Abstract
Mesenchymal stem cells (MSCs) have been extensively investigated for the treatment of various diseases. The therapeutic potential of MSCs is attributed to complex cellular and molecular mechanisms of action including differentiation into multiple cell lineages and regulation of immune responses via immunomodulation. The plasticity of MSCs in immunomodulation allow these cells to exert different immune effects depending on different diseases. Understanding the biology of MSCs and their role in treatment is critical to determine their potential for various therapeutic applications and for the development of MSC-based regenerative medicine. This review summarizes the recent progress of particular mechanisms underlying the tissue regenerative properties and immunomodulatory effects of MSCs. We focused on discussing the functional roles of paracrine activities, direct cell–cell contact, mitochondrial transfer, and extracellular vesicles related to MSC-mediated effects on immune cell responses, cell survival, and regeneration. This will provide an overview of the current research on the rapid development of MSC-based therapies.
Keywords: Regenerative potential, Integration of MSCs, Immunomodulation, Soluble factors, Cell–cell contact, Mitochondrial transfer, Extracellular vesicles
Introduction
Mesenchymal stem cells (MSCs), alternatively referred to as mesenchymal stromal cells, have been extensively investigated since their discovery in the bone marrow by Alexander Friedenstein and colleagues in the late 1960s [1, 2]. MSCs can migrate to injured sites, engraft, and differentiate into end-stage functional cells, thus repairing the injured tissue [3, 4]. More importantly, MSCs have also shown promising therapeutic effects due to their ability to modulate multiple immune cell types of both the innate and adaptive immune systems. MSCs can promote neovascularization, increase angiogenesis, enhance cell viability and/or proliferation, inhibit cell death, and modulate immune responses via paracrine and cell–cell contact effects as well as through extracellular vesicles [5, 6]. Recently, over 900 clinical trials worldwide have used MSCs to treat various diseases (www.clinicaltrials.gov), including bone/cartilage repair, diabetes, cardiovascular diseases, immune-related, and neurological disorders. MSCs are attractive candidates for treating various diseases because they can travel to injured sites, differentiate into multiple cell types, and regulate immunomodulation [7]. In particular, the role of homing in MSC-based therapies remains doubtful. Interestingly, despite some encouraging results from animal studies, some clinical trials have also shown no therapeutic efficacy of MSCs. Therefore, understanding the biology of MSCs and their role in treatment will be critical to determine their potential for various therapeutic applications. This review summarizes the mechanisms underlying the protective effects of MSCs and provides an overview of the recent developments in MSC-based therapy.
MSC identity
MSCs are classically defined as plastic-adherent, expanding, non-hematopoietic cells that can differentiate into osteoblasts (bone cells), adipocytes (fat cells), chondroblasts (cartilage cells) and myocytes (skeletal muscle cells) in vitro [8–10]. They express the cluster of differentiation (CD) surface markers including CD90, CD105, and CD73, but do not express CD11b, CD14, CD19, CD34, CD45 and human leukocyte antigen (HLA)-DR according to the International Society of Cell Therapy (ISCT) criteria [8, 9, 11]. However, this set of cell surface markers is not always applicable when identifying MSCs as pericytes and defining the cell markers. MSCs isolated from different tissues have different surface antigen molecules because these surface markers are influenced by many factors. The surface markers of MSCs isolated from the lung are distinct from those of the MSCs derived from the bone marrow [12]. Additional/alternative markers are being identified and confirmed for some specific sources of MSCs. For instance, CD146 is essential for MSC vigour and self-renewal as the dividing ability of MSCs is weakened or eliminated when CD146 is downregulated or silenced [13]. CD49d is detected in adipose-derived MSCs but not in BM-MSCs [14]. To date, markers for identification of MSCs are under investigation. There needs to be a more critical take on a field that has deviated from careful science.
Sources of MSCs
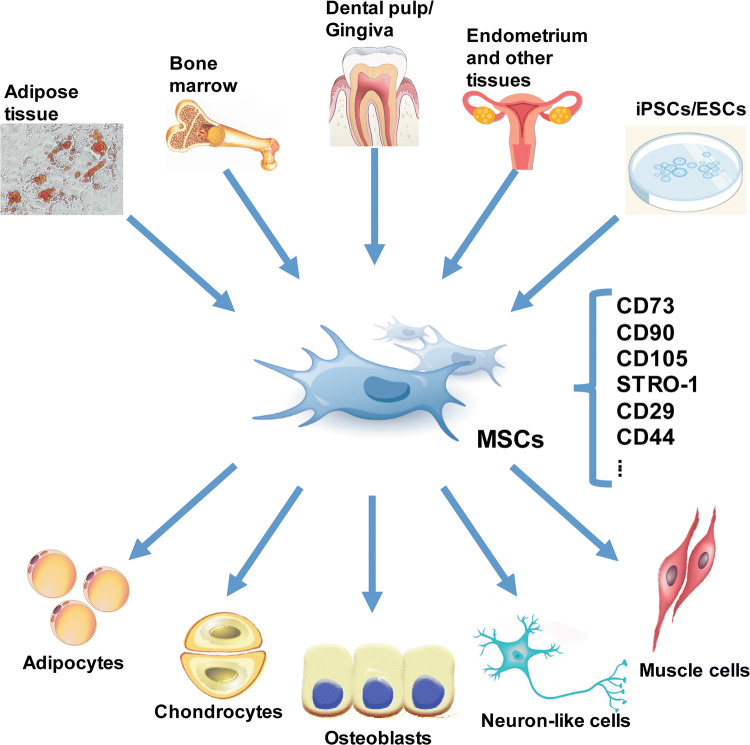
Although bone marrow is the conventional source of MSCs, MSCs or MSC-like cells can be isolated from almost any tissue of the human body. MSC-like cells have been isolated from a variety of foetal, neonatal, and adult tissues including adipose tissue, amniotic fluid, brain, compact bone, dermis, dental pulp, gingiva, foetal liver and lung, human islets, placenta, skeletal muscle, synovium, umbilical cord, peripheral blood and so on (Fig. 1) [14–24]. It is considered that MSCs refer to cells derived from the bone marrow, but not necessarily those from other sites such as adipose tissue, which are often termed as adipose-derived stem cells (ASCs). However, MSCs derived from different origins have different characteristics and differentiation potential [25, 26]. Moreover, MSCs from different sources display significant differences in the levels of several paracrine factors [27]. Currently, the most frequently reported sources of MSCs utilized in clinical trials are the bone marrow, adipose tissue, and umbilical cord. This is partially due to the accessibility, ease of isolation, and MSC-based repair efficacy. The characteristics and differentiation potential of the most commonly investigated MSCs derived from different tissues have been summarized in Table 1.
Fig. 1.
MSCs can be isolated from a variety of foetal, neonatal, and adult tissues, and can differentiate into different cell types. CD cluster of differentiation, ESCs embryonic stem cells, iPSCs induced pluripotent stem cells, MSCs mesenchymal stem cells
Table 1.
Characteristics and differentiation potential of the common different tissue-derived MSCs
| Source tissue | Characteristics | Differentiation potential | References |
|---|---|---|---|
| Adipose tissue | CD73, CD90, CD29, CD44, CD71, CD105, CD13, CD166, STRO-1 | Adipocyte, chondrocyte, osteoblast | [29–31] |
| Amniotic fluid | CD44, CD90, CD105, CD13, CD29, CD71, CD120a | Adipocyte, cardiomyocyte-like cell, chondrocyte, osteoblast | [32, 33] |
| Bone marrow | CD73, CD90, CD105, STRO-1 | Adipocyte, chondrocyte, osteoblast, tenocyte, vascular smooth muscle cell | [34–37] |
| Dental pulp | CD29, CD44, CD90, CD105 | Adipocyte, chondrocyte, osteoblast, neuron-like cell, odontoblast, myogenic lineages | [38–41] |
| Endometrium | CD29, CD90, CD73, CD105 | Adipocyte, chondrocyte, osteoblast | [42, 43] |
| Peripheral blood | CD44, CD90, CD105, HLA-ABC | Adipocyte, osteoblast, fibroblast | [44] |
| Placenta | CD29, CD73, CD90, CD105 | Adipocyte, chondrocyte, osteoblast, myotubular cell, pancreatic progenitor cell, neuron-like cell, retinal cell | [45, 46] |
| Synovium | CD44, CD90, CD105, CD147, STRO-1 | Adipocyte, chondrocyte, osteoblast, skeletal muscle cell | [29, 47, 48] |
| Skin | CD44, CD73, CD90, CD105, CD166, SSEA-4, Vimentin | Adipocyte, chondrocyte, osteoblast, neuron-like cell, pancreatic cell, endothelial cell | [49–51] |
| Umbilical cord | CD29, CD44, CD73, CD90, CD105 | Adipocyte, chondrocyte, osteoblast, skeletal muscle cell, endothelial cell, cardiomyocyte-like cell, neuron-like cell | [52, 53] |
Although MSCs can hypothetically be obtained from almost any tissue within the human body, the MSC surface markers, quality and isolated numbers are restricted by various donor characteristics. There are also practical limitations concerning the difficulty and invasiveness of the procurement process [25]. To select an adequate cell source, the practitioner must consider both advantages and disadvantages of procuring MSCs with regard to the difficulty and potential adverse effects of harvesting donor the cells. For instance, BM-MSCs have shown confirmed safety and effectiveness in multiple clinical trials, but their yields and differentiation potential are dependent on the donor characteristics (e.g., age). Moreover, isolation of cells from the bone marrow is often painful and carries the risk of infection. As adipose tissue is accessible and abundant, this source results in the isolation of stem cells that is 500 times more than the ones obtained from the bone marrow. Adipose tissue-derived MSCs have stronger immunosuppressive effects but have inferior osteogenic and chondrogenic potential as compared to the potential seen in BM-MSCs. The frequency of colony-forming cells from dental pulp is high compared to those from bone marrow, and the source materials are easily accessible as dental surgeries are fairly common. However, ectomesenchymal and periodontal tissues can affect the properties of dental pulp-derived MSCs [28]. MSCs derived from birth-related tissues (amnion, placenta and umbilical cord) demonstrate higher expansion and engraftment capacity, but these cells are not as useful as those from bone marrow or blood in terms of osteogenesis [25]. Obtaining MSCs from different tissues will demonstrate various characteristics that may differ due to the tissue source, health condition, and age of the donor. Thus, researchers have begun to differentiate MSCs from pluripotent stem cells, to circumvent the drawbacks of tissue-derived MSCs.
MSCs can be derived from pluripotent stem cells including human embryonic stem cells (hESCs) and induced pluripotent stem cells (iPSCs) [54, 55]. Despite no direct sequencing comparisons between pluripotent stem cell-derived MSCs and BM-MSCs, iPSC-MSCs indeed express typical MSC surface markers and undergo adipogenesis, osteogenesis, and chondrogenesis similar to that observed in adult BM-MSCs [55–57]. The functional characteristics of iPSC-MSCs have made the cells usable for tissue engineering and cellular therapeutics. More importantly, MSCs derived from pluripotent stem cells display a higher proliferative capacity and telomerase activity. These cells have a higher proliferative capacity (more than 50 passages), and lower cell senescence than that observed in BM-MSCs [55, 57, 58]. We also observed no teratogenic effects of iPSC-MSCs in animal studies, implying the safety of using iPSC-MSCs [55]. Furthermore, iPSC-MSCs from aged individuals were reported acquire a rejuvenation signature, which circumvents the ageing-associated drawbacks [59]. A very large number of functional MSCs can be clonally generated from a single-cell level, which maintains the homogeneity and functional quality of MSCs.
Moreover, compared with BM-MSCs, iPSC-MSCs are more insensitive to pro-inflammatory interferon (IFN)-γ-induced HLA-II expression, exhibiting stronger immune privilege, superior survival rates, and improved engraftment after transplantation. This means that pluripotent stem cell-derived MSCs have a stronger advantage in allogeneic transplantation [58]. Recently, the use of adult tissues, especially bone marrow, as a source of MSCs has decreased [60]. However, pluripotent stem cell-derived MSC-based therapy is in the early investigational stage and is not ready for clinical application as many challenges remain to be overcome. For instance, there are ethical issues in hESC application. Will the original tissue/cell of iPSCs ultimately affect the function and effect of MSCs in different diseases? Will iPSC reprogramming cause genome instability? Genome sequencing should thus be carried out to verify the correctness of each base in iPSCs. Direct comparisons using advanced techniques such as RNAseq indicating that pluripotent stem cell-derived MSCs are similar to MSCs derived from adult tissues will be favourable. The reprogramming method may also affect the function of MSCs, but existing reprogramming methods such as those using small molecular compounds can avoid the hidden dangers posed by virus-mediated reprogramming.
MSC functions
In addition to cells of the mesodermal lineage (i.e., adipocytes, chondrocytes, osteoblasts and skeletal myocytes), MSCs also can differentiate into cells of ectodermal origin and endodermal origin, such as hepatocytes and neuron-like cells [61, 62]. Significant progress has been achieved in tissue regeneration using MSCs in de-cellularized or synthetic scaffolds [63]. However, the encouraging regenerative potential of MSCs is mainly validated by in vitro functional assays. Upon allogeneic transplantation, MSCs have shown protective effects in a variety of injured models including damaged bone, cartilage [64], hepatic [65], myocardial [66], and neural tissues [67]. However, the therapeutic effects of MSCs are not attributed to poor cell retention [68].
It is becoming increasingly evident that the therapeutic effects of MSCs are largely attributed to the immunomodulatory function. MSCs exert immunomodulatory and anti-inflammatory effects by regulating lymphocytes associated with both innate and adaptive immune systems [68]. It is well documented that MSCs regulate the immune response in many diseases [69]. Accumulating evidences have demonstrated that MSCs can regulate T cell proliferation, function, balance T-helper (Th)1 and Th2 activity [69, 70], upregulate the functions of regulatory T cells (Tregs) [71], suppress B cell functions [72, 73], inhibit natural killer (NK) cell proliferation and function [74], and prevent dendritic cell (DC) maturation and activation [6, 57, 62]. MSCs can also stimulate proliferation and cytokine secretion in innate lymphoid cells (ILCs), a new family of lymphocyte-like cells, which play an important role in innate defences against pathogens [75, 76]. MSCs can regulate their immunomodulatory functions according to the micro-environmental inflammatory conditions. The plasticity of MSCs in immunomodulation is affected by the type and intensity of inflammatory stimuli conferred on MSCs. For instance, MSCs can suppress the polarization of Th1 and Th17, and promote Th2 polarization in graft-versus-host disease (GvHD) [77]. Meanwhile, MSCs can also inhibit Th2-dominant allergy by inhibiting IL-4 and IL-13 production [7]. Furthermore, MSCs promote the responses of lymphocytes in quiescent-state peripheral blood mononuclear cells (PBMCs) from patients with allergic rhinitis [70]. MSCs exert immunosuppressive effects or contribute to the fibrotic process under acute or chronic inflammatory conditions, respectively [62, 78]. Their immunomodulatory characteristics thus make MSCs a flexible and feasible strategy for treating various diseases.
The function of MSCs is known to decline with age, a process that may be implicated in the loss of tissue homeostasis leading to organ failure and aging-related diseases [79]. The proliferative and functional activity of MSCs is destined to decline during the process of senescence. The osteogenic activity of senescent MSCs deteriorates as a function of increasing lifespan, whereas the adipogenic differentiation potential of MSCs remains unchanged or is even enhanced [80]. For osteogenic induction, early passages MSCs or strategies to prevent senescence must be considered to yield longer osteogenesis and better quality. Furthermore, the immunomodulatory functions of MSCs are also reported to be compromised due to increased reactive oxygen species and oxidative stress in aged cells [81]. Therefore, MSC senescence may have a major impact on their therapeutic function. This calls for research on senescence and the development of efficient means to rejuvenate MSCs. Recently, several strategies have been explored to rejuvenate senescent MSCs, and subsequently enhance their functions. Overexpression of neuron-derived neurotrophic factor was found to rejuvenate aged BM-MSCs and improve their function in repairing the aged heart after ischemia [82]. microRNA (miR)-10a rejuvenated aged BM-MSCs and enhanced the cardiacprotection following infarction in mice via increased paracrine effects [83]. Furthermore, overexpressing FGF 21 in MSCs may delay their senescence during passaging in vitro [84]. Indeed, rejuvenating MSCs isolated from aged individuals or patients to enhance their functions is of great importance.
Therapeutic properties of MSCs
Their regenerative and immunomodulatory properties enable MSCs as a novel strategy for treating a wide variety of diseases including autoimmune diseases [85, 86], bone and cartilage diseases [3, 87], cardiovascular diseases [88, 89], inflammatory airway disorders [6, 90], liver diseases [91, 92], muscle diseases [93], neurodegenerative diseases [94, 95], spinal cord injuries [96] and so on. The osteogenic differentiation potential of MSCs makes them successful in treating and managing bone fractures [97]. The ability of MSCs to modulate immune responses is considered as a safe and feasible strategy to treat Crohn’s disease [98], systemic lupus erythematosus (SLE) [99, 100], rheumatoid arthritis (RA) [101], GvHD [102], Type I diabetes [103] and so on. MSCs also prevent allergic airway inflammation and reduce the symptoms of severe asthma [104–108]. Administration of MSCs functionally attenuates airway hyper-responsiveness (AHR), inflammatory cell infiltration, and mucus production in animal models [104, 109–113]. Upon transplantation, MSCs have shown various favourable effects in treating neurodegenerative diseases via enhanced neurogenesis, inflammation modulation, and abnormal protein aggregate clearance [94]. Thus, MSCs have shown promising results in the clinical application of stem cell therapy.
Clinical application of MSCs
The safety, feasibility and efficacy of MSC therapy for different diseases has been extensively investigated over the past decades. The recent development of MSC-based products for treating diseases provides a bridgehead from which MSCs can be implemented in clinical utility. Considering both the ongoing and completed clinical trials, MSC-based treatment appears to maintain the promise of safety and demonstrates that MSC administration is feasible. However, despite MSC application in the early stage of clinical trials, much work is needed before MSCs can pass from the bench to the bed-side [114]. Table 2 lists some of the clinical trials with outcomes involving the administration of MSCs. Some studies have shown beneficial effects, whereas some studies have shown no effects of MSCs. These mixed and contradictory results in clinical trials hamper the application of MSCs. Among 178 registered clinical trials using umbilical cord-derived MSCs between years 2007–2017, only 16% had status-completed by 27th October, 2018. During the same time, a total of 98 clinical studies were published. Although 74% of the publications reported some promising results, only 18% of the publications showed that this treatment was safe [115]. Although the safety of MSC transplantation was confirmed, less than 40% of the studies and clinical trials with available and published results showed positive improvements in the use of MSCs for patients with amyotrophic lateral sclerosis [116]. Administration of MSCs in clinical trials exhibited beneficial effects on diabetes. However, no significant therapeutic effect was observed and the clinical measures were rapidly restored to the baseline [117]. Compared to adult MSCs, clinical trials using iPSC-MSCs have just begun. The first clinical trial using iPSC-MSCs is now underway to test the clinical efficacy in human patients with steroid-resistant acute GvHD (ClinicalTrials.gov Identifier: NCT02923375). The utilized iPSC-MSCs have been found to be safe and well tolerated in the first cohort (of eight GvHD patients) enrolled in a phase I trial (https://www.cynata.com/graftversushostdisease) [118].
Table 2.
