Abstract
Background
Addressing the determinants of severe acute malnutrition (SAM) among children remains a challenge in Nepal. This study investigated the effect of maternal and social determinants of SAM among under-five children of Nepal.
Methods
We conducted a hospital-based unmatched case-control study with 256 under-five children (128 cases and 128 controls). The children aged 6–59 months were taken, and the cases and controls were defined based on mid-upper arm circumference (MUAC).
Results
Backward Stepwise logistic regression analysis of 6–59 months children showed that the odds of SAM were lower among male children (AOR = 0.50, 95% CI = 0.27–0.92), mothers from high socioeconomic status (AOR = 0.469, 95% CI = 0.26–0.83), breastfeeding 6–12 months (AOR = 0.21, 95% CI = 0.05–0.68), breastfeeding ≥13 months (AOR = 0.18, 95% CI = 0.05–0.54) and optimal complementary feeding (AOR = 0.40, 95% CI = 0.22–0.70). SAM was significantly higher among children of the age group 6–24 months (AOR = 2.57, 95% CI = 1.30–5.22) and children with a history of diarrhea (AOR = 1.75, 95% CI = 0.92–3.39).
Conclusions
In order to reduce the children's SAM, it is necessary to scale up services to improve the socioeconomic status which includes the education, occupation, and monthly income of the mother. Girls of age group 6–24 months were more likely to develop SAM. Two contributing factors to decrease SAM are the importance of exclusive breastfeeding practices and the availability and usage of soap in hand washing, which are ideal for low cost interventions. To reduce SAM in Nepal, a focus on enhancing complementary feeding through increased affordability of nutritious foods is also needed.
Keywords: Health sciences, Public health, Poverty, Sociology, Social organisation, Severe acute malnutrition, Under-five children, Case-control study, Social determinants, Nepal
Health sciences; Public health; Poverty; Sociology; Social organisation; Severe acute malnutrition; Under-five children; Case-control study; Social determinants; Nepal.
1. Introduction
Severe acute malnutrition (SAM) is a life-threatening situation-characterized by severe wasting (low weight-for-height) or the presence of nutritional edema and occurs due to insufficient consumption of nutrients [1]. The World Health Organization (WHO) recommends the use of MUAC and examination for bilateral pitting edema in children 6–59 months of age by trained community health workers and community members for early identification and referral of children with severe acute malnutrition (SAM) [2].
The burdens of childhood malnutrition include hampering the physical and cognitive development of children and the impact on the financial growth of individuals and the community [3, 4]. Children with SAM have nine times more risk of death compared to healthy children [5]. The UNICEF, WHO, World Bank global and child malnutrition indicate insufficient progress to reduce malnutrition in reaching the Sustainable Development Goals set for 2030 [4]. In 2016, 17 million under-five children suffered from SAM globally, and it is estimated that the majority (70–80%) of malnourished children live in lower and middle-income countries, including Nepal [4, 5, 6].
Malnutrition remains a serious obstacle to child survival, growth, and development in Nepal. In Nepal, approximately 50% of cases of under-five childhood mortality (39 per 1000 live births) is because of malnutrition [7]. According to the 2016 National Demographic and Health Survey of Nepal, more than one-third (36%) of under-five children are suffering chronic under-nutrition, and more than 10% are acutely under-nourished [7]. The prevalence of SAM among under-five children escalated to 2.6% (2006) from from 1.1% (2001) and remained consistent from 2006 to 2011 [7]. Moreover, a study from 2017 reported the prevalence of SAM among under-five children in Nepal was 4.14% [8]. The prevalence of SAM among under-five children in some areas of Nepal remains higher than the national average [9, 10]. Due to high prevalence of SAM in Nepal, the case fatality rate (numbers of death per 100 child-months) of children is around 5% each year [9].
UNICEF suggests that multiple direct and indirect causes are responsible for childhood malnutrition [11]. The most important causes of malnutrition are diseases and insufficient intake of nutrients in Nepal. Furthermore, feeding and care practices of infants and young children, especially breastfeeding, complementary feeding, provision of foods for pregnant and lactating women, sanitation and hygiene practices are inadequate in the greater part of Nepal [10, 11].
Globally, many studies conducted to identify factors affecting SAM among under-five children [12, 13, 14, 15]. In 2014, a study in Nepal found that low socioeconomic status, mother's age at birth >35, birth interval months <24 months, illiterate father, bottle feeding and not initiating complementary feeding at the age of 6 months were significantly associated with SAM [8].
Despite the increasing prevalence of SAM among children in Nepal, limited studies have been undertaken to understand the determinants of SAM. Moreover, data mainly in the context of the mother-child pair is scarce on the determinants of SAM in children. The current study, therefore, investigated the maternal profiles and social determinants of SAM in Nepal. The findings of the study give us the understanding to focus on the areas to sustain the reduction of SAM and improve the ongoing intervention programs in Nepal.
