Abstract
Background
People living with HIV/AIDS (PLWHA) are a vulnerable group who experience multiple physiological and psychological symptoms. A better understanding of unmet symptom management needs will allow researchers to design interventions that are more reflective of deficits in care and more effective at improving patient care. Few studies have focused on unmet needs for symptom management in PLWHA particularly in China. Factors influencing Chinese PLWHA symptom management needs are rarely discussed.
Aim
The purpose of this study was to investigate the unmet needs for symptom management of PLWHA and how their symptom burden, HIV perceived stigma, and self-management capacity contributes to HIV-related self-management practices in Shanghai, China.
Design
Study participants were recruited from the outpatient and inpatient HIV/AIDS wards in an infectious hospital in Shanghai, China. Self-administered questionnaires were implemented and medical charts were reviewed.
Results
A total of 367 participants was recruited from April to September 2017. The results show that 53.1% (195 of 367) of participants presented at least one unmet symptom management need and that symptom burden, as well as perceived stigma, reduced self-management capacity, and no employment significantly affected unmet symptom management needs.
Conclusion
The findings indicate that there is room for improvement in symptom management for Chinese PLWHA. Culturally appropriate interventions focusing on improving symptom burden, decreasing HIV perceived stigma, and enhancing self-management capacity can enhance symptom management in this population.
Keywords: HIV/AIDS, Symptom management, Symptom burden, China
Highlights
-
•
More than half (53.1%) of Chinese PLWHA had at least one unmet symptom management need.
1. Introduction
HIV is a significant health issue in China (Lo, 2018). According to the China CDC, the total number of people living with HIV/AIDS (PLWHA) was 849,602 as of September 2018 (China CDC, 2018). Current reports of the HIV epidemic in Shanghai, China estimate that approximately 29,463 people were infected with HIV at the end of November 2018 (Shanghai Municipal Health Commission, 2018). HIV-related expenses are costly from both an economic and human suffering standpoint (Liu et al., 2018).
2. Background
A symptom is defined as an objective perception of a physical, psychological, or social condition that may indicate a condition of disease (Hegyvary, 1991). For PLWHA, antiretroviral therapy (ART) has changed HIV to a chronic and manageable disease (Martinez et al., 2012). However, compared to other chronic illnesses (e.g., diabetes or hypertension), PLWHA are still a vulnerable group who experience multiple physiological and psychological symptoms resulting from the disease itself, from side effects of ART, and from other medications related to comorbidities (Lalanne et al., 2015; Roman & Chou, 2011).
Studies found that many PLWHA (30%) presented with high symptom burden, with seven or more symptoms at the same time being common (Wilson et al., 2016). Fatigue, fever, headache, nausea/vomiting, diarrhea, weight loss, pruritus/itching, chills, rash, sweat, dyspnea, cough, muscle pain/joint pain, numbness/pain in feet, and poor sleep were among the most prevalent and distressing physical symptoms for PLWHA (McGowan et al., 2014; Peltzer, 2013; Wakeham et al., 2010; Wilson et al., 2016). In addition, PLWHA also deal with burden related to psychosocial problems. Studies have shown that sleep disturbances and fatigue were one of the major unpleasant symptoms among Chinese PLWHA (Chen et al., 2013; Zhu et al., 2019). Further, Chinese PLWHA often face mental health crises after receiving their HIV diagnosis (Chen et al., 2011).
Fear, anxiety, sadness, and depression are common problems among PLWHA, and some of these symptoms are more prominent in the later stages of illness (Chu & Selwyn, 2011). Not surprisingly, the prevalence of depression was 46.5% among HIV-positive men who have sex with men (MSM) in Shanghai, China (Pan et al., 2017). Worrying about their health condition was one of the major symptoms PLWHA associated with depression, followed by feeling unhopeful about the future (Liu et al., 2018).
Untreated symptoms are likely to impact activities of daily living and can lead to poor quality of life and nonadherence to HIV regimens (Baran et al., 2014; Gay et al., 2011). Therefore, effective symptom management is essential for HIV-positive individuals to maintain their quality of life (Holzemer, 2002; Tsai, Hsiung, & Holzemer, 2002). A recent meta-analysis identified that self-management of pain and symptoms (such as fatigue, headache, etc.) in PLWHA is still under development (Nkhoma et al., 2018), which implies that PLWHA have a high need for effective self-management interventions.
Many symptom management interventions offered by healthcare providers (HCPs) might not be the need of PLWHA (Simpson et al., 2013). Therefore, self-report is the “gold standard” for understanding the symptom experience in PLWHA (Simpson et al., 2013; Walling et al., 2016). Thus, HCPs can solve the unpleasant symptoms on site after interviewed with PLWHA.
Unmet needs are defined as the differences between those services judged necessary and those services actually being received (Carr & Wolfe, 1976). Unmet need for symptom management is defined as the descriptions given by patients who have unmet needs in the current management of symptoms (Hwang et al., 2004). Measurement of patient-reported unmet needs for symptom management will reflecting the deficits in HIV care (Snyder et al., 2010; Walling et al., 2016). Thus, the level of unmet needs reported is an important indicator of whether inconsistences exist between patients' needs and HCP’ perceptions of the level of care they are providing.
The morbidities and distress resulting from HIV-related symptoms can lead to unmet needs across a range of domains. Current studies focus on the need for symptom management in the HIV-positive population; however, they do not specifically discuss the unmet symptom management needs of PLWHA (Chen et al., 2013; Fu, 2014; Shadloo et al., 2018). Studies have focused on descriptions of unmet symptom management needs in cancer (Walling et al., 2016) and end-of-life care (Khandelwal et al., 2017). One study found that psychiatric disorders were found in 50.2% for PLWHA in Iran and only 22% had received minimally adequate treatment (Shadloo et al., 2018). In China, one study has shown that the major needs of symptom management were rash, shortness of breath, and blurred vision (Fu, 2014). Chen, Shiu, et al. (2013) have also reported that Chinese HIV-positive individuals experienced digestive discomfort, skin rashes, numbness, memory loss, nightmares, and dizziness, along with depressive mood.
An understanding of the prevalence and presence of symptoms is important to guide and design an effective symptom management in PLWHA. Therefore, in this paper, we investigate the prevalence and potential factors of Chinese PLWHA self-perceived unmet needs and their current HIV-related symptoms.
