Key Points
Maximum diameter had a complex association with all-cause mortality.
MB was associated with more favorable disease characteristics and improved OS.
Abstract
Controversy exists regarding the definition and prognostic significance of bulk in advanced-stage (stage III/IV) Hodgkin lymphoma (ASHL), and bulk location (mediastinum vs other sites) further complicated the setting. This retrospective, multi-institutional study comprised 814 ASHL patients between 2000 and 2010 and aimed to evaluate the significance of bulk in ASHL. End points of interest included progression-free survival (PFS) and overall survival (OS). Covariates included maximum diameter and the site of bulky disease. SmoothHR and Kaplan-Meier analyses were used to assess for an association of PFS and OS with covariates. In the exploratory cohort (n = 683), maximum diameter had no association with PFS and a complex, U-shaped association with all-cause mortality on smoothHR analysis. Using 5 cm as a cutoff for bulk, Kaplan-Meier analyses confirmed the smoothHR results. The site of bulk was incorporated to divide patients into 2 groups. The mediastinal bulk (MB) type had more favorable characteristics than the nonbulky/non-MB (NB/NMB) type on age, histology, and bone marrow involvement (P < .001). The MB type was associated with better OS than the NB/NMB-type on univariable analysis (5-year OS, 92% vs 86%; HR, 0.53; 95% confidence interval, 0.34-0.84; P = .007). These findings persisted in the subgroup treated with chemotherapy alone and were confirmed in an independent validation cohort (n = 131). Our findings indicate that mediastinal bulk was associated with more favorable disease characteristics and improved OS in ASHL, and may be a surrogate of a more favorable biology.
Visual Abstract
Introduction
Bulky disease is commonly considered an adverse risk factor in lymphomas.1-5 In early-stage Hodgkin lymphoma (HL), its presence is sufficient to classify disease as ’unfavorable,’2 indicating the need for more intensive therapy.6-8 In advanced-stage Hodgkin lymphoma (ASHL), however, the significance of bulk remains unclear. In this setting, various definitions of bulk have been used in clinical trials and cohort reports. Mediastinal bulk (MB) is sometimes measured and recorded separately from other bulks. In some studies, MB was defined as a mediastinal/thoracic ratio >0.33 to 0.35 on chest radiographs. In other studies, bulk involving the mediastinum or other sites was defined as a maximal diameter on computed tomography (CT) scan that measured more than a given cutoff value (ranging from 5 to 10 cm).9-15 Additionally, studies have had varying conclusions regarding the prognostic significance of bulk in ASHL. Bulk was not associated with prognosis in the international prognostic score (IPS) analysis,16 the H89 trial,17 or the RATHL study.18 Conversely, bulk was associated with outcome in other trials.9,10,14,19
The prognostic significance of bulky disease may be complicated by confounding factors, and its presence may provide important insights into tumor biology. MB is more common in nodular sclerosis (NS) classical HL than in other subtypes of HL.20,21 Studies have demonstrated a close relationship in molecular signature between NS classical HL and primary mediastinal large B-cell lymphoma, another entity associated with bulky mediastinal involvement.22 Thus, the presence of MB in HL may provide biological information beyond a simple measure of tumor burden.
A preliminary cohort analysis in our institution revealed a complex association of size, location, and survival outcome in ASHL and generated the hypothesis that MB, differentiating from other bulky and nonbulky diseases, is associated with specific disease features and better survival. We undertook this retrospective multi-institutional study to investigate the significance of bulky disease in ASHL.
Methods
Study population
After institutional review board approval was obtained, data regarding ASHL patients treated at 6 institutions were collected retrospectively. The inclusion criteria were newly diagnosed, histologically proven classical HL or unclassified HL; age ≥15 years; Ann Arbor stage III or IV; treatment between January 2000 and December 2010; and availability of a CT or positron emission tomography (PET)/CT scan performed within 30 days prior to initiation of upfront therapy. Patients with nodular lymphocyte predominant HL or another concurrent malignancy were excluded.
Patients treated at 5 institutions (Memorial Sloan Kettering Cancer Center, University of Texas MD Anderson Cancer Center, Dana-Farber Cancer Institute, University of Turin, and Rambam Medical Center/Technion Israel Technical Institute) comprised the exploratory cohort. Patients treated at Princess Margaret Hospital were used as a validation cohort.
Data collection
Patient characteristics and outcomes.
Data regarding clinical characteristics, disease response to therapy, and patient outcomes were obtained from the medical records. The following patient and disease characteristics were recorded: age; sex; performance status according to the Eastern Cooperative Oncology Group (ECOG) scale; presence of B symptoms; Ann Arbor stage; serum lactate dehydrogenase level; histologic subtype; IPS; involvement of the bone marrow, spleen, liver, lung, bone, or other sites; and expression of CD20. Outcomes of interest included diagnosis with relapsed/refractory disease, death, and cause of death.
Image review and measurement of tumor size.
The maximal diameter of the largest site of disease was measured in the transverse plane by a local radiologist or radiation oncologist. The site of the largest lesion was recorded. Additionally, the maximum diameter of mediastinal disease was measured for patients who had a mediastinal involvement.
Response criteria
Treatment responses were assessed using standard criteria.23,24 Briefly, a complete remission (CR) was defined as no evidence of residual disease, including fluorodeoxyglucose negativity in subjects who underwent PET imaging. Additionally, patients were considered to have achieved a CR if their disease response was equivocal on posttreatment imaging but they did not require any additional therapy for ≥6 months after the completion of primary treatment. The definition of a partial remission (PR) was ≥50% reduction in sum of the product of the diameters of ≤6 of the largest dominant masses. The definition of stable disease was not meeting the criteria for a CR, PR, or progressive disease. The definition of progressive disease was the appearance of any new lesion or ≥50% increase in sum of the product of the diameters. Responses were assessed within 3 months after completion of upfront therapy.
