Abstract
Little research has explored the implications of stress inside and outside of the family as a risk factor for psychological symptoms in adolescents of depressed mothers. In a sample of 115 adolescents and their mothers with and without depression histories, adolescents’ family and peer stress exposure was measured through the Responses to Stress Questionnaire, and adolescents’ anxious/depressed symptoms were measured with the Youth Self Report and Child Behavior Checklist. Mothers reported their current depression symptoms on the Beck Depression Inventory-II. Results suggest that adolescents of mothers with depression histories and current depression symptoms experience more family and peer stress than adolescents of nondepressed mothers. In multiple linear regression analyses, current maternal depression symptoms moderated the relation between adolescent peer stress and adolescent anxious/depressed symptoms, such that peer stress was associated with anxious/depressed symptoms when maternal depression symptoms were average or high, but not when maternal depression symptoms were low.
Keywords: Maternal depression, Peer stress, Family stress, Adolescence
Overview
Exposure to stress is a key mechanism for the development of anxiety and depression [1, 2]. Children of mothers with a history of depression are at marked risk for anxiety and depression symptoms and disorder during adolescence [3–5], in part because they experience life stress at higher frequencies, at greater severities, and for longer durations than children of mothers without a history of depression [6, 7]. Heightened stress exposure within families of depressed mothers and its association with internalizing symptoms in children and adolescents is well-documented in previous research [8–11]. More recently, studies have demonstrated that these children may experience more stress outside of the home, as well, especially in their peer relationships [7, 12]. However, relatively little research has explored the implications of family and peer stress together as risk factors for the development of internalizing symptoms, and how children’s stress exposure interacts with mothers’ current depression symptoms in families with and without maternal depression histories. In the current study, we examine exposure to stress both within and outside the family in children and adolescents of mothers with and without depression histories, investigate associations with child and adolescent symptoms of anxiety and depression, and explore current maternal depression symptoms as a possible moderator of these associations.
Exposure to Stress in Offspring of Mothers With and Without Depression Histories
Experiences inside and outside of the family have important implications for child and adolescent development. During adolescence, time spent with peers grows, and peer relationships dramatically increase in salience and complexity. However, parental influence is not necessarily lost relative to peer influence during this time. Despite beliefs that the quality of the parent–child relationship degrades in the transition from childhood to adolescence, parents continue to provide critical socioemotional resources in the second decade of life [13–15]. As such, both family and peer domains provide integral contexts for stress exposure and are potential sources of risk for the development of psychological symptoms.
Family Stress
Children of depressed mothers are exposed to higher levels of family stress than children of nondepressed mothers [6]. Specifically, children are exposed to impaired parenting behaviors and caregiving practices associated with symptoms of depression [16]. Depressed mothers display fewer warm and responsive behaviors and more disengaged and intrusive behaviors than nondepressed mothers when interacting with their children. Depressed mothers tend to vacillate between disengaged and intrusive parenting, and the unpredictability of maternal behavior can be a source of child stress [17]. Children of depressed mothers are also exposed to heightened levels of marital discord and conflict [8, 10]. Research has demonstrated that in depressed couples, both partners display more disengaged behaviors, have more negative appraisals of their partners, and rate their marriages as less satisfactory as compared to nondepressed couples [18].
Peer Stress
Emerging research suggests that children of depressed mothers are also exposed to higher levels of peer stress than children of nondepressed mothers [7, 12]. Research with community samples suggests that adolescence brings increased exposure to stress within peer relationships, with the most common stressors including the loss of a close friend or romantic partner, gossip, and bullying [19]. Like family stressors, exposure to stress within peer relationships confers strong risk for psychopathology during the transition from childhood to adolescence [20], and several factors may make children of depressed mothers particularly vulnerable to peer stress. Depressed mothers may have few or conflicted interpersonal relationships, and as a consequence, modeling social interactions for their children may be scarce or maladaptive [3, 21]. Further, depressed mothers may be less adept at scaffolding skills that contribute to social competence in their children [e.g., emotion regulation; 22]. Accordingly, children of depressed mothers exhibit deficits in social competence and have poorer quality peer relationships as compared to children of nondepressed mothers [23–25].
Outstanding Questions in the Literature
How Do Family and Peer Stress Function Together in Association with Adolescent Psychological Symptoms?
Despite the salience of both family and peer stress for children of depressed mothers, few studies have examined family and peer stress together as sources of risk for the development of psychological symptoms and disorder. An exception is Feurer et al. [12], who examined family and peer stress in children of mothers with and without depression histories. Feurer et al. [12] found that children of mothers with a history of depression experienced more family stress and peer stress than children of mothers with no history of depression. After controlling for mothers’ current depression symptoms, they found that the association of maternal depression history with family stress was no longer significant; however, the association of maternal depression history with peer stress remained significant. These findings suggest that while family stress is closely linked to current maternal depression symptoms, peer stress may be more persistent and independent of current maternal depression symptoms and disorder. However, Feurer et al. [12] did not examine the associations of family and peer stress with symptoms of psychopathology in these children. Similarly, Gershon et al. [7] found that daughters of depressed mothers experienced significantly higher levels of chronic interpersonal stress than daughters of healthy mothers, including stress in relationships with their mothers and their peers. Nearly half of daughters of depressed mothers in this sample met criteria for a psychiatric disorder within 2.5 years of the study baseline, as compared to none of the daughters of healthy mothers, but the authors did not examine stress exposure as a predictor of psychopathology. Further, the authors did not account for the effect of current maternal depression symptoms in these associations.
What Role Do Current Maternal Depression Symptoms Play in Adolescent Psychological Symptoms?
Research has underscored the importance of considering mothers’ lifetime history of depression along with current depression symptoms to understand the implications of stress on children’s emotional and behavioral problems. Hammen et al. [24] found that although maternal history of depression predicted children’s lifetime diagnoses of psychopathology, current maternal depression symptoms (and not maternal depression history) predicted children’s current psychological functioning, including behavior problems, reduced social competence, and diagnoses within the previous six months. Hammen et al. [26] found that child stress surrounding maternal depression interacted with a composite measure of child stress (i.e., stressful events in 11 domains including family, peers, school, health, and finances) to predict depression in the child. Specifically, children with high maternal depression-related stress were significantly more depressed after exposure to greater general stress (i.e., elevated child stress composite) than children with low maternal depression-related stress. Hammen et al. [26] suggested that maternal depression symptoms are stressors themselves, and depression symptoms may compromise mothers’ abilities to buffer the effects of other stressful events in the life of the child. However, without measuring maternal depression-related child stress in addition to maternal depression symptoms, our ability to draw these conclusions are limited. Further, since child stress was represented as a composite score by Hammen et al. [26], specificity in the effect of subtypes of child stressors (i.e., family vs. peer) on child depression could not be determined.
The Current Study
In summary, three fundamental aspects of research have yet to be fully integrated to optimize our understanding of risk in adolescents of depressed mothers: (1) examining exposure to stress both within and outside the family in adolescents of mothers with and without depression histories, (2) extending this work to investigate the association of stress exposure with symptoms of psychopathology in adolescents, and (3) exploring current maternal depression symptoms as a possible moderator of these associations. Accordingly, these three areas constitute the focus for the current study.