3. Theoretical framework
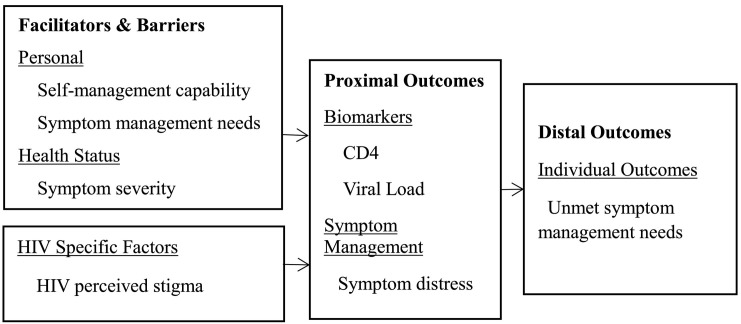
Based on the HIV-related self- and family management theoretical framework (Wang, Chen, et al., 2016), we revised the model to more closely fit the current study (see Fig. 1 ). This framework highlights the facilitators of and barriers to the PLWHA, as well as proximal and distal outcomes. We added potential HIV-related factors (e.g., HIV perceived stigma) as it was affected by unmet symptom management needs.
Fig. 1.
The modified symptom-management framework in the HIV-positive Chinese individuals.
Symptoms and stresses vary in PLWHA. For instance, while some individuals have more issues with disclosing their HIV status, others report health access difficulties (Wang, Chen, et al., 2016). In addition, some PLWHA have sought more family and social support while living with HIV (MacCarthy et al., 2018; Wang, Chen, et al., 2016). Particularly, PLWHA have reported higher needs when the symptoms were more severe (Osse, Vernooij-Dassen, Schade, & Grol, 2007).
In the current study, we hypothesized that personal factors (self-management capability and symptom management needs), health status (symptom severity), and HIV specific factors (HIV perceived stigma) will affect proximal outcome (biological outcome and symptom management) and distal outcome (unmet symptom management needs).
4. Methods
4.1. Study site
This cross-sectional study was conducted at Shanghai Public Health Clinical Center (SPHCC) in Shanghai, China from April to September 2017. SPHCC is an infectious disease hospital focusing on treating all the infectious diseases, including severe acute respiratory syndrome (SARS), HIV/AIDS, hepatitis B and C, and other sexually transmitted diseases. Patients with comorbidities and any infectious diseases are treated in the tertiary setting (Chen et al., 2010). As such, SPHCC is one of the preeminent infectious disease hospitals in Southern China. All study procedures were reviewed and approved by the institutional review board of the School of Nursing, Fudan University.
4.2. Sample
Study participants were recruited from the outpatient or inpatient wards with confirmed HIV diagnosis. Eligible participants were required to be: (a) HIV diagnosed, (b) receiving care at SPHCC, (c) able to read and communicate in Chinese/Mandarin and (d) aged over 18. Patients who were unable to complete the questionnaire, had other chronic diseases (such as heart disease, diabetes, tuberculosis) or severe cognitive impairment were excluded.
4.3. Measurement
Symptom management was assessed using a self-administered 49-item questionnaire as the outcome measure. This measure has been widely used and adapted from a pre-established survey (Holzemer, Hudson, Kirksey, Hamilton, & Bakken, 2001; Justice et al., 2001). Symptoms that were highly related to HIV (e.g., fatigue, fever, rash, diarrhea, and depression) were included in the questionnaire. Patients indicate for the previous four weeks what symptoms were present along with the symptom severity. If a symptom was present, then participants rate the degree of the need for symptom management (0 = No demand, 1 = Weak demand, 2 = Moderate demand, 3 = Strong demand). They then answer a follow-up question on whether their needs have been met (Yes/No/Not asked). Sample questions are: During the last 4 weeks, did you need help from HCPs to relieve your symptom of rash? If the answer is yes, then, the follow-up question is: During last 4 weeks, did you get the help from the HCP that you asked for? Patients who responded no to the latter question are identified as having an unmet need for that symptom (score = 1). The scores of the total unmet needs for symptom management range from 0 to 49, with higher scores indicating more unmet needs. The instrument has been shown to have good expert validity with a content validity index (CVI) of 0.918 and Cronbach's alpha coefficients of the needs and unmet needs domains at 0.968 and 0.954, respectively (Zhu, Hu, Guo, & Williams, 2019).
Symptom burden was adapted from a pre-established survey and assessed via paper-and-pencil questionnaire (Holzemer et al., 2001; Justice et al., 2001). The symptom burden questionnaire consisted of 23 somatic symptoms and 26 psychological symptoms. Patients were asked to rate each of the 49 items (a) the severity of symptoms on a scale from 0 (not at all) to 3 (very severe), and (b) how much the symptom distressed him or her on a scale from 0 (not at all) to 3 (very much) during the preceding 4 weeks. The total score was obtained by calculating a mean of the responses to all the items. Higher mean scores indicate more severe symptoms.
HIV perceived stigma was assessed using the Expanded Everyday Discrimination Scale (Williams et al., 2008), as described in a related paper (Zhu, Hu, Guo, & Williams, 2019). With the permission of the original author, we had the scale translated into Chinese by two experts on the current research team then back-translated by another two experts in English. Finally, the four experts reviewed the Chinese version and the English version for its equivalence to the original scale. The scale included 10 items and responses ranged from “almost every day” (1) to “never” (4). The score range was 10–40, with the higher score representing lower perceived stigma. The instrument showed good expert validity (CVR = 1.00), and Cronbach's alpha coefficient was 0.91 in the present study.
Self-management capacity was assessed by a single item: What do you think of your ability to manage your own health? The answer was rated on a Likert scale ranging from very good (1) to very bad (5). The higher the score, the lower the self-management capacity.
Demographic and clinical-related variables included gender, age, marital status, education level, current employment status, time since HIV diagnosis, ART use status, latest CD4+ T-cell count, and latest viral load (see Table 1 ).
Table 1.
