Abstract
Objective
Faecal microbiota transplantation (FMT) from healthy donors to patients with irritable bowel syndrome (IBS) has been attempted in two previous double-blind, placebo-controlled studies. While one of those studies found improvement of the IBS symptoms, the other found no effect. The present study was conducted to clarify these contradictory findings.
Design
This randomised, double-blind, placebo-controlled study randomised 165 patients with IBS to placebo (own faeces), 30 g FMT or 60 g FMT at a ratio of 1:1:1. The material for FMT was obtained from one healthy, well-characterised donor, frozen and administered via gastroscope. The primary outcome was a reduction in the IBS symptoms at 3 months after FMT (response). A response was defined as a decrease of 50 or more points in the total IBS symptom score. The secondary outcome was a reduction in the dysbiosis index (DI) and a change in the intestinal bacterial profile, analysed by 16S rRNA gene sequencing, at 1 month following FMT.
Results
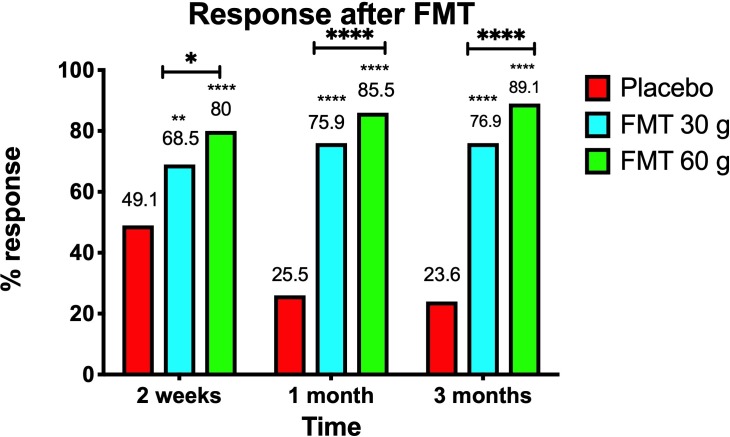
Responses occurred in 23.6%, 76.9% (p<0.0001) and 89.1% (p<00.0001) of the patients who received placebo, 30 g FMT and 60 g FMT, respectively. These were accompanied by significant improvements in fatigue and the quality of life in patients who received FMT. The intestinal bacterial profiles changed also significantly in the groups received FMT. The FMT adverse events were mild self-limiting gastrointestinal symptoms.
Conclusions
FMT is an effective treatment for patients with IBS. Utilising a well-defined donor with a normal DI and favourable specific microbial signature is essential for successful FMT. The response to FMT increases with the dose.
Trial registration
www.clinicaltrials.gov (NCT03822299) and www.cristin.no (ID657402).
Keywords: lactobacillus, irritable bowel syndrome, colonic microflora
Significance of this study.
What is already known on this study?
The intestinal bacterial profile of patients with irritable bowel syndrome (IBS) differs from that of healthy subjects.
The low bacterial diversity (dysbiosis) in patients with IBS might contribute to the pathophysiology of IBS.
Faecal microbiota transplantation (FMT) has been investigated in two previous double-blind, placebo-controlled studies. One of those studies found improvement of the IBS symptoms, whereas the other found no effect.
What are the new findings?
FMT is an effective treatment for IBS that improves abdominal symptoms, fatigue and quality of life.
The use of a superdonor is necessary for successful FMT.
How might it impact on clinical practice in the foreseeable future?
This study demonstrates the effectiveness of FMT in the treatment of IBS.
The use of frozen faeces administered via a gastroscope makes FMT easy to perform in the clinic.
Introduction
Irritable bowel syndrome (IBS) is a relatively common gastrointestinal disorder with an estimated prevalence of 11.2% in the global population.1 2 Although IBS does not increase mortality, it reduces the quality of life considerably.1 2 The aetiology of IBS is not completely understood, and there is no effective treatment for the condition.1 The gut microbiota in patients with IBS differs from that of the healthy subjects, including exhibiting a low bacterial diversity (dysbiosis).1 3–5 It is believed that microbiota dysbiosis is one of the factors contributing to the aetiology of IBS.1
The application of faecal microbiota transplantation (FMT) in several open-label trials with small cohorts of patients with IBS has produced good results.1 One recent randomised double-blind, placebo-controlled study of FMT found positive results for FMT, whereas another found no effect.6 7 The present study was carried out to resolve these contradictory findings.
Methods
Trial design
The patients included in this single-centre, randomised, double-blind, placebo-controlled, parallel-group study were seen twice: at the baseline and 1 month after transplantation. At the baseline visit, the patients provided a faecal sample and were asked to complete five questionnaires to assess their abdominal symptoms, fatigue and quality of life. At the second visit, the patients provided a faecal sample and completed a new set of questionnaires. The patients also completed similar sets of questionnaires at 2 weeks and 3 months after FMT, and returned them by post. The patients were asked to keep a diary to record bowel habits and register any adverse events. Polyethylene glycol and loperamide were allowed during the intervention as rescue medication. The frequency of using these rescue medications in the three intervention groups was not recorded.
Enrolment and randomisation of patients
Randomisation
The patients were randomised to the placebo (30 g of their own faeces), 30 g FMT and 60 g FMT groups at a ratio of 1:1:1 in blocks of six using a Web-based system (http://www.randomization.com) by a nurse who was not involved in the trial (figure 1). The patients delivered two faecal samples at the start of the trial to the same nurse: one was used for gut bacterial analysis in all patients, while the other was either used for transplantation (in patients randomised to placebo) or discarded (in patients randomised to ‘superdonor’ FMT, as described later). The researcher who prepared the transplant was not aware of the identity of the faecal sample used for transplantation. The patients and researchers involved in the study were blinded to the randomisation. The randomisation key was revealed to the researcher and patients after the trial had ended.
Figure 1.
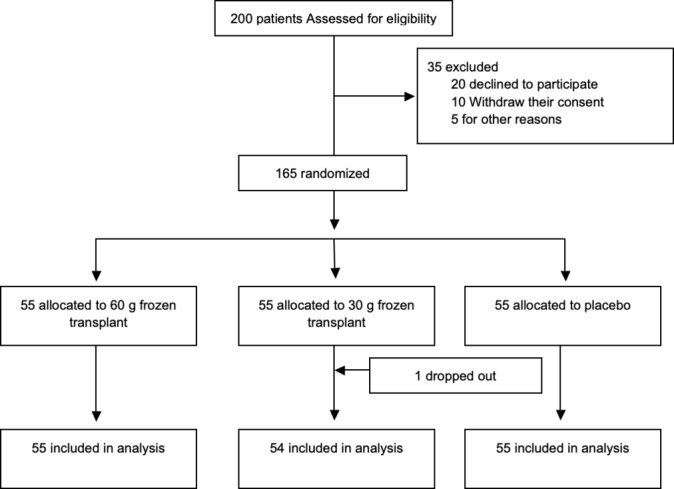
Consolidated standards of reporting trials) diagram showing the enrolment and randomisation of the patients.
