THE OPIOID EPIDEMIC
Opioid-related morbidity and mortality has reached epidemic levels in the United States, with tragic results.1 Since 2000, the national age-adjusted drug overdose rate has more than doubled, from 6.2 per 100 000 persons in 2000, to 14.7 per 100 000 in 2014.2 In 2015, there were over 33 000 deaths attributed to opioid overdose in the United States, an increase of nearly 5000 compared with the previous year.3,4 For the first time, drug overdose has surpassed firearms and motor vehicle trauma as the most common cause of accidental death among adults.4 Most strikingly, the overall life expectancy in the United States has dropped for the first time since 1993, particularly for those under age 65 years.5 The highest increase as the cause of death (with a 6.7% increase between 2014 and 2015) was from unintentional injuries, including drug overdoses.
Different than other drug problems, the opioid epidemic affects everyone. A recent Kaiser Family Foundation study found that more than half of respondents had a personal connection to prescription painkiller abuse, with 16% knowing someone who had died from prescription opioid overdose.6 The results were similar across multiple socioeconomic and demographic features. County-level estimates highlight that nearly every geographic area in the country has seen marked increases of opioid-related deaths.7
The epidemic appears to have been fueled by the prescription of opioids.8 Sales of these medications increased about fourfold since 1999, and deaths involving prescription opioids have risen in parallel.9,10 The increase in prescribing opioids occurred despite a lack of overall changes in the amount of pain reported.11,12 Extensive attention given to physician prescribing of opioids has only been seen since very recently. The Centers for Disease Control and Prevention (CDC) have recently released guidelines,13 prescription drug monitoring programs have been implemented14 and more stringent laws such as the one passed in Massachusetts in 2016, in which prescribers are obligated to prescribe no more than 7 days’ worth of opioids for a first prescription (with rare exception) and are required to counsel patients on the risks of opioids, have been used.15
With these actions, the trend appears to be changing and prescribing of opioids has leveled off. In 2015, there were 16.6 million fewer opioid pain prescriptions written in the United States as compared with the previous year.16 Some believe that physician prescribing is no longer the sustaining force behind the epidemic.17 Although encouraging, the overall news is still bad: because prescriptions have become more limited, some people who previously misused prescription opioids are turning to illicit substances, such as heroin.18 Heroin is now purer, less expensive, and more easily available than before, making for a deadly combination.19 A recent report from the CDC showed that heroin overdose-related death rates increased by 26% between 2013 and 2014, having more than tripled since 2010.2 Furthermore, the acute threat is not only from heroin but also from synthetic opioids, such as fentanyl, acetyl-fentanyl, and carfentanil, which are mixed with or sold as heroin. These drugs, often greater than 50 times more potent than morphine, have seen an unprecedented increase in production and distribution by illegal operations. From 2013 to 2014, the number of reported deaths from fentanyl increased by 426%.20
HOW DID WE GET HERE?
It is helpful to explore how the opioid crisis began. It is a complex issue with at least 3 driving forces:
First, there is a moral imperative for physicians to treat pain and relieve suffering. This point has been confirmed recently by The Declaration of Montréal, a document developed during the First International Pain Summit on September 3, 2010, that states that the access to pain management is a fundamental human right.21 Physicians feel an obligation to treat pain, and opioids are effective for this purpose.
Second, for many years, there was a perceived under-treatment of pain, termed “oligoanalgesia.” There were also significant disparities between those who received analgesic treatment for pain, particularly among racial and ethnic minorities22–24 as well as for differences in age.25 Organizations, such as the Department of Veterans Affairs, began collecting data on pain treatment as a marker for quality, going as far as pronouncing “pain as the fifth vital sign.”26 Soon, patient surveys, such as those developed by the Centers for Medicare and Medicaid Services and Press-Ganey began asking patients questions about their pain management with results tied to physician reimbursement.27,28 Physicians had little option but to treat pain more aggressively, and opioid prescriptions markedly increased.
Finally, it is important to recognize the effect the pharmaceutical industry has had on increased opioid use. Pharma began aggressively marketing the use of opioids for noncancer pain.29,30 For example, Purdue Pharma, the maker of OxyContin (an extended-release version of oxycodone) spent US $200 million marketing the drug in 2001 alone, and saw a nearly tenfold increase in the prescribing of the drug to nearly 6.2 million annual prescriptions in 2002.31 Distribution of opioids through the pharmaceutical supply chain increased from 96 morphine milligram equivalents per person in 1997 to 700 morphine milligram equivalents in 2007, an increase of more than 600%.1
IMPLICATIONS FOR TRANSPLANTATION
The most significant barrier to organ transplantation is the shortage of available organs. In 2006, there were over 95 000 people on organ transplant waiting lists and over 6300 deaths of patients who were unable to receive an organ.32 Now, the opioid overdose epidemic is changing the landscape. A recent New York Times article highlighted information from the New England Organ Bank, in which patients who died of an overdose provided 27% of the region’s donations in 2016, up from 4% in 2010.33 The article described that nationwide, about 12% of recent donations have come from drug overdose victims, more than double the rate in 2010.
