Abstract
Hypoglycemia is an important and harmful complication of Diabetes Mellitus (DM) that often occurs in inpatient or outpatient settings. Hypoglycemia can be divided into two types, i.e. primary hypoglycemia when hypoglycemia is the main diagnosis for admission, whereas secondary hypoglycemia if hypoglycemia occurs during hospitalization. Hypoglycemia during hospitalization or secondary hypoglycemia may arise from various risk factors, such as advanced age, comorbid diseases, type of diabetes, previous history of hypoglycemia, body mass index, hyperglycemia therapy given, as well as other risk factors such as inadequate glucose monitoring, unclear or unreadable physician instructions, limited health personnel, limited facilities, prolonged fasting and incompatibility of nutritional intake and therapy administered. Hypoglycemia can lead to medical and non-medical impacts, such as increased mortality, cardiovascular disorders, cerebrovascular disorders, and increased health care costs and length of stay. The incidence of inpatient hypoglycemia can actually be prevented by controlling modifiable risk factors and also giving education about hypoglycemia to patients and health workers. We performed a literature research in Pubmed, EBSCOhost, and Scopus to review the possible risk factors for inpatient hypoglycemia. Eleven studies were retrieved. We presented the result of these studies as well as a brief overview of the epidemiology, pathophysiology, impact and preventive strategy.
Keywords: Diabetes, Insulin, Metabolism, Metabolic disorder, Endocrinology, Hypoglycemia, Mortality, Risk factors, Hospitalization, Inpatient
Diabetes; Insulin; ; Metabolism; Metabolic disorder; Endocrinology; Hypoglycemia, Mortality, Risk factors, Hospitalization, Inpatient.
1. Introduction
Hypoglycemia is a complication of Diabetes Mellitus (DM) that often occurs and causes harmful effects for patients with diabetes. Hypoglycemia, based on the American Diabetes Association, is defined when blood glucose levels reach <70 mg/dL [1]. Basically, when hypoglycemia happens, counter-regulatory mechanisms begin to occur, and everyone has a different threshold [2]. The prevalence of severe hypoglycemia in type 1 diabetic patients is 0.2–3.2 episodes per patient per year, whereas in type 2 diabetic patients 0.1–0.7 per patient per year [3]. Mild hypoglycemia is often difficult to recognize, because diabetic patients did not realize or did not remember the hypoglycemic episodes, especially if the incidence of hypoglycemia has been experienced for more than a week [4]. Hypoglycemia was further classified as primary and secondary hypoglycemia. Primary hypoglycemia if it was the primary cause of hospital admission, and secondary if it occurred during hospitalization (inpatient hypoglycemia) [5]. Inpatient hypoglycemia may arise from various risk factors, individual risk factors and also institutional risk factors, such as advanced age, comorbid diseases, type of diabetes, previous history of hypoglycemia, body mass index, aggressive hyperglycemia therapy, inadequate glucose monitoring, unclear or unreadable physician instructions, limited health personnel, limited facilities, prolonged fasting and incompatibility of nutritional intake and therapy administered [1, 2, 6]. We aimed to systematically review the available studies regarding the risk factors of inpatient hypoglycemia, to provide a brief overview of inpatient hypoglycemia, including the epidemiology, pathophysiology, impact and preventive strategy.
2. Methods
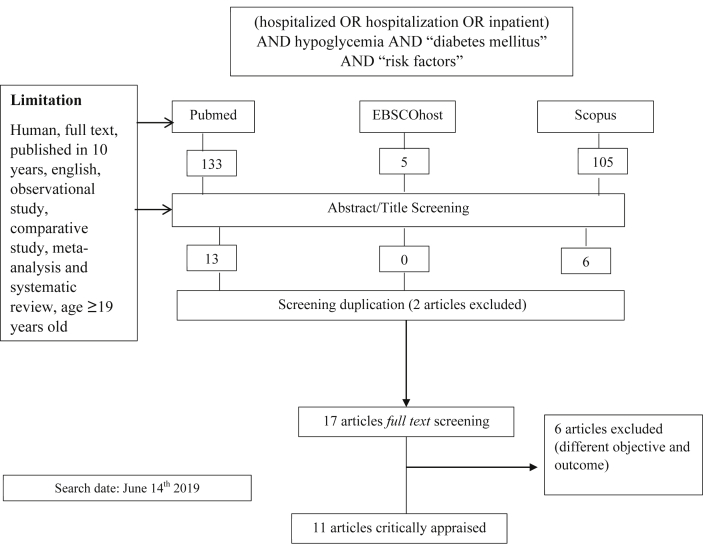
We performed a literature search in Pubmed, EBSCOhost, and Scopus on June 14th 2019 using the keywords (hospitalized OR hospitalization OR inpatient) AND hypoglycemia AND “diabetes mellitus” AND “risk factors”. The search was limited to English literatures that had human with age ≥19 years old as the subjects, published within 10 years. We sought to identify all the observational study, comparative study, meta-analysis and systematic review and 17 studies were identified. The study selection and critical appraisal was conducted by two reviewers to assess the studies' eligibility. Six studies were excluded because of having different objective and outcome, hence 11 studies were included. The selected articles were critically reviewed by using Newcastle Ottawa Scale (NOS). The relevant flowchart is depicted in Figure 1.