Statistical evaluation
Overall survival (OS) was calculated from the date of diagnosis to the date of death. Progression-free survival (PFS) was measured from the date of diagnosis to the date of tumor progression/recurrence or death from any cause. When no event occurred, patients were censored at the time of last follow-up.
The association between maximum diameter and disease progression or death was assessed using the Cox proportional hazards regression model with penalized spline (P-spline) smoothing methods. For these analyses, the smoothHR package (R version 3.2.3, http://www.r-project.org/) was used to provide pointwise estimates of hazard ratios (HRs) as a function of tumor size.25 Results were plotted as logarithm HR (ln HR) curves, using the covariate value of 5 cm as reference.
Patient, disease, and treatment characteristics were compared using the Wilcoxon rank sum and Fisher’s exact tests for continuous and categorical variables, respectively. PFS and OS times were estimated using the Kaplan-Meier method and compared between groups using the log-rank test. Univariate hazard estimates were generated with unadjusted Cox proportional hazards models. A stepwise Cox proportional hazards model was built for multivariable survival analysis, with covariates that were significant on univariable analysis entered in a hierarchical fashion using forward selection (P < .1 for inclusion). These analyses were performed using IBM SPSS Statistics Version 22.0.
Results
Baseline characteristics and treatment
In all, 683 cases with complete data were collected from 5 institutions, constituting the exploratory cohort. Baseline characteristics are shown in Table 1. The median age was 34 years (range, 15-86 years). Disease was stage III in 303 patients (44%) and stage IV in 380 (56%). Maximum diameter measured <5 cm in 269 patients (39%), 5 to 10 cm in 278 patients (41%), 10 to 15 cm in 115 patients (17%), and >15 cm in 21 patients (3%).
Table 1.
Patient characteristics and treatment in the whole cohort and according to disease size and location
| Whole cohort (N = 683) | Group 1 (n = 269), Dmax <5 cm | Group 2 (n = 274), MB | Group 3 (n = 118), non-MB | Group 4 (n = 22), MB and non-MB | P | |
|---|---|---|---|---|---|---|
| Diameter , cm | ||||||
| <5 | 269 (39.4) | 269 (100) | 0 | 0 | 0 | .000 |
| 5-10 | 278 (40.7) | 0 | 165 (60.2) | 96 (81.4) | 17 (77.3) | |
| 10-15 | 115 (16.8) | 0 | 92 (33.6) | 21 (17.8) | 2 (9.1) | |
| ≥15 | 21 (3.1) | 0 | 17 (6.2) | 1 (0.8) | 3 (13.6) | |
| Sex | ||||||
| Male | 370 (54.2) | 145 (53.9) | 137 (50.0) | 74 (62.7) | 14 (63.6) | .103 |
| Female | 313 (45.8) | 124 (46.1) | 137 (50.0) | 44 (37.3) | 8 (36.4) | |
| Age , y | ||||||
| Median (range) | 34 (15-86) | 41 (15-86) | 28 (15-85) | 42.5 (15-81) | 23.5 (16-58) | .000 |
| Histologic type | ||||||
| NS | 462 (67.6) | 151 (56.1) | 227 (82.8) | 69 (58.5) | 15 (68.2) | .000 |
| MC | 111 (16.3) | 59 (21.9) | 21 (7.7) | 27 (22.9) | 4 (18.2) | |
| LR | 10 (1.5) | 8 (3.0) | 2 (0.7) | 0 | 0 | |
| LD | 8 (1.2) | 2 (0.7) | 4 (1.5) | 2 (1.7) | 0 | |
| Unclassified | 92 (13.5) | 49 (18.2) | 20 (7.3) | 20 (16.9) | 3 (13.6) | |
| CD20 | ||||||
| Positive | 93 (13.6) | 41 (15.2) | 32 (11.7) | 16 (13.6) | 4 (18.2) | .565 |
| Negative | 507 (74.2) | 194 (72.1) | 207 (75.5) | 88 (74.6) | 18 (81.8) | |
| UK | 83 (12.2) | 34 (12.6) | 35 (12.8) | 14 (11.9) | 0 | |
| BM | ||||||
| Positive | 82 (12.0) | 45 (16.7) | 10 (3.6) | 26 (22.0) | 1 (4.5) | .000 |
| Negative | 567 (83.0) | 211 (78.4) | 252 (92.0) | 85 (72.0) | 19 (86.4) | |
| UK | 34 (5.0) | 13 (4.8) | 12 (4.4) | 7 (5.9) | 2 (9.1) | |
| ECOG PS * | ||||||
| 0 | 361 (55.4) | 143 (57.0) | 151 (57.6) | 58 (49.2) | 9 (42.9) | .058 |
| 1 | 250 (38.3) | 86 (34.3) | 101 (38.5) | 51 (43.2) | 12 (57.1) | |
| ≥2 | 41 (6.3) | 22 (8.8) | 10 (3.8) | 9 (7.6) | 0 | |
| UK | 31 | 18 | 12 | 0 | 1 | |
| B symptoms * | ||||||
| No | 311 (45.6) | 133 (49.6) | 126 (46.0) | 45 (38.1) | 7 (31.8) | .132 |
| Yes | 362 (53.1) | 129 (48.1) | 146 (53.3) | 72 (61.0) | 15 (68.2) | |
| UK | 10 (1.3) | 7 (2.3) | 2 (0.7) | 1 (0.8) | 0 | |