Summary of some clinical trials with outcomes involving MSC administration
| Disease | MSC S ource |
Dosage and delivery route | Efficacy | NCT number/reference |
|---|---|---|---|---|
| Amyotrophic lateral sclerosis | Autologous bone marrow-derived MSCs | 1 × 106 cells/kg, via 2 repeated intrathecal injections | Delayed disease progression | NCT01363401 |
| Autologous adipose-derived MSCs | 1 × 107 – 1 × 108 cells, via intrathecal injection | No effect | NCT01609283 | |
| Autologous bone marrow-derived MSCs | 15 × 106 cells, via intrathecal injection | Variable effects | NCT02881489 | |
| Type 2 diabetes mellitus | Autologous bone marrow-derived MSCs | Injected into the gastroduodenal artery/ pancreaticoduodenal artery | Improvement in daily insulin requirements. Nausea and vomiting were recognized | [119, 120] |
| Placental-derived MSCs | 1.35 × 106 cells/ kg, 3 intravenous infusions at 1-month intervals | Improvements in C-peptides, HbA1c levels, and insulin dosages. Nausea and vomiting were recognized | [121] | |
| Spinal cord injury | Autologous bone marrow-derived MSCs | 8 × 106 cells, via intrathecal administration | Improvement in ASIA score, EMG, and SEP; improvement in MRI imaging | [122] |
| Autologous bone marrow-derived MSCs | 89.7 × 106 cells, via intra-arterial or intravenous administration | No significant improvement | [123] | |
| Autologous bone marrow-derived MSCs | 1 × 106 cells, via intrathecal administration | Variable patterns of recovery | [124] | |
| Autologous bone marrow-derived MSCs | 7 × 105 to 1.2 × 106 cells, via intrathecal administration | Positive trend, but not statistically significant | [125] | |
| Stroke | Autologous bone marrow-derived MSCs | 50–60 × 106 cells, via intravenous administration | No improvement in all clinical scores | [126] |
| Autologous bone marrow-derived MSCs | 4.57 × 107 MSCs per intravenous infusion were administered amounting to 8.54 × 105 per kilogram body weight at two occasions (4 weeks apart) | Improvements in motor disability and cognitive impairment | [127] | |
| Umbilical cord-derived MSCs | 5 × 106–1 × 107 cells, via intraventricular administration | Safe and feasible | [128] |
The contradictory results in MSC clinical application may be caused by the heterogeneity of MSCs, which is the main problem that restricts the therapeutic benefit of MSCs. The heterogeneity of MSCs is influenced by the key parameters of MSCs including donor origin, tissue origin, passage number, expansion protocol, delivery dosage, route and so on. Additionally, multiple factors including the culture condition, the exact diseases intended to be targeted, and the local conditions of administration may also affect the immunomodulatory function of MSCs. These factors directly affect the outcome of MSC-based application. More importantly, many clinical trials have similar limitations in examining the effects of MSCs, including small size, lack of control arms in some cases, and inconsistent methods of isolating and using MSCs. Homogeneity and quality control are the most critical issues for the clinical application of MSCs. Larger studies with more randomized, blinded, strictly-regulated trials and longer follow-up times that show the beneficial effects of MSCs are also needed. This implies that the efforts of researchers and clinicians will focus on revealing the mechanisms that affect the effects of MSCs.
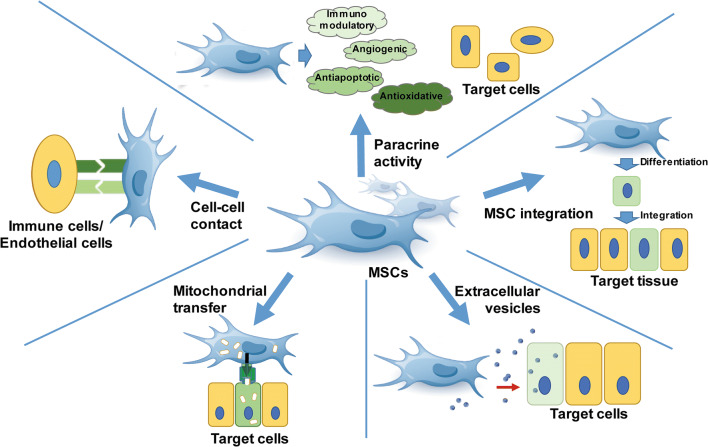
Mechanisms underlying MSC-based therapy
The therapeutic potentials of MSCs are mainly attributed to two aspects: first, replacement of the damaged tissue by differentiating into various cell lineages, and the second, regulation of immune responses by immunomodulatory function. Rather than long-term engraftment and differentiation of the integrated MSCs, a growing body of studies has shown that the protective effects of MSCs for damaged and diseased tissues are attributed to alternative immunomodulatory modes. The major mechanism underlying MSC-based therapy is the paracrine function, which secretes a variety of soluble factors to exert immunomodulatory, angiogenic, antiapoptotic and antioxidative effects [129, 130]. Cell–cell contact enables MSCs to modulate their immunosuppressive effects and promote cell viability. MSCs can transfer mitochondria to injured cells via tunnelling nanotubes (TNT) [131, 132]. Furthermore, MSCs reduce inflammation and increase cell proliferation during tissue repair via releasing exosomes that contain reparative peptides/proteins, mRNA, and microRNA (miRNA) (Fig. 2) [133, 134].
Fig. 2.
Mechanisms underlying MSC-based therapy. MSCs rescue and/or repair injured cells via differentiation into replacement cell types and by modulating immune responses. The immunomodulatory modes of MSCs include paracrine activity, cell–cell contact and interaction, mitochondrial transfer, and release of extracellular vesicles. The mechanisms involved in repair are not equivalent and MSCs can adapt their therapeutic effects according to diverse local microenvironments. MSCs mesenchymal stem cells
Integration of differentiated MSCs
MSCs have remarkable differentiation potential. After transplantation, differentiated MSCs can successfully integrate into the diseased host tissue. Integration of stem cells is necessary for the improvement of endogenous tissue repair, in order to replace the dead or damaged cells. MSCs and their progenitors can differentiate into chondrocytes and undergo chondrogenesis [135–137]. MSCs can differentiate into cardiomyocyte-like cells, integrate into host tissue, and enhance resident cell activity [138]. With the help of nano-biomaterials, MSCs have achieved better differentiation and functional integration for repairing myocardial infarction repair [139–141]. Transplanted MSCs can integrate into partially hepatectomized or toxic-injured liver for hepatic regeneration [142, 143]. Integration of MSCs has also demonstrated promising results in the treatment of neurodegenerative diseases. MSCs can integrate into the parenchyma of both the brain and the spinal cord. Intraparenchymal delivered MSCs were proven to be safe, and significantly delayed the loss of motor neurons [144]. Tzameret et al. found that intravitreally injected MSCs ameliorate retinal degeneration by integrating into the neural layers of the damaged retina [145]. Moreover, analysis of tissues after MSC transplantation revealed cell fusion between transplanted MSCs and cells of the recipient, albeit at a low frequency. MSC fusion was observed in many organs such as the brain, retina, the liver, muscles, and the gut where they participated in the reestablishment of tissue function [146]. The exact biological implication of MSC fusion is unclear. However, it is worth mentioning that cell fusion between MSCs and cancer cells enhances metastatic capacity and the characteristics of cancer stem cells by undergoing epithelial-mesenchymal transition, which is considered a key cell event in the process of tumour metastasis and invasion [147, 148]. Overall, the engraftment and differentiation efficacy of MSCs post-transplantation is very low which heavily limits their therapeutic effects. The differentiation potential of MSCs largely depends on donor age, tissue origin, cell passage numbers, cell densities, duration of cell culture and so on. Therefore, further investigation is needed to reveal the mechanisms of regulatory pathways and improve differentiation efficacy.
Soluble factors
Immunomodulatory factors
The low immunogenicity makes MSCs eligible for allogeneic transplantation. MSCs can inhibit CD4+ cell, CD8+ T cell, and NK cell proliferation and DC maturation, suppress plasma cell immunoglobulin production, and stimulate Treg proliferation by secreting transforming growth factor-β (TGF-β), hepatocyte growth factor (HGF), inducible indoleamine 2,3-dioxygenase (IDO), human leukocyte antigen class I molecule (HLA)-G5, prostaglandin E2 (PGE2), interleukin (IL)-6, IL-10, TNFα-stimulated gene protein (TSG)-6 and so on. Bartholomew A. et al. showed that MSCs suppress lymphocyte proliferation, alter lymphocyte reactivity to allogeneic target cells, and prolong skin graft survival following intravenous administration in MHC-mismatched baboons [149]. Furthermore, Di Nicola et al. demonstrated that soluble factors secreted by MSCs partly contribute to immunomodulatory capacity in a co-culture of MSCs with T-lymphocytes in a Transwell system, which excludes cell–cell contact. TGF-β or HGF are involved in the inhibition of T cell proliferation by the addition of a monoclonal antibody in the system [150]. The secreted TGF-β promotes the differentiation of naive T cells into Treg cells, thus improving systemic immune tolerance [151]. Furthermore, Zhong et al. demonstrated that the TGF-β1/Smad signalling pathway is involved in the immunomodulatory effects of MSCs in chronic allergic airway inflammation [152]. MSCs primed with IFN-γ will secrete IDO, which subdues the T-cell response to autoantigens and foetal alloantigens [153]. Furthermore, IDO catalyses the conversion of tryptophan to kynurenine, which inhibits T-cell proliferation [154]. Additionally, the primed MSCs secrete programmed death-ligand 1 (PD-L1), which co-inhibits the adaptive immune response in tissue allografts, autoimmune disease and other diseases [155]. MSC-secreted HLA-G5 suppresses T lymphocytes and NK function, and induces the expansion of CD4+CD25highFOXP3+ Treg cells [71]. MSCs regulate adaptive immune responses by secreting PGE2, which induces DCs to upregulate the anti-inflammatory cytokine IL-10, while reducing the secretion of pro-inflammatory tumour necrosis factor (TNF)-α and IL-12 [156, 157]. This will convert the pro-inflammatory Th1 cells to the anti-inflammatory Th2 cell phenotype. Meanwhile, naïve T cells differentiate into Treg cells, which further decrease the total number of T helper cells [156]. Moreover, MSCs exert immunomodulatory effects by secreting IL-6, which inhibits lymphocytes apoptosis [158]. In addition, MSC-derived nitric oxide (NO) [159], leukaemia inhibitory factor (LIF) [160], galectin-1, and semaphorin-3A [161] inhibit T lymphocyte proliferation. LIF suppresses T cell proliferation as well as promotes and maintains Tregs [162].
MSC-derived soluble factors also modulate macrophage behaviour. The pro-inflammatory phenotype M1 (classical-activated macrophage) transits to the anti-inflammation phenotype M2 (alternative-activated macrophage) in the presence of MSCs [163]. Tsyb et al. demonstrated that MSC-derived TSG-6, via the CD44 receptor, ameliorates macrophages to secrete inflammatory factors by inhibiting NF-κB activity. TSG-6 also inhibits the maturation and function of DCs [164, 165]. Zhang et al. found that galectin-1 from MSCs stimulates the formation of a tolerance immunophenotype on DCs via regulating the MAPK signalling pathway in DCs, thereby inhibiting their function [166]. The immunomodulatory effects of MSC-derived factors have been observed during both the antigen recognition/presentation stage and T cell activation stage of the immune response. Recent studies have shown that the immunosuppressive potency of MSCs is predominantly mediated by key molecules including Rap1 and IDO1 [167, 168]. Furthermore, novel strategies including hypoxia preconditioning and chemical pre-treatment can significantly enhance the immunosuppressive potency of MSCs [169, 170].
MSCs mediate immune responses via diverse modes of action. MSCs can be either immunosuppressive or immune-enhancing depending on the soluble factor levels in the microenvironment. Li et al. found that the degree of NO production acts as a switch in MSC-mediated immunomodulation. MSCs tend to promote T cell proliferation rather than immunosuppression when inducible nitric oxide synthase (iNOS), one of three key enzymes generating NO, is blocked. The level of iNOS/IDO plays a critical role in determining the pathophysiological roles of MSCs [171]. Cuerquis et al. further confirmed that MSCs induce a transient increase in IFN-γ and IL-2 synthesis by activating T cells before suppressing T-cell proliferation [172]. Therefore, in addition to MSC isolation protocols, their origins and dosages, the inflammatory state and level of soluble factors in immune diseases must also be considered before MSC intervention.
Angiogenic factors
It has been proven that the angiogenic (the sprouting of existing vessels) and arteriogenic (the growth of collateral vessels) properties of MSCs contribute to the amelioration of hind limb ischemia, coronary artery disease, and skin wound repair [55, 58, 173–176]. Angiogenesis is a complex multistep process that forms new blood networks, which requires endothelial cell growth and differentiation-associated soluble growth factors such as vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF) [177]. MSCs secrete VEGF, FGF, HGF, placental growth factor (PGF), monocyte chemotactic protein 1 (MCP-1), stromal cell-derived factor 1 (SDF-1), and angiopoietin-1 (Ang-1) that are critical for vascularization [178–183]. Several studies have reported the potential of increasing capillaries and newly formed vessels following MSC administration both in vitro and in vivo [184–186]. Hung et al. demonstrated that angiogenic factors including IL-6, MCP-1, and VEGF in MSC-conditioned medium inhibit apoptosis, increase survival, and stimulate angiogenesis of endothelial cells under hypoxic challenge [179]. IL-6 promotes angiogenesis and survival of endothelial cells [187]. MCP-1 has been proven as a critical chemoattractant for angiogenesis [188]. VEGF can promote MSC differentiation as well as regulate endothelial cell migration, differentiation and endothelialisation via activation of the mitogen-activated protein kinase (MAPK), phosphoinositide-3-kinase and Akt (PI3K/AKT), Src, and Rac pathways [189]. Overexpression of Erb-B2 receptor tyrosine kinase 4 (ERBB4) can rejuvenate aged MSCs and stimulate angiogenesis by regulating the PI3K/AKT and the MAPK/ERK pathways, leading to increased therapeutic effects for myocardial infarction [190]. MSCs promote angiogenesis via the SDF-1/C-X-C chemokine receptor type 4 (CXCR4) axis [191]. Moreover, Dong et al. found that myocardial CXCR4 is required for MSC-derived SDF-1, meditating repair in acute myocardial infarction [192]. MSC-derived angiogenic factors such as SDF-1 and HGF promote local angiogenesis [193, 194]. SDF-1 stimulates endothelial cell proliferation and capillary tube formation, whereas HGF promotes tyrosine phosphorylation in endothelial cells and smooth muscle cells via the c-Met receptor [195, 196]. Further, MSC-derived angiogenic soluble factors improve angiogenesis and restore blood supply in ischemic areas. However, it is unclear whether MSC-derived soluble factors account for the dominant mechanisms of action. The importance of hibernating cells and susceptible cells in the local region should also be considered [129, 197].
Anti-apoptotic factors
The multiple roles of apoptosis in regulating various physiological and pathological functions implicate its significance in disease treatment [198]. Moreover, MSCs can synthesise and secrete B-cell lymphoma 2 (BCL-2), survivin, VEGF, HGF, insulin-like growth factor-I (IGF-I), stanniocalcin-1 (STC1), TGF-β, FGF, and granulocyte–macrophage colony-stimulating factor (GM-CSF), which inhibit cellular apoptosis and restore tissue homeostasis [198–203]. BCL-2 is a classic inhibitor of apoptosis. An increased ratio of BCL-2 to BCL-2-associated X protein (BAX) results in cells that are less sensitive to the pathological stimuli and prevents cells from responding to apoptotic signals [204, 205]. Transplantation of autologous MSCs significantly downregulates Bax expression levels in the ischemic myocardium [206]. Zhang et al. demonstrated that the Bcl-2 signalling pathway, together with PI3K/Akt, closely participates in the anti-apoptotic action of MSCs against stroke [207]. Pan et al. demonstrated that MSCs ameliorate hepatic ischemia/reperfusion injuries via inactivation of the MEK/ERK signalling pathway in rats. Meanwhile, MSC-conditioned medium could down-regulate Bax, TNF receptor superfamily, member 6 (FAS), and caspase 3 (CASP3) levels in a human normal liver cell line under ischemic conditions, indicating the anti-apoptotic effects of MSC paracrine function [208]. MSC-derived chemokine (C motif) ligand (XCL1) has been reported to inhibit apoptosis in C2C12 cells [198]. However, direct XCL1 treatment showed no anti-apoptotic capacity.
In addition to the direct inhibition of apoptosis, MSC-secreted factors enhance cell survival by suppressing apoptotic pathways. The levels of VEGF, HGF, IGF-I, FGF, and GM-CSF in MSC culture medium have been found to be significantly elevated under hypoxic conditions [201]. Notably, upregulation of VEGF under hypoxia is greater than that of the other factors [199]. VEGF has been reported to inhibit serum starvation-induced vascular endothelial cell apoptosis via upregulating Bcl-2 expression [209]. VEGF also contributes to suppressing p53-mediated apoptosis via the activating phosphorylation of focal adhesion kinase (FAK), which is essential for regulating cell survival [210, 211].
Antioxidative factors
Reactive oxygen species (ROS), including oxygen ions, oxygen-free radicals, and peroxides, are byproducts of normal aerobic metabolism. ROS are involved in the regulation of multiple signalling pathways including cell proliferation, survival, and inflammation [212–214]. An imbalance between levels of ROS and antioxidant function leads to ROS-related diseases such as ageing, carcinogenesis, immune disorders, inflammation, multiple sclerosis, and neurodegeneration [129, 215]. Further, MSCs modulate the redox context via secretion of STC1, heme oxygenase-1 (HO-1), and glial-derived neurotrophic factor (GDNF) [216–218]. MSC-derived STC1 reduces ROS-induced apoptosis. Liu et al. demonstrated that STC1 suppresses angiotensin II-induced superoxide generation in cardiomyocytes via the uncoupling protein 3 (UCP3)-mediated anti-oxidant pathway [219]. Moreover, MSC-derived STC1 enhances the uncoupling respiration of mitochondria, reduces oxidative stress, and promotes the survival of alveolar epithelial cells under harmful microenvironments via upregulation of uncoupling protein 2 (UCP2) [220]. Furthermore, Ono et al. found that STC1 contributes to the ability of MSCs to ameliorate lung fibrosis via inhibition of the ROS/endoplasmic reticulum stress (ER-stress)/TGF-β1 pathway [221]. Oh et al. found that STC1 can also respond to activated macrophages by inhibiting activation of the NLRP3 inflammasome, which decreases mitochondrial ROS production [222]. MSC-derived antioxidative enzyme HO-1 protects against oxidative injury. Allogeneic MSC transplantation ameliorates the redox environment via upregulating HO-1 in a rat model of lipopolysaccharide (LPS)-induced acute lung injury [217]. Chen et al. further demonstrated that HO-1 exerts a protective effect by elevating the activity of nuclear factor-erythroid 2 (NF-E2) p45-related factor-2 (Nrf2), which is a transcription factor mediating the Nrf2-antioxidant response element signalling pathway [223, 224]. HO-1 also attenuates LPS-induced inflammatory and oxidative damage via the enhanced paracrine function of stem cells. Zarjou et al. found that the production of HGF, SDF-1 and VEGF is significantly reduced in HO-1−/− MSCs [225]. MSCs exert localized neuroprotection from oxidative stress by the secretion of GDNF [218, 226]. Lv et al. found that GDNF possibly prevents and repairs neuronal injury by regulating the MEK/ERK and the PI3K/AKT signalling pathways [227]. MSCs secrete different antioxidative factors in different experimental settings and diseases, probably due to the variation of ROS in localized microenvironments.