Participant characteristics and unmet needs for symptom management.
| Variables | Classification | N (%) | Unmet needs |
U or H (p) |
|---|---|---|---|---|
| Mean (SD) | ||||
| Age(y) (Mean = 38.6) | 18–30 | 102 (27.8) | 3.14 (5.34) | 2.167 (.539) |
| 31–40 | 131 (35.7) | 2.67 (5.00) | ||
| 41–50 | 72 (19.6) | 3.46 (5.80) | ||
| 51–78 | 62 (16.9) | 3.52 (5.82) | ||
| Gender | Male | 335 (91.3) | 3.19 (5.51) | 4941.000 (.439) |
| Female | 32 (8.7) | 2.13 (3.76) | ||
| Marital status | Married | 116 (31.6) | 2.81 (4.13) | 14,343.500 (.810) |
| Other (single, divorced, unknown) | 251 (68.4) | 3.23 (5.88) | ||
| Educational level | Elementary school | 25 (6.8) | 3.08 (3.63) | 2.528 (.470) |
| Middle school | 55 (15.0) | 3.38 (4.92) | ||
| High school | 70 (19.1) | 2.70 (5.22) | ||
| College or above | 217 (59.1) | 3.16 (5.74) | ||
| Current employment status | Yes | 163 (44.4) | 2.23(3.83) | 14,494.000 (.026)⁎ |
| No | 204 (55.6) | 3.79 (6.29) | ||
| Ward | Inpatient | 198 (54.0) | 3.33 (5.61) | 15,284.500 (.131) |
| Outpatient | 169 (46.0) | 2.83 (5.13) | ||
| Months HIV positive (mean = 28) | 1–6 | 141 (38.4) | 3.11 (4.66) | 1.736 (.629) |
| 7–18 | 57 (15.5) | 3.19 (6.71) | ||
| 19–36 | 59 (16.1) | 3.07 (5.90) | ||
| 37–286 | 110 (30.0) | 3.05 (5.28) | ||
| Taking ART | Yes | 307 (83.7) | 3.16 (5.54) | 9009.000 (.777) |
| No | 60 (16.3) | 2.77 (4.55) | ||
| Viral Load (copies/ml) | 0–499① | 126 (34.2) | 2.69 (4.79) | 51.959 (.000)⁎ ①,② < ③,④ |
| 500 and above② | 32 (8.7) | 3.00 (4.82) | ||
| Do not know③ | 77 (20.9) | 5.79 (6.59) | ||
| Never tested④ | 45 (12.2) | 5.69 (6.78) | ||
| CD4 count (cells/mm3) (Mean = 279) | 0–199 | 128 (34.8) | 2.78 (4.46) | 10.339 (0.070) |
| 200–299 | 56 (15.2) | 5.20 (8.22) | ||
| 300–399 | 40 (10.9) | 2.48 (4.12) | ||
| 400–499 | 30 (8.2) | 2.67 (5.75) | ||
| 500 and above | 47 (12.8) | 2.70 (5.03) |
Total N = 367, including missing data; p < .05.
4.4. Sample size
The sample size was determined according to the item numbers of the main scale being included in the survey. It was proposed that the sample size should range from 5 to 10 times the item numbers (Wu, 2010). Given that the main instrument symptom management for PLWHA applied in the survey contained 49 items, it was estimated that 350 participants would be enough.
4.5. Data collection
Potential participants were recruited from both the inpatient and outpatient wards at SPHCC. Study participants were informed of the study to ensure that participation was voluntary. After researchers securing study consent, all participants received a copy of their signed consent form. Participants received an electronic pill dispenser and an HIV care pamphlet after they completed the survey as the appreciation. The study surveys were completed within 20 min on average.
4.6. Data analysis
Data analysis was performed using Statistical Package for Social Sciences (SPSS), version 17.0. Means and standard deviations (SDs) were presented for continuous variables (e.g., age, symptom burden, HIV perceived stigma, self-management capability). Frequency and percentage were presented for categorical variables (e.g., gender, marital status, educational level, and unmet symptom management needs). Differences between unmet symptom management needs and demographic variables were analyzed. All assumptions for each statistical test were checked. Since those variables did not meet the assumptions for t-test or ANOVA, nonparametric alternatives (Kruskal-Wallis test, Mann-Whitney test) were used.
Pearson's correlation coefficient tests were used in the analysis of the correlation between unmet symptom management needs and symptom burden, HIV perceived stigma, and self-management capability. Multiple regression analysis was used to determine the unmet symptom management needs predicting factors of PLWHA by analyzing the significant independent variables (current employment status, recent viral load, symptom burden, HIV perceived stigma, and self-management capability) with unmet symptom management needs as a dependent variable. An initial investigation was conducted to ensure the non-violation of the regression assumptions of multicollinearity, normality, linearity, and homoscedasticity. Recent viral loads were dichotomized into two categories (viral load known vs unknown). Statistical significance was set at p ≤ .05.
5. Results
5.1. Characteristics of participants
A total of 450 eligible participants was contacted and 390 were recruited and completed the study. Data for 367 participants was analyzed, with an acceptance rate and validity rate of 87% and 94%, respectively. The mean age was 38.6 years and ranged from 18 to 78 years old. Most of the participants were male (91%) and had attended at least middle school or higher (34% middle or high school, 59% college or above). More than half (68%) of them were not married. The majority of participants were unemployed (56%), and from the inpatient (54%) ward. A large majority (84%) were currently taking ART. The mean of diagnosis time was 28 months, with 279 cells/mm3 for the latest CD4 count. More than one-third (34%) of the participants had their most recent HIV viral load undetectable at less than 500 copies/ml blood (see Table 1). In addition, mean score of HIV perceived stigma was 33.38 (SD: 7.29) and self-management capacity was 2.81 (SD: 1.16).
5.2. Symptom burden
Cronbach's alpha coefficient was 0.98 in the present study. Mean score for symptom burden was 0.29 (SD: 0.40) out of a total possible score of 3. Table 2 shows the rank order of individual symptom burden. Among the individual symptoms, fatigue had the highest score for symptom severity, followed by insomnia/abnormal dreams, fever, unwanted weight loss, and decreased appetite. For symptom distress, fatigue was most distressing, followed by insomnia/abnormal dreams, fever, decreased appetite, and unwanted weight loss.
Table 2.
Ten most severe, distress symptoms and symptom management needs reported by study participants.
| Rank | Symptom burden |
Symptom management needsc | |
|---|---|---|---|
| Severity (mean ± SD) | Distress (mean ± SD)c | ||
| 1 | Fatiguea (0.76 ± 0.93) | Fatiguea (0.58 ± 0.94) | Fatiguea (0.93 ± 1.23) |
| 2 | Insomnia/abnormal dreamsa (0.70 ± 0.96) | Insomnia/abnormal dreamsa (0.57 ± 0.91) | Fevera (0.83 ± 1.15) |
| 3 | Fevera (0.69 ± 1.03) | Fevera (0.56 ± 0.97) | Insomnia/abnormal dreamsa (0.81 ± 1.08) |
| 4 | Unwanted weight lossa (0.59 ± 0.99) | Decreased appetitea (0.47 ± 0.90) | Unwanted weight lossa (0.76 ± 1.20) |
| 5 | Decreased appetitea (0.57 ± 0.94) | Unwanted weight lossa (0.41 ± 0.86) | Decreased appetitea (0.72 ± 1.12) |
| 6 | Rasha (0.48 ± 0.82) | Little interest in doing thingsb (0.37 ± 0.77) | Blurry visiona (0.68 ± 1.12) |
| 7 | Feeling stressb (0.46 ± 0.85) | Feeling stressb (0.37 ± 0.81) | Difficulty concentratinga (0.68 ± 1.11) |
| 8 | Cougha (0.44 ± 0.81) | Feeling downb (0.37 ± 0.81) | Rasha (0.65 ± 1.04) |
| 9 | Memory lossa (0.43 ± 0.72) | Cougha (0.37 ± 0.80) | Memory lossa (0.64 ± 1.08) |
| 10 | Little interest in doing thingsb (0.42 ± 0.77) | Rasha (0.35 ± 0.77) | Feeling stressb (0.61 ± 1.03) |
Somatic symptoms.