2. Material and methods
2.1. Study site & study population
This study was carried out from June 2018 to October 2018 in Kanti Children's Hospital and Siddhi Memorial Hospital & Public Health Centre of Nepal. The Kanti Children's Hospital is a specialized hospital of Nepal for the treatment of sick children and located in the capital city- Kathmandu and run by the Government of Nepal. As of 2018, the hospital has a bed capacity of 320 (http://kantichildrenhospital.gov.np/director-message/). Again, the Siddhi Memorial Hospital & Public Health Centre is a specialized hospital for the treatment of sick children, women, and older adults, which is run by a non-government organization (NGO). It is located in Bhaktapur District of Nepal. As of 2016, it has a bed capacity of 50, and at present on average, 50 children come for consultations at the pediatric out-patient department every day.
The study was a hospital-based unmatched case-control study. The children were screened for their nutritional status by using mid-upper arm circumference (MUAC) measurement. Cases were children aged 6–59 months admitted in these two hospitals who were severely malnourished with MUAC <115 mm or bilateral pitting edema. The mothers of these malnourished children were questioned if they met the inclusion criteria and gave consent. The controls were labeled as well-nourished with a MUAC ≥125mm without bilateral pitting edema. Children with a chronic illness like HIV, Tuberculosis, and other congenital abnormalities that can hamper the feeding pattern of the child were excluded from the study. We carried out the study in accordance with the guidelines set out in the Helsinki Declaration, and all procedures involving human subjects were approved by the North South University Institutional Review Board (NSU-IRB 3532), the Kanti Children's Hospital Review Committee (reference number 191, date: 5 March 2018) and the Siddhi Memorial Hospital & Public Health Centre's review committee. Prior to data collection, a written, informed consent was taken by the mother of the children.
2.2. Sampling technique & sample size
Convenience sampling technique was used to collect the mothers and targeted children in each group following STROBE guideline (https://www.strobe-statement.org/index.php?id=available-checklists). Sample size of the study was calculated using the following formula assuming 5% significance level (i.e., = 1.96), 80% power (i.e., Zβ = 0.84) of the study, and a case-control ratio of 1:1 (r = 1).
The percentage of control exposed for age group 6–24 months was assumed at 60% (i.e., p2 = 0.60) with an odds ratio (OR) of 2.20 based on a case-control study done in Nepal [8]. Thus, we estimated a minimum of a sample size of 126 cases and an equal number of controls to obtain 80% power at the 5% significance level.
2.3. Variables of the study
Data regarding socio-demographic characteristics like age and gender of the child, urban living in last 2 years of the mother and child, parents’ education and occupation and environmental variables like source of water, hand washing habit for mother, availability of food for last 2 weeks and 3 times/day were collected using a semi-structured questionnaire from the mothers. Socioeconomic status (SES) for the mother was calculated based on a composite score considering the education and occupation of the mother, along with the monthly income of the family [16]. The Kuppuswamy scale classifies the study populations into high, middle, and poor SES. We took proximal factors like complementary or dietary feeding per day, duration of breastfeeding, and household care practice. We also included data of acute diarrhea history for a child in the last one month and use of health services after the current sickness of a child. We define the employed parents who get a monthly salary from their occupation.
Mid-upper arm circumference (MUAC) was measured by MUAC tape at the mid-point between the tip of the shoulder and the tip of the elbow. The readings were recorded to the nearest 0.1 cm. The measuring tape fitted firmly but did not create any pit in the upper arm. The lengths for children aged 6–24 months were measured in lying on a bed, and heights for children 25–59 months were recorded by standing in centimeter. Weight was measured in kilogram by the help of weighing machine. For measuring weight, the respondents were dressed lightly with barefoot.
2.4. Statistical analysis
We analyzed the data using software R. We presented the categorical variables as frequencies and percentages in the case and control groups. We investigated the association between SAM and exposure variables by using multivariable logistic regression analysis with a backward selection procedure. We carried out a calculation of adjusted OR (AOR) for each factor. A value of p < 0.05 was considered to be significant where the confidence interval for OR was set at 95% (95% CI).
3. Results
In this study, 256 children (128 were cases and 128 controls) were chosen to determine the maternal profiles and socio-demographic factors of the under-five children. The mean ± SD weight for height z-score (WHZ) of cases and controls was −2.584 ± 1.198 versus −0.287 ± 1.206 (p < 0.001), respectively (Table 1). Defining the cases and controls based on MUAC produces 72% similarity with the definition of WHZ < −3. A meta-analysis suggests that MUAC should be the primary indicator used in defining SAM in health facilities [17]. We define cases and controls based on MUAC. Table 1 indicates the difference of MUAC (or WHZ) between case and control is significant at 5% significance level.