Figure 1.
Flowchart of the study's method.
3. Result
From the 11 selected articles, one article is a cross-sectional study, three case-control studies, five retrospective cohort studies, and two prospective cohort studies. Some articles stated the risk factors of inpatient hypoglycemia, and the rests told about the impact of the hypoglycemic events (Table 1). And from New Castle Ottawa Scale that had converted to Agency for Healthcare Research and Quality (AHRQ) standard, most of the studies had a good quality, only one study had a fair quality (Table 2).
Table 1.
Description of selected studies.
| No. | Author | Years | Total subjects | Design (observation time) | Results |
|---|---|---|---|---|---|
| 1. | Akirov et al | 2018 | 5,301 patients | Prospective cohort (2011–2013) | The risk factors for inpatient hypoglycemia were age (OR 1.02 (1.01–1.02)), malignancy (OR 1.43 (1.1–1.9)), chronic renal failure (OR 1.42 (1.1–1.85)), cerebrovascular disease (OR 1.33 (1.02–1.73)) and also diabetes duration (OR 1.03 (1.02–1.03)), HbA1C (OR 1.06 (1.02–1.1)), insulin treatment (OR 3.94 (3.11–4.98)) [7]. |
| 2. | Curkendall et al | 2008 | 271,323 patients | Retrospective cohort study | Diabetic patients that had inpatient hypoglycemia had higher charges (38.9%), longer lengths of stay (3.0 days), higher mortality (odds ratio, 1.07; 95% CI, 1.02–1.11) [8]. |
| 3. | Borzi et al | 2016 | 3,167 patients | Cross-sectional | Hypoglycemia occurred in 19.4% of patients treated according to the insulin sliding-scale method versus 11.4% of patients treated with basal bolus (p < 0.01). More patients with hypoglycemia received sulfonylurea (28.3% versus 20.6%, p < 0.001). Significantly longer length of hospital-stay and increased in-hospital mortality were found in the group with hypoglycemia (12.7 ± 10.9 versus 9.6 ± 6.5 days; 8.8% versus 4.8%, p < 0.01) [9]. |
| 4. | Gianchandani et al | 2018 | 150 diabetic patients receiving hemodialysis | Retrospective cohort study | At least one glucose value less than 70 mg/dl was observed in 51% of hemodialysis patients, less than 54 mg/dl in 28%, and less than 40 mg/dl in 11%. A majority (61%) of all hypoglycemic episodes occurred in the 24 h prior to a hemodialysis session. Hypoglycemia more likely to occur in type 1 diabetic patient compare to type 2 diabetic patient (82.1% vs 42.6% p 0.003) [10]. |
| 5. | Gomez-Huelgas et al | 2015 | 5,447,725 patients | Retrospective cohort study (1997–2010) | There were 92.591 (1.7%) discharges with primary hypoglycemia and 154.510 (2.8%) with secondary hypoglycemia. Among patients discharged with a secondary diagnosis of hypoglycemia, 9.4% died compared with 6.6% of those without secondary hypoglycemia. Patients discharged with a diagnosis of secondary hypoglycemia had a longer length of stay than patients discharged without that diagnosis (12.04 [13.40] vs. 9.90 [11.34], p < 0.001) [5]. |
| 6. | Hsu et al | 2013 | 77,611 patients | Retrospective cohort study (1998–2009) | There were 1,844 hypoglycemic events (500 inpatients and 1,344 outpatients) among the 77.611 patients. Mild and severe hypoglycemia had a higher hazard ratios (HRs) for cardiovascular diseases (HR 2.09 (95% CI 1.63–2.67)), all-cause hospitalization (2.51 (2.00–3.16)), and total mortality (2.48 (1.41–4.38)). The comorbidities independently associated with hypoglycemia were hypertension (HR 1.75 95% CI 1.57–1.96); atrial fibrillation (1.96 (1.24–3.11)); liver cirrhosis (1.71 (1.17–2.48)); renal disease (3.26 (2.76–3.86)); mental disease (1.50 (1.30–1.73)); cancer (2.73 (2.12–3.50)); stroke (2.84 (2.31–3.48)); and CHD (2.04 (1.65–2.51)) [11]. |