According to the Organ Procurement and Transplantation Network, the total number of organ donors increased from 8203 to 15 070 during the last 20 years (an 84% increase).34 During the same period, the number of donors who died from drug overdoses increased from 29 to 848 (a staggering 2924% increase) (Figure 1). OPTN data from 2016 indicate that the annual total of donors will surpass that of 2015 by far with 1113 additional donors until November 30. Donors who died from drug overdose are more likely to be younger (median age, 31 years) than donors with a cause of death related to cardiovascular disease (median age, 47 years) or stroke (median age, 52 years).35 Moreover, donors who die from drug overdose typically have no medical comorbidities that would preclude donation, thus making them good candidates for donation.
FIGURE 1.
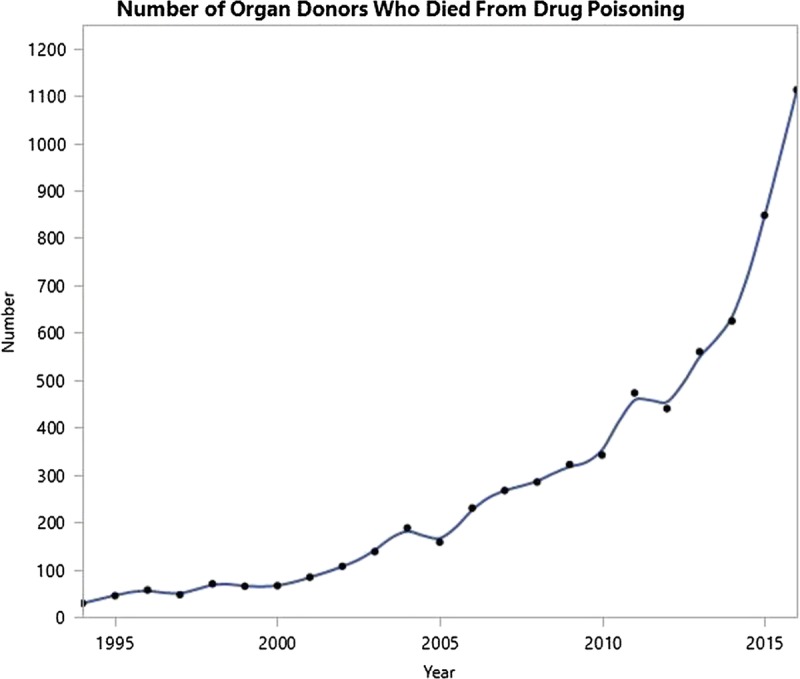
Number of organ donors who died from drug poisoning, January 1, 1994, to November 30, 2016. Source: Organ Procurement and Transplantation Network.
However, due to concerns over disease transmission (HIV, hepatitis B, and hepatitis C virus), these donors are underused by the transplant community. A recent study by Volk and colleagues36 demonstrated that the Public Health Service (PHS) Increased Risk label is associated with nonutilization of hundreds of organs per year even though the risk of disease transmission is approximately only 1 in 1000. Utilization rates were lower for donors designated as PHS positive as compared with PHS negative, for all organs except livers. Clearly, labeling organs as increased risk may result in wastage of otherwise standard kidneys.37
It is evident that there continues to be fear of increased disease transmission on the part of patients as well as treating physicians, even though these instances are rare and transplant centers can intervene with newer treatments. The use of nucleic acid testing provides a detection of new infections by 7 days. With modern screening and testing techniques, the risk of missed HIV and Hepatitis C diagnoses per 100 000 person years is 2.7 and 10.5, respectively.38 To put this in perspective, the risk of dying on the waitlist while waiting for a transplant is far greater than the risk of accepting an organ from an increased risk donor.34 To further improve organ utilization from donors whose cause of death is a drug overdose, it is imperative to educate patients and transplant center staff to the benefits as well as the low risk of disease transmission.
