Abstract
Background & objectives
This article examines whether women are less prone than men to Covid-19 infections and their complications.
Data sources
We reviewed available databases and searched systematically for publications. To be taken into account, data had to be broken down by gender. There was no study evaluation nor quantification synthesis, due to the large heterogeneity of the studies. Nineteen databases were selected. 73 publications were considered and 33 were selected, to which 12 more were added.
Results
Globally, the proportion of men and women who tested positive is comparable. However, men are about 60 % more likely to be severely ill or to die from the complications of Covid-19 than are women.
Limitations
The study was hampered by a large heterogeneity in testing and reporting of the data.
Conclusions
Although in the pandemic men die more frequently than women from Covid-19, it is not clear whether this is due to biological differences between men and women, differences in behavioral habits, or differences in the rates of co-morbidities.
Implications of key findings
Countries and studies should report their data by age, gender and co-morbidities. This may have implications in terms of vaccination strategies, the choice of treatments and future consequences for long-term health issues concerning gender equality.
Keywords: Covid-19, Sex difference, Gender difference, Complications, Fatality rate
1. Introduction
Unfortunately, it is well known that we are not all equal in adversity. It has been reported that older people and those with preexistent co-morbidities are at higher risk of dying from Covid-19 in the pandemic [[1], [2], [3]]. It is also possible that ethnic origin influences the prognosis of the Covid-19 infection, since diseases like diabetes and hypertension are more frequently found among patients of African origin [4]. Currently, it is unclear whether there is a direct link between race or ethnicity and the outcome of COVID-19 infection or whether race is a confounding factor due to the hidden effects of diabetes or hypertension, which are more prevalent, for instance, in the Afro-American population. [4]. The availability of health care resources may also play a major role, since access to health care systems may vary between countries or regions, but may also vary within a region according to socioeconomic factors or the presence of chronic diseases [5]. Analyses stratified by those factors should be carried out for the pandemic's data. The first publications from China and Italy reported higher fatality rates, due to the pandemic, in men than in women [6,7]. Following these publications, some authors suggested that the reduced susceptibility of women to viral infections could be attributed to the protection from the X chromosome as well as from sex hormones, which play an essential role in innate and adaptive immunity [8]. Therefore the current gender difference in the response to the pandemic raises a number of questions: here are a few of them.
Are women and men similarly vulnerable or is there a difference in susceptibility?
Are the biological and clinical immune responses identical? Are symptoms in women and men similar? What is the proportion of men and women who are hospitalized and transferred to intensive care units (ICU)? Are the responses to treatment and the recovery patterns similar in men and women? Are the fatality rates identical? And finally will the response to vaccines be comparable in men and women?
We review only some of the currently available data, notably the sex-difference in susceptibility to the Covid-19 infection and the concomitant risk of death. Indeed, it will not be possible to determine whether biological and clinical immune responses are the same in women and men until data becomes available regarding the cytokine release syndrome (CRS) and the production of antibodies are identified and systematically measured. Similarly there are not enough data to determine whether symptoms and imaging are comparable in women and men.
2. Methods
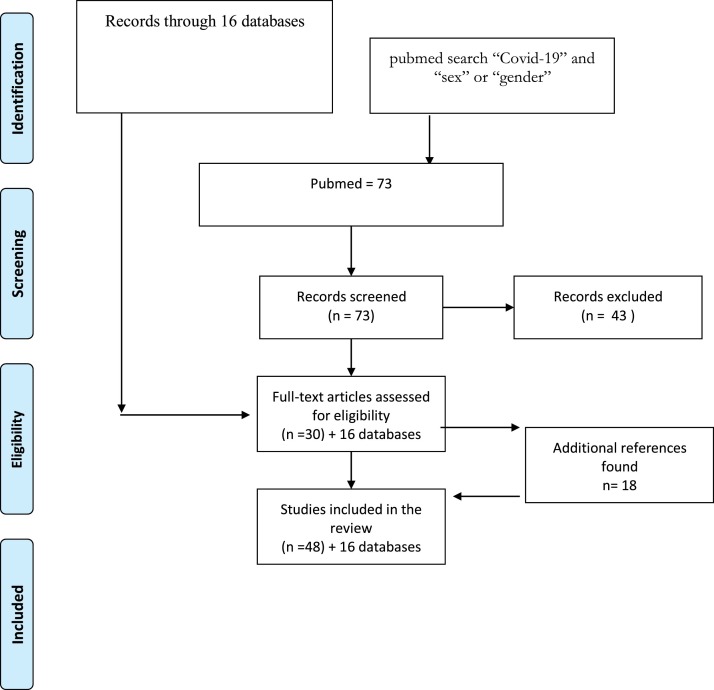
We conducted a thorough research of epidemiological databases, available in English, French, German, Spanish, Italian, and Dutch [6,9,26]. We collected data from 16 websites, such as “Our World on data”, https://coronavirus.jhu.edu/us-map and “https://globalhealth5050.org/covid19/ », (which are freely accessible websites presenting research, data or actions for gender equality in global health) (6, 9–24). We selected only the countries where data were presented by sex, either for prevalence of positive tests, or hospitalization or deaths. We completed the search on PubMed using the Mesh terms: “Covid-19” AND “sex” OR “gender”. Our search retrieved 73 items, but only 30 of these were related to the subject through 18 other articles were added to this review (Fig. 1 ) (25–64). Finally, we added personal data from our hospital (an inner-city, university, tertiary hospital located in Brussels) concerning the first hospitalized Covid-19 patients (personal communication). The study was accepted by the Ethical Review Board of the CHU St Pierre.
Fig. 1.
Flowchart of the selected studies and databases.
Statistics: We used only descriptive data from which we calculated the men to women death ratio for Europe.