| 7. | Ignaczak A et al | 2017 | 200 patients that had continuous intravenous insulin therapy | Prospective cohort study (2.5 ± 1.1 days) | Hypoglycemia was noted in 48% of patients with type 1 diabetes and in 20% of those with type 2 diabetes (p < 0.001), and most often in the second day of the administration of continuous intravenous insulin therapy [12]. |
| 8. | Kagansky et al | 2003 | 526 geriatric patients | Case-control study | The risk factors of hypoglycemia in elderly patients were sepsis (OR 6.4 95% CI 2.3–17.3), albumin level (OR 4.3 95% CI 2.9–6.5), malignancy (OR 2.6 95% CI 1.1–6.2), insulin secretagogues or insulin treatment (OR 1.9 95% CI 1.2–3.2), alkaline phosphatase (OR 1.7 95% CI 1.2–2.5), female sex (OR 1.7 95% CI 1.2–2.6), creatinine (OR 1.3 95% CI 1–1.6) [13]. |
| 9. | Maynard et al | 2006 | 130 patients | Case-control study | From multivariate analysis, the significant risk factors for hypoglycemia were nutritional interruption/discordance (OR 12.09 95% CI 1.23–118.05), prior hypoglycemic day (OR 31.18 95% CI 2.9–333.6), and insulin as outpatient treatment (OR 15.57 95% CI 1.39–174.8)6 |
| 10. | Nirantharakumar et al | 2012 | 6,347 patients | Retrospective cohort study (2007–2010) | The adjusted length of stay was increased by 1.51 (95% CI 1.35–1.68) times in mild to moderate hypoglycemia group, and 2.33 (95% CI 1.91–2.84) times in severe hypoglycemia group when compared with those without a hypoglycemic episode. The adjusted odds ratio for mortality was 1.62 (95% CI 1.16–2.27) in mild to moderate hypoglycemia group and 2.05 (95% CI 1.24–3.38) in severe hypoglycemia group in comparison with the non hypoglycemic group [14]. |
| 11. | Quilliam et al | 2011 | 1,339 cases and 13,390 controls | Nested case-control study | In multivariable modeling, previous emergency department hypoglycemia visits (odds ratio [OR] 9.48; 95% CI, 4.95–18.15) and previous outpatient hypoglycemia visits (OR 7.88; 95% CI, 5.68–10.93) were strongly predictive of inpatient hypoglycemia admission [15]. |
Table 2.
New Castle Ottawa Scale and Quality Assessment using AHRQ standard.
| No. | Study | Selection | Comparability | Outcome/Exposure | Total | Quality |
|---|---|---|---|---|---|---|
| 1. | Akirov et al | 4 | 2 | 2 | 8/9 | Good |
| 2. | Curkendall et al | 4 | 2 | 2 | 8/9 | Good |
| 3. | Borzi et al | 4 | 1 | 3 | 8/10 | Good |
| 4. | Gianchandani et al | 3 | 2 | 2 | 7/9 | Good |
| 5. | Gomez et al | 4 | 2 | 2 | 8/9 | Good |
| 6. | Hsu et al | 4 | 0 | 2 | 6/9 | Good |
| 7. | Ignaczak et al | 3 | 0 | 2 | 5/9 | Good |
| 8. | Kagansky et al | 2 | 2 | 3 | 7/9 | Good |
| 9. | Maynard et al | 3 | 1 | 3 | 7/9 | Good |
| 10. | Nirantharakumar et al | 4 | 0 | 2 | 6/9 | Good |
| 11. | Quilliam et al | 2 | 2 | 3 | 7/9 | Fair |
4. Discussion
4.1. Hypoglycemia classification
Based on the International Hypoglycemia Study Group, hypoglycemia can be classified into three types:
-
1.
Hypoglycemia alert value, if the blood glucose level is ≤ 70 mg/dL
-
2.
Clinically significant hypoglycemia, if blood glucose level is < 54 mg/dL
-
3.