Patients
Patients who fulfilled the Rome IV criteria for the diagnosis of IBS without red flags were recruited from those attending the outpatient clinic at Stord Hospital. All of the patients had been experiencing IBS symptoms for a long time (mean=17 years, range=9–25 years), and the onset of symptoms had not been associated with gastrointestinal or other infections. The medical history was obtained for all patients, and they underwent a complete physical examination as well as blood tests for full blood count, electrolytes and inflammatory markers including faecal calprotectin, liver tests and thyroid function tests. They also underwent a gastroscopy with duodenal biopsies and a colonoscopy with segmental biopsies to exclude other gastrointestinal diseases.
The patients had not previously consumed a low-fermentable oligo-, di-, monosaccharides and polyols diet. All of the recruited patients adhered to a diet consistent with the modified guidelines of the National Institute for Health and Care Excellence (NICE) at least for 3 months, which did not result in a marked improvement in symptoms, including in the bowel habit, abdominal pain or abdominal bloating/distension. These patients were considered as non-responders to a NICE-modified diet,8 and they stopped consuming that diet on entering the trial. They underwent a 12-hour course of IBS treatment lasting 2 days that provided with information delivered by a gastroenterologist, specialist nurse, psychiatrist, dietitian and physiotherapist.9 The patients’ symptoms improved slightly after participating in the course, which is consistent with previously published data related to a similar course.9
The following inclusion criteria were applied:
Aged 18–85 years.
Moderate-to-severe IBS symptoms, as indicated by a score of ≥175 on the IBS Severity Scoring System (IBS-SSS).
The exclusion criteria were as follows:
Presence of systemic disease, immune deficiency or treatment with immune-modulating medication.
Pregnant, planning pregnancy or lactating.
Having undergone any abdominal surgery, with the exception of appendectomy, cholecystectomy, caesarean section and hysterectomy.
Severe psychiatric disorder, or alcohol or drug abuse.
Use of probiotics or treatment with antibiotics within 8 weeks prior to study entry.
Use of IBS medication within the previous 3 months, with the exception of polyethylene glycol and loperamide.
Donor
A single superdonor was recruited and screened according to the European guidelines for donors for FMT.1 10 This involved interviewing him to obtain his medical history and lifestyle habits to exclude any exposure to infectious agents or risky social or sexual behaviour such as drug abuse. He also underwent a physical examination as well as blood tests to exclude gastrointestinal, metabolic or neurological disorders (full blood count, blood glucose, electrolytes and inflammatory markers), liver tests and thyroid function tests. Serology screening tests for HIV, syphilis and hepatitis A, B and C were also performed. Stool culturing was performed for pathogenic bacteria (Shigella spp., Salmonella spp., Campylobacter spp., Yersinia spp. and toxin-producing Clostridioides difficile). Rotavirus and stool ova and parasites were also examined. The findings of all of these tests and examinations were negative.
The donor was an athletic Caucasian male aged 36 years. He was a non-smoker, healthy, not taking any medication and had a BMI of 23.5 kg/m2. He was not related to any of the patients in the trial. His mother (a medical professional) confirmed that he was born via a vaginal delivery, breastfed and had been treated three times with antibiotics during his life. He trained for 1 hour five times weekly. The MoBa Food Frequency Questionnaire was used to determine his frequency of consuming 225 food items grouped according to the Norwegian meal patterns over the previous 12 months, and his answers were analysed using software for nutrient calculations.11 The superdonor’s diet was within the normal range of those of 35 previously examined healthy subjects.11 However, the superdonor regularly took dietary supplements rich in proteins, vitamins, fibre and minerals (online supplementary table 1) that made his diet richer than average in those substances.
gutjnl-2019-319630supp001.pdf (50.2KB, pdf)
His microbiota in a faecal sample was analysed using the GA-map Dysbiosis Test (Genetic Analysis, Oslo, Norway),3 which revealed a dysbiosis index (DI) of 1, indicating normobiosysis. Despite the donor having a DI of 1, deviation from the expected normal abundance was observed in 14 of the 39 bacteria markers. These deviating bacteria belong to the typical commensal bacteria species, and increases or decreases in their abundances are not considered to contribute to dysbiosis. In all, 12 of the bacteria were in the phylum Firmicutes, with one each in the phyla Proteobacteria and Verrucomicrobia. The other 25 more opportunistic bacteria markers that showed abundances similar to normal are important candidates in a dysbiotic condition (figure 2). The donor had donated his faeces in 18 months, and his faeces samples were tested every 3 months. The samples remained normobiotic, with only minor variations in the constituent bacteria (figure 3).
Figure 2.
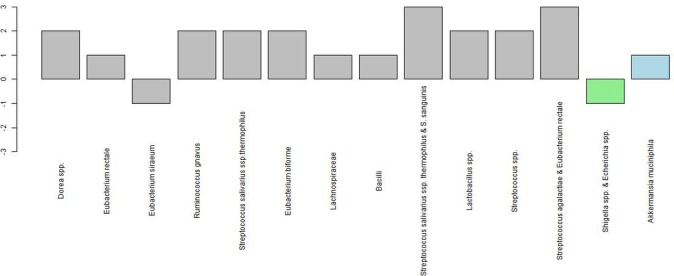
Although the superdonor was normobiotic, his bacterial profile deviated from the expected normal abundance in 14 of the 39 bacteria markers. The deviating bacteria belong to the typical commensal bacteria species that do not contribute to dysbiosis. In all, 12 of these bacteria belong to the phylum Firmicutes (grey), one to the phylum Proteobacteria (light green) and one to the phylum Verrucomicrobia (light blue).
Figure 3.
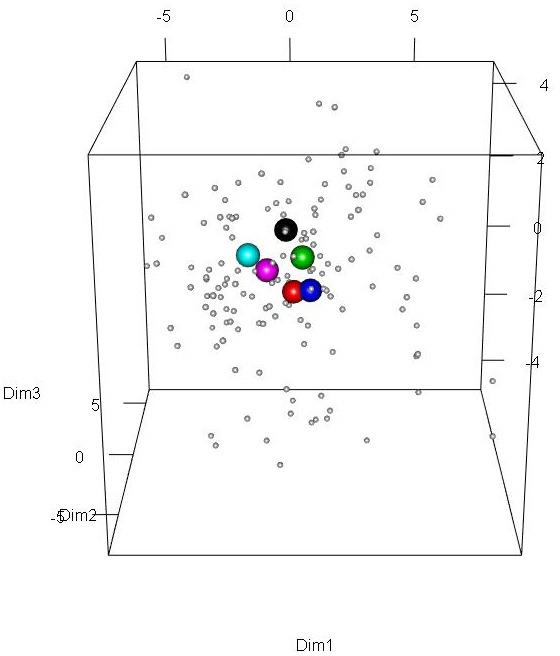
Scaled principal component analysis plot of faecal samples from the superdonor and patients before transplantation. The patient samples are indicated by small grey circles. The superdonor samples are indicated by the larger circles of different colours that indicate the sampling times: Black, 3 months; red, 6 months; green, 9 months; blue, 12 months; light blue, 15 months; and pink, 18 months. All of the superdonor samples are grouped closely together and remain in very similar positions over time.
Faecal sample collection, preparation and administration
Faecal samples from the superdonor and the patients were frozen immediately and kept at –20°C until they were delivered frozen to the laboratory on the same day. They were kept at –80°C in the laboratory, and thawed at 4°C for 2 days before transplantation. On the day of transplantation, the faecal samples were weighed, and 30 g and 60 g portions were mixed with 40 mL of sterile saline (0.9 NaCl), filtered through a 110 cm × 10 cm non-woven swab (One Med, Helsinki, Finland), drawn into 50 mL sterile syringes, sealed and kept at 4°C until the time of transplantation. Each transplant was administered to the distal duodenum via the working channel of a gastroscope, which was then flashed with another 40 mL of sterile saline.