| Spleen * | ||||||
| Positive | 236 (35.2) | 85 (32.9) | 89 (32.7) | 52 (44.1) | 10 (45.5) | .094 |
| Negative | 434 (64.8) | 173 (67.1) | 183 (67.3) | 66 (55.9) | 12 (54.5) | |
| UK | 13 | 11 | 2 | 0 | 0 | |
| Liver * | ||||||
| Positive | 73 (10.9) | 32 (12.4) | 26 (9.6) | 15 (12.7) | 0 | .241 |
| Negative | 597 (89.1) | 226 (87.6) | 246 (90.4) | 103 (87.3) | 22 (100) | |
| UK | 13 | 11 | 2 | 0 | 0 | |
| Lung * | ||||||
| Positive | 167 (24.9) | 49 (19.0) | 88 (32.4) | 24 (20.3) | 6 (27.3) | .003 |
| Negative | 503 (75.1) | 209 (81.0) | 184 (67.6) | 94 (79.7) | 16 (72.7) | |
| UK | 13 | 11 | 2 | 0 | 0 | |
| Bone * | ||||||
| Positive | 213 (31.8) | 84 (32.6) | 76 (27.9) | 45 (38.1) | 8 (36.4) | .228 |
| Negative | 457 (68.2) | 174 (67.4) | 196 (72.1) | 73 (61.9) | 14 (63.6) | |
| UK | 13 | 11 | 2 | 0 | 0 | |
| Stage | ||||||
| III | 303 (44.4) | 123 (45.7) | 119 (43.4) | 52 (44.1) | 9 (40.9) | .938 |
| IV | 380 (55.6) | 146 (54.3) | 155 (56.6) | 66 (55.9) | 13 (59.1) | |
| IPS * | ||||||
| 0-1 | 176 (26.1) | 75 (28.3) | 65 (24.0) | 28 (23.9) | 8 (36.4) | .159 |
| 2-3 | 343 (50.8) | 125 (47.2) | 154 (56.8) | 55 (47.0) | 9 (40.9) | |
| 4-6 | 156 (23.1) | 65 (24.5) | 52 (19.2) | 34 (29.1) | 5 (22.7) | |
| UK | 8 | 4 | 3 | 1 | 0 | |
| Treatment | ||||||
| Chemo | 533 (78.0) | 238 (88.5) | 182 (66.4) | 98 (83.1) | 15 (68.2) | .000 |
| CMT | 150 (22.0) | 31 (11.5) | 92 (33.6) | 20 (16.9) | 7 (31.8) | |
| Chemo regimen | ||||||
| ABVD | 530 (77.6) | 203 (74.4) | 202 (73.7) | 108 (91.5) | 17 (77.3) | .022 |
| Stanford V | 21 (3.1) | 6 (2.2) | 14 (5.1) | 0 | 1 (4.5) | |
| BEACOPP | 67 (9.8) | 28 (10.4) | 32 (11.7) | 4 (3.4) | 3 (13.6) | |
| BEACOPP + ABVD | 35 (5.1) | 17 (6.3) | 15 (5.5) | 2 (1.7) | 1 (4.5) | |
| Other | 30 (4.4) | 15 (5.6) | 11 (4.0) | 4 (3.4) | 0 |
Data are expressed as n or n (%), unless otherwise noted.
ABVD, doxorubicin, bleomycin, vinblastine, and dacarbazine; BEACOPP, bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone; BM, bone marrow; Chemo, chemotherapy; CMT, combined modality treatment; Dmax, maximal diameter; LD, lymphocyte depleted; LR, lymphocyte predominant; MC, mixed cellularity; NA, not available; PS, performance status; UK, unknown.
Missing values account for <5% and were thus not analyzed.
Upfront therapy consisted of chemotherapy alone in 533 patients (78%) and chemotherapy followed by radiotherapy (RT) (CMT) in 150 (22%). The most commonly used chemotherapy regimen was ABVD, which was administered to 530 patients (78%). 639 patients (94%) received at least 6 cycles of chemotherapy. Information about RT fields was available for 138 out of 150 patients treated with CMT. Of these, 89 patients (64%) were treated with total or subtotal lymphoid irradiation and 49 (35%) with localized irradiation. The median RT dose was 36.0 Gy (interquartile range, 30.6 to 40.0 Gy). Patients with large tumors (maximum diameter ≥5 cm) were more likely to receive RT (29% vs 12%, P < .001). Patients with PR to chemotherapy evaluated either by CT or PET were more likely to receive RT (supplemental Table 1).
Relationship between tumor bulk and survival
The median follow-up time was 59 months for all patients and 65 months for surviving patients. A total of 89 deaths and 146 diagnoses with relapsed/refractory disease were observed. The 5-year OS rate was 89% (95% confidence interval [CI], 86%-96%) and 5-year PFS was 84% (95% CI, 77%-89%).
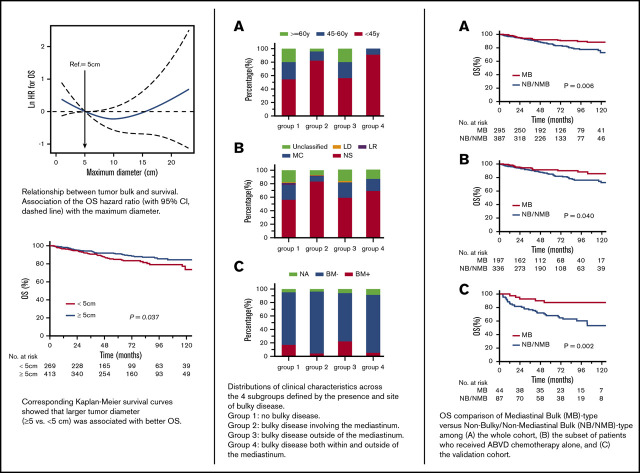
In a smoothHR analysis assessing the relationship between tumor bulk and PFS, the ln HR curve remained constant, indicating that there was no association between maximum diameter and PFS (Figure 1A). The significance of the slight rise at the distal end of the curve is unclear, because only 21 patients in the cohort (3%) had bulky disease measuring ≥15 cm. In agreement with these findings, Kaplan-Meier analyses showed no significant difference in PFS between patients with small vs large tumors based on multiple cutoff values (eg, cutoff value = 5 cm; 5-year PFS, 75% for <5 cm vs 73% for ≥5 cm, P = .9; Figure 1C).
Figure 1.