FUTURE PERSPECTIVE
The U.S. Surgeon General has made a call to “Turn the Tide” against the opioid epidemic, and has released several resources, including a comprehensive report about opioids and an online pledge that prescribers can take to indicate their willingness to prescribe opioids more carefully.39 Efforts like these, combined with the release of guidelines from the CDC and other groups, public policy interventions such as opioid laws and prescription drug monitoring programs, in addition to general education on the issue hopefully mean that a new generation of people will have less risk of becoming addicted to opioids. However, for the foreseeable future, the current population will continue to struggle with opioid use and its associated overdose deaths, with accompanying increases in available transplantable organs.
For the transplant community, it will be critical to comprehend the balance between “real risks” and “real benefits” in using increased risk donors in a sensitive but effective way. The finding that livers are the only organs from increased risk donors utilized in the same frequency as organs from non–high-risk donors indicates that the liver transplant community may be more familiar with this risk assessment, not least through a more direct exposure of novel Hepatitis C treatments. For the overall transplant community and the supervising agencies, it will be important to understand that the real risks of staying on dialysis or missing the opportunity to receive a life-saving liver, heart, or lung transplant will outweigh the risk of disease transmission by far.
Footnotes
The authors declare no funding or conflicts of interest.
Correspondence: Scott G. Weiner, MD, MPH, Department of Emergency Medicine Brigham and Women’s Hospital 75 Francis Street, NH-226 Boston, MA 02115. (sweiner@bwh.harvard.edu).
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC). CDC grand rounds: prescription drug overdoses - a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61:10–3. [PubMed] [Google Scholar]
- 2.Rudd RA, Aleshire N, Zibbell JE. Increases in drug and opioid overdose deaths—United States, 2000-2014 MMWR Morb Mortal Wkly Rep 2016. 641378–82 [DOI] [PubMed] [Google Scholar]
- 3.Ingrahan C. Heroin deaths surpass gun homicides for the first time, CDC data shows Washington Post; December 8, 2016. https://www.washingtonpost.com/news/wonk/wp/2016/12/08/heroin-deaths-surpass-gun-homicides-for-the-first-time-cdc-data-show/?utm_term=.78d08a9f6b74. Accessed January 1, 2017. [Google Scholar]
- 4.CDC. Wide-ranging online data for epidemiologic research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics; 2016. http://wonder.cdc.gov. Published 2016 Accessed January 1, 2017. [Google Scholar]
- 5.National Center for Health Statistics. Mortality in the United States, 2015. https://www.cdc.gov/nchs/products/databriefs/db267.html. Published 2015. Accessed January 1, 2017. [Google Scholar]
- 6.Kaiser Family Foundation. Kaiser Health Tracking Poll: November 2015. http://kff.org/health-reform/poll-finding/kaiser-health-tracking-poll-november-2015/. Published 2015. Accessed January 1, 2017. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Drug Poisoning Mortality: United States, 1999–2014. https://blogs.cdc.gov/nchs-data-visualization/drug-poisoning-mortality/. Accessed January 1, 2017. [Google Scholar]
- 8.Wright ER, Kooreman HE, Greene MS. The iatrogenic epidemic of prescription drug abuse: county-level determinants of opioid availability and abuse Drug Alcohol Depend 2014. 138209–15 [DOI] [PubMed] [Google Scholar]
- 9.Frenk SM, Porter KS, Paulozzi LJ. Prescription opioid analgesic use among adults: United States, 1999–2012. In: NCHS Data Brief. Hyattsville, MD: National Center for Health Statistics; 2015:1–8. [PubMed] [Google Scholar]
- 10.Okie S. A flood of opioids, a rising tide of deaths N Engl J Med 2010. 3631981–5 [DOI] [PubMed] [Google Scholar]
- 11.Chang H, Daubresse M, Kruszewski S. Prevalence and treatment of pain in EDs in the United States, 2000 to 2010 Am J Emerg Med 2014. 32421–31 [DOI] [PubMed] [Google Scholar]
- 12.Daubresse M, Chang H, Yu Y. Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000-2010 Med Care 2013. 51870–878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016 JAMA 2016. 3151624–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manasco AT, Griggs C, Leeds R. Characteristics of state prescription drug monitoring programs: a state-by-state survey Pharmacoepidemiol Drug Saf 2016. 25847–51 [DOI] [PubMed] [Google Scholar]