Measures
Abdominal symptoms, fatigue and quality of life
Abdominal symptoms were assessed using the IBS-SSS and the Birmingham IBS Symptom (Birmingham IBS-S) questionnaires.12 13 Fatigue was measured using the Fatigue Assessment Scale (FAS).14 Quality of life was measured using the IBS Quality of Life (IBS-QoL) and Short-Form Nepean Dyspepsia Index (SF-NDI) questionnaires.15–17 Higher IBS-QoL and lower SF-NDI scores indicate a better quality of life.
Patients whose total IBS-SSS score decreased by ≥50 points after FMT were considered responders. A decrease of ≥175 points in the IBS-SSS total score, a decrease of ≥4 points in the FAS score and an increase of ≥14 points in the IBS-QoL score were considered to indicate significant clinical improvements in abdominal symptoms, fatigue and quality of life, respectively.12 16 18 The responses were also analysed according to the European Medicines Agency and (EMA) and the Food and Drug Administration (FDA) using a composite responder endpoint.19 20 According to EMA, a responder should fulfil the response criteria for at least 50% of the observation time. The response criteria for IBS-D are an improvement at least 30% in the abdominal pain score and a 50% reduction in the number of days with at least one stool that that has consistency of 6 or seven as compared with the base line. The response criteria for IBS-C are a reduction at least 30% in the abdominal pain score and an increase of at least one complete spontaneous bowel movement per week as compared with the base line. In IBS-M, a responder is a patient who has at least 30% improvement in the abdominal pain score and a subjects global assessment of efficacy scale of the highest two improvement grades in a 7-point scale, or of the highest improvement grade in a 5-point scale as compared with the base line.
Faecal bacterial analysis
The faecal bacteria were analysed with the GA-map Dysbiosis Test using a method described in detail elsewhere.3 4 In brief, the test uses the 16S rRNA gene to determine both the bacterial profile and DI. It detects bacteria within five phyla (Firmicutes, Proteobacteria, Bacteroidetes, Tenericutes and Verrucomicrobia) that cover 10 bacterial classes, 36 genera and 32 species,3 which means that the test assesses >300 bacteria at different taxonomic levels.4 The DI is measured on a 5-point scale from 1 to 5 (severe dysbiosis), where DI values>2 indicate the presence of dysbiosis.3
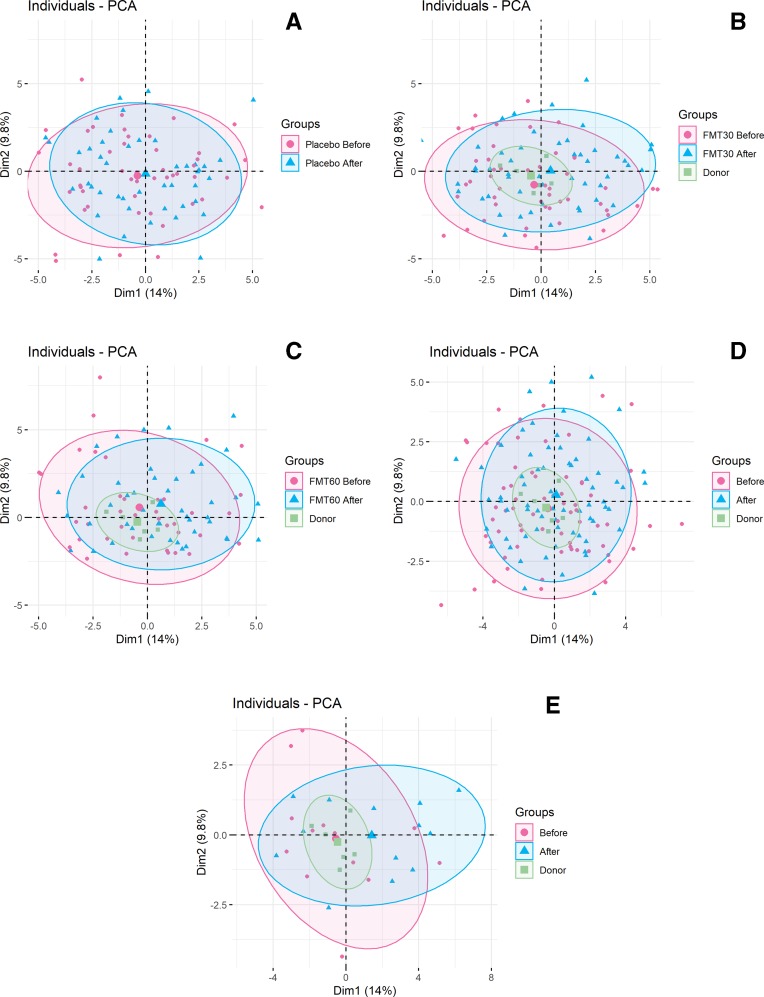
The GA-map Dysbiosis Test was also used to analyse the changes in the intestinal bacterial profile following transplantation, in which the bacterial abundance was quantified from –3 to +3, where 0 represents the normal value based on a previous analysis of faecal samples of 297 healthy subjects.3 In addition, principal component analysis (PCA) was used to plot scaled probe signals inside an ellipse that covered 80% of the samples within a group. The differences in the signals were analysed using the lmFit function in the limma package.21
Outcomes
The primary endpoint was a reduction in the IBS-SSS total score of ≥50 points at 3 months following transplantation,22 which the secondary endpoint was a change in the DI and intestinal bacterial profile.
Ethics
All subjects provided both oral and written consents to participate.
Statistical analysis
The sample size required in each arm of the trial was calculated by assuming that a placebo effect was 40% and an effect response was 80%. The total sample size was estimated to be 60 patients, with 20 in each arm (α=0.05, 1–β=0.80). We intended to assess 200 patients for eligibility mainly because a previous study employing a similarly calculated sample size failed to show any benefit of FMT, and also to allow for dropouts.7 Differences between the placebo, 30 g FMT and 60 g FMT groups in age and in IBS-SSS, Birmingham IBS-S, FAS, IBS-QoL and SF-NDI scores were analysed using one-way analysis of variance with Tukey’s multiple-comparisons test as a post-test. The differences between the placebo, 30 g FMT and 60 g FMT groups in sex, overall responses, numbers of included IBS subtypes, IBS-subtype responses, IBS-subtype dysbiosis and IBS-subtype medications, and differences in responses with sex and IBS duration were analysed using the χ2 test. The correlations between the changes in bacterial profile and the IBS-SSS and FAS scores were analysed using the non-parametric Spearman test. The paired t-test was used to calculate the differences in the bacterial profile and DI in the placebo, 30 g FMT and 60 g FMT groups between before and 1 month after transplantation. Wilcoxon’s test was applied in PCA to test for differences in the placebo, 30 g FMT and 60 g FMT before and 1 month after transplantation. These analyses were performed using GraphPad Prism (version 8, La Jolla, CA, USA). All authors had access to the study data and reviewed and approved the final manuscript.