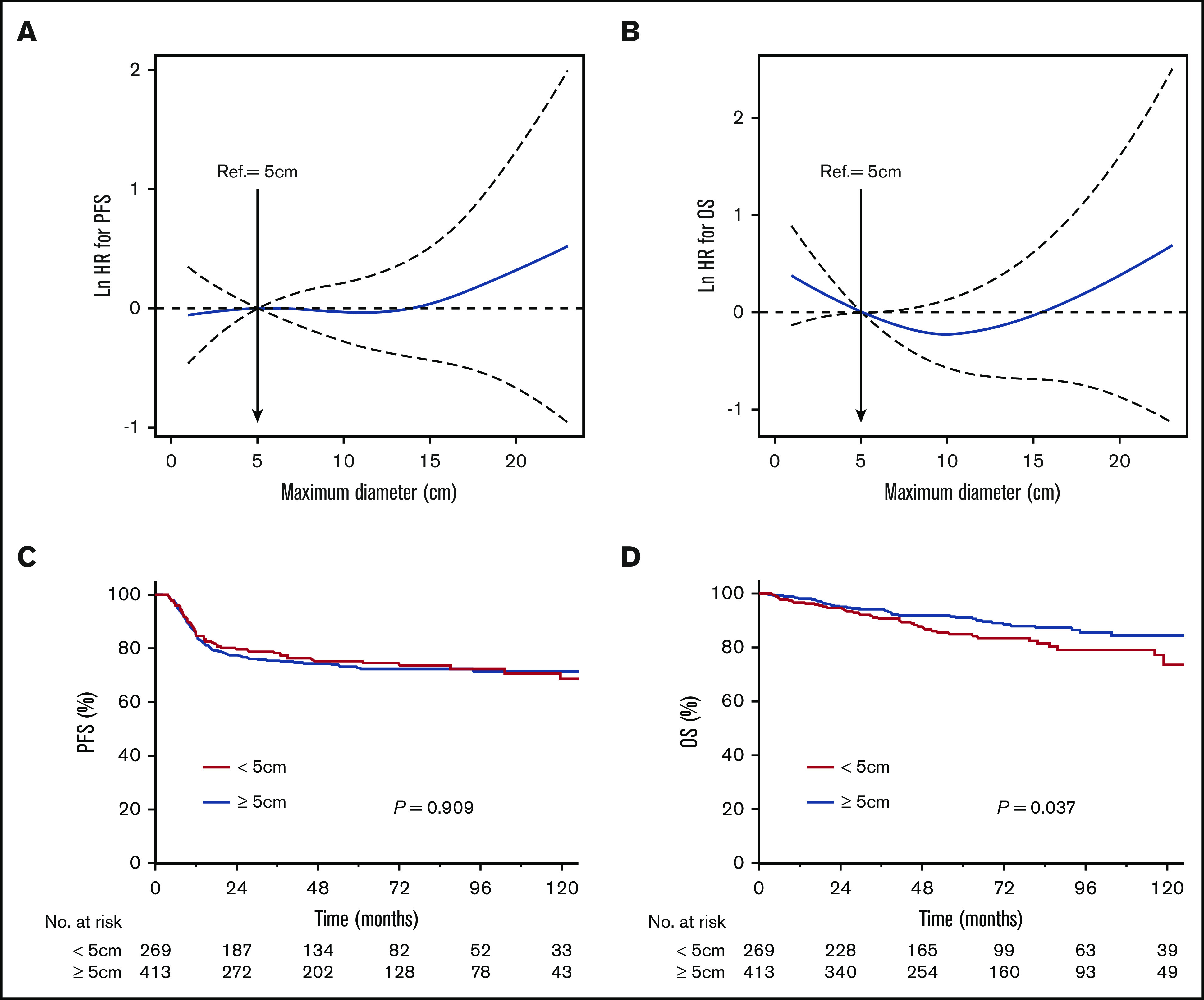
Relationship between tumor bulk and survival. Association of the estimated PFS (A) and OS (B) HR (with 95% CI, dashed line) with the maximum diameter. The nonlinear effect of maximum diameter on risk of relapse/death (A) and death (B) was modeled with a penalized spline expansion. Corresponding Kaplan-Meier survival curves show that larger tumor diameter (≥5 vs <5cm) had no effect on PFS (C) but was associated with better OS (D).
Conversely, a smoothHR analysis of maximum diameter and all-cause mortality revealed a U-shaped ln HR curve (Figure 1B), reflecting a complex relationship between tumor bulk and OS. The risk of death decreased with increasing tumor diameter until a value of ∼10 cm and then increased with tumor diameter. Based on Kaplan-Meier methods, a series of cutoff values for maximum diameter from 5 to 10 were used to validate the prognostic effect in OS. The larger maximum diameter group consistently showed better OS than the smaller maximum diameter group (cutoff value of 5 cm best distinguished 2 prognostic groups; Figure 1D, smallest P value). OS was significantly worse in patients with smaller tumor diameter (5-year OS, 85% for <5 cm vs 91% for ≥5 cm; P = .04).
Subgroups based on presence and site of bulk
Taking into consideration tumor size and location, 4 subgroups of patients were defined as follows: group 1, no bulky disease (maximum tumor diameter <5 cm); group 2, bulky disease (≥5 cm) involving the mediastinum; group 3, bulky disease (≥5 cm) outside of the mediastinum; and group 4, bulky disease (≥5 cm) both within and outside of the mediastinum
As shown in Table 1 and Figure 2, group 1 (no bulk) and group 3 (non-MB) had similar disease characteristics; however, these groups differed from groups 2 and 4 (MB) with respect to median age, histologic subtype, and bone marrow involvement.
Figure 2.