Cell–cell contact
MSCs exert their modulatory functions to host cells at damaged sites via paracrine action and direct cell–cell contact. MSCs modulate both autologous and allogeneic T lymphocytes via the expression of integrins (alpha 1 – alpha 6, alpha V, and beta 1 – beta 4), intercellular adhesion molecules (ICAM-1, ICAM-2), vascular cell adhesion protein (VCAM)-1, CD72, and CD58 (LFA-3) on their surfaces [6]. Accumulating evidence has shown that MSCs modulate T cells by the negative costimulatory molecule B7-H4, Fas-L/Fas interaction, or PD-L1/programmed death-1 (PD-1) pathways [228–230]. Kovach et al. demonstrated that the expression of ICAM-1 and VCAM-1 on MSCs is critical for maintaining their immunomodulatory functions on various subtypes of T cells [231]. The expression of PD-1 ligand on the surface of MSCs is critical for the contact-dependent inhibition of allogeneic Th17 differentiation [232]. Galectin-1 and galectin-3 are necessary for MSCs to inhibit the proliferation of CD4+ and CD8+ T cells [233].
Direct cell–cell contact is required for MSCs to induce Treg cells and in allergic diseases [106, 234]. It has been reported that increased gene expression of the Notch ligand, Delta-like 1, is essential for augmented Treg cell induction by toll-like receptor (TLR)-activated MSCs, which is dependent on cell–cell contact [7]. In addition, MSCs require cell–cell contact to reduce NK-cell cytotoxicity [235]. When co-cultured with MSCs, NK cells acquire CD73 expression, which makes the cells capable of converting adenosine 5′-monophosphate into adenosine for immunomodulatory purposes [236]. Li et al. found that cell–cell contact with pro-inflammatory macrophages enhances TSG-6 production by MSCs, thereby elevating the immunomodulatory effect of MSCs on T cells and macrophages. Pro-inflammatory macrophages in contact with MSCs also upregulate CD200 on stem cells, and skew the reprogramming of macrophages towards an anti-inflammatory phenotype through the interaction of CD200 with CD200R on pro-inflammatory macrophages [237]. Zhang et al. found that MSCs drive mature DCs to differentiate into regulatory DCs via contact-dependent activation of Jagged-2 [238]. Furthermore, direct cell–cell contact between MSCs and endothelial progenitor cells induces MSC differentiation towards a pericyte-like phenotype, which may benefit angiogenesis for cell-based tissue-engineered bone grafts [239]. However, intravenously administered MSCs inhibit endothelial cell proliferation and angiogenesis via cell–cell contact through modulation of the VE-Cadherin/β-catenin signalling pathways [240]. Therefore, the contact-dependent factors affecting the biology of adjacent responder cells and tissues should be carefully considered for optimization of the strategies involving MSCs.
Mitochondrial transfer
Mitochondria play important roles in the regulation of oxidative phosphorylation, generation of ATP, and cellular apoptosis. Dysfunctional mitochondria lead to excessive ROS production and cause oxidative damage in cells [241]. Accumulating evidence has suggested that mitochondrial transfer from MSCs is a novel strategy for the regeneration of various damaged cells via rescue of their respiratory activities. Accumulating evidence has shown that mitochondrial transfer occurs via TNTs, gap junctions, microvesicles, cell fusion and transfer of isolated mitochondria [132, 242–245]. So far, mitochondrial transfer from MSCs has demonstrated protective effects in lung injury, bronchial epithelial injury, allergic diseases, damaged cardiomyocytes, alkali-burnt corneal epithelial cells, kidney injury, ischemic damage, neurotoxicity, and spinal cord injury [132, 246–253]. Numerous studies have identified several signals including release of damaged mitochondria, mtDNA and mitochondrial products along with elevated ROS levels that trigger mitochondrial transfer from MSCs to the recipient cells [241].
Mitochondrial transfer through TNT has been intensively investigated between MSCs and damaged cells. Miro1 (mitochondrial Rho-GTPase 1, synonym: RhoT1), a calcium-sensitive adaptor protein, has been identified as one of the key regulators in mediating the transport of mitochondria. Miro1 binds the mitochondria to KIF5 motor protein together with other accessory proteins like Miro2, TRAK1, TRAK2, Myo10, and Myo19, thus forming a motor-adaptor complex that coordinates the mitochondrial movement at intercellular and intracellular levels [241, 242]. Knock-down of Miro1 in MSCs inhibits mitochondrial donation, thus reducing their therapeutic effects in bronchial epithelial injury [254]; in contrast, Miro1overexpression in MSCs leads to enhanced beneficial effects [242, 255, 256]. Apart from Miro1, Zhang et al. found that TNF-α induces TNT formation in MSCs via the TNF-α/NF-κB/TNFαIP2 signalling pathway, which facilitates mitochondrial transfer to cardiomyocytes. It has been reported that ROS signals can stimulate TNT formation [251]. Moreover, connexin 43 (CX43) is involved in regulating mitochondrial transfer from MSCs via TNT formation. CX43 overexpression in iPSC-MSCs enhances TNT formations and improves the mitochondrial transfer efficacy between MSCs and damaged epithelial cells. Knock-down of CX43 reduces TNT formation and thus decreases mitochondrial transfer from MSCs to damaged epithelial cells, impairing their immunomodulatory effects during allergic airway inflammation [105].
Additionally, gap junction channels play a critical role in mediating the mitochondrial transfer of MSCs. Islam et al. revealed that MSCs formed CX43-containing gap junction channels with alveolar epithelia in mice with acute lung injury, and released mitochondria-containing microvesicles that were subsequently engulfed by the epithelia. MSCs with genetically modified CX43 failed to adhere to alveolar epithelium and transfer mitochondria [132]. Pacak et al. demonstrated that cardiomyocytes could uptake the mitochondria isolated from MSCs through actin-dependent endocytosis [257]. Sinclair et al. summarized different modes of intercellular communication and mitochondrial transfer by MSCs. Retinoic acid, a gap junction potentiator, greatly enhances the mitochondrial transfer efficiency from BM-MSCs to neurons, and this effect is partially abrogated by 18β glycyrrhetinic acid, which is a gap junction potentiator [253]. Inhibiting microtubule/TNTs, gap junction formation, or microvesicle endocytosis abrogates the transfer of cytoplasmic material from MSCs to epithelial cells [258]. Notably, MSCs can donate mitochondria to macrophages via extracellular vesicles, thus promoting an anti-inflammatory macrophage phenotype in acute respiratory distress syndrome [259]. Different pathophysiological conditions may initialize different modes of mitochondrial transfer, though their potential mechanisms remain unclear. Therefore, clarifying the relative mechanisms involved in mitochondrial transfer will advance the understanding of molecules involved in this process and serve to improve MSC treatment.
Extracellular vesicles (exosomes)
Extracellular vesicles (EVs), the membrane-bound vesicles released by somatic cell, are involved in tissue repair, immunomodulation, and proliferation [260–262]. EVs are classified into exosomes (30–150 nm endosome-derived plasma membrane-coated vesicles), microvesicles (100–1000 nm non-endocytic origin vesicles) and apoptotic bodies (1–5 μm vesicles released by apoptotic cells) according to their size and biogenesis. The most common EV markers are ALG-2-interacting protein X (Alix), tetraspanin proteins CD9, CD63, CD81 and heat-shock protein (Hsp)60, Hsp70, and Hsp90. In addition, MSC-released EVs express unique surface antigens including CD44, CD73, CD90 and CD105 [263].
EVs, especially exosomes purified from MSCs have attracted great attention due to their regenerative, immunomodulatory, and even anti-tumour properties. Over the past decade, MSC-EVs have been found to exhibit various biological effects and have emerged as a novel approach for treating a variety of diseases. They overcome some limitations of MSC-based therapies including allogeneic immune rejection, malignant transformation, and premature cell differentiation. EVs have the unique capability to cross the blood–brain barrier, which is very important in the treatment of neurological disorders [263]. This means that EVs have better advantages in the clinic in the treatment of nervous system diseases as compared to the therapeutic potential of MSCs. Moreover, MSC-EVs can avoid the risk of genetic changes associated with stem cell transplantation for the treatment of nerve disorders [264, 265]. Remarkably, MSC-EVs can be modified to carry specific proteins or genes that promote cellular function and tissue repair. These characteristics make the EVs an ideal candidate of treatment for regenerative medicine.
MSC-EVs enhance angiogenesis owing to their specific protein and transcript contents related to angiogenic and proliferative function [266, 267]. Anderson et al. further demonstrated that the protein content in MSC exosomes mediates angiogenesis via regulation of the NF-κB signalling pathway [267]. Nakamura et al. reported that MSC-derived exosomes promote muscle regeneration by enhancing angiogenesis and myogenesis, which is partially mediated by miR-494 [268]. Feng et al. demonstrated that miR-22 in MSC exosomes prevents apoptosis and reduces the infarct size in the heart by targeting methyl CpG binding protein 2 (Mecp2) [269]. In addition, miR-223 in MSC-EVs is involved in mediating cardioprotection via targeting semaphorin-3A (Sema3A) and transcription 3 (Stat3) [270]. miR-19a contributes to the anti-apoptotic effects of MSC exosomes in cardioprotection [271]. MSC exosomal miRNAs (miR-21, miR-23a, miR-125b and miR-145) contribute to the suppression of myofibroblast formation by inhibiting TGF-β2/Smad2 signalling and reducing scar formation during wound healing [272]. Tomasoni et al. reported that MSC exosomes improve renal cell survival and proliferation by transferring the mRNA for insulin-like growth factor 1 receptor (IGF-1R), which increases the sensitization of proximal tubular cells to IGF-1 [273]. Currently, several strategies are under exploration that aim to enhance the exosomes released from MSCs. Hypoxia can facilitate MSCs to release exosomes, thus improving repair of cardiac tissues in a mouse model of myocardial infarction [274]. Compared with MSCs, exosomes derived from SDF1-overexpressing MSCs show enhanced therapeutic effects in myocardial infarction by increasing cardiac endothelial microvascular regeneration and inhibiting cardiomyocyte apoptosis in mice [275].
MSC-EVs modulate the immune system by induction of anti-inflammatory cytokines and Treg cells, by inhibition of B lymphocytes, regulation of macrophage polarization, and mobilization of neutrophils [260, 276]. Zhang et al. found that MSC-derived exosomes induce monocytes to differentiate into macrophages via the myeloid differentiation primary response gene 88 (MYD88)-dependent TLR signalling pathway. Exosome-induced macrophages lead to Treg cell expansion by secretion of more IL-10 as compared to the macrophages induced by lipopolysaccharide [134]. miR-146a enhances macrophage polarization to anti-inflammatory M2 macrophages [271]. Di Trapani et al. further demonstrated that the immunosuppressive effect of EVs on T cells, B cells, and NK cells is also mediated by PD-L1 expression on their surface [277]. Additionally, Galectin-1, an endogenous leptin on the EV surface, was also found to be involved in the immunosuppressive effects on T lymphocytes [278]. Kerkela et al. also emphasized the importance of 5′-ectonucleotidase (CD73), which actively produces immunosuppressive adenosine [279].
MSC-EVs have shown positive outcomes in treating cancer. Anti-angiogenic miRNAs such as miR-16 and miR-100 have been identified in MSC exosomes, which suppress angiogenesis by targeting VEGF in breast cancer cells [133, 280]. However, the crosstalk between MSCs and tumour cells through EVs can function either as a tumour suppressor or as a promoter [281, 282]. MSC exosomes may transfer CD73 on tumour cells, which can reduce activation of NK cell and T cell by metabolism of AMP to adenosine [283]. So far, MSC-derived exosomes have been reported to be involved in tumour growth, angiogenesis, metastasis, and invasion [284]. The discrepancy between these controversial behaviours may arise from issues related to different MSC sources, tumour types, stages of tumour growth, and genotypes. Therefore, the potential side effects of EV therapy must be carefully evaluated.
The target cell profile
One of the major mechanisms underlying MSC-based therapy is interaction with target cells. MSCs modulate their immunomodulatory effects by suppressing the proliferation and activity of T cells, promoting Treg cells, regulatory DCs and M2 macrophages in a myriad of inflammatory diseases [285]. In case of T cell suppression, Lin et al. examined the mRNA expression profiles in mouse T lymphocytes after MSC administration and found that 5 mRNAs including Ccl11, Ccl24, Il13, Il33, and Ear11 were significantly altered [109]. Wang et al. further identified more than 800 differentially expressed long non-coding RNAs (lncRNAs) in mouse T lymphocytes, and lncRNAs MM9LINCRNAEXON12105+ and AK089315 were finally identified as potential targets of MSC treatment in T cells [107]. MSCs and Treg cells have been found to work and interact in a synergistic manner. Engela et al. demonstrated that Treg cells can induce IDO secretion in MSCs, which results in TNF-α reduction and induction of IL-10 in Treg cells and effector cells [286]. Different subtypes of Treg cells generated by MSCs have been identified including CD4+CD25+Foxp3+ Treg cells and IL-10 producing type 1 Treg (Tr1) cells [287]. There is a complex cross-talk between MSCs and macrophages, which cannot be simply explained by MSC-derived anti-inflammatory factors. Braza et al. found that macrophages can phagocytose MSCs and alter their pro-inflammatory signature to M2 suppressive phenotype following contact with dead MSCs [288]. This behaviour may explain the profound long-term effects of MSC therapy. Therefore, the presence of MSCs alters the targeted cell profile, which in turn leads to further activation or ‘licensing’ of MSC therapy.
Challenges in MSC-based therapy
MSC-based therapies have made great progress over the last decades. However, the publications/clinical trials with mixed and contradictory results are preventing the advancement of MSCs into daily clinical application. These disparities are probably due to the large variability in key factors such as cell source (tissue, donor), dosage, administration route, and administration timing. Inconsistencies among these parameters significantly limit the therapeutic value of MSCs. Therefore, standardization of procedures of MSC isolation and expansion is crucial for upcoming clinical therapeutics. The in vivo administration route, timing, and dosage also require optimization. In this circumstance, an understanding of the characteristics and functional mechanisms of differently sourced MSCs is required. The therapeutic benefits of MSCs are contributed by their differentiation potential and immunomodulatory capacity. These potentials are strongly influenced by the tissue source of MSCs, the age and health condition of the donor or the ex vivo culture conditions before administration. Furthermore, the indications of the local disease microenvironment where MSCs are intended to be applied also determine the benefits of MSCs. As a result, preconditioning strategies are developed that boost the differentiation or immunomodulatory potential of MSCs in such scenarios. Hypoxic preconditioning is employed since physiological environments are often hypoxic, and MSCs cultured under such condition show enhanced viability and secretion of cytoprotective molecules. However, slight variations in the oxygen level may significantly influence the function of MSCs as they are highly sensitive to oxygen tension [289]. Preconditioning with cytokines such as IFN-γ or TNF-α enhances immunomodulatory factor secretion by MSCs, but such effects have been reported as temporary [69, 290]. Alternative tissue engineering approaches including three-dimensional culture and hydrogel encapsulation were employed to enhance MSC functions [291, 292]. The therapeutic potentials of MSCs are attributed to complex cellular and molecular mechanisms of action, and such mechanisms still require in-depth exploration for clinical application. Current researches have made great progress and are gaining advancements in enhancing the therapeutic properties of MSCs and creating specific criteria to establish the basics for clinical application of MSCs. Moreover, senescence of MSCs has also attracted significant attention during the past years. MSCs can only undergo very limited cell passages and prolonged expansion, inevitably leading to replicative senescence. MSCs isolated from aged individuals or from patients also exhibit a senescent phenotype and display decreased function.
Conclusion
The advantages of MSCs in immunomodulation and tissue repair have rendered the cells an important source for stem cell therapies. The potential and eligibility of allogeneic cells makes MSCs desirable for cellular transplantation. Based on the promising results in preclinical and clinical studies, the emerging commercially available MSC-based products have been approved globally. However, larger studies with more randomized, blinded, and controlled trials are desired to demonstrate the beneficial effects of MSCs. This implies that the mechanisms underlying MSC-based therapy should be addressed. So far, MSCs have been intensively investigated for their differentiation capacity, paracrine effects, flexible EV release, and direct-contact modulatory functions. Each mechanism contributes to the comprehensive process of MSC therapy. Nevertheless, mechanisms underlying the protective effects of MSCs still require further elucidation. MSCs can adapt therapeutic effects during the rescue and repair of damaged tissues according to diverse local microenvironments. Therefore, the in-depth mechanisms underlying the protective effects of MSCs require further investigation. Clarification of the predominant mechanisms in different situations will improve the safety, efficacy and outcomes of MSC-based therapy.
Acknowledgements
This work was supported by grants from National Natural Science Foundation of China (81471832, 81671882, 81770984, 81970863 and 81900919), the key grant from the Science and Technology Foundation of Guangdong Province of China (2015B020225001) and the Natural Science Foundation of Guangdong Province (2014A030313051, 2016A030308017, 2017A030313105).