- 15.The Commonwealth of Massachusetts. An Act relative to substance use, treatment, education and prevention. http://www.massmed.org/advocacy/key-issues/opioid-abuse/conference-committee-report--an-act-relative-to-substance-use,-treatment,-education-and-prevention-(pdf)/. Accessed January 1, 2017. [Google Scholar]
- 16.IMS Institute for Healthcare Informatics. Medicines Use and Spending in the U.S. https://static1.squarespace.com/static/54d50ceee4b05797b34869cf/t/5711197b45bf21650748e8ad/1460738430435/IMS+Health+2015.pdf. Published April 2016. Accessed January 1, 2017. [Google Scholar]
- 17.Kertesz SG. Turning the Tide or Riptide? the Changing Opioid Epidemic. Subst Abus. 2016:1–6. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 18.Jones CM, Logan J, Gladden RM. Vital signs: demographic and substance use trends among heroin users—United States, 2002–2013 MMWR Morb Mortal Wkly Rep 2015. 64719–25 [PMC free article] [PubMed] [Google Scholar]
- 19.Cicero TJ, Ellis MS, Surratt HL. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years JAMA Psychiatry 2014. 71821–6 [DOI] [PubMed] [Google Scholar]
- 20.Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013–2014 MMWR Morb Mortal Wkly Rep 2016. 65837–43 [DOI] [PubMed] [Google Scholar]
- 21.Declaration of Montréal. 2010. http://www.iasp-pain.org/DeclarationofMontreal?navItemNumber=582. Accessed January 1, 2017. [Google Scholar]
- 22.Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States Pain Med 2012. 13150–74 [DOI] [PubMed] [Google Scholar]
- 23.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care J Pain 2009. 101187–204 [DOI] [PubMed] [Google Scholar]
- 24.Cintron A, Morrison RS. Pain and ethnicity in the United States: a systematic review J Palliat Med 2006. 91454–73 [DOI] [PubMed] [Google Scholar]
- 25.Hwang U, Belland LK, Handel DA. Is all pain is treated equally? A multicenter evaluation of acute pain care by age Pain 2014. 1552568–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Department of Veterans Affairs. Pain as the fifth vital sign toolkit. https://www.va.gov/PAINMANAGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Published October 2000. Accessed January 1, 2017. [Google Scholar]
- 27.U.S. Department of Health & Human Services. HHS announces new actions to combat opioid epidemic. https://www.hhs.gov/about/news/2016/07/06/hhs-announces-new-actions-combat-opioid-epidemic.html. Published July 2016. Accessed January 1, 2017. [Google Scholar]
- 28.Hoffman J, Tavernise S. Vexing Question on Patient Surveys: Did We Ease Your Pain? New York Times. http://www.nytimes.com/2016/08/05/health/pain-treatment-hospitals-emergency-rooms-surveys.html?_r=0. Published August 2016. Accessed January 1, 2017. [Google Scholar]
- 29.Meier B. Pain Killer: A “Wonder” Drug’s Trail of Addiction and Death. 1st ed. Emmaus, Pa: Rodale Books; 2003. [Google Scholar]
- 30.Portenoy RK, Foley KM. Chronic use of opioid analgesics in non-malignant pain: report of 38 cases Pain 1986. 25171–86 [DOI] [PubMed] [Google Scholar]
- 31.Van Zee A. The promotion and marketing of oxycontin: commercial triumph, public health tragedy Am J Public Health 2009. 99221–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abouna GM. Organ shortage crisis: problems and possible solutions Transplant Proc 2008. 4034–8 [DOI] [PubMed] [Google Scholar]
- 33.Seelye KQ. As Drug Deaths Soar, a Silver Lining for Transplant Patients. New York Times, October 6, 2016. http://www.nytimes.com/2016/10/06/us/as-drug-deaths-soar-a-silver-lining-for-organ-transplant-patients.html. Accessed January 1, 2017. [Google Scholar]
- 34.Organ Procurement and Transplantation Network. http://optn.transplant.hrsa.gov/. Accessed January 1, 2017. [Google Scholar]
- 35.Goldberg DS, Blumberg E, McCauley M. Improving organ utilization to help overcome the tragedies of the opioid epidemic Am J Transplant 2016. 162836–2841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Volk M, Wilk A, Wolfe C, et al. The PHS Increased Risk label is associated with non-utilization of hundreds of organs per year [Abstract]. Am J Transplantation. 2016;16(suppl 3). [DOI] [PubMed] [Google Scholar]
- 37.Duan KI, Englesbe MJ, Volk ML. Centers for Disease Control High Risk Donors and kidney utilization Am J Transplant 2010. 10416–420 [DOI] [PubMed] [Google Scholar]
- 38.Ellingson K, Seem D, Nowicki M. Estimated risk of human immunodeficiency virus and hepatitis C virus infection among potential organ donors from 17 organ procurement organizations in the United States Am J Transplant 2011. 111201–1208 [DOI] [PubMed] [Google Scholar]
- 39.U.S. Surgeon General. Turn the Tide. http://turnthetiderx.org/. Accessed January 1, 2017. [Google Scholar]