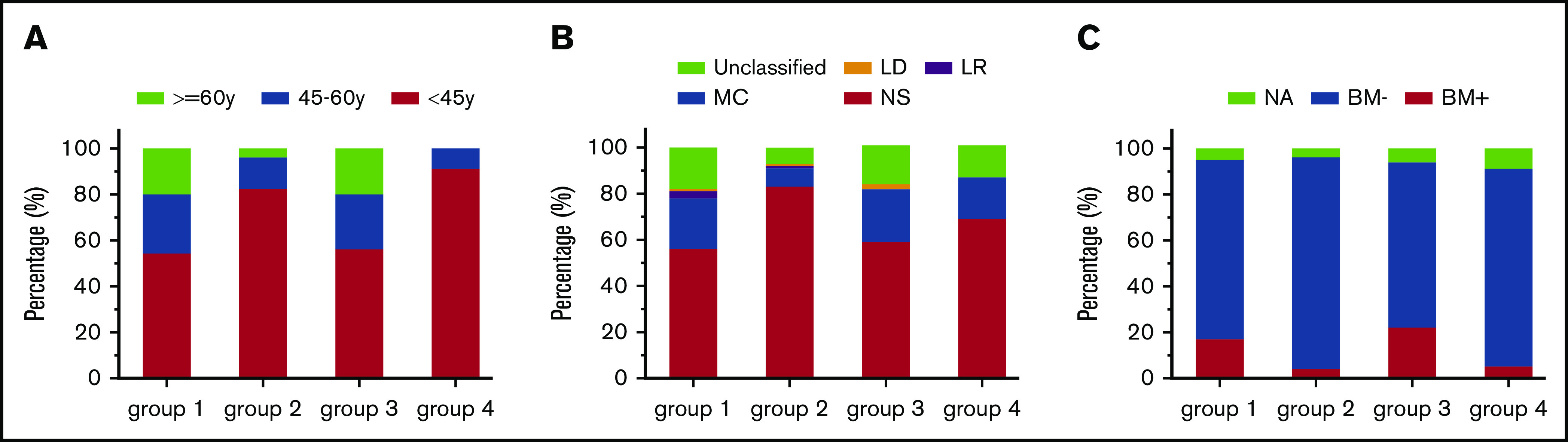
Distributions of clinical characteristics across the 4 subgroups defined by the presence and site of bulky disease. (A) Age. (B) Pathology subtype. (C) Bone marrow involvement. Group 1, no bulky disease (maximum tumor diameter <5 cm). Group 2, bulky disease (≥5 cm) involving the mediastinum. Group 3, bulky disease (≥5 cm) outside of the mediastinum. Group 4, bulky disease (≥5 cm) both within and outside of the mediastinum. LD, lymphocyte deleted; LR, lymphocyte rich.
Given the similarities between groups 1 and 3 and groups 2 and 4, 2 different types of ASHL were identified based on the presence of bulky (≥5 cm) mediastinal disease (with or without bulk at another site). Patients with MB-type ASHL (MB type, groups 2 and 4) had more favorable disease characteristics than those with nonbulky/non-MB type (NB/NMB type, groups 1 and 3), including younger age, more NS subtype, and less frequent bone marrow involvement (P < .001).
Outcomes of MB- vs NB/NMB-type ASHL
Disease response to chemotherapy and survival outcomes were compared between the MB- and NB/NMB-types (supplemental Table 2). The CR rate based on CT evaluation after initial chemotherapy was lower in MB-type patients than NB/NMB-type patients; however, CR rates based on PET evaluation were similar between the groups.
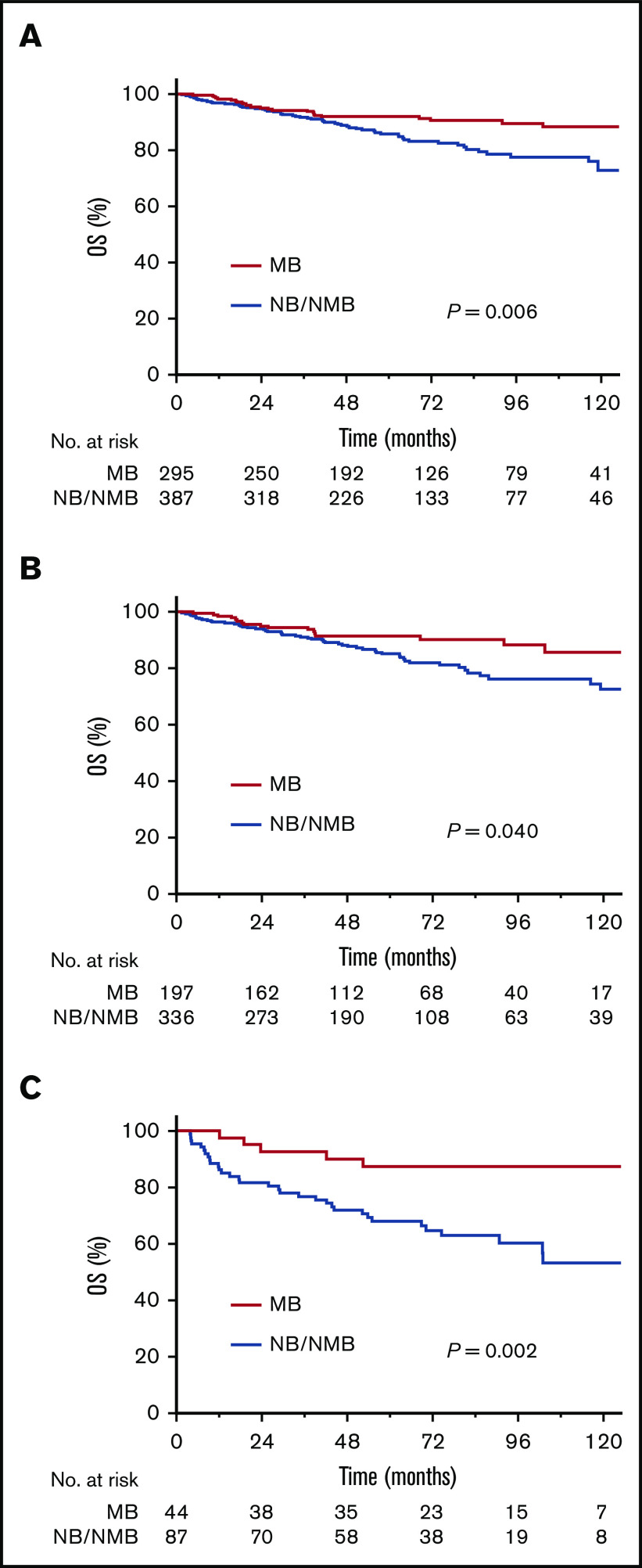
Relapse rates were similar for the 2 types. There was no statistically significant difference in PFS (5-year PFS, 74% for MB vs 74% for NB/NMB; P = .6). However, patients with MB type experienced significantly better OS (5-year OS, 92% for MB vs 86% for NB/NMB; P = .006) (Figure 3A). The cause of death analysis showed a higher, but not significant, proportion of disease-specific death (including HL and acute treatment toxicities) among MB-type compared to NB/NMB-type patients (19/27 [70%] vs 34/60 [57%]). There were 8 cases who died of a secondary malignancy (1 in MB and 7 in NB/NMB group) during follow-up.