Severe hypoglycemia, there is no specific limit of blood glucose levels, but causes cognitive impairment and requires external help to recover from this condition [16].
Another classification of hypoglycemia is based on the place where hypoglycemia occurs. Hypoglycemia is said to be primary hypoglycemia when hypoglycemia is the main cause for the patient to be admitted, while secondary hypoglycemia is hypoglycemia that occurs during the hospitalization or in some studies it was defined as inpatient hypoglycemia [5].
4.2. Inpatient hypoglycemia
Based on data from the National Diabetes Inpatient Audit in the United Kingdom in 2012, The prevalence of inpatient hypoglycemia was 22% and 11% of these events were severe incidence of hypoglycemia [17]. Based on a study conducted by Gomez et.al., inpatient hypoglycemia had higher prevalence compared to primary hypoglycemia (2.8% vs 1.7%). It was possibly caused by a tendency to maintain tighter glycemic control in hospitalized patient. The prevalence of inpatient hypoglycemia in Gomez et al, was lower than previous study (range from 7,7%–22%) because of the different hypoglycemia definition used by each study and also the different method for data collection. In Gomez et al they used the clinical data recorded in an administrative database, while others based on a point-of-care glucose measurement [5].
Hypoglycemia that occurs during hospitalization is further differentiated into spontaneous and iatrogenic hypoglycemia. Spontaneous hypoglycemia can occur in diabetic patients with multiple organ failure, malnutrition, and a history of drugs consumption which are the predisposing factors for hypoglycemia, while iatrogenic hypoglycemia results from overly aggressive treatment of hyperglycemia accompanied by a failure of the body to respond to a decrease in blood glucose levels, known as HAAF (hypoglycemia-associated autonomic failure) [1, 18].
HAAF is a phenomenon that can be found in type 1 diabetes, patients with severe comorbid diseases, old age, and patients with a history of recurrent hypoglycemia [1]. In type 1 DM there is an absolute disruption of β cells function so that there is no suppression of insulin secretion and increased glucagon secretion under hypoglycemic conditions [4]. In patients with a history of recurrent hypoglycemia there will be a decrease in blood glucose levels that trigger the counter-regulatory mechanism so that hypoglycemia can occur more severe and is not realized. In this condition there is an increased risk of 25 times greater to experience severe hypoglycemia [18, 19]. Hypoglycemia which is not realized basically is a reversible condition if the incidence of hypoglycemia can be avoided for 2–3 weeks [20].
Decreased catecholamine hormone response during hypoglycemia condition, in patient with HAAF will basically reduce the impact of catecholamine cardiotoxicity [21], but the ACCORD study (Action to control cardiovascular disease) and the ADVANCE study (Action in Diabetes and Vascular Disease)) found that strict blood glucose control, that will induce recurrent episodes of hypoglycemia that lead to HAAF, did not reduce the incidence of cardiovascular complications in diabetic patients, on the contrary will increase mortality due to cardiovascular events [22].
4.3. The risk factors of inpatient hypoglycemia
Hypoglycemia that occurs during hospitalization was caused by various risk factors, such as individual factors, management factors, and institutional factors. Individual factors that play a role in the occurrence of inpatient hypoglycemia were patient's age, severe comorbid diseases (sepsis, impaired renal function, malignancy, hypoalbuminemia [1], anemia, liver failure, and heart failure [2]), other endocrine disorders, such as insufficiency adrenal, growth hormone deficiency, hyperthyroidism or hypothyroidism [23], types and duration of diabetes [1], pregnancy [2], low body mass index [6], and improvement in patient's clinical status [23].
The management factors that can cause hypoglycemia are overly aggressive hyperglycemia therapy, changes in patient dietary intake and prolonged fasting [1], while the institutional factors that play a role are inadequate monitoring of blood glucose levels, discrepancies between dietary intake and hyperglycemia therapy, unreadable or unclear medical instruction, lack of coordination and communication between relevant departments, insufficient education for health workers, and inadequate number of health workers [2].
Quilliam et al, in a nested case control study, stated that previous emergency department hypoglycemia visits during six months period and previous outpatient hypoglycemia were the strong predictive factors for inpatient hypoglycemic event (OR 9.48; 95% CI 4.95–18.15 and OR 7.88; 95% CI 5.68–10.93) [15].