Psychological symptoms.
Possible range: 0–3.
5.3. Symptom management needs and unmet needs
Table 2 outlines the symptom management needs for PLWHA. In general, the ten top-scoring symptom management needs were mostly related to somatic symptoms like fatigue, fever, insomnia/abnormal dreams, unwanted weight loss, blurred vision, difficulty concentrating, rash, memory loss and diarrhea, with the exception of “feeling stress,” which was a psychological symptom. For this study, Cronbach's alpha values of the needs and unmet needs domains were 0.98 and 0.92, respectively. The mean score of total unmet symptom management needs was 3.10 (SD: 5.39, Range: 0–38). More than half (53%; N = 195) had at least one unmet need for symptom management in the 4 weeks before the interview. Unmet needs ranged from 2.5% for hump on back of neck/shoulders to 15% for fatigue. Fatigue, feeling stress, feeling down, insomnia/abnormal dreams, and feeling fearful were among the most common symptoms to result in unmet symptom management need (Table 3 ).
Table 3.
Ten most frequently reported unmet needs for symptom management.
| Rank | Item | Unmet need |
|
|---|---|---|---|
| N | %c | ||
| 1 | Fatiguea | 54 | 14.7 |
| 2 | Feeling stressb | 42 | 11.4 |
| 3 | Feeling downb | 41 | 11.2 |
| 4 | Insomnia/abnormal dreamsa | 38 | 10.4 |
| 5 | Feeling fearfulb | 38 | 10.4 |
| 6 | Little interest in doing thingsb | 34 | 9.3 |
| 7 | Feeling nervousb | 34 | 9.3 |
| 8 | Decreased appetitea | 33 | 9.0 |
| 9 | Self-abasementb | 31 | 8.4 |
| 10 | Muscle/joint paina | 29 | 7.9 |
Somatic symptoms.
Psychological symptom.
Percentage of participants reporting each symptom.
Significant differences for unmet needs were found in current employment status (Mann-Whitney U = 14,494.000, p = .026) and viral load (Kruskal-Wallis H = 51.959, p < .01). Being unemployed was associated with a higher likelihood of reporting unmet needs; post hoc tests revealed that PLWHA with recent viral load undetectable or barely detectable had a lower likelihood of reporting unmet needs than those with viral load untested or “do not know.” Detailed information is presented in Table 1. Symptom burden (r = 0.451, p < .01), HIV perceived stigma (r = −0.251, p < .01), and self-management capacity (r = 0.302, p < .01) were determined to be significantly associated with unmet symptom management needs.
5.4. Predictors of unmet symptom management needs
The combination of the variables showed that symptom burden, HIV perceived stigma, self-management capacity, and current employment status were significant predictors of overall unmet symptom management needs of PLWHA and explained 38% of the total variance (F = 41.545, p < .001). Symptom burden was the most significant predictor, and separately accounted for 29% of variance among unmet symptom management needs, followed by HIV perceived stigma (3.2%), self-management capacity (2.8%), and current employment status (2.7%). Beta weights showed that more symptom burden, more HIV perceived stigma, lower self-management capacity, and being unemployed predicted higher unmet symptom management needs (see Table 4 ).
Table 4.
Factors associated with unmet symptom management needs.
| Predicting variables | Unstandardized coefficient β | Standardized coefficient β | t-Test | p value | Collinearity statistics |
R2 change | F | |
|---|---|---|---|---|---|---|---|---|
| Tolerance | VIF | |||||||
| (Constant) | −0.041 | −0.021 | .983 | 41.545 | ||||
| Symptom burden | 6.597 | 0.447 | 8.513 | .000⁎ | 0.824 | 1.214 | 0.290 | |
| HIV perceived stigma | −0.124 | −0.156 | −3.618 | .002⁎ | 0.929 | 1.076 | 0.032 | |
| Self-management capacity | 0.925 | 0.189 | 3.543 | .000⁎ | 0.800 | 1.249 | 0.028 | |
| Current employment status | 2.302 | 0.193 | 3.988 | .000⁎ | 0.965 | 1.036 | 0.027 | |
R: 0.614; R2:0.377; Adjusted R2:0.368; VIF: Variance inflation factor.
p < .05.
6. Discussion
This paper presents the factors influencing unmet symptom management needs in PLWHA in Shanghai, China. The overall unmet symptom management needs score (3 out of 49) indicated that PLWHA's unmet needs for symptom management were relatively low. However, the unmet needs ranged from 3% for hump on back of neck/shoulders to 15% for fatigue. These results reflect the wide variation in unmet symptom management needs for PLWHA. Also, the study participants reported a high level of symptom burden and HIV-related stigma and low level of self-management capacity. In addition, for those who are currently unemployed, they often complained of high levels of unmet symptom management needs.
In this study, more than half (53%) of PLWHA reported at least one unmet symptom management need, which was significantly higher than for other studies. In cancer cases, only 15% (791 of 5422) of them complained of one or more unmet needs require for symptom management (Walling et al., 2016). However, it is worth noting that the above comparison comes from different assessment tools used in different settings and that the healthcare services studied were focused on symptoms experienced by participants in Western countries. Contrast this with our study, which examined patients receiving HIV care in China.
In addition, this study indicated that fatigue was one the major symptoms in both frequency and severity. Fatigue is among the most prevalent and distressing of symptoms among people living with many chronic illnesses (Solano, Gomes, & Higginson, 2006), including PLWHA in China (Barroso & Voss, 2013; Fan, Luo, Sun, Yang, & Yu, 2011; Leserman, Barroso, Pence, Salahuddin, & Harmon, 2008). Furthermore, fatigue was associated with worse health status (Dacosta Dibonaventura, Gupta, Cho, & Mrus, 2012) and had a negative impact on ART adherence (Gay et al., 2011). A study conducted with 190 newly diagnosed PLWHA in two hospitals in Beijing found that 42% patients request more medical attention for fatigue (Cai, 2017). However, fatigue is often overlooked and gets less attention from HCPs (Chen, Lee, et al., 2013). All of these studies strongly suggested that HCP in China should deliver a feasible and individually tailored intervention to combat fatigue, more rest or increasing exercise level should be considered for different individuals.