3. Results
3.1. Are women and men similarly vulnerable or is there a difference in susceptibility?
The only way to answer this question would require universal screening of men and women with a breakdown of data by age and gender. According to “Our World on data”, not all countries provide testing data [[9], [10], [11]]. Most countries only provide incomplete data and these concern analyses of tests for the presence of the virus thereby determining whether an individual is infected and not whether he or she has developed immunity (the presence of antibodies). Furthermore, it is often unclear how to interpret tests [[9], [10], [11]]. Some people are tested more than once, some countries report the number of tests performed, others the number of individuals that have been tested. There is also extensive heterogeneity in the number of false positive and negative results, among tests [[9], [10], [11]]. In some countries systematic virus testing by PCR, of large segments of the population, has begun, in others, mildly symptomatic patients were tested, in some others, only severely ill or hospitalized patients were tested. Moreover, the attitude towards testing geriatric patients and health providers who work with infected patients, varied considerably. This explains that the range in testing coverage differs tremendously between countries (while Iceland was testing close to 150 out of 1000 people, the UK was testing 13/1000 people) and demonstrates why the comparison of prevalence between countries is difficult [[9], [10], [11], [12]]. The pandemic started in China, spread to other Asian countries, before reaching Italy and then other European countries and the US. Consequently, diverse countries are at different stages of the epidemic trajectory, and it is difficult to compare or to pool data before the epidemic curve has been completed in the respective countries. This is well illustrated by dynamic graphs [9,10]. The presented data originate therefore from selected, non-random samples, and are characterized by considerable heterogeneity.
Very few countries provide categorization of their numbers by gender [11]. In Table 1 , we show the number of patients tested per one thousand habitants, as this reflects whether tests are largely available or only available in specific, limited circumstances. We report the proportion of positive tests in men or women when available (Table 1) [[9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26]]. In the meta-analysis conducted by Fu et al. comprising 42 studies in China, the proportion of male patients ranged from 29.0% to 77.0% (median 56.5 %) [25]. The proportion of males tested positive to Covid-19 was higher as compared to females in Asia (with the exception of South Korea), in South America, in the New York area [[9], [10], [11],26,27], but not in Canada and in some European countries (Estonia and in Belgium) [[9], [10], [11],14,16,18] where more women tested positive than men (Table 1). The proportions were quite comparable when considering global Europe, and were also comparable on board of the Diamond Princess cruise ship (Table 1) [9,28].
Table 1.
Adapted with permission from https://globalhealth5050.org/covid19/. Only data broken down by gender per country are presented (data collected from official government sources in each country) (last available 4.5.20). Definitions of cases and deaths may vary by country. Data to be used to understand the breakdown by gender within a country rather than cases or deaths per country. (ref 9-12).
| Region | Extraction date | People tested/1000 | Cases |
Deaths |
Deaths among confirmed cases |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | % male | % female | Total | % male | % female | % male | % female | Ratio - male:female | |||
| Europe | 1.349.347 | 49 % | 51 % | 122.318 | 61% | 39 % | 112% | 6,9% | 1,6 | ||
| Austria | 28.04.20 | 30,5 | 15.314 | 49 % | 51 % | 550 | 56 % | 44 % | 4,1% | 3,1% | 1,3 |
| Belgium | 28.04.20 | 30,5 | 47.682 | 37 % | 63 % | 5.286 | 51 % | 49 % | 153% | 8,6% | 1,8 |
| Croatia | 28.04.20 | 9,3 | 2.064 | 46 % | 54 % | 67 | |||||
| Czech Republic | 28.04.20 | 24.1 | 7.393 | 48 % | 52 % | 225 | |||||
| Denmark | 28.04.20 | 40.4 | 8.851 | 42 % | 58 % | 434 | 57 % | 43 % | 6,6% | 3,6% | 1,8 |
| Estonia | 41.6 | 1.700 | 55 % | 45 % | 55 % | ||||||