We first hypothesized that mothers’ histories of depression and current levels of mothers’ depression symptoms would be associated with higher levels of both family and peer stress for adolescents. Based on the results of Feurer et al. [12], we expected the relation between maternal history of depression and family stress (but not peer stress) to be accounted for by current maternal depression symptoms. Second, consistent with prior research, we hypothesized that mothers’ history of depression and current levels of mothers’ depression symptoms would be positively associated with adolescents’ symptoms of anxiety and depression. Third, we hypothesized that both family and peer stress would be associated with adolescents’ symptoms of anxiety and depression. Fourth, building on the work of Hammen et al. [26] and others, we tested possible interactions between current maternal depression symptoms and family and peer stress as predictors of adolescents’ symptoms of anxiety and depression. Specifically, our fourth hypothesis was that adolescents’ symptoms of anxiety and depression would be higher when levels of both family and peer stress, as well as maternal depression symptoms, were high.
Method
Participants
The sample included 115 mothers (M age = 41.49, SD = 6.15) with (n = 56) and without (n = 59) histories of depression and their adolescent children. Of the 56 mothers with histories of depression, six (10.7%) were currently in a major depressive episode (MDE), three (5.4%) had an MDE before the birth of their child, and 47 (83.9%) had an MDE within their child’s lifetime. Mothers were primarily Caucasian (69.1%), married or living with a partner (63.2%), and had at least a high school diploma or equivalent (93.0%). Adolescents were primarily male (54.8%) and Caucasian (67.0%). Of the non-Caucasian adolescents, 26.1% were African American, 3.5% were more than one ethnicity, 2.6% were Asian, and < 1% identified their ethnicity as being in the “other” category. Adolescents ranged from 9 to 15 years old (M age= 12.29, SD = 1.88); 16 (13.9% of the sample) were 9 years old.11.
Measures
Demographic Information
Mothers completed a basic demographic questionnaire, with items including maternal education, employment, and marital status and adolescent age, gender, and ethnicity.
History of Maternal Depression
Mothers’ histories of depression were assessed using the major depressive disorder (MDD) module of the Structured Clinical Interview for DSM-IV Diagnoses [SCID; 27]. This semi-structured interview was administered by clinical psychology doctoral students trained in administration of the SCID and DSM-IV classification and diagnostic criteria.
Current Symptoms of Maternal Depression
Mothers completed the Beck Depression Inventory-II [BDI-II; 28] to assess for current depression symptoms. The BDI-II is a 21-item self-report measure with a 4-point scale ranging from 0 to 3. The BDI-II has demonstrated adequate internal consistency and validity in distinguishing the severity of current MDD [29]. Internal consistency reliability for the current sample was α = 0.93.
Adolescent Family Stress
Adolescents’ experience with stressors within the family was measured using the Responses to Stress Questionnaire–Family Stress version [RSQ–FS; 30]. The RSQ–FS consists of 12 items that describe aspects of an adolescent’s family life that could potentially be stressful, including engaging in arguments with parents and siblings (e.g., “Arguing with your father”), witnessing arguments between family members (e.g., “Your parents arguing with each other”), and strained relationships with parents (e.g., “Having a hard time talking with your parents,” “Your parents not understanding you”) and siblings (e.g., “Competing with your siblings,” “Not being as close to your siblings as you’d like”). Respondents rate how stressful the experience has been in the past 6 months on a 4-point scale (1 = not at all, 2 = a little, 3 = somewhat, 4 = very). Adolescents completed the self-report version of the RSQ–FS about themselves, and mothers completed the parent-report version of the RSQ–FS about their adolescent. Internal consistency reliability for the current sample was α = 0.79 for adolescent report and α = 0.82 for parent report. For purposes of data reduction, a composite of the mother and adolescent reports was created by converting mother and adolescent reports to standardized z-scores and calculating the mean of the z-scores for each variable.
Adolescent Peer Stress
Adolescents’ experience with stressors within peer relationships and interactions was measured using the Responses to Stress Questionnaire–Peer Stress version [RSQ–PS; 30]. The RSQ–PS consists of 10 items that describe aspects of an adolescent’s social life that could potentially be stressful, including friendships (e.g., “Having someone stop being your friend”), romantic relationships (e.g., “Asking someone out on a date and being turned down”), peer pressure (e.g., “Being pressured by others to do things you don’t want to do”), social exclusion (e.g., “Not being invited to do things with others”), and bullying (e.g., “Being teased/hassled by friends or other people”). Respondents rate how stressful the experience has been in the past 6 months on a 4-point scale (1 = not at all, 2 = a little, 3 = somewhat, 4 = very). Adolescents completed the self-report version of the RSQ–PS about themselves, and mothers completed the parent-report version of the RSQ–PS about their adolescent. Internal consistency reliability for the current sample was α = 0.86 for adolescent report and α = 0.86 for parent report. For purposes of data reduction, a composite of the mother and adolescent reports was created by converting mother and adolescent reports to standardized z-scores and calculating the mean of the z-scores for each variable.
Adolescent Symptoms of Anxiety and Depression
Mothers completed the Child Behavior Checklist [CBCL; 31] about their adolescent, and adolescents completed the Youth Self Report [YSR; 31] about themselves, to report on symptoms and behaviors occurring over the past 6 months. The CBCL is a 112-item checklist for parents to report on their children and adolescents 6–18 years old. The YSR is a 112-item self-report for adolescents 11–18 years old. Behaviors are rated on a 3-point scale (0 = not true, 1 = somewhat or sometimes true, and 2 = very true or often true). The reliability and validity of the CBCL and YSR are well established. The present study focused on the Anxious/Depressed scale from the CBCL and YSR. The Anxious/Depressed scale includes 13 items that assess thoughts, feelings, and behaviors related to anxiety and depression. Internal consistency reliability for the current sample was α = 0.81 for the CBCL Anxious/Depressed scale and α = 0.81 for the YSR Anxious/Depressed scale. Twenty-four adolescents were younger than 11 years old (i.e., outside the age range for the YSR), and internal consistency was adequate (α = 0.80) for those adolescents on the YSR Anxious/Depressed scale. Again, for purposes of data reduction, a composite variable was created from mother and adolescent reports on the Anxious/Depressed scale by converting mother and adolescent reports to standardized z-scores and calculating the mean of the z-scores for each variable.
Procedure
Mothers with and without a history of depression were recruited from a Southeastern metropolitan area. Recruitment strategies included mass emails to university employees and fliers placed in waiting rooms at local mental health clinics. Interested mothers were screened on the phone prior to study enrollment. Mother-adolescent dyads were excluded from participation if mothers met criteria for bipolar disorder I or II via a structured phone interview. Dyads were also excluded if mothers reported a diagnosis of schizophrenia (history or current) in themselves, or a diagnosis of schizophrenia (history or current), pervasive developmental disorder, or intellectual disability in their adolescent. In families with multiple adolescents in the age range (i.e., 9 to 15 years old) meeting inclusion criteria, the oldest eligible adolescent was invited to participate in the study. During a single laboratory visit, mothers and their adolescents completed questionnaires and clinical assessments, a subset of which are included in the present analyses. For their participation, families received $100, as well as a pamphlet with information on parent-adolescent communication, parenting, and the effects of depression on parenting. All procedures were approved by the university institutional review board, and all participants provided informed consent.