Abbreviations
- AHR
Airway hyper-responsiveness
- Alix
ALG-2-interacting protein X
- Ang-1
Angiopoietin-1
- ASCs
Adipose-derived stem cells
- BAX
BCL-2-associated X protein
- BCL-2
B-cell lymphoma 2
- CASP3
Caspase 3
- CX43
Connexin 43
- CXCR4
Chemokine receptor type 4
- DC
Dendritic cell
- ER
Endoplasmic reticulum
- ERBB4
Erb-B2 receptor tyrosine kinase 4
- EVs
Extracellular vesicles
- FAK
Focal adhesion kinase
- FGF
Fibroblast growth factor
- GM-CSF
Granulocyte–macrophage colony-stimulating factor
- GDNF
Glial-derived neurotrophic factor
- GvHD
Graft-versus-host disease
- hESCs
Human embryonic stem cells
- HGF
Hepatocyte growth factor
- HLA
Human leukocyte antigen
- HLA-G5
Human leukocyte antigen class I molecule G5
- HO-1
Heme oxygenase-1
- Hsp
Heat-shock protein
- ICAM
Intercellular adhesion molecules
- IDO
Inducible indoleamine 2,3-dioxygenase
- IFN
Interferon
- IGF-I
Insulin-like growth factor-I
- IGF-1R
Insulin-like growth factor 1 receptor
- IL
Interleukin
- ILCs
Innate lymphoid cells
- iNOS
Inducible nitric oxide synthase
- iPSCs
Induced pluripotent stem cells
- ISCT
International Society of Cell Therapy
- LIF
Leukemia inhibitory factor
- lncRNAs
Long non-coding RNAs
- LPS
Lipopolysaccharide
- MAPK
Mitogen-activated protein kinase
- MCP-1
Monocyte chemotactic protein 1
- Mecp2
Methyl CpG binding protein 2
- Miro1
Mitochondrial Rho-GTPase 1
- miRNA
MicroRNA
- MSCs
Mesenchymal stem cells
- MYD88
Myeloid differentiation primary response gene 88
- NK
Natural killer
- NO
Nitric oxide
- Nrf2
Nuclear factor-erythroid 2 p45-related factor 2
- PBMCs
Peripheral blood mononuclear cells
- PD-1
Programmed death-1
- PD-L1
Programmed death-ligand 1
- PGE2
Prostaglandin E2
- PGF
Placental growth factor
- PI3K/AKT
Phosphoinositide-3-kinase and Akt
- RA
Rheumatoid arthritis
- ROS
Reactive oxygen species
- SDF-1
Stromal cell-derived factor 1
- Sema3A
Semaphorin-3A
- SLE
Systemic lupus erythematosus
- STC1
Stanniocalcin-1
- TGF-β
Transforming growth factor-β
- Th
T-helper
- TLR
Toll-like receptor
- TNF
Tumour necrosis factor
- TNTs
Tunnelling nanotubes
- Tr1
Type 1 Treg
- Tregs
Regulatory T cells
- TSG
TNFα-stimulated gene protein
- UCP
Uncoupling protein
- VCAM
Vascular cell adhesion protein
- VEGF
Vascular endothelial growth factor
- XCL1
Chemokine (C motif) ligand
Author contributions
X.L.F., Y.Z., X.L. wrote the manuscript; Q.L.F. designed and wrote the manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Spees JL, Lee RH, Gregory CA. Mechanisms of mesenchymal stem/stromal cell function. Stem Cell Res Ther. 2016;7(1):125. doi: 10.1186/s13287-016-0363-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friedenstein AJ, Piatetzky S, II, Petrakova KV. Osteogenesis in transplants of bone marrow cells. J Embryol Exp Morphol. 1966;16(3):381–390. [PubMed] [Google Scholar]
- 3.Vilquin JT, Rosset P. Mesenchymal stem cells in bone and cartilage repair: current status. Regen Med. 2006;1(4):589–604. doi: 10.2217/17460751.1.4.589. [DOI] [PubMed] [Google Scholar]
- 4.Kean TJ, Lin P, Caplan AI, Dennis JE. MSCs: delivery routes and engraftment, cell-targeting strategies, and immune modulation. Stem Cells Int. 2013;2013:732742. doi: 10.1155/2013/732742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caplan AI, Dennis JE. Mesenchymal stem cells as trophic mediators. J Cell Biochem. 2006;98(5):1076–1084. doi: 10.1002/jcb.20886. [DOI] [PubMed] [Google Scholar]
- 6.Fan XL, Zhang Z, Ma CY, Fu QL. Mesenchymal stem cells for inflammatory airway disorders: promises and challenges. Biosci Rep. 2019 doi: 10.1042/BSR20182160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li F, Guo X, Chen SY. Function and therapeutic potential of mesenchymal stem cells in atherosclerosis. Front Cardiovasc Med. 2017;4:32. doi: 10.3389/fcvm.2017.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ullah I, Subbarao RB, Rho GJ. Human mesenchymal stem cells - current trends and future prospective. Biosci Rep. 2015 doi: 10.1042/BSR20150025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The international society for cellular therapy position statement. Cytotherapy. 2006;8(4):315–317. doi: 10.1080/14653240600855905. [DOI] [PubMed] [Google Scholar]
- 10.Qin Y, Guan J, Zhang C. Mesenchymal stem cells: mechanisms and role in bone regeneration. Postgrad Med J. 2014;90(1069):643–647. doi: 10.1136/postgradmedj-2013-132387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nash ME, Fan X, Carroll WM, Gorelov AV, Barry FP, Shaw G, Rochev YA. Thermoresponsive substrates used for the expansion of human mesenchymal stem cells and the preservation of immunophenotype. Stem Cell Rev. 2013;9(2):148–157. doi: 10.1007/s12015-013-9428-5. [DOI] [PubMed] [Google Scholar]
- 12.Lama VN, Smith L, Badri L, Flint A, Andrei AC, Murray S, Wang Z, Liao H, Toews GB, Krebsbach PH, Peters-Golden M, Pinsky DJ, Martinez FJ, Thannickal VJ. Evidence for tissue-resident mesenchymal stem cells in human adult lung from studies of transplanted allografts. J Clin Invest. 2007;117(4):989–996. doi: 10.1172/JCI29713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yannarelli G, Pacienza N, Cuniberti L, Medin J, Davies J, Keating A. Brief report: The potential role of epigenetics on multipotent cell differentiation capacity of mesenchymal stromal cells. Stem Cells. 2013;31(1):215–220. doi: 10.1002/stem.1262. [DOI] [PubMed] [Google Scholar]
- 14.Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, Alfonso ZC, Fraser JK, Benhaim P, Hedrick MH. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13(12):4279–4295. doi: 10.1091/mbc.e02-02-0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campagnoli C, Roberts IA, Kumar S, Bennett PR, Bellantuono I, Fisk NM. Identification of mesenchymal stem/progenitor cells in human first-trimester fetal blood, liver, and bone marrow. Blood. 2001;98(8):2396–2402. doi: 10.1182/blood.V98.8.2396. [DOI] [PubMed] [Google Scholar]
- 16.Anker PS, Scherjon SA, Kleijburg-van der Keur C, Noort WA, Claas FH, Willemze R, Fibbe WE, Kanhai HH. Amniotic fluid as a novel source of mesenchymal stem cells for therapeutic transplantation. Blood. 2003;102(4):1548–1549. doi: 10.1182/blood-2003-04-1291. [DOI] [PubMed] [Google Scholar]
- 17.Erices A, Conget P, Minguell JJ. Mesenchymal progenitor cells in human umbilical cord blood. Br J Haematol. 2000;109(1):235–242. doi: 10.1046/j.1365-2141.2000.01986.x. [DOI] [PubMed] [Google Scholar]
- 18.De Bari C, Dell'Accio F, Tylzanowski P, Luyten FP. Multipotent mesenchymal stem cells from adult human synovial membrane. Arthritis Rheum. 2001;44(8):1928–1942. doi: 10.1002/1529-0131(200108)44:8<1928::AID-ART331>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 19.Kuznetsov SA, Mankani MH, Gronthos S, Satomura K, Bianco P, Robey PG. Circulating skeletal stem cells. J Cell Biol. 2001;153(5):1133–1140. doi: 10.1083/jcb.153.5.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tondreau T, Meuleman N, Delforge A, Dejeneffe M, Leroy R, Massy M, Mortier C, Bron D, Lagneaux L. Mesenchymal stem cells derived from CD133-positive cells in mobilized peripheral blood and cord blood: proliferation, Oct4 expression, and plasticity. Stem Cells. 2005;23(8):1105–1112. doi: 10.1634/stemcells.2004-0330. [DOI] [PubMed] [Google Scholar]
- 21.Carlotti F, Zaldumbide A, Loomans CJ, van Rossenberg E, Engelse M, de Koning EJ, Hoeben RC. Isolated human islets contain a distinct population of mesenchymal stem cells. Islets. 2010;2(3):164–173. doi: 10.4161/isl.2.3.11449. [DOI] [PubMed] [Google Scholar]
- 22.Paul G, Ozen I, Christophersen NS, Reinbothe T, Bengzon J, Visse E, Jansson K, Dannaeus K, Henriques-Oliveira C, Roybon L, Anisimov SV, Renstrom E, Svensson M, Haegerstrand A, Brundin P. The adult human brain harbors multipotent perivascular mesenchymal stem cells. PLoS ONE. 2012;7(4):e35577. doi: 10.1371/journal.pone.0035577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang F, Chen M, Chen W, Gu J, Yuan J, Xue Y, Dang J, Su W, Wang J, Zadeh HH, He X, Rong L, Olsen N, Zheng SG. Human gingiva-derived mesenchymal stem cells inhibit xeno-graft-versus-host disease via CD39-CD73-adenosine and IDO signals. Front Immunol. 2017;8:68. doi: 10.3389/fimmu.2017.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ukai R, Honmou O, Harada K, Houkin K, Hamada H, Kocsis JD. Mesenchymal stem cells derived from peripheral blood protects against ischemia. J Neurotrauma. 2007;24(3):508–520. doi: 10.1089/neu.2006.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berebichez-Fridman R, Montero-Olvera PR. Sources and clinical applications of mesenchymal stem cells: state-of-the-art review. Sultan Qaboos Univ Med J. 2018;18(3):e264–e277. doi: 10.18295/squmj.2018.18.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Via AG, Frizziero A, Oliva F. Biological properties of mesenchymal stem cells from different sources. Muscles Ligaments Tendons J. 2012;2(3):154–162. [PMC free article] [PubMed] [Google Scholar]
- 27.Wu M, Zhang R, Zou Q, Chen Y, Zhou M, Li X, Ran R, Chen Q. Comparison of the biological characteristics of mesenchymal stem cells derived from the human placenta and umbilical cord. Sci Rep. 2018;8(1):5014. doi: 10.1038/s41598-018-23396-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vasandan AB, Shankar SR, Prasad P, Sowmya Jahnavi V, Bhonde RR, Jyothi Prasanna S. Functional differences in mesenchymal stromal cells from human dental pulp and periodontal ligament. J Cell Mol Med. 2014;18(2):344–354. doi: 10.1111/jcmm.12192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakaguchi Y, Sekiya I, Yagishita K, Muneta T. Comparison of human stem cells derived from various mesenchymal tissues - Superiority of synovium as a cell source. Arthritis Rheum. 2005;52(8):2521–2529. doi: 10.1002/art.21212. [DOI] [PubMed] [Google Scholar]
- 30.Huibregtse BA, Johnstone B, Goldberg VM, Caplan AI. Effect of age and sampling site on the chondro-osteogenic potential of rabbit marrow-derived mesenchymal progenitor cells. J Orthopaed Res. 2000;18(1):18–24. doi: 10.1002/jor.1100180104. [DOI] [PubMed] [Google Scholar]
- 31.Danisovic L, Varga I, Polak S, Ulicna M, Hlavackova L, Bohmer D, Vojtassak J. Comparison of in vitro chondrogenic potential of human mesenchymal stem cells derived from bone marrow and adipose tissue. Gen Physiol Biophys. 2009;28(1):56–62. doi: 10.4149/gpb_2009_01_56. [DOI] [PubMed] [Google Scholar]
- 32.Gasiuniene M, Zentelyte A, Wojtas B, Baronaite S, Krasovskaja N, Savickiene J, Gielniewski B, Kaminska B, Utkus A, Navakauskiene R. DNA methyltransferases inhibitors effectively induce gene expression changes suggestive of cardiomyogenic differentiation of human amniotic fluid-derived mesenchymal stem cells via chromatin remodeling. J Tissue Eng Regen Med. 2019;13(3):469–481. doi: 10.1002/term.2800. [DOI] [PubMed] [Google Scholar]
- 33.Park J, Lee JH, Yoon BS, Jun EK, Lee G, Kim IY, You S. Additive effect of bFGF and selenium on expansion and paracrine action of human amniotic fluid-derived mesenchymal stem cells. Stem Cell Res Ther. 2018;9(1):293. doi: 10.1186/s13287-018-1058-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Charbord P, Livne E, Gross G, Haupl T, Neves NM, Marie P, Bianco P, Jorgensen C. Human bone marrow mesenchymal stem cells: a systematic reappraisal via the genostem experience. Stem Cell Rev. 2011;7(1):32–42. doi: 10.1007/s12015-010-9125-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang WG, Lou SQ, Ju XD, Xia K, Xia JH. In vitro chondrogenesis of human bone marrow-derived mesenchymal progenitor cells in monolayer culture: activation by transfection with TGF-beta2. Tissue Cell. 2003;35(1):69–77. doi: 10.1016/S0040-8166(02)00106-4. [DOI] [PubMed] [Google Scholar]
- 36.Violini S, Ramelli P, Pisani LF, Gorni C, Mariani P. Horse bone marrow mesenchymal stem cells express embryo stem cell markers and show the ability for tenogenic differentiation by in vitro exposure to BMP-12. BMC Cell Biol. 2009 doi: 10.1186/1471-2121-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Delorme B, Ringe J, Pontikoglou C, Gaillard J, Langonne A, Sensebe L, Noel D, Jorgensen C, Haupl T, Charbord P. Specific lineage-priming of bone marrow mesenchymal stem cells provides the molecular framework for their plasticity. Stem Cells. 2009;27(5):1142–1151. doi: 10.1002/stem.34. [DOI] [PubMed] [Google Scholar]
- 38.Arthur A, Rychkov G, Shi S, Koblar SA, Gronthos S. Adult human dental pulp stem cells differentiate toward functionally active neurons under appropriate environmental cues. Stem Cells. 2008;26(7):1787–1795. doi: 10.1634/stemcells.2007-0979. [DOI] [PubMed] [Google Scholar]
- 39.Wang YX, Ma ZF, Huo N, Tang L, Han C, Duan YZ, Jin Y. Porcine tooth germ cell conditioned medium can induce odontogenic differentiation of human dental pulp stem cells. J Tissue Eng Regen M. 2011;5(5):354–362. doi: 10.1002/term.321. [DOI] [PubMed] [Google Scholar]
- 40.Zhang WB, Walboomers XF, Shi ST, Fan MW, Jansen JA. Multilineage differentiation potential of stem cells derived from human dental pulp after cryopreservation. Tissue Eng. 2006;12(10):2813–2823. doi: 10.1089/ten.2006.12.2813. [DOI] [PubMed] [Google Scholar]
- 41.Luo LH, He Y, Wang XY, Key B, Lee BH, Li HQ, Ye QS. Potential roles of dental pulp stem cells in neural regeneration and repair. Stem Cells Int. 2018 doi: 10.1155/2018/1731289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu H, Wang F, Mei H, Wang S, Cheng L. Human adipose mesenchymal stem cells show more efficient angiogenesis promotion on endothelial colony-forming cells than umbilical cord and endometrium. Stem Cells Int. 2018;2018:7537589. doi: 10.1155/2018/7537589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang X, Liu L, Mou S, Zhao H, Fang J, Xiang Y, Zhao T, Sha T, Ding J, Hao C. Investigation of platelet-rich plasma in increasing proliferation and migration of endometrial mesenchymal stem cells and improving pregnancy outcome of patients with thin endometrium. J Cell Biochem. 2018 doi: 10.1002/jcb.28014. [DOI] [PubMed] [Google Scholar]
- 44.Zvaifler NJ, Marinova-Mutafchieva L, Adams G, Edwards CJ, Moss J, Burger JA, Maini RN. Mesenchymal precursor cells in the blood of normal individuals. Arthritis Res. 2000;2(6):477–488. doi: 10.1186/ar130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sabapathy V, Ravi S, Srivastava V, Srivastava A, Kumar S. Long-term cultured human term placenta-derived mesenchymal stem cells of maternal origin displays plasticity. Stem Cells Int. 2012;2012:174328. doi: 10.1155/2012/174328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oliveira MS, Barreto-Filho JB. Placental-derived stem cells: Culture, differentiation and challenges. World J Stem Cells. 2015;7(4):769–775. doi: 10.4252/wjsc.v7.i4.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yoshimura H, Muneta T, Nimura A, Yokoyama A, Koga H, Sekiya I. Comparison of rat mesenchymal stem cells derived from bone marrow, synovium, periosteum, adipose tissue, and muscle. Cell Tissue Res. 2007;327(3):449–462. doi: 10.1007/s00441-006-0308-z. [DOI] [PubMed] [Google Scholar]
- 48.De Bari C, Dell'Accio F, Vandenabeele F, Vermeesch JR, Raymackcrs JM, Luyten FP. Skeletal muscle repair by adult human mesenchymal stem cells from synovial membrane. J Cell Biol. 2003;160(6):909–918. doi: 10.1083/jcb.200212064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lorenz K, Sicker M, Schmelzer E, Rupf T, Salvetter J, Schulz-Siegmund M, Bader A. Multilineage differentiation potential of human dermal skin-derived fibroblasts. Exp Dermatol. 2008;17(11):925–932. doi: 10.1111/j.1600-0625.2008.00724.x. [DOI] [PubMed] [Google Scholar]
- 50.Vishnubalaji R, Manikandan M, Al-Nbaheen M, Kadalmani B, Aldahmash A, Alajez NM. In vitro differentiation of human skin-derived multipotent stromal cells into putative endothelial-like cells. BMC Dev Biol. 2012 doi: 10.1186/1471-213x-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shi CM, Cheng TM. Differentiation of dermis-derived multipotent cells into insulin-producing pancreatic cells in vitro. World J Gastroentero. 2004;10(17):2550–2552. doi: 10.3748/wjg.v10.i17.2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Conconi MT, Burra P, Di Liddo R, Calore C, Turetta M, Bellini S, Bo P, Nussdorfer GG, Parnigotto PP. CD105(+) cells from Wharton’s jelly show in vitro and in vivo myogenic differentiative potential. Int J Mol Med. 2006;18(6):1089–1096. [PubMed] [Google Scholar]
- 53.Wu KH, Zhou B, Lu SH, Feng B, Yang SG, Du WT, Gu DS, Han ZC, Liu YL. In vitro and in vivo differentiation of human umbilical cord derived stem cells into endothelial cells. J Cell Biochem. 2007;100(3):608–616. doi: 10.1002/jcb.21078. [DOI] [PubMed] [Google Scholar]
- 54.Trivedi P, Hematti P. Derivation and immunological characterization of mesenchymal stromal cells from human embryonic stem cells. Exp Hematol. 2008;36(3):350–359. doi: 10.1016/j.exphem.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lian Q, Zhang Y, Zhang J, Zhang HK, Wu X, Zhang Y, Lam FF, Kang S, Xia JC, Lai WH, Au KW, Chow YY, Siu CW, Lee CN, Tse HF. Functional mesenchymal stem cells derived from human induced pluripotent stem cells attenuate limb ischemia in mice. Circulation. 2010;121(9):1113–1123. doi: 10.1161/CIRCULATIONAHA.109.898312. [DOI] [PubMed] [Google Scholar]