| Finland | 28.04.20 | 18,5 | 4.740 | 48 % | 52 % | 145 | 52 % | 48 % | 3,3% | 2,8% | 1,2 |
| France | 28.04.20 | 11.1 | 128.339 | 14.579 | 60 % | 40 % | |||||
| Germany | 28.04.20 | 30.4 | 156.337 | 48 % | 52 % | 5.908 | 57 % | 43 % | 4,5% | 3,2% | 1,4 |
| Greece | 27.04.20 | 7,6 | 2.324 | 55% | 45 % | 132 | 76% | 24 % | 7,8% | 3,1% | 2,5 |
| Hungary | 29.04.20 | 8,5 | 2.727 | 300 | 51 % | 49 % | |||||
| Iceland | 28.04.20 | 147,6 | 1.795 | 50 % | 50 % | 10 | |||||
| Republic of Ireland | 27.04.20 | 31,0 | 19.666 | 42 % | 58 % | 903 | 53% | 47 % | 5,8% | 3,7% | 1,5 |
| Italy | 23.04.20 | 24,1 | 176.716 | 49 % | 51 % | 23.164 | 63 % | 37 % | 171% | 9,3% | 1,8 |
| Luxembourg | 28.04.20 | 76,9 | 3.741 | 51 % | 49 % | 89 | 56 % | 44 % | 2,6% | 2,1% | 1,2 |
| The Netherlands | 28.04.20 | 13,2 | 38.365 | 38 % | 62 % | 4.566 | 57 % | 43 % | 181% | 8,1% | 2,2 |
| Norway | 28.04.20 | 31,8 | 7.605 | 49 % | 51 % | 195 | 55 % | 45 % | 2,9% | 2,3% | 1,3 |
| Northern Ireland | 20.04.20 | 31,0 | 2.724 | 41 % | 59 % | 206 | 56 % | 44 % | 104% | 5,6% | 1,8 |
| Poland | 28.04.20 | 9,9 | 12.218 | 594 | 54 % | 46 % | |||||
| Portugal | 27.04.20 | 41,9 | 24.322 | 41 % | 59 % | 948 | 49 % | 51 % | 4,7% | 3,3% | 1,4 |
| Romania | 26.04.20 | 9,9 | 11.313 | 45 % | 55 % | 619 | 64% | 36 % | 7,9% | 3,5% | 2,3 |
| Serbia | 29.04.20 | 15,0 | 8.724 | 173 | 63 % | 37 % | |||||
| Spain | 28.04.20 | 28,9 | 204.856 | 44 % | 56 % | 15.853 | 58 % | 42 % | 102% | 5,8% | 1,8 |
| Sweden | 28.04.20 | 11,8 | 19.621 | 45 % | 55 % | 2.355 | 57 % | 43 % | 151% | 9,4% | 1,6 |
| Switzerland | 29.04.20 | 30,6 | 29.376 | 46 % | 54 % | 1.408 | 58 % | 42 % | 6,1% | 3,7% | 1,6 |
| UK (England, Wales) | 17.04.20 | 13,0 | 19.093 | 60 % | 40 % | ||||||
| UK (Scotland) | 19.04.20 | 13,0 | 2.272 | 53% | 47 % | ||||||
| Ukraine | 28.04.20 | 3,0 | 9.410 | 44 % | 56 % | 239 | 55 % | 45 % | 3,2% | 2,0% | 1,6 |
| Israel | 19.04.20 | 45,4 | 13.491 | 171 | 50 % | 50 % | |||||
| North America | |||||||||||
| Canada | 27.04.20 | 23,7 | 26.638 | 44 % | 56 % | 1.067 | 50 % | 50 % | 4,5% | 3,6% | 1,3 |
| USA | 28.04.20 | 20,6 | 1.035.765 | 31.586 | 57 % | 43 % | |||||
| Mexico | 27.04.20 | 0,6 | 15.529 | 58 % | 42 % | 1.434 | 68% | 32 % | 109% | 6,9% | 1,6 |
| Asia | |||||||||||
| China | 28.02.20 | 55.924 | 51 % | 49 % | 2.114 | 64% | 36 % | 4,7% | 2,8% | 1,7 | |
| Iran | 17.03.20 | 5,9 | 14.991 | 57 % | 43 % | 853 | 59 % | 41 % | 5,9% | 5,4% | 1,1 |
| India | 06.04.20 | 0,4 | 4.065 | 76 % | 24 % | 111 | 73 % | 27 % | 2,6% | 3,1% | 0,9 |
| Indonesia | 28.04.20 | 0,3 | 9.511 | 59 % | 41 % | 773 | 68% | 32 % | 9,3% | 6,4% | 1,5 |
| Japan | 26.04.20 | 1,5 | 13.084 | 57 % | 43 % | 372 | |||||
| Malaysia | 28.04.20 | 6,1 | 5.851 | 94 | 78% | 22 % | |||||
| Pakistan | 29.04.20 | 0,9 | 14.885 | 79% | 21 % | 327 | 74 % | 26 % | 2,0% | 2,8% | 0,7 |
| Philippines | 28.04.20 | 0,9 | 7.955 | 54 % | 46 % | 530 | 66% | 34 % | 8,2% | 4,9% | 1,7 |
| South Korea | 28.04.20 | 12,3 | 10.752 | 40 % | 60 % | 244 | 52 % | 48 % | 2,9% | 1,8% | 1,6 |
| Thailand | 27.04.20 | 1,1 | 2.938 | 55 % | 45 % | 52 | 77% | 23 % | 2,5% | 0,9% | 2,7 |
| Australia | 28.04.20 | 24,8 | 6.713 | 50 % | 50 % | 84 | 61% | 39 % | 1,5% | 1,0% | 1,5 |
| South america | |||||||||||
| Argentina | 27.04.20 | 1,3 | 3.892 | 50 % | 50 % | 192 | 65 % | 35 % | 6,3% | 3,5% | 1,8 |
| Colombia | 27.04.20 | 2,3 | 5.597 | 52 % | 48 % | 253 | 62 % | 38 % | 5,4% | 3,5% | 1,5 |
| Dominican Republic | 26.04.20 | 6.293 | 54 % | 46 % | 282 | 78% | 22 % | 6,5% | 2,1% | 3,0 | |
| Ecuador | 28.04.20 | 3,5 | 15.728 | 55 % | 45 % | 871 | 68% | 32 % | 6,9% | 3,9% | 1,8 |
| Peru | 26.04.20 | 11,4 | 28.699 | 62 % | 38 % | 782 | 71% | 29 % | 3,1% | 2,1% | 1,5 |
| Africa | |||||||||||
| South Africa | 19.04.20 | 4,1 | 3.142 | 45% | 55 % | 43 | 56% | 44 % | 1,7% | 1,1% | 1,5 |
3.2. What are the proportions of men and women who are hospitalized and transferred to intensive care units (ICU)?
Currently, the incidence, the prevalence and the COVID-19 fatality ratios are not well known. The reasons are, first, that the denominators of incidence and prevalence are not defined, mainly because random sampling of the population has not been carried out (samples are selective as mentioned previously) and secondly, multivariate analyses are needed to determine the exact effect of COVID-19 on adverse outcomes, given other risk factors such as gender, age or comorbidities.