Also, in this study, the top 10 most needed items were all related to somatic symptoms, except for one related to mental health. This echoed previously observed phenomenon that many Chinese people tend to keep their mental discomfort to themselves and rarely talk about the issues with others (Chen, Shiu, et al., 2013; Wang et al., 2016; Zhou & Hearst, 2016). Also, it might because in this study, more than half (54%) of the study participants were inpatient, which means that they were in need for the physical symptoms management. Other possibilities are that many PLWHA did not seek help for psychological symptoms because mental discomforts are highly stigmatized in Chinese society; therefore, they did not seek treatment for their psychological distress (Kagee & Martin, 2010). Furthermore, HIV is highly stigmatized in China (Burki, 2011), PLWHA are hesitate to seek psychosocial support generally (Yang et al., 2015).
Currently, there are no providers on site at the Shanghai infectious disease hospital to provide mental health assessment and treatment for PLWHA. This study highlights the need for improvement of mental health treatment and care for PLWHA. Several strategies can be used to improve mental health care for PLWHA. For example, special training should be provided for HCPs (nurses, social workers) who will be working with the PLWHA in order to help them identify mental health symptoms and referred to psychologist and/or psychiatrist. Also, educate PLWHA and general population to understand mental health is one parts of the overall health.
This study showed that symptom burden was a significant predictor of unmet symptom management needs, which is similar to several other publications (Cheng, Wong, & Koh, 2016; Li, Lin, Zhou, Xu, & Xu, 2019; Lo, Yates, & Chan, 2018). In Chinese culture, patients tend to trust advice coming only from their primary physicians (Chen et al., 2010). However, physicians often do not focus on educating patients with chronic diseases in self-management techniques. Nurses were the HCPs who could and should focus on assisting the unmet symptom needs of PLWHAs to perform adequate self-management.
In a collective culture like China's, nurses should aware of the social norms and how that can enhance self-management in PLWHA (Wang, Chen, et al., 2016). In addition, there are expectation gaps between HCPs and PLWHA. Studies reported that PLWHA expectation of services and the actual experience of services can be quite different (Norberg et al., 2019). In China, studies have shown that even when physicians provide an acceptable level of care to PLWHA, PLWHA may expect more and better care in various aspects, e.g., mental health (Chen et al., 2010).
In this study, symptom burden (29%) was the strongest factor predicting unmet needs. As shown in our results (Table 2), participants reported fatigue, insomnia, fever, unwanted weight loss, and decreased appetite. These physical symptoms can lead to mental distress (Chen, Shiu, et al., 2013). Taken together, the symptom burden can increase unmet needs in symptom management. These findings suggest the urgent need to design a culturally appropriate intervention to decrease symptom burden.
In this study, HIV perceived stigma also predicted unmet symptom management needs. When some HCPs mistreated PLWHA by categorizing them as “contagious,” PLWHA were discouraged from returning to those unfriendly providers (Alexandra, Brewington, Kathryn, Hayness, & Zaller, 2017). Also, perceived stigma can discourage them from seeking healthcare services and can delay their disclosure of their HIV status to HCP and their family members (Zhang, Miege, & Zhang, 2011). Social stigma especially is a barrier to seeking healthcare in the MSM population (Pilgrim et al., 2019). Thus, intervention to decrease HIV-related stigma in the society is urgent. While HCP delivering care to PLWHA, HCP should also use motivate interview skills to decrease stigma in PLWHA. Surveys assessing personal values regarding infectious disease, and especially HIV, should be conducted by all HCPs. Understanding HCPs' attitude toward PLWHA is key to providing quality care in this population. Those providers who are not perceived as kind and caring by PLWHA should be replaced.
In this paper, we found that self-management capacity was also associated with unmet symptom management needs. Positive relationships with HCP enhance self-management capacity, leading to better ART adherence and consequently, enhanced CD4 counts and stronger immune function. As a result of improved relationships PLWHA experience fewer symptoms and may not need additional care (Chen et al., 2018). Effective self-management is considered critical to quality of life (Chen, Shi, & Li, 2013). Previous research reports that self-management interventions are effective at improving PLWHA's pain and physical symptoms (Millard et al., 2016; Nkhoma, Seymour, & Arthur, 2015). However, with multiple comorbidities, PLWHA will need more assistance in keeping up all the self-management strategies (Coventry, Fisher, Kenning, Bee, & Bower, 2014). Therefore, HCPs should pay more attention to how patients to manage their unpleasant symptoms (Wang, Chen, et al., 2016).
Finally, in this paper, current PLWHA employment status also predicted unmet symptom management needs. That said, unemployed patients were more likely to have unmet needs for self-care. One study reported a similar result, showing that not being employed was associated with HIV-related symptom burden (Peltzer, 2013). It is possible that having a job can distract PLWHA from focusing on unpleasant symptoms. Therefore, assisting stable PLWHA to participate in more social activities might distract their attention from unpleasant symptoms.
7. Limitations
There are several limitations in this study. First, this is a cross-sectional study, which could carry result bias. Longitudinal research is thus needed to determine causal relationships. Second, most of the study participants were male. Therefore, we cannot assume HIV-positive women experiencing the similar symptoms burden. Third, this study was conducted in a metropolitan area in China, where patients have better access to healthcare services compared to PLWHA in more resourced-limited areas. Therefore, the results should not be generalized to other geographic areas in China. Fourth, symptom burden, current employment status, self-management capacity, and HIV perceived stigma explained only 38% of the total variance in unmet symptom management needs. The unexplained variance of the unmet needs for future studies to go beyond the factors investigated in the current project. Fifth, since our study only investigated from patients point, we suggest future research to study HCP’ attitude and behavior toward PLWHA's unmet symptom management needs.
8. Conclusion
Despite the limitations, this study presented several significant factors related to unmet needs for symptom management of PLWHA. We found that symptom burden, HIV perceived stigma, self-management capacity, and current employment status were significant predictors of overall symptom management unmet needs. To minimize unmet symptom management needs, future interventions should focus on improving symptom burden, decreasing HIV perceived stigma, and increasing self-management capacity. The study findings highlight that PLWHA experienced more unmet psychological symptom management needs in Shanghai, China. Therefore, it is urgent to tackle the barriers that influence PLWHA's behavior toward their psychological symptom management. Besides, it is necessary to train HCPs who are working with PLWHA on identification of mental health symptoms and to refer PLWHA to mental health care providers. With better understanding of PLWHA's unmet symptom management needs, HCP can design a tailored intervention for PLWHA. In addition, considering the long-term and the chronic nature of HIV infection, further study should consider assessing other potential factors such as social support (family, HCPs).