Figure 3.
OS comparison of MB type vs NB/NMB type. (A) Whole cohort. (B) Subset of patients who received ABVD chemotherapy alone. (C) Validation cohort.
To address the potential confounding effect of treatment differences on survival outcomes, the subgroup of patients treated with chemotherapy alone (78% of the cohort) was analyzed separately. In this group, as in the complete cohort, the MB type experienced better OS than the NB/NMB type (Figure 3B).
Univariable Cox regression analyses revealed that MB type was associated with better OS than NB/NMB type (HR, 0.53; 95% CI, 0.34-0.84; P = .007), but not with PFS (HR, 0.91; 95% CI, 0.67-1.23; P = .547) (supplemental Table 3). The significant association of subtype with OS was not observed based in a multivariable analysis accounting for age, ECOG performance status, and B symptoms. Factors associated with OS in the multivariate Cox regression analysis were age and ECOG performance, and IPS was associated with PFS.
Validation of findings in an independent cohort
One hundred thirty one patients treated at Princess Margaret Hospital were analyzed as an independent validation cohort. Of these, 44 patients (34%) were classified as MB type. MB type was associated with younger patient age than NB/NMB type, with a median age of 26 years (range, 16-78 years) vs 53 years (range, 17-82 years; P < .001). In MB-type patients, bone marrow involvement was significantly less frequent (9% vs 26%, P = .03), whereas NS histologic subtype was more common (82% vs 52%, P = .01). Patients with MB type had similar PFS but significantly better OS than NB/NMB-type patients (5-year OS, 87% for MB vs 68% for NB/NMB, P = .002; PFS 78% for MB vs 63% for NM/NMB, P = .4; Figure 3C).
Bulk effect within MB and NB/NMB subgroups
The relationship between maximum diameter and OS in each subtype was evaluated by Kaplan-Meier survival analysis. Within either MB or NB/NMB type, survival seemed similar independent of disease size, with a series of cutoff values (supplemental Figure 1A-B, cutoff value 10 cm).
Discussion
This multicenter retrospective study aimed to investigate the effect of disease bulk on prognosis in ASHL in the CT era. Using Cox proportional hazards models with P-spline smoothing methods, we found that tumor size had no association with PFS and a nonlinear, U-shaped relationship with OS. Likewise, based on Kaplan-Meier methods, bulk was not associated with PFS, while smaller tumor size (<5 cm) was associated with worse OS. We hypothesize that improved OS was observed in patients with larger tumors, because bulky mediastinal disease was associated with favorable disease characteristics, such as younger age, NS histology, and less frequent bone marrow involvement. Based on these observations, a specific MB type of ASHL was proposed, defined by the presence of bulky mediastinal disease (with or without bulk elsewhere). In further analysis, no association between tumor size and OS was observed within either MB or NB/NMB type. These findings were validated in an independent cohort.
The prognostic role of bulk in ASHL has been a subject of controversy, and inconsistent definitions of bulk have been used across studies.9-15 Tumor size has rarely been analyzed as a continuous variable. In the current study, a flexible approach was used to assess the association of survival outcomes with tumor size as a continuous measure. Smooth ln HR curves enable visual exploration of an outcome’s association with a continuous variable, without prior assumption of a specific functional form, and therefore provide more information than binary splitting with certain cutoffs.25,26 To our knowledge, the current study represents the first study to evaluate the bulk’s continuous effect on treatment outcome. It is worth noting that the results of these analyses do not depend on the value used as reference point.27 Kaplan-Meier survival analyses were used to validate the association between bulk and survival outcomes.
Contrary to previous recognition, survival curves showed a better OS for the bulk group than the nonbulk group. The nonlinear, U-shaped curve depicting tumor size and OS suggests a complex association. These may be explained, at least in part, by confounding factors. In this cohort, the site of the bulky disease was important prognostically. Specifically, the presence of MB, with or without bulk at another site, characterized a specific type of ASHL with unique disease characteristics and better OS. With bulk location information, the U-shaped hazard spline of OS for the complete cohort could be divided into 2 straight lines, reflecting 2 different types of effect with disease size on survival: MB type and NB/NMB type.
