Abstract
Aluminum accumulation, glutathione (GSH) and malondialdehyde (MDA) concentrations as well as catalase (CAT) and superoxide dismutase (SOD) activities were determined in erythrocytes and brain and liver homogenates of BALB/c mice treated with Al3+ (7.5 mg/kg/day (0.15 LD50) as AlCl3 (37.08 mg/kg/day), whereas HCl (30.41 mg/kg/day) was used as Cl− control, the treatments were performed for 21 days, i.p., in the presence and absence of rosmarinic acid (0.2805 mg/kg/day (0.05 LD50), 21 days, i.g.) or carvacrol (0.0405 mg/kg/day (0.05 LD50), 21 days, i.g.). The treatment with AlCl3 increased GSH concentration in erythrocytes only slightly and had no effect on brain and liver homogenates. Rosmarinic acid and carvacrol strongly increased GSH concentration in erythrocytes but decreased it in brain and liver homogenates. However, AlCl3 treatment led to Al accumulation in mice blood, brain, and liver and induced oxidative stress, assessed based on MDA concentration in the brain and liver. Both rosmarinic acid and carvacrol were able to counteract the negative Al effect by decreasing its accumulation and protecting tissues from lipid peroxidation. AlCl3 treatment increased CAT activity in mice brain and liver homogenates, whereas the administration of either rosmarinic acid or carvacrol alone or in combination with AlCl3 had no significant effect on CAT activity. SOD activity remained unchanged after all the treatments in our study. We propose that natural herbal phenolic compounds rosmarinic acid and carvacrol could be used to protect brain and liver against aluminum induced oxidative stress leading to lipid peroxidation.
Keywords: aluminum toxicity, rosmarinic acid, carvacrol, oxidative stress, lipid peroxidation, brain, liver
1. Introduction
Aluminum (Al) is the third most abundant chemical element found in nature and the most abundant metal in the Earth′s crust [1]. It is widely used in the medical, food, and pharmaceutical industries as a part of vaccines, for water purification, for packaging, and in agriculture, thus resulting in human exposure [2]. The toxicity of different Al forms depends on their physical behavior and relative solubility in water [1]. After delivery to target tissues, elevated Al3+ concentrations induce cytotoxicity which is a consequence of oxidative damage due to Al3+-induced formation of oxygen radicals [1,3,4,5,6,7]. Aluminum can cause nephrotoxicity [8], cardiotoxicity [9,10], hematotoxicity [11], hepatotoxicity [12], and bone and lung toxicity [9,10]. Aluminum easily crosses the blood–brain barrier and can accumulate in different regions of the brain [13,14], inducing neurotoxicity and contributing to neuronal death in neurodegenerative diseases such as Alzheimer′s disease and Parkinson′s disease [15,16,17]. Due to frequent human exposure to Al and the possible role of Al in neurodegenerative disorders, it is important to find substances that could potentially counteract the toxic effects.
There is accumulating evidence that natural herbal remedies and dietary compounds could have potential therapeutic use in the treatment of numerous neurodegenerative diseases [18]. Several studies have demonstrated that polyphenols and endogenous compounds could alleviate neuronal oxidative damage and inflammation [19,20] and counteract metabolic disorders associated with these diseases [21,22]. Rosmarinic acid is the ester of caffeic acid and 3,4-dihydroxyphenyl-lactic acid and one of the most abundant phenols in many well-known herbs of the Lamiaceae family [23], such as rosemary, sage, basil, mint, and thyme. Among the simple phenolic compounds, rosmarinic acid has been shown to possess very strong antioxidant activity [24]. Rosmarinic acid was demonstrated to have neuroprotective properties, attenuate oxidative stress and neuronal cell death in vitro [25,26,27], and to diminish inflammatory responses in experimental models of an ischemic stroke [18,28]. Carvacrol is a monoterpenoid phenol and a major constituent of oregano oil, which is widely used as a salad dressing, and numerous other essential oils [29]. Carvacrol exhibits strong antioxidative and hydrophobic properties associated with the substituted aromatic ring and hydrophilic properties associated with the phenolic OH group [29,30]. It has been demonstrated to exert antioxidative, anti-inflammatory, antibacterial, antiviral, antifungal, antiprotozoal, anticarcinogenic, antidiabetic, antinociceptive, cardioprotective, and neuroprotective activities [31,32,33]. Rosmarinic acid and carvacrol could be readily available potential remedies to counteract the toxic effects of Al. Therefore, in this study, we investigated the effects of rosmarinic acid and carvacrol on oxidative stress and antioxidant enzyme activity in Al-treated mice.
2. Results
We used in our study experimental setup where BALB/c mice were treated intraperitoneally with Al3+ 7.5 mg/kg/day [0.15 LD50] for 21 days, which is considered a very low dose of Al. During such exposure, we have not observed neither mice behavioral changes nor the changes at histological level. The main purpose of our study was to assess the first possible toxicological effects of low dose Al3+ exposure that usually occur at subcellular levels.
2.1. Cl− Controls
AlCl3 was used as the source of Al3+ in the study. To determine whether the effects observed are related to the Cl−, equimolar Cl− controls were performed for all endpoints studied, and the results showed no difference between control and HCl treatments.
2.2. Effects of AlCl3, Rosmarinic Acid, and Carvacrol Treatment on the Amount of Al in Mice Blood and Brain and Liver Tissues
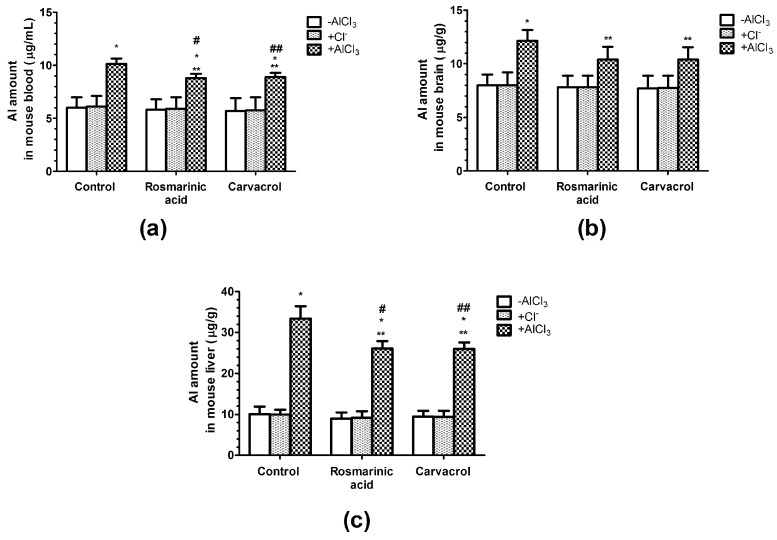
The amount of Al in mice blood was significantly increased by 69% compared to the vehicle control (6 µg/mL) in the case of AlCl3, whereas the administration of rosmarinic acid or carvacrol in the presence of AlCl3 decreased its effect by 30% (Figure 1a).
Figure 1.