- 56.Lian Q, Zhang Y, Liang X, Gao F, Tse HF. Directed differentiation of human-induced pluripotent stem cells to mesenchymal stem cells. Methods Mol Biol. 2016;1416:289–298. doi: 10.1007/978-1-4939-3584-0_17. [DOI] [PubMed] [Google Scholar]
- 57.Gao WX, Sun YQ, Shi J, Li CL, Fang SB, Wang D, Deng XQ, Wen W, Fu QL. Effects of mesenchymal stem cells from human induced pluripotent stem cells on differentiation, maturation, and function of dendritic cells. Stem Cell Res Ther. 2017;8(1):48. doi: 10.1186/s13287-017-0499-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sun YQ, Zhang Y, Li X, Deng MX, Gao WX, Yao Y, Chiu SM, Liang X, Gao F, Chan CW, Tse HF, Shi J, Fu QL, Lian Q. Insensitivity of human iPS cells-derived mesenchymal stem cells to interferon-gamma-induced hla expression potentiates repair efficiency of hind limb ischemia in immune humanized nod scid gamma mice. Stem Cells. 2015;33(12):3452–3467. doi: 10.1002/stem.2094. [DOI] [PubMed] [Google Scholar]
- 59.Spitzhorn LS, Megges M, Wruck W, Rahman MS, Otte J, Degistirici O, Meisel R, Sorg RV, Oreffo ROC, Adjaye J. Human iPSC-derived MSCs (iMSCs) from aged individuals acquire a rejuvenation signature. Stem Cell Res Ther. 2019;10(1):100. doi: 10.1186/s13287-019-1209-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Perez-Silos V, Camacho-Morales A, Fuentes-Mera L. Mesenchymal stem cells subpopulations: application for orthopedic regenerative medicine. Stem Cells Int. 2016;2016:3187491. doi: 10.1155/2016/3187491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284(5411):143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 62.Kim N, Cho SG. Clinical applications of mesenchymal stem cells. Korean J Intern Med. 2013;28(4):387–402. doi: 10.3904/kjim.2013.28.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Badylak SF, Weiss DJ, Caplan A, Macchiarini P. Engineered whole organs and complex tissues. Lancet. 2012;379(9819):943–952. doi: 10.1016/S0140-6736(12)60073-7. [DOI] [PubMed] [Google Scholar]
- 64.Pereira RF, Halford KW, O'Hara MD, Leeper DB, Sokolov BP, Pollard MD, Bagasra O, Prockop DJ. Cultured adherent cells from marrow can serve as long-lasting precursor cells for bone, cartilage, and lung in irradiated mice. Proc Natl Acad Sci USA. 1995;92(11):4857–4861. doi: 10.1073/pnas.92.11.4857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schwartz RE, Reyes M, Koodie L, Jiang YH, Blackstad M, Lund T, Lenvik T, Johnson S, Hu WS, Verfaillie CM. Multipotent adult progenitor cells from bone marrow differentiate into functional hepatocyte-like cells. J Clin Invest. 2002;109(10):1291–1302. doi: 10.1172/Jci200215182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dai WD, Hale SL, Martin BJ, Kuang JQ, Dow JS, Wold LE, Kloner RA. Allogeneic mesenchymal stem cell transplantation in postinfarcted rat myocardium - Short- and long-term effects. Circulation. 2005;112(2):214–223. doi: 10.1161/Circulationaha.104.527937. [DOI] [PubMed] [Google Scholar]
- 67.Bae JS, Han HS, Youn DH, Carter JE, Modo M, Schuchman EH, Jin HK. Bone marrow-derived mesenchymal stem cells promote neuronal networks with functional synaptic transmission after transplantation into mice with neurodegeneration. Stem Cells. 2007;25(5):1307–1316. doi: 10.1634/stemcells.2006-0561. [DOI] [PubMed] [Google Scholar]
- 68.Sharma K, Husain SY, Das P, Hussain M, Syed MA (2017) Regenerative Potential of Mesenchymal Stem Cells: Therapeutic Applications in Lung Disorders. In: Pham PV (ed) Liver, Lung and Heart Regeneration. Springer International Publishing, Cham, pp 77–117. doi:10.1007/978–3–319–46693–4_6
- 69.Gao F, Chiu SM, Motan DAL, Zhang Z, Chen L, Ji HL, Tse HF, Fu QL, Lian Q. Mesenchymal stem cells and immunomodulation: current status and future prospects. Cell Death Dis. 2016 doi: 10.1038/cddis.2015.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fan XL, Zeng QX, Li X, Li CL, Xu ZB, Deng XQ, Shi J, Chen D, Zheng SG, Fu QL. Induced pluripotent stem cell-derived mesenchymal stem cells activate quiescent T cells and elevate regulatory T cell response via NF-kappaB in allergic rhinitis patients. Stem Cell Res Ther. 2018;9(1):170. doi: 10.1186/s13287-018-0896-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Selmani Z, Naji A, Zidi I, Favier B, Gaiffe E, Obert L, Borg C, Saas P, Tiberghien P, Rouas-Freiss N, Carosella ED, Deschaseaux F. Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is required to suppress T lymphocyte and natural killer function and to induce CD4(+)CD25(high)FOXP3(+) regulatory T cells. Stem Cells. 2008;26(1):212–222. doi: 10.1634/stemcells.2007-0554. [DOI] [PubMed] [Google Scholar]
- 72.Augello A, Tasso R, Negrini SM, Amateis A, Indiveri F, Cancedda R, Pennesi G. Bone marrow mesenchymal progenitor cells inhibit lymphocyte proliferation by activation of the programmed death 1 pathway. Eur J Immunol. 2005;35(5):1482–1490. doi: 10.1002/eji.200425405. [DOI] [PubMed] [Google Scholar]
- 73.Corcione A, Benvenuto F, Ferretti E, Giunti D, Cappiello V, Cazzanti F, Risso M, Gualandi F, Mancardi GL, Pistoia V, Uccelli A. Human mesenchymal stem cells modulate B-cell functions. Blood. 2006;107(1):367–372. doi: 10.1182/blood-2005-07-2657. [DOI] [PubMed] [Google Scholar]
- 74.Spaggiari GM, Capobianco A, Abdelrazik H, Becchetti F, Mingari MC, Moretta L. Mesenchymal stem cells inhibit natural killer-cell proliferation, cytotoxicity, and cytokine production: role of indoleamine 2,3-dioxygenase and prostaglandin E2. Blood. 2008;111(3):1327–1333. doi: 10.1182/blood-2007-02-074997. [DOI] [PubMed] [Google Scholar]
- 75.Vacca P, Vitale C, Munari E, Cassatella MA, Mingari MC, Moretta L. Human innate lymphoid cells: their functional and cellular interactions in Decidua. Front Immunol. 2018 doi: 10.3389/fimmu.2018.01897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.van Hoeven V, Munneke JM, Cornelissen AS, Omar SZ, Spruit MJ, Kleijer M, Bernink JH, Blom B, Voermans C, Hazenberg MD. Mesenchymal stromal cells stimulate the proliferation and il-22 production of group 3 innate lymphoid cells. J Immunol. 2018;201(4):1165–1173. doi: 10.4049/jimmunol.1700901. [DOI] [PubMed] [Google Scholar]
- 77.Zhang L, Yu J, Wei W. Advance in targeted immunotherapy for graft-versus-host disease. Front Immunol. 2018;9:1087. doi: 10.3389/fimmu.2018.01087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Marigo I, Dazzi F. The immunomodulatory properties of mesenchymal stem cells. Semin Immunopathol. 2011;33(6):593–602. doi: 10.1007/s00281-011-0267-7. [DOI] [PubMed] [Google Scholar]
- 79.Li Y, Wu Q, Wang Y, Li L, Bu H, Bao J. Senescence of mesenchymal stem cells (Review) Int J Mol Med. 2017;39(4):775–782. doi: 10.3892/ijmm.2017.2912. [DOI] [PubMed] [Google Scholar]
- 80.Yang YK, Ogando CR, Wang See C, Chang TY, Barabino GA. Changes in phenotype and differentiation potential of human mesenchymal stem cells aging in vitro. Stem Cell Res Ther. 2018;9(1):131. doi: 10.1186/s13287-018-0876-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fafian-Labora JA, Morente-Lopez M, Arufe MC. Effect of aging on behaviour of mesenchymal stem cells. World J Stem Cells. 2019;11(6):337–346. doi: 10.4252/wjsc.v11.i6.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Song HF, He S, Li SH, Yin WJ, Wu J, Guo J, Shao ZB, Zhai XY, Gong H, Lu L, Wei F, Weisel RD, Xie J, Li RK. Aged human multipotent mesenchymal stromal cells can be rejuvenated by neuron-derived neurotrophic factor and improve heart function after injury. JACC Basic Transl Sci. 2017;2(6):702–716. doi: 10.1016/j.jacbts.2017.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dong J, Zhang ZH, Huang HS, Mo P, Cheng CF, Liu JW, Huang WZ, Tian CW, Zhang CY, Li J. miR-10a rejuvenates aged human mesenchymal stem cells and improves heart function after myocardial infarction through KLF4. Stem Cell Res Ther. 2018 doi: 10.1186/s13287-018-0895-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Salminen A, Kauppinen A, Kaarniranta K. FGF21 activates AMPK signaling: impact on metabolic regulation and the aging process. J Mol Med. 2017;95(2):123–131. doi: 10.1007/s00109-016-1477-1. [DOI] [PubMed] [Google Scholar]
- 85.Liang J, Zhang H, Kong W, Deng W, Wang D, Feng X, Zhao C, Hua B, Wang H, Sun L. Safety analysis in patients with autoimmune disease receiving allogeneic mesenchymal stem cells infusion: a long-term retrospective study. Stem Cell Res Ther. 2018;9(1):312. doi: 10.1186/s13287-018-1053-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Munir H, McGettrick HM. Mesenchymal stem cell therapy for autoimmune disease: risks and rewards. Stem Cells Dev. 2015;24(18):2091–2100. doi: 10.1089/scd.2015.0008. [DOI] [PubMed] [Google Scholar]
- 87.Shyam H, Singh SK, Kant R, Saxena SK. Mesenchymal stem cells in regenerative medicine: a new paradigm for degenerative bone diseases. Regen Med. 2017;12(2):111–114. doi: 10.2217/rme-2016-0162. [DOI] [PubMed] [Google Scholar]
- 88.White IA, Sanina C, Balkan W, Hare JM. Mesenchymal stem cells in cardiology. Methods Mol Biol. 2016;1416:55–87. doi: 10.1007/978-1-4939-3584-0_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Brychtova M, Thiele JA, Lysak D, Holubova M, Kralickova M, Vistejnova L. Mesenchymal stem cells as the near future of cardiology medicine - truth or wish? Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2019;163(1):8–18. doi: 10.5507/bp.2018.071. [DOI] [PubMed] [Google Scholar]
- 90.Broekman W, Khedoe P, Schepers K, Roelofs H, Stolk J, Hiemstra PS. Mesenchymal stromal cells: a novel therapy for the treatment of chronic obstructive pulmonary disease? Thorax. 2018;73(6):565–574. doi: 10.1136/thoraxjnl-2017-210672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang YH, Wu DB, Chen B, Chen EQ, Tang H. Progress in mesenchymal stem cell-based therapy for acute liver failure. Stem Cell Res Ther. 2018;9(1):227. doi: 10.1186/s13287-018-0972-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang Y, Li Y, Zhang L, Li J, Zhu C. Mesenchymal stem cells: potential application for the treatment of hepatic cirrhosis. Stem Cell Res Ther. 2018;9(1):59. doi: 10.1186/s13287-018-0814-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lee NK, Na DL, Chang JW. Killing two birds with one stone: The multifunctional roles of mesenchymal stem cells in the treatment of neurodegenerative and muscle diseases. Histol Histopathol. 2018;33(7):629–638. doi: 10.14670/HH-11-951. [DOI] [PubMed] [Google Scholar]
- 94.Volkman R, Offen D. Concise review: mesenchymal stem cells in neurodegenerative diseases. Stem Cells. 2017;35(8):1867–1880. doi: 10.1002/stem.2651. [DOI] [PubMed] [Google Scholar]
- 95.Lo Furno D, Mannino G, Giuffrida R. Functional role of mesenchymal stem cells in the treatment of chronic neurodegenerative diseases. J Cell Physiol. 2018;233(5):3982–3999. doi: 10.1002/jcp.26192. [DOI] [PubMed] [Google Scholar]
- 96.Dasari VR, Veeravalli KK, Dinh DH. Mesenchymal stem cells in the treatment of spinal cord injuries: a review. World J Stem Cells. 2014;6(2):120–133. doi: 10.4252/wjsc.v6.i2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee HY, Hong IS. Double-edged sword of mesenchymal stem cells: Cancer-promoting versus therapeutic potential. Cancer Sci. 2017;108(10):1939–1946. doi: 10.1111/cas.13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Garcia-Olmo D, Herreros D, Pascual I, Pascual JA, Del-Valle E, Zorrilla J, De-La-Quintana P, Garcia-Arranz M, Pascual M. Expanded adipose-derived stem cells for the treatment of complex perianal fistula: a phase II clinical trial. Dis Colon Rectum. 2009;52(1):79–86. doi: 10.1007/DCR.0b013e3181973487. [DOI] [PubMed] [Google Scholar]
- 99.Liang J, Zhang H, Hua B, Wang H, Lu L, Shi S, Hou Y, Zeng X, Gilkeson GS, Sun L. Allogenic mesenchymal stem cells transplantation in refractory systemic lupus erythematosus: a pilot clinical study. Ann Rheum Dis. 2010;69(8):1423–1429. doi: 10.1136/ard.2009.123463. [DOI] [PubMed] [Google Scholar]
- 100.Liang J, Gu F, Wang H, Hua B, Hou Y, Shi S, Lu L, Sun L. Mesenchymal stem cell transplantation for diffuse alveolar hemorrhage in SLE. Nat Rev Rheumatol. 2010;6(8):486–489. doi: 10.1038/nrrheum.2010.80. [DOI] [PubMed] [Google Scholar]
- 101.Ansboro S, Roelofs AJ, De Bari C. Mesenchymal stem cells for the management of rheumatoid arthritis: immune modulation, repair or both? Curr Opin Rheumatol. 2017;29(2):201–207. doi: 10.1097/bor.0000000000000370. [DOI] [PubMed] [Google Scholar]
- 102.Dunavin N, Dias A, Li M, McGuirk J. Mesenchymal stromal cells: what is the mechanism in acute graft-versus-host disease? Biomedicines. 2017;5(3):39. doi: 10.3390/biomedicines5030039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Moreira A, Kahlenberg S, Hornsby P. Therapeutic potential of mesenchymal stem cells for diabetes. J Mol Endocrinol. 2017;59(3):R109–R120. doi: 10.1530/JME-17-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sun YQ, Deng MX, He J, Zeng QX, Wen W, Wong DS, Tse HF, Xu G, Lian Q, Shi J, Fu QL. Human pluripotent stem cell-derived mesenchymal stem cells prevent allergic airway inflammation in mice. Stem Cells. 2012;30(12):2692–2699. doi: 10.1002/stem.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yao Y, Fan XL, Jiang D, Zhang Y, Li X, Xu ZB, Fang SB, Chiu S, Tse HF, Lian Q, Fu QL. Connexin 43-mediated mitochondrial transfer of ipsc-mscs alleviates asthma inflammation. Stem Cell Rep. 2018;11(5):1120–1135. doi: 10.1016/j.stemcr.2018.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fu QL, Chow YY, Sun SJ, Zeng QX, Li HB, Shi JB, Sun YQ, Wen W, Tse HF, Lian Q, Xu G. Mesenchymal stem cells derived from human induced pluripotent stem cells modulate T-cell phenotypes in allergic rhinitis. Allergy. 2012;67(10):1215–1222. doi: 10.1111/j.1398-9995.2012.02875.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang SY, Fan XL, Yu QN, Deng MX, Sun YQ, Gao WX, Li CL, Shi JB, Fu QL. The lncRNAs involved in mouse airway allergic inflammation following induced pluripotent stem cell-mesenchymal stem cell treatment. Stem Cell Res Ther. 2017;8(1):2. doi: 10.1186/s13287-016-0456-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Li X, Michaeloudes C, Zhang Y, Wiegman CH, Adcock IM, Lian Q, Mak JCW, Bhavsar PK, Chung KF. Mesenchymal stem cells alleviate oxidative stress-induced mitochondrial dysfunction in the airways. J Allergy Clin Immunol. 2018;141(5):1634–1645. doi: 10.1016/j.jaci.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 109.Lin YD, Fan XL, Zhang H, Fang SB, Li CL, Deng MX, Qin ZL, Peng YQ, Zhang HY, Fu QL. The genes involved in asthma with the treatment of human embryonic stem cell-derived mesenchymal stem cells. Mol Immunol. 2018;95:47–55. doi: 10.1016/j.molimm.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 110.Kavanagh H, Mahon BP. Allogeneic mesenchymal stem cells prevent allergic airway inflammation by inducing murine regulatory T cells. Allergy. 2011;66(4):523–531. doi: 10.1111/j.1398-9995.2010.02509.x. [DOI] [PubMed] [Google Scholar]
- 111.Mohammadian M, Boskabady MH, Kashani IR, Jahromi GP, Omidi A, Nejad AK, Khamse S, Sadeghipour HR. Effect of bone marrow derived mesenchymal stem cells on lung pathology and inflammation in ovalbumin-induced asthma in mouse. Iran J Basic Med Sci. 2016;19(1):55–63. [PMC free article] [PubMed] [Google Scholar]
- 112.Chuang YC, Liou CW, Chen SD, Wang PW, Chuang JH, Tiao MM, Hsu TY, Lin HY, Lin TK. Mitochondrial transfer from wharton’s jelly mesenchymal stem cell to MERRF cybrid reduces oxidative stress and improves mitochondrial bioenergetics. Oxid Med Cell Longev. 2017 doi: 10.1155/2017/5691215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fang SB, Zhang HY, Jiang AY, Fan XL, Lin YD, Li CL, Wang C, Meng XC, Fu QL. Human iPSC-MSCs prevent steroid-resistant neutrophilic airway inflammation via modulating Th17 phenotypes. Stem Cell Res Ther. 2018;9(1):147. doi: 10.1186/s13287-018-0897-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Squillaro T, Peluso G, Galderisi U. Clinical trials with mesenchymal stem cells: an update. Cell Transplant. 2016;25(5):829–848. doi: 10.3727/096368915X689622. [DOI] [PubMed] [Google Scholar]
- 115.Couto PS, Shatirishvili G, Bersenev A, Verter F. First decade of clinical trials and published studies with mesenchymal stromal cells from umbilical cord tissue. Regen Med. 2019;14(4):309–319. doi: 10.2217/rme-2018-0171. [DOI] [PubMed] [Google Scholar]
- 116.Gugliandolo A, Bramanti P, Mazzon E. mesenchymal stem cells: a potential therapeutic approach for amyotrophic lateral sclerosis? Stem Cells Int. 2019;2019:3675627. doi: 10.1155/2019/3675627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cho J, D’Antuono M, Glicksman M, Wang J, Jonklaas J. A review of clinical trials: mesenchymal stem cell transplant therapy in type 1 and type 2 diabetes mellitus. Am J Stem Cells. 2018;7(4):82–93. [PMC free article] [PubMed] [Google Scholar]
- 118.Attwood SW, Edel MJ. iPS-Cell technology and the problem of genetic instability-can it ever be safe for clinical use? J Clin Med. 2019;8(3):288. doi: 10.3390/jcm8030288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bhansali A, Upreti V, Khandelwal N, Marwaha N, Gupta V, Sachdeva N, Sharma RR, Saluja K, Dutta P, Walia R, Minz R, Bhadada S, Das S, Ramakrishnan S. Efficacy of autologous bone marrow-derived stem cell transplantation in patients with type 2 diabetes mellitus. Stem Cells Dev. 2009;18(10):1407–1416. doi: 10.1089/scd.2009.0164. [DOI] [PubMed] [Google Scholar]