9. Relevance to clinical practice
Unmet symptom management needs can negatively impact PLWHA's ability to cope and manage their illness, as well as limit their ability to access healthcare resources. It is urgent to design a culturally appropriate intervention to combat those unmet needs for symptom management.
First, HCPs should pay attention to PLWHA regarding their prevalent symptoms and encourage PLWHA to talk about how they are feeling and what they are doing now to identify mental health symptoms. Second, since nurses are at the forefront of clinical care and have the capacity to affect patients' emotional health and health behaviors, training nurses and social workers might be able to help to close the mental health treatment gap in PLWHA. Finally, self-management manuals and on-line videos should be provided to assist PLWHA find potential strategies to decrease their discomfort. Additionally, we recommend PLWHA to actively engage in social activities to help distract their attention from the unpleasant symptoms.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this study was funded by grants from the National Natural Science Foundation of China (Grant no. 71673057, PI: Yan Hu) and Nursing School, Fudan University(Grant no. FNF202013, PI: Ning Dong).
CRediT authorship contribution statement
Ning Dong:Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing.Wei-Ti Chen:Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing.Hongzhou Lu:Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing.Zheng Zhu:Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing.Yan Hu:Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing.Meijuan Bao:Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing.
Declaration of competing interest
The authors have no conflict of interest to declare.
Acknowledgements
We would like to thank Lijun Zha, Mingfeng Shi, Wei Li, Ye Li for recruiting participants. Finally, we thank all of the study participants.
References
- Alexandra M.S., Brewington K.M., Kathryn A.M., Hayness T.F., Zaller N.D. Measuring HIV-related stigma among healthcare providers: A systematic review. AIDS Care. 2017;29(11):1337–1345. doi: 10.1080/09540121.2017.1338654. [DOI] [PubMed] [Google Scholar]
- Baran R., Mulcahy F., Krznaric I., Monforte A.D., Samarina A., Xi H., Martinez M. Reduced HIV symptoms and improved health-related quality of life correlate with better access to care for HIV-1 infected women: The ELLA study. Journal of the International AIDS Society. 2014;17(4 Suppl 3):19616. doi: 10.7448/IAS.17.4.19616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barroso J., Voss J.G. Fatigue in HIV/AIDS and AIDS: An analysis of evidence. Journal of the Association of Nurses in AIDS Care. 2013;24(1 Suppl):S5–14. doi: 10.1016/j.jana.2012.07.003. [DOI] [PubMed] [Google Scholar]
- Burki T.K. Discrimination against people with HIV persists in China. Lancet. 2011;377(9762):286–287. doi: 10.1016/s0140-6736(11)60079-2. [DOI] [PubMed] [Google Scholar]
- Cai M.X. Peking Union Medical College; 2017. Investigation of palliative care needs among newly diagnosed people living with HIV in China. Dissertation. [Google Scholar]
- Carr W., Wolfe S. Unmet needs as sociomedical indicators. International Journal of Health Services. 1976;6(3):417–430. doi: 10.2190/MCG0-UH8D-0AG8-VFNU. [DOI] [PubMed] [Google Scholar]
- Chen D.C., Shi L.C., Li H. Influence of nursing intervention on self-management ability of HIV/AIDS patients. Journal of Nursing Science. 2013;28(9):36–37. [Google Scholar]
- Chen W.T., Lee S.Y., Shiu C.S., Simoni J.M., Pan C., Bao M., Lu H. Fatigue and sleep disturbance in HIV-positive women: A qualitative and biomedical approach. Journal of Clinical Nursing. 2013;22(9–10):1262–1269. doi: 10.1111/jocn.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.T., Shiu C., Yang J.P., Chuang P., Zhang L., Bao M.J., Lu H.Z. A structural equation model of patient-healthcare provider relationships and HIV-infected patient outcomes in Chinese populations. AIDS Care. 2018;30(3):383–390. doi: 10.1080/09540121.2017.1380778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.T., Shiu C.S., Simoni J.M., Fredriksen-Goldsen K., Zhang F., Zhao H. Optimizing HIV care by expanding the nursing role: Patient and provider perspectives. Journal of Advanced Nursing. 2010;66(2):260–268. doi: 10.1111/j.1365-2648.2009.05165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.T., Shiu C.S., Simoni J.M., Zhao H., Bao M.J., Lu H. In sickness and in health: A qualitative study of how Chinese women with HIV navigate stigma and negotiate disclosure within their marriages/partnerships. AIDS Care. 2011;23(Suppl. 1):120–125. doi: 10.1080/09540121.2011.554521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.T., Shiu C.S., Yang J.P., Simoni J.M., Fredriksen-Goldsen K., Lee T.S., Zhao H. Antiretroviral therapy (ART) side effect impacted on quality of life, and depressive symptomatology: A mixed-method study. Journal of AIDS & Clinical Research. 2013;4(6):218. doi: 10.4172/2155-6113.1000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng K.K.F., Wong W.H., Koh C. Unmet needs mediate the relationship between symptoms and quality of life in breast cancer survivors. Support Care Cancer. 2016;24(5):2025–2033. doi: 10.1007/s00520-015-2994-0. [DOI] [PubMed] [Google Scholar]
- China CDC Update on the AIDS/STD epidemic in China the third quarter of 2018. Chinese Journal of AIDS & STD. 2018;11:1075. [Google Scholar]
- Chu C., Selwyn P.A. An epidemic in evolution: The need for new models of HIV care in the chronic disease era. Journal of Urban Health. 2011;88(3):556–566. doi: 10.1007/s11524-011-9552-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coventry P.A., Fisher L., Kenning C., Bee P., Bower P. Capacity, responsibility, and motivation: A critical qualitative evaluation of patient and practitioner views about barriers to self-management in people with multimorbidity. BMC Health Services Research. 2014;14(1):536. doi: 10.1186/s12913-014-0536-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dacosta Dibonaventura M., Gupta S., Cho M., Mrus J. The association of HIV/AIDS treatment side effects with health status, work productivity, and resource use. AIDS Care. 2012;24(6):744–755. doi: 10.1080/09540121.2011.630363. [DOI] [PubMed] [Google Scholar]
