19 diagnoses and number of solid organs recovered for transplantation over time in France (A) and the USA (C). (B, D) Total number of transplants from deceased donors, with separate trend lines for kidney, liver, heart, and lung, over time in France (B) and the USA (D). Data were obtained from Public Health France (A), the National Organ Procurement Agency (B), Xu et al3 (C), and the United Network for Organ Sharing (D). Data accessed April 11, 2020. COVID-19=coronavirus disease 2019.
To the best of our knowledge, this is the first nationwide assessment of the effect of COVID-19 on organ donation and transplantation in France and the USA. As COVID-19 spreads rapidly across Europe to North America, South America, and other continents, health-care providers and leaders of medical institutions will make difficult decisions about how best to deploy limited medical resources.5 These choices could be especially devastating for the thousands of patients in need of an organ transplant. While living donor organ transplants could presumably be rescheduled for a future date, deceased donor organs must be procured immediately or the opportunity is lost.
Transplant professionals will need to adapt to these rapidly changing circumstances, provide reassurance to their patients, and remain poised to reinvigorate the valuable transplant infrastructure when the COVID-19 crisis begins to abate. By using the example of organ transplantation, which is a highly regulated field and has a specific centralised day-to-day reporting scheme at a federal level, we show how high-value medical procedures can be affected by the COVID-19 pandemic, with outcomes for vulnerable patient groups. Furthermore, detailed cartographic mapping of trends in organ donation and transplant activity will enable targeted interventions when the burdens of COVID-19 get lighter. Some organ procurement organisations and their networks will undoubtedly recover more quickly than others through best practices and effective communication with hospitals. Careful mapping will enable public health leaders and transplant organisations to identify areas where transplants have not recovered well and support is needed.
Acknowledgments
PPR declares investigator-initiated research grants from Merck, AbbVie, and CVS Caremark to the University of Pennsylvania. All other authors declare no competing interests. AL, OA, PPR, FB, and CJ contributed equally.
Supplementary Material
References
- 1.Levin A, Tonelli M, Bonventre J. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet. 2017;390:1888–1917. doi: 10.1016/S0140-6736(17)30788-2. [DOI] [PubMed] [Google Scholar]
- 2.American Society of Transplantation COVID-19 information. April 17, 2020. https://www.myast.org/covid-19-information
- 3.Xu B, Kraemer MUG, on behalf of the Open COVID-19 Data Curation Group Open access epidemiological data from the COVID-19 outbreak. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30119-5. published online Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Network for Organ Sharing Transplant trends. April 27, 2020. https://unos.org/data/transplant-trends/
- 5.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.