Table 1.
Mean and standard deviation (SD) of WAZ, WHZ and MUAC among 6–59 months children.
| Parameters | Case | Control | p-value |
|---|---|---|---|
| Weight for age z-score (WAZ) | -3.097 (1.072) | -0.712 (1.084) | <0.001 |
| Weight for height z-score (WHZ) | -2.584 (1.198) | -0.287 (1.206) | <0.001 |
| MUAC (cm) | 11.062 (0.413) | 13.638 (0.822) | <0.001 |
3.1. Effect of socio-demographic factors on SAM
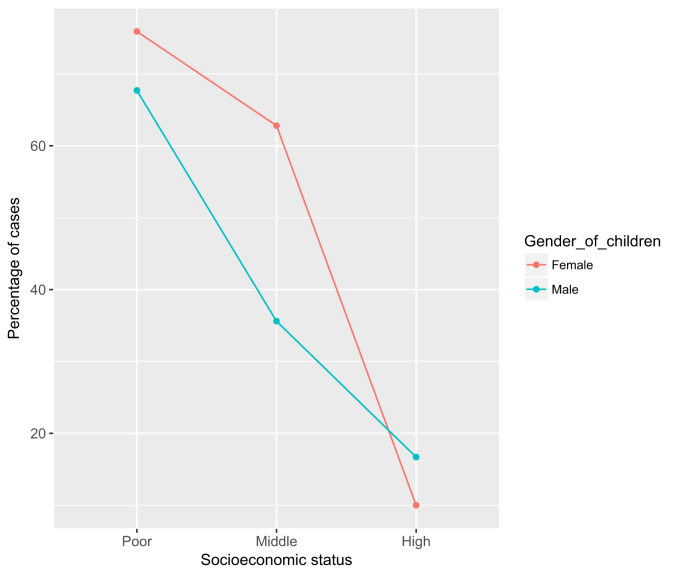
The descriptive statistics, along with the unadjusted odds ratios for the socio-demographic factors, are given in Table 2. Among the 256 children in the study, 75% were in the age group of 6–24 months, and 25% of them were in the age group of 25–59 months. Among them, 54.69% were boys, and 45.71% were girls. The majority (57.03%) of these children lived in urban areas, whereas 42.97% lived in rural areas. Figure 1 shows the relationship between mothers’ socioeconomic status (SES) and gender of children among the cases. It appears that improving SES can reduce the the gap between proportions of SAM for male and female children. The figure shows that female children are more prone to become cases from the poor and middle socioeconomic groups. The results of the unadjusted odds ratio from Table 2 indicates that there was a significant difference among cases and controls associated with family monthly income (OR = 0.29, 95% CI = 0.16–0.49). Among the 256 children, the majority of the fathers (64.56%) and mothers (58.98%) had more than eight years of schooling. The odds ratio for the socioeconomic status (SES) of the mother (OR = 0.07, 95% CI = 0.02–0.20, reference: poor) indicates that improving the mothers' education, occupation, and family monthly income can reduce the severe acute malnutrition to the children. The odds ratio shows the children of the mothers who belong to high SES had 93% less odds to have SAM compared to the children of the mothers who belonged to poor SES.
Table 2.
Effect of socio-demographic factors on SAM among 6–59 months children.