An MB type in classical ASHL has never been defined previously; however, results of other studies support the close association of bulk mediastinal disease and certain disease features. For example, in the EORTC 2088410 and UK LY0914 trials, patients who experienced a PR to chemotherapy defined by CT were more likely to have bulky mediastinal disease, young age, and NS subtype and were less likely to have bone marrow involvement. Work from the German Hodgkin Study Group and Memorial Sloan Kettering Cancer Center found that elderly patients were more likely to have mixed cellularity subtype and less likely to have mediastinal masses or NS subtype.21,28 In a review of the biology and classification of HL, NS classical HL was shown to affect more young adults than other subtypes of classical HL, accounting for the early peak in HL diagnoses in Western populations.20 These data are consistent with our results. The causes of death were further analyzed and showed a higher percentage of non–disease-specific deaths in the NB/NMB group. The non–disease-specific deaths may be at least partially attributed to the poorer crude OS in the NB/NMB group. Because of the distinct features of both disease and patient characteristics in MB, results of this subgroup should be reported separately in clinical studies whenever possible. In other lymphoma types, anatomic location of disease may reflect the tumor’s biology and molecular features.29,30 The bulky mediastinal disease that characterizes the MB type of ASHL suggests a possible link with primary mediastinal B-cell lymphoma.31,32 The molecular similarities between primary mediastinal B-cell lymphoma and NS classical HL support the potential relationship between these 2 entities.22,33
A major strength of the current study is the large cohort size. The robustness of better disease features and survival in MB type was confirmed by an independent cohort and subgroup analysis. However, this study does have limitations. First, given its retrospective nature and the heterogeneous treatments administered, it is possible that differences in the therapy influenced the conclusions; for example, patients with bulky disease were more likely to receive RT. To address the potential confounding effect of therapy, we analyzed separately the patients who received ABVD chemotherapy only. In this subgroup, we made the same observations as in the complete cohort, including the improved OS associated with MB type on univariate analysis. As a second limitation, bulk was defined by a single measurement of tumor diameter on axial CT slices. This measure may not reflect total disease burden as accurately as 3-dimensional features, such as metabolic tumor volume.34 On the other hand, a single measurement of tumor diameter, as used in this study, is easier to apply in daily clinical practice.
In conclusion, in this multicenter retrospective study of ASHL, a complex relationship between tumor diameter and survival was identified. Bulky mediastinal involvement was characterized by younger patient age, higher rates of NS subtype, less frequent bone marrow involvement, and better OS than NB/NMB disease. Our findings highlight the complexity of prognostic effect based on tumor size. Attention must be paid not only to the tumor diameter but also to the location of bulky disease and other clinical features. Future studies are warranted to explore the genomic and molecular features that define MB-type ASHL.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
This research was funded in part through the National Institutes of Health, National Cancer Institute Cancer Center Support Grant P30 CA008748, the Connecticut Cancer Foundation, and the Lymphoma Foundation.
Footnotes
For data sharing, e-mail the corresponding author, Joachim Yahalom (yahalomj@mskcc.org).
Authorship
Contribution: S.Q. and J.Y. designed the study, analyzed the data, and wrote the paper; J.Y. contributed to the study coordination; S.M. wrote portions of the manuscript; and all authors contributed to data collection and interpretation and approved the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Joachim Yahalom, Department of Radiation Oncology, Memorial Sloan Kettering Cancer Center, 1275 York Ave, New York, NY 10065; e-mail: yahalomj@mskcc.org.
References
- 1.Barrington SF, Mikhaeel NG, Kostakoglu L, et al. Role of imaging in the staging and response assessment of lymphoma: consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J Clin Oncol. 2014;32(27):3048-3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kriz J, Mueller RP, Mueller H, et al. Large mediastinal tumor mass as a prognostic factor in Hodgkin’s lymphoma. Is the definition on the basis of a chest radiograph in the era of CT obsolete? Strahlenther Onkol. 2012;188(11):1020-1024. [DOI] [PubMed] [Google Scholar]
- 3.Held G, Murawski N, Ziepert M, et al. Role of radiotherapy to bulky disease in elderly patients with aggressive B-cell lymphoma. J Clin Oncol. 2014;32(11):1112-1118. [DOI] [PubMed] [Google Scholar]
- 4.Ng AK, Dabaja BS, Hoppe RT, Illidge T, Yahalom J. Re-examining the role of radiation therapy for diffuse large B-cell lymphoma in the modern era. J Clin Oncol. 2016;34(13):1443-1447. [DOI] [PubMed] [Google Scholar]
- 5.Federico M, Bellei M, Marcheselli L, et al. Follicular lymphoma international prognostic index 2: a new prognostic index for follicular lymphoma developed by the international follicular lymphoma prognostic factor project. J Clin Oncol. 2009;27(27):4555-4562. [DOI] [PubMed] [Google Scholar]
- 6.Eich HT, Diehl V, Görgen H, et al. Intensified chemotherapy and dose-reduced involved-field radiotherapy in patients with early unfavorable Hodgkin’s lymphoma: final analysis of the German Hodgkin Study Group HD11 trial. J Clin Oncol. 2010;28(27):4199-4206. [DOI] [PubMed] [Google Scholar]
- 7.Kumar A, Burger IA, Zhang Z, et al. Definition of bulky disease in early stage Hodgkin lymphoma in computed tomography era: prognostic significance of measurements in the coronal and transverse planes. Haematologica. 2016;101(10):1237-1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.von Tresckow B, Plütschow A, Fuchs M, et al. Dose-intensification in early unfavorable Hodgkin’s lymphoma: final analysis of the German Hodgkin Study Group HD14 trial. J Clin Oncol. 2012;30(9):907-913. [DOI] [PubMed] [Google Scholar]