Hypoglycemic episodes are more common in patients with kidney disease. Its incidence is higher due to a decrease in the process of gluconeogenesis that 40% of it occurred in the kidney, decreased insulin degradation in peripheral tissues, decreased insulin clearance through the kidneys, anorexia and autonomic neuropathy. It is also difficult to control blood glucose level in diabetic patient with end-stage renal failure, due to metabolic acidosis, and uremia which increases insulin resistance, and also decreases insulin resistance and increases insulin degradation in post-dialysis patients [10, 24].
Hypoglycemia also occurs in diabetic patients with liver function disorders. The liver plays a role in carbohydrate metabolism, gluconeogenesis and glycogenolysis. Impaired liver function ultimately contributes to an increased risk of hypoglycemia [25]. Based on a study conducted by Kagansky et al, an increased risk of hypoglycemia can also occur in septic conditions (Odds Ratio (OR) 6.4 95% CI 2.3–17.3), malignancy (OR 2.6 95% IK 1.1–6.2), and decreased albumin levels (OR 4.3 95% IK 2.9–6.5) [13].
Pediatric and elderly patients are said to be the most vulnerable patients to hypoglycemia because of the decreased ability to recognize signs and symptoms of hypoglycemia and also failure to communicate their needs. In elderly patients there is also a decrease in counter-regulatory hormonal response and loss of autonomic nerve responses during hypoglycemia [16]. Akirov et al in a cohort study of 5301 patients found that, patients that had inpatient hypoglycemia tend to be older (mean age 74 ± 14 and 75 ± 13, respectively) compared to patients without hypoglycemia (72 ± 12 years) [26].
Hypoglycemia was also found in the use of oral anti-diabetic therapy. Hypoglycemia more commonly occurred in the use of sulfonylureas. In the United Kingdom Prospective Diabetes Study (UKPDS) study, it was said that at the early years we used glibenclamide, the incidence of mild hypoglycemia reached 31% [27]. The incidence of hypoglycemia in third generation sulfonylureas (glimepiride, glipizide, and glicazide) was found to be lower when compared to glibenclamide. This is possibly occur due to different half time of the drugs, and also other related factors, such as different effects on insulin sensitivity [28].
The use of insulin has long been reported to increase the risk of hypoglycemia in diabetic patients. The incidence of hypoglycemia is reported reaching 25% in patients who have used insulin for more than 5 years [28]. A prospective cohort study by Rudijanto et.al. in Indonesia stated that 100% of type 1 diabetic patients who used insulin have experienced hypoglycemic episodes and 99.4% of type 2 DM patients who used insulin have one episode of hypoglycemia [29]. DIAMOND study stated that hypoglycemia events was more frequent in patients that had sliding scale insulin therapy compare to basal bolus therapy (19.4% vs 11.4% p < 0,01) [9]. Ignaczak et al in a prospective cohort study that include 200 patients found that 24% patients had hypoglycemia episode after received continuous intravenous insulin therapy and it was more frequent happened in type 1 diabetic patients [12].
Administration of insulin therapy, especially for diabetic patients who are hospitalized must be accompanied by strictly monitored blood glucose levels. The following is a local guideline in Indonesia that is used to monitor blood glucose levels in hospitalized patients (adjusted to the condition and resources in Indonesia) (Table 3) [30].
Table 3.
Blood glucose monitoring for hospitalized patients [30].
| Intravenous insulin infusion | Fixed dose insulin therapy (subcutaneous insulin regimen) | Correctional dose insulin therapy(subcutaneous insulin regimen) |
|---|---|---|
| Evaluate blood glucose level every hour in the first 3 h Furthermore, blood glucose is monitored according to the aggressiveness of administering insulin |
Blood glucose curves (before breakfast, lunch, and dinner) are monitored 2–3 times a week | Blood glucose is monitored periodically in one day, for example every 6 h or before eating |
Strictly monitored blood glucose level is one of the strategies to prevent hypoglycemia in diabetic patients. The American Diabetes Association (ADA) and the American Association of Clinical Endocrinologists (AACE) recommended to monitor blood glucose levels every hour for administration of intravenous insulin infusion critically ill patients, and after the target of blood glucose (140–180 mg/dL) has been reached, it can be checked every 2–4 h [31].