| Factors | Categories | Case (%) | Control (%) | Unadjusted OR (CI) | p-value |
|---|---|---|---|---|---|
| Child age (Months) | 6–24 | 105 (82.0) | 87 (67.9) | Ref | |
| 25 & above | 23 (17.9) | 41 (32.0) | 0.46 (0.26–0.83) | 0.010 | |
| Child gender | Male | 58 (45.3) | 81 (63.3) | 0.48 (0.29–0.79) | 0.004 |
| Female | 70 (54.7) | 47 (36.7) | Ref | ||
| Primary residence in the last 2 years of mother | Urban | 70 (54.7) | 76 (59.4) | 0.83 (0.50–1.35) | 0.448 |
| Rural | 58 (45.3) | 52 (40.6) | Ref | ||
| Monthly income (NPR) | Below 25000 NPR | 102 (79.7) | 68 (53.1) | Ref | |
| 25000 & above NPR | 26 (20.3) | 60 (46.9) | 0.29 (0.16–0.49) | <0.001 | |
| Fathers' education | Illiterate | 34 (26.8) | 12 (9.4) | Ref | |
| <8 years schooling | 23 (18.1) | 21 (16.5) | 0.39 (0.16–0.92) | 0.035 | |
| >8 years schooling | 70 (55.1) | 94 (74.0) | 0.26 (0.12–0.53) | <0.001 | |
| Mothers' education | Illiterate | 48 (37.5) | 20 (15.6) | Ref | |
| <8 years schooling | 14 (10.9) | 23 (17.9) | 0.25 (0.10–0.58) | 0.001 | |
| >8 years schooling | 66 (51.6) | 85 (66.4) | 0.32 (0.17–0.59) | <0.001 | |
| Fathers' occupation | Unemployed | 8 (6.3) | 4 (3.2) | Ref | |
| Daily Laborer | 64 (50.4) | 38 (29.9) | 0.84 (0.21–2.86) | 0.790 | |
| Employed | 55 (43.3) | 85 (66.9) | 0.32 (0.08–1.07) | 0.761 | |
| Mothers' occupation | Housewife | 90 (70.3) | 83 (64.8) | Ref | |
| Daily Laborer | 28 (21.9) | 12 (9.38) | 2.15 (1.04–4.65) | 0.042 | |
| Employed | 10 (7.81) | 33 (25.8) | 0.28 (0.12–0.58) | 0.001 | |
| Family Types | Joint | 48 (37.5) | 47 (36.7) | Ref | |
| Nuclear | 80 (62.5) | 81 (63.3) | 0.97 (0.58–1.61) | 0.897 | |
| Number of Children | 1 | 40 (31.3) | 50 (39.1) | Ref | |
| 2 | 68 (53.1) | 54 (42.2) | 1.57 (0.91–2.73) | 0.104 | |
| ≥3 | 20 (15.6) | 24 (18.8) | 1.04 (0.50–2.15) | 0.912 | |
| Mother's Socio-economic status | Poor | 43 (33.6) | 17 (13.3) | Ref | |
| Middle | 81 (63.3) | 87 (68.0) | 0.37 (0.19–0.69) | 0.002 | |
| High | 4 (3.1) | 24 (18.7) | 0.07 (0.02–0.20) | <0.001 |
Bold values represent significant at 5% significance level.
Figure 1.
Mothers Socioeconomic status (SES) and gender of children among the 128 cases attending two hospitals of Nepal.
3.2. Effect of environmental factors on SAM
About half of the families of the cases (51.56%) used pond or river as a source of their water while 33.59% of the families from control group used pond or river as their source of water (Table 3). The results from Table 3 shows that the children who used water from river/pond were 2.10 times more odds to become cases compared to the children who used filter/tap water (OR = 2.10, 95% CI = 1.27–3.50). Approximately 75% of the mothers from case group and 92.19% of the mothers from control group used soap as their hand washing materials, and it had a significant effect on becoming cases (OR = 0.27, 95% CI = 0.12–0.58). We found a positive history of acute diarrhea during the last one month has a significant effect of becoming SAM (OR = 1.77, 95% CI = 1.03–3.08, reference: No acute diarrhea).
Table 3.
Effect of Environment factor on SAM among 6–59 months children.
| Factors | Categories | Case (%) | Control (%) | Unadjusted OR (CI) | p-value |
|---|---|---|---|---|---|
| Source of Water | Filter/tap | 62 (48.4) | 85 (66.4) | Ref | |
| Pond/River | 66 (51.6) | 43 (33.6) | 2.10 (1.27–3.50) | 0.003 | |
| Hand washing habit for mother | Regularly | 98 (76.6) | 106 (82.8) | 0.677 (0.36–1.25) | 0.215 |
| Occasionally | 30 (23.4) | 22 (17.2) | Ref | ||
| Hand Washing Materials for mother | Ash/Soil/None | 30 (23.4) | 10 (7.8) | Ref | |
| Soap | 98 (76.6) | 118 (92.2) | 0.27 (0.12–0.58) | <0.001 | |
| Acute diarrhea history for child/last 1 month | Yes | 45 (35.2) | 30 (23.4) | 1.77 (1.03–3.08) | 0.040 |
| No | 83 (64.8) | 98 (76.6) | Ref |
Bold values represent significant at 5% significance level.
3.3. Effect of proximal factors on SAM
In regards to daily complimentary or dietary food intake, 65.62% of the cases had less than three complementary or dietary feedings/day, while only 38.28% of the control groups had less than three dietary feedings/day. It appears from Table 4 that dietary feeding/day has a significant effect on SAM (OR = 0.32, 95% CI = 0.19–0.54). The majority of the mothers from cases (65.62%) and controls (85.94%) reported they had food available at home for the last two weeks. The results of odds ratio indicate the availability of food at home can reduce 69% of the odds of being SAM (OR = 0.31, 95% CI = 0.17–0.57). The Table indicates that the breastfeeding practice is excellent among the participants. The table shows 80.46% of the mothers from cases, and 95.31% of the mothers from controls practiced breastfeeding for more than six months. Besides, 48.44% of the mothers from cases and 71.88% of the mothers from controls practiced breastfeeding more than one year to their children. The results of odds ratios indicate that breastfeeding practice for more than six months can reduce the odds of SAM.