Data Analytic Strategy
Analyses were conducted using SPSS Version 26. Descriptive analyses were conducted for each of the key study variables (i.e., demographics, maternal self-reports of current depression symptoms, and composites of maternal reports and adolescent self-reports of adolescent family stress, adolescent peer stress, and adolescent anxious/depressed symptoms; Table 1). Descriptive statistics are presented for the full sample, dyads with a history of maternal depression, and dyads with no history of maternal depression. T tests or X2 tests determined whether mean differences between subgroups (i.e., maternal depression history versus no maternal depression history) were statistically significant. For ease of interpretation, descriptive statistics of the adolescent family stress, adolescent peer stress, and child anxious/depressed variables are presented as raw score composites. However, for all subsequent analyses (as mentioned previously), composites were created by converting mother and adolescent reports to standardized z-scores and calculating the mean of the z-scores for each variable. Bivariate correlations examined relations among the variables in the full sample and provided initial tests of the hypotheses (Table 2). A series of multiple linear regression analyses were subsequently conducted to examine main effects of maternal depression history and current maternal depression symptoms on adolescent family stress and adolescent peer stress in the full sample (Table 3). In addition, maternal depression history, current maternal depression symptoms, adolescent family stress, and adolescent peer stress were examined as predictors of adolescent anxious/depressed symptoms in the full sample (Table 4). Significant interactions were further examined using the plotting feature of the PROCESS macro for SPSS [32].
Table 1.
Sample characteristics, reported by group
| Measure | Full sample (N = 115) |
Depression history (n = 56) |
No depression history (n = 59) |
Statistic | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||
| Mother educationa | 93.04% | 91.07% | 94.92% | X2(1) = 0.66 | |||
| Mother employmentb | 85.96% | 80.36% | 91.38% | X2(1) = 2.87 | |||
| Mother marital statusc | 63.16% | 54.55% | 71.19% | X2(1) = 3.39 | |||
| Adolescent age | 12.28 | 1.89 | 12.29 | 1.93 | 12.27 | 1.87 | t (113) = − 0.04 |
| Adolescent genderd | 54.78% | 52.54% | 57.14% | X2(1) = 0.25 | |||
| Adolescent ethnicitye | 66.96% | 71.43% | 62.71% | X2(1) = 0.99 | |||
| Mother BDI-II | 10.66 | 10.43 | 14.93 | 11.28 | 6.60 | 7.67 | t (96.24) = − 4.61*** |
| Adolescent family stress | 1.89 | 0.47 | 2.01 | 0.51 | 1.78 | 0.40 | t (103.43) = − 2.66** |
| Adolescent peer stress | 1.62 | 0.46 | 1.71 | 0.48 | 1.53 | 0.42 | t (113) = − 2.09* |
| Adolescent anx/dep | 55.26 | 6.06 | 56.85 | 7.53 | 53.75 | 3.71 | t (79.87) = − 2.69** |
For ease of interpretation, raw scores on the adolescent family stress, peer stress, and anxious/depressed composites are presented prior to the z-score transformations used for all subsequent analyses
BDI-II Beck Depression Inventory-II, anx/dep anxious/depressed scale
p < 0.05.
p < 0.01.
p < 0.001
% Greater than high school diploma or equivalent
% Employed
% Married or partnered
% Male
% Caucasian
Table 2.
Correlations among key study variables
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother educationa | – | |||||||||
| 2. Mother employmentb | 0.32*** | – | ||||||||
| 3. Mother marital statusc | 0.15 | 0.03 | – | |||||||
| 4. Adolescent age | − 0.05 | 0.10 | − 0.08 | – | ||||||
| 5. Adolescent genderd | 0.04 | 0.06 | 0.08 | − 0.11 | – | |||||
| 6. Adolescent ethnicitye | − 0.11 | − 0.06 | 0.07 | 0.05 | 0.12 | – | ||||
| 7. Mother BDI-II | − 0.07 | − 0.29** | − 0.28** | − 0.10 | − 0.04 | − 0.06 | – | |||
| 8. Mother depression history | − 0.08 | − 0.16 | − 0.17 | 0.004 | − 0.05 | 0.002 | 0.40*** | – | ||
| 9. Adolescent family stress | − 0.06 | − 0.18* | − 0.02 | 0.10 | 0.11 | 0.11 | 0.40*** | 0.25** | – | |
| 10. Adolescent peer stress | 0.13 | − 0.03 | − 0.01 | 0.04 | − 0.05 | 0.03 | 0.28** | 0.19* | 0.43*** | – |
| 11. Adolescent anx/dep | 0.02 | − 0.27** | − 0.06 | 0.004 | 0.02 | 0.08 | 0.49*** | 0.25** | 0.57*** | 0.58*** |
BDI-II Beck Depression Inventory-II, anx/dep anxious/depressed scale
p < 0.05.
p < 0.01.
p ≤ 0.001
1 = greater than high school diploma or equivalent
1 = employed
1 = married or partnered
1 = male
1 = Caucasian
Table 3.
Maternal depression history and symptoms predicting adolescent family stress
| Predictor | b | 95% CI | β | t | sr2 | df | F | Adjusted R2 |
|---|---|---|---|---|---|---|---|---|
| Model | 104 | 3.68*** | 0.16 | |||||
| Mother education | − 0.11 | [− 0.66, 0.71] | − 0.03 | − 0.36 | < 0.001 | |||
| Mother employment | − 0.09 | [− 0.78, 0.19] | − 0.04 | − 0.38 | < 0.001 | |||
| Mother marital status | 0.17 | [− 0.27, 0.40] | 0.09 | 1.00 | 0.008 | |||
| Adolescent age | 0.09 | [− 0.01, 0.16] | 0.20 | 2.27* | 0.04 | |||
| Adolescent gender | 0.26 | [− 0.10, 0.53] | 0.15 | 1.70 | 0.02 | |||
| Adolescent ethnicity | 0.11 | [− 0.05, 0.40] | 0.09 | 0.98 | 0.007 | |||
| Mother depression history | 0.16 | [− 0.23, 0.44] | 0.10 | 1.00 | 0.008 | |||
| Mother BDI-II | 0.03 | [0.10, 0.05] | 0.36 | 3.61*** | 0.10 |
N = 113, BDI-II Beck Depression Inventory-II, CI confidence interval
p < 0.05.
p ≤ 0.001
Table 4.