We did however search national databases and registries that presented data in relation to gender. When possible, we further sought to classify the data by age and comorbidities. Male hospitalization rates were higher than female ones, in all countries which reported them, ranging from 55 % to 62 % (Table 1) [10,11,16,17,20,22]. The proportion of male admissions to the ICU was even higher ranging from 65 % to 74 % [10,11]. Throughout Europe, 73 % of all ICU admissions were for men (Table 1) [9,12]. Most, but not all, of early publications from China reported that men presented three times more often prolonged SARS-CoV-2 RNA shedding, had twice the risk of developing kidney disease as well as more frequent refractory pneumonia and metabolic associated fatty liver disease (MAFLD) [[29], [30], [31], [32], [33], [34]]. Similarly, in the Seattle and New York areas more men (63 % and 76 %) were admitted to the ICU [27,35]. In our own hospital the first 272 patients that were admitted had a median age of 60 years; 45 % had hypertension, 30 % diabetes and 20 % cardiovascular diseases. Sixty-six percent of these patients were men. Fifty seven out of 272 were admitted to the ICU, of which 63 % were men (personal communication).
3.3. What are the fatality rates for men and women?
Reported death rates vary tremendously between countries. But almost all of the data that broke numbers down by gender, reported a higher proportion of deaths among men than among women (ranging between 59 % and 69 %) (Table 1). With the exception of India and Pakistan, all other countries reported a male to female death ratio ranging between 3 and 1.1. Even in countries where fewer male than female cases were reported the death rates were still higher for males (Table 1).
The first report from China quoted a death rate of 2.8 % in men and 1.7 % in women [6]. In other series in China, more men than women died (73 % vs 27 %), and had higher fatality rates (3.6 % vs 1.6 %) [[36], [37], [38], [39], [40]]. This was also the case in Australia, Austria, Belgium, Denmark, France, Germany, Italy, Europe (in general), Seattle and New York (Table 1). In Italy, at all ages the lethality rate of Covid-19 was higher for men than for women (globally 13.3 % vs 7.4 % at ages 40−49: 1.1 % vs 0.4 %, 50−49 2.9 % vs 0.9 %, 60−69: 8.6 % vs 4.2 %, 70–79 23.1 % vs 13.9 %, 80–89 34.1 % vs 21.2 %, and above 90 : 36.6 % vs 21.4 % [23].
In New York, men accounted for 60.3 % of deaths and women for 39.7 %. An even higher proportion of men were admitted to the ICU (76.5 % vs 33.5 %), while more women were being discharged and more men died in each age class. [28]. Nevertheless, there is still a lack of data classified by age, sex and comorbidities.
4. Discussion
Earlier publications reported that men were more frequently infected with COVID‐19 than women, with men accounting for 60 % of infected patients [8]., This has also been reported for MERS‐COV and SARS‐COV [8]. Nevertheless, these data should be interpreted with great caution. Indeed, other publications did not report sex differences among people with seasonal coronaviruses and respiratory illnesses: among 84,957 episodes of respiratory illness, in Scotland, between 2007 and 2015, the global sex distribution was approximately equal, with 51.6 % of patients being female [38]. However, these authors reported greater numbers among males than females for certain infections such as CoV-229E, CoV−OC43, CoV-NL63 and influenza, with higher hospitalization and mortality rates in men [38]. Furthermore, there is a marked heterogeneity concerning the current pandemic as to who is being tested. In Iceland, a large proportion of the population has been tested (148 people per thousand inhabitants), whereas in other countries only severely symptomatic patients have been tested (11 per thousand in France). The number of tests is constantly increasing. The “picture” that we report here, therefore only reflects the situation at the beginning of May 2020. But if we rely on the most comprehensive available data, there seems to be no important difference in terms of infection prevalence between men and women (women have a 2 %–8 % lower exposure rate than men in some countries). The South Korea data are an exception. Indeed, in this series of 4.212 patients, only 37.7 % of the infected ones where male [29]. But the authors provided an explanation: the discrepancy was probably due to an increase of infected women, in a religious group of Daegu [29]. The Belgian data also are somewhat particular because they present data by sex and age group. They found a higher rate of infections in women before the age of 60 and a lower rate thereafter. It is possible, however, that these data are biased by the higher rate of women working in hospitals and more prone to be infected therefore [39,40]. About 70 % of confirmed infected health workers were found to be women, in Spain, the USA, Italy and Germany [[9], [10], [11], [12],[21], [22], [23]].
We don’t know much yet about the spectrum of symptoms in men and women. One series of 263 (63.1 %) women and 154 men (36.9 %) mildly-to-moderately affected patients, by COVID-19, reported that women were significantly more affected by olfactory and gustatory dysfunctions than men [41].
We did find data broken down by sex, for patients requiring hospitalization in some countries or areas (Denmark, France, New York, Belgium) [11,16,17,20,27]. In these areas, more men were hospitalized than women (between 57 % and 74 %). Similarly, in all countries reporting death rates from Covid19 infections, by sex, more men died than women (60 %–70 % of men) (Table 1) [11].
These data need also to be interpreted cautiously. There are many diverse ways to evaluate Covid-19 related mortality. For instance, the fatality ratio (the number of deaths divided by the number of confirmed cases) depends on how many tests are performed. When extensive screening occurs, the fatality ratio is lowered (Austria, Germany, Finland) [[9], [10], [11],15,21]. On the other hand, the mortality rate will rise, when deaths suspected to be related to Covid -19, in patients untested for the presence of the virus, are attributed to the pandemic (this is what happened in Belgium where about half of the deaths occurred in geriatric living facilities, but only 11 % of the patients who died had been tested for Covid 19) [16]. The fatality rate also depends on the country’s age pyramid (the older the population the higher the rate). This was the case in Italy [23].
As suggested by others, the difference in vulnerability towards the pandemic could be due to biological differences between men and women. But whether men are more susceptible to an infection or its increased severity, or whether woman have some natural protection against these viruses, is not clear [42].