- 120.Bhansali A, Asokumar P, Walia R, Bhansali S, Gupta V, Jain A, Sachdeva N, Sharma RR, Marwaha N, Khandelwal N. Efficacy and safety of autologous bone marrow-derived stem cell transplantation in patients with type 2 diabetes mellitus: a randomized placebo-controlled study. Cell Transplant. 2014;23(9):1075–1085. doi: 10.3727/096368913X665576. [DOI] [PubMed] [Google Scholar]
- 121.Jiang R, Han Z, Zhuo G, Qu X, Li X, Wang X, Shao Y, Yang S, Han ZC. Transplantation of placenta-derived mesenchymal stem cells in type 2 diabetes: a pilot study. Front Med. 2011;5(1):94–100. doi: 10.1007/s11684-011-0116-z. [DOI] [PubMed] [Google Scholar]
- 122.Jeon SR, Park JH, Lee JH, Kim DY, Kim HS, Sung IY, Choi GH, Jeon MH, Kim GG. Treatment of spinal cord injury with bone marrow-derived, cultured autologous mesenchymal stem cells. Tissue Eng Regenerat Med. 2010;7(3):316–322. [Google Scholar]
- 123.Sykova E, Homola A, Mazanec R, Lachmann H, Konradova SL, Kobylka P, Padr R, Neuwirth J, Komrska V, Vavra V, Stulik J, Bojar M. Autologous bone marrow transplantation in patients with subacute and chronic spinal cord injury. Cell Transplant. 2006;15(8–9):675–687. doi: 10.3727/000000006783464381. [DOI] [PubMed] [Google Scholar]
- 124.Pal R, Venkataramana NK, Jaan M, Bansal A, Balaraju S, Jaan M, Chandra R, Dixit A, Rauthan A, Murgod U, Totey S. Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia: a pilot clinical study. Cytotherapy. 2009;11(7):897–911. doi: 10.3109/14653240903253857. [DOI] [PubMed] [Google Scholar]
- 125.Karamouzian S, Nematollahi-Mahani SN, Nakhaee N, Eskandary H. Clinical safety and primary efficacy of bone marrow mesenchymal cell transplantation in subacute spinal cord injured patients. Clin Neurol Neurosur. 2012;114(7):935–939. doi: 10.1016/j.clineuro.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 126.Bhasin A, Srivastava MV, Kumaran SS, Mohanty S, Bhatia R, Bose S, Gaikwad S, Garg A, Airan B. Autologous mesenchymal stem cells in chronic stroke. Cerebrovasc Dis Extra. 2011;1(1):93–104. doi: 10.1159/000333381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tsang KS, Ng CPS, Zhu XL, Wong GKC, Lu G, Ahuja AT, Wong KSL, Ng HK, Poon WS. Phase I/II randomized controlled trial of autologous bone marrow-derived mesenchymal stem cell therapy for chronic stroke. World J Stem Cells. 2017;9(8):133–143. doi: 10.4252/wjsc.v9.i8.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ahn SY, Chang YS, Sung SI, Park WS. Mesenchymal stem cells for severe intraventricular hemorrhage in preterm infants: phase I dose-escalation clinical trial. Stem Cells Transl Med. 2018;7(12):847–856. doi: 10.1002/sctm.17-0219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Liang X, Ding Y, Zhang Y, Tse HF, Lian Q. Paracrine mechanisms of mesenchymal stem cell-based therapy: current status and perspectives. Cell Transplant. 2014;23(9):1045–1059. doi: 10.3727/096368913X667709. [DOI] [PubMed] [Google Scholar]
- 130.Gnecchi M, He H, Liang OD, Melo LG, Morello F, Mu H, Noiseux N, Zhang L, Pratt RE, Ingwall JS, Dzau VJ. Paracrine action accounts for marked protection of ischemic heart by Akt-modified mesenchymal stem cells. Nat Med. 2005;11(4):367–368. doi: 10.1038/nm0405-367. [DOI] [PubMed] [Google Scholar]
- 131.Cselenyak A, Pankotai E, Horvath EM, Kiss L, Lacza Z. Mesenchymal stem cells rescue cardiomyoblasts from cell death in an in vitro ischemia model via direct cell-to-cell connections. BMC Cell Biol. 2010;11:29. doi: 10.1186/1471-2121-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Islam MN, Das SR, Emin MT, Wei M, Sun L, Westphalen K, Rowlands DJ, Quadri SK, Bhattacharya S, Bhattacharya J. Mitochondrial transfer from bone-marrow-derived stromal cells to pulmonary alveoli protects against acute lung injury. Nat Med. 2012;18(5):759–765. doi: 10.1038/nm.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lee C, Mitsialis SA, Aslam M, Vitali SH, Vergadi E, Konstantinou G, Sdrimas K, Fernandez-Gonzalez A, Kourembanas S. Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension. Circulation. 2012;126(22):2601–2611. doi: 10.1161/CIRCULATIONAHA.112.114173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhang B, Yin Y, Lai RC, Tan SS, Choo AB, Lim SK. Mesenchymal stem cells secrete immunologically active exosomes. Stem Cells Dev. 2014;23(11):1233–1244. doi: 10.1089/scd.2013.0479. [DOI] [PubMed] [Google Scholar]
- 135.Noth U, Osyczka AM, Tuli R, Hickok NJ, Danielson KG, Tuan RS. Multilineage mesenchymal differentiation potential of human trabecular bone-derived cells. J Orthop Res. 2002;20(5):1060–1069. doi: 10.1016/S0736-0266(02)00018-9. [DOI] [PubMed] [Google Scholar]
- 136.Fukumoto T, Sperling JW, Sanyal A, Fitzsimmons JS, Reinholz GG, Conover CA, O'Driscoll SW. Combined effects of insulin-like growth factor-1 and transforming growth factor-beta1 on periosteal mesenchymal cells during chondrogenesis in vitro. Osteoarthr Cartilage. 2003;11(1):55–64. doi: 10.1053/joca.2002.0869. [DOI] [PubMed] [Google Scholar]
- 137.Satué M, Schüler C, Ginner N, Erben RG. Intra-articularly injected mesenchymal stem cells promote cartilage regeneration, but do not permanently engraft in distant organs. Sci Rep. 2019;9(1):10153. doi: 10.1038/s41598-019-46554-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Joshi J, Abnavi MD, Kothapalli CR. Synthesis and secretome release by human bone marrow mesenchymal stem cell spheroids within three-dimensional collagen hydrogels: Integrating experiments and modelling. J Tissue Eng Regen M. 2019;13(10):1923–1937. doi: 10.1002/term.2943. [DOI] [PubMed] [Google Scholar]
- 139.Han J, Park J, Kim BS. Integration of mesenchymal stem cells with nanobiomaterials for the repair of myocardial infarction. Adv Drug Deliv Rev. 2015;95:15–28. doi: 10.1016/j.addr.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 140.Pijnappels DA, Schalij MJ, Ramkisoensing AA, van Tuyn J, de Vries AA, van der Laarse A, Ypey DL, Atsma DE. Forced alignment of mesenchymal stem cells undergoing cardiomyogenic differentiation affects functional integration with cardiomyocyte cultures. Circ Res. 2008;103(2):167–176. doi: 10.1161/CIRCRESAHA.108.176131. [DOI] [PubMed] [Google Scholar]
- 141.Popara J, Accomasso L, Vitale E, Gallina C, Roggio D, Iannuzzi A, Raimondo S, Rastaldo R, Alberto G, Catalano F, Martra G, Turinetto V, Pagliaro P, Giachino C. Silica nanoparticles actively engage with mesenchymal stem cells in improving acute functional cardiac integration. Nanomedicine. 2018;13(10):1121–1138. doi: 10.2217/nnm-2017-0309. [DOI] [PubMed] [Google Scholar]
- 142.Aurich H, Sgodda M, Kaltwasser P, Vetter M, Weise A, Liehr T, Brulport M, Hengstler JG, Dollinger MM, Fleig WE, Christ B. Hepatocyte differentiation of mesenchymal stem cells from human adipose tissue in vitro promotes hepatic integration in vivo. Gut. 2009;58(4):570–581. doi: 10.1136/gut.2008.154880. [DOI] [PubMed] [Google Scholar]
- 143.Kuo TK, Hung SP, Chuang CH, Chen CT, Shih YRV, Fang SCY, Yang VW, Lee OK. Stem cell therapy for liver disease: Parameters governing the success of using bone marrow mesenchymal stem cells. Gastroenterology. 2008;134(7):2111–2121. doi: 10.1053/j.gastro.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Joyce N, Annett G, Wirthlin L, Olson S, Bauer G, Nolta JA. Mesenchymal stem cells for the treatment of neurodegenerative disease. Regen Med. 2010;5(6):933–946. doi: 10.2217/rme.10.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Tzameret A, Sher I, Belkin M, Treves AJ, Meir A, Nagler A, Levkovitch-Verbin H, Barshack I, Rosner M, Rotenstreich Y. Transplantation of human bone marrow mesenchymal stem cells as a thin subretinal layer ameliorates retinal degeneration in a rat model of retinal dystrophy. Exp Eye Res. 2014;118:135–144. doi: 10.1016/j.exer.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 146.Sottile F, Aulicino F, Theka I, Cosma MP. Mesenchymal stem cells generate distinct functional hybrids in vitro via cell fusion or entosis. Sci Rep. 2016;6:36863. doi: 10.1038/srep36863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhang LN, Kong CF, Zhao D, Cong XL, Wang SS, Ma L, Huang YH. Fusion with mesenchymal stem cells differentially affects tumorigenic and metastatic abilities of lung cancer cells. J Cell Physiol. 2019;234(4):3570–3582. doi: 10.1002/jcp.27011. [DOI] [PubMed] [Google Scholar]
- 148.Melzer C, von der Ohe J, Hass R. In vivo cell fusion between mesenchymal stroma/stem-like cells and breast cancer cells. Cancers. 2019 doi: 10.3390/cancers11020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Bartholomew A, Sturgeon C, Siatskas M, Ferrer K, McIntosh K, Patil S, Hardy W, Devine S, Ucker D, Deans R, Moseley A, Hoffman R. Mesenchymal stem cells suppress lymphocyte proliferation in vitro and prolong skin graft survival in vivo. Exp Hematol. 2002;30(1):42–48. doi: 10.1016/S0301-472X(01)00769-X. [DOI] [PubMed] [Google Scholar]
- 150.Di Nicola M, Carlo-Stella C, Magni M, Milanesi M, Longoni PD, Matteucci P, Grisanti S, Gianni AM. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood. 2002;99(10):3838–3843. doi: 10.1182/blood.V99.10.3838. [DOI] [PubMed] [Google Scholar]
- 151.Akiyama K, Chen C, Wang DD, Xu XT, Qu CY, Yamaza T, Cai T, Chen WJ, Sun LY, Shi ST. Mesenchymal-stem-cell-induced immunoregulation involves FAS-Ligand-/FAS-Mediated T cell apoptosis. Cell Stem Cell. 2012;10(5):544–555. doi: 10.1016/j.stem.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhong H, Fan X-L, Fang S-B, Lin Y-D, Wen W, Fu Q-L. Human pluripotent stem cell-derived mesenchymal stem cells prevent chronic allergic airway inflammation via TGF-β1-Smad2/Smad3 signaling pathway in mice. Mol Immunol. 2019;109:51–57. doi: 10.1016/j.molimm.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 153.Meisel R, Zibert A, Laryea M, Gobel U, Daubener W, Dilloo D. Human bone marrow stromal cells inhibit allogeneic T-cell responses by indoleamine 2,3-dioxygenase-mediated tryptophan degradation. Blood. 2004;103(12):4619–4621. doi: 10.1182/blood-2003-11-3909. [DOI] [PubMed] [Google Scholar]
- 154.Hwu P, Du MX, Lapointe R, Do M, Taylor MW, Young HA. Indoleamine 2,3-dioxygenase production by human dendritic cells results in the inhibition of T cell proliferation. J Immunol. 2000;164(7):3596–3599. doi: 10.4049/jimmunol.164.7.3596. [DOI] [PubMed] [Google Scholar]
- 155.Sheng HM, Wang Y, Jin YQ, Zhang QY, Zhang Y, Wang L, Shen B, Yin S, Liu W, Cui L, Li NL. A critical role of IFN gamma in priming MSC-mediated suppression of T cell proliferation through up-regulation of B7–H1. Cell Res. 2008;18(8):846–857. doi: 10.1038/cr.2008.80. [DOI] [PubMed] [Google Scholar]
- 156.Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105(4):1815–1822. doi: 10.1182/blood-2004-04-1559. [DOI] [PubMed] [Google Scholar]
- 157.Nemeth K, Leelahavanichkul A, Yuen PST, Mayer B, Parmelee A, Doi K, Robey PG, Leelahavanichkul K, Koller BH, Brown JM, Hu XZ, Jelinek I, Star RA, Mezey E (2009) Bone marrow stromal cells attenuate sepsis via prostaglandin E2dependent reprogramming of host macrophages to increase their interleukin10 production. Nat Med 15 (1):42-49. doi:10.1038/nm.1905. [DOI] [PMC free article] [PubMed]
- 158.Xu G, Zhang Y, Zhang L, Ren G, Shi Y. The role of IL-6 in inhibition of lymphocyte apoptosis by mesenchymal stem cells. Biochem Biophys Res Commun. 2007;361(3):745–750. doi: 10.1016/j.bbrc.2007.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sato K, Ozaki K, Oh I, Meguro A, Hatanaka K, Nagai T, Muroi K, Ozawa K. Nitric oxide plays a critical role in suppression of T-cell proliferation by mesenchymal stem cells. Blood. 2007;109(1):228–234. doi: 10.1182/blood-2006-02-002246. [DOI] [PubMed] [Google Scholar]
- 160.Nasef A, Mazurier C, Bouchet S, Francois S, Chapel A, Thierry D, Gorin NC, Fouillard L. Leukemia inhibitory factor: role in human mesenchymal stem cells mediated immunosuppression. Cell Immunol. 2008;253(1–2):16–22. doi: 10.1016/j.cellimm.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 161.Lepelletier Y, Lecourt S, Renand A, Arnulf B, Vanneaux V, Fermand JP, Menasche P, Domet T, Marolleau JP, Hermine O, Larghero J. Galectin-1 and semaphorin-3A are two soluble factors conferring T-cell immunosuppression to bone marrow mesenchymal stem cell. Stem Cells Dev. 2010;19(7):1075–1079. doi: 10.1089/scd.2009.0212. [DOI] [PubMed] [Google Scholar]
- 162.Di Ianni M, Del Papa B, De Ioanni M, Moretti L, Bonifacio E, Cecchini D, Sportoletti P, Falzetti F, Tabilio A. Mesenchymal cells recruit and regulate T regulatory cells. Exp Hematol. 2008;36(3):309–318. doi: 10.1016/j.exphem.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 163.Tsyb AF, Petrov VN, Konoplyannikov AG, Saypina EV, Lepechina LA, Kalsina S, Semenkova IV, Agaeva EV. In vitro inhibitory effect of mesenchymal stem cells on zymosan-induced production of reactive oxygen species. Bull Exp Biol Med. 2008;146(1):158–164. doi: 10.1007/s10517-008-0238-8. [DOI] [PubMed] [Google Scholar]
- 164.Jiang XX, Zhang Y, Liu B, Zhang SX, Wu Y, Yu XD, Mao N. Human mesenchymal stem cells inhibit differentiation and function of monocyte-derived dendritic cells. Blood. 2005;105(10):4120–4126. doi: 10.1182/blood-2004-02-0586. [DOI] [PubMed] [Google Scholar]
- 165.Oh JY, Lee RH, Yu JM, Ko JH, Lee HJ, Ko AY, Roddy GW, Prockop DJ. Intravenous mesenchymal stem cells prevented rejection of allogeneic corneal transplants by aborting the early inflammatory response. Mol Ther. 2012;20(11):2143–2152. doi: 10.1038/mt.2012.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Zhang Y, Ge XH, Guo XJ, Guan SB, Li XM, Gu W, Xu WG. Bone marrow mesenchymal stem cells inhibit the function of dendritic cells by secreting galectin-1. Biomed Res Int. 2017;2017:3248605. doi: 10.1155/2017/3248605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ding Y, Liang X, Zhang Y, Yi L, Shum HC, Chen Q, Chan BP, Fan H, Liu Z, Tergaonkar V, Qi Z, Tse HF, Lian Q. Rap1 deficiency-provoked paracrine dysfunction impairs immunosuppressive potency of mesenchymal stem cells in allograft rejection of heart transplantation. Cell Death Dis. 2018;9(3):386. doi: 10.1038/s41419-018-0414-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.He JG, Xie QL, Li BB, Zhou L, Yan D. Exosomes derived from IDO1-overexpressing rat bone marrow mesenchymal stem cells promote immunotolerance of cardiac allografts. Cell Transplant. 2018 doi: 10.1177/0963689718805375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sivanathan KN, Gronthos S, Grey ST, Rojas-Canales D, Coates PT. Immunodepletion and hypoxia preconditioning of mouse compact bone cells as a novel protocol to isolate highly immunosuppressive mesenchymal stem cells. Stem Cells Dev. 2017;26(7):512–527. doi: 10.1089/scd.2016.0180. [DOI] [PubMed] [Google Scholar]
- 170.Killer MC, Nold P, Henkenius K, Fritz L, Riedlinger T, Barckhausen C, Frech M, Hackstein H, Neubauer A, Brendel C. Immunosuppressive capacity of mesenchymal stem cells correlates with metabolic activity and can be enhanced by valproic acid. Stem Cell Res Ther. 2017;8(1):100. doi: 10.1186/s13287-017-0553-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Li W, Ren G, Huang Y, Su J, Han Y, Li J, Chen X, Cao K, Chen Q, Shou P, Zhang L, Yuan ZR, Roberts AL, Shi S, Le AD, Shi Y. Mesenchymal stem cells: a double-edged sword in regulating immune responses. Cell Death Differ. 2012;19(9):1505–1513. doi: 10.1038/cdd.2012.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Cuerquis J, Romieu-Mourez R, François M, Routy J-P, Young YK, Zhao J, Eliopoulos N. Human mesenchymal stromal cells transiently increase cytokine production by activated T cells before suppressing T-cell proliferation: effect of interferon-γ and tumor necrosis factor-α; stimulation. Cytotherapy. 2014;16(2):191–202. doi: 10.1016/j.jcyt.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 173.Siekmann AF, Affolter M, Belting HG. The tip cell concept 10 years after: new players tune in for a common theme. Exp Cell Res. 2013;319(9):1255–1263. doi: 10.1016/j.yexcr.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 174.Watt SM, Gullo F, van der Garde M, Markeson D, Camicia R, Khoo CP, Zwaginga JJ. The angiogenic properties of mesenchymal stem/stromal cells and their therapeutic potential. Brit Med Bull. 2013;108(1):25–53. doi: 10.1093/bmb/ldt031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Orlic D, Kajstura J, Chimenti S, Bodine DM, Leri A, Anversa P. Bone marrow stem cells regenerate infarcted myocardium. Pediatr Transplant. 2003;7:86–88. doi: 10.1034/j.1399-3046.7.s3.13.x. [DOI] [PubMed] [Google Scholar]
- 176.Zhang B, Wu XD, Zhang X, Sun YX, Yan YM, Shi H, Zhu YH, Wu LJ, Pan ZJ, Zhu W, Qian H, Xu WR. Human umbilical cord mesenchymal stem cell exosomes enhance angiogenesis through the Wnt4/beta-catenin pathway. Stem Cell Transl Med. 2015;4(5):513–522. doi: 10.5966/sctm.2014-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Merino-Gonzalez C, Zuniga FA, Escudero C, Ormazabal V, Reyes C, Nova-Lamperti E, Salomon C, Aguayo C. Mesenchymal stem cell-derived extracellular vesicles promote angiogenesis: potencial clinical application. Front Physiol. 2016 doi: 10.3389/fphys.2016.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kinnaird T, Stabile E, Burnett MS, Shou M, Lee CW, Barr S, Fuchs S, Epstein SE. Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation. 2004;109(12):1543–1549. doi: 10.1161/01.Cir.0000124062.31102.57. [DOI] [PubMed] [Google Scholar]