Table 4.
Effect of Proximal factor on SAM among 6–59 months children.
| Factors | Categories | Case (%) | Control (%) | Unadjusted OR (95% CI) | p-value |
|---|---|---|---|---|---|
| Complementary or diatary feeding/day | ≤3 times | 84 (65.62) | 49 (38.28) | Ref | |
| >3 times | 44 (34.38) | 79 (61.72) | 0.32 (0.19–0.54) | <0.001 | |
| Breastfeeding | <6 months | 25 (19.53) | 6 (4.69) | Ref | |
| 6–12 months | 41 (32.03) | 30 (23.43) | 0.32 (0.11–0.86) | 0.030 | |
| >12 months | 62 (48.44) | 92 (71.88) | 0.16 (0.06–0.39) | <0.001 | |
| Availability of food for the last 2 weeks | No | 44 (34.38) | 18 (14.06) | Ref | |
| Yes | 84 (65.62) | 110 (85.94) | 0.31 (0.17–0.57) | <0.001 | |
| Use of Health Services after the current sickness of child | After 24 hours | 42 (32.81) | 35 (27.34) | Ref | |
| Within 24 hours | 86 (67.19) | 93 (72.66) | 0.77 (0.45–1.31) | 0.34 |
Bold values represent significant at 5% significance level.
3.4. Stepwise regression
We used two stepwise logistic regression models with backward selection to identify maternal and social determinants that had significant associations with SAM among children of age 6–59 months and 6–24 months, respectively (Table 5). We consider the full model with the variables that were found with p-values <0.50 in Tables 2, 3, and 4.
Table 5.
Backward step-wise logistic regression provides the likelihood of the severe acute malnutrition among children of Nepal.
| Factors | Reference | Children 6–59 months |
Children 6–24 months |
|---|---|---|---|
| AOR (95% CI), p-value | AOR (95% CI), p-value | ||
| Child age (6–24 months) | 24 + months | 2.57 (1.30–5.22), 0.008 | - |
| Gender of the child (Boy) | Girls | 0.47 (0.26–0.84), 0.010 | 0.27 (0.13–0.54), <0.001 |
| Mother's socioeconomic status (High) | Poor | 0.15 (0.03–0.43), 0.002 | 0.032 (0.01–0.16), <0.001 |
| Mother socioeconomic status (Middle) | Poor | 0.63 (0.29–1.33), 0.225 | 0.35 (0.13–0.90), 0.033 |
| Acute diarrhea history for child in last 1 month (Yes) | No | 1.75 (0.92–3.39), 0.091 | - |
| Hand washing material for mother (Soap) | Ash/Soil/None | 0.44 (0.17–1.07), 0.078 | 0.30 (0.08–0.96), 0.051 |
| Complemetary or diatery feeding/day (>3 times) | ≤3 times | 0.40 (0.22–0.70), 0.002 | 0.54 (0.27–1.10), 0.091 |
| Breastfeeding (6–12 months) | <6 months | 0.31 (0.09–0.88), 0.036 | 0.17 (0.03–0.61), 0.027 |
| Breastfeeding (>12 motnhs) | <6 months | 0.22 (0.07–0.60), 0.005 | 0.20 (0.04–0.74), 0.027 |
3.4.1. Children aged 6–24 months
The results from multivariable analysis indicate that children from the mothers of high socioeconomic status had lower odds of SAM compared to the children from the mothers of poor socioeconomic status (adjusted odds ratio, AOR = 0.352, 95% CI = 0.129–0.898). It also appears from the analysis that the boys had less odds to become SAM compared to the girls (AOR = 0.237, 95% CI = 0.10–0.529). In the analysis, breastfeeding practices for more than 6 months and complementary or dietary feeding of more than 3 times a day in a child were associated with lower odds of SAM (AOR = 0.166, 95% CI = 0.034–0.608, reference: <6 months breastfeeding; AOR = 0.543, CI = 0.266–1.100, reference: ≤3 times complementary/dietary feeding, respectively). Mothers' handwashing habit using soap before feeding their child can reduce 70% of the odds of malnutrition to the children compared to the mothers who do not wash hands or use ash/soil for washing hands (AOR = 0.30, 95% CI = 0.08–0.95).