It has been previously reported that men suffering from all-cause infectious sepsis have a 70 % higher mortality rate than women and this is also the case for SARS and MERS respiratory infections (21.9 % vs 13.2 %) [43,44]. Women seem to have a more robust immune system [45]. It has been reported that women have stronger immune responses to infections and vaccinations than men. This is, among other factors, due to the documented effects of estrogens, progestogens and androgens [45]. For instance, estrogens suppress T and B cell lymphopoiesis and activates B cell function. Estrogen enhances humoral responses, B cell differentiation and immunoglobulin (Ig) production [45]. The difference in gender immune responses may also have a role in why women have a higher incidence (up to 15 times more for thyroiditis) of autoimmune diseases [45].
The presence of two X chromosomes in women emphasizes the immune system even if one is inactive. The immune regulatory genes encoded by X chromosome in women has been associated with lower viral load levels, and less inflammation in women than in men, with better immune responses and higher levels of CD4 + T cells, higher levels of antibodies that persist longer, higher levels of TLR7, which result in an increased resistance toward viral infections [45]. The production of inflammatory IL-6 after viral infection is lower in women than in men. Other genes involved in the immunological answer have been implicated and are localized on the X chromosome, like FOXP3 [46]. In any case, if estrogen decreases the risk of Covid-19, it is unlikely to do so by reducing the susceptibility rate, but rather by decreasing the severity of the disease. The worsening of the disease could also be associated with differences in ACE1 polymorphism. Indeed, a significant correlation was found between ACE1 D/I polymorphism and Covid-19 prevalence, when data from 33 countries were extracted (r2 = 0.41) [47].It should be noted that in that study, ACE1 D/I polymorphism was also correlated with Covid-19 mortality, when the data were corrected for the onset of mortality (r2 = 0.457) [47]. These data suggest that ACE1 D/I polymorphism may be a confounder in the spread of COVID19 and the outcome of the infection [47]. The D/I polymorphism of intron 16 of ACE1, located on chromosome 17, is associated with alterations in circulating and tissue concentrations of ACE. The deletion is associated with a reduced expression of ACE2 [47]. SARS-CoV-2 uses the SARS-CoV receptor ACE2 for entrance into the cell [48]. Sex differences in the expression of ACE genes have been reported [49,50]. In animal models, estradiol reduces renal ACE2 activity (it is increased in males and in ovarectomized mice) (50)
Data from epidemiologic-, in vitro-, and knock-out studies, in mice, suggest that SARS-CoV-2 infection involves the role of the transmembrane serine protease 2 (TMPRSS2). The latter is a cell-surface protein, expressed by epithelial cells among others of the aerodigestive tract [51]. Coronaviruses may depend on TMPRSS2 for viral entry and spread in the host. First viral hemagglutinin protein attaches to the angiotensin-converting enzyme 2 (ACE2), encoded, by the ACE2 gene [51]. Hemagglutinin is thereafter cleaved to activate internalization of the virus. This step may be dependent on TMPRSS2. TMPRSS2 was first identified in prostate cancer, where its expression is upregulated by prostate cancer cell lines in response to androgens [51]. Often there is a gene fusion between the TMPRSS2 and ERG genes [52]. This gene fusion is consequently controlled by androgen receptor signaling. In men, tumors with the TMPRSS2–ERG fusion have higher insulin/insulin-like growth factor signaling, and TMPRSS2–ERG may modify how hormonal risk factors such as obesity influence the risk of metastasis [52], although there seems to be no difference in expression of TMPRSS2 in lung tissue between men and women. Low levels of androgens in women may suffice to sustain TMPRSS2 expression, and. tumors with TMPRSS2–ERG fusion may be responsive to estrogen signaling. Further studies should evaluate TMPRSS2 polymorphisms and whether androgen modulators modify the TMPRSS2 expression and respiratory consequences of SARS-CoV-2 [52].
Aside from biological differences between men and women, there are also environmental differences that may play a role. It has also been documented that women are more attentive to hygiene measures such as hand washing than are men [53]. While this may be the case, it should probably influence rather the infection rates, rather than complication rates of the disease.
Alternatively, since the prevalence of infection seems to be quite similar between sexes, but the severity of the disease, the complications and the deaths rates much higher in men than women, it is also plausible that this may be due to a higher rate of co-morbidities in infected men than women, or to differences in behaviors between them. Not all of the reports support smoking as a predisposing factor in men or any subgroup for infection with SARS-CoV-2, since they reported only small proportions of smokers among the affected patients (actually much lower than the smoking prevalence in China) [54,55]. Nevertheless, it should be noted that worldwide a third of men smoke, whereas about 6 % of women do [55]. This difference in smoking habits results in much higher rates of disease and co-morbidities that are influenced by smoking [55]. There are, for instance, almost four times as many lung cancers in men than in women in France, Germany, Italy and South Korea, [55]. Men develop cardiovascular disease, hypertension and diabetes more frequently and at a younger age than women. These co-morbidities have been associated with an increased rate of death associated with Covid-19 infection [56]. Bots et al. reported that while the gap between sexes, in cases of cardiovascular disease narrowed between 1980 and 2010, Coronary heart disease (CHD) mortality was still on average about five times higher in men and the stroke mortality was twice as high. [57]. The pattern of the case fatality rate, seen for COVID-19, may therefore be comparable to that of other major causes of mortality in the elderly, such as heart disease, diabetes, or combined influenza and pneumonia [58].
This review is hampered by several limitations, as mentioned before: there is a marked heterogeneity concerning who is being tested, the tests that are used and the number of tests are increasing constantly. We only selected databases that presented data by sex and in languages that we understood.