Influence of AlCl3, rosmarinc acid, and carvacrol on the amount of Al in mice blood (a) and brain (b) or liver (c) tissues. (n = 9, * p < 0.001 vs. control, ** p < 0.001 vs. AlCl3, # p < 0.01 vs. rosmarinic acid in the absence of AlCl3, ## p < 0.01 vs. carvacrol in the absence of AlCl3).
After AlCl3 treatment, the amount of Al in mice brain and liver (Figure 1b,c) was significantly increased by 52.2% and 230% accordingly, compared to the vehicle control (8 µg/g in brain and 10 µg/g in liver). The administration of rosmarinic acid or carvacrol in the presence of AlCl3 decreased its effect by 40% in brain and by 30% in liver. (Figure 1b,c).
2.3. Effects of AlCl3, Rosmarinic Acid, and Carvacrol Treatment on the Concentration of Gsh in Mice Erythrocytes and Brain and Liver Homogenates
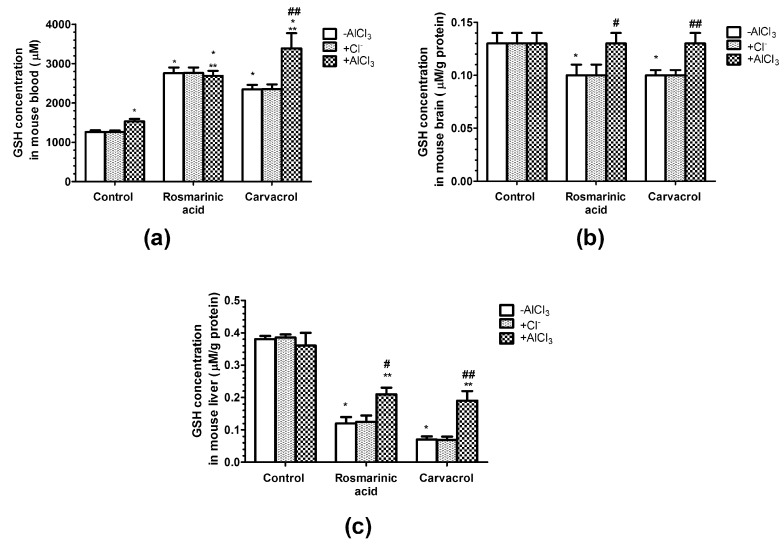
The concentration of the intracellular antioxidant GSH in mice erythrocytes was significantly increased by 22% in the case of AlCl3, by 219% in the case of rosmarinic acid, and by 87% in the case of carvacrol administration compared with the vehicle control (Figure 2a). In mice treated with both AlCl3 and rosmarinic acid, the significant increase in erythrocyte GSH concentration remained similar to that in the case of rosmarinic acid administration alone (214%). In mice treated with both AlCl3 and carvacrol, the increase in erythrocyte GSH concentration was significantly augmented by 270% compared with the vehicle control (Figure 2a).
Figure 2.
Influence of aluminum ions, rosmarinc acid, and carvacrol on the concentration of glutathione (GSH) in mice erythrocytes (a) and brain (b) or liver (c) homogenates. (n = 9, * p < 0.001 vs. control, ** p < 0.001 vs. AlCl3, # p < 0.01 vs. rosmarinic acid in the absence of AlCl3, ## p < 0.01 vs. carvacrol in the absence of AlCl3).
However, the different effects of AlCl3, rosmarinic acid, and carvacrol on GSH concentration was observed in mice brain and liver homogenates (Figure 2b,c). Rosmarinic acid and carvacrol treatment significantly decreased the GSH concentration in mice brain homogenates by 30%, whereas AlCl3 treatment alone or in combination with rosmarinic acid or carvacrol had no effect compared with the vehicle control (Figure 2b). AlCl3 treatment had no effect on GSH concentration in mice liver homogenates, whereas rosmarinic acid administration significantly decreased it by 68% alone or by 45% together with AlCl3 compared with the vehicle control (Figure 2c). A similar pattern was observed in the case of carvacrol administration—it significantly decreased the GSH concentration in mice liver homogenates by 92% alone or by 50% in combination with AlCl3 compared with the vehicle control (Figure 2c).
2.4. Effects of AlCl3, Rosmarinic Acid, and Carvacrol Treatment on the Concentration of MDA in Mice Erythrocytes and Brain and Liver Homogenates
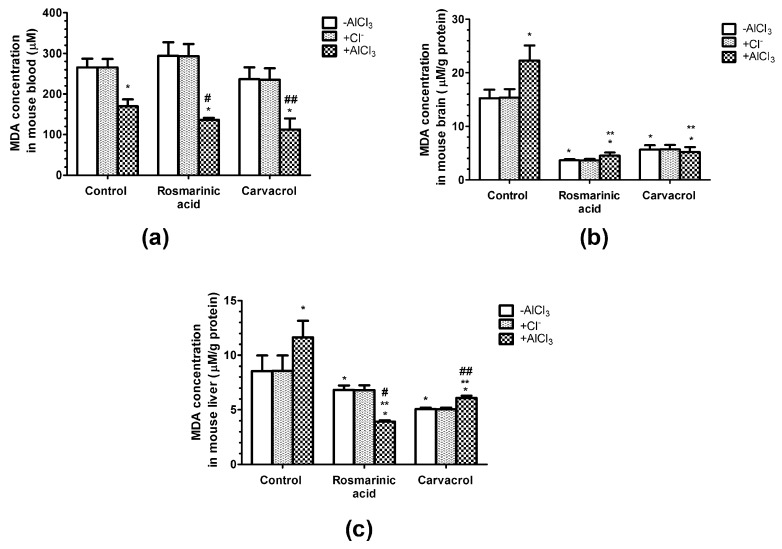
The concentration of the final product of lipid peroxidation (MDA) was significantly decreased by 36%, 48%, and 67% in mice erythrocytes treated with AlCl3 alone or in combination with rosmarinic acid and carvacrol, respectively, compared with the vehicle control (Figure 3a).
Figure 3.
Influence of aluminum ions, rosmarinc acid, and carvacrol on the concentration of malondialdehyde (MDA) in mice erythrocytes (a) and brain (b) or liver (c) homogenates. (n = 9, * p < 0.001 vs. control, ** p < 0.001 vs. AlCl3, # p < 0.001 vs. rosmarinic acid in the absence of AlCl3, ## p < 0.001 vs. carvacrol in the absence of AlCl3).
In mice brain homogenates, AlCl3 administration significantly increased the concentration of MDA by 46%, whereas rosmarinic acid administration alone or in combination with AlCl3 significantly decreased it by 76% and 70%, respectively, compared with the vehicle control (Figure 3b). Similarly, mice treated with carvacrol alone or in combination with AlCl3 showed significant decreases in MDA concentration by 63% and 66%, respectively (Figure 3b). Comparable effects of AlCl3, rosmarinic acid, and carvacrol treatments were observed in mice liver homogenates (Figure 3c). AlCl3 significantly increased the MDA concentration by 36%, whereas rosmarinic acid and carvacrol significantly decreased it by 20% and 41%, respectively, when administered alone and by 54% and 29%, respectively, in combination with AlCl3 (Figure 3c).