3.4.2. Children aged 6–59 months
The following maternal and child factors were significanlty associated with an increased likelihood of having SAM of the children in 6–59 months: age (6–24 months) (AOR = 2.57, 95% CI = 1.299–5.220, reference: 24 + months), girls (AOR = 2.13, reference: boys), poor socio-economic status of the mother (AOR = 8.06, reference = high), breastfeeding more than 6 months (AOR = 3.27, reference: <6 months) and complementary/dietary feeding more than 3 times a day (AOR = 2.53, reference: ≤3 times/day). Besides, children whose mothers had a habit of washing hands by soap were 56% less odds to experience SAM than the children whose mothers wash hands by ash/soil or did not have a habit of washing hands before feeding their children (AOR = 0.44, 95% CI = 0.174–1.069). It also appears that recent episodes of diarrhea may cause SAM among the children (AOR = 1.75, 95% CI = 0.919–3.389).
4. Discussion
Our study investigated the social determinants of severe acute malnutrition among children aged between 6 months and 59 months in two hospitals from Kathmandu and Bhaktapur district of Nepal. The results of this study showed that the age, gender of the child, monthly family income, mother's education, mother's occupation and frequency of complementary/dietary intake per day were significantly associated with SAM among under-five children.
SAM is more prevalent among girls than boys in Nepal. This could be assigned to the fact that girls are at more risk of health disparities compared to boys in the same age group, and more care and attention are provided to boys by their caregivers. Similar findings were found previously in India, Kenya, and Pakistan [17, 18, 19]. However, Solomon Demissie et al. found that boys were more at risk of SAM because of health inequalities compared to girls in Ethiopia [20].
In the present study, it was observed that age had a significant effect on the nutritional status of the children. The higher odds of SAM was found in 6–24 months age group compared to the 25–59 months age group children. Younger children (6–24 months) have a smaller stomach compared to the older children (25–59 months). Moreover, the younger children are in transition from milk based-diet to complementary feeding. Therefore, the frequency of feeding (both breastfeeding and complementary) practices for younger children should be more compared to the older children. But the practice of an optimal number of feeding could be less for the younger children in Nepal, and that's why these group of children are more likely to SAM compared to older children. The results of this study are found consistent with other countries like Ethiopia and South India [20, 21].
It is observed that socio-economic status has a significant effect on the nutritional status of the children. Mothers with higher education might have a better understanding of balanced dietary intake for the family members, thus enhances the nutritional status of their children [22]. Many studies found that maternal education had a positive and statistically significant effect on the nutritional status of the children [23, 24, 25, 26]. Moreover, illiterate mothers are trapped in unemployment or in low-skilled, poorly paid, and insecure employment who cannot contribute to the family monthly income significantly. Family monthly income plays a vital role to reduce the occurannce of SAM among under-five children [20, 27]. Unemployed mothers observed more malnourished children compared to employed mothers who get a monthly salary from their employment. Employed mothers can contribute to the family income and children from working mothers are less likely to live in poverty. Few studies conducted with under-five children in Egypt and Guatemala and found maternal employment had a positive and significant effect on nutritional status [28, 29].
This study reveals that children whose frequency of food intake was >3 times/day were 55% less likely to be severely malnourished. The knowledge and attitude of the parents, especially mothers concerning child feeding, might play a vital role in a child's eating frequency and behavior. Studies from Bangladesh and India indicate similar findings [23, 30]. Dietary intake >3 times is associated with SAM, and these findings suggest that the best feeding practices of under-five children are essential for their growth and immunity. Good feeding practice among under-five children helps to prevent acute malnutrition and growth retardation [31].
In this study, the duration of the breastfeeding was found to be significantly associated with severe acute malnutrition. Longer-duration breastfeeding is associated with protection against childhood infections, increases in intelligence, and can reduce the occurannce of SAM among under-five children. Similar findings were reported in India, and Madagascar [32, 33].
The conclusion drawn from this study about washing hands with soap before feeding the children is compatible with findings from Bangladesh and Kenya [34, 35]. Washing hands with soap before feeding the children can prevent diarrheal disease, maintain food hygiene, and help children to reduce the occurance of SAM.
From observations in these two hospitals of Nepal, we noticed some women were working away from their homes for extended periods, and their children were frequently left in the care of an elder sibling. Limitations include of not stratifying these working mothers in our study. Moreover, maternal age and birth spacing could be essential factors for SAM, but these variables were not included in the study. Recruiting cases at the hospital may have introduced a self-selection bias, as cases were selected based on MUAC only. Nevertheless, the study highlights at lower levels of socioeconomic status. The study hypotheses were suitably tested to confirm that mothers' education, mothers' occupation, and monthly income are associated with child nutritional status in that portion of the population.