To conclude : a breakdown of hospitalization rates in the ICU and death rates by sex, age and co-morbidities is necessary in order to answer the question of whether men are more at risk for Covid-19 than women [59,60]. These results may also have implications as treatments and vaccines are currently being tested on men and women [61]. Although women seem to die less frequently than men from the immediate consequences of the Covid-19 pandemic, women may be more exposed, given their predominant roles as caregivers within families and as front-line health-care workers [62]. Moreover, we do not yet know what the long-term consequences will be on women’s health. For instance, the pandemic will have dramatic consequences on economic issues, which often affect women more than men [63,64]
Contributors
Serge Rozenberg collected and analysed the literature data, and drafted the manuscript.
Jean Vandromme checked the literature data.
Charlotte Martin checked the literature data, and collected and analyzed data in the CHU St Pierre.
The manuscript was reviewed and approved by all co-authors.
Funding
The study was not funded.
Ethical approval
Our use of personal data from our hospital concerning the first hospitalized Covid-19 patients was approved by the Ethical Review Board of the CHU St Pierre.
Provenance and peer review
Peer review was directed by Irene Lambrinoudaki independently of Serge Rozenberg, an author and Maturitas editor, who was blinded to the process.
Declaration of Competing Interest
The authors declare that they have no present conflict of interest. In the past S Rozenberg received fees for advisory boards and lectures (Gedeon, Abbot, Mylan, UCB), or research grants (Amgen, Gedeon, and Mylan). Jean Vandromme: advisory boards and lectures (Gedeon). Charlotte Martin has nothing to declare.
Acknowledgement
We thank “Global Health 50/50 info@globalhealth5050.org” for the permission to reproduce their table.
References
- 1.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N., Cuomo-Dannenburg G., Thompson H., Walker PGT Fu H., Dighe A., Griffin J.T., BaguelinM Bhatia S., Boonyasiri A., Cori A., Cucunubá Z., FitzJohn R., Gaythorpe K., Green W., Hamlet A., Hinsley W., Laydon D., Nedjati-Gilani G., Riley S., van Elsland S., Volz E., Wang H., Wang Y., Xi X., Donnelly C.A., Ghani A.C., Ferguson N.M. Estimates of theseverity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;(March 30):30243–30247. doi: 10.1016/S1473-3099(20)30243-7. pii: S1473-3099(20)[Epub ahead of print] PubMed PMID: 32240634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du Y., Tu L., Zhu P., Mu M., Wang R., Yang P., Wang X., Hu C., Ping R., Hu P., Li T., Cao F., Chang C., Hu Q., Jin Y., Xu G. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020;(April 3) doi: 10.1164/rccm.202003-0543OC. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, February 12-March 28, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020;69(April3 (13)):382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bornstein S.R., Dalan R., Hopkins D., Mingrone G., Boehm B.O. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol. 2020;2:1–2. doi: 10.1038/s41574-020-0353-9. April[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ji Y., Ma Z., Peppelenbosch M.P. Q Pan potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8(April(4)):e480. doi: 10.1016/S2214-109X(20)30068-1. Epub 2020 Feb 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.https://www.worldometers.info/coronavirus/coronavirus-age-sex-demographics/.
- 7.Livingston E., Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020;17 doi: 10.1001/jama.2020.4344. Published online March. [DOI] [PubMed] [Google Scholar]
- 8.Li L.Q., Huang T., Wang Y.Q., Wang Z.P., Liang Y., Huang T.B., Zhang H.Y., Sun W., Wang Y.Q. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis [published online ahead of print, 2020 Mar 12] J Med Virol. 2020 doi: 10.1002/jmv.25757. doi:10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hasell J., Ortiz-Ospina E., Mathieu E., Ritchie H., Beltekian D., Roser M. 2020. Data on COVID-19 Testing.March 31.https://ourworldindata.org/covid-testing [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.https://coronavirus.jhu.edu/us-map.
- 11.https://globalhealth5050.org/covid19/.
- 12.http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/weekly-surveillance-report.
- 13.https://www.ecdc.europa.eu/en/covid-19-pandemic.
- 14.https://www.health.gov.au/resources/publications/covid-19-cases-in-australia-by-gender-and-age.
- 15.http://www9.health.gov.au/cda/source/rpt_5.cfm.
- 16.https://www.sozialministerium.at/Informationen-zum-Coronavirus/Neuartiges-Coronavirus-(2019-nCov).html.
- 17.https://epistat.wiv-isp.be/covid/.
- 18.https://files.ssi.dk/COVID19-overvaagningsrapport-07042020-wvp1.
- 19.https://www.koroonakaart.ee/en.
- 20.https://experience.arcgis.com/experience/d40b2aaf08be4b9c8ec38de30b714f26.
- 21.https://www.santepubliquefrance.fr/recherche/#search=COVID-19%20:%20point%20epidemiologique&sort=date.
- 22.https://ourworldindata.org/covid-testing#germany.
- 23.http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=italiano&id=5351&area=nuovoCoronavirus&menu=vuoto.
- 24.https://www.covid.is/data.