Results
Patients and responses
In all, 200 patients were initially assessed for eligibility, of which 164 patients completed the study (figure 1). The characteristics of these patients are summarised in table 1. Responses occurred after 3 months in 23.6%, 76.9% and 89.1% of the patients in the placebo, 30 g FMT and 60 g FMT groups, respectively (figure 4). There were significant response differences between 30 g FMT and 60 g FMT after 2 weeks, 1 month and 3 months (figure 4). The response to FMT did not differ between the IBS subtypes. However, IBS-C (constipation-predominant IBS) and IBS-M (mixed-diarrhoea-and-constipation IBS) patients in the placebo group exhibited significantly larger responses after 1 and 3 months (online supplementary table 2), which could have been at least partially due to the rescue medication used for constipation (polyethylene glycol) being more effective than that used for diarrhoea (loperamide). The responses in the placebo, 30 g FMT and 60 g FMT groups did not differ with sex (p=0.9, 0.5 and 0.6, respectively) or between patients with IBS for ≥10 and<10 years (p=0.9, 0.8 and 0.7, respectively). The total IBS-SSS scores for diarrhoea-predominant IBS (IBS-D), IBS-C and IBS-M patients in the 30 g FMT group at the endpoint of the trial (after 3 months) were 157.7±83.2 (mean±SD), 207.9±114.7 and 204±125.5, respectively, with corresponding values in the 60 g FMT group of 156.4±113.3, 189.2±123.0 and 158.9±127.1. The total IBS-SSS score did not differ between the IBS-subtype patients who received 30 g FMT and 60 g FMT (p=0.260 and 0.652, respectively).
Table 1.
Characteristics of patients at the trial baseline
| Overall | Placebo | 30 g FMT | 60 g FMT | P | |
| All patients | 164 | 55 | 54 | 55 | |
| Age, years | 39.9±9.0 | 41.2±13.7 | 39.2±12.4 | 39.3±13.2 | 0.672 |
| Sex, female/male | 133/32 | 47/8 | 40/14 | 46/9 | 0.189 |
| IBS-D | 63 | 21 | 22 | 20 | |
| IBS-C | 62 | 22 | 20 | 20 | 0.989 |
| IBS-M | 39 | 12 | 13 | 14 | |
| IBS-SSS score | 313.4±80.3 | 315.2±77.1 | 311.8±76.8 | 313.9±87.3 | 0.975 |
| Birmingham IBS-S score | 24.3±7.1 | 23.2±8.1 | 26.5±6.0 | 25.2±6.8 | 0.050 |
| IBS-QoL score | 113.5±21.8 | 117.8±19.7 | 109.1±22.7 | 113.4±22.4 | 0.117 |
| SF-NDI score | 30.2±7.7 | 29.9±1.6 | 29.7±7.1 | 30.9±8.4 | 0.728 |
| FAS score | 31.1±4.9 | 30.6±4.9 | 31.4±5.1 | 31.3±4.8 | 0.634 |
| DI | 2.8±1.1 | 2.7±1.1 | 2.8±1.0 | 2.9±1.0 | 0.781 |
| Patients with dysbiosis | (64) | (67) | (57) | (67) | 0.578 |
| PPI medication | 59 (35.8) | 21 (38.2) | 20 (36.4) | 18 (32.7) | 0.810 |
| Birth-control medication | 84 (50.9) | 25 (45.5) | 29 (52.7) | 30 (54.5) | 0.601 |
| Antimigraine medication | 12 (7.3) | 3 (5.5) | 5 (9.1) | 4 (7.3) | 0.764 |
| Medication against asthma/allergies | 18 (10.9) | 6 (10.9) | 7 (12.7) | 5 (9.1) | 0.829 |
| Medication with levothyroxine | 3 (1.8) | 1 (1.8) | 0 (0) | 2 (3.6) | 0.361 |
| Medication with heart/vascular drugs | 6 (3.6) | 3 (5.5) | 2 (3.6) | 1 (1.8) | 0.595 |
Data are mean±SD, n, n/n, (%) or n (%) values.
DI, dysbiosis index; FAS, Fatigue Assessment Scale; FMT, faecal microbiota transplantation; IBS, irritable bowel syndrome; IBS-QoL, IBS Quality of Life; IBS-SSS, IBS Severity Scoring System; PPI, proton-pump inhibitor; SF-NDI, Short-Form Nepean Dyspepsia Index.
Figure 4.
Responses of patients with IBS to placebo, 30 g FMT and 60 g FMT at different intervals after transplantation. **, p<0.001; ****, p<0.0001 compared with placebo. *, p<0.001; ***, p<0.0001 for 30 g FMT compared with 60 g FMT. IBS, irritable bowel syndrome; FMT, faecal microbiota transplantation.
gutjnl-2019-319630supp002.pdf (33.9KB, pdf)
Abdominal symptoms, fatigue and quality of life
Abdominal symptoms as measured using IBS-SSS and Birmingham IBS-S were significantly improved after 3 months for both 30 g FMT and 60 g FMT compared with placebo (table 2 and online supplementary table 3), as was fatigue as assessed using FAS (table 3) and the quality of life as assessed using IBS-QoL and SF-NDI (table 4 and online supplementary table 4). In more detail, there were clinical improvements in abdominal symptoms in 5.5%, 35.2% and 47.3% of the patients in the placebo, 30 g FMT and 60 g FMT groups, respectively, in fatigue in 21.8%, 53.7% and 52.7% of them, and in the quality of life in 7.3%, 61.1% and 58.2% of them (online supplementary table 5). The responses according to EMA/FDA composite responder endpoint, 3 months after FMT were 16.7%, 50% and 70.9% in the placebo, 30 g and 60 g groups, respectively. The responses in 30 g and 60 g groups versus placebo group were significant (p<0.0001, both). There was a significant difference in response between 30 g and 60 g groups (p=0.004).
Table 2.
IBS-SSS total scores and scores for the four items of the scale in placebo and FMT-treated patients following transplantation
| Time | Group | Total score | 1 | 2 | 3 | 4 |
| 0 | Placebo | 315.2±77.1 | 107.5±46.1 | 55.5±24.7 | 76.1±20.7 | 75.4±19.8 |
| 30 g FMT | 311.8±76.8 | 111.1±42.8 | 51.0±25.8 | 76.4±19.2 | 75.6±17.8 | |
| 60 g FMT | 313.3±87.3 | 106.5±45.8 | 55.0±25.4 | 78.6±18.1 | 75.6±20.8 | |
| 2 weeks | Placebo | 278.7±124.7 | 88.1±57.0 | 51.2±30.5 | 62.6±28.5 | 64.5±27.5 |
| 30 g FMT | 244.0±98.5** | 84.4±49.3 | 35.0±24.8** | 53.3±25.7** | 54.4±25.2* | |
| 60 g FMT | 184.6±96.3*** | 58.9±41.9**† | 32.7±26.0*** | 43.6±26.0*** | 48.2±26.4** | |
| 1 month | Placebo | 299.5±106.1 | 102.0±51.2 | 53.5±27.4 | 70.3±25.1 | 69.1±26.3 |
| 30 g FMT | 213.4±100.1*** | 97.7±47.8* | 36.9±22.8*** | 49.4±28.9*** | 50.9±29.1*** | |
| 60 g FMT | 186.8±107.0*** | 66.8±50.8*** | 33.7±24.6*** | 40.4±28.4*** | 46.4±26.8*** | |
| 3 months | Placebo | 307.0±87.1 | 112.0±69.7 | 56.8±31.8 | 73.1±22.3 | 71.7±22.0 |
| 30 g FMT | 186.3±109.0*** | 69.4±48.5*** | 30.5±21.7*** | 44.6±29.7*** | 45.3±30.9*** | |
| 60 g FMT | 166.8±117.9*** | 56.5±47.5*** | 30.4±26.4*** | 35.6±26.2*** | 40.2±27.1*** |
IBS-SSS items: 1, abdominal pain; 2, abdominal distension; 3, dissatisfaction with bowel habits; 4, interference with quality of life.