2.5. Effects of AlCl3, Rosmarinic Acid, and Carvacrol Treatment on the Activities of CAT and SOD in Mice Brain and Liver Homogenates
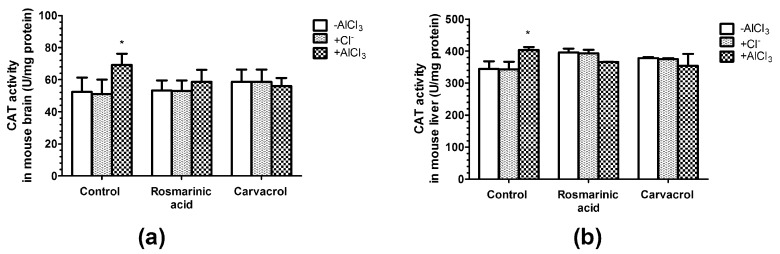
CAT activity was observed to be 32% higher (p < 0.05) in brain homogenates (Figure 4a) and 17% higher (p < 0.05) in liver homogenates (Figure 4b) among AlCl3-treated mice.
Figure 4.
Influence of aluminum ions, rosmarinc acid, and carvacrol on the activity of catalase (CAT) in mice brain (a) and liver (b) homogenates (n = 9, * p < 0.05 vs. control).
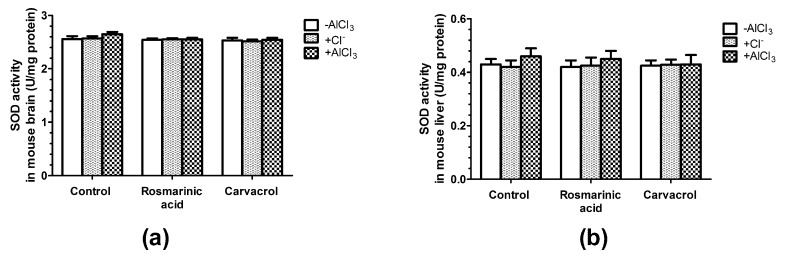
The administration of rosmarinic acid and carvacrol alone or in combination with AlCl3 had no significant effects on CAT activity (Figure 4a,b). Changes in SOD activity followed the same pattern; no effects were observed in the case of all treatments except with negligible changes noticed in mice treated with AlCl3 alone (Figure 5a,b).
Figure 5.
Influence of aluminum ions, rosmarinc acid, and carvacrol on the activity of superoxide dismutase (SOD) in mice brain (a) and liver (b) homogenates (n = 9).
3. Discussion
Numerous studies have demonstrated the toxicity of aluminum in various animal models [1]. The most important concern about aluminum exposure is related to its neurotoxic effects and its possible role in neurodegenerative disorders [6,34]. Most literature data about the low dose Al toxicity is based on the experiments where Al is administered orally. Direct evidence of neurotoxicity due to low doses of Al is controversial, e.g., Shoji et al. reported that 0.97–9.7 mg/kg/day Al per os for 60 days did not induce statistically significant behavioral changes in C57BL/6J mice [35], whereas Martinez et al. found that 8.3 mg/kg/day Al per os for 60 days promoted the development of mechanical allodynia, catalepsy, increased inflammation in the sciatic nerve, and systemic oxidative stress, and was able to be retained in the sciatic nerve [36].
The toxicity of soluble Al forms depends upon the delivered dose of Al3+ to target tissues. Elevated Al3+ concentrations lead to Al3+—induced formation of oxygen radicals causing lipid peroxidation, which results in cell membrane damage and oxidative stress [3,4,5,6,7]. Accumulating evidence obtained from in vitro, in vivo, and clinical studies supports the free radical scavenging properties of natural phenolic antioxidants [24]. In this study, we proposed that natural herbal phenolic compounds with strong antioxidant activity, such as rosmarinic acid [24] and carvacrol [29], could help to counteract the toxicity of Al.
Endogenous ROS are mainly produced in the mitochondrial inner membrane during the process of oxidative phosphorylation. The uncontrolled formation of free radicals and activated oxygen species is prevented by intracellular antioxidant systems [37]. Intracellular antioxidants include low molecular weight scavengers of oxidizing species (such as GSH), and enzymes that degrade superoxide and hydroperoxides [37,38]. GSH acts as the main non-enzymatic antioxidant that directly scavenges free radicals or serves as a substrate for the glutathione peroxidase, the enzyme that catalyzes the detoxification of H2O2 [37,39]. MDA is the end product of lipid peroxidation, and its level indicates the extent of oxidative stress [40,41,42].
We assessed Al amount, GSH and MDA concentrations as well as CAT and SOD activities in erythrocytes and brain and liver homogenates of BALB/c mice treated with Al3+ (7.5 mg/kg/day (0.15 LD50), 21 days, i.p.) in the presence and absence of rosmarinic acid (0.2805 mg/kg/day (0.05 LD50), 21 days, i.g.) or carvacrol (0.0405 mg/kg/day (0.05 LD50), 21 days, i.g.).
The Al amount in mice blood, brain and liver tissues increased after AlCl3 treatment by 69%, 52.2%, and 230% accordingly, compared to control values (Figure 1a–c). Rosmarinic acid or carvacrol diminished the accumulation of Al by 30% in blood, by 40% in brain, and by 30% in liver tissues (Figure 1a–c). Thus, the highest degree of protection from Al accumulation by rosmarinic acid or carvacrol was observed in brain in our study.
Our results showed that the concentration of intracellular antioxidant GSH in erythrocytes in mice treated with rosmarinic acid or carvacrol in either the presence or absence of Al3+ increased (p < 0.05; Figure 2a). This effect was even greater in the case of both carvacrol and Al. However, in brain (Figure 2b) and liver (Figure 2c) homogenates, the GSH concentration was not affected by Al3+ treatment but was diminished by rosmarinic acid and carvacrol (p < 0.05). Some studies have shown that Al3+ reduces the brain GSH contents in Sprague-Dawley rats (10 mg/kg/day, 45 days, i.p.) [43]. Viezeliene et al. also found that in BALB/c mice treated with Al3+ i.p. once (25 mg/kg, sample taken after 16 h), liver GSH activity was significantly decreased compared with normal controls [12]. However, other studies have indicated that Al3+ increases GSH levels in all brain regions of Swiss albino mice (50 mg/kg/d, 42 days, per os (p.o.)) [44]. These inconsistencies may be due to differences among animals, dosages, times, experimental conditions, or experimental procedures [45,46]. Thus, in our study, treatment with Al3+ (7.5 mg/kg/day [0.15 LD50], 21 days, i.p.) led to only a slight increase in GSH concentration in erythrocytes and had no significant effects on brain and liver homogenates. Rosmarinic acid promotes an increase in intracellular GSH concentrations [47]. However, the opposite effect—a decrease in GSH caused by flavonoids—has been reported in several studies [48,49]. In the case of a phenol ring containing dietary polyphenolics treatment, some GSH was oxidized to glutathione disulfide [49]. It has also been reported that both antioxidant and pro-oxidant activities could be observed at different doses of phenolic compounds [50]. Thus, the strongly increased concentration of the first-line non-enzymatic radical scavenger GSH in erythrocytes in our study (Figure 2a) could be related to the antioxidant properties of rosmarinic acid and carvacrol, and the decrease in GSH content (although to a lesser extent) in brain (Figure 2b) and liver (Figure 2c) to their pro-oxidant activities.