- 25.Fu L., Wang B., Yuan T., Chen X., Ao Y., Fitzpatrick T., Li P., Zhou Y., Lin Y.F., Duan Q., Luo G., Fan S., Lu Y., Feng A., Zhan Y., Liang B., Cai W., Zhang L., Du X., Li L., Shu Y., Zou H. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;(April 10) doi: 10.1016/j.jinf.2020.03.041. pii: S0163-4453(20)30170-5[Epub ahead of print] PubMed PMID: 32283155; PubMed Central PMCID: PMC7151416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Korean Society of Infectious Diseases Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35(March16(10)):e112. doi: 10.3346/jkms.2020.35.e112. eISSN 1598-6357·pISSN 1011-8934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., the Northwell COVID-19 Research Consortium, Barnaby D.P., Becker L.B., Chelico J.D., Cohen S.L., Cookingham J., Coppa K., Diefenbach M.A., Dominello A.J., Duer-Hefele J., Falzon L., Gitlin J., Hajizadeh N., Harvin T.G., Hirschwerk D.A., Kim E.J., Kozel Z.M., Marrast L.M., Mogavero J.N., Osorio G.A., Qiu M., Zanos T.P. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;(April 22) doi: 10.1001/jama.2020.6775. [Epub ahead of print] PubMed PMID: 32320003; PubMed Central PMCID: PMC7177629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mizumoto K., Kagaya K., Zarebski A., Chowell G. Estimating the asymptomaticproportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond princess cruise ship, Yokohama, Japan. Euro Surveill. 2020;2020(March(10)) doi: 10.2807/1560-7917.ES.2020.25.10.2000180. 25 PubMed PMID: 32183930; PubMed Central PMCID: PMC7078829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu K., Chen Y., Yuan J., Yi P., Ding C., Wu W., Li Y., Ni Q., Zou R., Li X., Xu M., Zhang Y., Zhao H., Zhang X., Yu L., Su J., Lang G., Liu J., Wu X., Guo Y., Tao J., Shi D., Yu L., Cao Q., Ruan B., Liu L., Wang Z., Xu Y., Liu Y., Sheng J., Li L. Factors associated with prolonged viral RNA shedding in patients with COVID-19. Clin Infect Dis. 2020;(April 9) doi: 10.1093/cid/ciaa351. pii: ciaa351[Epub ahead of print] PubMed PMID: 32271376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L., Li J., Yao Y., Ge S., Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;(March 20) doi: 10.1016/j.kint.2020.03.005. pii: S0085-2538(20)30255-6.[Epub ahead of print] PubMed PMID: 32247631; PubMed Central PMCID: PMC7110296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mo P., Xing Y., Xiao Y., Deng L., Zhao Q., Wang H., Xiong Y., Cheng Z., Gao S., Liang K., Luo M., Chen T., Song S., Ma Z., Chen X., Zheng R., Cao Q., Wang F., Zhang Y. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020;(March 16) doi: 10.1093/cid/ciaa270. [Epub ahead of print] PubMed PMID: 32173725.pii: ciaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zheng K.I., Gao F., Wang X.B., Sun Q.F., Pan K.H., Wang T.Y., Ma H.L., Liu W.Y., George J., Zheng M.H. Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism. 2020;(April 19) doi: 10.1016/j.metabol.2020.154244. [Epub ahead of print] PubMed PMID: 32320741; PubMed Central PMCID: PMC7166301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu J., Liu J., Zhao X., Liu C., Wang W., Wang D., Xu W., Zhang C., Yu J., Jiang B., CaoH Li L. Clinical characteristics of imported cases of COVID-19 in JiangsuProvince: a multicenter descriptive study. Clin Infect Dis. 2020;(February 29) doi: 10.1093/cid/ciaa199. pii:ciaa199[Epub ahead of print] PubMed PMID: 32109279;PubMed Central PMCID: PMC7108195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu R., Han H., Liu F., Lv Z., Wu K., Liu Y., Feng Y., Zhu C. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to feb 2020. Clin Chim Acta. 2020;505:172–175. doi: 10.1016/j.cca.2020.03.009. June Epub 2020 Mar 7. PubMed PMID: 32156607; PubMed Central PMCID: PMC7094385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bhatraju P.K., Ghassemieh B.J., Nichols M., Kim R., Jerome K.R., Nalla A.K., Greninger A.L., Pipavath S., Wurfel M.M., Evans L., Kritek P.A., West T.E., Luks A., Gerbino A., Dale C.R., Goldman J.D., O’Mahony S., Mikacenic C. Covid-19 in critically ill patients in the seattle region - case series. New England J. Med. 2020 doi: 10.1056/NEJMoa2004500. NEJMoa2004500. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., Ma K., Xu D., Yu H., Wang H., Wang T., Guo W., Chen J., Ding C., Zhang X., Huang J., Han M., Li S., Luo X., Zhao J., Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368(March 26) doi: 10.1136/bmj.m1091. m1091Erratum in: BMJ. 2020 Mar31;368:m1295. PubMed PMID: 32217556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;(March 27) doi: 10.1001/jamacardio.2020.1286. [Epub ahead of print] PubMed PMID: 32219363. [DOI] [PubMed] [Google Scholar]
- 38.Nickbakhsh S., Ho A., Marques D.F.P., McMenamin J., Gunson R.N., Murcia P.R. Epidemiology of seasonal coronaviruses: establishing the context for COVID-19 emergence. J Infect Dis. 2020;(April 15) doi: 10.1093/infdis/jiaa185. pii: jiaa185. [Epub ahead of print] PubMed PMID: 32296837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020[J] China CDC Weekly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- 40.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. (published online Feb 7.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lechien J.R., Chiesa-Estomba C.M., De Siati D.R., et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur. Arch. Otorhinolaryngol. 2020 doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Walter L.A., McGregor A.J. Sex- and gender-specific observations and implications for COVID-19. West J Emerg Med. 2020;(April 10) doi: 10.5811/westjem.2020.4.47536. [Epub ahead of print] PubMed PMID: 32302282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matsuyama R., Nishiura H., Kutsuna S., et al. Clinical determinants of the severity of Middle East respiratory syndrome (MERS): a systematic review and meta-analysis. BMC Public Health. 