Data are mean±SD values.
*p<0.05;**p<0.01; ***p<0.001 compared with placebo.
†p<0.05 compared with 30 g FMT.
FMT, faecal microbiota transplantation; IBS, irritable bowel syndrome; IBS-SSS, IBS Severity Scoring System.
Table 3.
FAS scores in placebo and FMT-treated patients
| Time | Group | Total score | Physical fatigue | Mental health |
| 0 | Placebo | 30.6±4.9 | 15.8±2.6 | 14.8±2.6 |
| 30 g FMT | 31.4±5.1 | 15.9±3.0 | 15.5±2.8 | |
| 60 g FMT | 31.3±4.8 | 15.9±2.8 | 15.4±2.6 | |
| 2 weeks | Placebo | 30.4±5.7 | 15.8±3.2 | 14.6±2.9 |
| 30 g FMT | 28.1±5.5 | 14.6±3.2 | 13.9±2.9 | |
| 60 g FMT | 28.4±6.0 | 14.5±3.0 | 13.9±3.4 | |
| 1 month | Placebo | 30.8±6.0 | 16.1±2.9 | 14.7±3.4 |
| 30 g FMT | 27.5±6.7* | 14.3±3.8* | 13.3±3.1* | |
| 60 g FMT | 27.8±6.2* | 14.5±3.4* | 13.4±3.2 | |
| 3 months | Placebo | 29.8±4.6 | 15.2±2.6 | 14.5±2.7 |
| 30 g FMT | 27.1±5.8* | 13.4±3.5* | 13.6±3.0 | |
| 60 g FMT | 27.0±6.3* | 14.1±3.4 | 13.1±3.1* |
Data are mean±SD values.
*p<0.05 compared with placebo.
FAS, Fatigue Assessment Scale; FMT, faecal microbiota transplantation.
Table 4.
IBS-QoL total scores and scores in the eight domains of the scale in placebo and FMT-treated patients
| Time | Group | Total score | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 0 | Placebo | 117.8±19.7 | 27.3±5.8 | 23.6±5.8 | 11.9±2.7 | 10.6±2.6 | 7.2±2.6 | 15.0±3.1 | 7.8±1.7 | 11.2±2.5 |
| 30 g FMT | 109.1±22.7 | 26.2±6.9 | 20.0±5.9** | 11.2±3.4 | 10.3±2.8 | 5.9±2.8 | 13.6±3.5 | 7.5±2.1 | 10.8±2.6 | |
| 60 g FMT | 113.4±22.4 | 27.4±6.7 | 21.4±5.5 | 11.5±2.8 | 10.6±2.7 | 6.7±2.8 | 14.1±3.4 | 7.7±1.7 | 10.8±2.8 | |
| 2 weeks | Placebo | 122.4±28.1 | 29.1±6.5 | 23.0±4.9 | 12.3±3.33 | 11.3±2.7 | 8.0±3.4 | 14.7±4.6 | 7.6±2.6 | 11.1±3.5 |
| 30 g FMT | 118.0±23.0 | 28.6±6.7 | 20.4±5.8* | 13.3±3.2 | 11.3±3.1 | 7.1±3.1 | 14.3±3.4 | 7.8±2.0 | 10.9±2.1 | |
| 60 g FMT | 124.5±25.1 | 31.1±6.6 | 23.3±5.9† | 13.4±3.7 | 12.0±2.7 | 8.3±2.8 | 15.5±3.5 | 8.1±1.9 | 11.7±2.7 | |
| 1 month | Placebo | 122.9±25.4 | 29.2±7.7 | 23.1±4.8 | 12.7±4.2 | 12.3±2.4 | 8.6±2.9 | 14.7±3.4 | 7.0±2.3 | 11.4±2.8 |
| 30 g FMT | 121.6±23.9 | 29.5±7.1 | 21.8±4.8 | 13.2±3.7 | 11.6±2.5 | 7.2±2.9* | 15.8±3.1 | 7.9±1.6 | 11.5±2.4 | |
| 60 g FMT | 127.7±25.5 | 31.1±6.7 | 23.0±5.1 | 13.9±3.5 | 12.1±2.4 | 8.6±3.3† | 15.1±3.9 | 8.2±2.0** | 11.7±2.8 | |
| 3 months | Placebo | 113.0±24.3 | 27.2±6.3 | 21.2±4.6 | 12.1±3.0 | 12.8±6.3 | 7.1±3.0 | 13.6±3.8 | 7.3±2.3 | 10.4±2.5 |
| 30 g FMT | 131.5±21.6*** | 32.1±6.9** | 24.1±5.2** | 14.0±3.0** | 12.6±2.9 | 8.8±3.2* | 16.1±2.6*** | 8.2±1.6* | 12.6±1.8**** | |
| 60 g FMT | 132.0±24.8*** | 32.5±6.7** | 24.0±4.7** | 14.5±3.4*** | 12.2±2.2 | 9.6±3.6*** | 15.7±3.5** | 8.3±1.6* | 12.1±2.6*** |
IBS-QoL domains: 1, dysphoria; 2, interference with daily activities; 3, body image; 4, health worries; 5, food avoidance; 6, social reaction; 7, sexual function; 8, impact on relationships.
*p<0.05; **p<0.01; ***p<0.001; ****p<0.0001 compared with placebo.
†p<0.05 compared with 30 g FMT.
FMT, faecal microbiota transplantation; IBS, irritable bowel syndrome; IBS-QoL, IBS Quality of Life.
gutjnl-2019-319630supp003.pdf (41KB, pdf)
gutjnl-2019-319630supp004.pdf (50.5KB, pdf)
gutjnl-2019-319630supp005.pdf (35.3KB, pdf)
Bacterial analysis
Some of the tubes containing faecal samples shattered during transportation to the laboratory for analysis, which resulted in the bacterial analyses of faecal samples before and after transplantation only being performed on 47, 42 and 39 patients in the placebo, 30 g FMT and 60 g FMT groups, respectively. The DI values before transplantation were 2.6±1.1, 2.8±1.1 and 2.7±0.9 in the placebo, 30 g FMT and 60 g FMT groups, respectively; the corresponding values after transplantation were 2.6±1.1, 2.6±1.1 and 2.4±1.1 (p=0.087, 0.508 and 0.262). Dysbiosis was present in 57%, 55% and 61% of the patients in the placebo, 30 g FMT and 60 g FMT groups before transplantation, respectively, in 53%, 50% and 39% of them after transplantation (p=0.836, 0.828 and 0.108, respectively).