Maternal depression and adolescent stress predicting adolescent anxious/depressed symptoms
| Block and predictor | b | 95% CI | β | t | sr2 | df | F | Adjusted R2 | ΔR2 |
|---|---|---|---|---|---|---|---|---|---|
| Block 1 | 105 | 1.81 | 0.05 | – | |||||
| Mother depression history | 0.32 | [0.02, 0.63] | 0.20 | 2.08* | 0.04 | ||||
| Block 2 | 102 | 10.36*** | 0.46 | 0.46*** | |||||
| Mother depression history | − 0.01 | [− 0.26, 0.24] | − 0.01 | − 0.11 | 0.00 | ||||
| Adolescent family stress | 0.25 | [0.10, 0.40] | 0.26 | 3.10** | 0.05 | ||||
| Adolescent peer stress | 0.40 | [0.24, 0.56] | 0.39 | 4.97*** | 0.12 | ||||
| Mother BDI-II | 0.02 | [0.01, 0.03] | 0.25 | 2.92** | 0.04 | ||||
| Block 3 | 99 | 11.80*** | 0.56 | 0.12*** | |||||
| Mother depression history | 0.07 | [− 0.16, 0.29] | 0.04 | 0.57 | 0.00 | ||||
| Adolescent family stress | 0.24 | [0.10, 0.38] | 0.26 | 3.31*** | 0.04 | ||||
| Adolescent peer stress | 0.31 | [0.16, 0.46] | 0.30 | 4.10*** | 0.06 | ||||
| Mother BDI-II | 0.02 | [0.004, 0.03] | 0.20 | 2.56** | 0.03 | ||||
| BDI-II × family stress | 0.01 | [− 0.003, 0.02] | 0.11 | 1.43 | 0.01 | ||||
| BDI-II × peer stress | 0.02 | [0.003, 0.03] | 0.20 | 2.44* | 0.02 | ||||
| Family stress × peer stress | 0.16 | [− 0.03, 0.35] | 0.14 | 1.64 | 0.01 |
All three blocks controlled for maternal education, employment, and martial status, as well as adolescent age, gender, and ethnicity. Maternal unemployment significantly predicted more adolescent anxious/depressed symptoms in the Block 1 (β = − 0.21, p = 0.03), but this effect disappeared after accounting for adolescent stress and mother depression symptoms in Block 2. The effects of the remaining covariates were nonsignificant and omitted from the table for brevity
N = 113, BDI-II Beck Depression Inventory-II, CI confidence interval
p < 0.05.
p < 0.01.
p ≤ 0.001
Missing Data
Of the 115 dyads in the full sample, one dyad had missing data on the mother employment variable and one dyad had missing data on the mother marital status variable. These two participants were retained in all analyses possible, but they were deleted listwise from analyses including the mother employment and mother marital status variables.
Power Analyses
We conducted power analyses using G*Power 3.1 to determine the effect size we would be able to detect in mean difference, correlation, and regression analyses [33]. With alpha set to 0.05 and power set to 0.80, we were able to medium mean differences between maternal depression history (n = 56) and no maternal depression history (n = 59) groups (d = 0.53 or larger) and small-to-medium correlations (r = 0.25 or larger) for the full sample (N = 115). In regression equations, we are able to detect small-to-medium effects. Specifically, we were able to detect small-to-medium effects (f2=0.12 or larger) when examining maternal depression history and symptoms as predictors of family stress and peer stress. We were able to detect small-to-medium effects (, , or larger) when examining maternal depression and adolescent stress as predictors of adolescent anxious/depressed symptoms.
Results
Preliminary Analyses
Tests of mean difference (t tests and X2 tests, as appropriate) were conducted to compare demographic variables (maternal education, employment, and marital status and adolescent age, gender, and ethnicity) in adolescents with and without mothers with histories of depression. Analyses revealed no significant differences on any of the demographic variables (Table 1; all p > 0.05). Further, the majority of demographic variables were not associated with key study variables in correlational analyses (Table 2). Maternal employment was associated with fewer current maternal depression symptoms on the BDI-II (r = − 0.29, p = 0.002), less exposure to family stress (r = − 0.18, p = 0.05), and fewer adolescent symptoms of anxiety and depression (r = − 0.27, p = 0.004). In addition, mothers who were married or partnered had fewer current maternal depression symptoms on the BDI-II (r = − 0.28, p = 0.003). However, taking a conservative approach, all demographic variables were included in regression analyses because of their potential confounding effects on adolescent exposure to stress and psychological symptoms [34–36]. Findings pertaining to covariates will only be reported in regression analyses when significant.
Descriptive Statistics
Table 1 displays means and standard deviations for current maternal depression symptoms, adolescent family stress, adolescent peer stress, and the child anxious/depressed scale for the full sample (N = 115), adolescents of mothers with a history of depression (n = 56), and adolescents of mothers without a history of depression (n = 59). The mean score for the full sample on current maternal depression symptoms on the BDI-II was in the minimal range [M = 10.66, SD = 10.43; 37]. Consistent with the goal of recruitment, which was to include mothers with and without histories of depression and current depression symptoms, there was considerable variability in scores on the BDI-II. Approximately 70% of mothers were in the minimal range (0–13), 14.8% of mothers were in the mild range (14–19), 9.6% of mothers were in the moderate range (20–28), and 6.1% of mothers were in the severe range (29–63). Descriptive data from the full sample reflects that family and peer stressors were “a little” stressful for adolescents in the past 6 months (family stress composite M = 1.89, SD = 0.47; peer stress composite M = 1.62, SD = 0.46). Anxious/depressed symptoms were approximately one-half standard deviation above the normative mean (anxious/depressed composite M = 55.26, SD = 6.06).
Comparisons Based on Maternal History of Depression
Table 1 also displays tests of mean differences by maternal depression history for the key study variables. Mothers with a history of depression reported significantly more current depression symptoms on the BDI-II (M = 14.93, SD = 11.28) than mothers with no history of depression (M = 6.60, SD = 7.67), t (96.24) = − 4.61, p < 0.001. There were also significant differences in adolescent stress experienced as a function of maternal history of depression for both the family and peer domains. In support of the first hypothesis, adolescents of mothers with a history of depression scored higher than adolescents of mothers with no history of depression on the family stress composite, t (103.43) = − 2.66, p = 0.009. Similarly, adolescents of mothers with a history of depression scored higher than adolescents of mothers with no history of depression on the peer stress composite, t (113) = − 2.09, p = 0.04. In support of the second hypothesis, adolescents of mothers with a history of depression scored higher on the anxious/depressed composite than adolescents of mothers with no history of depression, t (79.87) = − 2.69, p = 0.009.
Bivariate Correlation Analyses
Bivariate correlations were conducted with the full sample to examine associations among maternal depression symptoms, the adolescent family stress composite, the adolescent peer stress composite, and the adolescent anxious/depressed symptom composite (Table 2). Correlational analyses provide initial tests of the first, second, and third hypotheses. Consistent with the first hypothesis, current maternal depression symptoms were positively associated with both adolescent family stress (r = 0.40, p < 0.001) and adolescent peer stress (r = 0.28, p = 0.003). In support of the second hypothesis, current maternal depression symptoms were significantly correlated with adolescents’ anxious/depressed symptoms (r = 0.49, p < 0.001). In support of the third hypothesis, adolescent family stress (r = 0.57, p < 0.001) and adolescent peer stress (r = 0.58, p < 0.001) were positively associated with adolescents’ anxious/depressed symptoms.