4.4. The impact of inpatient hypoglycemia
Hypoglycemia can increase mortality rate in diabetic patients. Low blood glucose level was associated with the occurrence of prolonged QT interval and re-entrant arrhythmia that can cause sudden cardiac death [1, 2]. Lee AK et al, in a prospective cohort analysis of 1209 patients, found that after the episode of severe hypoglycemia, the 3-year cumulative incidence of coronary heart disease was 10.8% and of mortality was 28.3%. Severe hypoglycemia was associated with cardiovascular mortality (HR 1.64, 95% CI 1.27–3.2) [32]. The surge of sympathetic activity during hypoglycemic episodes has been suggested to be the underlying mechanism leading to destabilization of atherosclerotic plaques [11].
It is said in a study that patients who had experienced hypoglycemia would have a higher 7% risk of mortality compared to patients without a history of hypoglycemia [2]. DIAMOND study also said that the mortality during hospitalization was found more frequent in diabetic patients with hypoglycemia (8.8% vs 4.8% p < 0,01) [9].
Hypoglycemia can also induce cerebral ischemia due to the augmented blood flow to the frontal lobe cortex, the most vulnerable part of the brain in the episode of hypoglycemia and this condition will persist even after the patient has reached normoglycemia resulting in disruption of autoregulation blood flow mechanism. As a result, the risk of cerebral ischemia during any condition of hemodynamic stress is increased [4]. Hsu et al. found that diabetic patients with a history of hypoglycemia had higher rates of stroke compared to patients without a previous history of hypoglycemia (69.05 vs 27.97 per 1000 people per year) [11]. A cohort study conducted by Shih C J et al. also found that hypoglycemia would increase the risk of dementia [16].
In addition to medical effects, hypoglycemia also causes non-medical effects, such as increased health-costs and prolonged length of stay [8, 14]. A study conducted on more than 100,000 diabetic patients found that patients who experienced hypoglycemia during hospitalization will be hospitalized three days longer than patients without hypoglycemia, and in this study it was also found that the health-cost will increase up to 39% [8]. DIAMOND study also stated that longer duration of hospitalization found in diabetic patients that had hypoglycemia episode during hospitalization (12.7 ± 10.9 vs 9.6 ± 6.5 p < 0,01) [9].
4.5. The preventive strategies of inpatient hypoglycemia
Inpatient hypoglycemia is actually a preventable condition by performing some actions, such as appropriate monitoring blood glucose level, ensuring adequate dietary intake, adjusting the dose insulin administered with nutritional intake or patients' clinical condition, using basal bolus insulin regimen rather than oral anti-diabetic agent for hospitalized patient [33] and also recognizing precipitating factors of inpatient hypoglycemia as we have discussed before.
There are some precipitating factors for inpatient hypoglycemia that make physicians should pay more attention, such as the patients that had insulin or sulfonylurea therapy, received IV insulin therapy to treat high potassium level, had multiple organ failure and/or sepsis [33], had a history of hypoglycemia [34], and also had any other non-diabetic drugs that can induce hypoglycemia [33], such as quinolone, clarithromycin, metronidazole, trimethoprim-sulfamethoxazole, quinine, pentamidine, β-blocker, angiotensin converting enzyme inhibitor, angiotensin receptor blocker [4, 23], and tramadol [35]. In addition, daily evaluation of blood glucose level and adjustment insulin dose should be applied to the patients that had improvement in clinical condition, and also to them that had high dose steroid therapy in a short period of time.
Educating patients, family members, and also hospital staffs about how to recognize the risk factors, symptoms and treatment for hypoglycemia could be an alternative way to reduce the incidence of inpatient hypoglycemia [36]. Kilpatrick et al in a prospective cohort-intervention study in 2011 had found that alert process (divided the subjects into high risk and low risk of hypoglycemia), when combined with a good collaboration of educated and trained nurses-physician, resulted in a significant decrease by 68% in the rate of severe hypoglycemia in hospital [34].