MDA is the marker of lipid peroxidation, its increase is related to the negative effects on the fluidity and damage to cell membranes, and it is implicated as the most important parameter that shows the extent of oxidative stress [42]. In our study, MDA levels were decreased (p < 0.05) in the erythrocytes of mice that received Al3+ alone or in combination with rosmarinic acid and carvacrol (Figure 3a). However, MDA concentration significantly increased after Al3+ administration, whereas rosmarinic acid and carvacrol treatment alone or in combination with Al3+ resulted in highly decreased MDA levels in mice brain (Figure 3b) and liver (Figure 3c) homogenates. Our results indicate that AlCl3 induced oxidative stress in the brain and liver, and both rosmarinic acid and carvacrol were able to counteract the negative Al effect and protect against lipid peroxidation. The toxic effect of Al could be related to its accumulation in brain and liver to a higher extent than in the erythrocytes in the blood. This is in good agreement with observations showing that Al is mainly absorbed by the gastrointestinal tract and easily accumulates in body tissues [51,52], thus causing central nervous system toxicity, hepatotoxicity, nephrotoxicity, cardiotoxicity, and osteoporosis [53,54,55]. Rosmarinic acid has been shown to be neuroprotective, attenuating oxidative stress and neuronal cell death in vitro [25,26,27] and reducing inflammatory responses in experimental models of an ischemic stroke [18,28]. Rosmarinic acid treatment decreases MDA in rat liver [56], as well as in mice brain [57], kidney, and liver [57,58]. Carvacrol decreases the peroxidation of phospholipid liposomes in the presence of iron(III) and ascorbate [59], and inhibits low-density lipoprotein oxidation in a concentration dependent manner in an in vitro system using human aortic endothelial cells [60]. Reduced levels of MDA have also been found in homogenates of carvacrol-treated rat hearts [61,62]. The ability of rosmarinic acid and carvacrol to significantly diminish the levels of MDA in mice brain (Figure 3b) and liver (Figure 3c) in our study suggests the potential of these natural phenolic compounds to act as brain and liver protectants via the antioxidant effect.
SOD and CAT are considered primary enzymes of the antioxidant system, which is involved in the direct elimination of ROS. SOD converts superoxide anion to hydrogen peroxide and oxygen, and diminishes the toxic effects due to this radical or other free radicals derived from secondary reactions [37,38]. CAT is a hemoprotein that catalyzes the conversion of hydrogen to H2O [38]. Our results have shown that only AlCl3 treatment increased CAT activity (p < 0.05) in mice brain and liver homogenates (Figure 4a,b), whereas rosmarinic acid or carvacrol administration alone or in combination with Al3+ had no significant effects on CAT activity (Figure 4a,b). SOD activity remained unchanged after all treatments in our study (Figure 5a,b). The data on Al3+ influence on the activities of antioxidant enzymes is not consistent, and might depend on the dosage, treatment duration, and experimental conditions [45,46]. Al3+ was shown to decrease brain CAT activity in Swiss albino mice (50 mg/kg/day, 60 days, p.o.) [63], and decrease SOD activity in specific brain regions of Swiss albino mice (50 mg/kg/day, 42 days, p.o.) [44]. However, other studies have shown that Al3+ increases SOD activity in the brain in Swiss albino mice (100 mg/kg/day, 42 days, i.p.) [64]. Moreover, one report showed that brain CAT activity significantly decreased, whereas brain SOD activity was not altered in Al3+ treated Kunming mice (40 mg/kg/day, i.p., 28 days) [46]. The impact of rosmarinic acid and carvacrol on antioxidant enzyme activity also depends on their dosage. In our case, to avoid toxic effects and to mimic dietary consumption of these compounds, we used rosmarinic acid and carvacrol at doses corresponding to 0.05 LD50 (0.2805 mg/kg/day and 0.0405 mg/kg/day, respectively). Under these conditions, both rosmarinic acid and carvacrol were able to prevent lipid peroxidation by Al and to keep MDA at low levels (Figure 3). However, no significant effects of rosmarinic acid or carvacrol on brain and liver CAT (Figure 4) and SOD (Figure 5) activities were observed. Other studies have reported that CAT and SOD are activated by rosmarinic acid [65] and carvacrol [62]. However, much higher phenolic compound doses were administered in these investigations, at levels of up to 100 times higher than we used in our study.
4. Materials and Methods
4.1. Materials
Rosmarinic acid (>98%) was purchased from ChromaDex (Santa Ana, TX, USA). All other chemicals, including carvacrol (>98%) and AlCl3 (>99.9%), were from Sigma-Aldrich (St. Louis, MO, USA).
4.2. Animal Model
The experiments were performed on 4 to 6-week-old white male BALB/c laboratory mice weighing 20–25 g that were housed at 23 ± 2 °C with a 12 h light/dark cycle and free access to food and water. The mice were from the Vivarium of Lithuanian University of Health Sciences and were kept there during the experiments. According to the requirements of the EU Directive 2010/63/EU for animal experiments the study protocol was approved by the Lithuanian State Food and Veterinary Service, License No. G2–19. Mice were randomly allocated to nine groups (n = 9/group) kept in separate cages: vehicle control, AlCl3, rosmarinic acid, rosmarinic acid + AlCl3, carvacrol, carvacrol + AlCl3, and three Cl− control groups (HCl, rosmarinic acid + HCl, and carvacrol + HCl). AlCl3 dissolved in saline was injected intraperitoneally (i.p.) at a dose of 7.5 mg of Al3+/kg body weight (0.15 LD50) in the AlCl3, rosmarinic acid + AlCl3, and carvacrol + AlCl3 mouse groups for 21 days. In the Cl− control groups (HCl, rosmarinic acid + HCl, and carvacrol + HCl), mice received an equimolar to AlCl3 dose of Cl− as HCl (30.41 mg/kg/day for 21 days, i.p.). Mice in the vehicle control, rosmarinic acid, and carvacrol groups received an equal volume of saline in the same manner, mice in the rosmarinic acid, rosmarinic acid + HCl, and rosmarinic acid + AlCl3 groups received intragastric (i.g.) rosmarinic acid (0.2805 mg/kg body weight, corresponding to 0.05 LD50) for 21 days, and the mice in the carvacrol, carvacrol + HCl, and carvacrol + AlCl3 groups received carvacrol (0.0405 mg/kg body weight, corresponding to 0.05 LD50) for 21 days, all diluted in saline. To avoid toxic effects and to mimic dietary consumption of these compounds, we used rosmarinic acid and carvacrol at doses corresponding to 0.05 LD50 (0.2805 mg/kg/day and 0.0405 mg/kg/day, respectively). AlCl3 was used i.p. at a dose of 7.5 mg of Al3+/kg body weight (0.15 LD50) to avoid animal deaths due to excess accumulation of Al in prolonged experiment and to mimic low doses of Al found in vaccines. 81 mice were used in total.
4.3. Sample Preparation
After the exposure time, the blood samples were collected in the pre-heparinized tubes. The blood was centrifuged for 10 min at 800× g at 4 °C, and the plasma layers with debris were removed by aspiration. The erythrocytes were washed three times with a phosphate-buffered saline (pH 7.4) and kept on ice.