Linear Regression Analyses
Predicting Family and Peer Stress in Adolescents
To further test the first hypothesis, two separate linear regression analyses were conducted to examine the association of maternal depression history with adolescent stress (family and peer), controlling for current maternal depression symptoms and covariates (mother education, employment, and marital status, and adolescent age, gender, and ethnicity), with the full sample. In the first linear regression, we examined the association of maternal depression history with adolescent family stress, controlling for current maternal depression symptoms (Table 3). Maternal depression history (β = 0.10, p = 0.32) was not a significant predictor of adolescent family stress; however, current maternal depression symptoms were significantly associated with adolescent family stress (β = 0.36, p = 0.001). Adolescent age was also a significant predictor of family stress (β = 0.20, p = 0.03). Overall, the family stress model was significant, F(8, 104) = 3.68, p < 0.001, adjusted R2 = 0.16. In the second linear regression, we examined the association of maternal depression history with adolescent peer stress, controlling for current maternal depression symptoms. The peer stress model was nonsignificant, F(8, 104) = 1.44, p = 0.19, adjusted R2 = 0.03.
Predicting Symptoms of Anxiety and Depression in Adolescents
To test the second and third hypotheses, multiple linear regression analyses were conducted to examine the associations of maternal depression history, current maternal depression symptoms, adolescent family stress, and adolescent peer stress with adolescent anxious/depressed symptoms (Table 4). In the first block of the regression, we tested the effect of maternal depression history on adolescent anxious/depressed symptoms. Overall, the first block of the model predicting anxious/depressed symptoms was nonsignificant, F(7,105) = 1.81, p = 0.09, adjusted R2 = 0.05. In the second block of the regression, we tested the main effects of adolescent family stress, adolescent peer stress, and current maternal depression symptoms on adolescent anxious/depressed symptoms, controlling for maternal depression history. Consistent with the second and third hypotheses, adolescent family stress (β = 0.26, p = 0.003), adolescent peer stress (β = 0.39, p < 0.001), and current maternal depression symptoms (β = 0.25, p = 0.004) all significantly predicted adolescent anxious/depressed symptoms.
To test the fourth hypothesis, in the third block of the regression equation, we added three two-way interactions: Current Maternal Depression Symptoms × Adolescent Family Stress, Current Maternal Depression Symptoms × Adolescent Peer Stress, and Adolescent Family Stress × Adolescent Peer Stress. The main effects of adolescent family stress (β = 0.26, p = 0.001), adolescent peer stress (β = 0.30, p < 0.001), and current maternal depression symptoms (β = 0.20, p = 0.01) remained significant for adolescent anxious/depressed symptoms. The interaction of Current Maternal Depression Symptoms × Adolescent Peer Stress significantly predicted adolescent anxious/depressed symptoms (β = 0.20, p = 0.02). The interactions of Current Maternal Depression Symptoms × Adolescent Family Stress (β = 0.11, p = 0.16) and Adolescent Family Stress × Adolescent Peer Stress (β = 0.14, p = 0.10) were nonsignificant predictors of adolescent anxious/depressed symptoms. Overall, the third block of the model predicting anxious/depressed symptoms was significant, F(13, 99) = 11.80, p < 0.001, adjusted R2 = 0.56.
Results of the significant interaction of Current Maternal Depression Symptoms × Adolescent Peer Stress were plotted in PROCESS to better understand the nature of the interaction (see Fig. 1). The interaction tested the conditional effects of peer stress at three levels of maternal depression symptoms: one standard deviation below the mean (low), at the mean (average), and one standard deviation above the mean (high). Adolescent peer stress was only related to adolescent anxious/depressed symptoms when maternal depression symptoms were high [b = 0.57, t(113) = 6.80, p < 0.001] or average [b = 0.27, t(113) = 3.35, p = 0.001]. When maternal depression symptoms were low, adolescent peer stress was unrelated to adolescent anxious/depressed symptoms [b = 0.09, t(113) = 0.87 p = 0.39].
Fig. 1.
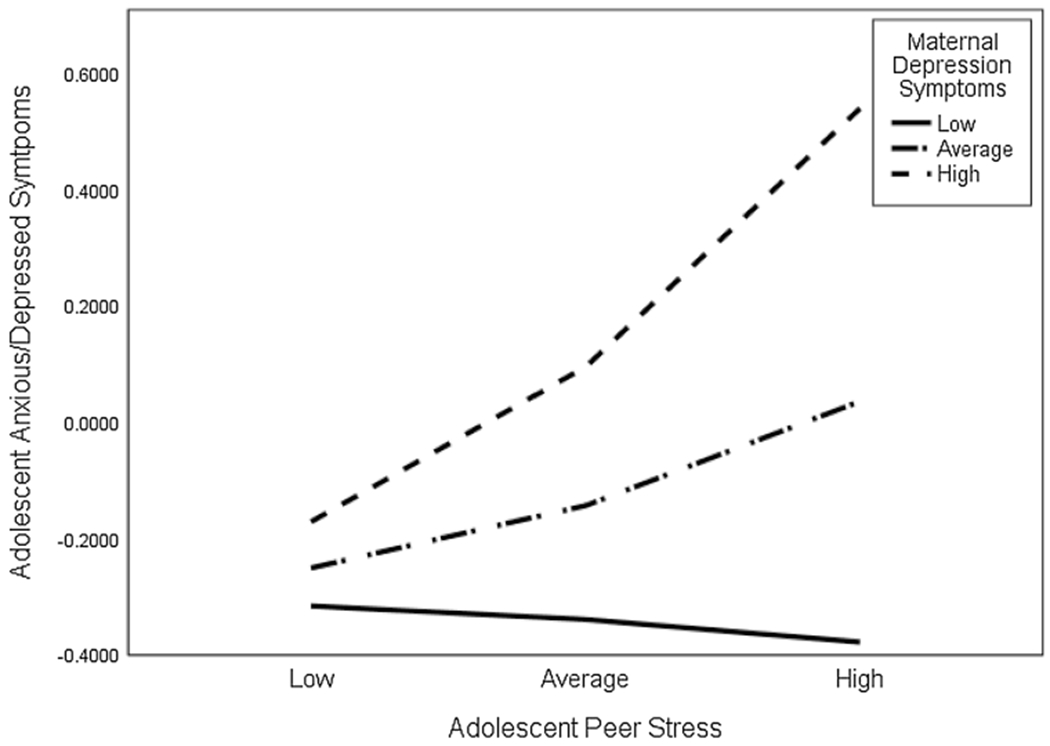
Interaction testing the conditional effects of adolescent peer stress on adolescent anxious/depressed symptoms at three levels of maternal depression symptoms: one standard deviation below the mean (low), at the mean (average), and one standard deviation above the mean (high)
Finally, we added the three-way interaction of Current Maternal Depression Symptoms × Adolescent Family Stress × Adolescent Peer Stress in a fourth block of the regression equation. There were no significant differences from the third block to the fourth block, and the three-way interaction of Current Maternal Depression Symptoms × Adolescent Family Stress × Adolescent Peer Stress did not significantly predict adolescent anxious/depressed symptoms (β = − 0.12, p = 0.31). The model fit improved significantly in the second (, p < 0.001) and third (, p < 0.001) blocks of the regression analyses but did not improve in the final block (, p = 0.31). Therefore, the results of block four are not reported in the final model or in Table 4.