- 9.Fabian CJ, Mansfield CM, Dahlberg S, et al. Low-dose involved field radiation after chemotherapy in advanced Hodgkin disease. A Southwest Oncology Group randomized study. Ann Intern Med. 1994;120(11):903-912. [DOI] [PubMed] [Google Scholar]
- 10.Aleman BM, Raemaekers JM, Tirelli U, et al. ; European Organization for Research and Treatment of Cancer Lymphoma Group . Involved-field radiotherapy for advanced Hodgkin’s lymphoma. N Engl J Med. 2003;348(24):2396-2406. [DOI] [PubMed] [Google Scholar]
- 11.Engert A, Diehl V, Franklin J, et al. Escalated-dose BEACOPP in the treatment of patients with advanced-stage Hodgkin’s lymphoma: 10 years of follow-up of the GHSG HD9 study. J Clin Oncol. 2009;27(27):4548-4554. [DOI] [PubMed] [Google Scholar]
- 12.Federico M, Luminari S, Iannitto E, et al. ; HD2000 Gruppo Italiano per lo Studio dei Linfomi Trial . ABVD compared with BEACOPP compared with CEC for the initial treatment of patients with advanced Hodgkin’s lymphoma: results from the HD2000 Gruppo Italiano per lo Studio dei Linfomi Trial. J Clin Oncol. 2009;27(5):805-811. [DOI] [PubMed] [Google Scholar]
- 13.Hoskin PJ, Lowry L, Horwich A, et al. Randomized comparison of the stanford V regimen and ABVD in the treatment of advanced Hodgkin’s Lymphoma: United Kingdom National Cancer Research Institute Lymphoma Group Study ISRCTN 64141244. J Clin Oncol. 2009;27(32):5390-5396. [DOI] [PubMed] [Google Scholar]
- 14.Johnson PW, Sydes MR, Hancock BW, Cullen M, Radford JA, Stenning SP. Consolidation radiotherapy in patients with advanced Hodgkin’s lymphoma: survival data from the UKLG LY09 randomized controlled trial (ISRCTN97144519). J Clin Oncol. 2010;28(20):3352-3359. [DOI] [PubMed] [Google Scholar]
- 15.Fermé C, Sebban C, Hennequin C, et al. Comparison of chemotherapy to radiotherapy as consolidation of complete or good partial response after six cycles of chemotherapy for patients with advanced Hodgkin’s disease: results of the groupe d’études des lymphomes de l’Adulte H89 trial. Blood. 2000;95(7):2246-2252. [PubMed] [Google Scholar]
- 16.Hasenclever D, Diehl V. A prognostic score for advanced Hodgkin’s disease. International Prognostic Factors Project on Advanced Hodgkin’s Disease. N Engl J Med. 1998;339(21):1506-1514. [DOI] [PubMed] [Google Scholar]
- 17.Brice P, Colin P, Berger F, et al. ; Groupe d’Etude des Lymphomes de l’Adulte . Advanced Hodgkin disease with large mediastinal involvement can be treated with eight cycles of chemotherapy alone after a major response to six cycles of chemotherapy: a study of 82 patients from the Groupes d’Etudes des Lymphomes de l’Adulte H89 trial. Cancer. 2001;92(3):453-459. [DOI] [PubMed] [Google Scholar]
- 18.Johnson P, Federico M, Kirkwood A, et al. Adapted treatment guided by interim PET-CT scan in advanced Hodgkin’s lymphoma. N Engl J Med. 2016;374(25):2419-2429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Borchmann P, Haverkamp H, Diehl V, et al. Eight cycles of escalated-dose BEACOPP compared with four cycles of escalated-dose BEACOPP followed by four cycles of baseline-dose BEACOPP with or without radiotherapy in patients with advanced-stage hodgkin’s lymphoma: final analysis of the HD12 trial of the German Hodgkin Study Group. J Clin Oncol. 2011;29(32):4234-4242. [DOI] [PubMed] [Google Scholar]
- 20.Mani H, Jaffe ES. Hodgkin lymphoma: an update on its biology with new insights into classification. Clin Lymphoma Myeloma. 2009;9(3):206-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Straus DJ, Gaynor JJ, Myers J, et al. Prognostic factors among 185 adults with newly diagnosed advanced Hodgkin’s disease treated with alternating potentially noncross-resistant chemotherapy and intermediate-dose radiation therapy. J Clin Oncol. 1990;8(7):1173-1186. [DOI] [PubMed] [Google Scholar]
- 22.Savage KJ, Monti S, Kutok JL, et al. The molecular signature of mediastinal large B-cell lymphoma differs from that of other diffuse large B-cell lymphomas and shares features with classical Hodgkin lymphoma. Blood. 2003;102(12):3871-3879. [DOI] [PubMed] [Google Scholar]
- 23.Cheson BD, Pfistner B, Juweid ME, et al. ; International Harmonization Project on Lymphoma . Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25(5):579-586. [DOI] [PubMed] [Google Scholar]
- 24.Cheson BD, Fisher RI, Barrington SF, et al. ; United Kingdom National Cancer Research Institute . Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059-3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meira-Machado L, Cadarso-Suárez C, Gude F, Araújo A. smoothHR: an R package for pointwise nonparametric estimation of hazard ratio curves of continuous predictors. Comput Math Methods Med. 2013;2013:745742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Çetinyürek Yavuz A, Lambert P. Smooth estimation of survival functions and hazard ratios from interval-censored data using Bayesian penalized B-splines. Stat Med. 2011;30(1):75-90. [DOI] [PubMed] [Google Scholar]
- 27.Cadarso-Suarez C, Meira-Machado L, Kneib T, Gude F. Flexible hazard ratio curves for continuous predictors in multi-state models: an application to breast cancer data. Stat Model. 2010;10(3):291-314. [Google Scholar]
- 28.Engert A, Ballova V, Haverkamp H, et al. ; German Hodgkin’s Study Group . Hodgkin’s lymphoma in elderly patients: a comprehensive retrospective analysis from the German Hodgkin’s Study Group. J Clin Oncol. 2005;23(22):5052-5060. [DOI] [PubMed] [Google Scholar]
- 29.Jaffe ES, Harris NL, Stein H, Isaacson PG. Classification of lymphoid neoplasms: the microscope as a tool for disease discovery. Blood. 2008;112(12):4384-4399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dunleavy K, Pittaluga S, Maeda LS, et al. Dose-adjusted EPOCH-rituximab therapy in primary mediastinal B-cell lymphoma. N Engl J Med. 2013;368(15):1408-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Savage KJ. Primary mediastinal large B-cell lymphoma. Oncologist. 2006;11(5):488-495. [DOI] [PubMed] [Google Scholar]
- 33.Rosenwald A, Wright G, Leroy K, et al. Molecular diagnosis of primary mediastinal B cell lymphoma identifies a clinically favorable subgroup of diffuse large B cell lymphoma related to Hodgkin lymphoma. J Exp Med. 2003;198(6):851-862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ceriani L, Martelli M, Zinzani PL, et al. Utility of baseline 18FDG-PET/CT functional parameters in defining prognosis of primary mediastinal (thymic) large B-cell lymphoma. Blood. 2015;126(8):950-956. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.