- Fan D., Luo Y., Sun R.J., Yang X.L., Yu H.J. Study on fatigue level of HIV/AIDS patients and its influencing factors. Journal of Nursing Science. 2011;26(17):40–42. [Google Scholar]
- Fu L. Fudan University; 2014. Development of the HIV/AIDS clinical nursing practice guidelines. Dissertation. [Google Scholar]
- Gay C., Portillo C.J., Kelly R., Coggins T., Davis H., Aouizerat B.E., Lee K.A. Self-reported medication adherence and symptom experience in adults with HIV. Journal of the Association of Nurses in AIDS Care. 2011;22(4):257–268. doi: 10.1016/j.jana.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegyvary S.T. Issues in outcomes research. Journal of Nursing Care Quality. 1991;5(2):1–6. [PubMed] [Google Scholar]
- Holzemer W.L. HIV and AIDS: The symptom experience. American Journal of Nursing. 2002;102(4):48–52. doi: 10.1097/00000446-200204000-00023. [DOI] [PubMed] [Google Scholar]
- Holzemer W.L., Hudson A., Kirksey K.M., Hamilton M.J., Bakken S. The Revised Sign & Symptom Check-List for HIV (SSC-HIVrev) Journal of the Association of Nurses in AIDS Care. 2001;12(5):60–70. doi: 10.1016/s1055-3290(06)60263-x. [DOI] [PubMed] [Google Scholar]
- Hwang S.S., Chang V.T., Cogswell J., Alejandro Y., Osenenko P., Morales E.…Kasimis B. Study of unmet needs in symptomatic veterans with advanced cancer: Incidence, independent predictors and unmet needs outcome model. Journal of Pain and Symptom Management. 2004;28(5):421–432. doi: 10.1016/j.jpainsymman.2004.02.023. [DOI] [PubMed] [Google Scholar]
- Justice A.C., Holmes W., Gifford A.L., Rabeneck L., Zackin R., Sinclair G.…Adult AIDS Clinical Trials Unit Outcomes Committee Development and validation of a self-completed HIV symptom index. Journal of Clinical Epidemiology. 2001;54(Suppl. 1):S77–S90. doi: 10.1016/s0895-4356(01)00449-8. [DOI] [PubMed] [Google Scholar]
- Kagee A., Martin L. Symptoms of depression and anxiety among a sample of South African patients living with HIV. AIDS Care. 2010;22(2):159–165. doi: 10.1080/09540120903111445. [DOI] [PubMed] [Google Scholar]
- Khandelwal N., Curtis J.R., Freedman V.A., Kasper J.D., Gozalo P., Engelberg R.A., Teno J.M. How often is end-of-life care in the United States inconsistent with patients’ goals of care? Journal of Palliative Medicine. 2017;20(12):1400–1404. doi: 10.1089/jpm.2017.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalanne C., Armstrong A.R., Herrmann S., Le Coeur S., Carrieri P., Chassany O., Duracinsky M. Psychometric assessment of health-related quality of life and symptom experience in HIV patients treated with antiretroviral therapy. Quality of Life Research. 2015;24(6):1407–1418. doi: 10.1007/s11136-014-0880-8. [DOI] [PubMed] [Google Scholar]
- Leserman J., Barroso J., Pence B.W., Salahuddin N., Harmon J.L. Trauma, stressful life events and depression predict HIV-related fatigue. AIDS Care. 2008;20(10):1258–1265. doi: 10.1080/09540120801919410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Lin Y., Zhou H., Xu Y., Xu Y. Supportive care needs and associated factors among Chinese cancer survivors: A cross-sectional study. Supportive Care in Cancer. 2019;27(1):287–295. doi: 10.1007/s00520-018-4315-x. [DOI] [PubMed] [Google Scholar]
- Liu H., Zhao M., Ren J., Qi X., Sun H., Qu L.…Cui Y. Identifying factors associated with depression among men living with HIV/AIDS and undergoing antiretroviral therapy: A cross-sectional study in Heilongjiang, China. Health and Quality of Life Outcomes. 2018;16(1):190. doi: 10.1186/s12955-018-1020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo C.Y. Securitizing HIV/AIDS: A game changer in state-societal relations in China? Globalization and Health. 2018;14(1):50. doi: 10.1186/s12992-018-0364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo W.T., Yates P., Chan R.J. Unmet supportive care needs and symptom burden in Taiwanese cancer survivors who have completed primary treatment. European Journal of Oncology Nursing. 2018;35:79–84. doi: 10.1016/j.ejon.2018.05.010. [DOI] [PubMed] [Google Scholar]
- MacCarthy S., Saya U., Samba C., Birungi J., Okoboi S., Linnemayr S. “How am I going to live?”: Exploring barriers to ART adherence among adolescents and young adults living with HIV in Uganda. BMC Public Health. 2018;18(1):1158. doi: 10.1186/s12889-018-6048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez J., Harper G., Carleton R.A., Hosek S., Bojan K., Clum G.…Adolescent Medicine Trials Network The impact of stigma on medication adherence among HIV-positive adolescent and young adult females and the moderating effects of coping and satisfaction with health care. AIDS Patient Care and STDs. 2012;26(2):108–115. doi: 10.1089/apc.2011.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan J., Sherr L., Rodger A., Fisher M., Miners A., Johnson M.…Lampe F. Effects of age on symptom burden, mental health and quality of life amongst people with HIV in the UK. Journal of the International AIDS Society. 2014;17(4 Suppl 3):19511. doi: 10.7448/IAS.17.4.19511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millard T., Aqius P.A., McDonald K., Slavin S., Girdler S., Elliott J.H. The positive outlook study: A randomised controlled trial evaluating online self-management for HIV positive gay men. AIDS and Behavior. 2016;20(9):1907–1918. doi: 10.1007/s10461-016-1301-5. [DOI] [PubMed] [Google Scholar]
- Nkhoma K., Norton C., Sabin C., Winston A., Merlin J., Harding R. Self-management interventions for pain and physical symptoms among people living with HIV: A systematic review of the evidence. Journal of Acquired Immune Deficiency Syndromes. 2018;79(2):206–225. doi: 10.1097/QAI.0000000000001785. [DOI] [PubMed] [Google Scholar]
- Nkhoma K., Seymour J., Arthur An educational intervention to reduce pain and improve pain management for Malawian people living with HIV/AIDS and their family carers: A randomized controlled trial. Journal of Pain and Symptom Management. 2015;50(1):80–90. doi: 10.1016/j.jpainsymman.2015.01.011. [DOI] [PubMed] [Google Scholar]
- Norberg A., Nelson J., Holly C., Jewell S.T., Lieggi M., Salmond S. Experiences of HIV-infected adults and healthcare providers with healthcare delivery practices that influence engagement in US primary healthcare settings: A qualitative systematic review. JBI Database of Systematic Reviews and Implementation Reports. 2019 doi: 10.11124/JBISRIR-2017-003756. [DOI] [PubMed] [Google Scholar]