- 179.Hung SC, Pochampally RR, Chen SC, Hsu SC, Prockop DJ. Angiogenic effects of human multipotent stromal cell conditioned medium activate the PI3K-Akt pathway in hypoxic endothelial cells to inhibit apoptosis, increase survival, and stimulate angiogenesis. Stem Cells. 2007;25(9):2363–2370. doi: 10.1634/stemcells.2006-0686. [DOI] [PubMed] [Google Scholar]
- 180.Kinnaird T, Stabile E, Burnett MS, Epstein SE. Bone marrow-derived cells for enhancing collateral development-Mechanisms, animal data, and initial clinical experiences. Circ Res. 2004;95(4):354–363. doi: 10.1161/01.Res.0000137878.26174.66. [DOI] [PubMed] [Google Scholar]
- 181.Zhang M, Mal N, Kiedrowski M, Chacko M, Askari AT, Popovic ZB, Koc ON, Penn MS. SDF-1 expression by mesenchymal stem cells results in trophic support of cardiac myocytes after myocardial infarction. Faseb J. 2007;21(12):3197–3207. doi: 10.1096/fj.06-6558com. [DOI] [PubMed] [Google Scholar]
- 182.Ratushnyy A, Ezdakova M, Yakubets D, Buravkova L. Angiogenic Activity of Human Adipose-Derived Mesenchymal Stem Cells Under Simulated Microgravity. Stem Cells Dev. 2018;27(12):831–837. doi: 10.1089/scd.2017.0262. [DOI] [PubMed] [Google Scholar]
- 183.Bao L, Meng Q, Li Y, Deng S, Yu Z, Liu Z, Zhang L, Fan H. C-Kit Positive cardiac stem cells and bone marrow–derived mesenchymal stem cells synergistically enhance angiogenesis and improve cardiac function after myocardial infarction in a paracrine manner. J Cardiac Fail. 2017;23(5):403–415. doi: 10.1016/j.cardfail.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 184.Sanz L, Santos-Valle P, Alonso-Camino V, Salas C, Serrano A, Vicario JL, Cuesta AM, Compte M, Sanchez-Martin D, Alvarez-Vallina L. Long-term in vivo imaging of human angiogenesis: critical role of bone marrow-derived mesenchymal stem cells for the generation of durable blood vessels. Microvasc Res. 2008;75(3):308–314. doi: 10.1016/j.mvr.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 185.Huang NF, Lam A, Fang Q, Sievers RE, Li S, Lee RJ. Bone marrow-derived mesenchymal stem cells in fibrin augment angiogenesis in the chronically infarcted myocardium. Regen Med. 2009;4(4):527–538. doi: 10.2217/rme.09.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Sorrell JM, Baber MA, Caplan AI. Influence of adult mesenchymal stem cells on in vitro vascular formation. Tissue Eng. 2009;15(7):1751–1761. doi: 10.1089/ten.tea.2008.0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Botto S, Streblow DN, DeFilippis V, White L, Kreklywich CN, Smith PP, Caposio P. IL-6 in human cytomegalovirus secretome promotes angiogenesis and survival of endothelial cells through the stimulation of survivin. Blood. 2011;117(1):352–361. doi: 10.1182/blood-2010-06-291245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Boomsma RA, Geenen DL. Mesenchymal stem cells secrete multiple cytokines that promote angiogenesis and have contrasting effects on chemotaxis and apoptosis. PLoS ONE. 2012 doi: 10.1371/journal.pone.0035685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Koch S, Tugues S, Li XJ, Gualandi L, Claesson-Welsh L. Signal transduction by vascular endothelial growth factor receptors. Biochem J. 2011;437:169–183. doi: 10.1042/Bj20110301. [DOI] [PubMed] [Google Scholar]
- 190.Liang X, Ding Y, Lin F, Zhang Y, Zhou X, Meng Q, Lu X, Jiang G, Zhu H, Chen Y, Lian Q, Fan H, Liu Z. Overexpression of ERBB4 rejuvenates aged mesenchymal stem cells and enhances angiogenesis via PI3K/AKT and MAPK/ERK pathways. Faseb J. 2019;33(3):4559–4570. doi: 10.1096/fj.201801690R. [DOI] [PubMed] [Google Scholar]
- 191.Qian D, Gong J, He Z, Hua J, Lin S, Xu C, Meng H, Song Z. Bone marrow-derived mesenchymal stem cells repair necrotic pancreatic tissue and promote angiogenesis by secreting cellular growth factors involved in the SDF-1 alpha /CXCR4 axis in rats. Stem Cells Int. 2015;2015:306836. doi: 10.1155/2015/306836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Dong F, Harvey J, Finan A, Weber K, Agarwal U, Penn MS. Myocardial CXCR4 expression is required for mesenchymal stem cell mediated repair following acute myocardial infarction. Circulation. 2012;126(3):314–324. doi: 10.1161/Circulationaha.111.082453. [DOI] [PubMed] [Google Scholar]
- 193.Pasquet M, Golzio M, Mery E, Rafii A, Benabbou N, Mirshahi P, Hennebelle I, Bourin P, Allal B, Teissie J, Mirshahi M, Couderc B. Hospicells (ascites-derived stromal cells) promote tumorigenicity and angiogenesis. Int J Cancer. 2010;126(9):2090–2101. doi: 10.1002/ijc.24886. [DOI] [PubMed] [Google Scholar]
- 194.Tao HY, Han ZB, Han ZC, Li ZJ. Proangiogenic features of mesenchymal stem cells and their therapeutic applications. Stem Cells Int. 2016 doi: 10.1155/2016/1314709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Zhou M, Liu Z, Liu C, Jiang XF, Wei ZQ, Qiao W, Ran F, Wang W, Qiao T, Liu CJ. Tissue engineering of small-diameter vascular grafts by endothelial progenitor cells seeding heparincoated decellularized scaffolds. J Biomed Mater Res. 2012;100(1):111–120. doi: 10.1002/jbm.b.31928. [DOI] [PubMed] [Google Scholar]
- 196.Kaga T, Kawano H, Sakaguchi M, Nakazawa T, Taniyama Y, Morishita R. Hepatocyte growth factor stimulated angiogenesis without inflammation: differential actions between hepatocyte growth factor, vascular endothelial growth factor and basic fibroblast growth factor. Vasc Pharmacol. 2012;57(1):3–9. doi: 10.1016/j.vph.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 197.Mirotsou M, Jayawardena TM, Schmeckpeper J, Gnecchi M, Dzau VJ. Paracrine mechanisms of stem cell reparative and regenerative actions in the heart. J Mol Cell Cardiol. 2011;50(2):280–289. doi: 10.1016/j.yjmcc.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kwon S, Ki SM, Park SE, Kim MJ, Hyung B, Lee NK, Shim S, Choi BO, Na DL, Lee JE, Chang JW. Anti-apoptotic effects of human Wharton’s jelly-derived mesenchymal stem cells on skeletal muscle cells mediated via secretion of XCL1. Mol Ther. 2016;24(9):1550–1560. doi: 10.1038/mt.2016.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Meirelles LD, Fontes AM, Covas DT, Caplan AI. Mechanisms involved in the therapeutic properties of mesenchymal stem cells. Cytokine Growth F R. 2009;20(5–6):419–427. doi: 10.1016/j.cytogfr.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 200.Rehman J, Traktuev D, Li J, Merfeld-Clauss S, Temm-Grove CJ, Bovenkerk JE, Pell CL, Johnstone BH, Considine RV, March KL. Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation. 2004;109(10):1292–1298. doi: 10.1161/01.CIR.0000121425.42966.F1. [DOI] [PubMed] [Google Scholar]
- 201.Togel F, Weiss K, Yang Y, Hu Z, Zhang P, Westenfelder C. Vasculotropic, paracrine actions of infused mesenchymal stem cells are important to the recovery from acute kidney injury. Am J Physiol Renal Physiol. 2007;292(5):F1626–1635. doi: 10.1152/ajprenal.00339.2006. [DOI] [PubMed] [Google Scholar]
- 202.Okazaki T, Magaki T, Takeda M, Kajiwara Y, Hanaya R, Sugiyama K, Arita K, Nishimura M, Kato Y, Kurisu K. Intravenous administration of bone marrow stromal cells increases survivin and Bcl-2 protein expression and improves sensorimotor function following ischemia in rats. Neurosci Lett. 2008;430(2):109–114. doi: 10.1016/j.neulet.2007.10.046. [DOI] [PubMed] [Google Scholar]
- 203.Wang SP, Wang ZH, Peng DY, Li SM, Wang H, Wang XH. Therapeutic effect of mesenchymal stem cells in rats with intracerebral hemorrhage: reduced apoptosis and enhanced neuroprotection. Mol Med Rep. 2012;6(4):848–854. doi: 10.3892/mmr.2012.997. [DOI] [PubMed] [Google Scholar]
- 204.Oltvai ZN, Milliman CL, Korsmeyer SJ. Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell. 1993;74(4):609–619. doi: 10.1016/0092-8674(93)90509-O. [DOI] [PubMed] [Google Scholar]
- 205.Green DR, Reed JC. Mitochondria and apoptosis. Science. 1998;281(5381):1309–1312. doi: 10.1126/science.281.5381.1309. [DOI] [PubMed] [Google Scholar]
- 206.Tang YL, Zhao Q, Qin X, Shen L, Cheng L, Ge J, Phillips MI. Paracrine action enhances the effects of autologous mesenchymal stem cell transplantation on vascular regeneration in rat model of myocardial infarction. Ann Thorac Surg. 2005;80(1):229–236. doi: 10.1016/j.athoracsur.2005.02.072. [DOI] [PubMed] [Google Scholar]
- 207.Zhang Y, Yu S, Tuazon JP, Lee JY, Corey S, Kvederis L, Kingsbury C, Kaneko Y, Borlongan CV. Neuroprotective effects of human bone marrow mesenchymal stem cells against cerebral ischemia are mediated in part by an anti-apoptotic mechanism. Neural Regen Res. 2019;14(4):597–604. doi: 10.4103/1673-5374.247464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Pan GZ, Yang Y, Zhang J, Liu W, Wang GY, Zhang YC, Yang Q, Zhai FX, Tai Y, Liu JR, Zhang Q, Chen GH. Bone marrow mesenchymal stem cells ameliorate hepatic ischemia/reperfusion injuries via inactivation of the MEK/ERK signaling pathway in rats. J Surg Res. 2012;178(2):935–948. doi: 10.1016/j.jss.2012.04.070. [DOI] [PubMed] [Google Scholar]
- 209.Gerber HP, Dixit V, Ferrara N. Vascular endothelial growth factor induces expression of the antiapoptotic proteins Bcl-2 and A1 in vascular endothelial cells. J Biol Chem. 1998;273(21):13313–13316. doi: 10.1074/jbc.273.21.13313. [DOI] [PubMed] [Google Scholar]
- 210.Kamarajan P, Bunek J, Lin Y, Nunez G, Kapila YL. Receptor-interacting protein shuttles between cell death and survival signaling pathways. Mol Biol Cell. 2010;21(3):481–488. doi: 10.1091/mbc.E09-06-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Liu ZY, Ganju RK, Wang JF, Schweitzer K, Weksler B, Avraham S, Groopman JE. Characterization of signal transduction pathways in human bone marrow endothelial cells. Blood. 1997;90(6):2253–2259. doi: 10.1182/blood.V90.6.2253. [DOI] [PubMed] [Google Scholar]
- 212.Redondo J, Sarkar P, Kemp K, Heesom KJ, Wilkins A, Scolding NJ, Rice CM. Dysregulation of mesenchymal stromal cell antioxidant responses in progressive multiple sclerosis. Stem Cells Transl Med. 2018;7(10):748–758. doi: 10.1002/sctm.18-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Blaser H, Dostert C, Mak TW, Brenner D. TNF and ROS crosstalk in inflammation. Trends Cell Biol. 2016;26(4):249–261. doi: 10.1016/j.tcb.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 214.Russell EG, Cotter TG. New insight into the role of reactive oxygen species (ROS) in cellular signal-transduction processes. Int Rev Cel Mol Bio. 2015;319:221–254. doi: 10.1016/bs.ircmb.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 215.Kreuz S, Fischle W. Oxidative stress signaling to chromatin in health and disease. Epigenomics. 2016;8(6):843–862. doi: 10.2217/epi-2016-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Ohkouchi S, Block GJ, Katsha AM, Kanehira M, Ebina M, Kikuchi T, Saijo Y, Nukiwa T, Prockop DJ. Mesenchymal stromal cells protect cancer cells from ROS-induced apoptosis and enhance the Warburg effect by secreting STC1. Mol Ther. 2012;20(2):417–423. doi: 10.1038/mt.2011.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Li J, Li D, Liu X, Tang S, Wei F. Human umbilical cord mesenchymal stem cells reduce systemic inflammation and attenuate LPS-induced acute lung injury in rats. J Inflamm. 2012;9(1):33. doi: 10.1186/1476-9255-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Whone AL, Kemp K, Sun M, Wilkins A, Scolding NJ. Human bone marrow mesenchymal stem cells protect catecholaminergic and serotonergic neuronal perikarya and transporter function from oxidative stress by the secretion of glial-derived neurotrophic factor. Brain Res. 2012;1431:86–96. doi: 10.1016/j.brainres.2011.10.038. [DOI] [PubMed] [Google Scholar]
- 219.Liu DJ, Huang LP, Wang YL, Wang W, Wehrens XHT, Belousova T, Abdelrahim M, DiMattia G, Sheikh-Hamad D. Human stanniocalcin-1 suppresses angiotensin II-induced superoxide generation in cardiomyocytes through UCP3-mediated anti-oxidant pathway. PLoS ONE. 2012 doi: 10.1371/journal.pone.0036994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Ono M, Ohkouchi S, Kanehira M, Tode N, Kobayashi M, Ebina M, Nukiwa T, Irokawa T, Ogawa H, Akaike T, Okada Y, Kurosawa H, Kikuchi T, Ichinose M. Mesenchymal stem cells correct inappropriate epithelial-mesenchyme relation in pulmonary fibrosis using stanniocalcin-1. Mol Ther. 2015;23(3):549–560. doi: 10.1038/mt.2014.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Ono M, Ohkouchi S, Kanehira M, Tode N, Kikuchi T, Ichinose M (2014) The Enhancement Of Stanniocalcin-1 (STC1) Secretion Increases The Ability Of Mesenchymal Stem Cells (MSCs) Reducing Bleomycin-Induced Lung Fibrosis In Mice Model Through Inhibition Of ROS/Endoplasmic Reticulum Stress (ER-Stress)/TGF?1 Pathway. In: C108. IS THERE ANYTHING THEY CAN'T DO? DIVERSE FUNCTIONAL ACTIVITIES OF MESENCHYMAL STEM AND STROMAL CELLS. American Thoracic Society International Conference Abstracts. American Thoracic Society, pp A5305-A5305. doi:10.1164/ajrccm-conference.2014.189.1_MeetingAbstracts.A5305
- 222.Oh JY, Ko JH, Lee HJ, Yu JM, Choi H, Kim MK, Wee WR, Prockop DJ. Mesenchymal stem/stromal cells inhibit the NLRP3 inflammasome by decreasing mitochondrial reactive oxygen species. Stem Cells. 2014;32(6):1553–1563. doi: 10.1002/stem.1608. [DOI] [PubMed] [Google Scholar]
- 223.Chen XX, Zhang YL, Wang WJ, Liu ZQ, Meng JG, Han ZH. Mesenchymal stem cells modified with heme oxygenase-1 have enhanced paracrine function and attenuate lipopolysaccharide-induced inflammatory and oxidative damage in pulmonary microvascular endothelial cells. Cell Physiol Biochem. 2018;49(1):101–122. doi: 10.1159/000492847. [DOI] [PubMed] [Google Scholar]
- 224.Zhang ZH, Zhu W, Ren HZ, Zhao X, Wang S, Ma HC, Shi XL. Mesenchymal stem cells increase expression of heme oxygenase-1 leading to anti-inflammatory activity in treatment of acute liver failure. Stem Cell Res Ther. 2017;8(1):70. doi: 10.1186/s13287-017-0524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Yu J, Li MC, Qu ZL, Yan D, Li DJ, Ruan QR. SDF-1/CXCR4-Mediated migration of transplanted bone marrow stromal cells toward areas of heart myocardial infarction through activation of PI3K/Akt. J Cardiovasc Pharm. 2010;55(5):496–505. doi: 10.1097/FJC.0b013e3181d7a384. [DOI] [PubMed] [Google Scholar]
- 226.Hoban DB, Howard L, Dowd E. Gdnf-secreting mesenchymal stem cells provide localized neuroprotection in an inflammation-driven rat model of Parkinson’s Disease. Neuroscience. 2015;303:402–411. doi: 10.1016/j.neuroscience.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 227.Lv BK, Li F, Fang J, Xu LM, Sun CM, Han JB, Hua T, Zhang ZF, Feng ZM, Wang QH, Jiang XD. Activated microglia induce bone marrow mesenchymal stem cells to produce glial cell-derived neurotrophic factor and protect neurons against oxygen-glucose deprivation injury. Front Cell Neurosci. 2016 doi: 10.3389/fncel.2016.00283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Consentius C, Reinke P, Volk HD. Immunogenicity of allogeneic mesenchymal stromal cells: what has been seen in vitro and in vivo? Regen Med. 2015;10(3):305–315. doi: 10.2217/Rme.15.14. [DOI] [PubMed] [Google Scholar]
- 229.Sivanathan KN, Gronthos S, Rojas-Canales D, Thierry B, Coates PT. Interferon-gamma modification of mesenchymal stem cells: implications of autologous and allogeneic mesenchymal stem cell therapy in allotransplantation. Stem Cell Rev. 2014;10(3):351–375. doi: 10.1007/s12015-014-9495-2. [DOI] [PubMed] [Google Scholar]
- 230.Duffy MM, Pindjakova J, Hanley SA, McCarthy C, Weidhofer GA, Sweeney EM, English K, Shaw G, Murphy JM, Barry FP, Mahon BP, Belton O, Ceredig R, Griffin MD. Mesenchymal stem cell inhibition of T-helper 17 cell- differentiation is triggered by cell-cell contact and mediated by prostaglandin E2 via the EP4 receptor. Eur J Immunol. 2011;41(10):2840–2851. doi: 10.1002/eji.201141499. [DOI] [PubMed] [Google Scholar]
- 231.Kovach TK, Dighe AS, Lobo PI, Cui Q. Interactions between MSCs and immune cells: implications for bone healing. J Immunol Res. 2015;2015:752510. doi: 10.1155/2015/752510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Luz-Crawford P, Noel D, Fernandez X, Khoury M, Figueroa F, Carrion F, Jorgensen C, Djouad F. Mesenchymal stem cells repress Th17 molecular program through the PD-1 pathway. PLoS ONE. 2012 doi: 10.1371/journal.pone.0045272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Sioud M, Mobergslien A, Boudabous A, Floisand Y. Mesenchymal stem cell-mediated T cell suppression occurs through secreted galectins. Int J Oncol. 2011;38(2):385–390. doi: 10.3892/ijo.2010.869. [DOI] [PubMed] [Google Scholar]
- 234.English K, Ryan JM, Tobin L, Murphy MJ, Barry FP, Mahon BP. Cell contact, prostaglandin E(2) and transforming growth factor beta 1 play non-redundant roles in human mesenchymal stem cell induction of CD4+CD25(High) forkhead box P3+ regulatory T cells. Clin Exp Immunol. 2009;156(1):149–160. doi: 10.1111/j.1365-2249.2009.03874.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Casado JG, Tarazona R, Sanchez-Margallo FM. NK and MSCs crosstalk: The sense of immunomodulation and their sensitivity. Stem Cell Rev Rep. 2013;9(2):184–189. doi: 10.1007/s12015-013-9430-y. [DOI] [PubMed] [Google Scholar]