The animals were terminated according to the rules defined by the EU Directive 2010/63/EU for animal experiments. Following that, the brain and liver were quickly removed, put on Petri dishes, and immediately cooled in an ice bath. Homogenates were prepared as described below. Protein concentrations in the brain and liver homogenate samples were determined by the Warburg-Christian method.
The erythrocytes and homogenate samples were coded for the endpoint measurements. The assessors have not got the information which sample belongs for which experimental group.
4.4. Determination of Al Amount in Blood and Target Tissues
The concentration of Al in mouse erythrocytes, liver and brain was evaluated by using an inductively coupled plasma mass spectrometer NexION 300 D (PerkinElmer, Inc. Shelton, CT, USA ). Tissue specimens were digested with 0.125 M NaOH at 90 °C. The digests were diluted to the appropriate volume and were analyzed according to the manufacturer′s recommendations for the detection of Al concentrations in biological samples. To ensure the accuracy of the analysis, we conducted internal and external quality control procedures, including the use of analytical high-purity water and reagents (Sigma-Aldrich Chemie GmbH, Taufkirchen, Germany), certified reference materials ClinCheck® Whole Blood Controls Level (Recipe Chemicals + Instruments GmbH, München, Germany), Standard Reference Material®−1577c bovine liver. We also conducted the control of labware for contamination with Al.
4.5. Determination of Glutathione Level
The amount of glutathione (GSH), an intracellular antioxidant, was assessed based on a reduced GSH reaction with the 5,5′-dithiobis-(2-nitrobenzoic acid) (DTNB) in an alkaline environment, which produces a yellow complex.
GSH concentration in erythrocytes was determined according to the method of Sedlak and Lindsay [66]. Erythrocytes (200 µL) were added to 1.8 mL of deionized water and 2 mL of 0.6 M HClO4. The mixture was centrifuged for 10 min at 3000× g and the upper aqueous layer was decanted to the test tube and used for the color reaction. Supernatant (1 mL) was added to 3 mL of 0.4 M Tris-HCl (pH 9.2) and 50 µL of DTNB stock solution (3.7 mg of DTNB + 1 mL ethanol). Light absorbance of the solution was determined spectrophotometrically at 412 nm.
GSH concentration in liver and brain homogenates was determined according to the method of Moron et al. [67]. Liver and brain homogenates were prepared with 6 volumes (w/v) of 5% trichloroacetic acid (TCA) solution. The homogenates were centrifuged at 10,000× g for 7 min to obtain GSH-containing supernatants. The supernatant (0.2 mL) was mixed with 2 mL of 0.6 mM DTNB in 0.2 M phosphate buffer (pH 8.0), and 0.8 mL of phosphate buffer was added to make a final reaction volume of 3 mL. The light absorbance of the solution was determined spectrophotometrically at 412 nm. A mixture of buffered DTNB solution containing 0.2 mL of 5% TCA was used as a reference. GSH concentration was expressed as µM/g protein or µM (in case of erythrocytes).
4.6. Determination of Malondialdehyde Level
The amount of malondialdehyde (MDA), a marker of lipid peroxidation, was estimated in erythrocytes, liver, and brain homogenates by measuring thiobarbituric acid reactive substances.
Thiobarbituric acid (2 mL of 0.5%) was added to the reaction mixture containing 2 mL of deionized water, 0.1 mL of erythrocytes, and 1 mL of 10% TCA solution. The mixture was heated for 30 min in a boiling water bath. After cooling in the ice bath, the mixture was centrifuged for 15 min at 3000× g at 4 °C. The supernatant was filtered through four layers of sterile gauze and the light absorbance was determined spectrophotometrically at 540 nm [68].
Liver and brain homogenates were prepared with nine volumes (w/v) of cold 1.15% KCl. H3PO4 (3 mL of 1%) and thiobarbituric acid (1 mL of 0.6%) aqueous solutions were added to 0.5 mL of the homogenates. The mixtures were heated for 45 min in a boiling water bath. After cooling, 4 mL of n-butanol was added and the solution was mixed vigorously. The butanol phase was separated by centrifugation. The light absorbance of the supernatants was then determined spectrophotometrically at 535 and 520 nm [69]. MDA concentrations were expressed as µM (in case of erythrocytes) or µM/g protein.
4.7. Catalase Activity Assay
The activity of catalase (CAT) in mice brain and liver homogenates was determined by the hydrogen peroxide reaction with ammonium molybdate, which produces a complex that absorbs light at 410 nm [70]. Enzyme activity units were equal to the amount of enzyme that consumes 1 µM H2O2 within a minute under the experimental conditions, and were reported as U/mg protein.
4.8. Superoxide Dismutase Activity Assay
The activity of superoxide dismutase (SOD) in mice brain and liver homogenates was determined according to the inhibition of nitroblue tetrazolium reduction rate in the non-enzymatic phenazine methosulfate-nicotinamide adenine dinucleotide system assessed spectrophotometrically at 540 nm [70]. The SOD activity was expressed as U/mg protein, where U was the relative unit of activity defined as the amount of SOD required for the inhibition of nitroblue tetrazolium reduction by 50%.
4.9. Statistics
Data are expressed as the mean ± standard error of the mean (n = 9). Statistical analysis was performed by one-way analysis of variance, followed by Tukey′s post-test using the Prism v. 5.04 software package (GraphPad Software Inc., La Jolla, CA, USA). A value of p < 0.05 was taken as the level of significance.
5. Conclusions
To conclude, we have shown that prolonged exposure to Al3+, even at considerably low doses (0.15 LD50), resulted in Al accumulation and induced oxidative stress in mice brain and liver, and rosmarinic acid and carvacrol were able to counteract the negative Al effect decreasing Al accumulation and protecting tissues from lipid peroxidation. Since aluminum-induced toxicity has been suggested to have a role in the development of neurodegenerative disorders, the natural herbal phenolic compounds rosmarinic acid and carvacrol widely used as foods or food additives in the food industry could be important candidates in the attenuation of oxidative stress and provide protection from related injuries.
Acknowledgments
The authors wish to thank the Open Access Centre for the Advanced Pharmaceutical and Health technologies for the support of this study.
Author Contributions
Conceptualization, J.B. (Juste Baranauskaite), I.S. and J.B. (Jurga Bernatoniene); methodology, I.S., A.L., A.K., R.L., R.M., U.Z.; validation, J.B. (Juste Baranauskaite), I.S., D.M.K. and J.B. (Jurga Bernatoniene); investigation, J.B. (Juste Baranauskaite), I.S., A.L., A.K., R.L., U.Z., J.B. (Jurga Bernatoniene); data curation, I.S., D.M.K., R.M., J.B. (Jurga Bernatoniene); writing—original draft preparation, J.B. (Juste Baranauskaite), D.M.K., J.B. (Jurga Bernatoniene); writing—review and editing, J.B. (Juste Baranauskaite), I.S., A.L., A.K., R.L., R.M., D.M.K., J.B. (Jurga Bernatoniene); visualization, J.B. (Juste Baranauskaite),, D.M.K., J.B. (Jurga Bernatoniene); supervision, J.B.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Sample Availability: Not available.