- Osse B.H., Vernooij-Dassen M.J., Schade E., Grol R.P. A practical instrument to explore patients’ needs in palliative care: The problems and needs in palliative care questionnaire short version. Palliative Medicine. 2007;21(5):391–399. doi: 10.1177/0269216307078300. [DOI] [PubMed] [Google Scholar]
- Pan R., Chen K., Zheng H., Liu C.X., Yao Y., Li L.L.…He N. Depressive symptoms and related factors among HIV-positive men who have sex with men in Shanghai. Fudan University Journal of Medical Sciences. 2017;44(4):430–434. [Google Scholar]
- Peltzer K. HIV-related symptoms and management in HIV and antiretroviral therapy patients in KwaZulu-Natal, South Africa: A longitudinal study. SAHARA J. 2013;10(2):96–104. doi: 10.1080/17290376.2013.870119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilgrim N., Musheke M., Raymond H.F., Keating R., Mwale J., Banda L.…Tun W. Quality of care and HIV service utilization among key populations in Zambia: A qualitative comparative analysis among female sex workers, men who have sex with men and people who use drugs. AIDS Care. 2019;31(4):460–464. doi: 10.1080/09540121.2018.1524119. [DOI] [PubMed] [Google Scholar]
- Roman E., Chou F.Y. Development of a Spanish HIV/AIDS symptom management guidebook. Journal of Transcultural Nursing. 2011;22(3):235–239. doi: 10.1177/1043659611404425. [DOI] [PubMed] [Google Scholar]
- Shadloo B., Amin-Esmaeili M., Motevalian A., Mohraz M., Sedaghat A., Gouya M.M., Rahimi-Movaghar A. Psychiatric disorders among people living with HIV/AIDS in IRAN: Prevalence, severity, service utilization and unmet mental health needs. Journal of Psychosomatic Research. 2018;110:24–31. doi: 10.1016/j.jpsychores.2018.04.012. [DOI] [PubMed] [Google Scholar]
- Shanghai Municipal Health Commission 2018. http://www.wsjsw.gov.cn/xwfb/20181130/62780.html Retrieved from.
- Simpson K.N., Hanson K.A., Harding G., Haider S., Tawadrous M., Khachatryan A.…Wu A.W. Patient reported outcome instruments used in clinical trials of HIV-infected adults on NNRTI-based therapy: A 10-year review. Health and Quality of Life Outcomes. 2013;11(1):164. doi: 10.1186/1477-7525-11-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder C.F., Blackford A.L., Brahmer J.R., Carducci M.A., Pili R., Stearns V.…Wu A.W. Needs assessments can identify scores on HRQOL questionnaires that represent problems for patients: An illustration with the supportive care needs survey and the QLQ-C30. Quality of Life Research. 2010;19(6):837–845. doi: 10.1007/s11136-010-9636-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solano J.P., Gomes B., Higginson I.J. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. Journal of Pain and Symptom Management. 2006;31(1):58–69. doi: 10.1016/j.jpainsymman.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Tsai Y.F., Hsiung P.C., Holzemer W.L. Symptom management in Taiwanese patients with HIV/AIDS. Journal of Pain and Symptom Management. 2002;23(4):301–309. doi: 10.1016/s0885-3924(01)00413-4. [DOI] [PubMed] [Google Scholar]
- Wakeham K., Harding R., Bamukama-Namakoola D., Levin J., Kissa J., Parkes-Ratanshi R.…Lalloo D.G. Symptom burden in HIV-infected adults at time of HIV diagnosis in rural Uganda. Journal of Palliative Medicine. 2010;13(4):375–380. doi: 10.1089/jpm.2009.0259. [DOI] [PubMed] [Google Scholar]
- Walling A.M., Keating N.L., Kahn K.L., Dy S., Mack J.M., Mallin J.…Tisnado D. Lower patient ratings of physician communication are associated with unmet need for symptom management in patients with lung and colorectal cancer. Journal of Oncology Practice. 2016;12(6):e654–e669. doi: 10.1200/JOP.2015.005538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K.R., Chen W.T., Zhang L., Bao M.J., Zhao H.X., Lu H.Z. Facilitators of and barriers to HIV self-management: Perspectives of HIV-positive women in China. Applied Nursing Research. 2016;32:91–97. doi: 10.1016/j.apnr.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Li B., Ungvari G.S., Ng C.H., Chiu H.F., Kou C.…Xiang Y.T. Poor mental health status and its associations with demographic characteristics and chronic diseases in Chinese elderly. Social Psychiatry and Psychiatric Epidemiology. 2016;51(10):1449–1455. doi: 10.1007/s00127-016-1271-y. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Gonzalez H.M., Williams S., Mohammed S.A., Moomal H., Stein D.J. Perceived discrimination, race and health in South Africa. Social Science & Medicine. 2008;67(3):441–452. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N.L., Azuero A., Vance D.E., Richman J.S., Moneyham L.D., Raper J.L.…Kempf M.C. Identifying symptom patterns in people living with HIV disease. Journal of the Association of Nurses in AIDS Care. 2016;27(2):121–132. doi: 10.1016/j.jana.2015.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu M.L. Chongqing University Press; Chongqing: 2010. Statistical analysis of questionnaires: SPSS operation and application. [Google Scholar]
- Yang J.P., Leu J., Simoni J.M., Chen W.T., Shiu C.S., Zhao H. “Please don’t make me ask for help”: Implicit social support and mental health in Chinese individuals living with HIV. AIDS and Behavior. 2015;19(8):1501–1509. doi: 10.1007/s10461-015-1041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Miege P., Zhang Y. Decentralization of the provision of health services to people living with HIV/AIDS in rural China: The case of three counties. Health Research Policy and Systems. 2011;9:9. doi: 10.1186/1478-4505-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Hearst N. Health-related quality of life of among elders in rural China: The effect of widowhood. Quality of Life Research. 2016;25(12):3087–3095. doi: 10.1007/s11136-016-1338-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z., Hu Y., Guo M., Williams A.B. Urban and rural differences: Unmet needs for symptom management in people living with HIV in China. Journal of the Association of Nurses in AIDS Care. 2019;30(2):206–217. doi: 10.1097/JNC.0000000000000025. [DOI] [PubMed] [Google Scholar]
- Zhu Z., Hu Y., Xing W., Guo M., Zhao R., Han S., Wu B. Identifying symptom clusters among people living with HIV on antiretroviral therapy in China: A network analysis. Journal of Pain and Symptom Management. 2019;57(3):617–662. doi: 10.1016/j.jpainsymman.2018.11.011. [DOI] [PubMed] [Google Scholar]