Discussion
Exposure to stress is an important risk factor for the development of anxiety and depression symptoms in adolescence, and adolescents of depressed mothers may be particularly vulnerable to the adverse effects of stress. However, much remains to be explored to understand how family and peer stress and maternal depression history and symptoms function together to confer risk in adolescents of depressed mothers. To address existing gaps in the research, the current study aimed to (1) examine exposure to stress both within and outside the family in adolescents with and without maternal depression histories, (2) extend this work to investigate the association of stress exposure with symptoms of anxiety and depression in adolescents, and (3) explore current maternal depression symptoms as a possible moderator of these associations.
Consistent with the first hypothesis, current maternal depression symptoms were associated with more family and peer stress for adolescents in bivariate analyses. Further, adolescents of mothers with a history of depression scored significantly higher than adolescents of mothers without depression histories on measures of family and peer stress. This set of findings replicates previous research showing that children of mothers with a history of depression and/or higher levels of current depression symptoms experience higher rates of both family and peer stress than children of mothers without depression [7, 12]. We also were interested in replicating the effects of Hammen et al. [24] and others, who found current maternal depression symptoms to be a better predictor of current child and adolescent functioning than maternal depression history. Correspondingly, when depression symptoms and history were simultaneously added to linear regression models predicting family and peer stress, current maternal depression symptoms were associated with adolescent stress, but maternal depression history was not. It should be noted that while the family stress model was significant, the peer stress model was nonsignificant. These findings differ slightly from those reported by Feurer et al. [12], who found that the association of maternal depression history with family stress was no longer significant after controlling for mothers’ current depression symptoms, but the association of maternal depression history with peer stress was maintained. As such, the test of the first hypothesis provided a replication of the findings of Hammen et al. [24] and a partial replication of the findings of Feurer et al. [12].
In support of the second hypothesis and consistent with prior research on children and adolescents of depressed mothers [3], a history of maternal depression and current maternal depression symptoms were positively associated with adolescents’ symptoms of anxiety and depression in independent samples t tests and bivariate correlations, respectively. When entered into a multivariate model, however, the association of maternal depression history with adolescent anxious/depressed symptoms was fully accounted for by adolescents’ experience of stress in the family, stress with peers, and current maternal depression symptoms. As such, the second hypothesis was partially supported. Thus, temporally proximal factors (i.e., current maternal depression symptoms) appear to take precedence over more distal factors (i.e., history of maternal depression) in determining risk for psychological symptoms in children and adolescents [24]. These findings suggest that reducing current depression symptoms in mothers could reduce symptoms of anxiety and depression in at-risk youth.
In support of the third hypothesis, both family and peer stress were significantly and independently related to higher levels of adolescents’ symptoms of anxiety and depression in bivariate analyses. These findings are consistent with research that has separately examined the relations between family and peer stress exposure and psychopathology [20, 38]. In addition, significant main effects emerged for both family and peer stress on adolescents’ anxious/depressed symptoms within a multivariate model. The current research provides a first step in examining how family and peer stress together are associated with adolescents’ psychological functioning, and the findings suggest that family stress, peer stress, and current maternal depression symptoms all have independent associations with adolescents’ symptoms of anxiety and depression. Finally, with regard to the fourth hypothesis, there was support for an interaction between current maternal depression symptoms and peer stress, but not family stress, as a predictor of adolescents’ anxious/depressed symptoms. The strongest association of peer stress and maternal depression symptoms with adolescent anxious/depressed symptoms was observed for high maternal depression symptoms and high peer stress (see Fig. 1).
The current study serves as a partial replication of the work of Feurer et al. [12], in that current maternal depression symptoms accounted for the association of maternal depression history with both adolescent family and peer stress. The current study also extends the work of Feurer et al. [12], Hammen et al. [26], and others to understand associations between stress exposure, current maternal depression symptoms, and symptoms of anxiety and depression in adolescents. Family stress was directly associated with higher levels of adolescents’ symptoms of anxiety and depression irrespective of mothers’ current depression symptoms. In contrast, the association between peer stress and adolescent anxious/depressed symptoms was moderated by current maternal depression symptoms; adolescent peer stress was only related to more adolescent anxious/depressed symptoms when mothers were currently experiencing average or high levels of depression symptoms. In the absence of maternal depression symptoms, peer stress was not associated with adolescents’ symptoms.
The current findings can be considered in the context of research examining impairment in parenting skills when maternal depression symptoms are current. Mothers with higher levels of depression symptoms may not be able to provide appropriate guidance and support to their children navigating changing peer relationships [39, 40], or they may encourage less adaptive ways of reacting to stressful peer situations [41]. Engaged mothers can be sources of support for adolescents experiencing stress in peer relationships and may help buffer adolescents’ stress exposure; however, depressed mothers are likely to be withdrawn and disengaged [17], and so may be less available to help adolescents manage stressful peer interactions [39, 40]. Additionally, depressed mothers may model disengagement coping strategies (e.g., avoidance, denial), which, in turn, adolescents may adopt in an attempt to manage peer stress [42]. These parenting behaviors could potentially undermine adolescents’ ability to learn from stressful situations, as well as more directly influence the development of maladaptive coping skills [41]. Thus, the association between peer stress and adolescents’ anxious/depressed symptoms may be heightened as a function of mothers’ current levels of depression symptoms. Research suggests other mechanisms by which the experience of maternal depression could contribute to peer problems in adolescents; for example, children and adolescents of depressed mothers show a heightened response to angry faces suggesting that they may be hyper-aware of or reactive to interpersonal stress [43]. A predisposition for increased reactivity to interpersonal stress may be magnified by exposure to mothers’ current depression symptoms.
The current study has several strengths and contributes to the growing body of literature on adolescents’ stress in family and peer domains, maternal depression, and adolescent mental health. First, the current study included a sample of mothers with and without a history of depression and measured mothers’ current depression symptoms to provide a broad test of the role of maternal depression in adolescents’ risk for symptoms of anxiety and depression. Second, we used a multi-method design, creating composites of adolescents’ self-reports and mothers’ reports of adolescents’ stressors and anxious/depressed symptoms rather than relying on a single reporter. Third, we examined stress both in the family and in peer relationships to provide a more nuanced understanding of the types of stress that may be particularly salient in the context of maternal depression.