5. Conclusion
Inpatient hypoglycemia is a complication of diabetes that cannot be ignored because it will increase morbidity and mortality in diabetic patients. This complication can be prevented by controlling modifiable risk factors and also providing education about hypoglycemia, both for health workers and patients and families.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This work was supported by the Universitas Indonesia International Indexed Publication Grants for Student's Final Projects (PITTA) number NKB-0547/UN2.R3.1/HKP.05.00/2019.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Carey M., Boucai L., Zonszein J. Impact of hypoglycemia in hospitalized patients. Curr. Diabetes Rep. 2013;13(1):107–113. doi: 10.1007/s11892-012-0336-x. [DOI] [PubMed] [Google Scholar]
- 2.Rubin D.J., Golden S.H. Hypoglycemia in non-critically ill, hospitalized patients with diabetes: evaluation, prevention, and management. Hosp. Pract. 2013;41(1):109–116. doi: 10.3810/hp.2013.02.1016. [DOI] [PubMed] [Google Scholar]
- 3.UK Hypoglycemia Study Group Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50:1140–1147. doi: 10.1007/s00125-007-0599-y. [DOI] [PubMed] [Google Scholar]
- 4.Bonaventura A., Montecucco F., Dallegri F. Update on strategies limiting iatrogenic hypoglycemia. Endocr Connect. 2015;4(3):R37–45. doi: 10.1530/EC-15-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gómez-Huelgas R., Guijarro-Merino R., Zapatero A., Barba R., Guijarro-Contreras A., Tinahones F. The frequency and impact of hypoglycemia among hospitalized patients with diabetes: a population-based study. J. Diabet. Complicat. 2015;29(8):1050–1055. doi: 10.1016/j.jdiacomp.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Maynard G.A., Huynh M.P., Renvall M. Iatrogenic inpatient Hypoglycemia : risk factors , treatment , and prevention. Diabetes Spectr. 2008;21:241–247. [Google Scholar]
- 7.Akirov A., Amitai O., Iraqi H.M., Cohen T.D., Shochat T., Eizenberg Y. Predictors of hypoglycemia in hospitalized patients with diabetes mellitus. Intern. Emerg. Med. 2018;13(3):343–350. doi: 10.1007/s11739-018-1787-0. [DOI] [PubMed] [Google Scholar]
- 8.Curkendall S.M., Natoli J.L., Alexander C.M., Nathanson B.H., Haidar T.D.R. Economic and clinical impact of inpatient diabetic hypoglycemia. Endocr. Pract. 2009;15(4):302–312. doi: 10.4158/EP08343.OR. [DOI] [PubMed] [Google Scholar]
- 9.Borzi V., Frasson G., Di Lillo R., Gerloni G., Augello G.G., Ceriello G.G.A. Risk factors for hypoglycemia in patients with type 2 diabetes, hospitalized in internal medicine wards: findings from the FADOI-DIAMOND study. Diabetes Res. Clin. Pract. 2016 doi: 10.1016/j.diabres.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 10.Gianchandani R.Y., Neupane S.H.M. Hypoglycemia in hospitalized hemodialysis patients with diabetes: an observational study. J. Diabet. Sci. Technol. 2018;12(1):33–38. doi: 10.1177/1932296817747620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsu P.F., Sung S.H., Cheng H.M., Yeh J.S., Liu W.L., Chan W.L. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: a nationwide population-based study. Diabetes Care. 2013;36(4):894–900. doi: 10.2337/dc12-0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ignaczak A., Czupryniak L. Risk factors for hypoglycaemia in in-patients with diabetes treated with continuous insulin intravenous infusion. Clin. Diabetol. 2017;6(2):41–47. [Google Scholar]
- 13.Kagansky N., Levy S., Rimon E., Cojocaru L., Fridman A., Ozer Z. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch. Intern. Med. 2008;163:1825–1829. doi: 10.1001/archinte.163.15.1825. [DOI] [PubMed] [Google Scholar]
- 14.Nirantharakumar K., Marshall T., Kennedy A., Narendran P., Hemming K., Coleman J.J. Short Report : treatment Hypoglycaemia is associated with increased length of stay and mortality in people with diabetes who are hospitalized. Diabet. Med. 2012:445–448. doi: 10.1111/dme.12002. [DOI] [PubMed] [Google Scholar]
- 15.Quilliam B.J., Simeone J.C., Ozbay A.B. Risk factors for hypoglycemia-related hospitalization in patients with type 2 Diabetes : a nested case – control study. Elsevier HS J. 2011;33(11):1781–1791. doi: 10.1016/j.clinthera.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 16.Riddle M.C., Bakris G., Blonde L., Boulton A.J.M., D’Alessio D., de Groot M.G.E. Standards of medical care in Diabetes 2018. Diabetes Care. 2018;41:555–562. [Google Scholar]