References
- 1.Willhite C.C., Karyakina N.A., Yokel R.A., Yenugadhati N., Wisniewski T.M., Arnold I.M., Momoli F., Krewski D. Systematic review of potential health risks posed by pharmaceutical, occupational and consumer exposures to metallic and nanoscale aluminum, aluminum oxides, aluminum hydroxide and its soluble salts. Crit. Rev. Toxicol. 2014;44:1–80. doi: 10.3109/10408444.2014.934439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arabsolghar R., Saberzadeh J., Khodaei F., Borojeni R.A., Khorsand M., Rashedinia M. The protective effect of sodium benzoate on aluminum toxicity in PC12 cell line. Res. Pharm Sci. 2017;12:391–400. doi: 10.4103/1735-5362.213984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fraga C.G., Oteiza P.I., Golub M.S., Gershwin M.E., Keen C.L. Effects of aluminum on brain lipid peroxidation. Toxicol. Lett. 1990;51:213–219. doi: 10.1016/0378-4274(90)90212-5. [DOI] [PubMed] [Google Scholar]
- 4.Gutteridge J.M., Quinlan G.J., Clark I., Halliwell B. Aluminium salts accelerate peroxidation of membrane lipids stimulated by iron salts. Biochim. Biophys. Acta. 1985;835:441–447. doi: 10.1016/0005-2760(85)90113-4. [DOI] [PubMed] [Google Scholar]
- 5.Savory J., Rao J.K., Huang Y., Letada P.R., Herman M.M. Age-related hippocampal changes in Bcl-2: Bax ratio, oxidative stress, redox-active iron and apoptosis associated with aluminum-induced neurodegeneration: Increased susceptibility with aging. Neurotoxicology. 1999;20:805–817. [PubMed] [Google Scholar]
- 6.Tomljenovic L. Aluminum and Alzheimer′s disease: After a century of controversy, is there a plausible link? J. Alzheimers Dis. 2011;23:567–598. doi: 10.3233/JAD-2010-101494. [DOI] [PubMed] [Google Scholar]
- 7.Zatta P., Lain E., Cagnolini C. Effects of aluminum on activity of krebs cycle enzymes and glutamate dehydrogenase in rat brain homogenate. Eur. J. Biochem. 2000;267:3049–3055. doi: 10.1046/j.1432-1033.2000.01328.x. [DOI] [PubMed] [Google Scholar]
- 8.Shelley R., Kim N.S., Parsons P., Lee B.K., Jaar B., Fadrowski J., Agnew J., Matanoski G.M., Schwartz B.S., Steuerwald A., et al. Associations of multiple metals with kidney outcomes in lead workers. Occup. Environ. Med. 2012;69:727–735. doi: 10.1136/oemed-2012-100765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garrosa M., Llanes F., Gayoso M.J. Histopathological changes in gerbil liver and kidney after aluminum subchronic intoxication. Histol. Histopathol. 2011;26:883–892. doi: 10.14670/HH-26.883. [DOI] [PubMed] [Google Scholar]
- 10.Bhadauria M. Combined treatment of HEDTA and propolis prevents aluminum induced toxicity in rats. Food Chem. Toxicol. 2012;50:2487–2495. doi: 10.1016/j.fct.2011.12.040. [DOI] [PubMed] [Google Scholar]
- 11.Turgut S., Bor-Kucukatay M., Emmungil G., Atsak P., Turgut G. The effects of low dose aluminum on hemorheological and hematological parameters in rats. Arch. Toxicol. 2007;81:11–17. doi: 10.1007/s00204-006-0119-8. [DOI] [PubMed] [Google Scholar]
- 12.Viezeliene D., Jansen E., Rodovicius H., Kasauskas A., Ivanov L. Protective effect of selenium on aluminium-induced oxidative stress in mouse liver in vivo. Environ. Toxicol. Pharmacol. 2011;31:302–306. doi: 10.1016/j.etap.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Banks W.A., Niehoff M.L., Drago D., Zatta P. Aluminum complexing enhances amyloid beta protein penetration of blood–brain barrier. Brain Res. 2006;1116:215–221. doi: 10.1016/j.brainres.2006.07.112. [DOI] [PubMed] [Google Scholar]
- 14.Kumar V., Bal A., Gill K.D. Impairment of mitochondrial energy metabolism in different regions of rat brain following chronic exposure to aluminium. Brain Res. 2008;1232:94–103. doi: 10.1016/j.brainres.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 15.Altschuler E. Aluminum-containing antacids as a cause of idiopathic Parkinson′s disease. Med. Hypotheses. 1999;53:22–23. doi: 10.1054/mehy.1997.0701. [DOI] [PubMed] [Google Scholar]
- 16.Walton J.R. Cognitive deterioration and associated pathology induced by chronic low-level aluminum ingestion in a translational rat model provides an explanation of Alzheimer′s disease, tests for susceptibility and avenues for treatment. Int. J. Alzheimers Dis. 2012;2012:914–947. doi: 10.1155/2012/914947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yokel R.A. The toxicology of aluminum in the brain: A review. Neurotoxicology. 2000;21:813–828. [PubMed] [Google Scholar]
- 18.Bigford G.E., Del Rossi G. Supplemental substances derived from foods as adjunctive therapeutic agents for treatment of neurodegenerative diseases and disorders. Adv. Nutr. 2014;5:394–403. doi: 10.3945/an.113.005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joseph J., Cole G., Head E., Ingram D. Nutrition, brain aging, and neurodegeneration. J. Neurosci. 2009;29:12795–12801. doi: 10.1523/JNEUROSCI.3520-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hashimoto M., Hossain S. Neuroprotective and ameliorative actions of polyunsaturated fatty acids against neuronal diseases: Beneficial effect of docosahexaenoic acid on cognitive decline in Alzheimer′s disease. J. Pharmacol. Sci. 2011;116:150–162. doi: 10.1254/jphs.10R33FM. [DOI] [PubMed] [Google Scholar]
- 21.Jones L.L., McDonald D.A., Borum P.R. Acylcarnitines: Role in brain. Prog. Lipid Res. 2010;49:61–75. doi: 10.1016/j.plipres.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Malaguarnera M. Carnitine derivatives: Clinical usefulness. Curr. Opin. Gastroenterol. 2012;28:166–176. doi: 10.1097/MOG.0b013e3283505a3b. [DOI] [PubMed] [Google Scholar]
- 23.Petersen M., Simmonds M.S. Rosmarinic acid. Phytochemistry. 2003;62:121–125. doi: 10.1016/S0031-9422(02)00513-7. [DOI] [PubMed] [Google Scholar]