5. Conclusion
The study explains the importance of improving the socioeconomic status that has a positive effect of reducing the malnutrition of under-five children in Nepal. The maternal socioeconomic status depends on the schooling, jobs, and monthly income of the mothers. Mother's academic training should be enhanced in Nepal; otherwise they would be stuck in unemployment or low-skilled, poorly paying, and precarious jobs that may lead their children to live in a poor socio-economic community. Additionally, girls in the 6–24 month age group are more likely to experience SAM than boys in a similar age range. An urgent need to encourage the value of breastfeeding and dietary consumption to ensure appropriate health treatment for their children is warned by evidence of harmful effects of stopping breastfeeding before six months and not offering the children nutritious food more than three times a day in this population. The value of breastfeeding practices and the availability and use of soap are two factors that lead to the reduction of SAM and are ideal for low cost interventions. The factors identified in the paper can help to explain the gaps of ongoing interventions to reduce SAM among under-five children in Nepal.
Declarations
Author contribution statement
A. Hossain: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
B. Niroula and S. Duwal: Conceived and designed the experiments; Performed the experiments.
S. Ahmed and M. Kibria: Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
All the authors acknowledge the participants for providing us the information to conduct the study. We would also like to thank the three anonymous reviewers and the editor for insightful comments that improved the presentation and clarity of our manuscript.
References
- 1.World Health Organization, World Food Programme, United Nations System Standing Committee on Nutrition & United Nations Children’s Fund (UNICEF) World Health Organization; 2007. . Community-Based Management of Severe Acute Malnutrition : a Joint Statement by the World Health Organization, the World Food Programme, the United Nations System Standing Committee on Nutrition and the United Nations Children's Fund.https://apps.who.int/iris/handle/10665/44295 [Google Scholar]
- 2.Collins S., Sadler K., Dent N. Key issues in the success of community-based management of severe malnutrition. Food Nutr. Bull. 2006;27:S49–82. doi: 10.1177/15648265060273S304. [DOI] [PubMed] [Google Scholar]
- 3.Black R.E., Victora C.G., Walker S.P. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–451. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 4.UNICEF/WHO/World Bank Group joint child malnutrition estimates Levels and Tends in Child Malnutrition. 2018. https://www.who.int/nutgrowthdb/2018-jme-brochure.pdf?ua=1
- 5.Ministry of Health and Population, Government of Nepal . February 2015. Nepal Health Sector Programme –2 Implementation Plan 2 (Nhsp -2.http://www.nhssp.org.np/NHSSP_Archives/jar/2015/01NHSP2_result_framework_indicator_february2015.pdf [Google Scholar]
- 6.UNICEF Report . December 2015. Prevention and Treatment of Severe Acute Malnutrition in East Asia and the Pacific.https://www.unicef.org/eap/media/1306/file [Google Scholar]
- 7.Ministry of Health Nepal 2016 Nepal Demographic and Health Survey. 2017. https://www.dhsprogram.com/pubs/pdf/fr336/fr336.pdf Published November.
- 8.Pravana N.K., Piryani S., Chaurasiya S.P. Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community- based case–control study. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-017084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministry of Health, Government of Nepal Annual Report Department of Health Services 2015-2016. 2017. https://phpnepal.org.np/publication/current-issue/recently-released/136-annual-report-of-department-ofhealth-services-2072-73-2015-2016 Published June, 73:522.
- 10.UNICEF. NEPAL . 2016. Integrated Management of Acute Malnutrition (IMAM) Guideline.http://www.chd.gov.np/downloads/1Nepal IMAMGuideline.pdf Published Online First. [Google Scholar]
- 11.UNICEF . Global Synthesis report; 2013. Evaluation of Community Management of Acute Malnutrition (CMAM)https://www.unicef.org/evaldatabase/files/Final_CMAM_synthesis_FINAL_VERSION_with_ExSum_translations.pdf Published May. [Google Scholar]
- 12.Haithar S., Kuria M.W., Sheikh A. Maternal depression and child severe acute malnutrition: a case-control study from Kenya. BMC Pediatr. 2018;18:1–9. doi: 10.1186/s12887-018-1261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dodos J., Altare C., Bechir M. Individual and household risk factors of severe acute malnutrition among under-five children in Mao, Chad: a matched case-control study. Arch. Publ. Health. 2018;76:1–9. doi: 10.1186/s13690-018-0281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Misra K., Kumar P., Basu S., Rai K. Aneja. Risk factors for severe acute malnutrition in children below 5 years of age in India: a case-control study. Indian J. Pediatr. 2014;8:762–765. doi: 10.1007/s12098-013-1127-3. [DOI] [PubMed] [Google Scholar]