- 17.Centre H., SCI . 2012. National Diabetes Inpatient Audit di UK. [Google Scholar]
- 18.Cryer P.E. Chapter 21: hypoglycemia in diabetes: pathophysiological mechanisms and diurnal variation. Prog. Brain Res. 2006;153(6):361–365. doi: 10.1016/S0079-6123(06)53021-3. [DOI] [PubMed] [Google Scholar]
- 19.Longo D.L., Kasper D.L., Jameson J.L., Fauci A.S., Hauser S.L.L.J., editors. Harrison’s Principles of Internal Medicine. eighteenth ed. The McGraw-Hill Comp.; 2012. hypoglycemia. [e-book] [Google Scholar]
- 20.Sequest E.R., Anderson J., Childs B., Cryer P., Dagogo-jack S., Fish L. Hypoglycemia and diabetes: a report of a workgroup of the American diabetes association and. The Endocrin. Soc. 2013;36:1384–1395. doi: 10.2337/dc12-2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seaquest E.R., Miller M.E., Bonds D.E., Feinglos M., Goff D.C., Peterson K. The Impact of frequent and unrecognized hypoglycemia on mortality in the ACCORD study. Diabetes Care. 2012;35:409–414. doi: 10.2337/dc11-0996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dluhy R.G., McMahon G.T. Intensive glycemic control in the ACCORD and ADVANCE trials. N. Engl. J. Med. 2008;358(24):2630–2633. doi: 10.1056/NEJMe0804182. [DOI] [PubMed] [Google Scholar]
- 23.Hulkower R.D., Pollack R.M., Zonszein J. Understanding hypoglycemia in hospitalized patients. Diabetes Manag. 2014;4:165–176. doi: 10.2217/DMT.13.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alsahli M.G.J. Hypoglycemia in patients with diabetes and renal disease. J. Clin. Med. 2015;4(5):948–964. doi: 10.3390/jcm4050948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gangopadhyay K.K.S.P. Consensus statement on dose modifications of antidiabetic agents in patients with hepatic impairment. Indian J. Endocr. Metab. 2017;21:341–354. doi: 10.4103/ijem.IJEM_512_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akirov A., Grossman A., Shochat T., Shimon I. Mortality among hospitalized patients with hypoglycemia: insulin related and noninsulin related. J. Clin. Endocrinol. Metab. 2017;102(2):416–424. doi: 10.1210/jc.2016-2653. [DOI] [PubMed] [Google Scholar]
- 27.UKPDS UK prospective study of therapies of maturity onset diabetes: I. Effect of diet, sulphonylurea, insulin or biguanide therapy on fasting glucose and bodyweight over one year. Diabetologia. 1983;24:404–411. [PubMed] [Google Scholar]
- 28.Amiel S.A., Dixon T., Mann R., Jameson K. Hypoglycaemia in type 2 diabetes. Diabet. Med. 2008;25(3):245–254. doi: 10.1111/j.1464-5491.2007.02341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rudijanto A., Saraswati M.R., Yunir E., Kumala P., Puteri H.H.S., Mandang V.V.V. Indonesia cohort of IO HAT study to evaluate diabetes management , control, and complications in retrospective and prospective periods among insulin-treated patients with type 1 and type 2 diabetes. Acta Med. Indones. 2018;50(1):26–37. [PubMed] [Google Scholar]
- 30.PERKENI . PB. Perkeni; Jakarta: 2015. Terapi insulin pada pasien diabetes mellitus; pp. 19–28. [Google Scholar]
- 31.Kelly J.L. Continuous insulin Infusion : when , where , and how. Diabetes Spectr. 2014;27(3):218–223. doi: 10.2337/diaspect.27.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee A.K., Warren B., Lee C.J., Mcevoy J.W., Matsushita K., Huang E.S. The association of severe hypoglycemia with incident cardiovascular events and mortality in adults with type 2 diabetes. Diabetes Care. 2018;41:104–111. doi: 10.2337/dc17-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Griffing K.L. Hypoglycemia prevention in hospital patients: a quality improvement project to prevent severe and recurrent hypoglycemia. Clin. Diabet. J. 2016;14(4):193–199. doi: 10.2337/cd15-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilpatrick C.R., Elliott M.B., Pratt E., Schafers S.J., Blackburn M.C., Heard K. Prevention of inpatient hypoglycemia with a real-time informatics alert. J. Hosp. Med. 2014;9(10):621–626. doi: 10.1002/jhm.2221. [DOI] [PubMed] [Google Scholar]
- 35.Senthilkumaran S., Ananth C., Menezes R.G.T.P. Tramadol-induced hypoglycemia: an unusual adverse effect. J. Anaesthesiol. Clin. Pharmacol. 2017;33(4):554–555. doi: 10.4103/0970-9185.222512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tomky D. Detection , prevention , and treatment of hypoglycemia in the hospital. Diabetes Spectr. 2005;18(1):39–44. [Google Scholar]