- 24.Zhou H., Fu B., Xu B., Mi X., Li G., Ma C., Xie J., Li J., Wang Z. Rosmarinic Acid Alleviates the Endothelial Dysfunction Induced by Hydrogen Peroxide in Rat Aortic Rings via Activation of AMPK. Oxid. Med. Cell. Longev. 2017;2017:7091904. doi: 10.1155/2017/7091904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee H.J., Cho H.S., Park E., Kim S., Lee S.Y., Kim C.S., Kim D.K., Kim S.J., Chun H.S. Rosmarinic acid protects human dopaminergic neuronal cells against hydrogen peroxide-induced apoptosis. Toxicology. 2008;250:109–115. doi: 10.1016/j.tox.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Choi H.R., Choi J.S., Han Y.N., Bae S.J., Chung H.Y. Peroxynitrite scavenging activity of herb extracts. Phytother. Res. 2002;16:364–367. doi: 10.1002/ptr.904. [DOI] [PubMed] [Google Scholar]
- 27.Qiao S., Li W., Tsubouchi R., Haneda M., Murakami K., Takeuchi F., Nisimoto Y., Yoshino M. Rosmarinic acid inhibits the formation of reactive oxygen and nitrogen species in RAW264.7 macrophages. Free Radic. Res. 2005;39:995–1003. doi: 10.1080/10715760500231836. [DOI] [PubMed] [Google Scholar]
- 28.Luan H., Kan Z., Xu Y., Lv C., Jiang W. Rosmarinic acid protects against experimental diabetes with cerebral ischemia: Relation to inflammation response. J. Neuroinflammation. 2013;10:28. doi: 10.1186/1742-2094-10-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedman M. Chemistry and multibeneficial bioactivities of carvacrol (4-isopropyl-2-methylphenol), a component of essential oils produced by aromatic plants and spices. J. Agric. Food Chem. 2014;62:7652–7670. doi: 10.1021/jf5023862. [DOI] [PubMed] [Google Scholar]
- 30.Soobrattee M.A., Neergheen V.S., Luximon-Ramma A., Aruoma O.I., Bahorun T. Phenolics as potential antioxidant therapeutic agents: Mechanism and actions. Mutat. Res. 2005;579:200–213. doi: 10.1016/j.mrfmmm.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 31.Baser K.H. Biological and pharmacological activities of carvacrol and carvacrol bearing essential oils. Curr. Pharm. Des. 2008;14:3106–3119. doi: 10.2174/138161208786404227. [DOI] [PubMed] [Google Scholar]
- 32.Nostro A., Papalia T. Antimicrobial activity of carvacrol: Current progress and future prospectives. Recent Pat. Antiinfect. Drug Discov. 2012;7:28–35. doi: 10.2174/157489112799829684. [DOI] [PubMed] [Google Scholar]
- 33.Suntres Z.E., Coccimiglio J., Alipour M. The bioactivity and toxicological actions of carvacrol. Crit. Rev. Food Sci. Nutr. 2015;55:304–318. doi: 10.1080/10408398.2011.653458. [DOI] [PubMed] [Google Scholar]
- 34.Maya S., Prakash T., Madhu K.D., Goli D. Multifaceted effects of aluminium in neurodegenerative diseases: A review. Biomed. Pharmacother. 2016;83:746–754. doi: 10.1016/j.biopha.2016.07.035. [DOI] [PubMed] [Google Scholar]
- 35.Shoji H., Irino Y., Yoshida M., Miyakawa T. Behavioral effects of long-term oral administration of aluminum ammonium sulfate in male and female C57BL/6J mice. Neuropsychopharmacol. Rep. 2018;38:18–36. doi: 10.1002/npr2.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martinez C.S., Vera G., Ocio J.A.U., Pecanha F.M., Vassallo D.V., Miguel M., Wiggers G.A. Aluminum exposure for 60days at an equivalent human dietary level promotes peripheral dysfunction in rats. J. Inorg. Biochem. 2018;181:169–176. doi: 10.1016/j.jinorgbio.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 37.Birben E., Sahiner U.M., Sackesen C., Erzurum S., Kalayci O. Oxidative stress and antioxidant defense. World Allergy Organ. J. 2012;5:9–19. doi: 10.1097/WOX.0b013e3182439613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Espinosa-Diez C., Miguel V., Mennerich D., Kietzmann T., Sanchez-Perez P., Cadenas S., Lamas S. Antioxidant responses and cellular adjustments to oxidative stress. Redox Biol. 2015;6:183–197. doi: 10.1016/j.redox.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dickinson D.A., Forman H.J. Glutathione in defense and signaling: Lessons from a small thiol. Ann. N Y Acad. Sci. 2002;973:488–504. doi: 10.1111/j.1749-6632.2002.tb04690.x. [DOI] [PubMed] [Google Scholar]
- 40.Siu G.M., Draper H.H. Metabolism of malonaldehyde in vivo and in vitro. Lipids. 1982;17:349–355. doi: 10.1007/BF02535193. [DOI] [PubMed] [Google Scholar]
- 41.Girotti A.W. Mechanisms of lipid peroxidation. J. Free Radic. Biol. Med. 1985;1:87–95. doi: 10.1016/0748-5514(85)90011-X. [DOI] [PubMed] [Google Scholar]
- 42.Del Rio D., Stewart A.J., Pellegrini N. A review of recent studies on malondialdehyde as toxic molecule and biological marker of oxidative stress. Nutr. Metab. Cardiovasc. Dis. 2005;15:316–328. doi: 10.1016/j.numecd.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 43.Abdel-Salam O.M.E., Hamdy S.M., Seadawy S.A.M., Galal A.F., Abouelfadl D.M., Atrees S.S. Effect of piracetam, vincamine, vinpocetine, and donepezil on oxidative stress and neurodegeneration induced by aluminum chloride in rats. Comp. Clin. Pathol. 2016;25:305–318. doi: 10.1007/s00580-015-2182-0. [DOI] [Google Scholar]
- 44.Al-Amin M.M., Reza H.M., Saadi H.M., Mahmud W., Ibrahim A.A., Alam M.M., Kabir N., Saifullah A.R., Tropa S.T., Quddus A.H. Astaxanthin ameliorates aluminum chloride-induced spatial memory impairment and neuronal oxidative stress in mice. Eur. J. Pharmacol. 2016;777:60–69. doi: 10.1016/j.ejphar.2016.02.062. [DOI] [PubMed] [Google Scholar]
- 45.Hussain S., Slikker W., Jr., Ali S.F. Age-related changes in antioxidant enzymes, superoxide dismutase, catalase, glutathione peroxidase and glutathione in different regions of mouse brain. Int. J. Dev. Neurosci. 1995;13:811–817. doi: 10.1016/0736-5748(95)00071-2. [DOI] [PubMed] [Google Scholar]
- 46.Li L., Jiao Y., Jin T., Sun H., Li S., Jin C., Hu S., Ji J., Xiang L. Phenolic alkaloid oleracein E attenuates oxidative stress and neurotoxicity in AlCl3-treated mice. Life Sci. 2017;191:211–218. doi: 10.1016/j.lfs.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 47.Gonzalez-Vallinas M., Reglero G., Ramirez de Molina A. Rosemary (Rosmarinus officinalis L.) Extract as a Potential Complementary Agent in Anticancer Therapy. Nutr. Cancer. 2015;67:1221–1229. doi: 10.1080/01635581.2015.1082110. [DOI] [PubMed] [Google Scholar]