The analysis of the faecal bacterial profiles obtained using the GA-map Dysbiosis Test showed significant changes in the abundance of bacteria in the 30 g FMT and 60 g FMT groups but not in the placebo group (online supplementary table 6). Alistipes spp. were increased for both 30 g FMT and 60 g FMT. Bacteroides and Prevotella spp. increased in the 30 g FMT group while Eubacterium hallii decreased, and Firmicutes spp. and Akkermansia muciniphila increased in the 60 g FMT group, while Dorea spp. decreased.
gutjnl-2019-319630supp006.pdf (91.5KB, pdf)
PCA and the differences in signals analysed using the lmFit function in the limma package showed changes in the bacterial profiles after transplantation in the placebo, 30 g FMT and 60 g FMT groups as well as in the responder and non-responder groups (figure 5). The same approach showed that the responders in both the 30 g FMT and 60 g FMT groups had higher signals for Eubacterium biforme, Lactobacillus spp. and Alistipes spp. after transplantation, and lower signals for Bacteroides spp. (online supplementary figure 1). These changes occurred in responders in the 30 g FMT and 60 g FMT groups but not in the placebo group (online supplementary figures 2–5).
Figure 5.
Scaled PCA plot of faecal samples before and after transplantation for placebo (A), 30 g FMT (B), 60 g FMT (C), responders (D) and non-responders (E). Faecal samples before and after transplantation are indicated by pink circles and blue triangles, respectively. The ellipses cover 80% of the samples within a group. FMT, faecal microbiota transplantation; PCA, principal component analysis.
gutjnl-2019-319630supp007.pdf (23.2KB, pdf)
gutjnl-2019-319630supp008.pdf (367.9KB, pdf)
gutjnl-2019-319630supp009.pdf (479.2KB, pdf)
gutjnl-2019-319630supp010.pdf (500.5KB, pdf)
gutjnl-2019-319630supp011.pdf (79.4KB, pdf)
The IBS-SSS score was significantly correlated with the concentrations of Lactobacillus spp. (p=0.002, r=–0.3) and Alistipes spp. (p=0.001, r=–0.3) but not with that of Eubacterium biforme (p=0.754, r=0.03) or Bacteroides spp. (p=0.458, r=0.06). The FAS score was correlated with the concentration of Alistipes spp. (p=0.007, =–0.2) but not that of Eubacterium biforme (p=0.137, r=0.1), Lactobacillus spp. (p=0.829, r=–0.02) or Bacteroides spp. (p=0.174, r=0.1).
Adverse events
Mild intermittent abdominal pain, diarrhoea or constipation occurred in the first 2 days after FMT (table 5). Two patients (a 52-year-old male and a 55-year-old female) developed diverticulitis at 2 and 3 months after FMT. Both had diverticulosis as verified by colonoscopy and had experienced several diverticulitis attacks before FMT.
Table 5.
Adverse events following transplantation in patients with IBS.
| Adverse event | Placebo | FMT total | 30 g FMT | 60 g FMT |
| Nausea | 9 (16.3) | 17 (15.6) | 8 (14.8) | 9 (16.4) |
| Abdominal pain/cramping/tenderness | 0 (0) | 21 (19.3)* | 11 (20.4) | 10 (18.2) |
| Diarrhoea | 2 (3.6) | 26 (23.9)* | 14 (25.9) | 12 (21.8) |
| Constipation | 1 (1.8) | 24 (22.0)* | 13 (24.1) | 11 (20) |
| Diverticulitis | 0 (0) | 2 (1.8) | 2 (1.8) | 0 (0) |
Data are n (%) values.
*, p<0.001 compared with placebo.
FMT, faecal microbiota transplantation; IBS, irritable bowel syndrome.
Discussion
The findings of this study show that FMT is an effective treatment for IBS that improves both the symptoms and quality of life regardless of the IBS subtype. About half of the patients experienced significant clinical improvements in abdominal symptoms, fatigue and quality of life. These improvements were accompanied by changes in the bacterial faecal profile but not in the DI. The clinical relevance of the dysbiosis has been questioned recently.4 23 It is notable that the scores in all IBS-QoL domains except for health worries improved after the patients received FMT. This is probably because the patients attended an IBS course prior to the trial, which is reported to improve the perceived knowledge of IBS.9 The response to FMT increased with the dose. The adverse events of FMT were mild self-limiting gastrointestinal symptoms. It is noteworthy that a cohort of patients with IBS stated that they would give up an average of 15 years of their life (corresponding to 25% of their remaining lifespan) while 14% would risk a 1-in-1000 chance of death to receive a treatment that would make them free of IBS symptoms.24
At 1 month following the FMT, higher concentrations of Eubacterium biforme, Lactobacillus spp. and Alistipes spp. and a lower concentration for Bacteroides spp. were observed in this study in both the 30 g FMT and 60 g FMT groups. The concentrations for Alistipes spp. and Lactobacillus spp. were inversely correlated with the IBS-SSS score, while the signal for Alistipes spp. was inversely correlated with the FAS score. These findings indicate an association between the clinical improvement and the changes found in the bacterial profile following FMT in the present patients.
The finding that frozen faeces samples were effective in FMT confirms previous observations for FMT in Clostridioides difficile and in patients with IBS.6 25 Furthermore, administering the transplants via the upper gastrointestinal route with the aid of a gastroscope seems to work well. These observations would eliminate the logistical problems associated with both FMT involving fresh faeces and the bowel preparation needed for administering such a transplant to the colon. Moreover, it might be possible to establish faeces banks for the routine clinical use of FMT.
It is difficult to compare the findings of the present study with those of previously reported randomised placebo-controlled trials.6 7 due to differences in the sizes of the patient cohorts, the forms and amounts of the transplants, the routes of administration and the donors used. Johnsen et al investigated 83 patients with either IBS-D or IBS-M in whom 50–80 g of a mixture of the faeces from two donors was introduced into the colon.6 Halkjaer et al included 51 patients with all IBS subtypes except unclassified IBS who received 50 g of a mixture of faeces from four donors in a capsule form for 12 days (totalling 600 g).7 In the present study, the response rate in the placebo group at 2 weeks after transplantation was 49.1%, which decreased to 24.5% after 1 month and 23.6% after 3 months following transplantation. The placebo-group response in this study at 3 months after transplantation was slightly lower than that of 30% reported by Johnsen et al.6 This difference could be due to the present placebo group containing almost twice as many patients as in that previous study. Moreover, the patients in the study of Johnsen et al were subjected to bowel preparation and colonoscopy, which is often painful and takes more time than the gastroscopy applied in the present study. This aspect could have affected the expectations of the patients and increased the placebo effect. Halkjaer et al 7 used a reduction in the IBS-SSS score as the primary end point rather than a response based on a definition of such a reduction in IBS-SSS score, which makes it difficult to compare the response in their placebo group with the present observations.