The present study has several limitations that can be addressed in future research. First, the study was cross-sectional and therefore the direction of the association among the variables could not be determined. A substantial literature has examined the dynamic relation between stress and psychopathology across development, and stress generation models have found evidence that internalizing symptoms and associated impairment can precipitate stress in an adolescent’s life [44]. Future research testing these associations in prospective longitudinal designs is needed. Second, family and peer stress were measured with a checklist rather than an interview [6, 45]. Although a checklist may not provide granularity about specific stressors, it quickly indicates the number of stressful experiences and the impact of those stressors on the individual. However, future research should include interviews or more detailed inventories to measure the duration, frequency, and severity of adolescent stressors [45]. Third, power analysis indicated that we were able to detect an effect of f2 = 0.12 or larger in the regression analyses predicting family and peer stress. With an effect size of f2 = 0.11, we were underpowered to detect an omnibus effect of maternal depression history and symptoms on peer stress. As such, future research should test these effects in larger samples to better understand the effects of maternal depression on peer stress. This is especially relevant, given our finding that peer stress and maternal depression symptoms interact in their association with adolescent symptoms of anxiety and depression. Fourth, there was variability in the depression histories of the mothers included in the study, such that the majority of the mothers had an MDE within the lifetime of their adolescent, and only a small percentage of mothers were currently depressed or had an MDE before their adolescent was born. The effects of maternal depression diagnostic status on adolescent stress and psychological symptoms should be examined in studies with larger samples of currently depressed and nondepressed mothers. Fifth, the current sample consists primarily of partnered and employed Caucasian mothers, and the study only included youths between 9 and 15 years old. As such, results may not generalize beyond this population. Finally, psychiatric diagnoses co-morbid to maternal MDD were not assessed in the current study. Parental substance use and anxiety, for example, have been shown to contribute to the variance in adolescent anxiety and depression symptoms and should be accounted for in future investigations [46, 47].
Summary
In summary, the findings from the current study expand on previous research that has shown that children and adolescents of depressed mothers experience heightened levels of stress within the family and in peer relationships. These two sources of stress independently constitute significant risk for symptoms of anxiety and depression. Adolescents are especially vulnerable to peer stress when their family environment is compromised by current depression symptoms in their mothers. It is noteworthy that teaching children and adolescents skills to cope with family stress has been shown to decrease internalizing problems in children with depressed mothers [48]; however, the role of teaching skills to cope with peer-related stressors and the development of internalizing problems remains to be explored. Adolescents may benefit from targeted intervention to learn skills to cope with stress both within and outside of the family. Future research should explore adolescent’s strategies for coping with family and peer stress in the presence of maternal depression to elucidate targets for intervention.
Acknowledgments
Funding This research was supported by a gift from Patricia and Rodes Hart, a gift from an anonymous donor, and Grant T32-MH18921 from the National Institute of Mental Health.
Footnotes
Although the ages of the youth in our sample encompass the transition to adolescence (i.e., 9 to 15), we will refer to our sample as “adolescents” throughout the paper.
Conflict of interest The authors declare that they have no conflict of interest.
Compliance with Ethical Standards
Ethical Approval All procedures were in accordance with ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent from all adult participants included in the study, and child participants provided assent.
References
- 1.Grant KE, Compas BE, Stuhlmacher AF, Thurm AE, McMahon SD, Halpert JA (2003) Stress and child and adolescent psychopathology: moving from markers to mechanisms of risk. Psychol Bull 129(3):447–466. 10.1037/0033-2909.129.3.447 [DOI] [PubMed] [Google Scholar]
- 2.Hammen C (2005) Stress and depression. Annu Rev Clin Psychol 1:293–319. 10.1146/annurev.clinpsy.1.102803.143938 [DOI] [PubMed] [Google Scholar]
- 3.Goodman SH, Rouse MH, Connell AM, Robbins-Broth M, Hall CM, Heyward D (2011) Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev 14(1):1–27. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- 4.Hammen C, Brennan P (2003) Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Arch Gen Psychiatry 60(3):253–260. 10.1001/archpsyc.60.3.253 [DOI] [PubMed] [Google Scholar]
- 5.Weissman MM, Berry OO, Warner V, Gameroff MJ, Skipper J, Talati A et al. (2016) A 30-year study of 3 generations at high risk and low risk for depression. JAMA Psychiatry 73(9):970–977. 10.1001/jamapsychiatry.2016.1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adrian C, Hammen C (1993) Stress exposure and stress generation in children of depressed mothers. J Consult Clin Psychol 61(2):354–359. 10.1037/0022-006X.61.2.354 [DOI] [PubMed] [Google Scholar]
- 7.Gershon A, Hayward C, Schraedley-Desmond P, Rudolph KD, Booster GD, Gotlib IH (2011) Life stress and first onset of psychiatric disorders in daughters of depressed mothers. J Psychiatr Res 45(7):855–862. 10.1016/j.jpsychires.2011.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fear JM, Champion JE, Reeslund KL, Forehand R, Colletti C, Roberts L, Compas BE (2009) Parental depression and interparental conflict: adolescent self-blame and coping responses. J Fam Psychol 23(5):762–766. 10.1037/a0016381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammen C, Brennan PA, Shih JH (2004) Family discord and stress predictors of depression and other disorders in adolescent children of depressed and nondepressed women. J Am Acad Child Adolesc Psychiatry 43(8):994–1002. 10.1097/01.chi.0000127588.57468.f6 [DOI] [PubMed] [Google Scholar]
- 10.Jaser SS, Langrock AM, Keller G, Merchant MJ, Benson M, Reeslund K (2005) Coping with the stress of parental depression II: adolescent and parent reports of coping and adjustment. J Clin Child Adolesc Psychol 34(1):193–205. 10.1207/s15374424jccp3401_18 [DOI] [PubMed] [Google Scholar]
- 11.Langrock AM, Compas BE, Keller G, Merchant MJ, Copeland ME (2002) Coping with the stress of parental depression: parents’ reports of children’s coping and emotional/behavioral problems. J Clin Child Adolesc Psychol 31(3):312–324. 10.1207/153744202760082577 [DOI] [PubMed] [Google Scholar]
- 12.Feurer C, Hammen CL, Gibb B (2016) Chronic and episodic stress in children of depressed mothers. J Clin Child Adolesc Psychol 45(3):270–278. 10.1080/15374416.2014.963859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown BB, Larson J (2009) Peer relationships in adolescence In: Lerner RM, Steinberg L (eds) Handbook of adolescent psychology, 3rd edn. Wiley, Hoboken, pp 74–103. 10.1002/9780470479193.adlpsy002004 [DOI] [Google Scholar]
- 14.Collins WA, Laursen B (2004) Parent–adolescent relationships and influences In: Lerner RM, Steinberg L (eds) Handbook of adolescent psychology, 2nd edn. Wiley, Hoboken, pp 331–361 [Google Scholar]