- 236.Chatterjee D, Tufa DM, Baehre H, Hass R, Schmidt RE, Jacobs R. Natural killer cells acquire CD73 expression upon exposure to mesenchymal stem cells. Blood. 2014;123(4):594–595. doi: 10.1182/blood-2013-09-524827. [DOI] [PubMed] [Google Scholar]
- 237.Li Y, Zhang D, Xu L, Dong L, Zheng J, Lin Y, Huang J, Zhang Y, Tao Y, Zang X, Li D, Du M. Cell-cell contact with proinflammatory macrophages enhances the immunotherapeutic effect of mesenchymal stem cells in two abortion models. Cell Mol Immunol. 2019 doi: 10.1038/s41423-019-0204-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Zhang B, Liu R, Shi D, Liu XX, Chen Y, Dou XW, Zhu XS, Lu CH, Liang W, Liao LM, Zenke M, Zhao RCH. Mesenchymal stem cells induce mature dendritic cells into a novel Jagged-2-dependent regulatory dendritic cell population. Blood. 2009;113(1):46–57. doi: 10.1182/blood-2008-04-154138. [DOI] [PubMed] [Google Scholar]
- 239.Loibl M, Binder A, Herrmann M, Duttenhoefer F, Richards RG, Nerlich M, Alini M, Verrier S. Direct cell-cell contact between mesenchymal stem cells and endothelial progenitor cells induces a pericyte-like phenotype in vitro. Biomed Res Int. 2014 doi: 10.1155/2014/395781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Menge T, Gerber M, Wataha K, Reid W, Guha S, Cox CS, Dash P, Reitz MS, Khakoo AY, Pati S. Human mesenchymal stem cells inhibit endothelial proliferation and angiogenesis via cell-cell contact through modulation of the VE-Cadherin/beta-Catenin signaling pathway. Stem Cells Dev. 2013;22(1):148–157. doi: 10.1089/scd.2012.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Paliwal S, Chaudhuri R, Agrawal A, Mohanty S. Regenerative abilities of mesenchymal stem cells through mitochondrial transfer. J Biomed Sci. 2018;25(1):31–31. doi: 10.1186/s12929-018-0429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Babenko VA, Silachev DN, Popkov VA, Zorova LD, Pevzner IB, Plotnikov EY, Sukhikh GT, Zorov DB. Miro1 enhances mitochondria transfer from multipotent mesenchymal stem cells (MMSC) to neural cells and improves the efficacy of cell recovery. Molecules. 2018 doi: 10.3390/molecules23030687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Torralba D, Baixauli F, Sanchez-Madrid F. Mitochondria know no boundaries: mechanisms and functions of intercellular mitochondrial transfer. Front Cell Dev Biol. 2016;4:107. doi: 10.3389/fcell.2016.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Sinha P, Islam MN, Bhattacharya S, Bhattacharya J. Intercellular mitochondrial transfer: bioenergetic crosstalk between cells. Curr Opin Genet Dev. 2016;38:97–101. doi: 10.1016/j.gde.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Feng Y, Zhu R, Shen J, Wu J, Lu W, Zhang J, Zhang J, Liu K. Human bone marrow mesenchymal stem cells rescue endothelial cells experiencing chemotherapy stress by mitochondrial transfer via tunneling nanotubes. Stem Cells Dev. 2019;28(10):674–682. doi: 10.1089/scd.2018.0248. [DOI] [PubMed] [Google Scholar]
- 246.Wanet A, Remacle N, Najar M, Sokal E, Arnould T, Najimi M, Renard P. Mitochondrial remodeling in hepatic differentiation and dedifferentiation. Int J Biochem Cell Biol. 2014;54:174–185. doi: 10.1016/j.biocel.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 247.Youle RJ, Narendra DP. Mechanisms of mitophagy. Nat Rev Mol Cell Biol. 2011;12(1):9–14. doi: 10.1038/nrm3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Boukelmoune N, Chiu GS, Kavelaars A, Heijnen CJ. Mitochondrial transfer from mesenchymal stem cells to neural stem cells protects against the neurotoxic effects of cisplatin. Acta Neuropathol Commun. 2018;6(1):139. doi: 10.1186/s40478-018-0644-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Watkins J, Basu S, Bogenhagen DF. A quantitative proteomic analysis of mitochondrial participation in p19 cell neuronal differentiation. J Proteome Res. 2008;7(1):328–338. doi: 10.1021/pr070300g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Ding WX, Yin XM. Mitophagy: mechanisms, pathophysiological roles, and analysis. Biol Chem. 2012;393(7):547–564. doi: 10.1515/hsz-2012-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Jiang D, Gao F, Zhang Y, Wong DS, Li Q, Tse HF, Xu G, Yu Z, Lian Q. Mitochondrial transfer of mesenchymal stem cells effectively protects corneal epithelial cells from mitochondrial damage. Cell Death Dis. 2016;7(11):e2467. doi: 10.1038/cddis.2016.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Jiang D, Xiong GY, Feng H, Zhang Z, Chen PK, Yan B, Chen L, Gandhervin K, Ma CY, Li C, Han S, Zhang YL, Liao C, Lee TL, Tse HF, Fu QL, Chiu K, Lian QZ. Donation of mitochondria by iPSC-derived mesenchymal stem cells protects retinal ganglion cells against mitochondrial complex I defect-induced degeneration. Theranostics. 2019;9(8):2395–2410. doi: 10.7150/thno.29422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Li H, Wang C, He T, Zhao T, Chen YY, Shen YL, Zhang X, Wang LL. Mitochondrial transfer from bone marrow mesenchymal stem cells to motor neurons in spinal cord injury rats via gap junction. Theranostics. 2019;9(7):2017–2035. doi: 10.7150/thno.29400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Ahmad T, Mukherjee S, Pattnaik BR, Kumar M, Singh S, Rehman R, Kumar M, Jha A, Wani M, Mabalirajan U, Ghosh B, Sinha Roy S, Agrawal A. Miro 1 knockdown in stem cells inhibits mitochondrial donation mediated rescue of bronchial epithelial injury. Biophys J. 2013;104(2):659a. doi: 10.1016/j.bpj.2012.11.3638. [DOI] [Google Scholar]
- 255.Ahmad T, Mukherjee S, Pattnaik B, Kumar M, Singh S, Kumar M, Rehman R, Tiwari BK, Jha KA, Barhanpurkar AP, Wani MR, Roy SS, Mabalirajan U, Ghosh B, Agrawal A. Miro1 regulates intercellular mitochondrial transport & enhances mesenchymal stem cell rescue efficacy. Embo J. 2014;33(9):994–1010. doi: 10.1002/embj.201386030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Zhang Y, Yu Z, Jiang D, Liang X, Liao S, Zhang Z, Yue W, Li X, Chiu SM, Chai YH, Liang Y, Chow Y, Han S, Xu A, Tse HF, Lian Q. iPSC-MSCs with high intrinsic MIRO1 and sensitivity to TNF-alpha yield efficacious mitochondrial transfer to rescue anthracycline-induced cardiomyopathy. Stem Cell Reports. 2016;7(4):749–763. doi: 10.1016/j.stemcr.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Pacak CA, Preble JM, Kondo H, Seibel P, Levitsky S, Del Nido PJ, Cowan DB, McCully JD. Actin-dependent mitochondrial internalization in cardiomyocytes: evidence for rescue of mitochondrial function. Biol Open. 2015;4(5):622–626. doi: 10.1242/bio.201511478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Sinclair KA, Yerkovich ST, Hopkins PM, Chambers DC. Characterization of intercellular communication and mitochondrial donation by mesenchymal stromal cells derived from the human lung. Stem Cell Res Ther. 2016;7(1):91. doi: 10.1186/s13287-016-0354-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Morrison TJ, Jackson MV, Cunningham EK, Kissenpfennig A, McAuley DF, O'Kane CM, Krasnodembskaya AD. Mesenchymal stromal cells modulate macrophages in clinically relevant lung injury models by extracellular vesicle mitochondrial transfer. Am J Respir Crit Care Med. 2017;196(10):1275–1286. doi: 10.1164/rccm.201701-0170OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Dostert G, Mesure B, Menu P, Velot É. How do mesenchymal stem cells influence or are influenced by microenvironment through extracellular vesicles communication? Front Cell Dev Biol. 2017;5:6–6. doi: 10.3389/fcell.2017.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200(4):373–383. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Lai RC, Tan SS, Yeo RWY, Choo ABH, Reiner AT, Su Y, Shen Y, Fu Z, Alexander L, Sze SK, Lim SK. MSC secretes at least 3 EV types each with a unique permutation of membrane lipid, protein and RNA. J Extracell Ves. 2016;5:29828–29828. doi: 10.3402/jev.v5.29828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Li Y, Cheng Q, Hu G, Deng T, Wang Q, Zhou J, Su X. Extracellular vesicles in mesenchymal stromal cells: A novel therapeutic strategy for stroke. Exp Ther Med. 2018;15(5):4067–4079. doi: 10.3892/etm.2018.5993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Konala VB, Mamidi MK, Bhonde R, Das AK, Pochampally R, Pal R. The current landscape of the mesenchymal stromal cell secretome: A new paradigm for cell-free regeneration. Cytotherapy. 2016;18(1):13–24. doi: 10.1016/j.jcyt.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Galieva LR, James V, Mukhamedshina YO, Rizvanov AA. Therapeutic potential of extracellular vesicles for the treatment of nerve disorders. Front Neurosci. 2019;13:163. doi: 10.3389/fnins.2019.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Montemurro T, Vigano M, Ragni E, Barilani M, Parazzi V, Boldrin V, Lavazza C, Montelatici E, Banfi F, Lauri E, Giovanelli S, Baccarin M, Guerneri S, Giordano R, Lazzari L. Angiogenic and anti-inflammatory properties of mesenchymal stem cells from cord blood: soluble factors and extracellular vesicles for cell regeneration. Eur J Cell Biol. 2016;95(6–7):228–238. doi: 10.1016/j.ejcb.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 267.Anderson JD, Johansson HJ, Graham CS, Vesterlund M, Pham MT, Bramlett CS, Montgomery EN, Mellema MS, Bardini RL, Contreras Z, Hoon M, Bauer G, Fink KD, Fury B, Hendrix KJ, Chedin F, El-Andaloussi S, Hwang B, Mulligan MS, Lehtio J, Nolta JA. Comprehensive proteomic analysis of mesenchymal stem cell exosomes reveals modulation of angiogenesis via nuclear factor-KappaB signaling. Stem Cells. 2016;34(3):601–613. doi: 10.1002/stem.2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Nakamura Y, Miyaki S, Ishitobi H, Matsuyama S, Nakasa T, Kamei N, Akimoto T, Higashi Y, Ochi M. Mesenchymal-stem-cell-derived exosomes accelerate skeletal muscle regeneration. Febs Lett. 2015;589(11):1257–1265. doi: 10.1016/j.febslet.2015.03.031. [DOI] [PubMed] [Google Scholar]
- 269.Feng YL, Huang W, Wani M, Yu XY, Ashraf M. Ischemic Preconditioning potentiates the protective effect of stem cells through secretion of exosomes by targeting Mecp2 via miR-22. PLoS ONE. 2014 doi: 10.1371/journal.pone.0088685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Wang X, Gu H, Qin D, Yang L, Huang W, Essandoh K, Wang Y, Caldwell CC, Peng T, Zingarelli B, Fan GC. Exosomal miR-223 contributes to mesenchymal stem cell-elicited cardioprotection in polymicrobial sepsis. Sci Rep. 2015;5:13721. doi: 10.1038/srep13721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Song Y, Dou H, Li X, Zhao X, Li Y, Liu D, Ji J, Liu F, Ding L, Ni Y, Hou Y. Exosomal miR-146a contributes to the enhanced therapeutic efficacy of interleukin-1beta-primed mesenchymal stem cells against sepsis. Stem Cells. 2017;35(5):1208–1221. doi: 10.1002/stem.2564. [DOI] [PubMed] [Google Scholar]
- 272.Fang S, Xu C, Zhang Y, Xue C, Yang C, Bi H, Qian X, Wu M, Ji K, Zhao Y, Wang Y, Liu H, Xing X. Umbilical cord-derived mesenchymal stem cell-derived exosomal micrornas suppress myofibroblast differentiation by inhibiting the transforming growth factor-beta/SMAD2 pathway during wound healing. Stem Cells Transl Med. 2016;5(10):1425–1439. doi: 10.5966/sctm.2015-0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Tomasoni S, Longaretti L, Rota C, Morigi M, Conti S, Gotti E, Capelli C, Introna M, Remuzzi G, Benigni A. Transfer of growth factor receptor mRNA via exosomes unravels the regenerative effect of mesenchymal stem cells. Stem Cells Dev. 2013;22(5):772–780. doi: 10.1089/scd.2012.0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Zhu LP, Tian T, Wang JY, He JN, Chen T, Pan M, Xu L, Zhang HX, Qiu XT, Li CC, Wang KK, Shen H, Zhang GG, Bai YP. Hypoxia-elicited mesenchymal stem cell-derived exosomes facilitates cardiac repair through miR-125b-mediated prevention of cell death in myocardial infarction. Theranostics. 2018;8(22):6163–6177. doi: 10.7150/thno.28021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Gong XH, Liu H, Wang SJ, Liang SW, Wang GG. Exosomes derived from SDF1-overexpressing mesenchymal stem cells inhibit ischemic myocardial cell apoptosis and promote cardiac endothelial microvascular regeneration in mice with myocardial infarction. J Cell Physiol. 2019;234(8):13878–13893. doi: 10.1002/jcp.28070. [DOI] [PubMed] [Google Scholar]
- 276.Khare D, Or R, Resnick I, Barkatz C, Almogi-Hazan O, Avni B. Mesenchymal stromal cell-derived exosomes affect mRNA expression and function of B-lymphocytes. Front Immunol. 2018;9:3053. doi: 10.3389/fimmu.2018.03053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Di Trapani M, Bassi G, Midolo M, Gatti A, Kamga PT, Cassaro A, Carusone R, Adamo A, Krampera M. Differential and transferable modulatory effects of mesenchymal stromal cell-derived extracellular vesicles on T, B and NK cell functions. Sci Rep. 2016;6:24120. doi: 10.1038/srep24120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Del Fattore A, Luciano R, Pascucci L, Goffredo BM, Giorda E, Scapaticci M, Fierabracci A, Muraca M. Immunoregulatory effects of mesenchymal stem cell-derived extracellular vesicles on T Lymphocytes. Cell Transplant. 2015;24(12):2615–2627. doi: 10.3727/096368915X687543. [DOI] [PubMed] [Google Scholar]
- 279.Kerkela E, Laitinen A, Rabina J, Valkonen S, Takatalo M, Larjo A, Veijola J, Lampinen M, Siljander P, Lehenkari P, Alfthan K, Laitinen S. Adenosinergic immunosuppression by human mesenchymal stromal cells requires co-operation with T cells. Stem Cells. 2016;34(3):781–790. doi: 10.1002/stem.2280. [DOI] [PubMed] [Google Scholar]
- 280.Pakravan K, Babashah S, Sadeghizadeh M, Mowla SJ, Mossahebi-Mohammadi M, Ataei F, Dana N, Javan M. MicroRNA-100 shuttled by mesenchymal stem cell-derived exosomes suppresses in vitro angiogenesis through modulating the mTOR/HIF-1alpha/VEGF signaling axis in breast cancer cells. Cell Oncol. 2017;40(5):457–470. doi: 10.1007/s13402-017-0335-7. [DOI] [PubMed] [Google Scholar]
- 281.Lopatina T, Gai C, Deregibus MC, Kholia S, Camussi G. Cross Talk between cancer and mesenchymal stem cells through extracellular vesicles carrying nucleic acids. Front Oncol. 2016;6:125. doi: 10.3389/fonc.2016.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Whiteside TL. Exosome and mesenchymal stem cell cross-talk in the tumor microenvironment. Semin Immunol. 2018;35:69–79. doi: 10.1016/j.smim.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Yang Y, Bucan V, Baehre H, von der Ohe J, Otte A, Hass R. Acquisition of new tumor cell properties by MSC-derived exosomes. Int J Oncol. 2015;47(1):244–252. doi: 10.3892/ijo.2015.3001. [DOI] [PubMed] [Google Scholar]
- 284.Zhou J, Tan X, Tan Y, Li Q, Ma J, Wang G. Mesenchymal stem cell derived exosomes in cancer progression, metastasis and drug delivery: a comprehensive review. J Cancer. 2018;9(17):3129–3137. doi: 10.7150/jca.25376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Carty F, Mahon BP, English K. The influence of macrophages on mesenchymal stromal cell therapy: passive or aggressive agents? Clin Exp Immunol. 2017;188(1):1–11. doi: 10.1111/cei.12929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Engela AU, Baan CC, Peeters AMA, Weimar W, Hoogduijn MJ. Interaction between adipose tissue-derived mesenchymal stem cells and regulatory T-Cells. Cell Transplant. 2013;22(1):41–54. doi: 10.3727/096368912x636984. [DOI] [PubMed] [Google Scholar]
- 287.Ayala-Cuellar AP, Kang JH, Jeung EB, Choi KC. Roles of mesenchymal stem cells in tissue regeneration and immunomodulation. Biomol Ther. 2019;27(1):25–33. doi: 10.4062/biomolther.2017.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Braza F, Dirou S, Forest V, Sauzeau V, Hassoun D, Chesne J, Cheminant-Muller MA, Sagan C, Magnan A, Lemarchand P. Mesenchymal stem cells induce suppressive macrophages through phagocytosis in a mouse model of asthma. Stem Cells. 2016;34(7):1836–1845. doi: 10.1002/stem.2344. [DOI] [PubMed] [Google Scholar]
- 289.Ferreira JR, Teixeira GQ, Santos SG, Barbosa MA, Almeida-Porada G, Goncalves RM. Mesenchymal stromal cell secretome: influencing therapeutic potential by cellular pre-conditioning. Front Immunol. 2018;9:2837. doi: 10.3389/fimmu.2018.02837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Zimmermann JA, Hettiaratchi MH, McDevitt TC. Enhanced immunosuppression of T cells by sustained presentation of bioactive interferon-gamma within three-dimensional mesenchymal stem cell constructs. Stem Cell Transl Med. 2017;6(1):223–237. doi: 10.5966/sctm.2016-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Bartosh TJ, Ylostalo JH, Mohammadipoor A, Bazhanov N, Coble K, Claypool K, Lee RH, Choi H, Prockop DJ. Aggregation of human mesenchymal stromal cells (MSCs) into 3D spheroids enhances their antiinflammatory properties. P Natl Acad Sci USA. 2010;107(31):13724–13729. doi: 10.1073/pnas.1008117107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Mao AS, Ozkale B, Shah NJ, Vining KH, Descombes T, Zhang LY, Tringides CM, Wong SW, Shin JW, Scadden DT, Weitz DA, Mooney DJ. Programmable microencapsulation for enhanced mesenchymal stem cell persistence and immunomodulation. P Natl Acad Sci USA. 2019;116(31):15392–15397. doi: 10.1073/pnas.1819415116. [DOI] [PMC free article] [PubMed] [Google Scholar]