The clinical efficacy of FMT is not affected by the choice of the donor in patients with Clostridioides difficile,5 26 whereas the success of FMT in inflammatory bowel disease and other disorders is donor-dependent.5 A new definition of superdonor has emerged for someone who is normobiotic and has a positive microbial signature, but an attempt to use stool pooling to produce a superdonor was not successful.5 Two randomised double-blind, placebo-controlled studies of FMT in patients with IBS produced conflicting results, which might have been due to variability in the donor stools used.6 7
What constitutes a positive microbial signature in an IBS superdonor remains unclear.5 Therefore, when choosing the superdonor in the present study, we had to consider the factors that might positively affect intestinal microbiota. Smoking/smoking cessation affects the gut microbiota negatively.27 28 To be born by caesarean section and/or be formula-fed affect the gut microbiota profile and reduce the bacterial diversity.29–32 Frequent treatment with antibiotics and/or a regular intake of non-antibiotic drugs have negative effects on the gut microbiota.33–35 Regular exercise and consuming a sport-specific diet are known to be associated with a favourable gut microbiota.36–38 Furthermore, the superdonor should not be a first-degree relative of any of the patients in a trial since the intestinal microbiota is affected by the genetic composition, and a superdonor and recipient with greater genetic similarity may also have greater similarities in their faecal microbiota.39 40 Thus, among the several candidate donors that we screened, we chose a donor who was a non-smoker, not taking any medication and had been treated only a few times with antibiotics. He was born via a vaginal delivery and breastfed, he trained regularly, consumed a sport-specific diet rich in protein and fibre, and was not related to any of the patients in the trial.
The present study utilised a single well-defined donor who was normobiotic with a bacterial signature that included an abundance of Streptococcus, Dorea, Lactobacillus and Ruminococcaceae spp. These four genera of bacteria have been reported to constitute favourable bacteria for a donor.5 41–43 Further studies involving well-defined donors are needed to identify their favourable bacterial signatures.
One strength of this clinical trial is that it involved a relatively large cohort of patients with IBS that included three of the IBS subtypes (including IBS-C) and used a single well-defined donor. Furthermore, it confirmed that frozen faeces samples obtained from a donor are effective in FMT, which facilitates their use in the clinic. However, the study also had limitations: it did not investigate the entire intestinal bacterial contents or the long-term effects of FMT, and it did not record the frequency of using rescue medication in the intervention groups. A simultaneous weakness and strength of the study was that it investigated a cohort of patients that had moderate-to-severe IBS symptoms despite adhering to a diet consistent with the modified NICE diet. This is a weakness because the outcome cannot be applied to the entire IBS population, while it is a strength since it showed that FMT succeeded when diet failed.
Acknowledgments
The authors thank Christina Casen (clinical director at the laboratory of Genetic Analysis) for fruitful discussions about intestinal microbiota.
Footnotes
Presented at: This study was previously presented as an abstract at UEG Week 2019 and at ESNM meeting 2019.
Contributors: MES designed the study, obtained the funding, administrated the study, recruited the patients, performed FMT, collected, analysed, and interpreted the data and drafted the manuscript, ABK analysed the bacterial profiles using PCA and critically revised of the manuscript for important intellectual content. OHG, JGH and TH contributed to the design of the study, to the analysis and interpretation of the data, and critically revised of the manuscript for important intellectual content.
Funding: The study was supported by grants from Helse Fonna (grant no. 40415) and Helse Vest (grant no. 192234).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The study was performed in accordance with the Declaration of Helsinki and was approved by the Regional Committee for Medical and Health Research Ethics West, Bergen, Norway (2017/1197/REK vest).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Data are stored at Helse Vest server and anonymous data are available upon reasonable request.
References
- 1. El-Salhy M, Mazzawi T. Fecal microbiota transplantation for managing irritable bowel syndrome. Expert Rev Gastroenterol Hepatol 2018;12:439–45. 10.1080/17474124.2018.1447380 [DOI] [PubMed] [Google Scholar]
- 2. El-Salhy M. Irritable bowel syndrome: diagnosis and pathogenesis. World J Gastroenterol 2012;18:5151–63. 10.3748/wjg.v18.i37.5151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Casén C, Vebø HC, Sekelja M, et al. . Deviations in human gut microbiota: a novel diagnostic test for determining dysbiosis in patients with IBS or IBD. Aliment Pharmacol Ther 2015;42:71–83. 10.1111/apt.13236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Enck P, Mazurak N. Dysbiosis in functional bowel disorders. Ann Nutr Metab 2018;72:296–306. 10.1159/000488773 [DOI] [PubMed] [Google Scholar]
- 5. Wilson BC, Vatanen T, Cutfield WS, et al. . The Super-Donor phenomenon in fecal microbiota transplantation. Front Cell Infect Microbiol 2019;9:2 10.3389/fcimb.2019.00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Johnsen PH, Hilpüsch F, Cavanagh JP, et al. . Faecal microbiota transplantation versus placebo for moderate-to-severe irritable bowel syndrome: a double-blind, randomised, placebo-controlled, parallel-group, single-centre trial. Lancet Gastroenterol Hepatol 2018;3:17–24. 10.1016/S2468-1253(17)30338-2 [DOI] [PubMed] [Google Scholar]
- 7. Halkjær SI, Christensen AH, Lo BZS, et al. . Faecal microbiota transplantation alters gut microbiota in patients with irritable bowel syndrome: results from a randomised, double-blind placebo-controlled study. Gut 2018;67:2107–15. 10.1136/gutjnl-2018-316434 [DOI] [PubMed] [Google Scholar]
- 8. Eswaran SL, Chey WD, Han-Markey T, et al. . A randomized controlled trial comparing the low FODMAP diet vs. modified NICE guidelines in US adults with IBS-D. Am J Gastroenterol 2016;111:1824–32. 10.1038/ajg.2016.434 [DOI] [PubMed] [Google Scholar]
- 9. Ringström G, Störsrud S, Lundqvist S, et al. . Development of an educational intervention for patients with irritable bowel syndrome (IBS) – a pilot study. BMC Gastroenterol 2009;9:10 10.1186/1471-230X-9-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cammarota G, Ianiro G, Tilg H, et al. . European consensus conference on faecal microbiota transplantation in clinical practice. Gut 2017;66:569–80. 10.1136/gutjnl-2016-313017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ostgaard H, Hausken T, Gundersen D, et al. . Diet and effects of diet management on quality of life and symptoms in patients with irritable bowel syndrome. Mol Med Rep 2012;5:1382–90. 10.3892/mmr.2012.843 [DOI] [PubMed] [Google Scholar]
- 12. Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395–402. 10.1046/j.1365-2036.1997.142318000.x [DOI] [PubMed] [Google Scholar]