- 48.Duthie S.J., Collins A.R. The influence of cell growth, detoxifying enzymes and DNA repair on hydrogen peroxide-mediated DNA damage (measured using the comet assay) in human cells. Free Radic. Biol. Med. 1997;22:717–724. doi: 10.1016/S0891-5849(96)00421-2. [DOI] [PubMed] [Google Scholar]
- 49.Galati G., Sabzevari O., Wilson J.X., O′Brien P.J. Prooxidant activity and cellular effects of the phenoxyl radicals of dietary flavonoids and other polyphenolics. Toxicology. 2002;177:91–104. doi: 10.1016/S0300-483X(02)00198-1. [DOI] [PubMed] [Google Scholar]
- 50.Ferguson L.R. Role of plant polyphenols in genomic stability. Mutat. Res. 2001;475:89–111. doi: 10.1016/S0027-5107(01)00073-2. [DOI] [PubMed] [Google Scholar]
- 51.Kumar V., Gill K.D. Aluminium neurotoxicity: Neurobehavioral and oxidative aspects. Arch. Toxicol. 2009;83:965–978. doi: 10.1007/s00204-009-0455-6. [DOI] [PubMed] [Google Scholar]
- 52.Krewski D., Yokel R.A., Nieboer E., Borchelt D., Cohen J., Harry J., Kacew S., Lindsay J., Mahfouz A.M., Rondeau V. Human health risk assessment for aluminium, aluminium oxide, and aluminium hydroxide. J. Toxicol. Environ. Health B Crit. Rev. 2007;10:1–269. doi: 10.1080/10937400701597766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yang Y., Wang H., Guo Y., Lei W., Wang J., Hu X., Yang J., He Q. Metal Ion Imbalance-Related Oxidative Stress Is Involved in the Mechanisms of Liver Injury in a Rat Model of Chronic Aluminum Exposure. Biol. Trace Elem. Res. 2016;173:126–131. doi: 10.1007/s12011-016-0627-1. [DOI] [PubMed] [Google Scholar]
- 54.Crisponi G., Fanni D., Gerosa C., Nemolato S., Nurchi V.M., Crespo-Alonso M., Lachowicz J.I., Faa G. The meaning of aluminium exposure on human health and aluminium-related diseases. Biomol. Concepts. 2013;4:77–87. doi: 10.1515/bmc-2012-0045. [DOI] [PubMed] [Google Scholar]
- 55.Geyikoglu F., Turkez H., Bakir T.O., Cicek M. The genotoxic, hepatotoxic, nephrotoxic, haematotoxic and histopathological effects in rats after aluminium chronic intoxication. Toxicol. Ind. Health. 2013;29:780–791. doi: 10.1177/0748233712440140. [DOI] [PubMed] [Google Scholar]
- 56.Hasanein P., Sharifi M. Effects of rosmarinic acid on acetaminophen-induced hepatotoxicity in male Wistar rats. Pharm. Biol. 2017;55:1809–1816. doi: 10.1080/13880209.2017.1331248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee A.Y., Hwang B.R., Lee M.H., Lee S., Cho E.J. Perilla frutescens var. japonica and rosmarinic acid improve amyloid-beta25-35 induced impairment of cognition and memory function. Nutr. Res. Pract. 2016;10:274–281. doi: 10.4162/nrp.2016.10.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang Y., Chen X., Yang L., Zu Y., Lu Q. Effects of rosmarinic acid on liver and kidney antioxidant enzymes, lipid peroxidation and tissue ultrastructure in aging mice. Food Funct. 2015;6:927–931. doi: 10.1039/C4FO01051E. [DOI] [PubMed] [Google Scholar]
- 59.Aeschbach R., Loliger J., Scott B.C., Murcia A., Butler J., Halliwell B., Aruoma O.I. Antioxidant actions of thymol, carvacrol, 6-gingerol, zingerone and hydroxytyrosol. Food Chem. Toxicol. 1994;32:31–36. doi: 10.1016/0278-6915(84)90033-4. [DOI] [PubMed] [Google Scholar]
- 60.Teissedre P.L., Waterhouse A.L. Inhibition of oxidation of human low-density lipoproteins by phenolic substances in different essential oils varieties. J. Agric. Food Chem. 2000;48:3801–3805. doi: 10.1021/jf990921x. [DOI] [PubMed] [Google Scholar]
- 61.Yu W., Liu Q., Zhu S. Carvacrol protects against acute myocardial infarction of rats via anti-oxidative and anti-apoptotic pathways. Biol. Pharm. Bull. 2013;36:579–584. doi: 10.1248/bpb.b12-00948. [DOI] [PubMed] [Google Scholar]
- 62.Chen Y., Ba L., Huang W., Liu Y., Pan H., Mingyao E., Shi P., Wang Y., Li S., Qi H., et al. Role of carvacrol in cardioprotection against myocardial ischemia/reperfusion injury in rats through activation of MAPK/ERK and Akt/eNOS signaling pathways. Eur. J. Pharmacol. 2017;796:90–100. doi: 10.1016/j.ejphar.2016.11.053. [DOI] [PubMed] [Google Scholar]
- 63.Singh T., Goel R.K. Neuroprotective effect of Allium cepa L. in aluminium chloride induced neurotoxicity. Neurotoxicology. 2015;49:1–7. doi: 10.1016/j.neuro.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 64.Jangra A., Kasbe P., Pandey S.N., Dwivedi S., Gurjar S.S., Kwatra M., Mishra M., Venu A.K., Sulakhiya K., Gogoi R., et al. Hesperidin and Silibinin Ameliorate Aluminum-Induced Neurotoxicity: Modulation of Antioxidants and Inflammatory Cytokines Level in Mice Hippocampus. Biol. Trace Elem. Res. 2015;168:462–471. doi: 10.1007/s12011-015-0375-7. [DOI] [PubMed] [Google Scholar]
- 65.Bacanli M., Aydin S., Taner G., Goktas H.G., Sahin T., Basaran A.A., Basaran N. Does rosmarinic acid treatment have protective role against sepsis-induced oxidative damage in Wistar Albino rats? Hum. Exp. Toxicol. 2016;35:877–886. doi: 10.1177/0960327115607971. [DOI] [PubMed] [Google Scholar]
- 66.Sedlak J., Lindsay R.H. Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman′s reagent. Anal. Biochem. 1968;25:192–205. doi: 10.1016/0003-2697(68)90092-4. [DOI] [PubMed] [Google Scholar]
- 67.Moron M.S., Depierre J.W., Mannervik B. Levels of glutathione, glutathione reductase and glutathione S-transferase activities in rat lung and liver. Biochim. Biophys. Acta. 1979;582:67–78. doi: 10.1016/0304-4165(79)90289-7. [DOI] [PubMed] [Google Scholar]
- 68.Seliutina C.N., Seliutin A., Pal A.I. Modification of estimation the concentrations of serum TBA-active product. Klin. Lab. Diagn. 2000:8–10. [PubMed] [Google Scholar]
- 69.Mihara M., Uchiyama M. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal. Biochem. 1978;86:271–278. doi: 10.1016/0003-2697(78)90342-1. [DOI] [PubMed] [Google Scholar]
- 70.Vermelho A.B., Couri S. Methods to Determine Enzymatic Activity. Bentham Science Publishers; Sharjah, U.A.E.: 2013. p. 334. [Google Scholar]