- 15.Macete E., Fumad V., Nhampossa T. Severe malnutrition among children under the age of 5 years admitted to a rural district hospital in southern Mozambique. Publ. Health Nutr. 2013;16:1565–1574. doi: 10.1017/S1368980013001080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh T., Sharma S., Nagesh S. Socio-economic status scales updated for 2017. Int. J. Res. Med. Sci. 2017 Jul;5(7):3264–3267. [Google Scholar]
- 17.Bliss J. Global Health: Science and Practice; 2018. Use of Mid-upper Arm Circumference by Novel Community Platforms to Detect, Diagnose, and Treat Severe Acute Malnutrition in Children: A Systematic Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel K.A., Langare S.D., Naik J.D. Gender inequality and bio-social factors in nutritional status among under five children attending anganwadis in an urban slum of a town in Western Maharashtra- India. J. Res. Med. Sci. 2013;18:341–345. [PMC free article] [PubMed] [Google Scholar]
- 19.Ndiku M., Jaceldo Siegl K., Singh P. Gender inequality in food intake and nutritional status of children under 5 years old in rural Eastern Kenya. Eur. J. Clin. Nutr. 2011;65:26–31. doi: 10.1038/ejcn.2010.197. [DOI] [PubMed] [Google Scholar]
- 20.Demissie S., Worku A. Magnitude and factors associated with malnutrition in children 6-59 Months of age in pastoral community of dollo ado district- Somali region- Ethiopia. Sci. J. Publ. Health. 2013;1:175. [Google Scholar]
- 21.Joseph B., Rebello A., Kullu P. Prevalence of malnutrition in rural Karnataka- South India: a comparison of anthropometric indicators. J. Health Popul. Nutr. 2002;20:239–244. [PubMed] [Google Scholar]
- 22.Abel Gebre, Reddy P. Surender, Mulugeta Afework, Sedik Yayo, Kahssay Molla. Prevalence of malnutrition and associated factors among under-five children in pastoral communities of Afar regional state, northeast Ethiopia: a community-based cross-sectional study. J. Nutr. Metabol. 2019 doi: 10.1155/2019/9187609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Musa M.K., Muhammad F., Lawal K.M. Risk factors of severe acute malnutrition among under-five Children : a hospital-based study in Bangladesh. J. Med. Sci. Health. 2017;3:13–21. [Google Scholar]
- 24.Ambadekar NN- Zodpey S.P. Risk factors for severe acute malnutrition in under-five children: a case-control study in a rural part of India. Publ. Health. 2017;142:136–143. doi: 10.1016/j.puhe.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 25.Wamani H., Åstrøm A.N., Peterson S. Predictors of poor anthropometric status among children under 2 years of age in rural Uganda. Publ. Health Nutr. 2006;9:320–326. doi: 10.1079/phn2006854. [DOI] [PubMed] [Google Scholar]
- 26.Dereje N. Determinants of severe acute malnutrition among under five children in shashogo woreda, southern Ethiopia: a community based matched case control study. J. Nutr. Food Sci. 2015;4 [Google Scholar]
- 27.Amosu A.M., Degun A.M., Atulomah N.O.S., Olanrewju M.F. A study of the nutritional status of under-5 children of low-income earners in a South- western Nigerian community. Curr. Res. J. Biol. Sci. 2011;3:P578–585. [Google Scholar]
- 28.Oddo V.M., Surkan P.J., Hurley K.M. Pathways of the association between maternal employment and weight status among women and children: qualitative findings from Guatemala. Matern. Child Nutr. 2018;14 doi: 10.1111/mcn.12455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rashad A.S., Sharaf M.F. Does maternal employment affect child nutrition status? New evidence from Egypt. Oxf. Dev. Stud. 2019;47:48–62. [Google Scholar]
- 30.Prashanth M.R., Savita M.R., Prashanth B. Risk factors for severe acute malnutrition in under-five children attending nutritional rehabilitation center of tertiary teaching hospital in Karnataka: a case control study. Int. J. Contemp. Pediatrics. 2017;4(5) [Google Scholar]
- 31.Pandey P., Singh S.K. Dietary determinant of severe acute malnutrition among infants: evidence from a case controlled study at a Central Indian district. South East Asia. J. Public Health. 2016;6:32–39. [Google Scholar]
- 32.Harimbola D.R., Mizumoto K. Individual and household risk factors for severe acute malnutrition among under-five children in the analamanga region, Madagascar. Int J MCH AIDS. 2018;7:217–225. doi: 10.21106/ijma.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ogbo F.A., Agho K., Ogeleka P. Infant feeding practices and diarrhoea in sub-Saharan African countries with high diarrhoea mortality. PloS One. 2017;12 doi: 10.1371/journal.pone.0171792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raihan M.J., Farzana F.D., Sultana S. Examining the relationship between socio-economic status, WASH practices and wasting. PloS One. 2017;12 doi: 10.1371/journal.pone.0172134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Null C., Stewart C.P., Pickering A.J. Effects of water quality, sanitation, handwashing and nutritional interventions on diarrhoea and child growth in rural Kenya: a cluster-randomised controlled trial. Lancet Glob Heal. 2018;6:e316–e329. doi: 10.1016/S2214-109X(18)30005-6. [DOI] [PMC free article] [PubMed] [Google Scholar]