- 13. Roalfe AK, Roberts LM, Wilson S. Evaluation of the Birmingham IBS symptom questionnaire. BMC Gastroenterol 2008;8:30 10.1186/1471-230X-8-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hendriks C, Drent M, Elfferich M, et al. . The fatigue assessment scale: quality and availability in sarcoidosis and other diseases. Curr Opin Pulm Med 2018;24:495–503. 10.1097/MCP.0000000000000496 [DOI] [PubMed] [Google Scholar]
- 15. Drossman DA, Patrick DL, Whitehead WE, et al. . Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol 2000;95:999–1007. 10.1111/j.1572-0241.2000.01941.x [DOI] [PubMed] [Google Scholar]
- 16. Wong RKM, Drossman DA. Quality of life measures in irritable bowel syndrome. Expert Rev Gastroenterol Hepatol 2010;4:277–84. 10.1586/egh.10.19 [DOI] [PubMed] [Google Scholar]
- 17. Arslan G, Lind R, Olafsson S, et al. . Quality of life in patients with subjective food hypersensitivity: applicability of the 10-item short form of the Nepean dyspepsia index. Dig Dis Sci 2004;49:680–7. 10.1023/B:DDAS.0000026318.81635.3b [DOI] [PubMed] [Google Scholar]
- 18. Drent M, Lower EE, De Vries J. Sarcoidosis-associated fatigue. Eur Respir J 2012;40:255–63. 10.1183/09031936.00002512 [DOI] [PubMed] [Google Scholar]
- 19. Agency EM. Guideline on the evaluation of medicinal products for the treatment of irritable bowel syndrome, 2014. Available: https://wwwemaeuropaeu/en/documents/scientific-guideline/guideline-evaluation-medicinal-products-treatment-irritable-bowel-syndrome-revision-1_enpdf
- 20. U.S. Department of Health and Human Services Food and Drug Aministration Center for Drug Evaluation and Research (CDER) Guidance for industry:irritable bowel syndrome-clinical evalution of drugs for treatment, 2012. Available: http://wwwfdagov/downloads/Drugs/Guidances/UCM205269pdf
- 21. Ritchie ME, Phipson B, Wu D, et al. . limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res 2015;43:e47 10.1093/nar/gkv007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bennet SMP, Böhn L, Störsrud S, et al. . Multivariate modelling of faecal bacterial profiles of patients with IBS predicts responsiveness to a diet low in FODMAPs. Gut 2018;67:872–81. 10.1136/gutjnl-2016-313128 [DOI] [PubMed] [Google Scholar]
- 23. Lloyd-Price J, Mahurkar A, Rahnavard G, et al. . Erratum: strains, functions and dynamics in the expanded human microbiome project. Nature 2017;551:256 10.1038/nature24485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Drossman DA, Morris CB, Schneck S, et al. . International survey of patients with IBS: symptom features and their severity, health status, treatments, and risk taking to achieve clinical benefit. J Clin Gastroenterol 2009;43:541–50. 10.1097/MCG.0b013e318189a7f9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee CH, Steiner T, Petrof EO, et al. . Frozen vs Fresh Fecal Microbiota Transplantation and Clinical Resolution of Diarrhea in Patients With Recurrent Clostridium difficile Infection. JAMA 2016;315:142–9. 10.1001/jama.2015.18098 [DOI] [PubMed] [Google Scholar]
- 26. Kassam Z, Lee CH, Yuan Y, et al. . Fecal microbiota transplantation for Clostridium difficile infection: systematic review and meta-analysis. Am J Gastroenterol 2013;108:500–8. 10.1038/ajg.2013.59 [DOI] [PubMed] [Google Scholar]
- 27. Capurso G, Lahner E. The interaction between smoking, alcohol and the gut microbiome. Best Pract Res Clin Gastroenterol 2017;31:579–88. 10.1016/j.bpg.2017.10.006 [DOI] [PubMed] [Google Scholar]
- 28. Biedermann L, Brülisauer K, Zeitz J, et al. . Smoking cessation alters intestinal microbiota: insights from quantitative investigations on human fecal samples using fish. Inflamm Bowel Dis 2014;20:1496–501. 10.1097/MIB.0000000000000129 [DOI] [PubMed] [Google Scholar]
- 29. Korpela K, Dikareva E, Hanski E, et al. . Cohort profile: Finnish health and early life microbiota (HELMi) longitudinal birth cohort. BMJ Open 2019;9:e028500 10.1136/bmjopen-2018-028500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yeung OY, Ng YF, Chiou J, et al. . A pilot study to determine the gut microbiota of Hong Kong infants fed with breast-milk and/or infant formula (P11-101-19). Curr Dev Nutr 2019;3 10.1093/cdn/nzz048.P11-101-19 [DOI] [Google Scholar]
- 31. Jakobsson HE, Abrahamsson TR, Jenmalm MC, et al. . Decreased gut microbiota diversity, delayed Bacteroidetes colonisation and reduced Th1 responses in infants delivered by caesarean section. Gut 2014;63:559–66. 10.1136/gutjnl-2012-303249 [DOI] [PubMed] [Google Scholar]
- 32. Rutayisire E, Huang K, Liu Y, et al. . The mode of delivery affects the diversity and colonization pattern of the gut microbiota during the first year of infants' life: a systematic review. BMC Gastroenterol 2016;16:86 10.1186/s12876-016-0498-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ianiro G, Tilg H, Gasbarrini A. Antibiotics as deep modulators of gut microbiota: between good and evil. Gut 2016;65:1906–15. 10.1136/gutjnl-2016-312297 [DOI] [PubMed] [Google Scholar]
- 34. Modi SR, Collins JJ, Relman DA. Antibiotics and the gut microbiota. J Clin Invest 2014;124:4212–8. 10.1172/JCI72333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Maier L, Pruteanu M, Kuhn M, et al. . Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 2018;555:623–8. 10.1038/nature25979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Murtaza N, Burke L, Vlahovich N, et al. . The effects of dietary pattern during intensified training on stool microbiota of elite race walkers. Nutrients 2019;11:261 10.3390/nu11020261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dalton A, Mermier C, Zuhl M. Exercise influence on the microbiome–gut–brain axis. Gut Microbes 2019;10:555–68. 10.1080/19490976.2018.1562268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Motiani KK, Collado MC, Eskelinen J-J, et al. . Exercise training modulates gut microbiota profile and improves endotoxemia. Med Sci Sports Exerc 2019. doi: 10.1249/MSS.0000000000002112. [Epub ahead of print: 16 Aug 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pinn DM, Aroniadis OC, Brandt LJ. Is fecal microbiota transplantation (FMT) an effective treatment for patients with functional gastrointestinal disorders (FGID)? Neurogastroenterol Motil 2015;27:19–29. 10.1111/nmo.12479 [DOI] [PubMed] [Google Scholar]
- 40. Pinn DM, Aroniadis OC, Brandt LJ. Is fecal microbiota transplantation the answer for irritable bowel syndrome? A single-center experience. Am J Gastroenterol 2014;109:1831–2. 10.1038/ajg.2014.295 [DOI] [PubMed] [Google Scholar]
- 41. Bull MJ, Plummer NT. Part 2: treatments for chronic gastrointestinal disease and gut dysbiosis. Integr Med 2015;14:25–33. [PMC free article] [PubMed] [Google Scholar]
- 42. Holvoet T, Joossens M, Wang J, et al. . Assessment of faecal microbial transfer in irritable bowel syndrome with severe bloating. Gut 2017;66:980–2. 10.1136/gutjnl-2016-312513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chong C, Bloomfield F, O’Sullivan J. Factors affecting gastrointestinal microbiome development in neonates. Nutrients 2018;10:274 10.3390/nu10030274 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gutjnl-2019-319630supp001.pdf (50.2KB, pdf)
gutjnl-2019-319630supp002.pdf (33.9KB, pdf)
gutjnl-2019-319630supp003.pdf (41KB, pdf)
gutjnl-2019-319630supp004.pdf (50.5KB, pdf)
gutjnl-2019-319630supp005.pdf (35.3KB, pdf)
gutjnl-2019-319630supp006.pdf (91.5KB, pdf)
gutjnl-2019-319630supp007.pdf (23.2KB, pdf)
gutjnl-2019-319630supp008.pdf (367.9KB, pdf)
gutjnl-2019-319630supp009.pdf (479.2KB, pdf)
gutjnl-2019-319630supp010.pdf (500.5KB, pdf)
gutjnl-2019-319630supp011.pdf (79.4KB, pdf)