2016;16(1):1203. doi: 10.1186/s12889-016-3881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Channappanavar R., Fett C., Mack M., et al. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017;198(10):4046–4053. doi: 10.4049/jimmunol.1601896. 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moulton V.R. Sex hormones in acquired immunity and autoimmune disease. Front. Immunol. 2018;9:2279. doi: 10.3389/fimmu.2018.02279. Published 2018 Oct 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Conti P., Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J Biol Regul Homeost Agents. 2020;34(April 7(2)) doi: 10.23812/Editorial-Conti-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 47.Delanghe J.R., Speeckaert M.M., De Buyzere M.L. COVID-19 infections are also affected by human ACE1 D/I polymorphism. Clin Chem Lab Med. 2020;(April 14) doi: 10.1515/cclm-2020-0425. pii: /j/cclm.ahead-of-print/cclm-2020-0425/cclm-2020-0425.xml. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 48.Itoyama S., Keicho N., Quy T., Phi N.C., Long H.T., Ha L.D., Ban V.V., Ohashi J., Hijikata M., Matsushita I., Kawana A., Yanai H., Kirikae T., Kuratsuji T., Sasazuki T. ACE1 polymorphism and progression of SARS. Biochem Biophys Res Commun. 2004;323(October 22(3)):1124–1129. doi: 10.1016/j.bbrc.2004.08.208. PMID: 15381116; PMCID: PMC7092806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wacker M.J., Godard M.P., McCabe E.H., Donnelly J.E., Kelly J.K. Sex difference in the association of the angiotensin converting enzyme I/D polymorphism and body mass index. Med Sci Monit. 2008;14(July(7)):CR353–7. [PubMed] [Google Scholar]
- 50.Liu J., Ji H., Zheng W., et al. Sex differences in renal angiotensin converting enzyme 2 (ACE2) activity are 17β-oestradiol-dependent and sex chromosome-independent. Biol Sex Differ. 2010;1(1):6. doi: 10.1186/2042-6410-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., Müller M.A., Drosten C., Pöhlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and Is blocked by a clinically proven protease inhibitor. Cell. 2020;(March 4) doi: 10.1016/j.cell.2020.02.052. S0092-8674(20)30229-4 Epub ahead of print PMID: 32142651; PMCID: PMC7102627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stopsack K.H., Mucci L.A., Antonarakis E.S., Nelson P.S., Kantoff P.W. TMPRSS2 and COVID-19: serendipity or opportunity for intervention? Cancer Discov. 2020;(April 10) doi: 10.1158/2159-8290.CD-20-0451. [Epub ahead of print] PubMed PMID: 32276929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnson H.D., Sholcosky D., Gabello K., Ragni R., Ogonosky N. Sex differences in public restroom handwashing behavior associated with visual behavior prompts. Percept Mot Skills. 2003;97(3 Pt 1):805–810. doi: 10.2466/pms.2003.97.3.805. [DOI] [PubMed] [Google Scholar]
- 54.Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med. 2020;(March 11) doi: 10.1016/S2213-2600(20)30117-X. Online ahead of print.PMID: 32171067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.H Ritchie and M Roser (2020) - "Smoking". Published online at OurWorldInData.org. Retrieved from: 'https://ourworldindata.org/smoking' [Online Resource].
- 56.Zhang P., Zhu L., Cai J., Lei F., Qin J.J., Xie J., Liu Y.M., Zhao Y.C., Huang X., Lin L., Xia M., Chen M.M., Cheng X., Zhang X., Guo D., Peng Y., Ji Y.X., Chen J., She Z.G., Wang Y., Xu Q., Tan R., Wang H., Lin J., Luo P., Fu S., Cai H., Ye P., Xiao B., Mao W., Liu L., Yan Y., Liu Y.M., Chen M.M., Zhang X.J., Wang X., Touyz R.M., Xia J., Zhang B.H., Huang X., Yuan Y., Rohit L., Liu P.P., Li H. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020;(April 17) doi: 10.1161/CIRCRESAHA.120.317134. [Epub ahead of print] PubMed PMID: 32302265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bots S.H., Peters S.A.E., Woodward M. Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010 BMJ. Global Health. 2017;(2) doi: 10.1136/bmjgh-2017-000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Promislow D.E.L. A geroscience perspective on COVID-19 mortality. J Gerontol A Biol Sci Med Sci. 2020;(April 17) doi: 10.1093/gerona/glaa094. pii: glaa094 [Epub ahead of print] PubMed PMID: 32300796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bhopal R. Covid-19 worldwide: we need precise data by age group and sex urgently. BMJ. 2020;3(369):m1366. doi: 10.1136/bmj.m1366. April PubMed PMID: 32245830. [DOI] [PubMed] [Google Scholar]
- 60.Dowd J.B., Andriano L., Brazel D.M., Rotondi V., Block P., Ding X., Liu Y., Mills M.C. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci U S A. 2020;(April 16) doi: 10.1073/pnas.2004911117. pii: 202004911. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wynants L., Van Calster B., Bonten M.M.J., Collins G.S., Debray T.P.A., De Vos M., Haller M.C., Heinze G., Moons K.G.M., Riley R.D., Schuit E., Smits L.J.M., Snell K.I.E., Steyerberg E.W., Wallisch C., van Smeden M. Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal. BMJ. 2020;7(369):m1328. doi: 10.1136/bmj.m1328. April PubMed PMID: 32265220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wenham C., Smith J., Morgan R. Gender and COVID-19 working group. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(March 14 (10227)):846–848. doi: 10.1016/S0140-6736(20)30526-2. Epub 2020 Mar 6. PubMed PMID: 32151325; PubMed Central PMCID: PMC7124625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gausman J., Langer A. Sex and gender disparities in the COVID-19 pandemic. J Womens Health (Larchmt). 2020;29(April(4)):465–466. doi: 10.1089/jwh.2020.8472. PubMed PMID: 32320331. [DOI] [PubMed] [Google Scholar]
- 64.https://data.unwomen.org/features/covid-19-and-gender-what-do-we-know-what-do-we-need-know.