- 15.Furman W, Buhrmester D (1985) Children’s perceptions of the personal relationships in their social networks. Dev Psychol 21(6):1016–1024. 10.1037/0012-1649.21.6.1016 [DOI] [Google Scholar]
- 16.Hammen C (2002) The context of stress in families of children with depressed parents In: Goodman S, Gotlib I (eds) Children of depressed parents: mechanisms of risk and implications for treatment. American Psychological Association, Washington, DC, pp 175–199 [Google Scholar]
- 17.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G (2000) Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev 20(5):561–592. 10.1016/S0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- 18.Jacob T, Johnson SL (1997) Parent–child interaction among depressed fathers and mothers: impact on child functioning. J Fam Psychol 11(4):391–409. 10.1037/0893-3200.11.4.391 [DOI] [Google Scholar]
- 19.Bakker MP, Ormel J, Verhulst FC, Oldehinkel AJ (2010) Peer stressors and gender differences in adolescents’ mental health: the TRAILS study. J Adolesc Health 46(5):444–450. 10.1016/j.jadohealth.2009.10.002 [DOI] [PubMed] [Google Scholar]
- 20.Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, Gulley LD et al. (2015) Depression from childhood into late adolescence: influence of gender, development, genetic susceptibility, and peer stress. J Abnorm Psychol 124(4):803–816. 10.1037/abn0000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodman SH, Gotlib IH (1999) Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev 106(3):458–490. 10.1037/0033-295X.106.3.458 [DOI] [PubMed] [Google Scholar]
- 22.Hoffman C, Crnic KA, Baker JK (2006) Maternal depression and parenting: implications for children’s emergent emotion regulation and behavioral functioning. Parent Sci Pract 6(4):271–295. 10.1207/s15327922par0604_1 [DOI] [Google Scholar]
- 23.Goodman SH, Brogan D, Lynch ME, Fielding B (1993) Social and emotional competence in children of depressed mothers. Child Dev 64(2):516–531. 10.1111/j.1467-8624.1993.tb02925.x [DOI] [PubMed] [Google Scholar]
- 24.Hammen C, Adrian C, Gordon D, Burge D, Jaenicke C, Hiroto D (1987) Children of depressed mothers: maternal strain and symptom predictors of dysfunction. J Abnorm Psychol 96(3):190–198. 10.1037/0021-843X.96.3.190 [DOI] [PubMed] [Google Scholar]
- 25.Lewinsohn PM, Olino TM, Klein DN (2005) Psychosocial impairment in offspring of depressed parents. Psychol Med 35(10):1493–1503. 10.1017/S0033291705005350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hammen C, Burge D, Adrian C (1991) Timing of mother and child depression in a longitudinal study of children at risk. J Consult Clin Psychol 59(2):341–345. 10.1037//0022-006X.59.2.341 [DOI] [PubMed] [Google Scholar]
- 27.First MB, Spitzer RL, Gibbon M, Williams JBW (2001) Structured clinical interview for DSM–IV–TR axis I disorders, research version, patient ed. (SCID-I/P). Biometrics Research, New York State Psychiatric Institute, New York [Google Scholar]
- 28.Beck AT, Steer RA, Brown GK (1996) Beck Depression Inventory manual, 2nd edn. The Psychological Corporation, San Antonio [Google Scholar]
- 29.Steer RA, Brown GK, Beck AT, Sanderson W (2001) Mean Beck Depression inventory-II scores by severity of major depressive episode. Psychol Rep 88(3):1075–1076. 10.2466/PR0.88.4.1075-1076 [DOI] [PubMed] [Google Scholar]
- 30.Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H (2000) Responses to stress in adolescence: measurement of coping and involuntary stress responses. J Consult Clin Psychol 68(6):976–992. 10.1037/0022-006X.68.6.976 [DOI] [PubMed] [Google Scholar]
- 31.Achenbach TM, Rescorla LA (2001) Manual for the ASEBA school-age forms & profiles. Research Center for Children, Youth, & Families, University of Vermont, Burlington [Google Scholar]
- 32.Hayes AF (2017) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach, 2nd edn. Guilford Press, New York [Google Scholar]
- 33.Erdfelder E, Faul F, Buchner A (1996) GPOWER: a general power analysis program. Behav Res Methods Instrum Comput 28(1):1–11. 10.3758/BF03203630 [DOI] [Google Scholar]
- 34.Kessler RC, Avenevoli S, Merikangas KR (2001) Mood disorders in children and adolescents: an epidemiologic perspective. Bio Psychiatry 49(12):1002–1014. 10.1016/S0006-3223(01)01129-5 [DOI] [PubMed] [Google Scholar]
- 35.Leech SL, Larkby CA, Day R, Day NL (2006) Predictors and correlates of high levels of depression and anxiety symptoms among children at age 10. J Am Acad Child Adolesc Psychiatry 45(2):223–230. 10.1097/01.chi.0000184930.18552.4d [DOI] [PubMed] [Google Scholar]
- 36.Salk RH, Hyde JS, Abramson LY (2017) Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull 143(8):783–822. 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beck AT, Steer RA, Ball R, Ranieri WF (1996) Comparison of beck depression inventories-IA and -II in psychiatric outpatients. J Pers Assess 67(3):588–597. 10.1207/s15327752jpa6703_13 [DOI] [PubMed] [Google Scholar]
- 38.Jenness JLJ, Hankin BL, Abela JRZ, Young JF, Smolen A (2011) Chronic family stress interacts with 5-HTTLPR to predict prospective depressive symptoms among youth. Depress Anxiety 28(12):1074–1080. 10.1002/da.20904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Morin HK, Bradshaw CP, Berg JK (2015) Examining the link between peer victimization and adjustment problems in adolescents: the role of connectedness and parent engagement. Psychol Violence 5(4):422–432. 10.1037/a0039798 [DOI] [Google Scholar]
- 40.Rueger SY, Malecki CK, Pyun Y, Aycock C, Coyle S (2016) A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychol Bull 142(10):1017–1067. 10.1037/bul0000058 [DOI] [PubMed] [Google Scholar]
- 41.Abaied JL, Rudolph KD (2011) Maternal influences on youth responses to peer stress. Dev Psychol 47(6):1776–1785. 10.1037/a0025439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Watson KH, Dunbar JP, Reising MM, Hudson K, Forehand R, Compas BE (2014) Observed parental responsiveness/warmth and children’s coping: cross-sectional and prospective relations in a family depression preventive intervention. J Fam Psychol 28(3):278–286. 10.1037/a0036672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Feurer C, Burkhouse KL, Siegle G, Gibb BE (2017) Increased pupil dilation to angry faces predicts interpersonal stress generation in offspring of depressed mothers. J Child Psychol Psychiatry 58(8):950–957. 10.1111/jcpp.1273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hammen C (1991) The generation of stress in the course of unipolar depression. J Abnorm Psychol 100:555–561. 10.1037//0021-843x.100.4.555 [DOI] [PubMed] [Google Scholar]
- 45.Harkness KL, Monroe SM (2016) The assessment and measurement of adult life stress: basic premises, operational principles, and design requirements. J Abnorm Psychol 125(5):727–745. 10.1037/abn0000178 [DOI] [PubMed] [Google Scholar]
- 46.Chassin L, Pitts SC, DeLucia C, Todd M (1999) A longitudinal study of children of alcoholics: predicting young adult substance use disorders, anxiety, and depression. J Abnorm Psychol 108(1):106–119. 10.1037/0021-843X.108.1.106 [DOI] [PubMed] [Google Scholar]
- 47.McClure EB, Brennan PA, Hammen C, Le Brocque RM (2001) Parental anxiety disorders, child anxiety disorders, and the perceived parent–child relationship in an Australian high-risk sample. J Abnorm Child Psychol 29(1):1–10. 10.1023/A:1005260311313 [DOI] [PubMed] [Google Scholar]
- 48.Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J et al. (2010) Coping and parenting: mediators of 12-month outcomes of a family group cognitive-behavioral preventive intervention with families of depressed parents. J Consult Clin Psychol 78(5):623–634. 10.1037/a0020459 [DOI] [PMC free article] [PubMed] [Google Scholar]


